Abstract
Background
Osteoarthritis (OA) is characterized by pain, functional impairments, muscle weakness, and joint stiffness. Since OA heightens reliance on heath care resources and exacerbates socioeconomic burden, remote OA rehabilitation using digital technologies is rapidly evolving.
Objective
The aim of this study was to analyze the efficacy of behavioral therapy–based digital interventions for patients with OA.
Methods
This study is a systematic review of randomized controlled trials (RCTs) that assessed the effects of behavioral therapy–based digital intervention tools for OA. These RCTs were searched from inception to June 2023 in the Web of Science, Embase, Cochrane Library, Ovid, and PubMed databases.
Results
Ten eligible RCTs comprising 1895 patients with OA were included. Digital tools based on either cognitive behavioral therapy (CBT) or behavior change technique (BCT) were investigated. All studies demonstrated low-to-moderate effects on pain reduction in the short term (standardized mean difference [SMD] –0.20, 95% CI –0.35 to –0.05). Six studies reported improvement in physical function (SMD –0.20, 95% CI –0.41 to 0.00), and 5 confirmed increased pain self-efficacy (SMD 0.22, 95% CI 0.02-0.42). In subgroup analysis, compared with CBT, BCT-based digital interventions demonstrated their effects on pain reduction (SMD –0.25, 95% CI –0.49 to 0.00) and physical function (SMD –0.26, 95% CI –0.54 to –0.01) in the short term. In addition, physiotherapist involvement in treatment had a positive effect on pain control (SMD –0.14, 95% CI –0.27 to –0.02). Furthermore, web-based digital tools improved physical function in the short term (SMD –0.28, 95% CI –0.54 to –0.01).
Conclusions
Moderate- and low-quality evidence supported that behavioral therapy–based digital tools improved pain intensity, physical function, and self-efficacy in the short term. However, affective interactions between patients and professionals may affect the clinical outcomes.
Trial Registration
PROSPERO CRD42023430716; https://tinyurl.com/yc49vzyy
Keywords: osteoarthritis, digital intervention, behavioral therapy, treatment, systematic review, meta-analysis, pain, impairment, quality of life, socioeconomic burden, psychotherapy-based digital intervention, patient, pain reduction
Introduction
Osteoarthritis (OA) is a prevalent joint disease affecting 29.7% of the population older than 40 years [1]. OA is characterized by pain, functional impairments, muscle weakness, joint stiffness, and reduced health-related quality of life (HRQoL) [2,3]. This causes heightened reliance on heath care resources and exacerbates socioeconomic burden [4,5]. Recent patient-centered guideline updates advocate for the implementation of rehabilitation interventions, including exercise therapy and educational programs as recommended nonpharmacological and nonsurgical treatment options [6,7]. These guidelines place a strong emphasis on the role of physical exercise, self-efficacy, and self-management strategies in the rehabilitation process for individuals with OA [8,9].
Psychological evidence–based auxiliary therapies have been integrated into the rehabilitation process to enhance rehabilitation outcomes [10]. These therapies provide a potent means of reinforcing patient education and behavior change. Behavioral theories, rooted in the social psychology of behavior change, are implemented as psychological evidence–based auxiliary therapies aimed at optimizing the positive components of interventions targeting patient health behaviors [11]. Many therapists incorporate physical therapy with behavioral therapy into their treatment protocols to alter observable maladaptive behavior patterns by eliciting new responses to given stimuli [12]. Behavioral science focuses on predicting, explaining, and altering behavior, encompassing approaches such as cognitive behavioral therapy (CBT) and behavior change techniques (BCTs) [13]. CBT, derived from the social cognitive theory, is a problem-focused approach that helps individuals identify and modify dysfunctional beliefs, thoughts, and behavior patterns contributing to their issues [14,15]. BCTs are considered active ingredients and include techniques such as feedback, self-monitoring, and behavior reinforcement. These techniques can be employed individually or in combination and in various forms [11,16]. Both CBT and BCT can enhance patients’ ability to self-manage chronic diseases, particularly among those experiencing anxiety, depression, and chronic pain [17-19]. However, study outcomes have been heterogeneous. Some have confirmed that CBT is beneficial for pain improvement [20-22] and that BCT could enhance physical activity compliance in patients with lower extremity OA [23-25], while others have argued that CBT has no effect on patients who catastrophize about pain or has only a small positive effect on pain [12,26].
The increased prevalence of OA has resulted in increasing demand for therapists [27]. To this end, remote OA rehabilitation using digital technologies (eg, telephones, websites, mobile apps) is rapidly evolving to alleviate the socioeconomic burden [28-30]. Digitalized rehabilitation is comparable to physical therapist supervision in terms of exercise quality, physical training supervision, and sport-specific self-efficacy [31,32]. Accumulating evidence has demonstrated long-term improvement in pain and physical function with digital-based rehabilitation in patients with OA [33,34]. Moreover, some studies have reported that internet-based CBT and BCT have led to significant improvements in physical activity and exercise behavior compared with traditional treatments [24,35,36].
Although several studies have investigated the impact of digital behavior change interventions based on the social cognitive theory on physical activity in patients with OA [34,37], several shortcomings remain. First, different digital tools differ in terms of the digital format and underlying behavioral theories, making it challenging to provide evidence-based recommendations for their development process. Second, existing studies have not fully explored broader outcome measures. In order to fully assess the rehabilitation outcomes of patients with OA, a wider range of outcome metrics should be considered to fully evaluate the effectiveness of digital tools based on behavioral therapies. Finally, considering that relevant studies were conducted 3-5 years ago and new digital interventions for knee OA have emerged since then, there is an urgent need for an up-to-date review and evaluation of digital intervention tools incorporating behavioral therapies. Therefore, the aim of this review was to assess the effectiveness of digital interventions based on behavioral therapies for patients with OA in terms of pain, physical function, disability, and HRQoL. In addition, subgroup analyses of digital tool formats, therapist involvement, and underlying behavioral theories were conducted.
Methods
Study Design
This review was performed in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses, Multimedia Appendix 1) [38] and guidelines published in the Cochrane Handbook of Systematic Evaluation [39]. This study protocol is registered with PROSPERO (International Register of Prospective Systematic Reviews: CRD42023430716).
Eligibility Criteria
Studies fulfilling the following criteria were included in this review and meta-analysis: randomized controlled trials (RCTs); participants with knee, hip, or ankle OA; comparing CBT- or BCT-based digital interventions with other treatments; and those addressing at least one component of pain, physical function, HRQoL, pain self-efficacy, or physical activity. Only peer-reviewed studies involving participants older than 18 years were eligible for inclusion. Studies published in any language other than English and those without sufficient data were excluded. In this review, the term “digital intervention” refers to any solution or technology that delivers health information from health care providers to patients over a distance.
Literature Search
The literature search was performed using Web of Science, Embase, Cochrane Library, Ovid, and PubMed databases, from date of inception to June 27, 2023 (Table S1 of Multimedia Appendix 2). In addition, the reference lists of relevant reviews and selected papers were manually examined for potentially relevant/eligible trials.
Study Selection
All duplicate references were removed. Subsequently, titles and abstracts were manually screened for potentially eligible studies by 2 reviewers (DZ and HY), and relevant RCTs were identified. The full text was then retrieved by both reviewers to assess eligibility for inclusion. Disagreements between the researchers were resolved through discussion or consultation with a third reviewer (BZ). The data were cross-validated by a third researcher (BZ) using EndNote 20 (Clarivate Analytics).
Data Extraction
Two independent reviewers (DZ and HY) collected the data. For continuous outcomes, the following data were extracted: mean (SD) and sample size at baseline and follow-up. For dichotomous outcomes, the number of cases and the total sample size were extracted. The dataset comprised study information, participant characteristics, type of behavioral therapy, type of digital tool, study duration, and outcome measures, including pain and function scores. If a study used multiple pain scales, the scale with the highest sensitivity to changes was used [40]. The function subscales of the Western Ontario and McMaster Universities Arthritis Index and the Knee Injury and Osteoarthritis Outcome Score/Hip dysfunction and Osteoarthritis Outcome Score Physical Function Shortform were used to assess functional improvement. Harmonized physical function was used, with higher scores indicating more severe physical dysfunction. The authors of studies with missing data were contacted. When the authors were unavailable, data were estimated using recommendations from the Cochrane Handbook (eg, estimation of SD from SEs) [39]. In trials in which SD was not reported, missing data were imputed from 95% CIs, SEs, P values, baseline changes, graphical representations, median (IQR), or SDs from baseline [41]. Trials in which imputations were not possible were excluded from the quantitative analysis.
The short-term effect was considered as follow-up period ≤6 months after randomization, and the long-term effect was considered as follow-up period >6 months after randomization. When >1 timepoint was available during the same follow-up period, the point closer to the end of the intervention was considered.
Risk of Bias Assessment
Risk of bias was assessed using the risk-of-bias tool in the Cochrane Handbook of Systematic Evaluation [42]. Seven domains, including random sequence generation, allocation concealment, blinding of participants and personnel, incomplete outcome data, selective reporting, and other biases, were used to evaluate quality of evidence [43]. Each domain was assigned a judgement of low, high, or unclear risk of bias. Furthermore, the quality level of this meta-analysis was evaluated according to GRADE (Grading of Recommendations Assessment, Development, and Evaluation) approach [44,45]. The quality of evidence was classified as high, moderate, low, or very low.
Data Analysis
A random-effects meta-analysis was performed using Review Manager version 5.4 (Cochrane Collaboration). Standardized mean differences (SMDs) were calculated to standardize the results to a uniform scale when studies assessed the same outcomes using different instruments. The SMDs for pain, physical function, HRQoL, pain self-efficacy, and physical activity were calculated by comparing interventions using behavioral therapy–based digital tools with other conventional methods. Therefore, a negative SMD value for pain and physical function and a positive SMD value for HRQoL, pain self-efficacy, and physical activity favor behavioral therapy–based digital tools. The magnitude of SMD was interpreted in accordance with the guidelines reported by Cohen [46], as follows: SMD <0.2 (small), 0.2-0.8 (medium), and >0.8 (large). For clinical interpretation, the mean differences were calculated.
Sensitivity and subgroup analyses were performed to assess the potential impact of the sources of heterogeneity. To investigate the potential impact of methodological quality on the estimates, we performed a sensitivity analysis by removing 1 study at a time, and trials with poor methodological quality were removed. Subgroups were defined in terms of the type of behavioral therapy (ie, CBT or BCT), type of digital tool (apps, wearable devices, and phones), and therapist involvement. The heterogeneity of the pooled studies was examined using the chi-square test and the I2 statistic, with I2>50% indicating substantial heterogeneity [47]. Publication bias was assessed by visual inspection of funnel plots and Egger test for meta-analyses ≥10 trials. All analyses were performed using Review Manager version 5.4.
Results
Study Selection and Characteristics
The initial search retrieved 1628 papers after removing duplicates, of which 1557 that did not fulfill the inclusion criteria were excluded. Two additional records were found: one through cross-referencing of bibliographies and the other by contacting the corresponding authors. Subsequently, 73 eligible full-text papers were reviewed, of which 10 RCTs were ultimately included in the quantitative analysis (Figure 1, Table 1) [24,35,36,48-53].
Figure 1.
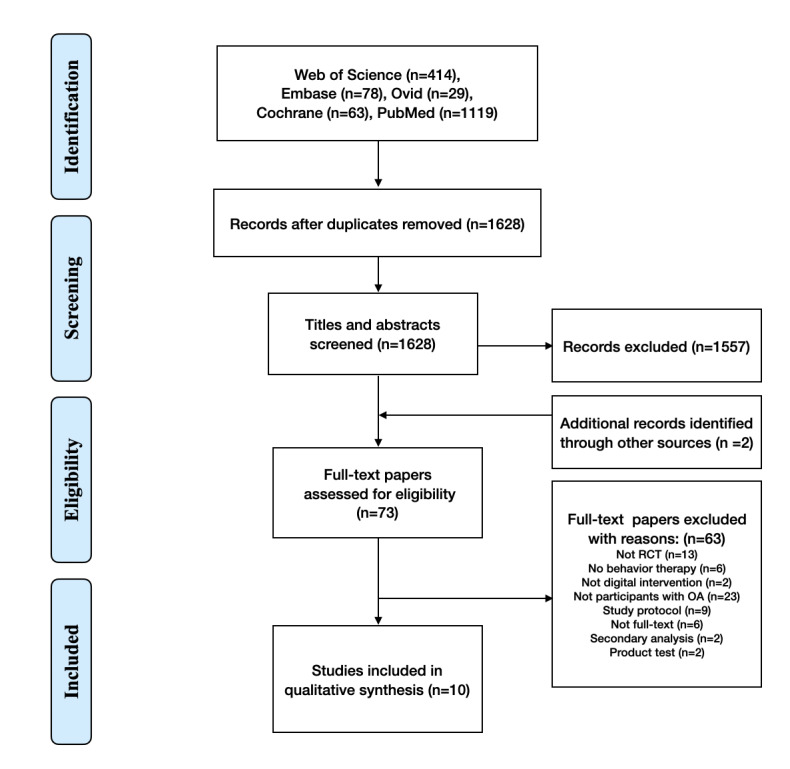
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart of the studies selected in this review. OA: osteoarthritis; RCT: randomized controlled trial.
Table 1.
Characteristics of the included studies.
| Study author(s) | Nationality | Participants | Outcome (primary or secondary) | Follow-up (months) | Postintervention attrition (%) | ||||
|
|
|
Intervention group | Control group |
|
|
Intervention group | Control group | ||
| Bennell et al [36] | Australia | SMS text message (n=56) | Non-SMS text message (n=54) | Exercise Adherence Rating Scale, days of the week to exercise (0-3), pain (Knee Injury and Osteoarthritis Outcome Score), overall mean knee pain (Numeric Rating Scale), symptoms (Knee Injury and Osteoarthritis Outcome Score), function (Knee Injury and Osteoarthritis Outcome Score), knee-related quality of life (Knee Injury and Osteoarthritis Outcome Score), health-related quality of life, self-efficacy: pain (Arthritis Self-Efficacy Scale), self-efficacy: function (Arthritis Self-Efficacy Scale), self-efficacy: other (Arthritis Self-Efficacy Scale), Behavioral Factors in Osteoarthritis Management Scale, Physical Activity Scale for the Elderly, Pain Catastrophizing Scale | 6 | 14.29 | 5.55 | ||
| Rini et al [48] | United States | Digital application (n=58) | Nonintervention (n=55) | Pain, self-efficacy in pain management, pain-related anxiety, pain-related functional interference, positive and negative emotions | 3 | 1.72 | 5.45 | ||
| Hinman et al [49] | Australia | Campaign advice and support (n=87) | Available services (n=88) | Overall mean knee pain (Numeric Rating Scale), Pain with Activities of Daily Living (Western Ontario and McMaster Universities Arthritis Index), mean pain while walking (Numeric Rating Scale), Pain Self-Efficacy (Arthritis Self-Efficacy Scale), Functional Self-Efficacy (Arthritis Self-Efficacy Scale), Fear of Movement, Physical Activity Scale for the Elderly, barriers to physical activity, benefits of physical activity, health-related quality of life | 6 | 5.74 | 13.63 | ||
| McCurry et al [50] | United States | Cognitive behavioral therapy-I (n=163) | Education (n=164) | Insomnia Severity Index, Flinders Fatigue Scale, Arthritis Pain Intensity and Interference with Activity, Brief Pain Inventory-short form, Patient Health Questionnaire-8 items, Measure of Depression | 12 | 14.72 | 6.09 | ||
| Pelle et al [26] | Netherlands | Dr Bart (n=214) | Conventional physiotherapy group (n=213) | Incidence rate ratio, pain, symptoms and dysfunction (Knee Injury and Osteoarthritis Outcome Score or Hip dysfunction and Osteoarthritis Outcome Score), quality of life (EQ-5D-3L), total hours of physical activity, Patient Activation Measure-13 items, knowledge skills confidence, Illness Perception Questionnaire cognitive and emotional perceptions | 6 | 39.25 | 22.07 | ||
| Mecklenburg et al [51] | United States | Hinge Health (n=101) | Education (n=61) | Pain, Physical Function Scale (Knee Injury and Osteoarthritis Outcome Score), Visual Analog Scale Pain, Visual Analog Scale Hardness Score, surgical intent | 3 | 33.33 | 40.98 | ||
| Nelligan et al [24] | Australia | Automatic Behavior Change SMS Support (n=103) | Web-based (n=103) | Physical Function (Western Ontario and McMaster Universities Osteoarthritis Index), Overall Mean Knee Pain (Numeric Rating Scale), Pain, Knee Quality of Life, Sport and Recreation (Knee Injury and Osteoarthritis Outcome Score), Assessment of quality of life-6D Physical Activity Scale, Arthritis Self-Efficacy Scale, Exercise Self-Efficacy Scale | 6 | 11.65 | 10.68 | ||
| Bennell et al [35] | Australia | Telephone counseling (n=84) | Nontelephone counseling (n=84) | Pain, physical function (Western Ontario and McMaster Universities Osteoarthritis Index), Numeric Rating Scale walking pain (range 0-10), Assessment of quality of life II, Physical Activity Scale for the Elderly, Athletic Activity Scale total activity time, step time (hours/day) | 18 | 14.29 | 16.67 | ||
| Kloek et al [52] | Netherlands | Web-based (n=109) | Conventional physiotherapy group (n=99) | Physical functioning, functions of daily living, functional limitations (Hip dysfunction and Osteoarthritis Outcome Score or Knee Injury and Osteoarthritis Outcome Score), self-perceived effects, arthritis self-efficacy scale, pain, and fatigue | 12 | 18.30 | 12.10 | ||
| Li et al [53] | Canada | Fitbit (immediate group) (n=26) | Education (delay group) (n=25) | Mean daily moderate to vigorous physical activity, Knee Injury and Osteoarthritis Outcome Score, Partners in Health Scale, Theory of Planned Behavior Questionnaire, Patient Health Questionnaire-9 items, Self-Reporting Habits Index | 9.75 | 7.70 | 4 | ||
Study Characteristics
In this qualitative analysis, 9 RCTs and 1 cluster RCT, comprising 1895 patients, were included (Tables S2-S4 [24,26,35,36,48-53] of Multimedia Appendix 2). The trials were conducted in Europe (2/10, 20%) [26,52], Oceania (4/10, 40%) [24,35,36,49], and North America (4/10, 40%) [48,50,51,53]. The sample sizes of the included trials ranged from 51 to 427; the mean age of the patients was 62.5 (SD 8.1) years, and females were predominant in the pooled population (1231/1895, 64.9%), which is consistent with the global prevalence of OA. Six studies recruited participants with knee OA only [24,35,36,49,51,53], whereas 4 recruited participants with both knee and hip OA [26,48,50,52]. CBT-based (4 studies) [35,48,50,51] and BCT-based (6 studies) [24,26,36,49,52,53] therapies were the most used behavioral therapies blended into the digital intervention for patients with OA. Three types of digital tools were used: apps or websites in 9 studies [24,26,35,36,48,49,51-53], wearable devices in 3 studies [51-53], and SMS text messages in 1 study [50]. Four studies included face-to-face communication with physical therapists or fitness instructors [36,51-53]. All trials reported short-term effects (up to 6 months after randomization) [24,26,35,36,48-53] and 6 reported long-term effects (>6 months after randomization) [24,26,35,50,52,53]. Pain intensity, physical function, HRQoL, pain self-efficacy, and physical activity were evaluated in 10, 6, 6, 5, and 5 trials, respectively.
Risk of Bias in the Included Trials
In general, the most frequent risks of bias for RCTs were incomplete outcomes (6/10, 60%) and blinding of participants/personnel (6/10, 60%). Other biases and selective reporting accounted for the second most frequent risks of bias (2/10, 20%). The overall confidence in the cumulative evidence varied from very low to moderate, with low confidence being the most commonly identified (Figure 2 [24,26,35,36,48-53], Table 2).
Figure 2.
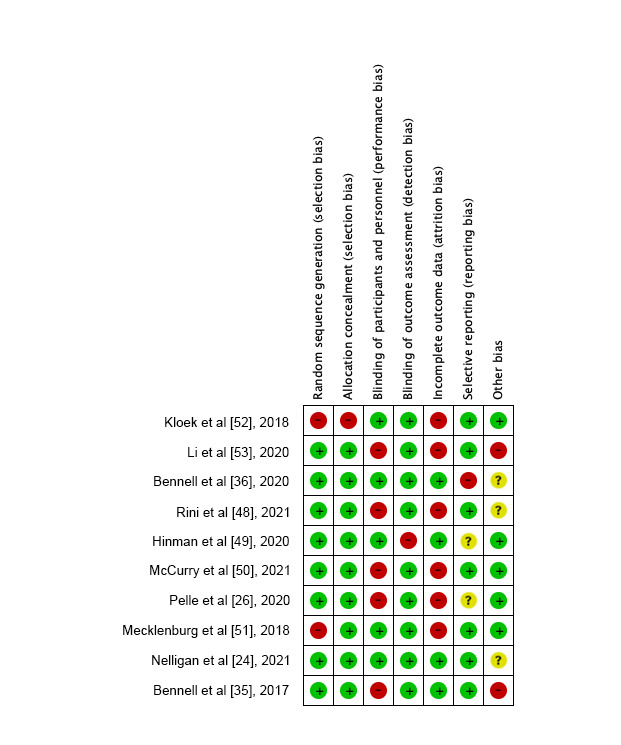
Risk of bias. Red indicates high risk, green indicates low risk, and yellow indicates unclear risk.
Table 2.
Summary of the findings for efficacy outcomes.a
| Outcome, time | Studies (patients), n | SMDb (95% CI) | I2 (%) | Quality of evidence assessment | |||||||
|
|
|
|
|
Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Ratingc | ||
| Pain (short-term) | 10 (1895) | –0.20 (–0.35 to 0.05) | 65 | –d | – | +e | + | + | Low | ||
| Pain (long-term) | 6 (1271) | –0.01 (–0.12 to 0.10) | 0 | – | + | + | + | + | Moderate | ||
| Physical function (short-term) | 6 (974) | –0.20 (–0.41 to 0.00) | 62 | – | – | + | + | + | Low | ||
| Physical function (long-term) | 3 (519) | –0.13 (–0.32 to 0.06) | 0 | – | + | + | + | + | Moderate | ||
| Health-related quality of life (short-term) | 6 (1137) | 0.28 (–0.05 to 0.61) | 86 | – | ––2f | + | + | + | Very low | ||
| Pain self-efficacy (long-term) | 5 (812) | 0.22 (0.02 to 0.42) | 10 | – | + | + | – | + | Low | ||
| Physical activity (short-term) | 5 (1086) | 0.05 (–0.07 to 0.17) | 0 | – | + | + | + | + | Moderate | ||
| Subgroup outcome | |||||||||||
|
|
Behavior therapy pain outcomes (short-term) | ||||||||||
|
|
|
BCTg | 6 (1137) | –0.25 (–0.49 to 0.00) | 74 | – | – | + | + | + | Low |
|
|
|
CBTh | 4 (758) | –0.10 (–0.24 to 0.05) | 0 | – | + | + | + | – | Low |
|
|
Behavior therapy pain outcomes (long-term) | ||||||||||
|
|
|
BCT | 4 (781) | –0.01 (–0.15 to 013) | 0 | – | + | + | + | + | Moderate |
|
|
|
CBT | 2 (490) | 0.00 (–0.18 to 0.17) | 0 | – | + | + | + | + | Moderate |
|
|
Physical function outcomes (short-term) | ||||||||||
|
|
|
BCT | 5 (659) | –0.28 (–0.54 to –0.01) | 67 | – | – | + | + | + | Low |
|
|
|
CBT | 2 (363) | –0.05 (–0.26 to 0.16) | 0 | – | + | + | + | – | Low |
|
|
Physical function outcomes (long-term) | ||||||||||
|
|
|
BCT | 2 (311) | –0.21 (–0.44 to 0.02) | 6 | – | + | + | + | – | Low |
|
|
|
CBT | 1 (208) | 0.00 (–0.28.0.27) | N/Ai | – | + | + | + | – | Low |
|
|
Pain outcomes with therapist involvement (short-term) | ||||||||||
|
|
|
With | 6 (1039) | –0.14 (–0.27 to –0.02) | 0 | – | + | + | + | + | Moderate |
|
|
|
Without | 4 (856) | –0.23 (–0.60 to 0.14) | 85 | – | ––2 | + | + | + | Very low |
|
|
Pain outcomes with therapist involvement (long-term) | ||||||||||
|
|
|
With | 5 (844) | –0.04 (–0.17 to 0.10) | 0 | – | + | + | + | + | Moderate |
|
|
|
Without | 1 (427) | 0.05 (–0.14 to 0.24) | N/A | – | + | + | + | – | Low |
|
|
Physical function outcomes with therapists (short-term) | ||||||||||
|
|
|
With | 4 (706) | –0.17 (–0.40 to 0.07) | 60 | – | – | + | + | + | Low |
|
|
|
Without | 2 (316) | –0.27 (–0.75 to 0.20) | 76 | – | – | + | + | + | Low |
|
|
Pain outcomes with digital tools (short-term) | ||||||||||
|
|
|
Telephone | 1 (282) | –0.09 (–0.33 to 0.14) | N/A | – | + | + | + | – | Low |
|
|
|
Web-based | 6 (1199) | –0.23 (–0.47 to 0.01) | 75 | – | ––2 | + | + | + | Very low |
|
|
|
Wearable | 3 (414) | –0.12 (–0.31 to 0.08) | 0 | – | + | + | + | – | Low |
|
|
Pain outcomes with digital tools (long-term) | ||||||||||
|
|
|
Telephone | 1 (282) | –0.03 (–0.27 to 0.20) | N/A | – | + | + | + | – | Low |
|
|
|
Web-based | 3 (738) | –0.02 (–0.16 to 0.12) | 0 | – | + | + | + | + | Moderate |
|
|
|
Wearable | 2 (251) | 0.05 (–0.20 to 0.30) | 0 | – | + | + | + | – | Low |
|
|
Physical function outcomes with digital tools (short-term) | ||||||||||
|
|
|
Web-based | 4 (659) | –0.28 (–0.54 to –0.01) | 67 | – | – | + | + | + | Low |
|
|
|
Wearable | 2 (363) | –0.05 (–0.26 to 0.16) | 0 | – | + | + | + | – | Low |
|
|
Physical function outcomes with digital tools (long-term) | ||||||||||
|
|
|
Web-based | 2 (311) | –0.21 (–0.44 to 0.02) | 6 | – | + | + | + | – | Low |
|
|
|
Wearable | 1 (208) | 0.00 (–0.28 to 0.27) | N/A | – | + | + | + | – | Low |
aA funnel plot and Egger test was used to judge publication bias (Figure S1 of Multimedia Appendix 2).
bSMD: standardized mean difference.
cGRADE (Grading of Recommendations Assessment, Development, and Evaluation) Working Group grades of evidence. High: further research is very unlikely to change our confidence in the estimate of effect; moderate: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate; low: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate; very low: we are very uncertain about the estimate.
d– indicates low-quality evidence.
e+ indicates high-quality evidence.
f––2 indicates a moderate to high degree of inconsistency.
gBCT: behavior change technique.
hCBT: cognitive behavioral therapy.
iN/A: not applicable. Since only 1 study was included, there was no heterogeneity in the analysis.
Main Outcomes
For pain reduction, 10 trials with 1895 patients reported a moderate effect of behavioral therapy–based digital tools in reducing pain in the short term (4-24 weeks) (SMD –0.20, 95% CI –0.35 to –0.05; P=.008; I2=58%), with low-quality evidence [24,26,35,36,48-53]. However, in the long-term follow-up (≥24 weeks), this effect was ambiguous when 6 trials with 1271 patients were included (SMD –0.01, 95% CI –0.12 to 0.10; P=.88; I2=0%), with moderate-quality evidence [26,35,49,50,52,53]. For physical function, low certainty evidence supported significant improvement in the short term (SMD –0.20, 95% CI –0.41 to 0.00; P=.05; I2=62%) from 6 trials with 974 patients [26,35,36,49,50,52]. However, its effect showed no significance in 3 trials with 519 patients in the long term (SMD –0.13, 95% CI –0.32 to 0.06; P=.18; I2=17%), with moderate-quality evidence [35,49,52]. Sensitivity analysis revealed that the results of physical function were unstable; therefore, these results should be interpreted with caution. For pain self-efficacy, low-quality evidence from 5 trials with 812 patients reported a positive effect (SMD 0.22, 95% CI 0.02-0.42; P=.03; I2=10%) [24,36,48,49,52]. However, for HRQoL, very low-quality evidence from 6 trials with 1137 patients demonstrated an uncertain effect (SMD 0.28, 95% CI –0.05 to 0.61; P=.10; I2=86%) [24,26,35,36,49,53]. Further, moderate quality evidence demonstrated an uncertain effect (SMD 0.05, 95% CI –0.07 to 0.17; P=.45; I2=0%) for physical activity [24,26,35,36,49]. All results are presented in Figure 3 [24,26,35,36,48-53].
Figure 3.
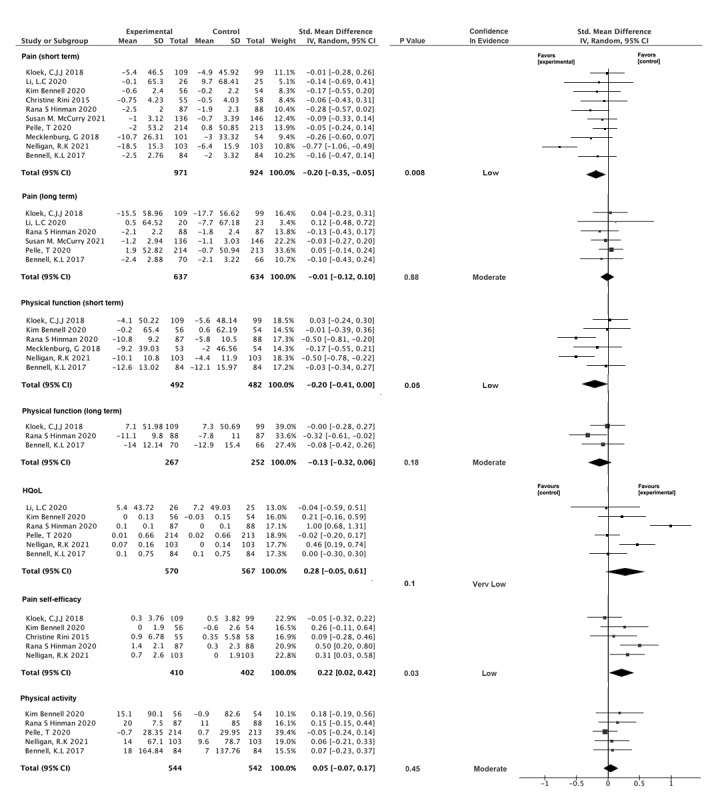
Main results of this study. HQoL: health-related quality of life.
Subgroup Analyses
Subgroup analyses of behavioral therapy, digital tools, and therapist involvement were performed, and significant improvements were found in the short-term intervention.
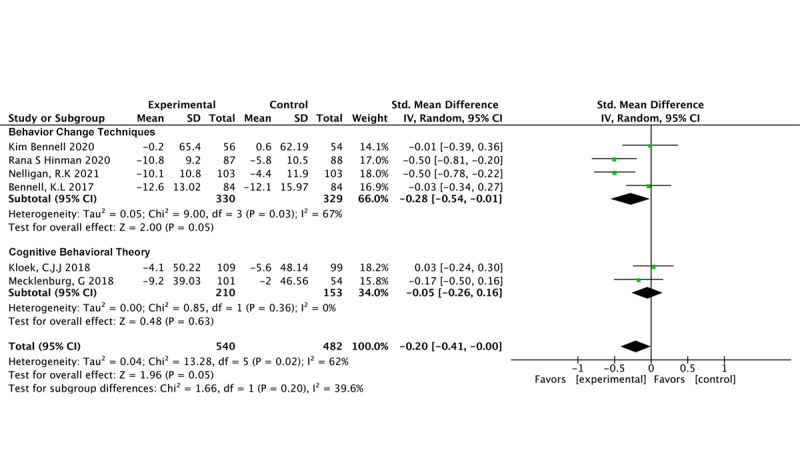
Behavioral Therapy
BCTs (6 studies, 1177 participants) demonstrated a significant impact on pain reduction (SMD –0.25, 95% CI –0.49 to 0.00; P=.05; I2=74%) [24,26,35,36,49,53]. However, our findings indicate that CBT (n=4 studies, n=758 participants) did not have a significant effect on pain (SMD –0.10, 95% CI –0.24 to 0.05; P=.19; I2=0%) [48,50-52] (Figure 4 [24,26,35,36,48-53]).
Figure 4.
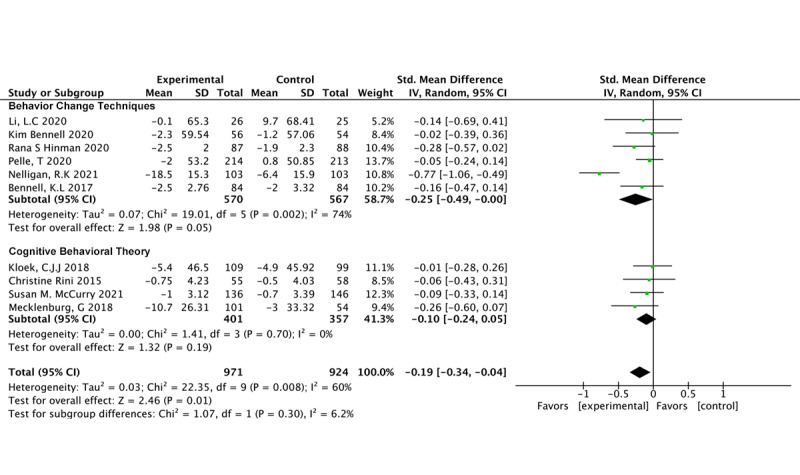
Pain outcomes in different behavioral therapy models.
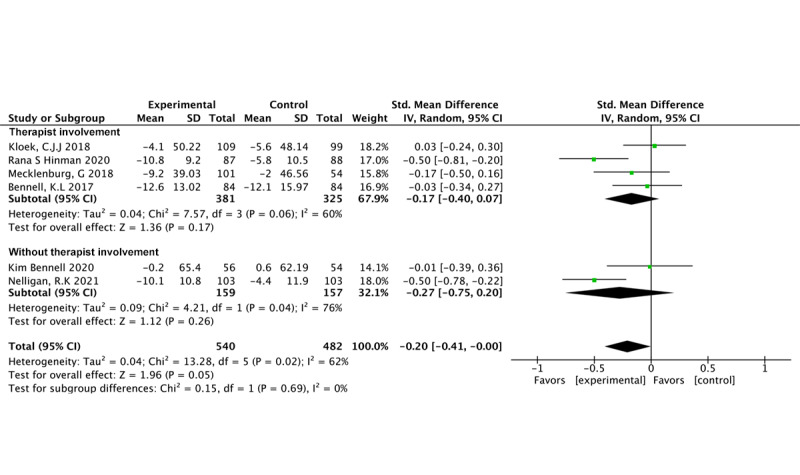
BCTs (4 studies, 659 participants) were found to significantly reduce physical functional impairment (SMD –0.28, 95% CI –0.54 to –0.01; P=.05; I2=67%) [24,35,36,49]. In contrast, our findings show that CBT (n=2 studies, n=363 participants) did not significantly affect pain (SMD –0.20, 95% CI –0.26 to 0.16; P=.63; I2=0%) [51,52] (Figure 5 [24,35,36,49,51,52]).
Figure 5.
Physical function outcomes in different behavioral therapy models.
Therapist Involvement
Six studies involving 1039 participants revealed significant effects favoring the intervention in pain reduction when therapist involvement was present (SMD –0.14, 95% CI –0.27 to –0.02; P=.02; I2=0%) [35,49-53]. Conversely, 4 studies involving 856 participants revealed no significant effects in pain reduction for interventions without therapist involvement (SMD –0.23, 95% CI –0.60 to 0.14; P=.22; I2=85%) [24,26,36,48] (Figure 6 [24,26,35,36,48-53]).
Figure 6.
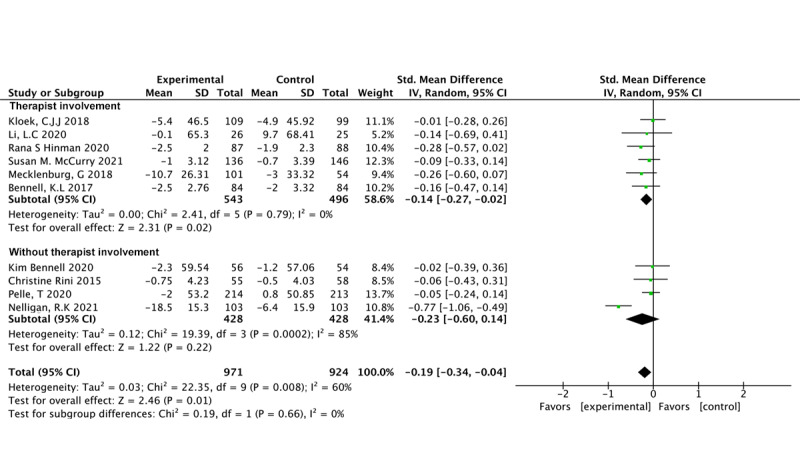
Pain outcomes related to therapist involvement.
Four studies involving 706 participants (SMD –0.17, 95% CI –0.40 to 0.07; P=.17; I2=60%) [35,49,51,52] and 2 studies involving 316 participants [24,36] (SMD –0.22, 95% CI –0.37 to –0.06; P=.26; I2=76%) revealed that therapist involvement did not result in significant improvements in physical functional impairment (Figure 7 [24,35,36,49,51,52]).
Figure 7.
Physical function outcomes related to therapist involvement.
Digital Tools
Neither the use of a mobile app/website (SMD –0.23, 95% CI –0.47 to 0.01; P=.06; I2=75%) [50], telephone communication (SMD –0.09, 95% CI –0.33 to 0.14; P=.44) [24,26,35,36,48,49] nor the use of a wearable device as a monitoring device (SMD –0.12, 95% CI –0.31 to 0.08; P=.24; I2=0%) [51-53] were associated with the effect in favor of the intervention (Figure 8 [24,26,35,36,48-53]).
Figure 8.
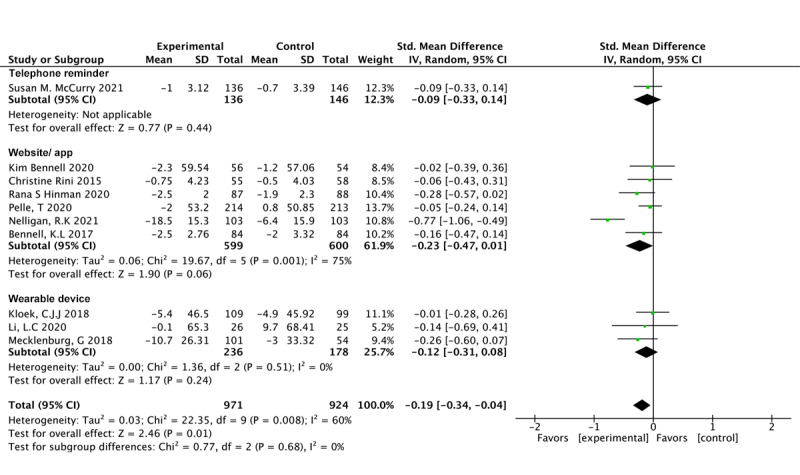
Pain outcomes with different digital tools.
Four studies involved 659 participants who used a mobile app/website and observed a significant effect in favor of the intervention in terms of physical dysfunction (SMD –0.28, 95% CI –0.54 to –0.01; P=.05; I2=67%) [24,35,36,49]. However, there was no difference for only 2 items involving wearables (SMD –0.05, 95% CI –0.26 to 0.16; P=.63; I2=0%) [51,52] (Figure 9 [24,35,36,49,51,52]).
Figure 9.
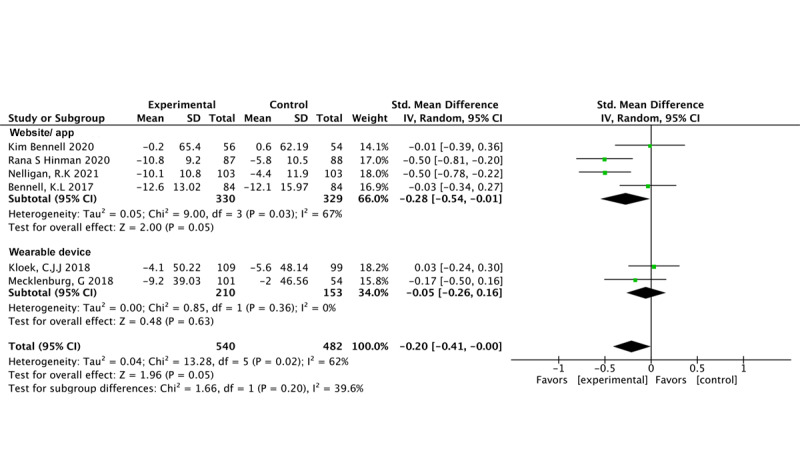
Physical function outcomes with different digital tools.
Risks of Bias Sensitivity Analysis
After excluding studies at high risk of bias, the results regarding randomization, allocation concealment, incomplete outcome reporting, selective reporting, and other biases demonstrated stability. However, instability was observed in the results when studies with unclear patient blinding were excluded. For outcomes related to physical function, studies excluding those at high risk of bias showed stability in allocation concealment and incomplete outcome reporting. Nevertheless, exclusion of trials with biases related to randomization, blinding, selective reporting, and other factors resulted in unstable findings. Therefore, these results warrant cautious interpretation (Table 3). Additionally, due to the inclusion of predominantly fewer than 10 studies, the potential impact of small-study effects was explored using only funnel plots. The inspection of funnel plots (Figure S1 of Multimedia Appendix 2) suggested small study effects/publication bias for the overall results in terms of pain in the short and medium terms.
Table 3.
Sensitivity of the studies.
| Variable | Number of studies (patients) | Standardized mean difference (95% CI) | I2 (%) | Overall effect P value | Subgroup differences P value | ||||||||
| Pain | |||||||||||||
|
|
Randomization | .52 | |||||||||||
|
|
|
High risk and unclear risk | 2 (363) | –0.12 (–0.37 to 0.13) | 26 | .34 |
|
||||||
|
|
|
Low risk | 8 (1532) | –0.22 (–0.40 to –0.04) | 65 | .02 |
|
||||||
|
|
Allocation concealment | .18 | |||||||||||
|
|
|
High risk and unclear risk | 1 (208) | –0.01 (–0.28 to 0.26) | 0 | .94 |
|
||||||
|
|
|
Low risk | 9 (1687) | –0.22 (–0.38 to –0.06) | 60 | .006 |
|
||||||
|
|
Blinding | .30 | |||||||||||
|
|
|
High risk and unclear risk | 6 (1216) | –0.11 (–0.23 to 0.00) | 0 | .05 |
|
||||||
|
|
|
Low risk | 4 (679) | –0.31 (–0.66 to 0.05) | 81 | .09 |
|
||||||
|
|
Incomplete outcome | .14 | |||||||||||
|
|
|
High risk and unclear risk | 5 (1123) | –0.09 (–0.20 to 0.03) | 0 | .15 |
|
||||||
|
|
|
Low risk | 5 (772) | –0.30 (–0.57 to –0.04) | 70 | .03 |
|
||||||
|
|
Selective reporting | .37 | |||||||||||
|
|
|
High risk and unclear risk | 4 (825) | –0.12 (–0.25 to 0.02) | 0 | .09 |
|
||||||
|
|
|
Low risk | 6 (1070) | –0.25 (–0.49 to 0.00) | 73 | .05 |
|
||||||
|
|
Other bias | .22 | |||||||||||
|
|
|
High risk and unclear risk | 4 (535) | –0.34 (–0.68 to 0.01) | 73 | .06 |
|
||||||
|
|
|
Low risk | 6 (1360) | –0.11 (–0.21 to –0.01) | 0 | .05 |
|
||||||
| Physical function | |||||||||||||
|
|
Randomization | .20 | |||||||||||
|
|
|
High risk and unclear risk | 4 (659) | –0.28 (–0.54 to –0.01) | 67 | .05 |
|
||||||
|
|
|
Low risk | 2 (363) | –0.05 (–0.26 to 0.16) | 0 | .63 |
|
||||||
|
|
Allocation concealment | .10 | |||||||||||
|
|
|
High risk and unclear risk | 1 (208) | 0.03 (–0.24 to 0.30) | N/Aa | .83 |
|
||||||
|
|
|
Low risk | 5 (814) | –0.26 (–0.47 to –0.04) | 58 | .02 |
|
||||||
|
|
Blinding | .71 | |||||||||||
|
|
|
High risk and unclear risk | 3 (343) | –0.27 (–0.73 to 0.19) | 79 | .25 |
|
||||||
|
|
|
Low risk | 3 (679) | –0.17 (–0.43 to 0.09) | 63 | .19 |
|
||||||
|
|
Incomplete outcome | .20 | |||||||||||
|
|
|
High risk and unclear risk | 2 (363) | –0.05 (–0.26 to 0.16) | 0 | .63 |
|
||||||
|
|
|
Low risk | 4 (659) | –0.28 (–0.54 to –0.01) | 67 | .05 |
|
||||||
|
|
Selective reporting | .71 | |||||||||||
|
|
|
High risk and unclear risk | 2 (285) | –0.27 (–0.75 to 0.21) | 75 | .27 |
|
||||||
|
|
|
Low risk | 4 (737) | –0.17 (–0.41 to 0.07) | 64 | .17 |
|
||||||
|
|
Other bias | .94 | |||||||||||
|
|
|
High risk and unclear risk | 3 (484) | –0.20 (–0.52 to 0.13) | 69 | .25 |
|
||||||
|
|
|
Low risk | 3 (538) | –0.21 (–0.53 to 0.11) | 70 | .19 |
|
||||||
aN/A: not applicable. Since only 1 study was included, there was no heterogeneity in the analysis.
Discussion
Main Findings
This systematic review and meta-analysis report provides moderate- to low-quality evidence regarding the therapeutic effects of 3 digital tools based on 2 behavioral therapies for patients with OA. Digital tools focusing on behavior change have shown short-term efficacy, including reductions in pain intensity and physical function impairment along with improvements in pain self-efficacy. However, our study did not find significant differences in sports and recreational activities or overall physical activity. Given the risk of bias in the included studies, the overall quality of evidence is moderate to low. Furthermore, the evidence quality regarding HRQoL outcomes is deemed very low; so, the findings should be interpreted with caution.
Our study compares the short-term and long-term effects of behavior theory–based digital interventions on pain. However, contrary to Safari et al’s [34] previous findings, we found no significant long-term effects of behavior theory–based digital interventions. This discrepancy may stem from the incomplete success of digital interventions in promoting adherence to prescribed exercise regimens among patients with musculoskeletal disease [30,54]. A recent review indicated that digital interventions have not been shown to enhance compliance with therapeutic exercise among patients with chronic musculoskeletal disease [30]. Therefore, further high-quality research is needed to conclusively determine the efficacy of these interventions for long-term therapeutic effects.
Among the 10 studies included, 9 observed positive changes in patient pain [24,26,35,36,48-51,53]. Current research integrates behavior therapy principles into digital interventions aimed at enhancing patients’ ability to modify their decision-making frameworks and guide behavior change in patients with OA [55]. The educational components of digital tools include pathophysiological and etiological information on OA, guideline-based therapies, exercise for OA management, and pain management strategies, and these are closely aligned with the social cognitive theories of health behavior [19]. These address motivational and volitional determinants of exercise behavior [31,56]. Our study suggests that such semisupervised, freely accessible interventions may be an effective option for reducing pain [24], as pain intensity correlates positively with the use of exercise, courses, and health self-management messaging functionalities [57]. Additionally, improvements in physical function impairment were observed in 6 studies. Research has demonstrated the impact of digital health interventions on physical function through exercise and aerobic training programs [58,59]. This is because the digital tools included in the studies mostly incorporate multicomponent exercises recommended by clinical guidelines, which can enhance balance and mobility [60,61].
Low-quality evidence revealed that a behavioral therapy–based digital tool had a positive effect on pain self-efficacy, which is consistent with previous research that found greater self-confidence activation in digital self-monitoring programs than in traditional management programs [33,62,63]. Self-efficacy refers to an individual’s perception of being capable of making positive changes in their lives can help them to be more likely to initiate and maintain positive behavior changes [64,65]. Previous studies have reported significant indirect effects of digital tools on health behaviors, and we suggest that self-efficacy could be used as an indirect mediator in clinical practice [65,66].
This review indicates that behavior therapy–based digital interventions have no significant impact on HRQoL, which is consistent with that reported in a previous systematic review [67]. However, the mechanisms underlying patients’ perceptions of quality of life remain unclear, necessitating validated behavior change measures such as patient activation measures to effectively assess such systems. Additionally, we found that behavior therapy–based digital interventions do not significantly influence physical activity levels [55,68]. This may be attributed to the lack of face-to-face supervision. Nonetheless, despite these findings, such interventions could potentially offer substantial public health benefits, despite the modest effect size.
Subgroup Findings
The effects of behavioral therapy were independently assessed in a subanalysis. However, our results were not consistent with those of previous studies in that only BCT-based digital tools had an impact on outcomes in patients with OA [16,20,33]. In previous studies, it was difficult to trace patient participation on a digital platform, and multiple variations could be introduced into the outcomes [69,70]. The underlying mechanism by which behavior change–based digital tools can reduce pain and physical function in patients with OA is that such interventions can elicit patient intentions and modify their decision-making structures [55]. The educational components of the digital tools include information regarding the pathology and etiology of OA, treatment according to guidelines, exercise for OA, and pain and symptom relief, which are closely related to the social cognitive theories of health behavior [19]. These factors examine the influences of motivation and willpower on exercise behavior [31,56]. Our research indicated that this semisupervised, freely accessible intervention may be effective for pain reduction [24].
Another interesting finding in our study was that physical therapist involvement was shown to be effective in pain reduction and physical function, although with low-quality evidence. This is consistent with previous evidence suggesting that communication and interaction with professionals can increase patient motivation [67,71]. Digital tools provide the opportunity to assume the role of an aid to assist patients in engaging in less complex exercises as part of independent home training [72,73]. However, it sometimes cannot replace physical therapists who achieve similar effects [31,74,75]. Typical digital intervention tools rely on self-management and lack timely reminders and professional communication [67,71]. Studies have shown that digital tools without therapist involvement do not offer significant advantages over conventional care interventions [26]. Therefore, future digital intervention tools should aim to blend traditional OA care with digital OA care solutions. Heath care should provide solutions for personalized, comprehensive, simple, reliable, and continuous mixed heath care [76,77].
Another finding is that digital tools based on website or application development show significantly better short-term improvements in physical function compared to wearable devices. This may be due to the complex wearing process of wearable devices, especially among older adults who may have resistance to wearing such devices and find them potentially hindering daily activities. Hence, future application development should fully consider patient characteristics and needs rather than solely relying on hospital staff knowledge and experience [78,79].
Clinical and Research Implications
This study confirms that digital tools combined with behavioral therapy, especially BCTs, have moderate and clinically meaningful treatment effects in patients with hip and knee OA in the short and long term. These findings echo the current guidelines that recommend rehabilitation, emphasizing exercise, self-efficacy, and self-management for patients with OA. As digital technologies rapidly evolve, the affective interaction between patients and professionals remains a crucial factor and should be considered in future studies.
Strengths and Limitations
This study has several limitations. First, we were unable to fully explore the reasons for heterogeneity because many covariates for behavioral therapy–based digital tools in OA were not usually reported in the trials. Second, subgroup analyses to explore the potential impact of a high risk of bias and characteristics of the population were limited by the small number of included trials or because the data were poorly reported. Third, despite the use of extensive search techniques, the evaluation may have been hampered by language bias because we only included studies published in English in the 5 databases. Therefore, we cannot guarantee that all potentially eligible studies were included. Fourth, this meta-analysis included only 10 studies, with 9 RCTs and 1 RCT cluster. Owing to this rather low number of studies, the Q-static was reduced in power, and I2 could have been biased. Finally, this study was prone to publication bias and other risks of bias and was limited only to the information reported in the studies.
Conclusions
We found moderate- and low-quality evidence supporting behavioral therapy–based digital tools improving pain intensity, physical function, and self-efficacy in the short term. Low- and very-low-quality evidence demonstrated uncertain effects of physical activity on HRQoL or its long-term effects. However, affective interactions between patients and professionals may affect clinical outcomes. Our findings should be evaluated by clinicians, stakeholders, and researchers, considering that most digital tools currently have low or very low certainty of evidence. Our findings highlight the need to conduct large-scale trials with high methodological quality.
Acknowledgments
This work was supported by the Shanghai Municipal Education Commission (2024AIYB014), Huashan Hospital, Fudan University Clinical Research Project (2023YN007), and Shanghai Soft Science Project (24692108200). We thank the members of our steering committee for their oversight and expert guidance. We also thank the stakeholders who contributed to our project management group and people with lived experience of receiving or providing exercise therapy for patients with osteoarthritis who took part in the stakeholder workshops and web-based surveys for their useful feedback.
Abbreviations
- BCT
behavior change technique
- CBT
cognitive behavioral therapy
- GRADE
Grading of Recommendations Assessment, Development, and Evaluation
- HRQoL
health-related quality of life
- OA
osteoarthritis
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- PROSPERO
International Register of Prospective Systematic Reviews
- RCT
randomized controlled trial
- SMD
standardized mean difference
PRISMA checklist.
Supplementary data, including search strategy, demographic data of the study participants, mechanisms for implementing the research intervention, functions of digital tools, and funnel plot for pain.
Data Availability
Data are available from the corresponding author on reasonable request.
Footnotes
Authors' Contributions: Conceptualization: BZ, DZ
Data curation: BZ
Formal analysis: BZ, XX
Funding acquisition: SZ
Investigation: HY, DZ
Methodology: BZ
Project administration: SZ
Resources: XX
Validation: DZ
Visualization: HY
Writing – original draft: BZ, DZ
Writing – review & editing: SZ, XX
Conflicts of Interest: None declared.
References
- 1.Arden Nigel, Nevitt Michael C. Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol. 2006 Feb;20(1):3–25. doi: 10.1016/j.berh.2005.09.007.S1521-6942(05)00108-7 [DOI] [PubMed] [Google Scholar]
- 2.Allen K, Thoma L, Golightly Y. Epidemiology of osteoarthritis. Osteoarthritis Cartilage. 2022 Feb;30(2):184–195. doi: 10.1016/j.joca.2021.04.020. https://linkinghub.elsevier.com/retrieve/pii/S1063-4584(21)00886-4 .S1063-4584(21)00886-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hunter DJ, March L, Chew M. Osteoarthritis in 2020 and beyond: a Lancet Commission. Lancet. 2020 Nov 28;396(10264):1711–1712. doi: 10.1016/S0140-6736(20)32230-3.S0140-6736(20)32230-3 [DOI] [PubMed] [Google Scholar]
- 4.Quicke J, Conaghan P, Corp N, Peat G. Osteoarthritis Cartilage. 2022 Feb;30(2):196–206. doi: 10.1016/j.joca.2021.10.003. https://linkinghub.elsevier.com/retrieve/pii/S1063-4584(21)00934-1 .S1063-4584(21)00934-1 [DOI] [PubMed] [Google Scholar]
- 5.Abramoff B, Caldera FE. Osteoarthritis: pathology, diagnosis, and treatment options. Med Clin North Am. 2020 Mar;104(2):293–311. doi: 10.1016/j.mcna.2019.10.007.S0025-7125(19)30113-0 [DOI] [PubMed] [Google Scholar]
- 6.Bannuru R, Osani M, Vaysbrot E, Arden N, Bennell K, Bierma-Zeinstra S, Kraus V, Lohmander L, Abbott J, Bhandari M, Blanco F, Espinosa R, Haugen I, Lin J, Mandl L, Moilanen E, Nakamura N, Snyder-Mackler L, Trojian T, Underwood M, McAlindon T. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019 Nov;27(11):1578–1589. doi: 10.1016/j.joca.2019.06.011. https://linkinghub.elsevier.com/retrieve/pii/S1063-4584(19)31116-1 .S1063-4584(19)31116-1 [DOI] [PubMed] [Google Scholar]
- 7.Rostron ZPJ, Green RA, Kingsley M, Zacharias A. Efficacy of exercise-based rehabilitation programs for improving muscle function and size in people with hip osteoarthritis: a systematic review with meta-analysis. Biology (Basel) 2021 Nov 30;10(12):1251. doi: 10.3390/biology10121251. https://www.mdpi.com/resolver?pii=biology10121251 .biology10121251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whittaker J, Truong L, Dhiman K, Beck C. Osteoarthritis year in review 2020: rehabilitation and outcomes. Osteoarthritis Cartilage. 2021 Feb;29(2):190–207. doi: 10.1016/j.joca.2020.10.005. https://linkinghub.elsevier.com/retrieve/pii/S1063-4584(20)31176-6 .S1063-4584(20)31176-6 [DOI] [PubMed] [Google Scholar]
- 9.Fan I, Govil D, Semciw A. The effectiveness of exercise based digital health interventions (requiring internet) in management of hip and knee osteoarthritis: a systematic review and meta-analysis. Osteoarthritis and Cartilage. 2022 Apr;30:S402. doi: 10.1016/j.joca.2022.02.540. [DOI] [Google Scholar]
- 10.Zhang L, Fu T, Zhang Q, Yin R, Zhu L, He Y, Fu W, Shen B. Effects of psychological interventions for patients with osteoarthritis: a systematic review and meta-analysis. Psychol Health Med. 2018 Jan;23(1):1–17. doi: 10.1080/13548506.2017.1282160. [DOI] [PubMed] [Google Scholar]
- 11.Haynes SN, O'Brien WH. Functional analysis in behavior therapy. Clinical Psychology Review. 1990 Jan;10(6):649–668. doi: 10.1016/0272-7358(90)90074-k. [DOI] [Google Scholar]
- 12.Sutton S. The contribution of behavioural science to primary care research: development and evaluation of behaviour change interventions. Prim Health Care Res Dev. 2011 Jun 22;12(04):284–292. doi: 10.1017/s1463423611000168. [DOI] [PubMed] [Google Scholar]
- 13.O'Leary A, Shoor S, Lorig K, Holman HR. A cognitive-behavioral treatment for rheumatoid arthritis. Health Psychol. 1988;7(6):527–44. doi: 10.1037//0278-6133.7.6.527. [DOI] [PubMed] [Google Scholar]
- 14.Early BP, Grady MD. Embracing the contribution of both behavioral and cognitive theories to cognitive behavioral therapy: Maximizing the richness. Clin Soc Work J. 2016 Jun 14;45(1):39–48. doi: 10.1007/s10615-016-0590-5. [DOI] [Google Scholar]
- 15.Longmore RJ, Worrell M. Do we need to challenge thoughts in cognitive behavior therapy? Clin Psychol Rev. 2007 Mar;27(2):173–87. doi: 10.1016/j.cpr.2006.08.001.S0272-7358(06)00081-X [DOI] [PubMed] [Google Scholar]
- 16.Hekler EB, Michie S, Pavel M, Rivera DE, Collins LM, Jimison HB, Garnett C, Parral S, Spruijt-Metz D. Advancing models and theories for digital behavior change interventions. Am J Prev Med. 2016 Nov;51(5):825–832. doi: 10.1016/j.amepre.2016.06.013. https://europepmc.org/abstract/MED/27745682 .S0749-3797(16)30241-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barlow J. How to use education as an intervention in osteoarthritis. Best Pract Res Clin Rheumatol. 2001 Oct;15(4):545–58. doi: 10.1053/berh.2001.0172.S152169420190172X [DOI] [PubMed] [Google Scholar]
- 18.Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns. 2002;48(2):177–87. doi: 10.1016/s0738-3991(02)00032-0.S0738399102000320 [DOI] [PubMed] [Google Scholar]
- 19.Jönsson Therese, Dell'Isola Andrea, Lohmander LS, Wagner P, Cronström Anna. Comparison of face-to-face vs digital delivery of an osteoarthritis treatment program for hip or knee osteoarthritis. JAMA Netw Open. 2022 Nov 01;5(11):e2240126. doi: 10.1001/jamanetworkopen.2022.40126. https://europepmc.org/abstract/MED/36326763 .2798148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lindberg MF, Aamodt A, Badawy M, Bergvad IB, Borchgrevink P, Furnes O, Gay C, Heir S, Holm I, Indrekvam K, Kise N, Lau B, Magnussen J, Nerhus TK, Rognsvåg Turid, Rudsengen DE, Rustøen Tone, Skou ST, Stubberud J, Småstuen Milada S, Lerdal A. The effectiveness of exercise therapy and education plus cognitive behavioral therapy, alone or in combination with total knee arthroplasty in patients with knee osteoarthritis - study protocol for the MultiKnee trial. BMC Musculoskelet Disord. 2021 Dec 20;22(1):1054. doi: 10.1186/s12891-021-04924-z. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-021-04924-z .10.1186/s12891-021-04924-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Larkin L, Gallagher S, Cramp F, Brand C, Fraser A, Kennedy N. Behaviour change interventions to promote physical activity in rheumatoid arthritis: a systematic review. Rheumatol Int. 2015 Oct;35(10):1631–40. doi: 10.1007/s00296-015-3292-3.10.1007/s00296-015-3292-3 [DOI] [PubMed] [Google Scholar]
- 22.Birch S, Stilling M, Mechlenburg I, Hansen TB. No effect of cognitive behavioral patient education for patients with pain catastrophizing before total knee arthroplasty: a randomized controlled trial. Acta Orthop. 2020 Feb;91(1):98–103. doi: 10.1080/17453674.2019.1694312. https://www.tandfonline.com/doi/abs/10.1080/17453674.2019.1694312?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Willett M, Duda J, Fenton S, Gautrey C, Greig C, Rushton A. Effectiveness of behaviour change techniques in physiotherapy interventions to promote physical activity adherence in lower limb osteoarthritis patients: A systematic review. PLoS One. 2019;14(7):e0219482. doi: 10.1371/journal.pone.0219482. https://dx.plos.org/10.1371/journal.pone.0219482 .PONE-D-18-07127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nelligan RK, Hinman RS, Kasza J, Crofts SJC, Bennell KL. Effects of a self-directed web-based strengthening exercise and physical activity program supported by automated text messages for people with knee osteoarthritis: a randomized clinical trial. JAMA Intern Med. 2021 Jun 01;181(6):776–785. doi: 10.1001/jamainternmed.2021.0991. https://europepmc.org/abstract/MED/33843948 .2778536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pearson J, Walsh N, Carter D, Koskela S, Hurley M. Developing a web-based version of an exercise-based rehabilitation program for people with chronic knee and hip pain: a mixed methods study. JMIR Res Protoc. 2016 May 19;5(2):e67. doi: 10.2196/resprot.5446. https://www.researchprotocols.org/2016/2/e67/ v5i2e67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pelle T, Bevers K, van der Palen J, van den Hoogen F, van den Ende C. Effect of the dr. Bart application on healthcare use and clinical outcomes in people with osteoarthritis of the knee and/or hip in the Netherlands; a randomized controlled trial. Osteoarthritis Cartilage. 2020 Apr;28(4):418–427. doi: 10.1016/j.joca.2020.02.831. https://linkinghub.elsevier.com/retrieve/pii/S1063-4584(20)30900-6 .S1063-4584(20)30900-6 [DOI] [PubMed] [Google Scholar]
- 27.Dantas LO, Salvini TDF, McAlindon TE. Knee osteoarthritis: key treatments and implications for physical therapy. Braz J Phys Ther. 2021;25(2):135–146. doi: 10.1016/j.bjpt.2020.08.004. https://europepmc.org/abstract/MED/33262080 .S1413-3555(20)30243-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang X, Hunter DJ, Vesentini G, Pozzobon D, Ferreira ML. Technology-assisted rehabilitation following total knee or hip replacement for people with osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019 Nov 03;20(1):506. doi: 10.1186/s12891-019-2900-x. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-019-2900-x .10.1186/s12891-019-2900-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hewitt S, Sephton R, Yeowell G. The effectiveness of digital health interventions in the management of musculoskeletal conditions: systematic literature review. J Med Internet Res. 2020 Jun 05;22(6):e15617. doi: 10.2196/15617. https://www.jmir.org/2020/6/e15617/ v22i6e15617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bunting J, Withers T, Heneghan N, Greaves C. Digital interventions for promoting exercise adherence in chronic musculoskeletal pain: a systematic review and meta-analysis. Physiotherapy. 2021 Jun;111:23–30. doi: 10.1016/j.physio.2020.08.001.S0031-9406(20)30403-X [DOI] [PubMed] [Google Scholar]
- 31.Durst J, Roesel I, Sudeck G, Sassenberg K, Krauss I. Effectiveness of human versus computer-based instructions for exercise on physical activity-related health competence in patients with hip osteoarthritis: randomized noninferiority crossover trial. J Med Internet Res. 2020 Sep 28;22(9):e18233. doi: 10.2196/18233. https://www.jmir.org/2020/9/e18233/ v22i9e18233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Allen K, Arbeeva L, Callahan L, Golightly Y, Goode A, Heiderscheit B, Huffman K, Severson H, Schwartz T. Physical therapy vs internet-based exercise training for patients with knee osteoarthritis: results of a randomized controlled trial. Osteoarthritis Cartilage. 2018 Mar;26(3):383–396. doi: 10.1016/j.joca.2017.12.008. https://linkinghub.elsevier.com/retrieve/pii/S1063-4584(17)31381-X .S1063-4584(17)31381-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shah N, Costello K, Mehta A, Kumar D. Applications of digital health technologies in knee osteoarthritis: narrative review. JMIR Rehabil Assist Technol. 2022 Jun 08;9(2):e33489. doi: 10.2196/33489. https://rehab.jmir.org/2022/2/e33489/ v9i2e33489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Safari R, Jackson J, Sheffield D. Digital self-management interventions for people with osteoarthritis: systematic review with meta-analysis. J Med Internet Res. 2020 Jul 20;22(7):e15365. doi: 10.2196/15365. https://www.jmir.org/2020/7/e15365/ v22i7e15365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bennell KL, Campbell PK, Egerton T, Metcalf B, Kasza J, Forbes A, Bills C, Gale J, Harris A, Kolt GS, Bunker SJ, Hunter DJ, Brand CA, Hinman RS. Telephone coaching to enhance a home-based physical activity program for knee osteoarthritis: a randomized clinical trial. Arthritis Care Res (Hoboken) 2017 Jan;69(1):84–94. doi: 10.1002/acr.22915. [DOI] [PubMed] [Google Scholar]
- 36.Bennell K, Nelligan RK, Schwartz S, Kasza J, Kimp A, Crofts SJ, Hinman RS. Behavior change text messages for home exercise adherence in knee osteoarthritis: randomized trial. J Med Internet Res. 2020 Sep 28;22(9):e21749. doi: 10.2196/21749. https://www.jmir.org/2020/9/e21749/ v22i9e21749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berry A, McCabe CS, Muir S, Walsh N. Digital behaviour change interventions to facilitate physical activity in osteoarthritis: a systematic review. Physical Therapy Reviews. 2018 Jul 02;23(3):197–206. doi: 10.1080/10833196.2018.1470747. [DOI] [Google Scholar]
- 38.Page Matthew J, McKenzie Joanne E, Bossuyt Patrick M, Boutron Isabelle, Hoffmann Tammy C, Mulrow Cynthia D, Shamseer Larissa, Tetzlaff Jennifer M, Akl Elie A, Brennan Sue E, Chou Roger, Glanville Julie, Grimshaw Jeremy M, Hróbjartsson Asbjørn, Lalu Manoj M, Li Tianjing, Loder Elizabeth W, Mayo-Wilson Evan, McDonald Steve, McGuinness Luke A, Stewart Lesley A, Thomas James, Tricco Andrea C, Welch Vivian A, Whiting Penny, Moher David. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71. doi: 10.1136/bmj.n71. https://www.bmj.com/lookup/pmidlookup?view=long&pmid=33782057 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, West Sussex, England: John Wiley & Sons Ltd, The Atrium; 1961. Mar, [Google Scholar]
- 40.Jüni Peter, Reichenbach S, Dieppe P. Osteoarthritis: rational approach to treating the individual. Best Pract Res Clin Rheumatol. 2006 Aug;20(4):721–40. doi: 10.1016/j.berh.2006.05.002.S1521-6942(06)00050-7 [DOI] [PubMed] [Google Scholar]
- 41.Moher D, Liberati Alessandro, Tetzlaff Jennifer, Altman Douglas G, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009 Aug 18;151(4):264–9, W64. doi: 10.7326/0003-4819-151-4-200908180-00135. https://www.acpjournals.org/doi/abs/10.7326/0003-4819-151-4-200908180-00135?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .0000605-200908180-00135 [DOI] [PubMed] [Google Scholar]
- 42.Wientzek AV, Vigl Matthäus, Steindorf Karen, Brühmann Boris, Bergmann Manuela M, Harttig Ulrich, Katzke Verena, Kaaks Rudolf, Boeing Heiner. The improved physical activity index for measuring physical activity in EPIC Germany. PLoS One. 2014;9(3):e92005. doi: 10.1371/journal.pone.0092005. https://dx.plos.org/10.1371/journal.pone.0092005 .PONE-D-13-46617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008 Apr 24;336(7650):924–926. doi: 10.1136/bmj.39489.470347.ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Salanti G, Del Giovane C, Chaimani A, Caldwell DM, Higgins JPT. Evaluating the quality of evidence from a network meta-analysis. PLoS One. 2014;9(7):e99682. doi: 10.1371/journal.pone.0099682. https://dx.plos.org/10.1371/journal.pone.0099682 .PONE-D-14-01780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.No authors listed A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2015 Jun 17;350:h3326. doi: 10.1136/bmj.h3326. [DOI] [PubMed] [Google Scholar]
- 46.Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York: Routledge; 2013. [Google Scholar]
- 47.Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Glasziou P, Jaeschke R, Akl EA, Norris S, Vist G, Dahm P, Shukla VK, Higgins J, Falck-Ytter Y, Schünemann Holger J, GRADE Working Group GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol. 2011 Dec;64(12):1294–302. doi: 10.1016/j.jclinepi.2011.03.017.S0895-4356(11)00182-X [DOI] [PubMed] [Google Scholar]
- 48.Rini Christine, Porter Laura S, Somers Tamara J, McKee Daphne C, DeVellis Robert F, Smith Meredith, Winkel Gary, Ahern David K, Goldman Roberta, Stiller Jamie L, Mariani Cara, Patterson Carol, Jordan Joanne M, Caldwell David S, Keefe Francis J. Automated Internet-based pain coping skills training to manage osteoarthritis pain: a randomized controlled trial. Pain. 2015 May;156(5):837–848. doi: 10.1097/j.pain.0000000000000121. https://europepmc.org/abstract/MED/25734997 .00006396-201505000-00011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hinman RS, Campbell PK, Lawford BJ, Briggs AM, Gale J, Bills C, Kasza J, Harris A, French SD, Bunker SJ, Forbes A, Bennell KL. Does telephone-delivered exercise advice and support by physiotherapists improve pain and/or function in people with knee osteoarthritis? Telecare randomised controlled trial. Br J Sports Med. 2020 Jul;54(13):790–797. doi: 10.1136/bjsports-2019-101183.bjsports-2019-101183 [DOI] [PubMed] [Google Scholar]
- 50.McCurry SM, Zhu W, Von Korff M, Wellman R, Morin CM, Thakral M, Yeung K, Vitiello MV. Effect of telephone cognitive behavioral therapy for insomnia in older adults with osteoarthritis pain: a randomized clinical trial. JAMA Intern Med. 2021 Apr 01;181(4):530–538. doi: 10.1001/jamainternmed.2020.9049. https://europepmc.org/abstract/MED/33616613 .2776286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mecklenburg G, Smittenaar P, Erhart-Hledik JC, Perez DA, Hunter S. Effects of a 12-week digital care program for chronic knee pain on pain, mobility, and surgery risk: randomized controlled trial. J Med Internet Res. 2018 Apr 25;20(4):e156. doi: 10.2196/jmir.9667. https://www.jmir.org/2018/4/e156/ v20i4e156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kloek Corelien J J, Bossen Daniël, Spreeuwenberg Peter M, Dekker Joost, de Bakker Dinny H, Veenhof Cindy. Effectiveness of blended physical therapist intervention in people with hip osteoarthritis, knee osteoarthritis, or both: a cluster-randomized controlled trial. Phys Ther. 2018 Jul 01;98(7):560–570. doi: 10.1093/ptj/pzy045. https://europepmc.org/abstract/MED/29788253 .4998860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li LC, Feehan LM, Xie H, Lu N, Shaw CD, Gromala D, Zhu S, Aviña-Zubieta J Antonio, Hoens AM, Koehn C, Tam J, Therrien S, Townsend AF, Noonan G, Backman CL. Effects of a 12-week multifaceted wearable-based program for people with knee osteoarthritis: randomized controlled trial. JMIR Mhealth Uhealth. 2020 Jul 03;8(7):e19116. doi: 10.2196/19116. https://mhealth.jmir.org/2020/7/e19116/ v8i7e19116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen H, Chuang T, Lin P, Lin Y, Chuang Y. Effects of messages delivered by mobile phone on increasing compliance with shoulder exercises among patients with a frozen shoulder. J Nurs Scholarsh. 2017 Jul;49(4):429–437. doi: 10.1111/jnu.12308. [DOI] [PubMed] [Google Scholar]
- 55.Tack C. A model of integrated remote monitoring and behaviour change for osteoarthritis. BMC Musculoskelet Disord. 2021 Aug 09;22(1):669. doi: 10.1186/s12891-021-04555-4. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-021-04555-4 .10.1186/s12891-021-04555-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xie S, Wang Q, Wang L, Wang L, Song K, He C. Effect of internet-based rehabilitation programs on improvement of pain and physical function in patients with knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J Med Internet Res. 2021 Jan 5;23(1):e21542. doi: 10.2196/21542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cenamor J. Use of health self-management platform features: The case of a specialist ehealth app. Technological Forecasting and Social Change. 2022 Dec;185:122066. doi: 10.1016/j.techfore.2022.122066. [DOI] [Google Scholar]
- 58.Batrakoulis A, Jamurtas AZ, Metsios GS, Perivoliotis K, Liguori G, Feito Y, Riebe D, Thompson WR, Angelopoulos TJ, Krustrup P, Mohr M, Draganidis D, Poulios A, Fatouros IG. Comparative efficacy of 5 exercise types on cardiometabolic health in overweight and obese adults: a systematic review and network meta-analysis of 81 randomized controlled trials. Circ: Cardiovascular Quality and Outcomes. 2022 Jun;15(6):e008243. doi: 10.1161/circoutcomes.121.008243. [DOI] [PubMed] [Google Scholar]
- 59.Solis-Navarro L, Gismero A, Fernández-Jané Carles, Torres-Castro R, Solá-Madurell Mireia, Bergé Clara, Pérez Laura Mónica, Ars Joan, Martín-Borràs Carme, Vilaró Jordi, Sitjà-Rabert Mercè. Effectiveness of home-based exercise delivered by digital health in older adults: a systematic review and meta-analysis. Age Ageing. 2022 Nov 02;51(11):afac243. doi: 10.1093/ageing/afac243. https://europepmc.org/abstract/MED/36346736 .6806169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang M, Wang W, Li M, Sheng H, Zhai Y. Efficacy of mobile health applications to improve physical activity and sedentary behavior: a systematic review and meta-analysis for physically inactive individuals. Int J Environ Res Public Health. 2022 Apr 18;19(8):4905. doi: 10.3390/ijerph19084905. https://www.mdpi.com/resolver?pii=ijerph19084905 .ijerph19084905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yadav L, Haldar A, Jasper U, Taylor A, Visvanathan R, Chehade M, Gill T. Utilising digital health technology to support patient-heath care provider communication in fragility fracture recovery: systematic review and meta-analysis. Int J Environ Res Public Health. 2019 Oct 22;16(20):4047. doi: 10.3390/ijerph16204047. https://www.mdpi.com/resolver?pii=ijerph16204047 .ijerph16204047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Seppen BF, den Boer P, Wiegel J, Ter Wee Marieke M, van der Leeden M, de Vries R, van der Esch M, Bos WH. Asynchronous mHealth interventions in rheumatoid arthritis: systematic scoping review. JMIR Mhealth Uhealth. 2020 Nov 05;8(11):e19260. doi: 10.2196/19260. https://mhealth.jmir.org/2020/11/e19260/ v8i11e19260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Baumeister H, Kraft R, Baumel A, Pryss R, Eva-Maria M. Digital Phenotyping and Mobile Sensing: New Developments in Psychoinformatics. Heidelberg: Cham: Springer International Publishing; 2022. Persuasive e-Health design for behavior change; pp. 347–364. [Google Scholar]
- 64.Resnick B. Self-efficacy. Middle Range Theory for Nursing. 2008:1–14. doi: 10.1891/9780826159922.0010. [DOI] [Google Scholar]
- 65.Nash VR, Ponto J, Townsend C, Nelson P, Bretz MN. Cognitive behavioral therapy, self-efficacy, and depression in persons with chronic pain. Pain Manag Nurs. 2013 Dec;14(4):e236–e243. doi: 10.1016/j.pmn.2012.02.006.S1524-9042(12)00045-8 [DOI] [PubMed] [Google Scholar]
- 66.Rabenbauer LM, Mevenkamp N. Factors in the effectiveness of e-health interventions for chronic back pain: how self-efficacy mediates e-health literacy and healthy habits. Telemed J E Health. 2021 Feb;27(2):184–192. doi: 10.1089/tmj.2019.0301. [DOI] [PubMed] [Google Scholar]
- 67.Valentijn PP, Tymchenko L, Jacobson T, Kromann J, Biermann CW, AlMoslemany MA, Arends RY. Digital health interventions for musculoskeletal pain conditions: systematic review and meta-analysis of randomized controlled trials. J Med Internet Res. 2022 Sep 06;24(9):e37869. doi: 10.2196/37869. https://www.jmir.org/2022/9/e37869/ v24i9e37869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Webb J, Stewart D. Let's Move with Leon. A randomised controlled trial of a UK digital intervention to improve physical activity in people with a musculoskeletal condition. Public Health. 2023 Apr;217:125–132. doi: 10.1016/j.puhe.2023.01.030. https://linkinghub.elsevier.com/retrieve/pii/S0033-3506(23)00045-8 .S0033-3506(23)00045-8 [DOI] [PubMed] [Google Scholar]
- 69.Yardley L, Spring BJ, Riper H, Morrison LG, Crane DH, Curtis K, Merchant GC, Naughton F, Blandford A. Understanding and promoting effective engagement with digital behavior change interventions. Am J Prev Med. 2016 Nov;51(5):833–842. doi: 10.1016/j.amepre.2016.06.015.S0749-3797(16)30243-4 [DOI] [PubMed] [Google Scholar]
- 70.Moller AC, Merchant G, Conroy DE, West R, Hekler E, Kugler KC, Michie S. Applying and advancing behavior change theories and techniques in the context of a digital health revolution: proposals for more effectively realizing untapped potential. J Behav Med. 2017 Feb;40(1):85–98. doi: 10.1007/s10865-016-9818-7. https://europepmc.org/abstract/MED/28058516 .10.1007/s10865-016-9818-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kroon Féline P B, van der Burg Lennart R A, Buchbinder Rachelle, Osborne Richard H, Johnston Renea V, Pitt Veronica. Self-management education programmes for osteoarthritis. Cochrane Database Syst Rev. 2014 Jan 15;2014(1):CD008963. doi: 10.1002/14651858.CD008963.pub2. https://europepmc.org/abstract/MED/24425500 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Clarkson P, Vassilev I, Rogers A, Brooks C, Wilson N, Lawson J, Adams J. Integrating a Web-Based Self-Management Tool (Managing Joint Pain on the Web and Through Resources) for People With Osteoarthritis-Related Joint Pain With a Web-Based Social Network Support Tool (Generating Engagement in Network Involvement): Design, Development, and Early Evaluation. JMIR Form Res. 2020 Nov 26;4(11):e18565. doi: 10.2196/18565. https://formative.jmir.org/2020/11/e18565/ v4i11e18565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hurley DA, Keogh A, Mc Ardle D, Hall AM, Richmond H, Guerin S, Magdalinski T, Matthews J. Evaluation of an e-learning training program to support implementation of a group-based, theory-driven, self-management intervention for osteoarthritis and low-back pain: pre-post study. J Med Internet Res. 2019 Mar 07;21(3):e11123. doi: 10.2196/11123. https://www.jmir.org/2019/3/e11123/ v21i3e11123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Slater H, Dear BF, Merolli MA, Li LC, Briggs AM. Use of eHealth technologies to enable the implementation of musculoskeletal Models of Care: Evidence and practice. Best Pract Res Clin Rheumatol. 2016 Jun;30(3):483–502. doi: 10.1016/j.berh.2016.08.006. https://linkinghub.elsevier.com/retrieve/pii/S1521-6942(16)30046-8 .S1521-6942(16)30046-8 [DOI] [PubMed] [Google Scholar]
- 75.Bender Jacqueline L, Radhakrishnan Arun, Diorio Caroline, Englesakis Marina, Jadad Alejandro R. Can pain be managed through the Internet? A systematic review of randomized controlled trials. Pain®. 2011;152(8):1740–1750. doi: 10.1016/j.pain.2011.02.012.00006396-201108000-00013 [DOI] [PubMed] [Google Scholar]
- 76.Östlind Elin, Ekvall Hansson E, Eek F, Stigmar K. Experiences of activity monitoring and perceptions of digital support among working individuals with hip and knee osteoarthritis - a focus group study. BMC Public Health. 2022 Aug 30;22(1):1641. doi: 10.1186/s12889-022-14065-0. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-022-14065-0 .10.1186/s12889-022-14065-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Stuhlreyer J, Roder C, Krug F, Zöllner Christian, Flor H, Klinger R. A digital application and augmented physician rounds reduce postoperative pain and opioid consumption after primary total knee replacement (TKR): a randomized clinical trial. BMC Med. 2022 Dec 05;20(1):469. doi: 10.1186/s12916-022-02638-0. https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-022-02638-0 .10.1186/s12916-022-02638-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Timmers T, Janssen L, van der Weegen W, Das D, Marijnissen W, Hannink G, van der Zwaard BC, Plat A, Thomassen B, Swen J, Kool RB, Lambers Heerspink FO. The effect of an app for day-to-day postoperative care education on patients with total knee replacement: randomized controlled trial. JMIR Mhealth Uhealth. 2019 Oct 21;7(10):e15323. doi: 10.2196/15323. https://mhealth.jmir.org/2019/10/e15323/ v7i10e15323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mrklas KJ, Barber T, Campbell-Scherer D, Green LA, Li LC, Marlett N, Miller J, Shewchuk B, Teare S, Wasylak T, Marshall DA. Co-Design in the development of a mobile health app for the management of knee osteoarthritis by patients and physicians: qualitative study. JMIR Mhealth Uhealth. 2020 Jul 10;8(7):e17893. doi: 10.2196/17893. https://mhealth.jmir.org/2020/7/e17893/ v8i7e17893 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist.
Supplementary data, including search strategy, demographic data of the study participants, mechanisms for implementing the research intervention, functions of digital tools, and funnel plot for pain.
Data Availability Statement
Data are available from the corresponding author on reasonable request.


