Abstract
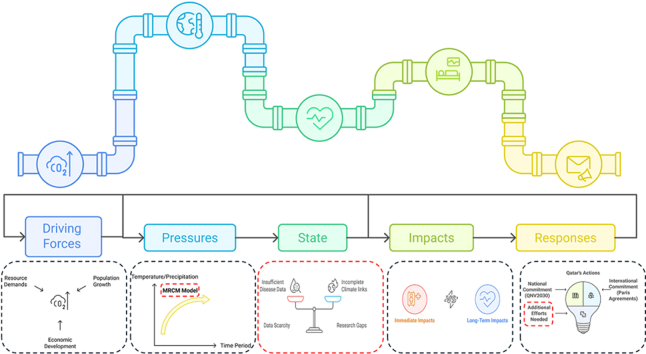
This study investigates the interactions between climate change and human health with a particular focus on Qatar, using the DPSIR (Driving Forces, Pressures, States, Impacts, Responses) framework. Key drivers, including economic development and population growth, contribute to increased greenhouse gas (GHG) emissions, exerting pressure on Qatar's climate through rising temperatures and altered precipitation patterns, as modeled by the MIT Regional Climate Model (MRCM). The findings reveal critical gaps in understanding the state of climate-health interactions, including insufficient disease data, incomplete climate-health linkages, and significant research gaps. These limitations hinder targeted responses to climate-sensitive diseases, which have shown an increase over the years. The study identifies the pathways through which climatic shifts contribute to immediate health risks, such as heat-related illnesses and respiratory conditions, as well as long-term impacts, including chronic diseases and mental health challenges. Despite Qatar's efforts through national and international strategies, the DPSIR analysis highlights the urgent need for enhanced research, improved data collection, and tailored actions to address these challenges. Strengthened adaptation, resilience-building, and emission reduction strategies remain essential for safeguarding public health in the face of accelerating climate change.
Keywords: Climate change impacts, Human health, Heat-related illness, Qatar, Vector-borne diseases
Graphical abstract
1. Introduction
Climate change refers to the long-term alteration in weather conditions within a specific region, characterized by shifts in temperature, precipitation patterns, and other climatic variables driven by both natural events and anthropogenic activities [1,2]. Human activities, particularly fossil fuel combustion, deforestation, and certain agricultural practices, are the primary drivers of GHG emissions, which trap heat in the Earth's atmosphere, resulting in global warming and climate change. Consequently, increasing global average temperatures, rising sea levels and declining air quality are the major outcomes of increased GHG emissions [3]. According to projections by the Intergovernmental Panel on Climate Change (IPCC), Earth's temperature is expected to rise by 1.4–5.8 °C by 2100, posing significant threats to the environment, human health, infrastructure, and overall productivity [4]. Studies conducted by Andric & Al-Ghamdi [5], and Vinodhkumar et al. [6] suggest a significant increase in temperature extremes, as well as in the intensity, frequency, and duration of heatwaves in the future. According to the projections, temperatures exceeding 45 °C are expected to occur for approximately 21 % of the year, exacerbating risks of heat-related illnesses and other health challenges. In response to these threats, international agreements such as the 2015 Paris Agreement aim to limit global warming to below 2 °C, with ambitious goals of achieving net-zero emissions by 2050 [7]. The importance of addressing the health impacts of climate change, particularly in vulnerable regions like Qatar, cannot be overstated. Climate change poses a variety of health risks through increased temperatures, air pollution, and water scarcity [8]. These impacts disproportionately affect vulnerable populations, including the elderly, children, and those with pre-existing health conditions [9]. The DPSIR framework provides a structured approach and is used in environmental management to analyze the cause-effect relationships between environmental and human systems [10]. This framework was initially proposed in a report by Smeets and Weterings (1999) to assist policymakers in comprehending information in indicator reports [11]. It serves as a tool for understanding the complex interactions between altered environmental conditions, particularly climate change, and human health and for identifying effective and sustainable management practices [12,13].
This study aims to map the health impacts of climate change globally, with a particular focus on Qatar. Utilizing the DPSIR framework, we identified the pathways through which climate change impacts human health [[14], [15], [16], [17], [18], [19]]. In addition, this paper identifies several key aspects.
-
•
A significant research gap and lack of health data in the region, which hinder efforts to address climate-related health challenges.
-
•
Projections from the MIT Regional Climate Model (MRCM), indicating rising temperatures and shifting precipitation patterns.
-
•
The need for additional initiatives to address the driving forces and pressures outlined in the DPSIR framework.
The novelty of this paper lies in its use of the DPSIR framework to explore the impact of climate change on human health in Qatar, a region where this type of analysis has been limited, offering fresh insights into how environmental changes are directly linked to health outcomes, providing a foundation for future research and policy interventions in the region.
2. Driving forces for climate change
The primary drivers of climate change are closely linked to the significant increase in GHG emissions influenced by economic growth, industrial activities, rapid population growth, and other contributing factors [7]. GHGs, including CO2, N2O, CH4, and water vapor, form a thermal barrier in the atmosphere that helps regulate Earth's temperature balance [20]. The natural process of GHG effect begins with solar radiation penetrating Earth's atmosphere and reaches the surface. When solar radiation reaches the atmosphere, GHGs absorb some of it and also absorb and re-emit radiation emitted by the Earth's surface. This absorption of heat warms the surface, which then emits infrared radiation back into space [21]. However, some of this emitted heat is absorbed by GHGs in the atmosphere and re-emitted in all directions, including back towards the Earth's surface. This process effectively traps heat in the lower atmosphere, contributing to the warming of the Earth's surface and lower atmosphere [22]. The greenhouse effect allows the Earth to maintain a temperature range suitable for supporting life. Without it, the Earth's average temperature would be much colder, making it difficult to support life on the planet. Anthropogenic activities disrupt natural balance, significantly increasing the GHG emissions contributing to the greenhouse effect [21,22].
Following the industrial revolution and the growth of human population, various human activities escalated to accommodate this increase. These activities include fossil fuel combustion, land use change and forestry, industrial processes, agriculture activities, and waste management [23]. Energy production and land use change and forestry practices contribute 89 % and 7 % of the total global CO2 gas, respectively.
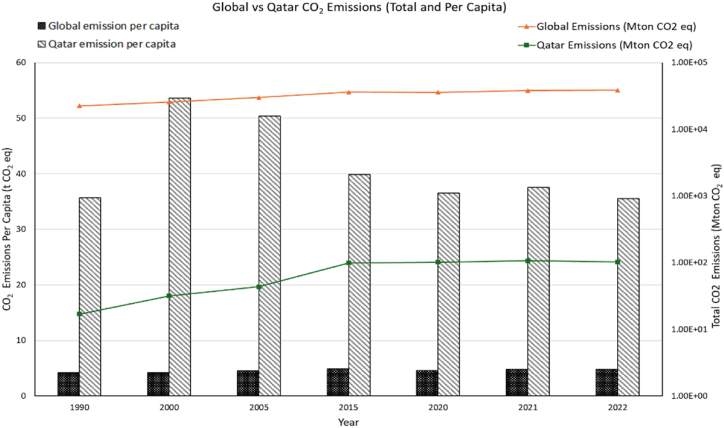
Fig. 1 presents CO2 emissions for Qatar compared to global emissions, both in total (Mton CO2 eq.) and per capita, from 1990 to 2022, based on the JRC/IEA (Joint Research Center/International Energy Agency) report published in 2023 [24]. The line graph represents total CO2 emissions while the bar graph represents CO2 emissions per capita. Global total emissions have substantially increased, rising by 71 % from 1990 to 2022, primarily due to industrialization and economic growth. In contrast, global CO2 emissions per capita have fluctuated: increasing by 16 % from 1990 to 2015, followed by a 6 % decrease until 2020, and a subsequent 5 % rise from 2020 to 2022. Qatar, known for its high per capita carbon footprint due to its heavy reliance on the oil and gas sector, ranks among the top CO2 emitters despite its small population [25]. As shown in Fig. 1, Qatar's total CO₂ emissions have increased since 1990, with per capita emissions remaining very high compared to global averages reflecting its high reliance on energy industry and relatively small population. Although Qatar's per capita CO2 emissions increased by 11 % from 1990 to 2015, they showed a slight decrease of 0.42 % from 1990 to 2022, reflecting global and local efforts to reduce emissions and adherence to reduction agreements. The energy sector is a major contributor to Qatar's GHG emissions, constituting nearly 50 % of total country emissions (Table 1) [[26], [27], [28], [29]]. Reducing emissions from this sector is critical for addressing climate change. Managing these emissions among population growth poses significant challenges and requires innovative strategies to balance economic development with environmental protection [30]. The significant increase in global CO2 emissions over the years has intensified climate change, leading to more frequent and severe climate events, which exert "pressure" on human health through rising temperatures, altered precipitation patterns and other environmental impacts.
Fig. 1.
CO2 emissions for Qatar compared to global emissions, both in total (Mton CO2 eq.) and per capita, from 1990 to 2022.
Table 1.
The percentage of GHG emissions from energy sector compared to the emission across all sectors in Qatar (2019–2022).
| Year | Total GHG emission (Mt CO2 eq.) | GHG emissions from the energy sector (Mt CO2 eq.) | GHG emissions from the energy sector (%) |
|---|---|---|---|
| 2019 | 192 | 95.1 | 49 % |
| 2020 | 191 | 97.4 | 51 % |
| 2021 | 198 | 97.6 | 49 % |
| 2022 | 195 | 101.5 | 52 % |
3. Climate as “Pressures” on human health
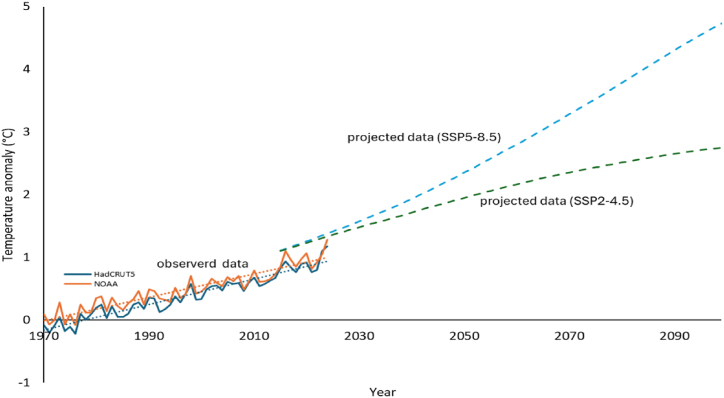
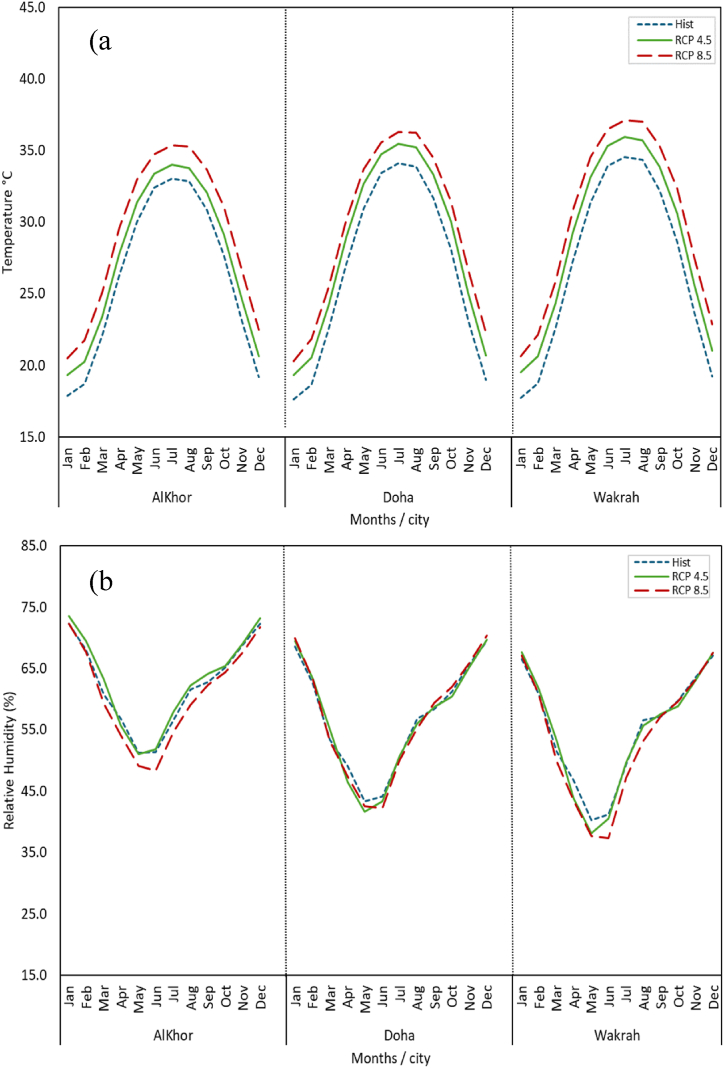
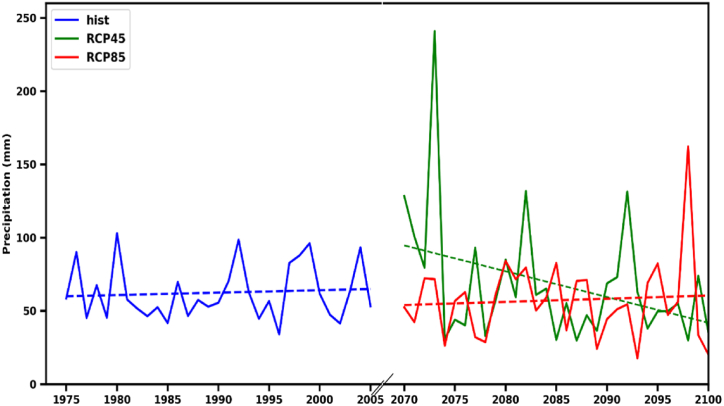
In this context, 'Pressure' refers to the direct environmental changes resulting from the driving forces of climate change. These environmental alterations have immediate implications for human health [3]. The global mean surface temperature, a key indicator of climate change, directly correlates with GHG emissions and increases quasi-linearly [31], underscoring the role of GHGs as primary drivers of climate change. Fig. 2 illustrates global temperature trends from 1970 to 2024 based on observed data from NOAA and HadCRUT5, alongside projected temperature changes from the Shared Socioeconomic Pathways (SSPs) SSP2-4.5 and SSP5-8.5 scenarios for 2015 to 2099 [[32], [33], [34]]. These scenarios represent different future pathways for temperature based on varying levels of GHG emissions and socio-economic conditions. The observed data from 1970 to 2024 show an increasing trend in global temperatures, indicating climate change. Projections for the past eight years (2016–2024) align well with observed data, effectively capturing current climate trends. The SSP2-4.5 scenario assumes moderate GHG emissions with some climate policies, while SSP5-8.5 anticipates high emissions due to economic growth and minimal climate policies. According to these scenarios, global temperature may rise by 2099 by 2.7 °C under SSP2-4.5 scenario and 4.7 °C under SSP5-8.5 scenario. KAUST (King Abdullah University of Science and Technology) team has conducted a study on selected climate variables in Qatar with high-resolution accuracy, utilizing the MIT Regional Climate Model (MRCM) to downscale global climate projections based on two Representative Concentration Pathways (RCP) scenarios, RCP 4.5 and RCP 8.5, to a 10 km resolution. RCP 4.5 and RCP 8.5 from the Coupled Model Intercomparison Project Phase 5 (CMIP5)—a global initiative for standardizing and comparing climate models to assess climate change—are analogous to SSP2-4.5 and SSP5-8.5 in CMIP6 (Phase 6). These scenarios are being used because they correspond to the same radiative forcing targets [35]. The MRCM, is an enhanced version of RegCM3, incorporates improvements to the land surface and convection schemes, which have been shown to improve the model's ability to simulate regional and diurnal variations in rainfall and circulation. The model was forced with initial and boundary conditions from three CMIP5 Global Climate Models—Community Climate System Model Version 4 (hereafter referred to as CCSM), Max-Planck-Institution Earth System Model running on Medium Resolution grid (hereafter referred to as MPI), and Norwegian community Earth System Model (NorESM)—selected for their strong performance in this region [[36], [37], [38]]. The dataset covers the historical period from 1975 to 2005 and projections under the RCP 4.5 and RCP 8.5 scenarios for the period 2070 to 2100, having daily temporal resolution. The resultant model simulations are bias corrected using ERA5 Land reanalysis datasets having the same spatial resolution of 10 km [39]. Ensemble means of the MRCM simulations were used to assess projected changes in temperature, relative humidity, and rainfall. Specifically, Fig. 3 (a, b) displays the annual cycles of monthly mean temperature and relative humidity at three different cities around Qatar (Doha, AlKhor, and Wakrah) under both historical conditions and future RCP 4.5 and RCP 8.5 scenarios. Additionally, Fig. 4 shows annual fluctuations of precipitation for Doha, comparing historical data (1975–2005) with future projections (2070–2100). Qatar experiences extreme summer temperatures, often accompanied by high humidity, while the cooler months bring limited rainfall [40]. As shown in Fig. 3a, the monthly mean temperatures of the three cities forms a bell-shaped curve, with the lowest mean temperature in January and December and the highest in July. The highest values for all months across the three cities occur under RCP 8.5 indicating higher mean temperatures are anticipated from 2070 to 2100 under high emission scenario RCP 8.5. The average increase in temperature across the three hot months (June, July and August) is approximately 2.35 °C, 2.22 °C, and 2.59 °C for Al Khor, Doha, and Wakrah, respectively compared with historical. Humidity in Qatar is very high, with the monthly mean relative humidity (RH) in the three cities showing a U-shaped curve. From November to February, RH ranges between 60 and 72 % in historical conditions, and is projected to be 61–73 % and 61–72 % under the future RCP 4.5 and RCP 8.5 scenarios, respectively. In the highest reported months for RH, the average percentage increase tends to be 1.1 %, 0.6 %, and 0.7 % for Al Khor, Doha and Wakrah respectively under RCP 4.5 scenario. Additionally, AlKhor city consistently has higher RH values than Wakrah city throughout the year. The annual precipitation under historical conditions (1975–2005) ranges from 34 mm to 103 mm indicating the dry climate of Qatar. Under the RCP 4.5 projection (2070–2100), precipitation pattern show periods of both increases and decreases precipitation compared to historical conditions, suggesting a shift towards greater variability. The RCP 8.5 scenario shows a similar trend with generally lower rainfall amounts compared to RCP 4.5. These projections highlight increased interannual variability, with some years experiencing higher-than-average rainfall and others significantly. This highlights the need for adaptive strategies to address both opportunities for increased water availability and risks associated with potential drought conditions.
Fig. 2.
Global temperature trends from 1970 to 2024, based on observed data from NOAA and HadCRUT5, and projected temperature changes from 2015 to 2099 under the SSP2-4.5 and SSP5-8.5 scenarios.
Fig. 3.
Annual cycles of monthly climatology of mean temperature and relative humidity (b) for Al-Khor, Doha and Wakrah during historical (1975–2005) and future projections (2070–2100), based on the ensemble mean of the MRCM model under the RCP 4.5 and RCP 8.5 scenarios.
Fig. 4.
Inter-annual variability of precipitation for Doha city during historical (1975–2005) and future projections (2070–2100) under RCP 4.5 and RCP 8.5 scenarios.
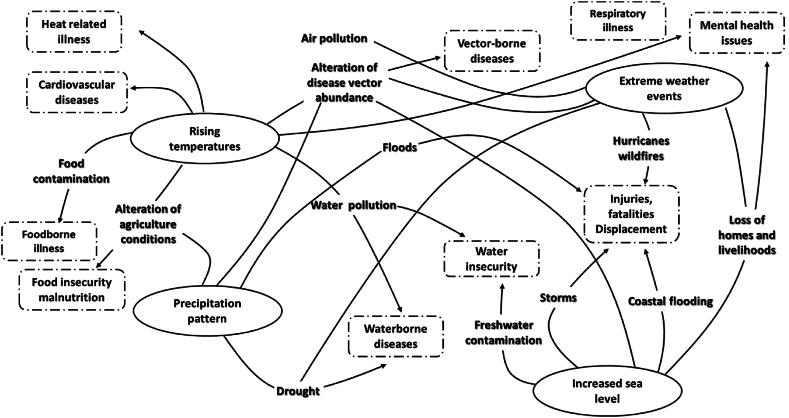
This detailed approach provides valuable insights into the anticipated regional climate trends and their potential impacts on Qatar. A similar trend in average temperature, average relative humidity, and average rainfall in Qatar was observed over 10-year period (2009–2019) [40]. The global mean surface temperature and various climate variables in Qatar shown in this paper, demonstrate a correlation between increased emissions and accelerated climate change, leading to more frequent and severe climate events. These pressures associated with climate change, including rising temperatures, precipitation pattern alterations, extreme weather events, and increased sea levels, all have significant impacts on human health. The interconnectedness between climate change events and their consequences on human health is evident, where similar outcomes can result from different events. Various human health impacts can have direct or indirect negative consequences of climate change events such as heat-related illness, respiratory diseases, cardiovascular diseases, infectious diseases, food and water insecurity, injuries and fatalities, and mental health issues (Fig. 5) [41,42]. Direct health impacts from rising temperatures include heat-related illnesses, cardiovascular diseases, and mental health issues, all directly linked to exposure to high temperatures and heat stress [3,43,44]. Indirect effects arise from rising temperatures, such as air and water pollution, food contamination, altering agriculture conditions, and expansion of the geographical and breeding seasons of disease vectors [45,46]. Elevated temperatures can promote the growth of pathogens, such as bacteria, in food increasing contamination risks and foodborne illness outbreaks [47]. Inadequate refrigeration and improper food handling are exacerbated by elevated temperatures, further increasing the risk of foodborne infections like salmonellosis. Warmer temperatures can also alter agriculture conditions, lead to reduced crop yields and challenging access to nutritious food contributing to food insecurity, especially in vulnerable communities [40]. Moreover, elevated temperatures can contribute to the spread of vector-borne diseases by creating more favorable conditions for the breeding and abundance of disease vectors like mosquitoes and ticks [19]. Tahir et al. [48] studied the effect of climate conditions such as temperature, and relative humidity on the distribution and abundance of mosquito species in Qatar, highlighting the potential public health risks associated with mosquito-borne diseases (VBDs) due to climate change. They identified Culex mosquitoes as the most prevalent, followed by Anopheles and Aedes species. It was found that higher temperatures and lower humidity levels positively influenced the presence of Anopheles and Aedes mosquitoes. Specifically, Aedes mosquitoes thrived in temperatures between 35 and 40 °C and relative humidity levels between 35 and 45 %. The study highlights that climate change significantly affects the distribution of mosquito species, which in turn can lead to an increased risk of VBDs. Rising temperatures accelerate the formation of air pollutants like ground-level ozone and fine particulate matter, worsening respiratory conditions such as asthma and bronchitis [49]. In terms of water quality, rising temperatures promote algal blooms and toxin production in surface water bodies, threatening drinking water sources and increasing the risk of waterborne diseases. Furthermore, reduced water availability due to climate change concentrates pollutants in water sources, exacerbating health risks [45]. Additionally, climate change can alter precipitation patterns, leading to changes in rainfall intensity, incidence, and distribution. Increased flooding, drought, alteration in agriculture conditions, and changing in breeding habitats of disease vectors are all consequences of these precipitation patterns changes [50]. Increased floods can result in injuries, displacement, and waterborne diseases. Conversely, droughts can increase water security and the prevalence of waterborne diseases [51]. Altered agricultural conditions may affect crop productivity, leading to food insecurity and malnutrition [52]. Furthermore, changes in precipitation patterns can influence the distribution and abundance of disease vectors such as mosquitoes by creating more breeding grounds, thereby increasing the transmission rates of vector-borne diseases [53]. Extreme weather events, such as hurricanes, floods, droughts, and wildfires, are intensified by climate change [54]. These events can cause physical injuries, deaths, damage to infrastructure, displacement, forced migration, and mental health issues [3]. Additionally, extreme weather events can increase the risk of vector-borne diseases, waterborne illness, and respiratory and cardiovascular diseases [[55], [56], [57]]. Lastly, the rise in sea levels is a result of climate change. Recent data on sea level trends indicate an average global sea level rise of approximately 1.5–1.9 mm per year from 1901 to 2010, accelerating to 2.8–3.6 mm per year between 1993 and 2010 [58]. Projections suggest that by 2100, sea levels could rise even higher than previous estimates with coastal flooding and storms causing injuries and fatalities. Coastal residents are relocating, losing homes and livelihoods due to flooding and erosion, causing mental health issues. Additionally, coastal flooding creates breeding habitats for diseases vectors which eventually lead to an increase in transmission of vector-borne disease. Rising sea levels can lead to intrusion of sea water into land and freshwater sources causing contamination and increase waterborne diseases [42].
Fig. 5.
Climate change as " Pressure" on human health.
4. The “State” of human health and shifts under the pressure of climate change
The state of human health is significantly shifting in response to climatic pressures. The risk of various disease incidences and occurrences is significantly increasing with the rise of climate change events such as temperature rise and alterations in precipitation patterns.
Table 2 summarizes the associations between various environmental factors and the incidence of diseases such as Campylobacter infections, dengue fever, influenza and pneumonia, malaria, cardiovascular mortality, and acute kidney injury (AKI). The environmental factors considered include temperature, precipitation, heatwaves, and rainfall, with different time lags in their effects on health outcomes. Based on the study designs and statistical models applied, the incidence rates are presented using measures such as odds ratio, incidence rate ratio (IRR), and relative risk (RR). A relative risk of 1.0 indicates no difference in risk between exposed and unexposed groups. A relative risk greater than 1.0 suggests a higher risk in the exposed group, while a relative risk below 1.0 indicates a reduced risk in the exposed group compared to the unexposed group [59]. For instance, Emeto et al. [60] found a positive association between the incidence of malaria and environmental factors like temperature and rainfall, with significantly higher incidence rates observed as temperature and rainfall increased. In contrast, Lim et al. [61] reported no significant change in AKI admissions during cold seasons (RR = 1.009). An extensive literature review was undertaken to evaluate the prevalence of climate-sensitive diseases in Qatar over several years, with the aim of tracking changes in disease incidence. However, the available data on diseases incidence in the region is scarce to nonexistent. A limited number of studies or reports documenting changes in human health in Qatar was found, with little to no connection to climate change. The government of Qatar published in 2019 a national data platform to publicly release data related to human health specifically, infectious and communicable diseases with no data about non-communicable diseases [62]. However, few data are available on the platform, and others are still pending.
Table 2.
Risk measures and associations for various diseases in relation to climate variables from global studies.
| Disease | Variable | Period | Lag time | Incidence Risk measure | Risk Level | model | Ref | |
|---|---|---|---|---|---|---|---|---|
| Incidence of Campylobacter infections | Temperature | Summer (April–September) | One week | IRR | 1.09 | Stable | Poisson regression model | [69] |
| Precipitation | 1.35 | Increase | ||||||
| Heat Wave | 0.90 | Stable | ||||||
| Heavy Precipitation | 2.20 | Increase | ||||||
| Temperature | Winter (October–May) | 1.20 | Increase | |||||
| Precipitation | 0.83 | Decrease | ||||||
| Heavy Precipitation | 0.93 | Stable | ||||||
| Incidence of dengue fever | Mean Temperature (28.46 °C) | January 1998 to December 2012 | Three months | IRR | 1.53 | Increase | Negative binomial model | [70] |
| Max Temperature (32.4 °C) | 1.30 | Increase | ||||||
| Min Temperature (23.3 °C) | 1.45 | Increase | ||||||
| mean Rainfall (103.97 mm) | 1.01 | Stable | ||||||
| ED visit due to Influenza and pneumonia | Max risk temperature (29.4 °C) | 2008–2017 (Summer) | 0–21 days | RRs | 1.26 | Increase | DLNM model | [71] |
| Max risk temperature (−9.0 °C) | 2008–2017 (Winter) | 2.68 | Increase | |||||
| Incidence of malaria | Temperature 97.5th (29.5 °C) | February 2000 to November 2009 | 0–15 weeks | logRR | 2.6 | Increase | DLNM model | [60] |
| Rainfall 97.5th (274 mm) | 17.2 | Increase | ||||||
| Cardiovascular Mortality | Temperature 90th (28.4 °C) | 2004–2010 | 21 days | RRs | 1.118 | Increase | DLNM model | [72] |
| Temperature 95th (29.4 °C) | 1.24 | Increase | ||||||
| Temperature 99th (31.2 °C) | 1.585 | Increase | ||||||
| Admissions for AKI | temperature (≥28.8 °C) | 2007–2014 (Warm season) | 0 days | RRs | 1.233 | Increase | DLNM model | [61] |
| Temperature (<28.8 °C) | 2007–2014 (cold season) | 0–1 days | 1.009 | Stable | ||||
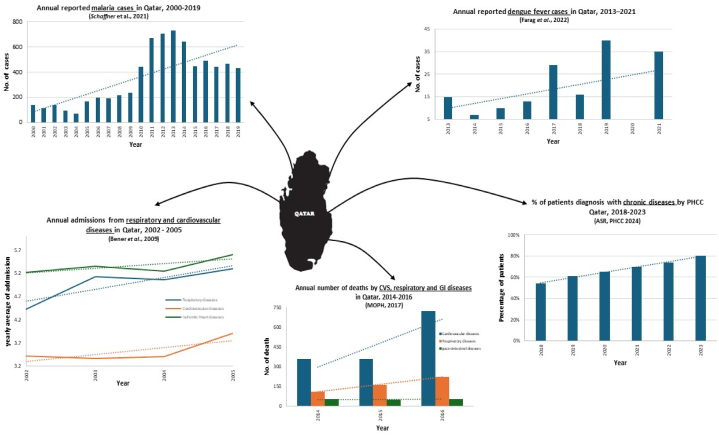
Fig. 6 represents some of the few studies available on the incidence and prevalence of certain climate-sensitive diseases in Qatar reported by different sources, including studies [[63], [64], [65]] and reports by the Ministry of Public Health (MOPH) and the Primary Health Care Corporation (PHCC) [66,67]. The reported diseases include vector-borne diseases such as malaria and dengue fever, chronic diseases, respiratory diseases, cardiovascular diseases (CVS), and gastrointestinal diseases (GI). Schaffner et al. [64] reported a significant increase in malaria cases in Qatar from 2010 to 2014, linked to the entry of migrant workers from malaria-endemic regions, particularly during the summer travel season. The study highlighted that the decline in cases after 2015 was likely due to enhanced public health measures, such as improved screenings and diagnostics. However, despite this decline, malaria case numbers remain higher than pre-2010 levels, reflecting the ongoing importation of cases and Qatar's continued vulnerability to climate-sensitive health. Most of these diseases have shown an increasing trend over the years, with a notable decrease in dengue fever cases during the COVID-19 pandemic in 2020, when only one case was reported compared to 40 and 35 cases in 2019 and 2021, respectively [65]. Among the few studies depicted in Fig. 6, only one study links the incidence of human health (non-communicable diseases) with air pollution, which identified as a pressure of climate change. The study conducted by Bener et al. [63] revealed a significant positive association between higher levels of air pollutants and patients admitted for respiratory and cardiovascular diseases over four consecutive years. Additionally, the Annual Statistical Report (ASR) for 2024 by PHCC indicates an increasing trend in patients diagnosed with chronic diseases such as hypertension, diabetes mellitus, asthma, kidney disorders, mental health disorders, cancer, and cardiovascular diseases from 2018 to 2023 [67]. Summarily, with the environmental changes given, the status of human health is highly critical, as the human health system faces massive pressures from these shifts. Intergovernmental Panel on Climate Change (IPCC) assessments have indicated that climate change has adversely affected human physical health and mental health globally, attributing these effects directly to changes in the climate system with very high confidence. The current state of human health due to climate change, as assessed by the IPCC in 2023, indicates increasing human mortality and morbidity in all regions due to extreme heat events, a rise in food-borne and water-borne diseases, the emergence of zoonotic diseases in new areas, and a link between mental health disorders and high temperatures [68]. Overall, the status of human health is increasingly unstable due to multiple threats that compromise the resilience of human systems and affect their functioning for future generations. While global GHG emissions continue to rise, driving significant climate changes, Qatar is experiencing and will continue to face increased risks of disease incidence due to its local climate conditions. This impact on human health is currently being observed, as illustrated in Fig. 6, and is projected to escalate with future climate change scenarios.
Fig. 6.
State of different climate sensitive diseases in Qatar based on Literature.
5. Climate “Impacts” on human health
Climate change affects human health unequally and in various ways, with both direct and indirect effects. Direct impacts include extreme weather events, such as heatwaves and hurricanes, which can cause injuries and fatalities. Heatwaves, for instance, can lead to heat exhaustion and heatstroke, while hurricanes can result in immediate physical harm and loss of life. Indirectly, climate change influences the spread of diseases. Shifts in temperature and precipitation create favorable conditions for disease-carrying vectors, such as mosquitoes and ticks. This can lead to outbreaks of illnesses, including dengue fever, West Nile virus, and Lyme disease. Warmer temperatures and altered rainfall patterns expand the habitats of these vectors, increasing the risk of disease transmission to humans. Rising sea levels exacerbate the impact of hurricanes by increasing the extent and severity of flooding. This not only displaces communities but also exposes more people to contaminated water and pollutants, leading to a rise in waterborne diseases and other health hazards. Moreover, climate change is increasing the frequency, intensity, and duration of extreme heat events. These heatwaves pose significant health risks, particularly to vulnerable populations such as the elderly, children, and those with pre-existing health conditions. Communities with limited resources are often less equipped to cope with and recover from these extreme weather events, further exacerbating health inequalities. Below are descriptions of some climate-sensitive diseases and the pathways through which climatic variables cause these diseases.
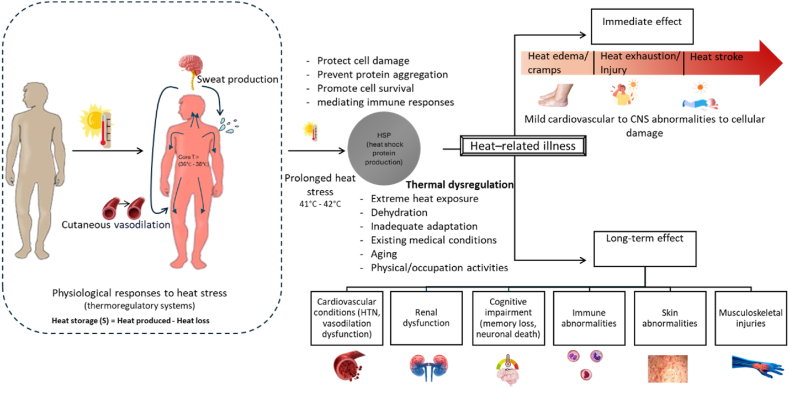
5.1. Heat-related illnesses
A growing body of evidence confirms the strong correlation between high temperatures, heatwaves, and increased morbidity and mortality globally [73]. Exposure to heat stress can cause immediate effects, ranging from mild conditions, such as heat edema, to life-threatening disorders like heatstroke, which involve cardiovascular and central nervous system abnormalities [74]. Long-term consequences of heat stress are associated with various heat-related illnesses, including cardiovascular conditions, respiratory diseases, renal dysfunction, immune abnormalities, cognitive impairment, skin disorders, and musculoskeletal injuries [[75], [76], [77], [78], [79], [80], [81]]. Additionally, a significant number of deaths globally in 2019 were associated with extreme heat [82].
Heat stress refers to an external heat load that results in elevated body heat storage and core body temperature [74]. The human body's heat balance can be described by the heat balance equation [83]:
| (1) |
The rate of heat storage (S) equals the difference between heat produced and heat loss. Heat production arises from metabolic rate () and external work , while heat loss occurs through evaporation (), convection (), radiation (), conduction (), and respiration . When heat production equals heat loss, heat storage (S) is zero, and the core body temperature remains stable. However, if heat production exceeds heat loss, such as during exercise or in hot environments, the body accumulates heat (positive heat storage), causing an increase in core temperature and prompting physiological responses to regulate it [84]. To maintain a core body temperature around 37 °C, the human body relies on thermoregulatory mechanisms, involving sensing of temperature changes, transmitting signals to central control (hypothalamus), and executing appropriate efferent responses. During heat stress, the human body regulates its core temperature through autonomic thermoeffector and behavioral responses [85]. The primary autonomic thermoeffector responses include sympathetically driven cutaneous vasodilation, which widens blood vessels in the skin to transfer heat to the environment, and eccrine sweating, which activates sweat glands to promote evaporative cooling. These processes depend on dry heat exchanges (conduction, convection, radiation) and wet heat exchanges (evaporation of sweat) to dissipate body heat [86]. In hot or humid environments, reduced thermal and water vapor gradients—such as when the surrounding temperature exceeds skin temperature or when the air is saturated with moisture—impair heat dissipation. These limits sweat evaporation and increases heat storage. In such uncompensable conditions, prolonged exposure leads to a progressive rise in body temperature, potentially compromising health if not addressed [87]. Prolonged exposure to thermal stress triggers additional physiological responses at the cellular level. Heat shock proteins (HSPs) are produced to prevent protein misfolding and aggregation under heat stress, while also mediating immune responses and promoting cell survival, making them critical for cytoprotection and systemic defense against environmental stimuli(such as heat stress) [88,89]. Under extreme conditions, such as intense physical or occupational activities in hot environments, the combination of increased metabolic heat production and restricted heat loss can overwhelm the body's thermoregulatory capacity. Failure of regulatory mechanisms, particularly in individuals with pre-existing medical conditions (e.g., cardiovascular, renal, or respiratory conditions), the elderly, children, those on specific medications, or those inadequately acclimatized or dehydrated, can result in thermal dysregulation and heat-related illnesses [90].
These illnesses can manifest immediate effects, such as heat injury or heat stroke, or long-term consequences, including cardiovascular collapse, organ dysfunction, and other potentially fatal outcomes [91]. Fig. 7 illustrates human body thermal regulation under heat stress and thermal dysregulation, which can lead to heat-related illnesses.
Fig. 7.
Understanding Heat stress: Physiological Responses and Heat Related illness.
5.2. Vector-borne diseases
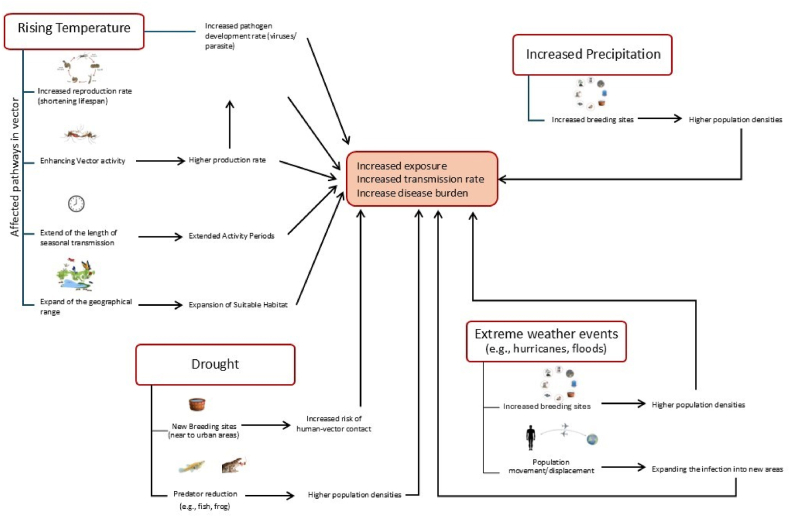
Vector-borne diseases (VBDs) are illnesses caused by infectious pathogens (viruses, bacteria, or parasites) that are transmitted from infected hosts (usually humans or animals) to uninfected individuals through the bite of a vector. Vectors are organisms such as mosquitoes, ticks, sandflies, bugs, tsetse flies, and lice that can carry and transmit pathogens between hosts, contributing to the spread of diseases [92]. VBDs represent over 17 % of all infectious diseases globally and are responsible for more than 700,000 deaths annually. For example, approximately 4 billion people across 128 countries are at the risk of developing dengue, resulting in an estimated 96 million cases annually [93]. Out of 15 VBDs commonly found in Arab countries, six are prevalent in Qatar. These include West Nile virus, leishmaniasis, Crimean-Congo hemorrhagic fever (CCHF), plague, malaria, and dengue fever [64,65,94]. Fazaludeen Koya et al. [95] conducted a systematic review focusing on the incidence of VBD in the Eastern Mediterranean region. Their study revealed an increasing trend in the incidence and re-emergence of VBD in this region over time, with higher reported incidence rates in urban areas. The global rise in VBDs is closely linked to climate change. This is partly due to the ectothermic nature of vectors, the temperature-dependent extrinsic incubation of pathogens, vector responses to changes in their environment, and outbreaks in areas previously unchallenged by such diseases [96]. Fig. 8 shows how each climatic change contributes to increase the transmission of VBDs. Rising temperatures, a key climatic change, play a significant role in vector and pathogen dynamics, affecting VBD transmission. Higher temperatures increase the production rates and activities of vectors, such as mosquitoes and ticks, which are ectothermic organisms whose body temperature is primarily influenced by their environment. Warmer temperatures lead to increased metabolic rates, leading to accelerated development and reproduction rates. This contributes to larger populations of vectors capable of transmitting diseases, ultimately impacting VBD transmission dynamics [97]. Additionally, temperature influences the rate at which pathogens, like the dengue virus, develop within vectors. A higher temperature leads to a faster development of the virus within the vector. In fact, if the pathogen's development rate is slow or the vector's survival is short, an infected vector may never become capable of transmitting infection [98]. For instance, Plasmodium falciparum protozoa require 13 days to develop at 25 °C, compared to 26 days at 20 °C, demonstrating how warmer temperatures accelerate their development cycle. Similar mosquito dengue is observed to spread faster in climates with higher temperature and humidity (optimum temperature 24–31 °C) [96]. Moreover, rising temperatures extend the length of seasonal transmission and expand the geographical range of vectors, turning previously inhospitable regions into suitable habitats [99]. It has been observed that a 2 °C temperature rise could extend the hypothetical transmission season by up to one month and increase the geographical area of suitability by 25–30 % [100]. As temperatures continue to rise, exposure and diseases transmission increase and eventually the burden of these diseases is expected to increase. Change in precipitation patterns can also lead to an increase in the transmission of VBDs. Both drought and increased precipitation can create favorable conditions for certain vectors, increasing the risk of human exposure [101]. Drought can impact VBD dynamics by altering breeding sites and reducing predator populations. Increased drought has prompted human communities to increase water storage in containers, creating more breeding sites for disease-carrying mosquitoes in urban areas and thus increasing the risk of exposure to humans [93]. Additionally, droughts can lead to a decline in mosquito predators like frogs and dragonflies, worsening the situation. With reduced water sources, habitats for aquatic predators such as fish, frogs, or aquatic insects that feed on mosquito larvae are diminished. This decrease in predator abundance can result in higher survival rates for mosquito larvae and, consequently, increased mosquito populations. The increased risk of dengue fever has been linked to drought in highly urban areas with limited water sources relying on water storage tanks [102]. Moreover, increases in human West Nile Virus (WNV) cases during droughts are attributed to mosquitoes exhibiting improved predator avoidance behaviors during mosquito oviposition (egg-laying) [99]. On the other hand, increased precipitation can provide more favorable aquatic environments for oviposition, larval development, and survival of certain vectors. This is due to the formation of unstable water pools, along with elevated humidity and surface moisture. Such favorable conditions can heighten the risk of diseases like malaria, dengue fever, and chikungunya [96]. During the winter season with rainfall, there was an increase in the abundance of Culex pipiens mosquitoes, which are known vectors for various diseases [103]. Extreme weather events like hurricanes and floods significantly impact the transmission dynamics of VBDs. Heavy rainfall associated with these events creates stagnant water pools, which increase breeding sites, leading to a sharp rise in vector populations and an increased risk of disease transmission. Additionally, floods can wash out vector habitats, spreading them to new areas and exposing more people to diseases [104]. Population displacement and water contamination further exacerbate the situation, increasing human vulnerability to VBDs [41].
Fig. 8.
Climate change: escalating the dynamics of vector-borne diseases.
5.3. Food and waterborne diseases
In addition to VBD, waterborne and foodborne diseases are also sensitive to climate change [105]. Waterborne and foodborne diseases result from ingesting pathogens or toxins through contaminated water or food. Conversely, vector-borne diseases arise from infections transmitted by arthropods, such as mosquitoes. Water-borne diseases, which can be infectious agent or toxic, are caused by exposure to contaminated water sources such as recreational water (e.g., swimming pools), non-recreational water (e.g., sanitation, industry, agriculture), and drinking water [106]. Foodborne diseases occur as a result of ingestion of contaminated food due to inadequate hygiene, cooking, or storage. These disease outbreaks, influenced by climatic shifts and environmental disruptions, peak in summer with higher temperatures and humidity, particularly among children [107]. Walker [108] highlighted that climate change affects food- and water-borne diseases through direct contamination events such as floods and sea-level rise, as well as indirectly through climatic factors that impact pathogen survival and transmission dynamics. The climatic variables that most affect these illnesses are increased air temperature, water temperature and precipitation. Cissé [105] described three key mechanisms by which climate variables influence foodborne diseases: (i) pathogen Abundance and Survival, (ii) human Exposure Factors, and (iii) transmission Dynamics. Increased temperature directly impacts the abundance, growth, and survival of foodborne pathogens in various environments, including crops and livestock. Warmer temperatures accelerate the replication cycles of pathogens like E. coli and Salmonella, increasing their prevalence in agricultural settings and potentially contaminating food during production and processing stages [109]. During summer months, Campylobacter infections increase due to favorable conditions like higher temperatures and humidity, which boosts bacterial growth in poultry and increases food contamination risks. Similarly, Salmonella infections rise in summer as warmer climates enhance bacterial survival in livestock contaminating food sources, leading to more human infections [110]. Additionally, prolonged periods of warm seasons can influence human behaviors related to food handling, storage, and consumption. Higher temperatures may alter cooking practices, food preferences, and storage conditions, potentially increasing the risk of food contamination and subsequent foodborne illnesses [111]. Extreme weather events, such as hurricanes and floods, contaminate food sources by spreading pathogens from sewage systems or agricultural runoff. In 2017, Hurricane Irma contaminated numerous commercial fruit and vegetable fields in Florida with pathogens and parasites, prompting the United States Food and Drug Administration (US FDA) to advise against consuming fresh produce exposed to floodwater. Furthermore, hurricanes disrupt food processing, preparation, and transport, leading to significant food waste. Changes in precipitation patterns can impact the movement and persistence of pathogens in the environment, influencing their transmission to humans through food consumption [112]. Climatic variables have also contributed to the increased rate of waterborne disease incidences. Firstly, elevated water temperatures directly impact the proliferation and survival of waterborne pathogens such as cholera and diarrheal diseases. Diarrheal diseases are the major cause of morbidity and mortality in South Asia, predominantly among children. Warmer temperatures accelerate the metabolic rates of these pathogens, increasing their reproduction cycles and overall abundance in aquatic environments. This phenomenon enhances the likelihood of human exposure through contaminated water sources. Cholera and typhoid are representative bacterial foodborne or waterborne infectious diseases, which are clearly associated with temperature increases [113]. Shayo et al. [114] reported that 2.1 billion people globally lack access to clean and safe drinking water, which leads to 2.2 million deaths annually from waterborne diseases.
Secondly, changes in precipitation patterns, including intense rainfall and flooding events, can trigger runoff from agricultural areas, sewage systems, and urban landscapes. This runoff carries pathogens such as Giardia, Cryptosporidium, and various pathogenic bacteria into surface waters and drinking water reservoirs, heightening the risk of waterborne disease outbreaks [115,116]. Additionally, alterations in water quality due to climatic factors such as increased turbidity or changes in pH levels can affect pathogen survival and persistence in water bodies. For instance, higher turbidity during heavy rainfall can shield pathogens from disinfection processes, compromising water safety. Moreover, natural disasters like hurricanes and cyclones can damage water infrastructure, leading to sewage overflows and contamination of drinking water supplies with pathogens. These events exacerbate the spread of waterborne diseases among affected populations. Drought increases waterborne diseases incidence by reducing water availability, worsening hygiene conditions, and increasing the likelihood of microbial contamination in drinking water and agricultural practices. Subsequent intense rainfall after droughts can cause surface water contamination spikes, leading to outbreaks such as Cryptosporidiosis and E. coli. For instance, the largest reported E. coli O157outbreak in New York in September 1999 was linked to contaminated well water following heavy rainfall after a period of drought [117]. In summary, climate change has considerable consequences on incidence and transfer of food and waterborne diseases, but these interactions are complex and dependent on various factors [47].
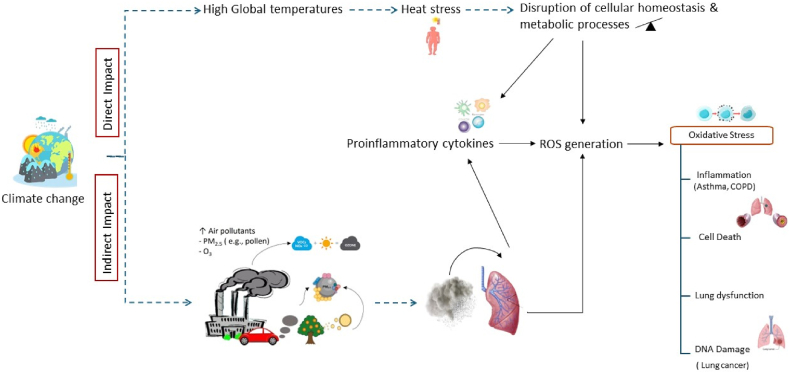
5.4. Respiratory diseases
Respiratory diseases are becoming increasingly prevalent due to climate change, posing a significant threat to public health. Climate change directly promotes respiratory illness or indirectly increases the risk of such diseases by exacerbating air pollution [118]. Studies have shown that extreme heat or extreme cold increases the mortality risk from respiratory diseases [119,120]. The relationship between temperature and mortality follows a 'U' shape, where both high and low temperatures increase the risk of mortality. Climate change affects respiratory health indirectly by influencing the weather pattern and air quality. Notably, the 2003 heat waves in Europe, with temperatures exceeding 35 °C, resulted in approximately 40,000 excess deaths [121]. Understanding the pathways linking climate change and air pollution is necessary to understand how this connection impacts respiratory health. Air pollution has become increasingly severe, leading to approximately 7 million premature deaths annually and a significant rise in hospitalizations and sick days due to related health issues [122]. The U.S. Environmental Protection Agency (US EPA) describes air pollution as contamination of the air by any chemical, physical, or biological materials that deteriorate air quality and negatively impact its characteristics [123]. In terms of ambient air quality, different air pollutants pose significant health risks. Among them particulate matter (PM2.5) and ground ozone (O3) are gaining considerable attention due to their ability to penetrate deeply into the lung and adverse effects on respiratory health. The global burden of disease attributed to O3 exposure is 254,000 excess mortality cases reported in 2015, while 4.2 million deaths were attributed to PM2.5 during the same year [124]. Ground-level O3, formed at the troposphere level, is primarily generated by chemical reaction nitrogen dioxide (NO2) and volatile organic compounds (VOCs) in the presence of sunlight and heat [125]. NO2 and VOCs are mainly emitted from traffic-related sources and industrial processes, while the heat effect induced by climate both accelerate chemical reaction in the atmosphere and lead to increased level of O3 [123]. PM2.5 is composed of liquid or solid fine particulate matter measuring 2.5 μm or less in diameter, originating from both primary sources (e.g., road dust, industrial emissions) and secondary sources (e.g., chemical reactions in the atmosphere). Because of their size, PM2.5 is of greater concern compared to other particulate matters. While larger particles are generally filtered out in the nose and throat, PM2.5 can bypass these defenses, entering the lung alveoli and potentially even the bloodstream. This poses significant health risks, including potentially life-threatening conditions [126]. O3 and PM2.5 like other air pollutants are contributing to respiratory diseases. Their mechanisms in causing these diseases can be similar to some extent. Exposure to both pollutants induces the production of reactive oxygen species (ROS). Additionally, O3 itself is considered ROS due to its oxidation properties. ROS are highly reactive molecules containing oxygen, typically produced as natural byproducts of cellular metabolism. Also, these pollutants can stimulate the release of proinflammatory cytokines, which can further exacerbate ROS production as part of the inflammatory response [127]. Excessive ROS production in the body leads to respiratory tract oxidative stress and inflammation. This stress triggers allergic reactions, morphological alterations in the tract, and compromises defense mechanisms. Increased airway responsiveness results in obstruction and reduced lung function. These responses collectively contribute to the development or progression of respiratory diseases such as asthma, chronic obstructive pulmonary disease (COPD), and respiratory infections [128]. The pathogenicity of PM2.5 depends on factors such as their size, composition, source, solubility, and capacity to generate ROS [129]. Xing et al. [130] have described various mechanisms by which PM2.5 damages respiratory system, including the ability to form ROS as Hydroxyl radicals (OH) which is responsible for oxidative stress and DNA damage causing respiratory illness or carcinogenesis effects. Additionally, excess ROS production induced by PM2.5 can decrease the antioxidant levels and elevate intracellular calcium concentrations. Abnormally high calcium concentrations activate inflammatory reactions, leading to inflammation and cell damage. PM2.5 exposure also stimulates the overexpression of inflammatory cytokines, leading to inflammation-related damage and increased inflammatory cell infiltration in the lungs. The health effects of air pollution can exhibit both short-term and long-term effects. Short-term effects include conditions like asthma, while long-term exposure can lead to more severe consequences such as lung cancer and cardiovascular diseases. PM2.5 exposure is associated with long-term effects [131], whereas O3 exposure is linked to short-term health impacts [128]. Another air pollutant affected by climate change is pollen, which can contribute to PM2.5 pollution and has shown significant effects in recent years. Higher temperature and increase levels of CO2 in the atmosphere due to climate change stimulate plant growth and produce more pollen and the pollen season tends to lengthen [132]. These changes have implications for individuals with allergic conditions, as they may experience more severe and prolonged allergy symptoms [121]. In general, certain groups are more vulnerable to the effects of air pollutants, including children, the elderly, and individuals with pre-existing medical conditions such as cardiovascular and respiratory diseases. On the other hand, the direct impact is related to physiological consequences of climate change on respiratory systems including inflammation, oxidative stress, and immune system suppression. Elevated temperatures can lead to the generation of ROS by disruption of cellular homeostasis and metabolic processes, causing oxidative damage to cells and tissues within the respiratory system [133]. This imbalance of oxidative stress triggers inflammation and tissue damage, worsening respiratory symptoms and disorders. Additionally, temperature fluctuations can stimulate the release of proinflammatory cytokines, potentially worsening existing respiratory conditions [122]. Changes in climate may also alter the immune response to respiratory infections, affecting infection severity and duration, while temperature shifts could impact the growth and survival of respiratory pathogens, influencing the prevalence and transmission of respiratory infections [123,134]. In summary, climate change can directly or indirectly cause respiratory diseases by inducing ROS production and causing oxidative stress, which contributes to the development or progression of respiratory diseases. Fig. 9 summarizes both the direct physiological impacts and indirect consequences of climate change on respiratory health.
Fig. 9.
Direct physiological impacts and indirect consequences of climate change on respiratory health.
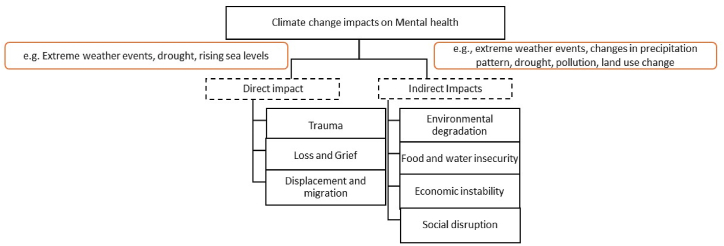
5.5. Mental health illnesses
Mental health is widely recognized as a crucial component of overall health, and its vulnerability to the effects of global climate change is increasingly evident. The consequences of climate change act as stressors for mental health, with a likely increase in the incidence and prevalence of mental illness, especially among vulnerable populations such as individuals with pre-existing conditions, children, and the elderly [135,136]. Environmental changes have led to the emergence of new psychological syndromes, such as climate anxiety and solastalgia, underscoring the significant threat posed by climate change to mental health. Solastalgia, introduced by philosopher Glenn Albrecht in 2005, merging "solace," "desolation," and "nostalgia," to capture the distress caused by direct exposure to environmental degradation within one's own community [137]. Climate anxiety, also referred to as climate change psychological distress (CCPD), is a chronic fear of environmental change that ranges from mild stress to serious clinical conditions, including anxiety, depression, and even suicide [138]. Climate change impacts on mental health can be categorized as direct or indirect. Direct impacts refer to the psychological consequences of exposure to climate-related events, such as floods, storms, wildfires, and gradual phenomena like droughts, which lead to acute stress, PTSD, depression, and grief. Such events also correlate with increased rates of depression and PTSD among survivors of hurricanes and floods, and higher suicide risks among affected communities [139]. Additionally, climate-related migration can contribute to violence and increase the risk of suicide. Depression and/or PTSD rates ranging from 20 % to 30 % have been documented among survivors of hurricanes, with similar rates observed among individuals affected by flooding [140,141]. Drought has also been linked to an increased risk of suicide among farmers [142]. Indirect impacts stem from broader social, economic, and environmental changes induced by climate change [143]. These include food and water insecurity, exacerbated by disruptions in agricultural productivity, economic instability due to job losses in affected industries like agriculture and tourism, and concerns over future access to clean water [144]. Furthermore, climate-induced environmental degradation and resource scarcity can drive involuntary migration, as communities seek safer and more stable living conditions.
This displacement disrupts social networks and can lead to conflicts, exacerbating mental health issues such as depression and anxiety [145]. Pollution, deforestation, and loss of biodiversity further compound these challenges, increasing exposure to environmental contaminants and reducing access to natural environments, both of which contribute to mental health problems [146]. Briefly, in each case, climate change acts as a catalyst, either directly or indirectly, contributing to mental health impacts and resulting mental disorders. Fig. 10 summarizes the direct and indirect impacts of climate change on mental health.
Fig. 10.
Direct and Indirect Impact of Climate change on Mental Health.
6. Actions taken as “Responses” to address the health impact of climate change
Actions referred to as “Responses” have been initiated to address the health impacts of climate change, supported by extensive evidence of its effects on both physical and mental health. Climate change impacts human health through direct effects on bodily systems or indirectly by transforming our environment into unhealthy conditions. The urgency of addressing climate-related health impacts is highlighted by mounting scientific evidence. These actions aim to prevent the factors driving climate change, reduce the subsequent pressures, restore current health conditions, and enhance adaptive strategies to effectively address these health impacts. Addressing these health impacts not only improves public health outcomes but also enhances societal resilience and reduces healthcare costs associated with climate-related illnesses.
Qatar is actively addressing climate change through comprehensive national strategies and international commitments. The nation faces significant climate challenges, such as sea level rise, flooding, and extreme temperatures affecting its coastal urban areas. To combat these issues, Qatar has implemented several key initiatives [147].
6.1. National commitments
-
•
Qatar National Vision 2030 (QNV 2030): Qatar National Vision 2030 (QNV 2030), launched in 2008, is a pioneering long-term strategy built on four pillars: economic, social, environmental, and human development. It aims to guide the nation towards sustainable growth by reducing reliance on fossil fuels, investing in renewable energy, and managing resources efficiently. The strategy aligns with the UN Sustainable Development Goals and seeks to position Qatar as a regional leader in environmental stewardship [148,149].
-
•
National Environment and Climate Change Strategy (QNE): Introduced in 2021, this strategy focuses on reducing GHG emissions, improving air quality, and promoting sustainable practices such as recycling and green building standards [150].
-
•
National Climate Change Action Plan (NCCAP): Launched in 2021, aims to cut GHG emissions by 25 % through mitigation and adaptation strategies. It focuses on key sectors, including oil and gas, power, and transportation, and includes measures such as carbon capture, energy efficiency, and renewable energy. The plan also emphasizes building resilience, improving infrastructure, and protecting biodiversity to reduce Qatar's vulnerability to climate change [151].
-
•
Nationally Determined Contribution (NDC): As part of the Paris Agreement, Qatar sets a goal to reduce GHG emissions intensity by 15 % by 2030 compared to 2010 levels. It includes actions such as exploring Carbon Capture and Storage (CCS) technology, improving water management and infrastructure and seeking international support for finance and technology. Regular reporting ensures transparency and alignment with Qatar's sustainable development goals [152].
-
•
Heat Stress Plan: In May 2021, Qatar introduced Ministerial Decision No. 17 to protect workers from heat stress by regulating working hours and setting guidelines for high temperatures. This decision aims to reduce heat-related illnesses and improve worker safety, reflecting Qatar's commitment to addressing climate-related health impacts [153].
-
•
Climate Change and Environmental Call (CCEC): The Qatar Research, Development, and Innovation Council (QRDI)/Qatar National Research Fund (QNRF), in collaboration with the Ministry of Environment and Climate Initiated CCEC in 2023, this research program supports projects that enhance environmental sustainability and reduce climate change effects.
6.2. International commitments
-
•
Qatar has demonstrated a strong commitment to international organizations and bodies focused on the environment and climate change. The nation ratified the United Nations Framework Convention on Climate Change (UNFCCC) in 1996, highlighting its early dedication to global climate efforts. In 2005, Qatar signed the Kyoto Protocol, signaling its participation in international endeavors to reduce GHG emissions. Qatar also signed the Paris Agreement on Climate Change in 2016 and ratified it in 2017, reaffirming its strong commitment to global climate action [154].
-
•
Qatar has actively contributed to both international and national events concerning climate change. Internationally, Qatar hosted the 18th session of the Conference of the Parties (COP18) to the UNFCCC in 2012, highlighting its role in global climate diplomacy. In 2021, Qatar participated in COP26 in Glasgow, where it presented its plans to reduce GHG emissions and contribute to global climate goals. Nationally, in 2022, Qatar hosted the 20th edition of the Doha Forum, focusing on Climate Change and Sustainability under the theme "Transforming for a New Era." [154].
-
•
Qatar is actively advancing climate resilience through initiatives such as its partnership with the Global Green Growth Institute (GGGI), which began operations in Doha in January 2022. GGGI is an international organization dedicated to promoting sustainable economic growth in developing countries and emerging economies. The GGGI Qatar office collaborates closely with the government and local stakeholders to implement green growth strategies and projects aimed at enhancing climate resilience and promoting sustainable practices [147].
Overall, Qatar is taking substantial steps to address climate change through national policies and international cooperation, aiming to enhance resilience, reduce emissions, and promote sustainable development. Moving forward, Qatar could further strengthen its efforts by enhancing public awareness, accelerating renewable energy deployment, and encouragement greater international collaboration for technology transfer and capacity building, specifying baselines for some targets allowing assessing the progress throughout the implementation.
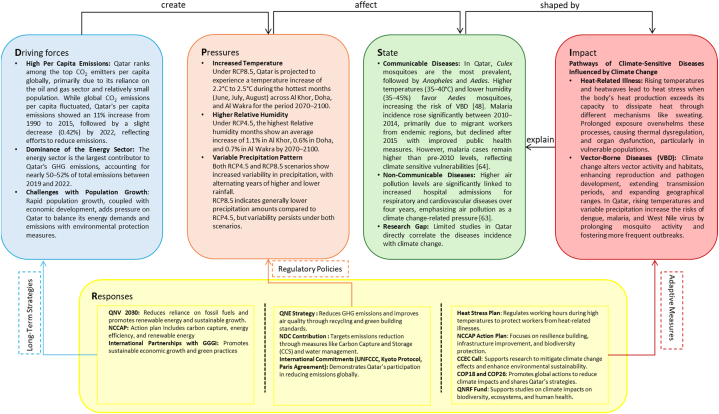
7. Conclusions and major findings from the detailed DPSIR framework for Qatar
This paper utilized the DPSIR framework to investigate the global impacts of climate change on human health, with a specific focus on Qatar. Fig. 11 presents a detailed DPSIR framework, integrating the key findings and analyses from each section of this paper. The framework identifies the primary drivers of climate change in Qatar, including its high CO₂ emissions per capita—among the highest globally—driven by the energy sector, rapid population growth, economic development, and resource demands. These drivers create significant climatic pressures, such as rising temperatures, higher relative humidity, and variable precipitation patterns, which pose serious risks to human health.
Fig. 11.
Detailed DPSIR framework for the impact of climate change on human health in Qatar.
Projections using the MRCM model indicate that Qatar will experience increases in temperature and altered precipitation patterns by 2070–2100, leading to adverse health impacts. These pressures influence the state of climate-sensitive diseases, including communicable and non-communicable diseases. For example, higher temperatures and lower humidity in Qatar favor Aedes mosquitoes, increasing the risk of vector-borne diseases like malaria. Similarly, rising air pollution levels are associated with increased hospital admissions for respiratory and cardiovascular diseases. Despite these clear risks, this study finds limited research in Qatar linking the incidence of such diseases directly to climate change, highlighting a critical research gap. The lack of comprehensive data on climate-sensitive diseases in the region hinders efforts to understand their prevalence and develop effective action plans. Climate-sensitive diseases in Qatar are shaped by pathways through which climate variables influence human health, including accelerated pathogen development, impaired thermoregulation, and inflammation triggered by air pollution. These pathways contribute to impacts that intensify health vulnerabilities associated with climate change, which in turn explain the state of these diseases in Qatar. At the conclusion of this paper, we summarize the national and international responses Qatar has implemented to address drivers, pressures, and impacts. These responses indirectly influence the state of climate-sensitive diseases by targeting other components of the DPSIR framework. Long-term strategies such as promoting renewable energy and sustainable growth address the drivers of climate change. Regulatory policies and actions, such as reducing GHG emissions and implementing carbon capture technologies, aim to alleviate climatic pressures. Meanwhile, adaptive measures, such as the Heat Stress Plan, target the reduction of health impacts caused by climate change.
This approach emphasizes the critical need to strengthen public health infrastructure, enhance surveillance systems, and accelerate evidence-based policies to reduce emissions and adapt to future climate projections. Although systems to address emissions are already in place, more rapid and effective actions are essential to address the escalating challenges posed by climate change and its growing impact on human health. By applying an integrated climate-health strategy, Qatar can effectively tackle societal challenges, build resilience, reduce health inequities, and promote sustainable development in the face of increasing climate-related risks.
CRediT authorship contribution statement
Haneen I. Eldos: Writing – review & editing, Writing – original draft, Project administration, Data curation, Conceptualization. Furqan Tahir: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. U.N. Athira: Data curation, Formal analysis, Investigation, Writing – review & editing. Hend O. Mohamed: Data curation, Investigation, Writing – review & editing. Bincy Samuel: Data curation, Investigation, Writing – review & editing. Sini Skariah: Data curation, Investigation, Writing – review & editing. Sami G. Al-Ghamdi: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – review & editing. Tareq Al-Ansari: Conceptualization, Investigation, Project administration, Supervision, Writing – review & editing. Ali A. Sultan: Conceptualization, Investigation, Project administration, Supervision, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This research was supported by the Qatar National Research Fund (QNRF) through the National Priorities Research Program – Cluster 14 Cycle, under the funded project number NPRP14C-0909-210008, and by Hamad Bin Khalifa University (HBKU), a member of Qatar Foundation (QF). Any opinions, findings, conclusions, or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the views of the QNRF, HBKU, or QF.
Contributor Information
Haneen I. Eldos, Email: hia4003@qatar-med.cornell.edu.
Ali A. Sultan, Email: als2026@qatar-med.cornell.edu.
References
- 1.Rao K.K., Al Mandous A., Al Ebri M., Al Hameli N., Rakib M., Al Kaabi S. Future changes in the precipitation regime over the Arabian Peninsula with special emphasis on UAE: insights from NEX-GDDP CMIP6 model simulations. Sci. Rep. Jan. 2024;14(1):151. doi: 10.1038/s41598-023-49910-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abbass K., Qasim M.Z., Song H., Murshed M., Mahmood H., Younis I. A review of the global climate change impacts, adaptation, and sustainable mitigation measures. Environ. Sci. Pollut. Control Ser. Jun. 2022;29(28):42539–42559. doi: 10.1007/s11356-022-19718-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ebi K.L., et al. Extreme weather and climate change: population health and health system implications. Annu. Rev. Publ. Health. Apr. 2021;42(1):293–315. doi: 10.1146/annurev-publhealth-012420-105026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma P., Chauhan A., Gupta A. “Climate change an existential dread”- a compendium study of climate change and its various effects,”. Webology. 2021:1407–1421. doi: 10.29121/WEB/V18I1/21. [DOI] [Google Scholar]
- 5.Andric I., Al-Ghamdi S.G. Climate change implications for environmental performance of residential building energy use: the case of Qatar. Energy Rep. Feb. 2020;6:587–592. doi: 10.1016/j.egyr.2019.09.030. [DOI] [Google Scholar]
- 6.Vinodhkumar B., Ullah S., Kumar T.V.L., Al-Ghamdi S.G. Amplification of temperature extremes in Arabian Peninsula under warmer worlds. Sci. Rep. Jul. 2024;14(1) doi: 10.1038/s41598-024-67514-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Santos F.D., Ferreira P.L., Pedersen J.S.T. The climate change challenge: a review of the barriers and solutions to deliver a Paris solution. Climate. May 2022;10(5):75. doi: 10.3390/cli10050075. [DOI] [Google Scholar]
- 8.Loucks D.P. The Impacts of Climate Change. Elsevier; 2021. Impacts of climate change on economies, ecosystems, energy, environments, and human equity: a systems perspective; pp. 19–50. [DOI] [Google Scholar]
- 9.Sarigiannis D., Gotti A., Karakitsios S. Health impact assessment of climate change mitigation and adaptation policies. ISEE Conference Abstracts. Sep. 2022;2022(1) doi: 10.1289/isee.2022.O-PK-36. [DOI] [Google Scholar]
- 10.Moss E.D., Evans D.M., Atkins J.P. Investigating the impacts of climate change on ecosystem services in UK agro-ecosystems: an application of the DPSIR framework. Land Use Policy. Jun. 2021;105 doi: 10.1016/j.landusepol.2021.105394. [DOI] [Google Scholar]
- 11.Tscherning K., Helming K., Krippner B., Sieber S., y Paloma S.G. Does research applying the DPSIR framework support decision making? Land Use Policy. Jan. 2012;29(1):102–110. doi: 10.1016/j.landusepol.2011.05.009. [DOI] [Google Scholar]
- 12.Patz J.A., Grabow M.L., Limaye V.S. When it rains, it pours: future climate extremes and health. Ann Glob Health. Nov. 2014;80(4):332. doi: 10.1016/j.aogh.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malmir M., Javadi S., Moridi A., Neshat A., Razdar B. A new combined framework for sustainable development using the DPSIR approach and numerical modeling. Geosci. Front. Jul. 2021;12(4) doi: 10.1016/j.gsf.2021.101169. [DOI] [Google Scholar]
- 14.Kabir M., et al. Climate change due to increasing concentration of carbon dioxide and its impacts on environment in 21st century; a mini review. J. King Saud Univ. Sci. Jul. 2023;35(5) doi: 10.1016/j.jksus.2023.102693. [DOI] [Google Scholar]
- 15.Bolan S., et al. Impacts of climate change on the fate of contaminants through extreme weather events. Sci. Total Environ. Jan. 2024;909 doi: 10.1016/j.scitotenv.2023.168388. [DOI] [PubMed] [Google Scholar]
- 16.Mahmood J., Guinto R.R. Impacts of climate change on human health: emerging evidence and Call to action. Malays. J. Med. Sci. Oct. 2022;29(5):1–4. doi: 10.21315/mjms2022.29.5.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kjellstrom T., Briggs D., Freyberg C., Lemke B., Otto M., Hyatt O. Heat, human performance, and occupational health: a key issue for the assessment of global climate change impacts. Annu. Rev. Publ. Health. Mar. 2016;37(1):97–112. doi: 10.1146/annurev-publhealth-032315-021740. [DOI] [PubMed] [Google Scholar]
- 18.Donatti C.I., Harvey C.A., Hole D., Panfil S.N., Schurman H. Indicators to measure the climate change adaptation outcomes of ecosystem-based adaptation. Clim. Change. Feb. 2020;158(3–4):413–433. doi: 10.1007/s10584-019-02565-9. [DOI] [Google Scholar]
- 19.Mojahed N., Mohammadkhani M.A., Mohamadkhani A. Climate crises and developing vector-borne diseases: a narrative review. Iran. J. Public Health. Dec. 2022 doi: 10.18502/ijph.v51i12.11457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kweku D., et al. Greenhouse effect: greenhouse gases and their impact on global warming. J Sci Res Rep. Feb. 2018;17(6):1–9. doi: 10.9734/JSRR/2017/39630. [DOI] [Google Scholar]
- 21.Kumar A. Biofuels: Greenhouse Gas Mitigation and Global Warming. Springer India; New Delhi: 2018. Global warming, climate change and greenhouse gas mitigation; pp. 1–16. [DOI] [Google Scholar]
- 22.Tuckett R. Reference Module in Chemistry, Molecular Sciences and Chemical Engineering. Elsevier; 2018. Greenhouse gases. [DOI] [Google Scholar]
- 23.Mehmood T., et al. Climate Change Alleviation for Sustainable Progression. CRC Press; Boca Raton: 2022. Mechanism behind sources and sinks of major anthropogenic greenhouse gases; pp. 114–150. [DOI] [Google Scholar]
- 24.Crippa M., et al. Publications Office of the European Union; Luxembourg: 2023. GHG Emissions of All World Countries- JRC/IEA 2023 Report. [DOI] [Google Scholar]
- 25.Al-Mohannadi S.A., Al-Mohannadi D.M. 2023. Qatar in the Energy Transition: Low Carbon Economy Challenges and Opportunities; pp. 109–126. [DOI] [Google Scholar]
- 26.Qatar Energy . Doha; 2019. Sustainability Report 2019. [Google Scholar]
- 27.Qatar Energy . Doha; 2020. Sustainability Report 2020. [Google Scholar]
- 28.Qatar Energy . Doha; 2021. Sustainability Report 2021. [Google Scholar]
- 29.Qatar Energy . Doha; 2022. Sustainability Report 2022. [Google Scholar]
- 30.Shannak S., Contestabile M. Does Qatar face a trade-off between economic growth and CO2 emissions? Front. Environ. Sci. 2022;10(Apr) doi: 10.3389/fenvs.2022.855971. [DOI] [Google Scholar]
- 31.Rahmstorf S., Foster G., Cahill N. Global temperature evolution: recent trends and some pitfalls. Environ. Res. Lett. May 2017;12(5) doi: 10.1088/1748-9326/aa6825. [DOI] [Google Scholar]
- 32.Fyfe J., Fox-Kemper B., Kopp R., Garner G. “Summary for policymakers of the working group I contribution to the IPCC sixth assessment report - data for figure SPM. 2021;8(v20210809) [Google Scholar]
- 33.Zhang H.-M., Huang B., Lawrimore J.H., Menne M.J., Smith T.M. 2019. NOAA Global Surface Temperature Dataset (NOAAGlobalTemp) [Google Scholar]
- 34.Morice C.P., et al. An updated assessment of near‐surface temperature change from 1850: the HadCRUT5 data set. J. Geophys. Res. Atmos. Feb. 2021;126(3) doi: 10.1029/2019JD032361. [DOI] [Google Scholar]
- 35.Tebaldi C., et al. Climate model projections from the scenario model Intercomparison project (ScenarioMIP) of CMIP6. Earth System Dynamics. Mar. 2021;12(1):253–293. doi: 10.5194/esd-12-253-2021. [DOI] [Google Scholar]
- 36.Gianotti R.L., Eltahir E.A.B. Regional climate modeling over the maritime continent. Part II: new parameterization for autoconversion of convective rainfall. J. Clim. Feb. 2014;27(4):1504–1523. doi: 10.1175/JCLI-D-13-00171.1. [DOI] [Google Scholar]
- 37.Gianotti R.L., Eltahir E.A.B. Regional climate modeling over the maritime continent. Part I: new parameterization for convective cloud fraction. J. Clim. Feb. 2014;27(4):1488–1503. doi: 10.1175/JCLI-D-13-00127.1. [DOI] [Google Scholar]
- 38.Im E.-S., Kang S., Eltahir E.A.B. Projections of rising heat stress over the western Maritime Continent from dynamically downscaled climate simulations. Global Planet. Change. Jun. 2018;165:160–172. doi: 10.1016/j.gloplacha.2018.02.014. [DOI] [Google Scholar]
- 39.Muñoz-Sabater J., et al. ERA5-Land: a state-of-the-art global reanalysis dataset for land applications. Earth Syst. Sci. Data. Sep. 2021;13(9):4349–4383. doi: 10.5194/essd-13-4349-2021. [DOI] [Google Scholar]
- 40.Karanisa T., Amato A., Richer R., Abdul Majid S., Skelhorn C., Sayadi S. Agricultural production in Qatar's hot arid climate. Sustainability. Apr. 2021;13(7):4059. doi: 10.3390/su13074059. [DOI] [Google Scholar]
- 41.Neira M., et al. Climate change and human health in the Eastern Mediterranean and Middle East: literature review, research priorities and policy suggestions. Environ. Res. Jan. 2023;216 doi: 10.1016/j.envres.2022.114537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dianati Tilaki R.A., Zazouli M.A., Ala A.R. Climate change and its consequences on human health: a review study. J. Adv. Environ. Health Res. Jan. 2021;9(1):1–6. doi: 10.32598/JAEHR.9.1.1188. [DOI] [Google Scholar]
- 43.Abrignani M.G., Lombardo A., Braschi A., Renda N., Abrignani V. Climatic influences on cardiovascular diseases. World J. Cardiol. Mar. 2022;14(3):152–169. doi: 10.4330/wjc.v14.i3.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Palinkas L.A., Wong M. Global climate change and mental health. Curr Opin Psychol. Apr. 2020;32:12–16. doi: 10.1016/j.copsyc.2019.06.023. [DOI] [PubMed] [Google Scholar]
- 45.Dupke S., et al. Impact of climate change on waterborne infections and intoxications. J. Health Monit. Jun. 2023;8(Suppl 3):62–77. doi: 10.25646/11402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Caminade C., McIntyre K.M., Jones A.E. Impact of recent and future climate change on vector‐borne diseases. Ann. N. Y. Acad. Sci. Jan. 2019;1436(1):157–173. doi: 10.1111/nyas.13950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anas M., Sami M.A., Siddiqui Z., Khatoon K., Zeyad M.T., Malik A. Microbiomes and the Global Climate Change. Springer Singapore; Singapore: 2021. Impact of climate change on the incidence and transfer of food- and water-borne diseases; pp. 123–144. [DOI] [Google Scholar]
- 48.Tahir F., et al. Assessing the impact of climate conditions on the distribution of mosquito species in Qatar. Front. Public Health. 2023;10(Jan) doi: 10.3389/fpubh.2022.970694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Eguiluz‐Gracia I., et al. The need for clean air: the way air pollution and climate change affect allergic rhinitis and asthma. Allergy. Sep. 2020;75(9):2170–2184. doi: 10.1111/all.14177. [DOI] [PubMed] [Google Scholar]
- 50.El-Sayed A., Kamel M. Climatic changes and their role in emergence and re-emergence of diseases. Environ. Sci. Pollut. Control Ser. Jun. 2020;27(18):22336–22352. doi: 10.1007/s11356-020-08896-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chowdhury F.R., et al. The association between temperature, rainfall and humidity with common climate-sensitive infectious diseases in Bangladesh. PLoS One. Jun. 2018;13(6) doi: 10.1371/journal.pone.0199579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.EL Bilali H., Henri Nestor Bassole I., Dambo L., Berjan S. Climate change and food security. J. Agric. For. Sep. 2020;66(3) doi: 10.17707/AgricultForest.66.3.16. [DOI] [Google Scholar]
- 53.Schmidt J.P., Park A.W., Kramer A.M., Han B.A., Alexander L.W., Drake J.M. Spatiotemporal fluctuations and triggers of ebola virus spillover. Emerg. Infect. Dis. Mar. 2017;23(3):415–422. doi: 10.3201/eid2303.160101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tong S., Ebi K. Preventing and mitigating health risks of climate change. Environ. Res. Jul. 2019;174:9–13. doi: 10.1016/j.envres.2019.04.012. [DOI] [PubMed] [Google Scholar]
- 55.Mora C., et al. Over half of known human pathogenic diseases can be aggravated by climate change. Nat. Clim. Change. Sep. 2022;12(9):869–875. doi: 10.1038/s41558-022-01426-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Khraishah H., et al. Climate change and cardiovascular disease: implications for global health. Nat. Rev. Cardiol. Dec. 2022;19(12):798–812. doi: 10.1038/s41569-022-00720-x. [DOI] [PubMed] [Google Scholar]
- 57.Campbell-Lendrum D., Prüss-Ustün A. Climate change, air pollution and noncommunicable diseases. Bull. World Health Organ. Feb. 2019;97(2):160–161. doi: 10.2471/BLT.18.224295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dvorak A.C., et al. Possible impacts of sea level rise on disease transmission and potential adaptation strategies, a review. J. Environ. Manag. Jul. 2018;217:951–968. doi: 10.1016/j.jenvman.2018.03.102. [DOI] [PubMed] [Google Scholar]
- 59.Noordzij M., van Diepen M., Caskey F.C., Jager K.J. Relative risk versus absolute risk: one cannot be interpreted without the other. Nephrol. Dial. Transplant. Apr. 2017;32(suppl_2):ii13–ii18. doi: 10.1093/ndt/gfw465. [DOI] [PubMed] [Google Scholar]
- 60.Emeto T.I., et al. Disparities in risks of malaria associated with climatic variability among women, children and elderly in the chittagong hill tracts of Bangladesh. Int. J. Environ. Res. Publ. Health. Dec. 2020;17(24):9469. doi: 10.3390/ijerph17249469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lim Y.-H., et al. Ambient temperature and hospital admissions for acute kidney injury: a time-series analysis. Sci. Total Environ. Mar. 2018;616–617:1134–1138. doi: 10.1016/j.scitotenv.2017.10.207. [DOI] [PubMed] [Google Scholar]
- 62.Planning and Statistics Authority, “Qatar Open Data Portal,” https://www.data.gov.qa/pages/default/.
- 63.Bener A., Dogan M., Ehlayel M.S., Shanks N.J., Sabbah A. The impact of air pollution on hospital admission for respiratory and cardiovascular diseases in an oil and gas-rich country. Eur Ann Allergy Clin Immunol. Jun. 2009;41(3):80–84. [PubMed] [Google Scholar]
- 64.Schaffner F., et al. Vectors and vector-borne diseases in Qatar: current status, key challenges and future prospects. J Eur Mosq Control Assoc. Nov. 2021;39(1):3–13. doi: 10.52004/JEMCA2021.x001. [DOI] [Google Scholar]
- 65.Farag E.A., et al. Dengue epidemiology in Qatar from 2013–2021: a retrospective study. Trop Med Infect Dis. Oct. 2022;7(11):329. doi: 10.3390/tropicalmed7110329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.MOPH . 2017. Qatar Health Report 2014-2016. [Google Scholar]
- 67.PHCC . Business health index & social protection health index; 2023. Annual Statistical Report. 2023. [Google Scholar]
- 68.IPCC . Jul. 2023. IPCC, 2023: Climate Change 2023: Synthesis Report. Contribution of Working Groups I, II and III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. IPCC, Geneva, Switzerland. [DOI] [Google Scholar]
- 69.Kuhn K.G., et al. Campylobacter infections expected to increase due to climate change in Northern Europe. Sci. Rep. Aug. 2020;10(1) doi: 10.1038/s41598-020-70593-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Choi Y., et al. Effects of weather factors on dengue fever incidence and implications for interventions in Cambodia. BMC Public Health. Dec. 2016;16(1):241. doi: 10.1186/s12889-016-2923-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lee H., Yoon H.-Y. Impact of ambient temperature on respiratory disease: a case-crossover study in Seoul. Respir. Res. Feb. 2024;25(1):73. doi: 10.1186/s12931-024-02699-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lubczyńska M.J., Christophi C.A., Lelieveld J. Heat-related cardiovascular mortality risk in Cyprus: a case-crossover study using a distributed lag non-linear model. Environ. Health. Dec. 2015;14(1):39. doi: 10.1186/s12940-015-0025-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Faurie C., Varghese B.M., Liu J., Bi P. Association between high temperature and heatwaves with heat-related illnesses: a systematic review and meta-analysis. Sci. Total Environ. Dec. 2022;852 doi: 10.1016/j.scitotenv.2022.158332. [DOI] [PubMed] [Google Scholar]
- 74.Cramer M.N., Gagnon D., Laitano O., Crandall C.G. Human temperature regulation under heat stress in health, disease, and injury. Physiol. Rev. Oct. 2022;102(4):1907–1989. doi: 10.1152/physrev.00047.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jacobsen A.P., et al. Climate change and the prevention of cardiovascular disease. Am J Prev Cardiol. Dec. 2022;12 doi: 10.1016/j.ajpc.2022.100391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chapman C.L., Johnson B.D., Parker M.D., Hostler D., Pryor R.R., Schlader Z. Kidney physiology and pathophysiology during heat stress and the modification by exercise, dehydration, heat acclimation and aging. Temperature (Austin) 2021;8(2):108–159. doi: 10.1080/23328940.2020.1826841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Roths M.S., Rudolph T.E., Freestone A., Baumgard L.H., Selsby J.T. PSIII-10 heat stress causes persistent multisystemic dysfunction. J. Anim. Sci. Apr. 2022;100(Supplement_2) doi: 10.1093/jas/skac064.315. 187–187. [DOI] [Google Scholar]
- 78.Spector J.T., Masuda Y.J., Wolff N.H., Calkins M., Seixas N. Heat exposure and occupational injuries: review of the literature and implications. Curr Environ Health Rep. Dec. 2019;6(4):286–296. doi: 10.1007/s40572-019-00250-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rony M.K.K., Alamgir H.M. High temperatures on mental health: recognizing the association and the need for proactive strategies—a perspective. Health Sci Rep. Dec. 2023;6(12) doi: 10.1002/hsr2.1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cantet J.M., Yu Z., Ríus A.G. Heat stress-mediated activation of immune-inflammatory pathways. Antibiotics (Basel) Oct. 2021;10(11) doi: 10.3390/antibiotics10111285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Williams M.L. Global warming, heat-related illnesses, and the dermatologist. Int J Womens Dermatol. Jan. 2021;7(1):70–84. doi: 10.1016/j.ijwd.2020.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Burkart K.G., et al. Estimating the cause-specific relative risks of non-optimal temperature on daily mortality: a two-part modelling approach applied to the Global Burden of Disease Study. Lancet. Aug. 2021;398(10301):685–697. doi: 10.1016/S0140-6736(21)01700-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sekiguchi Y., et al. Effects of heat acclimation following heat acclimatization on whole body heat exchange in trained endurance athletes. Int. J. Environ. Res. Publ. Health. May 2022;19(11):6412. doi: 10.3390/ijerph19116412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cramer M.N., Gagnon D., Laitano O., Crandall C.G. Human temperature regulation under heat stress in health, disease, and injury. Physiol. Rev. Oct. 2022;102(4):1907–1989. doi: 10.1152/physrev.00047.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sorensen C., Hess J. Treatment and prevention of heat-related illness. N. Engl. J. Med. Oct. 2022;387(15):1404–1413. doi: 10.1056/NEJMcp2210623. [DOI] [PubMed] [Google Scholar]
- 86.Yam Y.L.J. Body temperature and its regulation. Anaesth. Intensive Care Med. Aug. 2024;25(8):584–588. doi: 10.1016/j.mpaic.2024.06.014. [DOI] [Google Scholar]
- 87.Meade R.D., et al. Physiological factors characterizing heat-vulnerable older adults: a narrative review. Environ. Int. Nov. 2020;144 doi: 10.1016/j.envint.2020.105909. [DOI] [PubMed] [Google Scholar]
- 88.Adams W.M., Stearns R.L., Casa D.J. Exertional Heat Illness. Springer International Publishing; Cham: 2020. Exertional heat stroke; pp. 59–79. [DOI] [Google Scholar]
- 89.Leon L.R. Heat stroke and cytokines. Prog. Brain Res. 2007;162:481–524. doi: 10.1016/S0079-6123(06)62024-4. [DOI] [PubMed] [Google Scholar]
- 90.Wee J., et al. Effects of medications on heat loss capacity in chronic disease patients: health implications amidst global warming. Pharmacol. Rev. Nov. 2023;75(6):1140–1166. doi: 10.1124/pharmrev.122.000782. [DOI] [PubMed] [Google Scholar]
- 91.Kenny G.P., Notley S.R., Flouris A.D., Grundstein A. Exertional Heat Illness. Springer International Publishing; Cham: 2020. Climate change and heat exposure: impact on health in occupational and general populations; pp. 225–261. [DOI] [Google Scholar]
- 92.Shaw W.R., Catteruccia F. Vector biology meets disease control: using basic research to fight vector-borne diseases. Nat Microbiol. Aug. 2018;4(1):20–34. doi: 10.1038/s41564-018-0214-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bartlow A.W., et al. Forecasting zoonotic infectious disease response to climate change: mosquito vectors and a changing environment. Vet Sci. May 2019;6(2):40. doi: 10.3390/vetsci6020040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bin Ghouth A.S., Batarfi A.M., Melkat A.A., Elrahman S. Handbook of Healthcare in the Arab World. Springer International Publishing; Cham: 2021. Vector-borne diseases in Arab countries; pp. 1405–1420. [DOI] [Google Scholar]
- 95.Fazaludeen Koya S., Abdalla S.M., Kodama C., Keita M., Abubakar A. Vector-borne and zoonotic diseases in the eastern mediterranean region: a systematic review. J Epidemiol Glob Health. Feb. 2023;13(1):105–114. doi: 10.1007/s44197-023-00091-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Rawson T., Doohan P., Hauck K., Murray K.A., Ferguson N. Climate change and communicable diseases in the Gulf Cooperation Council (GCC) countries. Epidemics. Mar. 2023;42 doi: 10.1016/j.epidem.2023.100667. [DOI] [PubMed] [Google Scholar]
- 97.Beermann S., et al. Impact of climate change on vector- and rodent-borne infectious diseases. J. Health Monit. Jun. 2023;8(Suppl 3):33–61. doi: 10.25646/11401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Rocklöv J., Dubrow R. Climate change: an enduring challenge for vector-borne disease prevention and control. Nat. Immunol. May 2020;21(5):479–483. doi: 10.1038/s41590-020-0648-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.de Souza W.M., Weaver S.C. Effects of climate change and human activities on vector-borne diseases. Nat. Rev. Microbiol. Mar. 2024 doi: 10.1038/s41579-024-01026-0. [DOI] [PubMed] [Google Scholar]
- 100.Medlock J.M., Leach S.A. Effect of climate change on vector-borne disease risk in the UK. Lancet Infect. Dis. Jun. 2015;15(6):721–730. doi: 10.1016/S1473-3099(15)70091-5. [DOI] [PubMed] [Google Scholar]
- 101.Wu X., Lu Y., Zhou S., Chen L., Xu B. Impact of climate change on human infectious diseases: empirical evidence and human adaptation. Environ. Int. Jan. 2016;86:14–23. doi: 10.1016/j.envint.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 102.Lowe R., et al. Combined effects of hydrometeorological hazards and urbanisation on dengue risk in Brazil: a spatiotemporal modelling study. Lancet Planet. Health. Apr. 2021;5(4):e209–e219. doi: 10.1016/S2542-5196(20)30292-8. [DOI] [PubMed] [Google Scholar]
- 103.Tahir F., Dieng F.N., Al‐Ghamdi S.G. Sustainable Cities in a Changing Climate. Wiley; 2023. Building resilient health policies: incorporating climate change impacts for sustainable adaptation; pp. 251–262. [DOI] [Google Scholar]
- 104.Zain A., Sadarangani S.P., Shek L.P.-C., Vasoo S. Climate change and its impact on infectious diseases in Asia. Singap. Med. J. Apr. 2024;65(4):211–219. doi: 10.4103/singaporemedj.SMJ-2023-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cissé G. Food-borne and water-borne diseases under climate change in low- and middle-income countries: further efforts needed for reducing environmental health exposure risks. Acta Trop. Jun. 2019;194:181–188. doi: 10.1016/j.actatropica.2019.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Dhara V.R., Schramm P.J., Luber G. Climate change & infectious diseases in India: implications for health care providers. Indian J. Med. Res. Dec. 2013;138(6):847–852. [PMC free article] [PubMed] [Google Scholar]
- 107.Alcayna T., et al. Climate-sensitive disease outbreaks in the aftermath of extreme climatic events: a scoping review. One Earth. Apr. 2022;5(4):336–350. doi: 10.1016/j.oneear.2022.03.011. [DOI] [Google Scholar]
- 108.Walker J. The influence of climate change on waterborne disease and Legionella : a review. Perspect Public Health. Sep. 2018;138(5):282–286. doi: 10.1177/1757913918791198. [DOI] [PubMed] [Google Scholar]
- 109.Dietrich J., et al. Impact of climate change on foodborne infections and intoxications. J. Health Monit. Jun. 2023;8(Suppl 3):78–92. doi: 10.25646/11403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Semenza J.C., et al. Climate change impact assessment of food- and waterborne diseases. Crit. Rev. Environ. Sci. Technol. Apr. 2012;42(8):857–890. doi: 10.1080/10643389.2010.534706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Awad D.A., Masoud H.A., Hamad A. Climate changes and food-borne pathogens: the impact on human health and mitigation strategy. Clim. Change. Jun. 2024;177(6):92. doi: 10.1007/s10584-024-03748-9. [DOI] [Google Scholar]
- 112.Jung Y.-J., Khant N.A., Kim H., Namkoong S. Impact of climate change on waterborne diseases: directions towards sustainability. Water. Mar. 2023;15(7):1298. doi: 10.3390/w15071298. [DOI] [Google Scholar]
- 113.Bain R., et al. Global assessment of exposure to faecal contamination through drinking water based on a systematic review. Trop. Med. Int. Health. Aug. 2014;19(8):917–927. doi: 10.1111/tmi.12334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Shayo G.M., Elimbinzi E., Shao G.N., Fabian C. Severity of waterborne diseases in developing countries and the effectiveness of ceramic filters for improving water quality. Bull. Natl. Res. Cent. Jul. 2023;47(1):113. doi: 10.1186/s42269-023-01088-9. [DOI] [Google Scholar]
- 115.Wang X., Wang X., Cao J. Environmental factors associated with Cryptosporidium and Giardia. Pathogens. Mar. 2023;12(3):420. doi: 10.3390/pathogens12030420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Fenta L., Kebede A. Effect of climate change on food and water borne diseases outbreak: a mini review. Food Sci. Qual. Manag. 2019;88(Jul) doi: 10.7176/FSQM/88-02. [DOI] [Google Scholar]
- 117.Rose J.B., Daeschner S., Easterling D.R., Curriero F.C., Lele S., Patz J.A. Climate and waterborne disease outbreaks. J. AWWA (Am. Water Works Assoc.) Sep. 2000;92(9):77–87. doi: 10.1002/j.1551-8833.2000.tb09006.x. [DOI] [Google Scholar]
- 118.Andersen Z.J., Vicedo-Cabrera A.M., Hoffmann B., Melén E. Climate change and respiratory disease: clinical guidance for healthcare professionals. Breathe. Jun. 2023;19(2) doi: 10.1183/20734735.0222-2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Jacobson L. da S.V., de Oliveira B.F.A., Schneider R., Gasparrini A., Hacon S. de S. Mortality risk from respiratory diseases due to non-optimal temperature among Brazilian elderlies. Int. J. Environ. Res. Publ. Health. May 2021;18(11) doi: 10.3390/ijerph18115550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Achebak H., Rey G., Lloyd S.J., Quijal-Zamorano M., Méndez-Turrubiates R.F., Ballester J. Ambient temperature and risk of cardiovascular and respiratory adverse health outcomes: a nationwide cross-sectional study from Spain. Eur J Prev Cardiol. Feb. 2024 doi: 10.1093/eurjpc/zwae021. [DOI] [PubMed] [Google Scholar]
- 121.D'Amato G., et al. Climate change and air pollution: effects on pollen allergy and other allergic respiratory diseases. Allergo J Int. 2014;23(1):17–23. doi: 10.1007/s40629-014-0003-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Grigorieva E., Lukyanets A. Combined effect of hot weather and outdoor air pollution on respiratory health: literature review. Atmosphere. Jun. 2021;12(6):790. doi: 10.3390/atmos12060790. [DOI] [Google Scholar]
- 123.Tran H.M., et al. The impact of air pollution on respiratory diseases in an era of climate change: a review of the current evidence. Sci. Total Environ. Nov. 2023;898 doi: 10.1016/j.scitotenv.2023.166340. [DOI] [PubMed] [Google Scholar]
- 124.Cohen A.J., et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. May 2017;389(10082):1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ćurić M., Zafirovski O., Spiridonov V. Essentials of Medical Meteorology. Springer International Publishing; Cham: 2022. Air quality and health; pp. 143–182. [DOI] [Google Scholar]
- 126.Wang F., et al. Respiratory diseases are positively associated with PM2.5 concentrations in different areas of Taiwan. PLoS One. Apr. 2021;16(4) doi: 10.1371/journal.pone.0249694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Afzal S., Abdul Manap A.S., Attiq A., Albokhadaim I., Kandeel M., Alhojaily S.M. From imbalance to impairment: the central role of reactive oxygen species in oxidative stress-induced disorders and therapeutic exploration. Front. Pharmacol. Oct. 2023;14 doi: 10.3389/fphar.2023.1269581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kim S.-Y., Kim E., Kim W.J. Health effects of ozone on respiratory diseases. Tuberc. Respir. Dis. Dec. 2020;83(Supple 1):S6–S11. doi: 10.4046/trd.2020.0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wang Q., Liu S. The effects and pathogenesis of PM2.5 and its components on chronic obstructive pulmonary disease. Int. J. Chronic Obstr. Pulm. Dis. 2023;18:493–506. doi: 10.2147/COPD.S402122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Xing Y.-F., Xu Y.-H., Shi M.-H., Lian Y.-X. The impact of PM2.5 on the human respiratory system. J. Thorac. Dis. Jan. 2016;8(1):E69–E74. doi: 10.3978/j.issn.2072-1439.2016.01.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yang Z., et al. Health effects of long-term exposure to ambient PM2.5 in asia-pacific: a systematic review of cohort studies. Curr Environ Health Rep. Jun. 2022;9(2):130–151. doi: 10.1007/s40572-022-00344-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Capone P., Lancia A., D'Ovidio M.C. Interaction between air pollutants and pollen grains: effects on public and occupational health. Atmosphere. Oct. 2023;14(10):1544. doi: 10.3390/atmos14101544. [DOI] [Google Scholar]
- 133.Jacobs P.J., Oosthuizen M.K., Mitchell C., Blount J.D., Bennett N.C. Heat and dehydration induced oxidative damage and antioxidant defenses following incubator heat stress and a simulated heat wave in wild caught four-striped field mice Rhabdomys dilectus. PLoS One. Nov. 2020;15(11) doi: 10.1371/journal.pone.0242279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mirsaeidi M., Motahari H., Taghizadeh Khamesi M., Sharifi A., Campos M., Schraufnagel D.E. Climate change and respiratory infections. Ann Am Thorac Soc. Aug. 2016;13(8):1223–1230. doi: 10.1513/AnnalsATS.201511-729PS. [DOI] [PubMed] [Google Scholar]
- 135.Padhy S., Sarkar S., Panigrahi M., Paul S. Mental health effects of climate change. Indian J. Occup. Environ. Med. 2015;19(1):3. doi: 10.4103/0019-5278.156997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Walinski A., Sander J., Gerlinger G., Clemens V., Meyer-Lindenberg A., Heinz A. The effects of climate change on mental health. Dtsch Arztebl Int. Feb. 2023 doi: 10.3238/arztebl.m2022.0403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Albrecht G., et al. Solastalgia: the distress caused by environmental change. Australas. Psychiatry. Feb. 2007;15(1_suppl):S95–S98. doi: 10.1080/10398560701701288. [DOI] [PubMed] [Google Scholar]
- 138.de Jarnette J. Climate change psychological distress: an underdiagnosed cause of mental health disturbances. J. Am. Board Fam. Med. Jan. 2024;37(1):11–14. doi: 10.3122/jabfm.2023.230169R1. [DOI] [PubMed] [Google Scholar]
- 139.Clayton S. Climate change and mental health. Curr Environ Health Rep. Mar. 2021;8(1):1–6. doi: 10.1007/s40572-020-00303-3. [DOI] [PubMed] [Google Scholar]
- 140.Boscarino P.M.J.A., Hoffman D.S.N., Adams P.R.E., Figley P.C.R., Solhkhah M.R. Mental health outcomes among vulnerable residents after Hurricane Sandy: implications for disaster research and planning. Am J Disaster Med. Apr. 2014;9(2):97–106. doi: 10.5055/ajdm.2014.0147. [DOI] [PubMed] [Google Scholar]
- 141.Fernandez A., et al. Flooding and mental health: a systematic mapping review. PLoS One. Apr. 2015;10(4) doi: 10.1371/journal.pone.0119929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Carleton T.A. Crop-damaging temperatures increase suicide rates in India. Proc. Natl. Acad. Sci. USA. Aug. 2017;114(33):8746–8751. doi: 10.1073/pnas.1701354114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Cianconi P., Betrò S., Janiri L. The impact of climate change on mental health: a systematic descriptive review. Front. Psychiatr. 2020;11(Mar) doi: 10.3389/fpsyt.2020.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ramadan A.M.H., Ataallah A.G. Are climate change and mental health correlated? Gen Psychiatr. Nov. 2021;34(6) doi: 10.1136/gpsych-2021-100648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Torres J.M., Casey J.A. The centrality of social ties to climate migration and mental health. BMC Public Health. Dec. 2017;17(1):600. doi: 10.1186/s12889-017-4508-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Wigand M.E., Timmermann C., Scherp A., Becker T., Steger F. Climate change, pollution, deforestation, and mental health: research trends, gaps, and ethical considerations. Geohealth. Nov. 2022;6(11) doi: 10.1029/2022GH000632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Khan S.A., Al Rashid A., Koç M. Adaptive response for climate change challenges for small and vulnerable coastal area (SVCA) countries: Qatar perspective. Int. J. Disaster Risk Reduc. 2023;96 doi: 10.1016/j.ijdrr.2023.103969. Oct. [DOI] [Google Scholar]
- 148.Ajjur S.B., Al-Ghamdi S.G. Towards sustainable energy, water and food security in Qatar under climate change and anthropogenic stresses. Energy Rep. Jun. 2022;8:514–518. doi: 10.1016/j.egyr.2022.02.099. [DOI] [Google Scholar]
- 149.General Secretariat for Development Planning . Doha; 2008. Qatar National Vision 2030. [Google Scholar]
- 150.Lawler J., Mazzoni A., Shannak S. 2023. The Domestic Water Sector in Qatar; pp. 193–209. [DOI] [Google Scholar]
- 151.Al-Hababi R. 2023. The Evolvement of Qatar's Environmental Sustainability Policy: the Strategies, Regulations, and Institutions; pp. 17–35. [DOI] [Google Scholar]
- 152.Ministry of Municipality and Environment of the state of Qatar Nationally determined contribution (NDC) 2021. https://www.mme.gov.qa/pdocs/cview?siteID=2&docID=23348&year=2021
- 153.Labour and Social Affairs of the State of Qatar Heat stress legislation in Qatar. 2023. https://www.mol.gov.qa/admin/LawsDocuments/2020%20Heat%20Stress%20Guidance-r15.pdf Ministry of Administrative Development.
- 154.Qatar Ministry of Foreign Affairs, "Climate Change," Ministry of Foreign Affairs - Qatar, [Online]. Available: https://mofa.gov.qa/en/foreign-policy/international-cooperation/climate-change. [Accessed: Oct. 10, 2024].