Abstract
Introduction:
The objective of this study was to evaluate the influence of the instrumentation kinematics on endodontic postoperative pain.
Methods and Materials:
PubMed, Scopus, Web of Science, Lilacs, Cochrane Library and the System for Information on Gray Literature in Europe were searched electronically without time or language limitations up to June 2020. Subsequently, data extraction, quality assessment and meta-analysis were conducted. The meta-analysis was performed using random-effects inverse-variance methods, and heterogeneity was tested using the I2 index (P<0.05).
Results:
A total of 318 articles were successfully identified in the search. Sixteen studies were used in qualitative synthesis and fourteen used for quantitative synthesis. Meta-analysis showed that patients treated with reciprocating system had lower risk of pain 48 h after endodontic treatment (Risk ratio [RR]=1.04, 95% Confidence interval [CI]=1.01-1.06, P=0.003) (I2=0%), but the mean postoperative pain for the reciprocating system was greater 24 h post endodontic treatment (Standardized mean difference [SMD]=0.25, 95% CI=0.06 to 0.44, P=0.01) (I2=43%). Other time points presented similar rates of postoperative pain (P>0.05). The certainty of evidence ranges from very low to high.
Conclusions:
The rate of postoperative endodontic pain was low, and reciprocating systems evoked more pain within the 24 h interval. Overall, the incidence and level of postoperative pain did not vary between reciprocating and rotary systems. There is no consensus if there is a relationship between the kinematics (rotary and reciprocating) and the incidence of postoperative pain.
Key Words: Endodontics, Postoperative Pain, Reciprocating Systems, Rotary Systems, Systematic Review
Introduction
Postoperative endodontic pain is an undesirable clinical condition of multifactorial aetiology, and has an incidence of 3%–58% [1-3]. The main causes are insufficient instrumentation, extrusion of irrigants and debris via the apical foramen, untreated canals, lack of apical patency, presence of preoperative pain and periapical lesions [4, 5]. To avoid this situation, the endodontist must determine the appropriate working length [6], irrigate frequently during the chemical-mechanical preparation [7] and select the correct instruments [8, 9].
Ni-Ti instruments, in addition to providing a more centralized preparation of the root canal [10], promote less extrusion of debris compared with manual instruments [11, 12]. Extrusion of infected debris may exacerbate an existing inflammatory process or initiate periapical inflammation [13], causing postoperative pain [14] .
New instruments are increasingly being launched in the market. These files can be used in rotary or reciprocating kinematics [15, 16]. The concept of reciprocating instruments involves a single file for the preparation of the root canal [17]. The reciprocating motion involves an initial rotation of the instrument in a counter clockwise direction, during which the instrument penetrates and cuts the dentin, and then rotates in the opposite direction, during which the instrument is released [18]. Some studies have found that rotary instrumentation showed better results regarding extrusion of debris [19, 20]. In contrast, Silva et al. [21] observed that rotary instrumentation extruded more debris than the reciprocating instruments tested.
Clinically, there is no consensus on whether there is a relationship between the kinematics of the instrument and the incidence of postoperative pain. In their study Nekoofar et al. [5] concluded that postoperative pain was more frequent when using reciprocating instruments. However, Kherlakain et al. [18] and Molashashi et al. [22] verified that there was no relationship between the presence of pain and the kinematics used. To clarify this clinical issue, A systematic review was undertaken to compare postoperative pain after instrumentation with rotary and reciprocating systems and found less severe pain at 48 h with the reciprocation system [23] We conducted another meta-analysis on the same topic by including more trials and hence, providing evidence with more power.
The aim of this systematic review and meta-analysis is to evaluate the influence of rotary and reciprocating kinematics on the incidence of postoperative pain after endodontic treatment of permanent teeth. This study addresses the following PICO strategy [24] question: Do reciprocating systems (I) result in greater postoperative pain (O) than rotary systems (C) in patients undergoing endodontic treatment (P)?.
Methods and Materials
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (http://www.prisma-statement.org) [25]. It was also registered in the PROSPERO database under protocol CRD42016048379.
Literature search strategy
The search covered electronic databases and the reference lists of relevant articles published up to June 2020. The following electronic databases were searched: PubMed (Medline), Scopus, Web of Science, Lilacs, Cochrane Library and System for Information on Gray Literature in Europe (SiGLE), in a comprehensive and unrestricted manner with regard to the year or language of publication. The MeSH terms used were “permanent teeth”, “endodontics”, “root canal preparation”, “root canal therapy” and “postoperative pain”, adapted for each database. In addition, free terms related to each topic were included using the Boolean operators “AND” and “OR” to match the search terms (Table 1).
Table 1.
Search strategy used for each database
| Database | Strategy |
|---|---|
| PubMed (Medline) | #1 ((((((((((((((((((((((((Permanent teeth[MeSH Terms]) OR Permanent teeth[Title/Abstract]) OR Permanent Dentition[Title/Abstract]) OR Dentition, Secondary[Title/Abstract]) OR Dentition, Adult[Title/Abstract]) OR Permanent teeth[Title/Abstract]) OR Molar[MeSH Terms]) OR Molar[Title/Abstract]) OR Molars[Title/Abstract]) OR Endodontics[MeSH Terms]) OR Endodontics[Title/Abstract]) OR Endodontic treatment[Title/Abstract]) OR Root Canal Preparation[MeSH Terms]) OR Canal Preparation, Root[Title/Abstract]) OR Canal Preparations, Root[Title/Abstract]) OR Preparation, Root Canal[Title/Abstract]) OR Preparations, Root Canal[Title/Abstract]) OR Root Canal Therapy[MeSH Terms]) OR Root Canal Therapy[Title/Abstract]) OR Canal Therapies, Root[Title/Abstract]) OR Canal Therapy, Root[Title/Abstract]) OR Therapies, Root Canal[Title/Abstract]) OR Therapy, Root Canal[Title/Abstract]) OR Root Canal Treatment[Title/Abstract]) OR Root Canal Treatments[Title/Abstract] #2 ((((((((Reciprocating Systems[Title/Abstract]) OR Reciprocating System[Title/Abstract]) OR Reciprocating[Title/Abstract]) OR WaveOne[Title/Abstract]) OR Reciproc[Title/Abstract]) OR Unicone[Title/Abstract]) OR Endodontic Instrument[Title/Abstract]) OR Endodontic Instruments[Title/Abstract]) OR Nickel-titanium instruments[Title/Abstract] #3 ((((((((((((((((((((((((((Canal Instrumentation Technique[Title/Abstract]) OR Instrumentation Techniques[Title/Abstract]) OR Instrumentation Technique[Title/Abstract]) OR Rotary System[Title/Abstract]) OR Rotary Systems[Title/Abstract]) OR Rotary Preparation[Title/Abstract]) OR Rotary[Title/Abstract]) OR Protaper[Title/Abstract]) OR Protaper Next[Title/Abstract]) OR Revo-s[Title/Abstract]) OR Hyflex[Title/Abstract]) OR K3[Title/Abstract]) OR K3XF[Title/Abstract]) OR Hero 642[Title/Abstract]) OR Easy ProDesign Logic[Title/Abstract]) OR Easy ProDesign S[Title/Abstract]) OR One Shape[Title/Abstract]) OR Mtwo[Title/Abstract]) OR TF System[Title/Abstract]) OR F6 Skytaper[Title/Abstract]) OR Race[Title/Abstract]) OR F360[Title/Abstract]) OR Twisted File[Title/Abstract]) OR Biorace[Title/Abstract]) OR Hero Shaper[Title/Abstract]) OR Profile[Title/Abstract]) OR Protaper Gold[Title/Abstract] #4 ((((((Postoperative Pain[MeSH Terms]) OR Postoperative Pain[Title/Abstract]) OR Postoperative Pains[Title/Abstract]) OR Post Endodontic Pain[Title/Abstract]) OR Post Obturation Pain[Title/Abstract]) OR Post preparation pain[Title/Abstract]) OR Post treatment pain[Title/Abstract] #1 AND #2 AND #3 AND #4 |
| Scopus |
#1 TITLE-ABS-KEY(''Permanent Teeth'') OR TITLE-ABS-KEY(''Permanent Dentition'') OR TITLE-ABS-KEY(''Secondary Dentition'') OR TITLE-ABS-KEY(''Adult Dentition'') OR TITLE-ABS-KEY(Molar) OR TITLE-ABS-KEY(Molars) OR TITLE-ABS-KEY(Éndodontics) OR TITLE-ABS-KEY(''Endodontic Treatment'') OR TITLE-ABS-KEY(''Root Canal Preparation'') OR TITLE-ABS-KEY(''Root Canal Preparations'') OR TITLE-ABS-KEY(''Root Canal Therapy'') OR TITLE-ABS-KEY(''Root Canal Therapies'') OR TITLE-ABS-KEY(''Root Canal Treatment'') OR TITLE-ABS-KEY(''Root Canal Treatments'') #2 TITLE-ABS-KEY(''Reciprocating Systems'') OR TITLE-ABS-KEY(''Reciprocating System'') OR TITLE-ABS-KEY(Reciprocating) OR TITLE-ABS-KEY(WaveOne) OR TITLE-ABS-KEY(Unicone) OR TITLE-ABS-KEY(''Endodontic Instrument'') OR TITLE-ABS-KEY(''Endodontic Instruments'') OR TITLE-ABS-KEY(''Nickel-titanium instruments'') #3 TITLE-ABS-KEY(''Canal Instrumentation Technique'') OR TITLE-ABS-KEY(''Canal Instrumentation Techniques'') OR TITLE-ABS-KEY('Instrumentation Technique'') OR TITLE-ABS-KEY (''Rotary System'') OR TITLE-ABS-KEY(''Rotary Systems') OR TITLE-ABS-KEY(''Rotary Preparation'') OR TITLE-ABS-KEY(Rotary) OR TITLE-ABS-KEY(Protaper) OR TITLE-ABS-KEY (''Protaper Next'') OR TITLE-ABS-KEY (Revo-s) OR TITLE-ABS-KEY (Hyflex) OR TITLE-ABS-KEY(K3) OR TITLE-ABS-KEY(K3XF) OR TITLE-ABS-KEY(''Hero 642'') OR TITLE-ABS-KEY (''Easy ProDesign Logic'') OR TITLE-ABS-KEY (Easy ProDesign S'') OR TITLE-ABS-KEY(''One Shape'') OR TITLE-ABS-KEY (Mtwo) OR TITLE-ABS-KEY(''TF System'') OR TITLE-ABS-KEY(''F6 Skytaper'') OR TITLE-ABS-KEY(Race) OR TITLE-ABS-KEY(F360) OR TITLE-ABS-KEY(''Twisted File'') OR TITLE-ABS-KEY(Biorace) OR TITLE-ABS-KEY(''Hero Shaper'') OR TITLE-ABS-KEY(Profile) OR TITLE-ABS-KEY(''Protaper Gold'') #4 TITLE-ABS-KEY(''Postoperative Pain'') OR TITLE-ABS-KEY(''Postoperative Pains'') OR TITLE-ABS-KEY(''Post Endodontic Pain'') OR TITLE-ABS-KEY(''Post Obturation Pain'') OR TITLE-ABS-KEY(''Post preparation pain'') OR TITLE-ABS-KEY(''Post treatment pain'') #1 AND #2 AND #3 AND #4 |
| Web of Science |
#1 TS=(''Permanent Teeth'' OR ''Permanent Dentition'' OR ''Secondary Dentition'' OR ''Adult Dentition'' OR Molar OR Molars OR Endodontics OR ''Endodontic Treatment'' OR ''Root Canal Preparation'' OR ''Root Canal Preparations'' OR ''Root Canal Therapy'' OR ''Root Canal Therapies'' OR ''Root Canal Treatment'' OR ''Root Canal Treatments'') #2 TS=(''Reciprocating Systems'' OR ''Reciprocating System'' OR Reciprocating OR WaveOne OR Unicone OR ''Endodontic Instrument'' OR ''Endodontic Instruments'' OR ''Nickel-titanium instruments'') #3 TS=(''Postoperative Pain'' OR ''Postoperative Pains'' OR ''Post Endodontic Pain'' OR ''Post Obturation Pain'' OR ''Post preparation pain'' OR ''Post treatment pain'') #1 AND #2 AND #3 |
| Grey Literature |
#1 (''Permanent Teeth'' OR ''Permanent Dentition'' OR ''Secondary Dentition'' OR ''Adult Dentition'' OR Molar OR Molars OR Endodontics OR ''Endodontic Treatment'' OR ''Root Canal Preparation'' OR ''Root Canal Preparations'' OR ''Root Canal Therapy'' OR ''Root Canal Therapies'' OR ''Root Canal Treatment'' OR ''Root Canal Treatments'') #2 (''Reciprocating Systems'' OR ''Reciprocating System'' OR Reciprocating OR WaveOne OR Unicone OR ''Endodontic Instrument'' OR ''Endodontic Instruments'' OR ''Nickel-titanium instruments'') #3 (''Postoperative Pain'' OR ''Postoperative Pains'' OR ''Post Endodontic Pain'' OR ''Post Obturation Pain'' OR ''Post preparation pain'' OR ''Post treatment pain'') #1 AND #2 AND #3 |
| Cochrane Library |
#1 MeSH descriptor: [Dentition, Permanent] explode all trees>75 #2 MeSH descriptor: [Molar] explode all trees>2407 #3 MeSH descriptor: [Endodontics] explode all trees>1373 #4 MeSH descriptor: [Root Canal Preparation] explode all trees>640 #5 MeSH descriptor: [Root Canal Therapy] explode all trees>1071 #6 Root Canal Treatment > 1345 #7 #1 or #2 or #3 or #4 or #5 or #6>4292 #8 Reciprocating System*>73 #9 Reciproc>101 #10 WaveOne>47 #11 Endodontic Instrument*>579 #12 Nickel-titanium instruments>81 #13 #8 or #9 or #10 or #11 or #12>725 #14 MeSH descriptor: [Pain, Postoperative] explode all trees> 14898 #15 Post Endodontic Pain>227 #16 Post Obturation Pain>58 #17 Post preparation pain>1503 #18 Post treatment pain>18178 #19 #15 or #16 or #17 or #18>18435 #20 #7 and #13 and #19 |
| Lilacs |
#1 (mh:(Dentes Permanentes)) OR (mh:(Permanent Teeth)) OR (mh:(Dientes Permanentes)) OR (tw:(Dentes Permanentes)) OR (tw:(Permanent Teeth)) OR (tw:(Dientes Permanentes)) OR (mh:(Molar)) OR (tw:(Molar)) OR (mh:(Endodontia)) OR (tw:(Endodontia)) OR (mh:(Endodontics)) OR (tw:(Endodontics)) OR (mh:(Endodoncia)) OR (tw:(Endodoncia)) OR (mh:(Preparo de Canal Radicular)) OR (tw:(Preparo de Canal Radicular)) OR (mh:(Root Canal Preparation )) OR (tw:(Root Canal Preparation)) OR (mh:(Preparación del conducto radicular)) OR (tw:(Preparación del conducto radicular)) OR (mh:(Tratamento do Canal Radicular)) OR (tw:(Tratamento do Canal Radicular)) OR (mh:(Root Canal Therapy)) OR (tw:(Root Canal Therapy)) OR (mh:(El tratamiento de conducto)) OR (tw:(El tratamiento de conducto)) OR (tw:(Root Canal Treatment)) OR (tw:(Tratamiento de conducto)) #2 (tw:(Sistemas Reciprocantes)) OR (tw:(Sistema Reciprocante)) OR (tw:(Reciprocating Systems )) OR (tw:(Reciprocating System)) OR (tw:(Sistemas de movimiento alternativo)) OR (tw:(Sistema de movimiento alternativo)) OR (tw:(Reciprocante)) OR (tw:(Reciprocating)) OR (tw:(vaivén)) OR (tw:(WaveOne)) OR (tw:(Reciproc)) OR (tw:(Unicone)) OR (tw:(Endodontic Instrument )) OR (tw:(Endodontic Instruments)) OR (tw:(Instrumento endodôntico)) OR (tw:(Instrumentos endodônticos)) OR (tw:(instrumento endodóntico)) OR (tw:(instrumentos endodónticos)) OR (tw:(Nickel-titanium instruments)) OR (tw:(Instrumentos de níquel-titanio)) #3 (mh:(Postoperative Pain)) OR (tw:(Postoperative Pain)) OR (mh:(Dor Pós-Operatória)) OR (tw:(Dor Pós-Operatória)) OR (mh:(El dolor postoperatorio)) OR (tw:(El dolor postoperatorio)) OR (tw:(Postoperative Pains)) OR (tw:(Los dolores postoperatorios)) OR (tw:(Dores no pós-operatório)) OR (tw:(Post Endodontic Pain)) OR (tw:(Dor Pós Endodontia)) OR (tw:(Dolor poste radicular)) OR (tw:(Post Obturation Pain)) OR (tw:(Dolor poste obturación)) OR (tw:(Dor pós obturação)) OR (tw:(Post preparation pain)) OR (tw:(Dor pós preparação)) OR (tw:(Dolor después de la preparación)) OR (tw:(Post treatment pain)) OR (tw:(Dor pós-tratamento)) OR (tw:(Dolor post tratamiento)) #1 AND #2 AND #3 |
Eligibility criteria
The eligibility criteria for the terms used for the research were based on the population (patients undergoing endodontic treatment in permanent teeth), intervention (patients treated with reciprocating systems), control (patients treated with rotary systems) and outcomes (postoperative pain). Only randomized clinical trials (RCT) and controlled clinical trials were selected in this systematic review. Observational studies, case reports, case series, in vitro studies, literature reviews, editorials and letters to editor were excluded.
Screening and data extraction
Two independent reviewers (JCLN and LMF) retrieved relevant publications involving postoperative pain after endodontic treatment of permanent teeth. Titles and abstracts were analysed during the initial screening. Subsequently, full-texts articles that appeared to meet the inclusion criteria were retrieved to confirm eligibility. Disagreements were resolved by consensus after discussion with a third reviewer (TFRL). Both reviewers also performed data extraction by adding information to an electronic spreadsheet. The following information was retrieved: authors, country, study design, number of patients, age, type of teeth evaluated, pulp diagnosis, exclusion criteria, systems evaluated, working length, irrigant solution, postoperative pain evaluation method, time intervals, statistical analysis, results and conclusion. In the event that details were not clear to the reviewers, the authors were contacted by e-mail for clarification.
Quality assessment
“The Cochrane Collaboration Risk of Bias tool” [26] was used to assess the methodological quality of the studies. Risk of bias judgment was indicated as low risk, high risk or unclear risk. Two reviewers (JCLN and LMF) made assessments independently and any disagreements were resolved by consensus.
Certainty of evidence
The certainty of the evidence (CE) for each meta-analysis were determined for the outcome using the Grading of Recommendations Assessment, Development and Evaluation (GRADE). Randimized clinical trials receive an initial “high” certainty (26). Each body of evidence is given an initial confidence rating, which is subsequently downgraded if serious or very serious problems, related to risk of bias, inconsistency, indirectness, imprecision and publication bias, are present; or upgraded if the magnitude of effect is large or very large, or if the effect of all plausible confounding factors would be to reduce the effect, or suggest a spurious effect. Publication bias was detected through visual analysis of funnel plot, independet of the number of studies included in meta-analysis. According to factors that decrease or increase confidence in the results the quality of the evidence can vary from very low to high.
Meta-analysis
The extracted data were analysed using RevMan software (Review Manager v. 5.3, Nordic Cochrane Centre, Copenhagen, Denmark) to investigate the influence of reciprocating vs. rotary techniques on postoperative pain after endodontic treatment. Two types of meta-analyses were performed: (meta-analysis 1) dichotomous data (the prevalence of “no pain” (events) and the total number of teeth treated) were used to calculate the risk ration (RR) with 95% confidence interval (CI); (meta-analysis 2) continuous data (mean and standard deviation for pain, and sample number) were used to calculate the standard mean difference (SMD) with 95% CI. Random effects models were used and heterogeneity was tested using the I2 index. If some study present the individual/patient score, the mean and standard deviation, as well as the number of events, were calculated. So, the maximum number of trials were included in each analysis (P<0.05).
Results
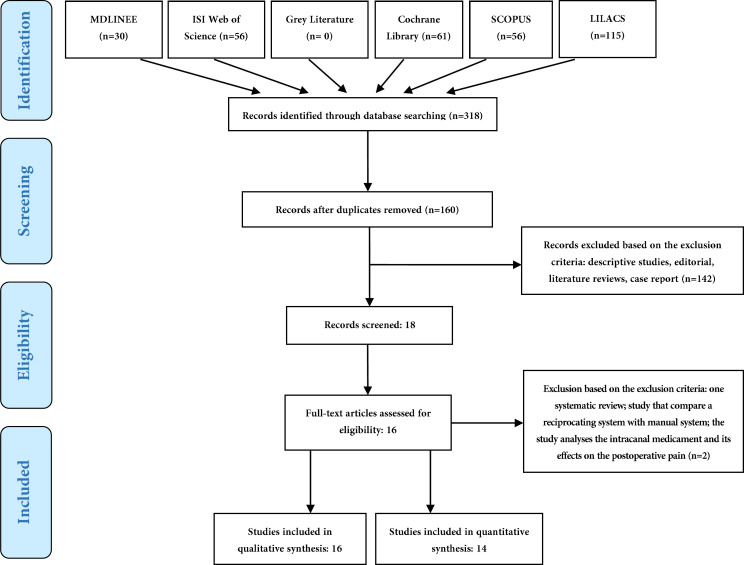
The search strategy is summarized in Figure 1. The initial search identified 318 potential articles. Mendeley software 2017 for OSX was used at this stage. After removal of duplicates, 130 articles remained. After reading the titles and abstracts, 18 articles were selected for full-text reading. Sixteen articles were selected for quantitative synthesis and data extraction. Fourteen articles were selected for the meta-analysis.
Figure 1.
Search strategy flowchart
The studies were published between 2012 and 2019 and involved a total of 2096 adult patients diagnosed with vital pulp or pulp necrosis. Endodontic treatment was performed on 2701 teeth. Neelakantan and Sharma [30] was the only study that included more than one tooth per patient. Reciprocating systems were used in 1259 teeth and rotary systems were used in 1302 teeth. Hand files were used for endodontic treatment of 110 teeth [22, 34, 38] and 30 were treated with TF Adaptive [29], which allows rotary and reciprocating motion. The Clinical trials were conducted in Italy [28, 29, 32], Brazil [18, 33, 40], India [30, 31, 39], Iran [5, 34, 37, 42] and Turkey [36, 38, 41]. The main differences between the studies were the type of teeth treated, pulp diagnosis, systems evaluated, working length, and time to evaluate postoperative pain (Table 2). In most articles, the endodontic treatment was performed at one visit, except for Nekoofar et al. [5].
Table 2.
Evidence table summarizing the characteristics of included studies
| Author | N | Age | Type of teeth | Pulp-diagnosis | Systems evaluated (n) | Working length (mm) | Main endodontic Irrigants | Follow-ups | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Gambarini et al. [ 28 ] | 60 | 21-72 | Premolars Molars | Pulp necrosis | Twisted File (30) Reciproc (30) |
0.0 a* | 5% NaOCl | 72 h | ||
| Gambarini et al. [ 29 ] | 90 | 19-73 | Premolars Molars | Pulp necrosis | Twisted File (30) WaveOne (30) TF Adaptive (30) |
0.0 a* | 5% NaOCl | 72 h | ||
| Neelakantan et al. [ 30 ] | 605 | 25-40 | Mandibular Molars | Symptomatic vital pulp | One Shape (605) Reciproc (605) |
0.5 b* | 3% NaOCl | 1, 2, 3, 4, 5, 6 and 7 days | ||
|
Nekoofar
et al. [ 5 ] |
42 | 11-55 | Premolars Molars | vital pulp | WaveOne (21) Protaper Universal (21) |
0.5 b | 2% Chlorhexidine | 6, 12, 18, 24, 48 and 72 h | ||
| Kherlakian et al. [ 18 ] | 210 | 19-73 | Premolars Molarss | Vital pulp | Protaper Next (70) WaveOne (70) Reciproc (70) |
0.5 b | 2.5% NaOCl | 24, 28, 72 h and 7 days. | ||
| Krithikhadatta et al . [ 31 ] | 148 | 18-55 | Premolars Molars | Vital/ necrotic pulp | WaveOne (49) Protaper Universal (49) MTwo (50) |
1 mm short | 5% NaOCl | Preop, 2, 4, 6, 12, 24, 36 and 48 h | ||
|
Pasqualini
et al . [ 32 ] |
47 | 16-60 | All type of teeth | Vital/ Necrotic Pulp | Protaper Universal (23) WaveOne (24) |
0.0 a | 5% NaOCl | 1,2 ,3, 4, 5, 6 and 7 days | ||
|
Relvas
et al . [ 33 ] |
78 | 18-64 | Mandibular teeth | Pulp necrosis | ProTaper Universal (39) Reciproc (39) |
0.0 a * | 2.5% NaOCl | 24, 72 h and 7 days | ||
|
Shokraneh
et al . [ 34 ] |
93 | 20-45 | Mandibular molars | Pulp necrosis | ProTaper Universal (31) WaveOne (32) Hand File (30) |
1 b | 5.25% NaOCl | 6, 12 18, 24, 36 and 72 h | ||
|
Zand
et al . [ 35 ] |
90 | 19-59 | Mandibular molars | Pulp necrosis | Race (45) Reciproc (45) |
0.5 b* | 2.5% NaOCl | 4, 12, 24, 48, 72 h and 7 days | ||
|
Arslan
et al. [ 36 ] |
56 | 19-48 | Molars | Vital pulp | Reciprocating SystemsG1-360º x 30º(14) G2.-270º x 30º(14) G3-150º x 30º(14) G4-Anti-spinning rotating system (14) |
0.5 b* | 1.25% NaOCl | 24, 72, 120 h and 7 days | ||
| Mollashahi et al. [ 37 ] | 150 | 20-50 | Molars | Symptomatic vital pulp | One Shape (50) Reciproc (50) Hand File (50) |
0.5 b* | 2.5% NaOCl | Preop, 6, 12, 24, 48 and 72 h | ||
|
ÇIÇEK
et al . [ 38 ] |
90 | 21-65 | Uni-radicular teeth | Pulp necrosis | Hand File (30) WaveOne (30) ProTaper Next (30) |
0.5 b | 5.25% NaOCl 2% Chlorhexidine |
12, 24 and 48 h | ||
|
Saha
et al . [ 39 ] |
210 | 18-55 | Premolars and Molars | Vital pulp | Self-Adjusting File (70) WaveOne Gold (70) ProTaper Next (70) |
- | 5.25% NaOCl | 24, 48 and 72 h | ||
|
Oliveira
et al. [40] |
58 | 18-66 | Molar | Asymptomatic vital pulp | Reciproc (29) ProTaper Next (29) |
1 b | 2.5% NaOCl | 24 h | ||
|
Adiguzel
et al. [41] |
69 | 21-65 | Mandibular molar | Pulp necrosis | Xp Endo Shaper (23) iRace (23) Reciproc Blue 23) |
1 b | 2.5% NaOCl | 24, 48, 72 h and 1 week | ||
RCT, randomized controlled trials; VAS, visual analogue scale; NRS, numerical rating scale; Preop: Preoperative; Sodium hypochlorite: NaOCl; a: point of apical locator; b: short
The quality of the articles was evaluated following the recommendations described by the Cochrane Collaboration [26] and its results are presented in Table 3. When was evaluated blindness of studies of participants and professionals, all articles showed a low risk of bias [5, 18, 22, 28-34, 36, 38-42]. Regarding the randomization and allocation of participants, almost all studies presented a low risk of bias [5, 18, 22, 28-34, 36, 38-41]. On the other hand, blinding of outcome assessors was an unclear risk for six studies [5, 18, 28-30, 36] and a low risk for ten articles [22, 31-34, 38-42]. The incomplete outcomes was a low risk of bias for most studies, except for Gambarini et al. [28] and Kherlakian et al. [18], which was an unclear risk. Concerning the outcomes, all articles have a low risk of bias [5, 18, 22, 28-34, 36, 38-42]. Nine studies presented a high risk of bias due to other sources of bias [5, 18, 22, 28, 29, 31, 32, 36, 42].
Table 3.
Risk of bias of selected studies
| Author | Random Sequence Generation | Allocation concealment | Binding of participants/ professionals | Blinding of outcome assessors | Incomplete outcomes | Relative outcome report | Other sources of bias |
|---|---|---|---|---|---|---|---|
| Gambarini et al. [ 28 ] | Low | Low | Low | Unclear | Low | Low | High |
| Gambarini et al. [ 29 ] | Low | Low | Low | Unclear | Unclear | Low | High |
| Neelakantan et al. [ 30 ] | Low | Low | Low | Unclear | Low | Low | Low |
| Nekoofar et al. [5] | Low | Low | Low | Unclear | Low | Low | High |
| Kherlakian et al. [18] | Low | Low | Low | Unclear | Unclear | Low | High |
| Krithikadatta et al. [31] | Low | Low | Low | Low | Low | Low | High |
| Pasqualini et al. [32] | Low | Low | Low | Low | Low | Low | High |
| Relvas et al. [33] | Low | Low | Low | Low | Low | Low | Low |
| Shokraneh et al. [34] | Low | Low | Low | Low | Low | Low | Low |
| Arslan et al. [ 36 ] | Low | Low | Low | High | Low | Low | High |
| Zand et al. [35] | Low | Unclear | Low | Low | Low | Low | High |
| Mollashahi et al. [ 37 ] | Low | Low | Low | Low | Low | Low | High |
| Çiçek et al. [38] | Low | Low | Low | Low | Low | Low | Low |
| Saha et al. [39] | Low | Low | Low | Low | Low | Low | Low |
| Oliveira et al. [40] | Low | Low | Low | Low | Low | Low | Low |
| Adiguzel et al. [41] | Low | Low | Low | Low | Low | Low | Low |
The results were presented separately in two meta-analysis with the data available in the studies included in this systematic review. One of the studies [36] presented its quantitative results only as graphics, which did not allow quantitative evaluation. These authors did not provide data for “no pain” separately from “mild pain”, hindering the analysis of cases without pain. Therefore, 14 studies were included in the meta-analysis.
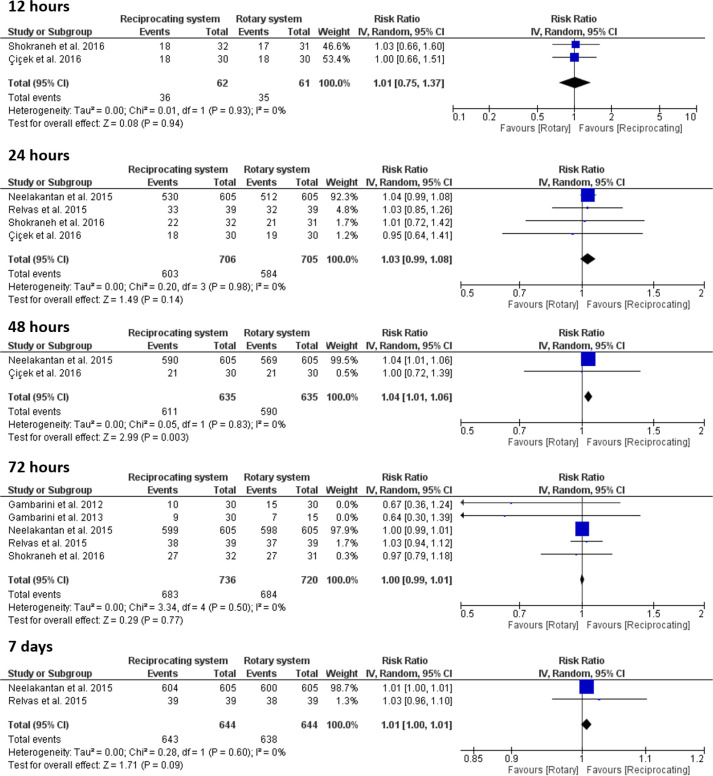
Meta-analysis 1, Dichotomous data: Figure 2 shows a forest plot for the prevalence of individuals with “no pain”. The results of the meta-analysis showed that the rotary system and the reciprocating system were similar at 12 h (RR=1.01, 95% CI=0.75 to 1.37, P=0.94) (I2=0%); 24 h (RR=1.03, 95% CI=0.99 to 1.08, P=0.14) (I2=0%); 72 h (RR=1.00, 95% CI=0.99 to 1.01, P=0.77) (I2=0%) and 7 days (RR=1.01, 95% CI=1.00 to 1.01, P=0.09) (I2=0%). However at 48 h, patients treated with reciprocating system showed lower risk of pain than patients treated with rotary system (RR=1.04, 95% CI=1.01-1.06, P=0.003) (I2=0%). The certainty of evidence ranges from very low to moderate (Table 4).
Figure 2.
Forest plot of prevalence of “no pain” (events) after endodontic treatment with reciprocating and rotary systems at different time intervals
Table 4.
Certainty of evidence of dichotomous data
| Participants (RCTs) | Indirectness | Imprecision | Overall certainty | Study event rates (%) | Relative effect (95% CI) | Anticipated absolute effects | ||
|---|---|---|---|---|---|---|---|---|
| Rotary | Reciprocanting | Risk with Rotary | Risk difference (Reciprocanting) | |||||
| 123 (2) | 12 h | |||||||
| very serious a,b | very serious c,d | Very low | 35/61 (57.4%) | 36/62 (58.1%) |
1.01 (0.75 to 1.37) |
574 per 1.000 | 6 more per 1.000 (from 143 fewer to 212 more) | |
| 1411 (4) | 24 h | |||||||
| serious b | not serious | Moderate | 584/705 (82.8%) | 603/706 (85.4%) |
1.03 (0.99 to 1.08) |
828 per 1.000 | 25 more per 1.000 (from 8 fewer to 66 more) | |
| 1270 (2) | 48 h | |||||||
| serious b | not serious | Moderate | 590/635 (92.9%) | 611/635 (96.2%) |
1.04 (1.01 to 1.06) |
929 per 1.000 | 37 more per 1.000 (from 9 more to 56 more) | |
| 1456 (5) | 72 h | |||||||
| serious b | not serious | Moderate | 684/720 (95.0%) | 683/736 (92.8%) |
1.00 (0.99 to 1.01) |
950 per 1.000 | 10 fewer per 1.000 (from 76 fewer to 76 more) | |
| 1288 (2) | 7 days | |||||||
| serious b | not serious | Moderate | 638/644 (99.1%) | 643/644 (99.8%) |
1.01 (1.00 to 1.01) |
991 per 1.000 | 10 more per 1.000 (from 0 fewer to 10 more) | |
CI: Confidence interval; RR: Risk ratio; a: Meta-analysis included only one pulp condition; b: Meta-analysis included studies that performed only one visit; c: Total number of events is less than 300; d: Upper or lower confidence limit crosses the effect size is greater than 25% of estimated effect in either direction
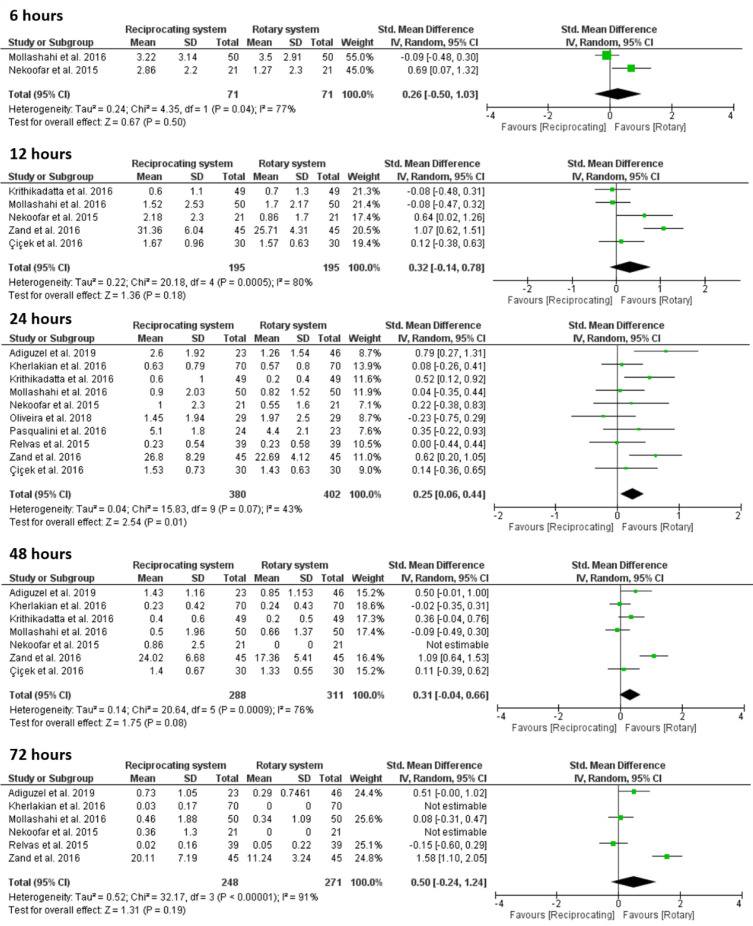
Meta-analysis 2, Continuous data. Figure 3 shows a forest plot for the postoperative pain intensity using the mean pain scores.
Figure 3.
Forest plot of postoperative pain after endodontic treatment with reciprocating and rotary systems at different time intervals
Meta-analysis of the quantitative evaluation of postoperative pain showed a greater pain level for the reciprocating system (n=380) than for the rotary system (n=402) within 24 h after endodontic treatment (SMD=0.25, 95% CI=0.06 to 0.44, P=0.01) (I2=43%). Considering the other time intervals, the reciprocating and rotary systems had similar rates of postoperative pain at 6 h (SMD=0.26, 95% CI=-0.50 to 1.03, P=0.50) (I2=77%); 12 h (SMD=0.32, 95% CI=-0.14 to 0.78, P=0.18) (I2=80%); 48 h (SMD=0.31, 95% CI=-0.04 to 0.66, P=0.08) (I2=76%); 72 h (SMD=0.50, 95% CI=-0.24 to 1.24, P=0.19) (I2=91%). The certainty of evidence ranges from very low to high (Table 5).
Table 5.
Certainty of evidence for continuous data
| Participants (RCTs ) | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Overall certainty | Study event rates (%) | Anticipated absolute effects a | |
|---|---|---|---|---|---|---|---|---|---|
| Rotary | Reciprocating | ||||||||
| 142 (2) | 6 h | ||||||||
| serious a | serious b | serious c | very serious d,e | strong association | Very low | 71 | 71 | SMD 0.26 SD higher (0.5 lower to 1.03 higher) | |
| 390 (3) | 12 h | ||||||||
| not serious | serious b | not serious | serious d | strong association | Moderate | 195 | 195 | SMD 0.32 SD higher (0.14 lower to 0.78 higher) | |
| 782 (10) | 24 h | ||||||||
| serious f | not serious | not serious | not serious | strong association | High | 402 | 380 | SMD 0.25 higher (0.06 higher to 0.44 higher) | |
| 599 (4) | 48 h | ||||||||
| not serious | serious b | not serious | not serious | strong association | High | 311 | 288 | SMD 0.31 SD higher (0.04 lower to 0.66 higher) | |
| 519 (6) | 72 h | ||||||||
| not serious | very serious b,g | very serious h,i | serious e | none | Very low | 271 | 248 | SMD 0.5 higher (0.24 lower to 1.24 higher) | |
SMD: Standardized mean difference; a: All included studies presented high risk of bias; b: Substantial or considerable heterogeneity; c: Meta-analysis included only one pulp condition; d: Total number of participants is less than 400; e: Upper or lower confidence limit crosses the effect size is greater than 0.5 in either direction
Discussion
This systematic review and meta-analysis compared the rate of postoperative pain between reciprocating and rotary systems, for which two analyses were performed. Initially, the absence of pain after endodontic treatment intervals was analysed within the time intervals of 12, 24, 48, 72 h and 7 days. Subsequently, the level of postoperative endodontic pain was analysed at the time intervals of 6, 12, 24, 48 and 72 h.
Six articles were included in the first analysis [28-30, 33, 34, 38]. The absence of pain after endodontic treatment was more frequent than the presence of pain, and there was no statistical difference between rotary and reciprocating systems, except for 48 h; patients treated with reciprocating system showed lower risk of pain. At 12 h, 24 h, 72 h and 7 days, the magnitude of the heterogeneity (I2) was 0%, which confirms the similarity of the surveys analysed at each time interval. Within 48 h, the I2 value was 50%, which confirms moderate heterogeneity of the studies analysed. Other researchers have also noted that the absence of pain is more common than its presence after endodontic treatment [43-45]. In a recent systematic review [46], no postoperative pain was reported in 60% of cases within the first 24 h, increasing to 89% after 7 days.
Ten articles were included in the second analysis [5, 18, 22, 31-33, 38, 40-42]. Statistically significant differences were detected only for the 24 h interval indicating that reciprocating systems caused more pain. Although a significant difference was observed, the level of postoperative pain detected at 24 h was low in most of the studies, expect for Pasqualini et al. [32], who reported a pain level of 5.1 on a 10-point scale, and Zand et al. [42], who reported a moderate pain. No statistical differences were found at intervals <24 h.
A recent review and meta-analysis [46] also studied the effects of different kinematics in the presence of postoperative pain. However, the authors searched only two databases, the search period was shorter than ours and there was a restriction on the language in the selection of articles. In addition, temporal analysis of pain was not performed as in the present review. The authors concluded that rotary systems were associated with fewer episodes of pain, whereas in this review such relationship was found only within 24 h.
Some clinical factors may also affect postoperative pain. Ng et al. [2] observed that sex, type of tooth and periapical lesion size may be relevant factors. Gotler et al. [3] found that the incidence of postoperative pain was higher in vital teeth than in necrotic teeth and in retreatment cases. On the other hand, Ince et al. [47] concluded that the postoperative pain did not differ between vital and necrotic teeth.
With regard to pulp and periradicular status, seven of the articles in this review included only teeth with necrotic pulp [28, 29, 33, 34, 38, 41, 42] and seven articles only teeth with vital pulp [5, 18, 22, 30, 36, 39, 40]. The other articles included teeth with vital and necrotic pulp [31, 32], making comparisons between studies difficult. Another factor that affects pain after endodontic treatment is preoperative pain [47, 48] and in this review, just one study measured pain before endodontic treatment [30].
Extrusion of debris during the chemical-mechanical preparation may also be related to a higher incidence of postoperative pain [46, 49]. There is a balance between microorganisms and host defence in chronic apical periodontitis [50]. However, when microorganisms are extruded apically during instrumentation, an imbalance occurs which may trigger an acute inflammatory reaction. It is also accepted that uncontaminated dentin and extruded pulp tissue may initiate an inflammatory process in the apical region [51, 52]. It is argued that hand instruments generally extrude more debris than Ni-Ti instruments [53-55], but there is no consensus on the extrusion of debris between rotary and reciprocating systems [16, 54]. Some authors agree that rotary instruments extrude less debris [19, 55, 56]. This could explain the lower presence of pain after 24 h when these systems are used. Robinson et al. [57] verified that reciprocating systems caused a greater accumulation of debris in isthmus areas than rotary systems, suggesting that this could lead to an unsuccessful treatment. In a systematic review, Caviedes-Bucheli et al. [58] verified that all instruments caused apical extrusion of debris; however, rotary instruments had less debris extrusion. By relating this finding to inflammation in the periapical region, the authors agreed that the design of the instrument is the most influential factor for neuropeptide expression after root canal preparation, regardless of the number of files or the type of movement [58].
Another factor that interferes with the extrusion of debris and incidence of postoperative pain is the working length [58]. In this review, some articles did not include this information [22, 29, 30, 33, 36, 39, 40, 42], which led us to contact the authors for clarification. It was concluded that in seven articles, the working length was established as 0.5 mm short of the apical foramen [5, 18, 22, 30, 36, 38, 42]; in four articles, the working length was at 0 mm from the apical locator [28, 29, 32, 33], and in four articles the teeth were instrumented 1 mm short [31, 34, 40, 41]. Some authors have verified that when the working length is 1 mm short, the extrusion of debris is reduced [59-61]. However, two randomized clinical studies verifying the effect of foraminal enlargement on postoperative pain found a low pain frequency, comparable with instrumentation 1 mm below the foramen [62, 63]. For this reason, the working length was not an exclusion criterion in this review.
Most of the articles included in the present systematic review performed endodontic treatment in one visit, with the exception of Nekoofar et al. [5]. These authors performed the treatment in two visits, however without using intracanal medication. For this meta-analysis, only the results of the first session were considered, because instrumentation with the rotary and reciprocating systems was performed at this visit. Su et al. [49] performed a systematic review and meta-analysis to understand the healing process and evaluate postoperative pain after treatment for infected obturator canals after a single visit versus multiple visits. They found that the pain experience within the first 72 h in patients undergoing a single visit (26%) was statistically lower than with multiple visits (37%). Possibly the better results for the single session may be related to immediate obturation [49]. In endodontically treated vital teeth, the frequency of postoperative pain did not differ between single and multiple sessions [45, 64].
The limitations of this systematic review are related to the inherent characteristics of any meta-analyses, associated with methodological differences among the studies, such as sample variation (in relation to sex, age, tooth type and endodontic diagnosis), different instrumentation protocols (in relation to working length, irrigating solutions and apical enlargement), different number of operators and number of sessions. In addition, pain is subjective and varies according to the personal experiences of each patient; it often cannot be measured accurately with the scales proposed in these studies. Endodontic post-treatment pain is related to multiple factors; the instrument used is only one factor. Therefore, the results of this meta-analysis should be interpreted with caution, and new studies with well-designed methodologies should be undertaken in the search for new scientific evidence on this important topic.
Conclusion
Based on the results of this meta-analysis, it can be concluded that the incidence of postoperative pain after the use of Ni-Ti instruments is low and that reciprocating systems evoked more pain within the first 24 h after treatment. Overall, the incidence and level of postoperative pain did not vary between reciprocating and rotary systems.
Conflict of Interest:
‘None declared’.
Acknowledgment
The first and second authors are grateful for the MSc scholarship received from CAPES.
References
- 1.Nagendrababu V, Gutmann JL. Factors associated with postobturation pain following single-visit nonsurgical root canal treatment: A systematic review. Quintessence Int. 2017;48(3):193–208. doi: 10.3290/j.qi.a36894. [DOI] [PubMed] [Google Scholar]
- 2.Ng YL, Glennon JP, Setchell DJ, Gulabivala K. Prevalence of and factors affecting post-obturation pain in patients undergoing root canal treatment. Int Endod J. 2004;37(6):381–91. doi: 10.1111/j.1365-2591.2004.00820.x. [DOI] [PubMed] [Google Scholar]
- 3.Gotler M, Bar-Gil B, Ashkenazi M. Postoperative pain after root canal treatment: a prospective cohort study. Int J Dent. 2012;2012:310467. doi: 10.1155/2012/310467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alves Vde O. Endodontic flare-ups: a prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110(5):e68–72. doi: 10.1016/j.tripleo.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 5.Nekoofar MH, Sheykhrezae MS, Meraji N, Jamee A, Shirvani A, Jamee J, Dummer PM. Comparison of the effect of root canal preparation by using WaveOne and ProTaper on postoperative pain: a randomized clinical trial. J Endod. 2015;41(5):575–8. doi: 10.1016/j.joen.2014.12.026. [DOI] [PubMed] [Google Scholar]
- 6.Seltzer S, Naidorf IJ. Flare-ups in endodontics: I. Etiological factors. J Endod. 1985;11(11):472–8. doi: 10.1016/S0099-2399(85)80220-X. [DOI] [PubMed] [Google Scholar]
- 7.Romualdo PC, de Oliveira KMH, Nemezio MA, Küchler EC, Silva RAB, Nelson-Filho P, Silva LAB. Does apical negative pressure prevent the apical extrusion of debris and irrigant compared with conventional irrigation? A systematic review and meta-analysis. Aust Endod J. 2017;43(3):129–37. doi: 10.1111/aej.12162. [DOI] [PubMed] [Google Scholar]
- 8.Elmsallati EA, Wadachi R, Suda H. Extrusion of debris after use of rotary nickel-titanium files with different pitch: a pilot study. Aust Endod J. 2009;35(2):65–9. doi: 10.1111/j.1747-4477.2008.00128.x. [DOI] [PubMed] [Google Scholar]
- 9.Mittal R, Singla MG, Garg A, Dhawan A. A Comparison of Apical Bacterial Extrusion in Manual, ProTaper Rotary, and One Shape Rotary Instrumentation Techniques. J Endod. 2015;41(12):2040–4. doi: 10.1016/j.joen.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 10.Gundappa M, Bansal R, Khoriya S, Mohan R. Root canal centering ability of rotary cutting nickel titanium instruments: A meta-analysis. J Conserv Dent. 2014;17(6):504–9. doi: 10.4103/0972-0707.144567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kustarci A, Akdemir N, Siso SH, Altunbas D. Apical extrusion of intracanal debris using two engine driven and step-back instrumentation techniques: an in-vitro study. Eur J Dent. 2008;2(4):233–9. [PMC free article] [PubMed] [Google Scholar]
- 12.Kuştarci A, Akpinar KE, Er K. Apical extrusion of intracanal debris and irrigant following use of various instrumentation techniques. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105(2):257–62. doi: 10.1016/j.tripleo.2007.06.028. [DOI] [PubMed] [Google Scholar]
- 13.Cunningham CJ, Mullaney TP. Pain control in endodontics. Dent Clin North Am. 1992;36(2):393–408. [PubMed] [Google Scholar]
- 14.Talebzadeh B, Nezafati S, Rahimi S, Shahi S, Lotfi M, Ghasemi N. Comparison of Manual and Rotary Instrumentation on Postoperative Pain in Teeth with Asymptomatic Irreversible Pulpitis: A Randomized Clinical Trial. Iran Endod J. 2016;11(4):273–9. doi: 10.22037/iej.2016.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Plotino G, Ahmed HM, Grande NM, Cohen S, Bukiet F. Current Assessment of Reciprocation in Endodontic Preparation: A Comprehensive Review--Part II: Properties and Effectiveness. J Endod. 2015;41(12):1939–50. doi: 10.1016/j.joen.2015.08.018. [DOI] [PubMed] [Google Scholar]
- 16.Çapar ID, Arslan H. A review of instrumentation kinematics of engine-driven nickel-titanium instruments. Int Endod J. 2016;49(2):119–35. doi: 10.1111/iej.12432. [DOI] [PubMed] [Google Scholar]
- 17.Yared G. Canal preparation using only one Ni-Ti rotary instrument: preliminary observations. Int Endod J. 2008;41(4):339–44. doi: 10.1111/j.1365-2591.2007.01351.x. [DOI] [PubMed] [Google Scholar]
- 18.Kherlakian D, Cunha RS, Ehrhardt IC, Zuolo ML, Kishen A, da Silveira Bueno CE. Comparison of the Incidence of Postoperative Pain after Using 2 Reciprocating Systems and a Continuous Rotary System: A Prospective Randomized Clinical Trial. J Endod. 2016;42(2):171–6. doi: 10.1016/j.joen.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 19.Bürklein S, Schäfer E. Apically extruded debris with reciprocating single-file and full-sequence rotary instrumentation systems. J Endod. 2012;38(6):850–2. doi: 10.1016/j.joen.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 20.Bürklein S, Benten S, Schäfer E. Quantitative evaluation of apically extruded debris with different single-file systems: Reciproc, F360 and OneShape versus Mtwo. Int Endod J. 2014;47(5):405–9. doi: 10.1111/iej.12161. [DOI] [PubMed] [Google Scholar]
- 21.Silva EJ, Carapiá MF, Lopes RM, Belladonna FG, Senna PM, Souza EM, De-Deus G. Comparison of apically extruded debris after large apical preparations by full-sequence rotary and single-file reciprocating systems. Int Endod J. 2016;49(7):700–5. doi: 10.1111/iej.12503. [DOI] [PubMed] [Google Scholar]
- 22.Mollashahi NF, Saberi EA, Havaei SR, Sabeti M. Comparison of Postoperative Pain after Root Canal Preparation with Two Reciprocating and Rotary Single-File Systems: A Randomized Clinical Trial. Iran Endod J. 2017;12(1):15–9. doi: 10.22037/iej.2017.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martins CM, De Souza Batista VE, Andolfatto Souza AC, Andrada AC, Mori GG, Gomes Filho JE. Reciprocating kinematics leads to lower incidences of postoperative pain than rotary kinematics after endodontic treatment: A systematic review and meta-analysis of randomized controlled trial. J Conserv Dent. 2019;22(4):320–31. doi: 10.4103/JCD.JCD_439_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maia LC, Antonio AG. Systematic reviews in dental research A guideline. J Clin Pediatr Dent. 2012;37(2):117–24. doi: 10.17796/jcpd.37.2.h606137vj3826v61. [DOI] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Higgins JP. Cochrane handbook for systematic reviews of interventions version 5.0. 1. The Cochrane Collaboration. 2008. http://www.cochrane-handbook.Org .
- 27.Ryan R,, Hill S. How to GRADE the quality of the evidence. Cochrane Consumers and Communication Group. Version 3.0. 2016. http://cccrg.cochrane.org/author-resources .
- 28.Gambarini G, Al-Sudani D, Di Carlo S, Pompa G, Pacifici A, Pacifici L, Testarelli L. Incidence and Intensivity of Postoperative Pain and Periapical Inflammation after Endodontic Treatment with Two Different Instrumentation Techniques. European Journal of Inflammation. 2012;10:99–103. [Google Scholar]
- 29.Gambarini G, Testarelli L, De Luca M, Milana V, Plotino G, Grande NM, Rubini AG, Al Sudani D, Sannino G. The influence of three different instrumentation techniques on the incidence of postoperative pain after endodontic treatment. Ann Stomatol (Roma). 2013;4(1):152–5. doi: 10.11138/ads.0152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Neelakantan P, Sharma S. Pain after single-visit root canal treatment with two single-file systems based on different kinematics--a prospective randomized multicenter clinical study. Clin Oral Investig. 2015;19(9):2211–7. doi: 10.1007/s00784-015-1448-x. [DOI] [PubMed] [Google Scholar]
- 31.Krithikadatta J, Sekar V, Sudharsan P, Velumurugan N. Influence of three Ni-Ti cleaning and shaping files on postinstrumentation endodontic pain: A triple-blinded, randomized, controlled trial. J Conserv Dent. 2016;19(4):311–6. doi: 10.4103/0972-0707.186442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pasqualini D, Corbella S, Alovisi M, Taschieri S, Del Fabbro M, Migliaretti G, Carpegna GC, Scotti N, Berutti E. Postoperative quality of life following single-visit root canal treatment performed by rotary or reciprocating instrumentation: a randomized clinical trial. Int Endod J. 2016;49(11):1030–9. doi: 10.1111/iej.12563. [DOI] [PubMed] [Google Scholar]
- 33.Relvas JB, Bastos MM, Marques AA, Garrido AD, Sponchiado EC Jr. Assessment of postoperative pain after reciprocating or rotary NiTi instrumentation of root canals: a randomized, controlled clinical trial. Clin Oral Investig. 2016;20(8):1987–93. doi: 10.1007/s00784-015-1692-0. [DOI] [PubMed] [Google Scholar]
- 34.Shokraneh A, Ajami M, Farhadi N, Hosseini M, Rohani B. Postoperative endodontic pain of three different instrumentation techniques in asymptomatic necrotic mandibular molars with periapical lesion: a prospective, randomized, double-blind clinical trial. Clin Oral Investig. 2017;21(1):413–8. doi: 10.1007/s00784-016-1807-2. [DOI] [PubMed] [Google Scholar]
- 35.Zand V, Lotfi M, Soroush MH, Abdollahi AA, Sadeghi M, Mojadadi A. Antibacterial Efficacy of Different Concentrations of Sodium Hypochlorite Gel and Solution on Enterococcus faecalis Biofilm. Iran Endod J. 2016;11(4):315–9. doi: 10.22037/iej.2016.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arslan H, Khalilov R, Doğanay E, Karatas E. The effect of various kinematics on postoperative pain after instrumentation: a prospective, randomized clinical study. J Appl Oral Sci. 2016;24(5):503–8. doi: 10.1590/1678-775720160136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mollashahi NF, Saberi EA, Havaei SR, Sabeti M. Comparison of Postoperative Pain after Root Canal Preparation with Two Reciprocating and Rotary Single-File Systems: A Randomized Clinical Trial. Iran Endod J. 2017;12(1) doi: 10.22037/iej.2017.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Çiçek E, Koçak MM, Koçak S, Sağlam BC, Türker SA. Postoperative pain intensity after using different instrumentation techniques: a randomized clinical study. J Appl Oral Sci. 2017;25(1):20–6. doi: 10.1590/1678-77572016-0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saha SG, Gupta RK, Bhardwaj A, Misuriya A, Saha MK, Nirwan AS. Comparison of the incidence of postoperative pain after using a continuous rotary system, a reciprocating system, and a Self-Adjusting File system in single-visit endodontics: A prospective randomized clinical trial. J Conserv Dent. 2018;21(3):333–8. doi: 10.4103/JCD.JCD_336_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Oliveira PS, da Costa KNB, Carvalho CN, Ferreira MC. Impact of root canal preparation performed by ProTaper Next or Reciproc on the quality of life of patients: a randomized clinical trial. Int Endod J. 2019;52(2):139–48. doi: 10.1111/iej.12990. [DOI] [PubMed] [Google Scholar]
- 41.Adiguzel M, Tufenkci P, Pamukcu II. Comparison of postoperative pain intensity following the use of three different instrumentation techniques: A randomized clinical trial. J Dent Res Dent Clin Dent Prospects. 2019;13(2):133–40. doi: 10.15171/joddd.2019.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zand V, Milani AS, Hassani Dehkharghani A, Rahbar M, Tehranchi P. Treatment of Necrotic Teeth Using Two Engine-Driven Systems and Patient's Postoperative Pain: A Double-Blind Clinical Trial. Iran Endod J. 2016;11(4):267–72. doi: 10.22037/iej.2016.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.DiRenzo A, Gresla T, Johnson BR, Rogers M, Tucker D, BeGole EA. Postoperative pain after 1- and 2-visit root canal therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(5):605–10. doi: 10.1067/moe.2002.121900. [DOI] [PubMed] [Google Scholar]
- 44.Wang C, Xu P, Ren L, Dong G, Ye L. Comparison of post-obturation pain experience following one-visit and two-visit root canal treatment on teeth with vital pulps: a randomized controlled trial. Int Endod J. 2010;43(8):692–7. doi: 10.1111/j.1365-2591.2010.01748.x. [DOI] [PubMed] [Google Scholar]
- 45.Singh S, Garg A. Incidence of post-operative pain after single visit and multiple visit root canal treatment: A randomized controlled trial. J Conserv Dent. 2012;15(4):323–7. doi: 10.4103/0972-0707.101888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pak JG, White SN. Pain prevalence and severity before, during, and after root canal treatment: a systematic review. J Endod. 2011;37(4):429–38. doi: 10.1016/j.joen.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 47.Ince B, Ercan E, Dalli M, Dulgergil CT, Zorba YO, Colak H. Incidence of postoperative pain after single- and multi-visit endodontic treatment in teeth with vital and non-vital pulp. Eur J Dent. 2009;3(4):273–9. [PMC free article] [PubMed] [Google Scholar]
- 48.Sathorn C, Parashos P, Messer H. The prevalence of postoperative pain and flare-up in single- and multiple-visit endodontic treatment: a systematic review. Int Endod J. 2008;41(2):91–9. doi: 10.1111/j.1365-2591.2007.01316.x. [DOI] [PubMed] [Google Scholar]
- 49.Su Y, Wang C, Ye L. Healing rate and post-obturation pain of single- versus multiple-visit endodontic treatment for infected root canals: a systematic review. J Endod. 2011;37(2):125–32. doi: 10.1016/j.joen.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 50.Siqueira JF Jr. Microbial causes of endodontic flare-ups. Int Endod J. 2003;36(7):453–63. doi: 10.1046/j.1365-2591.2003.00671.x. [DOI] [PubMed] [Google Scholar]
- 51.Seltzer S, Soltanoff W, Sinai I, Goldenberg A, Bender IB. Biologic aspects of endodontics 3 Periapical tissue reactions to root canal instrumentation. Oral Surg Oral Med Oral Pathol. 1968;26(5):694–705. doi: 10.1016/0030-4220(68)90442-8. [DOI] [PubMed] [Google Scholar]
- 52.Torneck CD. Reaction of rat connective tissue to polyethylene tube implants II. Oral Surg Oral Med Oral Pathol. 1967;24(5):674–83. doi: 10.1016/0030-4220(67)90215-0. [DOI] [PubMed] [Google Scholar]
- 53.Beeson TJ, Hartwell GR, Thornton JD, Gunsolley JC. Comparison of debris extruded apically in straight canals: conventional filing versus profile Taper series 29. J Endod. 1998;24(1):18–22. doi: 10.1016/S0099-2399(98)80206-9. [DOI] [PubMed] [Google Scholar]
- 54.Bidar M, Rastegar AF, Ghaziani P, Namazikhah MS. Evaluation of apically extruded debris in conventional and rotary instrumentation techniques. J Calif Dent Assoc. 2004;32(9):665–71. [PubMed] [Google Scholar]
- 55.Tanalp J, Güngör T. Apical extrusion of debris: a literature review of an inherent occurrence during root canal treatment. Int Endod J. 2014;47(3):211–21. doi: 10.1111/iej.12137. [DOI] [PubMed] [Google Scholar]
- 56.Saberi E, Ebrahimipour S, Saberi M. Apical Debris Extrusion with Conventional Rotary and Reciprocating Instruments. Iran Endod J. 2020;15:5. doi: 10.22037/iej.v15i1.23823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Robinson JP, Lumley PJ, Cooper PR, Grover LM, Walmsley AD. Reciprocating root canal technique induces greater debris accumulation than a continuous rotary technique as assessed by 3-dimensional micro-computed tomography. J Endod. 2013;39(8):1067–70. doi: 10.1016/j.joen.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 58.Caviedes-Bucheli J, Castellanos F, Vasquez N, Ulate E, Munoz HR. The influence of two reciprocating single-file and two rotary-file systems on the apical extrusion of debris and its biological relationship with symptomatic apical periodontitis A systematic review and meta-analysis. Int Endod J. 2016;49(3):255–70. doi: 10.1111/iej.12452. [DOI] [PubMed] [Google Scholar]
- 59.Martin H, Cunningham WT. The effect of endosonic and hand manipulation on the amount of root canal material extruded. Oral Surg Oral Med Oral Pathol. 1982;53(6):611–3. doi: 10.1016/0030-4220(82)90350-4. [DOI] [PubMed] [Google Scholar]
- 60.Myers GL, Montgomery S. A comparison of weights of debris extruded apically by conventional filing and Canal Master techniques. J Endod. 1991;17(6):275–9. doi: 10.1016/S0099-2399(06)81866-2. [DOI] [PubMed] [Google Scholar]
- 61.Surakanti JR, Venkata RC, Vemisetty HK, Dandolu RK, Jaya NK, Thota S. Comparative evaluation of apically extruded debris during root canal preparation using ProTaper™, Hyflex™ and Waveone™ rotary systems. J Conserv Dent. 2014;17(2):129–32. doi: 10.4103/0972-0707.128045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cruz Junior JA, Coelho MS, Kato AS, Vivacqua-Gomes N, Fontana CE, Rocha DG, da Silveira Bueno CE. The Effect of Foraminal Enlargement of Necrotic Teeth with the Reciproc System on Postoperative Pain: A Prospective and Randomized Clinical Trial. J Endod. 2016;42(1):8–11. doi: 10.1016/j.joen.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 63.Silva EJ, Menaged K, Ajuz N, Monteiro MR, Coutinho-Filho Tde S. Postoperative pain after foraminal enlargement in anterior teeth with necrosis and apical periodontitis: a prospective and randomized clinical trial. J Endod. 2013;39(2):173–6. doi: 10.1016/j.joen.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 64.Farokh-Gisour E, Parirokh M, Kheirmand Parizi M, Nakhaee N, Aminizadeh M. Comparison of Postoperative Pain Following One-Visit and Two-Visit Vital Pulpectomy in Primary Teeth: A Single-Blind Randomized Clinical Trial. Iran Endod J. 2018;13(1):13–9. doi: 10.22037/iej.v13i1.18205. [DOI] [PMC free article] [PubMed] [Google Scholar]