Abstract
Background
Most oral diseases are caused by poor oral hygiene, and with adequate oral hygiene measures, they are easily preventable. The use of folk songs to deliver oral health education may likely hold a huge potential for success and an increased likelihood of acceptability and sustainability among school children. Therefore, an investigation into the effectiveness of methods that would be culturally appropriate and sustainable, such as folk songs, is essential.
Aim
To determine the effect of traditional rhyme (folk song) as a tool for oral hygiene education among children in rural communities in Nigeria.
Materials and methods
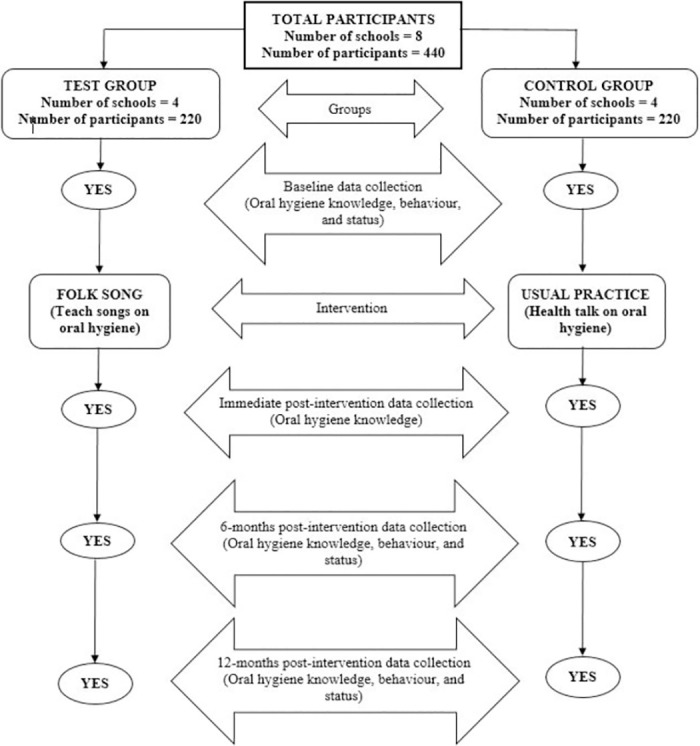
This is a school-based, assessor-blinded, two-arm cluster-randomised controlled trial that will assess the effectiveness of oral hygiene messages delivered through traditional rhyme (folk song) on children’s oral hygiene knowledge, attitude, practices, and oral hygiene status in two rural communities (Igboora and Idere) in Nigeria. The study will involve a minimum of 424 participants (aged 7–9 years) selected from eight primary schools using the cluster sampling technique. Four schools will be randomised into the test group to receive oral hygiene messages through folk songs, and the participants will sing the song for two weeks. The other four schools will be assigned to the control group, and the participants will receive the usual oral health talk on oral hygiene practices by a dentist. The participants’ oral hygiene knowledge, attitude, practice and status will be assessed at baseline, immediate, six, and twelve-month post-intervention. A modified World Health Organization (WHO) Children’s oral health survey questionnaire will be utilised for data collection. Oral examinations will be conducted to assess the participants’ dental caries experience and oral hygiene status using the dmft/DMFT and simplified oral hygiene indices, respectively.
Discussion
Folk songs are popular means of conveying messages in Nigeria, and using them to deliver oral health messages may be an effective, acceptable, and sustainable method among children. This study will provide empirical information about this innovative intervention to guide policy development, dental public health practice, and future studies.
Trial registration
Pan African Clinical Trial Registry-PACTR202010863892797 (October 2020).
Introduction
Oral diseases remain major public health problems with a substantial personal, social, and economic burden [1]. Worldwide, the prevalence of oral diseases like dental caries and periodontal diseases is high as they affect most people in high- middle- and low-income countries (HICs and LMICs) [1]. It is estimated that 2.4 billion people suffer from dental caries of permanent teeth, and 486 million children suffer from dental caries of primary teeth [2]. The global increase in the prevalence of dental caries [3, 4] highlights the need for primary prevention programmes, especially in LMICs, including sub-Saharan Africa, which has the highest burden of untreated dental caries [1, 5]. Dental caries are painful, negatively impact the quality of life, and may result in tooth loss and systemic infection that can lead to death in its advanced stage [6]. The treatment options for dental caries are costly, averaging 5% of the total health expenditure and 20% of out-of-pocket expenditure in developed countries [7]. In most developing countries, investment in oral health is low, and if treatment were available, the costs of dental caries in children alone would exceed the total healthcare budget [8]. Similarly, periodontal diseases contribute significantly to the global burden of oral disease, leading to pain, bleeding, bad breath, tooth loss, and adverse systemic illnesses [9]. Most epidemiological studies have observed significant relationships between socio-economic status and periodontal disease [10–13]. Low income and low education contribute to poor periodontal disease status [10–12]. There is an unequal burden of oral diseases affecting those in the rural areas more than those in the urban communities [13], and more among those living in slums than non-slum areas [12].
Most oral diseases like dental caries and periodontal problems are preventable [9]. Dental caries is one of the most common oral diseases that negatively impact the oral health-related quality of life of those affected [14]. While it can affect people over their life course [15], the risk is higher among children [15]. Given the cost of treatment and devastating effect on the quality of life, prevention of dental and other oral problems must be prioritised. The common preventive measures include maintaining good oral hygiene, eating a balanced diet with low refined-carbohydrate content, and regularly visiting the dental office for a check-up, early detection, and treatment of emerging oral problems [16, 17].
It is advocated that oral health education programs are instituted among the people living in Africa and the Middle East, including those in rural and underserved communities, to instil good hygiene practices among them [13]. There is an urgent need for educational interventions among Nigerian children with several reports stating that many of them have poor oral hygiene knowledge and behaviour [18–22]. These interventions are particularly useful when they are carried out among children who are just forming behaviours that affect their health [23, 24]. Helping children develop the habit of brushing twice daily and maintaining good oral hygiene is key to a lifetime of healthy smiles. Thus, exploring the roles of innovative methods such as oral hygiene songs, particularly folk songs with an inherent cultural motif at developing and probably sustaining good oral hygiene habits among children becomes pertinent.
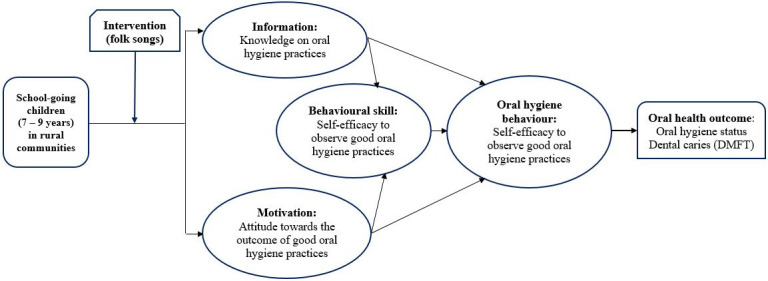
Educational interventions that are based on behavioural models, including the Information-Motivation-Bavioural Skill (IMB) model, are usually more successful than those without it [25]. The IMB model, a theoretical framework developed by Fisher and others [26], presupposes that the successful adoption of health behaviour is contingent on three key factors: adequate knowledge about the behavior, motivation (positive personal attitudes and social support) to engage in the behavior, and the possession of self-efficacy and appropriate skills to undertake the behaviour [26]. The IMB model is a widely recognized approach used in modifying health behaviours among different population groups, including children and adolescents [26–28].
Songs help in conveying messages to people, help them retain those messages, motivate them into action [29], and it has been used to successfully improve public health knowledge and behaviours [30]. The use of songs is an effective approach to educating children and adolescents about proper oral health practices [31]. Through music, children can learn and retain information about oral hygiene in an enjoyable manner, thereby forming healthy habits that last a lifetime [32]. Toothbrushing songs that are set to familiar tunes can be particularly effective, as they make learning about oral health engaging and accessible [31, 32]. To enhance the effectiveness of such songs, traditional melodies can be adapted to include lyrics that reinforce key oral hygiene concepts. Parents, guardians, and schoolteachers can all leverage the power of music to teach children the importance of brushing and maintaining good oral hygiene. Additionally, using songs as a reminder to brush regularly is a fun and engaging activity that can be shared between parents, guardians, and their children daily [33]. Although using folk songs to deliver oral health messages holds much promise, there is a lack of empirical information about its use among children in Nigeria. Hence, this study aims to determine the effect of traditional rhyme (folk song) as a tool for oral hygiene education among children in rural communities in Nigeria.
Materials and methods
Study design
The research is designed to be a cluster-randomised, assessor-blinded, controlled trial with two study groups—intervention and control. The randomised control design was adopted to provide a high level of evidence for the study. The IMB model will form the framework for the study (Fig 1).
Fig 1. Theoretical framework for the study.
Study location and site
The planned study sites are Igboora and Idere, two rural communities in Ibarapa Central Local Government Areas of Oyo State, Southwestern Nigeria, which are about seven kilometres apart. Farming and petty trading are common in the two communities, and Yoruba is the predominant tribe and language [34]. There are 80 basic schools (primary schools) in the two communities [35]. Most primary schools have classes from Primary one (Pry 1) to Primary six (Pry 6), while some end at Pry 5 [36]. Generally, most classes have five arms (A–E), and preliminary investigation shows that each class arm has an average of 25 pupils. The official entry age into primary school i.e. Pry 1 class is six years, while they exit Pry 6 and start secondary school at age 12 years [36, 37]. However, because the rule is not strictly upheld, some schools enroll children into the Pry 1 class at ages four and five years [36, 37]. Since the usual age of entry into primary school ranges between four to six years, those in Pry 4 are usually between 7–9 years old [37].
Study population
The study participants would comprise Pry 4 pupils from primary schools located in the two rural communities (Igboora and Idere) in Oyo State, Nigeria. The choice of the Primary 4 class pupils is for the following reasons: the pupils’ ages range from seven to nine years, and they usually would have started supervised but unassisted oral hygiene practices like tooth brushing [38, 39]. The age group (7–9 years) also has a higher likelihood of providing better responses during the interviews than younger people from the lower classes [40]. Moreover, pupils in the Pry 4 class are more likely to remain in their various schools through the proposed study period, unlike those in higher classes (Pry 5 and Pry 6) who may be nursing the idea of writing the secondary school qualifying examinations (common entrance examinations) and leaving their various schools while this study is still ongoing.
Eligibility criteria
Inclusion criteria
Healthy children with parental consent will be included in the study.
Exclusion criteria
Primary schools not registered with the Oyo State Government will be excluded from the study. Pupils who do not understand the Yoruba language will also be excluded because the intervention (folk song) is in the Yoruba language.
Sample size determination
The sample size for this study was determined using the formula for comparing two proportions [41]. The primary outcome is oral hygiene status. The prevalence (P1 = 38.4%) of children who had good oral hygiene from a previous study in Nigeria [42], was used for sample size calculation. An estimated 50% increase in the proportion of participants with good oral hygiene following the intervention (P2 = 57.6%) was used in calculating the minimum sample size. Other considerations were statistical power of 80%, a significance level of 5%, a non-response rate of 10%, an attrition rate of 20%, and an estimated design effect of 1.5. A minimum of 212 participants will be recruited per study group, making 424 for the two groups.
Sampling technique, recruitment, and randomisation
A two-stage cluster sampling technique will be employed for this study.
In the first stage, four schools from each of the two communities will be selected from the list of schools that would be obtained from the Ministry of Education, Oyo State, using the simple random sampling technique, making eight schools in total. In the second stage, an average of 55 participants will be selected from each selected school’s Pry 4 class arm using a proportionate sampling technique.
The schools will be the randomisation unit. The eight selected schools in the two communities (Igboora and Idere) will be randomised into either the test or the control group using the block randomisation method, aided by computer-generated numbers [43]. A website [44], for generating randomisation lists will be utilised for this purpose. Before using the website, the eight selected schools would have been assigned code numbers from “01” to “08”. The needed parameters will then be entered into the website and it would automatically generate the allocation sequence with the code numbers (schools) already assigned to the two study groups (Group A-Test; Group B-Control). Subsequently, the result of the randomization would be downloaded for future reference. The whole process of randomization will be conducted by an expert who is not familiar with the details of the study.
Baseline data collection
Interviewer-administered semi-structured questionnaire (S2 File) will be used for data collection. The questionnaire will be developed from the review of related local literature [12, 42, 45], and will be pretested and validated for use among the study participants. The oral examinations will be based on the WHO Oral Health Surveys: Basic Methods, 5th Edition [46]. Five trained and calibrated dentists will conduct the interview and oral examinations. The dentists will be trained by an expert in oral epidemiology using the WHO guideline [46]. The questionnaire will be used to collect information on the participants’ sociodemographic characteristics, oral hygiene knowledge, attitude, and practices. While the children will be the main respondents, their parents (preferably mothers) will be called by the research assistants to validate the information provided by the children regarding the sociodemographics and oral hygiene behaviour. The oral examination will assess the participants’ oral hygiene status (simplified oral hygiene index [47]) and their lifetime caries experience [sum of decayed, missing, and filled teeth (dmft/DMFT) [46, 48]]. Based on the simplified oral hygiene index (OHI-S), indexed teeth would be assessed. On the upper jaw/maxilla, the Right and Left First Molar (UR6, UL6) and Right Incisor (UR1) will be assessed. Similarly, both the Right and Left First Mandibular Molars (LR6, LL6) and the Left Mandibular First Incisor (LL1) will be examined in the low jaw/mandible [47]. If any of these teeth are absent, another designated tooth in the segment will be examined [47]. The oral examination will be done using a sterile wooden mouth spatula, probes, and dental mirrors. The oral examination will be conducted near the windows in the school halls, with the participants seated upright facing the window such that the examination is aided by good illumination from natural light. Baseline data collection will be conducted in both study groups (test and control) one week before delivering the interventions.
Intervention and control groups
The intervention will involve teaching the participants in the test group traditional rhyme (folk songs) on adequate oral hygiene measures and practices. The song was developed in English and Yoruba, the two major Nigerian languages in the two communities. While Yoruba is the primary language of the pupils, they are taught in English. The songs convey health messages, including the importance of twice-daily tooth brushing with pea-size fluoride-containing toothpaste, the need to brush the tongue, and simple tooth brushing techniques using toothbrushes with soft/medium-bristles. The song was co-developed and validated among selected schoolchildren, teachers, and parents/legal guardians [49].
There will be three intervention sessions lasting for one month. During the first session, one of the researchers (OO) will teach selected participants in the test group the two songs (English and Yoruba). Some participants will be asked to sing the songs to confirm if the pupils have learned them. Subsequently, all the participants will be asked to sing the songs several times. The first session of the intervention is estimated to last 40 minutes. The participants will be asked to continue singing the songs every morning in the school for one month, under the supervision of a teacher. This will be monitored through daily visits to the schools by designated research assistants to confirm that the participants are singing the songs as expected. The second session will take place two weeks after the first, and the researcher will ask the participants to sing the songs as a group several times. Similarly, the third session will take place two weeks after the second session (one month after the first session) and the students will also sing the songs in the presence of the researcher (OO). The second and third sessions are estimated to last for 20 minutes.
The participants in the control group will be exposed to conventional health education on adequate oral hygiene practices conducted by the dentist [50]. Similar to the test group, there will be three intervention sessions. The first session will last for 40 minutes and will involve expert-led health talks and question and answer with the participants. The second and third sessions will also take place after two and four weeks, respectively. The follow-up sessions will involve revising the oral health messages with the participants, lasting for about 20 minutes each. None of the participants (control and test groups) will be denied access to oral health talks that they may be exposed to away from school.
Post-intervention data collection
There will be three sessions of post-intervention assessments—Immediate, six, and 12 months. The immediate post-intervention assessment will collect information on the participants’ oral hygiene knowledge and attitude immediately after the second session of the intervention is completed. The 6-month post-intervention assessment will be conducted six months after the immediate post-intervention assessment. Information on the participants’ oral hygiene knowledge, attitude, and practices will be collected. Oral examinations will also be done to assess the participants’ oral hygiene status using the simplified oral hygiene index. The 12-month post-intervention assessment will be conducted 12 months after the immediate post-intervention assessment. It will involve oral health examinations to check the participants’ oral hygiene status and dental caries experience (dmft/DMFT), along with assessing the participants’ oral hygiene knowledge, attitude, and practices. The same questionnaire for the pre-intervention assessment will also be used for the post-intervention assessments. However, the immediate post-intervention assessment will not include oral examinations. The questionnaires for 6 and 12 months post-intervention data collection will include a question to assess if the participants have been taught oral hygiene practices (through songs or lectures) by pupils from other schools during the study period. This is to get data on the potential contamination and control for this during the data analysis (sub-analysis).
Figs 2 and 3 show the SPIRIT schedule and Flow diagram for the study, respectively.
Fig 2. The SPIRIT schedule for the study.
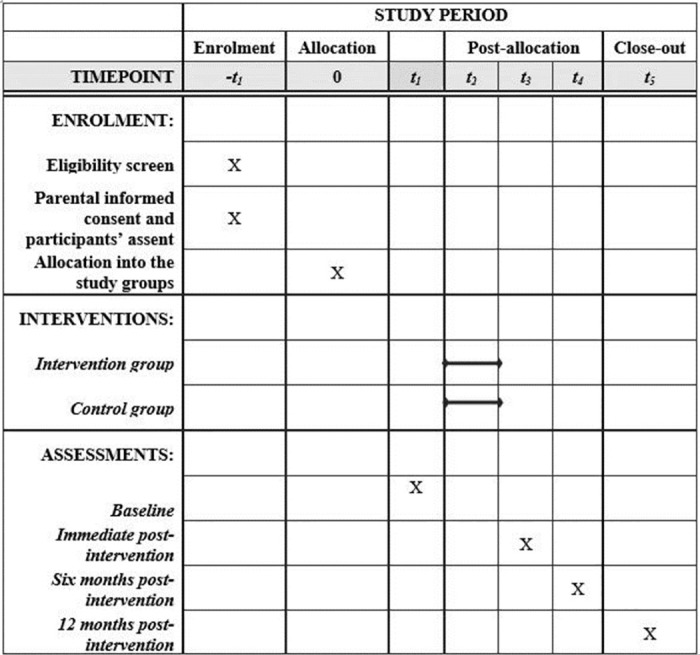
Fig 3. Flow diagram for the study.
Variables
Primary outcome variables
The participants’ oral health status will be the primary outcome variable. There would be three measures, including the caries experience, which would be based on the oral examination of the dmft/DMFT scores, current caries status [48], and oral hygiene status [47].
The DMFT/dmft will be calculated for each participant by summing up all the carious, filled, and missing teeth due to caries in their mouth. Subsequently, the mean DMFT and mean dmft will be calculated by dividing the sum of the DMFT/dmft scores for each group by the total number of participants in the group and reported separately for the two study groups. The caries prevalence would also be assessed by dividing the number of participants with at least one carious tooth over the total number of participants in each group.
The oral hygiene status will be assessed using the simplified Oral Hygiene Index (OHI-S) [47]. The maximum score for OHI-S is six. Based on their score, each participant will be assigned these three categories: “Good” (0.0–1.2), “Fair” (1.3–3.0), and “Poor” (3.1–6.0) [47].
Secondary outcome variables
The secondary outcome variables include participants’ oral hygiene knowledge, attitude, and practices. There will be six questions assessing the participants’ knowledge. Each correct answer will be awarded a score of “1” and the wrong option “0”. Each participant’s knowledge score will be compiled over six. Similarly, there will be five questions to assess their attitude. The options will be a Likert scale (strongly disagree to strongly agree). The best response, which indicates the most positive attitude to the statement on oral hygiene, will be given the highest score of “5” while the most negative response will be scored “1”. The total attitude score for all the participants will be computed with the maximum being “25” and the minimum being “5”. The participants’ oral hygiene practices that would be assessed include twice daily brushing, the presence of fluoride, and the size of dispensed toothpaste for brushing. Others are their technique of tooth brushing and how long before they changed their toothbrush.
Independent variables
The independent variables would include the participants’ study group, sociodemographic characteristics (age, gender, neighbourhood), and school-related characteristics (school type, class level).
Validity and reliability of the questionnaire
The questionnaire (Appendix I) contains mainly structured questions, with a few carefully selected open-ended questions to ensure valid responses. The questionnaire contained questions that will be easy to administer, and the importance of giving steady answers by the respondents will be emphasised. The questionnaire was face- and content-validated by dental public health experts, and they considered the questions adequate to answer the research questions and appropriate for the intended age group. The data collectors will be trained on the mode of administering the questionnaires to avoid interviewer bias. The questionnaires will be pretested among a minimum of 20 pupils in communities outside Igboora and Idere with similar relevant characteristics to the study population. The students will be asked to give feedback on the clarity of the questions and other useful information will be used to improve the questionnaire. The pretest will be done to assess the reliability of the questions, including the knowledge and attitude scales and their responses will be analysed using the test statistics of Cronbach’s reliability test. The five examiners will also individually provide oral examinations for all 20 pupils. The examiners’ agreement on the recorded scores for the simplified oral hygiene index and dmft/DMFT will be evaluated using the Cohen Kappa statistics.
Data management plan
Data handling plan
The questionnaires will be checked for errors daily, and necessary corrections will be made as soon as they are discovered. Each response on the questionnaire will then be coded and recoded on a coding sheet. The codes for each response on the questionnaire will then be entered into Statistical Package for Social Science (SPSS) Version 25, after which the coded data will be checked for errors by cross-checking 10% of the data.
Data analysis plan
Baseline data would be compared among the two study groups based on their sociodemographic characteristics and the baseline value of the outcome variables (oral hygiene status, DMFT/dmft, caries status, knowledge, attitude, and practice). Subsequently, the intervention effects on the outcome variables will be assessed over the study period (baseline, immediate, 6 months, and 12 months assessments). The effectiveness would also be compared between groups (test vs control) over the 12 months (baseline, 6 months, and 12-month assessment). An intention-to-treat analysis will be employed for this study [51]. A participant will remain in the originally assigned group, notwithstanding what happens during the study, such as deviation from the study protocol or loss to follow-up. The data obtained at the previous assessment will be recorded for those lost to follow up in the subsequent assessments. The level of statistical significance for all tests will be set at p < 0.05.
Ethical considerations
The study has been registered with the Pan African Clinical Trial Registry (PACTR202010863892797). Ethical approval was obtained from the University of Ibadan/University College Hospital Ethical Review Committee (Registration number: NHREC/05/01/2008a). The permission to carry out the study was also received from the Ministry of Education, Oyo State. The following ethical issues will be considered:
Written informed consent
A letter to the parents or legal guardians will request their consent for their children or ward to participate in the study. An information sheet stating the details of the study will be given to them to read, after which they will be asked if they understood what the study is about and what is expected of their children/wards. Parents/legal guardians who agree to allow their children/wards to participate in the study will be asked to sign a written Informed Consent form, and their children will subsequently sign the assent form.
Confidentiality of data
All information collected from respondents during this research will be kept confidential. All identifiable details of the participants will be separated from the coded details and collected data. The identifiable details and data entered on the computer will be password-protected and only accessible to the researchers and data entry clerks.
Right to withdraw from the study
Study participants who wish to withdraw from the study will be allowed to do so freely at any point in time and without any negative repercussions.
Beneficence/Non-maleficence
The study participants will benefit from the educational intervention during or immediately after the study, and the study does not pose any harm to the participants.
Dissemination
Findings from the study will be presented at both local and international conferences and published in peer-reviewed journals.
Discussion
A multi-disciplinary team comprising community dentists, paediatric dentists, restorative dentists, and music experts was established to develop a traditional rhyme (Folk Song) to be used as a tool for oral hygiene promotion among children in two rural communities in Nigeria. The team, together with children, teachers, and parents, co-developed a simple, memorable, and age-appropriate traditional song [49] as the platform for delivering oral hygiene behavioural change to children to enhance their self-efficacy with twice-daily tooth brushing.
To the best of our knowledge, this is one of the few studies to assess the effectiveness of traditional folk songs in improving children’s oral hygiene knowledge, attitude, and practices. Folk songs are very popular in Nigeria, and it is not just for entertainment but also to convey historical events and heritage and teach children about important virtues [52, 53]. This study aims to use folk songs to deliver oral health education to children in two rural communities—Igboora and Idere, Oyo State, Nigeria. The burden of oral health problems is high in Nigeria, like other African countries, and those in rural areas are more affected [13]. This is one of the reasons these communities were selected for the intervention. Like other rural communities in Nigeria, access to oral health services is also limited in these communities. However, the Department of Periodontology and Community Dentistry, University College Hospital/University of Ibadan, provides basic oral health care services to these communities through the Primary Oral Health Care clinics, and some of the investigators of this research are in charge of the clinics. This relationship would facilitate a quick uptake of outcomes of this research in the subsequent planning of intervention programmes from the dental clinics in responding to oral health challenges in the study sites.
Pupils in primary schools have been targeted for this intervention because the school provides an organised setting where the participants can be taught without distractions. It also gives the best opportunity for the participants to be followed up with a lesser risk of attrition. The intervention can also be easily sustained by incorporating it into their activities during the daily morning assembly.
A school/cluster-level randomisation will be employed to avoid having participants in the intervention and control groups in the same school, which may increase the risk of spillover [54]. There is no way some participants in a school would be taught these songs, and others in the control group would not be aware if they were in the same school. In the same vein, the distance of schools will be considered when selecting the schools for the study and schools close to each other would not be allowed to be in different study groups.
This study will consider several outcomes, including knowledge, attitude, practice, and oral health status (caries and oral hygiene). This would generate empirical information on the effectiveness of folk songs on each of these outcomes separately. A possible limitation in the outcome measurement is the dmft/DMFT.
The dmft/DMFT is a non-reversible index [48]; thus, the score at baseline would not reduce at the study completion even if the participant has treated carious teeth. To address this, the condition of the teeth (decayed, missing, and filled) would be noted at baseline. Hence, if a participant visited the dental clinic to fill a decayed tooth, such would be noted as an improvement in the caries experience during the final assessment 12 months post-intervention.
Supporting information
(DOC)
(DOCX)
Data Availability
No datasets were generated or analysed during the current study. All relevant data from this study will be made available upon study completion.
Funding Statement
Co-author initials: OI Funder: FDI World Dental Federation (https://www.fdiworlddental.org/) The funder had and will not have a role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Bernabe E, Marcenes W, Hernandez CR, Bailey J, Abreu LG, Alipour V, et al. Global, Regional, and National Levels and Trends in Burden of Oral Conditions from 1990 to 2017: A Systematic Analysis for the Global Burden of Disease 2017 Study. J Dent Res. 2020;99(4):362–373. doi: 10.1177/0022034520908533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017. Sep 14;390:1211–1259. doi: 10.1016/S0140-6736(17)32154-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bagramian RA, Garcia-Godoy F, Volpe AR. The global increase in dental caries: A pending public health crisis. Am J Dent. 2009;22(1):3–8. [PubMed] [Google Scholar]
- 4.Wen PYF, Chen MX, Zhong YJ, Dong QQ, Wong HM. Global Burden and Inequality of Dental Caries, 1990 to 2019. J Dent Res. 2022. Apr 1;101(4):392–399. doi: 10.1177/00220345211056247 [DOI] [PubMed] [Google Scholar]
- 5.Abid A, Maatouk F, Berrezouga L, Azodo C, Uti O, El-Shamy H, et al. Prevalence and Severity of Oral Diseases in the Africa and Middle East Region. Adv Dent Res. 2015. Jul 1;27(1):10–17. doi: 10.1177/0022034515582062 [DOI] [PubMed] [Google Scholar]
- 6.Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005. Sep;83(9):661–669. [PMC free article] [PubMed] [Google Scholar]
- 7.OECD. Health at a Glance 2017: OECD Indicators [Internet]. Paris: OECD Publishing; 2017 [cited 2022 Mar 14]. 1–44 p. (Health at a Glance). 10.1787/health_glance-2017-en [DOI]
- 8.Yee R, Sheiham A. The burden of restorative dental treatment for children in Third World countries. Int Dent J. 2002. Feb;52(1):1–9. [PubMed] [Google Scholar]
- 9.Nazir MA. Prevalence of periodontal disease, its association with systemic diseases and prevention. Int J Health Sci (Qassim). 2017;1(2):72–80. [PMC free article] [PubMed] [Google Scholar]
- 10.Albandar JM, Tinoco EMB. Global epidemiology of periodontal diseases in children and young persons. Periodontol 2000. 2002;29(1):153–176. doi: 10.1034/j.1600-0757.2002.290108.x [DOI] [PubMed] [Google Scholar]
- 11.Borrell LN, Burt BA, Neighbors HW, Taylor GW. Social factors and periodontitis in an older population. Am J Public Health. 2004;94(5):748–754. doi: 10.2105/ajph.94.5.748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Osuh ME, Oke GA, Lilford RJ, Owoaje E, Harris B, Taiwo OJ, et al. Prevalence and determinants of oral health conditions and treatment needs among slum and non-slum urban residents: Evidence from Nigeria. PLOS Glob Public Heal. 2022. Apr 22;2(4):e0000297. doi: 10.1371/journal.pgph.0000297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ogunbodede EO, Kida IA, Madjapa HS, Amedari M, Ehizele A, Mutave R, et al. Oral Health Inequalities between Rural and Urban Populations of the African and Middle East Region. Adv Dent Res. 2015. Jul 1;27(1):18–25. doi: 10.1177/0022034515575538 [DOI] [PubMed] [Google Scholar]
- 14.Lawal FB, Bankole OO. Impact of untreated dental caries on daily performances of children from low social class in an urban African population: The importance of pain. Pesqui Bras Odontopediatria Clin Integr. 2019. Oct 31;19:e4771. doi: 10.4034/PBOCI.2019.191.82 [DOI] [Google Scholar]
- 15.Broadbent JM, Foster Page LA, Thomson WM, Poulton R. Permanent dentition caries through the first half of life. Br Dent J. 2013. Oct 11;215(7):1–6. doi: 10.1038/sj.bdj.2013.991 [DOI] [PubMed] [Google Scholar]
- 16.Walsh T, Worthington H V., Glenny AM, Marinho VCC, Jeroncic A. Fluoride toothpastes of different concentrations for preventing dental caries. Cochrane Database Syst Rev. 2019. Mar 4;2019(3). CD007868 doi: 10.1002/14651858.CD007868.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO. Oral health [Internet]. Fact sheets. 2020 [cited 2020 Jun 19]. https://www.who.int/news-room/fact-sheets/detail/oral-health
- 18.Soroye M, Adegbulugbe C. Oral health status, knowledge of dental caries aetiology, and dental clinic attendance: A comparison of secondary school students in the rural and urban areas of Lagos. Port Harcourt Med J. 2016;10(2):42–49. [Google Scholar]
- 19.Idowu EA, Nwhator SO, Afolabi AO. Nigeria’s street children, epitome of oral health disparity and inequality. Pan Afr Med J. 2020. May 1;36:1–10. https://pubmed.ncbi.nlm.nih.gov/32774636/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alufa OO, Lucero-Prisno DE. Dental health promotion among Nigerian school children: Why a priority. Ann Med Surg. 2022. Oct 15];82:1–2. doi: 10.1016/j.amsu.2022.104691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lawal FB, Taiwo JO. Making a Case for Formal School-Based Oral Health Promotion: Oral Health Knowledge, Attitude and Practices of Pupils in Ibadan, Nigeria. Int Q Community Health Educ. 2018. Dec 20;38(2):99–105. doi: 10.1177/0272684X17749574 [DOI] [PubMed] [Google Scholar]
- 22.Sa’adu L, Musa O., Abu-Saeed K, Abu-Saeed Muhammad B. Knowledge and practices on oral health among junior secondary school students in Ilorin West Local Government Area of Nigeria. E-Journal Dent. 2012. Apr;2(2):170–175. [Google Scholar]
- 23.Pawlaczyk-Kamienska T, Torlinska-Walkowiak N, Borysewicz-Lewicka M. The relationship between oral hygiene level and gingivitis in children. Adv Clin Exp Med. 2018. Oct 1;27(10):1397–1401. doi: 10.17219/acem/70417 [DOI] [PubMed] [Google Scholar]
- 24.Kamińska A, Batkowska J, Wallner J, Wallner E, Szabelska A, Borowicz J. The dependence of dental caries on oral hygiene habits in preschool children from urban and rural areas in Poland. Ann Agric Environ Med. 2016;23(4):660–665. doi: 10.5604/12321966.1226863 [DOI] [PubMed] [Google Scholar]
- 25.Hagger MS, Weed M. DEBATE: Do interventions based on behavioral theory work in the real world? Int J Behav Nutr Phys Act. 2019;16(36):1–10. doi: 10.1186/s12966-019-0795-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fisher JD, Misovich SJ, Kimble DL, Fisher WA, Malloy TE. Changing AIDS risk behavior: Effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Heal Psychol. 1996;15(2):114–123. [DOI] [PubMed] [Google Scholar]
- 27.Goodell LS, Pierce MB, Amico KR, Ferris AM. Parental information, motivation, and behavioral skills correlate with child sweetened beverage consumption. J Nutr Educ Behav. 2012;44(3):240–245. doi: 10.1016/j.jneb.2010.07.012 [DOI] [PubMed] [Google Scholar]
- 28.Liu Z, Wei P, Huang M, Liu YB, Li L, Gong X, et al. Determinants of consistent condom use among college students in China: Application of the information-motivation-behavior skills (IMB) Model. PLoS One. 2014;9(9):e108976. doi: 10.1371/journal.pone.0108976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith JJ, Jain J, Ananda S, Sadhu B. Assessment of effect of health song on oral hygiene status among visually impaired children. J Indian Assoc Public Heal Dent. 2022;20(4):352. [Google Scholar]
- 30.Sheffield D, Irons JY. Songs for health education and promotion: a systematic review with recommendations. Public Health. 2021;198:280–289. doi: 10.1016/j.puhe.2021.07.020 [DOI] [PubMed] [Google Scholar]
- 31.Shetty V, Hegde AM, Varghese E, Shetty V. A Novel Music based Tooth Brushing System for Blind Children. J Clin Pediatr Dent. 2013;37(3):251–256. doi: 10.17796/jcpd.37.3.28v62k5114659g62 [DOI] [PubMed] [Google Scholar]
- 32.Hallam S. The power of music: Its impact on the intellectual, social and personal development of children and young people. Int J Music Educ. 2010;28(3):269–289. doi: 10.1177/0255761410370658 [DOI] [Google Scholar]
- 33.Nicholson JM, Berthelsen D, Abad V, Williams K, Bradley J. Impact of music therapy to promote positive parenting and child development. J Health Psychol [Internet]. 2008. Mar 1 [cited 2023 Apr 9];13(2):226–238. doi: 10.1177/1359105307086705 [DOI] [PubMed] [Google Scholar]
- 34.City Population. Oyo State, Nigeria [Internet]. Population Statistics, Charts, Map and Location. 2022 [cited 2022 Jan 10]. https://www.citypopulation.de/php/nigeria-admin.php?adm1id=NGA031
- 35.Federal Ministry of Education. Ondo State—Basic Schools List [Internet]. Open Education Data (OED), Nigeria. 2020 [cited 2023 Apr 10]. p. 2–3. http://fmebasic.intellisys.xyz/index.php/states-stats/plateau/52-states/oyo/169-oyo-state-basic-schools-list
- 36.Gabriel AOI. Historical analysis of federal government innovations in early childhood education in Nigeria, 1977–2008. Int J Acad Res Bus Soc Sci. 2013;3(1):63–84. [Google Scholar]
- 37.Ejieh MUC. Pre-primary education in Nigeria: Policy implementation and problems. Elem Educ Online. İlköğretim Online. 2006;5(1):58–64. [Google Scholar]
- 38.Sandström A, Cressey J, Stecksén-Blicks C. Tooth-brushing behaviour in 6–12 year olds. Int J Paediatr Dent. 2011. Jan 1;21(1):43–49. doi: 10.1111/j.1365-263X.2010.01080.x [DOI] [PubMed] [Google Scholar]
- 39.Chua DR, Hu S, Sim YF, Lim W, Lai BWP, Hong CHL. At what age do children have the motor development to adequately brush their teeth? Int J Paediatr Dent. 2022. Jul 1;32(4):598–606. doi: 10.1111/ipd.12938 [DOI] [PubMed] [Google Scholar]
- 40.de Leeuw E, Borgers N, Smits A. Pretesting Questionnaires for Children and Adolescents. In: Presser S, Rothgeb JM, Couper MP, Lessler JT, Martin E, Martin J, et al., editors. Methods for Testing and Evaluating Survey Questionnaires. New Jersey: John Wiley & Sons, Ltd; 2004. p. 409–29. [Google Scholar]
- 41.Kirkwood BR, Sterne JAC. Measurement error: assessment and implications. In: Goodgame F, Pinder V, Moore K, editors. Essential Medical Statistics. Second. Massachusetts: Blackwell Publishing Ltd; 2006. p. 429–446. [Google Scholar]
- 42.Folayan MO, Kolawole KA, Onyejaka NK, Agbaje HO, Chukwumah NM, Oyedele TA. General anxiety, dental anxiety, digit sucking, caries and oral hygiene status of children resident in a semi-urban population in Nigeria. BMC Oral Health. 2018;18(1):66–76. doi: 10.1186/s12903-018-0529-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kang M, Ragan BG, Park JH. Issues in outcomes research: An overview of randomization techniques for clinical trials. J Athl Train. 2008;43(2):215–221. doi: 10.4085/1062-6050-43.2.215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sealed Envelope Ltd. 2022. Create a blocked randomisation list. [Online] https://www.sealedenvelope.com/simple-randomiser/v1/lists [Accessed 19 Apr 2023].
- 45.Lawal FB, Oke GA. Clinical and sociodemographic factors associated with oral health knowledge, attitude, and practices of adolescents in Nigeria. SAGE Open Med. 2020. Jul 24;8:1–8. doi: 10.1177/2050312120951066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.World Health Organization. Oral Health Surveys: Basic Methods. 5th ed. Peterson PE, Baez RJ, editors. World Health Organization. Geneva, Switzerland: World Health Organization; 2013. 1–137 p. [Google Scholar]
- 47.Greene JC, Vermillion JR. The Simplified Oral Hygiene Index. J Am Dent Assoc. 1964. Jan;68(1):7–13. doi: 10.14219/jada.archive.1964.0034 [DOI] [PubMed] [Google Scholar]
- 48.Namal N, Vehid S, Sheiham A. Ranking countries by dental status using the DMFT and FS-T indices. Int Dent J. 2005. Dec 1;55(6):373–376. doi: 10.1111/j.1875-595x.2005.tb00049.x [DOI] [PubMed] [Google Scholar]
- 49.Ibiyemi O, Lawal F, Osuh M, Owoaje T, Idiga E, Fagbule O, et al. Developing an Oral Hygiene Education Song for Children and Teenagers in Nigeria. Int Dent J [Internet]. 2022. Jul 30; Available from: doi: 10.1016/j.identj.2022.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lawal F, Taiwo J. An audit of school oral health education program in a developing country. J Int Soc Prev Community Dent. 2014. Nov 1;4(4):S49–55. doi: 10.4103/2231-0762.144600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.White IR, Horton NJ, Carpenter J, Pocock SJ. Strategy for intention to treat analysis in randomised trials with missing outcome data. BMJ. 2011. Feb 7;342(7803):910–912. doi: 10.1136/bmj.d40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nzewi M. Folk music in Nigeria: a communion. African Music. 1980. Jul 1;6(1):6–21. [Google Scholar]
- 53.Ojukwu E, Obielozie E, Esimone C. Nigerian values and contemporary popular music: a new look. Ogirisi a New J African Stud. 2016. Jul 21;12:114–129. [Google Scholar]
- 54.Benjamin-Chung J, Arnold BF, Berger D, Luby SP, Miguel E, Colford JM, et al. Spillover effects in epidemiology: Parameters, study designs and methodological considerations. Int J Epidemiol. 2018. Feb 1;47(1):332–347. doi: 10.1093/ije/dyx201 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
Data Availability Statement
No datasets were generated or analysed during the current study. All relevant data from this study will be made available upon study completion.


