Abstract
Background
While inactivity and sedentarism among adolescents are increasing globally, technology-based interventions incorporating wearable activity trackers (WATs) demonstrate the potential to combat the situation. With a focus on schools as critical environments in which to perform interventions among adolescents, this meta-analytic review of literature aimed to examine the effectiveness of wearable trackers in objectively measured physical activity (PA).
Methods
A systematic search was conducted across six databases—PubMed, CENTRAL, Scopus, SPORTDiscus, the Web of Science Core Collection, and PsycINFO—between January 2012 and March 2024. The language was restricted to English only. Both randomized controlled trials and quasi-experiment studies were included. Risk of bias was assessed using Cochrane RoB2 and ROBINS-I tools. Subgroup analyses and sensitivity analyses were performed. Effect direction for a narrative synthesis was also conducted. GRADE criteria were applied to assess quality of evidence.
Results
Fifteen studies were finally included in the literature review, and ten were adopted for meta-analysis. No statistical significance was found in intervention outcomes involving WATs’ effect on PA, whether in terms of total daily steps, moderate-to-vigorous PA (MVPA), or calorie counts. However, the subgroup analysis revealed that one study using research-grade assessment showed a substantial positive effect on steps. There were no data reported regarding the effect of objectively measured sedentary behavior.
Conclusion
Further study is needed to explore whether wearable activity trackers raise or decrease PA among adolescents in schools.
Registration
PROSPERO, registration number: CRD42023421008.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-025-22170-z.
Keywords: Adolescents, Wearable activity trackers, Physical activity, Schools
Background
Physical inactivity is a risk factor for adiposity, non-communicable diseases (e.g., type 2 diabetes, cardiovascular diseases), several types of cancer and premature mortality [1–3]. More than a quarter of the global population is insufficiently active and people live increasingly sedentary lifestyles [4, 5].
Adolescents, who account for a significant proportion (16%) of the global population [6], appear to show significant decline in PA levels [7, 8]. It is estimated that approximately 80% of adolescents (11–19 years of age) around the world fall short of meeting PA guidelines of moderate-to-vigorous PA (MVPA) of 60 min per day [9]. Health throughout adolescence is essential for adult health and the health of the next generation; developing an active lifestyle from an early age exhibits positive association with adults’ participation in and maintenance of PA [9–11]. Extensive evidence has found a positive association between increasing PA in youth populations and a range of physical and psychosocial outcomes, including academic performance [12–15]. Therefore, it is imperative to identify plausible interventions to change unhealthy behaviors in young people.
The school environment is of prime importance when it comes to enhancing adolescents’ health behaviors, given their greater involvement in school activities compared to family or community settings [16]. In addition, schools provide infrastructure as well as skilled personnel to support safe participation in diverse forms of PA [17, 18]. Children and adolescents may have come to face heavier study burdens due to global educational policy, and this might have contributed to the decline of PA in schools during the 2000s [19]. However, school-day MVPA has in more recent years shown an increase under health promotion policies, and there is potential for PA interventions to improve adolescent health within school settings [19].
Traditional PA interventions, such as education, counseling and adaptation of more active curricula, have been widely adopted, demonstrating some success in causing behavioral changes in adolescents [20, 21]. However, such interventions are often time consuming and challenging to implement on a large-scale basis with uniform standards. This fact underscores the potential of technology-based interventions which can be convenient and feasible to integrate into classrooms [22–24]. Wearable activity trackers (WATs), known as “fitness trackers” or “physical activity monitors,” have achieved wide interest and demonstrated growth in their market shares over the past two decades [25]. In this review, wearable trackers are defined as electronic devices worn on the body (wrist, hip, or waist) to provide information regarding PA and sedentary behaviors [26]. A survey conducted among participants from 21 countries, including 371 adolescents, showed that 33.4% of teenagers were currently using wearable devices, and 26.1% had previously used wearables [27]. Meanwhile, wearable devices with distinctive features have advanced rapidly (i.e., sensors, engineering and algorithms), providing real-time physiological data and functions that collect large amounts of data that allow for more precise analyses [27]. The literature reveals that researchers and practitioners are increasingly interested in using WATs to promote healthy behavior among adolescents [28], based in part on promising examples of PA promotion among adults using wearables [29, 30]. In particular, wearables can be utilized to create higher-quality PE classes to increase MVPA, more active lessons to reduce non-screen time, or be integrated into school activities to enhance engagement, all of which show numerous advantages for use in the school environment [23].
The integration of behavior change techniques (BCTs) is key to wearables’ success in improving PA behaviors. Such techniques were categorized by Michie et al. [31], who identified 93 items as standardized behavior change approaches. Specific BCTs, such as self-monitoring, show promising results in promoting PA among adolescents [32, 33]. Compared with traditional interventions, combining BCTs with wearables requires minimal expertise or guidance and may lead to behavior changes [34, 35].
A growing number of studies have explored the use of wearable devices to promote PA for children and adolescents. In particular, four systematic reviews have synthesized evidence concerning the likelihood that WATs support changes in health behaviors among adolescents [36–39]. Nevertheless, due to a lack of high-quality evidence and inconsistent results, most studies have been inconclusive on this topic, except for one study which has demonstrated positive effects of WATs in PA enhancement among adolescents [39]. These reviews synthesized interventions that were implemented in multiple settings (including schools and families), focused on a wide age span, and they included participants with different health statuses, leaving them with a lack of strictly comparable data [36, 38, 39]. In addition, only two reviews reported using intervention devices (mostly Fitbit) with insufficient information (i.e., specific mode and intervening time) for application [36, 38]. Finally, all of the reviews conducted their database searches before 2020, and the exponential increase in demand for wearables may have resulted in rapid advancements of these devices throughout the more recent years; this leaves a gap in meta-analytic research on the topic.
To date, no review has evaluated the use of WATs as an intervention tool in promoting PA among adolescents in exclusively school-based settings. This review aims to examine the effectiveness of interventions that use WATs to promote PA among adolescents in school-based settings. There are three research objectives:
Describe the types and characteristics of wearables used among adolescents in school-based settings
Evaluate the effects of using wearables to change adolescents’ PA behavior in school environments
Propose recommendations for schools aiming to change adolescents’ PA behavior via the implementation of wearables
Method
Protocol
The systematic review was conducted according to Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) [40], with a supplement of Synthesis Without Meta-analysis (SWiM) items for extended guidance in constructing a narrative review [41].
Data source and search strategy
The search was conducted in six databases: PubMed, CENTRAL, Scopus, SPORTDiscus, the Web of Science Core Collection, and PsycINFO. The search focused on articles published between January 2012 and March 2024. The earliest year was selected as 2012 following the rationale outlined by Böhm et al. [37], whereby consumer wearables entered the market with proven validity and reliability from that period. There were four concepts in the search terms: (1) children/adolescents; (2) wearable activity tracker; (3) intervention program, and (4) PA / sedentary behavior (SB). Specifically, we adopted the definition of adolescents from the World Health Organization (WHO) as being 10–19 years old. Moreover, school settings referred to primary and secondary education sectors, including middle schools. This review’s search terms were adapted from previous reviews [36, 37]. Terms belonging to the same conceptual category, and those found in a title/ abstract/ keyword, were combined using the Boolean operator OR; all four concepts were combined using the Boolean operator AND. Detailed examples of the search strategies are shown in Additional file 1: S1 for search strategy.
The reference lists of relevant articles were examined in search of additional studies relevant for inclusion in this review. This practice is recommended for systematic reviews aiming to minimize the probability of overlooking potentially related articles [42].
Inclusion and exclusion criteria
Inclusion and exclusion criteria are shown in Table 1. Only year of publication and language (English) were applied as restrictions to the search.
Table 1.
Inclusion/Exclusion criteria
| Inclusion criteria | Exclusion criteria | ||
|---|---|---|---|
| Types of study to be included |
•Any kind of experimental designs, including pre-experimental trials, quasi-experimental trials and true-experimental trials •Studies with full-text papers and published in a peer-reviewed academic journal |
Types of study to be excluded | •Review articles, such as qualitative reviews, systematic reviews, and meta-analyses |
| Participants |
•Children and/or adolescents reported with an average age above 10 and under 19 •Healthy participants •Participants who are overweight/obese |
Participants | •Non-human participants |
| Intervention |
•Studies that used a wearable device as a sole intervention tool, or that included wearables as one component of the whole intervention •Intervention program carried out in the school environment, whether it was applicated during school time or was an after-school program |
Intervention | •Studies that used wearable devices only to evaluate an intervention rather than to intervene in behaviors |
| Outcomes | •PA-related variables measured with objective tools (i.e., device-based measures such as pedometers and accelerometers), such as step counts, light-, moderate- and vigorous-intensity PA and energy expenditure | Outcomes | •Studies with obese or overweight participants only focused on weight control or loss without any PA/SB outcomes |
| Comparators |
•No intervention •Wait-list •Passive comparison group that does not involve wearing an activity tracker |
Types of literature to be excluded |
•Conference proceedings, book chapters, dissertations •Protocols without results |
Heterogeneity
Statistical heterogeneity of the calculated effect size (ES) was conducted using the I2 test in three categories: low heterogeneity (I2 < 20%), moderate heterogeneity (20% < I2 < 50%), and high heterogeneity (I2 > 50%) [43]. The methodological heterogeneity of the studies included was carefully considered (e.g., study type, bias control and methods of statistical analysis). Subgroup analysis was conducted to examine the influence of clinical heterogeneity, including: intervention duration (2 years vs an average of 5 weeks), use of intervention tools (pedometer vs Fitbit vs Misfit), intervention context (BCT vs no BCT), intervention mode (weekdays vs those including weekends), assessment method (research-grade vs non-research-grade measurement) and assessment time (≥ 7d vs < 7d).
Quality assessment
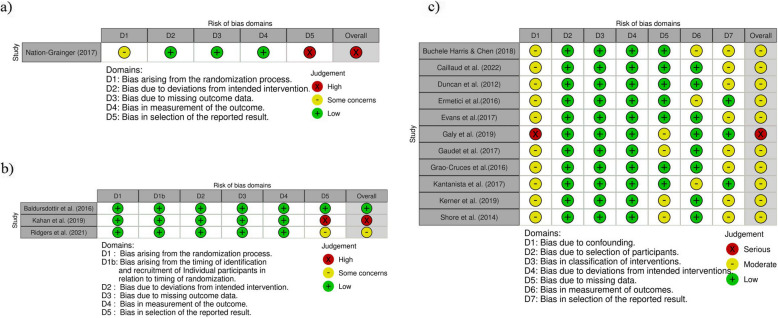
Two reviewers used assessment tools from the Cochrane Collaboration to assess the risk of bias. All disagreements were discussed with a third reviewer. For randomized controlled trials (RCTs), the tool was adapted from the revised tool for assessing risk of bias in randomized trials (RoB 2) [44]. The following domains were considered in individual RCTs: (1) random sequence generation, (2) incomplete outcome data, (3) measurement of outcomes, (4) selective reporting, (5) other bias (e.g., validity of outcome measures, sample size and baseline comparability of groups). Notably, allocation concealment and blinding (of participants and personnel) were disregarded as assessed domains because interventions with wearable trackers cannot be blinded. For cluster trials, an additional assessed domain was considered: bias due to the identification / recruitment of participants in clusters. There were three classifications for each domain in the adapted RoB 2: low risk, some concerns, and high risk [44]. For non-RCT experimental studies, the Risk of Bias in Non-randomized Studies – of Interventions (ROBINS-I) tool was employed [45]. Seven domains were considered for assessment: bias due to confounding, selection bias, bias in classification of intervention, bias due to deviation from intended interventions, attrition bias, bias in measurement of outcomes, and report bias. Each study was classified as critical, serious, moderate, or low under each domain.
The Grading of Recommendations, Assessment, Development and Evaluation approach (GRADE) was employed to assess the certainty of the evidence [46]. If sufficient publications were identified (n ≥ 10), the funnel-plot (visually asymmetry or not) with Egger’s regression test (p < 0.10 indicates the presence of publication bias) was conducted to test publication bias [47, 48].
Data extraction
The following details were extracted: study characteristics consisting of first author, country, year of publication, study design; demographic characteristics of participants: gender, age, sample size, overweight / obese; study design including wearable device type and amount of use, intervention mode and period, additional interventions, BCT use; outcomes such as step count, total PA, light-, moderate-, and vigorous PA, energy expenditure and sedentary time (ST), and assessment method; comparators; results of pre–post data, means and standard deviations of targeted outcomes, effect directions, and significant levels of pre–post differences or differences between groups.
The BCTs used in the intervention group were extracted by two reviewers according to the BCT taxonomy v1 [49]. Unreported or unclear information was obtained or clarified by contacting the authors; however, only two out of the eight replied [50, 51]. For studies with multiple outcomes, only results with data related to the targeted outcomes were extracted.
Data synthesis
For narrative synthesis, the included studies were grouped by study design, intervention, and outcomes. For the grouping by study design, RCTs, clustered-RCTs (CRCTs), and non-RCT experimental studies were analyzed separately. The grouping by intervention included multi-component interventions and sole wearable interventions, the separated analysis of targeted outcomes included total daily steps, MVPA and energy expenditure.
For continuous variables with different measurements, standardized mean difference (SMD) was selected as the effect estimate and calculated with the sample size of each group; mean and SD of PA outcomes from experiment groups and control groups [43]. We applied 95% confidence intervals (CI). Cohen’s d was chosen to represent the ES of SMD, and d < 0.20 was considered as trivial, 0.20–0.49 as small, 0.50–0.79 as moderate, and ≥ 0.80 as large [52]. All calculations were performed in Review Manager software (RevMan, 5.4.1, The Cochrane Collaboration, 2020) and Stata 17.
To avoid misrepresentation of the available evidence, and given the unavailability of a calculable SMD for all included studies, vote counting was adopted based on effect direction for additional synthesis [53].
Data presentation
Study characteristics and effect direction were summarized in tables. Quantitative syntheses (effect estimations of SMD) were visually displayed via forest plots and shown in the summary table. The results were presented in alphabetical order.
Results
Study selection
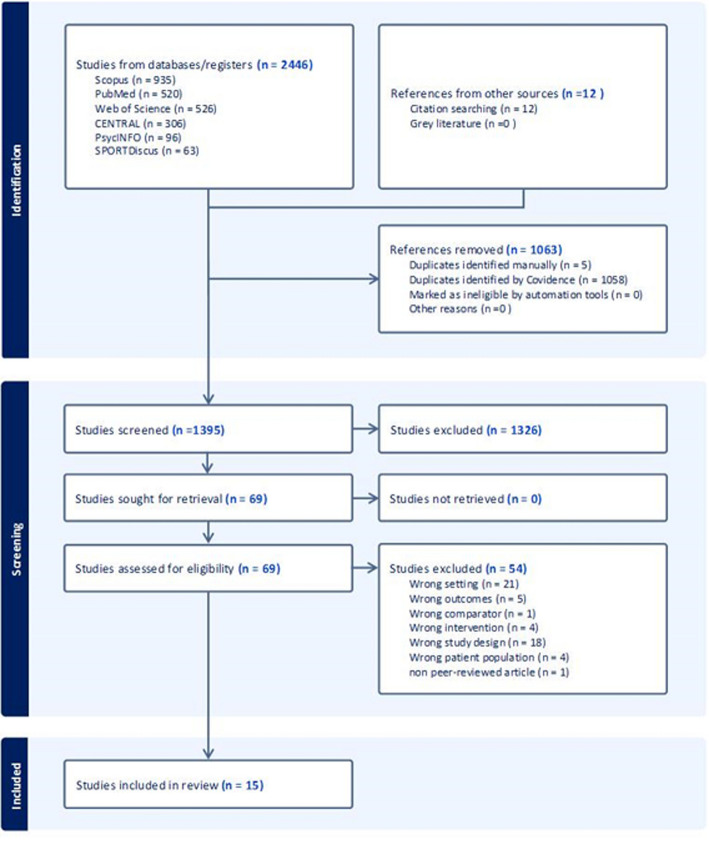
The systematic search process across databases yielded 2446 studies, and an additional 12 items were identified through citation searching. After the removal of 1063 duplicates, we screened 1395 studies’ titles and abstracts (resolving 20 conflicts); 69 remained for full-text screening. Finally, 15 studies were selected for inclusion after 13 conflicts were resolved. Characteristics of these 15 studies are shown in Table 2 [28, 50, 51, 54–65]. The flow of the study selection process is shown in Fig. 1: Flow of study selection from Covidence. Ten publications (n = 10) with 18 comparing groups (k = 18) were selected for ES calculation. All 15 included studies were synthesized with reference to effect direction.
Table 2.
Characteristics of included studies
| Study | Study design | Participant characteristics | Intervention characteristics | Comparator | Outcome | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of Participant | Age | Gender (female%) | OWe/Obesity | Wearable model | Worn site | Duration | Mode | BCT use | Additional component | Targeted outcome | Assessing methods | |||
| Baldursdottir et al. [54] (2016), Iceland | CRCTa |
CG:46(27) EG1:38(26) |
15 − 16 y |
CG: 65.4% EG1: 56% |
NRf |
Pedometer (NR) |
NR | 3 weeks | During weekday | YES | Diary | No PA intervention comparator | Steps |
CW-701 pedometer 3-day assessment |
| Buchele Harris & Chen [55] (2018), USA | QEb |
CG: 56(56) EG1: 31(31) EG2: 29(29) |
10–11 y | Total: 49.1% | Fitbit Charger + Heart Rate TM tracker | Wrist | 4 weeks | During school days | YES |
EG1: Extra activity |
No PA intervention vs Wearable + Extra activity vs Wearable | Steps; STg | NR | |
| Caillaud et al. [56] (2022), Australia | QE |
CG: 26(23) EG1: 57(41) |
CG: 10.4y EG: 10.9y |
CG: 61.5% EG1: 50.9% |
NR | Misfit Ray© activity tracker | Wrist | 5 weeks | During school days and weekends | YES |
Health education and behaviour change programme (iEngage) |
No PA intervention comparator | Steps, MVPA |
GENEActiv 3-day assessment |
| Duncan et al. [57] (2012), UK | Pre-Ec | EG1: 59(59) | 10.7 ± 0.4 y | 47.5% |
OW: 30.5% |
Pedometer (New Lifestyles, NL2000, Montana, USA) | Waist | 4 weeks | During school days | NO | Modified curriculum with PA education | Self-comparator | Steps | 5-day assessment |
| Ermetici et al. [58] (2016), Italy | Pre-E | EG1: 262(242) |
CG: 12.5(0.4)y EG: 12.5(0.4)y |
50% |
OW: 23.7% Obesity: 7.3% |
Pedometer (PE320-BL, Oregon Scientific Italia Srl) |
NR | 2 years | During school-year period | YES | Environmental changes; education | Self-comparator | Steps | 7-day assessment |
| Evans et al. [59] (2017), USA | QE |
CG: 10(10) EG1: 13(13) EG2: 19(19) |
12.3 + 0.34 y |
CG: 60% EG1: 31% EG2: 47% |
OW/ obese: CG: 60% EG1: 31% EG2: 42% |
Fitbit Charge | Wrist | 6 weeks | During intervened weeks |
YES (EG2) |
Educational sessions | No PA intervention vs Wearable vs Wearable + Sessions | MVPA; Steps |
Sensewear Armband Mini (SWA, Jawbone, San Francisco, CA) 7-day assessment |
| Galy et al. [60] (2019), Austrilia | Pre-E | EG1: 24(21) |
11.88 (0.57) |
NR | NR | Misfit Shine 2 | Wrist | 4 weeks | During intervened weeks | YES | Technology-Enabled Educational Program (iEngage) | Self-comparator | Steps |
GENEActiv 5-day assessment |
| Gaudet et al. [51] (2017), Canada | Pre-E (crossover) |
EG1: 23(16) EG2: 23(16) |
EG1: 13(0.3) EG2: 13(0.4) |
EG1: 52.2% EG2: 52.2% |
NR |
Fitbit model Charge HR; (FitBit Inc. San Francisco, USA) |
Wrist | 7 weeks | During intervened weeks | YES | NA | Self-comparator | Steps; MVPA; ST |
Actical accelerometers (Philips Respironics, Oregon, USA) 7-day assessment |
| Grao-Cruces et al. [61] (2016), Spain | Pre-E |
CG: 76(0) EG: 66(66) |
CG: 11.45 ± 0.5 EG: 11.29 ± 0.45 |
CG: 51.3% EG: 63.6% |
OW: CG: 27.6% EG: 33.3% |
Omron HJ-152-E2 pedometer (Omron, Hoofddorp, Netherlands) |
NR | 6 weeks | Weekdayand weekend | YES | Reinforced program | No PA intervention comparator | Steps | NR |
| Kahan & Lorenz [50] (2019), USA |
CRCT (crossover) |
EG1: 35(35) EG2: 46(50) EG3: 37(38) |
12.6 ± 1.0 y |
51.4% to 83.7% |
OW: 23.4% |
Yamax DigiWalker SW-200 pedometer |
Waist | 6 weeks | School day hours | YES | Workbook | Self-comparator | Steps | NR |
| Kantanista et al. [62] (2017), Poland | Pre-E |
EG1:26(26) EG21:28(28) EG22:28(28) |
EG1: 17.3 ± 0.89y EG2: 17.2 ± 0.94 y |
All female | NR | Yamax Digi-Walker SW 701 pedometer | NR | 7 weeks |
Every day |
YES (EG21& EG22) |
NA | Self-comparator | Steps |
Continuous Assessment |
| Kerner et al. [63] (2019), UK | Pre-E | EG1: 62(28) | 14–15y | EG1: 38.7% | NR | Fitbit Charge HR | Wrist | 5 weeks | Weekday and weekend | NO | NA | Self-comparator | MVPA |
ActiGraph GT9X triaxial accelerometer (ActiGraph, Pensacola, FL, USA) 7-day assessment |
| Nation-Grainger [64] (2017), United Arab Emirates | RCTd |
CG: 5(5) EG1: 5(5) |
14–15 y | All male | NR |
Galaxy Gear device |
Wrist | 6 weeks | PE class | YES | NA | No PA intervention comparator | Energy expenditure (calories) | NR |
| Ridgers et al. [28] (2021), Austrilia | CRCT |
CG: 131(130) EG1: 144(143) |
CG: 13.7(0.4) EG1: 13.8(0.4) |
CG: 56.4% EG1: 48.6% |
NR | Fitbit Flex | Wrist | 12 weeks | During intervened weeks | YES | Digital materials | Wait-list comparator | MVPA |
ActiGraph GT3X + accelerometer (Pensacola, FL, USA) 8-day assessment |
| Shore et al. [65] (2014), USA | QE |
CG: NR(46) EG1: NR(46) CG + EG1: 113(92) |
CG: 11.79(0.29) EG1: 11.91(0.37) |
CG: 54.3% EG1: 60.9% |
NR | New Lifestyle’s SW-401 DIGI-walker pedometer | Waist | 6 weeks | PE class on school days | YES | Enhanced curriculum | Regular PE activities vs Wearable + Enhanced curriculum | Steps | Continuous assessment |
aCluster randomized controlled trial
bQuasi-experimental studies
cPre-experiment
dRandomized controlled trial
eoverweight
fno report
gsedentary time
Fig. 1.
Flow of study selection from Covidence
Description of studies
The included studies were conducted in Europe (n = 6), North America (n = 5), Australia (n = 3), and Asia (n = 1). Regarding study type, there were four quasi-experimental studies, seven pre–post designed experimental studies, one RCT and three CRCTs. In total, 1303 unique participants (1006 = intervention; 297 = control) were included in samples ranging in size from 10 to 273. The mean ages of the control and intervention groups were 12.7 (± 1.67) years and 13.15 (± 2.15) years respectively. One study included only girls and one only boys; all the other studies included both boys and girls (except, in the case of one study, which did not provide a statement on gender). One third of the studies (n = 5) reported the proportion of participants who identified as overweight or obese; the rest did not report on this matter.
When it comes to the wearables used in these studies’ interventions, almost half (n = 7/15, 46.7%) used pedometers of various brands; one third (n = 5/15, 33.3%) used Fitbit activity wristbands, and the rest adopted other types including Galaxy Gear and Misfit. More than half (n = 8/15, 53.3%) were worn at wrist level; three were worn at waist level, and the remainder were unreported. While one study lasted for 2 years, the majority of interventions lasted less than 12 weeks (mean of the majority = 5.79 w) [58]. Days of device assessment to estimate PA levels varied greatly, from three to eight days. Regarding intervention mode, four studies performed their programs during weekdays, nine performed theirs during both weekdays and weekends, and two performed theirs in PE classes. Four studies targeted more than one outcome [51, 55, 56, 59]. The targeted ones included: total daily steps (12 studies), MVPA (5), ST (2), and energy expenditure (1).
Confidence in cumulative evidence
Results concerning the risk of bias in each domain are shown in Fig. 2: Risk of bias assessment results based on study type. Most of the studies were considered to carry moderate to high risk. One exception was rated as carrying a low risk of bias [54]. According to the funnel plot, most studies seem to be distributed symmetrically, except for one. However, the results of an Egger’s test (p = 0.606) indicate that there is no publication bias (see Additional file 2: S2 for funnel plot results). The overall evidence was considered low, and so was the evidence for each outcome based on the GRADE assessment (see Additional file 3: S3 for GRADE analysis).
Fig. 2.
Risk of bias assessment results based on study type. a risk of bias assessment result of the RCT study; b risk of bias assessment results of the CRCT studies; c risk of bias assessment results of non RCT studies (quasi-experimental studies and pre-post experimental studies without control group). Citation: McGuinness, LA, Higgins, JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Syn Meth. 2020; 1- 7. https://doi.org/10.1002/jrsm.1411
Meta-analysis
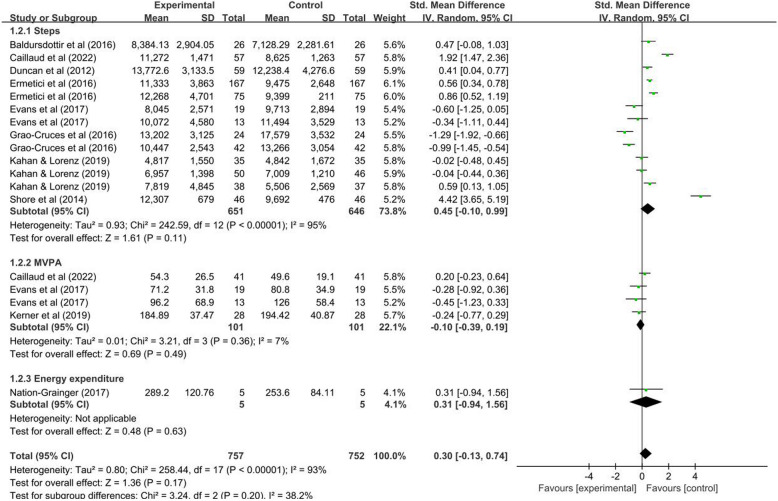
The individual studies’ ESs, based on outcomes, can be found in Fig. 3: Forest plots based on outcomes. Overall, no significant effect was found in PA improvement through the use of WATs among adolescents.
Fig. 3.
Forest plots based on outcomes
Total daily steps
No statistical significance was found in total daily steps before and after intervention (n = 8, k = 13; SMD = 0.45; 95% CI: –0.10 ~ 0.99; I2 = 95%, p = 0.000). To explain the high heterogeneity between studies and identify modifiable intervention factors, we formed six subgroups and conducted sensitivity analyses to assess the stability of the results (see Additional file 4: S4 for subgroup analyses). As all studies targeting steps as an outcome adopted multiple interventions (not using wearable trackers alone), subgroup analysis was not conducted for the grouping by multiple or solely wearable interventions. Each study implemented various intervention programs. Therefore, the context of programs was not included in the subgroup analysis.
In the subgroup analysis, studies that involved a two-year intervention showed a significant result (n = 1, k = 2; SMD = 0.68; CI: 0.39 ~ 0.97) [58], while studies with an average intervention duration of five weeks showed no significant differences (n = 8, k = 11; SMD = 0.40 CI: −0.33 ~ 1.14). There were no subgroup differences between the two groups with varied intervention durations (I2 = 0%, p = 0.49).
Studies utilizing intervention tools with a pedometer and Fitbit showed no statistical significance (n = 6, k = 10; SMD = 0.47; CI: −0.12 ~ 1.06; n = 1, k = 2; SMD = −0.49; CI: −0.99 ~ 0.01). However, one study using Misfit showed a significant positive effect (SMD = 1.92; CI: 1.47 ~ 2.36) [56]. Nevertheless, the results of the three groups adopting different tools suggested a subgroup difference (I2 = 96.1%, p = 0.000).
Studies that applied non–research-grade assessment showed no statistical significance (n = 7, k = 12; SMD = 0.32; CI: –0.22 ~ 0.86; I2 = 94%, p = 0.000) while the same one study, using research-grade assessment [56], showed a substantial positive effect on steps (SMD = 1.92; CI: 1.47 ~ 2.36). Significant subgroup difference was also indicated (I2 = 95%, p = 0.000).
MVPA
The ESs of studies that targeted MVPA demonstrated no statistical significance in effectiveness (n = 3, k = 4; SMD = –0.10; CI: –0.39 ~ 0.19; I2 = 7%, p = 0.36; see Additional file 4). Statistical heterogeneity was quite low although there were diverse clinical characteristics (i.e., multi-intervention, intervention assessment and duration) among the studies.
Energy expenditure
The one study that targeted energy expenditure [64] demonstrated no statistical significance (SMD = 0.31; CI: –0.94 ~ 1.56; see Additional file 4).
Narrative synthesis
Effects based on outcomes
For studies that targeted total daily steps (n = 12), half (n = 6) showed positive effects, while three contained conflicting results. The remaining studies did not report data on step counts. Regarding MVPA (n = 5), among four non-RCTs, half reported positive effects and half reported negative effects. Another CRCT [28] targeting MVPA indicated positive results. Only one study assessed energy expenditure, which showed a positive effect [65]. No statistics provided information concerning ST. Wearable tools chosen by most of the included studies in the current review (7/15 used pedometers) cannot provide data on ST. Detailed results regarding the direction of effects are shown in Additional file 5: S5 for effect direction results.
Effects based on BCT use
Most of the selected studies employed two (5/15, 33.3%) or three BCTs (5/15, 33.3%; see Additional file 5: S5 with extracted BCTs). The most frequently used BCTs were self-monitoring (n = 9/15) and goal-setting (n = 8/15). More positive effects (6/9, 66.7%) were found in studies using self-monitoring, and half (4/8, 50%) of studies using goal-setting showed positive results. Two studies adopted only one BCT (prompts / biofeedback); both showed positive effects. In studies where no BCT was used (n = 2), mixed results were found (one positive and one negative).
Discussion
Primary findings
Overall, current evidence did not demonstrate that using WATs in an intervention could improve or impede PA among adolescents in school-based settings. Nevertheless, including valid measurement tools and longer intervention durations might achieve more positive outcomes.
Comparison to previous reviews on included studies
In addition to the studies that were included in the four previously published systematic reviews on this topic, three studies were included as new evidence in this review [28, 50, 56]. In two of these three studies [28, 56], the year of publication was the reason for their omission from the previous reviews, whose searches were conducted before 2020. However, in the third case [50], the omission may have been due to the reviewers’ unique understanding regarding wearables as an intervention. This study did not report wearables as an intervention. However, the research group provided participants with unsealed pedometers (which could be viewed as an active intervention) [50]. Therefore, it was included in the current review.
Effects of wearables
One meta-analysis demonstrated moderate effects for wearables in increasing PA among school-aged children [39]. This review, however, focused on adolescents in school settings, could not provide evidence on PA (including steps, MVPA, or energy expenditure).
Clinical heterogeneity among studies makes comparisons questionable. We found that 10/10 studies included in our meta-analysis, and 11/15 of all included studies, used multiple interventions rather than solely wearables. Other interventions included additional PE sessions and materials. Diversity among additional sessions might have impeded the exploration of effectiveness of wearables on their own.
Moreover, the use of different BCT strategies makes it challenging to tell whether BCT use could add an additional effect, or to determine which elements were most effective. The most frequently used BCTs were goal-setting and self-monitoring, consistent with previous reviews [38, 39]. Although BCTs were recommended in PA behavior change [66], and clear specifications as well as realistic implications are essential [49], the use of BCTs was not clearly stated in most of the included studies.
In addition, assessment of PA behaviors during less than 7 days might not provide sufficient valid data to meet the required length of wear time for data analysis (≥ 10 h/d) [67], and this question of validity might affect outcome measures. However, because there were no statistical subgroup differences between groups (≥ 7d and < 7d) in the current review, the question requires further exploration.
One study [56] with research-grade assessment showed a large ES in terms of increasing step counts, which highlights the necessity of using valid measurement tools, although high heterogeneity in subgroups indicates caution regarding practical application based on the result. However, most studies (11/15) used non–research-grade devices, which may have provided invalid PA data and increased the probability of producing incomparable data [25].
It is a bit surprising that there was no significant effect on MVPA, which showed an increase in other reviews [38, 39]. The reason, based on the subgroup analysis of the steps mentioned above, might be due to an insufficient intervention duration of no more than 7 weeks. Only one study targeting energy expenditure showed no significance, possibly due to its high risk of bias [64].
It should also be noted that all studies targeting MVPA chose upgraded measurement tools such as accelerometers, and half of the studies targeting steps used pedometers. Pedometers showed validity when participants walked at a brisk (rather than slow) pace; meanwhile, step counts using pedometers might be influenced by adiposity and stature [68, 69]. Therefore, wearable devices should be chosen to measure suitable physical activities for adolescents. Notably, studies involving participants who did not achieve the guideline of 60 min/d MVPA [70] at baseline showed positive results (negative results in studies with active participants); this may be attributed to the fact that adolescents with lower PA levels might benefit more from PA interventions [71].
Influences of participants
Compared to children, adolescents experience more life changes (such as puberty) and environmental changes (such as rising workloads at school) [72]. They also tend to be less active [73]. The current review cannot make a conclusion for PA enhancement among adolescents, but the effectiveness of mHealth (such as gamified apps and wearable interventions) to improve insufficient PA has been synthesized [74]. The synthesis found that adolescent groups can benefit from mHealth and gain more compared to younger groups. Notably, the synthesis article [74] included adolescents with different health statuses (such as cancer survivors), so the result should be interpreted with caution when considering healthy groups only.
Among the five studies reporting on the proportion of overweight and obese participants, only one stated the intervention effects on healthy and participants separately from those who were overweight or obese; there was a positive intervention effect on PA changes for overweight and obese participants [58]. This is consistent with what was found in another study, whereby wearables were found to be effective in the prevention and treatment of obesity in adolescents by increasing PA [75]. Still, unreported proportions of overweight and obese participants of the included studies may confound the overall results of this review.
Influences of intervention approaches
In adults, interventions with multiple components integrating wearables proved more effective in PA behavior change than wearables alone, but the result was not shown among adolescents due to a lack of plausible and consistent evidence [29]. Interestingly, results from effect direction analysis showed that interventions applied during weekdays or school days, and during PE classes, all showed promising results while those applied on both weekdays and weekends did not. The results may be attributable to the familiar environment and the involvement of teachers in intra-curriculum activities [76]. Alternatively, these results may be due to incomparability of students’ PA status on weekdays and weekends [71]. Longer-term interventions (≥ 12 weeks) appear to be more effective in promoting and maintaining PA levels among adolescents [77]. In the current review, results also showed that long-term intervention programs (i.e., 2 years) increase step counts compared to short-term interventions (i.e., an average of 5 weeks). This indicates the importance of intervention duration in evoking behavioral change. When comparing intervention tools in our subgroup analysis, the most commonly used devices (i.e., pedometers and Fitbit) were inferior to Misfit for increasing step counts. However, this seems not to be associated with validation as Fitbit was demonstrated to be a valid measurement tool for counting steps [78]. Exploring the specific use of different devices used in interventions might help identify effective tools. One study reported that wrist-level wearables might be more effective than those worn at waist levels [39]; however, mixed results in the current review did not allow for a conclusion.
Influences of outcome measurement
All aforementioned review studies except one [39] included data from self-reports of PA. This may have given rise to indeterminate results, as self-reports may not be reliable for measuring PA among adolescents [79]; self-reports and device-based measures of PA should be compared cautiously [80, 81]. All studies included in the current review adopted device-based measurement, but validity and diverse characteristics across devices made comparison difficult.
Strengths and limitations
The greatest merit of this review is that it adopted both a meta-analysis and an evidence-based method of narrative synthesis (following Synthesis Without Meta-analysis guidelines) instead of relying on unstructured textual description. This approach has ensured a thorough analysis of current evidence in a rigorous literature review.
The limitations of this review should be noted. First, graph data from two studies were not extracted by ourselves for meta-analysis considering the inaccuracy of extraction by software; additionally, the primary numerical data were unobtainable from the authors. This might have led to biased conclusions due to the omission of data. Furthermore, the limited number of high-quality studies (such as RCT studies), combined with small sample sizes (< 10) in experimental studies might not have provided optimal evidence [82]. Nevertheless, after removing the study with the smallest sample size [64], the overall results of our meta-analysis remained unchanged. Third, a lack of data from non-English language studies might affect the overall results, as physical activity in regions such as Asia and Latin America might differ [5]. In addition, the lack of standardized intervention duration might also affect the overall results, as indicated in the analysis of MVPA. Finally, the lack of uniform information (i.e., BMI or socioeconomic status) might restrict generalization to such populations or regions.
Implications for future research
Future research requires increasingly well-designed studies (preferably RCTs) to generate more robust evidence regarding the effect of wearables among adolescents. To provide comparable results, the adoption of research-grade tools for outcome measures, or of validated wearable devices for proper activity among adolescents, should be considered. Furthermore, existing research has predominantly emphasized educational interventions and adapted physical activity programs. Nevertheless, future research should prioritize empirically validated strategies for integrating WATs into school-based interventions. Specifically, systematic integration of pedagogical approaches, such as physically active breaks and movement-based lessons, could be explored alongside personalized feedback mechanisms tailored to students’ developmental stages. It should be noted that it might be difficult to implement WATs in low socioeconomic populations. Therefore, researchers should adopt PA interventions that are suitable for different regions. Finally, research could include regions such as Latin America and Asia to form a global perspective.
Conclusion
This systematic review and meta-analysis did not find evidence that WATs increase objectively measured PA among healthy adolescents in school-based settings. However, our results found that total daily steps did increase when validated measurement tools were chosen or longer-term interventions were adopted. Nevertheless, the generalization of the results needs caution as the current evidence is of low quality. Future studies could be conducted on populations in other geographical regions, in addition to studying WATs integrated with specific strategies to adapt to the school environment.
Supplementary Information
Additional file 1. Search strategy. Provide detailed search strategies for each database, including specific terms and Boolean operations.
Additional file 2. Funnel plot of the included studies for meta-analysis based on outcomes. Demonstrate the result of publication bias of all included studies.
Additional file 3. Certainty of the evidence assessment based on outcomes. Demonstrate GRADE evaluation and reasons in each domain for the overall quality of evidence.
Additional file 4. Meta-analysis of effect of WATs based on outcomes. Demonstrate results, including effect sizes, confidence intervals, and P values of meta-analysis from each outcome (Steps, MVPA, ST, and calories) and subgroup analysis of outcome steps.
Additional file 5. Synthesis table for effect direction based on outcomes and BCT used in studies. Demonstrate results of effect direction and specific behavior change techniques used for all included studies.
Acknowledgements
We acknowledge TopEdit LLC for the linguistic editing and proofreading during the preparation of this manuscript.
Abbreviations
- WATs
Wearable activity trackers
- PA
Physical activity
- SB
Sedentary behavior
- MVPA
Moderate-to-Vigorous PA
- ST
Sedentary time
- WHO
World Health Organization
- BCTs
Behavior Change Techniques
- SMD
Standardized Mean Difference
- CI
Confidence Intervals
- ES
Effect Size
- RCT
Randomized Controlled Trials
- PRISMA
Preferred Reporting Items for Systematic reviews and Meta-Analyses
- RoB 2
the Risk of Bias 2
- ROBINS-I
the Risk of Bias in Non-randomized Studies-of Interventions
- GRADE
The Grading of Recommendations, Assessment, Development and Evaluation approach
Authors' contributions
XYC, FYW and HQZ contributed to the conception and design of the review and meta-analysis; XYC, HQZ and FYW performed the initial search of the databases; XYC and HQZ selected the eligible studies with disagreement resolved by FYW. XYC and FYW performed data screening and extraction. XYC and YL assessed the RoB of the included studies; XYC and HQZ conducted the GRADE assessment; XYC and SJZ extracted behavior change techniques (BCT) according to the BCT taxonomy v1; XYC, FYW and HQZ performed the statistical analyses; XYC, YL and SJZ drafted the manuscript. All authors contributed to the interpretation of the data, provided critical revisions to the intellectual content of the article, read, and approved the final manuscript. YHY completed the final proof of the manuscript and took primary responsibility for communication with the journal during the whole process for publication as the corresponding author.
Funding
Open access funding provided by Sichuan Province Science and Technology Support Program. This work was supported by Sichuan Province Science and Technology Support Program (2024NSFSC0539).
Data availability
All data is provided within the manuscript or supplementary information files.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Carrasquilla GD, García-Ureña M, Fall T, Sørensen TI, Kilpeläinen TO. Mendelian randomization suggests a bidirectional, causal relationship between physical inactivity and adiposity. Elife. 2022;11:e70386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hermelink R, Leitzmann MF, Markozannes G, Tsilidis K, Pukrop T, Berger F, et al. Sedentary behavior and cancer–an umbrella review and meta-analysis. Eur J Epidemiol. 2022;37:447–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ekelund U, Tarp J, Steene-Johannessen J, Hansen BH, Jefferis B, Fagerland MW, et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis. BMJ. 2019;366:l4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fang H, Jing Y, Chen J, Wu Y, Wan Y. Recent trends in sedentary time: a systematic literature review. Healthcare. 2021;9:969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. 2018;6:e1077–86. [DOI] [PubMed] [Google Scholar]
- 6.United Nations Population Fund. World population dashboard. 2022. https://www.unfpa.org/data/world-population-dashboard.
- 7.Schwarzfischer P, Gruszfeld D, Stolarczyk A, Ferre N, Escribano J, Rousseaux D, et al. Physical activity and sedentary behavior from 6 to 11 years. Pediatrics. 2019;143:e20180994. [DOI] [PubMed] [Google Scholar]
- 8.Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc Health. 2020;4:23–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Sluijs EMF, Ekelund U, Crochemore-Silva I, Guthold R, Ha A, Lubans D, et al. Physical activity behaviours in adolescence: current evidence and opportunities for intervention. Lancet. 2021;398:429–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Batista MB, Romanzini CLP, Barbosa CCL, Blasquez Shigaki G, Romanzini M, Ronque ERV. Participation in sports in childhood and adolescence and physical activity in adulthood: a systematic review. J Sports Sci. 2019;37:2253–62. [DOI] [PubMed] [Google Scholar]
- 11.Telama R, Yang X, Leskinen E, Kankaanpää A, Hirvensalo M, Tammelin T, et al. Tracking of physical activity from early childhood through youth into adulthood. Med Sci Sports Exerc. 2014;46:955–62. [DOI] [PubMed] [Google Scholar]
- 12.Biddle SJH, Ciaccioni S, Thomas G, Vergeer I. Physical activity and mental health in children and adolescents: an updated review of reviews and an analysis of causality. Psychol Sport Exerc. 2019;42:146–55. [Google Scholar]
- 13.Hale GE, Colquhoun L, Lancastle D, Lewis N, Tyson PJ. Review: physical activity interventions for the mental health and well-being of adolescents – a systematic review. Child Adolesc Ment Health. 2021;26:357–68. [DOI] [PubMed] [Google Scholar]
- 14.Guimarães JP, Fuentes-García JP, González-Silva J, Martínez-Patiño MJ. Physical activity, body image, and its relationship with academic performance in adolescents. Healthcare. 2023;11:602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen Z, Zhu L. Dose–response relationship between physical activity and cardiometabolic risk in obese children and adolescents: a pre-post quasi-experimental study. Front Physiol. 2023;14:1070653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neil-Sztramko SE, Caldwell H, Dobbins M. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst Rev. 2021;2021:CD007651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morton KL, Atkin AJ, Corder K, Suhrcke M, van Sluijs EMF. The school environment and adolescent physical activity and sedentary behaviour: a mixed-studies systematic review. Obes Rev. 2016;17:142–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kriemler S, Meyer U, Martin E, van Sluijs EMF, Andersen LB, Martin BW. Effect of school-based interventions on physical activity and fitness in children and adolescents: a review of reviews and systematic update. Br J Sports Med. 2011;45:923–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weaver RG, Tassitano RM, Tenório MCM, Brazendale K, Beets MW. Temporal trends in children’s school day moderate to vigorous physical activity: a systematic review and meta-regression analysis. J Phys Act Health. 2021;18:1446–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mannocci A, D’Egidio V, Backhaus I, Federici A, Sinopoli A, Ramirez Varela A, et al. Are there effective interventions to increase physical activity in children and young people? An umbrella review. Int J Environ Res Public Health. 2020;17:3528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moeini B, Rezapur-Shahkolai F, Bashirian S, Doosti-Irani A, Afshari M, Geravandi A. Effect of interventions based on regular physical activity on weight management in adolescents: a systematic review and a meta-analysis. Syst Rev. 2021;10:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu CC, Huang CW, Wang YC, Islam MdM, Kung WM, Weng YC, et al. mHealth research for weight loss, physical activity, and sedentary behavior: bibliometric analysis. J Med Internet Res. 2022;24:e35747. [DOI] [PMC free article] [PubMed]
- 23.Messing S, Rütten A, Abu-Omar K, Ungerer-Röhrich U, Goodwin L, Burlacu I, et al. How can physical activity be promoted among children and adolescents? A systematic review of reviews across settings. Front Public Health. 2019;7:341383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schipperijn J, Madsen CD, Toftager M, Johansen DN, Lousen I, Amholt TT, et al. The role of playgrounds in promoting children’s health – a scoping review. Int J Behav Nutr Phys Act. 2024;21:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strath SJ, Rowley TW. Wearables for promoting physical activity. Clin Chem. 2018;64:53–63. [DOI] [PubMed] [Google Scholar]
- 26.Strain T, Wijndaele K, Pearce M, Brage S. Considerations for the use of consumer-grade wearables and smartphones in population surveillance of physical activity. J Meas Phys Behav. 2022;5:8–14. [Google Scholar]
- 27.Shei RJ, Holder IG, Oumsang AS, Paris BA, Paris HL. Wearable activity trackers–advanced technology or advanced marketing? Eur J Appl Physiol. 2022;122:1975–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ridgers ND, Timperio A, Ball K, Lai SK, Brown H, Macfarlane S, et al. Effect of commercial wearables and digital behaviour change resources on the physical activity of adolescents attending schools in socio-economically disadvantaged areas: the RAW-PA cluster-randomised controlled trial. Int J Behav Nutr Phys Act. 2021;18:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brickwood K-J, Watson G, O’Brien J, Williams AD. Consumer-based wearable activity trackers increase physical activity participation: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2019;7:e11819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laranjo L, Ding D, Heleno B, Kocaballi B, Quiroz JC, Tong HL, et al. Do smartphone applications and activity trackers increase physical activity in adults? Systematic review, meta-analysis and metaregression. Br J Sports Med. 2021;55:422–32. [DOI] [PubMed] [Google Scholar]
- 31.Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health. 2011;26:1479–98. [DOI] [PubMed] [Google Scholar]
- 32.Allcott-Watson H, Chater A, Troop N, Howlett N. A systematic review of interventions targeting physical activity and/or healthy eating behaviours in adolescents: practice and training. Health Psychol Rev. 2024;18:117–40. [DOI] [PubMed] [Google Scholar]
- 33.Murray JM, Brennan SF, French DP, Patterson CC, Kee F, Hunter RF. Effectiveness of physical activity interventions in achieving behaviour change maintenance in young and middle aged adults: a systematic review and meta-analysis. Soc Sci Med. 2017;192:125–33. [DOI] [PubMed] [Google Scholar]
- 34.Düking P, Tafler M, Wallmann-Sperlich B, Sperlich B, Kleih S. Behavior change techniques in wrist-worn wearables to promote physical activity: content analysis. JMIR Mhealth Uhealth. 2020;8:e20820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lyons EJ, Lewis ZH, Mayrsohn BG, Rowland JL. Behavior change techniques implemented in electronic lifestyle activity monitors: a systematic content analysis. J Med Internet Res. 2014;16:e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ridgers ND, McNarry MA, Mackintosh KA. Feasibility and effectiveness of using wearable activity trackers in youth: a systematic review. JMIR Mhealth Uhealth. 2016;4:e129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Böhm B, Karwiese SD, Böhm H, Oberhoffer R. Effects of mobile health including wearable activity trackers to increase physical activity outcomes among healthy children and adolescents: systematic review. JMIR Mhealth Uhealth. 2019;7:e8298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Creaser AV, Clemes SA, Costa S, Hall J, Ridgers ND, Barber SE, et al. The acceptability, feasibility, and effectiveness of wearable activity trackers for increasing physical activity in children and adolescents: a systematic review. Int J Environ Res Public Health. 2021;18:6211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Casado-Robles C, Viciana J, Guijarro-Romero S, Mayorga-Vega D. Effects of consumer-wearable activity tracker-based programs on objectively measured daily physical activity and sedentary behavior among school-aged children: a systematic review and meta-analysis. Sports Med Open. 2022;8:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;2021:n71. [DOI] [PMC free article] [PubMed]
- 41.Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368:l6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Horsley T, Dingwall O, Sampson M. Checking reference lists to find additional studies for systematic reviews. Cochrane Database Syst Rev. 2011;8:2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane handbook for systematic reviews of interventions version 6.4 (updated August 2023). 2023. Available from www.training.cochrane.org/handbook.
- 44.Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 45.Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–94. [DOI] [PubMed]
- 47.Sterne JAC, Sutton AJ, Ioannidis JPA, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343 jul22 1:d4002–d4002. [DOI] [PubMed]
- 48.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46:81–95. [DOI] [PubMed] [Google Scholar]
- 50.Kahan D, Lorenz KA. Physical activity for lent: changes in and associations between religiosity, enjoyment, motivation, and physical activity. Res Q Exerc Sport. 2019;90:507–16. [DOI] [PubMed] [Google Scholar]
- 51.Gaudet J, Gallant F, Bélanger M. A bit of fit: minimalist intervention in adolescents based on a physical activity tracker. JMIR Mhealth Uhealth. 2017;5:e92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cohen J. A power primer. Psychol Bull. 1992;112:155–9. [DOI] [PubMed] [Google Scholar]
- 53.Thomson HJ, Thomas S. The effect direction plot: visual display of non-standardised effects across multiple outcome domains. Res Synth Methods. 2013;4:95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baldursdottir B, Taehtinen RE, Sigfusdottir ID, Krettek A, Valdimarsdottir HB. Impact of a physical activity intervention on adolescents’ subjective sleep quality: a pilot study. Glob Health Promot. 2017;24:14–22. [DOI] [PubMed] [Google Scholar]
- 55.Buchele Harris H, Chen W. Technology-enhanced classroom activity breaks impacting children’s physical activity and fitness. J Clin Med. 2018;7:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Caillaud C, Ledger S, Diaz C, Clerc G, Galy O, Yacef K. iEngage: a digital health education program designed to enhance physical activity in young adolescents. PLoS ONE. 2022;17:e0274644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Duncan M, Birch S, Woodfield L. Efficacy of an integrated school curriculum pedometer intervention to enhance physical activity and to reduce weight status in children. Eur Phy Educ Rev. 2012;18:396–407. [Google Scholar]
- 58.Ermetici F, Zelaschi RF, Briganti S, Dozio E, Gaeta M, Ambrogi F, et al. Association between a school-based intervention and adiposity outcomes in adolescents: the Italian “EAT” project. Obesity. 2016;24:687–95. [DOI] [PubMed] [Google Scholar]
- 59.Evans EW, Abrantes AM, Chen E, Jelalian E. Using novel technology within a school-based setting to increase physical activity: a pilot study in school-age children from a low-income. Urban Community Biomed Res Int. 2017;2017:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Galy O, Yacef K, Caillaud C. Improving pacific adolescents’ physical activity toward international recommendations: exploratory study of a digital education app coupled with activity trackers. JMIR Mhealth Uhealth. 2019;7:e14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Grao-Cruces A, Ruiz-López R, Moral-García J-E, Ruiz-Ariza A, Martínez-López EJ. Effects of a steps/day programme with evaluation in physical education on body mass index in schoolchildren 11–12 years of age. Kinesiology. 2016;48:132–41. [Google Scholar]
- 62.Kantanista A, Bronikowski M, Laudańska-Krzemińska I, Król-Zielińska M, Osiński W. Positive effect of pedometer-based walking intervention on body image and physical activity enjoyment in adolescent girls. Biomed Hum Kinet. 2017;9:34–42. [Google Scholar]
- 63.Kerner C, Burrows A, McGrane B. Health wearables in adolescents: implications for body satisfaction, motivation and physical activity. Int J Health Promot Educ. 2019;57:191–202. [Google Scholar]
- 64.Nation-Grainger S. ‘It’s just PE’ till ‘It felt like a computer game’: using technology to improve motivation in physical education. Res Pap Educ. 2017;32:463–80. [Google Scholar]
- 65.Shore SM, Sachs ML, DuCette JP, Libonati JR. Step-count promotion through a school-based intervention. Clin Nurs Res. 2014;23:402–20. [DOI] [PubMed] [Google Scholar]
- 66.McEwan D, Harden SM, Zumbo BD, Sylvester BD, Kaulius M, Ruissen GR, et al. The effectiveness of multi-component goal setting interventions for changing physical activity behaviour: a systematic review and meta-analysis. Health Psychol Rev. 2016;10:67–88. [DOI] [PubMed] [Google Scholar]
- 67.Mattocks C, Ness A, Leary S, Tilling K, Blair SN, Shield J, et al. Use of accelerometers in a large field-based study of children: protocols, design issues, and effects on precision. J Phys Act Health. 2008;5:S98–111. [DOI] [PubMed] [Google Scholar]
- 68.Jago R, Watson K, Baranowski T, Zakeri I, Yoo S, Baranowski J, et al. Pedometer reliability, validity and daily activity targets among 10- to 15-year-old boys. J Sports Sci. 2006;24:241–51. [DOI] [PubMed] [Google Scholar]
- 69.McNamara E, Hudson Z, Taylor SJC. Measuring activity levels of young people: the validity of pedometers. Br Med Bull. 2010;95:121–37. [DOI] [PubMed] [Google Scholar]
- 70.World Health Organization. WHO guidelines on physical activity and sedentary behavior. 2020. https://www.who.int/publications-detail-redirect/9789240015128.
- 71.Fairclough SJ, Boddy LM, Mackintosh KA, Valencia-Peris A, Ramirez-Rico E. Weekday and weekend sedentary time and physical activity in differentially active children. J Sci Med Sport. 2015;18:444–9. [DOI] [PubMed] [Google Scholar]
- 72.Vijayakumar N, Op de Macks Z, Shirtcliff EA, Pfeifer JH. Puberty and the human brain: insights into adolescent development. Neurosci Biobehav Rev. 2018;92:417–36. [DOI] [PMC free article] [PubMed]
- 73.Aubert S, Brazo-Sayavera J, González SA, Janssen I, Manyanga T, Oyeyemi AL, et al. Global prevalence of physical activity for children and adolescents; inconsistencies, research gaps, and recommendations: a narrative review. Int J Behav Nutr Phys Act. 2021;18:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Baumann H, Fiedler J, Wunsch K, Woll A, Wollesen B. mHealth interventions to reduce physical inactivity and sedentary behavior in children and adolescents: systematic review and meta-analysis of randomized controlled trials. JMIR Mhealth Uhealth. 2022;10:e35920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang W, Cheng J, Song W, Shen Y. The effectiveness of wearable devices as physical activity interventions for preventing and treating obesity in children and adolescents: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2022;10:e32435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.van de Kop JH, van Kernebeek WG, Otten RHJ, Toussaint HM, Verhoeff AP. School-based physical activity interventions in prevocational adolescents: a systematic review and meta-analyses. J Adolesc Health. 2019;65:185–94. [DOI] [PubMed] [Google Scholar]
- 77.Nguyen S, Häcker A-L, Henderson M, Barnett T, Mathieu M-E, Pagani L, et al. Physical activity programs with post-intervention follow-up in children: a comprehensive review according to categories of intervention. Int J Environ Res Public Health. 2016;13:664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fuller D, Colwell E, Low J, Orychock K, Ann Tobin M, Simango B, et al. Reliability and validity of commercially available wearable devices for measuring steps, energy expenditure, and heart rate: systematic review. JMIR mHealth and uHealth. 2020;8:e18694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Marasso D, Lupo C, Collura S, Rainoldi A, Brustio PR. Subjective versus objective measure of physical activity: a systematic review and meta-analysis of the convergent validity of the Physical Activity Questionnaire for Children (PAQ-C). Int J Environ Res Public Health. 2021;18:3413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hidding LM, Altenburg TM, Mokkink LB, Terwee CB, Chinapaw MJM. Systematic review of childhood sedentary behavior questionnaires: what do we know and what is next? Sports Med. 2017;47:677–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rääsk T, Mäestu J, Lätt E, Jürimäe J, Jürimäe T, Vainik U, et al. Comparison of IPAQ-SF and two other physical activity questionnaires with accelerometer in adolescent boys. PLoS ONE. 2017;12:e0169527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mayorga-Vega D, Bocanegra-Parrilla R, Ornelas M, Viciana J. Criterion-related validity of the distance- and time-based walk/run field tests for estimating cardiorespiratory fitness: a systematic review and meta-analysis. PLoS ONE. 2016;11:e0151671. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Search strategy. Provide detailed search strategies for each database, including specific terms and Boolean operations.
Additional file 2. Funnel plot of the included studies for meta-analysis based on outcomes. Demonstrate the result of publication bias of all included studies.
Additional file 3. Certainty of the evidence assessment based on outcomes. Demonstrate GRADE evaluation and reasons in each domain for the overall quality of evidence.
Additional file 4. Meta-analysis of effect of WATs based on outcomes. Demonstrate results, including effect sizes, confidence intervals, and P values of meta-analysis from each outcome (Steps, MVPA, ST, and calories) and subgroup analysis of outcome steps.
Additional file 5. Synthesis table for effect direction based on outcomes and BCT used in studies. Demonstrate results of effect direction and specific behavior change techniques used for all included studies.
Data Availability Statement
All data is provided within the manuscript or supplementary information files.