Abstract
Background
Most individuals experience more than one trauma. Hence, it is important to consider the count and types of traumas (polytraumatization) in relation to post-trauma mental health.
Method
The current study examined the relation of polytraumatization patterns to PTSD clusters (intrusions, avoidance, negative alterations in cognitions and mood [NACM], and alterations in arousal and reactivity [AAR]), depression, and impulsivity facets (lack of perseverance, lack of premeditation, negative urgency, sensation seeking) using a web-based sample of 346 participants. Age, gender, race, and ethnicity were covariates.
Results
Results of latent class analyses indicated a three-class solution: Low Experience, Moderate Experience – Predominent Threat/Indirect PTEs (Moderate Experience), and High Experience – Predominant Interpersonal PTEs (High/Interpersonal). Multinomial logistic regression results indicated that ethnicity and gender were significant covariates in predicting Low versus High/Interpersonal Class, and Moderate Experience versus High/Interpersonal Class membership, respectively. The High/Interpersonal Class had higher scores on most PTSD clusters, depression, and the impulsivity facets of lack of perseverance and negative urgency compared to the other classes. The Low and Moderate Experience Classes differed on PTSD’s avoidance and AAR clusters (lower in the former).
Conclusions
Individuals exposed to multiple PTE types, particularly interpersonal traumas, may be at risk for more severe post-trauma symptoms.
Keywords: Polytrauma, Interpersonal Trauma, Latent Class Analysis, Post-Trauma Mental Health
1. Introduction
Posttraumatic stress disorder (PTSD) is one of the few Diagnostic and Statistical Manual (DSM) diagnoses wherein the experience of a potentially traumatizing event (PTE) is a necessary diagnostic component [Criterion A; 1]. Most researchers and clinicians address the index event (most distressing or traumatic event) as influencing post-trauma mental health including PTSD symptoms [2] despite the fact that most individuals experience more than one lifetime PTE [polytraumatization; 3]. Hence, one needs to comprehensively assess the influence of all experienced PTEs on post-trauma mental health symptoms [2, 4]. Person-centered statistical approaches are well-suited to accomplish this goal by examining polytraumatization patterns in relation to post-trauma mental health [5, 6]; this is the focus of the current study.
Most individuals experience more than one type of PTE (e.g., motor vehicle accident, natural disaster) in their lifetime [7, 8]. Relative to experiencing single PTEs, the experience of multiple PTEs relates to poorer mental/physical health [3, 8–10]. These results prompt a need to consider potential factors inherent to the experience of multiple PTEs that could explain their greater impact [11–13]. First, the type of PTE matters in relation to psychopathology prevalence and severity [14]. As an example, the type of PTE influences the conditional risk of developing PTSD, and PTSD severity [15, 16]. Patterns of different PTE types may influence unique distal, proximal, and co-occurring mental health symptom outcomes [5, 17–19]. Second, the count of PTEs matters in relation to psychopathology prevalence and severity. A dose-response effect exists between increasing number of PTEs and poorer mental/physical health [20]. An increasing number of PTEs relates to greater depression and PTSD severity and poorer quality of life [10, 21]. A higher count of PTEs may influence sensitization and kindling effects, possibly lowering the threshold for emotional responding to aversive stimuli, and contributing to more severe behavioral and physiological reactions to later traumas [22, 23]. Third, the count of PTE types is an additional characteristic to consider; this refers to the number of different types of PTEs. There is a positive relation between the total number of different types of childhood PTEs and complex trauma, or the total number of different types of co-occurring symptoms [24–26]. The cumulative and additive effects of PTE types contributes to the development of PTSD, higher PTSD severity, and lower probability of remission over time, referred to as a “building block effect” [27, 28].
To account for the count, type, co-occurrence, and interactive impact of all PTEs [8, 9, 29], Cougle et al. [4] recommended assessing all PTEs and a subset of the index, most recent, and first PTE. The construct of polytraumatization [3] captures the experience of a broad array of PTEs (count and type); it is not restricted to focusing on certain PTE types [9], repeated experiences of a single PTE [30, 31], or the count of PTE types [32, 33]. Person-centered approaches such as latent class (LCA) and latent profile analysis (LPA) are recommended to examine such polytraumatization patterns. LCA/LPA identify meaningful subgroups of individuals with shared patterns of PTE experiences [5, 6] and permit an examination of the nature of meaningful subgroups of individuals based on the type and count of PTEs endorsed.
In the existing literature on polytraumatization patterns, relatively few studies have examined lifespan polytraumatization patterns [34]; rather most studies have examined PTEs occurring in one developmental period such as childhood [35]. Such an approach prevents an assessment of the cumulative impact of different PTEs across one’s lifespan. Studies assessing lifespan polytraumatization patterns (see Table 1) have indicated three [34, 36–38] or four [39–41] meaningful subgroups of participants; such results are consistent with a recent systematic review on lifespan polytrauma patterns [42]. The obtained subgroups generally differed both in PTE types (interpersonal versus indirect) and in degree of the amount of traumatic experiences (low, moderate, high). The results have been consistent despite the diversity of samples including type (e.g., university students [40], civilians [37, 39], victims of intimate partner violence [34]) and gender composition (e.g., solely females [34, 37], solely males [39]).
Table 1.
Summary of studies assessing lifespan polytrauma patterns.
| Study | Sample | Assessed PTEs | Optimal Class solution and Class Labels |
|---|---|---|---|
| Armour & Sleath (2014). | 2980 Danish young adults aged 24 years. | Physical assault, psychological aggression, injury, and sexual coercion across three exposure periods — parental, adolescence, and adulthood. | A 4-class solution: (1) Non-abused; (2) Emotionally abused; (3) Sexually abused; (4) Abused overall (highest probabilities for most PTEs). |
| Burns et al. (2016). | 14,564 U.S. non- institutionalized male civilians residing in households and group quarters. | Childhood PTEs (physical abuse, neglect, witness domestic violence); and lifetime PTEs (sexual assault, IPV, physical assault, being stalked, threatening event). | A 4-class solution: (1) Normative (low/no victimization); (2) High witnessing domestic violence and poly-victimization; (3) Adult victimization (elevated endorsement of adult interpersonal victimization); and (4) Childhood and adulthood poly-victimization. |
| Cavanaugh et al. (2013). | 19,816 U.S. females from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. | Childhood PTEs (physical abuse, neglect, witnessing domestic violence); and lifetime PTEs (physical IPV, other physical assault, sexual assault, being stalked). | A 3-class solution: (1) Class 1 (high probability of witnessing domestic violence in childhood, highest exposure to interpersonal violence); (2) Class 3 (low probabilities of all PTEs); and (3) Class 2 (Low probabilities on all interpersonal violence and abuse PTEs except sexual assault). |
| Golder et al. (2012). | 212 U.S. female victims of IPV. | CAN (emotional, physical and sexual abuse, emotional and physical neglect); and current IPV within 6 months (physical and sexual IPV, psychological IPV, IPV-related injury). | A 3-class solution: (1) High IPV-High CAN Victimization; (2) Low IPV-Low CAN Victimization; and (3) Low IPV-High CAN Victimization. |
| Holt et al. (2016). | 1211 U.S. first-year university students. | Peer victimization (relational, verbal, physical, sexual harassment, cyber); other victimization (dating violence, attempted/completed rape, childhood maltreatment). | 4-class solution: (1) Poly-victimization; (2) Minimal victimization; (3) Peer victimization (higher probabilities of relational/verbal peer victimization); (4) Poly-sexual (higher probabilities of dating violence and rape). |
| Sullivan et al. (2017). | 849 participants recruited through Amazon’s MTurk platform. | Lifetime PTEs assessed by the Trauma History Questionnaire (e.g., being mugged, robbery, home break-ins, car/work accident, natural/man-made disasters, situation with threat of death or injury, witnessing a death or serious injury, combat, sexual assault, assault with weapon) [118]. | 3-class solution: (1) High-Exposure; (2) Low Exposure; and (3) Moderate Exposure – Predominent Mugging/Accident. |
| Walsh et al. (2012). | 482 U.S. Females attending a STD clinic. | CM (physical and psychological abuse, neglect); CSA; IPV; ECV | 4-class solution: (1) Multiply Victimized (higher probability of most PTEs); (2) Low violence (below-average probability of most PTEs); (3) Predominantly ECV; and (4) Predominantly CM. |
Note. IPV is Intimate Partner Violence; CAN is childhood abuse and neglect; CM is childhood maltreatment; ECV is Exposure to Community Violence; CSA is Childhood Sexual Abuse.
Among the reviewed studies in Table 1, some limitations of the existing literature are apparent. One, most studies have assessed only interpersonal PTEs [36, 37, 39]. Second, few studies have used web-based surveys to study community samples, which allow for more anonymity and perhaps an increase in self-disclosure [38]. Third, limited studies have addressed the heterogeneity in PTSD symptoms clusters relating to polytraumatization patterns [34]. PTSD is a heterogeneous disorder [43] comprising of clusters of intrusions, effortful avoidance of internal and external trauma-related triggers, negative alterations in cognitions and mood (NACM), and alterations in arousal and reactivity (AAR) [1]. The PTSD symptom clusters differentially relate to psychopathology, supporting their discriminant validity [44–46]. Hence, it is beneficial and appropriate to conceptualize PTSD in terms of its different symptom clusters rather than as a unitary construct. Lastly, no study to our knowledge has examined relations between polytraumatization patterns and impulsivity facets. The UPPS Impulsivity Scale conceptualizes impulsivity as a multidimensional construct [47] comprised of four facets: lack of premeditation (tendency to act without careful thought), negative urgency (tendency to engage in impulsive behaviors in the context of negative affect), sensation seeking (tendency to seek excitement), and lack of perseverance (difficulty completing tasks and tendency to become easily bored). Research indicates that different types [48, 49] and degrees [50] of traumatic experiences relate differently to the ability to control impulsive tendencies including engagement in substance use [51, 52], and aggressive acts [53]. Thus, impulsivity is a relevant yet understudied construct in relation to traumatic experiences.
Accounting for the aforementioned limitations, the current study examined polytraumatization patterns (subtypes) in relation to post-trauma mental health. Using a web-based recruited sample with experiences of at least one PTE, we examined (1) latent subgroups of individuals based on their lifetime PTE type endorsements, and (2) the construct validity of the optimal latent class solution. On uncovering latent subgroups of individuals, we modeled proximal demographic covariates of the optimal class solution (age, gender, race and ethnicity) based on empirical evidence. Studies have shown that increasing count of PTEs (specifically interpersonal traumas) correlates with increasing age [38], and childhood-onset interpersonal traumas are associated with more severe psychopathology compared to traumas at other developmental periods [54].
Further, females are more likely to experience interpersonal traumas, and more likely to meet criteria for PTSD compared to males [55]. Regarding race and ethnicity, the differential exposure and differential vulnerability hypotheses suggest differences in post-trauma severity across racial and ethnic groups. The differential exposure hypothesis attributes between-group differences to differential degrees of PTE exposure [56]. For example, Whites experience fewer traumatic events compared to African Americans [16, 57, 58]. Conversely, the differential vulnerability hypothesis attributes between-group differences to increased vulnerability to stressors linked to racial and ethnic factors (e.g., history of discrimination, differences in coping styles) [56, 59]. Further, we included post-trauma mental health distal outcomes as dependent variables associated with the optimal class solution. Based on theoretical and empirical accounts, we examined PTSD, depression, and impulsivity in relation to polytraumatization patterns. PTSD is etiologically linked to the experience of a traumatic event [60], and experiencing multiple traumas relates to increasing PTSD severity [34, 36, 38]. The type of PTE is important; PTEs most associated with a PTSD diagnosis involve interpersonal violence including sexual assault [16, 19, 61] and combat-related stressors [61]. Referencing the relation between impulsivity and PTEs, engagement in impulsive behaviors may functionally help to reduce post-trauma negative affect [62–64]. Further, a cognitive explanation [65] states that difficulties in attention and information processing capacities following PTEs may lead individuals to behave impulsively to help them redirect their attention, or distract themselves from intrusive thoughts [66–68]. We additionally examined depression as a post-trauma mental health outcome in the current study based on its common occurrence following PTEs [69, 70]. Depression is a causal risk factor for PTEs, and may increase the risk of PTSD following the experience of PTEs [52, 71]. Shared risk/buffering factors [52, 71] and symptoms [71, 72] may account for the co-occurrence of PTSD and depression, and the high prevalence of depression following PTEs [69, 70]. Unsurprisingly, multiple TEs is associated with greater depression severity [34, 36].
In our study, we hypothesized finding a best-fitting three- or four-class solution [36, 38, 39], and finding a latent class with predominant interpersonal trauma types [37, 38, 73]. Further, we predicted that greater PTSD severity, depression severity, and impulsivity would relate to the experience of multiple PTEs. For the most part, the analyses regarding the relation of the optimal class solution and the dependent variables were exploratory in nature.
2. Method
2.1. Procedure and participants
The Institutional Review Board of University of North Texas approved the study. We recruited participants through Amazon’s Mechanical Turk (MTurk) platform [74]. The study (requiring approximately 30 minutes) included completing questionnaires assessing the impact of stressful life experiences. Relevant inclusion criteria included being 18 years old and older, living in North America, knowledge of the English language (by asking a question on this), and experiencing a PTE (measured by the Stressful Life Events Screening Questionnaire). After obtaining informed consent, participants completed the survey hosted on Psychdata.com, which is a secure data collection platform. We employed post-hoc validity checks to ensure data quality; we excluded data entered by individuals attempting the survey multiple times in an effort to meet study’s inclusionary criteria, and removed duplicate responses. We compensated participants 75 cents for study participation.
2.2. Exclusions, and sample characteristics
Among the 499 participants who completed the survey, we excluded 19 participants who attempted the questionnaire twice/thrice (n = 480). We further excluded participants (1) not meeting one or more of the inclusionary criteria (n = 120); (2) missing data on all measures (n = 11); and (3) missing more than 70% item-level data on any measure administered for the study (n = 3). Among 346 participants, missing data was minimal; one, four, and forty participants were missing three, two, and one PTSD Checklist for DSM-5 items [PCL-5; 75] respectively. Missing data was estimated using Maximum Likelihood in Mplus 7.31 software [76]. The sample of 346 participants averaged 33.61 years (SD = 9.53), and approximately half were female (n = 199, 57.70%). Most were employed full time (n = 226, 65.70%). The sample averaged 15.31 years of schooling (SD = 2.43). A majority identified themselves as White (n = 287, 83.20%) and not Hispanic/Latino (n = 295, 86%; see Table 2).
Table 2.
Descriptive information on demographics constructs for the entire sample and each latent class.
| Full Sample (n = 346) | Class 1 (n = 205) | Class 2 (n = 46) | Class 3 (n = 95) | |
|---|---|---|---|---|
| Mean (SD) | ||||
|
| ||||
| Age | 33.61 (9.53) | 33.63 (9.69) | 35.09 (10.29) | 32.88 (8.80) |
| Years of schooling | 15.31 (2.43) | 15.47 (2.25) | 15.31 (1.92) | 14.96 (2.97) |
|
| ||||
| n (% of total sample)* | ||||
|
| ||||
| Female | 199 (57.70%) | 125 (36.20%) | 8 (2.30%) | 66 (19.10%) |
|
| ||||
| Employment Status | ||||
|
| ||||
| Part time | 59 (17.20%) | 42 (12.20%) | 4 (1.20%) | 13 (3.80%) |
| Full time | 226 (65.70%) | 129 (37.50%) | 34 (9.90%) | 63 (18.30%) |
| Unemployed | 44 (12.80%) | 28 (8.10%) | 4 (1.20%) | 12 (3.50%) |
| Unemployed Student | 8 (2.30%) | 2 (.60%) | 2 (.60%) | 4 (1.20%) |
| Retired | 7 (2%) | 4 (1.20%) | 1 (.30%) | 2 (.60%) |
|
| ||||
| Relationship Status | ||||
|
| ||||
| Single | 123 (35.70%) | 71 (20.60%) | 17 (4.90%) | 35 (10.10%) |
| Living with significant other | 50 (14.50%) | 27 (7.80%) | 7 (2.0%) | 16 (4.60%) |
| Married | 149 (43.20%) | 94 (27.20%) | 19 (5.50%) | 36 (10.40%) |
| Divorced, separated, or widowed | 23 (6.70%) | 13 (3.80%) | 2 (.60%) | 8 (2.30%) |
|
| ||||
| Racial Status | ||||
|
| ||||
| White | 287 (83.20%) | 169 (49%) | 39 (11.30%) | 79 (22.90%) |
| Asian | 36 (10.40%) | 22 (6.40%) | 2 (.60%) | 12 (6.40%) |
| African American | 22 (6.40%) | 10 (2.90%) | 2 (.60%) | 10 (2.90%) |
| American Indian or Alaskan Native | 16 (4.60%) | 12 (3.50%) | 0 (0%) | 4 (1.20%) |
| Native Hawaiian/other Pacific Islander | 5 (1.40%) | 1 (.30%) | 1 (.30%) | 3 (.90%) |
|
| ||||
| Ethnicity | ||||
|
| ||||
| Hispanic or Latino | 39 (11.40%) | 15 (4.40%) | 1 (.30%) | 23 (6.70%) |
| Not Hispanic or Latino | 295 (86%) | 184 (53.60%) | 42 (12.20%) | 69 (20.10%) |
| Unknown | 9 (2.60%) | 4 (1.20%) | 2 (.60%) | 3 (.90%) |
|
| ||||
| Income | ||||
|
| ||||
| Less than $15,000 | 40 (11.60%) | 28 (8.10%) | 3 (.90%) | 9 (2.60%) |
| $15,000 – $24,999 | 46 (13.30%) | 28 (8.10%) | 4 (1.20%) | 14 (4.10%) |
| $25,000 – $34,999 | 55 (15.90%) | 26 (7.50%) | 5 (1.40%) | 24 (7%) |
| $35,000 – $49,999 | 53 (15.40%) | 31 (9%) | 9 (2.60%) | 13 (3.80%) |
| $50,000 – $64,999 | 53 (15.40%) | 35 (10%) | 6 (1.70%) | 12 (3.50%) |
| $65,000 – $79,999 | 34 (9.90%) | 17 (4.90%) | 5 (1.40%) | 12 (3.50%) |
| $80,000 and higher | 64 (18.60%) | 40 (11.60%) | 13 (3.80%) | 11 (3.20%) |
|
| ||||
| Lifetime PTEs endorsed | ||||
|
| ||||
| Life-threatening illness | 118 (34.20%) | 51 (14.80%) | 12 (3.50%) | 55 (15.90%) |
| Life-threatening accident | 157 (45.50%) | 79 (22.90%) | 25 (7.20%) | 53 (15.40%) |
| Physical force/weapon used (robbery/mugging) | 67 (19.40%) | 4 (1.20%) | 22 (6.40%) | 41 (11.90%) |
| Family member/romantic partner/friend died (accident, homicide, or suicide) | 187 (54.20%) | 94 (27.20%) | 25 (7.20%) | 68 (19.70%) |
| Physical force used to have sex | 99 (28/70%) | 27 (7.80%) | 1 (.30%) | 71 (20.60%) |
| Physical force/threat to try to have sex | 82 (23.80%) | 17 (4.90%) | 3 (.90%) | 62 (18%) |
| Touched body private parts | 133 (38.60%) | 50 (14.50%) | 1 (.30%) | 82 (23.80%) |
| Parent/caregiver physically harmed you | 132 (38.30%) | 47 (13.60%) | 19 (5.50%) | 66 (19.10%) |
| Partner/date, etc. physically harmed you | 158 (45.80%) | 54 (15.70%) | 25 (7.20%) | 79 (22.90%) |
| Threatened with a weapon | 120 (34.80%) | 16 (4.60%) | 43 (12.50%) | 61 (17.70%) |
| Present when someone was killed, injured, or assaulted | 109 (31.60%) | 43 (12.50%) | 32 (9.30%) | 34 (9.90%) |
| Repeated exposure to vivid trauma details | 81 (23.50%) | 31 (9%) | 22 (6.40%) | 28 (8.10%) |
Note.
All reported percentages are valid percentages to account for missing data; Class 1 is Low Experience; Class 2 is Moderate Experience – Predominent Threat/Indirect PTEs; Class 3 is High Experience–Predominant Interpersonal Trauma.
2.3. Measures
2.3.1. Stressful Life Events Screening Questionnaire [SLESQ; 77]
The SLESQ is a 14-item self-report measure assessing lifetime PTEs. Response options are dichotomous (yes/no). We added three items to be consistent with DSM-5 Criterion A [78]. The SLESQ has good 2-week item-level test-retest reliability and concurrent and convergent validity [77]. Participants endorsing more than one PTE specified and referenced their most distressing PTE while responding to the subsequent measure assessing PTSD symptoms. For the analyses, we used the first 12 SLESQ items as indicators; excluding item 13 because it is a catch-all item for other PTEs (does not provide specific information on the PTE type), and item 14 which assesses for the most distressing PTE (overlaps with items 1–12).
2.3.2. PTSD Checklist for DSM-5 [PCL-5; 75]
The PCL-5 is a 20-item self-report measure that assesses severity of PTSD symptoms referencing the past month. Response options range from 0 (Not at all) to 4 (Extremely). Participants responded to the PCL-5 referencing the most distressing event endorsed on the SLESQ. The PCL-5 has excellent internal consistency, good test-retest reliability, and good convergent and discriminant validity [79–81]. The item-level responses were summed to create four DSM-5 PTSD subscale scores of intrusions, avoidance, NACM, and AAR [1]. Cronbach’s α were .90, .89, .92, .87, respectively, in the current study. Probable PTSD is indicated by a score of 31 or higher [80]. Mean scores for the averaged PTSD symptom clusters (0–4 scale) were 1.77 (SD = 1.07), 1.88 (SD = 1.25), 1.56 (SD = 1.07), and 1.53 (SD = 1.07) for intrusions, avoidance, NACM, and AAR, respectively.
2.3.3. The UPPS Impulsive Behavior Scale [UPPS; 47]
The UPPS is a 45-item self-report measure assessing four impulsivity facets: lack of premeditation, negative urgency, sensation seeking, and lack of perseverance. Response options range from 1 (Agree Strongly) to 4 (Disagree Strongly). The facets have good internal consistency and convergent and divergent validity [47, 82, 83]. Cronbach’s α for the lack of premeditation, negative urgency, sensation seeking, and lack of perseverance facets were .88, .90, .90, and .87 respectively in the study sample. We used a past-month timeline of inquiry for consistency with PTSD ratings. Mean scores for the averaged UPPS subscale scores (1–4 scale) were 1.92 (SD = 0.52), 2.43 (SD = 0.63), 2.36 (SD = 0.69), and 2.03 (SD = 0.56) for lack of premeditation, negative urgency, sensation seeking, and lack of perseverance facets respectively.
2.3.4. Patient Health Questionnaire-9 [PHQ-9; 84]
The PHQ-9 is a 9-item self-report measure assessing DSM-IV depression symptoms over the past two weeks. The four response options range from 0 (not at all) to 3 (nearly everyday) [84]. It has good internal consistency (α = .91 in the current study), test-retest reliability (r = .84), construct validity, and diagnostic validity [84]. Mean score for the averaged PHQ-9 score (0–3 scale) was 1.01 (SD = .73).
2.4. Data Analysis
We conducted a latent class analysis (LCA) using Mplus 7.31 to categorize participants into latent subgroups based on their endorsed PTEs on the SLESQ. We used Maximum Likelihood estimation with robust standard errors (MLR) as the estimator. One- through six-class models were analyzed based on prior research [35, 38]. According to the recommended fit indices, the optimal class solution had lowest Bayesian Information Criterion (BIC) values, lowest sample-size adjusted BIC (SSABIC) values, a significant Lo–Mendell–Rubin Adjusted Likelihood Ratio Test value (LMR), a significant Bootstrapped Likelihood Ratio Test (BLRT) p value, relatively higher entropy values, and conceptual and interpretive meaning [85–87]. When comparing a K-class model with a K-1 class model, a significant LMR test indicates that the model with K classes is optimal [85]. LMR has been shown to be competent with a sample size comparable to the current study and with models of unequal sample size classes; a limitation is that it may over-extract classes [85]. A model with a 10-point lower BIC value has a 150:1 likelihood to be the better fitting model [88]. The SSABIC is considered as a more robust index compared to the BIC value index when considering all possible combinations of number of indicators and sample sizes [85].
Next, we examined the effects of relevant covariates (age, gender, race, and ethnicity) on latent class membership of the best-fitting class solution. Multinomial logistic regression analysis was used for regressing the latent class variable on the covariates. As distal dependent variables of latent class membership, we regressed PTSD symptom clusters, depression, and impulsivity facet scores on the latent class variable. We used the three-step approach (Bolck, Croon, and Hagenaars; BCH) to estimate class membership in relation to auxiliary variables of interest while accounting for misspecification bias [89, 90].
3. Results
3.1. LCA Results
Table 3 provides the LCA results (1–6 class solutions). We chose the 3-class solution as the optimal model. Considering several fit indices in selecting a class solution is recommended rather than relying on one index [85, 87]; most recommended fit indices indicated a 3-class solution. First, according to the LRT value guidelines, the 3-class solution was optimal [85, 87]. Second, although the BIC values increased beyond the 2-class solution, the increase of less than 10 points between the 2- and 3-class solutions was not substantial, hence indicating the 2- or 3-class solutions to be optimal [88]. In fact, the BIC values had a substantial increase of more than 10 points beyond the 3-class solution, indicating increasingly poorer model fit beyond the 3-class solution. Third, SSABIC values were decreasing between the 2- and 5-class solutions; the decrease was minimal from the 3-class to the 4-class solution indicating the 3-class solution to be a potential optimal model if supported by other fit indices [87]. Fourth, most existing literature on polytraumatization supports a 3-class solution [34, 36–38], and the three-class solution has interpretative value. Finally, entropy values were optimal for the 3-class solution compared to other potential models. Given the trend of significant p values until the 4-class solution, the BLRT indicated an optimal 5-class solution; however, the 5-class solution had no other substantial support as the optimal model based on recommended guidelines [85, 87].
Table 3.
Results of the latent class analyses.
| Model | AIC | BIC | SSABIC | Entropy | Adjusted Lo-Mendell – Rubin (p) | BLRT p value |
|---|---|---|---|---|---|---|
| 1 class | 5212.029 | 5258.186 | 5220.119 | |||
| 2 class | 4913.955 | 5010.116 | 4930.809 | .78 | 319.866 (p < .001) | p < .001 |
| 3 class | 4865.154 | 5011.318 | 4890.771 | .80 | 73.830 (p = .01) | p < .001 |
| 4 class | 4840.228 | 5036.397 | 4874.610 | .76 | 50.264 (p = .47) | p < .001 |
| 5-class | 4826.621 | 5072.793 | 4869.767 | .82 | 39.093 (p =.09) | p = .01 |
| 6-class | 4820.821 | 5116.997 | 4872.731 | .80 | 31.387 (p =.63) | p = .08 |
Note. AIC is Akaike Information Criterion, BIC is Bayesian Information Criterion, SSABIC is sample-size adjusted BIC, BLRT is Bootstrapped Likelihood Ratio Test
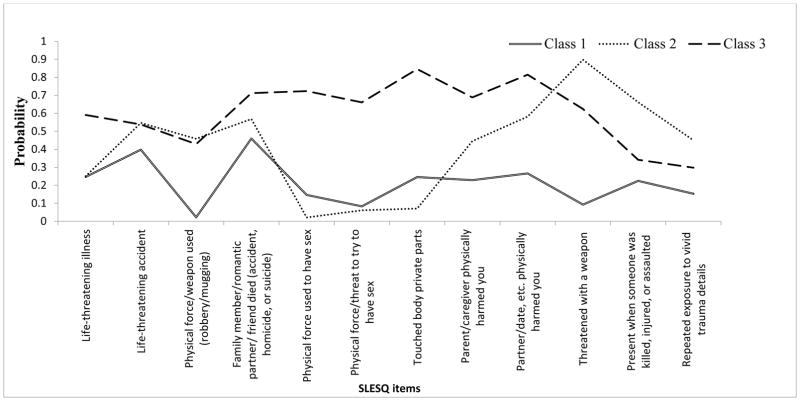
Figure 1 provides a graphical depiction of the 3-class solution. We labelled the classes based on significant patterns and predominant PTEs endorsed by class members, with the caveat the class names do not capture the entire complexity and heterogenity embedded in the experience of multiple PTEs. Class 1 members (n = 205; 59.25%) were characterized by relatively lower probability of endorsement of most PTEs compared to other classes. Thus, Class 1 was labelled “Low Experience.” Specifically, Class 1 members had a significantly lower probability of endorsing all PTEs compared to Class 3. Class 2 members (n = 46; 13.30%) had prominent endorsements of some PTEs such as being threatened with a weapon, witnessing someone being killed/injured/assaulted, and repeated exposure to vivid trauma details. Class 2 members had a higher probability of endorsing most PTEs compared to Class 1 members (excluding life-threatening illness, life-threatening accidents, having family member/close person die due to accident, homicide, or suicide, experiencing physical force to have sex, and experiencing physical force/threat to try to have sex). Class 2 had a predominance of vicarious and indirectly experienced PTEs and threat-based PTEs. Thus, Class 2 was labelled as Moderate Experience – Predominent Threat/Indirect PTEs (“Moderate Experience”).
Figure 1.
Latent profiles of participants based on their endorsed potentially traumatizing experiences across one’s lifetime.
Note. Class 1 is Low Experience; Class 2 is Moderate Experience – Predominent Threat/Indirect PTEs; Class 3 is High Experience – Predominant Interpersonal Trauma
Class 3 members (n = 95; 27.46%) were characterized by relatively greater probability of endorsing several PTEs (predominantly interpersonal physical and sexual abuse) compared to other classes. Compared to Class 2, Class 3 members had a significantly greater probability of endorsing most PTEs; and significantly less probability of endorsing some PTEs (threatened with a weapon, witnessing someone being killed, injured or assualted, repeated exposure to vivid trauma details). There was no significant differences across Classes 2 and 3 for the PTEs of life-threatening accident, having physical force/weapon used in robbery/mugging, and having a family member/close person die due to accident, homicide, or suicide. Thus, Class 3 was labelled as High Experience – Predominant Interpersonal Trauma (“High/Interpersonal”). Consistent with past research, we used the composite term of interpersonal trauma to cover several PTEs such as physical and sexual abuse, maltreatment, emotional abuse and incest, severe bullying, and witnessing domestic violence [91, 92].
3.2. LCA Covariate and Outcome Results
See Table 4 for detailed results of the multinomial logistic regression analyses for the covariates. For the covariate analyses, all classes were compared to the High/Interpersonal Class (default in Mplus). Results indicated that ethnicity (B = −1.59, z = −3.64, p < .001, OR =.20) was a significant predictor of the Low Experience Class compared to the High/Interpersonal Class membership. Being Hispanic decreased the chances of being in the Low Experience Class compared to the High/Interpersonal Class by 80%. In other words, being Hispanic increased the chances of being in the High/Interpersonal Class compared to the Low Experience Class. Further, gender (B = −5.23, z = −1.99, p = .05, OR =.01) was a marginally significant predictor of the Moderate Experience Class compared to the High/Interpersonal Class. Being female decreased the chances of being in the Moderate Experience Class compared to the High/Interpersonal Class by 99%. In other words, being female increased the chances of being in the High/Interpersonal Class compared to the Moderate Experience Class.
Table 4.
Results of multinomial logistic regression analyses for covariates with Class 3 as the reference class.
| Class 1 vs. 3 | Class 2 vs. 3 | |
|---|---|---|
| OR (95% CI) | ||
|
| ||
| Gender | .08 (.30 – 1.96) | .01 (.000003 – .93)p= .05 |
| Age | .99 (.96 – 1.02) | 1.07 (1.00 – 1.15) |
| Race | .99 (.45 – 2.18) | 2.07 (.31 – 14.04) |
| Ethnicity | .20 (.09 – .48)* | .05 (.002 – 1.22) |
Note. Class 1 is Low Experience; Class 2 is Moderate Experience Predominent Threat/Indirect PTEs; Class 3 is High Experience Predominant Interpersonal Trauma;
p < .001;
p < .01;
p < .05.
For the outcome analyses, all classes were compared to each other. Results indicated that primarily the High/Interpersonal Class differed from the other two classes on outcome variables (detailed in Table 5). The High/Interpersonal Class had higher scores on all PTSD symptom clusters, depression, and the lack of perseverance and negative urgency facets of impulsivity compared to the Low Experience Class. Further, the High/Interpersonal Class had higher scores on all PTSD symptom clusters except avoidance, depression, and the lack of perseverance and negative urgency facets of impulsivity compared to the Moderate Experience Class. The Low Experience and Moderate Experience Classes differed only on PTSD’s avoidance and AAR symptom clusters (lower in the former).
Table 5.
Latent class membership differences on outcome variables.
| Class 1a | Class 2b | Class 3c | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Variables | M | SE of M | M | SE of M | M | SE of M | Chi-square | p |
| PTSD intrusions | 7.42<c* | .40 | 8.10<c* | .91 | 12.29 | .54 | 50.63 | <.001 |
| PTSD avoidance | 3.09<c*, <b*** | .19 | 4.19 | .43 | 5.12 | .23 | 42.51 | <.001 |
| PTSD NACM | 9.11<c* | .57 | 9.77<c* | 1.30 | 15.48 | .73 | 45.29 | <.001 |
| PTSD AAR | 7.25<c*, <b*** | .48 | 9.96<c** | 1.09 | 13.41 | .64 | 55.11 | <.001 |
| Depression | 8.03<c* | .49 | 9.40<c** | 1.21 | 13.67 | .67 | 42.29 | <.001 |
| UPPS Lack of Premeditation | 20.82 | .42 | 20.49 | .99 | 22.53 | .73 | 4.49 | .11 |
| UPPS Lack of Perseverance | 19.80<c** | .43 | 19.41<c*** | .99 | 22.01 | .68 | 8.24 | .02 |
| UPPS Sensation Seeking | 28.08 | .64 | 30.14 | 1.41 | 28.92 | .98 | 1.76 | .42 |
| UPPS Negative Urgency | 28.11<c* | .57 | 28.34<c** | 1.61 | 32.64 | .82 | 20.05 | <.001 |
Note. NACM is negative alterations in mood and cognitions; AAR is alterations in arousal and reactivity; Class 1 is Low Experience; Class 2 is Moderate Experience – Predominent Threat/Indirect PTEs; Class 3 is High Experience–Predominant Interpersonal Trauma;
p < .001;
p < .01;
p < .05.
4. Discussion
Most prior research has examined the nature of an index or most distressing trauma on post-trauma mental health. Given that most trauma survivors have a history of multiple PTEs [3], exploring patterns of trauma experiences is essential to further characterizing polytraumatization patterns (subtypes). Thus, the current study examined polytraumatization subtypes and their relation with DSM-5 PTSD symptom clusters, depression, and impulsivity facets.
Consistent with prior research [34, 36, 37], three distinct subgroups of participants emerged. As implied by the class name, the High/Interpersonal Class was characterized by a high probability of experiencing multiple PTE types, with particularly high frequency of interpersonal PTEs (predominantly physical and sexual abuse). Our results indicating the presence of a predominantly interpersonal trauma class is conisstent with existing literature [42]. The second class, Moderate Experience, was characterized by high probability of being threatened by a weapon, repeated exposure to vivid trauma details, and observing someone else killed or injured, all of which were endorsed with greater frequency relative to the High/Interpersonal Class. Predominantly indirect or vicariously experienced PTEs and threat-based PTEs characterized this class, though there was some heterogeneity in this feature as some traumas, like being threatened with a weapon, involved a clear perpetrator. Finally, the Low Experience Class had a lower probability of all PTEs compared to the High/Interpersonal Class and a lower probability of most PTEs compared to the Moderate Experience Class. Thus, results reflect that participants can be meaningfully classified into subgroups based on their history (type and degree) of PTE endorsements.
The obtained class solution demonstrated construct validity. Overall, the High/Interpersonal Class predominantly characterized by interpersonal traumas reported more severe pathology in comparison to other classes. Specifically, the High/Interpersonal Class had higher scores on all DSM-5 PTSD symptom clusters relative to the Low Experience Class, and higher scores on all of the DSM-5 PTSD symptom clusters except avoidance relative to the Moderate Experience Class. Interpersonal traumas, that may begin earlier in life than other traumas [93, 94], are more likely to occur on a repeated basis than indirect traumas [93]; such repeated early-onset traumas are associated with greater PTSD severity relative to single traumas [95, 96]. Further. the intentional and initmate nature of interpersonal traumas may account for their detrimental impact on psychopathology and negative affect [97]. Unsurprisingly, our study findings are consistent with prior research indicating that interpersonal traumas (e.g., sexual assault) are associated with a greater likelihood of PTSD relative to indirect [e.g., learning of the death of a loved one; 98] or non-interpersonal index traumas [e.g., accidents or life-threatening illness; 99], greater arousal [100, 101], greater difficulties with attachment and relationships [102] which is a core NACM symptom, greater avoidance, and greater intrusion symptoms [94]. As with the rest of the trauma literature, prior studies on these topics were conducted based on the type or frequency of an index trauma rather than a profile of PTE experiences, which is unique to the current study.
The High/Interpersonal class reported greater depression severity relative to the Moderate Experience and Low Experience Classes. This finding is consistent with prior research indicating higher rates of depression among sexual assault victims [94]. Furthermore, some studies suggest that multiple traumas result in increasing depression severity for each additional trauma [103]. Additionally, PTSD and depression are highly comorbid [70], which may also explain the similar pattern of findings for PTSD and depression across classes. Thus, the current findings replicate prior work, while simultaneously adding to the literature by examining the influence of polytraumatization patterns on depression.
Finally, the High/Interpersonal Class reported higher scores on two dimensions of impulsivity, namely lack of perserverance (difficulty completing tasks and tendency to become easily bored) and negative urgency (tendency to engage in impulsive behaviors in the context of negative affect) compared to the other classes. Models of learned helplessness suggest that lack of perserverance is associated with repeated uncontrollable traumas [104], perhaps explaining the association between multiple traumas and lack of perserverance in the current study. Negative urgency has been proposed to serve a functional role for trauma-exposed individuals. Engagement in impulsive behaviors may reduce the intensity of negative emotions in the short-term [62–64]. This perhaps explains the association between chronic trauma exposure and substance use disorders and other behaviors of an impulsive nature [105].
There were fewer differences on assessed constructs across the Moderate Experience and Low Experience Classes. AAR scores were higher for the Moderate Experience Class relative to the Low Experience Class, possibly reflective of the dose-response relationship previously reported between between number of traumas and increased aousal [93]. Consistent with prior research on the link between indirect traumatic experiences and avoidance [106], avoidance scores were higher for the Moderate Experience vs. Low Experience Classes. Thus, experience of multiple PTEs overall (and particularly indirectly expereinced PTEs) resulted in a greater tendency toward avoidance of internal and external trauma reminders. As avoidance is conceptualized as a core symptom that maintains PTSD [107], this is a critical point of differentiation between subgroups of trauma survivors.
Among demographic characteristics, ethnicity and gender were significant covariates. Gender emerged as a significant predictor of subgroup membership. Specifically, females were significantly more likely to be classified in the High/Interpersonal vs. the Moderate Experience Class. Thus, when considering multiple PTEs among adults, women are more likely to be categorized in a class reflecting an experience of several PTEs, with a particularly high risk of interpersonal traumas, than men. Our results are consistent with a robust literature, usually conducted within index trauma types alone, suggesting that females are more likely to experience interpersonal traumas compared to men; men are more likely to experience non-interpersonal traumas including witnessing harm, death and injury to others, accidents, nonsexual assualts, and being mugged [108, 109]. In fact, women are more likely than men to experience violence in their romantic relationships, including physical and sexual domestic violence [110], perhaps partially explaining differences in exposure to interpersonal trauma by gender. Possibly, women who experience interpersonal trauma of one type (e.g., sexual assault) are more likely to experience interpersonal traumas of another type (e.g., physical assault), thereby increasing their likelihood of multiple trauma type experiences.
Related to another distinguishing demographic characteristic, Latinos were more likely to be categorized in the High/Interpersonal Class relative to the Low Experience Class, whereas the opposite was true for Non-Latinos. This is consistent with a robust literature suggesting that Latinos in the United States are at high risk for PTE experiences, particularly for those who have recently immigrated from countries with high rates of political violence [111]. Furthermore, prior research suggests that compared to Non-Latino trauma survivors, Latino trauma survivors tend to experience more PTSD symptoms of re-experiencing, fear, guilt, avoidance and numbing [112, 113]. Thus, not only are Latinos more likely to be categorized in the High/Interpersonal Class, they may experience more severe symptom presentations following the experience of a PTE. Given that these aforementioned analyses were exploratory in nature, one could factor in ethnicity as a moderating variable influencing polytraumatization patterns in future analyses.
Some study limitations require consideration. First, the sample was recruited and studied using an online survey, raising potential concerns about the validity of the findings and of the sample [114]. However, the anonymous nature of the online survey may have encouraged reporting of PTEs that may have otherwise gone unreported. Second, participants were aware of the inclusionary criteria including the required endorsement of a stressful life experience prior to study participation. Although we employed some validity checks, the knowledge of inclusionary criteria may have simultaneously increased the validity of the data [we only had participants endorsing PTE(s)] and created the potential to misrepresent information to be included in the study. Third, the study relied on self-report measures of all constructs which could have resulted in response biases. Fourth, while there was a good representation of both males and females in the study, the majority of participants were White, and did not report clinical levels of PTSD severity. Future research should explore these findings in a more diverse sample reporting greater clinical severity. Fifth, we did not collect data on symptom severity in relation to each PTE experienced; this is an area of future research. Finally, we did not assess dissociative symptoms that define the dissociative subtype of PTSD [115]. Future studies may benefit from examining the relation of these dissociative symptoms to lifespan polytraumatization patterns (particularly interpersonal traumas).
In conclusion, the current study results demonstrate that participants can be categorized into three distinct and meaningful subgroups based on lifespan PTE experiences; these subgroups differentially relate to PTSD symptom clusters, depression, and impulsivity facets. Individuals exposed to multiple PTE types, particularly those of an interpersonal nature, may be at the highest risk for severe post-trauma mental health symptoms [42]. Individuals in this class may require more preventive and/or remedial clinical services and allocation of mental health resources [116]. Clinically, a comprehensive assessment of all PTEs and corresponding post-trauma mental health symptoms is critical; such an understanding can help accurately define treatment targets. As an example, individuals experiencing multiple PTEs with predominantly interpersonal traumas may benefit from integrating trauma-focused treatments (targetting PTSD severity) and interventions targetting emotional regulation (targeting negative urgency). PTEs differ in the impact of clinical treatment [117]; and hence future research could explore if polytraumatization patterns are differentially associated with effectiveness of different trauma-focused clinical protocols. Lastly, our study demonstrates the need to use sophisticated person-centered approaches to understand the association between PTE patterns (count and types of PTEs) and post-trauma mental health.
Acknowledgments
The research described here was supported, in part, by grants from the National Institutes of Health (K23DA039327; L30DA038349) awarded to the third co-author.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 2.Kilpatrick DG, Resnick HS, Acierno R. Should PTSD criterion A be retained? Journal of Traumatic Stress. 2009;22:374–83. doi: 10.1002/jts.20436. [DOI] [PubMed] [Google Scholar]
- 3.Gustafsson PE, Nilsson D, Svedin CG. Polytraumatization and psychological symptoms in children and adolescents. European Child & Adolescent Psychiatry. 2009;18:274–83. doi: 10.1007/s00787-008-0728-2. [DOI] [PubMed] [Google Scholar]
- 4.Cougle JR, Kilpatrick DG, Heidi SRHS. Defining Traumatic Events: Research Findings and Controversies. Oxford University Press; 2012. [Google Scholar]
- 5.Scott-Storey K. Cumulative abuse: Do things add up? An evaluation of the conceptualization, operationalization, and methodological approaches in the study of the phenomenon of cumulative abuse. Trauma Violence Abuse. 2011:1–16. doi: 10.1177/1524838011404253. [DOI] [PubMed] [Google Scholar]
- 6.Nurius PS, Macy RJ. Heterogeneity among violence-exposed women applying person-oriented research methods. Journal of Interpersonal Violence. 2008;23:389–415. doi: 10.1177/0886260507312297. [DOI] [PubMed] [Google Scholar]
- 7.Carlson EB, Smith SR, Palmieri PA, Dalenberg C, Ruzek JI, Kimerling R, et al. Development and validation of a brief self-report measure of trauma exposure: the Trauma History Screen. Psychological Assessment. 2011;23:463–77. doi: 10.1037/a0022294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Higgins DJ, McCabe MP. Multiple forms of child abuse and neglect: Adult retrospective reports. Aggression and Violent Behavior. 2001;6:547–78. [Google Scholar]
- 9.Finkelhor D, Ormrod RK, Turner H. Polyvictimization and trauma in a national longitudinal cohort. Development and Psychopathology. 2007;19:149–66. doi: 10.1017/S0954579407070083. [DOI] [PubMed] [Google Scholar]
- 10.Agorastos A, Pittman JO, Angkaw AC, Nievergelt CM, Hansen CJ, Aversa LH, et al. The cumulative effect of different childhood trauma types on self-reported symptoms of adult male depression and PTSD, substance abuse and health-related quality of life in a large active-duty military cohort. Journal of Psychiatric Research. 2014;58:46–54. doi: 10.1016/j.jpsychires.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 11.Contractor AA, Caldas S, Fletcher S, Shea MT, Armour C. Empirically-derived lifespan polytraumatization typologies: A systematic review. doi: 10.1002/jclp.22586. Manuscipt submitted for publication. in review. [DOI] [PubMed] [Google Scholar]
- 12.Monroe SM, Harkness KL. ife stress, the" kindling" hypothesis, and the recurrence of depression: considerations from a life stress perspective. Psychological Review. 2007;112:417–45. doi: 10.1037/0033-295X.112.2.417. [DOI] [PubMed] [Google Scholar]
- 13.McFarlane AC. The longterm costs of traumatic stress: intertwined physical and psychological consequences. World Psychiatry. 2010;9:3–10. doi: 10.1002/j.2051-5545.2010.tb00254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu H, Petukhova MV, Sampson NA, Aguilar-Gaxiola S, Alonso J, Andrade LH, et al. Association of DSM-IV posttraumatic stress disorder with traumatic experience type and history in the World Health Organization world mental health surveys. JAMA Psychiatry. 2017;74:270–81. doi: 10.1001/jamapsychiatry.2016.3783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Santiago PN, Ursano RJ, Gray CL, Pynoos RS, Spiegel D, Lewis-Fernandez R, et al. A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: Intentional and non-intentional traumatic events. PLOS ONE. 2013;8:e59236. doi: 10.1371/journal.pone.0059236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Archives of General Psychiatry. 1998;55:626–32. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- 17.Wanklyn SG, Pukay-Martin ND, Belus JM, St Cyr K, Girard TA, Monson CM. Trauma types as differential predictors of posttraumatic stress disorder (PTSD), major depressive isorder (MDD), and their comorbidity. Canadian Journal of Behavioural Science. 2016 [Google Scholar]
- 18.Graham J, Legarreta M, North L, DiMuzio J, McGlade E, Yurgelun-Tod D. A preliminary study of DSM–5 PTSD symptom patterns in Veterans by trauma type. Military Psychology. 2016;28:115–22. [Google Scholar]
- 19.Smith HL, Summers BJ, Dillon KH, Cougle JR. Is worst-event trauma type related to PTSD symptom presentationand associated features? Journal of Anxiety Disorders. 2016;38:55–61. doi: 10.1016/j.janxdis.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 20.Turner RJ, LLoyd DA. Lifetime traumas and mental health: The significance of cumulative adversity. Journal of Health and Social Behavior. 1995;36:360–75. [PubMed] [Google Scholar]
- 21.Adams ZW, Moreland A, Cohen JR, Lee RC, Hanson RF, Danielson CK, et al. Polyvictimization: Latent profiles and mental health outcomes in a clinical sample of adolescents. Psychology of Violence. 2016;6:145–55. doi: 10.1037/a0039713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Post RM, Weiss SR. Sensitization and kindling phenomena in mood, anxiety, and obsessive–compulsive disorders: the role of serotonergic mechanisms in illness progression. Biological Psychiatry. 1998;44:193–206. doi: 10.1016/s0006-3223(98)00144-9. [DOI] [PubMed] [Google Scholar]
- 23.Schumm JA, Stines LR, Hobfoll SE, Jackson AP. The double-barreled burden of child abuse and current stressful circumstances on adult women. Journal of Traumatic Stress. 2005;18:467–76. doi: 10.1002/jts.20054. [DOI] [PubMed] [Google Scholar]
- 24.Briere J, Kaltman S, Green BL. Accumulated childhood trauma and symptom complexity. Journal of Traumatic Stress. 2008;21:223–6. doi: 10.1002/jts.20317. [DOI] [PubMed] [Google Scholar]
- 25.Cloitre M, Stolbach BC, Herman JL, Kolk BVD, Pynoos R, Wang J, et al. A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress. 2009;22:399–408. doi: 10.1002/jts.20444. [DOI] [PubMed] [Google Scholar]
- 26.Putnam KT, Harris WW, Putnam FW. Synergistic childhood adversities and complex adult psychopathology. Journal of Traumatic Stress. 2013;26:435–42. doi: 10.1002/jts.21833. [DOI] [PubMed] [Google Scholar]
- 27.Schauer M, Neuner F, Karunakara U, Klaschik C, Robert C, Elbert T. PTSD and the building block effect of psychological trauma among West Nile Africans. European Society for Traumatic Stress Studies Bulletin. 2003;10:5–6. [Google Scholar]
- 28.Kolassa IT, Ertl V, Eckart C, Kolassa S, Onyut LP, Elbert T. Spontaneous remission from PTSD depends on the number of traumatic event types experienced. Psychological Trauma Theory Research Practice and Policy. 2010;2:169–74. [Google Scholar]
- 29.Norris FH. Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. Journal of Consulting and Clinical Psychology. 1992;60:409–18. doi: 10.1037//0022-006x.60.3.409. [DOI] [PubMed] [Google Scholar]
- 30.Herman JL. Trauma and recovery: The aftermath of violence from domestic violence to political terrorism. New York, NY: Guilford Press; 1992. [Google Scholar]
- 31.Cloitre M, Courtois CA, Charuvastra A, Carapezza R, Stolbach BC, Green BL. Treatment of complex PTSD: Results of the ISTSS expert clinician survey on best practices. Journal of Traumatic Stress. 2011;24:615–27. doi: 10.1002/jts.20697. [DOI] [PubMed] [Google Scholar]
- 32.Follette VM, Polusny MA, Bechtle AE, Naugle AE. Cumulative trauma: The impact of child sexual abuse, adult sexual assault, and spouse abuse. Journal of Traumatic Stress. 1996;9:25–35. doi: 10.1007/BF02116831. [DOI] [PubMed] [Google Scholar]
- 33.Kira IA, Ashby JS, Lewandowski L, Alawneh AWN, Mohanesh J, Odenat L. Advances in continuous traumatic stress theory: Traumatogenic dynamics and consequences of intergroup conflict: The Palestinian adolescents case. Psychology. 2013;40:396–409. [Google Scholar]
- 34.Golder S, Connell CM, Sullivan TP. Psychological distress and substance use among community-recruited women currently victimized by intimate partners A latent class analysis and examination of between-class differences. Violence Against Women. 2012;18:934–57. doi: 10.1177/1077801212456991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Armour C, Elklit A, Christoffersen MN. A latent class analysis of childhood maltreatment: Identifying abuse typologies. Journal of Loss and Trauma. 2014;19:23–39. [Google Scholar]
- 36.Armour C, Sleath E. Assessing the co-occurrence of intimate partner violence domains across the life-course: Relating typologies to mental health. European Journal of Psychotraumatology. 2014:5. doi: 10.3402/ejpt.v5.24620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cavanaugh CE, Martins SS, Petras H, Campbell JC. Mental disorders associated with subpopulations of women affected by violence and abuse. Journal of Traumatic Stress. 2013;26:459–66. doi: 10.1002/jts.21821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sullivan E, Contractor AA, Gerber M, Neumann C. Examination of polytrauma typologies: A latent class analysis approach. Psychiatry Research. 2017;255:111–8. doi: 10.1016/j.psychres.2017.05.026. [DOI] [PubMed] [Google Scholar]
- 39.Burns CR, Lagdon S, Boyda D, Armour C. Interpersonal polyvictimization and mental health in males. Journal of Anxiety Disorders. 2016;40:75–82. doi: 10.1016/j.janxdis.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 40.Holt MK, Felix E, Grimm R, Nylund-Gibson K, Green JG, Poteat VP, et al. A Latent Class Analysis of Past Victimization Exposures as Predictors of College Mental Health. Psychology of Violence. 2016 [Google Scholar]
- 41.Walsh JL, Senn TE, Carey MP. Exposure to different types of violence and subsequent sexual risk behavior among female sexually transmitted disease clinic patients: A latent class analysis. Psychology of Violence. 2012;2:339–54. doi: 10.1037/a0027716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O'Donnell ML, Schaefer I, Varker T, Kartel D, Forbes D, Bryant RA, et al. A systematic review of person-centered approaches to investigating patterns of trauma exposure. Clinical Psychological Review. 2017;57:208–55. doi: 10.1016/j.cpr.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 43.Galatzer-Levy IR, Bryant RA. 636,120 ways to have posttraumatic stress disorder. Perspectives on Psychological Science. 2013;8:651–62. doi: 10.1177/1745691613504115. [DOI] [PubMed] [Google Scholar]
- 44.Contractor AA, Armour C, Forbes D, Elhai JD. PTSD’s underlying dimensions and their relation with impulsivity facets. The Journal of Nervous & Mental Disease. 2016;204:20–5. doi: 10.1097/NMD.0000000000000417. [DOI] [PubMed] [Google Scholar]
- 45.Contractor AA, Durham TA, Brennan JA, Armour C, Wutrick HR, Frueh CB, et al. DSM-5 PTSD’s symptom dimensions and relations with major depression’s symptom dimensions in a primary care sample. Psychiatry Research. 2014;215:146–53. doi: 10.1016/j.psychres.2013.10.015. [DOI] [PubMed] [Google Scholar]
- 46.Armour C, Contractor AA, Shea MT, Elhai JD, Pietrzak RH. Factor structure of the PCL-5: relationships among symptom clusters, anger, and impulsivity. Journal of Nervous & Mental Disease. 2016;204:108–15. doi: 10.1097/NMD.0000000000000430. [DOI] [PubMed] [Google Scholar]
- 47.Whiteside SP, Lynam DR. The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30:669–89. [Google Scholar]
- 48.Corstorphine E, Waller G, Lawson R, Ganis C. Trauma and multi-impulsivity in the eating disorders. Eating Behaviors. 2007;8:23–30. doi: 10.1016/j.eatbeh.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 49.Brodsky BS, Oquendo M, Ellis SP, Haas GL, Malone KM, Mann JJ. The relationship of childhood abuse to impulsivity and suicidal behavior in adults with major depression. American Journal of Psychiatry. 2001;158:1871–7. doi: 10.1176/appi.ajp.158.11.1871. [DOI] [PubMed] [Google Scholar]
- 50.Zlotnick C, Shea MT, Recupero P, Bidadi K, Pearlstein T, Brown P. Trauma, dissociation, impulsivity, and self-mutilation among substance abuse patients. American Journal of Orthopsychiatry. 1997;67:650–4. doi: 10.1037/h0080263. [DOI] [PubMed] [Google Scholar]
- 51.Khoury L, Tang YL, Bradley B, Cubells JF, Ressler KJ. Substance use, childhood traumatic experience, and posttraumatic stress disorder in an urban civilian population. Depression and Anxiety. 2010;27:1077–86. doi: 10.1002/da.20751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Breslau N. The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma Violence Abuse. 2009;10:198–210. doi: 10.1177/1524838009334448. [DOI] [PubMed] [Google Scholar]
- 53.Orth U, Wieland E. Anger, hostility, and posttraumatic stress disorder in trauma-exposed adults: A meta-analysis. Journal of Consulting and Clinical Psychology. 2006;74:698–706. doi: 10.1037/0022-006X.74.4.698. [DOI] [PubMed] [Google Scholar]
- 54.McCutcheon VV, Sartor CE, Pommer NE, Bucholz KK, Nelson EC, Madden PA, et al. Age at trauma exposure and PTSD risk in young adult women. Journal of Traumatic Stress. 2010;23:811–4. doi: 10.1002/jts.20577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tolin DF, Breslau N. Sex differences in risk of PTSD. PTSD Research Quarterly. 2007:18. [Google Scholar]
- 56.Dohrenwend BP, Dohrenwend BS. Social Status and Psychological Disorder: A Causal Inquiry. New York, NY: Wiley; 1969. [Google Scholar]
- 57.Ghafoori B, Barragan B, Tohidian N, Palinkas L. Racial and ethnic differences in symptom severity of PTSD, GAD, and depression in trauma-exposed, urban, treatment-seeking adults. Journal of Traumatic Stress. 2012;25:106–10. doi: 10.1002/jts.21663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Milan S, Zona K, Acker J, Turcios-Cotto V. Prospective risk factors for adolescent PTSD: Sources of differential exposure and differential vulnerability. Journal of Abnormal Child Psychology. 2013;41:339–53. doi: 10.1007/s10802-012-9677-9. [DOI] [PubMed] [Google Scholar]
- 59.Magruder KM, Frueh BC, Knapp RG, Johnson MR, Vaughan JA, Carson TC, et al. PTSD symptoms, demographic characteristics, and functional status among veterans treated in VA primary care clinics. Journal of Traumatic Stress. 2004;17:293–301. doi: 10.1023/B:JOTS.0000038477.47249.c8. [DOI] [PubMed] [Google Scholar]
- 60.Brewin CR, Holmes EA. Psychological theories of posttraumatic stress disorder. Clinical Psychology Review. 2003;23:339–76. doi: 10.1016/s0272-7358(03)00033-3. [DOI] [PubMed] [Google Scholar]
- 61.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity survey. Archives of General Psychiatry. 1995;52:1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 62.Marshall-Berenz EC, Vujanovic AA, MacPherson L. Impulsivity and alcohol use coping motives in a trauma-exposed sample: The mediating role of distress tolerance. Personality and Individual Differences. 2011;50:588–92. doi: 10.1016/j.paid.2010.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Weiss NH, Tull MT, Sullivan TP, Dixon-Gordon KL, Gratz KL. Posttraumatic stress disorder symptoms and risky behaviors among trauma-exposed inpatients with substance dependence: The influence of negative and positive urgency. Drug and Alcohol Dependence. 2015;155:147–53. doi: 10.1016/j.drugalcdep.2015.07.679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Weiss NH, Tull MT, Viana AG, Anestis MD, Gratz KL. Impulsive behaviors as an emotion regulation strategy: Examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders. 2012;26:453–8. doi: 10.1016/j.janxdis.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ben-Zur H, Zeidner M. Threat to life and risk-taking behaviors: A review of empirical findings and explanatory models. Personality and Social Psychology Review. 2009;13:109–28. doi: 10.1177/1088868308330104. [DOI] [PubMed] [Google Scholar]
- 66.Roberts JA, Pullig C, Manolis C. I need my smartphone: A hierarchical model of personality and cell-phone addiction. Personality and Individual Differences. 2015;79:13–9. [Google Scholar]
- 67.Billieux J. Problematic use of the mobile phone: a literature review and a pathways model. Current Psychiatry Reviews. 2012;8:299–307. [Google Scholar]
- 68.Wu AM, Cheung VI, Ku L, Hung EP. Psychological risk factors of addiction to social networking sites among Chinese smartphone users. Journal of Behavioral Addictions. 2013;2:160–6. doi: 10.1556/JBA.2.2013.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bonde JP, Utzon-Frank N, Bertelsen M, Borritz M, Eller NH, Nordentoft M. Risk of depressive disorder following disasters and military deployment: systematic review with meta-analysis. The British Journal of Psychiatry. 2016;208:330–6. doi: 10.1192/bjp.bp.114.157859. [DOI] [PubMed] [Google Scholar]
- 70.Rytwinski NK, Scur MD, Feeny NC, Youngstrom EA. The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: A meta-analysis. Journal of Traumatic Stress. 2013;26:299–309. doi: 10.1002/jts.21814. [DOI] [PubMed] [Google Scholar]
- 71.Strander VA, Thomsen CJ, Highfill-McRoy RM. Etiology of depression comorbidity in combat-related PTSD: A review of the literature. Clinical Psychology Review. 2014;34:87–98. doi: 10.1016/j.cpr.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 72.Spitzer RL, First MB, Wakefield JC. Saving PTSD from itself in DSM-V. Journal of Anxiety Disorders. 2007;21:233–41. doi: 10.1016/j.janxdis.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 73.Young-Wolff KC, Hellmuth J, Jaquier V, Swan SC, Connell C, Sullivan TP. Patterns of resource utilization and mental health symptoms among women exposed to multiple types of victimization: a latent class analysis. Journal of Interpersonal Violence. 2013;28:3059–83. doi: 10.1177/0886260513488692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Buhrmester M, Kwang T, Gosling SD. Amazon's Mechanical Turk a new source of inexpensive, yet high-quality, data? Perspectives on Psychological Science. 2011;6:3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- 75.Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) Scale available from the National Center for PTSD. 2013 at www.ptsd.va.gov.
- 76.Muthén LK, Muthén BO. Mplus user's guide. 5. Los Angeles, CA: Muthén & Muthén; 1998–2007. [Google Scholar]
- 77.Goodman LA, Corcoran C, Turner K, Yuan N, Green BL. Assessing traumatic event exposure: General issues and preliminary findings for the Stressful Life Events Screening Questionnaire. Journal of Traumatic Stress. 1998;11:521–42. doi: 10.1023/A:1024456713321. [DOI] [PubMed] [Google Scholar]
- 78.Elhai JD, Miller ME, Ford JD, Biehn TL, Palmieri PA, Frueh BC. Posttraumatic stress disorder in DSM-5: Estimates of prevalence and symptom structure in a nonclinical sample of college students. Journal of Anxiety Disorders. 2012;26:58–64. doi: 10.1016/j.janxdis.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 79.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress. 2015;28:489–98. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- 80.Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, et al. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment. 2016;28:1379–91. doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- 81.Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, et al. Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment. 2016;28:1392–403. doi: 10.1037/pas0000260. [DOI] [PubMed] [Google Scholar]
- 82.Whiteside SP, Lynam DR, Miller JD, Reynolds SK. Validation of the UPPS Impulsive Behavior Scale: A four-factor model of impulsivity. European Journal of Personality. 2005;19:559–74. [Google Scholar]
- 83.Smith GT, Fischer S, Cyders MA, Annus AM, Spillane NS, McCarthy DM. On the validity and utility of discriminating among impulsivity-like traits. Assessment. 2007;14:155–70. doi: 10.1177/1073191106295527. [DOI] [PubMed] [Google Scholar]
- 84.Kroenke K, Spitzer RL, Williams JBW. The PHQ 9 validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nylund K, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A monte carlo simulation study. Structural Equation Modeling. 2007;14:535–69. [Google Scholar]
- 86.Nylund K, Bellmore A, Nishina A, Graham S. Subtypes, severity, and structural stability of peer victimization: What does latent class analysis say? Child Development. 2007;78:1706–22. doi: 10.1111/j.1467-8624.2007.01097.x. [DOI] [PubMed] [Google Scholar]
- 87.DiStefano C, Kamphaus RW. Investigating subtypes of child development: A comparison of cluster analysis and latent class cluster analysis in typology creation. Educational and Psychological Measurement. 2006;66:778–94. [Google Scholar]
- 88.Raftery AE. Bayesian model selection in social research. Sociological Methodology. 1995;25:111–63. [Google Scholar]
- 89.Asparouhov T, Muthén B. Auxiliary variables in mixture modeling: Three-step approaches using Mplus. Structural Equation Modeling: A Multidisciplinary Journal. 2014;21:1–13. [Google Scholar]
- 90.Vermunt JK. Latent class modeling with covariates: Two improved three-step approaches. Political Analysis. 2010;18:450–69. [Google Scholar]
- 91.D’Andrea W, Ford J, Stolbach B, Spinazzola J, van der Kolk BA. Understanding interpersonal trauma in children: Why we need a developmentally appropriate trauma diagnosis. American Journal of Orthopsychiatry. 2012;82:187–200. doi: 10.1111/j.1939-0025.2012.01154.x. [DOI] [PubMed] [Google Scholar]
- 92.Pynoos RS, Fairbank JA, Steinberg AM, Amaya-Jackson L, Gerrity E, Mount M, et al. The National Child Traumatic Stress Network: Collaborating to improve the standard of care. Professional Psychology: Research and Practice. 2008;39:389–95. [Google Scholar]
- 93.Matlow RB, DePrince AP. The influence of victimization history on PTSD symptom expression in women exposed to intimate partner violence. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5:241–50. [Google Scholar]
- 94.Dworkin ER, Mota NP, Schumacher JA, Vinci C, Coffey SF. The unique associations of sexual assault and intimate partner violence with PTSD symptom clusters in a traumatized substance-abusing sample. Psychological Trauma: Theory, Research, Practice, and Policy. 2017;9:500–8. doi: 10.1037/tra0000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Avant EM, Swopes RM, Davis JL, Elhai JD. Psychological Abuse and Posttraumatic Stress Symptoms in College Students. Journal of Interpersonal Violence. 2011;26:3080–97. doi: 10.1177/0886260510390954. [DOI] [PubMed] [Google Scholar]
- 96.Green BL, Goodman LA, Krupnick JL, Corcoran CB, Petty RM, Stockton P, et al. Outcomes of Single Versus Multiple Trauma Exposure in a Screening Sample. Journal of Traumatic Stress. 2000;13:271–86. doi: 10.1023/A:1007758711939. [DOI] [PubMed] [Google Scholar]
- 97.Hart T, Hanks R, Bogner JA, Millis S, Esselman P. Blame attribution in intentional and unintentional traumatic brain injury: Longitudinal changes and impact on subjective well-being. Rehabilitation psychology. 2007;52:152. [Google Scholar]
- 98.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Medical comorbidity of full and partial posttraumatic stress disorder in US adults: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosomatic medicine. 2011;73:697–707. doi: 10.1097/PSY.0b013e3182303775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Green BL, Goodman LA, Krupnick JL, Corcoran CB, Petty RM, Stockton P, et al. Outcomes of single versus multiple trauma exposure in a screening sample. Journal of Traumatic Stress. 2000;13:271–86. doi: 10.1023/A:1007758711939. [DOI] [PubMed] [Google Scholar]
- 100.Griffing S, Lewis CS, Chu M, Sage RE, Madry L, Primm BJ. Exposure to interpersonal violence as a predictor of PTSD symptomatology in domestic violence survivors. Journal of Interpersonal Violence. 2006;21:936–54. doi: 10.1177/0886260506288938. [DOI] [PubMed] [Google Scholar]
- 101.Orr SP, Lasko NB, Metzger LJ, Berry NJ, Ahern CE, Pitman RK. Psychophysiologic assessment of women with posttraumatic stress disorder resulting from childhood sexual abuse. Journal of Consulting and Clinical Psychology. 1998;66:906–13. doi: 10.1037//0022-006x.66.6.906. [DOI] [PubMed] [Google Scholar]
- 102.Lahav Y, Elklit A. The cycle of healing - dissociation and attachment during treatment of CSA survivors. Child abuse & neglect. 2016;60:67–76. doi: 10.1016/j.chiabu.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 103.Suliman S, Mkabile SG, Fincham DS, Ahmed R, Stein DJ, Seedat S. Cumulative effect of multiple trauma on symptoms of posttraumatic stress disorder, anxiety, and depression in adolescents. Comprehensive Psychiatry. 2009;50:121–7. doi: 10.1016/j.comppsych.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 104.Overmier JB, Seligman ME. Effects of inescapable shock upon subsequent escape and avoidance responding. Journal of Comparative and Physiological Psychology. 1967;63:28–33. doi: 10.1037/h0024166. [DOI] [PubMed] [Google Scholar]
- 105.Kaufman TML, Baams L, Dubas JS. Microaggressions and depressive symptoms in sexual minority youth: The roles of rumination and social support. US: Educational Publishing Foundation; 2017. pp. 184–92. [Google Scholar]
- 106.Sheen K, Slade P, Spiby H. An integrative review of the impact of indirect trauma exposure in health professionals and potential issues of salience for midwives. Journal of Advanced Nursing. 2014;70:729–43. doi: 10.1111/jan.12274. [DOI] [PubMed] [Google Scholar]
- 107.Pineles SL, Mostoufi SM, Ready CB, Street AE, Griffin MG, Resik PA. Trauma reactivity, avoidant coping and PTSD symptoms: A moderating relationship? Journal of Abnormal Psychology. 2011;120:240–6. doi: 10.1037/a0022123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin. 2006;132:959–92. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- 109.Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, et al. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychological Medicine. 2015;46:327–43. doi: 10.1017/S0033291715001981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tjaden P, Thoennes N. Prevalence and Consequences of Male-to-female and Female-to-male Intimate Partner Violence as Measured by the National Violence Against Women Survey. Violence Against Women. 2000;6:142–61. [Google Scholar]
- 111.Eisenman DP, Gelberg L, Liu H, Shapiro MF. Mental health and health-related quality of life among adult Latino primary care patients living in the United States with previous exposure to political violence. Jama. 2003;290:627–34. doi: 10.1001/jama.290.5.627. [DOI] [PubMed] [Google Scholar]
- 112.Hall-Clark BN, Kaczkurkin AN, Asnaani A, Zhong J, Peterson AL, Yarvis JS, et al. Psychological Trauma Theory Research Practice and Policy. 2017. Ethnoracial Differences in PTSD Symptoms and Trauma-Related Cognitions in Treatment-Seeking Active Duty Military Personnel for PTSD. [DOI] [PubMed] [Google Scholar]
- 113.Alcántara C, Casement MD, Lewis-Fernández R. Conditional risk for PTSD among Latinos: A systematic review of racial/ethnic differences and sociocultural explanations. Clinical Psychology Review. 2013;33:107–19. doi: 10.1016/j.cpr.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wright KB. Researching internet-based populations: Advantages and disadvantages of online survey research, online questionnaire authoring software packages, and web survey services. Journal of Computer-Mediated Communication. 2005:10. [Google Scholar]
- 115.Wolf EJ, Miller MW, Reardon AF, Ryabchenko KA, Castillo D, Freund R. A Latent Class Analysis of dissociation and posttraumatic stress disorder. Evidence for a dissociative subtype. Archives of General Psychiatry. 2012;7:698–705. doi: 10.1001/archgenpsychiatry.2011.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Grasso DJ, Dierkhising CB, Branson CE, Ford JD, Lee R. Developmental patterns of adverse childhood experiences and current symptoms and impairment in youth referred for trauma-specific services. Journal of Abnormal Child Psychology. 2016;44:871–86. doi: 10.1007/s10802-015-0086-8. [DOI] [PubMed] [Google Scholar]
- 117.Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of psychiatry. 2005;162:214–27. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- 118.Green B. Trauma History Questionnaire. In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Lutherville, MD: Sidran Press; 1996. pp. 366–9. [Google Scholar]