Abstract
Epidermal cysts represent the most common cutaneous cysts. They arise following a localized inflammation of the hair follicle and occasionally after the implantation of the epithelium, following a trauma or surgery. Conventional epidermal cysts are about 5 cm in diameter; however, rare reports of cysts more than 5 cm are reported in the literature and are referred as “Giant epidermal cysts.” Epidermal cysts although common, can mimic other common benign lesions in the head and neck area. A thorough clinico-pathologic investigation is needed to diagnose these cutaneous lesions as they differ in their biologic behavior, treatment, and prognosis. We report a case of a giant epidermoid cyst in the scalp area of a young female patient which mimicked lipoma on clinical, as well as cyotological examination. We also present a brief review of epidermal cysts, their histopathological differential diagnosis, and their malignant transformation.
Keywords: Giant epidermal cyst, histopathology, keratinous cyst, scalp
What was known?
Epidermal cysts are the common keratinous cysts of skin.
Introduction
Epidermal cysts represent the most common cutaneous cysts. The epithelium inclusion cyst, Pilar or Trichilemmal cyst, Dermoid cyst, and Steatocystoma are the different types of keratinous cysts.[1] Epidermal/keratinous cysts are asymptomatic. In the past, these cysts were also known as sebaceous cysts. However, now the term “sebaceous cyst” has fallen into disuse.[1] One of the reasons for this comes from analysis of the lipids from epidermal cysts by thin layer chromatography.[2] This revealed characteristic patterns of lipid classes which resembled much more closely to the lipid pattern of epidermis than that of the sebaceous gland. This data provides biochemical support for the view that none of the epidermal cysts is of sebaceous origin.[2] Current terms include epidermal cyst, keratin cyst, epithelial cyst, and an epidermoid cyst.
Epidermoid cysts are dome-shaped lesions that often arise from a ruptured pilosebaceous follicle. They are asymptomatic, slowly enlarging, firm to fluctuant lesions that frequently appear on the trunk, neck, face, and scrotum or behind the ears. Occasionally, a dark keratin plug (a comedo) can be seen overlying the cyst cavity. These epithelial, walled cysts vary from a few millimeters to 5 cm in diameter. These cysts are mobile unless fibrosis is present.[1] They are most often benign and can recur after incomplete excision. In some cases, malignant degeneration occurs, resulting in the direct invasion of adjacent tissues and distant metastases.[3]
Conventional epidermal cysts are <5 cm in diameter. Giant epidermal cysts with a diameter of 5 cm or more are rare but have been reported.[4] We report a case of a giant epidermal cyst on the posterior scalp.
Case Report
A 23-year-old female patient was referred to our institution with a huge mass on the posterior scalp near the midline. The patient's parents gave the history that the mass on the posterior scalp was present since birth which gradually increased to the present size.
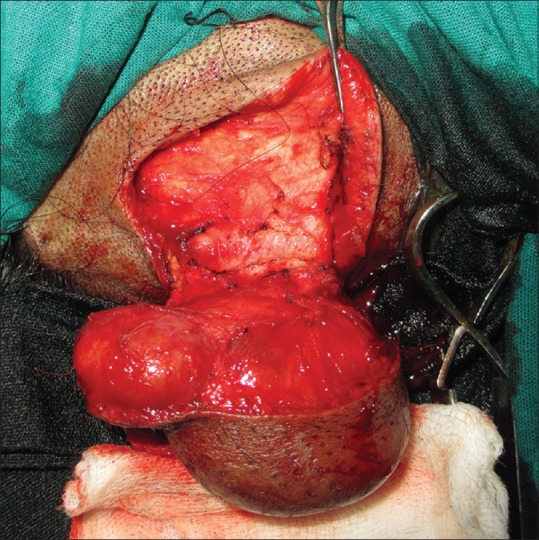
The swelling was painless and was gradually enlarging. On examination, there was a well-demarcated solitary pear-shaped sessile swelling in the occipital region near the midline measuring 7 cm × 6 cm in its greatest dimension [Figure 1]. On physical examination, no other swelling was noted elsewhere in the body.
Figure 1.

Large pear-shaped swelling on the scalp
The skin overlying the swelling was normal in color and texture but slightly stretched. The absence of hair on the surface of the swelling was noticed. There was no local rise in temperature associated with the swelling. The swelling was nontender, soft and putty in consistency, and mobile over the underlying structures. The surface of the swelling was lobular with smooth bumps. The swelling was fluctuant, compressible, and nonpulsatile. On radiographic examination, a soft tissue shadow of the cyst was seen at the occipital region without any bony erosion.
On the basis of the clinical examination, a provisional clinical diagnosis of lipoma was made.
Fine-needle aspiration cytologic (FNAC) was carried out to evaluate the nature of the contents of the cyst. Contents of the lesion were aspirated using a wide bore needle and was sent for microscopic examination. The section revealed the presence of numerous cells with empty cytoplasm and peripherally placed nucleus resembling adipocytes. Few keratin strands were also seen in the section. The FNAC diagnosis was given as lipoma.
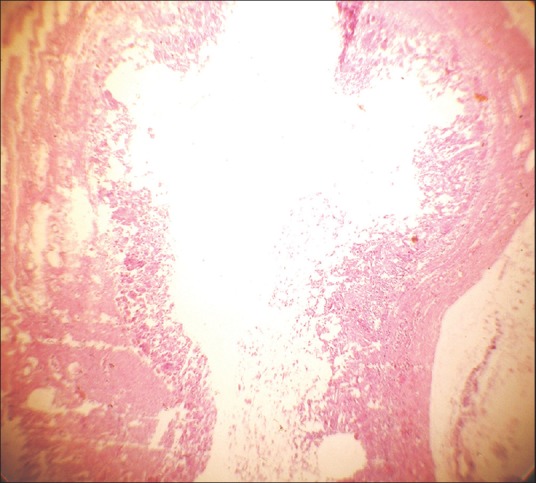
Surgical excision of the cyst was then planned under general anesthesia. The specimen was sent for histopathological examination [Figure 2].
Figure 2.
Lesion excised in toto
Findings
Soft tissue was received in 10% formalin. The tissue was soft, putty, and fluctuant inconsistency. On cutting the mass, muddy paste got extravasated [Figure 3], which resembled soggy keratin. The histological section revealed cyst wall and a cystic lumen with overlying epidermis [Figure 4]. The cyst wall showed signs of rupture and disintegration. The overlying cystic epithelium is disintegrated due to inflammation and was not evident in the section.
Figure 3.

Extravasated muddy paste on grossing
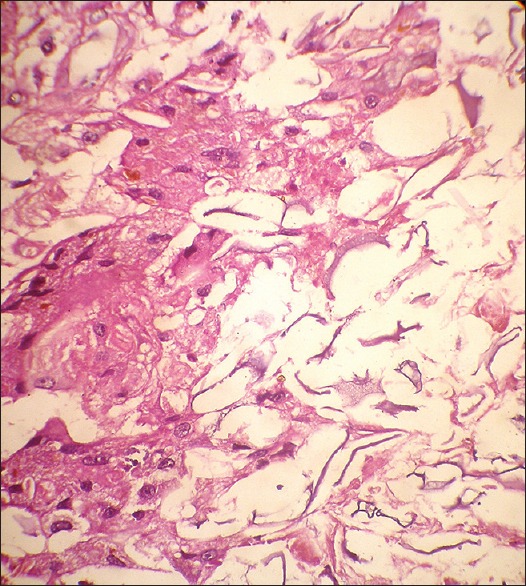
Figure 4.
Scanner view showing cyst lumen
Keratin flecks were seen with squamoid cells [Figure 5]. Spillage of keratin in the surrounding connective tissue provoked giant cell reaction, and many cholesterol clefts are also evident throughout the section that is usually referred to as “keratin granuloma” [Figure 6].
Figure 5.
Keratin flecks and squamoid cells
Figure 6.
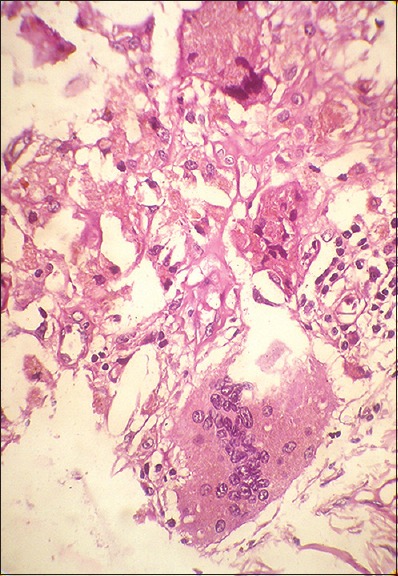
Keratin granuloma
The histopathological diagnosis of “epidermoid cyst” was given.
Discussion
Keratinous cysts are common lesions formed by invagination and cystic expansion of the epidermis or of the epithelium forming the hair follicle. These cysts have a tendency to rupture very easily thereby causing foreign body reaction. Ruptured epidermal cysts have been reported in 21.3% to 38.0% of cases, in the literature.[5] In such cases, the nature of the lesion is evident only by the presence of extruded keratin flakes surrounded by inflammatory cells and foreign body giant cells producing the “keratin granuloma.”[6]
In the present case, there was a rupture in the cyst causing disintegration of the overlying epithelium. Thus, commenting on which type of keratinous cyst was not possible. Hence, discussion includes brief review about general aspects and the complications of the keratinous cyst.
Keratinous cysts are lined by stratified epithelium, which may keratinize either with the formation of keratohyalin, forming a horny material resembling the epidermis or without the formation of keratohyalin, forming trichilemmal keratin.
Thus, keratinous cysts are divided into:
Epidermoid cysts (which consist of stratified squamous epithelium containing keratohyalin granules)
Trichilemmal cysts (which lack keratohyalin granules).[7]
Basic differences between epidermoid cysts and trichilemmal cysts are given in Table 1.
Table 1.
Basic differences between epidermoid cyst and pilar or trichilemmal cyst

Epidermoid cysts
Epidermoid cysts are common subcutaneous cysts that can occur anywhere in the body and 7% of them occur in the head and neck. It is defined as - “A simple cyst lined with stratified squamous epithelium and lumen is filled with cystic fluid or keratin and no other specialized structure.”[8] Epidermoid cysts can occur at any age from birth to 72 years; they usually become apparent in patients between 15 and 35 years. Males are more commonly affected. These are usually solitary, but multiple epidermal cysts can occur and may present as small or large masses. Thereby, epidermoid cysts which are more than 5 cm in size are termed as “giant epidermoid cysts.” Giant epidermoid cysts are comparatively rare especially in the head and neck area.[5,9] The size of the cyst is of significance as giant cysts (>5 cm) have more chances of malignant transformation as compared to conventional cysts. The present case is a case of giant epidermoid/keratinous cyst.
Etiopathogenesis
An epidermoid cyst is formed by the proliferation of epidermal cells within a circumscribed dermal space with retention of keratinous debris and cholesterol or sebaceous materials. These cysts are either congenital or acquired. Several theories of the formation of epidermoid cysts are known. A congenital epidermal cyst may be formed by trapping of displaced embryonic epithelial rests commonly occurring in the head and neck area.[5] An acquired epidermal cyst can result from occlusion of the pilosebaceous unit or implantation of viable epidermal cells in the dermis or subcutis.[5] It can be traumatic or surgical implantation of epithelial elements. Human papillomavirus (HPV) type 57 or 60 infections may be additional factors in the development of a palmoplantar epidermoid cyst.[10] Epidermoid cysts are also seen in patients with Gardner syndrome, particularly on the face and scalp.[5] They are also seen in basal cell nevus syndrome, and pachyonychia congenital.[11] Moghimi et al.[12] has described a case of perforated epidermoid cyst in association with Ehlers-Danlos syndrome.
Histologically, the cystic lining is comprised of stratified squamous epithelium resembling epidermis. Cases having areas of pseudostratified ciliated columnar epithelium are occasionally reported. A well-formed granular cell layer is present, and the lumen is filled with degenerating orthokeratin as its content. Dystrophic calcification and reactive foreign body reaction are commonly associated with the cystic capsule. This common property of the cyst to rupture and get inflamed is in part mediated by the horny material contained in the epidermoid cysts. Extracts of this material have been shown to be chemotactic for polymorphonucleocytes.[11] Jayalaxmi et al. reported an interesting case in which there was increased a number of melanocytes in the basal layer, large globular cells of melanocytic origin in the spinous layer, and hair-germ-like aggregates of basaloid cells and melanocytes.[6]
Malignant transformation
The feature that makes this cyst of diagnostic importance is the occurrence of secondary malignancies within the cyst. Malignancies occurring in the cyst include basal cell carcinoma, Bowen disease, squamous cell carcinoma, and even mycosis fungoides. Rarely, Paget's disease and Merkel cell carcinoma have also been reported.
Most common malignancy associated with the epidermoid cyst is squamous cell carcinoma. Basal cell carcinoma is the second most common malignancy occurring from this cyst. Exposure of the skin to ultraviolet radiation is the most common cause for the development of squamous cell carcinoma. HPV infection has also been stated as one of the causes. However, Anastasiosa et al. showed no etiological correlation between HPV and the development of squamous carcinoma in the small numbers of cases studied by them.[13] Squamous cell carcinoma is more likely to develop in an injured or chronically diseased skin.[10]
Trichilemmal cyst
These cysts are also known as Pilar cysts or Wen. They are known to arise from the outer root sheath epithelium and have a distinctive pattern of keratinization called trichilemmal keratinization.[14] Trichilemmal cysts are common, occurring in 5–10% of the population.[15] These cysts usually occur in areas with dense hair follicle concentrations; hence, 90% of these occur on the scalp.
One of the typical features of this cyst is that an overlying punctum is normally not present. Clinically, these cysts are indistinguishable from the epidermoid cysts. There are few clinical features that may favor the diagnosis of a trichilemmal cyst though none of them are absolutely characteristic. Trichilemmal cysts are firmer, and they get removed more easily through a surgical incision as compared to epidermoid cysts. Epidermoid cysts are 4–5 times more common than trichilemmal cysts. In some of these cysts (2% of cases), single or multiple foci of proliferating cells give rise to proliferating tumors, often called proliferating trichilemmal cysts or tumors.[6] Proliferating trichilemmal cysts grow rapidly and are known to occur de novo also.[16] They are easily enucleable with no punctum in contrast to epidermal cysts. Similar to trichilemmal cyst, proliferating trichilemmal tumor (PTT) has a predilection for the scalp but elderly females are more prone.[14,15]
Etiopathogenesis
Certain authors believe that the trichilemmal cyst originates from budding of the external root sheath of hair follicles as a result of genetic aberration. In this type of cyst, cells undergo an abrupt transition from the stratum spinosum to the keratinized layer skipping the formation of the granular layer.[6] The lesion is autosomal dominant and can run in families.[1]
Histopathology
The cyst contains homogeneous eosinophilic material which in contrast to the lamellated keratin flakes in an epidermoid cyst. Cholesterol clefts are common in the keratinous material present within the cyst content. 1/4th of cysts show calcification. These cysts also show a propensity to rupture with considerable foreign body giant cell reaction and thereby evoke inflammation in surrounding tissue like the previous cyst.
However, only a few reports in the literature have highlighted the immunologic nature of this reaction. The pathologic processes occurring in these cysts could be attributed to:
Rupture of the cyst with its accompanying inflammation; or
Loss of equilibrium between matrix metalloproteinases and their inhibitors
Adiponectin released by adjacent adipocytes may regulate the inflammatory responses in the area.[16]
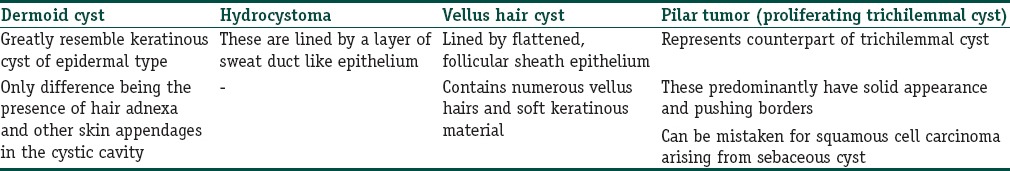
Various histological differential diagnosis for these cysts are given in Table 2.
Table 2.
Histopathological differential diagnosis
Malignant transformation
In some instances, malignant transformation of PTT occurs, and this malignant lesion presents some areas reminiscent of trichilemmal keratinization but shows severe atypia and invasion of the surrounding tissue.[14]
Trichilemmal carcinoma is a lesion commonly presenting as a slow growing epidermal papule, indurated plaque, or nodule that may ulcerate on the face or ears[16] and in rare instances may show the carcinomatous transformation.[17]
Apart from the overall malignant transformation rate, which varies from 0.033% to 9.2% in some articles,[18] to 1.5–10% in others,[19] certain other complications for these cysts are infection, Cock's peculiar tumor, abscess, cutaneous horn, which make this cyst an important diagnostic entity.[11,20]
Another feature to be noted in the present case was the clinical presentation of this lesion, which mimicked lipoma in its appearance. Even, FNAC findings revealed features of lipoma. However, this diagnostic discrepancy between clinical and histopathological features of this lesion is significant as the biological behavior, as well as the treatment of both these lesions vary. Table 3 describes the significant differences between these two entities.[20,21]
Table 3.
Differences between treatment and prognosis of lipoma and keratinous cyst

Conclusion
While dealing with scalp lesions, as well as other cutaneous lesions, of the head and neck region differential diagnosis of keratinous cysts should be kept in mind as these cysts carry certain complications such as cystic rupture, abscess, secondary, and infections, during their treatment. These cysts carry relatively more recurrence rate as compared to lipoma and certain other benign lesions mimicking these cysts. As also, these cysts require thorough histopathological examination and close follow-up due to their potential for malignant transformation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
What is new?
A rare case report of the giant congenital epidermal cyst with a review on various cysts containing keratinous material and their malignant transformation.
References
- 1.Zuber TJ. Minimal excision technique for epidermoid (sebaceous) cysts. Am Fam Physician. 2002;65:1409. [PubMed] [Google Scholar]
- 2.Nicolaides N, Levan NE, Fu HC. The lipid pattern of the wen (keratinous cyst of the skin) J Invest Dermatol. 1968;50:189–94. doi: 10.1038/jid.1968.23. [DOI] [PubMed] [Google Scholar]
- 3.Mackie RM. Tumours of the skin. In: Rook A, Wilkinson DS, Ebling FJ, editors. Textbook of Dermatology. 4th ed. Vol. 3. St. Louis: Blackwell Mosby Book Distributors; 1986. pp. 2405–6. [Google Scholar]
- 4.Kang SG, Kim CH, Cho HK, Park MY, Lee YJ, Cho MK. Two cases of giant epidermal cyst occurring in the neck. Ann Dermatol. 2011;23(Suppl 1):S135–8. doi: 10.5021/ad.2011.23.S1.S135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang CC, Ko SF, Huang HY, Ng SH, Lee TY, Lee YW, et al. Epidermal cysts in the superficial soft tissue: Sonographic features with an emphasis on the pseudotestis pattern. J Ultrasound Med. 2011;30:11–7. doi: 10.7863/jum.2011.30.1.11. [DOI] [PubMed] [Google Scholar]
- 6.Jayalakshmy PS, Subitha K, Priya PV, Johnson G. Pigmented epidermal cyst with dense collection of melanin: A rare entity. Report of a case with review of the literature. Indian Dermatol Online J. 2012;3:131–4. doi: 10.4103/2229-5178.96714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsujita-Kyutoku M, Danbara N, Yuri T, Nikaido Y, Hatano T, Tsubura A. Basal cell carcinoma arising from a keratinous cyst of the skin: A case report and review of the literature. Med Mol Morphol. 2005;38:130–3. doi: 10.1007/s00795-004-0285-9. [DOI] [PubMed] [Google Scholar]
- 8.Janarthanam J, Mahadevan S. Epidermoid cyst of submandibular region. J Oral Maxillofac Pathol. 2012;16:435–7. doi: 10.4103/0973-029X.102511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Im JT, Park BY. Giant epidermal cyst on posterior scalp. Arch Plast Surg. 2013;40:280–2. doi: 10.5999/aps.2013.40.3.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hegde PN, Prasad HL, Kumar YS, Sajitha K, Roy PS, Raju M, et al. A rare case of an epidermoid cyst in the parotid gland – Which was diagnosed by fine needle aspiration cytology. J Clin Diagn Res. 2013;7:550–2. doi: 10.7860/JCDR/2013/4857.2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dive AM, Khandekar S, Moharil R, Deshmukh S. Epidermoid cyst of the outer ear: A case report and review of literature. Indian J Otol. 2012;18:34–7. [Google Scholar]
- 12.Moghimi M, Soltani HR, Amini-Rad O. Ehlers-Danlos syndrome with muluscoid pseudo-tumor, spheroid and keratinous cyst – Report a rare case. Journal of Isfahan Medical School. 2011;28:1–7. [Google Scholar]
- 13.Anastasiosa KV, Alexandra G, Anthony K, Efthimios S. Malignant transformation in a typical epidermal cutaneous cyst. J Med Cases. 2012;3:254–6. [Google Scholar]
- 14.Lin CY, Jwo SC. Squamous cell carcinoma arising in an epidermal inclusion cyst. Chang Gung Med J. 2002;25:279–82. [PubMed] [Google Scholar]
- 15.Abrahão A, Daltoé P, Santos AV, Sugaya NN, Pinto DS. A rare case of intraoral trichilemmal cyst. J Oral Diagn. 2012;1:1–3. [Google Scholar]
- 16.Chang SJ, Sims J, Murtagh FR, McCaffrey JC, Messina JL. Proliferating trichilemmal cysts of the scalp on CT. AJNR Am J Neuroradiol. 2006;27:712–4. [PMC free article] [PubMed] [Google Scholar]
- 17.Ramaswamy AS, Manjunatha HK, Sunilkumar B, Arunkumar SP. Morphological spectrum of pilar cysts. N Am J Med Sci. 2013;5:124–8. doi: 10.4103/1947-2714.107532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alam K, Gupta K, Maheshwari V, Varshney M, Jain A, Khan AH. A large proliferating trichilemmal cyst masquerading as squamous cell carcinoma. Indian J Dermatol. 2015;60:104. doi: 10.4103/0019-5154.147854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sinha P, Lingegowda JB, Selvi RT. Malignant transformation in sebaceous cyst – A case report. Int J Med Health Sci. 2012;1:63–5.14. [Google Scholar]
- 20.Bolbandi AK, Klirishnappa P, Bennehalli A. Varied presentations of epithelial cysts. Int J Case Rep Images. 2012;3:65–7. [Google Scholar]
- 21.Pandya KA, Radke F. Benign Skin Lesions: Lipomas, Epidermal Inclusion Cysts, Muscle and Nerve Biopsies. Surg Clin N Am. 2009;89:677–687. doi: 10.1016/j.suc.2009.03.002. [DOI] [PubMed] [Google Scholar]


