Abstract
The video laryngoscope is a novel instrument for intubation that enables indirect visualization of the upper airway. It is recognized for its ability to enhance Cormack-Lehane grades in the management of difficult airways. Notably, video laryngoscopy is associated with equal or higher rates of intubation success within a shorter time frame than direct laryngoscopy.
Video laryngoscopy facilitates faster and easier visualization of the glottis and reduces the need for Magill forceps, thereby shortening the intubation time. Despite the advanced glottic visualization afforded by video laryngoscopy, nasotracheal tube insertion and advancement occasionally fail. This is particularly evident during nasotracheal intubation, where oropharyngeal blood or secretions may obstruct the visual field on the monitor, thereby complicating video laryngoscopy. Moreover, the use of Magill forceps is markedly challenging or nearly unfeasible in this context, especially in pediatric cases. Furthermore, the substantial blade size of video laryngoscopes may restrict their applicability in individuals with limited oral apertures.
This study aimed to review the literature on video laryngoscopy, discuss its clinical role in nasotracheal intubation, and address the challenges that anesthesiologists may encounter during the intubation process.
Keywords: Intubation, Nasotracheal; Oral Surgery; Ring, Adair, and Elwyn Tube; Video Laryngoscopes.
INTRODUCTION
Nasotracheal intubation (NTI) is often necessary for airway stability and surgical convenience in oral and maxillofacial surgery. The nasal Ring, Adair, and Elwyn endotracheal tube, with its appropriate prebent shape, is widely used. However, the challenges in NTI, compared to routine orotracheal intubation (OTI), are often heightened because of factors such as the predetermined curvature of the tube, the necessity to navigate through the nasal passages, and oral and maxillofacial complexities associated with patients. These complexities include trismus, reduced mouth opening, and facial deformities, all of which can contribute to difficult airway management [1].
Since the advancement of surgical procedures under general anesthesia in the 1920s, various direct laryngoscopes (DLs) have been developed [2,3]. DL has been utilized for intubation for over 50 years.
Subsequently, efforts have been made to enhance glottic visualization in difficult airways and increase the success rate of intubation. Video laryngoscopes (VL) have been in use since the 2000s, to date, several comparative studies comparing VL and DL have been published [4,5,6,7,8]. A VL is a device designed with a camera at the end of its blade that transmits real-time images to a video screen located on the upper part of the handle, allowing for indirect visualization of the airway [9].
VLs can be broadly categorized into two types: non-channeled, where the blade and endotracheal tube (ETT) are separate entities, and channeled, where the blade and ETT are integrated and inserted together, and the blade is subsequently removed. VLs have played a significant role in airway management, in both anticipated and unanticipated difficult airways [10,11].
In the existing literature on the application of VL for NTI, the specific advantages in oral and maxillofacial surgical contexts have not been as extensively documented as those in other areas of surgical practice [12,13].
This review article aimed to discuss the VL-assisted NTI technique used in oral maxillofacial surgery and its role in clinical practice.
ANATOMICAL CHALLENGES IN ORAL AND MAXILLOFACIAL SURGERY FOR NTI
Oral and maxillofacial surgeries present unique challenges in airway management, particularly during NTI. The intricate anatomy of the upper airway, often altered by facial anomalies or trauma, demands precise and adaptable intubation techniques. The nasal anatomy is a crucial component of the respiratory and olfactory systems and plays a pivotal role in airway filtration, humidification, and olfaction. The external nasal anatomy relevant to NTI includes the nasal vestibule, septum, bone, and cartilage. The internal nasal anatomy includes the turbinate (conchae) in the nasal cavity, posterior nasal aperture, adenoids, and Eustachian tube orifices in the nasopharynx and nasal mucosa. The nasopharynx and oropharynx through which the NTT passes, as well as the laryngopharynx including the epiglottis, arytenoids, and vocal cords, are seen with VL. The anatomy of the NTI is shown in Figure 1.
Fig. 1. Relevant anatomy during nasotracheal intubation (NTI). (a) Inferior nasal meatus Inferior turbinate, (b) nasopharynx, (c) oropharynx, (d) glottis.
NTI presents many challenges during oral and maxillofacial surgeries. These challenges include anatomical variations, limited space, access difficulties due to foreign bodies or lesions in the oral cavity, and difficulty in securing vision due to nasal or oral bleeding. Understanding the intricate anatomy and challenges of oral and maxillofacial surgery is important for effective airway management.
AN OVERVIEW OF VIDEO LARYNGOSCOPY
VLs can be primarily classified into non-channeled and channeled types. The non-channeled variety can be further divided by the shape of the blade into Macintosh or angulated subtypes [14].
A VL with a Macintosh blade has the same blade shape as standard DLs, allowing insertion into the mouth using DL techniques. The C-MAC (Karl Storz, Tuttlingen, Germany) and McGRATH® MAC (Aircraft Medical, Edinburgh, UK) are notable examples of VLs with Macintosh blades [5,15].
VLs with angulated blades are characterized by blades that are more acutely angled than Macintosh blades. Devices in this category include the GlideScope® VL (GVL) (Verathon Inc, Bothell, WA, USA), the C-MAC® D-BLADE (Karl Storz, Tuttlingen, Germany), and the McGRATH® Series 5 (Aircraft Medical, Edinburgh, UK) [16]. Typically, the blade is inserted along the center of the oral cavity without displacing the tongue, passing over the palate and the posterior pharynx, and advancing the blade tip accordingly [17,18]. The shape of the angulated blade, which is similar to the anatomical structure and angle of the oral cavity, allows the tip to be positioned closer to the glottis, thereby providing a better view of the glottic opening [19]. Despite this advantage, aligning the tube towards the glottis often presents challenges [17,18]. In such situations, a slight retraction of the blade can be helpful.
The channeled blade category includes the Airtraq® (Prodol Meditec, Vizcaya, Spain) and the Pentax Airway Scope® (Nihon Kohden, Tokyo, Japan) [20,21,22]. These devices feature an anatomical guide channel that aids in directing the ETT toward the glottis. The ETT is preloaded into the channel and the blade is inserted along the midline of the tongue without lateral displacement, before advancing toward the vallecula. Subsequently, the blade is lifted to visualize the glottis [22,23]. Once the glottis is centered on the monitor screen, the ETT is inserted into the trachea through the tube channel [24]. The classification of VLs is presented in Table 1.
Table 1. Classification of Video Laryngoscopes.
| Classification | Examples | ||||||
|---|---|---|---|---|---|---|---|
| Non-channeled videolaryngoscope | Macintosh blade | C-MAC® | McGRATH® MAC | ||||

|

|
||||||
| Angulated blade | GlideScope® | C-MAC® D-BLADE | McGRATH® Series 5 | ||||

|

|

|
|||||
| Channeled videolaryngoscope | Airtraq® | Pentax Airway Scope® | |||||

|

|
||||||
NTI DIFFICULTIES
For evaluating and predicting difficult airways and intubations, the acronym "LEMON" is used, which stands for look externally, evaluate the 3-3-2 rule, Mallampati classification (the ratio of tongue size to pharyngeal size), obstruction, and neck mobility. Additionally, the Cormack-Lehane (CL) classification, a grading system commonly used to describe the laryngeal view during DL, is also commonly used [25,26,27].
Difficult airways increase NTI difficulties. Anatomical distortions of the face, oral cavity, and pharynx can impede NTI. As the airway difficulty increases, the success rate of the first attempt at airway intubation decreases significantly. In cases with a CL classification of 3 or 4, indicating a more difficult airway, rapid and high-quality visualization of the glottis, success on the first attempt, and short time to intubation (TTI) are crucial. Studies have suggested that intubation under VL is recommended in such cases [26]. As the number of intubation attempts increases due to failed intubation, the risk of serious complications, such as hypoxemia, aspiration, bradycardia, and cardiac arrest, also increases [26,28,29,30]. Xue et al. reported that VL (glidescope) is more effective than DL during NTI of difficult airways performed by inexperienced surgeons [31].
VIDEO LARYNGOSCOPE TECHNIQUES AND MANEUVERS DURING DIFFICULT NTI
The NTI technique comprises three stages: first, the insertion of the nasotracheal tube (NTT) through the nostril, followed by the introduction of the VL blade into the oral cavity, and then, securing the glottic view via a video monitor. Second, the alignment and entry of the NTT toward the glottic opening is ensured. Third, the NTT is advanced into the trachea [32]. With DL, the most crucial step is to secure a glottic view through direct visualization. Conversely, with the VL, the most important step was to guide the NTT tip toward the glottis, as visualized on the monitor. While the use of VL facilitates an easier and clearer view of the glottis, it does not necessarily guarantee easier intubation [33,34]. During NTI with VL, optimal external laryngeal manipulation (OELM) may not always be necessary because the NTT does not pass through the mouth. However, the larger curvature and size of the blade used in VL can make it challenging to use Magill forceps to guide the NTT tip toward the glottis.
Potential difficulties and assistive maneuvers at each stage of NTI under VL are as follows.
1. Securing the glottic view
When using a DL, the patient’s head and neck are maintained in a sniffing position while the blade is inserted to displace the tongue and reach the vallecula. Upon lifting of the blade at this point, the oral, pharyngeal, and tracheal axes are aligned to enable direct visualization of the glottic view.
In contrast, VLs provide an indirect, expansive view in all directions from the camera at the tip, regardless of various blade angles across different types of VLs. Following general anesthetic induction, the NTT is inserted through a nostril while the patient is in the sniffing position, the VL is then inserted into the patient's mouth and naturally advanced following the anatomical curves within the oral cavity to position the blade tip at the vallecula. Then, it is gently lifted to visualize the glottis through the monitor. In patients with a short muscular neck, reduced range of motion in the neck, prominent chest, or mentosternal adhesions, insertion of a relatively large and curved blade of the VL into the oral cavity can be difficult. In such cases, tilting the head further backward and rotating the handle of the laryngoscope by approximately 90° counterclockwise to avoid contact with the chest can facilitate blade insertion. If a large epiglottis obscures the view of the glottis, attempting OELM or slightly retracting and advancing the blade tip positioned in the vallecula can gently lift and expose the glottis.
2. Alignment and entry of the NTT towards the glottic opening
During OTI using a DL, particularly with a Macintosh blade, the height of the laryngoscope blade itself facilitates the lateral displacement of the tongue. This secures a direct view of the glottis and also creates sufficient space for the passage of the ETT. In OTI, the ETT is inserted from the side of the mouth to avoid visual obstruction, and then, directed towards the glottic opening. With VL, the ETT is typically inserted centrally without displacing the tongue. This results in a narrower space for the ETT to pass through.
In NTI, the tube passes blindly through the nasal cavity, once the tip is visible on the VL monitor, the tube tip is guided towards the glottis by VL, which significantly influences the success of intubation.
1) OELM
When the tube tip appears on the monitor as skewed to the left, right, anterior, or posterior of the glottis, OELM by gentle grasping of the thyroid cartilage can be attempted to adjust its orientation towards the glottis. If the tube tip is positioned on the left or right side of the glottis, the thyroid cartilage should be gently pushed in the same direction. If it is anterior, the larynx is lifted in a cephalad direction. If it is posterior, the larynx is gently pressed downward to align the tube with the glottis.
2) NTT Rotation
If the tip is positioned on the left or right of the glottis, an adjustment can be made by rotating the NTT clockwise or counterclockwise from outside the nostril, respectively.
3) Adjusting the head position and reducing upward lifting of the blade
If the tip is positioned anteriorly, the blade can be lifted further or the patient's head can be flexed. Conversely, if the tip is posterior, the direction of the tip can be adjusted to align it with the glottis by reducing the lifting force on the blade or extending the patient's head to adjust the direction of the tip to align with the glottis [31].
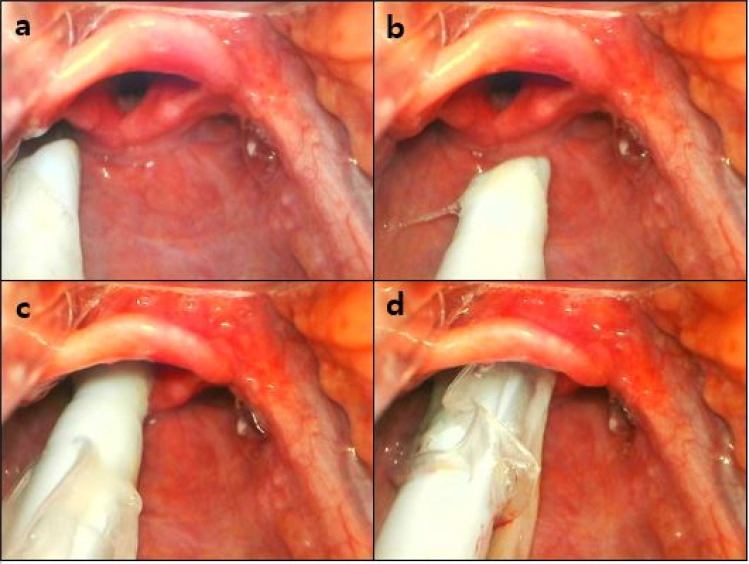
NTT rotation is achieved by reducing the upward lifting of the blade while maintaining a neutral head position as shown in Figures 2 and 3.
Fig. 2. Nasotracheal tube (NTT) rotation by reducing the upward lifting of the blade while keeping the head in a neutral position. (a) The tip is positioned to the left of the glottis. (b) The NTT is rotated 90 degrees clockwise to orient the tip towards the glottis. (c, d) To facilitate a smooth entry of the NTT into the trachea, the upward lifting force on the blade is reduced while the patient's head is maintained in a neutral position.
Fig. 3. Reduction of the upward lifting of the blade. (a) The tip is posterior to the glottis. (b) By reducing the lifting force on the blade, the direction of the tip can be adjusted to align with the glottis.
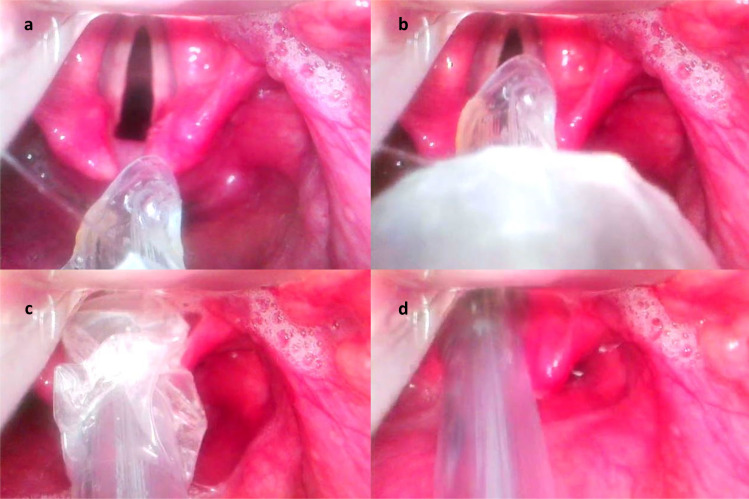
4) Cuff inflation
Inflating the cuff when the tube tip nears the entrance of the esophagus can shift the tip towards the glottis [35,36]. Once the tip passes through the glottis, the cuff is deflated and the tube is further advanced into the trachea. Cuff inflation is shown in Figure 4.
Fig. 4. Cuff inflation. (a) The tip is slightly posterior to the glottis. (b) Inflating the cuff can shift the tip towards the glottis. (c) Once the tip passes through the glottis, the cuff is deflated. (d) The tube is further advanced into the trachea.
3. Advancement of the NTT into the trachea
During OTI using a DL, the anatomical alignment of the oral, pharyngeal, and tracheal axes ensures a nearly straight path for tube insertion. However, with VL, although NTT can be delivered to the glottic entrance, advancement into the trachea can be challenging. This is because glottic visualization can be achieved without aligning the three axes. With NTI, the tube follows the blade curvature to reach the glottic entrance and the tip often points anteriorly to the tracheal axis. In such cases, a forceful insertion should be avoided. During NTI, using a stylet can be difficult and there may be less space to insert the Magill forceps.
1) Neutral head position
During NTI, the discrepancy between the axis of the blade tip and the tracheal axis may be greater in the sniffing position, making a neutral head position relatively more conducive to tracheal entry [35,37]. If the NTT points anteriorly, elevating the head and flexing the neck can help align the axis of the NTT with that of the trachea.
2) Reducing upward lifting of the blade
VL requires less lifting force and can facilitate better alignment of the NTT axis with the tracheal axis [35]. If entry into the trachea is difficult, reducing the lifting force on the blade may be useful [38]. Alternatively, retracting the blade by 1-2 cm to allow the glottis to drop downwards could aid in better alignment with the tracheal axis.
Rotating the bevel of the NTT anteriorly (a 90-degree turn to the right) so that the tip faces posteriorly can also facilitate entry into the trachea [33].
VL-FACILITATED GLOTTIC VIEW DURING NTI
VL provides improved glottic visualization of difficult airways, thereby enhancing intubation success [17]. Previous studies have reported that over 50% of difficult airways are not anticipated and the intubation of 16% of patients deemed low risk during preoperative airway assessments is complicated by poor glottic views during DL [39,40]. Another study reported higher rates of CL grade 1 without OELM during NTI of patients with Mallampati scores of I or II in a seated position, with the VL(McGrath) group showing higher rates than the DL group (83% vs. 57%; P = 0.019) [12]. In conditions, such as ankylosing spondylitis or cervical spine fixation, a clear glottic view can be even more challenging. Malik et al., in their intubation study using DL and VL in patients with cervical spine fixation, showed that VL improved CL grading (P < 0.001) without OELM, thus reducing the difficulty of intubation in patients with cervical spine injuries [41]. Similarly, other studies have demonstrated that patients with CL 3 or 4 during DL improved to CL 1 or 2 when VL is used, and OELM is required less [42,43]. These results suggest that the VL can minimize maneuvers necessary to direct the ETT toward the glottis, thereby reducing the number of intubation attempts.
REDUCTION OF TTI IN NTI UNDER VL
When using VLs, securing a glottic view does not require alignment of the three axes, and the enhanced glottic view [12,40,44,45] allows the practitioner to more quickly identify the vocal cords and target area for tube insertion. Additionally, because the NTT does not pass through the oral cavity, VL manipulation is simplified. The path from the nasopharynx to the trachea is mostly straight, reducing the need for tube manipulation, and thereby, shortening TTI, as indicated in several studies [12,45,46,47]. Jiang et al., in a systematic review of 14 randomized controlled trials comparing DL and VL in NTI, found that VL reduced intubation time (mean difference (MD), −6.72; 95% confidence interval (CI), −10.17 to −3.26; n = 1012; P < 0.05; I2 = 74%), by over 50 seconds, especially in operators with less experience [45]. Kwak et al. reported that the use of VL (McGrath) reduced TTI by 10.5 seconds (P = 0.004) compared to the use of DL in patients with normal airways, and that VL provided a better glottic view in routine NTI (P = 0.003) [12].
In patients with normal airways, VL improves CL grades, making OELM less necessary than DL. However, a better glottic view does not always result in successful intubation; therefore, there may be no significant difference in TTI compared to DL [19,48,49]. Even with an improved view of the glottic entrance using VL, NTT entry can be challenging if the axes of the oral cavity, pharynx, and trachea are not aligned, often necessitating adjustments to the direction of the NTT tip [15,17,50,51]. When using a channeled VL (e.g., Pentax AWS), the thicker blade can make manipulation of the ETT in the oropharynx difficult [52].
NTI EXPERIENCE and SUCCESS RATE UNDER VL
According to the guidelines of the Difficult Airway Society, repeated intubation attempts can decrease success rates and lead to potential injury and complications, potentially culminating in a "cannot intubate, cannot ventilate" scenario that requires invasive airway management. Therefore, maximizing the likelihood of success on the first attempt is recommended. VL, along with supraglottic airway devices and flexible scopes, are recommended for unanticipated difficult airways, underscoring the importance of enhancing the success rates of VL [10,53]. Current guidelines suggest that when individual techniques prove challenging, a combination of methods can be used [10,54]. One such technique includes VL combined with optical/video stylets, flexible intubation scopes, airway exchange catheters, retrograde-placed guidewires, and supraglottic airway placement. A previous study reported that VL (GlideScope) combined with a fiberscope resulted in significantly fewer airway injuries, improved success rates on the first attempt, and shortened TTI compared to using VL with a stylet [55].
Although some studies indicate no overall difference in the success rate of intubation between VL and DL during NTI [13,45], a meta-analysis by Jiang et al. reported that VL increases the first attempt success rate (relative risk (RR), 1.09; 95% CI, 1.00–1.17; n = 930; P = 0.04), especially in cases of difficult airways [45]. Park et al. reported higher success rates on the first attempt in groups using VL than in those using DL (93.8% vs. 74.8%, P < 0.001) [56].
DL requires extensive professional training and experience. In difficult airways, there is a possibility of intubation failure even among skilled anesthesiologists [30,57]. VL, with its superior ability to visualize the glottis, offers relatively high success rates for operators with less intubation experience. Studies comparing the use of VL with DL for NTI have shown a significant decrease in Intubation difficulty according to the Intubation Difficulty Scale (mean ± SD: Airtraq 0.1 ± 0.3, Glidescope 0.3 ± 0.6, respectively, vs Macintosh 0.8 ± 1.0; P = 0.013) [44]. Intubation Difficulty Scale data are shown in Appendix 1 [58].
In a study comparing the first-attempt success rates of 37 inexperienced operators who have performed fewer than six intubations, the success rate of the VL group was higher than that of the DL group (69% vs. 55%, P < 0.01) [59]. A meta-analysis targeting operators with limited experience found that VL increased the success rate of the first intubation attempt (RR 1.8, 95% CI 1.4 – 2.4) compared to DL, but this was not the case in the group with extensive experience (RR 1.0, 95% CI 0.94 – 1.20) [49]. Additionally, Yong et al. reported that VL significantly reduced the intubation learning curve and the time required in normal and difficult airway groups compared with DL (140 s vs. 158 s, 141 s vs. 221.5 s; both P < 0.05) [60]. Another study comparing the first-attempt intubation success rate between DL and VL according to the operator's level of training showed that in less experienced operators, the first-attempt success rate was significantly higher with VL (P = .003, P < .001), while among experienced operators, there was no significant difference (P = 0.561, P > 0.99) [56]. A 10-year study comparing the first-attempt success rates of VL and DL in emergency departments reported an overall increase in success rates from 87.8% to 95.2%, and an increase in the use of VL from 8.4% to 55.4% [61].
These studies suggest that VL offers a relatively high success rate and a shorter learning curve for less-experienced operators. This appears to be particularly beneficial for difficult airways and emergencies.
NTI COMPLICATIONS UNDER VL
In the first prospective study of all major airway events occurring across the United Kingdom during general anesthesia, intensive care unit, and emergency room settings, approximately 42% of the anesthetic events reported were primary airway events indicative of intubation difficulties, many of which were associated with head and neck cancer or airway obstruction [62]. Difficult airways during anesthesia, especially in operating rooms, are less common than those in the intensive care unit or emergency settings (0.4%) [63], and most complications occur during anesthesia induction [64]. Although airway management in the operating room is usually performed by experienced anesthesiologists, for elective operations, major complications include intubation difficulties due to failed attempts, pulmonary aspiration, and airway injury [62]. Other complications related to intubation include dental injury due to laryngoscope manipulation [65,66], esophageal intubation, hypoxemia, severe hemodynamic changes, and cardiac arrest. Minimizing these factors is crucial because of their impact on surgical outcomes [30].
VL, which does not rely on direct visual exposure of the glottis, significantly reduces the compression and distortion of the oropharyngeal structures compared with DL. This helps to avoid or minimize the risk of oropharyngeal tissue damage. Avoiding the use of Magill forceps also reduces the risk of oropharyngeal mucosal trauma. The reduced TTI with VL means a shorter contact time between the blade and the oropharyngeal mucosa. Jiang et al. reported a lower incidence of postoperative sore throat with VL (RR, 0.50; n = 234; P = 0.03), which could be related to these features [45]. Importantly, the increased first-attempt success rate of intubation with VL is likely related to the reduced complication rates.
A study comparing the contact forces exerted on the maxillary anterior teeth between DL and VL reported lower forces with the VL (141.1 ± 15.7 kg for DL vs 48.7 ± 6.7 kg for VL) [67], suggesting a potential reduction in dental injury.
Incidental esophageal intubation, which leads to a higher rate of oxygen desaturation than successful tracheal intubation, is reportedly reduced by VL [68,69,70]. Furthermore, a reduction in the number of intubation attempts and duration of VL during NTI is likely to decrease mucosal damage and the incidence of epistaxis [71].
During OTI, focusing solely on the monitor while inserting the tube into the oropharynx can increase the risk of injury [72]. Therefore, during NTI, it is important to visually confirm the insertion of the blade into the oral cavity, and not rely solely on a monitor [73].
Adequate preoxygenation before intubation, avoidance of excessive force, and minimization of unnecessary manipulation and the number of intubation attempts, can help to reduce complications.
The characteristics of studies of NTI under VL are listed in Table 2. Of the 8 included studies, 6 were randomized controlled trials, and two were systematic review and meta-analysis of randomised controlled trials [13,45].
Table 2. Characteristics of randomized controlled trials and systematic reviews on nasotracheal intubation under video laryngoscope.
| Study type | No (Study) | Included age | Exclusion criteria | Type of VL | Comparison | Experience | Improvement in the CL grade | Overall success | 1st attempt success | Time to intubation | Maneuver | Complications | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Xue F, et al. (2006) [31] | RCT | 156 | 18-59 | Known airway pathology, cervical spine injury | Glidescope | N/A | N/A | Lower rate of grade 3, 4 grade (0% vs 58.3%, P < 0.05) | N/A | 98.1% | 52.7 ± 12.3 s | OELM, change of HNP, reduced upward lifting, rotation of the NTT, blade is withdrawn 1-2 cm (glottis to drop down) | Dental damage, laceration of lips, tongue, pharyngolaryngeal tissues (N = 0) Mild burning sensation of the pharynx (N = 1) |
| Puchner W, et al. (2010) [44] | RCT | 60 | 18-80 | Any predictors of difficult airway management, risk factors for gastric aspiration, history of bleeding, severe bleeding from passage of the nasal tube, more than three intubation attempts, an intubation time exceeding 120 s | Airtraq, GlideScope | DL | familiar with the use of the three laryngoscopes and had performed more than 10 intubations before the start of the study | lower CL grading (P < 0.001) | Lower IDS (P = 0.013), lower difficult intubation (P = 0.001) | N/A | Similar in all groups | Rotation of the NTT, cuff inflation technique, Magill forceps use, OELM Similar in OELM, less upward lifting | Reduced postoperative sore throat (P = 0.048) |
| Suzuki A, et al. (2012) [52] | RCT | 90 | 18-72 | history of cervical spine injury, difficult airway, gastroesophageal reflux disease, body mass index > 35 kg/m2 | Pentax-AWS Airway Scope | DL | N/A | Improved glottic opening (P < 0.05) | 96.67% | N/A | Shorter in Group AWS-I (15 ± 5 sec) than Group AWS-D (28 ± 12 sec, P < 0.01) or Group DL (26 ± 11 sec, P < 0.05) | change of HNP, rotation and advancing-withdrawing of the NTT | No desaturation |
| Kwak HJ et al. (2016) [12] | RCT | 70 | 20-60 | Suspected difficult airway, cervical spine injury, bleeding tendency, required rapid sequence induction | McGrath | DL | N/A | Higher rate of grade 1 83% vs 91% (P = 0.019) | 91% vs 80% (P = 0.32) | N/A | 10.5 s shorter (P = 0.004) | Rotation of the NTT at the external nostrils, OELM, change of HNP, Magill forceps use Frequency of Magill forceps use was lower (6% vs 34%, P = 0.003) |
No difference in oropharyngeal bleeding |
| Sato (Boku) A, et al. (2017) [47] | RCT | 60 | 20-70 | No informed consent, patients with rhinostenosis, expected to be difficult intubation | McGrath MAC, Pentax airway scope | DL | Experienced (more than 6 years of experience) | Improved grade (P < 0.05) | N/A | N/A | McGrath MAC group was significantly shorter than that for Airway scope and DL (P < 0.01) | Magill forceps use, change of HNP, OELM No difference in Magill forceps use, OELM. Less often in change of HNP (P < 0.01) |
No difference in desaturation, lip bleeding, dental injury, mucosal bleeding, esophageal intubation, postoperative pharyngeal pain |
| Jiang J, et al (2019) [45] | Review | 1052(20) | >18 | Studies on manikins, cadavers, simulation studies, observational studies, chronic suppurative sinusitis, midface instability, suspected basilar skull fracture, coagulopathy, or limited mouth opening (< 3 cm) | Airtraq, Pentax AWS, McGrath MAC, C-MAC, Glidescope, McGrath, Airtraq without an integrated channel | DL | Inexperienced (N = 3) Experienced (N = 17) | Higher rate of grade 1(RR = 2.11) | No difference Easier intubation (P < 0.05) *Higher in difficult airway (RR = 1.29), no differenece in normal airway |
Higher (RR = 1.09) *No difference between operators' experience |
6.72 s shorter (P = 0.0001) | Rotation of the NTT, cuff inflation technique, OELM, use of stylet, Magill forceps use Less Magill forceps use (RR = 0.11) |
Lower incidence of postoperative sore throat (RR = 0.50) |
| Zhu H, et al. (2019) [46] | RCT | 99 | 18-60 | Awake NTI, history of reflux or diagnosed esophageal disease, severe obstructive sleep apnea, morbid obesity (body mass index > 40 kg/m2) | Non-channeled King Vision VL, McGrath MAC | DL | Experienced (more than 100 successful NTIs with each device) | Higher rate of grade 1 or 2 (P = 0.0004) | Easier intubation (P < 0.001) | Higher (100% vs 85%, P < 0.05) | King Vision and McGrath group was comparable (37.6 ± 7.3 s vs. 35.4 ± 8.8 s) VL was shorter than DL group (46.8 ± 10.4 s, P < 0.001). |
OELM, Magill forceps use, cuff inflation technique Number of assist maneuver: King vision-5, McGrath-4, Macintosh-18 (P < 0.0001) |
Lower incidence of sore throat (P < 0.01) No desaturation, dental injury No difference in bleeding and hoarseness |
| Gupta N, et al. (2021) [13] | Review | 597 (10) | > 18 | Not in English, without full text, excluded abstract, studies on manikins, cadavers, and simulation studies, patients with a base of skull fracture, coagulation abnormality, reduced mouth opening (< 3 cm), and midface instability | Glide scope, C-MAC D-blade, McGrath, True View EVO2, Pentax Airway scope | DL | N/A | Higher rate of grade 1, 2 (RR = 1.19) | no difference | Higher (RR = 1.10) | 9.04 s shorter (P < 0.001) | Cuff inflation technique, rotation of NTT, Magill forceps use, OELM Maneuvers required were significant higher with DL than with VL (R = 0.22) | No difference in nasal bleeding |
AWS-D, AWS was used and its tip was positioned posterior to the epiglottis for “direct” elevation; AWS-I, blade tip of Airway scope (AWS) was inserted into the vallecula to “indirectly” elevate the epiglottis for laryngeal exposure; CL grade, Cormack-Lehane grade; DL, direct laryngoscopy (Macintosh laryngoscopy); HNP, head and neck positon; IDS, intubation difficulty scale; N, number; N/A, not applicable; NTI, nasotracheal intubation; NTT, nasotracheal tube; OELM, optimal external laryngeal manipulation; RCT, randomized controlled trial; RR, relative risk; s, seconds; VL, video laryngoscopy, *, subgroup analysis.
CONCLUSION
VL has the potential to play a significant role in enhancing the outcomes and safety of patients requiring NTI for oral maxillofacial surgery. Its advantages over DL include better visualization of the glottis, a higher success rate on the first attempt, enhancing accessibility for less experienced physicians, and reducing airway trauma related to laryngoscopy and intubation. VL also has some limitations, such as blade insertion difficulties in patients with anatomical distortion of the head and neck and challenges when guiding the NTT tip into the visualized glottis. To overcome these challenges and improve the overall success rates, increased training, education, and usage are essential.
Appendix 1
Intubation Difficulty Scale score
Footnotes
- Seung-Hwa Ryoo: Conceptualization, Data curation, Writing – original Draft.
- Kyung Nam Park: Data curation, Resources, Software.
- Myong-Hwan Karm: Supervision, Writing – review & editing.
CONFLICTS OF INTEREST: The authors have no conflicts of interest to declare.
References
- 1.Hall CE, Shutt LE. Nasotracheal intubation for head and neck surgery. Anaesthesia. 2003;58:249–256. doi: 10.1046/j.1365-2044.2003.03034.x. [DOI] [PubMed] [Google Scholar]
- 2.Pieters BM, Eindhoven GB, Acott C, van Zundert AA. Pioneers of laryngoscopy: indirect, direct and video laryngoscopy. Anaesth Intensive Care. 2015;43 Suppl:4–11. doi: 10.1177/0310057X150430S103. [DOI] [PubMed] [Google Scholar]
- 3.Henderson J. Miller’s Anaesthesia. 7th ed. Philadelphia: Churchill Livingstone Elsevier; 2010. Airway Management in the Adult; pp. 1573–1610. [Google Scholar]
- 4.Kaplan MB, Ward DS, Berci G. A new video laryngoscope-an aid to intubation and teaching. J Clin Anesth. 2002;14:620–626. doi: 10.1016/s0952-8180(02)00457-9. [DOI] [PubMed] [Google Scholar]
- 5.Cavus E, Kieckhaefer J, Doerges V, Moeller T, Thee C, Wagner K. The c-mac videolaryngoscope: First experiences with a new device for videolaryngoscopy-guided intubation. Anesth Analg. 2010;110:473–477. doi: 10.1213/ANE.0b013e3181c5bce5. [DOI] [PubMed] [Google Scholar]
- 6.De Jong A, Molinari N, Conseil M, Coisel Y, Pouzeratte Y, Belafia F, et al. Video laryngoscopy versus direct laryngoscopy for orotracheal intubation in the intensive care unit: a systematic review and meta-analysis. Intensive Care Med. 2014;40:629–639. doi: 10.1007/s00134-014-3236-5. [DOI] [PubMed] [Google Scholar]
- 7.Huang HB, Peng JM, Xu B, Liu GY, Du B. Video laryngoscopy for endotracheal intubation of critically ill adults: a systemic review and meta-analysis. Chest. 2017;152:510–517. doi: 10.1016/j.chest.2017.06.012. [DOI] [PubMed] [Google Scholar]
- 8.Lewis SR, Butler AR, Parker J, Cook TM, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation. Cochrane Database Syst Rev. 2016;11:Cd011136. doi: 10.1002/14651858.CD011136.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Zundert A, Pieters B, Doerges V, Gatt S. Videolaryngoscopy allows a better view of the pharynx and larynx than classic laryngoscopy. Br J Anaesth. 2012;109:1014–1015. doi: 10.1093/bja/aes418. [DOI] [PubMed] [Google Scholar]
- 10.Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, et al. 2022 american society of anesthesiologists practice guidelines for management of the difficult airway*. Anesthesiology. 2022;136:31–81. doi: 10.1097/ALN.0000000000004002. [DOI] [PubMed] [Google Scholar]
- 11.Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, et al. Difficult airway society 2015 guidelines for management of unanticipated difficult intubation in adults†. BJA: British Journal of Anaesthesia. 2015;115:827–848. doi: 10.1093/bja/aev371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kwak HJ, Lee SY, Lee SY, Cho SH, Kim HS, Kim JY. Mcgrath video laryngoscopy facilitates routine nasotracheal intubation in patients undergoing oral and maxillofacial surgery: A comparison with macintosh laryngoscopy. J Oral Maxillofac Surg. 2016;74:256–261. doi: 10.1016/j.joms.2015.07.021. [DOI] [PubMed] [Google Scholar]
- 13.Gupta N, Gupta A, Sarma R, Batra A, Madan K. Video laryngoscopy vs. direct laryngoscopy for nasotracheal intubation in oromaxillofacial surgery: a systematic review and meta-analysis of randomized controlled trials. Korean J Anesthesiol. 2021;74:439–448. doi: 10.4097/kja.21234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McNarry AF, Patel A. The evolution of airway management - new concepts and conflicts with traditional practice. Br J Anaesth. 2017;119:i154–i166. doi: 10.1093/bja/aex385. [DOI] [PubMed] [Google Scholar]
- 15.Shippey B, Ray D, McKeown D. Case series: the mcgrath videolaryngoscope--an initial clinical evaluation. Can J Anaesth. 2007;54:307–313. doi: 10.1007/BF03022777. [DOI] [PubMed] [Google Scholar]
- 16.Agrò F, Barzoi G, Montecchia F. Tracheal intubation using a macintosh laryngoscope or a glidescope in 15 patients with cervical spine immobilization. Br J Anaesth. 2003;90:705–706. doi: 10.1093/bja/aeg560. [DOI] [PubMed] [Google Scholar]
- 17.Niforopoulou P, Pantazopoulos I, Demestiha T, Koudouna E, Xanthos T. Video-laryngoscopes in the adult airway management: a topical review of the literature. Acta Anaesthesiol Scand. 2010;54:1050–1061. doi: 10.1111/j.1399-6576.2010.02285.x. [DOI] [PubMed] [Google Scholar]
- 18.Asai T. Videolaryngoscopes: Do they truly have roles in difficult airways? Anesthesiology. 2012;116:515–517. doi: 10.1097/ALN.0b013e318246e866. [DOI] [PubMed] [Google Scholar]
- 19.Pieters BMA, Maas EHA, Knape JTA, van Zundert AAJ. Videolaryngoscopy vs. direct laryngoscopy use by experienced anaesthetists in patients with known difficult airways: a systematic review and meta-analysis. Anaesthesia. 2017;72:1532–1541. doi: 10.1111/anae.14057. [DOI] [PubMed] [Google Scholar]
- 20.Maharaj CH, O'Croinin D, Curley G, Harte BH, Laffey JG. A comparison of tracheal intubation using the airtraq or the macintosh laryngoscope in routine airway management: a randomised, controlled clinical trial. Anaesthesia. 2006;61:1093–1099. doi: 10.1111/j.1365-2044.2006.04819.x. [DOI] [PubMed] [Google Scholar]
- 21.Dhonneur G, Ndoko S, Amathieu R, Housseini LE, Poncelet C, Tual L. Tracheal intubation using the airtraq in morbid obese patients undergoing emergency cesarean delivery. Anesthesiology. 2007;106:629–630. doi: 10.1097/00000542-200703000-00027. [DOI] [PubMed] [Google Scholar]
- 22.Suzuki A, Toyama Y, Katsumi N, Kunisawa T, Sasaki R, Hirota K, et al. The pentax-aws((r)) rigid indirect video laryngoscope: clinical assessment of performance in 320 cases. Anaesthesia. 2008;63:641–647. doi: 10.1111/j.1365-2044.2008.05452.x. [DOI] [PubMed] [Google Scholar]
- 23.Suzuki A, Abe N, Sasakawa T, Kunisawa T, Takahata O, Iwasaki H. Pentax-aws (airway scope) and airtraq: Big difference between two similar devices. J Anesth. 2008;22:191–192. doi: 10.1007/s00540-007-0603-1. [DOI] [PubMed] [Google Scholar]
- 24.Hirabayashi Y, Seo N. Airway scope: Early clinical experience in 405 patients. J Anesth. 2008;22:81–85. doi: 10.1007/s00540-007-0580-4. [DOI] [PubMed] [Google Scholar]
- 25.Latimer AJ, Harrington B, Counts CR, Ruark K, Maynard C, Watase T, et al. Routine use of a bougie improves first-attempt intubation success in the out-of-hospital setting. Ann Emerg Med. 2021;77:296–304. doi: 10.1016/j.annemergmed.2020.10.016. [DOI] [PubMed] [Google Scholar]
- 26.Saracoglu KT, Yilmaz M, Turan AZ, Saracoglu A, Kus A, Alparslan V, et al. Evaluation of rescue techniques following failed laryngoscopy: a multicenter prospective observational study. North Clin Istanb. 2023;10:212–221. doi: 10.14744/nci.2021.76402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reed MJ, Dunn MJ, McKeown DW. Can an airway assessment score predict difficulty at intubation in the emergency department? Emerg Med J. 2005;22:99–102. doi: 10.1136/emj.2003.008771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kj D, Shekar B. Adverse events in failed first-pass intubation vs. successful first-pass intubation in the emergency department - an analytical hospital-based study. J Evid Based Med Healthc. 2021;8:283–287. [Google Scholar]
- 29.Pacheco GS, Hurst NB, Patanwala AE, Hypes C, Mosier JM, Sakles JC. First pass success without adverse events is reduced equally with anatomically difficult airways and physiologically difficult airways. West J Emerg Med. 2021;22:360–368. doi: 10.5811/westjem.2020.10.48887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004;99:607–613. doi: 10.1213/01.ANE.0000122825.04923.15. table of contents. [DOI] [PubMed] [Google Scholar]
- 31.Xue F, Zhang G, Liu J, Li X, Sun H, Wang X, et al. A clinical assessment of the glidescope videolaryngoscope in nasotracheal intubation with general anesthesia. J Clin Anesth. 2006;18:611–615. doi: 10.1016/j.jclinane.2006.03.018. [DOI] [PubMed] [Google Scholar]
- 32.Cook TM. A new practical classification of laryngeal view. Anaesthesia. 2000;55:274–279. doi: 10.1046/j.1365-2044.2000.01270.x. [DOI] [PubMed] [Google Scholar]
- 33.Levitan RM, Heitz JW, Sweeney M, Cooper RM. The complexities of tracheal intubation with direct laryngoscopy and alternative intubation devices. Ann Emerg Med. 2011;57:240–247. doi: 10.1016/j.annemergmed.2010.05.035. [DOI] [PubMed] [Google Scholar]
- 34.Lafferty BD, Ball DR, Williams D. Videolaryngoscopy as a new standard of care. Br J Anaesth. 2015;115:136–137. doi: 10.1093/bja/aev193. [DOI] [PubMed] [Google Scholar]
- 35.Chung YT, Sun MS, Wu HS. Blind nasotracheal intubation is facilitated by neutral head position and endotracheal tube cuff inflation in spontaneously breathing patients. Can J Anaesth. 2003;50:511–513. doi: 10.1007/BF03021066. [DOI] [PubMed] [Google Scholar]
- 36.Lin CH, Tseng KY, Su MP, Chuang WM, Hu PY, Cheng KI. Cuff inflation technique is better than magill forceps technique to facilitate nasotracheal intubation guiding by glidescope® video laryngoscope. Kaohsiung J Med Sci. 2022;38:796–803. doi: 10.1002/kjm2.12559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Manabe Y, Iwamoto S, Seto M, Sugiyama K. Appropriate head position for nasotracheal intubation by using lightwand device (trachlight) Anesth Prog. 2014;61:47–52. doi: 10.2344/0003-3006-61.2.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Russell T, Khan S, Elman J, Katznelson R, Cooper R. Measurement of forces applied during macintosh direct laryngoscopy compared with glidescope® videolaryngoscopy. Anaesthesia. 2012;67:626–631. doi: 10.1111/j.1365-2044.2012.07087.x. [DOI] [PubMed] [Google Scholar]
- 39.Paix AD, Williamson JA, Runciman WB. Crisis management during anaesthesia: difficult intubation. Qual Saf Health Care. 2005;14:e5. doi: 10.1136/qshc.2002.004135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yao WL, Wan L, Xu H, Qian W, Wang XR, Tian YK, Zhang CH. A comparison of the mcgrath® series 5 videolaryngoscope and macintosh laryngoscope for double-lumen tracheal tube placement in patients with a good glottic view at direct laryngoscopy. Anaesthesia. 2015;70:810–817. doi: 10.1111/anae.13040. [DOI] [PubMed] [Google Scholar]
- 41.Malik MA, Maharaj CH, Harte BH, Laffey JG. Comparison of macintosh, truview evo2®, glidescope®, and airwayscope® laryngoscope use in patients with cervical spine immobilization. Br J Anaesth. 2008;101:723–730. doi: 10.1093/bja/aen231. [DOI] [PubMed] [Google Scholar]
- 42.Asai T, Liu EH, Matsumoto S, Hirabayashi Y, Seo N, Suzuki A, et al. Use of the pentax-aws® in 293 patients with difficult airways. Anesthesiology. 2009;110:898–904. doi: 10.1097/ALN.0b013e31819c45e5. [DOI] [PubMed] [Google Scholar]
- 43.Jungbauer A, Schumann M, Brunkhorst V, Börgers A, Groeben H. Expected difficult tracheal intubation: a prospective comparison of direct laryngoscopy and video laryngoscopy in 200 patients. Br J Anaesth. 2009;102:546–550. doi: 10.1093/bja/aep013. [DOI] [PubMed] [Google Scholar]
- 44.Puchner W, Drabauer L, Kern K, Mayer C, Bierbaumer J, Rehak PH, et al. Indirect versus direct laryngoscopy for routine nasotracheal intubation. J Clin Anesth. 2011;23:280–285. doi: 10.1016/j.jclinane.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 45.Jiang J, Ma DX, Li B, Wu AS, Xue FS. Videolaryngoscopy versus direct laryngoscopy for nasotracheal intubation: A systematic review and meta-analysis of randomised controlled trials. J Clin Anesth. 2019;52:6–16. doi: 10.1016/j.jclinane.2018.08.029. [DOI] [PubMed] [Google Scholar]
- 46.Zhu H, Liu J, Suo L, Zhou C, Sun Y, Jiang H. A randomized controlled comparison of non-channeled king vision, mcgrath mac video laryngoscope and macintosh direct laryngoscope for nasotracheal intubation in patients with predicted difficult intubations. BMC Anesthesiol. 2019;19:166. doi: 10.1186/s12871-019-0838-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sato Boku A, Sobue K, Kako E, Tachi N, Okumura Y, Kanazawa M, et al. The usefulness of the mcgrath mac laryngoscope in comparison with airwayscope and macintosh laryngoscope during routine nasotracheal intubation: a randomaized controlled trial. BMC Anesthesiol. 2017;17:160. doi: 10.1186/s12871-017-0451-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lambert RC, Ban C, Rivera AU, Eckert GJ, Krishnan DG, Bennett JD. Comparison of direct laryngoscopy and video laryngoscopy in intubating a mannequin: Should video laryngoscopy be available to manage airway emergencies in the oral and maxillofacial surgery office? J Oral Maxillofac Surg. 2015;73:1901–1906. doi: 10.1016/j.joms.2015.03.056. [DOI] [PubMed] [Google Scholar]
- 49.Griesdale DE, Liu D, McKinney J, Choi PT. Glidescope® video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: a systematic review and meta-analysis. Can J Anaesth. 2012;59:41–52. doi: 10.1007/s12630-011-9620-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Taylor AM, Peck M, Launcelott S, Hung OR, Law JA, MacQuarrie K, et al. The mcgrath® series 5 videolaryngoscope vs the macintosh laryngoscope: a randomised, controlled trial in patients with a simulated difficult airway. Anaesthesia. 2013;68:142–147. doi: 10.1111/anae.12075. [DOI] [PubMed] [Google Scholar]
- 51.Noppens RR, Möbus S, Heid F, Schmidtmann I, Werner C, Piepho T. Evaluation of the mcgrath series 5 videolaryngoscope after failed direct laryngoscopy. Anaesthesia. 2010;65:716–720. doi: 10.1111/j.1365-2044.2010.06388.x. [DOI] [PubMed] [Google Scholar]
- 52.Suzuki A, Onodera Y, Mitamura SM, Mamiya K, Kunisawa T, Takahata O, et al. Comparison of the pentax-aws airway scope with the macintosh laryngoscope for nasotracheal intubation: a randomized, prospective study. J Clin Anesth. 2012;24:561–565. doi: 10.1016/j.jclinane.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 53.Asai T. Pentax-aws videolaryngoscope for awake nasal intubation in patients with unstable necks. Br J Anaesth. 2010;104:108–111. doi: 10.1093/bja/aep316. [DOI] [PubMed] [Google Scholar]
- 54.Aikins NL, Ganesh R, Springmann KE, Lunn JJ, Solis-Keus J. Difficult airway management and the novice physician. J Emerg Trauma Shock. 2010;3:9–12. doi: 10.4103/0974-2700.58668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mazzinari G, Rovira L, Henao L, Ortega J, Casasempere A, Fernandez Y, et al. Effect of dynamic versus stylet-guided intubation on first-attempt success in difficult airways undergoing glidescope laryngoscopy: A randomized controlled trial. Anesthesia & Analgesia. 2019;128 doi: 10.1213/ANE.0000000000004102. [DOI] [PubMed] [Google Scholar]
- 56.Park JW, Kim SY, Kim JW, Hong DY, Lee KR, Baek KJ, et al. A study of comparing the first-attempt success of endotracheal intubation and complication rates between glidescope video laryngoscopy and direct laryngoscopy in the emergency department. Journal of the Korean Society of Emergency Medicine. 2021;32:11–18. [Google Scholar]
- 57.Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med. 2013;20:71–78. doi: 10.1111/acem.12055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Adnet F, Borron SW, Racine SX, Clemessy JL, Fournier JL, Plaisance P, et al. The intubation difficulty scale (ids) proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology. 1997;87:1290–1297. doi: 10.1097/00000542-199712000-00005. [DOI] [PubMed] [Google Scholar]
- 59.Howard-Quijano KJ, Huang YM, Matevosian R, Kaplan MB, Steadman RH. Video-assisted instruction improves the success rate for tracheal intubation by novices. Br J Anaesth. 2008;101:568–572. doi: 10.1093/bja/aen211. [DOI] [PubMed] [Google Scholar]
- 60.Yong SA, Chaou CH, Yu SR, Kuan JT, Lin CC, Liu HP, et al. Video assisted laryngoscope facilitates intubation skill learning in the emergency department. J Acute Med. 2020;10:60–69. doi: 10.6705/j.jacme.202003_10(2).0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lee JK, Kang H, Choi HJ. Changes in the first-pass success rate with the glidescope video laryngoscope and direct laryngoscope: a ten-year observational study in two academic emergency departments. Clin Exp Emerg Med. 2016;3:213–218. doi: 10.15441/ceem.16.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: results of the fourth national audit project of the royal college of anaesthetists and the difficult airway society. Part 1: anaesthesia. Br J Anaesth. 2011;106:617–631. doi: 10.1093/bja/aer058. [DOI] [PubMed] [Google Scholar]
- 63.Kheterpal S, Healy D, Aziz MF, Shanks AM, Freundlich RE, Linton F, et al. Incidence, predictors, and outcome of difficult mask ventilation combined with difficult laryngoscopy: a report from the multicenter perioperative outcomes group. Anesthesiology. 2013;119:1360–1369. doi: 10.1097/ALN.0000435832.39353.20. [DOI] [PubMed] [Google Scholar]
- 64.Peterson GN, Domino KB, Caplan RA, Posner KL, Lee LA, Cheney FW. Management of the difficult airway: a closed claims analysis. Anesthesiology. 2005;103:33–39. doi: 10.1097/00000542-200507000-00009. [DOI] [PubMed] [Google Scholar]
- 65.Giraudon A, de Saint Maurice G, Biais M, Benhamou D, Nouette-Gaulain K. Dental injury associated with anaesthesia: an 8-year database analysis of 592 claims from a major french insurance company. Anaesth Crit Care Pain Med. 2018;37:49–53. doi: 10.1016/j.accpm.2017.04.007. [DOI] [PubMed] [Google Scholar]
- 66.Tan Y, Loganathan N, Thinn KK, Liu EHC, Loh NW. Dental injury in anaesthesia: a tertiary hospital’s experience. BMC Anesthesiology. 2018;18:108. doi: 10.1186/s12871-018-0569-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kato Y, Sakuma Y, Momota Y. Comparison of the contact force exerted on teeth by conventional macintosh laryngoscope versus video laryngoscopes. Anesth Prog. 2018;65:151–155. doi: 10.2344/anpr-65-03-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mosier JM, Whitmore SP, Bloom JW, Snyder LS, Graham LA, Carr GE, et al. Video laryngoscopy improves intubation success and reduces esophageal intubations compared to direct laryngoscopy in the medical intensive care unit. Crit Care. 2013;17:R237. doi: 10.1186/cc13061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sakles JC, Javedani PP, Chase E, Garst-Orozco J, Guillen-Rodriguez JM, Stolz U. The use of a video laryngoscope by emergency medicine residents is associated with a reduction in esophageal intubations in the emergency department. Acad Emerg Med. 2015;22:700–707. doi: 10.1111/acem.12674. [DOI] [PubMed] [Google Scholar]
- 70.Jiang J, Kang N, Li B, Wu AS, Xue FS. Comparison of adverse events between video and direct laryngoscopes for tracheal intubations in emergency department and icu patients-a systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med. 2020;28:10. doi: 10.1186/s13049-020-0702-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chandradeva K, Harshan D. The role of the hyper-angulated videolaryngoscope in nasotracheal intubation. Saudi J Anaesth. 2020;14:549–550. doi: 10.4103/sja.SJA_811_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pham Q, Lentner M, Hu A. Soft palate injuries during orotracheal intubation with the videolaryngoscope. Ann Otol Rhinol Laryngol. 2017;126:132–137. doi: 10.1177/0003489416678008. [DOI] [PubMed] [Google Scholar]
- 73.Thorley DS, Simons AR, Mirza O, Malik V. Palatal and retropharyngeal injury secondary to intubation using the glidescope® video laryngoscope. Ann R Coll Surg Engl. 2015;97:e67–e69. doi: 10.1308/003588415X14181254789727. [DOI] [PMC free article] [PubMed] [Google Scholar]