Abstract
This study aimed to collectively synthesize the available evidence on the effect of alveolar ridge preservation at the posterior maxilla in reducing maxillary sinus pneumatization after tooth extraction, and the necessity of sinus floor augmentation during implant placement. Database search, along with additional screening in the grey literature were conducted, to find clinical studies where ridge preservation was performed in the posterior maxilla, and was compared with normal healing. Eleven studies were included, with 185 and 203 sites for the test and control groups, respectively. Ridge preservation significantly decreased sinus pneumatization (SMD = − 0.88, 95% CI − 1.19 to − 0.58, p-value < 0.00001) and reduced the need for additional sinus floor augmentation when placing dental implants (OR = 0.18, 95% CI 0.09 to 0.36, p-value < 0.00001). Moreover, ridge height was significantly greater (SMD = 1.33, 95% CI 0.58 to 2.09, p-value = 0.0005), while ridge width did not show a statistical significance, compared to spontaneous healing (p-value = 0.053). Therefore, alveolar ridge preservation in the posterior maxilla decreases sinus pneumatization, as well as the need for sinus floor augmentation at the time of implant placement, along with its general benefits in preserving bone volume. Nevertheless, future comparisons are still needed, considering the small number of studies available.
Keywords: Alveolar bone grafting, Alveolar ridge augmentation, Bone substitutes, Dental implants, Tooth extraction
Subject terms: Dentistry, Periodontics, Dental implants
Introduction
The loss of alveolar bone structure following tooth extraction is an absolute outcome1–3. This phenomenon is more evident in the posterior region of the maxilla, which undergoes alveolar bone resorption that is further exacerbated by additional factors, namely the quality of bone and sinus pneumatization4,5. The latter has been related to certain considerations, such as genetics, the force of air pressure inside the sinus, and previous surgical procedures in the area. This generally leads to more bone resorption, compared with other regions of the jaw6,7.
Alveolar ridge preservation is a well-established procedure that has been proposed to limit the event of bone resorption following tooth extraction. Several reports have shown its benefit in reducing ridge resorption and maintaining acceptable bone volume8. Studies have indicated that no material or technique is superior to another and all methods lead to somewhat similar outcomes9–13.
With respect to the posterior area of the maxilla, various investigations have been performed to evaluate whether ridge preservation decreases sinus pneumatization and the need for additional sinus floor augmentation at the time of implant placement, compared to normal healing, in addition to its main advantage of preserving alveolar ridge dimensions4,7,14. However, these reports were based on a small number of cases, thus, not being able to present conclusive results, i.e., some studies demonstrated the efficacy of ridge preservation in reducing sinus pneumatization and further sinus procedures at the time of implant insertion15, while others did not show a significant benefit7. Additionally, previous systematic reviews focused on the posterior area overall (i.e., maxilla and mandible) to evaluate whether ridge preservation reduces the need for additional augmentation16,17. This does not provide sufficient insight, considering the major difference in the nature of this procedure between the two jaws (basic guided bone regeneration in the mandible versus sinus floor augmentation in the maxilla). Moreover, several recent reports concerning the maxillary posterior region have been published, which raises interest in further investigating this aspect7,14,15,18.
Therefore, the aim of this systematic review and meta-analysis was to collectively synthesize and evaluate the available evidence on the effect of ridge preservation in limiting the pneumatization of maxillary sinus after tooth extraction and the decreasing the necessity of further sinus floor augmentation during implant placement, in order to obtain more conclusive results, and provide considerations that support clinical practice.
Methods
This investigation was registered in the PROSPERO database (CRD42024590227) and performed following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement19.
In order to develop a robust search strategy and include suitable studies based on relevant criteria, the PICO protocol was implemented.
Population (P): patients with posterior maxillary teeth indicated for extraction.
Intervention (I): alveolar ridge preservation.
Comparator (C): normal/clot healing.
Outcome (O): primary outcomes: sinus pneumatization and the need for additional augmentation at the time of implant placement. secondary outcomes: alveolar ridge volumetric changes (height and width) at the final follow-up.
Therefore, the formulated search question was:
In patients having posterior maxillary teeth indicated for extraction (P), what is the clinical benefit of alveolar ridge preservation (I) in reducing maxillary sinus pneumatization, as well as the need for additional sinus floor augmentation at the time of implant placement (O), compared to spontaneous healing (C)?
Search strategy
Database search was carried out in MEDLINE/PubMed, Cochrane Central Register of Controlled Trials (CENTRAL), as well as Scopus. No restrictions, such as article language or the date of publication, were applied during the search process. A combination of MeSH terms and free keywords was used to find potential studies to be included. The set of keywords was (“ridge preservation” OR “socket preservation” OR “socket grafting”) AND (“maxilla” OR “maxillary” OR “molar”).
An additional search stage was done in the grey literature (Google Scholar), aiming to find more articles if available. The date of ending the overall literature search phase was May 20, 2025.
Study selection
Investigations selected for this systematic review and meta-analysis were (1) clinical studies (prospective and retrospective), where (2) alveolar ridge preservation was done in the posterior maxillary region, and (3) was compared to spontaneous healing, (4) focusing on the outcomes of sinus pneumatization, the need for additional sinus augmentation when placing implants, as well as the changes in alveolar ridge dimensions, (5) after a minimum of a 3-month follow-up period. Investigations that evaluated soft tissue changes only were excluded from this systematic review.
The literature search was performed independently by 2 reviewers (B.M, S.J). Disagreements concerning the inclusion of identified studies were overcome by discussion or seeking a third reviewer’s (A.P) opinion. To navigate and select suitable studies, Rayyan website (Rayyan, Qatar Computing Research Institute, Qatar Foundation) was utilized20. Screening through the references of the included studies was done also, attempting to find more potential studies to be added.
Data extraction
The data items compiled from the included studies were study design, sample size, extracted teeth, reasons for tooth extraction, baseline ridge dimensions (height and width), material used for ridge preservation, material for graft coverage (i.e., site closure), length of follow-up, and the outcomes of interest; sinus membrane pneumatization, need for additional sinus floor augmentation when placing dental implants, as well as ridge height and width changes compared to the baseline. Additional information related to the main outcomes were also extracted, represented by the method of measuring sinus pneumatization, and the minimum length of implants inserted in the grafted sites.
Risk of bias and quality assessment
The risk of bias in the randomized clinical trials (RCTs) was assessed with the revised Cochrane risk-of-bias tool for randomized trials (RoB 2)21. This tool includes five aspects or domains to evaluate, bias arising from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in measurement of the outcome, and bias in selection of the reported result. The level of bias for each study was determined based on the questions in the excel tool of RoB2.
Regarding the controlled clinical trials (CCTs), the Risk of Bias in Non-randomized Studies – of Interventions (ROBINS-I) tool was utilized22. This tool has 3 main aspects (pre-intervention, at intervention, post-intervention), divided into 7 domains to criticize. Each study was reported as having a low, moderate, or serious risk of bias.
The figure of the risk of bias in the included prospective clinical trials was created with the Risk of Bias Visualization Tool (robvis)23.
As for the retrospective studies, the Newcastle–Ottawa Scale (NOS) was implemented, which criticizes studies in relation to three aspects: selection of the sample, comparability of the groups, and assessment of the outcomes. A maximum of 9 points is given, based on certain considerations. Studies were judged to be of a good quality if they achieved a score of 7 or higher.
Data synthesis
Means and standard deviations (SD) of sinus pneumatization, as well as alveolar ridge width and height were collected from the included studies undergoing the meta-analysis. Ridge width at the closest point to the alveolar crest (1 mm below the crest, based on the included studies) was selected as the representative value of this outcome. For studies that did not report the height change in the center of the socket but presented the mean change in the buccal and palatal aspects, the combined mean and the pooled standard deviations were calculated using Cohen’s formula for the pooled standard deviation24, in order to obtain a similar format to the other investigations. Moreover, for trials that had two ridge preservation/control groups with a different sample size for each14,15, the data from the two relevant groups (i.e., means and SDs) were combined and used in the meta-analysis25. The number of cases needing additional sinus procedures at the time of implant placement was also extracted from the included studies to undergo meta-analysis.
Considering the different methods of measuring the continuous data, the related outcomes were analyzed using the standardized mean difference (SMD) with the 95% confidence interval (CI). As for the dichotomous data, they were pooled and presented as Odds ratio (OR) with the 95% CI. The extent of heterogeneity in the included studies under each of the outcomes was evaluated with the Chi2 test and I2 static, where I2 values of 25%, 50%, and 75% were considered to be low, moderate, and high heterogeneity, respectively26. When I2 values of 50% or higher were seen, the random-effect model was applied, in order to reduce the possible bias arising from methodological differences between the analyzed studies. If no evidence of significant heterogeneity was noted, the fixed-effects model was used.
To further validate the main results, subgroup analysis was performed, including prospective studies only. Since both randomized and non-randomized trials were included in this meta-analysis, an additional step was taken, where a design-adjusted approach was performed, in which the collective effect size from the non-randomized studies was first calculated, to decrease their magnitude on the main meta-analysis results. Then, these estimates of effect were pooled with the results of the randomized studies in additional meta-analyses3,27. Moreover, another subgroup analysis was conducted, including investigations where ridge preservation was performed using the same grafting material and membrane, in order to confirm the validity of the main analyses, based on the most homogenous trials.
Sensitivity analysis was also carried out, first by excluding each of the included studies under one meta-analysis at a time, and then by removing studies with potential risk of bias, aiming to evaluate the robustness of the meta-analysis, and investigate whether certain studies had a significant influence on the outcomes28,29.
P-values of < 0.05 represented a significant difference between the study and control groups. Forest plot for each meta-analysis was generated to illustrate the outcomes. All data were analyzed with the Review Manager software, version 5.4 (2020; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).
Certainty of evidence
The level of evidence was determined using the GRADE rating system30, which sets the quality of evidence from each of the meta-analysis outcomes as “high”, “moderate”, “low”, or “very low” based on several important aspects (risk of bias, imprecision, inconsistency, indirectness). The table of the certainty of evidence was generated using the GRADEpro website31.
Results
Literature screening outcomes
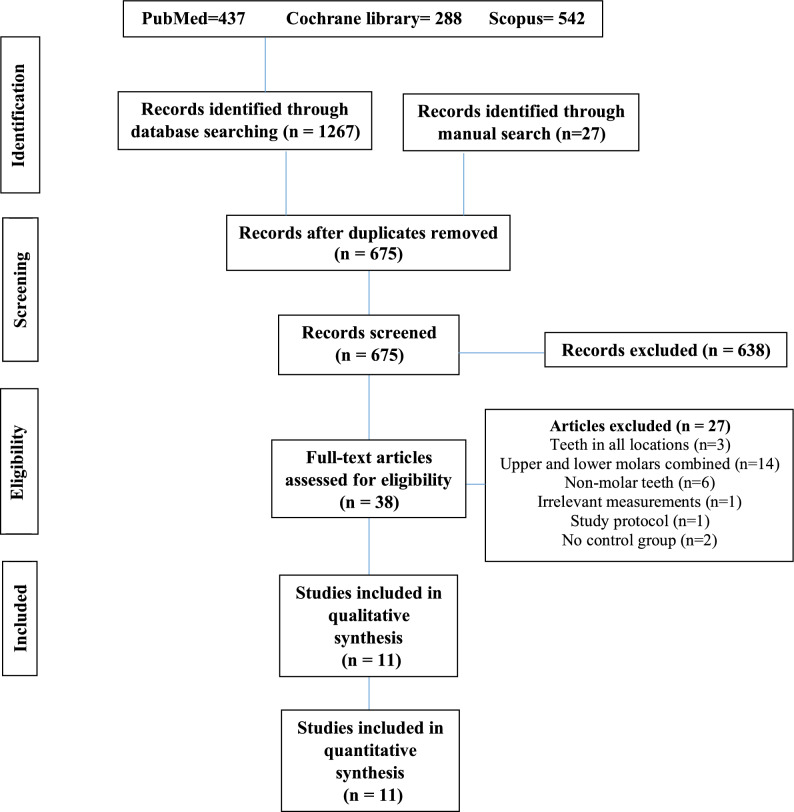
The number of articles identified from the databases and the manual search was 1294. Following the stage of removing the duplicates and screening the titles and abstracts for relevant papers, 38 studies reached the full-text assessment phase. This process led to the exclusion of 27 investigations. Consequently, 11 publications were included in this systematic review and meta-analysis (Fig. 1)4,7,9,14,15,18,32–36.
Fig. 1.
PRISMA flowchart of the search process.
Study characteristics
Table 1 presents the characteristics of the included studies.
Table 1.
Characteristics of the included studies.
| Study | Design | Sample | Tooth extracted | Reason for tooth extraction | Baselines ridge height (mm) | Baseline ridge width (mm) | Material for ridge preservation | Graft coverage | Follow-up |
|---|---|---|---|---|---|---|---|---|---|
| Dai 2025 | Retrospective case–control |
Test: 9 Control: 29 |
Molars | Periodontitis |
Test: 13.61 ± 2.9 Control: 14.54 ± 3.04 |
Test: 8.21 ± 2.04 Control: 7.40 ± 1.93 |
DBBM | Collagen membrane/Collagen sponge | 6–9 months |
| Khoury 2024 | CCT |
Test: 31 Control: 22 |
Premolars, molars | – |
Test: 11.78 ± 3.09 Control: 11.13 ± 2.12 |
– | DBBM | Collagen membrane | 6 months |
| Lam 2024 | RCT |
Test 1: 8 Test 2: 10 Control: 10 |
Second premolar, molars | Caries, endodontic failure, root/coronal fracture, periapical lesion/abscess |
Test 1: 5.9 ± 2.4 Test 2: 5.4 ± 2.2 Control: 6.8 ± 0.8 |
– |
Test 1: DBBM particles Test 2: DBBM blocks |
Collagen membrane | 4 months |
| Khaddour 2024 | Retrospective case–control |
Test: 17 Control: 22 |
Molars | Caries, endodontic failure, periodontitis, fatigue fracture |
Test: 13.61 ± 2.92 Control: 14.54 ± 3.04 |
Test: 8.21 ± 2.04 Control: 11.12 ± 1.46 |
A-PRF | Collagen sponge | 3 months |
| Wei 2022 | CCT |
Test: 18 Control: 18 |
Molars | Periodontitis |
Test: 4.09 ± 4.29 Control: 4.99 ± 4.53 |
Test: 5.60 ± 6.11 Control: 4.94 ± 5.22 |
DBBM | Collagen membrane + collagen sponge | 6 months |
| Shuman 2021 | RCT |
Test: 12 Control: 12 |
Molars | – |
Test: 9.36 ± 1.54 Control: 8.95 ± 1.51 |
– | DBBM | Platelet-rich fibrin | 6 months |
| Lee 2020 | RCT |
Test 1: 10 Test 2: 10 Control: 8 |
Molars | – | – | – |
Test 1: DBBM + EMD Test 2: DBBM |
Collagen membrane | 5 months |
| Cha 2019 | RCT |
Test: 20 Control: 19 |
Molars | Periodontitis, cracks, endodontic failure |
Test: 7.60 ± 0.42 Control: 2.84 ± 0.45 |
Test: 9.89 ± 0.98 Control: 7.81 ± 0.86 |
DBBM | Collagen membrane | 6 months |
| Lombardi 2018 | CCT |
Test: 13 Control: 13 |
First molars | – |
Test: 8.34 ± 3.25 Control: 6.40 ± 1.64 |
Test: 11.27 ± 1.71 Control: 12.06 ± 2.46 |
Synthetic nano-hydroxyapatite | Hemostatic sponge | 6 months |
| Levi 20,217 | Retrospective case–control |
Test: 21 Control: 42 |
Second premolar, molars | – |
Test: 8.79 ± 4.18 Control: 9.86 ± 4.73 |
– | DBBM | NR | 8 months |
| Rasperini 2010 | RCT |
Test: 6 Control: 8 |
Molars | Periodontitis |
Test: 19.3 ± 3.3 Control: 20.25 ± 5.96 |
– | DBBM | Collagen membrane | 6 months |
RCT: randomized clinical trial, CCT: controlled clinical trial, DBBM: deproteinized bovine bone mineral, A-PRF: advanced platelet-rich fibrin, EMD: enamel matrix derivatives.
The included investigations were published between 2010 and 2025. Five studies were randomized clinical trials (RCTs)4,14,15,18,32, three were controlled clinical trials (CCTs)7,9,33, and three were retrospective case–control studies34–36.
The total number of sites was 185 and 203 in the ridge-preservation and spontaneous-healing groups, respectively. The extracted teeth were molars in general in seven investigations4,15,18,32–35, first molars only in one15, while three studies included patients with premolars and molars to be extracted7,14,36. Six studies mentioned the reasons for tooth extraction. These encompassed periodontitis, endodontic failure, periapical lesions or abscess, as well as crown or root fracture4,14,15,33–35.
Baseline ridge heigh ranged between 4.09–19.3 mm in the ridge preservation groups, and 2.84–20.25 in the control groups. One study did not report baselines ridge height32. Regarding ridge width at the baseline, it was presented in four trials, being 5.60–11.27 mm in the test groups, and 4.94–12.06 mm in the control groups.
The material used for ridge preservation was deproteinized bovine bone mineral (DBBM) in seven of the included studies4,7,14,15,18,32,33. One of these had two tests groups, where enamel matrix derivative (EMD) was added to DBBM in one of the groups32. In one study, a synthetic nano-hydroxyapatite was used9.
The graft was covered with a collagen membrane in five studies4,7,14,15,32, a collagen membrane with a collagen sponge in one33, a hemostatic sponge in one9, and platelet-rich fibrin in one trial18.
The follow-up period was 3 months in one investigation32, 4 months in one14, five months in one32, 6 months in six4,9,15,18,33,35, and 8 months in one publicationl36. One study stated a range of 6–9 months of follow-up34.
Outcomes of the included studies
Ridge height was reported in ten out of the eleven included studies4,7,9,14,15,18,32,33,35,36. This ranged between a loss of 1.62 mm9 to a gain of 5.8 mm15 in the ridge preservation groups, while it was − 3.14 mm4 to + 5.64 mm15 in the control groups.
As for ridge width, this was − 5.27 mm4 to + 3.74 mm33 in the test groups, whereas a loss of 1.58–4.13 mm9,33 was noted in the normal-healing groups.
Regarding sinus pneumatization it was measured either from the alveolar crest area to the sinus floor4,9, the center of the socket to the sinus floor33, or from the sinus floor to its roof18,36. This recorded an increase of 0.14–0.88 mm when the sites underwent ridge preservation4,18. An increase of 0.59–2.02 mm was seen when areas left to heal spontaneously18,33. One study measured sinus volume, documenting a decrease of 0.7 cm3 in sites grafted with DBBM particles, an increase of 0.1 cm3 in sockets receiving DBBM blocks, and a pneumatization of 0.7 cm3 in the control group14.
When the alveolar ridge was preserved, 33 sites needed additional sinus procedures at the time of implant placement, which was less compared to the control groups, with 68 sites that underwent sinus floor augmentation when placing implants. The minimum length of the implants placed was mentioned in five investigations, being 6 mm in two7,14, and 8 mm in three trials4,32,33.
Table 2 summarizes the outcomes of the included studies.
Table 2.
Outcomes of the included studies.
| Study | Method of measuring sinus pneumatization | Sinus floor change / pneumatization | Ridge height change (mm) | Ridge width change (mm) | Minimum implant length (mm) | Need for sinus floor augmentation at implant placement |
|---|---|---|---|---|---|---|
| Dai 2025 | – | – | – | – | – |
Test: 4/9 Control: 23/29 |
| Khoury 2024 | – | – |
Test: 0.14 ± 2.94 Control: 0.17 ± 2.15 |
– | 6 |
Test: 4/31 Control: 7/22 |
| Lam 2024 | Define the volume of the sinus with a segmentation tool to be calculated by the software (CT) |
Sinus volume: Test 1 (3 sites): − 0.7 ± 0.8 cm3 Test 2 (5 sites): + 0.1 ± 0.3 cm3 Control (3 sites): + 0.7 ± 0.7 cm3 |
Test 1: + 0.9 ± 3.7 Test 2: + 1.0 ± 2.8 Control: − 2.7 ± 0.9 |
– | 6 |
Test 1: 3/7 Test 2: 4/10 Control: 8/9 |
| Khaddour 2024 | – | – |
Test: − 1.52 ± 0.76 Control: − 5.41 ± 1.93 |
Test: − 1.61 ± 0.96 Control: − 4.13 ± 1.16 |
– | – |
| Wei 2022 | Vertical distance of sinus floor level to the center of the socket (CBCT) |
Test: + 0.19 ± 0.45 mm Control: + 0.59 ± 0.63 mm |
Test: + 5.11 ± 4.36 Control: + 2.55 ± 3.77 |
Test: + 3.74 ± 4.17 Control: − 1.58 ± 4.61 |
8 |
Test: 3/18 Control: 9/18 |
| Shuman 2021 | Distance from sinus floor to sinus roof (CBCT) |
Test: + 0.88 ± 0.58 mm Control: + 2.02 ± 0.71 mm |
Test: 0.94 ± 0.41 Control: 1.79 ± 0.41 |
– | – | – |
| Lee 2020 | – | – |
Test 1: Buccal − 0.61 ± 0.40 palatal − 0.69 ± 0.62 Test 2: Buccal − 0.90 ± 0.65 palatal − 0.60 ± 0.37 Control: Buccal − 1.30 ± 1.12 palatal − 0.98 ± 0.66 |
Test 1: − 1.44 ± 0.54 Test 2: − 1.42 ± 0.26 Control: − 2.36 ± 1.03 |
8 |
Test 1: 3/9 Test 2: 3/8 Control: 4/5 |
| Cha 2019 | Distance between reference line* and sinus floor, at the center of the socket (CBCT) |
Test: + 0.14 ± 0.33 mm Control: + 1.16 ± 1.24 mm |
Test: + 0.16 ± 1.59 Control: − 3.14 ± 1.99 |
Test: − 5.27 ± 3.26 Control: − 3.53 ± 3.77 |
8 |
Test 8/14 Control 14/14 |
| Lombardi 2018 | Mean of 4 measurements: from sinus floor to the apices of the roots and to the center of the socket (CBCT) |
Test + 0.69 ± 0.48 mm Control + 1.04 ± 0.67 mm |
Test: − 1.62 ± 0.49 Control: − 2.01 ± 0.84 |
Test: − 2.73 ± 1.68 Control: − 3.63 ± 2.24 |
– |
Test 1/13 control: N/A |
| Levi 20,217 | Distance from sinus floor to sinus roof (panoramic) |
Test: + 0.30 ± 0.46 Control: + 1.30 ± 1.75 |
Test: − 0.32 ± 0.09 Control: − 1.26 ± 0.28 |
– | – | – |
| Rasperini 2010 | – | – |
Test: + 5.8 ± 2.4 Control: + 5.85 ± 3.57 |
– | NR** |
Test: 1/6 Control: 3/8 |
*Line of the crest levels of the adjacent neighboring teeth.
**No information on implant length. However, 8 mm of vertical residual bone was considered as the minimum to place an implant.
Risk of bias and quality assessment
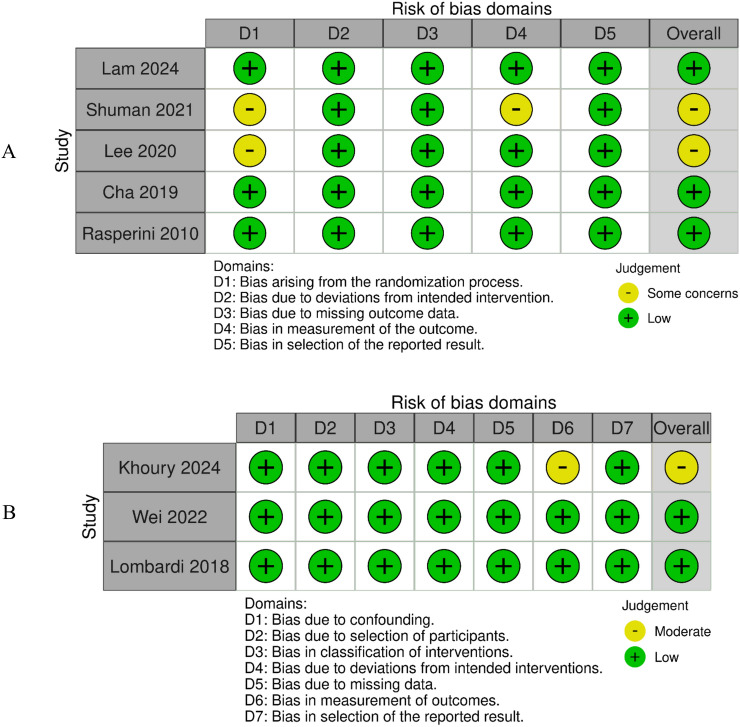
Three RCTs had a low risk of bias4,14,15, while two were assessed as having some concerns18,32, due to the unclear randomization process (Fig. 2A).
Fig. 2.
Risk of bias in each domain of the included randomized clinical trials (A), and controlled clinical trials (B).
As for the non-randomized studies, two showed low risk9,33, whereas one investigation had a moderate risk of bias7. The main reason was the insufficient information on measuring and reporting the outcomes (Fig. 2B).
Regarding the retrospective studies, two obtained 8/9 points35,36, whereas one gained 9 points34. Therefore, the included publications demonstrated good overall quality (Supplementary File 1).
Data synthesis
Need for additional sinus floor augmentation at implant placement
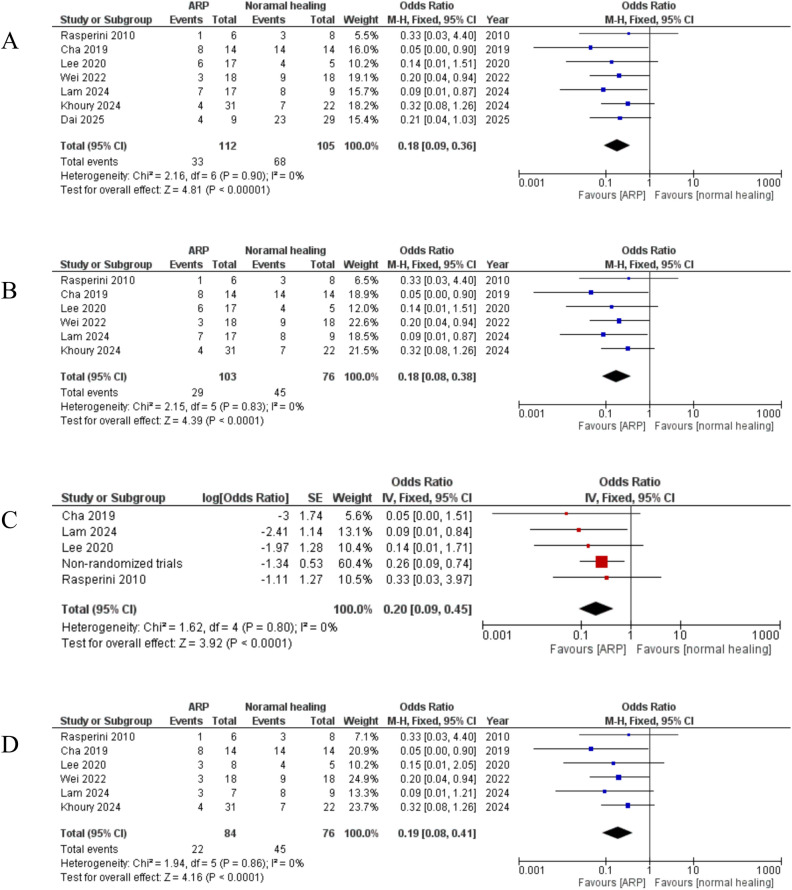
Seven articles were included4,7,14,15,32,33,36, with no heterogeneity among them (I2 = 0%); therefore, the fixed-effect model was utilized. These trials had a total of 112 sites in the ridge preservation groups, and 105 in the normal-healing groups. The results of the meta-analysis revealed that significantly fewer sites needed additional sinus floor augmentation at the time of implant placement when the alveolar ridge was preserved (OR = 0.18, 95% CI 0.09 to 0.36, p-value < 0.00001) (Fig. 3A).
Fig. 3.
Forest plot of the results of the meta-analysis of the need for additional sinus augmentation. (A) Including all studies, (B) analysis of prospective studies, (C) adjusting for non-randomized trials, (D) analysis of studies with the same material and membrane used for the procedure.
The same was noted when analyzing prospective clinical trials only, adjusting for non-randomized studies, and for the meta-analysis of studies with the same graft material and membrane (DBBM + collagen membrane) (Fig. 3B–D).
Sensitivity analysis by excluding each study at a time, and studies with potential bias7,32 led to the same outcome (highest p-value = 0.001, and p-value = 0.0002, respectively).
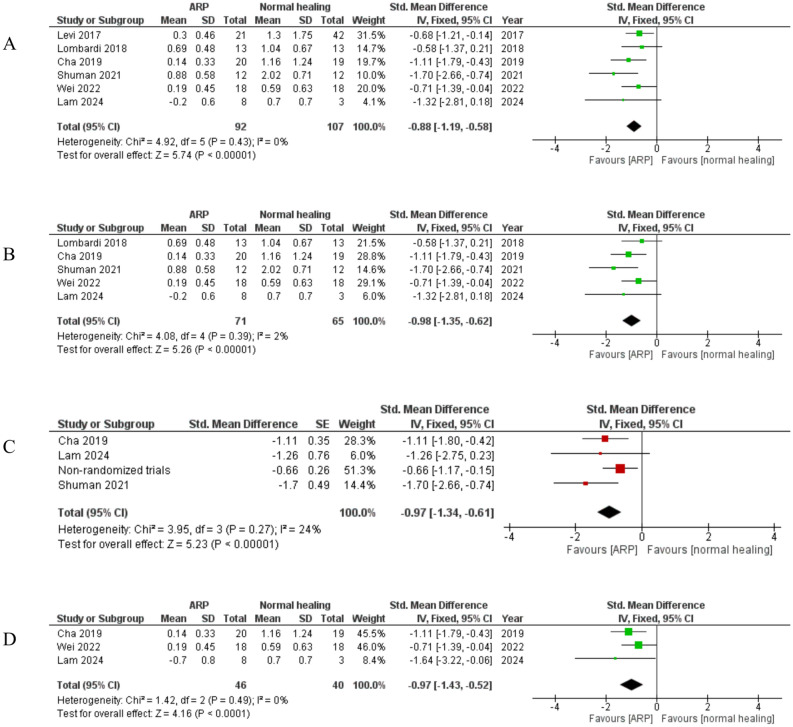
Sinus pneumatization
Six reports underwent the meta-analysis4,9,14,18,33,36. The total number of sites was 92 and 107 for the test and control groups, respectively. No heterogeneity was recorded (I2 = 0%). Meta-analysis of this outcome indicated less sinus pneumatization in the ridge preservation groups, with a notable statistical significance (SMD = − 0.88, 95% CI − 1.19 to − 0.58, p-value < 0.00001) (Fig. 4A).
Fig. 4.
Forest plot of the results of the meta-analysis of sinus pneumatization. (A) including all studies, (B) analysis of prospective studies, (C) adjusting for non-randomized trials, (D) analysis of studies with the same material and membrane used for the procedure.
A similar outcome was seen when including only prospective studies, adjusting for non-randomized trials, and analyzing studies with the same materials. (Fig. 4B–D).
Likewise, when conducting sensitivity analysis by excluding each trial at a time, as well as the investigation with possible bias18, the statistical significance remained (p-value < 0.0001 in both cases).
Ridge height
Ten studies were included in this meta-analysis4,7,9,14,15,18,32,33,35,36, having 172 and 167 sites for the ridge preservation and normal healing groups, respectively. A high level of heterogeneity was noted (I2 = 88%), thus the random-effect model was used. This meta-analysis showed significantly higher alveolar ridge height in the ridge preservation group (SMD = 1.33, 95% CI 0.58 to 2.09, p-value = 0.0005) (Fig. 5A).
Fig. 5.
Forest plot to demonstrate the results of the meta-analysis of ridge height. (A) including all studies, (B) analysis of prospective studies, (C) adjusting for non-randomized trials, (D) analysis of studies with the same material and membrane used for the procedure.
Subgroup analyses of prospective clinical trials only, adjusting for non-randomized studies, and of investigations using DBBM and collagen membrane resulted in a similar outcome (Fig. 5B–D).
The same results were recorded when removing each of the analyzed studies at a time (highest p-value = 0.006), and when excluding studies with a risk of bias7,18,32 from the meta-analysis (p-value = 0.003).
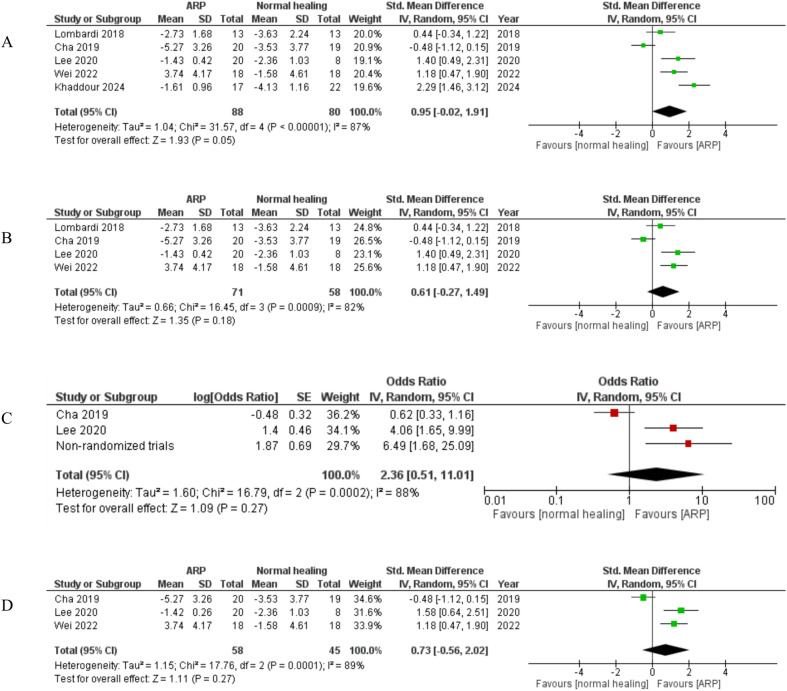
Ridge width
Five investigations were analyzed4,9,32,33,35, with 88 preserved sites and 80 sites left to heal spontaneously. High heterogeneity was seen (I2 = 87%). The outcome of this meta-analysis showed no significant difference between the groups (SMD = 0.95, 95% CI − 0.02 to 1.91, p-value = 0.053) (Fig. 6A).
Fig. 6.
Forest plot to demonstrate results of the meta-analysis of ridge width. (A) including all studies, (B) analysis of prospective studies, (C) adjusting for non-randomized trials, (D) analysis of studies with the same material and membrane used for the procedure.
The same result was noted when analyzing prospective studies only, and adjusting for non-randomized trials, as well as in the analysis of studies using DBBM and collagen membrane (Fig. 6B–D).
The absence of significant difference remained when excluding the study with potential bias32 (p-value = 0.47). In contrast, when removing each investigation at a time, the meta-analysis showed statistical significance (p-value = 0.0005) after excluding the study of Cha4, favoring the ridge preservation group.
Certainty of evidence
The level of evidence related to the outcome of sinus pneumatization, need for additional sinus augmentation, and alveolar ridge height was judged to be high. As for the evidence on ridge width, it was downgraded to be moderate. This was due to the inconsistency of the results from the analyzed investigations (Table 3).
Table 3.
Level of evidence according to the GRADE rating system.
| Certainty assessment | Number of patients | Effect | Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | ridge preservation | normal healing | Relative (95% CI) | Absolute (95% CI) | ||
| Need for sinus floor augmentation at implant placement | ||||||||||||
| 6 |
4 RCTs 2 CCTs |
not serious | not serious | not serious | not serious | none | 27/107 (25.2%) | 45/76 (59.2%) | OR 0.20 (0.08 to 0.38) | 367 fewer per 1,000 (from 488 to 237 fewer) | ⨁⨁⨁⨁High | CRITICAL |
| Sinus pneumatization | ||||||||||||
| 5 |
3 RCTs 2 CCTs |
not serious | not serious | not serious | not serious | none | 71 | 65 | – | SMD − 1.01 SD lower (1.38 lower to 0.64 lower) | ⨁⨁⨁⨁High | CRITICAL |
| Ridge height | ||||||||||||
| 7 |
4 RCTs 3 CCTs |
not serious | not serious | not serious | not serious | none | 122 | 91 | – | SMD 0.72 SD higher (0.22 higher to 1.22 higher) | ⨁⨁⨁⨁High | CRITICAL |
| Ridge width | ||||||||||||
| 4 |
2 RCTs 2 CCTs |
not serious | seriousa | not serious | not serious | none | 71 | 58 | – | SMD 0.61 SD higher (0.27 lower to 1.49 higher) | ⨁⨁⨁◯Moderatea | IMPORTANT |
Note that the certainty of evidence was assessed based on the results of the meta-analyses of prospective studies only, to ensure more homogeneity.
CI: confidence interval; OR: odds ratio; SMD: standardized mean difference; RCT: randomized clinical trial; CCT: controlled clinical trial.
aContradicting outcomes from the included studies.
Discussion
This systematic review and meta-analysis was carried out with the objective of investigating whether ridge preservation at the posterior maxillary region would reduce sinus pneumatization during the months following tooth extraction, as well as the need for further sinus procedures at the time of implant placement, in addition to its general advantage of limiting ridge resorption. Previous preliminary reports on this topic indicated a potential benefit of alveolar ridge preservation4,14,15. Therefore, collectively synthesizing the available evidence to provide more robust and conclusive results would be of great value.
Ridge resorption following tooth loss manifests itself at the highest extent during the first 6 months3,10. This will be more prominent on the horizontal aspect, with a reduction of 29–63%, than in the vertical dimension, which undergoes a reduction of 11–22%. It is noteworthy that most of this decrease in alveolar bone structure occurs during the first 3 months after tooth extraction37. The outcomes of the current meta-analysis revealed that ridge preservation limited the vertical loss of alveolar bone in the posterior maxilla and was able to maintain acceptable volume at the time of the final follow-up. This was also in line with other studies on ridge preservation in the molar area overall38–40. Therefore, this procedure would be recommended following the removal of posterior maxillary teeth. On the other hand, ridge width change was not significantly different, compared to spontaneous healing. The reason could be the low number of articles analyzed under this outcome. It is also important to keep in mind that the evidence on this outcome was downgraded, due to the inconsistency of the results from the analyzed investigations. This outcome was also not in agreement with what is reported in another systematic review16, which could be due to the inclusion of studies on the mandible and maxilla in that investigation. Conversely, when conducting sensitivity analysis and excluding the study of Cha4, the meta-analysis showed significantly less width loss when performing alveolar ridge preservation. This may have occurred by chance, considering the small number of studies, as mentioned previously. Taking these points into consideration, future clinical trials are encouraged, in order to explore this aspect and evaluate the benefit of ridge preservation in reducing ridge width change following tooth extraction.
The posterior region of the upper jaw is susceptible to more vertical deficiency due to the pneumatization of the maxillary sinus, which is responsible for 46% of the variation in the height of the alveolar ridge after tooth extraction4,14. The reason behind this phenomenon is still unclear, but could be related to the bone-remodeling process that inclines to be more of a resorptive pattern. This takes place due to the absence of physiological masticatory forces transferred to the bone through the tooth when it is present9. Previous research showed that sinus pneumatization is significant when second molars, or two or more adjacent posterior teeth are extracted41. Maxillary sinus pneumatization and the resultant height deficiency hinder proper implant placement. The current meta-analysis demonstrated that ridge preservation significantly reduced maxillary sinus pneumatization when it was compared to normal healing. Therefore, it could be utilized as a means to limit this event, until the region is ready for further rehabilitation. While the exact mechanism by which alveolar ridge preservation limits sinus pneumatization is not fully understood, it is suggested that following the extraction of posterior maxillary teeth, the absence of functional forces leads to bone remodeling, characterized by ridge resorption42. This process, often referred to as “disuse atrophy”, aligns with Wolff’s law, where bone adapts and remodels, because of the lack of mechanical stress9,43. Consequently, the maxillary sinus may expand inferiorly. Moreover, a previous animal study noted that sinus pneumatization is an opportunistic process, taking place in areas where no structures inhibit this phenomenon. This indicates that maintaining alveolar bone structure by means of ridge preservation could physically impede sinus pneumatization44. Nonetheless, future studies are still needed to gain deeper insights into this aspect.
Despite sinus floor augmentation procedures being effective in increasing the alveolar bone level and facilitating implant placement in the posterior maxilla,45 this kind of surgery is always accompanied with potential complications, including sinus membrane perforation or postoperative infection7. Thus, reducing the need for sinus lift procedure, at least the lateral approach, would potentially decrease the overall complications following implant installation in the posterior maxilla, which may improve patients’ experience, as well as implant success and survival rates. As indicated by many of the included studies, and based on the outcomes of this meta-analysis, ridge preservation in the posterior maxilla decreased the need for additional sinus augmentation procedures at the time of implant placement. Consequently, implementing this step could help clinicians to simplify implant insertion and avoid complex procedures in a good portion of their cases. Nevertheless, it is noteworthy that the minimum length of implants placed in the augmented sites varied across the analyzed studies, with some placing longer implants (8 mm) than others (6 mm). In addition, several investigations did not report this aspect. Therefore, the results may have been different if shorter implants were considered in all investigations. As a result, the benefit of ridge preservation in eliminating the need for sinus floor augmentation, even when choosing short implants, should be further explored and confirmed in future studies.
Several materials and techniques have been proposed for alveolar ridge preservation. Although the current literature does not indicate the superiority of a certain graft or membrane13,46, DBBM with collagen membrane have been used more frequently than other materials, which was also evident in the current systematic review. Therefore, to further validate the outcomes of this investigation, additional meta-analyses of studies that used DBBM covered by a collagen membrane were performed, in order to provide conclusions based on more homogenous clinical trials. The results remained consistent across all aspects, thus supporting the main outcomes on the efficacy of alveolar ridge preservation in the posterior maxillary region.
The strength of this study comes from collectively pooling the data from all the available studies on this topic, demonstrating the agreement in their results, and thus providing more robust conclusions with a good level of evidence. However, certain limitations should be kept in mind. The overall number of studies is still relatively small. Moreover, although gathering data from several investigations was done for each analysis, the number of cases remained low. As a result, future studies with a large number of cases and updated analyses when more clinical trials are available are essential, in order to further explore and confirm the conclusions drawn from the current systematic review.
Conclusions
Within the limitations of this study, it is concluded that alveolar ridge preservation in the posterior maxilla significantly decreases sinus pneumatization, as well as the need for sinus floor augmentation at the time of implant placement, along with its general benefits in preserving bone volume.
Supplementary Information
Acknowledgements
This research project is supported by the Second Century Fund (C2F), Chulalongkorn University.
Author contributions
Conceptualization and Methodology: Basel Mahardawi and Nikos Mattheos; Formal analysis and investigation: Basel Mahardawi and Sirimanas Jiaranuchart; Writing—original draft preparation: Basel Mahardawi, Sirida Arunjaroensuk, and Nikos Mattheos; Writing—review and editing: Nikos Mattheos, Kanit Dhanesuan, and Atiphan Pimkhaokham; Supervision: Atiphan Pimkhaokham and Kanit Dhanesuan. All authors read and approved the final version of this submission.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-025-06261-w.
References
- 1.Mahardawi, B. et al. Using autogenous tooth graft for alveolar ridge preservation: A systematic review and meta-analysis. J. Prosthet. Dent.10.1016/j.prosdent.2025.04.002 (2025). [DOI] [PubMed] [Google Scholar]
- 2.Mahardawi, B. et al. Autogenous tooth bone graft material prepared chairside and its clinical applications: A systematic review. Int. J. Oral Maxillofac. Surg.52, 132–141. 10.1016/j.ijom.2022.04.018 (2023). [DOI] [PubMed] [Google Scholar]
- 3.Mahardawi, B., Kyaw, T. T., Mattheos, N. & Pimkhaokham, A. The clinical efficacy of autogenous dentin blocks prepared chairside for alveolar ridge augmentation: A systematic review and meta-analysis. Clin. Oral Implants Res.34, 1025–1037. 10.1111/clr.14131 (2023). [DOI] [PubMed] [Google Scholar]
- 4.Cha, J. K. et al. Alveolar ridge preservation in the posterior maxilla reduces vertical dimensional change: A randomized controlled clinical trial. Clin. Oral Implants Res.30, 515–523. 10.1111/clr.13436 (2019). [DOI] [PubMed] [Google Scholar]
- 5.Farina, R., Pramstraller, M., Franceschetti, G., Pramstraller, C. & Trombelli, L. Alveolar ridge dimensions in maxillary posterior sextants: A retrospective comparative study of dentate and edentulous sites using computerized tomography data. Clin. Oral Implants Res.22, 1138–1144. 10.1111/j.1600-0501.2010.02087.x (2011). [DOI] [PubMed] [Google Scholar]
- 6.Barone, A. et al. Xenograft versus extraction alone for ridge preservation after tooth removal: A clinical and histomorphometric study. J. Periodontol.79, 1370–1377. 10.1902/jop.2008.070628 (2008). [DOI] [PubMed] [Google Scholar]
- 7.Khoury, E. J., Sagheb, K., Al-Nawas, B., König, J. & Schiegnitz, E. Does alveolar ridge preservation reduce the need for sinus floor elevation: A comparative study to spontaneous healing. Clin. Implant Dent. Relat. Res.10.1111/cid.13391 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Avila-Ortiz, G., Chambrone, L. & Vignoletti, F. Effect of alveolar ridge preservation interventions following tooth extraction: A systematic review and meta-analysis. J. Clin. Periodontol.46(Suppl 21), 195–223. 10.1111/jcpe.13057 (2019). [DOI] [PubMed] [Google Scholar]
- 9.Lombardi, T. et al. Efficacy of alveolar ridge preservation after maxillary molar extraction in reducing crestal bone resorption and sinus pneumatization: A multicenter prospective case-control study. BioMed Res. Int.2018, 9352130. 10.1155/2018/9352130 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahardawi, B. et al. Radiographic changes after alveolar ridge preservation using autogenous raw tooth particles versus xenograft: A prospective controlled clinical trial. Clin Oral Implants Res10.1111/clr.14348 (2024). [DOI] [PubMed] [Google Scholar]
- 11.Nct. Ridge Preservation After Tooth Extraction Using Cortical Versus Cancellous Freeze Dried Bone Allograft. https://clinicaltrials.gov/show/NCT01588444 (2012). [DOI] [PubMed]
- 12.Santos, A. et al. Autogenous mineralized dentin versus xenograft granules in ridge preservation for delayed implantation in post-extraction sites: A randomized controlled clinical trial with an 18 months follow-up. Clin. Oral Implants Res.32, 905–915. 10.1111/clr.13765 (2021). [DOI] [PubMed] [Google Scholar]
- 13.MacBeth, N., Trullenque-Eriksson, A., Donos, N. & Mardas, N. Hard and soft tissue changes following alveolar ridge preservation: A systematic review. Clin. Oral Implants Res.28, 982–1004. 10.1111/clr.12911 (2017). [DOI] [PubMed] [Google Scholar]
- 14.Lam, L., Ivanovski, S. & Lee, R. S. B. Alveolar ridge preservation in posterior maxillary teeth for reduction in the potential need for sinus floor elevation procedures: A pilot study. Clin. Oral Implants Res.10.1111/clr.14344 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rasperini, G., Canullo, L., Dellavia, C., Pellegrini, G. & Simion, M. Socket grafting in the posterior maxilla reduces the need for sinus augmentation. Int. J. Periodont. Restor. Dent.30, 265–273 (2010). [PubMed] [Google Scholar]
- 16.Wei, Y. P. et al. Alveolar ridge preservation at molar extraction sites: A systematic review and meta-analysis. J. Evid. Based Dent. Pract.25, 102074. 10.1016/j.jebdp.2024.102074 (2025). [DOI] [PubMed] [Google Scholar]
- 17.Fok, M. R., Pelekos, G. & Jin, L. Efficacy of alveolar ridge preservation in periodontally compromised molar extraction sites: A systematic review and meta-analysis. J. Clin. Med.13, 1198. 10.3390/jcm13051198 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shuman, M. & Alfeky, A. The efficacy of ridge preservation on maxillary sinus pneomatization and alveolar bone resoorption after extraction of posterior maxillary teeth. Egypt. Dent. J.67, 1069–1076. 10.21608/edj.2020.46229.1292 (2021). [Google Scholar]
- 19.Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ339, b2700. 10.1136/bmj.b2700 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ouzzani, M., Hammady, H., Fedorowicz, Z. & Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev.10.1186/s13643-016-0384-4 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sterne, J. A. C. et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ366, l4898. 10.1136/bmj.l4898 (2019). [DOI] [PubMed] [Google Scholar]
- 22.Sterne, J. A. et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ355, i4919. 10.1136/bmj.i4919 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGuinness, L. A. & Higgins, J. P. T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods12, 55–61. 10.1002/jrsm.1411 (2021). [DOI] [PubMed] [Google Scholar]
- 24.Cohen, J. Statistical Power Analysis for the Behavioral Sciences 2nd ed. (Routledge Academic, 1988). 10.4324/9780203771587.
- 25.Higgins, J. et al. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration (2011).
- 26.Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. Bmj327, 557–560. 10.1136/bmj.327.7414.557 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahardawi, B. et al. The accuracy of dental implant placement with different methods of computer-assisted implant surgery: A network meta-analysis of clinical studies. Clin. Oral Implants Res.10.1111/clr.14357 (2024). [DOI] [PubMed] [Google Scholar]
- 28.Mahardawi, B. et al. Use of autogenous tooth bone graft in osseous defects after the surgical removal of mandibular third molars: A systematic review and meta-analysis of randomized controlled trials. Int. J. Oral Maxillofac. Surg.10.1016/j.ijom.2025.02.003 (2025). [DOI] [PubMed] [Google Scholar]
- 29.Mahardawi, B. et al. The lack of keratinized mucosa as a risk factor for peri-implantitis: A systematic review and meta-analysis. Sci. Rep.13, 3778. 10.1038/s41598-023-30890-8 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guyatt, G. H. et al. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ336, 924–926. 10.1136/bmj.39489.470347.AD (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.GRADEpro GDT: GRADEpro Guideline Development Tool. McMaster University and Evidence Prime, 2021. Available from gradepro.org.
- 32.Lee, J. H. & Jeong, S. N. Effect of enamel matrix derivative on alveolar ridge preservation in the posterior maxilla: A randomized controlled clinical trial. Clin. Implant Dent. Relat. Res.22, 622–630. 10.1111/cid.12940 (2020). [DOI] [PubMed] [Google Scholar]
- 33.Wei, Y., Xu, T., Zhao, L., Hu, W. & Chung, K. H. Ridge preservation in maxillary molar extraction sites with severe periodontitis: A prospective observational clinical trial. Clin. Oral Investig.26, 2391–2399. 10.1007/s00784-021-04204-z (2022). [DOI] [PubMed] [Google Scholar]
- 34.Dai, A. et al. Effect of alveolar ridge preservation at periodontally compromised molar extraction sockets: A retrospective cohort study. J. Periodontol.96, 9–20. 10.1002/jper.24-0064 (2025). [DOI] [PubMed] [Google Scholar]
- 35.Khaddour, A. S. et al. Healing of extraction sites after alveolar ridge preservation using advanced platelet-rich fibrin: A retrospective study. Bioengineering10.3390/bioengineering11060566 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Levi, I., Halperin-Sternfeld, M., Horwitz, J., Zigdon-Giladi, H. & Machtei, E. E. Dimensional changes of the maxillary sinus following tooth extraction in the posterior maxilla with and without socket preservation. Clin. Implant Dent. Relat. Res.19, 952–958. 10.1111/cid.12521 (2017). [DOI] [PubMed] [Google Scholar]
- 37.Tan, W. L., Wong, T. L., Wong, M. C. & Lang, N. P. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin. Oral Implants Res.23(Suppl 5), 1–21. 10.1111/j.1600-0501.2011.02375.x (2012). [DOI] [PubMed] [Google Scholar]
- 38.Zhang, H. et al. Assessment of soft and hard tissue changes following micro crestal flap-Alveolar ridge preservation and augmentation at molar extraction sites in patients with stage III/IV periodontitis: A randomized controlled trial. J. Clin. Periodontol.10.1111/jcpe.14045 (2024). [DOI] [PubMed] [Google Scholar]
- 39.Sbordone, C. et al. Evaluation of volumetric dimensional changes in posterior extraction sites with and without ARP using a novel imaging device. Clin. Implant Dent. Relat. Res.19, 1044–1053. 10.1111/cid.12537 (2017). [DOI] [PubMed] [Google Scholar]
- 40.Lim, H. C., Shin, H. S., Cho, I. W., Koo, K. T. & Park, J. C. Ridge preservation in molar extraction sites with an open-healing approach: A randomized controlled clinical trial. J. Clin. Periodontol.46, 1144–1154. 10.1111/jcpe.13184 (2019). [DOI] [PubMed] [Google Scholar]
- 41.Sharan, A. & Madjar, D. Maxillary sinus pneumatization following extractions: A radiographic study. Int. J. Oral Maxillofac. Implants23, 48–56 (2008). [PubMed] [Google Scholar]
- 42.Wehrbein, H. & Diedrich, P. Progressive pneumatization of the basal maxillary sinus after extraction and space closure. Fortschr Kieferorthop53, 77–83. 10.1007/bf02164641 (1992). [DOI] [PubMed] [Google Scholar]
- 43.Frost, H. M. Wolff’s Law and bone’s structural adaptations to mechanical usage: An overview for clinicians. Angle Orthod.64, 175–188. 10.1043/0003-3219(1994)064%3c0175:Wlabsa%3e2.0.Co;2 (1994). [DOI] [PubMed] [Google Scholar]
- 44.Smith, T. D., Rossie, J. B., Cooper, G. M., Mooney, M. P. & Siegel, M. I. Secondary pneumatization of the maxillary sinus in callitrichid primates: Insights from immunohistochemistry and bone cell distribution. Anat. Rec. A Discov. Mol. Cell Evol. Biol.285, 677–689. 10.1002/ar.a.20209 (2005). [DOI] [PubMed] [Google Scholar]
- 45.Al-Dajani, M. Recent trends in sinus lift surgery and their clinical implications. Clin. Implant Dent. Relat. Res.18, 204–212. 10.1111/cid.12275 (2016). [DOI] [PubMed] [Google Scholar]
- 46.Canullo, L. et al. Dimensional and histomorphometric evaluation of biomaterials used for alveolar ridge preservation: A systematic review and network meta-analysis. Clin. Oral Investig.26, 141–158. 10.1007/s00784-021-04248-1 (2022). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.