Abstract
Objectives
The mental health impacts of the COVID-19 pandemic continue to be documented worldwide with systematic reviews playing a pivotal role. Here we present updated findings from our systematic review and meta-analysis on the mental health impacts among hospital healthcare workers during COVID-19.
Methods
We searched MEDLINE, CINAHL, PsycINFO, Embase and Web Of Science Core Collection between 1st January 2000 to 17th February 2022 for studies using validated methods and reporting on the prevalence of diagnosed or probable mental health disorders in hospital healthcare workers during the COVID-19 pandemic. A meta-analysis of proportions and odds ratio was performed using a random effects model. Heterogeneity was investigated using test of subgroup differences and 95 % prediction intervals.
Results
The meta-analysis included 401 studies, representing 458,754 participants across 58 countries. Pooled prevalence of depression was 28.5 % (95 % CI: 26.3–30.7), anxiety was 28.7 % (95 % CI: 26.5–31.0), PTSD was 25.5 % (95 % CI: 22.5–28.5), alcohol and substance use disorder was 25.3 % (95 % CI: 13.3–39.6) and insomnia was 24.4 % (95 % CI: 19.4–29.9). Prevalence rates were stratified by physicians, nurses, allied health, support staff and healthcare students, which varied considerably. There were significantly higher odds of probable mental health disorders in women, those working in high-risk units and those providing direct care.
Limitations
Majority of studies used self-report measures which reflected probable mental health disorders rather than actual diagnosis.
Conclusions
These updated findings have enhanced our understanding of at-risk groups working in hospitals. Targeted support and research towards these differences in mental health risks are recommended to mitigate any long-term consequences.
Keywords: Mental health disorders, Hospital healthcare workers, COVID-19, Anxiety, Depression, Post-traumatic stress disorder (PTSD)
1. Introduction
Despite stringent public health measures, the Coronavirus Disease 2019 (COVID-19) pandemic has continued to persist worldwide, with now >600 million people infected and 6.5 million deaths across 233 countries (World Health Organisation, 2021). As different COVID-19 variants (World Health Organisation, 2022) continue to trigger multiple waves of outbreaks worldwide (Hale et al., 2021; Hassan and Mahmoud, 2021), many are concerned that its extended nature and impacts may leave long-lasting mental health consequences (Holmes et al., 2020; Pfefferbaum and North, 2020).
More specifically, there are concerns that hospital healthcare workers' (HCW) mental health may be disproportionately affected as they continue to work in high-risk settings that are constantly overwhelmed with COVID-19 patients. Studies have shown that working in these settings early on in the pandemic have led to feelings of threat, uncertainty and fatigue among hospital HCWs as they face high infection risks, inadequate protective equipment, inconsistent communications, and increased workload (Digby et al., 2021; Ding et al., 2021; Hennein and Lowe, 2020; Joo and Liu, 2021; Liu et al., 2020). It is thus unsurprising that, consistent with findings on previous epidemics (Carmassi et al., 2020; De Brier et al., 2020; Preti et al., 2020), a number of early reviews have documented a wide range of mental health issues among hospital HCWs during the pandemic, such as depression (Salari et al., 2020b; Yan et al., 2021), anxiety (Raoofi et al., 2021; Salari et al., 2020b; Yan et al., 2021), post-traumatic stress disorder (PTSD) (Yan et al., 2021) and insomnia (Salari et al., 2020a; Salari et al., 2020b; Yan et al., 2021).
In view of these findings and the continuing spread of COVID-19, supporting hospital HCWs' mental health is of the upmost importance to prevent long lasting consequences that may lead to chronic mental health disorders. To do so effectively, we need to better understand the mental health impacts of the COVID-19 pandemic on hospital HCWs and identify groups that may be at a risk of mental health disorders during the COVID-19 pandemic. This is, however, challenging given that prevalence estimates from previous reviews (X. Li et al., 2021; Raoofi et al., 2021; Salari et al., 2020a; Salari et al., 2020b) have varied widely, with some reviews finding similar rates between HCWs and the general public (Cénat et al., 2021; Phiri et al., 2021; Raoofi et al., 2021), making it unclear to what extent working in hospitals, as opposed to other pandemic factors, have affected hospital HCWs' mental health. This resonates with a systematic review on the Severe Acute Respiratory Syndrome (SARS) outbreak that found inconclusive evidence on whether HCW status was a risk factor for mental health issues (Chau et al., 2021). There have also been inconsistent findings on at risk groups among hospital HCWs during the COVID-19 pandemic, with varied findings on whether mental health issues varies between profession (Olaya et al., 2021; Pappa et al., 2020; Santabárbara et al., 2021; Varghese et al., 2021; Wu et al., 2021), gender (Ching et al., 2021; Y. Li et al., 2021; Raoofi et al., 2021; Serrano-Ripoll et al., 2020; Varghese et al., 2021; Yuan et al., 2021; Zhao et al., 2021) and frontline status (frontline HCWs defined as those providing direct care or working in high risk settings) (Bell and Wade, 2020; Carmassi et al., 2020; De Brier et al., 2020; Galli et al., 2020; Muller et al., 2020). There is thus a clear need to better understand and update findings on the prevalence and trends in mental health disorders among hospital HCWs and to identify vulnerable groups at risk. The dynamic progression of the COVID-19 pandemic has also made it more important to consistently update findings and provide understanding on longitudinal trends to provide effective recommendations, which are important to help focus and design effective interventions and strategies to protect hospital HCWs mental health.
1.1. Aims and objectives
This systematic review and meta-analysis aim to review the literature to update findings and estimates on the prevalence of mental health disorders experienced by hospital HCWs during the COVID-19 pandemic. This study also aims to examine the literature to evaluate the prevalence of mental health disorders among individual healthcare professions and compare prevalence estimates of mental health disorders by gender (i.e., men and women), COVID-19 work setting (i.e., high and low risk units), and COVID-19 work roles (i.e., HCWs providing direct care to COVID-19 patients and those who do not).
2. Methods
This systematic review followed the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines when conducting this study (Moher et al., 2009) (S1 Appendix). The protocol for this systematic review and meta-analysis was pre-registered and submitted to PROSPERO (ID: CRD42020219174). Due to the rapid publication of studies, the research questions and systematic review went through several iterations (detailed in PROSPERO) to ensure its relevance and avoid duplication of efforts.
2.1. Search strategy
A systematic search of the following database was conducted: MEDLINE, CINAHL, PsycINFO via EBSCOhost, Embase via Emabase.com, and Web Of Science Core Collection via webofknowledge.com. Searches were restricted to peer review articles, from 1st January 2000 to 17th February 2022, and English publications.
Search terms were derived from previous reviews and in consultation with a specialist librarian using the PRESS checklist (McGowan et al., 2016). Key concepts included healthcare workers, mental health, and coronavirus. Related terms, database specific MESH terms, truncation and proximity commands were used in the search. (A sample search strategy is shown in S2A Appendix). Endnote X9 was used to retrieve searches and remove duplicated citations.
2.2. Inclusion and exclusion criteria
Prior to any screening, inclusion and exclusion criteria were pre-defined. Studies were included if they: (1) reported prevalence rates of any outcome related a mental health disorder defined by the diagnostic and statistical manual of mental disorders 5th edition (DSM-V) (American Psychiatric Association, 2013), (2) reported data on any HCWs who have worked in a tertiary or secondary level hospital during the COVID-19 pandemic, (3) and used validated methods (self-report measurement tools or diagnostic interviews) to identify the presence of a mental health disorder.
Studies were excluded if they: (1) were not published in the English language, (2) were not a primary study, (3) were published as an editorial, communication or brief report, (4) full-text were unobtainable (5) did not report the use of valid cut offs or scoring methods (6) were not peer-reviewed or (7) used purposive sampling in their study design that was based on the presence of mental health conditions or lack thereof.
2.3. Operational definition - presence of a mental health disorder
The presence of a mental health disorder in this systematic review is defined as those meeting the validated criteria on diagnostic interviews for mental health disorders as defined by the DSM-V (American Psychiatric Association, 2013). Where diagnostic interviews are not used, the presence of clinically significant symptoms that are likely to indicate a probable mental health disorder will be applied instead. This is defined as those meeting optimal cut-offs on measurement tools that have been validated against diagnostic interviews and using validated methods when estimating the likelihood of mental health disorder present in an individual.
2.4. Study selection
The first author BL screened all studies' title and abstract using the pre-defined criteria. When title and abstract were not clear, studies were reviewed at full text by BL. A random 10 % of studies at the title and abstract stage, and full text stage were screened independently by a second reviewer from the research team (DG, HS, CH, AJ, MVR, GK or BD). Conflicts were resolved by an independent third reviewer. After resolving conflicts, the first author's inter-rater agreement with second reviewers was at 98.7 % at the title and abstract and 98 % at the full text stage.
2.5. Data extraction
Following full-text screening, BL independently completed the risk of bias assessment and data extraction. Data extracted from the included studies are as follows: (1) author details, (2) study design, (3) coronavirus outbreak setting, (4) outcomes measured, (5) measurement tools, (6) recruitment dates, (7) mean or median age, (8) country of study, (9) overall sample size of hospital HCWs, (10) subgroup sample size (i.e., physicians, nurses, allied health staff, support staff, non-medical staff, healthcare students, hospital HCWs working in high risk or low risk units, hospital HCWs providing direct care or do not provide direct care, and gender), and the number of hospital HCWs overall and in subgroups who meet the criteria for a mental health disorder (See Appendix 2B for full list of occupations included in profession subgroups). Total and stratified prevalence rates were calculated as number of sample meeting criteria for a mental health disorder divided by total sample size. When only percentage was reported for prevalence rates, the number of participants with a mental health disorder was recalculated by multiplying point prevalence rates with total sample size. When multiple reports of the same dataset were found, they were merged and reported as one dataset to avoid double counting studies. When studies used both interviews and self-report measures, only prevalence data measured by interviews were extracted for analysis due to their increased validity and reliability. When studies reported incomplete or inconsistent data, authors were contacted for more information. All data extraction went through a second check by a second reviewer.
2.6. Quality assessment
The checklist for prevalence studies (Munn et al., 2015) from the Joanna Briggs institute (JBI) was used to assess a study's risk of bias with regards to their recruitment sample frame, sampling methods, validity and reliability of outcome measurement, statistical methodology and reporting, and overall and subgroup response rate (see S2C Appendix for further details). When there were disagreements, they were resolved through discussions between reviewers until there was a consensus.
2.7. Data synthesis
A meta-analysis of proportions was conducted using R (R Core Team, 2013), and the packages meta, metafor and dmetar (Balduzzi et al., 2019; Harrer et al., 2019a; Harrer et al., 2019b; Viechtbauer, 2010; Wang, 2018). Due to the variability between studies, it is assumed that there is no one true effect size and thus a random effects model, using the restricted maximum likelihood method (REML), was used to pool prevalence rates (Borenstein and Higgins, 2013). Prevalence rates were transformed using the Freeman-Tukey Double arcsine transformation and back transformed for ease of interpretation, as recommended by Barendregt et al. (2013) to address, if any, imbalanced weighting from extreme estimates and non-normal distribution of prevalence rates in the meta-analysis. The variability in prevalence estimates that was due to heterogeneity was assessed using standard to test for significant heterogeneity and to determine low (<25 %), moderate (25 %–50 %), and high (>75 %) heterogeneity among studies (Higgins et al., 2003).
2.8. Subgroup analyses
2.8.1. Subgroup analyses by study level characteristics
Subgroup analyses were conducted on overall pooled prevalence rates when there were four or more studies (Fu et al., 2011), with test of subgroup differences using Q tests for categorical predictors (i.e. measurement tools, region and risk of bias). Test of subgroup difference between countries was considered inappropriate as there was insufficient studies (<4 studies) in the majority of countries. As such, the studies were categorised post-hoc according to regions categorised by the World Health Organisation regions (i.e., Africa, Americas, South-East Asia, Europe, Eastern Mediterranean, Western Pacific), as these regions have been shown to have significantly different prevalence of mental health issues when estimated for the general public (Nochaiwong et al., 2021).
2.8.2. Subgroup analyses by sub-populations
Stratified prevalence rates were estimated in individual professions to compare differences between prevalence rates among the different professions. To avoid false positives common in subgroup analyses where there is high heterogeneity (Higgins and Thompson, 2004), as well as to quantify the effect of working in high-risk units, providing direct care to COVID-19 patients and gender on prevalence rates, pooled odds ratios (OR) were estimated for these sub-populations. Studies were only included in the OR analyses if they reported prevalence rates for both groups of interest (e.g., prevalence rates for both men and women). To estimate pooled ORs, log odds ratios were calculated and derived from prevalence rates reported by individual studies, pooled using a random effects model (REML method) and then back transformed for ease of interpretation (Borenstein and Higgins, 2013). To reduce type 1 error from having low numbers of studies and heterogenous findings, the Hartung-Knapp method was used to estimate confidence intervals for ORs (Hartung and Knapp, 2001a, Hartung and Knapp, 2001b; IntHout et al., 2014). HCWs in low-risk units, HCWs who do not provide direct care (referred as no direct care henceforth) and men were used as the reference group in their respective OR analyses. Significance thresholds of p < 0.05 were used in all analysis.
2.9. Sensitivity analysis
Sensitivity analysis was performed by excluding each included study to identify any influential outliers that have significant influence on overall estimates and heterogeneity by assessing externally standardised residuals, difference in fits values (DFFITS), Cook's distance, covariance ratios, DFBETAS, leave one out statistics, hat values and weights (Viechtbauer and Cheung, 2010). Prediction intervals (PI) were estimated when there were four or more studies to predict where 95 % of future estimates would lie (Borenstein et al., 2017).
2.10. Publication bias
Publication bias was assessed by visually inspecting funnel plots in conjunction with Egger test of asymmetry. A p-value <0.05 in Egger's test indicated significant publication bias.
3. Results
3.1. COVID-19 - overall
In total there were 401 included studies from 392 unique datasets, with 18 longitudinal studies that reported on the prevalence rates across different timepoints (Fig. 1). The included studies represented a total of 458,754 hospital HCWs across 58 countries (refer to S3A and S3B Appendices for study characteristics). Overall, five DSM-V mental health disorder were identified and reported by the included studies: depression, anxiety, PTSD, insomnia, and alcohol or substance use disorder (A/SUD). Two studies used diagnostic interviews, and the rest used validated self-report measurement tools and validated cut-offs that reflected a probable mental health disorder (refer to S3C Appendix for details on measurement tools used by studies and the corresponding cut-offs, sensitivity and specificity).
Fig. 1.
PRISMA flowchart.
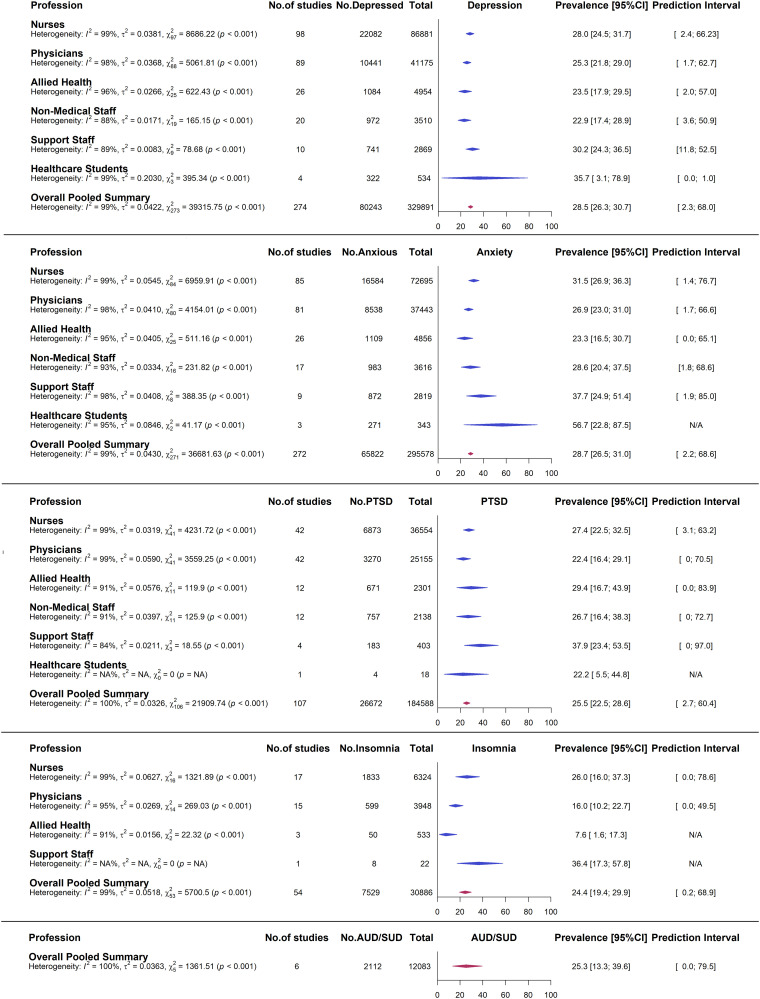
A summary of overall pooled estimates is displayed in Fig. 2 (details in S4A to S8A Appendices). Overall meta-analytic pooling of individual estimates yielded an overall summary estimate of 28.5 % for depression (95 % CI: 26.3 %–30.7 %), 28.7 % for anxiety (95 % CI: 26.5 %–31.0 %), 25.5 % for PTSD (95 % CI: 22.5 %–28.6 %), 24.4 % for insomnia (95 % CI: 19.4 %–29.9 %) and 25.3 % for A/SUD (95 % CI: 13.3 %–39.6 %). In all estimates heterogeneity was high ( = 99 %–100 %) and significant (p < 0.001), and prediction intervals were wide. Studies conducted in China accounted for the most weight in all the estimates (24.3 % to 25.4 %), followed by studies conducted in the United States (5.6 % to 16.9 %) (See S4B to S8B Appendices for prevalence rates estimated for the 58 countries).
Fig. 2.
Forest plot of overall and stratified pooled prevalence estimates by individual professions.
3.2. Subgroup analysis by study level characteristics
Subgroup analyses were conducted by measurement tools and WHO regions when there were more than four studies in each subgroup (Fig. 3). Due to the lack of studies, subgroup analysis by measurement tools and region could not be conducted for A/SUD pooled rates. The test for subgroup differences showed statistically significant differences between estimates produced by the different measurement tools used for depression (=56.7, df = 6, p < 0.001), anxiety (=95.7, df = 5, p < 0.001), PTSD (=21.7, df = 5, p < 0.001) and insomnia (=47.9, df = 1, p < 0.001).
Fig. 3.
Forest plot of subgroup analysis by study level characteristics.
In terms of WHO regions, results showed statistically significant differences between the WHO regions' overall pooled prevalence rates for depression (=29.1, df = 5, p < 0.0001), anxiety (=43.8, df = 5, p < 0.0001) and PTSD (=11.3, df = 3, p = 0.01).
3.3. Subgroup analysis by risk of bias
A summary of the overall risk of bias is displayed in Fig. 4. There was low risk of bias in the sample frames used by 174 datasets (44 %), sampling methods used by 140 datasets (36 %), study's sample size in 259 datasets (66 %), study details reported in 342 datasets (87 %), subgroup coverage in 14 datasets (4 %), consistency in measurement across participants in 392 datasets (100 %), statistical calculation of prevalence rates in 350 datasets (89 %) and for response rate in 61 datasets (16 %) (details in S3A Appendix, S3B Appendix, S3C Appendix Appendices). Overall, the studies show a mixed risk of bias across the results, with low risk of bias to accuracy and precision of the results but higher risk towards generalisability and representation of overall hospital HCW population. In the subgroup analysis, test of subgroup differences found no significant differences between estimates by JBI risk of bias criteria except for sample size, which significantly influenced depression (=11.6, df = 1, p < 0.001), anxiety (=14.5, df = 1, p = 0.0001), PTSD (=7.41, df = 1, p < 0.01) and insomnia (=5.1, df = 1, p = 0.02) rates (Fig. 5).
Fig. 4.
Risk of bias summary.
Fig. 5.
Forest plot of subgroup analysis by JBI risk of bias criteria.
3.4. Prevalence estimates stratified by professional characteristics
A summary of pooled prevalence rates for all outcomes among individual professions are displayed in Fig. 2. Results show that the pooled prevalence rates of depression was similar among nurses (28.0 %, 95 % CI: 24.5 %–31.7 %) and support staff (30.2 %, 95 % CI: 24.3 %–36.5 %), which was higher than physicians (25.3 %, 95 % CI: 21.8 %–29.0 %), allied health (23.5 %, 95 % CI: 17.9 %–39.5 %) and non-medical staff (22.9 %, 95 % CI: 17.4 %–28.9 %), but was lower than healthcare students (35.7 %, 95 % CI: 3.1 %–78.9 %) (S4C to H Appendix).
In terms of pooled anxiety rates, it was most prevalent among healthcare students (56.7 %, 95 % CI: 22.8 %–87.5 %), followed respectively by support staff (37.7 %, 95 % CI: 24.9 %–51.4 %), nurses (31.5 %, 95 % CI: 26.9 %–36.3 %), physicians (26.9 %, 95 % CI: 23.0 %–31.0 %), non-medical staff (28.6 %, 95 % CI: 20.4 %–37.5 %) and allied health (23.3 %, 95 % CI: 16.5 %–30.7 %) (S5C to H Appendix).
PTSD was most prevalent in support staff (37.9 %, 95 % CI: 23.4 %–53.5 %), followed by allied health (29.4 %, 95 % CI: 16.7 %–43.9 %), nurses (27.4 %, 95 % CI: 22.5 %–32.5 %), non-medical staff (26.7 %, 95 % CI: 16.4 %-38.3 %), physicians (22.4 %, 95 % CI: 16.4 %–29.1 %) and healthcare students (22.2 %, 95 % CI: 5.5 %–44.8 %) (details in S6C to H Appendix).
Insomnia pooled prevalence rate was highest in support staff (36.4 %, 95 % CI: 17.3 %–57.8 %), followed by nurses (26.0 %, 95 % CI: 16.0 %–37.3 %), physicians (16.0 %, 95 % CI: 10.2 %–22.7 %) and lowest in allied health (7.6 %, 95 % CI: 1.6 %–17.3 %) (details in S7C to H Appendix).
No studies reported A/SUD rates by different professions.
Heterogeneity was high and significant for all estimates ( = 84 %–99 %, p < 0.001). Prediction intervals were all wide and predicted wide ranges of pooled rates, indicating highly varied predicted rates.
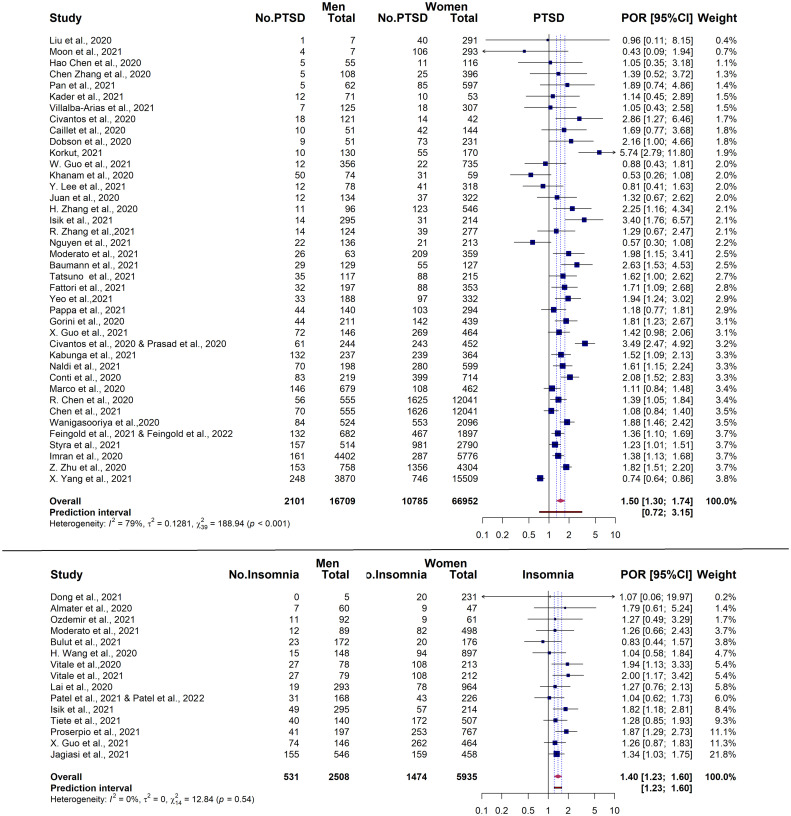
3.5. Odds ratio comparing prevalence rates of probable mental health disorders in Hospital HCWs working in high and low risk units
When comparing prevalence rates between hospital HCWs working in high risk and low risk department, high risk units had significantly higher pooled ORs for depression (OR = 1.35, no. studies = 19, 95 % CI: 1.04–1.76, t = 2.39, p = 0.03), anxiety (OR = 1.38, no. studies = 17, 95 % CI: 1.11–1.73, t = 3.12, p < 0.01), PTSD (OR = 1.59, no. studies = 12, 95 % CI: 1.26–2.02, t = 4.32, p < 0.01), and insomnia (OR = 1.33, no. studies = 4, 95 % CI = 1.06–1.66, t = 3.99, p = 0.03) (Fig. 6). There were no study reporting AUD rates by high or low risk units.
Fig. 6.
Forest plot of odds ratio comparing the prevalence of probable mental health disorders in Hospital HCWs working in high risk and low risk units.
Heterogeneity was high ( > 75 %) and significant (p < 0.001) for depression and anxiety estimates comparing high and low risk units. Heterogeneity was moderate but significant for PTSD ( = 62 %, p < 0.01), whereas it was low and not significant for insomnia OR ( = 0 %, p = 0.68). All prediction intervals predicted wide ranges of ORs and predicted non-significant effects in future estimates.
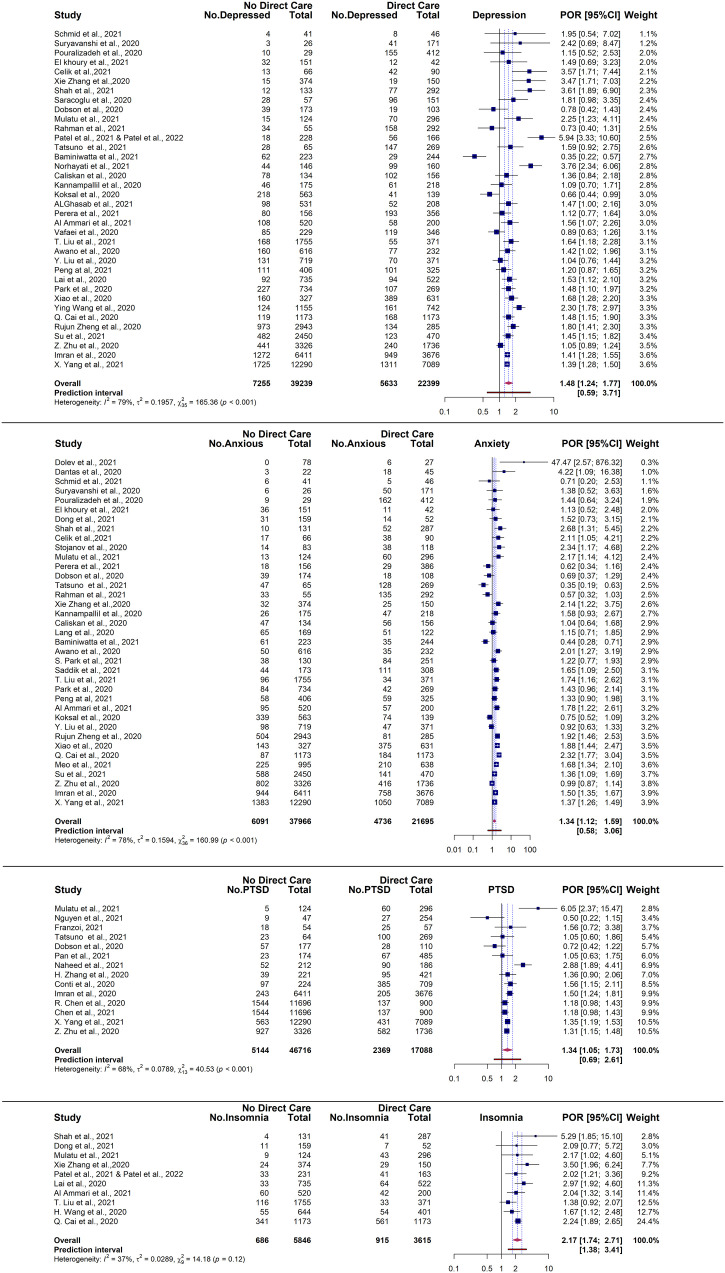
3.6. Odds ratio comparing prevalence rates of probable mental health disorders in Hospital HCWs providing direct care to COVID-19 patients and those who do not
When comparing prevalence rates between Hospital HCWs who provide direct care and those who do not, those who provided direct care had significantly higher pooled ORs for depression (OR = 1.48, no. studies = 36, 95 % CI: 1.24–1.77, t = 4.55, p < 0.0001), anxiety (OR = 1.34, no. studies = 37, 95 % CI: 1.12–1.59, t = 3.38, p < 0.01), PTSD (OR = 1.34, no. studies = 14, 95 % CI: 1.05–1.73, t = 2.56, p = 0.02) and insomnia (OR = 2.17, no. studies = 10, 95 % CI: 1.74–2.71, t = 7.90, p< 0.0001) (Fig. 7). There was significant and high heterogeneity in OR estimates for depression and anxiety ( = 78 %–79 %, p < 0.001). Heterogeneity was moderate but significant for PTSD ( = 68 %, p < 0.001), while insomnia pooled OR was not significantly heterogeneous and moderate (p = 0.12, = 37 %). Prediction intervals for all OR estimates predicted non-significant effects, with the exception of insomnia, which had prediction intervals between 1.38 and 3.41.
Fig. 7.
Forest plot of prevalence odds ratio comparing the prevalence of probable mental health disorders in Hospital HCWs providing direct care and no direct care.
3.7. Odds ratio comparing prevalence rates of probable mental health disorders in men and women
When evaluating the OR for gender, pooled estimates show that women had significantly higher prevalence of depression (OR = 1.40, no. studies = 79, 95 % CI: 1.26–1.56, t = 6.34, p < 0.0001), anxiety (OR = 1.50, no. studies = 70, 95 % CI: 1.29–1.74, t = 5.47, p < 0.0001), PTSD (OR = 1.50, no. studies = 40, 95 % CI: 1.30–1.74, t = 5.55, p < 0.0001), and insomnia (OR = 1.40, no. studies = 15, 95 % CI: 1.23–1.60, t = 5.54, p < 0.0001).
As seen in Fig. 8, there was significant and high heterogeneity (p < 0.01, > 77 %) between studies in all estimates except insomnia OR, where it was low and not significant (p = 0.54, = 0 %). Prediction intervals did not predict significantly higher rates of depression, anxiety and PTSD but predicted significantly higher rates of insomnia for women in future estimates.
Fig. 8.
Forest plot of prevalence odds ratio comparing the prevalence of probable mental health disorders in women and men.
3.8. Sensitivity analysis
In the overall pooled estimates, removal of influential outliers did not change any estimates by 4.7 % and heterogeneity remained high (I^2 = 99 %) and significant (p < 0.001).
In the stratified analysis for individual professions, with the exception of healthcare students' pooled depression rates, removing outliers had no substantial or significant influence on pooled rates or their heterogeneity, with estimates differing by 3.1 % at most and heterogeneity remaining high and significant (I^2 = 85.0 %-99.2 %, p < 0.001). With regards to healthcare students, removing the one outlier decreased pooled depression rates by 19.3 %. The remaining three studies had a combined pooled rate of 16.4 % (95 % CI 6.6 %–29.3 %) but heterogeneity remained high and significant ( = 82.3 %, p < 0.001), indicating that the high original pooled rates may be dependent on one study.
In the odds ratio analysis comparing prevalence rates between high risk and low risk units, one influential outlier was detected for insomnia OR but when removed did not change the significance of the effect, the overall effect size, and heterogeneity (OR = 1.40, no. studies = 3, 95 % CI = 1.14–1.72, t = 6.95, p = 0.02). No influential outliers were detected in depression, anxiety, and PTSD OR estimates.
No influential outliers were detected for any direct care OR estimates.
When influential outliers were removed in the OR estimates for gender, significance, effect size and prediction intervals were not affected substantially in depression (OR = 1.43, no. studies = 78, 95 % CI: 1.31–1.56, t = 8.20, p < 0.0001), anxiety (OR = 1.53, no. studies = 68, 95 % CI: 1.38–1.69, t = 8.24, p < 0.0001) and insomnia (OR = 1.42, no. studies = 14, 95 % CI: 1.21–1.65, t = 4.82, p < 0.001). Heterogeneity remained significant but was reduced to a moderate level in depression (p < 0.0001, I^2 = 73.5 %) and anxiety estimates (p < 0.0001, I^2 = 71.3 %), which suggests that the high heterogeneity in the original estimate may be a result of extreme outliers. Heterogeneity in insomnia OR estimates remained low and non-significant (p = 0.47, I^2 = 0 %).
3.9. Publication bias
There was significant publication bias detected in the overall prevalence estimates for depression (Egger's test: p < 0.001), anxiety (Egger's test: p < 0.001) and PTSD (Egger's test: p < 0.001) (funnel plots displayed in S9 Appendix), with smaller studies producing higher prevalence rates. No publication bias was detected for insomnia (Egger's test: p = 0.40) and AUD/SUD (Egger's test: p = 0.12).
3.10. Longitudinal COVID-19 studies
18 datasets conducted in 11 countries during COVID-19 reported the prevalence of probable mental health disorders across different timepoints (details in S10 Appendix) (Algattas et al., 2021; Baumann et al., 2021; Cai et al., 2020; Castioni et al., 2021; Chene et al., 2021; De Kock et al., 2022; Doulias et al., 2021; Gündoğmuş et al., 2021; Katsuta et al., 2021; Lasalvia et al., 2021; Lasalvia et al., 2020; Li et al., n.d.; Magnavita et al., 2021a, Magnavita et al., 2021b; Magnavita et al., 2020; Moore et al., 2021; Mosolova et al., 2021; Noaimi et al., 2021; Schmid et al., 2021; Shechter et al., 2021; Th'ng et al., 2021). Due to the variation in timepoints, differences in context, and the small number of studies, the temporal relationship between prevalence rates of mental health outcomes and the COVID-19 pandemic were narratively synthesised to avoid combining quantitative data inappropriately.
Two studies (Katsuta et al., 2021; Moore et al., 2021) compared pre-pandemic rates with COVID-19 rates in hospital HCWs. One study (Katsuta et al., 2021) (n- 1 = 2529, n-T2 = 2501) found no significant difference in the prevalence of depression pre-pandemic and during the COVID-19 pandemic among hospital HCWs. Similar results were found for the prevalence of anxiety in Moore et al. (2021) study among medical students (n-T1 = 3775, n-T2 = 836), which found no significant difference in both timepoints.
Eight datasets from 11 studies (Baumann et al., 2021; De Kock et al., 2022; Lasalvia et al., 2021; Lasalvia et al., 2020; Magnavita et al., 2021a, Magnavita et al., 2021b; Magnavita et al., 2020; Noaimi et al., 2021; Schmid et al., 2021; Shechter et al., 2021; Th'ng et al., 2021), investigated the progression of mental health outcomes across different timepoints as part of follow up assessments. One study (Shechter et al., 2021) followed participants (T1 to T6-n = 230) over six timepoints over 10 weeks. They found that the high prevalence of PTSD found during baseline decreased by 34.9 % over the first five timepoints but did not decrease further in the last timepoint. In another study (Baumann et al., 2021) with emergency department (ED) physicians (n-T1 = 262, n-T2 = 252), PTSD also decreased after two months but at a lower rate of 7 %. With regards to depression, the prevalence of depression significantly increased by 11.4 % over 8 months in one dataset (Magnavita et al., 2021a, Magnavita et al., 2021b; Magnavita et al., 2020) (n-T1 = 180, n-T2 = 152, n-T3 = 120), and 14 % over 12 months in another (Lasalvia et al., 2021; Lasalvia et al., 2020) (n-T1 = 2195, n-T2 = 917). In four other datasets (De Kock et al., 2022; Noaimi et al., 2021; Schmid et al., 2021; Th'ng et al., 2021), with an average follow up duration of 8.5 months (2–13 months), the prevalence of depression did not significantly change from baseline and remained high. In terms of the prevalence of anxiety, five datasets (De Kock et al., 2022; Magnavita et al., 2021a, Magnavita et al., 2021b; Magnavita et al., 2020; Noaimi et al., 2021; Schmid et al., 2021; Th'ng et al., 2021) with an average follow up duration of 8 months (2–13 months), showed that it remained similar to baseline rates. Only one dataset (Magnavita et al., 2021a, Magnavita et al., 2021b; Magnavita et al., 2020) reported on the prevalence of insomnia (n-T1 = 180, n-T2 = 152, n-T3 = 120), which showed significantly lower prevalence of insomnia after eight months.
Two studies reported prevalence rates of probable mental health disorders before and one month after COVID-19 outbreaks in their local area (Cai et al., 2020; Doulias et al., 2021). In Cai et al. (2020) study, they investigated two separate samples of nurses (n-T1 = 709, n-T2 = 621) recruited from the same sample frame in the two different timepoints. Their results show that the prevalence of depression, anxiety, and PTSD had a significant decrease after the outbreaks, but insomnia remained similar to baseline rates. Doulias et al. (2021) had similar results in their repeated measures study (n-T1: 93, n-T2: 103) with regards to the prevalence of depression and anxiety, showing a large decrease in prevalence rates of both outcomes.
One study (Li et al., n.d.) looked at hospital nurses' (T1 & T2-n = 356) levels of PTSD symptoms assessed before and after they worked in the COVID-19 units. Results showed that there was a significant and large increase in the prevalence of clinically significant PTSD symptoms after they have worked in COVID-19 units.
One study (Algattas et al., 2021) with a small sample of neuropsychology residents (n = 17) found that the prevalence of depression during a COVID-19 outbreak was significantly lower than rates found before the outbreak.
Two repeated measures study (Gündoğmuş et al., 2021; Mosolova et al., 2021) compared prevalence rates during the peaks of the first and second COVID-19 outbreak in their local area. One study (Gündoğmuş et al., 2021) (n-T1: 1051, n-T2: 1409) reported that depression and anxiety prevalence rates among hospital HCWs was significantly higher during the second wave of COVID-19 outbreak compared to the first wave. This was consistent with Mosolova et al. (2021) study (n-T1: 1090, n-T2: 1105), which showed a significant increase in the prevalence of anxiety in the second wave of COVID-19.
Two studies (Castioni et al., 2021; Chene et al., 2021) compared prevalence rates before and after lockdown measures were implemented in their local area. Chene et al. (2021) results (n-T1: 1565, n-T2: 1109) showed that after lockdown, no significant changes were observed in the prevalence of depression and anxiety. Consistent with this, Castioni et al.'s (2021) result (n = 272) showed that the prevalence of anxiety remained the same but the prevalence of depression significantly increased after lockdown.
4. Discussion
To estimate the impact of the COVID-19 pandemic on hospital HCWs mental health, this study systematically reviewed the literature and conducted a meta-analysis of studies reporting on probable mental health disorders in hospital HCWs. The results from this study's meta-analysis of 392 datasets during the COVID-19 pandemic suggest that a substantial proportion of hospital HCWs working during COVID-19 experienced clinically significant symptoms of depression (28.5 %), anxiety (28.7 %), PTSD (25.5 %), insomnia (24.4 %), and A/SUD (25.3 %). Notably, this is the first review, to the authors' knowledge, to shed light on the high rates of A/SUD in hospital HCWs. While A/SUD research among hospital HCWs is still limited, likely due to the impacts of stigma and professional concerns with their participation in A/SUD studies, these findings have nonetheless highlighted a clear need for further research on A/SUD in hospital HCWs. With regards to published findings on other mental health outcomes, preliminary estimates from early reviews on hospital HCWs have widely varied (X. Li et al., 2021; Raoofi et al., 2021; Salari et al., 2020a; Salari et al., 2020b), likely due to the differences in the number of studies, sample size and methodology. Nonetheless, overall findings from this study echo those from these previous reviews, that the prevalence of mental health issues in hospital HCWs is high and concerning. In addition, findings from this study have provided an updated and more precise estimate of the overall estimated prevalence of mental health issues being experienced by hospital HCWs during COVID-19, which has remained high even with newer studies, additional countries, a substantially larger sample size and the addition of clinically significant thresholds. Given these findings and the ongoing nature of the COVID-19 pandemic, it is evident that support is imminently needed to prevent, reduce, and treat these clinically significant symptoms of mental health disorders found in hospital HCWs working during COVID-19.
When compared to the most recent estimates for the general public (GP) during COVID-19, our findings indicate that hospital HCWs overall had a higher prevalence of depression (HCWS: 28.5.0 % vs GP: 22.6 %) and anxiety (HCWS: 28.7 % vs GP: 22.4 %) (Phiri et al., 2021). This is not surprising given the increases in workloads, infection risks, uncertainty, and feelings of threat during the pandemic (Ding et al., 2021; Joo and Liu, 2021; Liu et al., 2020), which may have increased the likelihood of developing depression and anxiety in hospital HCWs during this time. The same, however, could not be said about the prevalence rates of PTSD (HCWs: 25.5 % vs GP: 23.2 %) and insomnia (HCWS: 24.4 % vs GP: 22.9) in hospital HCWs, which have been comparable to the general public (Phiri et al., 2021). Given these findings it cannot be disregarded that the prevalence of mental health issues in hospital HCWs, such as PTSD and insomnia, may be explained partly, if not fully, by distressing experiences in the community that have been associated with mental health issues during the COVID-19 pandemic, such as the risk of infections in the community, lockdowns, quarantines, impacts on families and social distancing (Brooks et al., 2020; Sheen et al., 2022; Yuan et al., 2021). Thus, when developing mental health support strategies for hospital HCWs it is important to consider the impact of a pandemic across the different domains of their lives as well as the direct impacts of their healthcare roles.
When interpreting findings, it is also important to recognise there was high heterogeneity in the overall estimates, which is common to meta-analyses of prevalence and consistent with previous reviews (X. Li et al., 2021; Raoofi et al., 2021; Salari et al., 2020a; Salari et al., 2020b). To further investigate the extent of this heterogeneity, prediction intervals were estimated, providing insight into the distribution and predicted range of future estimates (Barker et al., 2021; Borenstein et al., 2017). Our analysis identified wide ranges of predicted prevalence rates that indicate, while on average there may be a high prevalence of probable mental health disorders in hospital HCWs during the COVID-19 pandemic, it is likely that prevalence rates vary substantially between different settings, groups, or study design. In our findings, sample size and publication bias were both found to significantly affect effect sizes. Both factors showed that higher risk and smaller studies were more likely to find a higher average in prevalence rates. Prevalence estimates were also found to significantly differ between different WHO regions and measurement tools, which is likely explained by the national differences in COVID-19's spread and responses, and the considerable differences in optimal specificity and sensitivity in the measurement tools used (S2 Appendix). As such, it is important to consider these factors when interpreting findings. However, while these factors may impact findings, there is low certainty they had a large and significant impact as there were still large amounts of unexplained heterogeneity in respective subgroup analyses. Another important factor to consider when interpreting findings is clinical heterogeneity (e.g., participant characteristics) which our findings indicate could also explain differences in outcomes given consistent findings within specific subgroup estimates.
4.1. Healthcare professions
When analysed by healthcare professions, findings demonstrate that clinical symptoms of depression, anxiety, PTSD, and insomnia were highly prevalent across all studied healthcare professions. There were, however, variations in prevalence rates of different mental health outcomes among different professions, suggesting that different professions may be susceptible to different mental health impacts. In terms of depression only physicians, nurses, support staff and healthcare students had higher rates than estimates for the general public (Phiri et al., 2021). With regards to physicians, hospital nurses and healthcare students, pre-pandemic studies largely supports that mental health issues have been evident in this cohort since pre-pandemic (Chen and Meier, 2021; Dyrbye et al., 2006; Gheshlagh et al., 2017; Rotenstein et al., 2016; Tung et al., 2018; Xie et al., 2020). This is has been attributed to their high workload, work-related stress and high levels of burnout associated with their work (Almutairi et al., 2022; Chen and Meier, 2021; Koutsimani et al., 2019). This makes it unclear to what extent pandemic factors alone have affected their rates of depression symptoms while working in hospitals during this time. Nevertheless, it is likely that pandemic factors exacerbated their existing vulnerabilities, placing them at a higher risk of developing depression symptoms during the COVID-19 pandemic. In contrast, support staff and other healthcare professionals have largely been left out of pre-pandemic research. This is concerning given that translating evidence from other professions may not be effective due to the differences in work related stress, roles, and tasks. Based on these findings it is recommended that further research examine profession specific factors that may be influencing the prevalence of depression symptoms in hospital HCWs to support further development of targeted mental health support strategies within hospital systems.
With regards to findings on anxiety, there is little pre-pandemic research indicating this was a pre-existing issue for hospital HCWs overall, suggesting that the high rates of anxiety found in this study may be explained by pandemic factors. This is affirmed by the literature showing that sources of anxiety in hospital HCWs during coronavirus outbreaks, including COVID-19, largely revolves around nosocomial infection risks, such as fear of being infected (De Brier et al., 2020; Serrano-Ripoll et al., 2020), fear of infecting others (i.e., family and community members) (Barello et al., 2020; Kisely et al., 2020), and PPE adequacy (Kisely et al., 2020; Troglio Da Silva and Neto, 2021). The trends in our findings also support this pattern of anxiety, showing the highest rates of anxiety in nurses, physicians, support staff and healthcare students, all of whom have patient facing intensive roles and thus more risks of infection. In contrast, allied health staff who have less patient contact, such as pharmacists and lab technicians, were found to have the lowest rates of anxiety, comparable to rates found in the general public (Phiri et al., 2021). Of note, non-medical staff had higher rates of anxiety than the general public even though they were likely to have little patient contact. This could be a reflection of their lack of specialised training and experience, which have been suggested to increase worries of infections and mental health issues during coronavirus outbreak (De Brier et al., 2020; Kisely et al., 2020). This re-emphasises the need for healthcare organisations to incorporate strategies that help all hospital HCWs feel safe during this time. Though, it is important to note that concerns around high infection risks among HCWs were raised in the early stages of COVID-19 (Erdem and Lucey, 2021) and infection risks may have reduced with improvements in the healthcare system over the course of the COVID-19 pandemic. Early evidence from the United States have demonstrated that HCWs' risk of infection in the workplace have reduced as hospitals improve their infection control procedures, PPE use and vaccination rates (Braun et al., 2021; Damluji et al., 2021; Dunbar et al., 2021; Jacob et al., 2021; Moghadas et al., 2021). While new variants of COVID-19 may create a resurgence of infections again, it is not certain whether these high anxiety rates persist, and if they do, whether nosocomial infection risks still play a significant role. Nevertheless, given that anxiety symptoms can be a precursor to depression (Batterham et al., 2013), support strategies will still benefit from focusing on reducing anxiety symptoms in addition to depression symptoms to reduce the overall high rates of mental health issues in hospital HCWs during the COVID-19 pandemic and future infectious disease outbreaks.
With PTSD findings, interpretation needs to consider that findings may not be reflective of post-traumatic stress reactions but rather hospital HCWs' ongoing and acute experiences with traumatic stress as assessment of symptoms in included studies largely occurred during outbreaks which doesnt account for delayed onset of PTSD symptoms. In the findings, while overall rates of PTSD in hospital HCWs were similar to those in the general public, nurses, allied health, non-medical staff and support staff were more likely to experience PTSD symptoms than the general public (Phiri et al., 2021). Again, infection risks may be playing an important role here, however, indirectly. Due to increased infection risks, rates of quarantine have been significantly higher in hospitals HCWs compared to the general public (Kumar et al., 2020) and have been found to be associated with PTSD symptoms (Brooks et al., 2020; Brophy et al., 2020; Carmassi et al., 2020). While an effective measure to reduce nosocomial outbreaks of COVID-19 in hospitals (Grzelakowska and Kryś, 2021; Huang et al., 2021), studies have demonstrated that quarantine procedures can have severe psychological impact due to feelings of threat, restrain and social isolation (Basso et al., 2021; Brooks et al., 2020; Gómez-Durán et al., 2020). These were likely intensified as hospital HCWs face repeated quarantine and its' consequences due to their work in hospitals. Another contributing factor could be the social stigma and social rejection (Ding et al., 2021; Gómez-Durán et al., 2020; Schubert et al., 2021; Yuan et al., 2021) faced by these professional groups due to their work, which have been found to increase experiences of PTSD symptoms (Yuan et al., 2021). Nurses, allied health, non-medical staff and support staff may have been exposed more frequently to these negative social experiences given their increased contact with patients and the public outside of clinical activities.
4.2. Frontline setting
In addition to professional differences, it is also important to consider the impacts of occupational factors on hospital HCWs' mental health, such as working in high-risk units and providing direct care to infected patients. Our findings suggest that both these factors have led to significantly higher odds of developing depression, anxiety, PTSD and insomnia symptoms compared to their counterparts, with highly consistent evidence for insomnia and moderately consistent for PTSD. Overall, these findings re-enforce that proximity to risk is likely to be a determinant of distress during traumatic events (May and Wisco, 2016) and highlights the need for strategies and interventions to support these at-risk groups during the COVID-19 pandemic and in future infectious disease outbreaks. However, while these findings affirm those from previous coronavirus outbreaks (De Brier et al., 2020; Kisely et al., 2020; Preti et al., 2020; Serrano-Ripoll et al., 2020), it has contradicted recent results from a living meta-analysis (Bell and Wade, 2020) that have shown exposure to COVID-19 patients do not significantly increase risk of PTSD. This could likely be a result of conflating hospital HCWs with general HCWs and severe symptoms with mild in their meta-analysis (Bell and Wade, 2020) and thus increasing the rates of PTSD symptoms in their non-exposed group, leading to a non-significant effect. This suggests that the effect found in our meta-analysis may only be reflective of those working in hospitals and PTSD symptoms that are at a clinically significant threshold. Nevertheless, our overall findings still echoes Bell and Wade's (Bell and Wade, 2020) recommendations that trauma focused support may not be a pertinent focus in pandemic responses in the overarching healthcare system. When we look at the overall impact on PTSD symptoms in hospital HCWs, there is some basis to their recommendations as overall rates are comparable to the general public, which may mean that reducing traumatic stress during COVID-19 would be more effective on a national level and will likely have a significant cascading effect in reducing traumatic stress in hospital HCWs overall. Within the healthcare system our findings suggest that trauma focused support, such as psychological first aid (Ruzek et al., 2007), may instead be more appropriate for specific groups at-risk due to their profession or proximity to infection risks, as opposed to a macro level response from healthcare organisations.
4.3. Gender
Attention should also be given to hospital HCWs who are women. Our findings clearly indicate they have been impacted more than men across multiple outcomes, with consistent evidence in regard to insomnia and with the exception of extreme cases, depression, and anxiety. However, while this supports evidence from previous coronavirus outbreaks (Carmassi et al., 2020; Kisely et al., 2020; Serrano-Ripoll et al., 2020), and the COVID-19 pandemic (Batra et al., 2020; Zhao et al., 2021), it is again unclear to what extent working in hospitals and pandemic factors are impacting their mental health. It is well documented that women make up a large proportion of the healthcare workforce, such as nurses (World Health Organisation, 2020) who have been implicated to have higher rates of mental health issues in this study's findings and may explain women's higher likelihood of experiencing mental health issues. In addition, the mental health of women has also been found to be impacted more in the general public during pandemics (Xiong et al., 2020) and out of pandemics (Wang et al., 2016). Nonetheless, while it is not certain that the hospital system or pandemic factors are the main causal factor, pandemic factors likely played a significant role in exacerbating existing mental health vulnerabilities among hospital HCWs who are women. It is also important to note that findings have rejected that biological vulnerabilities, such as hormones, explain the gender differences in mental health outcomes (Wang et al., 2016), which underscores the importance of examining and addressing social factors that are influencing disparities in mental health outcomes between men and women working in hospitals.
4.4. Long term mental health trajectories
Turning to longitudinal trends, findings were weak due to paucity of research, but they suggested that probable mental health disorders were most prevalent in hospital HCWs leading into and during an outbreak but decreased after outbreaks. Similar findings have been identified among the general public during COVID-19 (Bourmistrova et al., 2022; Robinson et al., 2022), showing rates of mental health issues decreasing as the COVID-19 pandemic progressed, implying that acute mental health responses are likely to be more severe than long-term mental health responses. Though, despite the decrease, prevalence rates remained at concerning rates and persisted among hospital HCWs over time. Previous findings suggest that this particularly occurs for those working in high-risk settings that may be at risk of long-term mental health issues after infectious disease outbreaks (Chau et al., 2021). Given these findings, mental health strategies should consider strategies to mitigate any long-term impacts. Longitudinal findings from a small number of studies, also supports that pre-pandemic mental health issues were likely present and translated into higher mental health risks during the COVID-19 pandemic. This highlights the importance of long-term strategies to address systemic issues that have left hospital HCWs vulnerable to mental health issues during traumatic events such as infectious disease outbreaks. Given these findings and the low certainty in findings due to a paucity in longitudinal research, follow-up research is recommended, specifically on those who are at higher risk, such as those providing direct care to COVID-19 patients and HCWs working high risk departments.
4.5. Limitations
While this review has attempted to strengthen confidence when interpreting findings using conservative methodology, it is not without its limitations. First, the findings are only as robust as the studies included, which have mostly used self-report measures, reducing the certainty that estimates truly reflect mental health diagnoses. However, we have minimised uncertainty with this by only including studies that use measurement tools and cut offs that have been validated against diagnostic interviews. While not reflective of actual mental health diagnoses, our findings still show for the first time the proportion of hospital HCWs experiencing mental health issues at a clinical level that have a high probability to lead to a mental health disorder, if not present already, and requires immediate clinical assessment (Bressler et al., 2018; Kroenke et al., 2007; Nieuwenhuijsen et al., 2003).
It also cannot be rejected that studies were missed in the selection process. Due to the lack of multilingual reviewers in this study, non-English studies were not included. In addition, not all studies were screened twice, however, evidence suggests that partial dual screening can still be an acceptable procedure (Taylor-Phillips et al., 2017; Waffenschmidt et al., 2019). Despite these limitations, our review with 401 studies is the most comprehensive to date on mental health outcomes of hospital HCWs during COVID-19. As such, there is very low risk of missing studies significantly impacting results.
5. Conclusion
In sum, findings are overall still emerging and there is growing certainty in the evidence to suggest that there are specific groups of hospital HCWs at higher risk of mental health issues. Thus, it is certain that further research is needed to inform the development of mental health support strategies that are targeted. This is especially true for those outside of the nursing and physician professions, such as allied health, non-medical and support staff in hospital settings, where there is a lack of evidence to effectively rely on. At this time, findings also highlight that those working in direct proximity of COVID-19 patients, working in high-risk units and women hospital HCWs are at significant risk of mental health issues and should be a priority in staff support within hospitals. More importantly, with re-occurring outbreaks from new COVID-19 variants, mental health issues in hospital HCWs may continue to persist and should not be neglected. As such, we echo the many pervious calls for further research, and development of effective interventions and initiatives to support hospital HCWs as they continue to support their communities while facing the many challenges of the COVID-19 pandemic.
The following are the supplementary data related to this article.
Prisma checklist.
Methods supplement.
Summary table of study characteristics.
Included studies references.
Measurement tools and cut off scores.
Depression forest plots.
Anxiety forest plots.
PTSD forest plots.
Insomnia forest plots.
AUD forest plot.
Funnel plots.
COVID-19 longitudinal studies summary table.
Funding source
Preparation of this paper was supported using award money from the Victorian COVID-19 Research Fund-Stream B, State Government of Victoria. The funders of this study had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
CRediT authorship contribution statement
Formal analysis, data curation, investigation, writing – original draft: Brian Lee En Chyi
Methodology: Brian Lee En Chyi, Mathew Ling, Leanne Boyd, Jade Sheen
Conceptualization, supervision, writing – review & editing: Mathew Ling, Leanne Boyd, Craig Olsson, Jade Sheen.
All authors have contributed and approved the final manuscript.
Conflict of interest
The authors declare that there is no conflict of interest.
Acknowledgements
The authors would like to acknowledge and thank Dawson Peter Grace, Mikhayl von Riebon, Gayatri Kumar, Caitlyn Ann Herrick, Hiba Sidiqui, Anuradhi Jayasinghe and Britney Dellios for their assistance with screening, data extraction and data checking.
References
- Algattas H., Roy S., Agarwal N., Maroon J. COVID-19 impact in neurosurgery residency: grit during pandemic. World Neurosurg. 2021;151:e395–e398. doi: 10.1016/j.wneu.2021.04.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almutairi H., Alsubaiei A., Abduljawad S., Alshatti A., Fekih-Romdhane F., Husni M., Jahrami H. Prevalence of burnout in medical students: a systematic review and meta-analysis. Int. J. Soc. Psychiatry. 2022;68(6):1157–1170. doi: 10.1177/00207640221106691. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association D.-T.F. 5th ed. American Psychiatric Publishing, Inc; Arlington, VA, US: 2013. Diagnostic and Statistical Manual of Mental Disorders: DSM-5™. [Google Scholar]
- Balduzzi S., Rücker G., G S. How to perform a meta-analysis with R: a practical tutorial. Evid. Based Ment. Health. 2019:153–160. doi: 10.1136/ebmental-2019-300117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barello S., Falcó-Pegueroles A., Rosa D., Tolotti A., Graffigna G., Bonetti L. The psychosocial impact of flu influenza pandemics on healthcare workers and lessons learnt for the COVID-19 emergency: a rapid review. Int. J. Public Health. 2020;65:1205–1216. doi: 10.1007/s00038-020-01463-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barendregt J.J., Doi S.A., Lee Y.Y., Norman R.E., Vos T. Meta-analysis of prevalence. J. Epidemiol. Community Health. 2013;67:974–978. doi: 10.1136/jech-2013-203104. [DOI] [PubMed] [Google Scholar]
- Barker T.H., Migliavaca C.B., Stein C., Colpani V., Falavigna M., Aromataris E., Munn Z. Conducting proportional meta-analysis in different types of systematic reviews: a guide for synthesisers of evidence. BMC Med. Res. Methodol. 2021;21:1–9. doi: 10.1186/s12874-021-01381-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basso M., Visintini E., Achil I., Fabris S., Mattiussi E., Danielis M., Palese A. The experience of individuals placed in quarantine: a systematic review, meta-summary, and meta-synthesis. Public Health Nurs. 2021;38:627–636. doi: 10.1111/phn.12910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batra K., Singh T.P., Sharma M., Batra R., Schvaneveldt N. Investigating the psychological impact of COVID-19 among healthcare workers: a meta-analysis. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17239096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batterham P.J., Christensen H., Calear A.L. Anxiety symptoms as precursors of major depression and suicidal ideation. Depress. Anxiety. 2013;30:908–916. doi: 10.1002/da.22066. [DOI] [PubMed] [Google Scholar]
- Baumann B.M., Cooper R.J., Medak A.J., Lim S., Chinnock B., Frazier R., Roberts B.W., Epel E.S., Rodriguez R.M., Mycyk M.B. Emergency physician stressors, concerns, and behavioral changes during COVID-19: a longitudinal study. Acad. Emerg. Med. 2021;28:314–324. doi: 10.1111/acem.14219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell V., Wade D. 2020. Live Meta-analysis: Mental Health of Clinical Staff Working in High Exposure Compared to Low Exposure Roles in High-Risk Epidemic and Pandemic Health Emergencies (Updated 2020.10.04), Open Science Framework. [Google Scholar]
- Borenstein M., Higgins J.P., Hedges L.V., Rothstein H.R. Basics of meta-analysis: I(2) is not an absolute measure of heterogeneity. Res. Synth. Methods. 2017;8:5–18. doi: 10.1002/jrsm.1230. [DOI] [PubMed] [Google Scholar]
- Borenstein M., Higgins J.P.T. Meta-analysis and subgroups. Prev. Sci. 2013;14:134–143. doi: 10.1007/s11121-013-0377-7. [DOI] [PubMed] [Google Scholar]
- Bourmistrova N.W., Solomon T., Braude P., Strawbridge R., Carter B. Long-term effects of COVID-19 on mental health: a systematic review. J. Affect. Disord. 2022;299:118–125. doi: 10.1016/j.jad.2021.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun K.M., Moreno G.K., Buys A., Somsen E.D., Bobholz M., Accola M.A., Anderson L., Rehrauer W.M., Baker D.A., Safdar N., Lepak A.J., O’Connor D.H., Friedrich T.C. Viral sequencing to investigate sources of SARS-CoV-2 infection in US healthcare personnel. Clin. Infect. Dis. 2021;73:e1329–e1336. doi: 10.1093/cid/ciab281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bressler R., Erford B.T., Dean S. A systematic review of the posttraumatic stress disorder checklist (PCL) J. Couns. Dev. 2018;96:167–186. [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brophy J.T., Keith M.M., Hurley M., McArthur J.E. Sacrificed: Ontario healthcare workers in the time of COVID-19. New Solut. 2020;30:267–281. doi: 10.1177/1048291120974358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Z., Cui Q., Liu Z., Li J., Gong X., Liu J., Wan Z., Yuan X., Li X., Chen C., Wang G. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J. Psychiatr. Res. 2020;131:132–137. doi: 10.1016/j.jpsychires.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi C., Foghi C., Dell'Oste V., Cordone A., Bertelloni C.A., Bui E., Dell'Osso L. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. 2020;292 doi: 10.1016/j.psychres.2020.113312. 113312-113312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castioni D., Galasso O., Rava A., Massè A., Gasparini G., Mercurio M. Has the COVID-19 pandemic changed the daily practices and psychological state of orthopaedic residents? Clin. Orthop. Relat. Res. 2021:1947–1954.. doi: 10.1097/CORR.0000000000001728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cénat J.M., Blais-Rochette C., Kokou-Kpolou C.K., Noorishad P.-G., Mukunzi J.N., McIntee S.-E., Dalexis R.D., Goulet M.-A., Labelle P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chau S.W.H., Wong O.W.H., Ramakrishnan R., Chan S.S.M., Wong E.K.Y., Li P.Y.T., Raymont V., Elliot K., Rathod S., Delanerolle G., Phiri P. History for some or lesson for all? A systematic review and meta-analysis on the immediate and long-term mental health impact of the 2002–2003 severe acute respiratory syndrome (SARS) outbreak. BMC Public Health. 2021;21:670. doi: 10.1186/s12889-021-10701-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C., Meier S.T. Burnout and depression in nurses: a systematic review and meta-analysis. Int. J. Nurs. Stud. 2021;124 doi: 10.1016/j.ijnurstu.2021.104099. [DOI] [PubMed] [Google Scholar]
- Chene G., Nohuz E., Cerruto E., Moret S., Atallah A., Saoud M. Psychological impact on healthcare workers in obstetrics and gynecology in France in 18 french university hospitals during the first Covid-19 lockdown: a prospective observational study. J. Psychosom. Obstet. Gynaecol. 2021:1–8. doi: 10.1080/0167482X.2021.2014812. [DOI] [PubMed] [Google Scholar]
- Ching S.M., Ng K.Y., Lee K.W., Yee A., Lim P.Y., Ranita H., Devaraj N.K., Ooi P.B., Cheong A.T. Psychological distress among healthcare providers during COVID-19 in Asia: systematic review and meta-analysis. PLOS ONE. 2021;16 doi: 10.1371/journal.pone.0257983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damluji A.A., Wei S., Bruce S.A., Haymond A., Petricoin E.F., Liotta L., Maxwell G.L., Moore B.C., Bell R., Garofalo S., Houpt E.R., Trump D., deFilippi C.R. Seropositivity of COVID-19 among asymptomatic healthcare workers: a multi-site prospective cohort study from northern Virginia, United States. Lancet Reg. Health Am. 2021;2 doi: 10.1016/j.lana.2021.100030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Brier N., Stroobants S., Vandekerckhove P., De Buck E. Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS & COVID-19): a rapid systematic review. PLOS ONE. 2020;15 doi: 10.1371/journal.pone.0244052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Kock J.H., Latham H.A., Cowden R.G., Cullen B., Narzisi K., Jerdan S., Munoz S.-A., Leslie S.J., McNamara N., Boggon A., Humphry R.W. The mental health of NHS staff during the COVID-19 pandemic: two-wave Scottish cohort study. BJPsych. Open. 2022:8. doi: 10.1192/bjo.2021.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Digby R., Winton-Brown T., Finlayson F., Dobson H., Bucknall T. Hospital staff well-being during the first wave of COVID-19: staff perspectives. Int. J. Ment. Health Nurs. 2021;30:440–450. doi: 10.1111/inm.12804. [DOI] [PubMed] [Google Scholar]
- Ding S., Deng S., Zhang Y., Wang Q., Yang X. 2021. Experiences of Front-Line Medical Staffs Fighting Against Coronavirus Disease 2019: A Meta-Synthesis of Qualitative Studies. [Google Scholar]
- Doulias T., Thrikandiyur A.A., Titus N., Soundararasha K., Coxon A., Amarantidis E., Arulampalam T. Junior doctors’ wellbeing at peak and post-peak pandemic: a repeated cross-sectional study. Ann. R. Coll. Surg. Engl. 2021;105(1):43–51. doi: 10.1308/rcsann.2021.0272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunbar E., Godbout E., Pryor R., Rozycki H.J., Bearman G. Impact of coronavirus disease 2019 (COVID-19) vaccination program on healthcare worker infections in an academic hospital. Infect. Control Hosp. Epidemiol. 2021:1–2. doi: 10.1017/ice.2021.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyrbye L.N., Thomas M.R., Shanafelt T.D. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad. Med. 2006;81 doi: 10.1097/00001888-200604000-00009. [DOI] [PubMed] [Google Scholar]
- Erdem H., Lucey D.R. Healthcare worker infections and deaths due to COVID-19: a survey from 37 nations and a call for WHO to post national data on their website. Int. J. Infect. Dis. 2021;102:239–241. doi: 10.1016/j.ijid.2020.10.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu R., Gartlehner G., Grant M., Shamliyan T., Sedrakyan A., Wilt T.J., Griffith L., Oremus M., Raina P., Ismaila A., Santaguida P., Lau J., Trikalinos T.A. Conducting quantitative synthesis when comparing medical interventions: AHRQ and the effective health care program. J. Clin. Epidemiol. 2011;64:1187–1197. doi: 10.1016/j.jclinepi.2010.08.010. [DOI] [PubMed] [Google Scholar]
- Galli F., Pozzi G., Ruggiero F., Mameli F., Cavicchioli M., Barbieri S., Canevini M.P., Priori A., Pravettoni G., Sani G., Ferrucci R. A systematic review and provisional metanalysis on psychopathologic burden on health care workers of coronavirus outbreaks. Front Psychiatry. 2020;11:1001. doi: 10.3389/fpsyt.2020.568664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gheshlagh R., Parizad N., Dalvand S., Zarei M., Farajzadeh M., Karami M., Sayehmiri K. The prevalence of job stress among nurses in Iran: a meta-analysis study. Nurs. Midwifery Stud. 2017;6:143–148. [Google Scholar]
- Gómez-Durán E.L., Martin-Fumadó C., Forero C.G. Psychological impact of quarantine on healthcare workers. Occup. Environ. Med. 2020;77:666–674. doi: 10.1136/oemed-2020-106587. [DOI] [PubMed] [Google Scholar]
- Grzelakowska K., Kryś J. The impact of COVID-19 on healthcare workers’ absenteeism: infections, quarantines, sick leave — a database analysis of the Antoni Jurasz University Hospital No. 1. in Bydgoszcz, Poland. Med. Res. J. 2021;6:47–52. [Google Scholar]
- Gündoğmuş İ., Ünsal C., Bolu A., Takmaz T., Ökten S.B., Aydın M.B., Uçar H., Gündüz A., Kul A.T. The comparison of anxiety, depression and stress symptoms levels of healthcare workers between the first and second COVID-19 peaks. Psychiatry Res. 2021;301 doi: 10.1016/j.psychres.2021.113976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale T., Angrist N., Hale A.J., Kira B., Majumdar S., Petherick A., Phillips T., Sridhar D., Thompson R.N., Webster S., Zhang Y. Government responses and COVID-19 deaths: global evidence across multiple pandemic waves. PLOS ONE. 2021;16 doi: 10.1371/journal.pone.0253116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrer M., Cuijpers P., Furukawa T., Ebert D. 2019. Doing Meta-Analysis in R: A Hands-On Guide. [Google Scholar]
- Harrer M., Cuijpers P., Furukawa T., Ebert D.D. 2019. dmetar: Companion R Package for the Guide'Doing Meta-Analysis in R', R Package Version 0.0. [Google Scholar]
- Hartung J., Knapp G. On tests of the overall treatment effect in meta-analysis with normally distributed responses. Stat. Med. 2001;20:1771–1782. doi: 10.1002/sim.791. [DOI] [PubMed] [Google Scholar]
- Hartung J., Knapp G. A refined method for the meta-analysis of controlled clinical trials with binary outcome. Stat. Med. 2001;20:3875–3889. doi: 10.1002/sim.1009. [DOI] [PubMed] [Google Scholar]
- Hassan E.M., Mahmoud H.N. Impact of multiple waves of COVID-19 on healthcare networks in the United States. PLOS ONE. 2021;16 doi: 10.1371/journal.pone.0247463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennein R., Lowe S. A hybrid inductive-abductive analysis of health workers’ experiences and wellbeing during the COVID-19 pandemic in the United States. PLOS ONE. 2020;15 doi: 10.1371/journal.pone.0240646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J., Thompson S. Higgins JP, Thompson SGControlling the risk of spurious findings from meta-regression. Stat Med 23(11), 1663–1682. Stat. Med. 2004;23:1663–1682. doi: 10.1002/sim.1752. [DOI] [PubMed] [Google Scholar]
- Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Q., Mondal A., Jiang X., Horn M.A., Fan F., Fu P., Wang X., Zhao H., Ndeffo-Mbah M., Gurarie D. SARS-CoV-2 transmission and control in a hospital setting: an individual-based modelling study. R. Soc. Open Sci. 2021:8. doi: 10.1098/rsos.201895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IntHout J., Ioannidis J.P.A., Borm G.F. The hartung-knapp-sidik-jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med. Res. Methodol. 2014;14:25. doi: 10.1186/1471-2288-14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob J.T., Baker J.M., Fridkin S.K., Lopman B.A., Steinberg J.P., Christenson R.H., King B., Leekha S., O’Hara L.M., Rock P., Schrank G.M., Hayden M.K., Hota B., Lin M.Y., Stein B.D., Caturegli P., Milstone A.M., Rock C., Voskertchian A., Reddy S.C., Harris A.D. Risk factors associated with SARS-CoV-2 seropositivity among US health care personnel. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.1283. e211283-e211283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joo J.Y., Liu M.F. Nurses’ barriers to caring for patients with COVID-19: a qualitative systematic review. Int. Nurs. Rev. 2021;68:202–213. doi: 10.1111/inr.12648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katsuta N., Ito K., Fukuda H., Seyama K., Hori S., Shida Y., Nagura R., Nojiri S., Sato H. Elevated depressive symptoms among newer and younger healthcare workers in Japan during the COVID-19 pandemic. Neuropsychopharmacol. Rep. 2021;41:544–547. doi: 10.1002/npr2.12217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369 doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koutsimani P., Montgomery A., Georganta K. The relationship between burnout, depression, and anxiety: a systematic review and meta-analysis. Front. Psychol. 2019;10 doi: 10.3389/fpsyg.2019.00284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W., Monahan P.O., Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Kumar S.S., Kumar A., Kirtana J., Singh A.K., Shankar S.H., Khan M.A., Srivastava A.K., Kaur R., Wig N. Risk factors and outcome among COVID-19 exposed and quarantined healthcare workers: a study on the status of existing practices of standard precautions. J. Family Med. Prim. Care. 2020;9:5355–5359. doi: 10.4103/jfmpc.jfmpc_1579_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasalvia A., Bodini L., Amaddeo F., Porru S., Carta A., Poli R., Bonetto C. The sustained psychological impact of the COVID-19 pandemic on health care workers one year after the outbreak-a repeated cross-sectional survey in a tertiary Hospital of North-East Italy. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph182413374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasalvia A., Bonetto C., Porru S., Carta A., Tardivo S., Bovo C., Ruggeri M., Amaddeo F. Psychological impact of COVID-19 pandemic on healthcare workers in a highly burdened area of north-East Italy. Epidemiol. Psychiatr. Sci. 2020;30 doi: 10.1017/S2045796020001158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Yu H., Yang W., Mo Q., Yang Z., Wen S., Zhao F., Zhao W., Tang Y., Ma L., Zeng R., Zou X., Lin H. Depression and anxiety among quarantined people, community workers, medical staff, and general population in the early stage of COVID-19 epidemic. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.638985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li et al., n.d., X.C. Li Y. Zhou X.Y. Xu , Factors associated with the psychological well-being among front-line nurses exposed to COVID-2019 in China: a predictive study. J. Nurs. Manag. [DOI] [PubMed]
- Li Y., Scherer N., Felix L., Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: a systematic review and meta-analysis. PLOS ONE. 2021;16 doi: 10.1371/journal.pone.0246454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu M., Zhang N., Wang W., Chen Q., Chen W., Lin Q. Experiences of nurses fighting Coronavirus Disease 2019 (COVID-19): a qualitative meta-integration. Am. J. Nurs. Sci. 2020;9(6):394–401. 2020. [Google Scholar]
- Magnavita N., Soave P.M., Antonelli M. A one-year prospective study of work-related mental health in the intensivists of a COVID-19 hub hospital. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18189888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnavita N., Soave P.M., Antonelli M. Prolonged stress causes depression in frontline workers facing the COVID-19 pandemic-a repeated cross-sectional study in a COVID-19 hub-Hospital in Central Italy. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18147316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnavita N., Soave P.M., Ricciardi W., Antonelli M. Occupational stress and mental health among anesthetists during the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17218245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May C.L., Wisco B.E. Defining trauma: how level of exposure and proximity affect risk for posttraumatic stress disorder. Psychol. Trauma Theory Res. Pract. Policy. 2016;8:233–240. doi: 10.1037/tra0000077. [DOI] [PubMed] [Google Scholar]
- McGowan J., Sampson M., Salzwedel D.M., Cogo E., Foerster V., Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J. Clin. Epidemiol. 2016;75:40–46. doi: 10.1016/j.jclinepi.2016.01.021. [DOI] [PubMed] [Google Scholar]
- Moghadas S.M., Vilches T.N., Zhang K., Wells C.R., Shoukat A., Singer B.H., Meyers L.A., Neuzil K.M., Langley J.M., Fitzpatrick M.C., Galvani A.P. medRxiv : the preprint server for health sciences; 2021. The Impact of Vaccination on COVID-19 Outbreaks in the United States. 2020.2011.2027.20240051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., The P.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- Moore C.J.S., Blencowe N.S., Hollén L., van Hamel C. Interim foundation year one (FiY1) and preparedness for foundation year 1: a national survey of UK foundation doctors. Med. Teach. 2021:1–7. doi: 10.1080/0142159X.2021.2015065. [DOI] [PubMed] [Google Scholar]
- Mosolova E., Sosin D., Mosolov S. Stress, anxiety, depression and burnout in frontline healthcare workers during two peaks of COVID-19 pandemic in Russia. Psychiatry Res. 2021;306 doi: 10.1016/j.psychres.2021.114226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller A.E., Hafstad E.V., Himmels J.P.W., Smedslund G., Flottorp S., Stensland S.Ø., Stroobants S., Van de Velde S., Vist G.E. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munn Z., Moola S., Lisy K., Riitano D., Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int. J. Evid. Based Healthc. 2015;13:147–153. doi: 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- Nieuwenhuijsen K., de Boer A.G.E.M., Verbeek J.H.A.M., Blonk R.W.B., van Dijk F.J.H. The depression anxiety stress scales (DASS): detecting anxiety disorder and depression in employees absent from work because of mental health problems. Occup. Environ. Med. 2003;60(Suppl. 1):i77–i82. doi: 10.1136/oem.60.suppl_1.i77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noaimi H.M.A., Noaimi M.M.A., Fayez F.M.A., Mushkhes H.Q.A., Al Ani W. The impact of COVID-19 pandemic on mental health of health care workers of Bahrain Defence Force Royal Medical Services. Bahrain Med. Bull. 2021;43:580–587.. [Google Scholar]
- Nochaiwong S., Ruengorn C., Thavorn K., Hutton B., Awiphan R., Phosuya C., Ruanta Y., Wongpakaran N., Wongpakaran T. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Sci. Rep. 2021;11:10173. doi: 10.1038/s41598-021-89700-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olaya B., Pérez-Moreno M., Bueno-Notivol J., Gracia-García P., Lasheras I., Santabárbara J. Prevalence of depression among healthcare workers during the COVID-19 outbreak: a systematic review and meta-analysis. J. Clin. Med. 2021:10. doi: 10.3390/jcm10153406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020;383:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Phiri P., Ramakrishnan R., Rathod S., Elliot K., Thayanandan T., Sandle N., Haque N., Chau S.W.H., Wong O.W.H., Chan S.S.M., Wong E.K.Y., Raymont V., Au-Yeung S.K., Kingdon D., Delanerolle G. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: a systematic review and meta-analysis. EClinicalMedicine. 2021;34 doi: 10.1016/j.eclinm.2021.100806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preti E., Di Mattei V., Perego G., Ferrari F., Mazzetti M., Taranto P., Di Pierro R., Madeddu F., Calati R. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr. Psychiatry Rep. 2020;22:43. doi: 10.1007/s11920-020-01166-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . 2013. R: A Language and Environment for Statistical Computing, Vienna, Austria. [Google Scholar]
- Raoofi S., Pashazadeh Kan F., Rafiei S., Khani S., Hosseinifard H., Tajik F., Masoumi M., Raoofi N., Ahmadi S., Aghalou S., Torabi F., Dehnad A., Hoseinipalangi Z., Rezaei S., Shabaninejad H., Ghashghaee A. Anxiety during the COVID-19 pandemic in hospital staff: systematic review plus meta-analysis. BMJ Support. Palliat. Care. 2021 doi: 10.1136/bmjspcare-2021-003125. bmjspcare-2021-003125 Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Robinson E., Sutin A.R., Daly M., Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022;296:567–576. doi: 10.1016/j.jad.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotenstein L.S., Ramos M.A., Torre M., Segal J.B., Peluso M.J., Guille C., Sen S., Mata D.A. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316:2214–2236. doi: 10.1001/jama.2016.17324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruzek J.I., Brymer M.J., Jacobs A.K., Layne C.M., Vernberg E.M., Watson P.J. Psychological first aid. J. Ment. Health Couns. 2007;29:17–49. [Google Scholar]
- Salari N., Khazaie H., Hosseinian-Far A., Ghasemi H., Mohammadi M., Shohaimi S., Daneshkhah A., Khaledi-Paveh B., Hosseinian-Far M. The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: a systematic review and meta-analysis. Glob. Health. 2020;16:92. doi: 10.1186/s12992-020-00620-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Khazaie H., Hosseinian-Far A., Khaledi-Paveh B., Kazeminia M., Mohammadi M., Shohaimi S., Daneshkhah A., Eskandari S. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum. Resour. Health. 2020;18:100. doi: 10.1186/s12960-020-00544-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santabárbara J., Bueno-Notivol J., Lipnicki D.M., Olaya B., Pérez-Moreno M., Gracia-García P., Idoiaga-Mondragon N., Ozamiz-Etxebarria N. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: a rapid systematic review (on published articles in Medline) with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;107 doi: 10.1016/j.pnpbp.2021.110244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmid B., Schulz S.M., Schuler M., Göpfert D., Hein G., Heuschmann P., Wurmb T., Pauli P., Meybohm P., Rittner H.L. Impaired psychological well-being of healthcare workers in a German department of anesthesiology is independent of immediate SARS-CoV-2 exposure - a longitudinal observational study. Ger. Med. Sci. 2021;19 doi: 10.3205/000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert M., Ludwig J., Freiberg A., Hahne T.M., Romero Starke K., Girbig M., Faller G., Apfelbacher C., Von Dem Knesebeck O., Seidler A. Stigmatization from work-related COVID-19 exposure: a systematic review with meta-analysis. Int. J. Environ. Res. Public Health. 2021;18:6183. doi: 10.3390/ijerph18126183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serrano-Ripoll M.J., Meneses-Echavez J.F., Ricci-Cabello I., Fraile-Navarro D., Fiol-deRoque M.A., Pastor-Moreno G., Castro A., Ruiz-Pérez I., Zamanillo Campos R., Gonçalves-Bradley D.C. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J. Affect. Disord. 2020;277:347–357. doi: 10.1016/j.jad.2020.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shechter A., Chiuzan C., Shang Y., Ko G., Diaz F., Venner H.K., Shaw K., Cannone D.E., McMurry C.L., Sullivan A.M., Rivera R.R., Vose C., Shapiro P.A., Abdalla M. Prevalence, incidence, and factors associated with posttraumatic stress at three-month follow-up among New York City healthcare workers after the first wave of the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2021;19 doi: 10.3390/ijerph19010262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheen J., Clancy E.M., Considine J., Dwyer A., Tchernegovski P., Aridas A., Lee B.E., Reupert A., Boyd L. “did you bring it home with You?” a qualitative investigation of the impacts of the COVID-19 pandemic on victorian frontline healthcare workers and their families. Int. J. Environ. Res. Public Health. 2022;19 doi: 10.3390/ijerph19084897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor-Phillips S., Geppert J., Stinton C., Freeman K., Johnson S., Fraser H., Sutcliffe P., Clarke A. Comparison of a full systematic review versus rapid review approaches to assess a newborn screening test for tyrosinemia type 1. Res. Synth. Methods. 2017;8:475–484. doi: 10.1002/jrsm.1255. [DOI] [PubMed] [Google Scholar]
- Th'ng F., Rao K.A., Ge L., Mao D., Neo H.N., Molina J.A.D., Seow E. A one-year longitudinal study: changes in depression and anxiety in frontline emergency department healthcare workers in the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph182111228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troglio Da Silva F.C., Neto M.L.R. Psychiatric disorders in health professionals during the COVID-19 pandemic: a systematic review with meta-analysis. J. Psychiatr. Res. 2021;140:474–487. doi: 10.1016/j.jpsychires.2021.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tung Y.J., Lo K.K.H., Ho R.C.M., Tam W.S.W. Prevalence of depression among nursing students: a systematic review and meta-analysis. Nurse Educ. Today. 2018;63:119–129. doi: 10.1016/j.nedt.2018.01.009. [DOI] [PubMed] [Google Scholar]
- Varghese A., George G., Kondaguli S.V., Naser A.Y., Khakha D.C., Chatterji R. Decline in the mental health of nurses across the globe during COVID-19: a systematic review and meta-analysis. J. Glob. Health. 2021;11 doi: 10.7189/jogh.11.05009. 05009-05009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viechtbauer W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010;1(3):2010. [Google Scholar]
- Viechtbauer W., Cheung M.W.L. Outlier and influence diagnostics for meta-analysis. Res. Synth. Methods. 2010;1:112–125. doi: 10.1002/jrsm.11. [DOI] [PubMed] [Google Scholar]
- Waffenschmidt S., Knelangen M., Sieben W., Bühn S., Pieper D. Single screening versus conventional double screening for study selection in systematic reviews: a methodological systematic review. BMC Med. Res. Methodol. 2019;19:132. doi: 10.1186/s12874-019-0782-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang K., Lu H., Cheung E.F.C., Neumann D.L., Shum D.H.K., Chan R.C.K. “Female preponderance” of depression in non-clinical populations: a meta-analytic study. Front. Psychol. 2016;7 doi: 10.3389/fpsyg.2016.01398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang N. 2018. How to Conduct a Meta-Analysis of Proportions in R: A Comprehensive Tutorial. [Google Scholar]
- World Health Organisation . World Health Organisation; Geneva: 2020. State of the World's Nursing 2020: Investing in Education, Jobs and Leadership. [Google Scholar]
- World Health Organisation . 2021. WHO Coronavirus Disease (Covid-19) Dashboard. [Google Scholar]
- World Health Organisation . 2022. Tracking SARS-CoV-2 Variants. [Google Scholar]
- Wu T., Jia X., Shi H., Niu J., Yin X., Xie J., Wang X. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 2021;281:91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie N., Qin Y., Wang T., Zeng Y., Deng X., Guan L. Prevalence of depressive symptoms among nurses in China: a systematic review and meta-analysis. PLOS ONE. 2020;15 doi: 10.1371/journal.pone.0235448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan H., Ding Y., Guo W. Mental health of medical staff during the coronavirus disease 2019 pandemic: a systematic review and meta-analysis. Psychosom. Med. 2021;83:387–396. doi: 10.1097/PSY.0000000000000922. [DOI] [PubMed] [Google Scholar]
- Yuan K., Gong Y.-M., Liu L., Sun Y.-K., Tian S.-S., Wang Y.-J., Zhong Y., Zhang A.-Y., Su S.-Z., Liu X.-X., Zhang Y.-X., Lin X., Shi L., Yan W., Fazel S., Vitiello M.V., Bryant R.A., Zhou X.-Y., Ran M.-S., Bao Y.-P., Shi J., Lu L. Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review. Mol. Psychiatry. 2021;26:4982–4998. doi: 10.1038/s41380-021-01036-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y.-J., Jin Y., Rao W.-W., Li W., Zhao N., Cheung T., Ng C.H., Wang Y.-Y., Zhang Q.-E., Xiang Y.-T. The prevalence of psychiatric comorbidities during the SARS and COVID-19 epidemics: a systematic review and meta-analysis of observational studies. J. Affect. Disord. 2021;287:145–157. doi: 10.1016/j.jad.2021.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Prisma checklist.
Methods supplement.
Summary table of study characteristics.
Included studies references.
Measurement tools and cut off scores.
Depression forest plots.
Anxiety forest plots.
PTSD forest plots.
Insomnia forest plots.
AUD forest plot.
Funnel plots.
COVID-19 longitudinal studies summary table.