Abstract
Background
A sinus of Valsalva aneurysm (SoVA) is a rare cardiac condition caused by the dilation of a coronary sinus. If untreated, it can commonly lead to valvular dysfunction, arrhythmias, or rupture.
Case Summary
A 71-year-old patient with hypertension and hyperlipidemia presented with an embolic stroke. Multimodality imaging revealed a large, 7.0 cm × 5.6 cm SoVA originating from the noncoronary sinus and causing nearly complete obstruction of the left atrium. The aneurysm was surgically repaired, and the patient made a full recovery.
Discussion
In rare cases, a stroke may be the initial presentation of a SoVA. The probable cause of the patient’s stroke was attributed to thrombus formation within the SoVA that embolized.
Take-Home Messages
This case emphasizes the importance of multimodality imaging for the diagnosis of a SoVA and for planning surgical repair. Additionally, clinicians should consider a SoVA in the differential diagnosis for a patient presenting with a stroke.
Key Words: aortic root repair, computed tomography, coronary angiography, multimodality cardiac imaging, noncoronary sinus, sinus of Valsalva aneurysm, stroke, transesophageal echocardiogram, transthoracic echocardiogram
Visual Summary
History of Presentation
A 71-year-old man presented to the emergency department with a 2-hour history of right-sided hemiparesis, aphasia, and facial palsy. A computed tomography (CT) scan of the brain showed a left middle cerebral artery (MCA) infarction. On admission, his blood pressure was elevated at 154/90 mm Hg, and his heart rate was 78 beats/min. No other pertinent physical examination findings were noted besides his presenting neurologic deficits. The patient received tenecteplase and underwent mechanical thrombectomy for treatment of his stroke, with resulting neurologic improvement. He was admitted for a comprehensive stroke evaluation.
Take-Home Messages
-
•
This case highlights the importance of multimodality imaging for diagnosis of a SoVA and for planning surgical repair.
-
•
SoVAs can lead to embolic strokes.
-
•
Clinicians should consider SoVAs in the differential diagnosis for a patient presenting with a stroke.
Past Medical History
The patient’s medical history included hypertension and hyperlipidemia. He denied any previous history of stroke or transient ischemic attacks. He also denied alcohol or drug use, but he reported a remote history of tobacco use. There was no significant family history of cardiovascular or neurologic conditions. The patient was physically active at baseline.
Differential Diagnosis
Potential causes of the patient’s stroke included cardiac arrhythmia (atrial fibrillation or atrial flutter), plaque rupture, malignant disease, patent foramen ovale (PFO), cardiac thrombus, cardiac myxoma, cardiac cyst, and aneurysm.
Investigations
Magnetic resonance imaging (MRI) of the brain revealed multifocal acute infarcts in the left MCA territory suggestive of an embolic origin. An electrocardiogram showed normal sinus rhythm with a first-degree atrioventricular block, without evidence of ischemic changes or previous myocardial infarctions. Telemetry monitoring revealed no arrhythmias. The laboratory work-up was significant for a low-density lipoprotein cholesterol level of 71 mg/dL and a hemoglobin A1c value of 6.2%. The patient was started on a daily aspirin and antihypertensive and lipid-lowering medications.
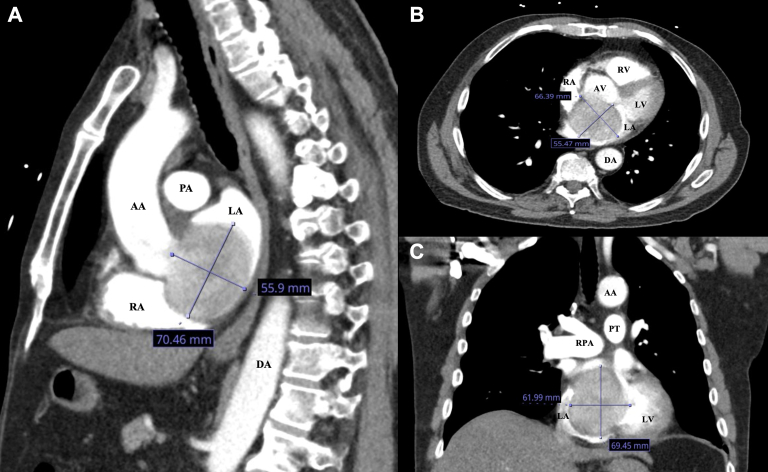
A follow-up CT scan of the brain showed no signs of hemorrhagic conversion. Imaging of the left and right internal and external carotid arteries revealed <25% stenosis. A nongated CT scan of the chest, abdomen, and pelvis identified no evidence of adenopathy or metastatic disease but raised concerns for a large, 7.0 cm × 5.6 cm masslike cardiac lesion suspected to be a myxoma or cyst. The masslike lesion caused nearly complete obstruction of the left atrium (LA) (Figures 1A to 1C).
Figure 1.
Initial Nongated Computed Tomography of the Chest in Sagittal, Axial, and Coronal Views
Findings concerning for a large 7.0 cm × 5.6 cm masslike cardiac lesion suspected to be a myxoma or a cyst in (A) sagittal, (B) axial, and (C) coronal views. The masslike lesion caused nearly complete obstruction of the left atrium (LA). AA = ascending aorta; AV = aortic valve; DA = descending aorta; LV = left ventricle; PA = pulmonary artery; PT = pulmonary trunk; RA = right atrium; RPA = right pulmonary artery; RV = right ventricle.
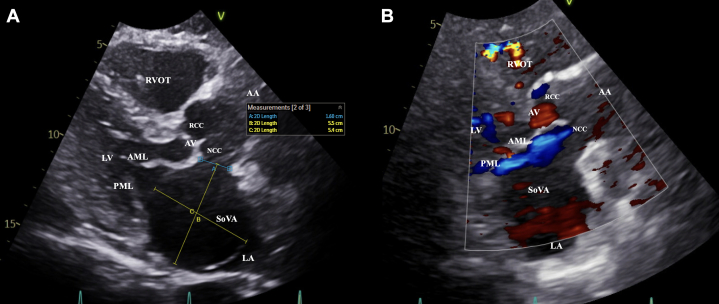
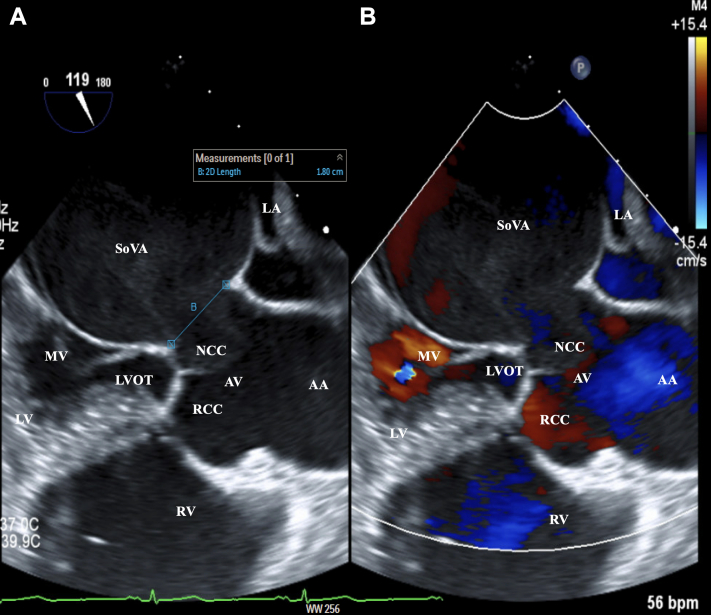
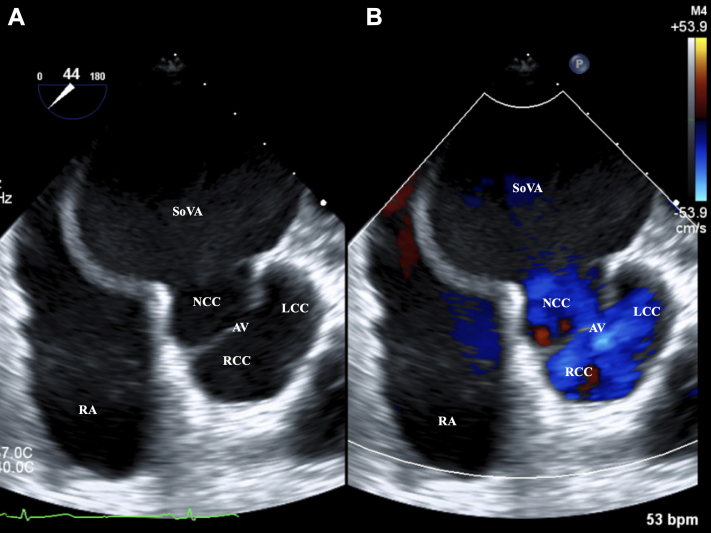
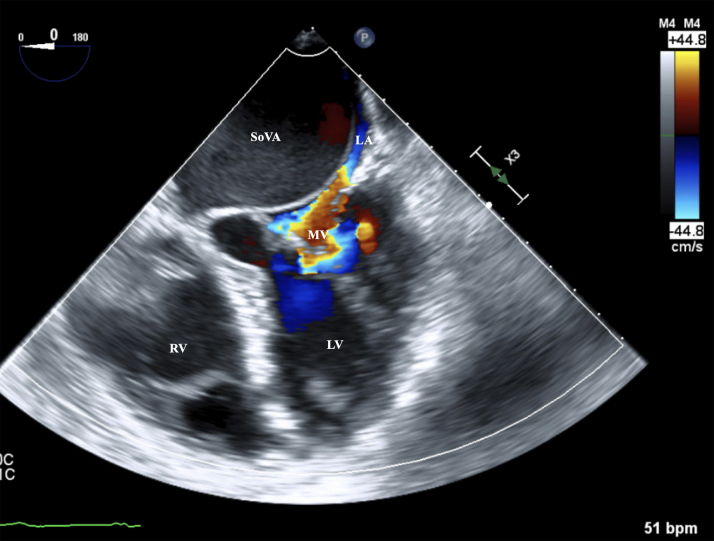
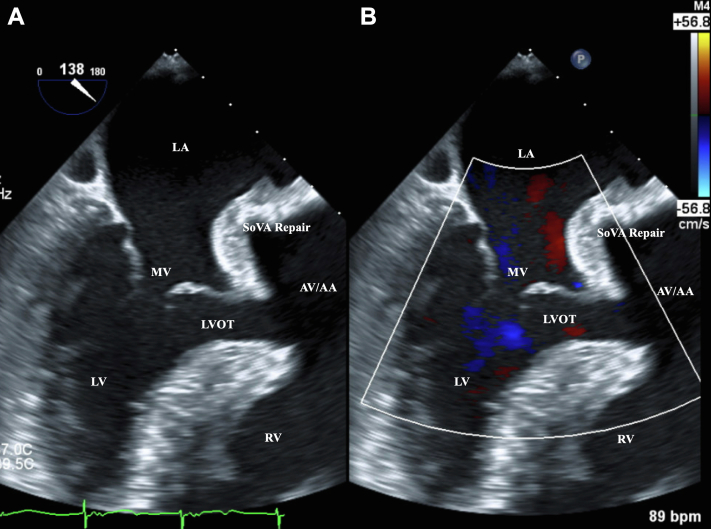
Transthoracic echocardiography (TTE) revealed a left ventricular ejection fraction of 65% without segmental or regional wall motion abnormalities. The right ventricular size and systolic function were normal. There was no significant valvular stenosis or regurgitation. TTE demonstrated a large sinus of Valsalva aneurysm (SoVA) originating from the noncoronary sinus. The aneurysmal sac was protruding into the LA and causing nearly complete obstruction (Figures 2A and 2B, Videos 1 and 2). A PFO could not be definitively ruled out because of limited visualization. Cardiothoracic surgery was consulted, and surgical repair of the SoVA was recommended. Preoperative coronary angiography showed mild coronary artery disease and confirmed the presence of the SoVA on contrast injection. There was no evidence of contrast extravasation to suggest rupture (Video 3). A 3-dimensional reconstruction of the SoVA that was created using the initial nongated CT scan of the chest provided enhanced visualization (Video 4). Preoperative transesophageal echocardiography (TEE) further reconfirmed the SoVA. The neck of the aneurysm sac measured 1.8 cm (Figures 3A, 3B, 4A, 4B, and 5, Video 5, Video 6, Video 7).
Figure 2.
Initial Transthoracic Echocardiography in the Parasternal Long-Axis View With Color Doppler
A large sinus of Valsalva aneurysm (SoVA) originating from the noncoronary sinus, protruding into the left atrium (LA), and causing nearly complete obstruction. (A) The aneurysm measured 5.5 cm × 5.4 cm, and the aneurysm sac measured 1.6 cm on the parasternal long-axis view. (B) A communication is shown from the noncoronary sinus into the aneurysmal sac by using color Doppler. AML = anterior mitral leaflet; AV = aortic valve; NCC = noncoronary cusp; PML = posterior mitral leaflet; RCC = right coronary cusp; RVOT = right ventricle outflow tract; other abbreviations as in Figure 1.
Figure 3.
Preoperative Transesophageal Echocardiography in the Midesophageal Long-Axis View With Color Doppler
A large sinus of Valsalva aneurysm (SoVA) originating from the noncoronary sinus, protruding into the left atrium (LA), and causing nearly complete obstruction. (A) The large aneurysm sac measured 1.8 cm. (B) A communication is shown from the noncoronary sinus into the aneurysmal sac by using color Doppler. bpm = beats/min; MV = mitral valve; LVOT = left ventricular outflow tract; other abbreviations as in Figures 1 and 2.
Figure 4.
Preoperative Transesophageal Echocardiography in the Midesophageal Aortic Valve Short-Axis View With Color Doppler
(A) A large sinus of Valsalva aneurysm (SoVA) originating from the noncoronary sinus. (B) A communication is shown from the noncoronary sinus into the aneurysmal sac by using color Doppler. LCC = left coronary cusp; other abbreviations as in Figures 1 and 2.
Figure 5.
Preoperative Transesophageal Echocardiography in the Midesophageal 4-Chamber View With Color Doppler
The figure shows a large sinus of Valsalva aneurysm originating from the non-coronary sinus protruding into the left atrium, causing a near-complete obstruction on preoperative transesophageal echocardiogram in mid-esophageal four-chamber view. LA = left atrium; SoVA = sinus of Valsalva aneurysm. Abbreviations as in Figures 1 and 3.
Management
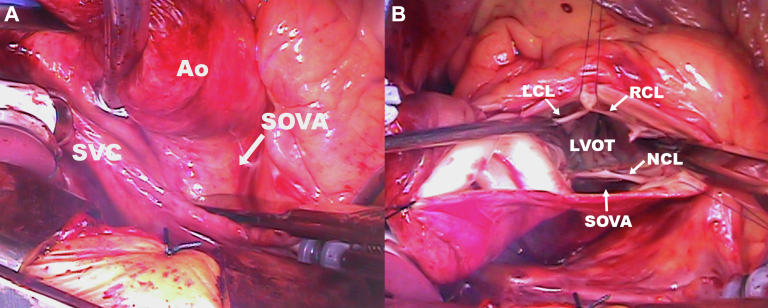
Intraoperative findings revealed evidence of a SoVA originating from the noncoronary sinus, with nearly complete obstruction of the LA (Figures 6A and 6B). The patient underwent successful surgical repair of the SoVA aneurysm, with an aortic valve and aortic root replacement with coronary artery reimplantation through a Bentall procedure using a porcine composite graft and reconstruction of the aortomitral curtain using a patch. During the procedure, a PFO was identified and subsequently closed. Postoperative TEE confirmed the successful repair of the SoVA (Figures 7A and 7B, Video 8). A tissue sample of the aneurysm was sent for pathologic examination, with only degenerative changes identified.
Figure 6.
Intraoperative Images of the SoVA
(A) Findings of a large sinus of Valsalva aneurysm (SoVA). (B) A transverse aortotomy was performed and the aortic valve was exposed, revealing a 7-cm aneurysm behind the aorta (Ao) and severely compressing the left atrium. LCL = left coronary leaflet; LVOT = left ventricular outflow tract; NCL = noncoronary leaflet; RCL = right coronary leaflet; SVC = superior vena cava.
Figure 7.
Postoperative Transesophageal Echocardiography in the Midesophageal Long-Axis View With Color Doppler
(A) The surgically repaired sinus of Valsalva aneurysm (SoVA). (B) A communication is no longer present after surgical repair using color Doppler. Abbreviations as in Figure 1, Figure 2, Figure 3.
Outcome and Follow-Up
The patient made a full recovery in the cardiovascular intensive care unit, with no complications. The probable cause of his stroke was attributed to thrombus formation within the SoVA that embolized. The patient is scheduled for outpatient follow-up with neurology, cardiology, and cardiothoracic surgery after completing inpatient rehabilitation.
Discussion
A SoVA is a rare cardiac condition caused by the dilation of 1 of the 3 coronary sinuses (left, right, or noncoronary sinus). SoVAs account for <1% of all cases of open heart surgery, with the right coronary sinus being the most commonly affected (in approximately 90% of cases). The noncoronary and left coronary sinuses are the least frequently involved. Men are affected more commonly than women, with a male-to-female ratio of approximately 4:1.1, 2, 3, 4 SoVAs can be congenital or acquired, often resulting from a weakness between the aortic media and the annulus fibrosus. Contributing factors to their development include previous trauma, connective tissue disorders, hypertension, arteriosclerosis, and infections (eg, endocarditis, tuberculosis, or syphilis).5 The patient had no significant previous medical history except for hypertension. He had no previous imaging or echocardiograms performed before his presentation.
Most patients with an unruptured SoVA are asymptomatic, but as the aneurysm enlarges, they can develop chest pain, dyspnea, syncope, valvular dysfunction (aortic regurgitation), ventricular outflow tract obstructions, or cardiac arrhythmias (heart block).6 In our patient, TTE and TEE imaging surprisingly did not show evidence of aortic regurgitation or outflow tract obstruction. Rarely, an embolic stroke may be the initial presentation of a SoVA.7,8 As a SoVA enlarges, the risk for thrombus development can increase in response to stagnation of blood within the aneurysm sac. MRI in our patient showed multifocal infarcts in the left MCA territory suggestive of an embolic origin. The cause of the patient’s stroke was suspected to be the result of thrombus arising from the SoVA that embolized. Because our patient received tenecteplase on arrival to the emergency department, there was a limited evaluation for thrombus on imaging.
In cases of SoVA rupture, patients typically present with severe chest pain, heart failure, hemodynamic instability, or cardiac arrest. If left untreated, a patient’s prognosis is poor, with a median life expectancy of <1 year after rupture.4 Surgical repair is indicated in asymptomatic patients with an aneurysm larger than 5.5 cm or documented progression of more than 0.5 cm per year. The thresholds for intervention may vary on the basis of the presence of other genetic conditions or connective tissue disorders.9 Surgical repair was also pursued in our patient because the SoVA caused nearly complete obstruction of the LA. If left untreated, this could have led to hemodynamic compromise and deterioration of the mitral valve as the aneurysm continued to grow. Surgical repair typically involves an open approach through median sternotomy and cardiopulmonary bypass. On the basis of the size and involvement of the SoVA, replacement of the aortic valve or aortic root may also be required.10 In the case of large SOVAs, as in our patient, primary patch repair of the aneurysm is performed, along with aortic valve and root replacement with coronary reimplantation. The diagnosis and surgical planning for the patient’s SoVA required a coordinated effort from a multidisciplinary team and the use of multimodality imaging techniques, including CT, TTE, TEE, and coronary angiography.
Conclusions
A SoVA originating from the noncoronary sinus and resulting in nearly complete obstruction of the LA is rare. A detailed clinical history, a multidisciplinary team approach, and multimodality imaging were required for a prompt diagnosis and surgical repair to prevent recurrent strokes or potential rupture of the aneurysm.
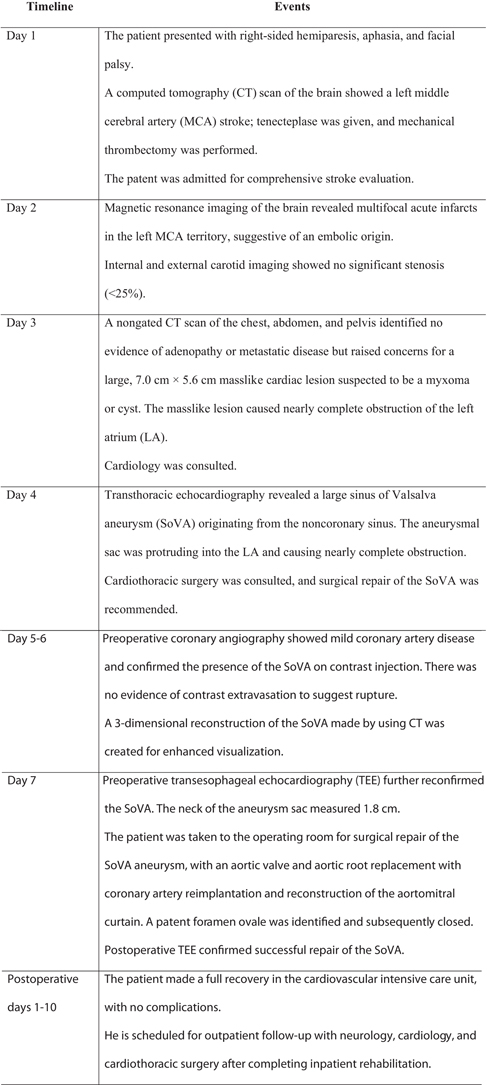
Visual Summary.
Timeline of Clinical Course and Treatment
| Timeline | Events |
|---|---|
| Day 1 | The patient presented with right-sided hemiparesis, aphasia, and facial palsy. A computed tomography (CT) scan of the brain showed a left middle cerebral artery (MCA) stroke; tenecteplase was given, and mechanical thrombectomy was performed. The patent was admitted for comprehensive stroke evaluation. |
| Day 2 | Magnetic resonance imaging of the brain revealed multifocal acute infarcts in the left MCA territory, suggestive of an embolic origin. Internal and external carotid imaging showed no significant stenosis (<25%). |
| Day 3 | A nongated CT scan of the chest, abdomen, and pelvis identified no evidence of adenopathy or metastatic disease but raised concerns for a large, 7.0 cm × 5.6 cm masslike cardiac lesion suspected to be a myxoma or cyst. The masslike lesion caused nearly complete obstruction of the left atrium (LA). Cardiology was consulted. |
| Day 4 | Transthoracic echocardiography revealed a large sinus of Valsalva aneurysm (SoVA) originating from the noncoronary sinus. The aneurysmal sac was protruding into the LA and causing nearly complete obstruction. Cardiothoracic surgery was consulted, and surgical repair of the SoVA was recommended. |
| Day 5-6 | Preoperative coronary angiography showed mild coronary artery disease and confirmed the presence of the SoVA on contrast injection. There was no evidence of contrast extravasation to suggest rupture. A 3-dimensional reconstruction of the SoVA made by using CT was created for enhanced visualization. |
| Day 7 | Preoperative transesophageal echocardiography (TEE) further reconfirmed the SoVA. The neck of the aneurysm sac measured 1.8 cm. The patient was taken to the operating room for surgical repair of the SoVA aneurysm, with an aortic valve and aortic root replacement with coronary artery reimplantation and reconstruction of the aortomitral curtain. A patent foramen ovale was identified and subsequently closed. Postoperative TEE confirmed successful repair of the SoVA. |
| Postoperative days 1-10 | The patient made a full recovery in the cardiovascular intensive care unit, with no complications. He is scheduled for outpatient follow-up with neurology, cardiology, and cardiothoracic surgery after completing inpatient rehabilitation. |
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Acknowledgments
The authors thank our colleagues within the West Virginia University Heart and Vascular Institute for their assistance in this clinical case.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Initial TTE in Parasternal Long Axis View
Initial TTE in Parasternal Long Axis View With Color Doppler
Preoperative Coronary Angiography Identifying the Sinus of Valsalva Aneurysm Upon Contrast Injection
3D Reconstruction of the Sinus of Valsalva Aneurysm Using the Initial Nongated CT of the Chest
Preoperative TEE in Mid-Esophageal Long Axis View With Color Doppler
Preoperative TEE in Mid-Esophageal Aortic Valve Short Axis View With Color Doppler
Preoperative TEE in Mid-Esophageal Four Chamber View With Color Doppler
Postoperative TEE in Mid-Esophageal Long Axis View With Color Doppler
References
- 1.Arcario M.J., Lou S., Taylor P., et al. Sinus of Valsalva aneurysms: a review with perioperative considerations. J Cardiothorac Vasc Anesth. 2021;35(11):3340–3349. doi: 10.1053/j.jvca.2020.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Takach T.J., Reul G.J., Duncan J.M., et al. Sinus of Valsalva aneurysm or fistula: management and outcome. Ann Thorac Surg. 1999;68(5):1573–1577. doi: 10.1016/s0003-4975(99)01045-0. [DOI] [PubMed] [Google Scholar]
- 3.Dev V., Goswami K.C., Shrivastava S., et al. Echocardiographic diagnosis of aneurysm of the sinus of Valsalva. Am Heart J. 1993;126:930–936. doi: 10.1016/0002-8703(93)90709-i. [DOI] [PubMed] [Google Scholar]
- 4.Feldman D.N., Roman M.J. Aneurysms of the sinuses of Valsalva. Cardiology. 2006;106:73–81. doi: 10.1159/000092635. [DOI] [PubMed] [Google Scholar]
- 5.Fishbein M.C., Obma R., Roberts W.C. Unruptured sinus of Valsalva aneurysm. Am J Cardiol. 1975;35:918–922. doi: 10.1016/0002-9149(75)90129-0. [DOI] [PubMed] [Google Scholar]
- 6.Pólos M., Șulea C.M., Benke K., et al. Giant unruptured sinus of Valsalva aneurysm successfully managed with valve-sparing procedure – a case report. J Cardiothorac Surg. 2020;15(1):6. doi: 10.1186/s13019-020-1061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stöllberger C., Seitelberger R., Fenninger C., et al. Aneurysm of the left sinus of Valsalva. An unusual source of cerebral embolism. Stroke. 1996;27(8):1424–1426. doi: 10.1161/01.str.27.8.1424. [DOI] [PubMed] [Google Scholar]
- 8.Ravishankar M., Ghergherehchi A., Liu J., et al. Large sinus of Valsalva aneurysm complicated by thrombus formation. Methodist Debakey Cardiovasc J. 2020;16(3):e8–e10. doi: 10.14797/mdcj-16-3-e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hiratzka L.F., Bakris G.L., Beckman J.A., et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. J Am Coll Cardiol. 2010;55:e27–e129. doi: 10.1016/j.jacc.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 10.Weinreich M., Yu P.J., Trost B. Sinus of Valsalva aneurysms: review of the literature and an update on management. Clin Cardiol. 2015;38(3):185–189. doi: 10.1002/clc.22359. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Initial TTE in Parasternal Long Axis View
Initial TTE in Parasternal Long Axis View With Color Doppler
Preoperative Coronary Angiography Identifying the Sinus of Valsalva Aneurysm Upon Contrast Injection
3D Reconstruction of the Sinus of Valsalva Aneurysm Using the Initial Nongated CT of the Chest
Preoperative TEE in Mid-Esophageal Long Axis View With Color Doppler
Preoperative TEE in Mid-Esophageal Aortic Valve Short Axis View With Color Doppler
Preoperative TEE in Mid-Esophageal Four Chamber View With Color Doppler
Postoperative TEE in Mid-Esophageal Long Axis View With Color Doppler