Abstract
Objectives
This study examined the relationship between temporomandibular joint (TMJ) dysfunctions and obscurity grades of interpreted anterior and posterior borders of the articular disc (Da and Dp, respectively) by 3.0 T pseudodynamic MRI.
Methods
Da and Dp were classified into seven obscurity grades, and the Dp contour was classified into three types. The grades, types and TMJ function were compared by 3.0 T pseudodynamic MRI.
Results
Unobscured Da images at condylar positions posterior to the articular eminence were associated with normal TMJ function (P = 0.046 < 0.05). Unobscured Dp images at condylar positions anterior to the articular eminence were associated with normal TMJ function (P = 0.033 < 0.05). In addition, unobscured Dp images following flap insertion were associated with normal TMJ function (P = 0.043 < 0.05). There was no statistical relationship between Dp contour types and TMJ movement, but any change observed in the Dp contour during mouth opening was associated with abnormal TMJ function (P = 0.040 < 0.05).
Conclusions
Grading of Da and Dp obscurity based on how well the areas were defined in the images, identifying the condylar positions in relation to the glenoid fossa and articular eminences, and observing the changes in Dp contour types were useful for diagnosing TMJ abnormalities.
Keywords: temporomandibular joint, magnetic resonance imaging, temporomandibular joint articular disc, articular ligament
Introduction
Previously, we have reported that 3.0 T pseudodynamic MRI of the temporomandibular joint (TMJ) can help assess condylar head and articular disc movement as well as determine normal and abnormal TMJ function. A point system by trajectory and velocity patterns based on 3.0 T pseudodynamic MRI identified the affected side and determined the extent of morbidity in the anterior and posterior articular disc and condylar head. The Kruskal–Wallis test indicated that discs with adhesion and perforation had significantly fewer points than discs with anterior displacement (with and without reduction) and discs with no abnormality (P = 0.019 < 0.05). The typical abnormal movement pattern of discs with anterior disc displacement (with and without reduction) and pathological structural changes in the articular disc (such as adhesion and perforation) could be identified.1
Many studies have investigated anatomy2–4 and MRI of posterior attachment (PA) morphology5–8 because PA may affect jaw movement and cause clinical symptoms, especially pain, in TMJ disorders. Of the three PA components (temporal, condylar and intermediate), the appearance rate of the temporal posterior attachment (TPA) and condylar posterior attachment (CPA) parts in the mouth closed, mouth slightly opened or mouth fully opened position is different.9,10 Obscurity due to disc perforation has been reported as a characteristic MR finding in one study.11 There is some controversy concerning the normal range of the angle (−10° to +10° or up to +30°) between the vertical orientation of the condyle centre (12 o'clock position) and the posterior band (PB)–PA junction in the mouth closed position.10,12,13 Many authors have reported a change in signal intensity and increased vascularity of PA,14,15 but PB morphology and morphological changes in the articular disc during mouth opening were not evaluated. The relationship between obscurity and movement of the articular disc and diagnostic importance of obscurity are unclear.
This study aimed to clarify the relationship between TMJ dysfunction and obscurity grades of the interpreted anterior and posterior borders of the articular disc (Da and Dp, respectively) by 3.0 T pseudodynamic MRI.
Materials and methods
The materials and methods for pseudodynamic imaging were the same as described in detail in the primary report.1 Pseudodynamic images of nine volunteers (six males and three females; 24–35 years old median, 26.5 years; eight with and one without TMJ arthrosis) were used for interpretation of Da and Dp contours. Informed consent and ethical approval was obtained.
Condylar positions
Figure 1 shows the condylar positions defined according to the relationship of the condylar head (Cd) point (highest protrusion of the Cd, where the perpendicular line from the posterior mandibular ramus meets the Cd) to the lowest point of articular eminence and highest point of glenoid fossa. Condylar positions were examined in relation to flap insertion steps.
Figure 1.

Condylar positions. Cd, condylar head; Em, lowest articular eminence; TMJ, temporomandibular joint; position 0, posterior to fossa; position 1, between fossa and 1/2 of posterior slope of Em; position 2, between 1/2 of posterior slope of Em and Em; position 3, between Em and 1/3 of anterior slope of Em; position 4, anterior to 1/3 of anterior slope of Em
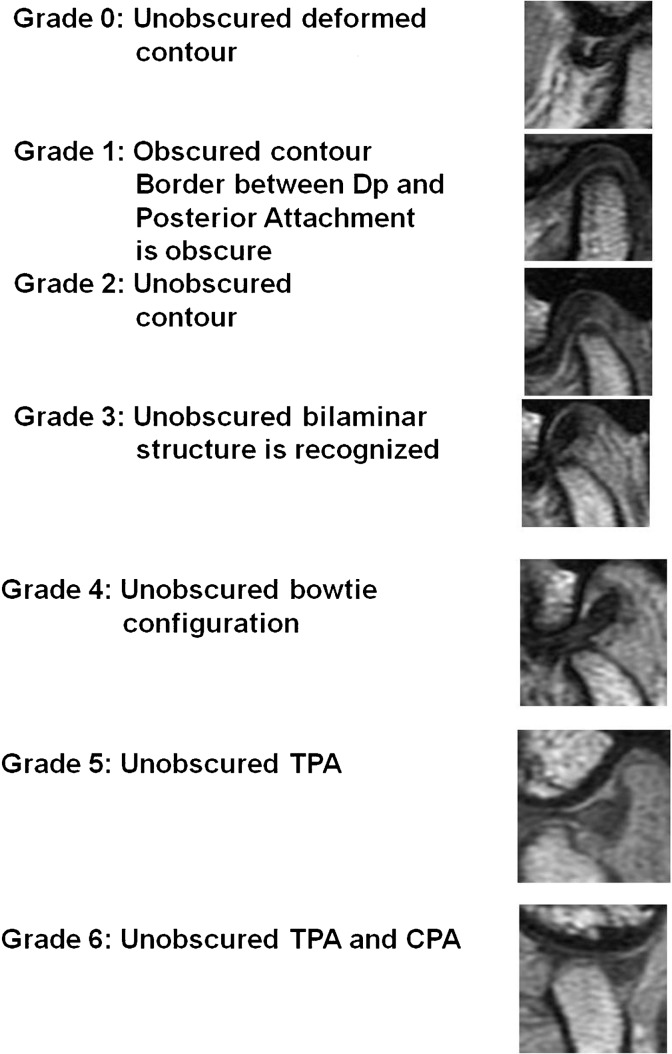
Articular disc contour grades and TMJ movement
Da (where the posterior border of the anterior attachment showing low signal intensity is separated from the surrounding area in the anterior band of the articular disc) and Dp (where a bow tie configuration is derived from TPA and CPA) were interpreted and classified into seven grades (Figures 2 and 3). Statistical assessment was performed using SPSS II for Windows (Version 11.0.1J; SPSS Inc., Chicago, IL). The Mann–Whitney U-test was used to compare average Da and Dp grades at condylar positions 0–2 (posterior to the articular eminence) and at 3 and 4 (anterior to the articular eminence). P-values of < 0.05 were considered significant.
Figure 2.
Anterior border (Da) contour grades
Figure 3.
Posterior border (Dp) contour grades
Appearance rate of grade 3 and grades 4–6
The appearance rate of grade 3 was evaluated in the mouth slightly opened position (condylar position 1 or 2), and those of grades 4–6 were evaluated in the mouth opened position (condylar position 3 or 4) following flap insertion in each TMJ. This rate was calculated in eight normal-movement TMJs and nine abnormal-movement TMJs. One TMJ that showed severe “folding” was excluded. The Pearson χ2 test was used to analyse the appearance rate of grade 3 and grades 4–6. P-values of < 0.05 were considered significant.
Dp contour types and TMJ movement
Dp contour types are shown in Figure 4. The contour types observed the most, following flap insertion, were determined as the TMJ contour types. After excluding the TMJ that showed severe “folding”, the remaining Dp contour types were analysed by the Pearson χ2 test. P-values of < 0.05 were considered significant.
Figure 4.
Posterior border (Dp) contour types. (a) Concave (C-type); (b) Flat (F-type); (c) Convex (V-type)
Change in Dp contours following flap insertion
The Pearson χ2 test was used to analyse changes in Dp contours during normal and abnormal TMJ movement. P-values of < 0.05 were considered significant.
Results
Condylar position
Figure 5 shows the relationship between condylar positions (0–4) and flap insertion steps (0–5) of 18 TMJs in 9 volunteers. When only one flap was inserted, the condylar position count increased in a few of the TMJs, possibly because of overbite and overjet (vertical and horizontal distance between upper and lower anterior incisal teeth in the mouth closed position). When two or more flaps were inserted, the condylar position count decreased with limited mouth opening. Condylar positions varied between TMJs with limited mouth opening and those without.
Figure 5.

The relationship between condylar (Cd) positions (0–4) and flap steps (0–5) of nine volunteers
Articular disc contour grades and TMJ movement
Table 1 shows the results of the Mann–Whitney U-test performed to evaluate the relationship between TMJ movement (normal and abnormal) and average Da and Dp grades at condylar positions 0–2, 3 and 4. Da could be detected (high grade) during normal TMJ movement when the condyle was situated posterior to the articular eminence (condylar positions 0–2) (P = 0.046 < 0.05). Dp could be detected (high grade) during normal TMJ movement when the condyle was situated anterior to the articular eminence (condylar positions 3 and 4) (P = 0.033 < 0.05).
Table 1. Results of the Mann–Whitney U-test for relationship between the average anterior border (Da) and posterior border (Dp) grades at condylar positions 0–2 and positions 3 and 4 during temporomandibular joint movement (normal and abnormal) by pseudodynamic analysis.
| Average of obscurity grading | TMJ movement by pseudodynamic analysis | Numbers of TMJs | Mann–Whitney U-test | Wilcoxon (W) | Z | Significance probability (two-tailed) |
| Da | Normal | 6 | 15 | 93 | −1.99 | 0.046* |
| Condylar position 0–2 | Abnormal | 12 | ||||
| Da | Normal | 6 | 28 | 106 | −0.79 | 0.433 |
| Condylar position 3–4 | Abnormal | 12 | ||||
| Dp | Normal | 8 | 32 | 87 | −0.71 | 0.475 |
| Condylar position 0–2 | Abnormal | 10 | ||||
| Dp | Normal | 8 | 21 | 76 | −2.14 | 0.033* |
| Condylar position 3–4 | Abnormal | 10 |
*P < 0.05; TMJ, temporomandibular joint
Appearance rate of grade 3 and grades 4–6
Table 2 shows the results of the Pearson χ2 test performed to evaluate the relationship between TMJ movement (normal and abnormal) and the appearance rate of Dp grade 3 and grades 4–6.
Table 2. Results of the Pearson x2 test performed to evaluate the relationship between condylar posterior border (Dp) grades (36) and temporomandibular joint (TMJ) movement (normal and abnormal) by pseudodynamic analysis.
| TMJ movement by pseudodynamic analysis |
|||
| Normal | Abnormal | ||
| Grade 3 (visible) | 5 (62.5%) | 4 (44.4%) | 9 |
| Grade 3 (not visible) | 3 (37.5%) | 5 (55.6%) | 8 |
| 8 (100%) | 9 (100%) | 17 | |
| Pearson χ2 test: | |||
| significance probability (two-tailed) P = 0.457 > 0.05 | |||
| TMJ movement by pseudodynamic analysis |
|||
| Normal | Abnormal | ||
| Grade 4 (visible) | 0 (0%) | 1 (11.1%) | 1 |
| Grade 5 (visible) | 4 (50.0%) | 8 (88.9%) | 12 |
| Grade 6 (visible) | 4 (50.0%) | 0 (0%) | 4 |
| 8 (100%) | 9 (100%) | 17 | |
| Pearson χ2 test: | (TMJs) | ||
| significance probability (two-tailed) P = 0.043 < 0.05 | |||
Grade 3 (unobscured bilaminar structure) was observed in 62.5% (5/8) of normal TMJs and 44.4% (4/9) of abnormal TMJs in the mouth slightly opened position (flaps 1 or 2). Dp at grade 3 was high during normal movement, but not significantly so (P = 0.457).
Grade 4 (unobscured bow tie configuration without TPA and CPA) was not observed in normal TMJs (0/8), but was observed in 11.1% (1/9) of abnormal TMJs. Grade 5 (unobscured TPA) was observed in 50% (4/8) of normal TMJs and 88.9% (8/9) of abnormal TMJs. Grade 6 (unobscured TPA and IPA) was observed in 50% (4/8) of normal TMJs but was not observed in abnormal TMJs (0/9). Grades 4–6 following flap insertion were observed in 100% (4 Grade 5 and 4 Grade 6 of 8; and 1 Grade 4 and 8 Grade 5 of 9) of normal and abnormal movement TMJs. Higher Dp grades (Grades 4–6) were observed in normal TMJs (P = 0.043 < 0.05).
Dp contour types and TMJ movement
Table 3 shows the results of the Pearson χ2 test performed to evaluate the relationship between Dp (C-, F- and V-types) and TMJ movement (normal and abnormal). V-type contour was observed in 10 TMJs, constituting approximately 60% (10/17 = 58.8%) of all Dp contours, whereas F- and C-type contours were observed in only five and two TMJs, respectively. There was no statistical relationship between Dp contour type and TMJ movement (normal and abnormal) (P = 0.762).
Table 3. Results of the Pearson χ2 test performed to evaluate the relationship between posterior border (Dp) contour types (C-, F- and V-types) and temporomandibular joint (TMJ) movements (normal and abnormal) by pseudodynamic analysis.
| TMJ movement by pseudodynamic analysis |
TMJs | |||
| Normal | Abnormal | |||
| Contour types | C-type | 1 | 1 | 2 |
| F-type | 3 | 2 | 5 | |
| V-type | 4 | 6 | 10 | |
| Total | 8 | 9 | 17 | |
Pearson χ2 test: significance probability (two-tailed) P = 0.762 > 0.05
C-type, concave; F-type, flat; V-type, convex
Change in Dp morphology following flap insertion
Table 4 shows the changes in Dp contours during mouth opening. Among the eight TMJs that did not show a functional abnormality, seven showed no change in Dp contour according to the condylar position during opening, whereas, among the nine TMJs with a functional abnormality, six showed changes in Dp contour according to the condylar position during mouth opening. Table 5 shows the result of the Pearson χ2 test performed to evaluate changes in Dp contour following flap insertion. TMJs showed significant changes in Dp contour according to the condylar position during mouth opening (P = 0.040 < 0.05).
Table 4. Relationship between changes in posterior border (Dp) contour types during mouth opening and temporomandibular joint (TMJ) movements (normal and abnormal) by pseudodynamic analysis.
| TMJ movement by pseudodynamic analysis |
||
| Normal | Abnormal | |
| Change in Dp contour types | 1 | 6 |
| From V or C to F | 1 | 3 |
| From V to F | (2) | |
| From C to F | (1) | (1) |
| Between C and V | 3 | |
| From C to V | (2) | |
| From V to C | (1) | |
| No change in Dp contour types | 7 | 4 |
| V | 6 | 3 |
| F | 1 | |
| Folding | 1 | |
| Total | 8 | 10 |
C-type, concave; F-type, flat; V-type, convex
Table 5. Results of the Pearson χ2 test performed to evaluate the relationship between changes in posterior border (Dp) contour types during mouth opening and temporomandibular joint (TMJ) movements (normal and abnormal) by pseudodynamic analysis.
| TMJ movement by pseudodynamic analysis |
TMJs | ||
| Normal | Abnormal | ||
| Changes in Dp contour types | 1 | 6 | 7 |
| No change in Dp contour types | 7 | 4 | 11 |
| Total | 8 | 10 | 18 |
Pearson χ2 test: significance probability (two-tailed) P = 0.040 < 0.05
Discussion
Grading of Da and Dp
Da and Dp grades are generally related to condylar positions rather than flap insertion steps owing to the latter affecting the distance between upper and lower anterior incisal teeth. Da and Dp grades were compared at similar condylar positions to analyse obscurity.
Da grading
Unobscured images of the anterior border of the articular disc at condylar positions posterior to the articular eminence were associated with normal TMJ function. The anterior border of the articular disc at condylar positions posterior to the articular eminence was easily identified following flap insertion. The average Da grade increased depending on how easy it was to compare early and late images during flap insertion without suppressing the surrounding structures such as the anterior articular attachment, condylar head and temporal muscle.
Dp grading — Condylar positions 0–2
No significant difference was found between normal and abnormal movement at condylar positions 0–2. This was because almost all TMJs were Grade 0 at condylar position 0. The PB–PA junction in the mouth closed position is obscured on 3.0 T MRI.1 It seems doubtful that the normal angular range between the vertical orientation of the condyle centre (12 o'clock position) and the PB–PA junction can be identified in the mouth closed position. Compared with previous results of 73.6%10 and 73%11 in normal TMJs, and 43.5%10 and 32%11 in abnormal TMJs as evaluated by 1.5 T static MRI, our results of the Grade 3 appearance rate (unobscured bilaminar structure) (62.5% in normal TMJs and 44.4% in abnormal TMJs) were almost the same, but slightly lower in normal TMJs.
Condylar positions 3 and 4
Unobscured Dp images at condylar positions anterior to the articular eminence were associated with normal TMJ function.
Compared with results obtained with 1.5 T static MRI (Grade 5 (normal 32.5%) and Grade 6 (normal 67.5%),8 Grade 5 (normal 44.7%, abnormal 30.4%),10 Grade 5 (normal 86%, abnormal 35%), and Grade 4 (normal 14%, abnormal 65%)),11 more structural abnormality was observed in abnormal TMJs as observed in our results obtained with 3.0 T pseudodynamic MRI in the mouth opened positions (Grade 6, normal 50% and abnormal 0%; Grade 5, normal 50% and abnormal 88.9%; Grade 4, normal 0% and abnormal 11.1%). Obscured Dp images following flap insertion were associated with abnormal TMJ function.
These differences are believed to be due to differences in the equipment and imaging sequences. Moreover, because we had only one volunteer with a normal TMJ and the comparison was made between abnormal TMJs, with and without joint movement abnormality, it was possible that there was a disc disorder without significant movement abnormalities.
The onset of morphological abnormality is related to a decrease in CPA tension due to thickening of the PB under the disc surface,10 which may cause CPA to become thinner. Signal averaging owing to adjacent structures7 in MRI may be another reason. CPA cannot be clearly delineated on 1.5 T MRI because of spatial resolution;10 however, sufficient information concerning obscurity grades on the posterior border of the disc was obtained by 3.0 T pseudodynamic MRI following flap insertion.
Explanations for poor visualization of PA include reactive inflammatory changes,4 perforation or disruption,11 disc displacement and deformity.11 Degenerative changes including thinning and an increase in the intradiscal signal made it difficult to observe the disc; however, this was also experienced in TMJs where the disc was displaced during lateral or rotational movement.16
When evaluating articular disc movement and morphological changes, we observed that disc morphology in the mouth closed position (with or without pathological changes) was affected by movement, resulting in suppression and a change in the shape of the articular disc. This knowledge of the change in shape advances the understanding of articular disc pathology. Hence, elasticity of the articular disc may decrease before an apparent pathological change of the disc occurs. These alterations in the architecture of internal tissues, which were otherwise histologically normal, have been referred to as “remodelling effects”.3 Several types of pathological changes, such as disc perforation and disc adhesion (between the disc–PA tissue and the bone surface of temporal component), have been determined by pseudodynamic analysis.1
Dp contour type
Dp contour type and articular disc movement
The general mechanics of PA (TPA and CPA) can be explained as follows:2–4,7,12,13 PA is narrow in the mouth closed position, and the MR image of PA that is apparent in the mouth slightly and fully opened position is not shown. The appearance of PA during mouth opening is likely to be due to the piston-like action exerted by the condyle on PA as it vacates the glenoid fossa. PA does not behave like an elastic ligament and is not structurally designed to develop high elastic tensile stress when stretched. The disc is attached posteriorly, and hence TPA and CPA do not exert much distraction force on the disc either. Thus, TPA prevents complete displacement of the articular disc. Articular disc movement is thought to be normal when the posterior contour of the articular disc is convex.3 The posterior contour of the articular disc may change from convex to flat to concave when abnormal movement occurs. It is hypothesized that when this contour becomes concave, it is stretched towards the posterior superior and posterior inferior directions attached by TPA and CPA. Therefore, we evaluated the correlation between Dp contour type and TMJ movement.
Of all Dp contour types, V-type contour constituted about 60%, despite it not being the basic Dp contour type; however, C-type contour was rarely observed. Because there was no relationship between Dp contour type and TMJ movement, the basic type did not change during mouth opening.
Change in Dp morphology during mouth opening
We evaluated the relationship between morphological change in Dp and TMJ movements during flap insertion. The results showed no change in 7 of 8 TMJs of the functionally normal group; however, in 6 of 10 TMJs of the functionally abnormal group the disc type changed during TMJ movement. Normally, changes may occur in the area of the condyle during mouth opening; however, if the Dp contour is V- or F-type, it will not change in morphology. The articular disc showing F-type contour during final stages of mouth opening was considered a normal phenomenon in response to slight pulling of the articular disc by TPA. However, when the disc morphology changed from type V or C to F, V to C, or vice versa, the elasticity of the articular disc was lost and remodelling effects were expected to occur.
In conclusion, unobscured Da images at condylar positions posterior to the articular eminence were associated with normal TMJ function (P = 0.046 < 0.05). Unobscured Dp images at condylar positions anterior to the articular eminence were also associated with normal TMJ function (P = 0.033 < 0.05). Unobscured Dp images following flap insertion were associated with normal TMJ function (P = 0.043 < 0.05). Changes in Dp contour types during mouth opening were significant (P = 0.040 < 0.05). Pathological changes of the disc were revealed, to a certain extent, when the amount to which Da and Dp were obscured was categorized into seven grades. The decrease in articular disc elasticity that occurs before apparent pathological changes of the disc may indicate remodelling effects. Several pathological changes such as disc adhesion and disc perforation may also be the cause. The grade relating to the amount to which Da and Dp were obscured, condylar positions and Dp contour changes were useful for diagnosing abnormalities.
Acknowledgments
We would like to thank all the volunteers who participated in our study.
Research number of the ethical committee of Medical and Dental Hospital of the University of Tokushima: 432.
This study was supported in part by a Grant-in-Aid for Science Research of the Ministry of Education, Culture, Sports, Science, and Technology (Scientific Research (C), 2008–2010, Research Number 20592203).
References
- 1.Iwasaki H, Kubo H, Harada M, Nishitani H. Temporomandibular joint and 3.0T pseudodynamic magnetic resonance imaging. Part 1 evaluation of condylar and disc dysfunction. Dentomaxillofac Radiol 2010;39475–485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rees LA. The structure and function of the mandibular joint. Br Dent J 1954;96:125–133 [Google Scholar]
- 3.Scapino RP. Histopathology of the disc and posterior attachment in disc displacement internal derangement of the TMJ, In:Magnetic resonance of the temporomandibular joint New York:Thieme,1990:63–73 [Google Scholar]
- 4.Scapino RP. The posterior attachment: its structure, function, and appearance in TMJ imaging studies. Part 1. Craniomandib Disord Fac Oral Pain 1991;5:83–95 [PubMed] [Google Scholar]
- 5.Drace JE, Enzmann DR. Defining the normal temporomandibular joint: closed-, partially open-, and open-mouth MR imaging of asymptomatic subjects. Radiology 1990;177:67–71 [DOI] [PubMed] [Google Scholar]
- 6.Drace JE, Young SW, Enzmann DR. TMJ meniscus and bilaminar zone: MR imaging of the substructure diagnostic landmarks and pitfalls of interpretation. Radiology 1990;177:73–76 [DOI] [PubMed] [Google Scholar]
- 7.Scapino RP. The posterior attachment: its structure, function, and appearance in TMJ imaging studies Part 2. Craniomandib Disord Fac Oral Pain 1991;5:155–166 [PubMed] [Google Scholar]
- 8.Haiter-Neto F, Hollender L, Barclay P, Maravilla KR. Disc position and the bilaminar zone of the temporomandibular joint in asymptomatic young individuals by magnetic resonance imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:372–378 [DOI] [PubMed] [Google Scholar]
- 9.Hollender L, Barclay P, Maravilla K, Terry Y. The depiction of the bilaminar zone of the temporomandibular joint by magnetic resonance imaging. Dentomaxillofac Radiol 1998;27:45–47 [DOI] [PubMed] [Google Scholar]
- 10.Katzberg RW, Tallents RH. Normal and abnormal temporomandibular joint disc and posterior attachment as depicted by magnetic resonance imaging in symptomatic and asymptomatic subjects. J Oral Maxillofac Surg 2005;63:1155–1161 [DOI] [PubMed] [Google Scholar]
- 11.Kuribayashi A, Okochi K, Kobayashi K, Kurabayashi T. MRI findings of temporomandibular joints with disk perforation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;106:419–425 [DOI] [PubMed] [Google Scholar]
- 12.Sommer OJ, Aiger F, Rudisch A, Gruber H, Fritsch H, Millesi W, et al. Cross-sectional and functional imaging of the temporomandibular joint: radiology, pathology, and basic biomechanics of the jaw. Radiographics 2003;23:e14 [Epub]. [DOI] [PubMed] [Google Scholar]
- 13.Tomas X, Pomes J, Berenguer J, Quinto L, Nicolau C, Mercader JM, et al. MR imaging of temporomandibular joint dysfunction: a pictorial review. Radiographics 2006;26:765–781 [DOI] [PubMed] [Google Scholar]
- 14.Sano T, Westesson PL. Magnetic resonance imaging of the temporomandibular joint. Increased T2 signal in the retrodiskal tissue of painful joints. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;79:511–516 [DOI] [PubMed] [Google Scholar]
- 15.Suenaga S, Hamamoto S, Kawano K, Higashida Y, Noikura T. Dynamic MR imaging of the temporomandibular joint in patients with arthrosis: relation between contrast enhancement of the posterior disc attachment and joint pain. Am J Roentogenol 1996;166:1475–1481 [DOI] [PubMed] [Google Scholar]
- 16.Katzberg RW, Westesson PL, Tallents RH, Anderson R, Kurita K, Manzione JV, Jr, et al. Temporomandibular joint: MR assessment of rotational and sideways disk displacements. Radiology 1988;169:741–748 [DOI] [PubMed] [Google Scholar]