Abstract
Recognizing the characteristics of the zygomatic process of the maxilla (ZPM) has several applications in implant dentistry and orthodontics. The present study evaluated the relationship between ZPM morphology, as obtained from panoramic images, and sinus pneumatization within the ZPM, according to cone-beam computed tomography (CBCT). CBCT and panoramic images of 300 patients were obtained, and the patients were divided into three age groups: Group I (15–34 years), Group II (35–55 years), and Group III (≥ 55 years). ZPM morphology was classified into J-shaped and non-J-shaped types based on panoramic images. The ZPM volume, maxillary sinus volume, and extent of sinus pneumatization within the ZPM were measured using CBCT scans, and their relationship to ZPM morphology classification was evaluated. Statistical analyses were performed using the Shapiro–Wilk test, one-way ANOVA, independent sample t-test, Mann–Whitney U test, Kruskal–Wallis test, and chi-square test (α = 0.05). Participants ranged in age from 17 to 82 years, and 67% were female. Most ZPMs were J-shaped (75%). J-shaped ZPMs had significantly greater sinus volume (1.83 ± 0.81 cm3), sinus pneumatization (53.56 ± 12.60%), and ZPM volume (3.50 ± 0.98 cm3) compared to non-J-shaped ZPMs (P < 0.05). Male participants had significantly larger ZPM volumes than females (P = 0.039). Sinus pneumatization and maxillary sinus volume were comparable across age groups and between gender. The presence of a non-J-shaped ZPM might be associated with less sinus pneumatization than J-shaped ZPMs, regardless of the patient’s age or gender. Therefore, non-J-shaped ZPMs might offer more bone availability for various applications in dentistry.
Keywords: Cone-beam computed tomography, Maxillary sinus pneumatization, Radiography, Panoramic, Zygomatic process of the maxilla
Introduction
The zygomatic process of the maxilla (ZPM) connects the maxillary bone to the zygoma at the zygomaticomaxillary suture (Angelieri et al. 2017a, b). It forms the superolateral border of the maxillary sinus and is continuous with the alveolar process inferiorly (Iwanaga et al. 2019). On panoramic radiographs, this process may appear as a U-shaped, V-shaped, or J-shaped radiopaque structure above the first maxillary molar (Perschbacher 2012; Karjodkar 2019, Ongole and N 2021). Several factors—such as age, the masticatory system, the presence of posterior teeth, and interference from a prominent zygomaticomaxillary suture (ZMS)—can influence the ZPM’s shape, density, and volume through sinus pneumatization, thereby altering its radiographic borders (Maddux and Butaric 2017; Mallya and Lam 2018; Ito et al. 2022).
The characteristics of the ZPM have important applications in implant dentistry and orthodontics. In orthodontics, the ZPM is considered a reliable site for extra-alveolar skeletal anchorage due to its favorable bone density, which supports screws for miniplate fixation (Präger et al. 2015; Arango et al. 2022). In implantology, zygomatic implants are an alternative approach for rehabilitating patients with severely atrophic maxillae or highly pneumatized sinuses, avoiding the need for complex bone augmentation procedures (Fortin 2017; Pellegrino et al. 2020). Evaluating bone availability in both the maxilla and zygoma is essential for determining implant–bone contact, the insertion path, and the appropriate surgical technique (Uchida et al. 2001; Moro et al. 2021). In zygomatic implant placement, the ZPM plays a key role in providing apical fixation (Fortin 2017). Additionally, ensuring maximum bone contact between zygomatic implants and the ZPM is vital to prevent complications such as fixation loss, mucosal fenestration, prosthetic failure, and to ensure implant stability (Filho et al. 2016; Fortin 2017). The ZPM has also been identified as a reliable donor site for bone augmentation prior to implant placement (Gellrich et al. 2013; Younes et al. 2025). It can be used in sinus lift procedures or in particulate form for reconstructing peri-implant defects (Kainulainen et al. 2002; Johansson et al. 2010). However, atrophy in this area may contraindicate bone harvesting (Held et al. 2005). Therefore, assessing ZPM morphology and volume—both of which can be affected by maxillary sinus pneumatization—is essential.
Sinus pneumatization is a key factor influencing the amount of bone available for implant placement or bone graft harvesting in both the alveolar process and the ZPM. While previous studies have reported on sinus pneumatization in the alveolar process (Cavalcanti et al. 2018; Elsayed et al. 2019, 2023; Alqahtani et al. 2020; Wu et al. 2022), to our knowledge, pneumatization within the ZPM has not yet been thoroughly investigated. An increase in maxillary sinus volume beyond 20 cm3 has been identified as a predictive risk factor for zygomaticomaxillary complex fractures due to trauma. Pneumatization extending into the ZPM can enlarge the surface area of the zygomatic buttress and reduce its resistance to trauma (Buller et al. 2023). It may also limit bone availability and increase the risk of sinus-related complications (Gracco et al. 2010; Präger et al. 2015). Therefore, evaluating the extent of sinus pneumatization within the ZPM is important for treatment planning in both implantology and orthodontics.
Routine dental examinations and treatment planning are commonly conducted using panoramic radiographs (Choi 2011). However, the accuracy of panoramic imaging in assessing three-dimensional structures like the ZPM must be confirmed using more advanced imaging techniques. Cone-beam computed tomography (CBCT) is a reliable method for evaluating bone density and availability in the ZPM (Kopecka et al. 2014; Anbiaee et al. 2022). The present study aimed to assess the relationship between ZPM morphology, as visualized on panoramic images, and the extent of sinus pneumatization within the ZPM using CBCT.
Method and materials
The study participants
The protocol for this cross-sectional study was approved by the Ethics Committee of Mashhad University of Medical Sciences (Code: IR.MUMS.DENTISTRY.REC.1403.105). CBCT and panoramic images of patients referred to two private oral radiology centers in Mashhad, Khorasan-e-Razavi, Iran, between June 2023 and June 2024 were evaluated. All eligible patients who met the following inclusion criteria during this period were included:
Patients over 15 years of age, to ensure complete maturation of the ZMS (Angelieri et al. 2017a, b).
No history of trauma, sinus or maxillary tumors, sinus surgery, or systemic diseases affecting the maxillary sinus or facial bones.
Availability of both CBCT and panoramic images.
Visualization of the ZMS in CBCT images.
Proper image quality in both CBCT and panoramic radiographs.
The participants’ age and gender were recorded. Patient ages were divided into three groups: Group I (15–34 years, youth group), Group II (35–55 years, middle-aged group), and Group III (≥ 55 years, elderly group).
All CBCT scans were obtained using a CBCT device (Planmeca, Helsinki, Finland) with a field of view (FOV) of 20 × 10 cm and standard exposure settings. Panoramic images were taken with the Planmeca Promax 2DS3 device.
The ZPM morphology classification
Based on the presence or absence of the medial wall (Karjodkar 2019, Ongole and N 2021), the shape of the ZPM on panoramic images was classified as either J-shaped or non-J-shaped (Fig. 1). The latter group included both V-shaped and U-shaped ZPMs.
Fig. 1.
The classification of ZPM according to panoramic view: A) J-shaped; B) U-shaped; and C) V-shaped
The ZMS identification
CBCT images were analyzed using Romexis Viewer software (v6.4.6; Planmeca), with the layer thickness set to 0.6 mm. Head orientation was adjusted for each patient (Fig. 2). To identify the lateral border of the ZPM in the axial plane, the first slice in which the ZMS became visible was selected, and a vertical line (red line) was aligned with the ZMS (Figs. 3A, 3B). The posterior limit of the ZPM in the coronal section was identified as the first slice where the lower border of the zygoma made contact with the maxilla (Fig. 3C).
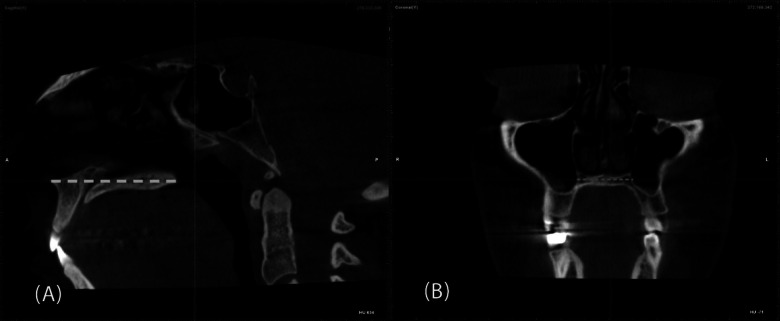
Fig. 2.
Adjusting the orientation of the patient’s head: A) In the sagittal plane, the anterior and posterior nasal spines were connected (yellow dashed line). Then, the horizontal plane was adjusted in a way that became parallel to the yellow dashed line; B) In the coronal plane, a pink dashed line was drawn along the floor of the nasal cavity. The head position was adjusted so that this pink line became parallel to the horizontal plane, ensuring standardized orientation across all cases
Fig. 3.
Localization of ZMS: A) In the axial view, the first section in which ZMS was identified was selected (yellow arrow points to ZMS); B) the vertical plane (red line) was aligned with the ZMS; C) in the coronal view, the first section, in which the lower border of the zygoma connects to the maxilla, was selected (pink arrow)
Evaluation of the ZPM volume and sinus pneumatization
Manual segmentation, without applying threshold values, was used for volumetric measurements using the Free Region Grow Tool in Romexis Viewer software (v6.4.6; Planmeca). The reliability and accuracy of this method have been validated in previous studies through physical and software-based comparisons (Reham Ashraf et al. 2017, Mohamed and Abdalh 2023).
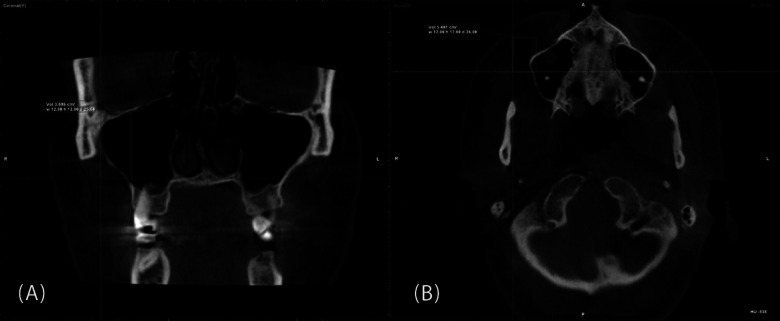
To evaluate ZPM volume, the Measure Cube tool was selected from the Annotation menu, and a cube was drawn in the coronal view to define the boundaries of the ZPM (Fig. 4A). The medial side of the cube was defined by a tangential line drawn along the buccal border of the alveolar process of the maxilla. The inferior and superior boundaries were defined by the nasal and orbital floors, respectively. In the axial section, the posterior boundary was the point of connection between the zygoma and maxilla (green line), and the anterior boundary was the anterior wall of the maxilla (Fig. 4B).
Fig. 4.
Drawing the measuring cube: A) In the coronal section, the inferior side of the cube was aligned with an imaginary line extending from the nasal floor. The medial side of the cube aligns with the imaginary line that is tangential to the buccal part of the alveolar process of the maxilla (red line), and the orbital floor forms the superior side of the cube; B) In the axial section, the anterior wall of the maxilla forms the anterior side of the cube, the lateral side of the cube is aligned to the ZMS (vertical red line), and the posterior side of the cube is aligned with the horizontal green line, which defined the junction between the zygoma and maxilla
Within this cube, the ZPM volume was measured using the Free Region Grow Tool in the Annotation menu, starting from the nasal floor in the axial view (Fig. 5A). Subsequently, the boundaries of the sinus were outlined, and the volume of sinus pneumatization within the ZPM was calculated (Fig. 5B). All measurements were performed by a radiologist (F.N.) and a final-year dental student (E.L.). Inter-rater agreement was assessed using Kappa statistics.
Fig. 5.
Measuring the ZPM volume and the level of maxillary sinus pneumatization into the ZPM: A) After selecting the free region grow tool, in the axial section, mark the bony border of the ZPM in the cube until it reaches the orbital floor. B) After measuring the ZPM volume, select the free region grow tool again and start marking the border of the maxillary sinus in the ZPM (yellow line highlights the ZPM border)
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics version 27 (IBM Corp., Armonk, NY, USA). Data normality was assessed using the Shapiro–Wilk test. The Mann–Whitney U test, independent samples t-test, one-way ANOVA, Kruskal–Wallis test, and chi-square test were used for data analysis. To ensure the adequacy of the sample size, the effect size was calculated. A p-value of < 0.05 was considered statistically significant.
Results
The kappa coefficient was 0.89, indicating a very good level of agreement between the evaluators. When comparing ZPM volume, sinus volume, and sinus pneumatization between the J-shaped and non-J-shaped groups, the results demonstrated large to very large effect sizes. Specifically, Cohen’s d was 0.83 for ZPM volume, 1.30 for sinus volume, and 1.83 for sinus pneumatization. Consequently, the sample size was deemed adequate.
Most participants (67%) were female, with a mean age of 47.3 years (range: 17 to 82 years). The majority of ZPMs (75%) were classified as J-shaped. Table 1 presents the distribution of J-shaped and non-J-shaped ZPM morphology across demographic groups. Chi-square test results showed that ZPM morphology was not significantly associated with either gender or age group.
Table 1.
The relationship between the ZPM morphology and participants demographic variables
| Variables | Categories | ZPM* Morphology | P value | ||
|---|---|---|---|---|---|
| J-shaped | Non-J-shaped | Total | |||
| Gender | Male | 72 (24.8) | 27 (8.3) | 99 (33.0) | 0.807 |
| Female | 153 (50.3) | 48 (16.8) | 201 (67.0) | ||
| Total | 225 (75.0) | 75 (25.0) | 300 (100) | ||
| Age range | 15–34 years | 84 (25.5) | 18 (8.5) | 102 (34.0) | 0.331 |
| 35–54 years | 66 (24.8) | 33 (8.3) | 99 (33.0) | ||
| ≥ 55 years | 75 (24.8) | 24 (8.3) | 99 (33.0) | ||
| Total | 225 (75.0) | 75 (25.0) | 300 (100.0) | ||
*ZPM = Zygomatic process of the maxilla
Table 2 displays ZPM volume, sinus volume, and sinus pneumatization based on demographic variables and ZPM morphology. According to the independent samples t-test, male participants had significantly larger ZPM volumes than female participants (P = 0.039). However, sinus volume and sinus pneumatization did not significantly differ by gender. One-way ANOVA indicated that ZPM volume and sinus volume were comparable across age groups, while the Kruskal–Wallis test showed that sinus pneumatization was also similar among the different age groups.
Table 2.
Mean ± standard deviation of the ZPM volume (cm3), sinus volume (cm3), and maxillary sinus pneumatization (%) based on demographic variables and the ZPM morphology
| Variables | Categories | ZPM* volume | Sinus volume | Pneumatization |
|---|---|---|---|---|
| Gender | Male | 3.61 ± 1.12 | 1.60 ±.93 | 44.78 ± 19.46 |
| Female | 3.15 ± 0.97 | 1.56 ±.87 | 46.29 ± 18.72 | |
| P value | 0.039† | 0.818 | 0.846 | |
| Age range | 15–34 years | 3.26 ± 0.85 | 1.57 ±.77 | 47.58 ± 14.20 |
| 35–54 years | 3.08 ±.77 | 1.46 ±.88 | 43.41 ± 21.00 | |
| ≥ 55 years | 3.34 ± 1.27 | 1.68 ± 1.02 | 47.74 ± 19.61 | |
| P value | 0.571 | 0.624 | 0.719 | |
| ZPM morphology | J-shaped | 3.50 ± 0.98 | 1.83 ± 0.81 | 53.56 ± 12.60 |
| Non-J-shaped | 2.69 ± 0.98 | 0.82 ± 0.66 | 27.95 ± 17.49 | |
| P value | 0.001‡ | < 0.001‡ | < 0.001† |
*ZPM = Zygomatic process of the maxilla
†Values less than 0.05 represent a significant difference between the groups according to the independent sample t-test
‡Values less than 0.05 represent a significant difference between the groups according to the Mann–Whitney U test
With respect to ZPM morphology, the J-shaped group demonstrated significantly higher values in all parameters: sinus volume (1.83 ± 0.81 cm3), maxillary sinus pneumatization (53.56 ± 12.60%), and ZPM volume (3.50 ± 0.98 cm3), compared to the non-J-shaped group (P < 0.05).
Discussion
This study provides novel insights into the relationship between maxillary sinus pneumatization within the ZPM and its morphological variations as observed in panoramic radiographs. ZPM morphology on panoramic images has previously been classified into J-shaped, U-shaped, and V-shaped categories (Karjodkar 2019, Ongole and N 2021). In this study, the U-shaped and V-shaped forms were combined into a single non-J-shaped group to reduce inter-observer variability.
The results indicated that ZPM volume, sinus volume, and sinus pneumatization within the ZPM were significantly higher in the J-shaped group compared to the non-J-shaped group. According to Mallya and Lam (Mallya and Lam 2018), when the sinus extends deeply into the ZPM, the walls of the process tend to be thinner, resulting in a J-shaped appearance. Conversely, limited sinus penetration is associated with thicker ZPM walls, leading to non-J-shaped forms. This finding is clinically relevant, as Buller et al. (Buller et al. 2023) reported that a maxillary sinus volume exceeding 20 cm3 and increased sinus height are risk factors for zygomaticomaxillary complex fractures. Therefore, patients with J-shaped ZPMs—indicating greater maxillary sinus pneumatization—may be more susceptible to such fractures than those with non-J-shaped ZPMs. These results highlight the importance of careful radiographic interpretation of ZPM morphology, especially in treatment planning for implant placement and orthodontic anchorage. While previous studies have primarily focused on sinus pneumatization in the alveolar process of the maxilla (Cavalcanti et al. 2018; Elsayed et al. 2019, 2023; Alqahtani et al. 2020; Wu et al. 2022), this is the first study to evaluate sinus pneumatization specifically within the ZPM.
As demonstrated in the present study, non-J-shaped ZPMs may offer greater bone availability due to reduced sinus pneumatization. Bone availability in this region is critical for several clinical applications, including the placement of zygomatic implants, insertion of orthodontic mini-screws, and harvesting of bone grafts. Zygomatic implants are commonly used in cases of severe maxillary atrophy, and the ZPM is frequently considered a suitable site for apical fixation (Filho et al. 2016; Pellegrino et al. 2020). In orthodontics, the ZPM serves as a common site for extra-alveolar skeletal anchorage. Präger et al. (Präger et al. 2015) reported that, in most cases, the ZPM provides sufficient bone for screw placement. However, excessive sinus pneumatization can reduce bone quality and compromise mini-screw stability, potentially leading to failure. Bone availability is also a key factor when evaluating the ZPM as a donor site for bone grafting (Held et al. 2005).
In this study, sinus pneumatization was assessed through volumetric measurements of both the sinus and ZPM using CBCT imaging within Romexis Viewer software. The validity and reliability of this method have been supported by previous research. Ashraf et al. (Reham Ashraf et al. 2017) validated the accuracy of Romexis Viewer for volumetric analysis by comparing CBCT-based manual segmentation with physical volumes determined by the water displacement method—considered the gold standard in volumetric assessment. Their findings showed an excellent correlation (r = 0.989), confirming the precision of CBCT-based measurements for maxillary sinus volumetry. In contrast, most prior studies have evaluated sinus pneumatization in the alveolar process of the maxilla using linear measurements obtained from panoramic images or CBCT scans (Cavalcanti et al. 2018; Elsayed et al. 2019, 2023; Alqahtani et al. 2020; Wu et al. 2022). For instance, Alqahtani et al. (Alqahtani et al. 2020) assessed pneumatization by measuring the vertical distance between the sinus floor and the inferior border of the alveolar ridge after posterior tooth extraction. Similarly, Elsayed et al. (Elsayed et al. 2019) evaluated the distance from the sinus floor to the apices of posterior teeth—both using panoramic radiographs. Unlike those studies, the present investigation used CBCT, which offers superior accuracy in assessing the volume of maxillofacial structures (Abdinian et al. 2017). However, it is important to note that CBCT comes with higher cost and increased radiation exposure, which is why panoramic radiographs are more commonly used in routine dental evaluations. Despite these limitations, our findings showed a significant correlation between ZPM morphology on panoramic images and CBCT-derived measurements of ZPM volume, sinus volume, and sinus pneumatization. This suggests that panoramic radiographs can provide valuable preliminary information for treatment planning, especially when CBCT is not readily available.
The results indicated that the level of maxillary sinus pneumatization within the ZPM was higher in the elderly group; however, no statistically significant differences were observed among the age groups. Similar to the present findings, previous studies have also reported no correlation between sinus volume and age (Sahlstrand-Johnson et al. 2011; Bornstein et al. 2019; Gulec et al. 2020; Marino et al. 2020). In contrast, another study measured maxillary sinus pneumatization into the alveolar process using CBCT in 293 patients and reported that the level of maxillary sinus pneumatization in 18–34 years old participants was significantly higher than that of 35–59 years old and ≥ 60 years old participants (Wu et al. 2022). However, their age distribution was uneven, with most participants falling within the 18–34 age group. In contrast, the present study had a more balanced age distribution. Additionally, their study measured sinus pneumatization into the alveolar process, while the current research focused specifically on pneumatization within the ZPM. Several factors—such as sex, age, tooth loss, malocclusion, growth patterns of the jaws, orthodontic treatment, and surgical interventions—can influence maxillary sinus dimensions (Dinç and İçöz 2024).
Sexual dimorphism is often observed in craniofacial structures, particularly in the zygomatic region (Schlager and Rüdell 2017; Nagare et al. 2018). In the current study, ZPM volume was significantly higher in male participants than in females. Although males also had a higher mean sinus volume within the ZPM, the difference was not statistically significant. This result is consistent with the findings of Takahashi et al. (Takahashi et al. 2016) and Arija et al. (Ariji et al. 1994). Maddux et al. (Maddux and Butaric 2017) suggested that the superior-inferior dimension of the zygomaticomaxillary interface influences sinus pneumatization. In contrast, Bornstein et al. (Bornstein et al. 2019), Luz et al. (Luz et al. 2018), and Anbiaee et al. (Anbiaee et al. 2018) found that male participants had significantly larger maxillary sinus volumes than females. Larger zygomaticomaxillary interfaces may allow for greater lateral expansion of the sinus, which could explain the increased sinus volume seen in males. Men generally have larger craniofacial dimensions, including broader zygomaticomaxillary interfaces, which may contribute to this anatomical difference.
Since neither age nor gender was significantly associated with ZPM morphology on panoramic images, it is suggested that a J-shaped ZPM may indicate greater sinus pneumatization, regardless of the patient’s demographic background. This finding reinforces the importance of radiographic morphology as a potentially reliable indicator of sinus pneumatization.
This study had several limitations. The sample may not fully represent diverse populations. Additionally, because women tend to visit dental and radiology clinics more frequently than men (Hamasha et al. 2018), a total population sampling method was employed, resulting in a sample in which approximately two-thirds of participants were female. Furthermore, edentulous patients were not analyzed separately. Edentulous individuals often exhibit increased maxillary sinus volume due to ongoing pneumatization, while dentate individuals typically do not show significant changes in sinus dimensions following tooth loss (Bornstein et al. 2019). However, the extent of pneumatization specifically within the ZPM in edentulous patients remains unclear. Future research with larger, more diverse samples and a specific focus on edentulous patients is therefore warranted.
Conclusion
Within the limitations of the present study, the following conclusions can be drawn:
The J-shaped morphology of the ZPM on panoramic radiographs was associated with greater ZPM volume, sinus volume, and degree of maxillary sinus pneumatization into the ZPM.
Male patients had a larger ZPM volume than female patients; however, sinus volume and the level of pneumatization were comparable between genders.
Age was not associated with ZPM volume, sinus volume, or the degree of maxillary sinus pneumatization into the ZPM.
Acknowledgements
The current study was extracted from a master thesis and authors wish to thank the research deputy of Mashhad University of Medical Sciences for providing support to do this work.
Author contributions
F.N. and N.A. made a substantial contribution to the concept and design of the study, supervised the study, methodology, and reviewing the final manuscript. E.L. and M.H. participated in collecting and analyzing data, interpretation of data and preparing the first draft of the manuscript. Finally, all authors have read and approved the final manuscript.
Funding
This study was funded by the Mashhad University of Medical Sciences, Mashhad, Iran (code: 4030262).
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. The protocol of this study was approved by the Ethics Committee of Mashhad University of Medical Sciences (code: IR.MUMS.DENTISTRY.REC.1403.105).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abdinian M, Faghihian R, Safi M (2017) Comparison of linear and angular measurement accuracy between cone beam computed tomography images and panoramic radiography. SRM J Res Dent Sci 8:14–20. 10.4103/srmjrds.srmjrds_26_16 [Google Scholar]
- Alqahtani S, Alsheraimi A, Alshareef A, Alsaban R, Alqahtani A, Almgran M, Eldesouky M, Al-Omar A (2020) Maxillary Sinus Pneumatization Following Extractions in Riyadh Saudi Arabia: A Cross-Sectional Study. Cureus 12:e6611. 10.7759/cureus.6611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anbiaee N, Bagherpour A, AhmadianYazdi A, Khodabakhsh R (2018) Relationship of Maxillary Sinus Volume and Pneumatization with Age and Gender. J Mashhad Dent School 42:200–194. 10.22038/jmds.2018.11455 [Google Scholar]
- Anbiaee N, Shafieian R, Shiezadeh F, Shakeri M, Naqipour F (2022) Correlation between gray values in cone-beam computed tomography and histomorphometric analysis. Imaging Sci Dent 52:375–382. 10.5624/isd.20220051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelieri F, Franchi L, Cevidanes LHS, Hino CT, Nguyen T, McNamara JA Jr (2017) Zygomaticomaxillary suture maturation: A predictor of maxillary protraction? Part I - A classification method. Orthod Craniofac Res 20:85–94. 10.1111/ocr.12143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelieri F, Ruellas AC, Yatabe MS, Cevidanes LHS, Franchi L, Toyama-Hino C, De Clerck HJ, Nguyen T, McNamara JA Jr (2017) Zygomaticomaxillary suture maturation: Part II-The influence of sutural maturation on the response to maxillary protraction. Orthod Craniofac Res 20:152–163. 10.1111/ocr.12191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arango E, Plaza-Ruíz SP, Barrero I, Villegas C (2022) Age differences in relation to bone thickness and length of the zygomatic process of the maxilla, infrazygomatic crest, and buccal shelf area. Am J Orthod Dentofac Orthop 161:510-518.e511. 10.1016/j.ajodo.2020.09.038 [DOI] [PubMed] [Google Scholar]
- Ariji Y, Kuroki T, Moriguchi S, Ariji E, Kanda S (1994) Age changes in the volume of the human maxillary sinus: a study using computed tomography. Dentomaxillofac Radiol 23:163–168. 10.1259/dmfr.23.3.7835518 [DOI] [PubMed] [Google Scholar]
- Bornstein MM, Ho JKC, Yeung AWK, Tanaka R, Li JQ, Jacobs R (2019) A Retrospective Evaluation of Factors Influencing the Volume of Healthy Maxillary Sinuses Based on CBCT Imaging. Int J Periodontics Restorative Dent 39:187–193. 10.11607/prd.3722 [DOI] [PubMed] [Google Scholar]
- Buller J, Bömelburg C, Kruse T, Zirk M (2023) Does maxillary sinus size affect the risk for zygomatic complex fractures? Clin Anat 36:564–569. 10.1002/ca.23986 [DOI] [PubMed] [Google Scholar]
- Cavalcanti MC, Guirado TE, Sapata VM, Costa C, Pannuti CM, Jung RE, César Neto JB (2018) Maxillary sinus floor pneumatization and alveolar ridge resorption after tooth loss: a cross-sectional study. Braz Oral Res 32:e64. 10.1590/1807-3107BOR-2018.vol32.0064 [DOI] [PubMed] [Google Scholar]
- Choi JW (2011) Assessment of panoramic radiography as a national oral examination tool: review of the literature. Imaging Sci Dent 41:1–6. 10.5624/isd.2011.41.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinç K, İçöz D (2024) Maxillary sinus volume changes in individuals with different craniofacial skeletal patterns: CBCT study. BMC Oral Health 24:1516. 10.1186/s12903-024-05341-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsayed SA, Alolayan AB, Alahmadi A, Kassim S (2019) Revisited maxillary sinus pneumatization narrative of observation in Al-Madinah Al-Munawwarah, Saudi Arabia: A retrospective cross-sectional study. Saudi Dent J 31:212–218. 10.1016/j.sdentj.2018.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsayed SA, Alassaf MS, Elboraey MO, Mohamado LL, Huwaykim DA, Albouq AK, Shahada MO (2023) The Impact of Maxillary Sinus Pneumatization on the Quality of the Alveolar Bone in Dentated and Edentulous Patients: A Cone-Beam Computed Tomography Radiographic Analysis. Cureus 15:e46005. 10.7759/cureus.46005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filho, H., W. Amaral, C. Curra, P. Santos and C. Cardoso (2016) Zygomatic implant: Late complications in a period of 12 years of experience. Rev Clin Periodoncia Implantol Rehabil Oral 10. 10.1016/j.piro.2016.03.007
- Fortin Y (2017) Placement of Zygomatic Implants into the Malar Prominence of the Maxillary Bone for Apical Fixation: A Clinical Report of 5 to 13 Years. Int J Oral Maxillofac Implants 32:633–641. 10.11607/jomi.5230 [DOI] [PubMed] [Google Scholar]
- Gellrich NC, Bormann KH, Tehranchian S, Kokemüller H, Suarez-Cunqueiro MM (2013) Containment and contouring (CoCoon) technique: a biologically adequate approach to less invasive autogenous preimplant augmentation of bone. Br J Oral Maxillofac Surg 51:880–886. 10.1016/j.bjoms.2012.11.001 [DOI] [PubMed] [Google Scholar]
- Gracco A, Tracey S, Baciliero U (2010) Miniscrew insertion and the maxillary sinus: an endoscopic evaluation. J Clin Orthod 44:439–443 [PubMed] [Google Scholar]
- Gulec M, Tassoker M, Magat G, Lale B, Ozcan S, Orhan K (2020) Three-dimensional volumetric analysis of the maxillary sinus: a cone-beam computed tomography study. Folia Morphol (Warsz) 79:557–562. 10.5603/FM.a2019.0106 [DOI] [PubMed] [Google Scholar]
- Hamasha AA, Alshehri A, Alshubaiki A, Alssafi F, Alamam H, Alshunaiber R (2018) Gender-specific oral health beliefs and behaviors among adult patients attending King Abdulaziz Medical City in Riyadh. Saudi Dent J 30:226–231. 10.1016/j.sdentj.2018.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Held U, Bormann KH, Schmelzeisen R, Gellrich NC (2005) Augmentation of alveolar ridge defects: autologous bone transplant from the zygomatic alveolar crest–a new technique. Schweiz Monatsschr Zahnmed 115:692–703 [PubMed] [Google Scholar]
- Ito K, Hirahara N, Muraoka H, Okada S, Kondo T, Andreu-Arasa VC, Sakai O, Kaneda T (2022) Normal Variants of the Oral and Maxillofacial Region: Mimics and Pitfalls. Radiographics 42:506–521. 10.1148/rg.210073 [DOI] [PubMed] [Google Scholar]
- Iwanaga J, Wilson C, Lachkar S, Tomaszewski KA, Walocha JA, Tubbs RS (2019) Clinical anatomy of the maxillary sinus: application to sinus floor augmentation. Anat Cell Biol 52:17–24. 10.5115/acb.2019.52.1.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson LA, Isaksson S, Lindh C, Becktor JP, Sennerby L (2010) Maxillary sinus floor augmentation and simultaneous implant placement using locally harvested autogenous bone chips and bone debris: a prospective clinical study. J Oral Maxillofac Surg 68:837–844. 10.1016/j.joms.2009.07.093 [DOI] [PubMed] [Google Scholar]
- Kainulainen VT, Sàndor GK, Oikarinen KS, Clokie CM (2002) Zygomatic bone: an additional donor site for alveolar bone reconstruction. Technical note. Int J Oral Maxillofac Implants 17:723–728 [PubMed] [Google Scholar]
- Karjodkar FR (2019) Essentials of Oral & Maxillofacial Radiology. Jaypee Brothers Medical Publishers Pvt, Limited [Google Scholar]
- Kopecka D, Simunek A, Streblov J, Slezak R, Capek L (2014) Measurement of the Interantral Bone in Implant Dentistry Using Panoramic Radiography and Cone Beam Computed Tomography: A Human Radiographic Study. West Indian Med J 63:503–509. 10.7727/wimj.2013.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luz J, Greutmann D, Wiedemeier D, Rostetter C, Rücker M, Stadlinger B (2018) 3D-evaluation of the maxillary sinus in cone-beam computed tomography. Int J Implant Dent 4:17. 10.1186/s40729-018-0128-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddux SD, Butaric LN (2017) Zygomaticomaxillary Morphology and Maxillary Sinus Form and Function: How Spatial Constraints Influence Pneumatization Patterns among Modern Humans. Anat Rec 300:209–225. 10.1002/ar.23447 [DOI] [PubMed] [Google Scholar]
- Mallya S, Lam E (2018) White and Pharoah's oral radiology: principles and interpretation, 8th edn. Elsevier Health Sciences, pp 485–6
- Marino MJ, Riley CA, Wu EL, Weinstein JE, Emerson N, McCoul ED (2020) Variability of Paranasal Sinus Pneumatization in the Absence of Sinus Disease. Ochsner J 20:170–175. 10.31486/toj.19.0053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohamed W, Abdalh A (2023) Comparison Of Different Imaging Software For Measuring Volume Of The Maxillary Sinus. Egypt Orthod J 63:35–44. 10.21608/eos.2023.182689.1063 [Google Scholar]
- Moro SA, Thomé G, Padovan LEM, da Silva RD, Tiossi R, Fontão FNGK (2021) A Zygomatic Bone Study Using Virtual Dental Implant Planning Software. J Oral Implantolog 48:171–176. 10.1563/aaid-joi-D-20-00149 [DOI] [PubMed] [Google Scholar]
- Nagare SP, Chaudhari RS, Birangane RS, Parkarwar PC (2018) Sex determination in forensic identification, a review. J Forensic Dent Sci 10:61–66. 10.4103/jfo.jfds_55_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ongole R, N PB (2021) Textbook of oral medicine, oral diagnosis and oral radiology e-book, 3rd edn. Elsevier Health Sciences, p 797
- Pellegrino G, Grande F, Ferri A, Pisi P, Gandolfi MG, Marchetti C (2020) Three-Dimensional Radiographic Evaluation of the Malar Bone Engagement Available for Ideal Zygomatic Implant Placement. Methods Protoc 3:52. 10.3390/mps3030052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perschbacher S (2012) Interpretation of panoramic radiographs. Australian Dent J 57:40–45. 10.1111/j.1834-7819.2011.01655.x [DOI] [PubMed] [Google Scholar]
- Präger TM, Brochhagen HG, Mischkowski R, Jost-Brinkmann PG, Müller-Hartwich R (2015) Bone condition of the maxillary zygomatic process prior to orthodontic anchorage plate fixation. J Orofac Orthop 76:3–13. 10.1007/s00056-014-0261-5 [DOI] [PubMed] [Google Scholar]
- Reham Ashraf H, Mushira MD, Reham Mohammed H (2017) Accuracy of planmeca promax 3D MID® cone beam computed tomography machinein volumetric measurements of maxillary sinus : : A diagnostic accuracy study. Reham Ashraf Hussien, Cairo [Google Scholar]
- Sahlstrand-Johnson P, Jannert M, Strömbeck A, Abul-Kasim K (2011) Computed tomography measurements of different dimensions of maxillary and frontal sinuses. BMC Med Imaging 11:8. 10.1186/1471-2342-11-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlager S, Rüdell A (2017) Sexual Dimorphism and Population Affinity in the Human Zygomatic Structure—Comparing Surface to Outline Data. Anat Rec 300:226–237. 10.1002/ar.23450 [DOI] [PubMed] [Google Scholar]
- Takahashi Y, Watanabe T, Iimura A, Takahashi O (2016) A Study of the Maxillary Sinus Volume in Elderly Persons Using Japanese Cadavers. Okajimas Folia Anat Jpn 93:21–27. 10.2535/ofaj.93.21 [DOI] [PubMed] [Google Scholar]
- Uchida Y, Goto M, Katsuki T, Akiyoshi T (2001) Measurement of the maxilla and zygoma as an aid in installing zygomatic implants. J Oral Maxillofac Surg 59:1193–1198. 10.1053/joms.2001.26725 [DOI] [PubMed] [Google Scholar]
- Wu X, Cai Q, Huang D, Xiong P, Shi L (2022) Cone-beam computed tomography-based analysis of maxillary sinus pneumatization extended into the alveolar process in different age groups. BMC Oral Health 22:393. 10.1186/s12903-022-02445-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Younes R, Husseini B, Younes JR, Ghosn N, Najjar J, Sayegh PEL, Fawaz P, and Bouserhal J (2025) Digital evaluation of the zygomatic buttress intra-oral donor site dimensions in different vertical facial growth types. J Stomatol Oral Maxillofac Surg 102268. 10.1016/j.jormas.2025.102268 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.