Porphyrins and 64Cu have emerged as a novel synergic option for applications in PET molecular imaging.
Porphyrins and 64Cu have emerged as a novel synergic option for applications in PET molecular imaging.
Abstract
Porphyrins and 64Cu have emerged as a novel synergic option for applications in PET molecular imaging. Both the characteristics and photophysical properties of macrocyclic porphyrins and the relatively long half-life of the copper isotope, in addition to the increased tumor-specific uptake of porphyrins compared to normal cells, make this complex an attractive option not only for diagnosis but also for therapeutic applications. Herein, we present an overview of the latest results on the development of PET agents based on porphyrins and 64Cu, including methods used to improve the selectivity of these macrocycles when conjugated with biological units such as monoclonal antibodies, peptides or proteins.
1. Introduction
The use of porphyrins in medical applications has captured the attention of the scientific community since they have shown great advantages over other common methods used in the diagnosis and treatment of diseases. It is well known that typical cancer therapies (chemotherapy, surgery and radiation therapy) could generate extensive damage to patients. The way in which porphyrins act on biological tissues relies on singlet oxygen generation, which is the main key in the cytotoxic role of these agents. In the diagnosis field, these macrocyclic compounds could be a great choice due to their ability to form stable complexes with several metallic species including copper, gallium, zinc, technetium, and palladium, among other radionuclides that are used in nuclear medicine.1–3 The advantage of using porphyrins is not just because of the complex's stability, but also due to its easy modification, either before or after the macrocycle formation, by adding biological moieties or other species of pharmacological interest.4
Another interesting point on the use of porphyrins as probes relies on the photophysical properties of these macrocycles to generate, as mentioned before, singlet oxygen. These species have found applications in multiple fields including organic synthesis,5 wastewater treatment,6,7 sterilization processes,8 and medicine, especially in photodynamic therapy (PDT).9,10 The use of photosensitized dyes like porphyrins has captured the attention of the scientific community mainly due to their minimum secondary effects compared with conventional therapies.9
2. Porphyrins
2.1. Synthetic methods
The word porphyrin is derived from the Greek word porphyria, meaning “purple”, as these systems exhibit intense absorption in the UV and visible (UV-vis) region given their highly conjugated structures. Porphyrins are macrocyclic systems made by condensation of the pyrrole ring and aldehyde units conjugated by methane bridges; as a result, the final structure of porphyrin systems bears a highly conjugated structure.
The first experiments for porphyrin synthesis were conducted by Rothemund,11,12 who in the 1930s reacted pyrrole and formaldehyde under reflux at 90–95 °C in an inert atmosphere for thirty hours. Then the mixture was cooled and extracted with pyridine and, after the purification process, the yield was 1 mg of porphyrin for each pyrrole gram. The final product was soluble in pyridine and chloroform and slightly soluble in ether and methanol. The extreme synthesis conditions make this method unfavorable for employing sensitive aldehydes, and given its poor yield, industrial applications of this methodology are not economically viable.
Later on during the 1960s, Adler and Longo used the same starting materials (pyrrole and benzaldehyde) under propionic acid reflux at 141 °C;13 they observed that under these conditions, it was possible to use a wider selection of substituted aldehydes, which increased the synthesis yield to 20%.14 The main problem that this methodology faces is that it is unfavorable with aldehydes that bear sensitive groups; another drawback was the level of impurities, making the purification process difficult, mainly with porphyrins that could not precipitate or crystallize, without mentioning the poor reproducibility.
More recently in the 1980s, the strategy reported by Lindsey et al.,15 using chloroform or dichloromethane, acid catalysis (CF3COOH or BF3OEt2) and oxidant media (DDQ or p-chloranil), was found to be more reliable and reproducible. The advantages of this methodology come from its relatively mild conditions, making it possible to use a broad variety of aldehydes, easy purification process, and relatively high yield (30–40%).
2.2. Photochemical behavior
Porphyrins bear 26 π delocalized electrons responsible of their optical, electronic, magnetic and redox characteristics. These features can be easily modulated by changing the structure of the aldehyde or by adding metals at the macrocyclic center, which have captured the attention of several research groups. Due to their high number of delocalized electrons, porphyrins can absorb several wavelengths in the UV-vis region, showing a well-defined spectrum composed of two bands: the first one is denoted as the Soret band located between 400–500 nm, which is attributed to the S0 → S2 transition; the second group of bands is named Q-bands (four bands in free base porphyrins) located between 500–700 nm, attributed to the S0 → S1 transition. In the case of metallated porphyrins, the four Q-bands turned into two bands due to the increase of symmetry in the macrocycle. Porphyrins can also absorb photons resulting in photo-excited states, which have a relatively long lifetime; as a consequence of this absorption, they exhibit strong fluorescence maxima located at 600–800 nm due to S1 → S0 transitions and the quantum yield rises by 10%.16
2.3. Porphyrins as singlet oxygen generators and their applications in PDT
Singlet oxygen was first described by Khan and Kasha in 1963; they interpreted the chemiluminescence generated by the reaction of hypochlorite–peroxide to be due to singlet oxygen generation.17
The electronic structure of oxygen is composed of a ground state 3∑–g (spin triplet) and two lowest-energy excited electronic states (singlet excited states), 1Δg and 1∑+g, with energy states of 95 and 158 kJ, respectively.18 Singlet species have different stabilities that are based on their aqueous lifetimes which are 10–6–10–3 s for 1Δg, and 10–11–10–9 s for 1∑+g, correspondingly.19 Although these species are named singlet, their reactivity is not the same; while 1∑+g has a higher energy and is not known to react with other molecules,20,21 1Δg has a different behavior, as this species is the one known as “singlet oxygen”.22,23
The mechanism by which photosensitized molecules generate singlet oxygen has been well described24–26 and follows the following steps: once the photosensitizer absorbs photons, transition between the ground state (S0) to the singlet excited state (Sn) yields a lowest excited singlet state (S1), which through intersystem crossing generates a triplet state (T1). This species is capable of reacting in two ways: type I and type II mechanisms (Fig. 1).
Fig. 1. Singlet oxygen diagram generation. Figure adapted from ref. 19.
The type I mechanism involves free radicals, which are derived from electron transfer or hydrogen-atom abstraction between the sensitizer and other organic molecules (eqn (1)). Once these radicals are generated, they can react with oxygen, which creates a superoxide radical anion. In the type II mechanism, singlet oxygen is generated by the energy transfer from the photosensitizer (in the triplet state) to the oxygen molecule (eqn (2)). Before degradation by photobleaching, each photosensitizer molecule can generate 103–105 molecules of singlet oxygen.
 |
1 |
 |
2 |
An important characteristic of singlet oxygen lies on its lifetime and capability to react with several molecules, among them are biomolecules (unsaturated lipids and α-amino-acid residues), and its capability to diffuse (45 nm),27 making it possible to diffuse across a single cell length.
Several porphyrin analogues have been developed for PDT; among them, HPPH (Fig. 2) has been demonstrated to have excellent results and limited skin phototoxicity.1,28,29 The clinical trials of HPPH have shown its efficacy against lung, esophagus, head and neck cancer.30–32
Fig. 2. 2-(1-Hexyloxyethyl)-2-devinyl pyropheophorbide-a, brand name Photochlor.

2.4. Porphyrins as chelating agents
Porphyrins bear a vacant center, which is an ideal site to host different metallic cations.33–35 It is well known that porphyrins act as tetradentate ligands, making it possible to coordinate species that have a minimum coordination number of 4; higher coordination numbers are possible through ligands that can be either neutral or anionic.36 In the case of divalent metals like Zn2+, Mg2+, Cu2+, Fe2+, Co2+ and Ni2+, it is possible to obtain electronically neutral compounds. The structure of these complexes could be either square-planar or octahedral. For trivalent metals like Fe3+ and Mn3+, an anionic axial ligand is necessary to form an electrically neutral complex, whose geometry could be pentacoordinate square-pyramidal or hexacoordinate complexes. In the case of an eight-coordinate species, it forms a sandwich compound that has a square antiprism geometry.37 Structurally, the interaction between metals and porphyrin has been well established and it is formed by two main types of interactions: σ-interaction is established by the nitrogen lone pairs directed to the center of the macrocycle, and π-interaction is made by pπ and/or dπ with nitrogen pπ orbitals.38
Since the conditions to incorporate a metal center into the porphyrin core are quite facile, and given that the photophysical properties of these metallated compounds change, compared with the free base porphyrin, several types of metalloporphyrins have been developed and have applications in fields such as catalysis,39,40 dye sensitized solar cells (DSSCs),41 and sensors,42 and in the development of novel drugs.43
3. Metallic radionuclides
Given the short half-life of traditional PET isotopes (11C, 13N, 15O and 18F), they are only useful to investigate some biological processes that happen in short times.44 Although these radioisotopes are the most commonly used, it is necessary to produce other radionuclides with a longer half-life that better match the biokinetics of new molecules like proteins, peptides, antibodies and nanoparticles, which are biological targets of interest. There is a broad variety of metallic radionuclides that meet this characteristic, including isotopes of zirconium, yttrium, indium, gallium, cobalt, and copper, some of them listed in Table 1, which have the potential to be used in the development of new agents in the field of radiopharmaceutical research.45–49
Table 1. Main characteristics of metallic radionuclides.
| Radionuclide | Half-life (h) | Production | Decay mode | E β + max (keV) |
| 60Cu | 0.4 | Cyclotron | β+ (92.5%) | 3920 |
| 60Ni(p,n)60Cu | EC (7.5%) | |||
| 61Cu | 3.3 | Cyclotron | β+ (61.5%) | 1220 |
| 61Ni(p,n)61Cu | EC (38.5%) | |||
| 62Cu | 0.16 | Generator | β+ (98%) | 2910 |
| 62Zn/62Cu | EC (2%) | |||
| 64Cu | 12.7 | Cyclotron | β+ (17.6%) | 656 |
| 64Ni(p,n)64Cu | EC (43.9%) | |||
| 64Ni(d,2n)64Cu | β– (38.5%) | |||
| 67Cu | 61.83 | Cyclotron | β– (100%) | 575 |
| 68Zn(p,2p)67Cu | ||||
| 70Zn(p,α)67Cu | ||||
| 55Co | 17.5 | Cyclotron | β+ (76%) | 570 |
| 58Ni(p,α)55Co | EC (24%) | |||
| 66Ga | 9.5 | Cyclotron | β+ (57%) | 4153 |
| 63Zn(p,n)66Ga | EC (43%) | |||
| 68Ga | 1.1 | Cyclotron | β+ (89%) | 1880 |
| 68Zn(p,n)68Ga | EC (11%) | |||
| Generator | ||||
| 68Ge/68Ga | ||||
| 86Y | 14.7 | Cyclotron | β+ (31.95%) | 2335 |
| 86Sr(p,n)86Y | EC (68.05%) | |||
| 89Zr | 78.4 | Cyclotron | β+ (22.75%) | 1744 |
| 89Y(p,n)89Zr | EC (77.25%) |
The research in this field has not just been focused on the development of radionuclides, but also on the design of novel ligands that could chelate and transport these metals to the target tissue, including two main types of chelating agents: open-chain chelators and macrocyclic chelators.50,51
3.1. From the copper age to nuclear medicine
3.1.1. Nature of copper
The first records on the use of copper date back to 5000 B.C. The name is derived from the Latin word cuprum; some authors believe that the origin of the name is from aes cyprium (the metal of Cyprus), as this metal was mainly mined in Cyprus during the Roman era. The early uses of this metal were in the manufacture of weapons and tools. Eventually, the interest in copper increased mainly due to the advances on metallurgy and as result, alloys like bronze (copper with tin) and brass (copper and zinc) expanded the use of copper. With the birth of electricity in the nineteenth century, the uses of this metal increased due to its good electrical properties, among them its high electrical conductivity (59.6 × 107 S m–1). More recently, copper found new applications in superconductivity research, giving origin to high-temperature copper-oxide-based semiconductors.52
Copper is a chemical element with atomic number 29, located at the position of transition metals on the periodic table. It is a soft, malleable and ductile metal. It is documented that copper is distributed on Earth but in different quantities, approximately 68 ppm in the Earth's crust, 0.003 ppm in seawater, and as an important point, 1.0 ppm is distributed in the human body. One of the most accessible oxidation states of copper is Cu(ii); meanwhile, Cu(i) and Cu(iii) are species present just using some specific donors that stabilize the oxidation state. Cu(ii) is known for its borderline hardness, its ionic radius is 57–73 pm, and it bears a coordination number of 4–6, making it suitable to form five membered chelate rings. One interesting aspect is that once copper forms complexes with macrocyclic chelators, it shows better kinetic inertness and in vivo stability, compared with those of a linear chelate. This is mainly due to the macrocyclic effect.53
3.1.2. Copper and biological aspects
Copper has been applied in the medical field because of the role it plays in many physiological functions such as neurotransmitter biosynthesis, tissue formation and enzyme functions.54,55 This metal has important functions not only in some synthetic pathways, it is important to mention that irregularities in its levels may also lead to some diseases like Menkes and Wilson's syndrome, which are the consequence of a deficiency (caused by mutations in the copper-transporter gene ATP7A-chromosome) or an overload in concentration of copper (the result of a mutation in the ATP7A gene-chromosome), respectively.56
Given the important role that copper plays in tissue formation, some authors proposed that its presence is critical in the process of angiogenesis and therefore in tumor growth;57,58 taking into account that tumor cells need high concentrations of copper to grow, in contrast to normal cells, novel types of therapies have been targeted to modify the supply of this metal and as a result the process of vasculature formation could be changed, altering the progress of tumor growth.56,59 Several chelating agents have been developed in order to assess their ability to inhibit endothelial cell proliferation. The earlier assays in this kind of therapy were focused on the treatment of Wilson's disease, using penicillamine and triethylenetetramine,60,61 but due to the high toxicity of these chelates, derivatives of cis, cis-1,3,4,-triaminocyclohexane (TACH) have been developed (Fig. 3).
Fig. 3. TACH derivatives.
The other treatment approach uses the REDOX properties of Cu(i), as it can be oxidized by H2O2 generating a hydroxyl radical by a Fenton or even by Haber–Weiss reaction. Evidence suggests that inhibition of some antioxidant enzymes and production of radicals could be classified as a treatment for cancer;62,63 compounds like Casiopeina64 and thiosemicarbazones61 have been evaluated to inhibit tumor cell proliferation following this rationale (Fig. 4).
Fig. 4. Casiopeina and thiosemicarbazone derivatives.
Finally, taking into account the cellular homeostasis, regulated by several proteins, researchers have demonstrated that proteasome plays a crucial role in the timely degradation of proteins, making it possible to maintain the cellular equilibrium by processes like protein quality control, antigen processing, apoptosis, etc.65–67 It is important to emphasize that cancer cells are more sensitive to proteasome inhibition than normal cells (Fig. 5).
Fig. 5. Proteasome inhibitors.
3.2. The use of copper in positron emission tomography (PET)
Copper has two stable isotopes (63Cu and 65Cu, relative abundances of 69.17% and 30.83%, respectively) and 27 known radioisotopes, but just four of them have been employed in molecular imaging (60Cu, 61Cu, 62Cu, and 64Cu).68 The interest in these radionuclides lies in their decay modes and broad range of half-lives (Table 1).48,69 However, in recent years, the interest of the global research community has been focused on the properties of 64Cu, from its production to its application in the medical field. As an example of the increasing interest in this radionuclide, it is worth mentioning that the International Atomic Energy Agency (IAEA) recently launched a Coordinated Research Project (CRP) entitled “Copper-64 radiopharmaceuticals for theranostic applications”70 with the main objective of formulating guidelines to enhance and strengthen the expertise and capability of member states in the production, quality control, preclinical and possible clinical application of copper-64 radiopharmaceuticals with theranostic properties.71–75
When talking about 64Cu, one important topic is its production, which can either proceed using a reactor or a cyclotron; the different methods of production lead to products with varying quality in terms of radiochemical and chemical impurities, in addition to yield and specific activity. Production by a reactor can lead to high or low specific activity, depending on whether the production is by direct activation (n,γ) on a Cu target, or indirect activation through a (n,p) reaction on a Zn target, respectively. The neutron-induced reaction on a 64Zn target has a good yield, but the co-production of 65Zn (t1/2 = 245 days) as a contaminant species is a great disadvantage.48,76 As an alternative, the use of a medical cyclotron has shown better results in the production of 64Cu, in terms of both yield and specific activity.77–81 A high specific activity 64Cu is best achieved using isotopically enriched targets via the 64Ni(p,n) reaction.82
As previously mentioned, the great interest in 64Cu lies in two main aspects: its characteristics of radioactive decay and coordination chemistry. I) Radioactive decay: this radionuclide bear a T1/2 = 12.7 h, and decays 17.4% β+, 39% β– and 43.6% E.C. The low positron energy (Emax = 0.65 MeV) and the lack of abundant high energy γ-emissions make this radionuclide suitable not just as a diagnosis probe but also as a therapeutic agent.47,83,84 II) Coordination chemistry: the chemistry of copper compounds has been limited to three oxidation states (I–III). However, most Cu(i) complexes show high lability, limiting their applications for radiopharmaceutical production, while Cu(iii) is a rare species that is possible to attain only with the use of strong π-donating ligands. Cu(ii), on the other hand, due to its softness, can form complexes with species like amines, imines, and bidentate ligands (such as bipyridine).85 These complexes can have a broad variety of geometries including square planar, distorted square planar, trigonal pyramidal, square pyramidal and distorted octahedral. As a consequence of this “rich chemistry”, several types of chelators have been developed in order to transport or stabilize Cu(ii) species, e.g. cyclam and cyclen moieties, sarcophagine chelators, and cross-bridged tetraamine ligands86 (Fig. 6).
Fig. 6. Most known bifunctional chelates and their derivatives, adapted from ref. 48.
4. Porphyrins as [64Cu]Cu chelates
The use of porphyrins as 64Cu chelates has demonstrated several advantages over their counterparts based on cyclam and cyclen moieties.87 Among these, it is worth mentioning that:
1) The multiple pathways of tumor accumulation.88 Porphyrins may interact with tumor cells in different ways; one of them involves the interaction with low-density lipoproteins (LDLs). Porphyrin-LDL particles are internalized by endocytosis and taking into account that tumor cells have a hyperproliferation metabolism, their need for this kind of molecule is increased. As a result, the cellular uptake of LDL-bound porphyrins is facilitated,89–91 and upon degradation of LDLs by lysosomes, porphyrins are released intracellularly. In the same way, the increased expression of transferrin receptors in cancer tissues could be a strategy to internalize porphyrins and form a complex based on transferrin-bound porphyrins and as a result, the macrocycle could be accumulated in the tumor stroma.92,93 The second process that is responsible for porphyrin tumor accumulation involves the ability of this macrocycle to form aggregates, which could be phagocyted by tumor-associated macrophages that have the potential to reduce tumor growth and destroy neoplastic tissues.94–96
2) Another advantage that makes porphyrins excellent options to be used as 64Cu chelates is their complex stability under physiological conditions. Novel protocols that improve the conditions, yield and labeling time of these macrocycles have been recently described, making it possible to explore the development of a radiopharmaceutical-kit that could be used at room temperature.97
The first report on the radiolabeling of porphyrins using 64Cu was documented in 1957, and was evaluated in neoplastic tissues.91 Later on, in the 1980s Wilson et al. used 64Cu-labelled porphyrins to detect brain tumors, but the results were not convincing because PET technology was on its earliest stages of development and the spatial resolution was poor98 (Fig. 7).
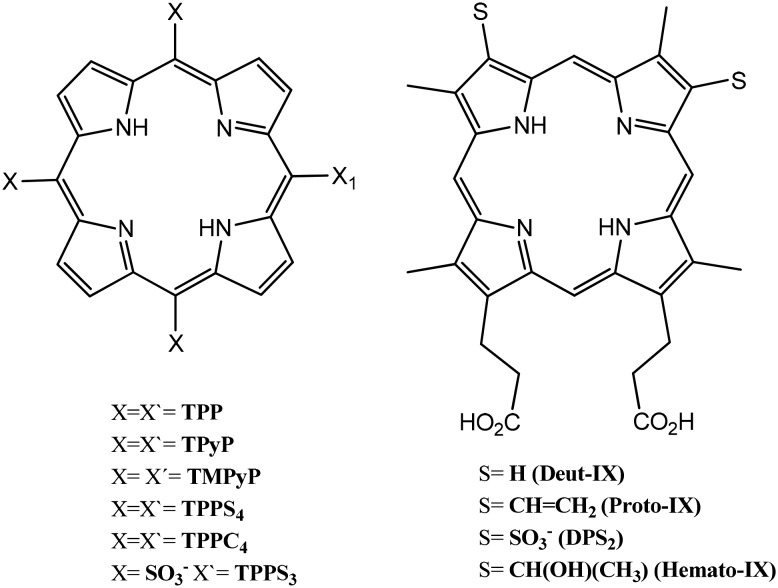
Fig. 7. Porphyrins structures studied earlier with PET.
The group of Fazaeli et al.99 labelled a penta-fluoro phenyl porphyrin using 64Cu; however due to the harsh reaction conditions used to incorporate the copper nuclei (reflux at 100 °C, 1 h) it is difficult to use this strategy with biological moieties. The specific activity was on the order of 14–16 GB mmol–1 and the radiochemical purity was >97%. Biodistribution results showed that after 2 h of injection most of the activity was concentrated in the kidney and liver, with the urinary tract being the main route of excretion, because of the fluoride properties.100,101
Other kinds of modified porphyrins have been developed in order to improve either uptake or clearance. Fazaeli et al.102 developed a complex based on a fluoro phenyl porphyrin grafted on nanoporous MCM-41 silica in order to obtain a carrier system for delivery of PET tracers. Biodistribution studies show major uptake by the kidney, stomach and tumor, resulting in a promising compound that has high tumor targeting efficiency and fast clearance. On the other hand, Huang et al.103 and Cheng et al.104 have synthetized a series of porphyrin-PEG polymers labeled with 64Cu that could help to evaluate renal function; PEG incorporation to the porphyrin core improves its stability, and the results of renal function evaluation showed that the clearance reached 60% of the injected dose (collected in urine).
The group of Luo and Wu105 developed a multifunctional nanoparticle system based on poly(vinyl alcohol)-porphyrin (PPNs), which was labeled with 64Cu; the advantage of these molecules is that they integrate PET, PDT, PTT (photothermal therapy), and even drug delivery functions. Upon irradiation by near infrared light, PPNs could be activated to release reactive oxygen species, heat, and drugs simultaneously in the tumor sites.
The group of Li et al.106 developed a theranostic strategy based on nanoporphyrins labeled with 64Cu (64Cu Nps); this compound initiated tumor accumulation 4 h after injection, and reached the maximum level of uptake at 16 h. After 24 h, the radiolabelled compound was found primarily at the implanted tumors with low-background signaling in the rest of the body.
5. Conjugated based on 64Cu-porphyrins and biological molecules
The main goal of functionalizing porphyrins with biological units is to enhance the tumor uptake and therefore decrease side effects. In this aspect, porphyrins have been successfully functionalized under mild conditions, making it possible to keep the biological moiety intact and hence retain the high-target specificity. Reports following this approach include macromolecules from peptides to proteins and antibodies.1,107–109
Roberts et al.110 reported the use of N-4-nitrobenzyl-5-(4-carboxyphenyl)-10,15,20-tris(4-sulfophenyl) porphine conjugated with polyclonal rabbit immunoglobulin G (RIgG), and the conjugate porphyrin–RIgG was radiolabeled with 64Cu (Fig. 8), obtaining a radiolabeling yield of 60%, probably due to the presence of the antibody that could reduce the metallation process by steric hindrance. The specific activity was 18 MBq mg–1 suggesting an average of two porphyrins per antibody unit. On the other hand, coupling was not specific for any region of the antibody as a consequence of the free amino groups present on the antibody. This poor specificity on conjugation resulted in a reduced immunoreactivity of around 60%, compared with that of the unmodified antibody.111–114 The advantage of using these kinds of conjugates is that it is possible to combine the properties of porphyrin (as a chelating agent and its photophysical properties) with the high specificity reaction of the antibody–antigen, which explains why the use of monoclonal antibodies (mABs) has emerged as a novel therapeutic tool against several diseases, among them cancer.115
Fig. 8. Conjugate based on porphyrin–monoclonal antibody.
Fawwaz et al.116 evaluated the activity of a porphyrin conjugated with an antibody (via esterification), using a molar ratio of 1 : 10, respectively; after purification they determined a ratio of 2 porphyrins per antibody. The conjugate was labeled with 64CuCl, and an ELISA assay was conducted, resulting in 72% immunoreactivity.
In 2013 Mukai et al. evaluated a conjugate based on 64Cu-porphyrin–peptide (Fig. 9). The percentage of conjugation between the porphyrin and peptide was 11%. The radiolabeling was performed using mild conditions (pH 6, 50 °C and two hours of reaction) in order to avoid radiolysis, obtaining specific activities of 96.2 MBq nmol–1 for [64Cu]PPIX-PEG6-BBN and 1440 MBq nmol–1 for [64Cu]Cu-PPIX. In order to establish a specific comparison, similar studies were carried out using [64Cu]Cu-DOTA-PEG6-BBN, which was obtained with a specific activity of 3–6 MBq nmol–1 and a radiochemical purity of 97%, while the radiochemical purity of [64Cu]Cu-PPIX-PEG6-BBN was 96.7%. The PC-3 human prostatic carcinoma cell line was used to evaluate the specificity, and [64Cu]Cu-PPIX-PEG6-BBN showed a higher uptake than [64Cu]Cu-PPIX, suggesting a synergic role between hydrophobicity by PPIX and the association effect between GRP and BBN.117
Fig. 9. [64Cu] PPIX-PEG6-BBN.
The use of a porphyrin unit, folate (for target delivery to FR-expressing tumor cells), and a peptide linker was reported by Shi et al.118 (Fig. 10). The radiolabeling yield for this compound was almost quantitative (99.9%), obtaining a radiochemical purity of 98% and a specific activity of 2.66 × 106 GBq mol–1. The labeling conditions (60 °C, 10–20 minutes of reaction in DMSO) made this strategy less convenient to human use; however, it is worth mentioning that the metalloporphyrin showed high stability in physiological media.
Fig. 10. Porphyrin–folate conjugate.
Liu et al.119–121 have used nanoparticles based on lipids or phospholipids conjugated with porphyrin. Porphysomes could act as drug-delivery systems (due to the properties of liposomes); on the other hand, they exhibited the photonic properties of the porphyrin. Once radiolabeling was performed they obtained radiochemical purities higher than 98% and a radiochemical yield (decay-uncorrected) of 95%, while the specific activity was 36 mCi μmol–1 (2800 Ci μmol–1 per nanoparticle). It is worth noting that porphysomes were cleared by the hepatobiliary route, and as a result, high concentrations in the liver and spleen were detected and none in the bladder. This is a great advantage because a high concentration of the radiotracer in the bladder results in a darkening of the image, making it difficult to obtain a diagnosis. These 64Cu-porphysomes were evaluated in order to compare their response in prostate cancer and compared with 18F-FDG, resulting in a superior tumor-to-prostate selectivity.122
Finally, the strategy “Multimodal Image-Guided Surgical” used by Muhanna et al.123 has demonstrated excellent results in head and neck cancer, by using a porphyrin lipoprotein (PLP) labeled with 64Cu (mimicking nanoparticles) that was able to detect the primary tumor and metastatic nodes. The high accuracy of detection of the PLP relies on the fact that both preoperative PET and intraoperative fluorescence imaging are feasible for the identification of unknown primaries and recurrent tumors.
Conclusions
Positron emission tomography has emerged as a multidisciplinary technique in which people with specialization (physicists, chemists, engineers, pharmacologists, medical doctors, veterinary doctors, computer scientists and mathematicians) generate each day advances that result in better diagnosis giving the patient a chance for a better quality of life. As a clear example: the progress and improvements in the development of metallic radionuclides (as PET tracers) that have arisen as an option that could overcome the common disadvantages of conventional PET radionuclides of the main sequence CNOF (11C, 13N, 15O and 18F) given their short half-lives.
The use of 64Cu and porphyrins has been demonstrated to be an excellent approach to obtain a theranostic couple (PET diagnosis from 64Cu and photodynamic therapy from porphyrins). It is clear that there is a long way to go when talking about the design and improvement of molecules with theranostic capabilities, and the synthesis of novel porphyrin-conjugates that could behave in a selective way against some diseases or disorders (using peptides, monoclonal antibodies or lipids) seems to be the right approach. More importantly, having the capability to chelate longer half-life metallic radionuclides will make it possible for the PET technique be available for a greater number of people even in places where cyclotrons are not yet available.
Conflicts of interest
There are no conflicts to declare.
Acknowledgments
This research was supported by UNAM-DGAPA Grant PAPIIT-IT202518, CONACYT Grand APN-2017-4837, and the International Atomic Energy Agency CRP code F22067 and RC 20569. E. Aguilar-Ortiz received a Postdoctoral fellowship from Programa de Becas Posdoctorales-DGAPA-UNAM. The authors want to thank Mrs. Josefina Bolado, Head of the Scientific Paper Translation Department, from División de Investigación at Facultad de Medicina, UNAM, for editing the English-language version of this manuscript.
Biographies

Edgar Aguilar-Ortíz
Dr. Edgar A. Aguilar-Ortiz is a postdoctoral research fellow at the National Autonomous University of Mexico (UNAM) in the Faculty of Medicine. He received his BS in Chemistry from the Faculty of Chemistry and his MSc and PhD degrees from the Material Research Institute (UNAM). During his doctoral studies, he was a visiting scholar at the University of Montreal in the Polymers Department (2014–2015). His areas of interest include the study of optical properties of porphyrins for photodynamic therapy, synthesis of macrocyclic compounds for biological applications, radiolabeling of organic macrocylics using metallic radionuclides, and functionalization of organic compounds with biological moieties using click chemistry techniques.

Amir R. Jalilian
Prof. Amir R. Jalilian is a Technical Officer at the Radioisotope Products and Radiation Technology Section at the International Atomic Energy Agency (IAEA). He performed his Pharm Doctoral thesis under the supervision of Prof. Abbas Shafiee in 1995. After his graduation, he obtained a PhD degree in Radiopharmacy in 2000. He continued his profession at the University of Alberta, Canada and Yale School of Medicine, USA, as a post-doctoral fellow. Prof. Jalilian's research interests cover applied targeted tumor diagnosis and therapy using radiolabeled compounds. During the last 18 years, he has been active in the development of radiopharmaceuticals in developing countries leading to completion of clinical trials and the marketing of some radiopharmaceuticals in some countries.

Miguel A. Ávila-Rodríguez
Dr. Miguel A. Avila-Rodriguez is a tenured Associate Professor and Head of the Cyclotron and Radiopharmaceutical Labs at the National Autonomous University of Mexico (UNAM). He received his PhD degree in Medical Physics from the University of Wisconsin-Madison (USA). After that, he was a postdoctoral researcher fellow at the University of Alberta in the Edmonton PET Centre (Canada), and at the University of Turku in the Turku PET Centre (Finland). His area of expertise is in the production of non-conventional radionuclides for medical applications and radiopharmaceuticals for PET molecular imaging. He is well-known for his contributions in the production of metallic radionuclides.
References
- Vahidfar N., Jalilian A. R. Recent Patents and Topics on Imaging. 2005;5:3–12. [Google Scholar]
- Hambright P., Fawwaz R., Valk P., McRae J., Bearden A. J. Bioinorg. Chem. 1975;5:87–92. doi: 10.1016/s0006-3061(00)80224-0. [DOI] [PubMed] [Google Scholar]
- Lakouas K. D., Huglo D., Mordon S., Vermandel M. Photodiagn. Photodyn. Ther. 2017;18:236–243. doi: 10.1016/j.pdpdt.2017.03.002. [DOI] [PubMed] [Google Scholar]
- Mody D. T. J. Porphyrins Phthalocyanines. 2000;4:362–367. [Google Scholar]
- Nowakowska M., KKȩpczyńskipczyński M. J. Photochem. Photobiol., A. 1998;116:251–256. [Google Scholar]
- Gerdes R., Bartels O., Schneider G., Wöhrle D., Schulz-Ekloff G. Polym. Adv. Technol. 2001;12:152–160. [Google Scholar]
- Gerdes R. J. Photochem. Photobiol., A. 1997;111:65–74. [Google Scholar]
- Oleinick N. L., Antunez A. R., Clay M. E., Rihter B. D., Kenney M. E. Photochem. Photobiol. 1993;57:242–247. doi: 10.1111/j.1751-1097.1993.tb02282.x. [DOI] [PubMed] [Google Scholar]
- Ethirajan M., Chen Y., Joshi P., Pandey R. K. Chem. Soc. Rev. 2011;40:340–362. doi: 10.1039/b915149b. [DOI] [PubMed] [Google Scholar]
- Dougherty T. J. Photochem. Photobiol. 1987;45:879–889. doi: 10.1111/j.1751-1097.1987.tb07898.x. [DOI] [PubMed] [Google Scholar]
- Rothemund P. J. Am. Chem. Soc. 1936;58:625–627. [Google Scholar]
- Rothemund P. J. Am. Chem. Soc. 1935;57:2010–2011. [Google Scholar]
- Adler A. D., Longo F. R., Finareli J. D., Goldsmacher J., Assour J., Korsakoff L. J. Org. Chem. 1967;32:476. [Google Scholar]
- Adler A., Longo F., Shergalis W. J. Am. Chem. Soc. 1964;15:3145–3149. [Google Scholar]
- Lindsey J. S., Schreiman I. C., Hsu H. C., Kearney P. C., Marguerettaz A. M. J. Org. Chem. 1987;52:827–836. [Google Scholar]
- Spellane P. J., Gouterman M., Antipas A., Kim S., Liu Y. C. Inorg. Chem. 1980;19:386–391. [Google Scholar]
- Khan A. U., Kasha M. J. Chem. Phys. 1963;39:2105–2106. [Google Scholar]
- Herzberg G., Molecular Spectra Vol I, D. Van Nostrand Company Inc., 1950. [Google Scholar]
- Long C. A., Kearns D. R. J. Am. Chem. Soc. 1975;97:2018–2020. [Google Scholar]
- Scurlock R. D., Wang B., Ogilby P. R. J. Am. Chem. Soc. 1996;118:388–392. [Google Scholar]
- Bodesheim M., Schmidt R. J. Phys. Chem. A. 1997;101:5672–5677. [Google Scholar]
- Foote C. S. Acc. Chem. Res. 1968;1:104–110. [Google Scholar]
- Clennan E. L., Pace A. ChemInform. 2005;36:6665–6691. [Google Scholar]
- Bonnett R. Chem. Soc. Rev. 1995;24:19–33. [Google Scholar]
- DeRosa M. C., Crutchley R. J. Coord. Chem. Rev. 2002;233–234:351–371. [Google Scholar]
- Ogilby P. R. Chem. Soc. Rev. 2010;39:3181–3209. doi: 10.1039/b926014p. [DOI] [PubMed] [Google Scholar]
- Sharman W. M., Allen C. M., van Lier J. E. Methods Enzymol. 2000;319:376–400. doi: 10.1016/s0076-6879(00)19037-8. [DOI] [PubMed] [Google Scholar]
- Loewen G. M., Pandey R., Bellnier D., Henderson B., Dougherty T. Lasers Surg. Med. 2006;38:364–370. doi: 10.1002/lsm.20354. [DOI] [PubMed] [Google Scholar]
- Bellnier D. A., Greco W. R., Loewen G. M., Nava H., Oseroff A. R., Dougherty T. J. Lasers Surg. Med. 2006;38:439–444. doi: 10.1002/lsm.20340. [DOI] [PubMed] [Google Scholar]
- Bellnier D. A., Greco W. R., Loewen G. M., Nava H., Oseroff A. R., Dougherty T. J. Cancer Chemother. Pharmacol. 2006;57:40–45. doi: 10.1007/s00280-005-0015-6. [DOI] [PubMed] [Google Scholar]
- Chen Y., Miclea R., Srikrishnan T., Balasubramanian S., Dougherty T. J., Pandey R. K. Bioorg. Med. Chem. Lett. 2005;15:3189–3192. doi: 10.1016/j.bmcl.2005.05.019. [DOI] [PubMed] [Google Scholar]
- Magne M. L., Rodriguez C. O., Autry S. A., Edwards B. F., Theon A. P., Madewell B. R. Lasers Surg. Med. 1997;20:202–209. doi: 10.1002/(sici)1096-9101(1997)20:2<202::aid-lsm12>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- Lemon C. M., Brothers P. J., Boitrel B. Dalton Trans. 2011;40:6591. doi: 10.1039/c0dt01711f. [DOI] [PubMed] [Google Scholar]
- John Plater M., Aiken S., Bourhill G. Tetrahedron. 2002;58:2415–2422. [Google Scholar]
- Fleischer E. B. Acc. Chem. Res. 1970;3:105–112. [Google Scholar]
- Rossin R., Pan D., Qi K., Turner J. L., Sun X., Wooley K. L., Welch M. J. J. Nucl. Med. 2005;46:1210–1218. [PubMed] [Google Scholar]
- Scheidt W. R. Acc. Chem. Res. 1977;10:339–345. [Google Scholar]
- Tatsumi K., Hoffmann R. J. Am. Chem. Soc. 1981;103:3328–3341. [Google Scholar]
- Olguín J., Müller-Bunz H., Albrecht M. Chem. Commun. 2014;50:3488–3490. doi: 10.1039/c4cc00497c. [DOI] [PubMed] [Google Scholar]
- Suijkerbuijk B. M. J. M., Klein Gebbink R. J. M. Angew. Chem., Int. Ed. 2008;47:7396–7421. doi: 10.1002/anie.200703362. [DOI] [PubMed] [Google Scholar]
- Urbani M., Grätzel M., Nazeeruddin M. K., Torres T. Chem. Rev. 2014;114:12330–12396. doi: 10.1021/cr5001964. [DOI] [PubMed] [Google Scholar]
- Ishihara S., Labuta J., Van Rossom W., Ishikawa D., Minami K., Hill J. P. Phys. Chem. Chem. Phys. 2014;16:9713–9746. doi: 10.1039/c3cp55431g. [DOI] [PubMed] [Google Scholar]
- Lum C. T., Wong A. S.-T., Lin M. C., Che C.-M., Sun R. W.-Y. Chem. Commun. 2013;49:4364–4366. doi: 10.1039/c2cc37366a. [DOI] [PubMed] [Google Scholar]
- Miller P. W., Long N. J., Vilar R., Gee A. D. Angew. Chem., Int. Ed. 2008;47:8998–9033. doi: 10.1002/anie.200800222. [DOI] [PubMed] [Google Scholar]
- Ramogida C. F., Orvig C. Chem. Commun. 2013;49:4720–4739. doi: 10.1039/c3cc41554f. [DOI] [PubMed] [Google Scholar]
- Cutler C. S., Hennkens H. M., Sisay N., Huclier-Markai S., Jurisson S. S. Chem. Rev. 2013;113:858–883. doi: 10.1021/cr3003104. [DOI] [PubMed] [Google Scholar]
- Bhattacharyya S., Dixit M. Dalton Trans. 2011;40:6112–6128. doi: 10.1039/c1dt10379b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadas T. J., Wong E. H., Weisman G. R., Anderson C. J. Curr. Pharm. Des. 2007;13:3–16. doi: 10.2174/138161207779313768. [DOI] [PubMed] [Google Scholar]
- Ikotun O. F., Lapi S. E. Future Med. Chem. 2011;3:599–621. doi: 10.4155/fmc.11.14. [DOI] [PubMed] [Google Scholar]
- Price E. W., Orvig C. Chem. Soc. Rev. 2014;43:260–290. doi: 10.1039/c3cs60304k. [DOI] [PubMed] [Google Scholar]
- Boros E., Scott Lin Y.-H. L., Ferreira C. O., Patrick B. O., Hafeli U. J., Adam M., Orvig C. Dalton Trans. 2011;40:6253–6259. doi: 10.1039/c0dt01458c. [DOI] [PubMed] [Google Scholar]
- Conry R. R., Copper: Inorganic and Coordination Chemistry Based in part on the article Copper: Inorganic and Coordination Chemistry by Rebecca R. Conry and Kenneth D. Karlin which appeared in the Encyclopedia of Inorganic Chemistry, in Encyclopedia of Inorganic Chemistry, 1st edn, 2006. [Google Scholar]
- Matteson D. S., Larson G. L. J. Am. Chem. Soc. 1969;91:6541–6542. [Google Scholar]
- Festa R. A., Thiele D. J. Curr. Biol. 2011;21:R877–R883. doi: 10.1016/j.cub.2011.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutsenko S. Curr. Opin. Chem. Biol. 2010;14:211–217. doi: 10.1016/j.cbpa.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santini C. Chem. Rev. 2014;114:815–862. doi: 10.1021/cr400135x. [DOI] [PubMed] [Google Scholar]
- Eatock M. M., Schätzlein A., Kaye S. B. Cancer Treat. Rev. 2000;26:191–204. doi: 10.1053/ctrv.1999.0158. [DOI] [PubMed] [Google Scholar]
- Xie H., Kang Y. J. Curr. Med. Chem. 2009;16:1304–1314. doi: 10.2174/092986709787846622. [DOI] [PubMed] [Google Scholar]
- Wang F., Jiao P., Qi M., Frezza M., Dou Q. P., Yan B. Curr. Med. Chem. 2010;17:2685–2698. doi: 10.2174/092986710791859315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walshe J. M. Lancet. 1982;1:643–647. doi: 10.1016/s0140-6736(82)92201-2. [DOI] [PubMed] [Google Scholar]
- Liu M.-C., Lin T.-S., Cory J. G., Cory A. H., Sartorelli A. C. J. Med. Chem. 1996;39:2586–2593. doi: 10.1021/jm9600454. [DOI] [PubMed] [Google Scholar]
- Kong Q., Beel J. A., Lillehei K. O. Med. Hypotheses. 2000;55:29–35. doi: 10.1054/mehy.1999.0982. [DOI] [PubMed] [Google Scholar]
- Fang J., Nakamura H., Iyer A. K. J. Drug Targeting. 2007;15:475–486. doi: 10.1080/10611860701498286. [DOI] [PubMed] [Google Scholar]
- Trejo-Solís C., Palencia G., Zuñiga S., Rodríguez-Ropon A., Osorio-Rico L., Torres Luvia S., Gracia-Mora I., Marquez-Rosado L., Sánchez A., Moreno-Gracía M. E., Cruz A., Bravo-Gómez M. E., Ruiz-Ramírez L., Rodríguez-Enriquez S., Sotelo J. Neoplasia. 2005;7:563–574. doi: 10.1593/neo.04607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eytan E., Ganoth D., Armon T., Hershko A. Proc. Natl. Acad. Sci. U. S. A. 1989;86:7751–7755. doi: 10.1073/pnas.86.20.7751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hough R., Pratt G., Rechsteiner M. J. Biol. Chem. 1987;262:8303–8313. [PubMed] [Google Scholar]
- Voges D., Zwickl P., Baumeister W. Annu. Rev. Biochem. 1999;68:1015–1068. doi: 10.1146/annurev.biochem.68.1.1015. [DOI] [PubMed] [Google Scholar]
- Blower P. J., Lewis J. S., Zweit J. Nucl. Med. Biol. 1996;23:957–980. doi: 10.1016/s0969-8051(96)00130-8. [DOI] [PubMed] [Google Scholar]
- Niccoli Asabella A., Cascini G. L., Altini C., Paparella D., Notaristefano A. BioMed Res. Int. 2014;2014:786463. doi: 10.1155/2014/786463. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Copper-64 Radiopharmaceuticals for Theranostic Applications. (2017). Available at: https://www.iaea.org/projects/crp/f22067.
- Boschi A., Martini P., Janevik-Ivanovska E., Duatti A. Drug Discovery Today. 2018:1489–1501. doi: 10.1016/j.drudis.2018.04.002. [DOI] [PubMed] [Google Scholar]
- Ferrari C., Niccoli Asabella A., Villano C., Giacobbi B., Coccetti D., Panichelli P., Rubini G. BioMed Res. Int. 2015;2015:129764. doi: 10.1155/2015/129764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalilian A. R., Osso Jr J. Iran. J. Nucl. Med. 2017;25:1–10. [Google Scholar]
- Biggin C., Harris M., Hedt A., Jeffery C. J. Nucl. Med. 2017;58:1014–1014. [Google Scholar]
- Avila-Rodriguez M. A., Rios C., Carrasco-Hernandez J., Manrique-Arias J. C., Matinez-Hernandez R., Gracía-Pérez F. O., Jalilian A. R., Martinez-Rodriguez E., Romero-Piña M. E., Diaz-Ruiz A. EJNMMI Res. 2017;7:98. doi: 10.1186/s13550-017-0346-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinn K. R., Chaudhuri T. R., Cheng T.-P., Steven Morris J., Meyer W. A. Cancer. 1994;73:774–778. doi: 10.1002/1097-0142(19940201)73:3+<774::aid-cncr2820731305>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- McCarthy D. W., Shefer R. E., Klinkowstein R. E., Bass L. A., Margeneau W. H., Cutler C. S., Anderson C. J., Welch M. J. Nucl. Med. Biol. 1997;24:35–43. doi: 10.1016/s0969-8051(96)00157-6. [DOI] [PubMed] [Google Scholar]
- Szelecsényi F., Blessing G., Qaim S. M. Appl. Radiat. Isot. 1993;44:575–580. [Google Scholar]
- Avila-Rodriguez M. A., Nye J. A., Nickles R. J. Appl. Radiat.Appl. Radiat. Isot.Isot. 2007;65:1115–1120. doi: 10.1016/j.apradiso.2007.05.012. [DOI] [PubMed] [Google Scholar]
- Manrique-Arias J. C., Avila-Rodriguez M. A. Appl. Radiat. Isot. 2014;89:37–41. doi: 10.1016/j.apradiso.2014.01.024. [DOI] [PubMed] [Google Scholar]
- Xie Q., Zhu H., Wang F., Meng X., Ren Q., Xia C., Yang Z. Molecules. 2017;22:641. doi: 10.3390/molecules22040641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun X., Anderson J. C. Methods Enzymol. 2004;386:237–261. doi: 10.1016/S0076-6879(04)86011-7. [DOI] [PubMed] [Google Scholar]
- Obata A., Kasamatsu S., Lewis J. S., Furukawa T., Takamatsu S., Toyohara J., Asai T., Welch M. J., Adamas S. G., Saji H., Yonekura Y., Fujibayashi Y. Nucl. Med. Biol. 2005;32:21–28. doi: 10.1016/j.nucmedbio.2004.08.012. [DOI] [PubMed] [Google Scholar]
- Connett J. M., Anderson C. J., Gou L. W., Schwarz S. W., Zinn K. R., Rogers B. E., Siegel B. A., Philpott G. W., Welch M. J. Proc. Natl. Acad. Sci. U. S. A. 1996;93:6814–6818. doi: 10.1073/pnas.93.13.6814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin R. B., Hard and Soft Acids and Bases. in Encyclopedia of Inorganic Chemistry, ed. R. B. King, R. H. Crabtree, C. M. Lukehart, D. A. Atwood and R. A. Scott, John Wiley and Sons, Ltd, 2006. [Google Scholar]
- Anderson C. J., Ferdani R. Cancer Biother.Radiopharm. 2009;24:379–393. doi: 10.1089/cbr.2009.0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryden F., Boyle R. W. Adv. Inorg. Chem. 2016;68:141–221. [Google Scholar]
- Osterloh J., Vicente M. G. H. J. Porphyrins Phthalocyanines. 2002;06:305–324. [Google Scholar]
- Jori G., Reddi E. Int. J. Biochem. 1993;25:1369–1375. doi: 10.1016/0020-711x(93)90684-7. [DOI] [PubMed] [Google Scholar]
- Kessel D. Cancer Lett. 1986;33:183–188. doi: 10.1016/0304-3835(86)90023-6. [DOI] [PubMed] [Google Scholar]
- Bases R., Brodie S. S., Rubenfeld S. Cancer. 1958;11:259–263. doi: 10.1002/1097-0142(195803/04)11:2<259::aid-cncr2820110206>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- Nakajima S., Moriyama T., Hayashi H., Sakata I., Nakae Y., Takemura T. Cancer Lett. 2000;149:221–226. doi: 10.1016/s0304-3835(99)00367-5. [DOI] [PubMed] [Google Scholar]
- Hamblin M. R., Newman E. L. J. Photochem. Photobiol., B. 1994;26:45–56. doi: 10.1016/1011-1344(94)85035-6. [DOI] [PubMed] [Google Scholar]
- Lewis C. E., Leek R., Harris A., McGee J. O. J. Leukocyte Biol. 1995;57:747–751. doi: 10.1002/jlb.57.5.747. [DOI] [PubMed] [Google Scholar]
- Elgert K. D., Alleva D. G., Mullins D. W. J. Leukocyte Biol. 1998;64:275–290. doi: 10.1002/jlb.64.3.275. [DOI] [PubMed] [Google Scholar]
- Korbelik M., Krosl G., Chaplin D. J. Cancer Res. 1991;51:2251–2255. [PubMed] [Google Scholar]
- Kilian K., Pęgier M., Pyrzyńska K. Spectrochim. Acta, Part A. 2016;159:123–127. doi: 10.1016/j.saa.2016.01.045. [DOI] [PubMed] [Google Scholar]
- Firnau G., Maass D., Wilson B. C., Jeeves W. P. Prog. Clin. Biol. Res. 1984;170:629–636. [PubMed] [Google Scholar]
- Fazaeli Y. J. Radioanal. Nucl. Chem. 2013;295:255–263. [Google Scholar]
- Shah P., Westwell A. D. J. Enzyme Inhib. Med. Chem. 2007;22:527–540. doi: 10.1080/14756360701425014. [DOI] [PubMed] [Google Scholar]
- Swallow S. Prog. Med. Chem. 2015;54:65–133. doi: 10.1016/bs.pmch.2014.11.001. [DOI] [PubMed] [Google Scholar]
- Fazaeli Y., Feizi S., Jalilian R. A., Hejrani A. Appl. Rad. Isot. 2016;112:13–19. doi: 10.1016/j.apradiso.2016.03.003. [DOI] [PubMed] [Google Scholar]
- Huang H., Hernandez R., Geng J., Sun H., Song W., Cheng F., Graves A. S., NicklesJ R., Cheng C., Cai W. Biomaterials. 2016;76:25–32. doi: 10.1016/j.biomaterials.2015.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng L., Jiang D., Kamkaew A., Valdovinos F. H., Im H.-Y., Feng L., Englang G. C., Goel S., Barnhart E. T., Liu Z., Cai W. Adv. Funct. Mater. 2017;27:1–10. doi: 10.1002/adfm.201702928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y., Wu H., Feng C., Xiao K., Yang X., Liu Q., Lin T.-Y., Zhang H., Walton H. J., Ajena Y., Hu Y., Lam S. K., Li Y. Theranostics. 2017;7:3901–3914. doi: 10.7150/thno.20190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Lin T.-Y., Luo Y., Liu Q., Xiao W., Guo W., Lac D., Zhang H., Feng C., Wachsmann-Hogiu S., Walton H. J., Cherry R. S., Rowland J. D., Kukis D., Pan C., Lam S. K. Nat. Commun. 2012;5:1–15. doi: 10.1038/ncomms5712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Josefsen B. L., Boyle W. R. Theranostics. 2012;9:916–966. doi: 10.7150/thno.4571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waghorn P. A. J. Labelled Compd. Radiopharm. 2014;57:304–309. doi: 10.1002/jlcr.3166. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Lovell J. F. Theranostics. 2012;2:905–915. doi: 10.7150/thno.4908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts J. C., Newmyer S. L., Mercer-Smith J. A., Schreyer S. A., Lavallee D. K. Appl. Radiat. Isot. 1989;40:775–781. doi: 10.1016/0883-2889(89)90096-8. [DOI] [PubMed] [Google Scholar]
- Bullous A. J., Alonso C. M. A., Boyle R. W. Photochem. Photobiol. Sci. 2011;10:721. doi: 10.1039/c0pp00266f. [DOI] [PubMed] [Google Scholar]
- Mew D., Wat C. K., Towers G. H., Levy J. G. J. Immunol. 1983;130:1473–1477. [PubMed] [Google Scholar]
- Del Governatore M., Hamblin M. R., Piccinini E. E., Ugolini G., Hasan T. Br. J. Cancer. 2000;82:56–64. doi: 10.1054/bjoc.1999.0877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milgrom L. R., Neill F. O. Science. 1995;51:2137–2144. [Google Scholar]
- García Merino A. Neurologia. 2011;26:301–306. doi: 10.1016/j.nrl.2010.10.005. [DOI] [PubMed] [Google Scholar]
- Fawwaz R., Bohdiewicz P., Lavallee D., Wang T., Oluwole S., Newhouse J., Alderson P. Nucl. Med. Biol. 1990;17:65–72. doi: 10.1016/0883-2897(90)90009-p. [DOI] [PubMed] [Google Scholar]
- Mukai H., Wada Y., Watanabe Y. Ann. Nucl. Med. 2013;27:625–639. doi: 10.1007/s12149-013-0728-2. [DOI] [PubMed] [Google Scholar]
- Shi J., Liu W. B. T., Chen J., Green D., Jaffray D., Wilson C. B., Wang F., Zheng G. Theranostics. 2011;1:363–370. doi: 10.7150/thno/v01p0363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu T. W., MacDonald T. D., Shi J., Wilson B. C., Zheng G. Angew. Chem., Int. Ed. 2012;51:13128–13131. doi: 10.1002/anie.201206939. [DOI] [PubMed] [Google Scholar]
- Luo D., Goel S., Liu H.-J., Carter A. K., Jiang D., Geng J., Kutyreff J. C., Engle W. J., Huang W.-C., Shao S., Fang C., Cai W., Lovell F. J. ACS Nano. 2017;11:12482–12491. doi: 10.1021/acsnano.7b06578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin C. S., Cui L., Wang F., Chen J., Zheng G. Adv. Healthcare Mater. 2014;3:1240–1249. doi: 10.1002/adhm.201300651. [DOI] [PubMed] [Google Scholar]
- Jin C. S., Overchuk M., Cui L., Wilson C. B., Bristow G. R., Chen J., Zheng G. Prostate. 2016;76:1169–1181. doi: 10.1002/pros.23203. [DOI] [PubMed] [Google Scholar]
- Muhanna N., Cui L., Chan H., Burgess L., Jin S. C., MacDonald D. T., Huynh E., Wang F., Chen J., Irish C. J., Zheng G. Clin. Cancer Res. 2016;22:961–970. doi: 10.1158/1078-0432.CCR-15-1235. [DOI] [PubMed] [Google Scholar]