Abstract
Objective
The objective of this study was to investigate the impact of chronic low back pain (CLBP) on patients’ personal and professional lives, and management strategies applied to treat CLBP.
Methods
A 60‐question survey was developed, and respondents from 16 countries with a self‐reported physician's diagnosis of CLBP were recruited via an online market research survey panel. Respondents were stratified as having mild, moderate, or severe pain. Target sample sizes per country and for pain severity were set. Data were weighted according to the known population and prevalence of CLBP in each country and the number of respondents from that country.
Results
Results from 9642 CLBP patients indicated that almost a quarter of patients with severe CLBP report a psychological comorbidity. Prescription pain medications were more commonly used by patients with severe CLBP (56%) than those with mild (20%) or moderate (34%) CLBP. Among those with severe CLBP who had been prescribed pain medication, 58% were prescribed opioids, with 1 in 4 patients using opioids for more than 5 years. Patients were primarily managed by general practitioners/primary care physicians, physiotherapists, neurologists, or orthopedic surgeons. CLBP negatively impacted patients’ daily activities, social lives, and work productivity.
Conclusion
Chronic low back pain has pronounced effects on patients’ personal relationships, ability to work, and daily living. Almost 1 in four patients with severe CLBP reported a psychological comorbidity. Adherence to guidelines appears inconsistent, which is noteworthy as a substantial subgroup of patients with severe CLBP had been prescribed opioid medication for more than 5 years. Improved education is required to support healthcare professionals (HCPs) in identifying and understanding the complex biopsychosocial needs of CLBP patients to optimize pain management and to encourage referral of CLBP patients to physiotherapists and psychologists.
Keywords: biopsychosocial model, chronic low back pain, international patient survey, pain management, psychological comorbidity
INTRODUCTION
Low back pain is considered by the World Health Organization (WHO) as a disease of priority due to its prevalence and pervasive effect on most societies across the world. 1 Global chronic low back pain (CLBP) prevalence is currently estimated to be around 9%–10%. 2 , 3
Chronic low back pain represents a significant economic and societal burden. 1 , 4 , 5 It is the leading cause of work absence globally and affects work performance. 1 Some estimates place the direct and indirect costs of all chronic pain to be 3%–10% of various countries’ gross domestic product (GDP), 6 , 7 , 8 and for CLBP specifically, societal costs are estimated to be between €8000 and €19,000 per patient annually. 9
At a personal level, CLBP may negatively impact patients financially due to medical costs, as well as placing a substantial burden on patients’ physical health and mental well‐being, 10 causing them to experience a dramatically lower general quality of life, 5 , 11 , 12 , 13 , 14 increased risk of psychological comorbidities, 15 , 16 and even a shorter lifespan. 11 , 17
There is clear evidence that chronic pain has a significant societal and economic impact that causes individual suffering. 4 , 5 , 10 , 18 , 19 However, most studies investigating the individual impact of chronic pain are conducted at a pan‐European or individual country level, or are focused on cancer pain, 4 , 5 , 10 , 20 , 21 , 22 , 23 and the existing literature highlights that the understanding of the impact of chronic noncancer pain on patients is limited. In addition, chronic pain is frequently poorly managed and there are few proven effective treatment strategies; once chronic pain is established, it becomes notoriously difficult to treat. 24 Hence, more effective strategies that improve patients’ quality of life are needed; current approaches need to be reconsidered within the context of the pervasive impact of chronic pain on patients, which needs to be understood in more detail. Although CLBP is the most common type of chronic noncancer pain, to the best of our knowledge, there have not been large‐scale, international studies that investigate the holistic impact of CLBP on the individual, and the management and treatment strategies applied.
Consequently, the purpose of this international survey is to investigate the impact of CLBP on patients’ physical well‐being and their personal and professional lives, as well as to understand the treatment strategies in practice. To this end, an expert multidisciplinary steering committee panel was formed to develop an international survey investigating the personal and professional impact of CLBP experienced by a large population of patients across 16 countries.
METHODS
Survey development and design
The survey instrument was developed in collaboration with an international, multidisciplinary steering committee of paid consultants, consisting of healthcare professionals (HCPs): three pain specialists, a psychologist, a physiotherapist, and a nurse, five members representing patient organizations, as well as a health economist and an employer representative. The market research company, Ipsos SA, supported the development and execution of the survey.
Based on insights from the steering committee, a comprehensive survey instrument of 60 questions was devised comprising a screener (nine questions) and six core themes, including demographics (eight questions), diagnosis (four questions), treatment (13 questions), personal impact (13 questions), support and welfare (six questions), and employment (seven questions) (Table S1). The survey instrument included a combination of validated scales, newly designed questions, and free‐form text.
Using the Brief Pain Inventory (BPI), 25 patients rated their worst, least, current, and average pain severity over the previous 24 h on an 11‐point numeric rating scale. As part of the screener, respondents also reported their average pain over the past 7 days, and this was used to stratify respondents (with 0 = no pain, 1–3 = mild pain, 4–6 = moderate pain, and 7–10 = severe pain). In addition, the interference items of the BPI were used to assess interference of pain with daily activities, using a 0 (does not interfere) to 10 (completely interferes) response scale. The Stanford Presenteeism Scale (SPS‐6) 26 was used in 1 question to evaluate how employed patients felt their CLBP impacted their work performance and productivity.
The survey (including screening) was designed to allow completion within 25 min. Two chronic pain patient representatives from the steering committee vetted the survey to ensure it could be completed within the estimated time frame, instructions were clear, and the questions were understandable, relevant, and appropriate from a patient perspective.
Survey materials were initially developed in English. Once finalized, the documents were translated into each necessary language by the Ipsos SA vendor. The approved, country‐specific versions of the documents were scripted for each country separately.
For quality control purposes, a pilot survey was tested among a limited number of participants in each of the survey countries (approximately 10% of the relevant country sample size). No changes were made to the survey following pilot testing; therefore, data collected during pilot testing were included in the final analysis.
Survey methodology
Recruitment
The online survey was conducted in 16 countries (Australia, Belgium, Finland, France, Germany, Israel, Italy, Netherlands, Norway, Romania, Russia, Spain, Sweden, Switzerland, Turkey, and the United Kingdom) between March and June 2019. Respondents were recruited from panels of individuals who volunteered to take part in online market research surveys. The recruitment process was conducted in compliance with the necessary market research regulations at a country and European level—including the Market Research Society (MRS), European Pharmaceutical Market Research Association (EphMRA), European Society for Opinion and Marketing Research (ESOMAR), General Data Protection Regulation (GDPR), as well as the British Healthcare Business Intelligence Association (BHBIA) guidelines for UK‐based respondents. 27 , 28 , 29 , 30 In line with these guidelines, participant consent was obtained as part of the survey, ensuring compliance with GDPR and all ethical regulations, such as preserving confidentiality and allowing participants to withdraw from the survey at any time.
All participants were compensated for their time, with varied incentives depending on country‐specific rules by using a points system (based on fair market value in the relevant country) designed to eliminate bias or skewing of particular populations. 31
Sample
Target sample sizes were set for each country in order to ensure recruitment of the planned ratios of patients with mild or moderate to severe CLBP. The sample sizes were determined by a variety of factors including the feasibility per country (influenced by total population and population of CLBP patients), timings, and budget requirements. A combined sample target was set for patients with moderate or severe pain, rather than separate targets for each pain severity group. The aim was to have the biggest sample size possible (within budget and timing) to ensure a robust sample size at both a global and individual country level. The planned recruitment quotas for the total number of CLBP patients varied between 250 and 1000 patients per country depending on population size and specific requests (eg, country representatives from the funding companies requested a sample size of 1000 to support local data publication). The majority of countries had a planned quota of 500 patients.
Inclusion criteria were as follows: participants had to be ≥18 years of age, must not have completed a survey about CLBP in the 4 weeks prior, must have been experiencing low back pain for at least 12 weeks at the time of taking the survey, and must have reported that they had received a diagnosis of CLBP from a physician. An 11‐point numeric rating scale was used to assess average pain over the past 7 days, with those scoring 0 (indicating no pain) excluded from the survey. Respondents were screened at the start of the survey to include only those who fulfilled these inclusion criteria. In addition, the screener was designed to collect demographic data, including country, regions, and age, for which quotas were set. Once quotas were met, further qualifying respondents were barred from progressing to the survey.
Quality control
To ensure that only quality survey data were analyzed, criteria were applied to filter nonsensical and meaningless responses, including trick/red herring and straight liner tests, open‐end answers review, and monitoring respondent length of interview against survey length. Data from completed surveys that did not pass these controls, or were completed in under 3 min, were discarded.
Weighting
Weighting is a process of adjusting the influence of groups or sub‐groups within survey data so that the results reflect those of a defined population. Data were weighted according to the known population 32 and prevalence of CLBP in each country, and the number of survey respondents from that country — this ensured that when analyzing the results at a global level, countries with a bigger sample size were not over‐represented compared with countries with a smaller sample size. For non‐EU5 countries, prevalence data were not available, so the global average of 15% was used for the weighting of these countries. 1 Results shown indicate weighted percentages throughout and weighted counts in tables and figures.
Data protection
Patients’ answers were anonymized to ensure confidentiality and avoid bias during data collection and analysis. The survey was conducted in compliance with the MRS, EphMRA, ESOMAR, GDPR, as well as the BHBIA guidelines for UK‐based respondents.
Analysis
Data from 16 countries were collected via the online survey between March and June 2019, and descriptive statistical methods were applied for the totality, as well as for individual countries, using the Dimensions tool (as part of Unicom Intelligence solutions, previously known as IBM SPSS Data Collection and Dimensions). A confidence interval (CI) of 95% was applied, and analysis consisted of frequencies, means, medians, top two or three boxes, bottom two or three boxes (for scale and grid questions), and standard deviations. In each scenario (international and individual countries), patients were grouped by pain severity.
In addition, multiple cross‐tabs analyses and comparisons between different groups were also performed as per the descriptive data analysis to explore potential relationships between factors that could influence CLBP or patients’ attitudes and experiences.
The purpose of the survey was to better understand the impact of CLBP on patients’ lives, and descriptive data analysis was applied to achieve this.
RESULTS
Overview
Results reported here are focused on the impact of CLBP on patients’ personal and professional lives, and management strategies applied to treat patients. Interim survey results from 8990 patients from 14 countries covering the six survey themes were presented at the 2019 European Pain Federation, The Professional Society for Health Economics and Outcomes Research, and Societal Impact of Pain congresses. 33 , 34 , 35 , 36 , 37 , 38
Screening survey
Of the 120,361 people initially recruited, 21,911 passed the screening and began the survey, while 98,450 were screened out (Figure 1). The data from the 4321 respondents who were over quota, 7333 respondents who began the survey but did not complete it, and 615 respondents who did not pass quality control checks were not analyzed. Data were available for 9642 patients. The top 5 reasons for respondents to be screened out included not experiencing low back pain, not having CLBP (defined as low back pain for more than 12 weeks), not having a medical diagnosis of CLBP confirmed by a physician, being under 18 years of age, and having participated in a survey on CLBP in the last 4 weeks.
FIGURE 1.
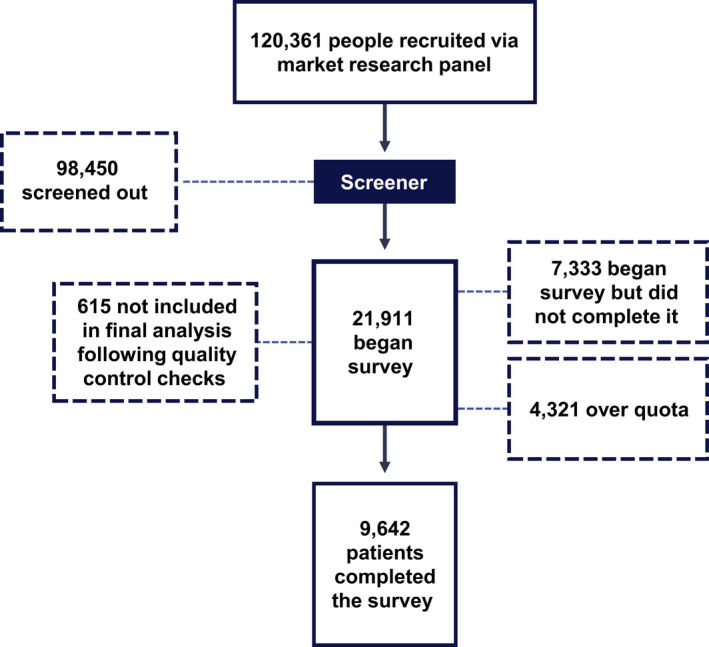
Design and results from screening survey
Patient characteristics
Baseline demographics
Forty‐six percent of respondents were female, and 54% were male. Most respondents were over 40 years old, and the mean age was 51 (Table 1). Of patients who completed the survey, 964 (10%) had mild CLBP, 4734 (49%) had moderate CLBP, and 3944 (41%) had severe CLBP. Results shown indicate weighted percentages throughout and weighted counts in tables and figures.
TABLE 1.
Baseline demographics of patients who completed the survey, and mean number of work days missed in an average month due to CLBP
| Pain severity | Total | |||
|---|---|---|---|---|
| Mild, weighted | Moderate, weighted | Severe, weighted | ||
| Total, % (N) | 100 (964) | 100 (4734) | 100 (3944) | 100 (9642) |
| Gender, % (n) | ||||
| Male | 66 (633) | 55 (2622) | 50 (1978) | 54 (5232) |
| Female | 34 (331) | 44 (2104) | 50 (1961) | 46 (4396) |
| Mean (SD) age, years | 52 (15.58) | 52 (4.85) | 50 (14.99) | 51 (15.01) |
| Registered disabled due to CLBP, % (n) | 14 (139) | 20 (940) | 34 (1333) | 25 (2431) |
| Main income earner, % (n) | ||||
| Yes | 68 (652) | 69 (3255) | 72 (2828) | 70 (6734) |
| No | 31 (295) | 30 (1418) | 28 (1088) | 29 (2801) |
| Don't know | 2 (17) | 1 (61) | 1 (28) | 1 (107) |
| Mean number of work days missed in an average month due to CLBP | 3.7 | 4.2 | 5.4 | 4.8 |
Percentages are rounded to the nearest integer and are based on weighted data. Weighted counts included in brackets.
Abbreviations: CLBP, chronic low back pain; SD, standard deviation.
Clinical characteristics, healthcare utilization, and medication usage
Fifty‐two percent, 49%, and 43% of patients with mild, moderate, and severe CLBP, respectively, received a diagnosis more than 5 years prior to participating in the survey (Table 2).
TABLE 2.
Clinical characteristics, healthcare utilization, and medication usage of patients who completed the survey
| Pain severity | Total (n = 9642) | |||
|---|---|---|---|---|
| Mild, weighted (n = 964) | Moderate, weighted (n = 4734) | Severe, weighted (n = 3944) | ||
| Clinical characteristics | ||||
| Time since CLBP diagnosis, % (n) | ||||
| Less than 5 years | 39 (379) | 42 (1980) | 50 (1984) | 45 (4343) |
| More than 5 years | 52 (496) | 49 (2302) | 43 (1710) | 47 (4509) |
| Don't know | 9 (90) | 10 (452) | 6 (249) | 8 (791) |
| Diagnosed comorbidities | ||||
| Mean number of diagnosed comorbidities | 2.0 | 2.5 | 2.9 | 2.6 |
| Types of diagnosed comorbidities, % (n) | ||||
| Chronic pain other than low back pain | 20 (197) | 28 (1310) | 44 (1745) | 34 (3253) |
| Heart and circulatory disease | 30 (286) | 32 (1534) | 33 (1297) | 32 (3117) |
| Arthritis (osteoarthritis and rheumatoid arthritis) | 18 (170) | 26 (1220) | 32 (1242) | 27 (2632) |
| Muscle, bone or joint diseases other than arthritis (including osteoporosis) | 16 (155) | 21 (991) | 28 (1091) | 23 (2237) |
| Digestive diseases (including irritable bowel syndrome, stomach ulcers, bowel disease) | 15 (145) | 23 (1100) | 25 (993) | 23 (2238) |
| A psychological condition (eg, anxiety, depression) | 14 (139) | 19 (892) | 23 (892) | 20 (1924) |
| Obesity | 14 (138) | 17 (812) | 20 (769) | 18 (1720) |
| Respiratory disease (including asthma, chronic obstructive pulmonary disease) | 10 (95) | 15 (716) | 19 (737) | 16 (1548) |
| Diabetes | 9 (87) | 10 (466) | 16 (617) | 12 (1170) |
| Thyroid diseases (including hyperactive or hypoactive thyroid, Graves’ disease) | 8 (79) | 13 (595) | 15 (608) | 13 (1282) |
| Liver, kidney and pancreas diseases (including pancreatitis, kidney disease) | 11 (103) | 11 (516) | 12 (463) | 11 (1082) |
| Neurological diseases (including stroke, epilepsy, multiple sclerosis, Parkinson's disease) | 3 (27) | 6 (302) | 9 (361) | 7 (690) |
| Other | 10 (92) | 8 (387) | 7 (258) | 8 (737) |
| Cancer | 3 (26) | 5 (245) | 4 (172) | 5 (443) |
| None | 17 (164) | 13 (596) | 9 (341) | 11 (1101) |
| Healthcare utilization | ||||
| HCPs involved in treatment of patients’ CLBP since diagnosis | ||||
| Mean number of different HCPs involved in treatment of patients’ CLBP | 2.4 | 2.6 | 2.9 | 2.7 |
| Top 4 types of HCP involved in treatment of CLBP patients, % (n) | ||||
| General practitioner or primary care physician | 57 (547) | 58 (2747) | 58 (2269) | 58 (5564) |
| Physiotherapist | 40 (381) | 42 (1996) | 42 (1636) | 42 (4013) |
| Neurologist | 25 (236) | 28 (1343) | 30 (1172) | 29 (2750) |
| Orthopedic surgeon | 26 (255) | 28 (1315) | 31 (1209) | 29 (2779) |
| Surgery | ||||
| Have undergone surgery for CLBP, % (n) | 12 (112) | 12 (586) | 21 (839) | 16 (1538) |
| Medication usage | ||||
| Medication currently taken | ||||
| Mean number of medications currently taken to manage CLBP | 1.3 | 1.6 | 2.0 | 1.7 |
| Top 4 types of medications currently taken to manage CLBP, % (n) | ||||
| Pain relief you buy yourself without a prescription (eg, paracetamol, ibuprofen, creams, patches) | 51 (494) | 58 (2750) | 56 (2189) | 56 (5433) |
| Prescribed pain relief (eg, naproxen, celecoxib, tramadol, oxycodone, morphine) | 20 (191) | 34 (1593) | 56 (2216) | 42 (4000) |
| Sedatives and muscle relaxants (eg, benzodiazepines) | 12 (115) | 18 (868) | 32 (1268) | 23 (2251) |
| Injections (eg, cortisone, local anesthetics) | 6 (62) | 16 (739) | 26 (1006) | 19 (1806) |
| Opioid use among patients taking prescribed pain relief, % (n) | ||||
| Yes | 35 (66) | 42 (665) | 58 (1280) | 50 (2011) |
| No | 55 (105) | 46 (731) | 30 (658) | 37 (1493) |
| Don't know | 11 (20) | 12 (197) | 13 (278) | 12 (496) |
| Duration of opioid use among patients taking prescribed pain relief, who knew they were taking opioids, % (n) | ||||
| Less than 5 years | 57 (37) | 58 (385) | 68 (869) | 64 (1292) |
| More than 5 years | 23 (15) | 34 (223) | 26 (330) | 28 (569) |
| Don't know | 20 (13) | 8 (56) | 6 (80) | 7 (150) |
Percentages are rounded to the nearest integer and are based on weighted data. Weighted counts included in brackets.
Abbreviations: CLBP, chronic low back pain; HCP, healthcare professional.
Patients across all pain severity categories reported, on average, between 2 and 3 comorbidities, although around twice as many patients with mild pain reported no comorbidities compared with patients with severe pain (17% vs. 9%). Of the comorbidities reported, the most common were chronic pain other than CLBP, cardiovascular disease, and arthritis (Table 2). Incidence of other chronic pain and arthritis was higher in patients with severe CLBP than with moderate or mild CLBP, but heart and circulatory diseases affected similar percentages of patients regardless of CLBP severity. Psychological comorbidities were also common among patients with CLBP, affecting nearly a quarter (23%) of patients with severe CLBP, and 19% and 14% of patients with moderate and mild CLBP, respectively.
Patients in each severity category had consulted between 2 and 3 different types of HCPs for their CLBP (Table 2). The top 4 types of HCPs involved in the treatment of patients’ CLBP since diagnoses were general practitioners or primary care physicians (58%), physiotherapists (42%), neurologists (29%), and orthopedic surgeons (29%). Numbers of patients seeing each type of physician varied little across the severity categories. Other types of HCPs were all seen by <20% of patients.
Patients with severe CLBP were almost twice as likely to have had surgery for their CLBP than those with mild or moderate CLBP; just over a fifth (21%) of patients with severe CLBP had undergone surgery, compared with 12% of patients with moderate and 12% of patients with mild CLBP.
In terms of pain management, the number of medications currently taken by patients to manage their CLBP increased with severity, rising from 1.3 in patients with mild CLBP to 2.0 in patients with severe CLBP. The most common medication used at the time of survey, in over half of patients, regardless of pain severity, was over‐the‐counter pain relief (mild, 51%; moderate, 58%; and severe, 56%).
Prescription pain medications were commonly used across all pain severities, although a higher percentage of patients with severe pain (56%) took them than those with mild or moderate pain (20% and 34%, respectively).
Taking opioids was common across all 3 pain categories, although the percentage of patients using opioids increased with severity: 35%, 42%, and 58% of patients with mild, moderate, and severe CLBP, respectively (Table 2). Patients also reported long‐term use of opioids to treat their CLBP; of those who responded that they knew they were taking opioids, 23%, 34%, and 26% with mild, moderate, and severe CLBP, respectively, had been taking them for more than 5 years (Table 2).
Personal impact of CLBP
Impact on daily function
Results from patients’ self‐reported impact of CLBP on their daily activities suggested an increase with pain severity. Patients selected a score on the Brief Pain Inventory scale, an 11‐point scale from 0 to 10, with 0 meaning no interference, and 10 meaning complete interference; patients with mild CLBP scored means of 1.2–2.4, patients with moderate CLBP scored means of 2.5–4.3, and patients with severe CLBP scored means of 4.5–6.2 for impact on activities surveyed.
Table 3 summarizes the effect of pain on patients’ day‐to‐day lives, with the level of impact increasing with pain severity. Mild pain had the least impact, especially on social function, with a mean interference score of 1.2 on patients’ relation to other people. In contrast, patients with severe CLBP reported that their pain had an impact score of between 5 and 6 on all activities, except relation to other people, where they reported an average impact of 4.5.
TABLE 3.
Mean scores for interference of pain with daily activities
| Pain severity | Total (n = 9642) | |||
|---|---|---|---|---|
| Mild, Weighted (n = 964) | Moderate, weighted (n = 4734) | Severe, weighted (n = 3944) | ||
| Mean interference of pain with daily activities | ||||
| Normal work | 2.4 | 4.3 | 6.2 | 4.9 |
| General activity | 2.2 | 4.2 | 6.2 | 4.8 |
| Mood | 2.0 | 4.0 | 6.0 | 4.6 |
| Enjoyment of life | 2.1 | 3.9 | 5.9 | 4.5 |
| Walking ability | 1.9 | 3.7 | 5.8 | 4.4 |
| Sleep | 1.8 | 3.7 | 5.6 | 4.3 |
| Relation with other people | 1.2 | 2.5 | 4.5 | 3.2 |
Patients selected a score on the Brief Pain Inventory scale, an 11‐point scale from 0 to 10, with 0 meaning no interference, and 10 meaning complete interference
Emotional/social impact
Patients reported a number of negative effects on their emotional state and social lives. When asked which positive or negative emotions they were experiencing (from a predefined list), on the day of taking the survey, patients most commonly reported feeling resigned (31%, 35%, and 35% for mild, moderate, and severe CLBP, respectively), frustrated (17%, 30%, and 35% for mild, moderate, and severe CLBP, respectively), and sad (19%, 23%, and 34% for mild, moderate, and severe CLBP, respectively). In general, the number of patients experiencing these negative emotions increased with CLBP severity. The number of patients experiencing positive emotions decreased with pain severity. Positive emotions were less commonly experienced among all patients than negative emotions; notably, it was more common for patients with mild CLBP to feel calm (30%), hopeful (18%), and determined (17%) than those with moderate (20%, 15%, and 12%, respectively) or severe (12%, 14%, and 10%, respectively) CLBP. Very few patients (5%, 3%, and 2% with mild, moderate, and severe CLBP, respectively) responded that they felt happy (Figure S1).
CLBP adversely affected patients’ interpersonal relationships and social lives, with the level of impact increasing with severity. When asked to rate their agreement with statements about the effect of pain on their social lives, almost half of all patients with severe CLBP had missed out on important social events or gatherings (47%) and avoided making commitments (44%). Twice as many patients with severe CLBP reported that they felt any given negative social impact compared with those with mild CLBP, including feeling: guilty about the effect their pain had on those close to them (38%), that their family or friends did not understand their situation (32%), and that their CLBP had made them distant to their friends (31%) (Figure 2).
FIGURE 2.
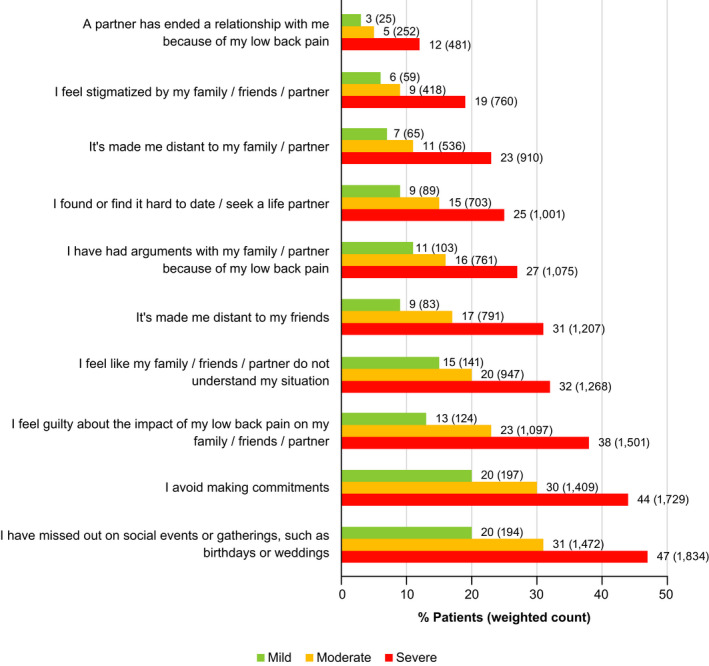
Effect on social life as a result of CLBP, split by CLBP severity. Percentages and weighted counts are shown of patients who agreed with the statements. To count as agreement, patients had to respond “strongly agree” or “somewhat agree.” CLBP, chronic low back pain
Impact of CLBP on employment
Impact on ability to work
Across all CLBP severities, similar numbers of patients described themselves as the main income earners in their households: 72% of patients with severe CLBP, and 68% and 69% of patients with mild and moderate CLBP, respectively (Table 1). However, CLBP had a negative impact on patients’ ability to work.
Patients across all severity groups who were employed (including self‐employed, voluntary workers, and unpaid careers) reported that they had missed work due to their pain: those with severe CLBP missed an average of 5.4 days of work per month, while those with moderate and mild CLBP missed 4.2 and 3.7 days per month, respectively (Table 1).
Patients’ experience at work was also negatively affected, and this effect increased with CLBP severity (Figure 3). Patients were asked if they agreed or disagreed with three positive and three negative statements about the impact of their CLBP on work. Results showed that patients with severe CLBP had more negative experiences at work than those with mild or moderate CLBP. Patients received less pleasure from their work, and their CLBP reduced their ability to perform tasks (Figure 3).
FIGURE 3.
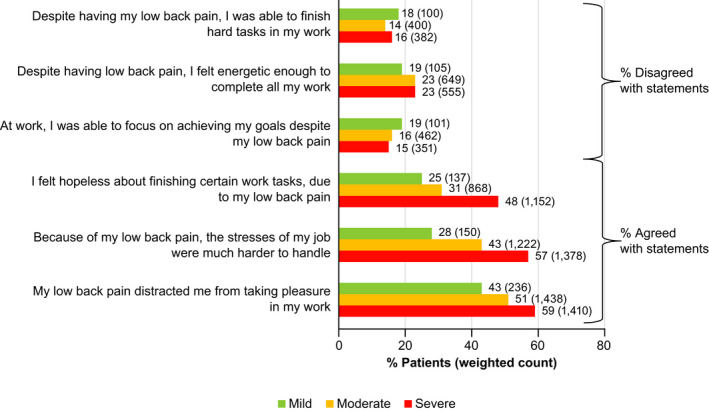
Patients’ agreement with positive and negative statements about work, according to the Stanford Presenteeism Scale. 17 To count as agreement, patients had to respond “strongly agree” or “somewhat agree.” To count as disagreement, patients had to select “somewhat disagree” or “strongly disagree”
Impact on personal experience at work
Patients were asked about the impact their CLBP had on other aspects of work, including those affecting their relationships with other colleagues, how they feel they are perceived, and general job satisfaction. Eighteen percent of patients with mild or with moderate CLBP, and 16% of patients with severe CLBP, disagreed with the statement “I feel satisfied with my job,” and 34%, 24%, and 22% disagreed with the statement “I feel supported by my employer,” respectively. Patients also agreed with a number of statements about the negative effects of CLBP on their working lives. For each of the negative statements, a higher percentage of patients with severe CLBP than with moderate or mild CLBP agreed (Figure 4).
FIGURE 4.
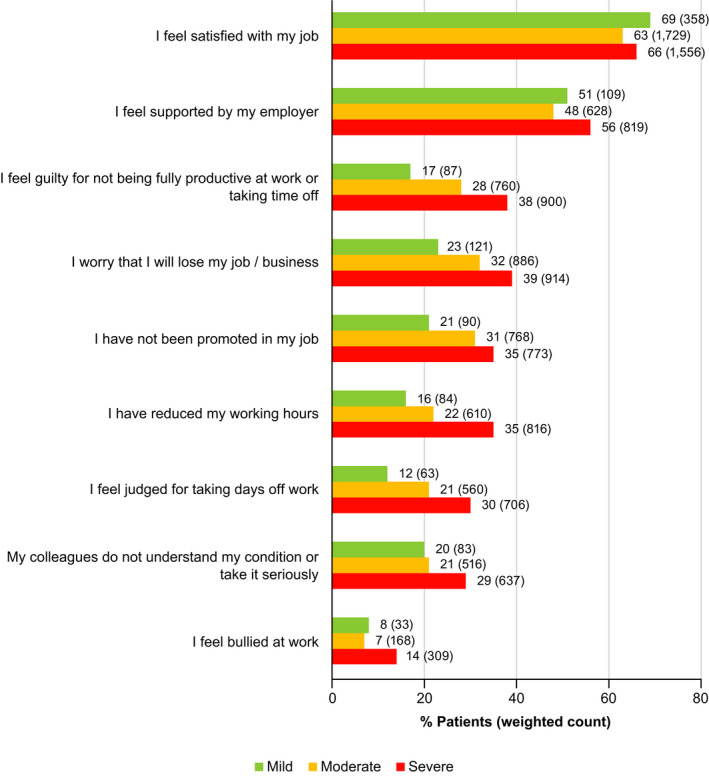
Percentages and weighted counts of patients who agreed with statements about feelings toward their work. To count as agreement, patients had to respond “strongly agree” or “somewhat agree”
Around 1 in 3 patients with moderate (32%) or severe (39%) CLBP, respectively, were worried about losing their job/business, compared with 1 in 5 patients with mild CLBP (23%) (Figure 4). Notably, more than a third of patients with severe CLBP (35%) had reduced their working hours due to CLBP (Figure 4).
DISCUSSION
This survey provides an in‐depth evaluation of the wide‐reaching impact that CLBP has, as experienced by a large, international sample of almost 10,000 CLBP patients. The results further support those from previous, localized studies showing that CLBP affects multiple aspects of patients’ lives, including their personal and professional lives, their emotional and social well‐being, and their overall quality of life. 4 , 5 , 10
Results show that comorbidities among patients were common, with twice the rate of psychological comorbidities (23%) than estimated among the general European population (11%). 39 Psychological distress and/or depressive mood is associated with increased risk for pain chronicity, 40 and depression among CLBP patients is associated with higher pain scores and lower quality of life, as well as lower work productivity and increased healthcare use. 41 The results from this survey further validate guidelines that recommend patients be assessed and managed within a biopsychosocial model, 42 given how these factors impact experience, outcomes, and quality of life and that earlier intervention can reduce the risk of developing or exacerbating a chronic pain syndrome. 43 , 44
The effects of early intervention and the early identification of psychosocial risk factors are recognized in National Institute of Health and Care Excellence (NICE) pain guidelines. 45 , 46 In alignment with guidelines, patients reported that they are primarily treated by general practitioners and secondly by physiotherapists. Physiotherapists may implement best practice by promoting self‐management, the notion of positive health, integrating health and occupational interventions, and/or exercise advice, 47 , 48 , 49 although the details of the treatment approach were not determined within this survey. Despite 1 in 5 patients in this survey reporting a psychological comorbidity, psychologists were not among the top 4 HCPs involved in CLBP patients’ care. Taken together, these data indicate inconsistent adherence to treatment guidelines and limited understanding of the benefits of biopsychosocial interventions. This may be due to stigma that patients associate with requiring mental health support 50 or inadequate health literacy, which is reported in among half of chronic pain patients. 51 From a clinical perspective, these results could also indicate adherence to outdated models of care or a lack of resources for offering a range of HCP services in individual countries. For example, pain specialists who coordinate and provide biopsychosocial management options were not included in the top 4 HCPs involved in the treatment of patients’ CLBP since diagnosis. A lack of education regarding the benefits of early, biopsychosocial interventions to improve patient outcomes in CLBP may also have been a factor. 43 , 52 , 53 , 54
The data showed that, of the 42% of patients taking prescribed pain relief for their CLBP, half knew that they were taking opioids. While opioids can provide relief for acute pain, these drugs become less effective when pain progresses to a chronic state. 55 , 56 Furthermore, the effects of opioid analgesia may be diminished in patients with psychological comorbidities, who represent a sizable proportion of CLBP patients in this survey. 54 However, a subgroup of patients with severe CLBP who were taking opioids had been doing so for more than 5 years, which is concerning, since many are also experiencing psychological comorbidities, and patients with anxiety and depression are at higher risk of opioid addiction. This can fuel the fear‐avoidance model, in which patients become further sensitized and maintain chronic pain as a result of avoidant behavior based on pain‐related fear and anxiety. 57 The latest NICE pain guidelines published in 2019, 45 and the 2018 guidelines that were available at the time of data collection, do not recommend the use of opioids for the treatment of CLBP. 46 However, the data within this survey indicate poor adherence to opioid‐prescribing guidance.
The most recent NICE guidelines have expanded existing routine screening for psychological comorbidities in patients with CLBP to form part of a risk assessment to identify potential problems that could arise from opioid use. 45 , 46 Given that improved adherence to guidelines has been linked to improved patient outcomes, 47 , 48 updates to guidelines should also be supported by better education for students and qualified HCPs regarding the causes, prognoses, and effectiveness of different management approaches for CLBP. 43 , 52 Indeed, chronic pain has been acknowledged within the 11th edition of the International Classification of Diseases to improve the classification, diagnostic coding, and early identification of chronic pain. 58
Consistent with the previous findings from surveys on general chronic pain and CLBP, 18 , 19 , 59 the social function of patients in this survey was negatively affected, with effects increasing with pain severity. Many patients reported effects such as distance from, or tension between, friends and family. The finding that CLBP was a barrier to patients’ social activities and negatively affected their personal relationships has not previously been reported in this level of detail in an international, large‐scale survey, and illustrates novel and important aspects of the personal and social burden of CLBP on the individual patients. The effect of CLBP on the social function of patients is likely to be a risk factor for further psychological problems and comorbidities, such as depression and anxiety, as evidenced by the fear‐avoidance model. 17 , 60
Regarding patients’ professional lives and employment, over a third of patients with severe CLBP had reduced the number of hours they worked, and CLBP of all severities caused patients to miss days of work. Notably, patients reported psychological consequences and reduced enjoyment of work; the fact that patients worry about losing their job and are concerned about taking time off due to CLBP have, to the best of our knowledge, not previously been reported in an international, large‐scale survey of CLBP patients. The mental strain associated with job insecurity and workplace hostility may be worse for the health of workers than unemployment 61 and are associated with onset of CLBP. 62 In addition, chronic musculoskeletal pain, psychological comorbidity, and pain‐related fear of movement are associated with low work productivity and negative impacts on work‐related outcomes. 6 , 63 , 64 Taken together, the evidence suggests a 2‐way association between CLBP severity and work‐related impact, with patients facing both physical and emotional barriers in the workplace. 65 , 66 This further supports previous research by the Lancet Low Back Pain Series Working Group and others, which highlights the need for improved communications between employers and patients in the workplace, as well as streamlined integration between healthcare services, employers, and social services to fully support CLBP patients. 44 , 67 , 68
The findings from this survey provide additional insights into the detailed personal, social, and professional impact of CLBP across a widespread, international population, with patients reporting their condition was a barrier to social activities and caused them to experience negative feelings about work. The strong association between the social burden of CLBP and comorbidities such as anxiety and sleep disorders has been documented in studies in individual countries, 69 and for chronic pain in general, each recognizing the importance of considering the psychosocial effects of pain when classifying and treating patients. 70 , 71 The social effects of chronic pain not only affect the individual, but also their relationships, and the emotional and social consequences of pain affect the pain itself. 72 , 73 There is evidence that only an intensive biopsychosocial regimen has clinically meaningful outcomes in CLBP, 44 , 74 and the results from this survey support the fact that pain and psychological distress are closely intertwined.
Strengths and limitations
Online surveys provide a means of reaching many people in a cost‐effective manner, with low barriers to participation. This allowed for a large, international population to be reached within many regions of the same country, providing a wider, more complete perspective of the patient experience. An increased sample size means that results are less likely to be influenced by outlier data.
It should be noted that online surveys provide cross‐sectional data and may not be representative of the entire CLBP population 75 ; respondents are limited to those who have access to the internet, who actively volunteer to participate in and receive compensation for market research, and have adequate literacy skills. Care was taken during the conception and design of the survey to take the literacy level into consideration and to use patient‐friendly language throughout. This type of survey also relies on patients’ self‐reported experiences, which can be subject to recall, participation, or self‐selection bias. This can, to some extent, be overcome using weighting procedures, 31 which were employed within this methodology.
Conclusions around the use of opioids in the study population are limited by the inability of the survey to differentiate between strong and weak opioids. Weak opioids (eg, tramadol, a schedule IV controlled substance) have a better safety profile, including a lower risk of misuse, than strong opioids (eg, morphine, oxycodone, and hydrocodone, which are schedule II controlled substances). 76 As a result, a distinction between strong and weak opioids is typically made when prescribing or describing medications for chronic pain. Likewise, the survey is also limited by the inability to provide more specific information on the use of medications beyond the 4 broad categories of “pain relief you buy yourself without a prescription,” “prescribed pain relief,” “sedatives and muscle relaxants,” and “injections.” There is likely substantial overlap among these groups. NSAIDs, for example, may be obtained with or without a prescription (based on type of NSAID). Likewise, benzodiazepines would be included in both the “sedatives and muscle relaxants” and the prescription pain relief groups.
CONCLUSIONS
Data from this large, international survey offer clinically relevant insights describing the pronounced effect of CLBP on patients’ personal relationships, ability to work, and feelings about work. In terms of CLBP management, adherence to best practice guidelines is inconsistent and may be due to multiple factors, including a lack of education for HCPs. Concerted efforts should be directed at improving education for HCPs regarding the complex biopsychosocial needs of CLBP patients and the associated risks of opioid use in this context. HCPs should be encouraged to refer CLBP patients to physiotherapists and psychologists to support a biopsychosocial management approach.
CONFLICTS OF INTEREST
Bart Morlion and David Roomes have received grants for clinical research, consultancy activities, and speaker's activities from a number of pharmaceutical companies, including Pfizer Ltd and Eli Lilly and Company. Brona Fullen has received non‐restrictive educational grants and/or consultancy activities from pharmaceutical companies including Pfizer Ltd and Eli Lilly and Company. Joop van Griensven, Steven Linton, and Serge Perrot have received non‐restrictive grants for consultancy activities from Pfizer Ltd and Eli Lilly and Company. Craig Beck and Lucy Abraham are employees of Pfizer Ltd with stock and/or stock options. Stefan Wilhelm is an employee and shareholder of Eli Lilly and Company. Cristina Constantinescu is an employee of Ipsos SA, who were paid consultants to Pfizer Ltd and Eli Lilly and Company for this study and the development of this manuscript.
Supporting information
Fig S1
Table S1
ACKNOWLEDGMENTS
We thank the members of the steering committee who provided expert input into the development of the survey and analysis of the survey data: Prof. Lars Arendt‐Nielsen, Prof. Vincenzo Atella, Mr. Antony Chuter, Prof. Karen Facey, Ms. Fiona Hodson, Dr. Hermenegildo Marcos, Mariano Votta, and Ms. Donna Walsh. Open Access funding provided by IReL. [Correction added on 20 May 2022, after first online publication: IReL funding statement has been added.]
Fullen B, Morlion B, Linton SJ, Roomes D, van Griensven J, Abraham L, et al. Management of chronic low back pain and the impact on patients’ personal and professional lives: Results from an international patient survey. Pain Pract. 2022;22:463–477. 10.1111/papr.13103
Funding information
The survey and data acquisition were provided by Ipsos SA and funded by Pfizer Ltd. and Eli Lilly and Company. All authors agreed to publish the data. Medical writing support was provided by Ellen Barker, Zoe Sycamore and Angelique Cabral at 90TEN Ltd., Editorial Support, in the form of copyediting and formatting, was provided by Alex Frings of Engage Scientific Solutions and was funded by Pfizer and Eli Lilly and Company.
DATA AVAILABILITY STATEMENT
Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions, and exceptions, Pfizer may also provide access to the related individual de‐identified participant data. See https://www.pfizer.com/science/clinical‐trials/trial‐data‐and‐results for more information.
REFERENCES
- 1. Lodato EM, Kaplan W. Priority medicines for Europe and the world "a public health approach to innovation" update on the 2004 background paper. In: Kaplan W, Wirtz VJ, Mantel‐Teeuwisse A, Stolk P, Duthey B, Laing R, editors. Priority medicines for Europe and the world: 2013 updated background paper. Geneva: World Health Organization; 2013. p. 1–122. [Google Scholar]
- 2. Global Burden of Disease Study 2013 Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Park TSW, Kuo A, Smith MT. Chronic low back pain: a mini‐review on pharmacological management and pathophysiological insights from clinical and pre‐clinical data. Inflammopharmacology. 2018;26:881–98. [DOI] [PubMed] [Google Scholar]
- 4. Breivik H, Eisenberg E, O’Brien T. The individual and societal burden of chronic pain in Europe: the case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health. 2013;13:1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287–333. [DOI] [PubMed] [Google Scholar]
- 6. Patel AS, Farquharson R, Carroll D, Moore A, Phillips CJ, Taylor RS, et al. The impact and burden of chronic pain in the workplace: a qualitative systematic review. Pain Pract. 2012;12:578–89. [DOI] [PubMed] [Google Scholar]
- 7. Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13:715–24. [DOI] [PubMed] [Google Scholar]
- 8. Phillips CJ. The cost and burden of chronic pain. Rev Pain. 2009;3:2–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Geurts JW, Willems PC, Kallewaard JW, van Kleef M, Dirksen C. The impact of chronic discogenic low back pain: costs and patients’ burden. Pain Res Manag. 2018;2018:4696180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Husky MM, Ferdous Farin F, Compagnone P, Fermanian C, Kovess‐Masfety V. Chronic back pain and its association with quality of life in a large French population survey. Health Qual Life Outcomes. 2018;16:195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wettstein M, Eich W, Bieber C, Tesarz J. Pain intensity, disability, and quality of life in patients with chronic low back pain: does age matter? Pain Med. 2019;20:464–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cayea D, Perera S, Weiner DK. Chronic low back pain in older adults: what physicians know, what they think they know, and what they should be taught. J Am Geriatr Soc. 2006;5411:1772–7. [DOI] [PubMed] [Google Scholar]
- 13. Gerhardt A, Hartmann M, Blumenstiel K, Tesarz J, Eich W. The prevalence rate and the role of the spatial extent of pain in nonspecific chronic back pain – a population‐based study in the south‐west of Germany. Pain Med. 2014;15:1200–10. [DOI] [PubMed] [Google Scholar]
- 14. Gerhardt A, Hartmann M, Schuller‐Roma B, Blumenstiel K, Bieber C, Eich W, et al. The prevalence and type of Axis‐I and Axis‐II mental disorders in subjects with non‐specific chronic back pain: results from a population‐based study. Pain Med. 2011;12:1231–40. [DOI] [PubMed] [Google Scholar]
- 15. Rudy TE, Weiner DK, Lieber SJ, Slaboda J, Boston JR. The impact of chronic low back pain on older adults: a comparative study of patients and controls. Pain. 2007;131:293–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Glombiewski JA, Hartwich‐Tersek J, Rief W. Depression in chronic back pain patients: prediction of pain intensity and pain disability in cognitive‐behavioral treatment. Psychosomatics. 2010;51:130–6. [DOI] [PubMed] [Google Scholar]
- 17. Mathew J, Singh SB, Garis S, Diwan AD. Backing up the stories: the psychological and social costs of chronic low‐back pain. Int J Spine Surg. 2013;7:e29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pain Alliance Europe Survey on chronic pain and your work life: a survey in 14 European countries. 2018;2020. Available from: https://www.pae‐eu.eu/wp‐content/uploads/2018/07/PAE‐Survey‐2018‐Pain‐And‐Your‐Work‐Life.pdf. Accessed 30 Sept 2020.
- 19. Pain Alliance Europe Chronic pain and stigma. 2019;2020. Available from: www.pae‐eu.eu/wp‐content/uploads/2019/09/2019‐Survey‐PAE‐final‐short‐report.pdf. Accessed 30 Sept 2020.
- 20. Wolff R, Clar C, Lerch C, Kleijnen J. Epidemiology of chronic non‐malignant pain in Germany. Article in German. Schmerz. 2011;25:26–44. [DOI] [PubMed] [Google Scholar]
- 21. Turk DC, Wilson HD, Cahana A. Treatment of chronic non‐cancer pain. Lancet. 2011;377:2226–35. [DOI] [PubMed] [Google Scholar]
- 22. Pérez C, Margarit C, Serrano M. Survey of European patients assessing their own noncancer chronic pain: results from Spain. Curr Med Res Opin. 2013;29:643–51. [DOI] [PubMed] [Google Scholar]
- 23. Reid KJ, Harker J, Bala MM, Truyers C, Kellen E, Bekkering GE, et al. Epidemiology of chronic non‐cancer pain in Europe: narrative review of prevalence, pain treatments and pain impact. Curr Med Res Opin. 2011;27:449–62. [DOI] [PubMed] [Google Scholar]
- 24. Russo M, Deckers K, Eldabe S, Kiesel K, Gilligan C, Vieceli J, et al. Muscle control and non‐specific chronic low back pain. Neuromodulation. 2018;21:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stanhope J. Brief Pain Inventory review. Occup Med. 2016;66:496–7. [DOI] [PubMed] [Google Scholar]
- 26. Turpin RS, Ozminkowski RJ, Sharda CE, Collins JJ, Berger ML, Billotti GM, et al. Reliability and validity of the Stanford Presenteeism Scale. J Occup Environ Med. 2004;46:1123–33. [DOI] [PubMed] [Google Scholar]
- 27. Market Research Society (MRS) Guidelines for online research. 2014;2020. Available from: http://www.mrs.org.uk/pdf/2014‐09‐01%20Online%20Research%20Guidelines.pdf. Accesses 30 Sept 2020.
- 28. European Pharmaceutical Market Research Association (EphMRA) Code of conduct. 2018;2020. Available from: http://www.ephmra.org/media/2278/ephmra‐code‐of‐conduct‐august‐2018‐gdpr‐update‐v5‐for‐issue.pdf. Accesses 30 Sept 2020.
- 29. European Society for Opinion and Marketing Research (ESOMAR) Guidelines for online research. 2011;2020. Available from: https://ana.esomar.org/documents/esomar‐grbn‐global‐guideline‐on‐online‐research‐. Accesses 30 Sept 2020.
- 30. British Healthcare Business Intelligence Association Legal and ethical guidelines for online research. 2019;2020. Available from: https://www.bhbia.org.uk/guidelines‐and‐legislation/legal‐and‐ethical‐guidelines. Accessed 21 Feb 2022.
- 31. Hays RD, Liu H, Kapteyn A. Use of internet panels to conduct surveys. Behav Res. 2015;47:685–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Population Reference Bureau 2016 world population data sheet. 2016;2020. Available from: https://www.prb.org/wp‐content/uploads/2016/08/prb‐wpds2016‐web‐2016.pdf. Accesses 30 Sept, 2020.
- 33. Van Griensven J, Beck C, Abraham L, Wilhelm S, Constantinescu C, Morlion B. Methodology to assess impact and burden of chronic low back pain on patients’ physical and emotional health – global survey of >9,000 patients across 16 countries. Presented at 11th Congress of The European Pain Federation (EFIC). September 4–7, 2019.
- 34. Van Griensven J, Beck C, Abraham L, Wilhelm S, Constantinescu C, Morlion B. Demographic data and clinical characteristics of patients with chronic low back pain – results from a global 8,990 patient survey: Citizens’ Research. Presented at 11th Congress of The European Pain Federation (EFIC). September 4–7, 2019.
- 35. Perrot S, Arendt‐Nielsen L, Beck C, Abraham L, Wilhelm S, Constantinescu C, et al. Treatment patterns of chronic low back pain patients – initial results from a global 8,990 patient survey: Citizens’ Research. Presented at 11th Congress of The European Pain Federation (EFIC). September 4–7, 2019.
- 36. Van Griensven J, Linton SJ, Beck C, Abraham L, Wilhelm S, Constantinescu C, et al. Impact of chronic low back pain from physical, psychological and social perspectives – initial results from a global 8,990 patient survey: Citizens’ Research. Presented at the Societal Impact of Pain Symposium. November 7, 2019.
- 37. Morlion B, Arendt‐Nielsen L, Abraham L, Beck C, Wilhelm S, Constantinescu C, et al. PMS28 healthcare service utilisation by patients with chronic low back pain – results from a global 8,990 patient survey: citizens’ research. Value Health. 2019;22:S698. doi: 10.1016/j.jval.2019.09.1572 [DOI] [Google Scholar]
- 38. Roomes D, Abraham L, Beck C, Wilhelm S, Constantinescu C, Carboni V. PMS26 impact of chronic low back pain on employment and productivity – results from a global 8,990 patient survey: citizens’ research. Value Health. 2019;22:S698. doi: 10.1016/j.jval.2019.09.1570 [DOI] [Google Scholar]
- 39. Demyttenaere K, Bruffaerts R, Posada‐Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–90. [DOI] [PubMed] [Google Scholar]
- 40. Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine (Phila Pa 1976). 2002;27:e109–20. [DOI] [PubMed] [Google Scholar]
- 41. Tsuji T, Matsudaira K, Sato H, Vietri J. The impact of depression among chronic low back pain patients in Japan. BMC Musculoskelet Disord. 2016;17:447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Oliveira CB, Maher CG, Pinto RZ, Traeger AC, Lin C‐W, Chenot J‐F, et al. Clinical practice guidelines for the management of non‐specific low back pain in primary care: an updated overview. Eur Spine J. 2018;27:2791–803. [DOI] [PubMed] [Google Scholar]
- 43. Hill JC, Whitehurst DGT, Lewis M, Bryan S, Dunn KM, Foster NE, et al. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. Lancet. 2011;378:1560–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Buchbinder R, van Tulder M, Öberg B, Costa LM, Woolf A, Schoene M, et al. Low back pain: a call for action. Lancet. 2018;391:2384–8. [DOI] [PubMed] [Google Scholar]
- 45. National Institute for Health and Care Excellence Managing low back pain and sciatica. 2019;2020. Available from: https://pathways.nice.org.uk/pathways/low‐back‐pain‐and‐sciatica/managing‐low‐back‐pain‐and‐sciatica.pdf. Accessed 30 Sept, 2020.
- 46. National Institute for Health and Care Excellence Low back pain and sciatica in over 16s: assessment and management. 2018;2020. Available from: https://www.nice.org.uk/guidance/ng59/resources/low‐back‐pain‐and‐sciatica‐in‐over‐16s‐assessment‐and‐management‐pdf‐1837521693637. Accessed 30 Sept, 2020. [PubMed]
- 47. Rutten GM, Degen S, Hendriks EJ, Braspenning JC, Harting J, Oostendorp RA. Adherence to clinical practice guidelines for low back pain in physical therapy: do patients benefit? Phys Ther. 2010;90:1111–22. [DOI] [PubMed] [Google Scholar]
- 48. Epstein‐Sher S, Jaffe DH, Lahad A. Are they complying? Physicians’ knowledge, attitudes, and readiness to change regarding low back pain treatment guideline adherence. Spine (Phila Pa 1976). 2017;42:247–52. doi: 10.1097/BRS.0000000000001714 [DOI] [PubMed] [Google Scholar]
- 49. Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391:2368–83. [DOI] [PubMed] [Google Scholar]
- 50. Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychol Sci Public Interest. 2014;15:37–70. [DOI] [PubMed] [Google Scholar]
- 51. Mackey LM, Blake C, Casey M‐B, Power CK, Victory R, Hearty C, et al. The impact of health literacy on health outcomes in individuals with chronic pain: a cross‐sectional study. Physiotherapy. 2019;105:346–53. [DOI] [PubMed] [Google Scholar]
- 52. Mariano TY, Urman RD, Hutchison CA, Jamison RN, Edwards RR. Cognitive behavioral therapy (CBT) for subacute low back pain: a systematic review. Curr Pain Headache Rep. 2018;22:15. [DOI] [PubMed] [Google Scholar]
- 53. Nicholas MK, Linton SJ, Watson PJ, Main CJ, the "Decade of the Flags" Working Group . Early identification and management of psychological risk factors ("yellow flags") in patients with low back pain: a reappraisal. Phys Ther. 2011;91:737–53. [DOI] [PubMed] [Google Scholar]
- 54. Briggs EV, Battelli D, Gordon D, Kopf A, Ribeiro S, Puig MM, et al. Current pain education within undergraduate medical studies across Europe: Advancing the Provision of Pain Education and Learning (APPEAL) study. BMJ Open. 2015;5:e006984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Wasan AD, Michna E, Edwards RR, Katz JN, Nedeljkovic SS, Dolman AJ, et al. Psychiatric comorbidity is associated prospectively with diminished opioid analgesia and increased opioid misuse in patients with chronic low back pain. Anesthesiology. 2015;123:861–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Borsook D, Youssef AM, Simons L, Elman I, Eccleston C. When pain gets stuck: the evolution of pain chronification and treatment resistance. Pain. 2018;159:2421–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Arteta J, Cobos B, Hu Y, Jordan K, Howar DK. Evaluation of how depression and anxiety mediate the relationship between pain catastrophizing and prescription opioid misuse in a chronic pain population. Pain Med. 2016;17:295–303. [DOI] [PubMed] [Google Scholar]
- 58. Treede R‐D, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD‐11). Pain. 2019;160:19–27. [DOI] [PubMed] [Google Scholar]
- 59. Gouveia N, Rodrigues A, Eusébio M, Ramiro S, Machado P, Canhão H, et al. Prevalence and social burden of active chronic low back pain in the adult Portuguese population: results from a national survey. Rheumatol Int. 2016;36:183–97. [DOI] [PubMed] [Google Scholar]
- 60. Carley JA, Karp JF, Gentili A, Marcum ZA, Reid MC, Rodriguez E, et al. Deconstructing chronic low back pain in the older adult: step by step evidence and expert‐based recommendations for evaluation and treatment: part IV: depression. Pain Med. 2015;16:2098–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kim TJ, von dem Knesebeck O. Is an insecure job better for health than having no job at all? A systematic review of studies investigating the health‐related risks of both job insecurity and unemployment. BMC Public Health. 2015;15:985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Yang H, Haldeman S, Lu ML, Baker D. Low back pain prevalence and related workplace psychosocial risk factors: a study using data from the 2010 National Health Interview Survey. J Manipulative Physiol Ther. 2016;39:459–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sell L, Lund HL, Holtermann A, Søgaard K. The interactions between pain, pain‐related fear of movement and productivity. Occup Med (Lond). 2014;64:376–81. [DOI] [PubMed] [Google Scholar]
- 64. Keus Van De Poll M, Bergström G, Jensen I, Nybergh L, Kwak L, Lornudd C, et al. Cost‐effectiveness of a problem‐solving intervention aimed to prevent sickness absence among employees with common mental disorders or occupational stress. Int J Environ Res Public Health. 2020;17:5234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Deeney C, O'Sullivan L. Work related psychosocial risks and musculoskeletal disorders: potential risk factors, causation and evaluation methods. Work. 2009;34:239–48. [DOI] [PubMed] [Google Scholar]
- 66. Vignoli M, Guglielmi D, Balducci C, Bonfiglioli R. Workplace bullying as a risk factor for musculoskeletal disorders: the mediating role of job‐related psychological strain. Biomed Res Int. 2015;2015:712642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Grant M, Rees S, Underwood M, Froud R. Obstacles to returning to work with chronic pain: in‐depth interviews with people who are off work due to chronic pain and employers. BMC Musculoskelet Disord. 2019;20:486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Linton SJ, Boersma K, Traczyk M, Shaw W, Nicholas M. Early workplace communication and problem solving to prevent back disability: results of a randomized controlled trial among high‐risk workers and their supervisors. J Occup Rehabil. 2016;26:150–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Inoue S, Taguchi T, Yamashita T, Nakamura M, Ushida T. The prevalence and impact of chronic neuropathic pain on daily and social life: a nationwide study in a Japanese population. Eur J Pain. 2017;21:727–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Turk DC, Fillingim RB, Ohrbach R, Patel KV. Assessment of psychosocial and functional impact of chronic pain. J Pain. 2016;17:T21–49. [DOI] [PubMed] [Google Scholar]
- 71. Monti S, Caporali R. Chronic pain: the burden of disease and treatment innovations. Reumatismo. 2015;67:35–44. [DOI] [PubMed] [Google Scholar]
- 72. Dueñas M, Ojeda B, Salazar A, Mico JA, Failde I. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016;9:457–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Edwards RR, Dworkin RH, Sullivan MD, Turk DC, Wasan AD. The role of psychosocial processes in the development and maintenance of chronic pain. J Pain. 2016;17:T70–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. van Erp RMA, Huijnen IPJ, Jakobs MLG, Kleijnen J, Smeets R. Effectiveness of primary care interventions using a biopsychosocial approach in chronic low back pain: a systematic review. Pain Pract. 2019;19:224–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Scherpenzeel AC, Bethlehem JG. How Representative are Online Panels? Problems of Coverage and Selection and Possible Solutions. In: Das M, Ester P, Kaczmirek L, editors. Social and behavioral research and the internet: advances in applied methods and research strategies. 1st edn, New York, NY: Routledge; 2011. p. 105–32. [Google Scholar]
- 76. Reines SA, Goldmann B, Harnett M, Lu L. Misuse of tramadol in the united states: an analysis of the national survey of drug use and health 2002–2017. Subst Abuse. 2020;14:1178221820930006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig S1
Table S1
Data Availability Statement
Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions, and exceptions, Pfizer may also provide access to the related individual de‐identified participant data. See https://www.pfizer.com/science/clinical‐trials/trial‐data‐and‐results for more information.


