Abstract
Objectives
To evaluate the health-condition of military police officers and firefighters. To identify risk factors for not being medically ready for duty.
Design
Cross-sectional study.
Setting
Data were extracted from medical records during annual periodic health assessments of police officers and firefighters serving with the military police in Paraná, Brazil.
Participants
6621 police officers (5927 men and 694 women) and 1347 firefighters (1257 men and 90 women) who underwent health assessments between July 2018 and June 2019 were analysed. Pregnant women were excluded.
Outcome measures
Data included variables such as sex, age, anthropometric measurements, lifestyle, comorbidities and laboratory tests. Multiple logistic regression was used to estimate the probability of not being medically ready for active duty.
Results
Overall, police officers had worse health status than firefighters and greater prevalence of overweight and obesity, regardless of sex. Musculoskeletal diseases were the most commonly reported disease by police officers and firefighters of both sexes. Among men, hypertension was the second most prevalent disease, followed by psychiatric diseases and dyslipidaemia. Among women, psychiatric diseases were the second most prevalent. Male police officers ≥40 years old presented the highest probability of not being considered ready for duty (40.1%). The probability of male police officers between the ages of 31 and 40 not being ready was similar to that for male firefighters >40 years old. There was a higher chance of not being medically ready professionals with diseases such as diabetes mellitus (OR 2.95, 95% CI 1.97 to 5.03), dyslipidaemia (OR 2.65, 95% CI 1.96 to 3.58), hypertension (OR 2.29, 95% CI 1.85 to 4.70), high total cholesterol (OR 2.16, 95% CI 1.93 to 2.42), and heart disease (OR 2.13, 95% CI 1.32 to 3.45).
Conclusions
There was a high prevalence of chronic diseases and modifiable cardiovascular risk factors among police officers and firefighters. Healthy protective measures should be offered frequently, particularly to police officers at an earlier age.
Keywords: preventive medicine, internal medicine, epidemiology
Strengths and limitations of this study.
Few studies have compared the health condition of military police officers and firefighters.
This study included female police officers and firefighters therefore our findings may contribute to research in this subset of the population.
The study used a cross-sectional design, wherein casual relationships could not be inferenced from the results.
Our findings may not be generalised to other professional groups.
New fields of research can be developed from the results.
Introduction
The public safety sector is essential for the maintenance of social order. The military police in Paraná, South of Brazil, has been responsible for training military police officers and firefighters to fulfil this noble mission for 167 years. Although they are considered to be physically and psychologically fit when they start their careers, these workers are exposed to various work-related risk factors that can cause their physical and mental health to deteriorate.1 2
Police work involves long working days and very stressful situations, often in violent areas.1 Police officers also face unexpected situations that require strength, dexterity and physical fitness.2 Firefighters face additional risks, when they are exposed to smoke from chemical and biological hazards.1 Studies have shown that police officers and firefighters have a shorter life expectancy than the general population and high mortality and morbidity, especially due to cardiovascular disease (CVD).2
Although firefighters are subjected to physical demands, the prevalence of being overweight and obese among them is similar to the general population. The high prevalence of CVD risk factors remains a concern since firefighters are called on to exert maximal effort under stressful conditions.3 4 There is a variable prevalence of cardiovascular risk factors such as hypertension, dyslipidaemia, obesity, diabetes mellitus, smoking and metabolic syndrome among police officers.5
Several studies have investigated the health status of police officers and firefighters, focusing primarily on cardiovascular, chronic and psychiatric diseases. However, few have investigated the prevalence of their morbidities with sex and age in that population, or have estimated their risk of having unsuitable health status for their daily work activities. It is imperative that police officers and firefighters attain and maintain physical fitness for both their overall health and ability to perform job tasks safely and effectively. The present study sought to evaluate the health condition of military police officers and firefighters and to identify risk factors for not being medically ready for active duty.6
Participants and methods
Study design and evaluated population
This observational study investigated the general health status of military police officers and firefighters in Paraná between June 2018 and July 2019. Pregnant women were excluded from the study. A total of 7968 individuals were included: 6621 police officers (5927 men, 694 women) and 1347 firefighters (1257 men, 90 women), which comprised 43.4% of the military police officers and firefighters in Paraná. Participants underwent a medical assessment during the annual health inspections that comprised clinical history, physical examination and laboratory tests. An exercise stress test (ET) on a treadmill was performed by individuals aged 40 years or over. Participants were divided according to sex and age (for males: ≤30 years old, 31–40 years old and ≥41 years old; for females: ≤30 years old and ≥31 years old) to identify a subset of the study population with the greatest prevalence of chronic diseases. Women were analysed separately because of their biological and behavioural characteristics, highlighting the sex differences in cardiometabolic, obesity and physical performance parameters.
Data collection
The participants were military police officers and firefighters performing regular duties who underwent an elective medical assessment during the annual health inspections. Data were collected from standardised electronic health records.
Race category was determined according to the answer given to a standard question on self-declared ethnicity, based on the method used by the Brazilian Institute of Geography and Statistics national census survey which classifies individuals as white, brown, black, yellow or indigenous.7 A semistructured anamnesis was used to investigate the presence of chronic diseases, such as diabetes mellitus, hypertension, musculoskeletal, cardiovascular, endocrine, respiratory, neurological and psychiatric diseases, among others. If the answer was yes for any disease, the treatment used was asked. Smoking status was examined in the patient interview.
The International Physical Activity Questionnaire was applied to assess physical activity. It is widely used to estimate the frequency and duration of physical activity levels and has been validated for Brazil.8 Participants were classified as inactive or insufficiently active if they did no physical activity or less than 150 min per week; as active if they did between 150 and 300 min of moderate physical activity or 75 min of intense activity per week or an equivalent combination; and as highly active if they did more than 300 min per week of moderate to intense activity.9
The Alcohol Use Disorders Identification Test–Concise questionnaire was used to assess alcohol consumption. The questionnaire assigns a score on a scale from 0 to 12. For men, a score of 0–3 indicates low risk, 4–5 indicates moderate risk, 6–7 indicates high risk and 8–12 indicates severe risk. For women, a score of 0–2 indicates low risk, 3–5 indicates moderate risk, 6–7 indicates high risk and 8–12 indicates severe risk.10
Blood pressure was measured using a portable device (Welch Allyn Tycos DS48 Pocket aneroid sphygmomanometer) attached to the left arm while the participant was in a sitting position and after at least 5 min of rest. Participants were asked to refrain from smoking or consuming caffeine or alcohol for 30 min prior to measurement. They were instructed by a doctor or trained nurse to relax as much as possible and not to talk during the measurement procedure. The arm was supported at heart level and the bladder of the cuff encircled at least 80% of the arm circumference. When the two measurements were divergent, a third measurement was performed and the mean of the measurements was used for statistical analysis.11 High blood pressure was defined by systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg. Uncontrolled hypertension was defined as systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg in patients taking antihypertensive medications.12
Body mass index (BMI) was calculated according to the formula (weight (kg)/height squared (m2)). Participants were classified into four categories based on WHO guidelines: low weight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2) and obese (≥30 kg/m2).13 Waist circumference (WC) was measured horizontally at the midpoint between the lower edge of the ribs and the top of the iliac crest. A WC≥94 cm for men or ≥80 cm for women was considered as a risk factor for metabolic complications.14
Participants were considered as not medically ready for duty if the results of their ET were suggestive of ischaemia, cardiac arrhythmia, or if they presented with poor health condition, such as disabling musculoskeletal diseases, uncontrolled hypertension or diabetes mellitus. Whenever necessary, they were referred for specialised medical care.
Laboratory assessment
Blood samples were collected by venepuncture after 12 hours of fasting. Total cholesterol and triglycerides were determined by colorimetric assay, and glucose by the hexokinase method. Total cholesterol and triglycerides serum levels were considered ideal if they were <200 mg/dL and <150 mg/dL, respectively.15 A glucose serum level <99 mg/dL was considered normal.16 Uncontrolled diabetes was defined by fasting plasma glucose >130 mg/dL in patients taking antidiabetic medications.16
Cardiorespiratory assessment
Participants aged 40 years old or older without a history of CVD were monitored by a cardiologist while they underwent an ET on a treadmill. Participants were instructed to avoid exhausting activities in the 24 hours prior to the examination, and to eat light food, and not to smoke or drink coffee in the 3 hours prior to the examination. Electrodes were placed on the chest and attached to an ECG machine. Resting ECG, heart rate and blood pressure were measured prior to starting the exercise regimen. Once no limiting factors were detected on the baseline ECG, the participant was placed on a treadmill with a protocol designed to increases in intervals during the exercise. Blood pressure and heart rate were monitored throughout, and the participant was monitored for any developing symptoms, such as chest pain, shortness of breath, dizziness or extreme fatigue.
The most common protocol used for treadmill exercise stress testing was the Bruce protocol. This protocol is divided into successive 3-min stages, which requires the patient to walk faster and at a steeper gradient. The testing protocol could be adjusted according to the participant’s tolerance, aiming for 6–12 min of exercise duration.17 The Ellestad protocol for treadmill testing has a fixed inclination of 10% and a velocity of 1.7 mph for 3 min, 3 mph for 2 min, 4 mph for 2 min and finally 5 mph for 3 min.18 Oxygen consumption was estimated by the formula (male: VO2=1.11×(60–0.55×age); female: VO2=1.11×(48–0.37×age)).
Participants were questioned about any symptoms that they experienced during exercise. All participants were monitored closely during the recovery period until their heart rate and ECG were back to baseline. Indications for terminating the test were: participant request due to severe symptoms (ie, chest pain, shortness of breath or fatigue), severe exercise-induced hypotension or hypertension, horizontal or down sloping ST depression ≥1 mm or ST-segment elevation, new bundle branch block, atrioventricular block, ventricular arrhythmia, reaching maximal heart rate or completing all stages.
Statement of patient and public involvement
Participants were not involved in the design, conduction or analysis of this study. The results will be shared with the participants and the general population through the publication of this article.
Statistical analysis
Data are shown as mean±SD, median (minimum and maximum values) or percentages. An independent samples Student’s t test was used to compare continuous variables, while Fisher’s exact test or the χ2 test was used to compare categorical variables. For the univariate and multivariate analysis, logistic regression models were adjusted for factors associated with the results of the clinical assessment (ready or not ready). Variables with p<0.05 in the univariate analysis were included in the multivariate model. Interaction was assessed for firefighters/police officers and each variable was considered for the multivariate model. If present, the interaction term was included in the model adjusted for other variables. The Wald test was used to assess statistical significance. The OR for not being medically ready for active duties and 95% CI are shown. The Kolmogorov-Smirnov normality test was used to examine whether variables were normally distributed and two-sided p<0.05 were considered statistically significant. Data were analysed using Stata V.14.1 StataCorp LP.
Results
Among the 6621 police officers, 74.1% declared themselves as white, 20,3% as brown (mixed heritage) and 4.6% as black, while among the 1347 firefighters, 78.8% declared themselves as white, 15.9% as brown (mixed heritage) and 3.4% as black. Regarding rank, 12.4% of all individuals held the rank of officer and 87.6% were privates. Table 1 shows the general, clinical, and laboratory characteristics of the police officers and firefighters by sex. Both male and female police officers were significantly older, had longer length of service and higher BMI and WC than firefighters. Systolic and diastolic blood pressure was significantly higher in male police officers than in male firefighters. In addition, the prevalence of overweight and obesity was greater among police officers than firefighters of both sexes. A significantly higher percentage of police officers had WC above the ideal, whereas a significantly higher percentage of firefighters was within the ideal BMI range.
Table 1.
General, clinical and laboratory characteristics of police officers and firefighters, according to sex
| Male | Female | |||||
| Police officers (N=5927) | Firefighters (N=1257) |
P value* | Police officers (N=694) | Firefighters (N=90) |
P value* | |
| Age (years) | 37.6±7.8 | 36.5±8.2 | <0.001 | 32.7±6.5 | 29±4.2 | <0.001 |
| Length of service (years) | 13.5±8.9 | 12.5±9.6 | <0.001 | 7.6±6.7 | 4.2±4.5 | <0.001 |
| Weight (kg) | 85.2±12.3 | 82.3±11.6 | <0.001 | 65.6±10.6 | 62.3±6.5 | <0.001 |
| BMI (kg/m2) | 27.6±3.6 | 26.6±3.3 | <0.001 | 24.2±3.4 | 22.8±1.9 | <0.001 |
| BMI<18.5% | 0.1 | 0.2 | <0.001 | 1.4 | 0.0 | <0.001 |
| 18.5–24.9% | 23.2 | 33.5 | <0.001 | 64.1 | 91.1 | <0.001 |
| 25–29.9% | 54.6 | 51.4 | <0.001 | 28.4 | 8.9 | <0.001 |
| ≥30 % | 22.0 | 15.0 | <0.001 | 6.1 | 0.0 | <0.001 |
| Waist circumference (cm) | 93.9±10 | 90.4±9.5 | <0.001 | 78.6±9.8 | 74.4±5.8 | <0.001 |
| Normal % | 51.0 | 67.6 | <0.001 | 59.8 | 82.2 | <0.001 |
| Increased %* | 49.0 | 32.4 | <0.001 | 40.2 | 17.8 | <0.001 |
| SBP (mm Hg) | 122.3±12.1 | 120.7±10.8 | <0.001 | 112.8±11.3 | 111.3±8.8 | 0.150 |
| DBP (mm Hg) | 78.7±9.1 | 77.6±8.6 | <0.001 | 72.4±8.8 | 71±7.5 | 0.099 |
| Musculoskeletal diseases % | 9.4 | 9.9 | 0.686 | 6.5 | 6.7 | 0.872 |
| Systemic hypertension % | 8.4 | 5.0 | <0.001 | 2.4 | 0.0 | 0.264 |
| Psychiatric diseases % | 3.8 | 2.0 | 0.002 | 6.2 | 3.3 | 0.396 |
| Dyslipidaemia % | 3.4 | 1.6 | 0.001 | 0.72 | 0.0 | 0.917 |
| Diabetes mellitus % | 1.5 | 0.72 | 0.034 | 0.9 | 0.0 | 0.548 |
| Antihypertensives %† | 6.9 | 3.7 | <0.001 | 2.2 | 2.2 | 0.970 |
| Antidepressants % | 2.8 | 1.6 | 0.015 | 5.2 | 2.2 | 0.218 |
| Smoking % | 8.4 | 5.0 | <0.001 | 5.6 | 1.1 | 0.115 |
| Glucose>99 mg/dL % | 12.4 | 10.2 | 0.044 | 4.3 | 1.2 | 0.267 |
| Total cholesterol>190 mg/dL % | 53.1 | 49.4 | 0.025 | 41.9 | 40.5 | 0.889 |
| Triglycerides>150 mg/dL % | 38.8 | 27.2 | <0.001 | 15.1 | 14.3 | 0.973 |
*Increased waist circumference=males ≥94 cm and females ≥80 cm.
†Antihypertensives: ACE inhibitor, diuretic, beta blocker or calcium channel blocker.
BMI, body mass index; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Musculoskeletal diseases were the most commonly self-reported diseases in all groups. In men, hypertension was the second most prevalent disease, followed by psychiatric diseases and dyslipidaemia. Among women, psychiatric diseases were the second most prevalent.
Morbidities, except for musculoskeletal diseases, were significantly more prevalent among male police officers than among male firefighters while there was no difference in the prevalence of comorbidities between female police officers and female firefighters. The most widely used medications were antihypertensive drugs and antidepressants while smoking was more prevalent among police officers than firefighters. Regarding the laboratory assessment, a significantly higher percentage of male police officers had fasting glucose, total cholesterol and triglyceride serum levels above the normal range in comparison to male firefighters.
Table 2 shows the clinical and laboratory characteristics of male police officers and male firefighters by age group, in an attempt to identify a subset of the population with the highest prevalence of risk factors for CVD chronic diseases. Increased WC was more prevalent among police officers in all age groups. Musculoskeletal diseases were the most prevalent disorder in police officers and firefighters in all age groups, without statistically significant differences between them. The prevalence of hypertension was significantly greater among police officers ≥31 years old while psychiatric diseases, dyslipidaemia and diabetes mellitus were more prevalent among police officers >40 years old with their prevalence increasing with age. Excessive alcohol consumption was more frequent among firefighters >40 years old. Police officers did significantly less physical activity than firefighters in all age groups. Cardiac arrhythmia, the abnormality most frequently detected by the ET, was significantly more prevalent among police officers than among firefighters >40 years old. Finally, a significantly greater number of police officers than firefighters were considered to not be medically ready for duty across all age groups.
Table 2.
Univariate analysis of clinical and laboratory data for male police officers and male firefighters by age group
| Male | ||||||
| Age≤30 years | Age 31–40 years | Age>40 years | ||||
| Police officers (n=1307) |
Firefighters (n=361) |
Police officers (n=2336) |
Firefighters (n=459) |
Police officers (n=2284) |
Firefighters (n=437) |
|
| LoS (years) | 4±2.5 | 3.6±2.7* | 10±5.7 | 9.1±6.2** | 22.5±5 | 23.4±5** |
| BMI (kg/m2) | 26.3±3.3 | 25.6±2.8*** | 27.4±3.3 | 26.4±3*** | 28.4±3.7 | 27.7±3.7*** |
| WC≥94 cm (n, %) | 374 (28.6) | 57 (15.8) *** | 1088 (46.6) | 128 (27.9) *** | 1442 (63.1) | 222 (50.8) *** |
| Musculoskeletal disease (n, %) | 76 (5.8) | 18 (5) | 232 (9.9) | 55 (12) | 252 (11) | 51 (11.7) |
| Systemic hypertension (n, %) | 16 (1.2) | 4 (1.1) | 101 (4.3) | 8 (1.7) ** | 382 (16.7) | 51 (11.7) ** |
| Psychiatric diseases (n, %) | 23 (1.8) | 2 (0.6) | 89 (3.8) | 12 (2.6) | 116 (5.1) | 11 (2.5) * |
| Dyslipidaemia (n, %) | 6 (0.5) | 1 (0.3) | 53 (2.3) | 5 (1.1) | 141 (6.2) | 14 (3.2) * |
| Diabetes mellitus (n, %) | 1 (0.1) | 0 (0) | 10 (0.4) | 0 (0) | 80 (3.5) | 9 (2.1) * |
| CVD (n, %) | 5 (0.4) | 2 (0.6) | 17 (0.7) | 6 (1.3) | 44 (1.9) | 7 (1.6) |
| Smoking (n, %) | 98 (7.5) | 16 (4.4) | 188 (8.1) | 20 (4.4) ** | 214 (9.4) | 27 (6.2) * |
| Alcohol consumption (n, %)† | 114 (8.7) | 33 (9.1) | 232 (9.9) | 48 (10.5) | 308 (13.5) | 69 (15.8) * |
| PA<150 min/week (n, %) | 342 (26.2) | 32 (8.9) *** | 739 (31.6) | 67 (14.6) *** | 801 (35.1) | 113 (25.9) *** |
| PA≥150 min/week (n, %) | 442 (33.8) | 148 (41) *** | 888 (38) | 211 (46) *** | 963 (42.2) | 221 (50.6) *** |
| PA≥300 min/week (n, %) | 523 (40) | 181 (50.1) *** | 709 (30.4) | 181 (39.4) *** | 520 (22.8) | 103 (23.6) *** |
| Laboratory tests | ||||||
| Gluc. >99 mg/dL (n, %) | 37 (3.0) | 9 (2.6) | 161 (7.2) | 22 (5.2) | 503 (22.8) | 89 (21.4) |
| TC>190 mg/dL (n, %) | 462 (37.7) | 110 (33.2) | 1199 (54.6) | 209 (50.2) | 131 (60.2) | 249 (61.8) |
| TG>150 mg/dL (n, %) | 285 (23.0) | 46 (13.7) *** | 860 (38.9) | 114 (27.0) *** | 1039 (47.5) | 156 (38.5) ** |
| Exercise stress test | ||||||
| Ischaemia | 0 (0) | 0 (0) | 6 (2.2) | 3 (5.2) | 90 (4.3) | 21 (5.2) |
| Arrhythmia (n, %) | 0 (0) | 0 (0) | 19 (6.9) | 2 (3.5) | 171 (8.2) | 16 (4) ** |
| High blood pressure (n, %) | 0 (0) | 0 (0) | 9 (3.3) | 4 (6.9) | 120 (5.8) | 15 (3.7) |
| Conclusion not ready (n, %) | 236 (18.1) | 34 (9.4) *** | 662 (28.3) | 68 (14.8) *** | 904 (39.6) | 128 (29.3) *** |
**p<0.05; **p<0.01; ***p<0.001.
†Excessive consumption of alcoholic beverages: Alcohol Use Disorders Identification Test–Concise score≥4.
BMI, body mass index; CVD, cardiovascular disease; Gluc, fasting glucose; LoS, length of service; PA, physical activity; TC, total cholesterol; TG, triglycerides; WC, waist circumference.
All of the clinical characteristics were similar between female police officers and female firefighters ≤30 years old, save for physical activity. Female police officers >30 years old had longer length of service, higher BMI and higher WC. There was no significant difference in the prevalence of not being ready for duty between female police officers and female firefighters (table 3).
Table 3.
Univariate analysis of clinical and laboratory data for female police officers and female firefighters by age group
| Female | ||||
| Age≤30 years | Age>30 years | |||
| Police officers (n=299) |
Firefighters (n=57) |
Police officers (n=395) |
Firefighters (n=33) |
|
| LoS (years) | 3.4±2.6 | 3.5±3.2 | 10.9±7.1 | 5.4±6.1*** |
| BMI (kg/m2) | 23.4±2.9 | 22.8±1.8 | 24.8±3.6 | 22.7±2.1*** |
| WC≥80 cm (n, %) | 82 (27.4) | 10 (17.5) | 197 (49.9) | 6 (18.2)*** |
| Musculoskeletal disease (n, %) | 13 (4.4) | 5 (8.8) | 32 (8.1) | 1 (3) |
| SH (n, %) | 2 (0.7) | 0 (0) | 15 (3.8) | 0 (0) |
| Psychiatric diseases (n, %) | 10 (3.3) | 1 (1.8) | 33 (8.4) | 2 (6.1) |
| Dyslipidaemia (n, %) | 2 (0.7) | 0 (0) | 3 (0.8) | 0 (0) |
| Diabetes mellitus (n, %) | 1 (0.3) | 0 (0) | 1 (0.3) | 0 (0) |
| Heart disease (n, %) | 0 (0) | 0 (0) | 2 (0.5) | 0 (0) |
| Smoking (n, %) | 13 (4.4) | 0 (0) | 26 (6.6) | 1 (3) |
| Alcohol consumption (n, %) Ɨ | 12 (4) | 3 (5.3) | 12 (3) | 1 (3) |
| PA<150 min/week (n, %) | 76 (25.4) | 2 (3.5)*** | 117 (29.6) | 4 (12.1) |
| PA≥150 min/week (n, %) | 93 (31.1) | 25 (43.9)*** | 138 (34.9) | 14 (42.4) |
| PA≥300 min/week (n, %) | 130 (43.5) | 30 (52.6)*** | 140 (35.4) | 15 (45.5) |
| Laboratory tests | ||||
| Gluc. >99 mg/dL (n, %) | 4 (1.4) | 1 (1.8) | 14 (4.8) | 28 (100) |
| TC>190 mg/dL (n, %) | 116 (39.9) | 23 (42.6) | 116 (38.9) | 10 (35.7) |
| TG>150 mg/dL (n, %) | 42 (14.4) | 8 (14.8) | 40 (13.8) | 3 (10.7) |
| Exercise stress test | ||||
| Ischaemia (n, %) | 0 (0) | 0 (0) | 8 (8) | 0 (0) |
| Arrhythmia (n, %) | 0 (0) | 0 (0) | 1 (1) | 1 (50)* |
| High blood pressure (n, %) | 0 (0) | 0 (0) | 4 (4) | 0 (0) |
| Conclusion not ready (n, %) | 36 (12) | 5 (8.8) | 69 (17.5) | 3 (9.1) |
**p<0.05; **p<0.01; ***p<0.001.
†Excessive consumption of alcoholic beverages: AUDIT-C score≥3.
BMI, body mass index; Gluc, fasting glucose; Los, length of service; PA, physical activity; SH, systemic hypertension; TC, total cholesterol; TG, triglycerides; WC, waist circumference.
After adjusting the multivariate model for predicting unhealthy conditions and using the explanatory variables of police officer/firefighter, sex and age, the probability of these workers being considered as not ready for active duty could be estimated (table 4).
Table 4.
Univariate and multivariate logistic regression model for explanatory variables
| Variable | Classification | Not ready | P value* | P value† | OR | 95% CI |
| Firefighter/police officer | Firefighter (ref.) | 17.7% | ||||
| Police officer | 28.8% | <0.001 | <0.001 | 1.50 | 1.27 to 1.77 | |
| Sex and age group | Female≤30 years (ref.) | 11.5% | ||||
| Female>30 years | 16.8% | 0.036 | 0.597 | 1.12 | 0.73 to 1.74 | |
| Male≤30 years | 16.2% | 0.027 | 0.024 | 1.52 | 1.06 to 2.19 | |
| Male 31–40 years | 26.1% | <0.001 | <0.001 | 2.03 | 1.43 to 2.89 | |
| Male>40 years | 37.9% | <0.001 | <0.001 | 2.55 | 1.79 to 3.62 | |
| Waist circumference | Normal (ref.) | 18.8% | ||||
| Increased‡ | 36.7% | <0.001 | <0.001 | 1.63 | 1.45 to 1.83 | |
| Physical activity | 300 min/week (ref.) | 19.2% | ||||
| ≥150 min/week | 26.8% | <0.001 | <0.001 | 1.31 | 1.14 to 1.51 | |
| <150 min/week | 35.6% | <0.001 | <0.001 | 1.67 | 1.44 to 1.93 | |
| Smoking | No (ref.) | 25.8% | ||||
| Yes | 41.1% | <0.001 | <0.001 | 1.75 | 1.45 to 2.12 | |
| Alcohol consumption | Low risk (ref.) | 25.4% | ||||
| Moderate to severe risk § | 39.8% | <0.001 | <0.001 | 1.44 | 1.22 to 1.70 | |
| Hypertension | No (ref.) | 24.5% | ||||
| Yes | 57.5% | <0.001 | <0.001 | 2.29 | 1.88 to 2.79 | |
| Dyslipidaemia | No (ref.) | 25.9% | ||||
| Yes | 60.9% | <0.001 | <0.001 | 2.65 | 1.96 to 3.58 | |
| Diabetes mellitus | No (ref.) | 26.4% | ||||
| Yes | 66.7% | <0.001 | <0.001 | 2.95 | 1.85 to 4.70 | |
| Heart disease | No (ref.) | 26.7% | ||||
| Yes | 49.4% | <0.001 | 0.002 | 2.13 | 1.32 to 3.45 | |
| Psychiatric diseases | No (ref.) | 26.6% | ||||
| Yes | 35.8% | <0.001 | 0.039 | 1.33 | 1.02 to 1.74 | |
| Total cholesterol | ≤190 mg/dL (ref.) | 18.2% | ||||
| >190 mg/dL | 36.1% | <0.001 | <0.001 | 2.16 | 1.93 to 2.42 |
*Univariate logistical regression model and Wald test, p<0.05.
†Multivariate logistical regression model and Wald test, p<0.05.
‡Women≥80 cm; men≥94 cm.
§Excessive consumption of alcoholic beverages: Alcohol Use Disorders Identification Test–Concise score≥4 (men), ≥3 (women).
Ref., Reference group.
The multivariate logistic regression model included the explanatory variables shown in table 5. The best health profiles were found among female firefighters while the worst health profiles were found among male firefighters ≥40 years old and male police officers ≥30 years old. Furthermore, male police officers >40 years old presented the highest probability of not being medically ready for active duty.
Table 5.
Probability of a police officer or firefighter being classified as not ready for duty
| Profile | Probability of not being ready* | ||
| Profession | Sex | Age (years) | |
| Firefighter | Female | ≤30 | 7.0% |
| Firefighter | Female | >30 | 10.1% |
| Firefighter | Male | ≤30 | 10.3% |
| Police officer | Female | ≤30 | 12.4% |
| Firefighter | Male | 31–40 | 17.1% |
| Police officer | Female | >30 | 17.4% |
| Police officer | Male | ≤30 | 17.8% |
| Firefighter | Male | >40 | 26.3% |
| Police officer | Male | 31–40 | 27.9% |
| Police officer | Male | >40 | 40.1% |
*Multivariate logistic regression model.
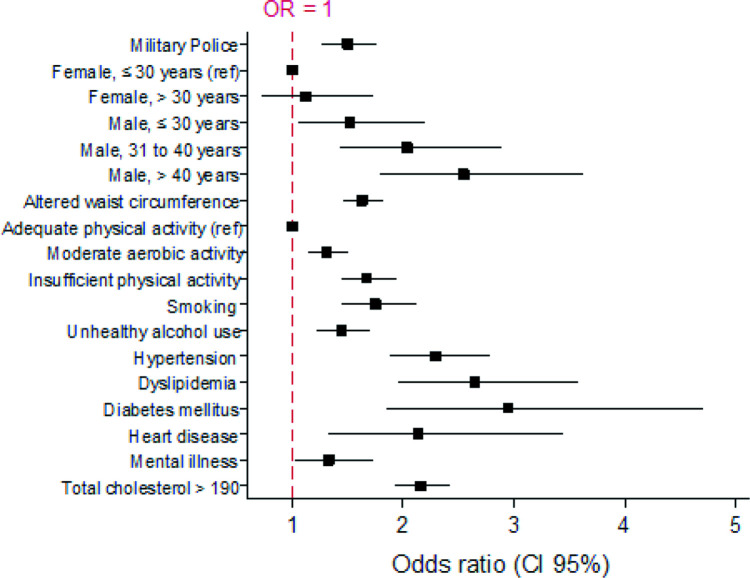
The main non-modifiable risk factors associated with not being medically ready for duty were: being a police officer (OR 1.50, 95% CI 1.27 to 1.77), being male aged 31–40 years (OR 2.03, 95% CI 1.43 to 2.89), and being≥40 years old (OR 2.55 95% CI 1.79 to 3.62). Moreover, the following modifiable risk factors were identified: high WC (OR 1.63, 95% CI 1.45 to 1.83), physical inactivity (OR 1.67, 95% CI 1.44 to 1.93), smoking (OR 1.75, 95% CI 1.45 to 2.12) and excessive consumption of alcohol (OR 1.44, 95% CI 1.22 to 1.70). The medical conditions associated with not being medically ready for duty were hypertension (OR 2.29, 95% CI 1.85 to 4.70), dyslipidaemia (OR 2.65, 95% CI 1.96 to 3.58), diabetes mellitus (OR 2.95, 95% CI 1.97 to 5.03), heart disease (OR 2.13, 95% CI 1.32 to 3.45), psychiatric diseases (OR 1.33, 95% CI 1.02 to 1.74) and high serum levels of total cholesterol (OR 2.16, 95% CI 1.93 to 2.42) (figure 1).
Figure 1.
Multivariate logistic regression analysis of characteristics associated with not being medically ready for duty. Ref, reference.
Discussion
This is the largest study of the epidemiological profile of military police officers and firefighters in Paraná. The probability of male police officers between the ages of 31 and 40 not being ready was similar to that of male firefighters >40 years old, indicating that the health condition of male police officers deteriorates earlier. Our findings indicate that the priority for regular medical assessment should be given to this subset of male police officers >30 years old and firefighters >40 years old, who in some cases already had increased WC, diabetes mellitus, CVD and dyslipidaemia, in order to facilitate access to healthcare interventions and to stimulate healthy daily habits.
Several modifiable risk factors for CVD were observed, including increased WC, obesity, physical inactivity and smoking. They were more common among participants over 30 years old, which suggests that in addition to ageing, work-related risk factors may play a central to role in the deterioration of health condition.2–5 This finding underlies the need for better planning and investment in prevention and early diagnosis in this population. Furthermore, behaviour interventions to encourage healthy habits should be implemented in order to help to modify the profile of chronic diseases.
Similar to our findings, Nogueira et al found a prevalence of 54.3% for overweight and 14.7% for obesity in a study that investigated the relationship between cardiorespiratory fitness and body composition in 4237 Brazilian firefighters in the Federal District.19 Damacena et al recently reported that the prevalence of obesity was 10.99% among male firefighters (N=892) and that there was an overall high prevalence of overweight of 48.65%. Recent online survey of 2398 female career firefighters, one may consider female firefighters to have been successful in overcoming the occupational risks, such as a challenging nutritional environment, inconsistent schedules, limited time for fitness and the metabolic impact of shift work, that expose firefighters to increased risk of obesity.20 21 Although females still represent a small percentage of the police force and firefighting service, they are an integral part of the workforce and medical attention tailored to their specific needs may lead to better health outcomes.
A study that investigated the prevalence of metabolic syndrome and its risk factors among 10 348 Chinese police officers, found a high prevalence of hypertriglyceridaemia (40.8%), hypertension (38.2%) and abdominal obesity (25.7%).22 In our study, total cholesterol, triglycerides and glucose serum levels were above the ideal range in a large number of police officers and firefighters of both sexes and all age groups, but particularly among male police officers, suggesting a greater risk for metabolic diseases in this population. The analysis by age group revealed that the prevalence of obesity and high WC increased with age. The association of weight status and increased risk for atherosclerotic CVD was greater among older firefighters highlighting the aging-related increase in CVD risk, and that additional screening may be necessary among older firefighters to ensure that they are healthy enough to continue with the strenuous and stressful work of firefighting.23 Low levels of physical activity, unhealthy eating habits, demanding jobs, sleep disorders and stress, which are common during the course of a police officer’s or firefighter’s working life, may also help to explain the high prevalence of CVD in these populations.24 25
The duties performed by police officers and firefighters were associated with musculoskeletal disorders, particularly lower back pain, suggesting the need for preventive measures and ergonomic control programmes in the workplace.26–28
A study by Han et al compared the prevalence of chronic diseases among 860 221 public-sector workers in South Korea and found that police officers had a significantly higher risk for angina pectoris, acute myocardial infarction and cerebrovascular disease, while firefighters were more susceptible to post-traumatic stress disorders.1 In the present study, psychiatric diseases were more prevalent among police officers, particularly among women over 30 years old. The close correlation between occupational stress and mental illness has been observed in previous studies.29 30 The different instruments used for work-related psychological assessments in these studies prevent comparison of these findings. Although police officers and firefighters reported that they were receiving psychiatric treatment, this may not reflect the true prevalence of this health issue, as some participants may have omitted this information for fear of stigmatisation. The overall prevalence of smoking among police officers and firefighters was lower than in the general population in the state of Paraná which is 11.3%.31 The high prevalence of mental diseases, alcoholism, smoking and substance abuse among police officers and firefighters highlights not only the need for better medical assessment to ensure timely diagnosis and treatment, but also the need for public policies to promote preventive health measures.
The present study has certain limitations that must be mentioned. First, the cross-sectional design does not allow causal relationship between risk factors and comorbidities to be established. Nevertheless, the study population was recruited after a thorough medical assessment to ensure that healthy candidates are accepted in the police and firefighting services. In addition, the study population underwent an elective medical assessment and had not requested a medical examination of their own accord. The fact that only the serum levels of total cholesterol were measured, and not high-density lipoprotein or low-density lipoprotein, prevented a more detailed assessment of CVD risk.
Furthermore, the low number of women (11.7% of police officers and 7.2% of firefighters) underpowered the statistical analysis of this subgroup of workers. Lastly, the specific nature of the study population does not allow for the generalisation of the findings to other populations.
Long-term longitudinal studies are needed to understand the effect of the different activities carried out by police officers and firefighters on their health status. The identification of the causes of the deterioration of their health condition may allow for the adoption of prompt interventions to prevent disease evolution and promote both physical and mental health.
Conclusions
Our study highlights the need for regular medical assessments and follow-ups of police officers and firefighters, as well as for the promotion of preventive healthcare. These measures need to be offered earlier and more frequently for police officers. The health condition of female police officers and firefighters should not be neglected as they are exposed to the same work-related risk factors as men and, consequently, may also present a high prevalence of CVD risk factors and chronic diseases. It should be stressed that the police officers and firefighters included in this study were working under normal conditions and were unaware of their medical status. This scenario may adversely affect both the workers’ own health and the health of others when they are performing their duties.
Supplementary Material
Acknowledgments
The authors would like to thank all the police officers and firefighters who took part in this study.
Footnotes
Contributors: ARdS was responsible for data collection, planning the study, analysis and interpretation of the data and writing the manuscript. MFKI and MO assisted with the planning of the study and interpretation of the results. MO was responsible for statistical analysis. FCB took part in the interpretation of the data and supervised the writing of the manuscript. All authors contributed to the editing and reviewing of this paper. ARdS is the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. The data are available from the corresponding author upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Health Sciences Department, Federal University of Paraná Reference number 85780418.0.0000.0102. Participants gave informed consent to participate in the study before taking part.
References
- 1.Han M, Park S, Park JH, et al. Do police officers and firefighters have a higher risk of disease than other public officers? A 13-year nationwide cohort study in South Korea. BMJ Open 2018;8:e019987. 10.1136/bmjopen-2017-019987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Violanti JM, Ma CC, Fekedulegn D, et al. Associations between body fat percentage and fitness among police officers: a statewide study. Saf Health Work 2017;8:36–41. 10.1016/j.shaw.2016.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moffatt SM, Stewart DF, Jack K, et al. Cardiometabolic health among United States firefighters by age. Prev Med Rep 2021;23:101492. 10.1016/j.pmedr.2021.101492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poston WSC, Haddock CK, Jahnke SA, et al. The prevalence of overweight, obesity, and substandard fitness in a population-based firefighter cohort. J Occup Environ Med 2011;53:266–73. 10.1097/JOM.0b013e31820af362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zimmerman FH. Cardiovascular disease and risk factors in law enforcement personnel: a comprehensive review. Cardiol Rev 2012;20:159–66. 10.1097/CRD.0b013e318248d631 [DOI] [PubMed] [Google Scholar]
- 6.Sörensen L, Smolander J, Louhevaara V, et al. Physical activity, fitness and body composition of Finnish police officers: a 15-year follow-up study. Occup Med 2000;50:3–10. 10.1093/occmed/50.1.3 [DOI] [PubMed] [Google Scholar]
- 7.7IBGE, Síntese de indicadores sociais . Uma análise das Condições de Vida dA População Brasileira. Available: http://www.ibge.gov.br/homeestatistica/populacao/condicaodevida/indicadoresminimos/sinteseindicsociais2010/SIS_2010.pdf [Accessed 24 Jun 2021].
- 8.Matsudo S, Araújo T, Matsudo V. Questionário Internacional de Atividade Física (IPAQ): estudo de validade E reprodutibilidade no Brasil. Rev Bras Ativ Fís Saúde 2012;6:5–18 https://rbafs.org.br/RBAFS/article/view/931 [Google Scholar]
- 9.Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA 2018;320:2020–8. 10.1001/jama.2018.14854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bush K, Kivlahan DR, McDonell MB, et al. The audit alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. ambulatory care quality improvement project (ACQUIP). alcohol use disorders identification test. Arch Intern Med 1998;158:1789–95. 10.1001/archinte.158.16.1789 [DOI] [PubMed] [Google Scholar]
- 11.Malachias M, Plavnik FL, Machado CA, et al. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol 2016;107:1–6. 10.5935/abc.20160151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barroso WKS, Rodrigues CIS, Bortolotto LA. Diretrizes brasileiras de hipertensão arterial–2020. Arq Bras Cardiol 2021;116:516–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization . Bmi classification: who, 2006. Available: http://apps.who.int/bmi/index.jsp?introPage=intro_3.html [Accessed 10 Set 2020].
- 14.World Health Organization . Obesity: preventing and managing the global epidemic. Report of a world Health organization consultation. who obesity technical report series, no. 284. Geneva: World Health Organization, 2000: 256. [PubMed] [Google Scholar]
- 15.Jellinger PS, Handelsman Y, Rosenblit PD, et al. American association of clinical endocrinologists and American College of endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract 2017;23:1–87. 10.4158/EP171764.APPGL [DOI] [PubMed] [Google Scholar]
- 16.American Diabetes Association . Standards of Medical Care in Diabetes-2019 Abridged for Primary Care Providers. Clin Diabetes 2019;37:11–34. 10.2337/cd18-0105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bruce RA. Methods of exercise testing. step test, bicycle, treadmill, isometrics. Am J Cardiol 1974;33:715–20. 10.1016/0002-9149(74)90211-2 [DOI] [PubMed] [Google Scholar]
- 18.Ellestad MH, Allen W, Wan MC, et al. Maximal treadmill stress testing for cardiovascular evaluation. Circulation 1969;39:517–22. 10.1161/01.CIR.39.4.517 [DOI] [PubMed] [Google Scholar]
- 19.Nogueira EC, Porto LGG, Nogueira RM, et al. Body composition is strongly associated with cardiorespiratory fitness in a large Brazilian military firefighter cohort: the Brazilian firefighters study. J Strength Cond Res 2016;30:33–8. 10.1519/JSC.0000000000001039 [DOI] [PubMed] [Google Scholar]
- 20.Damacena FC, Batista TJ, Ayres LR, et al. Obesity prevalence in Brazilian firefighters and the association of central obesity with personal, occupational and cardiovascular risk factors: a cross-sectional study. BMJ Open 2020;10:e032933. 10.1136/bmjopen-2019-032933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jahnke SA, Kaipust C, Jitnarin N, et al. Prevalence and predictors of obesity among women in the fire service. Occup Environ Med 2022;79:289–94. 10.1136/oemed-2021-107590 [DOI] [PubMed] [Google Scholar]
- 22.Zhang J, Liu Q, Long S, et al. Prevalence of metabolic syndrome and its risk factors among 10,348 police officers in a large city of China: a cross-sectional study. Medicine 2019;98:e17306. 10.1097/MD.0000000000017306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hollerbach BS, Mathias KC, Stewart D, et al. A cross-sectional examination of 10-year atherosclerotic cardiovascular disease risk among US firefighters by age and weight status. J Occup Environ Med 2020;62:1063–8. 10.1097/JOM.0000000000002057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Poston WSC, Haddock CK, Jahnke SA, et al. An examination of the benefits of health promotion programs for the National fire service. BMC Public Health 2013;13:805. 10.1186/1471-2458-13-805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Choi B, Schnall P, Dobson M, et al. Exploring occupational and behavioral risk factors for obesity in firefighters: a theoretical framework and study design. Saf Health Work 2011;2:301–12. 10.5491/SHAW.2011.2.4.301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choi B, Steiss D, Garcia-Rivas J, et al. Comparison of body mass index with waist circumference and skinfold-based percent body fat in firefighters: adiposity classification and associations with cardiovascular disease risk factors. Int Arch Occup Environ Health 2016;89:435–48. 10.1007/s00420-015-1082-6 [DOI] [PubMed] [Google Scholar]
- 27.MCdS M, SGd A, RVCd O. Impacto das atividades profissionais Na saúde física E mental DOS policiais civis E militares do Rio de Janeiro (RJ, Brasil). Ciênc Saúde Coletiva 2011;16:2199–209. [DOI] [PubMed] [Google Scholar]
- 28.Benyamina Douma N, Côté C, Lacasse A. Quebec serve and protect low back pain study: a web-based cross-sectional investigation of prevalence and functional impact among police officers. Spine 2017;42:1485–93. 10.1097/BRS.0000000000002136 [DOI] [PubMed] [Google Scholar]
- 29.Schilling R, Colledge F, Ludyga S, et al. Does cardiorespiratory fitness moderate the association between occupational stress, cardiovascular risk, and mental health in police officers? Int J Environ Res Public Health 2019;16:2349. 10.3390/ijerph16132349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Purba A, Demou E. The relationship between organisational stressors and mental wellbeing within police officers: a systematic review. BMC Public Health 2019;19:1286. 10.1186/s12889-019-7609-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brasil. Ministério da Saúde . Vigitel Brasil 2019: vigilância de fatores de risco E proteção para doenças crônicas POR inquérito telefônico: estimativas sobre frequência E distribuição sociodemográfica de fatores de risco E proteção para doenças crônicas nas capitais DOS 26 estados brasileiros E no Distrito federal em 2019. Brasília: Ministério da Saúde, 2019. http://www.crn1.org.br/wp-content/uploads/2020/04/vigitel-brasil-2019-vigilancia-fatores-risco.pdf? [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. The data are available from the corresponding author upon reasonable request.