Highlights
-
•
This umbrella review of 70 systematic reviews (43 with meta-analyses) highlights with low-to-moderate certainty that exercise therapy and leisure-time physical activity provide small benefits for managing pain and disability in low back pain (LBP) and preventing recurrence. Exercises such as Pilates, motor control, and yoga show particular promise in short-term outcomes.
-
•
Minor adverse events, including post-exercise soreness and temporary pain increases, were reported in less than 31% of reviews, predominantly linked to yoga. No serious adverse events were identified, but harms of exercise therapy and physical activity remain underexplored in the reviews.
-
•
Motor control and Pilates were favored in network meta-analyses for reducing pain, though evidence certainty is low. Further research is needed to address limitations in data on adverse outcomes and long-term benefits.
Keywords: Physical activity, Exercise therapy, Management, Prevention, Low back pain
Abstract
Purpose
The purpose of this umbrella review was to synthesize the evidence from systematic reviews on the benefits and harms of exercise therapy and physical activity (PA) for the secondary prevention and management of low back pain (LBP).
Methods
An umbrella review was conducted to evaluate the effectiveness of exercise therapy and PA in the management and secondary prevention of LBP. A systematic search was performed in MEDLINE, CINAHL, Scopus, Web of Science, Cochrane Database of Systematic Reviews, and Physiotherapy Evidence Database (PEDro), including reference lists of relevant reviews, covering studies published between January 1, 2010 and May 20, 2024. Eligible studies were systematic reviews of randomized controlled trials and observational studies, with or without meta-analyses. The primary outcome for secondary prevention was LBP recurrence, while for management, primary outcomes included pain intensity and disability, with adverse events as secondary outcomes. Data were extracted across immediate, short-term, intermediate, and long-term follow-up periods. The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) framework was used to assess the certainty of evidence, and the Assessment of Multiple Systematic Reviews tool (AMSTAR) tool was applied by 2 independent reviewers (JC, QL, and/or DXMW) to evaluate the quality of the included reviews. The study was prospectively registered on the Open Science Framework (OSF).
Results
A total of 70 systematic reviews were included, 43 with meta-analyses, 7 with network meta-analyses, and 20 without meta-analyses. Six (out of 10) reviews with meta-analyses for secondary prevention indicated a small benefit from general exercises and leisure-time PA (low-to-moderate certainty). For LBP management, 35 (out of 36) reviews reported that exercise therapies such as Pilates, motor control, mixed exercise, Tai Chi, water-based exercises, and yoga showed small beneficial effects on pain and disability compared to minimal intervention mainly in the short-term (low-to-moderate certainty). Seven network meta-analyses favored motor control and Pilates over other forms of exercise to reduce pain (low certainty). Adverse events were reported in less than 31% of the reviews, predominantly involving post-exercise soreness and temporary increases in pain, mainly in yoga-related studies. Adverse events were considered minor, and no serious adverse events were reported.
Conclusion
There is low-to-moderate certainty that exercise therapy and leisure-time PA are beneficial for improving pain and preventing the recurrence of LBP. However, evidence on the potential harms of these interventions is limited, and adverse events related to exercise and PA remain under-investigated.
Graphical abstract
1. Introduction
Low back pain (LBP) is a significant contributor to the global prevalence of disability.1 While many individuals find significant relief from an episode of LBP within 6–12 weeks, about two-thirds will experience a recurrence within 12 months.2 Despite its high prevalence, treatment options for LBP, such as pain medication, spinal injections, and surgery, often result in small clinical benefits, leading to a significant economic burden on both individuals and healthcare systems.3,4 Recently, a shift in management towards a patient-centered approach, focusing on the implementation of effective care that supports people to adopt healthy lifestyles, has been strongly advocated worldwide.5, 6, 7
For overall health benefits, the World Health Organization (WHO) recommends that people should engage in at least 150–300 min of moderate-intensity or at least 75–150 min of vigorous-intensity aerobic physical activity (PA), performed in any domain (e.g., recreational or incidental), throughout the week.8 Additionally, the WHO clinical guidelines for the management of chronic LBP recommend structured exercise programs, which may include aerobic exercise, muscle strength training, stretching, flexibility or mobilizing exercises, yoga, core strengthening, motor control exercise, and functional restoration exercise. Evidence from previous large observational studies also suggests that regular engagement in PA is associated with longevity and lower incidence of chronic diseases, whereas an excessively sedentary lifestyle is associated with a shorter lifespan and health span,9,10 and recent 2020 global guidelines acknowledge that “all activity counts”, regardless of dosage, intensity, or type.8
For managing LBP, the benefits of different types and amounts of PA remain uncertain.11 For instance, moderate levels of PA, particularly during leisure time (e.g., walking, jogging, and recreational sports), may have a protective effect against LBP. However, high levels of PA (defined as ≥21 metabolic equivalent task (MET)-h per week) do not appear to offer additional benefits and may sometimes show no clear association with LBP. Individuals who engage in both heavy domestic activities (e.g., vigorous gardening or heavy yard work) and heavy recreational PA (involving high bouts of light, moderate, and vigorous activity combined) have reported a higher risk of experiencing LBP episodes compared to those who avoid heavy PAs.12
Exercises such as Pilates, core strengthening, yoga, and Tai Chi are frequently recommended for LBP management due to their demonstrated benefits in improving flexibility, strength, and overall physical function.13 While LBP guidelines generally emphasize maintaining PA, there is variation in the types of exercise modalities recommended (e.g., aerobic exercises, walking, yoga, strengthening), and not all guidelines reflect the most current evidence. Systematic reviews of LBP guidelines have identified inconsistencies in recommendations, contributing to confusion among healthcare providers and patients regarding the most effective interventions.14,15 This lack of clarity may negatively affect patient care and outcomes, highlighting the need for evidence-based updates to ensure the delivery of optimal care for individuals with LBP.16
Recent systematic reviews of guidelines for LBP have highlighted the lack of clarity in recommendations, particularly regarding the most effective interventions and treatment approaches.15 Furthermore, some systematic reviews have noted the variability in the recommendations provided by different guidelines, which can lead to confusion among healthcare providers and patients, and may negatively impact patient care.17,18 As a result, efforts are needed to ensure recommendations are based on the latest evidence to improve the quality of care and outcomes for individuals suffering from LBP.
The current knowledge on the benefits and harms of exercise and PA in managing and preventing LBP is yet to be mapped, systematically synthesized, and disseminated through a comprehensive high-quality report. Therefore, this umbrella review aims to synthesize the evidence on the benefits and harms of exercise and PA for the management and secondary prevention of LBP.
2. Methods
2.1. Data sources and searches
We systematically searched, extracted, and analyzed data from published systematic reviews with or without meta-analysis that investigated the role of PA and exercise therapy in the secondary prevention and/or management of LBP. This review was prospectively registered on Open Science Framework (registration DOI: https://doi.org/10.17605/OSF.IO/9PQ7B) and is reported according to the Preferred Reporting Items for Overviews of Reviews (PRIOR) statement.19
A systematic literature search was performed in the following electronic databases: MEDLINE, CINAHL, Scopus, Web of Science, Cochrane Database of Systematic Reviews, Physiotherapy Evidence Database (PEDro), and through backward citation searching20 of relevant systematic reviews and clinical guidelines from January 1, 2010 to May 20, 2024. The full search strategy can be found in Supplementary Table 1.
Two pairs of reviewers (QL and DXMW, QL and JC) independently screened all retrieved studies for eligibility in 2 stages: (a) titles and abstracts, and (b) full texts. Disagreements between reviewers were resolved by consensus or arbitration by a third reviewer (PHF). Supplementary Table 2 provides a list of ineligible reviews excluded after full-text screening. Relevant studies identified by the search were managed using EndNote 20 (Clarivate, London, UK) to remove duplicates and Covidence (Covidence Global Ltd, Melbourne, VIC, Australia) to complete the screening.
2.2. Eligibility criteria
2.2.1. Types of reviews
We included systematic reviews with or without meta-analysis of observational studies and/or randomized controlled trials (RCTs) published in peer-reviewed journals that investigated exercise therapy and PA interventions for non-specific LBP. No language restriction was applied, and only reviews that investigated the role of PA and/or exercise therapy in the adult population were included.
We considered the WHO definition of PA, which states that “physical activity is defined as any bodily movement produced by skeletal muscles that requires energy expenditure”.21 We classified PA interventions as any unstructured activity not requiring direct supervision by a health care professional. Exercise therapy was defined as a regimen or planned activity designed, prescribed, and directly supervised by a health care professional, focusing either on the management or prevention of LBP.22
We defined “systematic review” as a report that explicitly described clear research questions, with defined literature searches, inclusion criteria, and critical appraisal methods (e.g., Cochrane risk-of-bias tool for randomized trials).23 Network meta-analyses were eligible if they provided direct effects for PA or exercise interventions.
2.2.2. Systematic reviews on secondary prevention of LBP: Observational and RCT studies
For the secondary prevention of LBP, we included reviews of RCTs and/or observational studies that aimed to evaluate the effectiveness of exercise therapy and/or PA interventions on the recurrence of LBP as a primary aim. We defined recurrence of LBP as 1 or multiple episodes of LBP after a period of no symptoms or after an improved LBP status.24 For reviews of secondary prevention of LBP, we accepted any comparator group.
For the management of LBP, we included reviews of RCTs if at least 80% of the original studies aimed to evaluate the effectiveness of exercise therapy (including comparison interventions where the attributable effect of exercise could be isolated, i.e., exercise plus medication compared to same medication alone) in adults (aged ≥20 years) or PA interventions compared to minimal interventions. Eligible interventions encompassed all types of exercise, with no exclusions based on setting, mode of delivery, or degree of personalization (standardized vs. individualized).
Minimal intervention was defined as an intervention that typically employed minimal, non-invasive, non-surgical methods to manage and alleviate pain, including usual care, education, no intervention, waitlist control, or pharmacological treatment (i.e., analgesics).
2.3. Exclusion criteria
Reviews that focused on specific populations, such as children or adolescents, pregnant women, specific working populations or athletes, were excluded. Reviews that included a population with general musculoskeletal disorders (e.g., musculoskeletal pain, osteoarthritis) were excluded if data for the prevention or management were not provided separately for people with LBP. Furthermore, reviews that included studies of head-to-head comparisons, such as strengthening exercises vs. aerobic exercises, or with manual therapy were also excluded.
We followed a decision tree (Supplementary Fig. 1) to guide the process of inclusion, data extraction, and reporting of reviews (i.e., descriptive or analytical).
2.4. Outcomes
2.4.1. Systematic reviews of exercise therapy and PA for secondary prevention
The primary outcome for reviews on secondary prevention of LBP was the risk of experiencing a recurrence of LBP. We extracted estimates of LBP recurrence, such as odds ratios (ORs), risk ratios (RRs), and hazard ratios (HRs). Data on adverse events related to exercise or PA interventions were also extracted when available. All data points presenting the pertinent outcome measures were incorporated. In cases where reviews did not report specific time points, we referred to the original studies to retrieve the necessary information.
2.4.2. Systematic reviews of exercise therapy and PA for the management of LBP
The primary outcome for reviews on the management of LBP was pain and disability, measured with any instrument and reported as between-group differences along with corresponding 95% confidence intervals (95%CIs). When different instruments were used for the same clinical outcome, we presented results as mean differences and 95%CI on a common 0–100 scale. Dichotomous outcomes were converted, if necessary, to RRs and corresponding 95%CIs.
When data were presented as standardized mean differences (SMDs), we attempted to convert the data to mean difference (MD) on a 0–100 scale. When this was not possible, primary studies included in the reviews were identified, and the meta-analysis was re-calculated to present the results as MD. However, if it was not feasible due to the inability to identify primary studies, we included it in the forest plot as SMD.
Adverse events were considered secondary outcomes. We extracted data for adverse events when these were reported in the original reviews.
Treatment effect estimates were extracted and grouped into immediate (<6 weeks post-intervention), short-term (6 weeks to <3 months), intermediate (3 months to <8 months), and long-term follow-up (≥ 8 months).
2.4.3. Systematic reviews employing network meta-analysis
We included systematic reviews that employed a network meta-analysis provided that the review reported results from rankings of exercise and/or PA interventions based on direct estimate effects and Surface Under the Cumulative Ranking Curve Analyses (SUCRA) and presented the rank of exercise and/or PA interventions for the management of LBP for pain and/or disability outcomes.
2.5. Data extraction and management
Two pairs of reviewers (QL and DXMW, QL and JC) independently extracted data from eligible reviews using a pre-piloted Microsoft Excel 2024 form (Microsoft, Redmond, WA, USA). The accuracy of data extraction was confirmed by a third reviewer (PHF or PRB), and disagreements were resolved by consensus (QL, DXMW, and JC). The following data were extracted: type of review (e.g., Cochrane or non-Cochrane review), information on the type of exercise and PA and treatment regimen (e.g., dosage and duration of treatment), adverse events, number of studies included in the systematic review, and outcomes (recurrence outcomes, pain, and disability) and certainty of evidence.
Specific measurement tools were prioritized if reviews used different questionnaires to assess the same outcome for the management of LBP. We used the following hierarchy for extraction: a larger number of included studies and sample size. In addition, if the included review reported data separately for disability, we prioritized the Roland-Morris Disability Questionnaire (RMDQ) and Oswestry Disability Index (ODI).25
2.6. Methodological quality of systematic reviews
Two reviewers (JC and QL) independently assessed the methodological quality of the included systematic reviews using the Assessment of Multiple Systematic Reviews tool (AMSTAR).26 The AMSTAR is a 16-point tool for the assessment of the methodological quality of systematic reviews, with good inter-rater agreement, reliability, and content validity. For each of the 16 items, a score of 0 (answer “no”), 1 (answer “yes”), or 0.5 (answer “partial yes”) was given, summed up, and converted to a percentage (%) scale. The quality was rated as high (AMSTAR score: 11–16), moderate (AMSTAR score: 6–10), low (AMSTAR score: 1–5), or critically low (AMSTAR score <1).27
2.7. Risk of bias (RoB) of studies included in the systematic reviews
We extracted the risk of bias assessments from the reviews based on the original or revised version of the RoB.28 For reviews that used a different RoB tool, such as the Jadad or PEDro scales,29 2 independent reviewers (JC and QL) assessed the bias of each included trial that contained data for the outcomes of interest using the Cochrane RoB Version 2 (https://www.riskofbias.info/).
2.8. Certainty of evidence
The certainty of the evidence for effect estimates was assessed by 2 independent reviewers (JC and QL) using the Grading of Recommendations Assessments, Development, and Evaluation (GRADE).30 We reviewed GRADE ratings of all comparisons provided in the included reviews or graded the certainty of evidence ourselves when the review was not provided. Independent reviewers (JC and QL) also re-analyzed GRADE ratings provided in reviews when there was not an adequate justification for their grading process, or when there were significant changes in the evidence base since the original GRADE assessment. A third reviewer (PRB) was engaged to resolve any discrepancies when consensus was not reached.
The GRADE system rates the quality of evidence as high quality (further research is very unlikely to change our confidence in the estimate of effect), moderate quality (further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate), low quality (further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate), and very low quality (any estimate of effect is very uncertain). Supplementary Table 3 describes the grading process utilized by the reviewers in instances where the strength of evidence required re-assessment (i.e., inadequate reporting of the grading process, changes in the evidence base) or when it was not provided in the reviews. Evidence quality was initially set as “high” and was downgraded based on the following criteria: limitation in study design (risk of bias), inconsistency, indirectness, imprecision, and publication.31
2.9. Examining the overlap of included reviews
To address overlapping citations in systematic reviews with meta-analysis, we used a graphical cross-tabulation method known as a citation matrix, described by Pieper et al.32 This matrix lists the overlapping systematic reviews in columns and the included primary studies in rows. The degree of overlap is quantified using a measure called the corrected covered area (CCA),33 which is expressed as a percentage (%).
Overlap was categorized as very high (CCA > 15%), high (CCA: 11%–15%), moderate (CCA: 6%–10%), or slight (CCA: 0%–5%). High overlap in citations was detected through a process of acknowledging and transparently addressing the inclusion of the same studies across multiple analyses or reviews. The following formula was used to calculate CCA:
| Eq. (1) |
c = Number of included reviews
r = Number of publications of primary studies (number of rows)
N = Total number of primary study occurrences across all reviews (i.e., counting duplicates).
2.10. Data synthesis
For systematic reviews on the management of LBP that included a meta-analysis, we constructed forest plots to display the effectiveness of exercise and/or PA for the outcomes of pain and disability separately. Using Review Manager (RevMan) software Version 5.4 (Cochrane, London, UK), we re-analyzed the data provided in the systematic reviews to generate the forest plots. Due to high variability or methodological differences between studies, we opted not to present pooled estimated effects. Instead, the forest plots display individual study effect sizes and their 95%CIs, providing a clearer visual representation of the data.
Where appropriate, a random-effects model was used, reflecting the assumption of heterogeneity across studies. The forest plots report key details, including the number of included studies, authors, publication year, number of trials, direction of effect, heterogeneity, and GRADE assessment. All data were sourced from the systematic reviews.
Continuous pain and disability outcomes were converted on a scale of 0 (no pain) to 100 (worst pain) and were presented as MDs (95%CI). When a review reported the pooled estimates as SMD, we re-analyzed the data and presented estimates and 95%CIs as MDs. When 1 or more trials included in a review were regarded as not appropriate for that comparison (e.g., 1 trial had an exercise comparator),34 we excluded the trial and re-analyzed the data. For systematic reviews that did not include a meta-analysis, results were reported in a narrative summary format.
2.11. Protocol deviations
-
•
We stated in our registered protocol (https://doi.org/10.17605/OSF.IO/9PQ7B) that we would extract data on quality-of-life and return to work as a secondary outcome. During the data extraction process, we noticed that very few reviews reported data on quality-of-life and return-to-work and, therefore, decided not to include this outcome in the current report.
-
•
In our protocol, we initially specified that we would extract data from exercises and PA compared with any intervention. For consistency, and to facilitate the interpretability of our results, we only report here the results of comparisons with minimal intervention (i.e., pharmacological, usual care, and conservative treatments).
-
•
We collected data from all-time points available in the included reviews and categorized them as immediate (<6 weeks post-intervention), short (6 weeks to <3 months), intermediate (3 months to <8 months), and long-term follow-up (≥8 months), which was a departure from the original protocol that initially would focus on short-term follow-up (<3 months) only.
-
•
During the review process, we made an ad hoc decision to exclude occupational activity from the findings. This decision was not initially specified in the protocol but was implemented to focus on leisure-time and structured PA. The rationale for this exclusion was to improve the focus of the umbrella review due to the considerable variation in the methods used to measure each work-related activity, such as frequent lifting and bending/twisting of the spine. In addition, occupational PA can vary significantly in intensity and type (e.g., sedentary vs. manual labor), making it harder to compare with structured or leisure-time PA.
3. Results
3.1. Characteristics of the included systematic reviews
A total of 7611 records were identified. After excluding 3758 duplicates, 3853 records were screened for eligibility. Titles and abstracts were screened by 2 independent reviewers (JC and QL or QL and DXMW), and then 241 full texts were screened, with 70 systematic reviews included. The flowchart in Fig. 1 illustrates the selection process. Reasons for exclusion can be found in Supplementary Table 2.
Fig. 1.
Study selection flowchart. RCT = randomized controlled trial; SR = systematic review.
The 70 systematic reviews included were published between January 2010 and May 2024. Of these, 43 reviews conducted a meta-analysis, 7 reviews were network meta-analyses, and 20 reviews were reviews without meta-analysis. Together, the reviews included over 95,000 participants, covering more than 30 types of exercises or PA programs compared with minimal intervention. A total of 10 reviews assessed PA for the secondary prevention of LBP; 4 reviews were randomized controlled trials (RCTs) and 6 reviews were observational (cohort) studies.
Of the 70 systematic reviews included, 45 reviews (64%) focused on chronic LBP, 6 reviews (9%) included people with acute and subacute LBP,35, 36, 37, 38, 39, 40 3 reviews (4%) provided no information on the duration of LBP (i.e., acute or chronic) in the included studies,11,41,42 and 6 reviews (9%) included studies focusing on both acute and chronic LBP.35,36,38,39,43,44 Results regarding the specificities of the exercises (i.e., dosage, type, outcome measures and follow-up period) can be found in Supplementary Table 4.
3.2. Overlap of included reviews
We assessed the overlap of primary studies among the included systematic reviews with meta-analysis by employing a citation matrix, which facilitated the calculation of the CCA approach. The total number of times that studies appeared in reviews (N) was 397, while the number of rows (primary studies) (r) was 256, with each review encompassing an average of 43 systematic reviews with meta-analysis (c). The CCA was 0.0131, which corresponded to a CCA percentage of 1.31%. More details of overlapping citations can be found in Supplementary Fig. 2.
3.3. Summary of types of exercise therapy and PA
3.3.1. Systematic reviews on secondary prevention of LBP (n = 10)
For secondary prevention of LBP, 10 reviews were included,11,42,45, 46, 47, 48, 49, 50, 51, 52 of which, 6 reviews had a cohort design11,47,49, 50, 51, 52 and 4 reviews were RCTs.42,45,46,48 Six reviews11,42,45, 46, 47, 48 also conducted a meta-analysis. Included systematic reviews with meta-analysis are presented in Table 1. Reviews that did not present a meta-analysis can be found in Supplementary Table 4.
Table 1.
Systematic reviews with meta-analysis on secondary prevention of LBP.
| Study | Studies and study design (participants (n)) | Adverse events | Study characteristics (population and intervention) |
Outcome of interest and main findings |
Certainty of evidence |
|---|---|---|---|---|---|
| Shiri et al.47 | 36 cohort studies (n = 158, 475) |
NR | People with a history of LBP (past 6–12 months, frequent LBP, chronic LBP), mean age: NR Exposure: Regular engagement in leisure-time PA (e.g., sports) Comparison: People not regularly active in leisure time |
People who engage in moderate/highly leisure-time PA (active) may reduce the risk of having chronic LBP by 11%–16% compared to those who do not (inactive). | |
| Association between leisure-time PA and LBP LBP in the past month |
|||||
| Active vs. inactive: 5 cohort studies (n = 4974) RR = 0.98 (95%CI: 0.84–1.14); I2 = 66%, p = 0.01 |
Moderate | ||||
| Moderate vs. low PA: 3 cohort studies (n = NR) RR = 0.93 (95%CI: 0.80–1.08); I2 = 11%, p = 0.32 |
Low | ||||
| High vs. low PA: 4 cohort studies (n = 982) RR = 0.85 (95%CI: 0.53–1.37); I2 = 87%, p = 0.00 |
Low | ||||
| LBP in the past 6–12 months | |||||
| Active vs. inactive: 16 cohort studies (n = NR) RR = 0.97 (95%CI: 0.92–1.01); I2= 46%, p = 0.02 |
Low | ||||
| Moderate vs. low PA: 10 cohort studies (n = NR) RR = 0.96 (95%CI: 0.87–1.07); I2 = 0%, p = 0.47 |
Moderate | ||||
| High vs. low PA: 11 cohort studies (n = NR) RR = 0.90 (95%CI: 0.77–1.05); I2 = 51%, p = 0.02 |
Low | ||||
| High vs. low or moderate PA: 5 cohort studies (n = NR) RR = 1.01 (95%CI: 0.89–1.15); I2 = 7%, p = 0.36 |
Low | ||||
| Alzahrani et al.11,b | 24 cohort studies (n = 89, 438) |
NR | People with LBP, ages range from 18 to 100 years Intervention: PA exposure (considering leisure-time PA e.g., walking, general exercises, aerobic exercises); Volume of PA was defined by MET-h/week Comparison: NA |
Engaging in PA may reduce the risk of LBP recurrence. | |
| Levels of PA vs. LBP | |||||
| Medium (>11.89 MET-h/week and <21 MET-h/week) vs. low-level leisure-time PA and LBP: 6 cohort studies (n = 55,072) RR = 0.90 (95%CI: 0.85–0.96); I2 = 43%, p = 0.002 |
Moderate | ||||
| High (≥21 MET-h/week) vs. low-level PA and LBP: 9 cohort studies (n = 34,366) RR = 1.00 (95%CI: 0.92–1.08); I2 = 33%; p = 0.94 |
Moderate | ||||
| Alalmaee et al.46,a | 6 RCTs (n = 8632) |
NR | People with no LBP at study entry, mean age = 34 years Intervention: General exercises Comparison: Control (i.e., drug therapy and usual care) |
Meta analysis revealed a significant reduction in the incidence of LBP in the intervention group compared to the control group. | |
| Incidence of LBP | |||||
| OR = 0.59 (95%CI: 0.40–0.86); I2 = 81%, p = 0.007 | Very low | ||||
| Steffens et al.48 | 6 RCTs (n = 1232) |
NR | People with no LBP at study entry but with a history of LBP, mean age = 39 years Intervention: Exercises (e.g., endurance training, strengthening, and stretching) with or without educational interventions Comparison: Control (e.g., no intervention), minimal intervention (e.g., education) |
Exercises delivered with or without education reduced the risk of LBP compared to the control group. | |
| Exercises vs. control/minimal intervention LBP episode |
|||||
| Short-term: 4 RCTs (n = 898) RR = 0.65 (95%CI: 0.50–0.86); I2 = 67.9% |
Low | ||||
| Long-term: 2 RCTs (n = 334) RR = 1.04 (95%CI: 0.73–1.49); I2 = 0% |
Very low | ||||
| Choi et al.45 | 13 RCTs (n = 1520) |
NR | People with current LBP or who have a history of at least 1 episode of LBP, mean age NR Intervention: Exercises (i.e., strengthening) Comparison: No intervention or usual care |
Exercises were more effective than no intervention for reducing the rate of recurrences at 1 year. | |
| Time to LBP recurrence | |||||
| Medium-term (6 months to 2 years):1 RCT (n = 69) HR = 0.43 (95%CI: 0.21–0.87) p = 0.020 |
NA | ||||
| Long-term (2–5 years): 1 RCT (n = 66) MD = 0.50 (95%CI: 0.28–0.90) p = 0.021 |
NA | ||||
| Specific McKenzie exercises vs. minimal intervention (e.g., booklet) Number of people with LBP |
|||||
| Medium-term (6 months to 2 years):2 RCTs (n = 294) RR = 0.75 (95%CI: 0.42–1.35) |
Moderate | ||||
| Long-term (2 months to 5 years):1 RCT (n = 89) | NA | ||||
| MD = –0.72 (95%CI: 0.57–0.92) | |||||
| Shiri et al.42 | 8 RCTs (n = 1634) |
NR | People with current LBP or who have a history of at least 1 episode of LBP, mean age NR Intervention: Exercises (i.e., strengthening, stretching, aerobic fitness, endurance, coordination exercises, yoga) Comparison: Usual care. |
Exercise reduced the risk of LBP and disability by 33%. | |
| Risk of LBP | |||||
| Short-term (<9 months): 8 RCTs (n = 1634). RR = 0.67 (95%CI: 0.53–0.85); I2 = 23%, p = 0.25 |
Moderate |
This review included a study with people who presented with LBP at the study entry.
This systematic review also included cross-sectional data, but for our review we only extracted data from cohort studies.
Abbreviations: 95%CI = 95% confidence interval; HR = hazard ratio; LBP = low back pain; MD = mean difference; MET = metabolic equivalent of task; NA = not applicable; NR = not reported; OR = odds ratio; PA = physical activity; RCTs = randomized controlled trials; RR = risk ratio.
Six reviews of observational studies investigated non-structured and non-supervised PA categorized as leisure-time (e.g., walking, gardening, recreational PA, sports, general exercises) as the exposure.11,47,49, 50, 51, 52 The reviews of RCTs varied widely in terms of exercises and PA dosage, ranging from 1 to 144 sessions. Program durations across reviews of RCTs spanned from 2 weeks to as long as 104 weeks.
Regarding PA exposure in reviews of cohort studies, the range of PA exposure extended from 3 months to 28 years. Reviews of observational studies lacked sufficient information on the frequency and amount of PA undertaken by participants. Only 1 review47 categorized PA exposure during leisure time, prescribing a regimen of at least 1 to 2 sessions per week, with each session lasting for a minimum of 0.5–1.0 h. Characteristics of the included reviews are presented in Supplementary Table 4.
3.3.2. Systematic reviews on the management of LBP (n = 60)
Sixty reviews for the management of LBP were included,13, 34, 35, 36, 37, 38, 39, 40, 41,43,44,53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101 more than 30 different types of supervised exercises reported, including aerobic or progressive resistance training (i.e., walking and running) (n = 4, 7%);53, 54, 55, 56 aquatic exercises (i.e., hydrotherapy, water-based aerobic) (n = 3, 5%);57, 58, 59 back school (n = 3, 5%);60, 61, 62 Baduanjin exercises (n = 1, 2%);63 general exercises (i.e., strengthening, stretching, endurance training) (n = 4, 7%);38,40,64,65 McKenzie exercises (n = 1, 2%);66 mind–body (i.e., a form of multicomponent exercise that includes Tai Chi, Pilates, and yoga) (n = 1, 2%);34 mixed, exercises (i.e., Pilates, yoga, Tai Chi, strengthening, aerobic) (n = 18, 30%);13,36,37,44,67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79,100 motor control (i.e., stabilization exercises) (n = 4, 7%);38,80, 81, 82 Pilates (n = 9, 15%);41,43,83, 84, 85, 86, 87, 88, 89 yoga (n = 7, 15%);35,90, 91, 92, 93, 94,101 sling exercises (n = 2, 3%);95,96 and Tai Chi (n = 1, 2%).97
Exercise dosage ranged from 3 to 168 sessions, and the length of programs ranged from 2 to 12 months. Exercise frequency ranged from 1 to 5 times per week, and 44 (73%) of the included reviews reported an average duration of exercise sessions of at least 40 min. The time points assessed ranged from 2 weeks to 12 months.
3.4. Methodological quality of the included systematic reviews
Overall, the included reviews presented moderate to high methodological quality, with an average AMSTAR score of 12.18. A total of 53 (76%)11,13,34,37,39,40, 41, 42, 43, 44, 45,47, 48, 49, 51,53,55, 56, 57, 58, 59, 60, 61, 62,64,66,67,69,70, 71, 72, 73,75, 76, 77, 78, 79,81, 82, 83, 84,87, 88, 89, 90, 91,93,94,96, 97, 98, 99, 100 of the 70 included reviews were assessed as being of high quality (AMSTAR score 11–16), with 15 reviews35,36,46,50,52,54,65,68,74,80,92,94,95,101,102 rated as moderate quality (AMSTAR score 6–10) and 2 reviews38,85 rated as low quality (AMSTAR score 0–5). The most common biases identified included the lack of reporting of conflicts of interest (neither reported by the reviews nor by their included studies), followed by a lack of reporting of publication bias and a pre-determined protocol before conducting the review. Cochrane reviews presented higher methodological quality compared to non-Cochrane reviews. The results of the AMSTAR quality assessment are presented in Supplementary Table 5 and Supplementary Fig. 3.
3.5. Secondary prevention of LBP
3.5.1. Systematic reviews with meta-analysis (n = 6)
We included 2 reviews11,47 of cohort studies investigating the association between PA and recurrence of LBP, and 4 reviews42,45,46,48 of RCTs focusing on the prevention of a new episode of LBP with exercise therapy. Two reviews presented overlapping (>15%, very high) of primary studies.46,48
Overall, the 2 reviews11,47 of observational studies found that people who engaged in moderate levels of PA, particularly during leisure time, had a lower risk of a recurring LBP episode compared with those who did not. The certainty of the evidence for the included reviews ranged between moderate11,45,47 and very low.46, 47, 48 Reviews that included RCTs showed that exercises and PA programs (including general exercises and leisure-time PA) reduced the risk of a recurring episode of LBP at least for the short-term.42,45,46,48 However, 2 reviews46,48 showed low to very low certainty of evidence due to the small number of studies included as well as inconclusive evidence. Adverse events were not reported in any of these reviews. Table 1 provides the characteristics and main findings of the included reviews with a meta-analysis for the secondary prevention of LBP.
3.5.2. Systematic reviews without meta-analysis (n = 4)
Four reviews18,50, 51, 52 assessed the effects of PA and exercise on secondary prevention of LBP but did not conduct a meta-analysis due to high heterogeneity among the included studies. These reviews explored the correlation between exposure to PA and LBP in adult populations and included only cohort studies. The PA exposure included a mix of interventions, such as walking, running, general exercises, and strengthening. The timeframes ranged from short-term (3 months) to long-term (15 years) follow-ups.
The results showed some potential benefits of PA for LBP;49,50 however, 1 review51 highlighted that people who engaged in some types of exercise or PA, such as stretching or the use of weight-training machines, presented an increased risk of having a recurrent episode of LBP compared with those who did not perform any PA. The characteristics of the included reviews without meta-analysis can be seen in Supplementary Table 4.
3.6. Management of LBP
3.6.1. Systematic reviews of RCTs with meta-analysis (n = 37)
A total of 37 reviews conducted a meta-analysis to summarize the effects of exercise therapy on the management of LBP. The exercise interventions included supervised and prescribed aquatic exercises (n = 2, 5%);57,59 aerobic or progressive resistance training (n = 2, 5%);53,56 mixed exercises (n = 7, 18%);37,67,70,72, 73, 74,100 general exercises (n = 2, 5%);38,40 back school (n = 3, 8%);60, 61, 62 Baduanjin exercise (n = 1, 2%);63 motor control exercises (i.e., stabilization exercises) (n = 4, 10%);39,80, 81, 82 Pilates (n = 6, 16%);41,43,83,84,88,89 Tai Chi (n = 1, 2%);97 yoga (n = 3, 2%);35,90,91 sling exercises (n = 2, 5%);95,96 mind-body exercises (n = 1, 2%);34 proprioceptive neuromuscular facilitation (PNF) (n = 1, 2%);98 trunk-focused exercises (n = 1, 2%);99 and McKenzie exercises (n = 1, 2%).66
For the outcome of pain, 18% of the included reviews reported data on the immediate effects of the intervention (<6 weeks), all reviews included data for short-term (6 weeks to <3 months), 33% for intermediate-term (3 to <8 months), and 39% for long-term effects (≥8 months). For disability, 24% of reviews reported results for immediate, 87% for short-term, 30% for intermediate, and 39% for long-term results. Of the 37 reviews that conducted a meta-analysis, 72% focused on chronic LBP, 21% included people with subacute and chronic LBP, and 6% focused on acute LBP only.
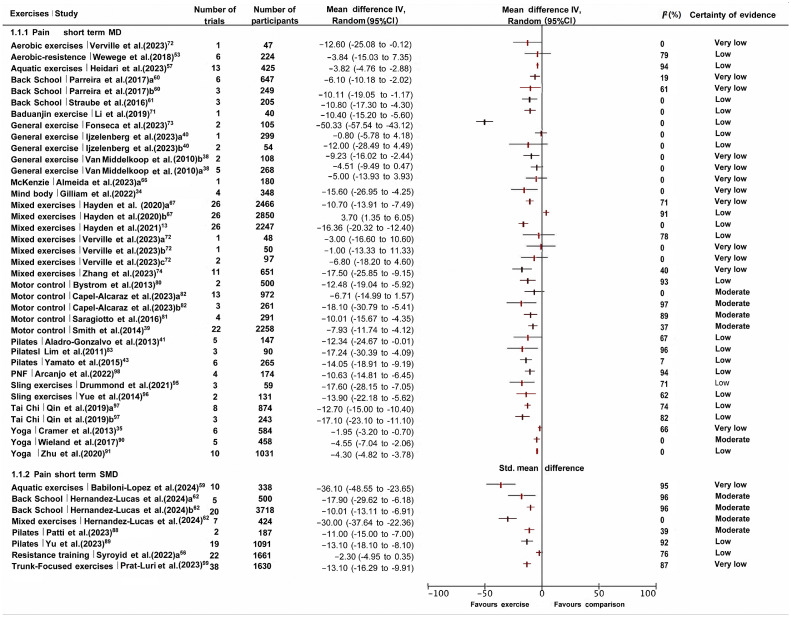
Forest plots on the effects of exercises compared to minimal interventions for the outcomes of pain and disability in the short-term are provided in Fig. 2, Fig. 3 and Supplementary Figs. 5–9. One review37 was excluded from the forest plots as there was no data available.
Fig. 2.
Included systematic reviews with meta-analysis for the management of low back pain (LBP) with exercises vs. minimal interventions for pain in the short-term follow-up (6 weeks to < 3 months). Short-term indicates a follow-up assessment of 3 months. Only studies providing results that could be converted to a 0–100-point scale are presented. Hayden et al67's study included individual participant data (IPD) analysis. a Same study but with a different comparison. The control group was usual care. b Same study but with different comparisons. The control group had no intervention or waitlist. Ijzelenberg et al.40 and Almeida et al.66 studied acute and subacute LBP. 95%CI = 95% confidence interval; IV = inverse variance; MD = mean difference; PNF = proprioceptive neuromuscular facilitation; SMD = standardized mean difference; Std. = Standard deviation.
Fig. 3.
Included systematic reviews with meta-analysis for the management of low back pain (LBP) with exercises vs. minimal interventions for disability in the short-term (6 weeks to < 3 months). Short-term indicates a follow-up assessment of 3 months. Only studies providing results that could be converted to a 0–100-point scale are presented. a Same study but with a different comparison. The control group was medical care (i.e., defined by the review as healthcare professional visits for medical and pharmacological assistance). b Same study but with different comparisons. The control group had no intervention or waitlist. Ijzelenberget al.40 and Almeida et al.66 studied acute and subacute LBP. 95%CI = 95% confidence interval; IV = inverse variance; MD = mean difference; PNF = proprioceptive neuromuscular facilitation; SMD = standardized mean difference; Std. = Standard deviation.
For the outcome of pain in the short-term, 20 (80%)34,35,37,39,40,43,53,57,61,63,67,80,83,84,90,91,95,97,98,100 of the included reviews showed positive results for exercise interventions (i.e., aquatic, motor control, mixed exercise, Tai Chi, yoga, PNF, sling exercise), and 5 reviews (20%)96,60,41,38,81 provided inconclusive evidence on the effectiveness of exercises (i.e., back school, McKenzie, mixed exercises, and Pilates) compared to minimal intervention in all follow-up periods investigated (i.e., short/med/long). The exercise interventions included a total of 27 different minimal interventions (e.g., usual care, education, no intervention, waitlist control, or pharmacological treatment), and 11 distinct comparisons38,41,60,66,81,83,90,95,97,98,100 presented very low certainty of evidence, and 3 studies43,95,98 presented low to moderate certainty (i.e., mixed exercises, motor control, and yoga) that exercises were beneficial for LBP management. Results for the outcome of pain in the immediate, intermediate, and long-term follow-ups can be found in Supplementary Figs. 5 and 6.
For disability in the short-term follow-up, 19 (79%) reviews showed positive results (small effect) for exercises (i.e., Pilates, mixed exercises, Tai Chi, yoga, sling exercise, PNF, and motor control), while 5 reviews60,66,67,81,83 provided uncertain evidence of the effectiveness of exercises compared to minimal interventions. Only 1 review67 showed that conservative management was more effective than mixed exercises (MD = 1.9, 95%CI: 0.03–3.80; 25 studies, n = 2778) in the short-term, with moderate certainty of evidence. The certainty of evidence was classified as low in 79% of the included reviews comparing different types of exercises to minimal intervention. The results for disability in the immediate, intermediate, and long-term follow-ups can be found in Supplementary Figs. 7–9.
3.6.2. Systematic reviews without meta-analysis (n = 16)
A total of 16 reviews36,44,54,55,58,64,65,68,69,85, 86, 87,92, 93, 94,101 reporting on the management of LBP did not conduct a meta-analysis, most commonly due to high heterogeneity among studies. The exercises evaluated in the 16 reviews included aerobic (n = 2, 13%);54,55 yoga (n = 4, 25%);92, 93, 94,101 Pilates (n = 3, 19%);85, 86, 87 general exercises (i.e., strengthening) (n = 2, 13%);64,65 mixed exercises (i.e., walking, stretching, strengthening, core exercises) (n = 4, 25%);36,44,68,69 and aquatic exercises (n = 1, 6%).58 Overall, the included reviews reported that exercises were effective in reducing LBP and LBP-related disability compared to minimal interventions, mostly in the short-term; however, the methodological quality was low to moderate.
3.6.3. Systematic reviews using a network meta-analysis (n = 7)
Seven systematic reviews13,71,75, 76, 77, 78, 79 that employed a network meta-analysis approach and ranked treatments based on direct effects and SUCRA values to evaluate the effectiveness of different exercise programs for the management and secondary prevention of LBP were included. The key findings are summarized in Table 2.
Table 2.
Characteristics of included reviews with network meta-analysis for management and secondary prevention of LBP.
| Study | Studies and study design (participants (n)) |
Study characteristics (population and intervention) |
Outcome of interest and main findings |
Adverse events | GRADE |
|---|---|---|---|---|---|
| Secondary prevention of LBP | |||||
| Huang et al.79,a | 40 RCTs (n = NR) |
People without LBP at study entry, with previous or mild LBP, mean age NR Intervention: Exercises (i.e., strengthening of the multifidus muscle) Comparison: No intervention or usual care |
Exercise, both alone and combined with education, effectively prevented LBP episodes; OR = 0.59 (95%CI: 0.41–0.82) and OR = 0.59 (95%CI: 0.36–0.92), respectively. For secondary prevention of LBP-related work absenteeism, exercise alone and in combination with education ranked the highest, with SUCRA values of 99.0% and 60.2%, respectively. |
NR | Moderate |
| Management of LBP | |||||
| Li et al.71,b | 75 RCTs (n = 5254) |
People with chronic LBP, mean age range: 20.1–70.4 years Intervention: Exercises (i.e., yoga, Pilates, sling, Tai Chi, water-based exercises, mixed exercises) Comparison: Control (i.e., no exercise or conventional physiotherapy) |
Tai Chi and yoga were the most effective intervention for both pain and disability. However, yoga showed better results. For pain, Tai Chi showed significant reduction compared to no exercise (SMD = –2.42; 95%CI: –3.81 to –1.03). For disability, yoga showed better physical function compared to no intervention (SMD = –1.81; 95%CI: –2.78 to –0.83). Based on the SUCRA analysis, the most effective 3 interventions for pain relief were Tai Chi (97.8%), yoga (93.5%), and Pilates (87.6%). For disability, the most effective 3 interventions were yoga (95.6%), core or stabilization exercise (86.3%), and sling exercise (81.4%). |
Adverse events were generally mild and non-serious (back school, water-based exercises, and mixed exercises), with few instances of severe pain or increased severity of symptoms (yoga). | Moderate |
| Fernandez-Rodriguez et al.78 | 118 RCTs (n = 9710) |
People with chronic LBP, mean age range: 18–61 years Intervention: Exercises (including aerobic, strength, combined, core-based, McKenzie, Pilates, stretching, or mind-body) Comparison: Control (i.e., no exercise, or usual care, or any of the structured exercises mentioned above) |
In 28 direct comparisons, all types of exercises improved pain and disability compared to control, except for stretching (for reducing pain) and McKenzie exercises (for reducing disability). According to the SUCRA analysis, Pilates (93%), mind–body (82.9%), and core-based exercises (66.2%) showed the highest likelihood of reducing pain and disability. For disability, Pilates (98.0%), strength (77.7%), and core-based exercises (69.8%) also ranked the highest. |
NR | Low to very low |
| Shi et al.77 | 36 RCTs (n = 3050) |
People with chronic LBP, mean age range: 18–61 years Intervention: Any structured PA aerobic, strength, combined, core-based, McKenzie, Pilates, stretching, or mind–body Comparison: No exercise and/or usual care |
Tai Chi presented superior efficacy for pain compared to usual care (3 RCTs, SMD = –1.29, 95%CI: –2.16 to –0.41). For disability, yoga outperformed usual care (5 RCTs, SMD = –1.45, 95%CI: –0.75 to –0.15). Pilates was the most effective therapy for chronic LBP in reducing pain intensity and improving disability, followed by Tai Chi. According to the SUCRA analysis, Pilates (86.6%), Tai Chi (77.2%), and yoga (67.6%) demonstrated the highest likelihood of reducing pain. For disability, Pilates (98.4%), Qigong (61.6%), Tai Chi (59.5%), and yoga (59.0%) presented the highest likelihood. |
NR | Low to moderate |
| Gianola et al.75 | 46 RCTs (n = 8765) |
People with acute and subacute LBP, mean age = 40.4 years Intervention: General exercises, medication (i.e., muscle relaxants, NSAIDs), back school, acupuncture, McKenzie, stretching, spinal manipulation, TENS Comparison: Inert treatment (i.e., sham/placebo treatment or no treatment) |
At immediate-term, general exercise was the most effective management for pain (SMD = –1.40, 95%CI: –2.41 to –0.40) and disability (SMD = –0.71, 95%CI: –1.16 to –0.26). In the SUCRA analysis, the most effective management for pain was general exercise (89.2%), and the least effective was inert treatment (10.7%) in the immediate term. For disability, CBT (68.5%) and exercise (66.5%) were the highest interventions in the long-term. |
26 studies (56.5%) reported adverse events. | Low |
| Hayden et al.13,c | 217 RCTs (n = 20,969) |
People with non-specific LBP, mean age 44 years Intervention: Exercises (e.g., strengthening, Pilates, yoga, flexibility, McKenzie, stretching, aerobic and mixed exercises) Comparison: Placebo, education, back school, mixed interventions (not exercises), relaxation, NSAIDs, and psychological therapy |
Pilates (MD = –13.1, 95%CI: –18.6 to –7.7, 10 trials, 780 participants), McKenzie (MD = –16.1, 95%CI: –19.5 to –12.8, 1 trial, 45 participants), and functional restoration (MD = –25.3, 95%CI: –38.1 to –12.5, 1 trial, 75 participants) were more effective than other types of exercises for improving function. Pilates (MD = –21.8, 95%CI: –29.6 to –214.1, 11 trials, 800 participants) and McKenzie (MD = –14.1, 95%CI: –27.7 to –0.4, 2 trials, 170 participants) were more effective for pain. | NR | Low |
| Owen et al.76,d | 89 RCTs (n = 5578) |
People with chronic LBP, mean age range: 20–70 years Intervention: Strengthening, exercises, Pilates, water-based, yoga, McKenzie, aerobic, and stretching Comparison: No intervention, passive treatment (i.e., manual therapy, massage) and general practitioner management, education, or psychological intervention |
On direct comparisons, Pilates (SMD = –1.86, 95%CI: –2.54 to –1.19), strengthening (SMD = –1.14, 95%CI: –1.71 to –0.56), and stabilization/motor control (SMD = –1.18, 95%CI: –1.53 to –0.74) had the highest likelihood of being the most effective intervention for reducing pain and improving physical function. According to the SUCRA analysis, Pilates (100%) was more likely to be the best treatment for pain compared to the control. Resistance training and motor stabilization/control showed the highest SUCRA (80%) for disability. |
Low-quality evidence showed that exercise did not cause serious harm and that, when adverse events are reported, they are limited to muscle soreness and increased pain. | Low |
Network meta-analysis exploring strategies to prevent LBP.
Only results comparing minimal intervention were extracted. This review also provided results comparing conventional rehabilitation.
The review does not provide specific information about the SUCRA.
The review did not specifically report SUCRA rankings for disability.
Abbreviations: 95%CI = 95% confidence interval; CBT = cognitive behavioral therapy; LBP = low back pain; MD = mean difference; NR = not reported; NSAIDs = nonsteroidal anti-inflammatory drugs; OR = odds ratio; RCTs = randomized controlled trials; SMD = standardized mean difference; SUCRA = Surface Under the Cumulative Ranking curve; TENS = transcutaneous electrical nerve stimulation.
All network meta-analyses reported data on LBP intensity and disability outcomes, and 1 review102 presented the incidence of LBP as the primary outcome (reported as OR and the associated 95% credibility interval (95%Crl)). Five network meta-analyses13,71,76, 77, 78 included studies on people with chronic LBP, while 1 review75 included studies on people with acute and subacute LBP.
The 7 network meta-analyses13,71,75, 76, 77, 78, 79 reported on a variety of exercise programs and PA concerning types of exercise, dosage, and frequency. The interventions encompassed a variety of exercise therapies, such as back school, aerobic, water-based exercise, strengthening exercise, core-based exercise, McKenzie, Pilates, Tai Chi, Qigong, and yoga. The duration of these programs ranged from 1 to 24 weeks, and the frequency varied from 1 to 2 times per week. These findings highlighted the heterogeneity in the design of exercise interventions across the studies, reflecting the diverse approaches and strategies employed to address LBP.
With low certainty of evidence, Pilates exercises emerged as the predominant exercise modality investigated to reduce LBP intensity, with SUCRA ranging from 86% to 98% compared to other types of exercises (i.e., Tai Chi, core-based exercise, mind–body) in the short-term follow-up in 3 network meta-analyses.76, 77, 78 However, results from 2 reviews found that Tai Chi77 and yoga71 were comparable to Pilates in decreasing pain intensity. Reviews that included studies on Pilates did not provide specific details on the duration, frequency, or intensity of Pilates sessions.
Similarly, for disability outcomes, Pilates and mixed exercise showed positive results in the short-term, with low certainty of evidence. One review primarily76 focused on comparing the effectiveness of different exercise modalities for LBP intensity and physical function. While disability was not explicitly mentioned in the SUCRA rankings, the effectiveness of certain modalities in improving physical function may also reduce disability.
For secondary prevention of LBP, 1 network meta-analysis79 was identified. This review showed that both exercise combined with education (OR = 0.59, 95%Crl: 0.41–0.82) and exercise alone (OR = 0.59, 95%Crl: 0.36–0.92) reduced the odds of LBP episodes.
3.6.4. Reports of adverse events
Adverse events related to exercises were reported in 22 reviews focusing on management,35, 36, 37, 38,43,51,59, 60, 61, 62, 63,66, 70,72,75,81,86,89, 90, 91,93,100 and in 1 review focusing on secondary prevention of LBP.51 Five reviews indicated36,38,61,63,66 the absence of any adverse events in the primary studies, whereas 12 reviews35,37,59,60,62,72,81,89,90,91,93,100 documented mild to moderate events observed in the included studies. These events were mostly related to a temporary worsening of pain following exercise.
Specifically for secondary prevention of LBP, 5 reviews (50%)36,45,48,63,99 reported that none of the included studies reported any adverse events. Only 1 review51 reported that restricted lateral bending range of motion, limited lumbar lordosis, and reduced hamstring flexibility are predictive of developing LBP. However, no reference to adverse events like injuries or complications was made in the included cohort studies.
The majority of adverse events reported through the primary studies for management of LBP included exacerbation of LBP and post-exercise mild adverse events (i.e., muscle soreness), and they were reported by reviews specifically examining the effects of yoga on managing LBP.35,72,90,91
4. Discussion
In this review, we synthesized evidence on the types and doses of PA and exercise interventions for managing and preventing LBP from reviews published between 2010 and 2024. For secondary prevention, 10 reviews11,42,45, 46, 47, 48, 49, 50, 51, 52 were included, covering non-structured PA like walking and gardening, with exercise programs ranging from 1 to 144 sessions over 2 to 104 weeks. Cohort studies showed PA exposure spanning from 3 months to 28 years. For LBP management, 61 reviews13,34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44,53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101 covered over 30 types of exercises, with program lengths between 2 and 12 months, and session frequency from 1 to 5 times per week, lasting at least 40 min (minimum 15 min).
Although the included reviews highlighted the potential benefits of exercise and PA interventions in managing LBP, it is important to acknowledge the different quality of reviews and degrees of certainty in the evidence, including how different types and dosages of exercises and PA can impact LBP differently and the significance of these strategies in both the management and secondary prevention of LBP.103 The quantification of overlap within meta-analyses was essential for understanding the extent to which primary studies are shared among the systematic reviews, thereby highlighting the redundancy and potential bias in the synthesized evidence.
Considering overlap citation, we did not limit the intervention type or LBP condition (e.g., acute or chronic). CCA across all included reviews was 0.0131 (<1.31%). This low number might suggest that overlap citation was not an issue for the included reviews with meta-analysis.104 Although the meta-analyses focused on exercises and physical activity, the examined comparisons were diverse (e.g., medication, education, no intervention, usual care, etc.).
4.1. Current knowledge of exercise therapy and PA in LBP
Regarding secondary prevention of LBP, included reviews suggested that various types of PA, including walking, sports, running, and some combinations of leisure activities (domestic and commuting) were not associated with the risk of developing LBP.47 Most of the included reviews showed beneficial results of exercises and PA for preventing the recurrence of LBP.11,46,48 However, it is important to note the limited number of reviews (n = 10) included11,42,45, 46, 47, 48, 49, 50, 51, 52 in this umbrella review focusing specifically on PA as a preventive approach for new episodes of LBP.
This umbrella review focused on identifying, summarizing, and systematically investigating the quality of reviews and certainty of evidence addressing exercise therapy and PA. For secondary prevention, summarizing the evidence was difficult as the measure of LBP recurrence and definition of recurrence varied across the included reviews (e.g., sick leave, time to a new episode, number of recurrences). Despite the apparent simplicity of assessing recurrence rates and total number of recurrences, research indicates that variations in definitions can significantly impact the interpretation of benefits.24 This is reflected in the outcomes found in this umbrella review, where different definitions of recurrences yielded different results. However, with low to moderate certainty evidence, we found that engaging in leisure-time PA (n = 2 reviews of cohort studies)11,47 and exercise (n = 4 reviews of RCTs on exercise types such as strengthening and McKenzie exercises)42,45,46,48 was protective against the recurrence of LBP at 1 year compared to minimal interventions (e.g., usual care, education).
Reviews on secondary prevention of LBP varied significantly in terms of participant inclusion, dosage, and the specific interventions (i.e., types of PA and exercise) assessed. For example, the follow-up of the individual studies included in the systematic reviews ranged from 1 year to 5 years, and some reviews11,47 aimed to compare different intensities of PA (e.g., moderate vs. low, high vs. moderate); the dosage of exercises was poorly described in those reviews. Furthermore, the presence of participants with pre-existing LBP at the start of the study could potentially bias the results and conclusions regarding the effectiveness of the preventive measures studied. Reviews also highlighted the importance of interpreting results carefully, since the descriptions of the interventions and duration of symptoms in the individual studies included in the reviews were generally poor.
For the management of LBP, there is an increasing acknowledgment of the potential benefits of exercise to reduce pain and LBP-related disability. Many different exercise programs have been proposed for the management of LBP, including Pilates, back school, motor control, general exercises (i.e., aerobic, stretching, and strengthening), Tai Chi, sling exercise, McKenzie, water-based exercises, and yoga. In this umbrella review, evidence of moderate certainty was found for pain reduction with mixed exercises (n = 2 reviews, immediate-term and short-term),13,100 motor control and yoga (n = 4 reviews, short-term),39,81,90,91 back school (n = 1 review, short-term),60 and motor control (n = 1 review, long-term) exercises.81 For disability, mixed exercises (n = 2 reviews, short-term);13,100 mixed exercises, motor control, and yoga (n = 3 reviews, intermediate-term);81,90,91 and mixed and motor control exercises (n = 2 reviews, long-term follow-up)81,100 presented moderate certainty of evidence.
The majority of reviews that conducted meta-analyses demonstrated statistically significant improvements in pain in the short-term (small effect).43 These findings add to the growing recognition of tailored exercise programs as effective in LBP management but also emphasize the need for clearer definitions and standardized intervention descriptions across studies. It is crucial to determine whether these changes are clinically relevant and lead to meaningful benefits for individuals when compared with other treatments. In reviews that employed a network meta-analysis approach, where exercise types are ranked according to their effectiveness, Pilates exercises, followed by Tai Chi and core exercises, were superior to other exercise interventions for reducing pain and disability in the short-term. However, the certainty of evidence was moderate to low.
Reviews that included RCTs seldom reported adverse events (31%), suggesting a potential underreporting of this important outcome. Some reviews noted mild adverse events for yoga (n = 4),35,72,90,91 mixed exercises (n = 3),13,70,100 Pilates (n = 1),43 motor control exercises (n = 1),81 back school (n = 1),60 and water-based exercises (n = 1),59 which included a temporary increase in pain and muscle soreness, though it remained ambiguous whether these effects were observed in participants with acute, subacute, or chronic LBP. The low percentage of reviews examining adverse events (30%) underscored the necessity for future studies to assess and report the safety, in addition to the effectiveness, of exercise and PA interventions for LBP management. Furthermore, only 39% of the reviews included long-term outcomes for pain and disability (defined as follow-up periods >8 months). Reporting long-term outcomes is essential because it provides a more comprehensive understanding of how interventions impact the management of LBP over time.105
4.2. A blueprint for future research
Clear definition of LBP recurrence: Provide a precise and unambiguous definition of the recurrence of LBP. Clearly outlining the parameters for the recurrence of LBP will help standardize the evaluation process and facilitate a more accurate interpretation of the results.
Investigation of adverse events: A comprehensive investigation and reporting of adverse events related to exercise and PA must be addressed. Assessing and reporting adverse events can provide valuable insights into the safety and potential risks associated with the interventions, thus offering a more holistic understanding of their overall impact on pain intensity, disability, and prevention of LBP.
Tailored exercise regimens: Include studies that present a tailored exercise regimen considering the frequency, duration, and intensity of PA based on specific health objectives and individual needs.
4.3. Strengths and limitations
This umbrella review has some major strengths and some limitations that should be acknowledged. In the examination of preventive measures for LBP, there was a limited number of reviews that specifically investigated exercises or PA interventions (n = 10).11,42,45, 46, 47, 48, 49, 50, 51, 52 These identified gaps in the current body of literature underscore the need for further research and investigation in this field.
When considering reviews on secondary prevention of LBP, the definition of outcomes for the recurrence of LBP varied considerably. For example, some reviews (n = 6) included cohort studies,11,47,49, 50, 51, 52 while others (n = 4) included RCTs.42,45,46,48 It is crucial to acknowledge the inherent limitations of cohort studies, particularly in terms of establishing causation, due to the observational nature of their design. Throughout our review process, efforts were made to maintain consistency in the selection of studies. This approach aimed to provide a more comprehensive understanding of secondary prevention strategies for LBP. Nevertheless, the nuanced nature of the available evidence underscores the importance of interpreting findings with a recognition of the inherent constraints posed by the study designs and outcomes investigated. Few studies clearly describe how recovery from the previous episode of LBP was defined, so it is unclear whether participants had recovered and were therefore truly at risk of recurrence, or for how long they had recovered before entering the study. Additionally, few reviews clearly defined recovery from previous LBP episodes or examined adverse events, leaving conclusions on these aspects uncertain.
Another inherited limitation of this umbrella review is the lack of clear definitions of short- and long-term follow-ups in reviews of management, which could lead to potential bias in the results. To overcome this limitation, we made a conscientious attempt to establish a specific classification system for short- and long-term follow-ups. Moreover, our inclusion criteria relied on the information provided in the original systematic reviews, which reflected the descriptions of RCTs or observational studies they included.
To improve the comprehensiveness of the evidence, our inclusion criteria accommodated systematic reviews with and without meta-analysis that compared exercises or PA with minimal interventions (as per definition). However, during the evaluation of the primary studies included in the systematic reviews, we noted reviews that included studies comparing different forms of exercise. To address this issue, we established inclusion criteria stipulating that at least 80% of the reviews should focus on comparing exercise interventions with minimal interventions for both management and prevention to be eligible.
4.4. Implications for clinicians and future research
The substantial growth in evidence over the past 14 years consistently highlights a plethora of benefits from engaging in exercise and PA for individuals living with LBP. It is encouraging to note the positive trend, emphasizing the advantages of incorporating exercises and PA into LBP management strategies. However, it is crucial to maintain a nuanced perspective and acknowledge that uncertainties persist, particularly regarding the certainty of evidence and the effectiveness of exercise and PA in preventing recurrence of LBP.
Some forms of exercise therapy appeared to be superior to others, and some forms of PA (e.g., leisure-time PA) were more effective in reducing recurrent LBP than others. However, we encourage clinicians to conduct a holistic assessment of the available evidence, considering the certainty of the evidence, availability of resources and training, and the target population. It is crucial to involve patients in these discussions so that recommendations can be tailored toward individual needs and preferences. Additionally, implementing preventive strategies that incorporate functional body movements in the appropriate dosage can be instrumental in reducing the risk of developing LBP.
5. Conclusion
Our findings indicate that, overall, most types of exercises and PA programs were effective in preventing and managing LBP, mainly in the short-term with small to moderate effects. However, it is important to note that there was a moderate to low level of certainty in the evidence. In terms of secondary prevention, engaging in leisure-time PA was effective in preventing recurrences of LBP. Moreover, for the management of LBP, while most exercises were effective for improving pain and disability in the short-term, some specific forms—including Pilates, back school, and yoga—appeared to be more beneficial.
It is crucial to highlight that the potential adverse effects of exercise and PA interventions have not been comprehensively investigated or systematically reported. Considering this, future studies should address this gap to further enhance our understanding in the field.
Authors’ contributions
JC developed the protocol, search strategy, selected studies, and wrote the manuscript; QL and DXMW assisted in data extraction and analysis; PHF supported the development of protocol and provided supervision; PRB, EK-YH, CAS, ES, MLF, PJM, and AH contributed to the interpretation of the data. All authors have read and approved the final version of the manuscript, and agree with the order of authorship.
Competing interests
The authors declare that they have no competing interests.
Acknowledgments
We thank Kanchana Ekanayake, the Academic Liaison Librarian, for her invaluable assistance in developing the comprehensive search strategy. Additionally, we thank Sydney Informatics Hub, a statistical consultant from the University of Sydney, for his support in data interpretation. This research was funded by the Medical Research Future Fund - MRFF 2019 (Rapid Applied Research Translation- RART award). JC is funded by an Australian Government Research Training Program Scholarship – RTP. PHF and MLF are funded by National Health and Medical Research Council of Australia Research Fellowships. ES is funded by the National Health and Medical Research Council (NHMRC) Leadership Fellow level 2.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary materials associated with this article can be found in the online version at doi:10.1016/j.jshs.2025.101038.
Supplementary materials
References
- 1.Sebbag E., Felten R., Sagez F., et al. The world-wide burden of musculoskeletal diseases: A systematic analysis of the World Health Organization Burden of Diseases Database. Ann Rheum Dis. 2019;78:844–848. doi: 10.1136/annrheumdis-2019-215142. [DOI] [PubMed] [Google Scholar]
- 2.da Silva T., Mills K., Brown B.T., et al. Recurrence of low back pain is common: A prospective inception cohort study. J Physiother. 2019;65:159–165. doi: 10.1016/j.jphys.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Hartvigsen J., Hancock M.J., Kongsted A., et al. What low back pain is and why we need to pay attention. The Lancet. 2018;391:2356–2367. doi: 10.1016/S0140-6736(18)30480-X. [DOI] [PubMed] [Google Scholar]
- 4.Zouch J., Comachio J., Bussieres A., et al. Influence of initial health care provider on subsequent health care utilization for patients with a new onset of low back pain: A scoping review. Phys Ther. 2022;102:pzac150. doi: 10.1093/ptj/pzac150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ho E.K., Chen L., Simic M., et al. Psychological interventions for chronic, non-specific low back pain: Systematic review with network meta-analysis. BMJ. 2022;376 doi: 10.1136/bmj-2021-067718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ostelo R. Lancet Series: The “magnum opus” regarding the evidence on low back pain. Spine (Phila Pa 1976) 2018;43:1239–1240. doi: 10.1097/BRS.0000000000002786. [DOI] [PubMed] [Google Scholar]
- 7.Buchbinder R., Underwood M., Hartvigsen J., et al. The Lancet Series call to action to reduce low value care for low back pain: An update. Pain. 2020;161(Suppl. 1):S57–S64. doi: 10.1097/j.pain.0000000000001869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bull F.C., Al-Ansari S.S., Biddle S., et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Foster N.E., Anema J.R., Cherkin D., et al. Prevention and treatment of low back pain: Evidence, challenges, and promising directions. The Lancet. 2018;391:2368–2383. doi: 10.1016/S0140-6736(18)30489-6. [DOI] [PubMed] [Google Scholar]
- 10.Park J.H., Moon J.H., Kim H.J., et al. Sedentary lifestyle: Overview of updated evidence of potential health risks. Korean J Fam Med. 2020;41:365–373. doi: 10.4082/kjfm.20.0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alzahrani H., Mackey M., Stamatakis E., et al. The association between physical activity and low back pain: A systematic review and meta-analysis of observational studies. Sci Rep. 2019;9:8244. doi: 10.1038/s41598-019-44664-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hubscher M., Ferreira M.L., Junqueira D.R., et al. Heavy domestic, but not recreational, physical activity is associated with low back pain: Australian twin low BACK pain (AUTBACK) study. Eur Spine J. 2014;23:2083–2089. doi: 10.1007/s00586-014-3258-2. [DOI] [PubMed] [Google Scholar]
- 13.Hayden J.A., Ellis J., Ogilvie R., et al. Some types of exercise are more effective than others in people with chronic low back pain: A network meta-analysis. J Physiother. 2021;67:252–262. doi: 10.1016/j.jphys.2021.09.004. [DOI] [PubMed] [Google Scholar]
- 14.de Campos T.F. Low back pain and sciatica in over 16s: Assessment and management NICE Guideline [NG59] J Physiother. 2017;63:120. doi: 10.1016/j.jphys.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 15.Comachio J., Ferreira M.L., Mork P.J., et al. Clinical guidelines are silent on the recommendation of physical activity and exercise therapy for low back pain: A systematic review. J Sci Med Sport. 2024;27:257–265. doi: 10.1016/j.jsams.2024.01.003. [DOI] [PubMed] [Google Scholar]
- 16.Becker A., Chenot J.F., Niebling W., Kochen M.M. Guidelines for back pain. Z Orthop Ihre Grenzgeb. 2004;142:716–719. doi: 10.1055/s-2004-832488. [DOI] [PubMed] [Google Scholar]
- 17.Schreijenberg M., Koes B.W., Lin C.C. Guideline recommendations on the pharmacological management of non-specific low back pain in primary care–Is there a need to change? Expert Rev Clin Pharmacol. 2019;12:145–157. doi: 10.1080/17512433.2019.1565992. [DOI] [PubMed] [Google Scholar]
- 18.Oliveira C.B., Maher C.G., Pinto R.Z., et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: An updated overview. Eur Spine J. 2018;27:2791–2803. doi: 10.1007/s00586-018-5673-2. [DOI] [PubMed] [Google Scholar]
- 19.Pollock M., Fernandes R.M., Pieper D., et al. Preferred reporting items for overviews of reviews (PRIOR): A protocol for development of a reporting guideline for overviews of reviews of healthcare interventions. Syst Rev. 2019;8:335. doi: 10.1186/s13643-019-1252-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hirt J., Nordhausen T., Fuerst T., et al. Guidance on terminology, application, and reporting of citation searching: The TARCiS statement. BMJ. 2024;385 doi: 10.1136/bmj-2023-078384. [DOI] [PubMed] [Google Scholar]
- 21.Caspersen C.J., Powell K.E., Christenson G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–131. [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization . World Health Organization; Geneva, Switzerland: 2023. WHO guideline for non-surgical management of chronic primary low back pain in adults in primary and community care settings. [PubMed] [Google Scholar]
- 23.Uman L.S. Systematic reviews and meta-analyses. J Can Acad Child Adolesc Psychiatry. 2011;20:57–59. [PMC free article] [PubMed] [Google Scholar]
- 24.Stanton T.R., Latimer J., Maher C.G., et al. Definitions of recurrence of an episode of low back pain: A systematic review. Spine (Phila Pa 1976) 2009;34:E316–E322. doi: 10.1097/BRS.0b013e318198d073. [DOI] [PubMed] [Google Scholar]
- 25.Chiarotto A., Boers M., Deyo R.A., et al. Core outcome measurement instruments for clinical trials in nonspecific low back pain. Pain. 2018;159:481–495. doi: 10.1097/j.pain.0000000000001117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shea B.J., Reeves B.C., Wells G., et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shea B.J., Hamel C., Wells G.A., et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol. 2009;62:1013–1020. doi: 10.1016/j.jclinepi.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 28.Higgins J.P., Altman D.G., Gotzsche P.C., et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Armijo-Olivo S., da Costa B.R., Cummings G.G., et al. PEDro or Cochrane to assess the quality of clinical trials? A meta-epidemiological study. PLoS One. 2015;10 doi: 10.1371/journal.pone.0132634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guyatt G.H., Oxman A.D., Vist G.E., et al. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huguet A., Hayden J.A., Stinson J., et al. Judging the quality of evidence in reviews of prognostic factor research: Adapting the GRADE framework. Syst Rev. 2013;2:71. doi: 10.1186/2046-4053-2-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pieper D., Antoine S.L., Mathes T., et al. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67:368–375. doi: 10.1016/j.jclinepi.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 33.Hennessy E.A., Johnson B.T. Examining overlap of included studies in meta-reviews: Guidance for using the corrected covered area index. Res Synth Methods. 2020;11:134–145. doi: 10.1002/jrsm.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gilliam J.R., George S.Z., Norman K.S., et al. Mind-body exercise performed by physical therapists for reducing pain and disability in low back pain: A systematic review with meta-analysis. Arch Phys Med Rehabil. 2023;104:776–789. doi: 10.1016/j.apmr.2022.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cramer H., Lauche R., Haller H., et al. A systematic review and meta-analysis of yoga for low back pain. Clin J Pain. 2013;29:450–460. doi: 10.1097/AJP.0b013e31825e1492. [DOI] [PubMed] [Google Scholar]
- 36.Ford J.J., Bower S.E., Ford I., et al. Effects of specific muscle activation for low back pain on activity limitation, pain, work participation, or recurrence: A systematic review. Musculoskelet Sci Pract. 2020;50 doi: 10.1016/j.msksp.2020.102276. [DOI] [PubMed] [Google Scholar]
- 37.Searle A., Spink M., Ho A., et al. Exercise interventions for the treatment of chronic low back pain: A systematic review and meta-analysis of randomised controlled trials. Clin Rehabil. 2015;29:1155–1167. doi: 10.1177/0269215515570379. [DOI] [PubMed] [Google Scholar]
- 38.van Middelkoop M., Rubinstein S.M., Verhagen A.P., et al. Exercise therapy for chronic nonspecific low back pain. Best Pract Res Clin Rheumatol. 2010;24:193–204. doi: 10.1016/j.berh.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 39.Smith B.E., Littlewood C., May S. An update of stabilisation exercises for low back pain: A systematic review with meta-analysis. BMC Musculoskelet Disord. 2014;15:416. doi: 10.1186/1471-2474-15-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.IJzelenberg W., Oosterhuis T., Hayden J.A., et al. Exercise therapy for treatment of acute non-specific low back pain: A Cochrane systematic review and meta-analysis of randomised controlled trials. Arch Phys Med Rehabil. 2024;105:1571–1584. doi: 10.1016/j.apmr.2024.02.732. [DOI] [PubMed] [Google Scholar]
- 41.Aladro-Gonzalvo A.R., Araya-Vargas G.A., Machado-Diaz M., et al. Pilates-based exercise for persistent, non-specific low back pain and associated functional disability: A meta-analysis with meta-regression. J Bodyw Mov Ther. 2013;17:125–136. doi: 10.1016/j.jbmt.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 42.Shiri R., Coggon D., Falah-Hassani K. Exercise for the prevention of low back pain: Systematic review and meta-analysis of controlled trials. Am J Epidemiol. 2018;187:1093–1101. doi: 10.1093/aje/kwx337. [DOI] [PubMed] [Google Scholar]
- 43.Yamato T.P., Maher C.G., Saragiotto B.T., et al. Pilates for low back pain. Cochrane Database Syst Rev. 2015;2015 doi: 10.1002/14651858.CD010265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kuss K., Becker A., Quint S., et al. Activating therapy modalities in older individuals with chronic non-specific low back pain: A systematic review. Physiotherapy. 2015;101:310–318. doi: 10.1016/j.physio.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 45.Choi B.K., Verbeek J.H., Tam W.W., et al. Exercises for prevention of recurrences of low-back pain. Cochrane Database Syst Rev. 2010;2010 doi: 10.1002/14651858.CD006555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alalmaee K.A., Allubly A.M., Alsaileek Z.A., et al. Preventive strategies for low back pain: A systematic review and meta-analysis. Ann Med Health Sci Res. 2020;10:959–963. [Google Scholar]
- 47.Shiri R., Falah-Hassani K. Does leisure time physical activity protect against low back pain? Systematic review and meta-analysis of 36 prospective cohort studies. Br J Sports Med. 2017;51:1410–1418. doi: 10.1136/bjsports-2016-097352. [DOI] [PubMed] [Google Scholar]
- 48.Steffens D., Maher C.G., Pereira L.S., et al. Prevention of low back pain: A systematic review and meta-analysis. JAMA Intern Med. 2016;176:199–208. doi: 10.1001/jamainternmed.2015.7431. [DOI] [PubMed] [Google Scholar]
- 49.Oliveira C.B., Pinheiro M.B., Teixeira R.J., et al. Physical activity as a prognostic factor of pain intensity and disability in patients with low back pain: A systematic review. Eur J Pain. 2019;23:1251–1263. doi: 10.1002/ejp.1395. [DOI] [PubMed] [Google Scholar]
- 50.Hendrick P., Milosavljevic S., Hale L., et al. The relationship between physical activity and low back pain outcomes: A systematic review of observational studies. Eur Spine J. 2011;20:464–474. doi: 10.1007/s00586-010-1616-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sadler S.G., Spink M.J., Ho A., et al. Restriction in lateral bending range of motion, lumbar lordosis, and hamstring flexibility predicts the development of low back pain: A systematic review of prospective cohort studies. BMC Musculoskelet Disord. 2017;18:179. doi: 10.1186/s12891-017-1534-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Heneweer H., Staes F., Aufdemkampe G., et al. Physical activity and low back pain: A systematic review of recent literature. Eur Spine J. 2011;20:826–845. doi: 10.1007/s00586-010-1680-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wewege M.A., Booth J., Parmenter B.J. Aerobic vs. resistance exercise for chronic non-specific low back pain: A systematic review and meta-analysis. J Back Musculoskelet Rehabil. 2018;31:889–899. doi: 10.3233/BMR-170920. [DOI] [PubMed] [Google Scholar]
- 54.Lawford B.J., Walters J., Ferrar K. Does walking improve disability status, function, or quality of life in adults with chronic low back pain? A systematic review. Clin Rehabil. 2016;30:523–536. doi: 10.1177/0269215515590487. [DOI] [PubMed] [Google Scholar]
- 55.Sany S.A., Mitsi M., Tanjim T., et al. The effectiveness of different aerobic exercises to improve pain intensity and disability in chronic low back pain patients: A systematic review. F1000Res. 2022;11:136. doi: 10.12688/f1000research.75440.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Syroyid Syroyid I., Cavero-Redondo I., Syroyid Syroyid B. Effects of resistance training on pain control and physical function in older adults with low back pain: A systematic review with meta-analysis. J Geriatr Phys Ther. 2022;46:E113–E126. doi: 10.1519/JPT.0000000000000374. [DOI] [PubMed] [Google Scholar]
- 57.Heidari F., Mohammad Rahimi N., Aminzadeh R. Aquatic exercise impact on pain intensity, disability and quality of life in adults with low back pain: A systematic review and meta-analysis. Biol Res Nurs. 2023;25:527–541. doi: 10.1177/10998004231162327. [DOI] [PubMed] [Google Scholar]
- 58.Christakou A., Boulnta F. The effectiveness of hydrotherapy in patients with chronic low back pain. Physiotherapy Quart. 2020;28:32–38. [Google Scholar]
- 59.Babiloni-Lopez C., Fritz N., Ramirez-Campillo R., et al. Water-based exercise in patients with nonspecific chronic low-back pain: A systematic review with meta-analysis. J Strength Cond Res. 2024;38:206–219. doi: 10.1519/JSC.0000000000004635. [DOI] [PubMed] [Google Scholar]
- 60.Parreira P., Heymans M.W., van Tulder M.W., et al. Back schools for chronic non-specific low back pain. Cochrane Database Syst Rev. 2017;8 doi: 10.1002/14651858.CD011674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Straube S., Harden M., Schroder H., et al. Back schools for the treatment of chronic low back pain: Possibility of benefit but no convincing evidence after 47 years of research-systematic review and meta-analysis. Pain. 2016;157:2160–2172. doi: 10.1097/j.pain.0000000000000640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hernandez-Lucas P., Leiros-Rodriguez R., Lopez-Barreiro J., García-Soidán J.L. The effects of back schools on non-specific back pain: A systematic review and meta-analysis. J Pers Med. 2024;14:272. doi: 10.3390/jpm14030272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Li H., Ge D., Liu S., et al. Baduanjin exercise for low back pain: A systematic review and meta-analysis. Complement Ther Med. 2019;43:109–116. doi: 10.1016/j.ctim.2019.01.021. [DOI] [PubMed] [Google Scholar]
- 64.Gordon R., Bloxham S. A systematic review of the effects of exercise and physical activity on non-specific chronic low back pain. Healthcare (Basel) 2016;4:22. doi: 10.3390/healthcare4020022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lemieux J., Abdollah V., Powelske B., et al. Comparing the effectiveness of group-based exercise to other non-pharmacological interventions for chronic low back pain: A systematic review. PLoS One. 2020;15 doi: 10.1371/journal.pone.0244588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Almeida M.O., Narciso Garcia A., Menezes Costa L.C., et al. The McKenzie method for (sub)acute non-specific low back pain. Cochrane Database Syst Rev. 2023;4 doi: 10.1002/14651858.CD009711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hayden J.A., Wilson M.N., Stewart S., et al. Exercise treatment effect modifiers in persistent low back pain: An individual participant data meta-analysis of 3514 participants from 27 randomised controlled trials. Br J Sports Med. 2020;54:1277–1278. doi: 10.1136/bjsports-2019-101205. [DOI] [PubMed] [Google Scholar]
- 68.Vadala G., Russo F., De Salvatore S., et al. Physical activity for the treatment of chronic low back pain in elderly patients: A systematic review. J Clin Med. 2020;9:1023. doi: 10.3390/jcm9041023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Frizziero A., Pellizzon G., Vittadini F., et al. Efficacy of core stability in non-specific chronic low back pain. J Funct Morphol Kinesiol. 2021;6:37. doi: 10.3390/jfmk6020037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hernandez-Lucas P., Leiros-Rodriguez R., Lopez-Barreiro J., et al. Prevention of non-specific back pain through exercise and education: A systematic review and meta-analysis. J Back Musculoskelet Rehabil. 2024;37:585–598. doi: 10.3233/BMR-230252. [DOI] [PubMed] [Google Scholar]
- 71.Li Y., Yan L., Hou L., et al. Exercise intervention for patients with chronic low back pain: A systematic review and network meta-analysis. Front Public Health. 2023;11 doi: 10.3389/fpubh.2023.1155225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Verville L., Ogilvie R., Hincapie C.A., et al. Systematic review to inform a World Health Organization (WHO) clinical practice guideline: Benefits and harms of structured exercise programs for chronic primary low back pain in adults. J Occup Rehabil. 2023;33:636–650. doi: 10.1007/s10926-023-10124-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Soares Fonseca L., Pereira Silva J., Bastos Souza M., et al. Effectiveness of pharmacological and non-pharmacological therapy on pain intensity and disability in older people with chronic nonspecific low back pain: A systematic review with meta-analysis. Eur Spine J. 2023;32:3245–3271. doi: 10.1007/s00586-023-07857-4. [DOI] [PubMed] [Google Scholar]
- 74.Zhang S.K., Gu M.L., Zhang T., et al. Effects of exercise therapy on disability, mobility, and quality of life in the elderly with chronic low back pain: A systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2023;18:513. doi: 10.1186/s13018-023-03988-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gianola S., Bargeri S., Del Castillo G., et al. Effectiveness of treatments for acute and subacute mechanical non-specific low back pain: A systematic review with network meta-analysis. Br J Sports Med. 2022;56:41–50. doi: 10.1136/bjsports-2020-103596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Owen P.J., Miller C.T., Mundell N.L., et al. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med. 2020;54:1279–1287. doi: 10.1136/bjsports-2019-100886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shi J., Hu Z.Y., Wen Y.R., et al. Optimal modes of mind-body exercise for treating chronic non-specific low back pain: Systematic review and network meta-analysis. Front Neurosci. 2022;16 doi: 10.3389/fnins.2022.1046518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fernandez-Rodriguez R., Alvarez-Bueno C., Cavero-Redondo I., et al. Best exercise options for reducing pain and disability in adults with chronic low back pain: Pilates, strength, core-based, and mind-body. A network meta-analysis. J Orthop Sports Phys Ther. 2022;52:505–521. doi: 10.2519/jospt.2022.10671. [DOI] [PubMed] [Google Scholar]
- 79.Huang R., Ning J., Chuter V.H., et al. Exercise alone and exercise combined with education both prevent episodes of low back pain and related absenteeism: Systematic review and network meta-analysis of randomised controlled trials (RCTs) aimed at preventing back pain. Br J Sports Med. 2020;54:766–770. doi: 10.1136/bjsports-2018-100035. [DOI] [PubMed] [Google Scholar]
- 80.Bystrom M.G., Rasmussen-Barr E., Grooten W.J. Motor control exercises reduces pain and disability in chronic and recurrent low back pain: A meta-analysis. Spine (Phila Pa 1976) 2013;38:E350–E358. doi: 10.1097/BRS.0b013e31828435fb. [DOI] [PubMed] [Google Scholar]
- 81.Saragiotto B.T., Maher C.G., Yamato T.P., et al. Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst Rev. 2016;2016 doi: 10.1002/14651858.CD012004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Capel-Alcaraz A.M., Castro-Sanchez A.M., Mataran-Penarrocha G.A., et al. Effects of motor control exercises in patients with chronic nonspecific low back pain: A systematic review and meta-analysis. Clin J Sport Med. 2023;33:579–597. doi: 10.1097/JSM.0000000000001175. [DOI] [PubMed] [Google Scholar]
- 83.Lim E.C., Poh R.L., Low A.Y., et al. Effects of Pilates-based exercises on pain and disability in individuals with persistent nonspecific low back pain: A systematic review with meta-analysis. J Orthop Sports Phys Ther. 2011;41:70–80. doi: 10.2519/jospt.2011.3393. [DOI] [PubMed] [Google Scholar]
- 84.Miyamoto G.C., Costa L.O., Cabral C.M. Efficacy of the Pilates method for pain and disability in patients with chronic nonspecific low back pain: A systematic review with meta-analysis. Braz J Phys Ther. 2013;17:517–532. doi: 10.1590/S1413-35552012005000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wells C., Kolt G.S., Marshall P., et al. The effectiveness of pilates exercise in people with chronic low back pain: A systematic review. PLoS One. 2014;9 doi: 10.1371/journal.pone.0100402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Posadzki P., Lizis P., Hagner-Derengowska M. Pilates for low back pain: A systematic review. Complement Ther Clin Pract. 2011;17:85–89. doi: 10.1016/j.ctcp.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 87.Patti A., Bianco A., Paoli A., et al. Effects of pilates exercise programs in people with chronic low back pain: A systematic review. Medicine (Baltimore) 2015;94:e383. doi: 10.1097/md.0000000000000383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Patti A., Thornton J.S., Giustino V., et al. Effectiveness of pilates exercise on low back pain: A systematic review with meta-analysis. Disabil Rehabil. 2024;46:3535–3548. doi: 10.1080/09638288.2023.2251404. [DOI] [PubMed] [Google Scholar]
- 89.Yu Z., Yin Y., Wang J., et al. Efficacy of pilates on pain, functional disorders and quality of life in patients with chronic low back pain: A systematic review and meta-analysis. Int J Environ Res Public Health. 2023;20:2850. doi: 10.3390/ijerph20042850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wieland L.S., Skoetz N., Pilkington K., et al. Yoga treatment for chronic non-specific low back pain. Cochrane Database Syst Rev. 2017;1 doi: 10.1002/14651858.CD010671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhu F., Zhang M., Wang D., et al. Yoga compared to non-exercise or physical therapy exercise on pain, disability, and quality of life for patients with chronic low back pain: A systematic review and meta-analysis of randomized controlled trials. PLoS One. 2020;15 doi: 10.1371/journal.pone.0238544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Diaz A.M., Kolber M.J., Patel C.K., Hanney W.J. The efficacy of yoga as an intervention for chronic low back pain: A systematic review of randomized controlled trials. Am J Lifestyle Med. 2013;7:418–430. [Google Scholar]
- 93.Chang D.G., Holt J.A., Sklar M., Groessl E.J. Yoga as a treatment for chronic low back pain: A systematic review of the literature. J Orthop Rheumatol. 2016;3:1–8. [PMC free article] [PubMed] [Google Scholar]
- 94.Posadzki P., Ernst E. Yoga for low back pain: A systematic review of randomized clinical trials. Clin Rheumatol. 2011;30:1257–1262. doi: 10.1007/s10067-011-1764-8. [DOI] [PubMed] [Google Scholar]
- 95.Drummond C., Lebedeva V., Kirker K., Masaracchio M. Sling exercise in the management of chronic low back pain: A systematic review and meta-analysis. J Strength Cond Res. 2024;38:1822–1833. doi: 10.1519/JSC.0000000000004135. [DOI] [PubMed] [Google Scholar]
- 96.Yue Y.S., Wang X.D., Xie B., et al. Sling exercise for chronic low back pain: A systematic review and meta-analysis. PLoS One. 2014;9 doi: 10.1371/journal.pone.0099307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Qin J., Zhang Y., Wu L., et al. Effect of Tai Chi alone or as additional therapy on low back pain: Systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 2019;98 doi: 10.1097/MD.0000000000017099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Arcanjo F.L., Martins J.V.P., Mote P., et al. Proprioceptive neuromuscular facilitation training reduces pain and disability in individuals with chronic low back pain: A systematic review and meta-analysis. Complement Ther Clin Pract. 2022;46 doi: 10.1016/j.ctcp.2021.101505. [DOI] [PubMed] [Google Scholar]
- 99.Prat-Luri A., de Los Rios-Calonge J, Moreno-Navarro P., et al. Effect of trunk-focused exercises on pain, disability, quality of life, and trunk physical fitness in low back pain and how potential effect modifiers modulate their effects: A systematic review with meta-analyses. J Orthop Sports Phys Ther. 2023;53:64–93. doi: 10.2519/jospt.2023.11091. [DOI] [PubMed] [Google Scholar]
- 100.Hayden J.A., Ellis J., Ogilvie R., et al. Exercise therapy for chronic low back pain. Cochrane Database Syst Rev. 2021;9 doi: 10.1002/14651858.CD009790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sharma M., Haider T. Yoga as an alternative and complementary treatment for patients with low back pain: A systematic review. J Evid Based Integr Med. 2013;18:48–53. [Google Scholar]
- 102.Huang J., Park H.Y. Effect of pilates training on pain and disability in patients with chronic low back pain: A systematic review and meta-analysis based on randomized controlled trials. Phys Act Nutr. 2023;27:16–29. doi: 10.20463/pan.2023.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Castellini G., Iannicelli V., Briguglio M., et al. Are clinical practice guidelines for low back pain interventions of high quality and updated? A systematic review using the AGREE II instrument. BMC Health Serv Res. 2020;20:970. doi: 10.1186/s12913-020-05827-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lunny C., Brennan S.E., Reid J., et al. Overviews of reviews incompletely report methods for handling overlapping, discordant, and problematic data. J Clin Epidemiol. 2020;118:69–85. doi: 10.1016/j.jclinepi.2019.09.025. [DOI] [PubMed] [Google Scholar]
- 105.Foster N.E. Barriers and progress in the treatment of low back pain. BMC Med. 2011;9:108. doi: 10.1186/1741-7015-9-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.