Abstract
Background
The antitumor efficacy of immune checkpoint inhibitors (ICIs) has increasingly emerged during the last few years. However, there is a need to identify the safety profile of these agents more comprehensively, including liver toxicity.
Materials and methods
Herein, we performed a meta-analysis to assess the risk of all-grade and grade 3–4 hypertransaminasemia in cancer patients receiving ICIs—as monotherapy or in combination with other anticancer agents. All the relevant trials were retrieved through EMBASE, Cochrane Library, and PubMed/Medline databases; eligible studies were selected according to PRISMA statement. The pooled relative risk (RR) and 95% confidence interval (CI) were extracted.
Results
Fifty-nine studies were included. The pooled RRs for all-grade AST and ALT increase were 1.45 (95% CI 1.26–1.67) (Supplementary Fig. 3) and 1.51 (95% CI 1.29–1.77) in patients receiving ICIs monotherapy and immune-based combinations compared to control treatment, respectively. The pooled RRs for grade 3–4 AST and ALT increase were 2.16 (95% CI 1.77–2.64) and 2.3 (95% CI 1.91–2.77).
Conclusions
According to our results, ICIs monotherapy and immune-based combinations were associated with higher risk of all-grade and grade 3–4 hypertransaminasemia. Monitoring liver function should be recommended in cancer patients treated with ICIs monotherapy or immune-based combination, and in case of underlying liver disease, a careful risk–benefit assessment appears as a mandatory need.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00262-023-03366-x.
Keywords: Hypertransaminasemia, Liver toxicity, Cancer, Immunotherapy, Immune checkpoint inhibitors, ALT
Introduction
The global cancer burden is destined to increase in the next few years, and cancer represents a serious threat to public health worldwide. In fact, the rising proportion of adults and elderly patients are two important factors underlying the increase in cancer-related mortality, and although the incidence of some solid tumors has decreased in some countries, the limited efficacy of systemic treatments in several setting and diseases remains a crucial issue [1].
The advent of immune checkpoint inhibitors (ICIs) has represented a therapeutic revolution over the last ten years [2], with immunotherapy representing an effective treatment strategy in multiple hematological and solid tumors, as reported in several practice-changing clinical trials [3–7]. ICIs, whose mechanism of action is based on the activation of the immune system, are able to modulate T lymphocytes and to target immune checkpoints such as programmed cell death protein 1 (PD-1), programmed cell death ligand 1 (PD-L1), and cytotoxic t lymphocyte-associated protein 4 (CTLA-4). ICIs, as monotherapy or in combination with other anticancer agents, have achieved unprecedented results in melanoma, renal cell carcinoma (RCC), non-small cell lung cancer (NSCLC), hepatocellular carcinoma (HCC), colorectal cancer, urothelial carcinoma (UC), and several others [8–14]. Although the safety profile of ICIs monotherapy and immune-based combinations is considered acceptable, ICIs have a specific set of treatment-related adverse events, which are commonly defined as immune-related adverse events (irAEs). IrAEs are determined by an erroneous activation of the immune system and may affect multiple organ systems, ranging from liver to thyroid, lung, pancreas, and skin [15, 16]. In addition, the type and grade of irAEs may widely vary according to the type of ICI, the tumor type, and the immune-based combination, since the concomitant use of systemic chemotherapy or tyrosine kinase inhibitors may increase not only the anticancer activity but also adverse events, which sometimes are even life-threatening [17–19].
According to findings from clinical trials, ICIs are deemed to determine hepatotoxicity in a percentage ranging from 1 to 10% of cases, with patients often presenting with elevation of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) [20]. From a temporal perspective, these alterations are frequently observed between 6 and 14 weeks after the start of treatment and most of these adverse events are managed by corticosteroid use, while the addition of other immunosuppressive treatments is evaluated in case of lack of response to corticosteroids [21, 22]. Since the use of ICIs and immune-based combinations is destined to grow in cancer patients, further investigations to comprehensively characterize the impact of these events are needed. Based on these premises, in the MOUSEION-05 we aimed at investigating the risk of all-grade and grade 3–4 hypertransaminasemia in randomized controlled clinical trials (RCTs) assessing ICIs monotherapy and immune-based combinations in cancer patients.
Materials and methods
Search strategy
All phase II and III clinical trials published from June 15, 2008, to November 10, 2022, evaluating immunotherapy and immune-based combinations in cancer patients were retrieved by five different authors. Keywords used for searching on EMBASE, Cochrane Library, and PubMed/ Medline were the following: “immunotherapy” OR “nivolumab” OR “ipilimumab” OR “atezolizumab” OR “pembrolizumab” OR “durvalumab” OR “avelumab” OR “tremelimumab” OR “immune checkpoint inhibitors” OR “immunotherapy” AND “hypertransaminasemia” OR “increased AST” OR “increased ALT” OR “hepatotoxicity” AND “cancer” OR “cancer patients.” Only articles written in the English language and published in peer-reviewed journals were included. Proceedings of the main international oncological meetings (such as European Society of Medical Oncology [ESMO], American Society of Clinical Oncology [ASCO], American Association for Cancer Research [AACR], and European CanCer Organization [ECCO]) were also searched from 2008 onward for relevant trials and/or abstracts.
Selection criteria
Trials retrieved from the first analysis we conducted were subsequently restricted to: 1) prospective phase II and III RCTs in cancer patients; 2) participants receiving ICIs monotherapy or immune-based combinations; and 3) studies with available data in terms of all-grade and grade 3–4 hypertransaminasemia in the immune-based combination group and the control arm. Clinical trials with two different immunotherapy arms were split in two sections in the analysis.
Data extraction
The following data were extracted for each publication: 1) RCT general information (author, year, phase); 2) interventions and dosage of drugs; 3) number of cancer patients; and 4) available outcomes in terms of all-grade and grade 3–4 hypertransaminasemia.
Available outcomes were measured as relative risks (RRs) and 95% confidence intervals (CIs). Five separate authors conducted the search and identification independently. The meta-analysis was conducted according to Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines (Supplementary) [23].
Statistical design
All statistical analyses were performed using R Studio.
RRs were used to analyze dichotomous variables, including all-grade and grade 3–4 hypertransaminasemia in cancer patients treated with ICIs monotherapy and immune-based combinations versus control treatment. Forest plots were used to assess RRs. Statistical heterogeneity between the included trials was examined using the Chi-square test and the I2 statistic; substantial heterogeneity was considered to be present when the I2 value was greater than 50% or there was a low P value (< 0.10) in the Chi-square test [24]. When no heterogeneity was noted, the fixed effects model was used, while the random-effects model was applied in the presence of significant heterogeneity.
Results
Selected studies
A total of 6586 potentially relevant reports were identified, which were restricted to 59 following independent evaluation of five authors [25–82]. We excluded 6522 records as non-pertinent reports (editorials, case reports, ongoing studies/trials in progress, review articles, preclinical studies, retrospective studies, systematic reviews and meta-analyses, single-arm trials, non-randomized trials, etc.). Eligible studies were identified and selected as shown in Supplementary Fig. 2; a summary of the included trials is presented in Table 1.
Table 1.
Summary of the included studies
| Reference | Phase | Malignancy | Treatment arm | Control arm |
|---|---|---|---|---|
|
Powles T et al. (A) [25] |
3 | UC | Durvalumab + tremelimumab | Chemotherapy |
|
Powles T et al. (B) [25] |
3 | UC | Durvalumab | Chemotherapy |
|
Goldman et al. (A) [26] |
3 | SCLC | Durvalumab + carboplatin + etoposide | Carboplatin + etoposide |
|
Goldman et al. (B) [26] |
3 | SCLC | Durvalumab + tremelimumab + carboplatin + etoposide | Carboplatin + etoposide |
|
Renouf DJ et al [27] |
2 | PDAC | Durvalumab + tremelimumab + chemotherapy | Chemotherapy |
|
Robert C et al [28] |
3 | Melanoma | Nivolumab | Dacarbazine |
|
Borghaei H et al [29] |
3 | Non-squamous NSCLC | Nivolumab | Docetaxel |
|
Brahmer J et al [30] |
3 | Squamous NSCLC | Nivolumab | Docetaxel |
|
Larkin J et al [31] |
3 | Melanoma | Nivolumab | Chemotherapy |
|
Gillison ML [32] |
3 | HNT | Nivolumab | Chemotherapy |
|
Cella D et al [33] |
3 | RCC | Nivolumab + ipilimumab | Sunitinib |
|
Wu YL et al [34] |
3 | NSCLC | Nivolumab | Docetaxel |
|
Reardon DA et al [35] |
3 | Glioblastoma | Nivolumab | Bevacizumab |
|
Janjigian YY et al [36] |
3 | GC/GEJC | Nivolumab + chemotherapy | Chemotherapy |
|
Choueiri T et al [37] |
3 | RCC | Nivolumab + cabozantinib | Sunitinib |
|
Hamanishi et al [38] |
3 | Ovarian cancer | Nivolumab | Chemotherapy |
|
Hayashi H et al [39] |
3 | NSCLC | Nivolumab | Chemotherapy |
|
Schmid P et al [40] |
3 | TNBC | Atezolizumab + nab-paclitaxel | Nab-paclitaxel |
|
Socinski MA et al [41] |
3 | Non-squamous NSCLC | Atezolizumab + bevacizumab + chemotherapy | Bevacizumab + chemotherapy |
|
Powles T et al [42] |
3 | UC | Atezolizumab | Chemotherapy |
|
Eng C et al. (A) [43] |
3 | CRC | Atezolizumab + cobimetinib | Regorafenib |
|
Eng C et al. (B) [43] |
3 | CRC | Atezolizumab | Regorafenib |
|
West H et al [44] |
3 | Non-squamous NSCLC | Atezolizumab plus chemotherapy | Chemotherapy |
|
Finn RS et al [45] |
3 | HCC | Atezolizumab + bevacizumab | Sorafenib |
|
Mittendorf EA et al [46] |
3 | TNBC | Atezolizumab + chemotherapy | Chemotherapy |
|
Herbst RS et al [47] |
3 | NSCLC | Atezolizumab | Chemotherapy |
|
Emens LA et al [41] |
2 | HER2 + BC | Atezolizumab + TDM1 | Placebo + TDM1 |
|
Felip E et al [48] |
3 | NSCLC | Atezolizumab | BSC |
|
Bellmunt J et al [49] |
3 | UC | Atezolizumab | Observation |
|
Miles D et al [50] |
3 | TNBC | Atezolizumab + chemotherapy | Placebo + chemotherapy |
|
Cho BC et al [51] |
2 | NSCLC | Atezolizumab + tiragolumab | Atezolizumab + placebo |
|
Kelley RK et al [52] |
3 | HCC | Atezolizumab + cabozantinib | Sorafenib |
|
Mettu NB et al [53] |
2 | CRC | Atezolizumab + bevacizumab + chemotherapy | Chemotherapy + bevacizumab |
|
Huober J et al [54] |
3 | HER2 + BC | Atezolizumab + pertuzumab + trastuzumab + chemotherapy | Placebo + pertuzumab + trastuzumab + chemotherapy |
|
Pal SK et al [55] |
3 | RCC | Atezolizumab | Placebo |
|
Powles T et al [83] |
3 | CRPC | Atezolizumab + enzalutamide | Enzalutamide |
|
Bang YJ et al [56] |
3 | GC/GEJC | Avelumab | Chemotherapy |
|
Barlesi F et al [57] |
3 | NSCLC | Avelumab | Docetaxel |
|
Motzer RJ et al [58] |
3 | RCC | Avelumab + axitinib | Sunitinib |
|
Powles T et al [59] |
3 | UC | Avelumab | BSC |
|
Moehler et al [60] |
3 | GC/GEJC | Avelumab | Chemotherapy |
|
Lee NY et al [61] |
3 | HNT | Avelumab + chemoradiotherapy | Chemoradiotherapy |
|
Pujade-Lauraine E. et al [62] |
3 | Ovarian cancer | Avelumab | PLD |
|
Pujade-Lauraine E. et al [62] |
3 | Ovarian cancer | Avelumab ± PLD | PLD |
|
Monk BJ et al [63] |
3 | Ovarian cancer | Chemotherapy—> manteinance avelumab | Chemotherapy—> observation |
|
Monk BJ et al [63] |
3 | Ovarian cancer | Chemotherapy + avelumab—> manteinance avelumab | Chemotherapy—> observation |
|
Redman J et al [64] |
2 | CRC | mFOLFOX + bevacizumab + AdCEA vaccine + avelumab | mFOLFOX + bevacizumab |
|
RS Herbst et al [65] |
2/3 | NSCLC | Pembrolizumab | Docetaxel |
|
Mok TSK et al [66] |
3 | NSCLC | Pembrolizumab | Chemotherapy |
|
Bellmunt J et al [67] |
3 | UC | Pembrolizumab | Chemotherapy |
|
Powles T et al [68] |
3 | RCC | Pembrolizumab + axitinib | Sunitinib |
|
Schmid P et al [69] |
3 | TNBC | Pembrolizumab + chemotherapy | Chemotherapy |
|
Ferrucci PF et al [70] |
2 | Melanoma | Pembrolizumab + dabrafenib + trametinib | Placebo + dabrafenib + trametinib |
|
Tolaney SM et al [71] |
2 | Breast Cancer | Pembrolizumab + eribulina | Eribulina |
|
Motzer RJ et al [72] |
3 | RCC | Pembrolizumab + lenvatinib | Everolimus + lenvatinib / sunitinib |
|
Awad MM et al [73] |
2 | Non-squamous NSCLC | Pembrolizumab + chemotherapy | Chemotherapy |
|
Colombo N et al [74] |
3 | Cervical Cancer | Pembrolizumab + chemotharapy + bevacizumab | Placebo + chemotherapy + bevacizumab |
|
Powles T et al. (A) [75] |
3 | UC | Pembrolizumab + chemotherapy | Chemotherapy |
|
Powles T et al. (B) [76] |
3 | UC | Pembrolizumab | Chemotherapy |
|
Sun JM et al [77] |
3 | Oesophageal Cancer | Pembrolizumab + chemotherapy | Placebo + chemotherapy |
|
Winer EP et al [76] |
3 | TNBC | Pembrolizumab | Chemotherapy |
|
Diaz LA et al [78] |
3 | CRC | Pembrolizumab | Chemotherapy |
|
Makker V et al [79] |
3 | Endometrial cancer | Pembrolizumab + lenvatinib | Chemotherapy |
|
Chung HC et al [80] |
3 | GC/GEJC | Pembrolizumab | Chemotherapy |
|
Reckamp KL et al [81] |
2 | NSCLC | Pembrolizumab + ramucirumab | Chemotherapy |
BC breast cancer, CRC colorectal cancer, GC/GEJC gastric cancer/gastroesophageal cancer, HCC hepatocellular carcinoma, HNT head and neck cancer, NSCLC non-small cell lung cancer, PDAC pancreatic ductal adenocarcinoma, RCC renal cell carcinoma, SCLC small cell lung cancer, TNBC triple negative breast cancer, UC urothelial cancer
All-grade AST and ALT increase
The pooled RRs for all-grade AST and ALT increase were 1.45 (95% CI 1.26–1.67) (Supplementary Fig. 2) and 1.51 (95% CI 1.29–1.77) (Supplementary Fig. 3), in patients receiving ICIs monotherapy and immune-based combinations compared to control arm, respectively. Both analyses were associated with substantial heterogeneity (I2 of 57% and 64%, respectively), and thus, a random effect model was used.
Grade 3–4 AST and ALT increase
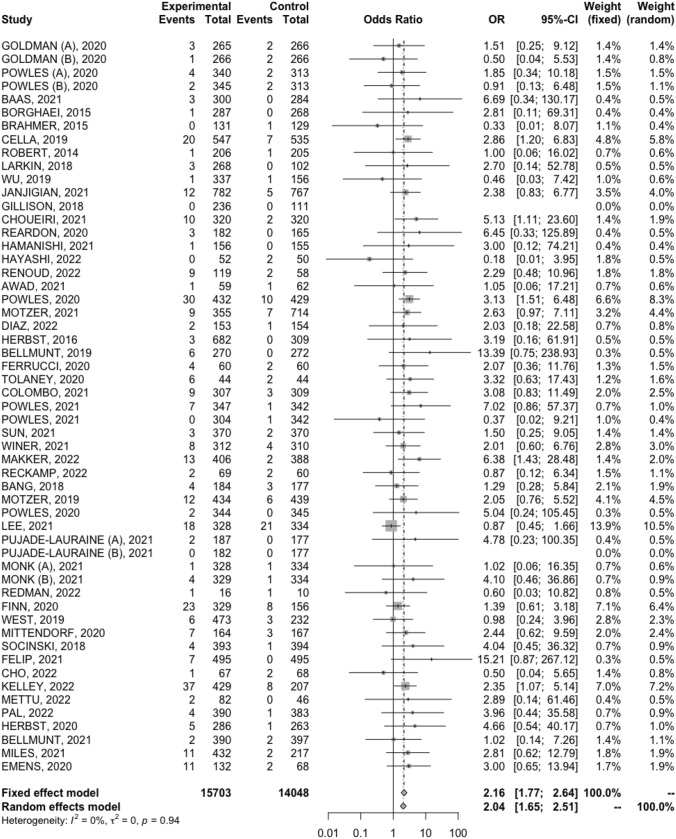
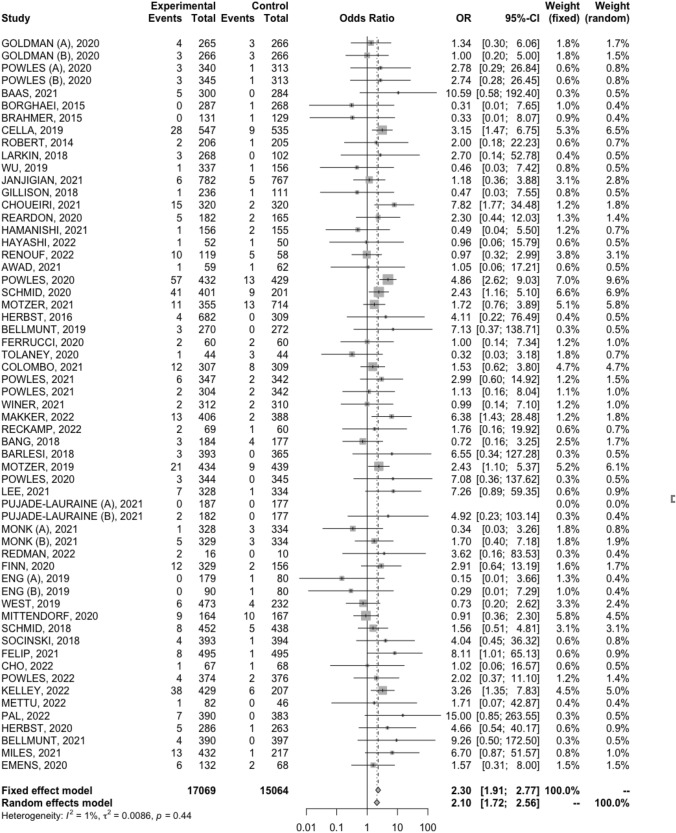
The pooled RRs for grade 3–4 AST and ALT increase were 2.16 (95% CI 1.77–2.64) (Fig. 1) and 2.3 (95% CI 1.91–2.77) (Fig. 2) for patients treated with ICIs monotherapy and immune-based combinations compared to control arm, respectively. A fixed effect model was used since the analyses presented low heterogeneity.
Fig. 1.
Forest plot of comparison between ICIs monotherapy and immune-based combinations versus control arm in cancer patients; the outcome was the relative risk (RR) of grade 3–4 AST increase
Fig. 2.
Forest plot of comparison between ICIs monotherapy and immune-based combinations versus control arm in cancer patients; the outcome was the relative risk (RR) grade 3–4 ALT increase
Discussion
The impact of ICIs monotherapy and immune-based combinations has represented an unprecedented step forward in the systemic treatment for cancer patients, with these agents which have been associated with robust, and even long-lasting responses [82–84]. However, irAEs may represent an issue in this setting, and few data are available in terms of risk and incidence of hepatotoxicity, including increased low-grade and high-grade AST and ALT serum levels [85, 86]. To the best of the authors’ knowledge, our study represents the most comprehensive and up-to-date meta-analysis in the literature to systematically assess the risk of all-grade and grade 3–4 hypertransaminasemia in cancer patients receiving ICIs monotherapy and immune-based combinations. In MOUSEION-05, more than 30.000 patients from 59 clinical trials were included in the analysis. Higher risk of all-grade and grade 3–4 hypertransaminasemia was reported in cancer patients treated with immunotherapy compared with control treatments. Of note, the highest RR was observed for grade 3–4 AST and ALT increase–2.16 (95% CI 1.77–2.64) and 2.3 (95% CI 1.91–2.77), respectively.
Among irAEs, liver toxicity is frequently underestimated due to several reasons, including its ambiguous clinical presentation and its lower incidence compared with other common adverse events [87]. In fact, all-grade and grade 3–4 hypertransaminasemia are commonly unnoticed since these events may be totally asymptomatic or paucisymptomatic. Given the increased incidence of these toxicities, monitoring liver function should be recommended in cancer patients treated with ICIs monotherapy or immune-based combination, and in case of underlying liver disease, a careful risk–benefit assessment appears as a mandatory need. In addition, clinicians are called to suspect and to be aware of these events associated with immunotherapy, and liver function test, physical examination, clinical judgment, and medical history—before the start as well as during immune-based combinations—are fundamental tools in cancer immunotherapy. ICIs monotherapy and immune-based combinations are now the standard for the treatment of several tumor types, as recommended by several international guidelines following the results of landmark clinical trials in this setting [88–92]. However, these treatments have not yet been approved in several countries or have been approved in the last few months, and thus, clinicians have still limited experience of immune-based combinations in everyday clinical practice. Thus, clinical experience plays and will play a fundamental role in the balance between antitumor activity, safety, and quality of life. At the same time, the timing itself of these irAEs is important to determine whether these toxicities are due to ICIs or other anticancer drugs in patients treated with combination strategies, something that changes the management itself of toxicities.
Some strengths and limitations of our meta-analysis should be highlighted. Among the strengths of this study, our analysis included 59 phase II and III RCTs by using the most updated data in terms of all-grade and grade 3–4 hypertransaminasemia. In addition, we included an overall large number of cancer patients. However, some limitations should also be underlined. First, the current meta-analysis was based on pooled data, and thus, the presence of single-patient variables was not included. Secondly, although the random-effects model was performed to reduce heterogeneities across studies, the analysis regarding all-grade AST and ALT increase presented substantial heterogeneity, and thus, our findings should be interpreted cautiously. Thirdly, the trials included in the meta-analysis evaluated widely different ICIs monotherapy and immune-based combinations. All these anticancer agents—ranging from systemic chemotherapy to tyrosine kinase inhibitors and other antiangiogenic drugs—present different and not superimposable safety profiles, and thus, this element could have produced some bias affecting our results. Moreover, a possible overlap in side effects between different agents should be considered, something that could have introduced some bias. For example, it is not possible to clarify with absolute certainty if a specific event is related to immunotherapy or other anticancer drugs included in immune-based combinations as well as other concomitant medications and dietary and lifestyle factors. Similarly, the data were extracted from registration trials, where the time of the onset of the event was not reported. In addition, the presence of selection bias cannot be excluded, since all cancer patients were selected subjects enrolled into high-quality trials conducted at academic centers and with good performance status. Publication bias due to the higher publishing possibility of studies with positive results could not be excluded. Lastly, our study was not a network meta-analysis, and thus, it was not possible to determine which combination may be more hepatotoxic than the other.
However, despite the limitations affecting the current analysis, we think that this piece of evidence emphasizes both the importance of a correct patient's stratification due to any underlying liver impairment, as well as the need to carefully supervise regular blood tests and to better customize therapeutic decisions. Beyond the efficacy of these novel combination strategies, clinicians should pay attention to these frequently underestimated adverse events.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
None.
Author contributions
A.R. wrote the main manuscript text and performed the statistical analysis. A.R. prepared figures 1-5 and table 1. V.M., V.T., E.T., A.M., and M.R. contributed to data acquisition. V.M., R.D.L., M.S., and F.M. contributed to the conception, design, and manuscript revision. All authors approved the final version of the manuscript.
Declarations
Conflict of interest
The author has no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties. No writing assistance was utilized in the production of this manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Matteo Santoni and Francesco Massari equally contributing to this work.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Zhang Y, Zhang Z. The history and advances in cancer immunotherapy: understanding the characteristics of tumor-infiltrating immune cells and their therapeutic implications. Cell Mol Immunol. 2020;17(8):807–821. doi: 10.1038/s41423-020-0488-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xie J, Fu L, Jin L. Immunotherapy of gastric cancer: past, future perspective and challenges. Pathol Res Pract. 2021;218:153322. doi: 10.1016/j.prp.2020.153322. [DOI] [PubMed] [Google Scholar]
- 4.Mollica V, Santoni M, Matrana MR, Basso U, De Giorgi U, Rizzo A, Maruzzo M, Marchetti A, Rosellini M, Bleve S, Maslov D, Tawagi K, Philon E, Blake Z, Massari F. Concomitant proton pump inhibitors and outcome of patients treated with nivolumab alone or plus ipilimumab for advanced renal cell carcinoma. Target Oncol. 2022;17(1):61–68. doi: 10.1007/s11523-021-00861-y. [DOI] [PubMed] [Google Scholar]
- 5.Rosellini M, Marchetti A, Mollica V, Rizzo A, Santoni M, Massari F. Prognostic and predictive biomarkers for immunotherapy in advanced renal cell carcinoma. Nat Rev Urol. 2022 doi: 10.1038/s41585-022-00676-0. [DOI] [PubMed] [Google Scholar]
- 6.Yang Y. Cancer immunotherapy: harnessing the immune system to battle cancer. J Clin Invest. 2015;125(9):3335–3337. doi: 10.1172/JCI83871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Riley RS, June CH, Langer R, Mitchell MJ. Delivery technologies for cancer immunotherapy. Nat Rev Drug Discov. 2019;18(3):175–196. doi: 10.1038/s41573-018-0006-z.PMID:30622344;PMCID:PMC6410566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Viscardi G, Tralongo AC, Massari F, Lambertini M, Mollica V, Rizzo A, Comito F, Di Liello R, Alfieri S, Imbimbo M, Della Corte CM, Morgillo F, Simeon V, Lo Russo G, Proto C, Prelaj A, De Toma A, Galli G, Signorelli D, Ciardiello F, Remon J, Chaput N, Besse B, de Braud F, Garassino MC, Torri V, Cinquini M, Ferrara R. Comparative assessment of early mortality risk upon immune checkpoint inhibitors alone or in combination with other agents across solid malignancies: a systematic review and meta-analysis. Eur J Cancer. 2022;177:175–185. doi: 10.1016/j.ejca.2022.09.031. [DOI] [PubMed] [Google Scholar]
- 9.Sangro B, Sarobe P, Hervás-Stubbs S, Melero I. Advances in immunotherapy for hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol. 2021;18(8):525–543. doi: 10.1038/s41575-021-00438-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Llovet JM, Castet F, Heikenwalder M, Maini MK, Mazzaferro V, Pinato DJ, Pikarsky E, Zhu AX, Finn RS. Immunotherapies for hepatocellular carcinoma. Nat Rev Clin Oncol. 2022;19(3):151–172. doi: 10.1038/s41571-021-00573-2. [DOI] [PubMed] [Google Scholar]
- 11.Cuevas LM, Daud AI. Immunotherapy for melanoma. Semin Cutan Med Surg. 2018;37(2):127–131. doi: 10.12788/j.sder.2018.028. [DOI] [PubMed] [Google Scholar]
- 12.Ruiz-Cordero R, Devine WP. Targeted therapy and checkpoint immunotherapy in lung cancer. Surg Pathol Clin. 2020;13(1):17–33. doi: 10.1016/j.path.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Reck M, Remon J, Hellmann MD. First-line immunotherapy for non-small-cell lung cancer. J Clin Oncol. 2022;40(6):586–597. doi: 10.1200/JCO.21.01497. [DOI] [PubMed] [Google Scholar]
- 14.Santoni M, Rizzo A, Mollica V, Matrana MR, Rosellini M, Faloppi L, Marchetti A, Battelli N, Massari F. The impact of gender on the efficacy of immune checkpoint inhibitors in cancer patients: the MOUSEION-01 study. Crit Rev Oncol Hematol. 2022;170:103596. doi: 10.1016/j.critrevonc.2022.103596. [DOI] [PubMed] [Google Scholar]
- 15.Rizzo A, Santoni M, Mollica V, Logullo F, Rosellini M, Marchetti A, Faloppi L, Battelli N, Massari F. Peripheral neuropathy and headache in cancer patients treated with immunotherapy and immuno-oncology combinations: the MOUSEION-02 study. Expert Opin Drug Metab Toxicol. 2021;17(12):1455–1466. doi: 10.1080/17425255.2021.2029405. [DOI] [PubMed] [Google Scholar]
- 16.Marrone KA, Ying W, Naidoo J. Immune-related adverse events from immune checkpoint inhibitors. Clin Pharmacol Ther. 2016;100(3):242–251. doi: 10.1002/cpt.394. [DOI] [PubMed] [Google Scholar]
- 17.Suzman DL, Pelosof L, Rosenberg A, Avigan MI. Hepatotoxicity of immune checkpoint inhibitors: an evolving picture of risk associated with a vital class of immunotherapy agents. Liver Int. 2018;38(6):976–987. doi: 10.1111/liv.13746. [DOI] [PubMed] [Google Scholar]
- 18.Wang W, Lie P, Guo M, He J. Risk of hepatotoxicity in cancer patients treated with immune checkpoint inhibitors: a systematic review and meta-analysis of published data. Int J Cancer. 2017;141(5):1018–1028. doi: 10.1002/ijc.30678. [DOI] [PubMed] [Google Scholar]
- 19.Puzanov I, Diab A, Abdallah K, et al. Managing toxicities associated with immune checkpoint inhibitors: consensus recommendations from the society for immunotherapy of cancer (SITC) toxicity management working group. J Immunother Cancer. 2017;5:95. doi: 10.1186/s40425-017-0300-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Champiat S, Lambotte O, Barreau E, et al. Management of immune checkpoint blockade dysimmune toxicities: a collaborative position paper. Ann Oncol. 2016;27(4):559–574. doi: 10.1093/annonc/mdv623. [DOI] [PubMed] [Google Scholar]
- 21.Peeraphatdit TB, Wang J, Odenwald MA, Hu S, Hart J, Charlton MR. Hepatotoxicity from immune checkpoint inhibitors: a systematic review and management recommendation. Hepatology. 2020;72(1):315–329. doi: 10.1002/hep.31227. [DOI] [PubMed] [Google Scholar]
- 22.Tian Y, Abu-Sbeih H, Wang Y. Immune checkpoint inhibitors-induced hepatitis. Adv Exp Med Biol. 2020;995:159–164. doi: 10.1007/978-3-030-02505-2_8. [DOI] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higgins JPT, Thomas J, Chandler J, et al. Cochrane hand-book for systematic reviews of interventions. 2. Chichester (UK): John Wiley and Sons; 2019. [Google Scholar]
- 25.Powles T, van der Heijden MS, Castellano D, Galsky MD, Loriot Y, Petrylak DP, Ogawa O, Park SH, Lee JL, De Giorgi U, Bögemann M, Bamias A, Eigl BJ, Gurney H, Mukherjee SD, Fradet Y, Skoneczna I, Tsiatas M, Novikov A, Suárez C, Fay AP, Duran I, Necchi A, Wildsmith S, He P, Angra N, Gupta AK, Levin W, Bellmunt J (2020) DANUBE study investigators. Durvalumab alone and durvalumab plus tremelimumab versus chemotherapy in previously untreated patients with unresectable, locally advanced or metastatic urothelial carcinoma (DANUBE): a randomised, open-label, multicentre, phase 3 trial. Lancet Oncol 21(12):1574–1588 10.1016/S1470-2045(20)30541-6 [DOI] [PubMed]
- 26.Goldman JW, Dvorkin M, Chen Y, Reinmuth N, Hotta K, Trukhin D, Statsenko G, Hochmair MJ, Özgüroğlu M, Ji JH, Garassino MC, Voitko O, Poltoratskiy A, Ponce S, Verderame F, Havel L, Bondarenko I, Każarnowicz A, Losonczy G, Conev NV, Armstrong J, Byrne N, Thiyagarajah P, Jiang H, Paz-Ares L. CASPIAN investigators. durvalumab, with or without tremelimumab, plus platinum-etoposide versus platinum-etoposide alone in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): updated results from a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2021;22(1):51–65. doi: 10.1016/S1470-2045(20)30539-8. [DOI] [PubMed] [Google Scholar]
- 27.Renouf DJ, Loree JM, Knox JJ, Topham JT, Kavan P, Jonker D, Welch S, Couture F, Lemay F, Tehfe M, Harb M, Aucoin N, Ko YJ, Tang PA, Ramjeesingh R, Meyers BM, Kim CA, Du P, Jia S, Schaeffer DF, Gill S, Tu D, O'Callaghan CJ. The CCTG PA.7 phase II trial of gemcitabine and nab-paclitaxel with or without durvalumab and tremelimumab as initial therapy in metastatic pancreatic ductal adenocarcinoma. Nat Commun 26. 2022;13(1):5020. doi: 10.1038/s41467-022-32591-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robert C, Long GV, Brady B, Dutriaux C, Maio M, Mortier L, Hassel JC, Rutkowski P, McNeil C, Kalinka-Warzocha E, Savage KJ, Hernberg MM, Lebbé C, Charles J, Mihalcioiu C, Chiarion-Sileni V, Mauch C, Cognetti F, Arance A, Schmidt H, Schadendorf D, Gogas H, Lundgren-Eriksson L, Horak C, Sharkey B, Waxman IM, Atkinson V, Ascierto PA. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med. 2015;372(4):320–330. doi: 10.1056/NEJMoa1412082. [DOI] [PubMed] [Google Scholar]
- 29.Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, Chow LQ, Vokes EE, Felip E, Holgado E, Barlesi F, Kohlhäufl M, Arrieta O, Burgio MA, Fayette J, Lena H, Poddubskaya E, Gerber DE, Gettinger SN, Rudin CM, Rizvi N, Crinò L, Blumenschein GR, Jr, Antonia SJ, Dorange C, Harbison CT, Graf Finckenstein F, Brahmer JR. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373(17):1627–1639. doi: 10.1056/NEJMoa1507643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brahmer J, Reckamp KL, Baas P, Crinò L, Eberhardt WE, Poddubskaya E, Antonia S, Pluzanski A, Vokes EE, Holgado E, Waterhouse D, Ready N, Gainor J, Arén Frontera O, Havel L, Steins M, Garassino MC, Aerts JG, Domine M, Paz-Ares L, Reck M, Baudelet C, Harbison CT, Lestini B, Spigel DR. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373(2):123–135. doi: 10.1056/NEJMoa1504627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Larkin J, Minor D, D'Angelo S, Neyns B, Smylie M, Miller WH, Jr, Gutzmer R, Linette G, Chmielowski B, Lao CD, Lorigan P, Grossmann K, Hassel JC, Sznol M, Daud A, Sosman J, Khushalani N, Schadendorf D, Hoeller C, Walker D, Kong G, Horak C, Weber J. Overall survival in patients with advanced melanoma who received nivolumab versus investigator's choice chemotherapy in checkmate 037: a randomized, controlled, open-label phase iii trial. J Clin Oncol. 2018;36(4):383–390. doi: 10.1200/JCO.2016.71.8023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gillison ML, Blumenschein G, Jr, Fayette J, Guigay J, Colevas AD, Licitra L, Harrington KJ, Kasper S, Vokes EE, Even C, Worden F, Saba NF, Iglesias Docampo LC, Haddad R, Rordorf T, Kiyota N, Tahara M, Monga M, Lynch M, Li L, Ferris RL. CheckMate 141: 1-year update and subgroup analysis of nivolumab as first-line therapy in patients with recurrent/metastatic head and neck cancer. Oncologist. 2018;23(9):1079–1082. doi: 10.1634/theoncologist.2017-0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cella D, Grünwald V, Escudier B, Hammers HJ, George S, Nathan P, Grimm MO, Rini BI, Doan J, Ivanescu C, Paty J, Mekan S, Motzer RJ. Patient-reported outcomes of patients with advanced renal cell carcinoma treated with nivolumab plus ipilimumab versus sunitinib (CheckMate 214): a randomised, phase 3 trial. Lancet Oncol. 2019;20(2):297–310. doi: 10.1016/S1470-2045(18)30778-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wu YL, Lu S, Cheng Y, Zhou C, Wang J, Mok T, Zhang L, Tu HY, Wu L, Feng J, Zhang Y, Luft AV, Zhou J, Ma Z, Lu Y, Hu C, Shi Y, Baudelet C, Cai J, Chang J. Nivolumab versus docetaxel in a predominantly chinese patient population with previously treated advanced nsclc: checkmate 078 randomized phase iii clinical trial. J Thorac Oncol. 2019;14(5):867–875. doi: 10.1016/j.jtho.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 35.Reardon DA, Brandes AA, Omuro A, Mulholland P, Lim M, Wick A, Baehring J, Ahluwalia MS, Roth P, Bähr O, Phuphanich S, Sepulveda JM, De Souza P, Sahebjam S, Carleton M, Tatsuoka K, Taitt C, Zwirtes R, Sampson J, Weller M. Effect of nivolumab vs bevacizumab in patients with recurrent glioblastoma: the checkmate 143 phase 3 randomized clinical trial. JAMA Oncol. 2020;6(7):1003–1010. doi: 10.1001/jamaoncol.2020.1024.PMID:32437507;PMCID:PMC7243167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Janjigian YY, Shitara K, Moehler M, Garrido M, Salman P, Shen L, Wyrwicz L, Yamaguchi K, Skoczylas T, Campos Bragagnoli A, Liu T, Schenker M, Yanez P, Tehfe M, Kowalyszyn R, Karamouzis MV, Bruges R, Zander T, Pazo-Cid R, Hitre E, Feeney K, Cleary JM, Poulart V, Cullen D, Lei M, Xiao H, Kondo K, Li M, Ajani JA. First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): a randomised, open-label, phase 3 trial. Lancet. 2021;398(10294):27–40. doi: 10.1016/S0140-6736(21)00797-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Choueiri TK, Powles T, Burotto M, Escudier B, Bourlon MT, Zurawski B, Oyervides Juárez VM, Hsieh JJ, Basso U, Shah AY, Suárez C, Hamzaj A, Goh JC, Barrios C, Richardet M, Porta C, Kowalyszyn R, Feregrino JP, Żołnierek J, Pook D, Kessler ER, Tomita Y, Mizuno R, Bedke J, Zhang J, Maurer MA, Simsek B, Ejzykowicz F, Schwab GM, Apolo AB, Motzer RJ. CheckMate 9ER investigators nivolumab plus cabozantinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2021;384(9):829–841. doi: 10.1056/NEJMoa2026982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hamanishi J, Takeshima N, Katsumata N, Ushijima K, Kimura T, Takeuchi S, Matsumoto K, Ito K, Mandai M, Nakai H, Sakuragi N, Watari H, Takahashi N, Kato H, Hasegawa K, Yonemori K, Mizuno M, Takehara K, Niikura H, Sawasaki T, Nakao S, Saito T, Enomoto T, Nagase S, Suzuki N, Matsumoto T, Kondo E, Sonoda K, Aihara S, Aoki Y, Okamoto A, Takano H, Kobayashi H, Kato H, Terai Y, Takazawa A, Takahashi Y, Namba Y, Aoki D, Fujiwara K, Sugiyama T, Konishi I. Nivolumab versus gemcitabine or pegylated liposomal doxorubicin for patients with platinum-resistant ovarian cancer: open-label, randomized trial in japan (NINJA) J Clin Oncol. 2021;39(33):3671–3681. doi: 10.1200/JCO.21.00334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hayashi H, Sugawara S, Fukuda Y, Fujimoto D, Miura S, Ota K, Ozawa Y, Hara S, Tanizaki J, Azuma K, Omori S, Tachihara M, Nishino K, Bessho A, Chiba Y, Haratani K, Sakai K, Nishio K, Yamamoto N, Nakagawa K. A randomized phase II study comparing nivolumab with carboplatin-pemetrexed for EGFR-mutated NSCLC with resistance to EGFR tyrosine kinase inhibitors (WJOG8515L) Clin Cancer Res. 2022;28(5):893–902. doi: 10.1158/1078-0432.CCR-21-3194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schmid P, Adams S, Rugo HS, Schneeweiss A, Barrios CH, Iwata H, Diéras V, Hegg R, Im SA, Shaw Wright G, Henschel V, Molinero L, Chui SY, Funke R, Husain A, Winer EP, Loi S, Emens LA. IMpassion130 trial investigators atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med. 2018;379(22):2108–2121. doi: 10.1056/NEJMoa1809615. [DOI] [PubMed] [Google Scholar]
- 41.Socinski MA, Jotte RM, Cappuzzo F, Orlandi F, Stroyakovskiy D, Nogami N, Rodríguez-Abreu D, Moro-Sibilot D, Thomas CA, Barlesi F, Finley G, Kelsch C, Lee A, Coleman S, Deng Y, Shen Y, Kowanetz M, Lopez-Chavez A, Sandler A, Reck M. IMpower150 study group atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 2018;378(24):2288–2301. doi: 10.1056/NEJMoa1716948. [DOI] [PubMed] [Google Scholar]
- 42.Powles T, Durán I, van der Heijden MS, Loriot Y, Vogelzang NJ, De Giorgi U, Oudard S, Retz MM, Castellano D, Bamias A, Fléchon A, Gravis G, Hussain S, Takano T, Leng N, Kadel EE, 3rd, Banchereau R, Hegde PS, Mariathasan S, Cui N, Shen X, Derleth CL, Green MC, Ravaud A. Atezolizumab versus chemotherapy in patients with platinum-treated locally advanced or metastatic urothelial carcinoma (IMvigor211): a multicentre, open-label, phase 3 randomised controlled trial. Lancet. 2018;391(10122):748–757. doi: 10.1016/S0140-6736(17)33297-X. [DOI] [PubMed] [Google Scholar]
- 43.Eng C, Kim TW, Bendell J, Argilés G, Tebbutt NC, Di Bartolomeo M, Falcone A, Fakih M, Kozloff M, Segal NH, Sobrero A, Yan Y, Chang I, Uyei A, Roberts L, Ciardiello F. IMblaze370 investigators atezolizumab with or without cobimetinib versus regorafenib in previously treated metastatic colorectal cancer (IMblaze370): a multicentre, open-label, phase 3, randomised, controlled trial. Lancet Oncol. 2019;20(6):849–861. doi: 10.1016/S1470-2045(19)30027-0. [DOI] [PubMed] [Google Scholar]
- 44.West H, McCleod M, Hussein M, Morabito A, Rittmeyer A, Conter HJ, Kopp HG, Daniel D, McCune S, Mekhail T, Zer A, Reinmuth N, Sadiq A, Sandler A, Lin W, Ochi Lohmann T, Archer V, Wang L, Kowanetz M, Cappuzzo F. Atezolizumab in combination with carboplatin plus nab-paclitaxel chemotherapy compared with chemotherapy alone as first-line treatment for metastatic non-squamous non-small-cell lung cancer (IMpower130): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20(7):924–937. doi: 10.1016/S1470-2045(19)30167-6. [DOI] [PubMed] [Google Scholar]
- 45.Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, Kudo M, Breder V, Merle P, Kaseb AO, Li D, Verret W, Xu DZ, Hernandez S, Liu J, Huang C, Mulla S, Wang Y, Lim HY, Zhu AX, Cheng AL. IMbrave150 investigators atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 2020;382(20):1894–1905. doi: 10.1056/NEJMoa1915745. [DOI] [PubMed] [Google Scholar]
- 46.Mittendorf EA, Zhang H, Barrios CH, Saji S, Jung KH, Hegg R, Koehler A, Sohn J, Iwata H, Telli ML, Ferrario C, Punie K, Penault-Llorca F, Patel S, Duc AN, Liste-Hermoso M, Maiya V, Molinero L, Chui SY, Harbeck N. Neoadjuvant atezolizumab in combination with sequential nab-paclitaxel and anthracycline-based chemotherapy versus placebo and chemotherapy in patients with early-stage triple-negative breast cancer (IMpassion031): a randomised, double-blind, phase 3 trial. Lancet. 2020;396(10257):1090–1100. doi: 10.1016/S0140-6736(20)31953-X. [DOI] [PubMed] [Google Scholar]
- 47.Herbst RS, Giaccone G, de Marinis F, Reinmuth N, Vergnenegre A, Barrios CH, Morise M, Felip E, Andric Z, Geater S, Özgüroğlu M, Zou W, Sandler A, Enquist I, Komatsubara K, Deng Y, Kuriki H, Wen X, McCleland M, Mocci S, Jassem J, Spigel DR. Atezolizumab for first-line treatment of PD-L1-selected patients with NSCLC. N Engl J Med. 2020;383(14):1328–1339. doi: 10.1056/NEJMoa1917346. [DOI] [PubMed] [Google Scholar]
- 48.Felip E, Altorki N, Zhou C, Csőszi T, Vynnychenko I, Goloborodko O, Luft A, Akopov A, Martinez-Marti A, Kenmotsu H, Chen YM, Chella A, Sugawara S, Voong D, Wu F, Yi J, Deng Y, McCleland M, Bennett E, Gitlitz B, Wakelee H. IMpower010 investigators adjuvant atezolizumab after adjuvant chemotherapy in resected stage IB-IIIA non-small-cell lung cancer (IMpower010): a randomised, multicentre, open-label, phase 3 trial. Lancet. 2021;398(10308):1344–1357. doi: 10.1016/S0140-6736(21)02098-5. [DOI] [PubMed] [Google Scholar]
- 49.Bellmunt J, Hussain M, Gschwend JE, Albers P, Oudard S, Castellano D, Daneshmand S, Nishiyama H, Majchrowicz M, Degaonkar V, Shi Y, Mariathasan S, Grivas P, Drakaki A, O'Donnell PH, Rosenberg JE, Geynisman DM, Petrylak DP, Hoffman-Censits J, Bedke J, Kalebasty AR, Zakharia Y, van der Heijden MS, Sternberg CN, Davarpanah NN, Powles T. IMvigor010 study group adjuvant atezolizumab versus observation in muscle-invasive urothelial carcinoma (IMvigor010): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2021;22(4):525–537. doi: 10.1016/S1470-2045(21)00004-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Miles D, Gligorov J, André F, Cameron D, Schneeweiss A, Barrios C, Xu B, Wardley A, Kaen D, Andrade L, Semiglazov V, Reinisch M, Patel S, Patre M, Morales L, Patel SL, Kaul M, Barata T, O'Shaughnessy J. IMpassion131 investigators primary results from IMpassion131, a double-blind, placebo-controlled, randomised phase III trial of first-line paclitaxel with or without atezolizumab for unresectable locally advanced/metastatic triple-negative breast cancer. Ann Oncol. 2021;32(8):994–1004. doi: 10.1016/j.annonc.2021.05.801. [DOI] [PubMed] [Google Scholar]
- 51.Cho BC, Abreu DR, Hussein M, Cobo M, Patel AJ, Secen N, Lee KH, Massuti B, Hiret S, Yang JCH, Barlesi F, Lee DH, Ares LP, Hsieh RW, Patil NS, Twomey P, Yang X, Meng R, Johnson ML. Tiragolumab plus atezolizumab versus placebo plus atezolizumab as a first-line treatment for PD-L1-selected non-small-cell lung cancer (CITYSCAPE): primary and follow-up analyses of a randomised, double-blind, phase 2 study. Lancet Oncol. 2022;23(6):781–792. doi: 10.1016/S1470-2045(22)00226-1. [DOI] [PubMed] [Google Scholar]
- 52.Kelley RK, Rimassa L, Cheng AL, Kaseb A, Qin S, Zhu AX, Chan SL, Melkadze T, Sukeepaisarnjaroen W, Breder V, Verset G, Gane E, Borbath I, Rangel JDG, Ryoo BY, Makharadze T, Merle P, Benzaghou F, Banerjee K, Hazra S, Fawcett J, Yau T. Cabozantinib plus atezolizumab versus sorafenib for advanced hepatocellular carcinoma (COSMIC-312): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2022;23(8):995–1008. doi: 10.1016/S1470-2045(22)00326-6. [DOI] [PubMed] [Google Scholar]
- 53.Mettu NB, Ou FS, Zemla TJ, Halfdanarson TR, Lenz HJ, Breakstone RA, Boland PM, Crysler OV, Wu C, Nixon AB, Bolch E, Niedzwiecki D, Elsing A, Hurwitz HI, Fakih MG, Bekaii-Saab T. Assessment of capecitabine and bevacizumab with or without atezolizumab for the treatment of refractory metastatic colorectal cancer: a randomized clinical trial. JAMA Netw Open. 2022;5(2):e2149040. doi: 10.1001/jamanetworkopen.2021.49040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huober J, Barrios CH, Niikura N, Jarząb M, Chang YC, Huggins-Puhalla SL, Pedrini J, Zhukova L, Graupner V, Eiger D, Henschel V, Gochitashvili N, Lambertini C, Restuccia E, Zhang H. IMpassion050 trial investigators. atezolizumab with neoadjuvant anti-human epidermal growth factor receptor 2 therapy and chemotherapy in human epidermal growth factor receptor 2-positive early breast cancer: primary results of the randomized phase iii impassion050 trial. J Clin Oncol. 2022;40(25):2946–2956. doi: 10.1200/JCO.21.02772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pal SK, Uzzo R, Karam JA, Master VA, Donskov F, Suarez C, Albiges L, Rini B, Tomita Y, Kann AG, Procopio G, Massari F, Zibelman M, Antonyan I, Huseni M, Basu D, Ci B, Leung W, Khan O, Dubey S, Bex A. Adjuvant atezolizumab versus placebo for patients with renal cell carcinoma at increased risk of recurrence following resection (IMmotion010): a multicentre, randomised, double-blind, phase 3 trial. Lancet. 2022;400(10358):1103–1116. doi: 10.1016/S0140-6736(22)01658-0. [DOI] [PubMed] [Google Scholar]
- 56.Bang YJ, Ruiz EY, Van Cutsem E, Lee KW, Wyrwicz L, Schenker M, Alsina M, Ryu MH, Chung HC, Evesque L, Al-Batran SE, Park SH, Lichinitser M, Boku N, Moehler MH, Hong J, Xiong H, Hallwachs R, Conti I, Taieb J. Phase III, randomised trial of avelumab versus physician's choice of chemotherapy as third-line treatment of patients with advanced gastric or gastro-oesophageal junction cancer: primary analysis of JAVELIN Gastric 300. Ann Oncol. 2018;29(10):2052–2060. doi: 10.1093/annonc/mdy264.PMID:30052729;PMCID:PMC6225815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Barlesi F, Vansteenkiste J, Spigel D, Ishii H, Garassino M, de Marinis F, Özgüroğlu M, Szczesna A, Polychronis A, Uslu R, Krzakowski M, Lee JS, Calabrò L, Arén Frontera O, Ellers-Lenz B, Bajars M, Ruisi M, Park K. Avelumab versus docetaxel in patients with platinum-treated advanced non-small-cell lung cancer (JAVELIN Lung 200): an open-label, randomised, phase 3 study. Lancet Oncol. 2018;19(11):1468–1479. doi: 10.1016/S1470-2045(18)30673-9. [DOI] [PubMed] [Google Scholar]
- 58.Motzer RJ, Penkov K, Haanen J, Rini B, Albiges L, Campbell MT, Venugopal B, Kollmannsberger C, Negrier S, Uemura M, Lee JL, Vasiliev A, Miller WH, Jr, Gurney H, Schmidinger M, Larkin J, Atkins MB, Bedke J, Alekseev B, Wang J, Mariani M, Robbins PB, Chudnovsky A, Fowst C, Hariharan S, Huang B, di Pietro A, Choueiri TK. Avelumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2019;380(12):1103–1115. doi: 10.1056/NEJMoa1816047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Powles T, Park SH, Voog E, Caserta C, Valderrama BP, Gurney H, Kalofonos H, Radulović S, Demey W, Ullén A, Loriot Y, Sridhar SS, Tsuchiya N, Kopyltsov E, Sternberg CN, Bellmunt J, Aragon-Ching JB, Petrylak DP, Laliberte R, Wang J, Huang B, Davis C, Fowst C, Costa N, Blake-Haskins JA, di Pietro A, Grivas P. Avelumab maintenance therapy for advanced or metastatic urothelial carcinoma. N Engl J Med. 2020;383(13):1218–1230. doi: 10.1056/NEJMoa2002788. [DOI] [PubMed] [Google Scholar]
- 60.Moehler M, Dvorkin M, Boku N, Özgüroğlu M, Ryu MH, Muntean AS, Lonardi S, Nechaeva M, Bragagnoli AC, Coşkun HS, Cubillo Gracian A, Takano T, Wong R, Safran H, Vaccaro GM, Wainberg ZA, Silver MR, Xiong H, Hong J, Taieb J, Bang YJ. Phase III trial of avelumab maintenance after first-line induction chemotherapy versus continuation of chemotherapy in patients with gastric cancers: results from JAVELIN gastric 100. J Clin Oncol. 2021;39(9):966–977. doi: 10.1200/JCO.20.00892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lee NY, Ferris RL, Psyrri A, Haddad RI, Tahara M, Bourhis J, Harrington K, Chang PM, Lin JC, Razaq MA, Teixeira MM, Lövey J, Chamois J, Rueda A, Hu C, Dunn LA, Dvorkin MV, De Beukelaer S, Pavlov D, Thurm H, Cohen E. Avelumab plus standard-of-care chemoradiotherapy versus chemoradiotherapy alone in patients with locally advanced squamous cell carcinoma of the head and neck: a randomised, double-blind, placebo-controlled, multicentre, phase 3 trial. Lancet Oncol. 2021;22(4):450–462. doi: 10.1016/S1470-2045(20)30737-3. [DOI] [PubMed] [Google Scholar]
- 62.Pujade-Lauraine E, Fujiwara K, Ledermann JA, Oza AM, Kristeleit R, Ray-Coquard IL, Richardson GE, Sessa C, Yonemori K, Banerjee S, Leary A, Tinker AV, Jung KH, Madry R, Park SY, Anderson CK, Zohren F, Stewart RA, Wei C, Dychter SS, Monk BJ. Avelumab alone or in combination with chemotherapy versus chemotherapy alone in platinum-resistant or platinum-refractory ovarian cancer (JAVELIN Ovarian 200): an open-label, three-arm, randomised, phase 3 study. Lancet Oncol. 2021;22(7):1034–1046. doi: 10.1016/S1470-2045(21)00216-3. [DOI] [PubMed] [Google Scholar]
- 63.Monk BJ, Colombo N, Oza AM, Fujiwara K, Birrer MJ, Randall L, Poddubskaya EV, Scambia G, Shparyk YV, Lim MC, Bhoola SM, Sohn J, Yonemori K, Stewart RA, Zhang X, Perkins Smith J, Linn C, Ledermann JA. Chemotherapy with or without avelumab followed by avelumab maintenance versus chemotherapy alone in patients with previously untreated epithelial ovarian cancer (JAVELIN Ovarian 100): an open-label, randomised, phase 3 trial. Lancet Oncol. 2021;22(9):1275–1289. doi: 10.1016/S1470-2045(21)00342-9. [DOI] [PubMed] [Google Scholar]
- 64.Redman JM, Tsai YT, Weinberg BA, Donahue RN, Gandhy S, Gatti-Mays ME, Abdul Sater H, Bilusic M, Cordes LM, Steinberg SM, Marte JL, Jochems C, Kim SS, Marshall JL, McMahon S, Redmond E, Schlom J, Gulley JL, Strauss J. A randomized phase II Trial of mFOLFOX6 + bevacizumab alone or with adcea vaccine + avelumab immunotherapy for untreated metastatic colorectal cancer. Oncologist. 2022;27(3):198–209. doi: 10.1093/oncolo/oyab046.PMID:35274710;PMCID:PMC8914498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Herbst RS, Baas P, Kim DW, Felip E, Pérez-Gracia JL, Han JY, Molina J, Kim JH, Arvis CD, Ahn MJ, Majem M, Fidler MJ, Castro G, Jr, Garrido M, Lubiniecki GM, Shentu Y, Im E, Dolled-Filhart M, Garon EB. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387(10027):1540–1550. doi: 10.1016/S0140-6736(15)01281-7. [DOI] [PubMed] [Google Scholar]
- 66.Mok TSK, Wu YL, Kudaba I, Kowalski DM, Cho BC, Turna HZ, Castro G, Jr, Srimuninnimit V, Laktionov KK, Bondarenko I, Kubota K, Lubiniecki GM, Zhang J, Kush D, Lopes G. KEYNOTE-042 investigators pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet. 2019;393(10183):1819–1830. doi: 10.1016/S0140-6736(18)32409-7. [DOI] [PubMed] [Google Scholar]
- 67.Bellmunt J, de Wit R, Vaughn DJ, Fradet Y, Lee JL, Fong L, Vogelzang NJ, Climent MA, Petrylak DP, Choueiri TK, Necchi A, Gerritsen W, Gurney H, Quinn DI, Culine S, Sternberg CN, Mai Y, Poehlein CH, Perini RF, Bajorin DF. KEYNOTE-045 investigators pembrolizumab as second-line therapy for advanced urothelial carcinoma. N Engl J Med. 2017;376(11):1015–1026. doi: 10.1056/NEJMoa1613683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Powles T, Plimack ER, Soulières D, Waddell T, Stus V, Gafanov R, Nosov D, Pouliot F, Melichar B, Vynnychenko I, Azevedo SJ, Borchiellini D, McDermott RS, Bedke J, Tamada S, Yin L, Chen M, Molife LR, Atkins MB, Rini BI. Pembrolizumab plus axitinib versus sunitinib monotherapy as first-line treatment of advanced renal cell carcinoma (KEYNOTE-426): extended follow-up from a randomised, open-label, phase 3 trial. Lancet Oncol. 2020;21(12):1563–1573. doi: 10.1016/S1470-2045(20)30436-8. [DOI] [PubMed] [Google Scholar]
- 69.Schmid P, Cortes J, Pusztai L, McArthur H, Kümmel S, Bergh J, Denkert C, Park YH, Hui R, Harbeck N, Takahashi M, Foukakis T, Fasching PA, Cardoso F, Untch M, Jia L, Karantza V, Zhao J, Aktan G, Dent R, O'Shaughnessy J. KEYNOTE-522 investigators pembrolizumab for early triple-negative breast cancer. N Engl J Med. 2020;382(9):810–821. doi: 10.1056/NEJMoa1910549. [DOI] [PubMed] [Google Scholar]
- 70.Ferrucci PF, Di Giacomo AM, Del Vecchio M, Atkinson V, Schmidt H, Schachter J, Queirolo P, Long GV, Stephens R, Svane IM, Lotem M, Abu-Amna M, Gasal E, Ghori R, Diede SJ, Croydon ES, Ribas A, Ascierto PA. KEYNOTE-022 international team KEYNOTE-022 part 3: a randomized, double-blind, phase 2 study of pembrolizumab, dabrafenib, and trametinib in BRAF-mutant melanoma. J Immunother Cancer. 2020;8(2):e001806. doi: 10.1136/jitc-2020-001806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tolaney SM, Barroso-Sousa R, Keenan T, Li T, Trippa L, Vaz-Luis I, Wulf G, Spring L, Sinclair NF, Andrews C, Pittenger J, Richardson ET, 3rd, Dillon D, Lin NU, Overmoyer B, Partridge AH, Van Allen E, Mittendorf EA, Winer EP, Krop IE. Effect of eribulin with or without pembrolizumab on progression-free survival for patients with hormone receptor-positive, ERBB2-negative metastatic breast cancer: a randomized clinical trial. JAMA Oncol. 2020;6(10):1598–1605. doi: 10.1001/jamaoncol.2020.3524.PMID:32880602;PMCID:PMC7489368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Motzer R, Alekseev B, Rha SY, Porta C, Eto M, Powles T, Grünwald V, Hutson TE, Kopyltsov E, Méndez-Vidal MJ, Kozlov V, Alyasova A, Hong SH, Kapoor A, Alonso Gordoa T, Merchan JR, Winquist E, Maroto P, Goh JC, Kim M, Gurney H, Patel V, Peer A, Procopio G, Takagi T, Melichar B, Rolland F, De Giorgi U, Wong S, Bedke J, Schmidinger M, Dutcus CE, Smith AD, Dutta L, Mody K, Perini RF, Xing D, Choueiri TK. CLEAR trial investigators lenvatinib plus pembrolizumab or everolimus for advanced renal cell carcinoma. N Engl J Med. 2021;384(14):1289–1300. doi: 10.1056/NEJMoa2035716. [DOI] [PubMed] [Google Scholar]
- 73.Awad MM, Gadgeel SM, Borghaei H, Patnaik A, Yang JC, Powell SF, Gentzler RD, Martins RG, Stevenson JP, Altan M, Jalal SI, Panwalkar A, Gubens M, Sequist LV, Saraf S, Zhao B, Piperdi B, Langer CJ. Long-term overall survival from KEYNOTE-021 cohort g: pemetrexed and carboplatin with or without pembrolizumab as first-line therapy for advanced nonsquamous NSCLC. J Thorac Oncol. 2021;16(1):162–168. doi: 10.1016/j.jtho.2020.09.015. [DOI] [PubMed] [Google Scholar]
- 74.Colombo N, Dubot C, Lorusso D, Caceres MV, Hasegawa K, Shapira-Frommer R, Tewari KS, Salman P, Hoyos Usta E, Yañez E, Gümüş M, Hurtado O, de Mendoza M, Samouëlian V, Castonguay V, Arkhipov A, Toker S, Li K, Keefe SM, Monk BJ. KEYNOTE-826 investigators pembrolizumab for persistent, recurrent, or metastatic cervical cancer. N Engl J Med. 2021;385(20):1856–1867. doi: 10.1056/NEJMoa2112435. [DOI] [PubMed] [Google Scholar]
- 75.Powles T, Csőszi T, Özgüroğlu M, Matsubara N, Géczi L, Cheng SY, Fradet Y, Oudard S, Vulsteke C, Morales Barrera R, Fléchon A, Gunduz S, Loriot Y, Rodriguez-Vida A, Mamtani R, Yu EY, Nam K, Imai K, Homet Moreno B, Alva A. KEYNOTE-361 investigators pembrolizumab alone or combined with chemotherapy versus chemotherapy as first-line therapy for advanced urothelial carcinoma (KEYNOTE-361): a randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22(7):931–945. doi: 10.1016/S1470-2045(21)00152-2. [DOI] [PubMed] [Google Scholar]
- 76.Winer EP, Lipatov O, Im SA, Goncalves A, Muñoz-Couselo E, Lee KS, Schmid P, Tamura K, Testa L, Witzel I, Ohtani S, Turner N, Zambelli S, Harbeck N, Andre F, Dent R, Zhou X, Karantza V, Mejia J, Cortes J. KEYNOTE-119 investigators pembrolizumab versus investigator-choice chemotherapy for metastatic triple-negative breast cancer (KEYNOTE-119): a randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22(4):499–511. doi: 10.1016/S1470-2045(20)30754-3. [DOI] [PubMed] [Google Scholar]
- 77.Sun JM, Shen L, Shah MA, Enzinger P, Adenis A, Doi T, Kojima T, Metges JP, Li Z, Kim SB, Cho BC, Mansoor W, Li SH, Sunpaweravong P, Maqueda MA, Goekkurt E, Hara H, Antunes L, Fountzilas C, Tsuji A, Oliden VC, Liu Q, Shah S, Bhagia P, Kato K. KEYNOTE-590 investigators Pembrolizumab plus chemotherapy versus chemotherapy alone for first-line treatment of advanced oesophageal cancer (KEYNOTE-590): a randomised, placebo-controlled, phase 3 study. Lancet. 2021;398(10302):759–771. doi: 10.1016/S0140-6736(21)01234-4. [DOI] [PubMed] [Google Scholar]
- 78.Diaz LA, Jr, Shiu KK, Kim TW, Jensen BV, Jensen LH, Punt C, Smith D, Garcia-Carbonero R, Benavides M, Gibbs P, de la Fourchardiere C, Rivera F, Elez E, Le DT, Yoshino T, Zhong WY, Fogelman D, Marinello P, Andre T. KEYNOTE-177 investigators pembrolizumab versus chemotherapy for microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer (KEYNOTE-177): final analysis of a randomised, open-label, phase 3 study. Lancet Oncol. 2022;23(5):659–670. doi: 10.1016/S1470-2045(22)00197-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Makker V, Colombo N, Casado Herráez A, Santin AD, Colomba E, Miller DS, Fujiwara K, Pignata S, Baron-Hay S, Ray-Coquard I, Shapira-Frommer R, Ushijima K, Sakata J, Yonemori K, Kim YM, Guerra EM, Sanli UA, McCormack MM, Smith AD, Keefe S, Bird S, Dutta L, Orlowski RJ, Lorusso D. Study 309–KEYNOTE-775 investigators lenvatinib plus pembrolizumab for advanced endometrial cancer. N Engl J Med. 2022;386(5):437–448. doi: 10.1056/NEJMoa2108330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chung HC, Kang YK, Chen Z, Bai Y, Wan Ishak WZ, Shim BY, Park YL, Koo DH, Lu J, Xu J, Chon HJ, Bai LY, Zeng S, Yuan Y, Chen YY, Gu K, Zhong WY, Kuang S, Shih CS, Qin SK. Pembrolizumab versus paclitaxel for previously treated advanced gastric or gastroesophageal junction cancer (KEYNOTE-063): a randomized, open-label, phase 3 trial in Asian patients. Cancer. 2022;128(5):995–1003. doi: 10.1002/cncr.34019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Reckamp KL, Redman MW, Dragnev KH, Minichiello K, Villaruz LC, Faller B, Al Baghdadi T, Hines S, Everhart L, Highleyman L, Papadimitrakopoulou V, Neal JW, Waqar SN, Patel JD, Gray JE, Gandara DR, Kelly K, Herbst RS. Phase II randomized study of ramucirumab and pembrolizumab versus standard of care in advanced non-small-cell lung cancer previously treated with immunotherapy-lung-map S1800A. J Clin Oncol. 2022;40(21):2295–2306. doi: 10.1200/JCO.22.00912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Powles T, Yuen KC, Gillessen S, Kadel EE, 3rd, Rathkopf D, Matsubara N, Drake CG, Fizazi K, Piulats JM, Wysocki PJ, Buchschacher GL, Jr, Alekseev B, Mellado B, Karaszewska B, Doss JF, Rasuo G, Datye A, Mariathasan S, Williams P, Sweeney CJ. Atezolizumab with enzalutamide versus enzalutamide alone in metastatic castration-resistant prostate cancer: a randomized phase 3 trial. Nat Med. 2022;28(1):144–153. doi: 10.1038/s41591-021-01600-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Massari F, Mollica V, Rizzo A, Cosmai L, Rizzo M, Porta C. Safety evaluation of immune-based combinations in patients with advanced renal cell carcinoma: a systematic review and meta-analysis. Expert Opin Drug Saf. 2020;19(10):1329–1338. doi: 10.1080/14740338.2020.1811226. [DOI] [PubMed] [Google Scholar]
- 84.Thompson JA, Schneider BJ, Brahmer J, et al. NCCN guidelines insights: management of immunotherapy-related toxicities. Version. J Natl Compr Canc Netw. 2020;18(3):230–241. doi: 10.6004/jnccn.2020.0012. [DOI] [PubMed] [Google Scholar]
- 85.Kennedy LB, Salama AKS. A review of cancer immunotherapy toxicity. CA Cancer J Clin. 2020;70(2):86–104. doi: 10.3322/caac.21596. [DOI] [PubMed] [Google Scholar]
- 86.Luo J, Beattie JA, Fuentes P, et al. Beyond steroids: immunosuppressants in steroid-refractory/resistant immune related adverse events. J Thorac Oncol. 2021;S1556–0864(21):02291–2297. doi: 10.1016/j.jtho.2021.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rini BI, Atkins MB, Plimack ER et al. (2021) Characterization and Management of Treatment-emergent Hepatic Toxicity in Patients with Advanced Renal Cell Carcinoma Receiving First-line Pembrolizumab plus Axitinib. Results from the KEYNOTE-426 Trial. Eur Urol Oncol S2588–9311(21): 00113–9 [DOI] [PubMed]
- 88.Albiges L, Powles T, Staehler M, et al. Updated European association of urology guidelines on renal cell carcinoma: immune checkpoint inhibition is the new backbone in first-line treatment of metastatic clear-cell renal cell carcinoma. Eur Urol. 2019;76(2):151–156. doi: 10.1016/j.eururo.2019.05.022. [DOI] [PubMed] [Google Scholar]
- 89.Rizzo A, Mollica V, Santoni M, Ricci AD, Rosellini M, Marchetti A, Montironi R, Ardizzoni A, Massari F. Impact of clinicopathological features on survival in patients treated with first-line immune checkpoint inhibitors plus tyrosine kinase inhibitors for renal cell carcinoma: a meta-analysis of randomized clinical trials. Eur Urol Focus. 2022;8(2):514–521. doi: 10.1016/j.euf.2021.03.001. [DOI] [PubMed] [Google Scholar]
- 90.Powles T (2021) ESMO Guidelines Committee. Electronic address: clinicalguidelines@esmo.org. Recent eUpdate to the ESMO Clinical Practice Guidelines on renal cell carcinoma on cabozantinib and nivolumab for first-line clear cell renal cancer: Renal cell carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 32(3): 422–423 [DOI] [PubMed]
- 91.Massari F, Rizzo A, Mollica V, et al. Immune-based combinations for the treatment of metastatic renal cell carcinoma: a meta-analysis of randomised clinical trials. Eur J Cancer. 2021;154:120–127. doi: 10.1016/j.ejca.2021.06.015. [DOI] [PubMed] [Google Scholar]
- 92.Michielin O, van Akkooi ACJ, Ascierto PA, Dummer R, Keilholz U. ESMO guidelines committee electronic address: clinicalguidelines@esmo.org. Cutaneous melanoma: ESMO clinical practice Guidelines for diagnosis, treatment and follow-up†. Ann Oncol. 2019;30(12):1884–1901. doi: 10.1093/annonc/mdz411. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.