Abstract
Over 75% of surviving extremely preterm infants do not experience major neurodevelopmental disabilities. However, more than half experience challenges in communication, coordination, attention, learning, social, and executive function skills. These “minor” challenges can adversely impact educational and social functioning resulting in physical, behavioral, and social health issues in adulthood. We will review assessment tools for social-emotional and adaptive functional skills in early childhood as these determine family and early childhood supports.We highlight bronchopulmonary dysplasia as an example of the critical intersections of parent well-being, medical and developmental adaptive trajectories in infancy and early childhood, and partnerships between child neurologists and community medical and developmental professionals. We examine studies of engaging parents to promote developmental trajectories, with a focus on supporting parent-child interactions that underlie communication, social-adaptive behaviors, and learning. Recommendations for neurodevelopmental surveillance of extremely preterm infants can also be applied to infants with other risk factors for altered neurodevelopment.
Epidemiology of regulatory and social-emotional behavior dysfunction in preterm infants
Advances in neonatal intensive care have improved survival for the earliest preterm infants.1-3 With these advances has come a decrease in some of the major morbidities of extremely preterm birth, including severe retinopathy of prematurity, severe intraventricular hemorrhage, and late-onset sepsis especially in infants >24 weeks.4-6 However, there has not been a decrease in the diagnosis of bronchopulmonary dysplasia (BPD) despite the increasing use of lung protective strategies, in part due to increased survival of the most preterm infants with the most immature lungs.7,8 Major medical comorbidities after extreme prematurity increase an infant’s risk for developmental delays in early childhood.1,9-15 In many neonatal trials and networks, ongoing surveillance and outcomes have traditionally included assessment for cerebral palsy, cognitive delays, hearing and visual deficits.1,12-15 It has become increasingly recognized that these tests, which are often conducted at 2 years due to the difficulties and expense of longer-term follow-up, do not correlate tightly with subsequent school-age outcomes and do not identify the specific developmental supports required to optimize preschool functioning and kindergarten readiness.16-19 Importantly, 75% of survivors of preterm birth do not have major neurodevelopmental disability by these measures.20
The preterm behavioral phenotype is characterized by co-occurrence of internalizing behaviors such as anxiety, and externalizing behaviors with challenges in attention and social skills.21 Several cohorts have drawn increasing attention to the prevalence of these longer term behavioral challenges. The Extremely Low Gestational Age Newborns (ELGAN) multi-center cohort identified 34% of adolescents to have at least one psychiatric or behavioral health disorder including anxiety, attention-deficit/hyperactivity disorder, or major depression.22 Risk factors for attention deficit hyperactivity disorder or executive function difficulties include perinatal inflammatory markers, neonatal co-morbidities, and family characteristics.23,24
Perinatal brain injury associated with prematurity has most commonly been assessed via cranial ultrasound in the NICU.25-28 Cranial ultrasound abnormality severity and location of injury has been correlated with risk of cerebral palsy, epilepsy and cognitive impairment,29 although developmental trajectories shift between age 2 and later childhood and adolescent assessments.19,30,31 There are more complex relationships between cranial ultrasound findings, communicative and social delays, and behavioral traits that can be precursors for an autism spectrum disorder. Although preterm infants have an increased risk of positive autism screenings, cranial ultrasound abnormalities were not correlated with incidence of early problems on the Child Behavior Checklist or diagnosis of autism at 10 years in the ELGAN cohort.30,32 This differs from EPICURE and other cohorts which have found associations between positive autism screening and ventricular enlargement on ultrasound and cerebellar injuries at term equivalent using MRI.33-36 These diagnostic complexities may reflect differences in imaging inclusion of cerebellar injury or isolated ventricular enlargement, as well as nuances of understanding behavioral symptoms such as hypersensitivity to input, or co-occurring language and cognitive delays that can be captured in constructs such as pretend play, social interactions, and empathetic behaviors.37,38
Bronchopulmonary dysplasia (BPD) is associated with a spectrum of developmental delays in early childhood.39,40 The mechanism for this association is likely multifactorial, and includes inflammatory complications that predispose to both chronic lung disease and brain injury, extreme prematurity with its prolonged exposure to positive pressure ventilation and neurosedative medication limiting opportunities for normal interactions in the NICU, and chronic respiratory insufficiency in and after the NICU limiting energy for play and typical development. In the NICHD Neonatal Research Network cohort, increasing BPD severity was associated with increased withdrawn behavior and multi-domain developmental problems, but with less sleep problems and aggressive behaviors; some but not all behavioral problems were mediated by delays in cognitive, language and motor skills.41 Later in childhood, school age children with a history of BPD have been noted across multiple studies to experience more difficulties with school, repeating grades or requiring special services, and challenges in executive function.42-46 Infants with the most severe BPD who require mechanical ventilation at 36 weeks corrected age are at highest risk for developmental concerns through childhood. These children are at higher risk for global developmental delays and autism spectrum concerns which further increases if they have chronic respiratory failure requiring tracheostomy and home mechanical ventilation.43-46
Assessment of regulatory and social-emotional behaviors
Although behavioral and adaptive functioning is traditionally assessed in school-age children, increasing attention to these skills in early childhood reflects the increased recognition of the importance of emerging regulatory and adaptive behaviors as a potential indicator of subsequent dysfunction. Earlier screening in these domains also facilitates opportunities to coach parent-child interaction, aiming to increase responsiveness to early childhood cues and improve feeding, sleep, developmental and social-emotional competencies.47
Infants with surgical co-morbidities and severe BPD are often exposed to significant neurosedative medications and a prolonged NICU length of stay well past their corrected term equivalent. These critically ill infants often receive limited assessments of developmental skills due to ventilator dependence. Additionally, parent uncertainty and caregiver variation may limit opportunities for soothing an infant’s dysregulated state control and mitigating responses to procedural stressors.48
An ideal measurement strategy in this population would 1) incorporate behavioral regulation as an aspect of developmental trajectories; 2) be observable including on ventilator-dependent patients; 3) require a less lengthy examination due to the medical fragility of this patient population; 4) allow sequential use during the first 1000 days to evaluate trajectories rather than relying on one-time assessments; 5) need less specialized training to allow standardization between centers with limited practitioners capable of performing longer standardized assessments; 6) facilitate partnership with parents, nurses, and allied health specialists to allow sequential core measures and trained developmental observations; 7) incorporate screening and support for parent mental health and parent-child interaction, especially supporting teachable moments that impact early developmental trajectories.
Given the gaps that exist in commonly utilized screening tools, and different perceived abilities to screen for regulatory and social-emotional function across infancy and early childhood, we now review some of the most frequently used measures in neonatal follow-through programs by age range, time required, psychometric properties and populations studied, with comments on opportunities and limitations. Our goal is to synthesize pragmatic strategies across primary care, child neurology, home visiting and neonatal follow-through programs.
Bayley Scales of Infant and Toddler Development
Traditional measurement of early childhood development for former preterm infants includes the norm-referenced Bayley Scales of Infant and Toddler Development (BSID), which has undergone substantial revisions in recent years; the BSID-II reported a mental and psychomotor developmental index; the BSID-III allowed scoring in cognitive, language and motor composite scores and added parent reports of Adaptive Behavior and Social Emotional Skills (ABAS).49-51 The ABAS and the Greenspan Social Emotional Chart were the basis of these parent questionnaires.52,53 The newest iteration, the BSID-IV, now assesses 5 domains: cognitive, language, motor, social-emotional and adaptive behavior.54 Adaptive content has been taken from the Vineland Adaptive Behavior Scales and updated based on feedback.55 The BSID-IV normative sample was stratified according to the 2017 United States census data by age, sex, race/ethnicity, and parent education level. To ensure representation of a full ability range, the BSID-IV special needs sample included children with Down syndrome, autism spectrum disorder, language delay, specific language impairment, developmental delay, motor impairment, those born moderate-late preterm and very-extremely preterm, and those with prenatal alcohol and drug exposure. Other advantages to the BSID-IV include its correlations with the Wechsler Preschool and Primary Scale of Intelligence (WPPSI-IV) and Peabody Developmental Motor Scales (PDMS II), and the scale’s widespread use in neonatal follow-up programs worldwide.56,59 Disadvantages include the loss to follow-up common in neonatal follow-up programs, certification requirement, need for in-person assessment in children who may have multiple other medical appointments, and time requirement of 30-70 minutes depending on the child’s age.
Ages and Stages Questionnaire-3rd Edition
General pediatric offices most commonly screen childhood development using tools like the Ages and Stages Questionnaire.-3rd Edtion (ASQ-3).58,59 Questions are written at a 4th to 6th grade level, take 10–15 minutes to complete, and are available in Arabic, English, French, Spanish, Chinese and Vietnamese and several other languages. Scoring requires 2-3 minutes of professional time; domain scores are classified as 1) reassuring; 2) need to monitor and rescreen in 2 months; or 3) refer for additional assessments. Areas screened in these questionnaires include gross motor, fine motor, communication, problem-solving, and personal-social. The ASQ-3 normative sample included 18,527 questionnaires for children from diverse racial and socioeconomic backgrounds. Psychometric properties included test-retest reliability at 0.91, inter-rater reliability at 0.92, concurrent validity with the Battelle Developmental Inventory at 0.82 to 0.88, with sensitivity of 0.86 and specificity of 0.85. The advantages of ASQ-3 are cumulative experience of 30 years, robust selection of items based on sources including Gesell Developmental Observation Scale, the Bayley Scales of Infant Development, the Battelle Developmental Inventory, and Developmental Resources: Behavioral Sequences for Assessment and Program Planning.49-51,60-62 The parent-reported age-based questionnaires are embedded within most primary care electronic medical records, which can facilitate proactive access to early intervention services and parenting supports without a requirement for trained examiners or intensive specialty clinic access. It also may be easier to understand developmental trajectories using a parent questionnaire-based approach in circumstances where repeat intensive BSID evaluations are not feasible.63 In order to minimize risk of confusion between primary care screening and specialist hands-on surveillance, primary care offices should be an important place to emphasize that developmental screening can never be done using one instrument at one time alone and must continue at regular intervals until kindergarten entry and during the school years.
When considering an appropriate toolkit for screening early childhood development that includes behavioral and adaptive competencies, it is important to determine what resources are in place to ensure the success of a given strategy. An ideal toolkit should encompass appropriate measures that minimize testing burden, support longitudinal trajectory assessments, evaluate important functioning domains that promote kindergarten readiness, and allow collaboration between primary care, subspecialists and early intervention teams.
Building on recent recommendations from the American Academy of Pediatrics to support primary care medical homes, a recent guideline provided a framework for monitoring preterm infants for neurodevelopmental outcomes in early childhood.64 This framework consolidates contemporary outcomes research over the past two decades , and stratifies prematurity and NICU experiences by degree of risk for adverse developmental and behavioral outcomes. Table 1 presents a summary of instruments recommended for high-risk infant neurodevelopmental follow-up during the first 1,000 days of life based on psychometric evidence as comprehensive maximum data sets. Table 1 represents recommended and current practices for interdisciplinary focused teams who can prioritize comprehensive assessments at age 2-2.5 years, but who may not reasonably see all high-risk children currently prioritized in neonatal research networks. They are ideal when there are early child educators and rehabilitation therapists credentialed in the Bayley IV or Battelle Developmental Inventory, 2nd Edition or Mullens Scale of Early Learning 63as well as accessible and trained rehabilitation therapists from physical, occupational and speech therapy. It should be noted that the Peabody Developmental Motor Scale, 2nd Edition59 and Preschool Language Scales, 5th Edition 57 require trained pediatric motor therapists as well as trained pediatric speech language professionals.
Table 1:
Instruments recommended for high-risk infant neurodevelopmental follow-up during based on psychometric evidence in a well-staffed and well-resourced specialty clinic.
| Domain | Screening | Diagnostic |
|---|---|---|
| Multidomain | Ages & Stages Questionnaires®, Third Edition; |
Developmental: Bayley Scales of Infant and Toddler Development, Fourth Edition; Battelle Developmental Inventory, Second Edition; Developmental Profile 4 (DP™-4); Mullen Scales of Early Learning Adaptive Functioning: Adaptive Behavior Assessment System™, Third Edition; Pediatric Evaluation of Disability Inventory Computer Adaptive Test; Vineland Adaptive Behavior Scales, Third Edition; Warner Initial Developmental Evaluation of Adaptive and Functional Skills™ |
| Neurological | General Movements Assessment (0 to 5 months) | Hammersmith Infant Neurological Assessment (2 to 24 months) |
| Motor | Alberta Infant Motor Scale (0 to 18 months) | Peabody Developmental Motor Scales, Second Edition |
| Language | Communication and Symbolic Behavior Scales Developmental Profile™ (6 to 24 months) | Preschool Language Scales, Fifth Edition |
| Socioemotional | Brief Infant-Toddler Social and Emotional Assessment (12 to 36 months) | Ages & Stages Questionnaires®: Social-Emotional, Second Edition; Child Behavior Checklist (1.5 to 5 years); Infant-Toddler Social & Emotional Assessment – Revised (1 to 3 years); Greenspan Social-Emotional Growth Chart (0 to 42 months) |
| Sensory Processing | - | Test of Sensory Functions in Infants (4 to 18 months); Sensory Profile 2 |
In many settings, there may be limited resources to conduct comprehensive surveillance at ongoing intervals through early childhood. In the setting of limited clinic capacity and an increasingly recognized range of communicative, developmental and social behavioral disorders that place infants at high risk for an autism spectrum disorder, we propose an alternative hybrid model that relies upon teamwork between fetal and neonatal neurologists, primary care practices, and high-risk infant follow-through clinics. Table 2 highlights a proposed collaborative tool kit that minimizes the requirement for trained examiners and lengthy appointment times.
Table 2.
Proposed collaborative model of high-risk neurodevelopmental screening and surveillance
| Domain | Screening tool | Surveillance |
|---|---|---|
| Motor | ASQ-3. Gross and Fine Motor Motor Quotient |
AIMS HINE |
| Communication | ASQ-3 Receptive and Expressive Language | Capute CLAMS |
| Cognitive | ASQ-3 Cognitve | Capute CAT |
| Adaptive | ASQ-3 Personal-Social | WIDEA-FS |
| Social-Emotional | ASQ-3 :Social-Emotional | BITSEA;ASQ-SE-2 M-CHAT-R/F |
AIMS=Alberta Infant Motor Scale.119,120 ASQ-3 =Ages and Stages Questionnaires -3rd Edition. Capute CAT=Clinical Adaptive Test 3. Capute CLAMS= Clinical Linguistic and Auditory Milestone Scale.121,122 WIDEA-FS= Warner Initial Developmental Evaluation of Adaptive and Functional Skills. BITSEA= Brief Infant Toddler Social -Emotional Assessment. ASQ-SE-2=Ages and Stages Questionnaire-Social Emotional-2nd Edition.73 M-CHAT-R/F= Modified Checklist for Autism in Toddlers, Revised, with Follow-Up.
HINE=Hammersmith Infant Neurological Exam123
Since the purpose of this paper is to focus on screening and surveillance of social-emotional and adaptive functioning, we will describe these measures in more detail.
Social-emotional development in children under 6 years of age encompasses both attainment of social-emotional developmental milestones as well as early childhood mental health. Typical development in young children includes assessment of joint attention, social interest, pretend play, understanding the perspectives of other people, developing emotional regulation, and emerging prosocial skills like taking turns and sharing. To the extent that some of these milestones are developmental, their assessment can be considered a strength-based approach. Other assessments are more mental-health-focused. In early childhood this includes externalizing behaviors, such as aggression, temper tantrums and noncompliance; internalizing behaviors such as sadness or anxiety, social withdrawal, or physical symptoms. These symptoms are the early childhood equivalent of behavior health disorders. There is significant overlap between socio-emotional development, attention-deficit/hyperactivity disorder (ADHD) and autism-related symptoms.
In this review we considered properties of assessment tools; a focus on assessing developmental attainment, mental health or both; and repeatability in a longitudinal surveillance context. Some psychometric evaluations of measures were conducted in children of a wider age range, with limited study in children under 6. Many assessments require purchase (Appendix).
Adaptive:
The Warner Inventory of Developing and Emerging Adaptive and Functional Skills (WIDEA-FS) was developed to assess emerging self-care, mobility, communicative, and social skills in early childhood. This tool has been used in many early childhood populations including those receiving neurological neonatal intensive care, infants with neonatal encephalopathy, preterm infants with retinopathy of prematurity or in neuroprotective trials of extreme prematurity, in non-microcephalic congenital Zika virus, and in inborn errors of metabolism.65-67 In preterm infants it has been validated against the CAT/CLAMS and Bayley scales; the WIDEA-FS has been used to assess development in infants with BPD in a phone or electronic questionnaire format.68-70
Social:
The Infant Toddler Social Emotional Assessment (ITSEA) was developed to assess internalizing, externalizing, and regulatory behaviors between 1 and 3 years as well as social competencies and has been used in diverse at risk community samples.71 A short version of this evaluation tool, the Brief Infant Toddler Social Emotional Assessment (BITSEA), has 34 items, takes 10 minutes to administer and score, and has been used in the US Neonatal Research Network.72 The BITSEA includes items that serve as indicators of autism spectrum disorders and clinically significant behavior stressors (internalizing, externalizing, dysregulation) that require discussions to insure appropriate management and intervention strategies. It gives total scores for social-emotional problems (including internalizing and externalizing behavior) and social-emotional competence.
The ASQ SE-2 is a caregiver report questionnaire for children as young as 1 month of age.73 It assesses socio-emotional development including self-regulation, compliance, social communication, adaptive functioning, autonomy, affect and social interaction. It takes 10-15 minutes to complete. It has shown excellent internal consistency and inter-rater reliability, high agreement with other measures and good predictive validity.
The Child Behavior Checklist is a caregiver report questionnaire, with a preschool version that can be used as young as 1.5 years of age.74 It assesses mental health constructs of internalizing and externalizing behavior. A systematic review found that it correctly classified 84% of children with emotional and behavioral problems.75
The Greenspan Social-Emotional Growth Chart is a caregiver-report questionnaire that can be used from birth to 3.5 years, which focuses on development of social-emotional skills.53 It showed good construct validity with the BSID-III, excellent internal consistency, and predictive validity as a screening tool for autism spectrum disorders with a sensitivity of 0.87 and specificity of 0.90.
Parent interaction in promoting emerging early childhood socio-emotional competencies
There is increasing evidence that promoting parent understanding of infant states and cues and participating in care during the NICU stay supports parent wellbeing as well as infant growth and regulatory behaviors. Preterm infants experience more feeding and sleeping difficulties and procedural stressors that are accompanied by infant disorganization.76 Parents of very preterm infants need to be more sensitive and responsive, but they themselves are under psychological stress dealing with the family disruptions of preterm birth and prolonged hospital stays.77 This places families at high risk for difficulties in parent–child interactions, heightening the risk of problems with early childhood social-emotional development. Even for preterm children with medical risk factors, a stimulating home environment and sensitive parent–infant relationship are associated with better neurodevelopmental outcomes.78,79 A Cochrane review on early intervention for preterm infants concluded that early intervention programs that focused on the parent–child relationship were more effective than programs focused on the child or the parent alone.80
It is critical to recognize that high-risk infant neurodevelopmental follow-up includes an evaluation of the nature and quality of early parent-child interactions, defined as reciprocal dyadic relationships between the primary caregiver and the child. Such interactions provide a reliable measure of early parent-child attachment and bonding, known to influence a child's development, particularly cognitive, language, and socioemotional outcomes. Most existing parent-child interaction measures suitable for use in a clinical (rather than research) setting require highly trained professionals to observe and code the interaction in a controlled (rather than naturalistic) setting, either in vivo or via videotape recordings. While direct observational measures are considered the "gold standard," less time-consuming methods such as parent interviews and self-report on standardized rating scales can also provide useful information. Many articles have summarized the current state of evidence regarding parent-child interaction assessments, including various measures.81-85 -
We propose the following key recommendations to facilitate the incorporation of relational assessment of parent-child interaction in a family centered high-risk infant neurodevelopmental follow-through during the first 1,000 days of life.
While mother-child interactions are typically the focus of parent-child interaction assessments, father-child interactions should be considered where applicable for a comprehensive assessment due to their potential associations with child outcomes and mother-child interactions.
In addition to structured assessments of parent-child interactions, naturalistic observations of parent-child interactions in various contexts should be considered.
Understanding the underlying relational dynamics and identifying appropriate intervention targets require both observations of parent-child interactions and understanding parental perceptions and expectations of their child.
Given that parenting practices are strongly influenced by culture and vary across cultures, observations of parent-child interactions should take into account parental cultural contexts, as well as family socioeconomic status and theoretical frameworks.
Early neonatal hospitalizations, either directly or indirectly, impact parental mental health, parenting behaviors, and parenting experiences. Therefore, screening for these conditions is essential for a reliable assessment of parent-child interactions.
Given the bidirectional nature of parent-child interactions, child neonatal clinical and neurodevelopmental contexts must be considered alongside parental and family contexts.
Current psychometric evidence of early parent-child interaction assessments is generally weak.86 As a result, exercising caution when implementing and interpreting these assessments in the absence of a more holistic assessment is advised.
A critical issue in developmental pediatrics is how best to implement parenting supports to promote parent participation and understanding of their child's development.87 Several engagement strategies for parents have been undertaken, including early kangaroo mother care, Newborn Individualized Developmental Care and Assessment Program, Vermont Mother-Infant Interaction, and the Canadian Family Integrated Care models.88-93 The Dutch post-NICU-discharge responsive parenting program, called TOP, has started to be reimbursed by health insurers and now forms part of routine care in the Netherlands.94 Several model programs are moving toward the types of comprehensive, multilevel interventions that will be needed to transform the system of supports for premature infants and their families.95-106
Positive Parenting Program (Triple P)
The Positive Parenting Program (Triple P) was designed to provide parents with a supportive behavioral health network linked to both pediatric and parental concerns.107,108 The Baby Triple P for Preterm Infants focuses on normalizing preterm parenting by providing feedback and information on each child’s early developmental signals and response repertoire.110
The emphasis is on creating a safe environment for learning about parenting and building positive parent-infant relationships. Parents learn adaptive coping skills for managing stress and for navigating shared partner caregiving. This intervention addresses health, development, parenting, and caregiver well-being. As parents learn to recognize infant cues, manage regulatory and sleep challenges, feel supported by their partners, and have access to community resources, they can experience themselves as their infant's first and competent teachers. They also learn which behavior interventions are most helpful in promoting their child's learning.
Triple P has shown preventive efficacy for children with a diverse variety of behavioral, family, medical, and social risks. Baby Triple P demonstrated that at 2 years' corrected age, children in the intervention group had significantly increased cognitive, motor, and social communication skills compared with controls.110 In addition, infants in the intervention group demonstrated increased competencies in symbolic play, a key developmental area involving imitation, social learning, and problem solving. All effect sizes were mild to moderate, but this is significant in the context of a low-cost intervention that can be widely disseminated.
Hospital to Home: Optimizing the Preterm Infant’s Environment (H-HOPE)
H-HOPE aims to engage parents of preterm infants in regular caregiving by teaching them how to understand and respond to infant cues when infants are 30-36 weeks’ gestational age.111 The programmatic goal is to facilitate infant behavioral organization around feeding routines and bundled activities to respect the infant’s sleep, pain, and quiet activities.112 A nurse/developmental–family support advocacy team provides maternal education and social support on infant-directed use of auditory, tactile, visual, and vestibular stimuli. H-HOPE intervention integrates parenting, medical, and developmental interventions in a proactive participatory framework that is family-centered, parent-mediated, and interdisciplinary. This enables the intervention to continue at home when professionals are absent.
When compared to usual care, H-HOPE participants demonstrated increased parenting confidence, improved short-term oral motor organization, cranial growth, and early motor skills. H-HOPE also reduced overall in-hospital costs, optimized post-discharge adherence to medical and developmental follow-up, and increased parent–infant interactive engagement.111,112
Learning Games Developmental Activities in The Infant Health& Development Program (IHDP)
The Learning Games curriculum focuses on how parent-mediated developmental interventions can minimize the effect that poverty has on at-risk preterm children.109 The IHDP was an 8-site, multicenter study with enrollment in 1985 to 1986, consisting of home visits every week for the first year and every other week for the second and third year. Visits focused on problem-solving training for parents to increase their general adaptational and parenting skills. The program also included daily center-based education between chronological ages 12 and 36 months, parent support groups, and intensive pediatric follow-up care. At age 3 years, children received access to early Head Start and early childhood community-based education programs.109,114 Motivation was regarded as a key component of adaptation and success and was influential in the development of Head Start program goals emphasizing psychological and socioemotional development. The IHDP demonstrated that preterm children with access to integrated medical, parenting, and developmental activities had improved chances of being developmentally on track at age 3 years and subsequently experienced improved academic success. Importantly, parents who struggled in school themselves were better able to partner with the child’s teachers and advocate for the child’s supports, promoting inclusion and success.109
Summary
From a research perspective, it would be ideal to collect robust data on a broad array of related constructs. In reality, measurement is limited by participant burden, psychometric properties of available measures, and availability of trained staff to administer and ensure robust follow-up. To understand childhood trajectories and the impact of interventions, a pragmatic approach may be for multiple coordinated centers to coalesce around a core set of brief essential measures, with understanding that a fuller more ideal set of measures may be employed in certain scenarios. To accomplish this goal we must form partnerships with primary care physicians and parents to promote emerging developmental, regulatory and social competences. Just as neurodevelopmental surveillance must go beyond major neonatal morbidities and major neurodevelopmental impairment, we must realize that risk does not equal disability, that parenting supports after critical illness must be proactive and accessible, and activity-based interventions of mobility, play, exploration and social communication are critically important for learning.113-115
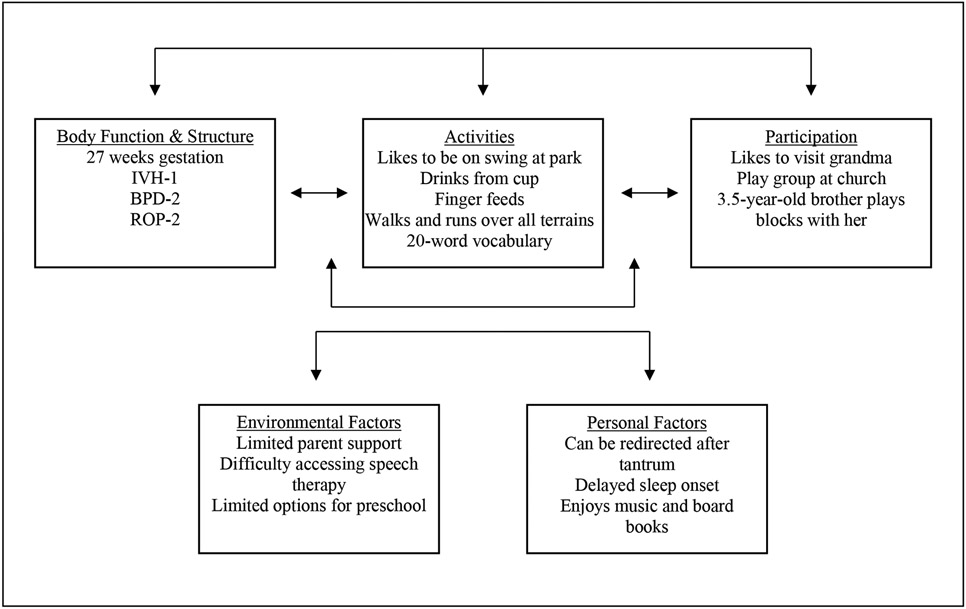
One way to conceptualize our outcome framework is to use the ICF model illustrated in Figure 1. The International Classification of Functioning, Disability and Health (ICF) model offers a framework for measuring child outcomes. The strengths of this model are a that it offers a whole child approach focusing on how impairments (at organ system level) and activities (whole person level) impact child functioning and the context of facilitators and barriers to participation (home, school, community). The ICF model can be applied to considering the whole child as illustrated by this 2 year old who survived extreme prematurity and experienced stage 2 BPD as well as communicative delays and limitations in family and community resources.115
Fig. 1.
ICF-Model: 2-year-old girl with extreme prematurity with communication delays and limited family and community resources
Our neurodevelopmental follow-through efforts must emphasize that parent mental health is a critical mediator of child development and regulatory skills during feeding, play and sleep.101-105,116,113Our biopsychosocial framework of engagement, functioning and child and family wellbeing can lead to a better understanding of how the immature brain adapts and benefits from postnatal experience-dependent plasticity.91,117,118
Parent well being is a critical determinant of early childhood dyadic learning; therefore, supporting early childhood learning requires close attention to explicitly teaching vulnerable parents their essential roles and supporting their engagement. Social disadvantage increases the risk of suboptimal parent physical and behavioral health. Social disadvantage also decreases the chance that the child will have a quality medical home, access to subspecialists and care coordination, and access to early intervention, habilitative therapies, and quality early childhood education. Our framework helps us partner in a comprehensive and compassionate way to promote activities essential for exploration, communication, regulatory behaviors, and early learning. 104,107,109,112,114,118 These efforts can scaffold developmental plasticity in early childhood for long-term socio-emotional and developmental competencies essential to school and community success.
Highlights:
Though 75% of extrtemely preterm infants do not experience major neurodevelopmental disability at age 2, the majority of survivors are at risk for a spectrum of of communication, coordination, attentionlearning, social and executive function challenges.
We highlight social emotional and adaptive skill measures as they help families in understanding their child and can be linked to parent-mediated interventions to support emerging developmental competencies.
Scaffolding parenting skills during the stressors of neonatal intensive care, early childhood, and preschool years helps children’s developmental functioning and optimizes parental well being.
Acknowledgements:
Dr. Msall’s efforts were supported in part by The Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (UA6MC32492), the Life Course Intervention Research Network Preterm Research Node and in part by NIH NICHD R01HD105234.
Dr. Lagatta’s efforts were supported in part by NIH NHLBI K23 136525. Dr. Bora’s efforts were supported in part by University Hospitals Cleveland Medical Center and Case Western Reserve University School of Medicine's Joint Strategic Research Investment.
Appendix: social-emotional measures
| Assessment tool | Domains tested |
Age range |
Screening or standardized assessment |
Primary purpose | Type of test |
Test procedure |
Equipment/manual cost |
Time to administer/score (min) |
telehealth applicable |
|---|---|---|---|---|---|---|---|---|---|
| Ages and Stages Questionnaire Social Emotional 2 | social-emotional | 1- 72 months | standardized assessment | Social-emotional development | Norm | Parent-report | $275 manual. See link for more info: https://agesandstages.com/about-asq/why-screening-matters/social-emotional-screening/ | <10 minutes | yes |
| Child Behavior Checklist 1.5-5 (part of the ASEBA) | social-emotional | 1.5- 5 years | standardized assessment | Social-emotional development and internalizing/externalizing behavior | Norm | Parent-report | Manual $45 pack of 50 forms $30 | 10 minutes | yes |
| Strengths and Difficulties Questionnaire (SDQ) 2-4 years | social-emotional | 2-4 years | standardized assessment | Externalizing/internalizing behavior (plus some social-emotional development) | Norm | Parent-report | free | 5 minutes | yes |
| Baby Pediatric Symptom Checklist/Preschool Pediatric Symptom Checklist (part of Survey of Wellbeing of Young Children SWYC) | social-emotional | 1-65 months | standardized assessment | Norm | Parent-report | free | <5 minutes | yes | |
| Brief Infant Toddler Social and Emotional assessment (BITSEA) | social-emotional | 12-36 months | screening/standa rdized assessment | Social-emotional development and internalizing/externalizing behavior | Norm | Parent-report | $170.71 kit | 7-10 minutes | yes |
| Devereux Early Childhood Assessment for Infants and Toddlers | social-emotional | 1-36 months | ? | Norm | Parent-report | $199/95 manual | <10 minutes | yes | |
| Greenspan Social-Emotional Growth Chart | social-emotional | 0-42 months | standardized assessment | Social-emotional development | Norm | Parent-report | $115 manual | <10 minutes | yes |
| Infant Toddler Social and Emotional assessment (ITSEA) | social-emotional | 12-35 months | standardized assessment | Social-emotional development and internalizing/externalizing behavior | Norm | Parent-report | $286-348 for ITSEA and BITSEA | 20-30 minutes | yes |
| M-P-R (a part of the Merrill-Palmer-Revised Scales of Development-social emotional) | social-emotional | 1-78 months | standardized assessment | Norm | Parent-report | $925 for full M-P-R | <5 minutes | yes | |
| The Behavior Assessment System for Children Second Edition (BASC-3) | social-emotional | 2-22 years | standardized assessment | Social-emotional development and internalizing/externalizing behavior | Norm | Structured developmental history, observation system, parent-report, self-report and teacher-report | $146 for BASC-3 Manual and 10 Q-global Interpretive Summary Report usages | 10-20 minutes | yes |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Zayegh AM, Doyle LW, Boland RA, et al. Trends in survival, perinatal morbidities and two-year neurodevelopmental outcomes in extremely low-birthweight infants over four decades. Paediatr Perinat Epidemiol. Sep 2022;36(5):594–602. doi: 10.1111/ppe.12879 [DOI] [PubMed] [Google Scholar]
- 2.Torchin H, Morgan AS, Ancel PY. International comparisons of neurodevelopmental outcomes in infants born very preterm. Semin Fetal Neonatal Med. Jun 2020;25(3):101109. doi: 10.1016/j.siny.2020.101109 [DOI] [PubMed] [Google Scholar]
- 3.Cheong JL, Spittle AJ, Burnett AC, Anderson PJ, Doyle LW. Have outcomes following extremely preterm birth improved over time? Semin Fetal Neonatal Med. Jun 2020;25(3):101114. doi: 10.1016/j.siny.2020.101114 [DOI] [PubMed] [Google Scholar]
- 4.Morgan AS, Mendonga M, Thiele N, David AL. Management and outcomes of extreme preterm birth. BMJ. Jan 10 2022;376:e055924. doi: 10.1136/bmj-2021-055924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doyle LW, Darlow BA. The changing face of neonatal intensive care for infants born extremely preterm (<28 weeks' gestation). Semin Perinatol. Dec 2021;45(8):151476. doi: 10.1016/j.semperi.2021.151476 [DOI] [PubMed] [Google Scholar]
- 6.Doyle LW, Cheong JLY. Changing outcomes for infants born extremely preterm. Semin Perinatol. Dec 2021;45(8):151475. doi: 10.1016/j.semperi.2021.151475 [DOI] [PubMed] [Google Scholar]
- 7.Lee SM, Sie L, Liu J, Profit J, Lee HC. Evaluation of Trends in Bronchopulmonary Dysplasia and Respiratory Support Practice for Very Low Birth Weight Infants: A Population-Based Cohort Study. J Pediatr. Apr 2022;243:47–52.e2. doi: 10.1016/j.jpeds.2021.11.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Latini G, De Felice C, Giannuzzi R, Del Vecchio A. Survival rate and prevalence of bronchopulmonary dysplasia in extremely low birth weight infants. Early Hum Dev. Jun 2013;89 Suppl 1:S69–73. doi: 10.1016/S0378-3782(13)70020-3 [DOI] [PubMed] [Google Scholar]
- 9.Schmidt B, Asztalos EV, Roberts RS, et al. Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months: results from the trial of indomethacin prophylaxis in preterms. JAMA. Mar 05 2003;289(9):1124–9. doi: 10.1001/jama.289.9.1124 [DOI] [PubMed] [Google Scholar]
- 10.Schmidt B, Roberts RS, Davis PG, et al. Prediction of Late Death or Disability at Age 5 Years Using a Count of 3 Neonatal Morbidities in Very Low Birth Weight Infants. J Pediatr. Nov 2015;167(5):982–6.e2. doi: 10.1016/j.jpeds.2015.07.067 [DOI] [PubMed] [Google Scholar]
- 11.Clyman RI, Saha S, Jobe A, Oh W. Indomethacin prophylaxis for preterm infants: the impact of 2 multicentered randomized controlled trials on clinical practice. J Pediatr. Jan 2007;150(1):46–50.e2. doi: 10.1016/j.jpeds.2006.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bassler D, Stoll BJ, Schmidt B, et al. Using a count of neonatal morbidities to predict poor outcome in extremely low birth weight infants: added role of neonatal infection. Pediatrics. Jan 2009;123(1):313–8. doi: 10.1542/peds.2008-0377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stoll BJ, Hansen NI, Bell EF, et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993-2012. JAMA. Sep 08 2015;314(10):1039–51. doi: 10.1001/jama.2015.10244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bell EF, Hintz SR, Hansen NI, et al. Mortality, In-Hospital Morbidity, Care Practices, and 2-Year Outcomes for Extremely Preterm Infants in the US, 2013-2018. JAMA. Jan 18 2022;327(3):248–263. doi: 10.1001/jama.2021.23580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmidt B, Anderson PJ, Doyle LW, et al. Survival without disability to age 5 years after neonatal caffeine therapy for apnea of prematurity. JAMA. Jan 18 2012;307(3):275–82. doi: 10.1001/jama.2011.2024 [DOI] [PubMed] [Google Scholar]
- 16.Duncan AF, Matthews MA. Neurodevelopmental Outcomes in Early Childhood. Clin Perinatol. Sep 2018;45(3):377–392. doi: 10.1016/j.clp.2018.05.001 [DOI] [PubMed] [Google Scholar]
- 17.Synnes A, Hicks M. Neurodevelopmental Outcomes of Preterm Children at School Age and Beyond. Clin Perinatol. Sep 2018;45(3):393–408. doi: 10.1016/j.clp.2018.05.002 [DOI] [PubMed] [Google Scholar]
- 18.O'Shea TM, Joseph RM, Allred EN, et al. Accuracy of the Bayley-II mental development index at 2 years as a predictor of cognitive impairment at school age among children born extremely preterm. J Perinatol. Jul 2018;38(7):908–916. doi: 10.1038/s41372-017-0020-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taylor GL, Joseph RM, Kuban KCK, et al. Changes in Neurodevelopmental Outcomes From Age 2 to 10 Years for Children Born Extremely Preterm. Pediatrics. May 2021;147(5)doi: 10.1542/peds.2020-001040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boland RA, Cheong JLY, Doyle LW. Changes in long-term survival and neurodevelopmental disability in infants born extremely preterm in the post-surfactant era. Semin Perinatol. Dec 2021;45(8):151479. doi: 10.1016/j.semperi.2021.151479 [DOI] [PubMed] [Google Scholar]
- 21.Johnson S, Marlow N. Preterm birth and childhood psychiatric disorders. Pediatr Res. May 2011;69(5 Pt 2):11R–8R. doi: 10.1203/PDR.0b013e318212faa0 [DOI] [PubMed] [Google Scholar]
- 22.Frazier JA, Cochran D, Kim S, et al. Psychiatric Outcomes, Functioning, and Participation in Extremely Low Gestational Age Newborns at Age 15 Years. J Am Acad Child Adolesc Psychiatry. Jul 2022;61(7):892–904.e2. doi: 10.1016/j.jaac.2021.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cochran DM, Jensen ET, Frazier JA, et al. Association of prenatal modifiable risk factors with attention-deficit hyperactivity disorder outcomes at age 10 and 15 in an extremely low gestational age cohort. Front Hum Neurosci. 2022;16:911098. doi: 10.3389/fnhum.2022.911098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Joseph RM, Hooper SR, Heeren T, et al. Maternal Social Risk, Gestational Age at Delivery, and Cognitive Outcomes among Adolescents Born Extremely Preterm. Paediatr Perinat Epidemiol. Sep 2022;36(5):654–664. doi: 10.1111/ppe.12893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. Apr 1978;92(4):529–34. doi: 10.1016/s0022-3476(78)80282-0 [DOI] [PubMed] [Google Scholar]
- 26.Guzzetta F, Shackelford GD, Volpe S, Perlman JM, Volpe JJ. Periventricular intraparenchymal echodensities in the premature newborn: critical determinant of neurologic outcome. Pediatrics. Dec 1986;78(6):995–1006. [PubMed] [Google Scholar]
- 27.Bassan H, Benson CB, Limperopoulos C, et al. Ultrasonographic features and severity scoring of periventricular hemorrhagic infarction in relation to risk factors and outcome. Pediatrics. Jun 2006;117(6):2111–8. doi: 10.1542/peds.2005-1570 [DOI] [PubMed] [Google Scholar]
- 28.Al-Abdi SY. A severity score for intraventricular hemorrhage in preterm neonates. Saudi Med J. Dec 2011;32(12):1313–4. [PubMed] [Google Scholar]
- 29.Rees P, Callan C, Chadda KR, et al. Preterm Brain Injury and Neurodevelopmental Outcomes: A Meta-analysis. Pediatrics. Dec 01 2022;150(6)doi: 10.1542/peds.2022-057442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Campbell H, Check J, Kuban KCK, et al. Neonatal Cranial Ultrasound Findings among Infants Born Extremely Preterm: Associations with Neurodevelopmental Outcomes at 10 Years of Age. J Pediatr. Oct 2021;237:197–205.e4. doi: 10.1016/j.jpeds.2021.05.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mukerji A, Shah V, Shah PS. Periventricular/Intraventricular Hemorrhage and Neurodevelopmental Outcomes: A Meta-analysis. Pediatrics. Dec 2015;136(6):1132–43. doi: 10.1542/peds.2015-0944 [DOI] [PubMed] [Google Scholar]
- 32.Kuban KC, O'Shea TM, Allred EN, Tager-Flusberg H, Goldstein DJ, Leviton A. Positive screening on the Modified Checklist for Autism in Toddlers (M-CHAT) in extremely low gestational age newborns. J Pediatr. Apr 2009;154(4):535–540.e1. doi: 10.1016/j.jpeds.2008.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Movsas TZ, Pinto-Martin JA, Whitaker AH, et al. Autism spectrum disorder is associated with ventricular enlargement in a low birth weight population. J Pediatr. Jul 2013;163(1):73–8. doi: 10.1016/j.jpeds.2012.12.084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Limperopoulos C, Bassan H, Gauvreau K, et al. Does cerebellar injury in premature infants contribute to the high prevalence of long-term cognitive, learning, and behavioral disability in survivors? Pediatrics. Sep 2007;120(3):584–93. doi: 10.1542/peds.2007-1041 [DOI] [PubMed] [Google Scholar]
- 35.Limperopoulos C, Chilingaryan G, Sullivan N, Guizard N, Robertson RL, du Plessis AJ. Injury to the premature cerebellum: outcome is related to remote cortical development. Cereb Cortex. Mar 2014;24(3):728–36. doi: 10.1093/cercor/bhs354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Johnson S, Hollis C, Kochhar P, Hennessy E, Wolke D, Marlow N. Autism spectrum disorders in extremely preterm children. J Pediatr. Apr 2010;156(4):525–31.e2. doi: 10.1016/j.jpeds.2009.10.041 [DOI] [PubMed] [Google Scholar]
- 37.Hofheimer JA, Sheinkopf SJ, Eyler LT. Autism risk in very preterm infants--new answers, more questions. J Pediatr. Jan 2014;164(1):6–8. doi: 10.1016/j.jpeds.2013.09.054 [DOI] [PubMed] [Google Scholar]
- 38.Msall ME. Central nervous system connectivity after extreme prematurity: understanding autistic spectrum disorder. J Pediatr. Apr 2010;156(4):519–21. doi: 10.1016/j.jpeds.2009.12.035 [DOI] [PubMed] [Google Scholar]
- 39.Ehrenkranz RA, Walsh MC, Vohr BR, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. Dec 2005;116(6):1353–60. doi: 10.1542/peds.2005-0249 [DOI] [PubMed] [Google Scholar]
- 40.Jensen EA, Dysart K, Gantz MG, et al. The Diagnosis of Bronchopulmonary Dysplasia in Very Preterm Infants. An Evidence-based Approach. Am J Respir Crit Care Med. Sep 15 2019;200(6):751–759. doi: 10.1164/rccm.201812-2348OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brumbaugh JE, Bell EF, Grey SF, et al. Behavior Profiles at 2 Years for Children Born Extremely Preterm with Bronchopulmonary Dysplasia. J Pediatr. Apr 2020;219:152–159.e5. doi: 10.1016/j.jpeds.2019.12.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.DeMauro SB. Neurodevelopmental outcomes of infants with bronchopulmonary dysplasia. Pediatr Pulmonol. Nov 2021;56(11):3509–3517. doi: 10.1002/ppul.25381 [DOI] [PubMed] [Google Scholar]
- 43.Sobotka SA, Lynch E, Msall ME, Graham RJ. Early childhood developmental skills of children with tracheostomies and ventilators recently discharged home. Pediatr Pulmonol. Mar 2023;58(3):853–865. doi: 10.1002/ppul.26265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Annesi CA, Levin JC, Litt JS, Sheils CA, Hayden LP. Long-term respiratory and developmental outcomes in children with bronchopulmonary dysplasia and history of tracheostomy. J Perinatol. Nov 2021;41(11):2645–2650. doi: 10.1038/s41372-021-01144-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cammack B, Noel-MacDonnell J, Cuna A, Manimtim W. Impact of tracheostomy on language and cognitive development in infants with severe bronchopulmonary dysplasia. J Perinatol. Feb 2020;40(2):299–305. doi: 10.1038/s41372-019-0540-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.DeMauro SB, D'Agostino JA, Bann C, et al. Developmental outcomes of very preterm infants with tracheostomies. J Pediatr. Jun 2014;164(6):1303–10.e2. doi: 10.1016/j.jpeds.2013.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Spittle AJ, Anderson PJ, Tapawan SJ, Doyle LW, Cheong JLY. Early developmental screening and intervention for high-risk neonates - From research to clinical benefits. Semin Fetal Neonatal Med. Jun 2021;26(3):101203. doi: 10.1016/j.siny.2021.101203 [DOI] [PubMed] [Google Scholar]
- 48.Msall ME. Physiological stress and brain vulnerability: understanding the neurobiology of connectivity in preterm infants. Ann Neurol. Oct 2011;70(4):523–4. doi: 10.1002/ana.22614 [DOI] [PubMed] [Google Scholar]
- 49.Bayley N. Bayley Scales of Infant Development. San Antonio, TX: The Psychological Corporation; 1969. [Google Scholar]
- 50.Bayley N. Bayley Scales of Infant Development. 2nd ed. San Antonio, TX: The Psychological Corporation; 1993. [Google Scholar]
- 51.Bayley N. Bayley Scales of Infant and Toddler Development. 3rd ed. San Antonio, TX: Pearson; 2006. [Google Scholar]
- 52.Harrison PL, Oakland T. Adaptive behavior assessment system - Third edition (ABAS-3): Manual. Western Psychological Services. [Google Scholar]
- 53.Greenspan SI. Greenspan social-emotional growth chart: A screening questionnaire for infants and young children. San Antonio, TX: Harcourt Assessment; 2004. [Google Scholar]
- 54.Bayley N, Aylward GP. Bayley Scales of Infant and Toddler Development. Bloomington, MN: NCS Pearson; 2019. [Google Scholar]
- 55.Sparrow S, Cicchetti D, Saulnier C. Vineland adaptive Behavior Scales. 3rd ed: Pearson; 2016. [Google Scholar]
- 56.Wechsler D. Wechsler Preschool and Primary Scale of Intelligence. 4th ed: NCS Pearson, Incorporated; 2014. [Google Scholar]
- 57.Zimmerman I, Steiner V, Pond R. The Preschool Language Scale-5. Pearson; 2011. [Google Scholar]
- 58.Squires J, Bricker D. Ages & Stages Questionnaires, Third Edition (ASQ-3). Baltimore, MD: Paul H. Brookes Publishing; 2009. [Google Scholar]
- 59.Folio M, Fewell R. Peabody Developmental Motor Scales. Examiner's Manual. 2nd Edn. Austin, Texas: Pro-Ed, 2000. [Google Scholar]
- 60.Knobloch H, Stevens FM, Malone AF. Manual of developmental diagnosis : the administration and interpretation of the revised Gesell and Amatruda developmental and neurologic examination. Hagerstown, Md: Harper & Row; 1980. [Google Scholar]
- 61.Newborg J. Battelle Developmental Inventory: Second Edition. Riverside; 2005. [Google Scholar]
- 62.Cohen MA, Gross PJ. The developmental resource : behavioral sequences for assessment and program planning. New York, NY: Grune & Stratton; 1979. [Google Scholar]
- 63.Mullen EM. Mullen Scales of Early Learning: AGS Edition. American Guidance Services, Minneapolis, MN, 1995. [Google Scholar]
- 64.Davis BE, Leppert MO, German K, et al. Primary Care Framework to Monitor Preterm Infants for Neurodevelopmental Outcomes in Early Childhood. Pediatrics. Jul 01 2023;152(1)doi: 10.1542/peds.2023-062511 [DOI] [PubMed] [Google Scholar]
- 65.Mulkey SB, Arroyave-Wessel M, Peyton C, et al. Neurodevelopmental Abnormalities in Children With In Utero Zika Virus Exposure Without Congenital Zika Syndrome. JAMA Pediatr. Mar 01 2020;174(3):269–276. doi: 10.1001/jamapediatrics.2019.5204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wu YW, Mathur AM, Chang T, et al. High-Dose Erythropoietin and Hypothermia for Hypoxic-Ischemic Encephalopathy: A Phase II Trial. Pediatrics. Jun 2016;137(6)doi: 10.1542/peds.2016-0191 [DOI] [PubMed] [Google Scholar]
- 67.Duffner PK, Granger C, Lyon N, et al. Developmental and functional outcomes in children with a positive newborn screen for Krabbe disease: a pilot study of a phone-based interview surveillance technique. J Pediatr. Aug 2012;161(2):258–63.e1. doi: 10.1016/j.jpeds.2012.01.044 [DOI] [PubMed] [Google Scholar]
- 68.Peyton C, Wroblewski K, Park J, et al. Validity of The Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA-FS): a daily activity criterion checklist for infants and toddlers. Pediatr Res. Nov 2021;90(5):1052–1057. doi: 10.1038/s41390-020-01342-0 [DOI] [PubMed] [Google Scholar]
- 69.Peyton C, Msall ME, Wroblewski K, Rogers EE, Kohn M, Glass HC. Concurrent validity of the Warner Initial Developmental Evaluation of Adaptive and Functional Skills and the Bayley Scales of Infant and Toddler Development, Third Edition. Dev Med Child Neurol. Mar 2021;63(3):349–354. doi: 10.1111/dmcn.14737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lagatta JM, Zhang L, Yan K, et al. Prospective Risk Stratification Identifies Healthcare Utilization Associated with Home Oxygen Therapy for Infants with Bronchopulmonary Dysplasia. J Pediatr. Dec 2022;251:105–112.e1. doi: 10.1016/j.jpeds.2022.07.040 [DOI] [PubMed] [Google Scholar]
- 71.Carter AS, Briggs-Gowan MJ, Jones SM, Little TD. The Infant-Toddler Social and Emotional Assessment (ITSEA): factor structure, reliability, and validity. J Abnorm Child Psychol. Oct 2003;31(5):495–514. doi: 10.1023/a:1025449031360 [DOI] [PubMed] [Google Scholar]
- 72.Briggs-Gowan MJ, Carter AS, Irwin JR, Wachtel K, Cicchetti DV. The Brief Infant-Toddler Social and Emotional Assessment: screening for social-emotional problems and delays in competence. J Pediatr Psychol. Mar 2004;29(2):143–55. doi: 10.1093/jpepsy/jsh017 [DOI] [PubMed] [Google Scholar]
- 73.Squires J, Bricker D, Twombly E. Ages and stages questionnaires: Social emotional. 2nd ed. Baltimore, MD: Brookes Publishing; 2015. [Google Scholar]
- 74.Achenbach TA, Rescorla LA. Child behavior checklist 1.5-5. Lutz, FL: PAR, Inc; 2000. [Google Scholar]
- 75.Kim JY, Ha EH. Cluster Analysis of the Child Behavior Checklist 1.5-5 for Preschool Children Diagnosed With a Mental Disorder. Psychol Rep. Aug 2020;123(4):1403–1424. doi: 10.1177/0033294119844980 [DOI] [PubMed] [Google Scholar]
- 76.Schmid G, Schreier A, Meyer R, Wolke D. Predictors of crying, feeding and sleeping problems: a prospective study. Child Care Health Dev. Jul 2011;37(4):493–502. doi: 10.1111/j.1365-2214.2010.01201.x [DOI] [PubMed] [Google Scholar]
- 77.Bilgin A, Wolke D. Regulatory Problems in Very Preterm and Full-Term Infants Over the First 18 Months. J Dev Behav Pediatr. May 2016;37(4):298–305. doi: 10.1097/DBP.0000000000000297 [DOI] [PubMed] [Google Scholar]
- 78.Spittle A, Orton J, Anderson PJ, Boyd R, Doyle LW. Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database Syst Rev. Nov 24 2015;2015(11):CD005495. doi: 10.1002/14651858.CD005495.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Spittle A, Treyvaud K. The role of early developmental intervention to influence neurobehavioral outcomes of children born preterm. Semin Perinatol. Dec 2016;40(8):542–548. doi: 10.1053/j.semperi.2016.09.006 [DOI] [PubMed] [Google Scholar]
- 80.Msall ME. Neurodevelopmental surveillance in the first 2 years after extremely preterm birth: evidence, challenges, and guidelines. Early Hum Dev. 2006. Mar;82(3):157–66. doi: 10.1016/j.earlhumdev.2005.12.016. Epub 2006 Mar 10. [DOI] [PubMed] [Google Scholar]
- 81.Clark R, Tluczek A, Moore EC, Evenson AL. Assessment of Early Parent–Child Relationships. 2nd ed: Oxford Academic; 2020. [Google Scholar]
- 82.Nascimento TF, Bocchi SCM, Trenado RM, Cerezo MA, Jensen R. Instruments to measure interaction of mothers and newborns: A systematic review. Infant Behav Dev. May 2023;71:101825. doi: 10.1016/j.infbeh.2023.101825 [DOI] [PubMed] [Google Scholar]
- 83.Gridley N, Blower S, Dunn A, Bywater T, Whittaker K, Bryant M. Psychometric Properties of Parent-Child (0-5 years) Interaction Outcome Measures as Used in Randomized Controlled Trials of Parent Programs: A Systematic Review. Clin Child Fam Psychol Rev. Jun 2019;22(2):253–271. doi: 10.1007/s10567-019-00275-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Leclère C, Viaux S, Avril M, et al. Why synchrony matters during mother-child interactions: a systematic review. PLoS One. 2014;9(12):e113571. doi: 10.1371/journal.pone.0113571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mahoney G, Spiker D, Boyce G. Topics in Early Childhood Special Education. Clinical Assessments of Parent-Child Interaction: Are Professionals Ready To Implement This Practice? 1996. p. 26–50. [Google Scholar]
- 86.Mahoney G, Spiker D, Boyce G. Clinical Assessments of Parent-Child Interaction: Are Professionals Ready To Implement This Practice? Topics In Early Childhood Special Educatlon 1996. p. 26–50. [Google Scholar]
- 87.Grunberg VA, Geller PA, Hoffman C, Patterson CA. A biopsychosocial model of NICU family adjustment and child development. J Perinatol. Apr 2023;43(4):510–517. doi: 10.1038/s41372-022-01585-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cong S, Wang R, Fan X, et al. Skin-to-skin contact to improve premature mothers' anxiety and stress state: A meta-analysis. Matern Child Nutr. Oct 2021;17(4):el3245. doi: 10.1111/mcn.13245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Franck LS, Waddington C, O'Brien K. Family Integrated Care for Preterm Infants. Crit Care Nurs Clin North Am. Jun 2020;32(2):149–165. doi: 10.1016/j.cnc.2020.01.001 [DOI] [PubMed] [Google Scholar]
- 90.Ohlsson A, Jacobs SE. NIDCAP: a systematic review and meta-analyses of randomized controlled trials. Pediatrics. Mar 2013;131(3):e881–93. doi: 10.1542/peds.2012-2121 [DOI] [PubMed] [Google Scholar]
- 91.Neel ML. Parenting Style Interventions in Parents of Preterm and High-Risk Infants: Controversies, Cost, and Future Directions. Clin Perinatol. Mar 2023;50(1):179–213. doi: 10.1016/j.clp.2022.10.008 [DOI] [PubMed] [Google Scholar]
- 92.Mclean MA, Scoten OC, Yu W, et al. Lower Maternal Chronic Physiological Stress and Better Child Behavior at 18 Months: Follow-Up of a Cluster Randomized Trial of Neonatal Intensive Care Unit Family Integrated Care. J Pediatr. Apr 2022;243:107–115.e4. doi: 10.1016/j.jpeds.2021.12.055 [DOI] [PubMed] [Google Scholar]
- 93.Church PT, Grunau RE, Mirea L, et al. Family Integrated Care (FICare): Positive impact on behavioural outcomes at 18 months. Early Hum Dev. Dec 2020; 151:105196. doi: 10.1016/j.earlhumdev.2020.105196 [DOI] [PubMed] [Google Scholar]
- 94.Jeukens-Visser M, Koldewijn K, van Wassenaer-Leemhuis AG, Flierman M, Nollet F, Wolf MJ. Development and nationwide implementation of a postdischarge responsive parenting intervention program for very preterm born children: The TOP program. Infant Ment Health J. May 2021;42(3):423–437. doi: 10.1002/imhj.21902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Griffith T, Singh A, Naber M, et al. Scoping review of interventions to support families with preterm infants post-NICU discharge. J Pediatr Nurs. 2022;67:e135–e149. doi: 10.1016/j.pedn.2022.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Baraldi E, Allodi MW, Löwing K, Smedler AC, Westrup B, Ådén U. Stockholm preterm interaction-based intervention (SPIBI) - study protocol for an RCT of a 12-month parallel-group post-discharge program for extremely preterm infants and their parents. BMC Pediatr. Feb 01 2020;20(1):49. doi: 10.1186/s12887-020-1934-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dell'Aversana V, Tofani M, Valente D. Emotional Regulation Interventions on Developmental Course for Preterm Children: A Systematic Review of Randomized Control Trials. Children (Basel). Mar 22 2023;10(3)doi: 10.3390/children10030603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Franck LS, Shellhaas RA, Lemmon ME, et al. Parent Mental Health and Family Coping over Two Years after the Birth of a Child with Acute Neonatal Seizures. Children (Basel). Dec 22 2021;9(1)doi: 10.3390/children9010002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Spittle AJ, Thompson DK, Olsen JE, Kwong A, Treyvaud K. Predictors of long-term neurodevelopmental outcomes of children born extremely preterm. Semin Perinatol. Dec 2021;45(8):151482. doi: 10.1016/j.semperi.2021.151482 [DOI] [PubMed] [Google Scholar]
- 100.Olsen JE, Lee KJ, Spittle AJ, et al. The causal effect of being born extremely preterm or extremely low birthweight on neurodevelopment and social-emotional development at 2 years. Acta Paediatr. Jan 2022;111(1):107–114. doi: 10.1111/apa.16098 [DOI] [PubMed] [Google Scholar]
- 101.McCarty DB, Letzkus L, Attridge E, Dusing SC. Efficacy of Therapist Supported Interventions from the Neonatal Intensive Care Unit to Home: A Meta-Review of Systematic Reviews. Clin Perinatol. Mar 2023;50(1):157–178. doi: 10.1016/j.clp.2022.10.004 [DOI] [PubMed] [Google Scholar]
- 102.Finlayson F, Olsen J, Dusing SC, Guzzetta A, Eeles A, Spittle A. Supporting Play, Exploration, and Early Development Intervention (SPEEDI) for preterm infants: A feasibility randomised controlled trial in an Australian context. Early Hum Dev. Dec 2020; 151:105172. doi: 10.1016/j.earlhumdev.2020.105172 [DOI] [PubMed] [Google Scholar]
- 103.Nina Banerjee P, McFadden K, Shannon JD, Davidson LL. Preterm Birth and Other Measures of Infant Biological Vulnerability: Associations with Maternal Sensitivity and Infant Cognitive Development. Matern Child Health J. Apr 2023;27(4):698–710. doi: 10.1007/s10995-023-03590-y [DOI] [PubMed] [Google Scholar]
- 104.Anderson PJ, Treyvaud K, Spittle AJ. Early developmental interventions for infants born very preterm - what works? Semin Fetal Neonatal Med. Jun 2020;25(3):101119. doi: 10.1016/j.siny.2020.101119 [DOI] [PubMed] [Google Scholar]
- 105.Hintz SR, deRegnier RA, Vohr BR. Outcomes of Preterm Infants: Shifting Focus, Extending the View. Clin Perinatol. Mar 2023;50(1):1–16. doi: 10.1016/j.clp.2022.10.001 [DOI] [PubMed] [Google Scholar]
- 106.Orkin J, Major N, Esser K, et al. Coached, Coordinated, Enhanced Neonatal Transition (CCENT): protocol for a multicentre pragmatic randomised controlled trial of transition-to-home support for parents of high-risk infants. BMJ Open. Jul 07 2021;11(7):e046706. doi: 10.1136/bmjopen-2020-046706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sanders MR, Kirby JN, Tellegen CL, Day JJ. The Triple P-Positive Parenting Program: a systematic review and meta-analysis of a multi-level system of parenting support. Clin Psychol Rev. Jun 2014;34(4):337–57. doi: 10.1016/j.cpr.2014.04.003 [DOI] [PubMed] [Google Scholar]
- 108.Sanders MR, Divan G, Singhal M, et al. Scaling Up Parenting Interventions is Critical for Attaining the Sustainable Development Goals. Child Psychiatry Hum Dev. Oct 2022;53(5):941–952. doi: 10.1007/s10578-021-01171-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Blair C, Ramey CT, Hardin JM. Early intervention for low birthweight, premature infants: participation and intellectual development. Am J Ment Retard. Mar 1995;99(5):542–54. [PubMed] [Google Scholar]
- 110.Colditz PB, Boyd RN, Winter L, et al. A Randomized Trial of Baby Triple P for Preterm Infants: Child Outcomes at 2 Years of Corrected Age. J Pediatr. Jul 2019;210:48–54.e2. doi: 10.1016/j.jpeds.2019.01.024 [DOI] [PubMed] [Google Scholar]
- 111.White-Traut R, Brandon D, Kavanaugh K, et al. Protocol for implementation of an evidence based parentally administered intervention for preterm infants. BMC Pediatr. Mar 24 2021;21(1):142. doi: 10.1186/s12887-021-02596-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.White-Traut R, Rankin KM, Pham T, Li Z, Liu L. Preterm infants' orally directed behaviors and behavioral state responses to the integrated H-HOPE intervention. Infant Behav Dev. Nov 2014;37(4):583–96. doi: 10.1016/j.infbeh.2014.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Treyvaud K, Doyle LW, Lee KJ, et al. Family functioning, burden and parenting stress 2 years after very preterm birth. Early Hum Dev. Jun 2011;87(6):427–31. doi: 10.1016/j.earlhumdev.2011.03.008 [DOI] [PubMed] [Google Scholar]
- 114.Ramey CT, Bryant DM, Wasik BH, Sparling JJ, Fendt KH, LaVange LM. Infant Health and Development Program for low birth weight, premature infants: program elements, family participation, and child intelligence. Pediatrics. Mar 1992;89(3):454–65. [PubMed] [Google Scholar]
- 115.DA Fonseca Filho GG, Lopes AC, Bezerra RB, et al. Assessment of child development in premature babies based on the ICF biopsychosocial model. Eur J Phys Rehabil Med. Aug 2021;57(4):585–592. doi: 10.23736/S1973-9087.20.06543-0 [DOI] [PubMed] [Google Scholar]
- 116.Hendson L, Church PT, Banihani R. Follow-up care of the extremely preterm infant after discharge from the neonatal intensive care unit. Paediatr Child Health. Oct 2022;27(6):359–371. doi: 10.1093/pch/pxac058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cheong JLY, Burnett AC, Treyvaud K, Spittle AJ. Early environment and long-term outcomes of preterm infants. J Neural Transm (Vienna). Jan 2020;127(1):1–8. doi: 10.1007/s00702-019-02121-w [DOI] [PubMed] [Google Scholar]
- 118.Church PT, Banihani R, Watson J, Chen WTN, Ballantyne M, Asztalos E. The E-Nurture Project: A Hybrid Virtual Neonatal Follow Up Model for 2021. Children (Basel). Feb 12 2021;8(2)doi: 10.3390/children8020139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Piper M, Darrah J. Motor assessment of the developing infant. 2nd ed. St. Louis, MO: Elsevier Health Sciences; 2021. p. 1–7. [Google Scholar]
- 120.Piper MC, Pinnell LE, Darrah J, Maguire T, Byrne PJ. Construction and validation of the Alberta Infant Motor Scale (AIMS). Can J Public Health. 1992;83 Suppl 2:S46–50. [PubMed] [Google Scholar]
- 121.Capute AJ, Accardo PJ. The infant neurodevelopmental assessment: a clinical interpretive manual for CAT-CLAMS in the first two years of life, part 1. Curr Probl Pediatr. Aug 1996;26(7):238–57. doi: 10.1016/s0045-9380(06)80061-7 [DOI] [PubMed] [Google Scholar]
- 122.Capute AJ, Accardo PJ. The infant neurodevelopmental assessment: a clinical interpretive manual for CAT-CLAMS in the first two years of life, Part 2. Curr Probl Pediatr. Sep 1996;26(8):279–306. doi: 10.1016/s0045-9380(96)80008-9 [DOI] [PubMed] [Google Scholar]
- 123.Romeo DM, Cioni M, Scoto M, Mazzone L, Palermo F, Romeo MG. Neuromotor development in infants with cerebral palsy investigated by the Hammersmith Infant Neurological Examination during the first year of age. Eur J Paediatr Neurol. Jan 2008;12(1):24–31. doi: 10.1016/j.ejpn.2007.05.006 [DOI] [PubMed] [Google Scholar]