Key Points
Question
Can physical activity interventions boost mental health (ie, cognitive function, psychological well-being, internalizing, and externalizing problems) in children and adolescents with neurodevelopmental disorders?
Findings
This systematic review and meta-analysis included 76 studies involving 3007 participants. Physical activity interventions were associated with significant benefits for overall mental health and its subgroups in children and adolescents with neurodevelopmental disorders.
Meaning
The results indicate that physical activity interventions could serve as alternative or adjunctive evidence-based approaches to boost mental health, including cognitive function, psychological well-being, internalizing, and externalizing problems, in children and adolescents with different types of neurodevelopmental disorders.
This systematic review and meta-analysis assesses the association of physical activity interventions and mental health in children and adolescents with neurodevelopmental disorders.
Abstract
Importance
Children and adolescents with neurodevelopmental disorders experience mental health issues and are encouraged to be brought together in real-life treatment. However, physical activity, which is a promising method for boosting mental health, has only been examined in children and adolescents with certain types of neurodevelopmental disorders.
Objective
To examine the association of physical activity interventions with mental health (ie, cognitive function, psychological well-being, internalizing, and externalizing problems) in children and adolescents with neurodevelopmental disorders and to identify possible moderators.
Data Sources
Studies were searched from inception to May 2023 through Web of Science, PsycINFO, SPORTDiscus, MEDLINE, CINAHL, and ERIC.
Study Selection
Randomized clinical trials or nonrandomized designs applying physical activity interventions and reporting at least 1 mental health outcome in children and adolescents aged 5 to 17 years with neurodevelopmental disorders were included. Two independent reviewers selected and assessed the studies.
Data Extraction and Synthesis
Random multilevel meta-analysis using Hedges g was performed. Data extraction and risk-of-bias assessment were conducted by multiple reviewers. Heterogeneity, publication bias, sensitivity analysis, and moderator analysis were examined to substantiate the results.
Main Outcomes and Measures
The main outcomes were mental health related to cognitive function, psychological well-being, internalizing, or externalizing problems measured by neurocognitive tasks or subjective questionnaires.
Results
A total of 76 studies involving 3007 participants were included in systematic review, 59 of which were used for meta-analysis. The findings indicated that physical activity interventions were associated with significant benefits for overall mental health (g, 0.67; 95% CI, 0.50-0.85), cognitive function (g, 0.74; 95% CI, 0.53-0.95), psychological well-being (g, 0.56; 95% CI, 0.16-0.96), internalizing (g, 0.72; 95% CI, 0.34-1.10), and externalizing problems (g, 0.58; 95% CI, 0.28-0.89). Moderators were also identified: frequency, total sessions, and total duration for overall mental health; total sessions, and total duration for cognitive function; session duration and frequency for psychological well-being; physical activity type for internalizing problems; and session duration for externalizing problems. Moderator analyses showed that type of neurodevelopmental disorder did not modify the associations between physical activity and overall mental health or its subgroups.
Conclusions and Relevance
The findings in this study suggest that children and adolescents with different types of neurodevelopmental disorders may be grouped together when performing physical activity interventions, which were confirmed to be beneficial to overall mental health and its subgroups in this new diagnostic population, but that physical activity interventions should be tailored when targeting different mental health domains.
Introduction
Neurodevelopmental disorders (NDDs) represent a new diagnostic category for a wide range of neurological and psychiatric disorders,1,2 including attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder (ASD), intellectual disability, specific learning disorder, communication disorders, and motor disorders (eg, developmental coordination disorder), according to the Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (DSM-5).3 The level of overlap between these disorders and their constituent symptoms is high,1 supporting the rationale for considering them together, especially in children and adolescents, among whom intellectual disability, ASD, and learning and motor disorders often have comorbid ADHD.4,5,6 Moreover, NDDs often present beyond neurodevelopmental symptoms, generally extending to mental health issues.1
In the framework proposed by Lubans et al,7 cognitive function, psychological well-being, and psychological ill-being (ie, internalizing and externalizing problems) are considered important determinants of mental health in youth. In children with NDDs, 89% with ADHD exhibit at least 1 executive dysfunction.8 Internalizing (eg, anxiety and depression) and externalizing (eg, aggression and disruptive behavior disorders) problems are also prevalent in children and adolescents with ASD9,10,11,12 and ADHD.13 Comorbid mental disorders may affect quality of life, long-term prognosis, and treatment choice for individuals with NDDs.14 Without adequate treatment, these symptoms persist through childhood, adolescence, and even adulthood. It is urgent to bridge the gaps in mental health research and clinical practice in NDDs.
Physical activity is a promising treatment to boost mental health in youth.7 Recent reviews have found that physical activity interventions in general improve a range of mental health outcomes in children and adolescents with typical development15 and those with certain types of NDDs.16,17,18,19,20,21 However, contradictory results are observed across NDDs. For example, Liang et al detected physical activity–induced benefit for working memory in children and adolescents with ADHD16 but not in those with ASD.19 Yang et al17 found a significant effect size of physical activity interventions for psychological health in children and adolescents with intellectual disability, while nonsignificant effect sizes were examined for internalizing and externalizing problems in those with ADHD.21 As such, it seems difficult to determine the association of physical activity interventions with mental health when considering NDDs together.
Moderators are also relevant to the direction or magnitude of intervention-induced effects.22 Lubans et al7 postulated that components of physical activity (eg, frequency, intensity, time, and type) may moderate the physical activity–induced benefits for mental health in children and adolescents. Intensity and intervention sessions (short term vs long term) were found to be moderators between physical activity interventions and executive function in those with ADHD.16 Meanwhile, physical activity type and time (duration per week) were identified as moderators between physical activity interventions and mental health (including cognitive function and psychological health) in those with intellectual disability, with methodology (eg, study design) and participant characteristics (eg, age) also playing a moderating role.17
Therefore, this study aimed to examine the association between physical activity interventions and overall mental health and its subgroups, including cognitive function, psychological well-being, internalizing, and externalizing problems, in children and adolescents with NDDs, guided by the framework proposed by Lubans et al7 and to identify possible moderators related to methodology, participant characteristics, and physical activity components.
Methods
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guideline.23 The protocol was registered in PROSPERO (CRD42023429638).
Search Strategy
A systematic search was performed using Web of Science, PsycINFO, SPORTDiscus with full text, MEDLINE, CINAHL Complete, and ERIC from inception to May 2023. The specific search terms are shown in the eAppendix in Supplement 1, determined by previous reviews.17,24 The search was limited to English language, human-related, and peer-reviewed articles.
Selection Criteria
We included randomized clinical trials and nonrandomized studies investigating the physical activity–induced effects on mental health in children and adolescents (aged 5-17 years) diagnosed with NDDs by standardized diagnostic tools or parent reports. Either short-term (1 session without repeating) or long-term (≥1 session/week for ≥2 weeks) physical activity interventions conducted in field or clinical trials were allowed. Studies using healthy children or adolescents as control groups were excluded. Mental health outcomes were required to be related to cognitive function, psychological well-being, internalizing, or externalizing problems measured by neurocognitive tasks or subjective questionnaires.7 According to DSM-5,3 cognitive functions include complex attention, executive function, learning and memory, language, perceptual motor, and social cognition. Psychological well-being comprises self-esteem, subjective well-being, quality of life, and psychological resilience.7 Internalizing problems are directed inward and pertain to emotional domain, while externalizing problems are directed outward and pertain to behavioral domain.25 Both preclinically and clinically diagnosed internalizing and externalizing problems were included.
Study Selection and Data Extraction
Two reviewers (C.L. and X.L.) independently scrutinized studies based on titles, abstracts, and full-length texts, and extracted data related to methodology, participant characteristics, intervention components, and mental health outcomes. Physical activity was determined as aerobic exercise or cognitively engaging exercise according to the content.16 When discrepancy appeared in study selection and data extraction, discussion was conducted until a consensus was reached.
Risk-of-Bias Assessment
Version 2 of the Risk of Bias in Randomized trials (RoB 2)26 and the Risk of Bias in Non-randomized Studies-of Interventions (ROBINS-I)27 were adopted to assess risk of bias by 2 independent reviewers (C.L. and X.L.). In case of discrepancies, discussions were conducted until the 2 reviewers reached 100% agreement.
Data Analysis
A multilevel meta-analysis using a random model and restricted maximum likelihood estimation was performed using the metafor package in R version 4.3.1 (R Foundation). Hedges g was used to handle bias in a small sample size28 and was calculated by means, standard deviations, and sample sizes. Data of pretest and the first posttest in both intervention and control group were adopted. If these data were unavailable, studies were excluded from the meta-analysis. The pooled effect sizes of subtopics under each mental health subgroup would be calculated if there were more than 3 effect sizes. Effect sizes reflecting the physical activity–induced effects on same indicator within 1 study were synthesized. Positive effect sizes indicated the positive physical activity–induced effects. Hedges g was classified as small (<0.2), moderate (0.5), or large (>0.8).29 I2 statistic was used to indicate the degree of heterogeneity as small (≤25%), medium (50%), or large (≥75%).30 By using multilevel meta-analysis, distribution of variance across sampling (level 1), within studies (level 2), and between studies (level 3) was examined. The 95% prediction interval (95% PI) of pooled effect size was also calculated as an absolute measure of heterogeneity.31
Six potential categorical moderators, including NDD type, study design (randomized clinical trial vs nonrandomized design), physical activity type (eg, aerobic exercise and cognitively engaging exercise), setting (clinical vs field), intervention sessions (short term vs long term), and intervention intensity (eg, moderate and vigorous), and 4 potential continuous moderators (session duration, frequency, total sessions, and total duration) were examined. Cochran Q statistics, the Akaike information criterion, and the bayesian information criterion were computed to compare the models. To examine the nonlinear moderating effects and the possible interactions of potential continuous moderators, the meta-CART package was used.32 A tree model was constructed when interactions were identified.
Effect sizes with residuals exceeding 3 standard deviations were excluded to examine sensitivity.33 A multilevel extension of the Egger regression test34 and a contour-enhanced funnel plot35 with filled missing effect sizes were used to assess publication bias. A sunset funnel plot was drawn to show the median power of included effect sizes and the replicability of studies.36 The threshold for significance was a 2-sided P < .05.
Results
The selection process is illustrated in eFigure 1 in Supplement 1. In total, 5890 studies were identified. After screening titles and abstracts, 102 studies were retrieved. Finally, 72 studies from database search and 4 studies from citation search were included in systematic review,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112 59 of which37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,58,59,60,61,62,63,64,66,68,70,71,72,74,75,76,77,78,81,83,84,85,86,87,88,90,91,92,93,94,95,96,97,103,105,106,109,110,111,112 were used for meta-analysis.
Study Characteristics
eTable 1 in Supplement 1 presents the characteristics of the 76 included studies (3007 total participants). The study distribution of NDDs was as follows: 31 included ADHD,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67 19 included ASD,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86 6 included developmental coordination disorder,87,88,89,90,91,92 15 included intellectual disability,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107 and 5 included learning disorder.108,109,110,111,112 Fifty-two studies were randomized clinical trials,37,38,39,40,41,43,45,46,48,49,50,51,52,53,54,55,56,58,60,62,63,66,67,68,69,70,72,73,75,76,78,79,81,83,84,85,86,88,89,90,91,92,93,94,96,97,103,105,106,108,109,110 and 24 were nonrandomized trials.42,44,47,57,59,61,64,65,71,74,77,80,82,87,95,98,99,100,101,102,104,107,111,112 Sample sizes ranged from 12 to 145, with a total of 3007 participants. Thirty-three studies reported the intervention settings with 2 in clinical trials50,66 and 31 in field.37,38,39,40,41,42,43,45,47,49,51,56,60,61,64,67,70,72,74,76,85,86,87,89,92,94,95,99,103,108,110 Fifty-four studies applied cognitively engaging exercise,38,39,40,43,44,47,50,51,55,58,60,61,62,64,65,66,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,87,88,89,90,91,93,94,95,96,97,99,103,104,105,106,107,108,109,111,112 14 adopted aerobic exercise,37,41,42,45,46,48,49,57,59,63,86,92,101,110 5 combined aerobic exercise and cognitively engaging exercise,52,53,54,56,67 and 3 had multiple intervention groups that adopted either aerobic exercise or cognitively engaging exercise.98,100,102 Five studies were short term,39,41,48,57,110 and 71 were long term.37,38,40,42,43,44,45,46,47,49,50,51,52,53,54,55,56,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,111,112 Session duration (5-120 minutes/session), frequency (once/week to 7 times/week), total sessions (1-144 sessions), and total duration (5-16 680 minutes) varied across studies. Only 20 studies reported intensity with 3 light to moderate,44,63,81 5 moderate,37,41,42,49,79 9 moderate to vigorous39,53,54,56,57,64,66,71,110 and 3 vigorous.48,92,108 Risk-of-bias assessments are presented in eFigures 2 and 3 in Supplement 1.
Meta-Analysis Results
Physical activity interventions had a moderate to large pooled effect size for overall mental health (g, 0.67; 95% CI, 0.50 to 0.85; P < .001; 95% PI, −0.67 to 2.02), based on 140 effect sizes from 59 studies. Total heterogeneity (total I2, 78.50%) was explained by both within-study (level 2 I2, 21.90%) and between-study level (level 3 I2, 56.60%).
Regarding cognitive function, eFigure 4 in Supplement 1 shows a moderate to large pooled effect size (g, 0.74; 95% CI, 0.48 to 0.99; P < .001; 95% PI, −0.86 to 2.33), based on 82 effect sizes from 44 studies. Total heterogeneity (total I2, 83.86%) was completely explained by between-study level. The pooled effect sizes for 6 subtopics under cognitive function were computed: cognitive flexibility (g, 0.49; 95% CI, 0.31 to 0.66; P < .001), inhibitory control (g, 0.54; 95% CI, 0.18 to 0.91; P = .006), working memory (g, 0.40; 95% CI, 0.14 to 0.67; P = .007), high-level executive function (g, 0.83; 95% CI, 0.25 to 1.41; P = .01), complex attention (g, 1.47; 95% CI, 0.66 to 2.27; P = .002), and behavior-rating executive function (g, 0.40; 95% CI, 0.14 to 0.65; P = .006), all significant.
eFigure 5 in Supplement 1 indicates a moderate pooled effect size for psychological well-being (g, 0.56; 95% CI, 0.16 to 0.96; P = .01; 95% PI, −0.43 to 1.54), based on 10 effect sizes from 9 studies. Total heterogeneity (total I2, 60.39%) was completely explained by between-study level. Due to the limited number of studies, the pooled effect size was calculated for only 1 subtopic under psychological well-being, quality of life, g, 0.26; 95% CI, −0.07 to 0.60; P = .10.
eFigure 6 in Supplement 1 shows a moderate to large pooled effect size for internalizing problems (g, 0.72; 95% CI, 0.34 to 1.10; P < .001; 95% PI, −0.77 to 2.21), based on 26 effect sizes from 15 studies. Total heterogeneity (total I2, 75.35%) was explained by both within-study (level 2 I2, 38.45%) and between-study level (level 3 I2, 36.90%). The pooled effect sizes for 2 subtopics under internalizing problems were examined: anxiety and depression (g, 0.81; 95% CI, 0.31 to 1.32; P = .003) and somatic complaints (g, 0.29; 95% CI, −0.79 to 1.37; P = .37).
Regarding externalizing problems (eFigure 7 in Supplement 1), a moderate pooled effect size was detected (g, 0.58; 95% CI, 0.28 to 0.89; P < .001; 95% PI, −0.37 to 1.54), based on 22 effect sizes from 14 studies. Total heterogeneity (total I2, 60.38%) was completely explained by between-study level. The pooled effect sizes for 2 subtopics under externalizing problems were available: conduct disorders (g, 0.61; 95% CI, 0.19 to 1.04; P = .008) and oppositional defiant disorders (g, 0.38; 95% CI, −0.02 to 0.79; P = .06).
Moderator analyses
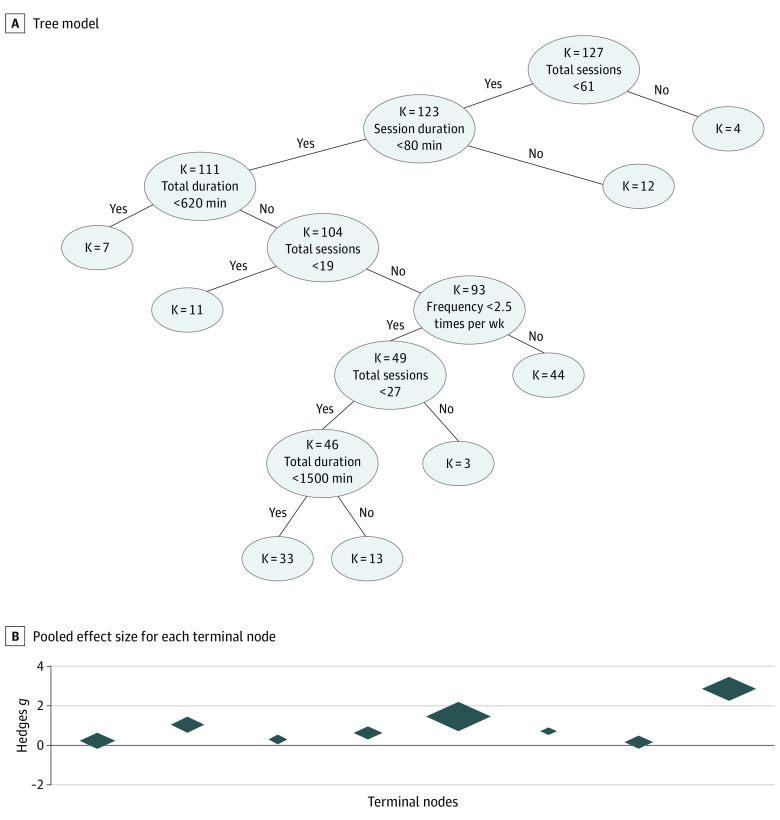
Tables 1 and 2 show that the physical activity–induced benefit for overall mental health was moderated by frequency (F1,125 = 4.04; P = .04) total sessions (F1,138 = 25.68; P < .001), and total duration (F1,138 = 18.57; P < .001), indicating that interventions with higher frequency (1-6 times/week), more total sessions (1-144 sessions), or longer total duration (5-7200 minutes) generated greater benefits. No categorical moderator was detected. The model with these 3 moderators (QE123 = 343.71; P < .001; Akaike information criterion, 275.93; bayesian information criterion, 293.00) was better than the model without any moderators (Cochran Q139 = 489.56; P < .001; Akaike information criterion, 295.68; bayesian information criterion, 304.21). Interactions between session duration, frequency, total sessions, and total duration were identified and are presented in Figure 1.
Table 1. Categorical Moderator Analyses for the Effect Size of Physical Activity for Overall Mental Health.
| Categorical moderator | Value | No. of studies | No. of effect sizes | Hedges g (95% CI) | F statistic | P value |
|---|---|---|---|---|---|---|
| Type of NDD | ADHD | 28 | 81 | 0.65 (0.39 to 0.91) | F4,135 = 0.99 | .42 |
| ASD | 14 | 32 | 0.52 (0.14 to 0.89) | |||
| DCD | 5 | 8 | 0.47 (−0.18 to 1.13) | |||
| ID | 8 | 12 | 0.97 (0.46 to 1.48) | |||
| LD | 4 | 7 | 1.13 (0.41 to 1.84) | |||
| Type of study | Nonrandomized | 13 | 35 | 0.50 (0.11 to 0.89) | F1,138 = 0.98 | .32 |
| RCT | 46 | 105 | 0.72 (0.52 to 0.92) | |||
| Type of physical activity | Aerobic exercise | 11 | 25 | 0.65 (0.22 to 1.08) | F2,137 = 0.01 | .99 |
| Aerobic exercise and cognitively engaging exercise | 4 | 8 | 0.66 (−0.05 to 1.37) | |||
| Cognitively engaging exercise | 44 | 107 | 0.68 (0.47 to 0.89) | |||
| Setting | Clinical | 2 | 4 | 0.51 (−0.57 to 1.59) | F1,78 = 0.03 | .87 |
| Field | 27 | 76 | 0.60 (0.32 to 0.88) | |||
| Intervention sessions | Short term | 4 | 7 | 0.71 (0.01 to 1.40) | F1,138 = 0.01 | .93 |
| Long term | 55 | 133 | 0.67 (0.49 to 0.86) | |||
| Intervention intensity | Light to moderate physical activity | 3 | 5 | 0.97 (−0.04 to 1.97) | F3,31 = 0.32 | .81 |
| Moderate physical activity | 5 | 9 | 0.38 (−0.42 to 1.18) | |||
| Moderate to vigorous physical activity | 7 | 19 | 0.63 (−0.03 to 1.30) | |||
| Vigorous physical activity | 2 | 2 | 0.44 (−0.83 to 1.71) |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; ASD, autism spectrum disorders; DCD, developmental coordination disorder; ID, intellectual disability; LD, learning disorder; NDD, neurodevelopmental disorder; RCT, randomized clinical trial.
Table 2. Continuous Moderator Analyses for the Effect Size of Physical Activity for Overall Mental Health.
| Continuous moderator | Range | No. of studies | No. of effect sizes | Intercept (95% CI)a | β (95% CI)b | F statistic | P value |
|---|---|---|---|---|---|---|---|
| Session duration, min/session | 5-90 | 59 | 140 | 1.04 (0.53 to 1.55) | −0.01 (−0.02 to 0.00) | F1,138 = 2.30 | .13 |
| Frequency, times/wk | 1-6 | 53 | 128 | 0.24 (−0.22 to 0.69) | 0.16 (0.00 to 0.33) | F1,125 = 4.04 | .04 |
| Total sessions, No. | 1-144 | 59 | 140 | 0.21 (−0.02 to 0.44) | 0.02 (0.01 to 0.02) | F1,138 = 25.68 | <.001 |
| Total duration, min | 5-7200 | 59 | 140 | 0.25 (0.00 to 0.49) | 0.00 (0.00 to 0.00) | F1,138 = 18.57 | <.001 |
Intercept indicates estimated effect size when moderator was 0.
β indicates change in effect size associated with increasing value of continuous moderator by 1.
Figure 1. Meta-CART Analysis 127 Effect Sizes for Overall Mental Health Outcomes.
The figure shows the meta-CART structure with splitting information at each internal node and the number of effect sizes (k) at each subgroup implied by a terminal node. The diamonds represent the 95% CI of each pooled effect size for each terminal node.
Moderators were also detected for the 4 subgroups of mental health, although several moderator analyses were unavailable due to the limited studies (eTables 2-5 in Supplement 1). Regarding categorical moderator, only physical activity type for internalizing problems was identified. No categorical moderators were found for cognitive function, psychological well-being, or externalizing problems. Continuous moderators were as follows: total sessions and total duration for cognitive function; session duration and frequency for psychological well-being; and session duration for externalizing problems. No continuous moderator was detected for internalizing problems. The inclusion of the corresponding moderators improved the model for each subgroup of mental health. Moreover, interaction between session duration and total sessions was observed for externalizing problems (eFigure 8 in Supplement 1).
Sensitivity Analysis and Publication Bias
Five outliers were detected for overall mental health. The removal of outliers resulted in a smaller but still significant pooled effect size (g, 0.61; 95% CI, 0.48 to 0.73; P < .001). The Egger test showed that the funnel plot was asymmetric (F1,138 = 28.96; P < .001). Twenty-four missing effect sizes located in significance areas were observed (Figure 2), indicating that publication bias did not explain the asymmetry. The sunset funnel plot (Figure 3) suggested that when assuming the true effect size for overall mental health was 0.67, the median power was 44.2%. The probability of replicating these studies was 55.60%.
Figure 2. Significance and Confidence Contours–Enhanced Funnel Plot for Overall Mental Health Outcomes.
The vertical solid line represents the pooled effect size (Hedges g = 0.67), the vertical dashed line represents the adjusted pooled effect size, the orange line is the Egger regression line. Significance contours at .05 and .01 levels are noted by the blue shaded area. Hollow dots represent included effect sizes; solid dots, missing effect sizes.
Figure 3. Sunset Funnel Plot for Overall Mental Health Outcomes.

The vertical solid line represents the pooled effect size (Hedges g = 0.67), the vertical dash line represents the adjusted pooled effect size. Significance contours at .05 and .01 levels are noted by the shaded area. medpower indicates the median power of all included effect sizes. d33% and d66% indicate the true effect sizes necessary for achieving 33% and 66% levels of median power. E, O, and PTES show the results of a test of excess significance. R-index denotes the expected replicability of findings.
For the 4 subgroups of mental health, only 3 outliers were found for cognitive function and 1 for internalizing problems. After removing outliers, the pooled effect sizes for cognitive function (g, 0.74; 95% CI, 0.53 to 0.95; P < .001) and internalizing problems (g, 0.67; 95% CI, 0.31 to 1.04; P < .001) remained significant.
According to the Egger test, funnel plots for psychological well-being (F1,8 = 0.29; P = .60), internalizing (F1,24 = 2.29; P = .14), and externalizing problems (F1,20 = 0.08; P = .78) were symmetric; the funnel plot for cognitive function was not (F1,80 = 13.59; P < .001). According to eFigures 9-12 in Supplement 1, all missing effect sizes were in significance areas, indicating no publication bias. The median power and the replicate index for each subgroup of mental health are shown in eFigures 13-16 in Supplement 1.
Discussion
Consistent with previous studies,16,17,18,19,20,21 our systematic review and meta-analysis indicated that physical activity interventions were associated with benefits for overall mental health and its 4 subgroups, including cognitive function, psychological well-being, internalizing, and externalizing problems when grouping children and adolescents with different types of NDDs together.
When it comes to mental health, it is necessary to consider all cognitive functions, psychological well-being, internalizing, and externalizing problems, because of the close relationships among them.7 Cognitive function provides a core foundation for psychological well-being and ill-being,113 while comorbid mental disorders contribute to cognitive impairment, especially in children and adolescents with NDDs.14 Our moderator analyses found that physical activity interventions with more total sessions, longer total duration, or higher frequency generated greater benefits for overall mental health. Total sessions, total duration, and frequency could affect intervention fidelity and, by extension, intervention validity.114 Of note, the effect size of physical activity interventions was largest when there were more than 61 total sessions and was nonsignificant when the total duration was less than 620 minutes or the session duration greater than 80 minutes, shown by our meta-CART analysis (Figure 1). Therefore, when targeting overall mental health, total duration greater than 620 minutes and session duration less than 80 minutes are primary considerations, on which basis more total sessions and higher frequency are recommended. Although excessive weekly physical exercise can lead to overtraining symptoms,115 frequently repeated practice may help enhance the physical activity–induced benefits in children with NDDs.24
The finding that physical activity interventions improved cognitive function in children and adolescents with NDDs was also identified in healthy youth.116 The finding was particularly consistent with a previous review examining the association between long-term physical activity interventions and cognitive function in youth,117 as our moderator analysis showed a significant effect size of long-term interventions but not of short-term interventions. A meta-analysis further found the benefits of long-term high-intensity interval training for executive function in healthy youth.118 However, no related studies were identified in the current review. Future studies are recommended to examine the effect of high-intensity interval training on cognitive function in children and adolescents with NDDs. Moreover, we found a moderate to large effect size, while a previous meta-analysis focusing on all individuals with NDDs observed a smaller one.24 Children and adolescents may benefit more from physical activity interventions because of the considerable development in executive function after early childhood and adolescence.119 Our moderator analyses further found that physical activity interventions with more total sessions (1-144 sessions) or longer total duration (5-7200 minutes) showed greater benefits for cognitive function. However, we did not find a moderating effect of session duration, unlike Sung et al24 Physical activity interventions of same session duration but different intensity may generate different effects. One experimental study120 targeting young healthy adults concluded that 20-minute moderate-intensity exercise had a more prolonged effect on executive function than 20-minute low-intensity exercise. When controlling for intensity, different session durations may also induce different levels of benefits. For example, vigorous exercise of 30 minutes was more beneficial for cognitive function in adolescents than that of 60 minutes.121
In the current systematic review and meta-analysis, physical activity interventions promoted psychological well-being, in line with a previous meta-analysis targeting typically developing children.15 Our moderator analysis showed that high-frequency physical activity of 40 minutes per session was optimal for psychological well-being. Results also indicated that extending session duration would decrease the effect size in the range between 40 and 60 minutes per session. Ojanen122 proposed an inverted U relationship between exercise session duration and psychological state, and a subsequent study123 using frontal electroencephalographic asymmetry found that 30 minutes of physical activity might be the peak point, supporting our results. Similarly, we found that increasing session duration also resulted in a reduction in the effect size for externalizing problems in the range of 30 to 90 minutes per session, suggesting that 30 minutes per session was the optimal dose. The clear relationship between externalizing problems and psychological well-being in children and adolescents gives an explanation.124,125 According to eFigure 8 in Supplement 1, when session duration exceeded 38 minutes per session, sessions beyond 27 would compensate for the decrease in the effect size for externalizing problems caused by the increase in session duration. Therefore, when targeting both psychological well-being and externalizing problems, high-frequency physical activity interventions of 40 minutes per session and more than 27 sessions are recommended. Still, the relationship between psychological well-being and exercise beyond 40 to 60 minutes per session requires further research.
Comparing to the small effect size of physical activity interventions previously found for internalizing problems in healthy children and adolescents,126 we observed a moderate to large one. The benefit of physical activity interventions appears to be more robust in young people with NDDs. The finding agreed with a previous review showing that whether adolescents had a clinical diagnosis moderated the physical activity–induced benefit for internalizing problems.127 Healthy people are at lower risk of experiencing internalizing problems than individuals with NDDs,128 suggesting the ceiling effect of physical activity interventions in healthy children and adolescents.127,129 In the current review, larger effect size for internalizing problems was identified through aerobic exercise than cognitively engaging exercise. Aerobic exercise generally focuses on the physiological benefits of physical activity,130 whereas cognitively engaging exercise gives more attention to cognitive performance.131 An experimental study132 supported that, finding an improvement in executive function of school children in cognitively engaging exercise but not aerobic exercise. The neurochemical basis of aerobic exercise, like the stimulation of endorphins and the increase in neurotransmitters,133 may explain the greater benefits of aerobic exercise for psychological well-being than cognitively engaging exercise.
As mentioned, the associations between physical activity interventions and mental health outcomes were varied across NDDs. However, we did not find the moderating effect of type of NDDs for either overall mental health or its subgroups. On the one hand, although NDDs present differently in reality, they have shared pathogenic mechanism in nature.134 On the other hand, there are multiple pathways, including neurobiological, psychosocial, and behavioral, through which physical activity interventions could affect mental health in youth,7 leading to the similar effect sizes across NDDs.
Strengths and Limitations
The strengths of our study are the examination of a broader array of mental health outcomes and the inclusion of children and adolescents with NDDs not limited to ADHD and ASD in a single study. We also examined several moderators that influenced the effect size of physical activity interventions for different mental health domains. However, our study is not without limitations. First, the distribution of NDDs was uneven, which might lead to biased results. Second, several moderator analyses were based on limited studies, which might be underpowered. In addition to ADHD and ASD, children and adolescents with other types of NDDs should be given more attention. The presence of psychological well-being needs more research. Clinical physical activity intervention studies should report more detailed information about methodology (eg, settings) and physical activity components (eg, intensity), and more potential moderators should be examined, for example, type of comparison group, which was a moderator between physical activity interventions and externalizing problems in adolescents,127 but was not examined in the current study.
Conclusions
The findings in this study indicate that physical activity interventions could serve as alternative or adjunctive evidence-based approaches to boosting mental health, including cognitive function, psychological well-being, internalizing, and externalizing problems, in children and adolescents with different types of NDDs. Significant moderators were also evident. Physical activity interventions should be tailored when targeting different mental health domains in this population group.
eTable 1. Descriptive characteristics of included studies
eTable 2. Moderator analyses for the effect size of physical activity for cognitive function
eTable 3. Moderator analyses for the effect size of physical activity for psychological well-being
eTable 4. Moderator analyses for the effect size of physical activity for internalizing problems
eTable 5. Moderator analyses for the effect size of physical activity for externalizing problems
eFigure 1. PRISMA selection flow diagram
eFigure 2.1. Summary of risk of bias assessment for each item presented as a percentage across all included randomized studies
eFigure 2.2. Risk of bias assessment for each included randomized study
eFigure 3.1. Summary of risk of bias assessment for each item presented as a percentage across all included non-randomized studies
eFigure 3.2. Risk of bias assessment for each included non-randomized study
eFigure 4. Forest plot for the effect sizes of physical activity for cognitive function
eFigure 5. Forest plot for the effect sizes of physical activity for psychological well-being
eFigure 6. Forest plot for the effect sizes of physical activity for internalizing problems
eFigure 7. Forest plot for the effect sizes of physical activity for externalizing problems
eFigure 8. The meta-CART analysis result of 19 effects sizes that examine the effect of physical activity on externalizing problems
eFigure 9. Significance and confidence contours-enhanced funnel plot for cognitive function
eFigure 10. Significance and confidence contours-enhanced funnel plot for psychological well-being
eFigure 11. Significance and confidence contours-enhanced funnel plot for internalizing problems
eFigure 12. Significance and confidence contours-enhanced funnel plot for externalizing problems
eFigure 13. Sunset funnel plot for cognitive function
eFigure 14. Sunset funnel plot for psychological well-being
eFigure 15. Sunset funnel plot for internalizing problems
eFigure 16. Sunset funnel plot for externalizing problems
eAppendix. Search terms
Data sharing statement
References
- 1.Thapar A, Cooper M, Rutter M. Neurodevelopmental disorders. Lancet Psychiatry. 2017;4(4):339-346. doi: 10.1016/S2215-0366(16)30376-5 [DOI] [PubMed] [Google Scholar]
- 2.Francés L, Quintero J, Fernández A, et al. Current state of knowledge on the prevalence of neurodevelopmental disorders in childhood according to the DSM-5: a systematic review in accordance with the PRISMA criteria. Child Adolesc Psychiatry Ment Health. 2022;16(1):27. doi: 10.1186/s13034-022-00462-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013. [Google Scholar]
- 4.Jensen CM, Steinhausen HC. Comorbid mental disorders in children and adolescents with attention-deficit/hyperactivity disorder in a large nationwide study. Atten Defic Hyperact Disord. 2015;7(1):27-38. doi: 10.1007/s12402-014-0142-1 [DOI] [PubMed] [Google Scholar]
- 5.Buckley N, Glasson EJ, Chen W, et al. Prevalence estimates of mental health problems in children and adolescents with intellectual disability: a systematic review and meta-analysis. Aust N Z J Psychiatry. 2020;54(10):970-984. doi: 10.1177/0004867420924101 [DOI] [PubMed] [Google Scholar]
- 6.Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921-929. doi: 10.1097/CHI.0b013e318179964f [DOI] [PubMed] [Google Scholar]
- 7.Lubans D, Richards J, Hillman C, et al. Physical activity for cognitive and mental health in youth: a systematic review of mechanisms. Pediatrics. 2016;138(3):e20161642. doi: 10.1542/peds.2016-1642 [DOI] [PubMed] [Google Scholar]
- 8.Kofler MJ, Irwin LN, Soto EF, Groves NB, Harmon SL, Sarver DE. Executive functioning heterogeneity in pediatric ADHD. J Abnorm Child Psychol. 2019;47(2):273-286. doi: 10.1007/s10802-018-0438-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caamaño M, Boada L, Merchán-Naranjo J, et al. Psychopathology in children and adolescents with ASD without mental retardation. J Autism Dev Disord. 2013;43(10):2442-2449. doi: 10.1007/s10803-013-1792-0 [DOI] [PubMed] [Google Scholar]
- 10.van Steensel FJA, Bögels SM, Perrin S. Anxiety disorders in children and adolescents with autistic spectrum disorders: a meta-analysis. Clin Child Fam Psychol Rev. 2011;14(3):302-317. doi: 10.1007/s10567-011-0097-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mazurek MO, Kanne SM, Wodka EL. Physical aggression in children and adolescents with autism spectrum disorders. Res Autism Spectr Disord. 2013;7(3):455-465. doi: 10.1016/j.rasd.2012.11.004 [DOI] [Google Scholar]
- 12.Kaat AJ, Lecavalier L. Disruptive behavior disorders in children and adolescents with autism spectrum disorders: a review of the prevalence, presentation, and treatment. Res Autism Spectr Disord. 2013;7(12):1579-1594. doi: 10.1016/j.rasd.2013.08.012 [DOI] [Google Scholar]
- 13.İpÇİ M, İncİ İzmİr SB, TÜrkÇapar MH, Özdel K, ArdiÇ ÜA, Ercan ES. Psychiatric comorbidity in the subtypes of ADHD in children and adolescents with ADHD according to DSM-IV. Noro Psikiyatr Ars. 2020;57(4):283-289. doi: 10.29399/npa.24807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hansen BH, Oerbeck B, Skirbekk B, Petrovski BÉ, Kristensen H. Neurodevelopmental disorders: prevalence and comorbidity in children referred to mental health services. Nord J Psychiatry. 2018;72(4):285-291. doi: 10.1080/08039488.2018.1444087 [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez-Ayllon M, Cadenas-Sánchez C, Estévez-López F, et al. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis. Sports Med. 2019;49(9):1383-1410. doi: 10.1007/s40279-019-01099-5 [DOI] [PubMed] [Google Scholar]
- 16.Liang X, Li R, Wong SHS, Sum RKW, Sit CHP. The impact of exercise interventions concerning executive functions of children and adolescents with attention-deficit/hyperactive disorder: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2021;18(1):68. doi: 10.1186/s12966-021-01135-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang W, Liang X, Sit CHP. Physical activity and mental health in children and adolescents with intellectual disabilities: a meta-analysis using the RE-AIM framework. Int J Behav Nutr Phys Act. 2022;19(1):80. doi: 10.1186/s12966-022-01312-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yu JJ, Burnett AF, Sit CH. Motor skill interventions in children with developmental coordination disorder: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2018;99(10):2076-2099. doi: 10.1016/j.apmr.2017.12.009 [DOI] [PubMed] [Google Scholar]
- 19.Liang X, Li R, Wong SHS, et al. The effects of exercise interventions on executive functions in children and adolescents with autism spectrum disorder: a systematic review and meta-analysis. Sports Med. 2022;52(1):75-88. doi: 10.1007/s40279-021-01545-3 [DOI] [PubMed] [Google Scholar]
- 20.Dastamooz S, Sadeghi-Bahmani D, Farahani MHD, et al. The efficacy of physical exercise interventions on mental health, cognitive function, and ADHD symptoms in children and adolescents with ADHD: an umbrella review. EClinicalMedicine. 2023;62(62):102137. doi: 10.1016/j.eclinm.2023.102137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zang Y. Impact of physical exercise on children with attention deficit hyperactivity disorders: evidence through a meta-analysis. Medicine (Baltimore). 2019;98(46):e17980. doi: 10.1097/MD.0000000000017980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kazdin aerobic exercise. Mediators and mechanisms of change in psychotherapy research. Annu Rev Clin Psychol. 2007;3:1-27. doi: 10.1146/annurev.clinpsy.3.022806.091432 [DOI] [PubMed] [Google Scholar]
- 23.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(71):n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sung MC, Ku B, Leung W, MacDonald M. The effect of physical activity interventions on executive function among people with neurodevelopmental disorders: a meta-analysis. J Autism Dev Disord. 2022;52(3):1030-1050. doi: 10.1007/s10803-021-05009-5 [DOI] [PubMed] [Google Scholar]
- 25.Forns M, Abad J, Kirchner T. Internalizing and externalizing problems. In: Encyclopedia of Adolescence. Levesque RJR, ed. Springer; 2011:1464-1469. doi: 10.1007/978-1-4419-1695-2_261 [DOI] [Google Scholar]
- 26.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 27.Sterne JAC, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4:863. doi: 10.3389/fpsyg.2013.00863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hedges LV, Olkin I. Statistical Methods for Meta-Analysis. Academic Press; 2014. [Google Scholar]
- 30.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539-1558. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 31.Borenstein M, Higgins JPT, Hedges LV, Rothstein HR. Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Res Synth Methods. 2017;8(1):5-18. doi: 10.1002/jrsm.1230 [DOI] [PubMed] [Google Scholar]
- 32.Li X, Dusseldorp E, Su X, Meulman JJ. Multiple moderator meta-analysis using the R-package Meta-CART. Behav Res Methods. 2020;52(6):2657-2673. doi: 10.3758/s13428-020-01360-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Murdoch EM, Lines RLJ, Crane MF, et al. The effectiveness of stress regulation interventions with athletes: a systematic review and multilevel meta-analysis of randomised controlled trials. Int Rev Sport Exerc Psychol. 2021;0(0):1-37. doi: 10.1080/1750984X.2021.1977974 [DOI] [Google Scholar]
- 34.Fernández-Castilla B, Declercq L, Jamshidi L, Beretvas SN, Onghena P, Van den Noortgate W. Detecting selection bias in meta-analyses with multiple outcomes: a simulation study. J Exp Educ. 2021;89(1):125-144. doi: 10.1080/00220973.2019.1582470 [DOI] [PubMed] [Google Scholar]
- 35.Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol. 2008;61(10):991-996. doi: 10.1016/j.jclinepi.2007.11.010 [DOI] [PubMed] [Google Scholar]
- 36.Schimmack U. A revised introduction to the R-Index. Replicability-Index: Improving the Replicability of Empirical Research . Accessed January 30, 2023. https://replicationindex.com/2016/01/31/a-revised-introduction-to-the-r-index/
- 37.Ahmed G, Mohamed S. Effect of regular aerobic exercises on behavioral, cognitive and psychological response in patients with attention deficit-hyperactivity disorder. Life Sci J. 2011;8(2):392-397. [Google Scholar]
- 38.Altszuler AR, Morrow AS, Merrill BM, et al. The effects of stimulant medication and training on sports competence among children with ADHD. J Clin Child Adolesc Psychol. 2019;48(sup1):S155-S167. doi: 10.1080/15374416.2016.1270829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Benzing V, Chang YK, Schmidt M. Acute physical activity enhances executive functions in children with ADHD. Sci Rep. 2018;8(1):12382. doi: 10.1038/s41598-018-30067-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Benzing V, Schmidt M. The effect of exergaming on executive functions in children with ADHD: a randomized clinical trial. Scand J Med Sci Sports. 2019;29(8):1243-1253. doi: 10.1111/sms.13446 [DOI] [PubMed] [Google Scholar]
- 41.Chang YK, Liu S, Yu HH, Lee YH. Effect of acute exercise on executive function in children with attention deficit hyperactivity disorder. Arch Clin Neuropsychol. 2012;27(2):225-237. doi: 10.1093/arclin/acr094 [DOI] [PubMed] [Google Scholar]
- 42.Chang YK, Hung CL, Huang CJ, Hatfield BD, Hung TM. Effects of an aquatic exercise program on inhibitory control in children with ADHD: a preliminary study. Arch Clin Neuropsychol. 2014;29(3):217-223. doi: 10.1093/arclin/acu003 [DOI] [PubMed] [Google Scholar]
- 43.Chang SH, Shie JJ, Yu NY. Enhancing executive functions and handwriting with a concentrative coordination exercise in children with ADHD: a randomized clinical trial. Percept Mot Skills. 2022;129(4):1014-1035. doi: 10.1177/00315125221098324 [DOI] [PubMed] [Google Scholar]
- 44.Chou CC, Huang CJ. Effects of an 8-week yoga program on sustained attention and discrimination function in children with attention deficit hyperactivity disorder. PeerJ. 2017;5:e2883. doi: 10.7717/peerj.2883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Silva LAD, Doyenart R, Henrique Salvan P, et al. Swimming training improves mental health parameters, cognition and motor coordination in children with attention deficit hyperactivity disorder. Int J Environ Health Res. 2020;30(5):584-592. doi: 10.1080/09603123.2019.1612041 [DOI] [PubMed] [Google Scholar]
- 46.Dehkordian P, Hamid N, Beshlideh K. Mehrabizade Honarmand M. The effectiveness of mindful parenting, social thinking and exercise on quality of life in ADHD children. Int J Pediatr. 2017;5(2):4295-4302. https://efaidnbmnnnibpcajpcglclefindmkaj/https://ijp.mums.ac.ir/article_7900_05dd8622fc835ee06ad4896b6dfa4a8e.pdf [Google Scholar]
- 47.García-Gómez A, Rodríguez-Jiménez M, Guerrero-Barona E, Rubio-Jiménez JC, García-Peña I, Moreno-Manso JM. Benefits of an experimental program of equestrian therapy for children with ADHD. Res Dev Disabil. 2016;59:176-185. doi: 10.1016/j.ridd.2016.09.003 [DOI] [PubMed] [Google Scholar]
- 48.Gawrilow C, Stadler G, Langguth N, Naumann A, Boeck A. Physical activity, affect, and cognition in children with symptoms of ADHD. J Atten Disord. 2016;20(2):151-162. doi: 10.1177/1087054713493318 [DOI] [PubMed] [Google Scholar]
- 49.Hattabi S, Bouallegue M, Ben Yahya H, Bouden A. Rehabilitation of ADHD children by sport intervention: a Tunisian experience. Tunis Med. 2019;97(7):874-881. [PubMed] [Google Scholar]
- 50.Jensen PS, Kenny DT. The effects of yoga on the attention and behavior of boys with attention-deficit/ hyperactivity disorder (ADHD). J Atten Disord. 2004;7(4):205-216. doi: 10.1177/108705470400700403 [DOI] [PubMed] [Google Scholar]
- 51.Kadri A, Slimani M, Bragazzi NL, Tod D, Azaiez F. Effect of taekwondo practice on cognitive function in adolescents with attention deficit hyperactivity disorder. Int J Environ Res Public Health. 2019;16(2):204. doi: 10.3390/ijerph16020204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kang KD, Choi JW, Kang SG, Han DH. Sports therapy for attention, cognitions and sociality. Int J Sports Med. 2011;32(12):953-959. doi: 10.1055/s-0031-1283175 [DOI] [PubMed] [Google Scholar]
- 53.Lee SK, Song J, Park JH. Effects of combination exercises on electroencephalography and frontal lobe executive function measures in children with ADHD: a pilot study. Biomed Res-India; 2017:28. [Google Scholar]
- 54.Liang X, Qiu H, Wang P, Sit CHP. The impacts of a combined exercise on executive function in children with ADHD: a randomized controlled trial. Scand J Med Sci Sports. 2022;32(8):1297-1312. doi: 10.1111/sms.14192 [DOI] [PubMed] [Google Scholar]
- 55.Ludyga S, Mücke M, Leuenberger R, et al. Behavioral and neurocognitive effects of judo training on working memory capacity in children with ADHD: a randomized controlled trial. Neuroimage Clin. 2022;36:103156. doi: 10.1016/j.nicl.2022.103156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Memarmoghaddam M, Torbati HT, Sohrabi M, Mashhadi A, Kashi A. Effects of a selected exercise program on executive function of children with attention deficit hyperactivity disorder. J Med Life. 2016;9(4):373-379. [PMC free article] [PubMed] [Google Scholar]
- 57.Miklós M, Komáromy D, Futó J, Balázs J. Acute physical activity, executive function, and attention performance in children with attention-deficit hyperactivity disorder and typically developing children: an experimental study. Int J Environ Res Public Health. 2020;17(11):4071. doi: 10.3390/ijerph17114071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Oh Y, Joung YS, Jang B, et al. Efficacy of hippotherapy versus pharmacotherapy in attention-deficit/hyperactivity disorder: a randomized clinical trial. J Altern Complement Med. 2018;24(5):463-471. doi: 10.1089/acm.2017.0358 [DOI] [PubMed] [Google Scholar]
- 59.Orangi MB, Yaali R, Ghorbanzadeh B, Loprinzi P, Ebdalifar A. The effect of aerobic exercise with nonlinear pedagogy on anxiety, depression, motor proficiency and cognitive ability of boys with attention deficit hyperactivity disorder. J Rehabil Sci Res. 2021;8:144-150. doi: 10.30476/JRSR.2021.91068.1163 [DOI] [Google Scholar]
- 60.Pan CY, Chu CH, Tsai CL, Lo SY, Cheng YW, Liu YJ. A racket-sport intervention improves behavioral and cognitive performance in children with attention-deficit/hyperactivity disorder. Res Dev Disabil. 2016;57:1-10. doi: 10.1016/j.ridd.2016.06.009 [DOI] [PubMed] [Google Scholar]
- 61.Pan CY, Tsai CL, Chu CH, Sung MC, Huang CY, Ma WY. Effects of physical exercise intervention on motor skills and executive functions in children with ADHD: a pilot study. J Atten Disord. 2019;23(4):384-397. doi: 10.1177/1087054715569282 [DOI] [PubMed] [Google Scholar]
- 62.Rezaei M, Salarpor Kamarzard T, Najafian Razavi M. The effects of neurofeedback, yoga interventions on memory and cognitive activity in children with attention deficit/hyperactivity disorder: a randomized controlled trial. Ann Appl Sport Sci. 2018;6(4):17-27. doi: 10.29252/aassjournal.6.4.17 [DOI] [Google Scholar]
- 63.Sabzi AH, Dana A, Salehian MH, Shaygan Yekta H. The effect of water treadmill exercise on children with attention deficit hyperactivity disorder. Int J Pediatr. 2021;9(6):13671-13681. doi: 10.22038/ijp.2021.57015.4466 [DOI] [Google Scholar]
- 64.Verret C, Guay MC, Berthiaume C, Gardiner P, Béliveau L. A physical activity program improves behavior and cognitive functions in children with ADHD: an exploratory study. J Atten Disord. 2012;16(1):71-80. doi: 10.1177/1087054710379735 [DOI] [PubMed] [Google Scholar]
- 65.Wang S. Yoga for emotional control in children with ADHD. Rev Bras Med Esporte. 2023;29:1-4. doi: 10.1590/1517-8692202329012022_0391 [DOI] [Google Scholar]
- 66.Zhang Z, Li R, Zhou Z, Wang P, Yang B, Wang X. The effect of physical activity on quality of life and parenting stress in children with attention-deficit/hyperactivity disorder: a randomized controlled trial. Disabil Health J. 2023;16(1):101377. doi: 10.1016/j.dhjo.2022.101377 [DOI] [PubMed] [Google Scholar]
- 67.Ziereis S, Jansen P. Effects of physical activity on executive function and motor performance in children with ADHD. Res Dev Disabil. 2015;38:181-191. doi: 10.1016/j.ridd.2014.12.005 [DOI] [PubMed] [Google Scholar]
- 68.Aithal S, Karkou V, Makris S, Karaminis T, Powell J. A dance movement psychotherapy intervention for the wellbeing of children with an autism spectrum disorder: a pilot intervention study. Front Psychol. 2021;12:588418. doi: 10.3389/fpsyg.2021.588418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Arslan E, Ince G, Akyüz M. Effects of a 12-week structured circuit exercise program on physical fitness levels of children with autism spectrum condition and typically developing children. Int J Dev Disabil. 2020;68(4):500-510. doi: 10.1080/20473869.2020.1819943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Borgi M, Loliva D, Cerino S, et al. Effectiveness of a standardized equine-assisted therapy program for children with autism spectrum disorder. J Autism Dev Disord. 2016;46(1):1-9. doi: 10.1007/s10803-015-2530-6 [DOI] [PubMed] [Google Scholar]
- 71.Caputo G, Ippolito G, Mazzotta M, et al. Effectiveness of a multisystem aquatic therapy for children with autism spectrum disorders. J Autism Dev Disord. 2018;48(6):1945-1956. doi: 10.1007/s10803-017-3456-y [DOI] [PubMed] [Google Scholar]
- 72.Chan AS, Sze SL, Siu NY, Lau EM, Cheung MC. A chinese mind-body exercise improves self-control of children with autism: a randomized controlled trial. PLoS One. 2013;8(7):e68184. doi: 10.1371/journal.pone.0068184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chan AS, Han YMY, Sze SL, Lau EM. Neuroenhancement of memory for children with autism by a mind-body exercise. Front Psychol. 2015;6:1893. doi: 10.3389/fpsyg.2015.01893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.García-Gómez A, Lopez Risco M, Carlos Rubio J, Guerrero E, Magdalena Garcia-Pena I. Effects of a program of adapted therapeutic horse-riding in a group of autism spectrum disorder children. Electron J Res Educ Psychol. 2014;12(1):107-128. doi: 10.14204/ejrep.32.13115 [DOI] [Google Scholar]
- 75.Greco G, de Ronzi R. Effect of karate training on social, emotional, and executive functioning in children with autism spectrum disorder. J Phys Educ Sport. 2020;20(4):1637-1645. doi: 10.7752/jpes.2020.04223 [DOI] [Google Scholar]
- 76.Greco G. Multilateral training using physical activity and social games improves motor skills and executive function in children with autism spectrum disorder. Eur J Spec Educ Res. 2020;5(4). doi: 10.5281/zenodo.3712294 [DOI] [Google Scholar]
- 77.Harris A, Williams JM. The impact of a horse-riding intervention on the social functioning of children with autism spectrum disorder. Int J Environ Res Public Health. 2017;14(7):776. doi: 10.3390/ijerph14070776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ji C, Yang J. Effects of physical exercise and virtual training on visual attention levels in children with autism spectrum disorders. Brain Sci. 2021;12(1):41. doi: 10.3390/brainsci12010041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ji C, Yang J, Lin L, Chen S. Executive function improvement for children with autism spectrum disorder: a comparative study between virtual training and physical exercise methods. Children (Basel). 2022;9(4):507. doi: 10.3390/children9040507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kaur M, Eigsti IM, Bhat A. Effects of a creative yoga intervention on the joint attention and social communication skills, as well as affective states of children with autism spectrum disorder. Res Autism Spectr Disord. 2021;88:101860. doi: 10.1016/j.rasd.2021.101860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rafiei Milajerdi H, Sheikh M, Najafabadi MG, Saghaei B, Naghdi N, Dewey D. The effects of physical activity and exergaming on motor skills and executive functions in children with autism spectrum disorder. Games Health J. 2021;10(1):33-42. doi: 10.1089/g4h.2019.0180 [DOI] [PubMed] [Google Scholar]
- 82.Narasingharao K, Pradhan B, Navaneetham J. Efficacy of structured yoga intervention for sleep, gastrointestinal and behaviour problems of ASD children: an exploratory study. J Clin Diagn Res. 2017;11(3):VC01-VC06. doi: 10.7860/JCDR/2017/25894.9502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pan CY, Chu CH, Tsai CL, Sung MC, Huang CY, Ma WY. The impacts of physical activity intervention on physical and cognitive outcomes in children with autism spectrum disorder. Autism. 2017;21(2):190-202. doi: 10.1177/1362361316633562 [DOI] [PubMed] [Google Scholar]
- 84.Phung JN, Goldberg WA. Promoting executive functioning in children with autism spectrum disorder through mixed martial arts training. J Autism Dev Disord. 2019;49(9):3669-3684. doi: 10.1007/s10803-019-04072-3 [DOI] [PubMed] [Google Scholar]
- 85.Tse CYA, Lee HP, Chan KSK, Edgar VB, Wilkinson-Smith A, Lai WHE. Examining the impact of physical activity on sleep quality and executive functions in children with autism spectrum disorder: a randomized controlled trial. Autism. 2019;23(7):1699-1710. doi: 10.1177/1362361318823910 [DOI] [PubMed] [Google Scholar]
- 86.Tse ACY. Brief report: impact of a physical exercise intervention on emotion regulation and behavioral functioning in children with autism spectrum disorder. J Autism Dev Disord. 2020;50(11):4191-4198. doi: 10.1007/s10803-020-04418-2 [DOI] [PubMed] [Google Scholar]
- 87.Alloway TP, Warn C. Task-specific training, learning, and memory for children with developmental coordination disorder: a pilot study. Percept Mot Skills. 2008;107(2):473-480. doi: 10.2466/pms.107.2.473-480 [DOI] [PubMed] [Google Scholar]
- 88.Damanpak S, Sabzi AH. The effect of selected motor games on executive functions of children with developmental coordination disorders. Int J Pediatr. 2022;10(2):15449-15459. doi: 10.22038/ijp.2021.57638.4523 [DOI] [Google Scholar]
- 89.Sit CHP, Yu JJ, Wong SHS, Capio CM, Masters R. A school-based physical activity intervention for children with developmental coordination disorder: a randomized controlled trial. Res Dev Disabil. 2019;89:1-9. doi: 10.1016/j.ridd.2019.03.004 [DOI] [PubMed] [Google Scholar]
- 90.Tsai CL. The effectiveness of exercise intervention on inhibitory control in children with developmental coordination disorder: using a visuospatial attention paradigm as a model. Res Dev Disabil. 2009;30(6):1268-1280. doi: 10.1016/j.ridd.2009.05.001 [DOI] [PubMed] [Google Scholar]
- 91.Tsai CL, Wang CH, Tseng YT. Effects of exercise intervention on event-related potential and task performance indices of attention networks in children with developmental coordination disorder. Brain Cogn. 2012;79(1):12-22. doi: 10.1016/j.bandc.2012.02.004 [DOI] [PubMed] [Google Scholar]
- 92.Tsai CL, Chang YK, Chen FC, Hung TM, Pan CY, Wang CH. Effects of cardiorespiratory fitness enhancement on deficits in visuospatial working memory in children with developmental coordination disorder: a cognitive electrophysiological study. Arch Clin Neuropsychol. 2014;29(2):173-185. doi: 10.1093/arclin/act081 [DOI] [PubMed] [Google Scholar]
- 93.Atak E, Hajebrahimi F, Algun ZC. The effect of Dual-Task balance exercises on cognitive functions among children with mild and borderline mental retardation: a randomized controlled trial. Eur J Physiother. 2022;26:1-9. doi: 10.1080/21679169.2022.2113138 [DOI] [Google Scholar]
- 94.Chen MD, Tsai HY, Wang CC, Wuang YP. The effectiveness of racket-sport intervention on visual perception and executive functions in children with mild intellectual disabilities and borderline intellectual functioning. Neuropsychiatr Dis Treat. 2015;11:2287-2297. doi: 10.2147/NDT.S89083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Choi PHN, Cheung SY. Effects of an 8-week structured physical activity program on psychosocial behaviors of children with intellectual disabilities. Adapt Phys Activ Q. 2016;33(1):1-14. doi: 10.1123/AphysicalactivityQ.2014-0213 [DOI] [PubMed] [Google Scholar]
- 96.Giagazoglou P, Arabatzi F, Kellis E, Liga M, Karra C, Amiridis I. Muscle reaction function of individuals with intellectual disabilities may be improved through therapeutic use of a horse. Res Dev Disabil. 2013;34(9):2442-2448. doi: 10.1016/j.ridd.2013.04.015 [DOI] [PubMed] [Google Scholar]
- 97.İlhan EL, Kirimoglu H, Fi̇lazoglu Cokluk G. The effect of special physical education and sports program on the quality of life of the children with mental retardation. Nigde Univ J Phys Educ Sport Sci. 2013;7(1):1-8. [Google Scholar]
- 98.Maïano C, Ninot G, Erraïs B. Effects of alternated sport competition in perceived competence for adolescent males with mild to moderate mental retardation. Int J Rehabil Res. 2001;24(1):51-58. doi: 10.1097/00004356-200103000-00007 [DOI] [PubMed] [Google Scholar]
- 99.Maïano C, Ninot G, Bruant G, Bilard J. Effects of alternated basketball competition on perceived competence in adolescents with intellectual disabilities over a period of 13 months: a research note. Int J Disabil Dev Educ. 2002;49(4):413-420. doi: 10.1080/1034912022000028376 [DOI] [Google Scholar]
- 100.Ninot G, Bilard J, Delignières D, Sokolowski M. Effects of integrated sport participation on perceived competence for adolescents with mental retardation. Adapt Phys Activ Q. 2000;17(2):208-221. doi: 10.1123/apaq.17.2.208 [DOI] [Google Scholar]
- 101.Ninot G, Bilard J, Delignières D. Effects of integrated or segregated sport participation on the physical self for adolescents with intellectual disabilities. J Intellect Disabil Res. 2005;49(Pt 9):682-689. doi: 10.1111/j.1365-2788.2005.00407.x [DOI] [PubMed] [Google Scholar]
- 102.Ninot G, Maïano C. Long-term effects of athletics meet on the perceived competence of individuals with intellectual disabilities. Res Dev Disabil. 2007;28(2):176-186. doi: 10.1016/j.ridd.2006.02.008 [DOI] [PubMed] [Google Scholar]
- 103.Özer D, Baran F, Aktop A, Nalbant S, Ağlamış E, Hutzler Y. Effects of a Special Olympics Unified Sports soccer program on psycho-social attributes of youth with and without intellectual disability. Res Dev Disabil. 2012;33(1):229-239. doi: 10.1016/j.ridd.2011.09.011 [DOI] [PubMed] [Google Scholar]
- 104.Özkan Z, Kale R. Investigation of the effects of physical education activities on motor skills and quality of life in children with intellectual disability. Int J Dev Disabil. 2021;69(4):578-592. doi: 10.1080/20473869.2021.1978267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Perić DB, Milićević-Marinković B, Djurović D. The effect of the adapted soccer programme on motor learning and psychosocial behaviour in adolescents with Down syndrome. J Intellect Disabil Res. 2022;66(6):533-544. doi: 10.1111/jir.12881 [DOI] [PubMed] [Google Scholar]
- 106.Pise V, Pradhan B, Gharote M. Effect of yoga practices on psycho-motor abilities among intellectually disabled children. J Exerc Rehabil. 2018;14(4):581-585. doi: 10.12965/jer.1836290.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ryuh Y, Choi P, Oh J, Chen CC, Lee Y. Impact of inclusive soccer program on psychosocial development of children with and without intellectual disabilities. J Dev Phys Disabil. 2019;31(5):691-705. doi: 10.1007/s10882-019-09670-8 [DOI] [Google Scholar]
- 108.Bluechardt MH, Shephard RJ. Using an extracurricular physical activity program to enhance social skills. J Learn Disabil. 1995;28(3):160-169. doi: 10.1177/002221949502800305 [DOI] [PubMed] [Google Scholar]
- 109.Emami Kashfi T, Sohrabi M, Saberi Kakhki A, Mashhadi A, Jabbari Nooghabi M. Effects of a motor intervention program on motor skills and executive functions in children with learning disabilities. Percept Mot Skills. 2019;126(3):477-498. doi: 10.1177/0031512519836811 [DOI] [PubMed] [Google Scholar]
- 110.Huang CJ, Tu HY, Hsueh MC, Chiu YH, Huang MY, Chou CC. Effects of acute aerobic exercise on executive function in children with and without learning disability: a randomized controlled trial. Adapt Phys Activ Q. 2020;37(4):404-422. doi: 10.1123/apaq.2019-0108 [DOI] [PubMed] [Google Scholar]
- 111.Milligan K, Sibalis A, McKeough T, et al. Impact of mindfulness martial arts training on neural and behavioral indices of attention in youth with learning disabilities and co-occurring mental health challenges. Mindfulness (N Y). 2019;10(10):2152-2164. doi: 10.1007/s12671-019-01161-3 [DOI] [Google Scholar]
- 112.Topa Ş, Demirci P, Demirci N. The effects of game and physical activity lessons in children with learning disabilities. Kinesiol Slov. 2018;24(3):47-55. [Google Scholar]
- 113.Gale CR, Cooper R, Craig L, et al. Cognitive function in childhood and lifetime cognitive change in relation to mental wellbeing in four cohorts of older people. PLoS One. 2012;7(9):e44860. doi: 10.1371/journal.pone.0044860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Santacroce SJ, Maccarelli LM, Grey M. Intervention fidelity. Nurs Res. 2004;53(1):63-66. doi: 10.1097/00006199-200401000-00010 [DOI] [PubMed] [Google Scholar]
- 115.Position Stand ACSM. American College of Sports Medicine position stand. the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;30(6):975-991. [DOI] [PubMed] [Google Scholar]
- 116.Álvarez-Bueno C, Pesce C, Cavero-Redondo I, Sánchez-López M, Martínez-Hortelano JA, Martínez-Vizcaíno V. The effect of physical activity interventions on children’s cognition and metacognition: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(9):729-738. doi: 10.1016/j.jaac.2017.06.012 [DOI] [PubMed] [Google Scholar]
- 117.Heinze K, Cumming J, Dosanjh A, et al. Neurobiological evidence of longer-term physical activity interventions on mental health outcomes and cognition in young people: a systematic review of randomised controlled trials. Neurosci Biobehav Rev. 2021;120:431-441. doi: 10.1016/j.neubiorev.2020.10.014 [DOI] [PubMed] [Google Scholar]
- 118.Leahy AA, Mavilidi MF, Smith JJ, et al. Review of high-intensity interval training for cognitive and mental health in youth. Med Sci Sports Exerc. 2020;52(10):2224-2234. doi: 10.1249/MSS.0000000000002359 [DOI] [PubMed] [Google Scholar]
- 119.Best JR, Miller PH, Jones LL. Executive functions after age 5: changes and correlates. Dev Rev. 2009;29(3):180-200. doi: 10.1016/j.dr.2009.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Tsukamoto H, Takenaka S, Suga T, et al. Impact of exercise intensity and duration on postexercise executive function. Med Sci Sports Exerc. 2017;49(4):774-784. doi: 10.1249/MSS.0000000000001155 [DOI] [PubMed] [Google Scholar]
- 121.Hatch LM, Dring KJ, Williams RA, Sunderland C, Nevill ME, Cooper SB. Effect of differing durations of high-intensity intermittent activity on cognitive function in adolescents. Int J Environ Res Public Health. 2021;18(21):11594. doi: 10.3390/ijerph182111594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ojanen M. Can the true effects of exercise on psychological variables be separated from placebo effects. Int J Sport Psychol. 1994;25:63-80. [Google Scholar]
- 123.Woo M, Kim S, Kim J, Petruzzello SJ, Hatfield BD. Examining the exercise-affect dose-response relationship: does duration influence frontal EEG asymmetry? Int J Psychophysiol. 2009;72(2):166-172. doi: 10.1016/j.ijpsycho.2008.12.003 [DOI] [PubMed] [Google Scholar]
- 124.Houck G, Kendall J, Miller A, Morrell P, Wiebe G. Self-concept in children and adolescents with attention deficit hyperactivity disorder. J Pediatr Nurs. 2011;26(3):239-247. doi: 10.1016/j.pedn.2010.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Jamison TR, Schuttler JO. Examining social competence, self-perception, quality of life, and internalizing and externalizing symptoms in adolescent females with and without autism spectrum disorder: a quantitative design including between-groups and correlational analyses. Mol Autism. 2015;6(1):53. doi: 10.1186/s13229-015-0044-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Andermo S, Hallgren M, Nguyen TTD, et al. School-related physical activity interventions and mental health among children: a systematic review and meta-analysis. Sports Med Open. 2020;6(1):25. doi: 10.1186/s40798-020-00254-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Spruit A, Assink M, van Vugt E, van der Put C, Stams GJ. The effects of physical activity interventions on psychosocial outcomes in adolescents: a meta-analytic review. Clin Psychol Rev. 2016;45:56-71. doi: 10.1016/j.cpr.2016.03.006 [DOI] [PubMed] [Google Scholar]
- 128.Baraskewich J, McMorris CA. Internalizing mental health issues in individuals with neurodevelopmental disorders: implications for practitioners. Curr Dev Disord Rep. 2019;6:1-8. doi: 10.1007/s40474-019-0154-9 [DOI] [Google Scholar]
- 129.Boyd KR, Hrycaiko DW. The effect of a physical activity intervention package on the self-esteem of pre-adolescent and adolescent females. Adolescence. 1997;32(127):693-708. [PubMed] [Google Scholar]
- 130.van der Fels IMJ, Hartman E, Bosker RJ, et al. Effects of aerobic exercise and cognitively engaging exercise on cardiorespiratory fitness and motor skills in primary school children: a cluster randomized controlled trial. J Sports Sci. 2020;38(17):1975-1983. doi: 10.1080/02640414.2020.1765464 [DOI] [PubMed] [Google Scholar]
- 131.Martins RMG, Mazzoli E, Duncan MJ, Clark CCT, Eyre ELJ. The acute effects of cognitively demanding physical activity on inhibitory and affective responses in children: an online-based mixed methods approach. Children (Basel). 2022;9(12):1896. doi: 10.3390/children9121896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Schmidt M, Jäger K, Egger F, Roebers CM, Conzelmann A. Cognitively engaging chronic physical activity, but not aerobic exercise, affects executive functions in primary school children: a group-randomized controlled trial. J Sport Exerc Psychol. 2015;37(6):575-591. doi: 10.1123/jsep.2015-0069 [DOI] [PubMed] [Google Scholar]
- 133.Heijnen S, Hommel B, Kibele A, Colzato LS. Neuromodulation of aerobic exercise—a review. Front Psychol. 2016;6(6):1890. doi: 10.3389/fpsyg.2015.01890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Parenti I, Rabaneda LG, Schoen H, Novarino G. Neurodevelopmental disorders: from genetics to functional pathways. Trends Neurosci. 2020;43(8):608-621. doi: 10.1016/j.tins.2020.05.004 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Descriptive characteristics of included studies
eTable 2. Moderator analyses for the effect size of physical activity for cognitive function
eTable 3. Moderator analyses for the effect size of physical activity for psychological well-being
eTable 4. Moderator analyses for the effect size of physical activity for internalizing problems
eTable 5. Moderator analyses for the effect size of physical activity for externalizing problems
eFigure 1. PRISMA selection flow diagram
eFigure 2.1. Summary of risk of bias assessment for each item presented as a percentage across all included randomized studies
eFigure 2.2. Risk of bias assessment for each included randomized study
eFigure 3.1. Summary of risk of bias assessment for each item presented as a percentage across all included non-randomized studies
eFigure 3.2. Risk of bias assessment for each included non-randomized study
eFigure 4. Forest plot for the effect sizes of physical activity for cognitive function
eFigure 5. Forest plot for the effect sizes of physical activity for psychological well-being
eFigure 6. Forest plot for the effect sizes of physical activity for internalizing problems
eFigure 7. Forest plot for the effect sizes of physical activity for externalizing problems
eFigure 8. The meta-CART analysis result of 19 effects sizes that examine the effect of physical activity on externalizing problems
eFigure 9. Significance and confidence contours-enhanced funnel plot for cognitive function
eFigure 10. Significance and confidence contours-enhanced funnel plot for psychological well-being
eFigure 11. Significance and confidence contours-enhanced funnel plot for internalizing problems
eFigure 12. Significance and confidence contours-enhanced funnel plot for externalizing problems
eFigure 13. Sunset funnel plot for cognitive function
eFigure 14. Sunset funnel plot for psychological well-being
eFigure 15. Sunset funnel plot for internalizing problems
eFigure 16. Sunset funnel plot for externalizing problems
eAppendix. Search terms
Data sharing statement