Abstract
Background and Aims
Although coronavirus disease 2019 (COVID-19) has affected endoscopy services globally, the impact on trainees has not been evaluated. We aimed to assess the impact of COVID-19 on procedural volumes and on the emotional well-being of endoscopy trainees worldwide.
Methods
An international survey was disseminated over a 3-week period in April 2020. The primary outcome was the percentage reduction in monthly procedure volume before and during COVID-19. Secondary outcomes included potential variation of COVID-19 impact between different continents and rates and predictors of anxiety and burnout among trainees.
Results
Across 770 trainees from 63 countries, 93.8% reported a reduction in endoscopy case volume. The median percentage reduction in total procedures was 99% (interquartile range, 85%-100%), which varied internationally (P < .001) and was greatest for colonoscopy procedures. Restrictions in case volume and trainee activity were common barriers. A total of 71.9% were concerned that the COVID-19 pandemic could prolonged training. Anxiety was reported in 52.4% of respondents and burnout in 18.8%. Anxiety was independently associated with female gender (odds ratio [OR], 2.15; P < .001), adequacy of personal protective equipment (OR, 1.75; P = .005), lack of institutional support for emotional health (OR, 1.67; P = .008), and concerns regarding prolongation of training (OR, 1.60; P = .013). Modifying existing national guidelines to support adequate endoscopy training during the pandemic was supported by 68.9%.
Conclusions
The COVID-19 pandemic has led to restrictions in endoscopic volumes and endoscopy training, with high rates of anxiety and burnout among endoscopy trainees worldwide. Targeted measures by training programs to address these key issues are warranted to improve trainee well-being and support trainee education.
Abbreviations: COVID-19, coronavirus disease 2019; IQR, interquartile range; OR, odds ratio; PPE, personal protective equipment
The coronavirus disease 2019 (COVID-19) pandemic has had a profound impact on the provision of GI endoscopy services worldwide, with the radical curtailment of elective procedures to restrict disease transmission.1 Consequently, multiple gastroenterology and endoscopy societies have published rigorous recommendations on triaging endoscopy procedures, appropriate use of personal protective equipment (PPE), and postprocedure decontamination for GI endoscopy during the pandemic.2, 3, 4, 5 Surveys from Italy and North America have reported over 75% reductions in procedure numbers in many centers.6 , 7 As institutions attempt to limit periendoscopic exposure to COVID-19 and conserve PPE, this will inevitably impact trainee engagement in hands-on endoscopy procedures.
The COVID-19 pandemic creates challenges for endoscopy trainees for several reasons. For trainees who are in direct contact with patients, providing clinical care during a pandemic can evoke fear and anxiety regarding personal safety and viral transmission.8 , 9 Trainees also face social isolation because of restricted contact with their families and friends.10 These concerns can be further exacerbated by inconsistency in scheduling, both because of trainees being quarantined and redeployed to other services.11 Finally, trainees may be concerned about delays in competency acquisition and future job security.
Novice endoscopists must become proficient in a range of diagnostic and therapeutic modalities during a training period, often of finite duration. Because it remains unclear when endoscopy units will fully resume regular activities, endoscopists-in-training may be concerned about attaining and maintaining competence in procedural skills. Additionally, trainee exposure to inpatient and ambulatory GI patients may be significantly reduced if institutions are limiting contact between consulting services and inpatients and canceling nonessential office visits. Shortages of PPE could worsen these issues because trainees may be the first to be excluded when there is inadequate PPE.
Despite these issues, there are no published data on the impact of the COVID-19 on endoscopy training and trainee well-being. Therefore, in this international survey we aimed to assess the impact of the COVID-19 pandemic on endoscopy trainees, including procedure numbers, barriers to training, and the physical and emotional well-being of trainees. We also aimed to explore variation in this impact internationally.
Methods
Survey design
A 37-item survey (Appendix 1, available online at www.giejournal.org) was developed through consensus by an international group of representatives from 10 countries with expertise in endoscopy training and education. The survey was conducted using the SurveyMonkey platform (SVMK Inc, San Mateo, Calif, USA) and was structured into the following domains:
-
1.
Demographics, including age, gender, country of training and specialization
-
2.
Monthly endoscopy volumes before and during COVID-19
-
3.
Training and availability of PPE
-
4.
Impact on physical, mental, and emotional well-being
The survey was reviewed and authorized for multicenter distribution by the ethics committee of the Institute for Clinical and Experimental Medicine, Thomayer Hospital, Prague, Czech Republic (reference: 9170/7.4.202; G-20-16;8.4.2020), which waived the need for formal ethics application.
Outcomes
The primary outcome studied was the percentage reduction in the monthly volume of hands-on endoscopy procedures performed by trainees as a result of COVID-19. This was studied using 2 methods: as a comparison over two 30-day periods before and during the COVID-19 pandemic and as a categorical variable according to trainee indication of an overall reduction in procedure volume. Endoscopy procedures studied comprised EGD, colonoscopy, EUS, ERCP, and upper GI bleed hemostasis (included within the EGD numbers), for supervised, unsupervised, and total numbers. Secondary outcomes were barriers to hands-on training and the impact on residual training opportunities; changes to institutional case volume; trainee concerns regarding competency development and prolongation of training; and anxiety, assessed using the Generalized Anxiety Disorder-7 scale,12 and rates of burnout, measured using the single-item burnout scale.13 For each outcome, analyses were compared across continents to denote international variation in survey responses.
Survey distribution
At the beginning of April 2020, the EndoTrain survey was distributed to trainees both directly and indirectly via program directors, trainee representatives, and representatives within national and international societies (Supplementary Table 1, available online at www.giejournal.org). The survey was open for 3 weeks from April 11 to May 2, 2020.
Statistical analysis
All continuous variables were subjected to normality assessment (Shapiro-Wilk) and presented as medians with interquartile ranges (IQRs) or means and standard errors as appropriate. For each procedure, trainees who did not indicate any procedures in a given modality over the 2 comparison periods were excluded from analyses to identify active trainees for each procedure category. Pairwise comparisons of procedural numbers were performed at the trainee-level between pre–COVID-19 and COVID-19 periods using Wilcoxon signed-rank tests. Nonparametric data across procedure types and continents were compared using the Kruskal-Wallis test, followed by Dunn’s test for pairwise comparisons. Continuous variables were compared across continents using 1-way analysis of variance. Categorical data were compared using the Pearson χ2 test.
Binary logistic regression analysis was performed for univariable and multivariable analysis of factors associated with anxiety in endoscopy trainees. The Generalized Anxiety Disorder-7 scale outcomes were stratified into 2 groups by composite score: <5 and ≥5 (indicating at least mild anxiety). A forward stepwise approach to factor selection was used and outcomes presented as odds ratios (ORs) and 95% confidence intervals. Statistical analyses were performed using SPSS v26 (IBM Corp, Arkmont, NY, USA) and Prism v8 (GraphPad Corp, San Diego, Calif, USA), with P < .05 considered statistically significant.
Results
Baseline demographics
In total, 1199 respondents participated in the international training survey. After excluding incomplete responses (n = 429, 35.8%), 770 trainees from 63 countries within 6 continents (Supplementary Table 2 and Supplementary Fig. 1, available online at www.giejournal.org) were included for analysis. Trainee characteristics and the differences across continents are presented in Table 1 .
Table 1.
Baseline characteristics of trainees stratified by continent
| Total (n = 770) |
North America (n = 205) |
Europe (n = 323) |
Australia/New Zealand (n = 40) |
Asia (n = 90) |
South America (n = 99) |
Africa (n = 13) |
P value | |
|---|---|---|---|---|---|---|---|---|
| Mean age, y (standard error) | 32.6 (.2) | 32.4 (.2) | 32.4 (.3) | 33.0 (.7) | 33.4 (.8) | 32.3 (.5) | 36.6 (1.5) | .11 |
| Male | 417 (56.9) | 115 (59.9) | 157 (50.5) | 26 (66.7) | 67 (80.7) | 45 (46.4) | 7 (63.6) | <.001 |
| Specialty | <.001 | |||||||
| Adult GI | 603 (78.3) | 152 (74.2) | 274 (84.8) | 32 (80.0) | 81 (90.0) | 55 (55.6) | 9 (69.2) | |
| Internal medicine | 24 (3.1) | 1 (.5) | 15 (4.6) | 1 (2.5) | 2 (2.2) | 3 (2.0) | 2 (15.4) | |
| Pediatric GI | 76 (9.9) | 52 (25.4) | 6 (1.9) | 0 (.0) | 6 (6.7) | 12 (12.1) | 0 (.0) | |
| Surgery | 59 (7.7) | 0 (.0) | 27 (8.4) | 7 (17.5) | 1 (1.1) | 22 (22.2) | 2 (15.4) | |
| Other | 8 (1.0) | 0 (.0) | 1 (.3) | 0 (.0) | 0 (.0) | 7 (7.1) | 0 (.0) | |
| Mean years of training (standard error) | 2.7 (.1) | 2.0 (.1) | 3.2 (.1) | 1.9 (.2) | 2.5 (.3) | 2.6 (.3) | 4.8 (1.5) | <.001 |
| Advanced endoscopy-focused training (vs general GI) | 135 (17.5) | 9 (4.9) | 57 (17.7) | 7 (17.5) | 22 (24.4) | 35 (35.4) | 5 (38.5) | <.001 |
Values are n (%) unless otherwise defined. All percentages are based on the number of respondents per question.
The top 3 countries of respondents were the United States (n = 169), United Kingdom (n = 132), and Spain (n = 82). The mean age of respondents was 32.6 (standard error, .2), with a male-to-female preponderance (56.9% vs 43.1%). Respondent specialties were adult gastroenterology (78.3%), pediatric gastroenterology (9.9%), surgery (7.7%), internal medicine (3.1%), and other (1.0%). The main focus of endoscopy training consisted of upper GI endoscopy (87.5%), lower GI endoscopy (83.1%), ERCP (20.4%), and EUS (13.0%).
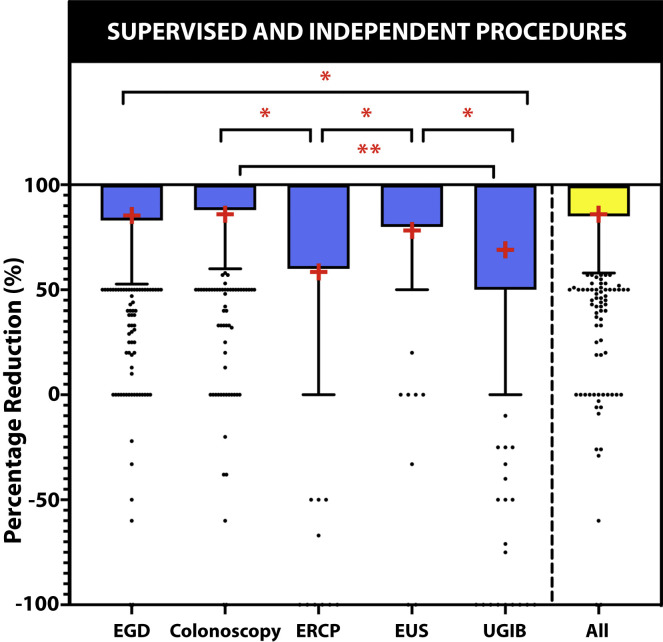
Impact of COVID-19 on trainee procedural volumes
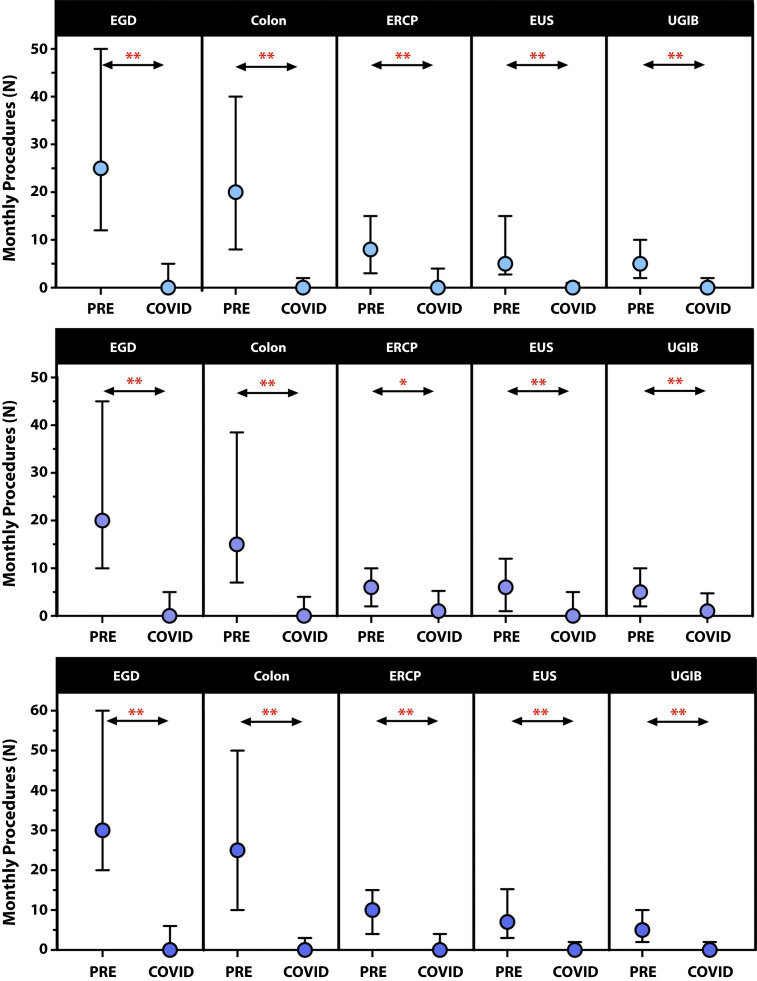
Overall, 770 trainees (93.8%) reported a reduction in their monthly endoscopy case volume attributable to COVID-19. By procedure type, the differences in estimated monthly volumes before and during COVID-19 are presented in Figure 1 , with significant (P < .0001) decrements over the two 30-day periods. Across all modalities (Fig. 2 ), the median percentage reduction in procedural volume was 99% (IQR, 85%-100%). This did not vary significantly by trainee specialty (P = .658) or whether procedures were performed under supervision or independently (P = .614) but varied by procedure type (P < .001). On subgroup analysis, percentage reductions were greater for colonoscopy (median, 100%; IQR, 88%-100%) compared with ERCP (median, 100%; IQR, 60%-100%; P = .003) and upper GI bleeding procedures (median, 100%; IQR, 50%-100%; P < .001). This outcome also varied across continents (P < .001), with significantly greater percentage reductions observed in Europe (median, 100%; IQR, 91%-100%) and North America (median, 99%; IQR, 88%-100%) compared with Asia (median, 87%; IQR, 75%-97%) and South America (median, 91%; IQR, 70%-100%).
Figure 1.
Comparison of trainee-reported number of supervised procedures (A), independent procedures (B), and total procedures (C) in the 30-day period before (PRE) and during COVID-19 (COVID). Symbols and error bars represent the median and interquartile ranges. ∗.0001 < P < .05, ∗∗P < .0001. Colon, Colonoscopy; UGIB, upper GI bleeding hemostasis.
Figure 2.
Box-and-whisker plots illustrating the percentage reduction in total (supervised and independent) procedures performed by trainees during the COVID-19 pandemic. Boxes cover medians and lower interquartile range, whereas the whiskers represent the lower 90th percentile. The mean percentage reduction is indicated by +. ∗.0001 < P < .05, ∗∗P < .0001. UGIB, Upper GI bleeding hemostasis.
Barriers to training
Of the 770 trainees (93.8%) who reported a reduction in endoscopy procedural volumes during the COVID-19 study period, the reasons cited included changes to institutional policy to exclude trainees from procedures (79.9%), lack of cases (58.3%), shortage of available PPE (28.8%), redeployment to another clinical area (24.0%), and personal reasons (10.2%). Access to endoscopy training remained accessible on an ad hoc basis to 60.5% of trainees (n = 466), with rates varying internationally (Table 2 ). Of these, 36.1% (n = 168) could perform endoscopy on patients at low risk or negative for COVID-19 and 7.9% (n = 37) on unsupervised procedures only; 46.7% (n = 359) reported access to ad hoc emergency cases and 15.4% (n = 119) to intensive care unit cases. Only 6.2% (n = 29) reported no restrictions on their endoscopy privileges. Reductions in institutional endoscopy case volume because of COVID-19 were reported by 98.2% of trainees, with 73.5% of trainees reporting a decrease of ≥50% and 3.6% reporting the cancellation of all endoscopy activity.
Table 2.
Impact of COVID-19 on endoscopy training stratified by continent
| Total (n = 770) |
North America (n = 205) |
Europe (n = 323) |
Australia/New Zealand (n = 40) |
Asia (n = 90) |
South America (n = 99) |
Africa (n = 13) |
P value | |
|---|---|---|---|---|---|---|---|---|
| Reduced endoscopy exposure | 722 (93.8) | 201 (98.1) | 302 (93.5) | 38 (95.0) | 86 (95.6) | 82 (82.8) | 13 (100.0) | <.001 |
| Endoscopy opportunities available | ||||||||
| None (no endoscopy) | 304 (39.5) | 80 (39.0) | 166 (51.4) | 20 (50.0) | 17 (18.9) | 18 (18.2) | 3 (23.0) | <.001 |
| No restrictions | 29 (3.8) | 4 (2.0) | 14 (4.3) | 5 (12.5) | 4 (4.4) | 1 (1.0) | 1 (7.7) | .02 |
| Unsupervised cases | 40 (5.2) | 3 (1.5) | 19 (5.9) | 3 (7.5) | 9 (10.0) | 4 (4.0) | 2 (15.3) | .02 |
| Only low-risk/negative COVID patients | 174 (22.6) | 66 (32.2) | 34 (10.5) | 10 (25.0) | 28 (31.1) | 32 (32.3) | 4 (30.8) | <.001 |
| Change in institutional endoscopy volume | <.001 | |||||||
| Decreased 1%-24% | 13 (1.7) | 1 (.5) | 3 (1.0) | 1 (2.5) | 3 (3.4) | 5 (5.2) | 0 (.0) | |
| Decreased 25%-49% | 61 (8.1) | 10 (4.9) | 23 (7.3) | 8 (20.0) | 13 (14.8) | 6 (6.2) | 1 (8.3) | |
| Decreased 50%-74% | 211 (28.0) | 37 (18.2) | 94 (29.8) | 19 (47.5) | 31 (35.2) | 26 (26.8) | 4 (33.3) | |
| Decreased 75%-99% | 327 (43.3) | 114 (56.2) | 130 (41.3) | 7 (17.5) | 35 (39.8) | 36 (37.1) | 5 (41.7) | |
| Decreased 100% | 28 (3.7) | 3 (1.5) | 15 (4.8) | 0 (.0) | 1 (1.1) | 8 (8.3) | 1 (8.3) | |
| Not affected | 14 (1.9) | 3 (1.5) | 5 (1.6) | 0 (.0) | 1 (1.1) | 5 (5.2) | 0 (.0) | |
| Decreased (unknown) | 101 (13.4) | 35 (17.2) | 45 (14.3) | 5 (12.5) | 4 (4.6) | 11 (11.3) | 1 (8.3) | |
| Mean % reduction in procedures per month during COVID-19 (standard error) | ||||||||
| EGD | 85.3 (1.3) | 90.4 (1.1) | 89.6 (1.2) | 78.2 (5.3) | 81.9 (2.5) | 65.1 (9.4) | 78.6 (5.9) | <.001 |
| Colonoscopy | 85.8 (2.6) | 92.1 (1.1) | 90.1 (1.4) | 76.7 (5.9) | 79.2 (2.8) | 59.8 (2.4) | 83.7 (6.2) | <.001 |
| ERCP | 70.5 (4.2) | 70.0 (9.5) | 72.4 (6.9) | 63.3 (1.7) | 65.1 (9.6) | 71.8 (8.3) | 88.9 (.1) | .99 |
| EUS | 78.2 (7.7) | 56.3 (2.6) | 82.6 (4.4) | 85.0 (7.2) | 94.3 (3.1) | 94.4 (3.9) | 100.0 (.0) | .60 |
| All | 86.2 (1.2) | 90.1 (1.1) | 90.0 (1.2) | 78.7 (5.2) | 81.4 (2.4) | 69.4 (8.5) | 80.9 (5.6) | <.001 |
| PPE adequate in endoscopy unit | 476 (67.6) | 154 (79.4) | 218 (73.9) | 27 (69.2) | 47 (61.0) | 27 (31.0) | 3 (25.0) | <.001 |
| Taken off work for COVID-19–related reasons | 168 (23.9) | 24 (12.4) | 91 (30.9) | 4 (10.3) | 18 (23.7) | 24 (27.6) | 7 (58.3) | <.001 |
Values are n (%) unless otherwise defined. All percentages are based on the number of respondents per question.
PPE, personal protective equipment.
Personal protective equipment
Regarding PPE, 73.7% (n = 520) received training on the use of PPE for COVID-19 patients, and 50.5% (n = 356) received training specific to managing COVID-19 in their endoscopy unit. This was mainly delivered through face-to-face teaching (34.0%, n = 121), virtual teaching (22.4%, n = 80), or written communication (43.5%, n = 155). The level of PPE used within the endoscopy unit was believed to be adequate in 67.6% (n = 476), but this varied internationally (P < .001) (Table 2); 47.0% (n = 331) believed that a lack of PPE was contributory to reductions in institutional endoscopy case volume. Endoscopy-specific practice guidelines on PPE use were available for 89.2% of respondents (628). PPE policy within the endoscopy unit was predominantly directed by national guidelines (47.4%), individual unit/hospital policy (33.0%), or international guidelines (19.6%).
Physical and mental well-being
Concerns on training
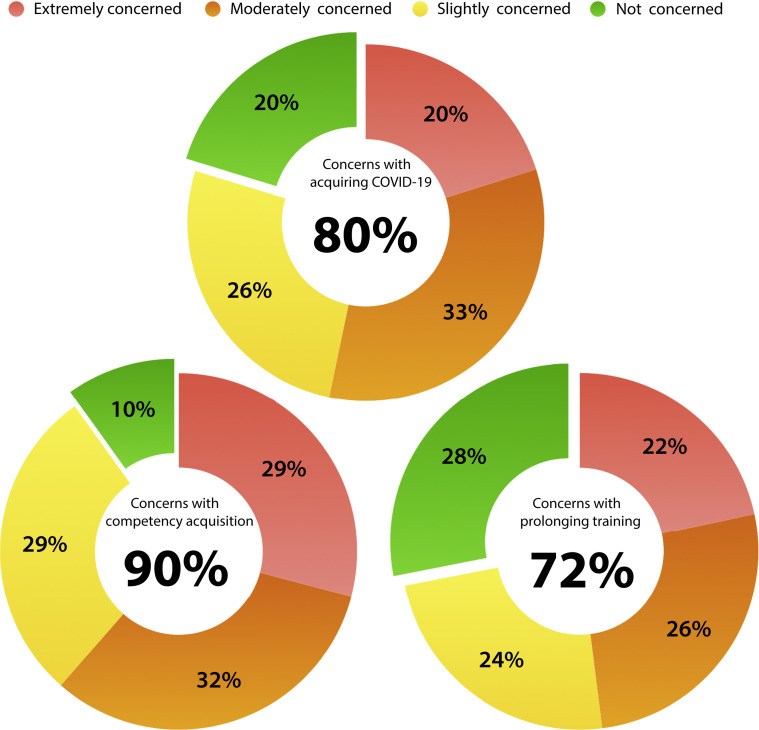
Trainees were asked to rate their level of concern regarding the impact of COVID-19 on the outcome of their endoscopy training (Table 3 , Fig. 3 ). Concerns with competency development were raised by 90.1% of trainees (n = 629) across continents (P = .844). Concerns regarding the need to prolong specialty training to reach the required competency were raised by 71.9% of respondents (n = 502). This concern varied internationally (P < .001), with the lowest proportion of concerned trainees in North America (49.5%). In total, 68.9% of trainees (n = 472) believed that existing national/international guidelines should be modified to better support endoscopy training during the COVID-19 pandemic.
Table 3.
Impact of COVID-19 on trainee well-being and on the use of alternate endoscopy education resources, stratified by continent
| Total (n = 770) |
North America (n = 205) |
Europe (n = 323) |
Australia/New Zealand (n = 40) |
Asia (n = 90) |
South America (n = 99) |
Africa (n = 13) |
P value | |
|---|---|---|---|---|---|---|---|---|
| Concerns | ||||||||
| Acquiring COVID-19 | 618 (88.3) | 187 (96.4) | 228 (78.1) | 36 (92.3) | 75 (98.7) | 82 (94.3) | 10 (83.3%) | <.001 |
| Competency development | 629 (90.1) | 176 (89.3) | 260 (89.3) | 34 (87.2) | 68 (90.7) | 79 (90.8) | 12 (100) | .844 |
| Prolonging training | 502 (71.9) | 96 (49.5) | 230 (79) | 33 (84.6) | 55 (73.3) | 78 (89.7) | 10 (83.3) | <.001 |
| Calls for changes to guidelines to support training | 472 (68.9) | 133 (69.3) | 175 (61.4) | 29 (74.4) | 56 (75.7) | 68 (81.0) | 11 (100) | .001 |
| Anxiety | .164 | |||||||
| None | 311 (44.7) | 86 (44.3) | 127 (44.1) | 22 (56.4) | 39 (52.0) | 32 (36.8) | 5 (41.7) | |
| Mild | 231 (33.2) | 61 (31.4) | 104 (36.1) | 14 (35.9) | 21 (28.0) | 30 (34.5) | 1 (8.3) | |
| Moderate | 99 (14.2) | 29 (14.9) | 39 (13.5) | 2 (5.1) | 11 (14.7) | 14 (16.1) | 4 (33.3) | |
| Severe | 54 (7.8) | 18 (9.3) | 18 (6.3) | 1 (2.6) | 5 (5.3) | 11 (12.6) | 2 (16.7) | |
| Burnout | 130 (18.8) | 42 (21.8) | 53 (18.4) | 1 (2.6) | 12 (16.0) | 18 (20.7) | 4 (36.4) | .058 |
| Institutional support | 467 (67.4) | 175 (90.7) | 195 (67.7) | 27 (69.2) | 41 (54.7) | 25 (28.7) | 4 (36.4) | <.001 |
Values are n (%). All percentages are based on the number of respondents per question.
Figure 3.
Concerns raised by endoscopy trainees attributable to the COVID-19 pandemic.
Physical health impact of COVID-19
Concerns of acquiring COVID-19 were expressed by 79.3% of trainees (Fig. 3). In total, 23.9% (n = 168) reported taking time off work for COVID-19–related reasons; 76.8% (n = 129) took time off for themselves and the remaining 23.4% (n = 39) for a household member. Of trainees affected, 14.7% (n = 19) tested positive, 52.7% (n = 68) negative, 30.2% (n = 39) were not tested, and 2.3% (n = 3) preferred not to answer.
Anxiety and burnout
Anxiety and burnout were assessed in 695 trainees (Table 3). The following anxiety levels were reported according to Generalized Anxiety Disorder-7 criteria: no anxiety (47.6%, n = 331), mild (33.2%, n = 231), moderate (14.2%, n = 99), and severe anxiety (7.8%, n = 54). On multivariable analysis (Table 4 ), factors associated with anxiety in trainees included female gender (OR, 2.15; P < .001), adequacy of PPE (OR 1.75, P = .005), concerns over prolongation of training (OR, 1.60; P = .013), and lack of availability of institutional support for emotional health (OR, 1.67; P = .008). Up to 18.8% of trainees met the criteria for burnout; burnout correlated positively with the severity of anxiety (Supplementary Fig. 2, available online at www.giejournal.org). Institutional provision of emotional support strategies during the COVID-19 pandemic was available to 67.4% of trainees (n = 467).
Table 4.
Multivariable analysis of factors associated with anxiety in endoscopy trainees
| Factor | No. of cases | Anxiety (%) | Univariable analysis |
Multivariable analysis |
||
|---|---|---|---|---|---|---|
| Odds ratio (95% confidence interval) | P value | Odds ratio (95% confidence interval) | P value | |||
| Trainee age | ||||||
| Per year | N/A | 1.01 (.98-1.05) | .577 | |||
| Sex | ||||||
| Male | 288 | 46.8 | Reference | |||
| Female | 380 | 66.0 | 2.20 (1.64-3.02) | <.001∗ | 2.15 (1.52-3.05) | <.001∗ |
| Region | ||||||
| North America | 194 | 55.7 | Reference | |||
| Europe | 288 | 55.9 | 1.01 (.70-1.46) | .960 | ||
| South America | 87 | 63.2 | 1.37 (.81-2.30) | .237 | ||
| Australia | 39 | 43.6 | .62 (.31-1.23) | .170 | ||
| Asia | 75 | 48.0 | .74 (.43-1.25) | .259 | ||
| Africa | 12 | 58.3 | 1.12 (.34-3.64) | .857 | ||
| Years in training | ||||||
| Per year | N/A | .96 (.89-1.02) | .170 | |||
| Specialty | ||||||
| Surgery | 50 | 56.0 | Reference | |||
| Adult GI | 546 | 54.0 | .92 (.52-1.66) | .789 | ||
| Internal medicine | 20 | 70.0 | 1.83 (.60-5.55) | .283 | ||
| Pediatric GI | 73 | 57.5 | 1.07 (.52-2.20) | .866 | ||
| Other | 6 | 83.3 | 3.93 (.43-36.12) | .227 | ||
| Reduced endoscopy exposure | ||||||
| Yes | 654 | 55.8 | Reference | |||
| No | 41 | 46.3 | .68 (.36-1.29) | .239 | ||
| Redeployment | ||||||
| No | 536 | 58.5 | Reference | |||
| Yes | 159 | 54.3 | 1.19 (.83-1.70) | .350 | ||
| Perceived adequacy of PPE | ||||||
| Yes | 471 | 50.3 | Reference | |||
| No | 224 | 65.6 | 1.89 (1.36-2.62) | <.001 | 1.75 (1.18-2.57) | .005∗ |
| Training on PPE | ||||||
| Yes | 513 | 54.0 | Reference | |||
| No | 182 | 58.8 | 1.22 (.86-1.71) | .264 | ||
| Time off work because of COVID-19 | ||||||
| No | 528 | 54.5 | Reference | |||
| Yes | 167 | 57.5 | .89 (.63-1.26) | .506 | ||
| Concerns with developing COVID-19 | ||||||
| No | 81 | 51.9 | ||||
| Yes | 614 | 55.7 | 1.17 (.73-1.86) | .513 | ||
| Concerns with competency acquisition | ||||||
| No | 69 | 43.5 | ||||
| Yes | 626 | 56.5 | 1.69 (1.03-2.79) | .040∗ | ||
| Concerns with prolongation of training | ||||||
| No | 82 | 42.1 | Reference | |||
| Yes | 302 | 60.4 | 2.10 (1.50-2.94) | <.001∗ | 1.60 (1.10-2.32) | .013∗ |
| Availability of institutional support for emotional / mental health | ||||||
| Yes | 467 | 50.7 | Reference | |||
| No | 226 | 64.2 | 1.74 (1.25-2.41) | .001∗ | 1.67 (1.14-2.45) | .008∗ |
PPE, Personal protective equipment; N/A, not appropriate.
P < .05.
Discussion
To our knowledge, this is the first study to comprehensively evaluate the impact of COVID-19 on endoscopy trainees. Survey responses from 770 trainees across 63 countries indicated that COVID-19 has had a profound adverse effect on endoscopy volume worldwide, with reductions in training opportunities for most trainees (93.8%) and a drastic median reduction in case volume of 99% (IQR, 85%-100%). This has raised concerns among trainees in regard to competency development (90%) and the potential need to prolong training to achieve endoscopic competence (72%). These concerns were among the cited factors leading to COVID-19–associated anxiety (52.4%) and burnout (18.8%) among trainees. These results highlight the urgent call to action for institutions, training programs, GI societies, and accreditation councils to address the 2 overarching issues identified: reductions in endoscopic training opportunities and the emotional welfare of trainees.
The emphasis on minimum endoscopy procedure numbers as a competence safeguard is ubiquitous across international training settings.14 These serve to indicate readiness for certification, credentialing, and program completion. Although training in all procedures was disrupted by COVID-19, the decrement was most pronounced for colonoscopy and less so for emergency procedures (ERCP and GI bleeding). This is important because colonoscopy is regarded as a core endoscopic skill. Over 50% of trainees estimated a reduction in institutional endoscopy volumes of 75% or more, in line with international recommendations to curb elective procedures. However, the exclusion of trainees was another major barrier, with PPE shortages and redeployment being contributory. The significant impact of COVID-19 has raised doubts among trainees over whether endoscopic competence in various procedures is realistically achievable within the duration of their training, with a substantial proportion expressing concerns that training will need to be prolonged. Addressing these issues could potentially have disruptive implications at many levels: restructuring of training curricula and schedules, redistribution of endoscopy cases between junior and senior trainees, delays in entering the workforce, financial strain, and negative effects on trainees’ mental well-being.
Indeed, relatively little has been published on the physical and mental well-being of endoscopy trainees, even before COVID-19. From our survey, COVID-19 affected trainees beyond reductions in endoscopy training opportunities: 79.3% had concerns of acquiring COVID-19, and a significant proportion of trainees had to take time off work for COVID-19–related reasons. Inadequate PPE was raised as a concern by a third of respondents and was independently associated with increased anxiety. Overall, 52.4% of trainees met criteria for at least mild generalized anxiety, with 22.0% reaching a threshold score of ≥10, which has 89% sensitivity and 82% specificity for clinically significant anxiety.12 , 15 Predictors of anxiety included female gender (consistent with population-based studies),16 concerns regarding prolongation of training, inadequate PPE, and a lack of emotional and mental health support. Anxiety levels positively correlated with burnout, which was identified in 18.8% of trainees. Burnout is a consequence of unmitigated chronic stress that requires urgent intervention because it can lead to emotional exhaustion, depersonalization, negativity, and impaired professional performance,17 including suboptimal medical care and medical error.18 , 19 The association between the availability of emotional support and lower anxiety levels suggests that training programs should strongly consider implementing support strategies to proactively address anxiety and burnout in trainees and promote their well-being. Formalized interventions to improve trainee well-being, such as group stress management and resiliency training, may also play a positive role in improving job satisfaction and well-being.16 , 20, 21, 22 Additionally, attending gastroenterologists need to proactively engage with trainees to discuss their learning gaps and career development and devise individualized curricula.
Internationally, there was significant heterogeneity in survey responses for both primary and secondary outcomes (Table 1, Table 2, Table 3). These may be partially explained by locoregional differences in severity and the phase of the COVID-19 pandemic during the survey period. Nearly 50% of respondents were from the United States, United Kingdom, and Spain, which were in the acceleration to plateau phase in the 30 days leading up to the survey.23 This is likely to account for the reductions in exposure to endoscopy training, institutional caseloads, uptake of PPE, and time off work from COVID-19. It is possible that as COVID-19 caseloads subside, training opportunities will slowly resume, although trainee exposure is still likely to be impacted because of prolonged turnaround times for decontamination and demand for PPE, in addition to the possibility of further disruptions during the “second wave.” This may be related to global inequalities in health care, as evidenced by variations in availability of PPE, with adequate PPE reported by 79% of North American trainees but only 31% of South American trainees. The structure of training programs is another relevant factor. Although concerns over competency development was consistent globally (P = .84), concerns over prolongation of training varied (P < .001). This may reflect differences in training systems and accreditation policies across countries.
Our study has several limitations. Surveys are vulnerable to bias and misinterpretation inherently. Data validation was performed by excluding respondents who provided incomplete responses of primary outcome data, did not indicate a training modality, and where endoscopy numbers performed each month in a given modality exceeded 100. It was also not possible to estimate the response rate because the survey was disseminated through multiple national and international societies and organizations. Not all countries and specialties were represented, which might affect the generalizability of findings. Next, our data provide a snapshot of training in time and were not matched to regional differences in pandemic activity. Our completion rate was limited at 65%, with a further dropout rate of 11% for completing all survey questions. Contributory factors include the length of the survey, complexity of individual questions, and dissemination only in English, which may have affected comprehension. Additional data, such as unit-level information and lifetime procedure counts, were not collected. Finally, baseline data for anxiety and burnout could not be retrospectively captured in a valid manner, and therefore the high rates of anxiety cannot be directly attributed to COVID-19 alone.
The effects of COVID-19 are projected to persist until at least 2022.24 As such, an urgent review of endoscopy training is warranted to adapt accordingly and provide direction. In our survey, 68.9% of respondents indicated that guidelines should be modified to support training. Training programs should openly recognize that minimum procedural numbers may not be achievable in some countries and adopt mitigation strategies. First, emphasis should shift toward maximizing gains from evidence-based, hands-off training interventions. For beginners, simulation-based training can be used to develop technical25 , 26 and nontechnical skills27 and to accelerate time to achievement of competence.28 Although simulation training requires performance feedback to be optimally effective,29 self-assessment with benchmark videos and computerized feedback are viable alternatives.30 , 31 For all trainees, cognitive competencies can be developed through distance education using educational resources, webinars, and open access social media education, such as structured conversations on Twitter.32 All 3 major American GI societies have high-quality, expert-led, endoscopy training videos, notably the American Society for Gastrointestinal Endoscopy with its catalogue of education materials in GI Leap and online learning platform.32 , 33 Second, determination of competence should rely less on attaining minimum numbers and more on the use of objective and validated methods of competency assessment. This is best achieved through the use of objective performance tools with strong validity evidence, such as the Assessment of Competency in Endoscopy,34 Direct Observation of Procedural Skills,35, 36, 37 and the Gastrointestinal Endoscopy Competency Assessment Tool,38 which can allow trainers to target feedback provision in a formative manner and to benchmark global competence for summative sign-off.35 Despite these measures, it may be necessary for some trainees to extend their endoscopy training.39 Additionally, it will be important for institutions and private practices to ensure that new faculty are closely mentored to promote continued skills development. With meaningful application of evidence-based training paradigms, the GI community can mitigate the ongoing impact of COVID-19 on trainees and ensure that they achieve the cognitive, technical, and integrative competencies needed for independent endoscopic practice.
The recent literature on the impact of COVID-19 on trainees stems from individual experiences and expert opinion.10 , 33 Our trainee-centered survey has now quantified the impact of COVID-19 on procedural volumes and on the well-being of endoscopy trainees and shown how this varies internationally across different continents. As countries engage in collaborative endeavors to tackle the global impact of COVID-19, we hope that our findings will help to inform future strategies to mitigate the impact of the pandemic on endoscopy training.
In conclusion, worldwide, the COVID-19 pandemic has led to drastic reductions in endoscopy volumes performed by trainees, which is causing concerns regarding competency development and possible prolongation of training. This has precipitated anxiety and burnout among trainees. Institutions, program directors, and GI societies should provide clarity on curricular requirements and support the educational and emotional needs of trainees during this challenging time.
In this article, we aimed to assess the impact of COVID-19 on procedural volumes and the emotional well-being of endoscopy trainees worldwide. Our study showed that the COVID-19 pandemic has led to drastic reductions in endoscopic volumes and restrictions on endoscopy training, with detrimental effects on trainee well-being, including high rates of anxiety and burnout among trainees worldwide. Therefore, existing curricular requirements and delivery of endoscopy training should be urgently reviewed and adapted to support the educational and emotional needs of trainees during the COVID-19 pandemic.
Footnotes
DISCLOSURE: The following authors disclosed financial relationships: R. Khan: ResearchsupportfromAbbvie,Ferring Pharmaceuticals, and Pendopharm. M. Żorniak: ResearchsupportfromUnited European Gastroenterology. S. C. Grover: Researchsupportfrom Abbvie, Ferring Pharmaceuticals, Pendopharm, Janssen, and Takeda; personalfeesfrom Lupin Pharmaceuticals. All other authors disclosed no financial relationships.
See CME section, p. 960.
If you would like to chat with an author of this article, you may contact Dr Siau at keithsiau@nhs.net.
Supplementary data
References
- 1.Repici A., Maselli R., Colombo M. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest Endosc. 2020;92:192–197. doi: 10.1016/j.gie.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lui R.N., Wong S.H., Sánchez-Luna S.A. Overview of guidance for endoscopy during the coronavirus disease 2019 pandemic. J Gastroenterol Hepatol. 2020;35:749–759. doi: 10.1111/jgh.15053. [DOI] [PubMed] [Google Scholar]
- 3.Chiu P.W.Y., Ng S.C., Inoue H. Practice of endoscopy during COVID-19 pandemic: position statements of the Asian Pacific Society for Digestive Endoscopy (APSDE-COVID statements) Gut. 2020;69:991–996. doi: 10.1136/gutjnl-2020-321185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sultan S., Lim J.K., Altayar O. AGA Institute rapid recommendations for gastrointestinal procedures during the COVID-19 pandemic. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.03.072. Epub 2020 Mar 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gralnek I.M., Hassan C., Beilenhoff U. ESGE and ESGENA Position Statement on gastrointestinal endoscopy and the COVID-19 pandemic. Endoscopy. 2020;52:483–490. doi: 10.1055/a-1155-6229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Repici A., Pace F., Gabbiadini R. Endoscopy units and the COVID-19 outbreak: a multi-center experience from Italy. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.04.003. Epub 2020 Apr 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forbes N., Smith Z.L., Spitzer R.L. Changes in gastroenterology and endoscopy practices in response to the COVID-19 pandemic: results from a North American survey. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.04.071. Epub 2020 May 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rambaldini G., Wilson K., Rath D. The impact of severe acute respiratory syndrome on medical house staff: a qualitative study. J Gen Intern Med. 2005;20:381–385. doi: 10.1111/j.1525-1497.2005.0099.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong S.H., Lui R.N., Sung J.J. Covid-19 and the digestive system. J Gastroenterol Hepatol. 2020;35:744–748. doi: 10.1111/jgh.15047. [DOI] [PubMed] [Google Scholar]
- 10.Shah R., Satyavada S., Ismail M. COVID-19 pandemic through the lens of a gastroenterology fellow: looking for the silver lining. Gastrointest Endosc. 2020 doi: 10.1016/j.gie.2020.03.3852. Epub 2020 Apr 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palchaudhuri S., Gabre J., Prenner S. Adapting a GI fellowship to a pandemic: novel approaches to accommodating a novel virus. Dig Dis Sci. 2020;65:1562–1565. doi: 10.1007/s10620-020-06306-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spitzer R.L., Kroenke K., Williams J.B.W. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 13.Dolan E.D., Mohr D., Lempa M. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern Med. 2015;30:582–587. doi: 10.1007/s11606-014-3112-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Siau K., Hawkes N.D., Dunckley P. Training in endoscopy. Curr Treat Options Gastroenterol. 2018;16:345–361. doi: 10.1007/s11938-018-0191-1. [DOI] [PubMed] [Google Scholar]
- 15.Rutter L.A., Brown T.A. Psychometric properties of the Generalized Anxiety Disorder Scale-7 (GAD-7) in outpatients with anxiety and mood disorders. J Psychopathol Behav Assess. 2017;39:140–146. doi: 10.1007/s10862-016-9571-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stein M.B., Sareen J. Clinical practice. Generalized anxiety disorder. N Engl J Med. 2015;373:2059–2068. doi: 10.1056/NEJMcp1502514. [DOI] [PubMed] [Google Scholar]
- 17.Rotenstein L.S., Torre M., Ramos M.A. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320:1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.West C.P., Dyrbye L.N., Shanafelt T.D. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283:516–529. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- 19.Amir M., Dahye K., Duane C. Medical student and resident burnout: a review of causes, effects, and prevention. J Fam Med Dis Prev. 2018;4:094. [Google Scholar]
- 20.Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020 doi: 10.1001/jama.2020.3972. Epub 2020 Mar 12. [DOI] [PubMed] [Google Scholar]
- 21.Chaukos D., Chad-Friedman E., Mehta D.H. SMART-R: a prospective cohort study of a resilience curriculum for residents by residents. Acad Psychiatry. 2018;42:78–83. doi: 10.1007/s40596-017-0808-z. [DOI] [PubMed] [Google Scholar]
- 22.West C.P., Dyrbye L.N., Rabatin J.T. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174:527–533. doi: 10.1001/jamainternmed.2013.14387. [DOI] [PubMed] [Google Scholar]
- 23.Johns Hopkins University COVID-19 map. Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html Available at:
- 24.Kissler S.M., Tedijanto C., Goldstein E. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368:860–868. doi: 10.1126/science.abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grover S.C., Garg A., Scaffidi M.A. Impact of a simulation training curriculum on technical and nontechnical skills in colonoscopy: a randomized trial. Gastrointest Endosc. 2015;82:1072–1079. doi: 10.1016/j.gie.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 26.Grover S.C., Scaffidi M.A., Khan R. Progressive learning in endoscopy simulation training improves clinical performance: a blinded randomized trial. Gastrointest Endosc. 2017;86:881–889. doi: 10.1016/j.gie.2017.03.1529. [DOI] [PubMed] [Google Scholar]
- 27.Walsh C.M., Scaffidi M.A., Khan R. A non-technical skills curriculum incorporating simulation-based training improves performance in colonoscopy among novice endoscopists: a randomized controlled trial. Dig Endosc. 2020 doi: 10.1111/den.13623. Epub 2020 Jan 7. [DOI] [PubMed] [Google Scholar]
- 28.Siau K., Hodson J., Neville P. Impact of a simulation-based induction programme in gastroscopy on trainee outcomes and learning curves. World J Gastrointest Endosc. 2020;12:98–110. doi: 10.4253/wjge.v12.i3.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kruglikova I., Grantcharov T.P., Drewes A.M. The impact of constructive feedback on training in gastrointestinal endoscopy using high-fidelity virtual-reality simulation: a randomised controlled trial. Gut. 2010;59:181–185. doi: 10.1136/gut.2009.191825. [DOI] [PubMed] [Google Scholar]
- 30.Scaffidi M.A., Walsh C.M., Khan R. Influence of video-based feedback on self-assessment accuracy of endoscopic skills: a randomized controlled trial. Endosc Int Open. 2019;7:E678–E684. doi: 10.1055/a-0867-9626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vilmann A.S., Norsk D., Svendsen M.B.S. Computerized feedback during colonoscopy training leads to improved performance: a randomized trial. Gastrointest Endosc. 2018;88:869–876. doi: 10.1016/j.gie.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 32.American Society for Gastrointestinal Endoscopy American Society for Gastrointestinal Endoscopy: guidance for trainees during the COVID-19 pandemic. Gastrointest Endosc. 2020 doi: 10.1016/j.gie.2020.05.032. Epub 2020 May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Keswani R.N., Sethi A., Repici A. How to maximize trainee education during the COVID-19 pandemic: perspectives from around the world. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.05.012. Epub 2020 May 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.ASGE Training Committee. Sedlack R.E., Coyle W.J. ASGE’s assessment of competency in endoscopy evaluation tools for colonoscopy and EGD. Gastrointest Endosc. 2014;79:1–7. doi: 10.1016/j.gie.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 35.Siau K., Crossley J., Dunckley P. Colonoscopy direct observation of procedural skills assessment tool for evaluating competency development during training. Am J Gastroenterol. 2020;115:234–243. doi: 10.14309/ajg.0000000000000426. [DOI] [PubMed] [Google Scholar]
- 36.Siau K., Dunckley P., Feeney M. ERCP assessment tool: evidence of validity and competency development during training. Endoscopy. 2019;51:1017–1026. doi: 10.1055/a-0991-0044. [DOI] [PubMed] [Google Scholar]
- 37.Siau K., Crossley J., Dunckley P. Direct observation of procedural skills (DOPS) assessment in diagnostic gastroscopy: nationwide evidence of validity and competency development during training. Surg Endosc. 2020;34:105–114. doi: 10.1007/s00464-019-06737-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Walsh C.M. In-training gastrointestinal endoscopy competency assessment tools: types of tools, validation and impact. Best Pract Res Clin Gastroenterol. 2016;30:357–374. doi: 10.1016/j.bpg.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 39.Siau K., Morris A.J., Murugananthan A. Variation in exposure to endoscopic haemostasis for acute upper gastrointestinal bleeding during UK gastroenterology training. Frontline gastroenterol. 2019 doi: 10.1136/flgastro-2019-101351. Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.