Highlights
-
•
People with legal involvement had higher odds of treatment in acute settings.
-
•
People with housing instability had higher odds of treatment in acute settings.
-
•
Opioid use treatment in a doctor's office was associated with receiving medication.
Keywords: Criminal legal involvement, Homelessness, Opioid use disorder, MOUD, Substance use treatment
Abstract
Background
Individuals with criminal legal involvement (CLI), housing instability, or Medicaid insurance may experience barriers accessing substance use treatment in certain settings. Previous research has found individuals in these groups are less likely to receive medications for opioid use disorder (MOUD), but the role treatment setting may play in low rates of MOUD is unclear.
Methods
We conducted a cross-sectional study using nationally representative survey data from 2015 to 2021. We estimated the proportion of individuals who had CLI, housing instability, or Medicaid insurance who received substance use treatment in a variety of settings. We used multivariable logistic regressions to estimate the associations between group and the receipt of MOUD across treatment settings.
Results
Individuals with CLI, housing instability, or Medicaid insurance were more likely to receive substance use treatment in hospitals, rehabilitation, and mental health facilities compared with individuals not in these groups. However, all groups accessed substance use treatment in doctors’ offices at similar rates. Treatment at a doctor's office was associated with the highest likelihood of receiving MOUD (aOR 4.73 [95% CI: 2.2.15-10.43]). Across multiple treatment settings, Individuals with CLI or housing instability were less likely to receive MOUD.
Conclusions
Individuals with CLI, housing instability, or Medicaid insurance are more likely to access substance use treatment at locations associated with lower rates of MOUD use. MOUD access across treatment settings is needed to improve engagement and retention in treatment for patients experiencing structural disadvantage or who have low incomes.
1. Introduction
Individuals who experience criminal legal involvement (CLI) and/or housing instability have higher rates of opioid use and mortality than the general population (Winkelman et al., 2018). Opioid-related risks are compounded by lower rates of medication for opioid use disorder (MOUD) among these groups (Finlay et al., 2021). Additionally, people experiencing CLI and/or housing instability are primarily insured through Medicaid, which may be associated with barriers to MOUD (Knudsen and Studts, 2019). Higher rates of opioid-related mortality may, in part, be due to unique barriers to treatment such as transportation, lapses in health insurance, stigma, trauma, comorbid mental health diagnosis, restrictive treatment guidelines, and limited care coordination during release from incarceration (Englander et al., 2022; Howell et al., 2022; Hyshka et al., 2017).
Substance use treatment can be provided in different settings including hospitals, rehabilitation facilities, mental health facilities, SAMHSA-certified opioid treatment programs (OTP), and primary care practices. The referral system for substance use treatment is disjointed and difficult to navigate, which may affect where patients receive care (Blevins et al., 2018). Additionally, MOUD access may vary across settings and states. For example, only 18 states have requirements for the use of MOUD in residential treatment facilities (O'Brien et al., 2022). Within specialty substance use treatment facilities, MOUD is more common in outpatient than residential or detoxification facilities (Dunn et al., 2019; Hartung et al., 2022). However, little is known about where individuals with CLI, housing instability, or Medicaid insurance access treatment and whether treatment patterns are related to MOUD use.
Understanding where individuals with OUD receive treatment can help inform efforts to expand access to MOUD for individuals with CLI and/or housing instability. In this study we used nationally representative data to describe past year substance use treatment rates at a variety of treatment settings among individuals with opioid use treatment need. We also explored whether CLI, housing instability, or Medicaid insurance was associated with rates of MOUD in each treatment setting.
2. Methods
2.1. Data source
For this analysis we pooled 2015-2021 data from the National Survey on Drug Use and Health (NSDUH). The NSDUH is a nationally representative survey of non-institutionalized US population aged 12 years and older. It provides information on substance use, receipt of treatment, social determinants of health, and demographic characteristics. In 2019, the NSDUH survey added questions about whether an individual received MOUD in the past year. This change did not affect the variables used to identify the study population, key groups, or treatment setting. In 2021, the NSDUH was redesigned so that substance use disorders were defined using the Diagnostic and Statistical Manual of Mental Disorders (DSM)-V criteria. Additionally, the redesign changed how questions were asked about the receipt of treatment for specific substances in the past year. These changes affected the variables we used to identify the study population using 2021 data but did not affect the identification of key groups. Prior to 2020, interviews were conducted in-person using computer assisted instruction and audio computer assisted self-interview for sensitive topics. Beginning in 2020, the interview was conducted both in-person and virtually.
2.2. Study sample
Our study sample included adults aged 18 and older with treatment need for opioid use. We defined treatment need for opioid use as meeting DSM criteria and/or having received recent treatment for opioid use. Using 2015-2020 data, we identified respondents meeting DSM-IV criteria for opioid abuse or dependence and/or who's last substance use treatment was for heroin or prescription pain relievers. Using 2021 data, we identified respondents meeting DSM-V criteria for heroin or prescription pain reliever use disorder and/or who received treatment for heroin or prescription pain reliever use in the past year.
2.3. Criminal legal involvement, housing instability, and Medicaid insurance
We created non-mutually exclusive binary indicators for individuals with CLI, housing instability, or Medicaid insurance in the past year. CLI was defined as any arrests, probation, or parole in the past year. Housing instability was defined as moving 3 or more times in the past year. For comparison we created a “no-barrier” group defined as not having CLI, housing instability, or Medicaid insurance in the past year.
2.4. Substance use treatment
Using 2015-2021 data we determined whether an individual received past year illicit substance (does not include alcohol) use treatment in each setting. We generated non-mutually exclusive binary indicators for whether an individual received substance use treatment in a hospital (inpatient and/or emergency department), rehabilitation facility (inpatient and/or outpatient), mental health facility, or doctor's office in the past year. Using 2019-2021 data, we generated a binary indicator for whether respondents received MOUD in the past year. This information was not available in before 2019.
2.5. Sociodemographic variables
The sociodemographic characteristics we used in this study included sex (female and male), race/ethnicity (Black, White, Other, and Hispanic), age (18-25, 26-34, 35-49, and 50+), income (<100% federal poverty line [FPL], 100-200% FPL, and >200% FPL), and residence (rural and urban). Race and ethnicity groups were mutually exclusive with the “other” category including Asian/Pacific Islander, Native American, and multiple race categories. Income classification was based on the total reported family size and income. Residence was determined using 2013 Rural/Urban continuum codes, with rural defined as living in a nonmetro county.
2.6. Statistical analysis
We first tabulated the sociodemographic characteristics of respondents with a treatment need for opioid use in each group (i.e., CLI, housing instability, Medicaid, no barrier). Next, we tabulated the proportion of individuals with opioid treatment need who received treatment in each treatment setting by group. Then, we assessed associations between CLI, housing instability, Medicaid, and sociodemographic characteristics and receipt of treatment in each specific setting. We estimated the adjusted odds ratios of receiving treatment in each specific setting for individuals experiencing CLI, housing instability, and/or Medicaid insurance using separate multivariable logistic regressions for each setting.
Next, using 2019-2021 data we assessed associations with the receipt of MOUD. First, we estimated the overall relationship between treatment setting, group (i.e., CLI, housing instability, Medicaid insurance), and receipt of MOUD. Among all individuals who received any treatment we estimated the adjusted odds ratio of receiving MOUD using a multivariable logistic regression. To further explore the associations between group and the receipt of MOUD we next estimated separate multivariable logistic regressions for individuals who received treatment at each specific treatment setting. All analysis were adjusted for individuals’ sex, race and ethnicity, age, income, and rural residence. We repeated these analyses, excluding 2021 data, in a sensitivity analysis to assess whether the survey design changes effected our findings. All analysis used appropriate weights to account for NSDUH's complex survey design.
3. Results
3.1. Sociodemographic characteristics
Using 2015-2021 NSDUH data, we identified 3,535 adults with a treatment need for opioid use. Of these respondents 1,084 had past year CLI, 410 experienced unstable housing, 1,600 had Medicaid insurance, and 1,487 experienced none of these barriers in the past year (Table 1). This sample represented an annualized weighted totals for each group of 691,000 (95% CI: 623,000-759,000), 250,000 (95% CI: 212,000-287,000), 1,076,000 (95% CI: 986,000-1,166,000), and 1,187,000 (95% CI: 1,069,000-1,306,000), respectively.
Table 1.
Sociodemographic characteristics of study population by criminal legal involvement, unstable housing, and Medicaid insurance—United States, 2015-2021
| Weighted % (95% CI) |
||||
|---|---|---|---|---|
| Characteristic | Criminal Legal Involvement n=1084 |
Unstable Housing n=410 |
Medicaid Insurance n=1,600 |
No Barrier n=1487 |
| Weighted Sample Size | 691,000 (623,000-759,000) |
250,000 (212,000-287,000) |
1,076,000 (986,000-1,166,000) |
1,187,000 (1,069,000-1,306,000) |
| Sex | ||||
| Female | 41.4% (36.0-47.1) | 46.6% (38.3-55.0) | 53.5% (49.7-57.2) | 38.4% (34.1-42.9) |
| Male | 58.6% (52.9-64.1) | 53.5% (45.0-61.7) | 46.6% (42.8-50.4) | 61.6% (57.1-65.9) |
| Race/Ethnicity | ||||
| Black | 10.1% (7.3-14.0) | 16.8% (10.4-26.1) | 11.2% (8.7-14.3) | 8.2% (5.6-11.7) |
| White | 72.0% (66.8-76.7) | 61.0% (51.9-69.3) | 70.2% (66.1-73.9) | 77.5% (73.2-81.3) |
| Other | 7.6% (5.2-11.1) | 8.2% (4.9-13.4) | 7.1% (5.2-9.5) | 3.8% (2.5-5.5) |
| Hispanic | 10.2% (7.8-13.4) | 14.1% (8.3-22.7) | 11.6% (9.0-15.0) | 10.6% (7.8-14.2) |
| Age | ||||
| 18-25 | 17.6% (15.1-20.3) | 23.5% (18.9-28.8) | 10.9% (9.2-12.9) | 13.5% (12.0-15.1) |
| 26-34 | 33.3% (29.2-37.8) | 30.2% (23.3-38.2) | 29.1% (25.4-33.2) | 23.2% (20.4-26.3) |
| 35-49 | 32.4% (27.7-37.5) | 22.2% (16.8-28.6) | 34.2% (30.3-38.3) | 30.3% (27.5-33.2) |
| 50+ | 16.7% (11.7-23.2) | 24.2% (16.4-34.1) | 25.8% (21.2-31.0) | 33.1% (28.9-37.6) |
| Income | ||||
| <100% FPLa | 45.0% (39.1-51.1) | 50.5% (42.1-58.8) | 50.4% (45.9-54.9) | 13.1% (10.5-16.4) |
| 100-200% FPL | 24.6% (21.1-28.4) | 20.9% (15.7-27.2) | 28.1% (25.6-30.8) | 21.0% (18.2-24.2) |
| >200% FPL | 30.4% (24.7-36.7) | 28.7% (21.9-36.5) | 21.5% (18.0-25.4) | 65.8% (62.6-69.0) |
| Residence | ||||
| Rural | 18.2% (15.1-21.8) | 16.7% (10.9-24.7) | 16.7% (13.8-20.0) | 14.1% (11.8-16.8) |
| Urban | 81.8% (78.2-84.9) | 83.3% (75.3-89.1) | 83.4% (80.0-86.3) | 85.9% (83.2-88.2) |
Federal Poverty Line
A majority of individuals with past year CLI, unstable housing, or no barrier where male while a higher proportion of individuals with Medicaid insurance were female (53.5%; 95% CI: 49.7-57.2) (Table 1). Individuals experiencing CLI or housing instability were more likely to be age 18-25 (17.6%; 95% CI: 15.1-20.3 and 23.5%; 95% CI: 18.9-28.8, respectively) or 26-34 (33.3%; 95% CI: 29.2-37.8 and 30.2%; 95% CI: 23.3-38.2, respectively) compared to individuals experiencing neither barrier (13.5%; 95% CI: 10.5-16.4 and 23.2%; 95% CI: 20.4-26.3). A substantially higher percentage of individuals experiencing CLI (45.0%; 95% CI: 39.1-51.1), housing instability (50.5%; 95% CI: 42.1-58.8), and Medicaid insurance (50.4%; 95% CI: 45.9-54.9) had incomes below the FPL compared to individuals in the no-barrier group (13.1%; 95% CI: 10.5-16.4).
3.2. Treatment setting
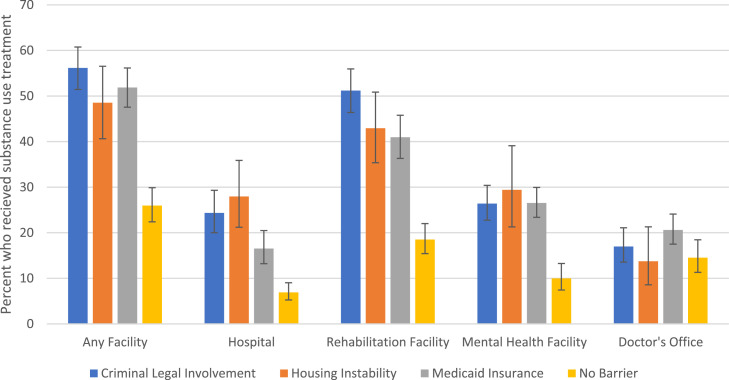
A larger proportion of individuals with opioid treatment need and CLI (56.2% [95% CI: 51.4-60.8]), housing instability (48.5% [95% CI: 40.6-56.5]), or Medicaid insurance (51.9% [95% CI: 47.6-56.2]) reported receiving substance use treatment in the past year than individuals not in these groups (26.0% [95% CI: 22.4-29.9]) (Fig. 1). This difference was most pronounced at rehabilitation facilities where 51.2% (95% CI: 46.4-56.0%) of all individuals with CLI and 42.9% (95% CI: 35.4-50.9%) of all individuals with housing instability received treatment but only 18.5% (95% CI: 15.4-22.0%) of individuals with neither received treatment. Despite differences in overall treatment rates, all groups received treatment in doctors’ offices at similar rates (ranging from 13.8% to 20.6%). Excluding 2021 data did not affect the proportion of individuals who received treatment in each setting (Supplementary Figure 1).
Fig. 1.
Percent of individuals with criminal legal involvement, housing instability, and Medicaid insurance who received substance use treatment in each treatment setting—United States, 2015-2021
Both past year CLI (aOR: 2.01; 95% CI: 1.57-2.58) and Medicaid insurance (aOR: 2.03; 95% CI: 1.62-2.55) were associated with increased odds of receiving any substance use treatment (Table 2). Compared to White respondents, Black (aOR: 0.46; 95% CI: 0.28-0.75), Hispanic (aOR: 0.62; 95% CI: 0.39-0.98), and respondents of another race (aOR: 0.48; 95% CI: 0.28-0.81) were less likely to receive any substance use treatment. Housing instability was associated with increased odds of receiving substance use treatment in a hospital (aOR: 2.32; 95% CI: 1.51-3.56) and mental health facility (aOR: 1.77; 95% CI: 1.07-2.94). Similarly, past year CLI was associated with increased odds of treatment in all settings except a doctor's office. Medicaid insurance was associated with increased odds of treatment in all settings except a hospital. Income was not a statistically significant predictor of receipt of treatment in any treatment setting.
Table 2.
Association of sociodemographic characteristics with treatment location—United States, 2015-2021
| Adjusted Odds Ratio of receiving treatment at each setting (95% CI) |
|||||
|---|---|---|---|---|---|
| Characteristic | Any Treatment | Hospital | Rehabilitation Facility | Mental Health Facility | Doctor's Office |
| Housing | |||||
| Stable | Ref | Ref | Ref | Ref | Ref |
| Unstable | 1.28 (0.86-1.92) | 2.32 (1.51-3.56)a | 1.40 (0.97-2.03) | 1.77 (1.07-2.94)c | 0.85 (0.48-1.50) |
| CLId | |||||
| No PY CLI | Ref | Ref | Ref | Ref | Ref |
| PY CLI | 2.01 (1.57-2.58)a | 2.81 (1.93-4.10)a | 2.68 (2.08-3.47)a | 1.49 (1.07-2.08)c | 0.90 (0.66-1.22) |
| Insurance | |||||
| No PY Medicaid | Ref | Ref | Ref | Ref | Ref |
| PY Medicaid | 2.03 (1.62-2.55)a | 1.39 (0.95-2.03) | 1.78 (1.38-2.30)a | 2.17 (1.67-2.83)a | 1.63 (1.20-2.21)b |
| Sex | |||||
| Male | Ref | Ref | Ref | Ref | Ref |
| Female | 0.98 (0.77-1.25) | 1.11 (0.73-1.67) | 1.00 (0.76-1.32) | 1.03 (0.81-1.31) | 1.14 (0.81-1.61) |
| Race | |||||
| White | Ref | Ref | Ref | Ref | Ref |
| Black | 0.46 (0.28-0.75)b | 0.90 (0.47-1.72) | 0.57 (0.36-0.90)c | 0.53 (0.30-0.92)c | 0.25 (0.10-0.62)b |
| Other | 0.48 (0.28-0.81)b | 0.86 (0.39-1.91) | 0.57 (0.33-1.01) | 0.78 (0.40-1.53) | 0.33 (0.17-0.64)b |
| Hispanic | 0.62 (0.39-0.98)c | 0.92 (0.58-1.47) | 0.54 (0.34-0.86)c | 0.84 (0.49-1.42) | 0.69 (0.35-1.36) |
| Age | |||||
| 18-25 | Ref | Ref | Ref | Ref | Ref |
| 26-34 | 1.68 (1.35-2.08)a | 1.08 (0.71-1.63) | 1.44 (1.14-1.83)b | 1.35 (1.03-1.76)c | 2.09 (1.42-3.05)a |
| 35-49 | 1.73 (1.31-2.28)a | 0.96 (0.65-1.41) | 1.47 (1.08-2.00)c | 1.43 (1.03-1.97)c | 1.88 (1.28-2.76)b |
| 50+ | 0.97 (0.61-1.51) | 1.00 (0.54-1.87) | 0.81 (0.50-1.29) | 0.91 (0.54-1.54) | 1.26 (0.68-2.33) |
| Income | |||||
| <100% FPLe | Ref | Ref | Ref | Ref | Ref |
| 100-200% FPL | 0.73 (0.49-1.06) | 0.95 (0.64-1.42) | 0.80 (0.57-1.13) | 0.81 (0.55-1.21) | 0.70 (0.43-1.13) |
| >200% FPL | 0.78 (0.54-1.14) | 0.89 (0.59-1.33) | 0.75 (0.53-1.06) | 0.90 (0.61-1.33) | 0.99 (0.59-1.67) |
| Residence | |||||
| Urban | Ref | Ref | Ref | Ref | Ref |
| Rural | 0.80 (0.60-1.08) | 0.55 (0.34-0.87)c | 0.90 (0.68-1.18) | 0.70 (0.48-1.01) | 1.17 (0.0.82-1.68) |
P<0.001
P<0.01
P<0.05
Criminal Legal Involvement
Federal Poverty Line
3.3. Receipt of medication for opioid use disorder
Among all treated individuals from 2019-2021, substance use treatment at a doctor's office was associated with increased odds of receiving MOUD (aOR: 4.73; 95% CI: 2.15-10.43) (Table 3). Receiving substance use treatment in a hospital, rehabilitation facility, or mental health facility was not associated with the receipt of MOUD. Experiencing past year CLI was associated with lower odds of receiving MOUD (aOR: 0.23; 95% CI: 0.11-0.49). Housing instability was also associated with lower odds (aOR: 0.32; 95% CI: 0.10-1.01), but this finding was not statistically significant (P=0.053). Other sociodemographic characteristics were not associated with the receipt of MOUD.
Table 3.
Association of treatment location and sociodemographic characteristics with receipt of medications for opioid use disorder among all treated individuals—United States, 2019-2021
| aOR of Receiving MOUD (95% CI) n=581 |
|
|---|---|
| Hospital | |
| No past year treatment | Ref |
| Past year SUD treatment | 0.70 (0.29-1.70) |
| Rehabilitation Facility | |
| No past year treatment | Ref |
| Past year SUD treatment | 1.83 (0.65-5.16) |
| Mental Health Facility | |
| No past year treatment | Ref |
| Past year SUD treatment | 0.86 (0.48-1.57) |
| Doctor's Office | |
| No past year treatment | Ref |
| Past year SUD treatment | 4.73 (2.15-10.43)a |
| Housing | |
| Stable | Ref |
| Unstable | 0.32 (0.10-1.01) |
| CLIb | |
| No PY CLI | Ref |
| PY CLI | 0.23 (0.11-0.49)a |
| Insurance | |
| No PY Medicaid | Ref |
| PY Medicaid | 1.73 (0.86-3.48) |
| Sex | |
| Male | Ref |
| Female | 0.87 (0.10-1.01) |
| Race | |
| White | Ref |
| Black | 0.40 (0.94-1.73) |
| Other | 2.61 (0.78-8.77) |
| Hispanic | 0.90 (0.30-2.74) |
| Age | |
| 18-25 | Ref |
| 26-34 | 2.15 (0.85-5.47) |
| 35-49 | 1.63 (0.70-3.79) |
| 50+ | 1.35 (0.39-4.69) |
| Income | |
| <100% FPLc | Ref |
| 100-200% FPL | 1.05 (0.51-2.17) |
| >200% FPL | 1.61 (0.65-3.95) |
| Residence | |
| Urban | Ref |
| Rural | 0.54 (0.24-1.21) |
P<0.001
Criminal Legal Involvement
Federal Poverty Line
Among individuals treated in doctors’ offices, experiencing housing instability was associated with reduced likelihood of receiving MOUD (aOR: 0.10; 95% CI: 0.02-0.43) (Table 4). Housing instability was also associated with reduced odds of receiving MOUD among individuals treated in hospitals (aOR: 0.09; 95% CI: 0.02-0.46) and rehabilitation facilities (aOR: 0.28; 95% CI: 0.08-0.96). The association with reduced odds of receiving MOUD among those treated in mental health facilities (aOR: 0.34; 95% CI: 0.11-1.01) was not statistically significant (p=0.053). Similarly, experiencing criminal legal involvement was associated with reduced odds of receiving MOUD among individuals treated in rehabilitation (aOR: 0.26; 95% CI: 0.12-0.57) or mental health facilities (aOR: 0.22; 95% CI: 0.09-0.59). Individuals with Medicaid insurance received MOUD at similar rates to those without Medicaid insurance across types of treatment setting. In a sensitivity analysis excluding 2021 data the standard errors were larger, reducing statistical significance, but the odds ratio estimates were largely unaffected (Supplementary Tables 3 and 4).
Table 4.
Association of sociodemographic characteristics with receipt of medications for opioid use disorder, among individuals treated in each specific treatment setting—United States, 2019-2021
| Adjusted Odds Ratio of receiving MOUD (95% CI) |
||||
|---|---|---|---|---|
| Hospital n=175 |
Rehabilitation Facility n=466 |
Mental Health Facility n=314 |
Doctor's Office n=251 |
|
| Housing | ||||
| Stable | Ref | Ref | Ref | Ref |
| Unstable | 0.09 (0.02-0.46)a | 0.28 (0.08-0.96)b | 0.34 (0.11-1.01) | 0.10 (0.02-0.43)a |
| CLIc | ||||
| No PY CLI | Ref | Ref | Ref | Ref |
| PY CLI | 1.18 (0.39-3.54) | 0.26 (0.12-0.57)a | 0.22 (0.09-0.59)a | 0.72 (0.18-2.89) |
| Insurance | ||||
| No PY Medicaid | Ref | Ref | Ref | Ref |
| PY Medicaid | 1.19 (0.42-3.38) | 1.92 (0.95-3.88) | 2.32 (0.89-6.06) | 1.13 (0.35-3.60) |
| Sex | ||||
| Male | Ref | Ref | Ref | Ref |
| Female | 0.24 (0.08-0.75)b | 0.78 (0.39-1.54) | 0.75 (0.32-1.77) | 0.73 (0.28-1.94) |
| Race | ||||
| White | Ref | Ref | Ref | Ref |
| Black | 1.46 (0.06-33.52) | 0.39 (0.09-1.74) | 0.17 (0.03-1.05) | 0.08 (0.01-0.59)a |
| Other | 4.60 (0.84-25.18) | 3.47 (0.1.04-11.64)b | 4.06 (1.20-13.76) | 0.35 (0.06-1.91) |
| Hispanic | 0.76 (0.19-3.10) | 0.71 (0.21-2.40) | 0.36 (0.09-1.44) | 1.22 (0.25-5.89) |
| Age | ||||
| 18-25 | Ref | Ref | Ref | Ref |
| 26-34 | 2.32 (0.58-9.40) | 1.95 (0.71-5.34) | 2.45 (0.76-7.84) | 1.25 (0.23-6.90) |
| 35-49 | 1.30 (0.38-4.43) | 1.74 (0.73-4.17) | 1.94 (0.65-5.78) | 0.87 (0.17-4.32) |
| 50+ | 0.04 (0.00-0.31) a | 0.89 (0.24-3.28) | 4.26 (0.70-25.71) | 1.29 (0.17-9.90) |
| Income | ||||
| <100% FPLd | Ref | Ref | Ref | Ref |
| 100-200% FPL | 1.23 (0.41-3.67) | 1.12 (0.53-2.37) | 1.06 (0.40-2.81) | 0.89 (0.32-2.52) |
| >200% FPL | 0.58 (0.17-1.99) | 1.57 (0.62-3.97) | 3.70 (1.08-12.64)b | 0.99 (0.30-3.29) |
| Residence | ||||
| Urban | Ref | Ref | Ref | Ref |
| Rural | 0.14 (0.03-0.59)a | 0.48 (0.20-1.15) | 1.28 (0.33-4.95) | 0.0 (0.19-2.58) |
P<0.01
P<0.05
Criminal Legal Involvement
Federal Poverty Line
Regressions included controls for other treatment settings.
4. Discussion
We found that individuals with CLI, housing instability, or Medicaid insurance received substance use treatment in hospitals, rehabilitation, and mental health facilities at higher rates than individuals not in these groups, but all groups had similar treatment rates at doctor's offices. Incarceration or housing instability may interrupt care and reduce the likelihood of having a primary care physician, receiving care in outpatient settings, and being prescribed MOUD (Joudrey et al., 2019). We also found that Doctors’ offices were the only treatment setting associated with increased odds of receiving MOUD. Overall, individuals experiencing CLI or housing instability have higher substance use treatment rates, but in settings less likely to provide standard of care. Thus, among those treated, receipt of MOUD is much lower compared with individuals not experiencing CLI or housing instability.
We also showed that low rates of MOUD among individuals experiencing CLI or housing instability were not only due to accessing different treatment settings, but lower odds of receiving MOUD. We build on previous research that describes treatment disparities at specialty substance use treatment facilities, by showing these inequities persist across multiple treatment settings (Han et al., 2022; Shearer et al., 2022; Stahler et al., 2022). This could be due to factors such as prescribers’ perceptions of MOUD adherence and stigmatizing views of CLI and housing instability (Howell et al., 2022).
Currently, substance use treatment for people experiencing CLI and housing instability is disruptive and more often in acute settings. Care transitions from incarceration and hospitalization should prioritize minimally disruptive models of care and programs that provide comprehensive primary care, MOUD, and address barriers associated with CLI and housing instability (Englander et al., 2022; Shavit et al., 2017). Alternatively, increasing Medicaid reimbursement rates or providing financial incentives for quality measures could increase MOUD access across settings.
4.1. Limitations
This study has limitations, which may impact the interpretation of the results. In 2021, the NSDUH underwent substantial changes which may affect the identification of individuals with treatment need for opioid use who are included in the study. However, these changes are less likely to bias the associations between group (i.e., CLI, housing instability, or Medicaid insurance) and treatment location or receipt of MOUD. We also conducted a sensitivity analysis excluding 2021 data to assess whether the survey changes substantially effected our results. Because the NSDUH survey does not specify where individuals received MOUD we included controls for receipt of treatment at other locations when estimating the association between group and receipt of MOUD among individuals treated at each location. Additionally, the NSDUH relies on self-report which could affect our findings if individuals do not remember, report, or misclassify the location(s) where they received treatment. However, this is unlikely to bias results between groups. The NSDUH does not sample individuals currently experiencing homelessness and so we created a proxy for housing instability.
Conclusion
In a nationally representative sample of individuals with opioid use treatment need, we found substantial differences in the types of treatment facilities accessed by individuals experiencing CLI, housing instability, Medicaid insurance, and those not in these groups. Individuals experiencing CLI or housing instability had higher treatment rates in settings that offered less MOUD and were less likely to receive MOUD across multiple treatment settings. Linkage to treatment should prioritize low-barrier settings which provide continued access to MOUD for individuals with CLI or housing instability.
Role of funding
Riley D Shearer was supported by NIH MSTP grant T32 GM008244.
CRediT authorship contribution statement
Riley D. Shearer: Conceptualization, Methodology, Formal analysis, Data curation, Writing – original draft. Benjamin A. Howell: Conceptualization, Methodology, Writing – review & editing. Utsha G. Khatri: Conceptualization, Methodology, Resources, Writing – review & editing. Tyler N.A. Winkelman: Conceptualization, Methodology, Writing – review & editing, Supervision.
Declaration of Competing Interest
None
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.dadr.2023.100179.
Appendix. Supplementary materials
References
- Blevins C.E., Rawat N., Stein M.D. Gaps in the substance use disorder treatment referral process: provider perceptions. J. Addict. Med. 2018;12:273–277. doi: 10.1097/ADM.0000000000000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn K.E., Huhn A.S., Strain E.C. Differential adoption of opioid agonist treatments in detoxification and outpatient settings. J. Subst. Abuse Treat. 2019;107:24–28. doi: 10.1016/j.jsat.2019.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Englander H., Gregg J., Levander X.A. Envisioning minimally disruptive opioid use disorder care. J. Gen. Intern. Med. 2022:1–5. doi: 10.1007/s11606-022-07939-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay A.K., Harris A.H.S., Timko C., Yu M., Smelson D., Stimmel M., Binswanger I.A. Disparities in access to medications for opioid use disorder in the veterans health administration. J. Addict. Med. 2021;15:143–149. doi: 10.1097/ADM.0000000000000719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B.H., Doran K.M., Krawczyk N. National trends in substance use treatment admissions for opioid use disorder among adults experiencing homelessness. J. Subst. Abuse Treat. 2022;132 doi: 10.1016/j.jsat.2021.108504. [DOI] [PubMed] [Google Scholar]
- Hartung D.M., Markwardt S., Johnston K., Geddes J., Baker R., Leichtling G., Hildebran C., Chan B., Cook R.R., McCarty D., Ghitza U., Korthuis P.T. Association between treatment setting and outcomes among Oregon Medicaid patients with opioid use disorder: a retrospective cohort study. Addict. Sci. Clin. Pract. 2022;17:45. doi: 10.1186/s13722-022-00318-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell B.A., Earnshaw V.A., Garcia M., Taylor A., Martin K., Fox A.D. The stigma of criminal legal involvement and health: a conceptual framework. J. Urban Health. 2022;99:92–101. doi: 10.1007/s11524-021-00599-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyshka E., Anderson J.T., Wild T.C. Perceived unmet need and barriers to care amongst street-involved people who use illicit drugs. Drug Alcohol Rev. 2017;36:295–304. doi: 10.1111/dar.12427. [DOI] [PubMed] [Google Scholar]
- Joudrey P.J., Khan M.R., Wang E.A., Scheidell J.D., Edelman E.J., McInnes D.K., Fox A.D. A conceptual model for understanding post-release opioid-related overdose risk. Addict. Sci. Clin. Pract. 2019;14:17. doi: 10.1186/s13722-019-0145-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudsen H.K., Studts J.L. Physicians as mediators of health policy: acceptance of Medicaid in the context of buprenorphine treatment. J. Behav. Health Serv. Res. 2019;46:151–163. doi: 10.1007/s11414-018-9629-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien M.L., Stewart M.T., Shields M.C., White M., Dubenitz J., Dey J., Mulvaney-Day N. Residential treatment and medication treatment for opioid use disorder: The role of state Medicaid innovations in advancing the field. Drug Alcohol Depend. Rep. 2022 doi: 10.1016/j.dadr.2022.100087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shavit S., Aminawung J.A., Birnbaum N., Greenberg S., Berthold T., Fishman A., Busch S.H., Wang E.A. Transitions clinic network: challenges and lessons in primary care for people released from prison. Health Aff. 2017;36:1006–1015. doi: 10.1377/hlthaff.2017.0089. [DOI] [PubMed] [Google Scholar]
- Shearer R.D., Shippee N.D., Vickery K.D., Stevens M.A., Winkelman T.N.A. A longitudinal cross-sectional analysis of substance use treatment trends for individuals experiencing homelessness, criminal justice involvement, both, or neither - United States, 2006-2018. Lancet Reg. Health - Americas. 2022;7 doi: 10.1016/j.lana.2021.100174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahler G.J., Mennis J., Stein L.A.R., Belenko S., Rohsenow D.J., Grunwald H.E., Brinkley-Rubinstein L., Martin R.A. Treatment outcomes associated with medications for opioid use disorder (MOUD) among criminal justice-referred admissions to residential treatment in the U.S., 2015–2018. Drug Alcohol Depend. 2022;236 doi: 10.1016/j.drugalcdep.2022.109498. [DOI] [PubMed] [Google Scholar]
- Winkelman T.N.A., Chang V.W., Binswanger I.A. Health, polysubstance use, and criminal justice involvement among adults with varying levels of opioid use. JAMA Netw. Open. 2018;1 doi: 10.1001/jamanetworkopen.2018.0558. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.