Abstract
Abstract
Background
The use of different electronic devices is increasing among students due to rapid advancements in digital technology. The prevalence of computer vision syndrome (CVS) has increased among school children after the COVID-19 pandemic. Different symptoms of CVS, such as eye strain, headache, blurred vision and visual discomfort, have become major public health problems. This study aimed to assess the prevalence of CVS, identify its risk factors, evaluate parental awareness and examine the impact of COVID-19 on screen time among primary school children in Dhaka, Bangladesh.
Methods
Primary data were collected from the parents of 500 primary school students aged 5–14 years using a convenience sampling method through face-to-face interviews. A structured questionnaire was administered to collect demographic information, screen usage patterns, ambient conditions and details regarding the children’s academic performance. The Computer Vision Syndrome Questionnaire scale was used to assess the prevalence and severity of CVS. Various statistical analyses were performed, including χ2 tests, Fisher’s exact tests and logistic regression, to identify significant predictors of CVS (p<0.05).
Results
Findings revealed that 16.4% of children were affected by CVS, with key risk factors including age, school year, maternal education and daily screen time. Children with CVS commonly reported headaches and itchy eyes, which negatively impacted their academic performance. Surprisingly, 67.4% of parents were unaware of CVS, and the odds of developing CVS were 3.74 times higher among children using electronic devices for more than 4 hours daily.
Conclusions
The study explored the low prevalence of CVS among primary school students in Dhaka, Bangladesh. Several symptoms, like headaches and eye discomfort, were identified that impaired their academic performance. Additionally, many parents were largely unaware of CVS. Therefore, it is necessary to take proper strategies to be aware of the consequences and lessen the prevalence of CVS to save our future generation.
Keywords: Child, Cross-Sectional Studies, Health, Internet, PUBLIC HEALTH
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The use of a semi-purposive convenience sampling method may limit the generalisability of the findings to a broader population.
This study relied on parental reporting for children’s screen time, as well as ocular and extraocular symptoms, which may introduce recall and reporting biases.
This study measured academic performance using only three subjects, limiting its representation of overall achievement.
Other factors that are not incorporated in this study may influence the computer vision syndrome among children.
Introduction
The use of different electronic devices is increasing among students due to rapid advancements in digital technology. With the rise in screen time, a growing number of students are experiencing a range of eye and vision-related problems collectively known as computer vision syndrome (CVS).1 CVS also refers to a set of eye and vision issues caused by prolonged use of digital devices such as computers, tablets and smartphones.2 As a result, concern over CVS, characterised by headaches, blurred vision and other visual discomforts from extended screen time, has escalated.3 Globally, approximately 60 million people are affected by CVS, with an additional 1 million new cases reported each year.4 A review of 103 cross-sectional studies with 66 577 participants found that the prevalence of CVS was 69.0%, with a higher incidence reported among women compared with men.5 In Ethiopia, 69.5% of computer users in Debre Tabor Town reported experiencing CVS, with common symptoms including blurred vision, eyestrain and eye irritation.6 In China, the shift to online learning during the pandemic resulted in a significant increase in screen time for students, with 74.32% of those studying online experiencing higher rates of CVS compared with 50.79% of students attending in-person classes.7
Moreover, in Saudi Arabia, a study found that 82.2% of university students reported neck or shoulder pain as the most common symptom of prolonged computer use. Additionally, 66.5% of respondents reported headaches, while 51.5% experienced varying degrees of dry eyes.3 In Sri Lanka, 67.4% of office workers reported experiencing CVS.8 A previous study indicated that 68.16% of university students in Bangladesh suffer from symptoms such as headaches, decreased vision and eye discomfort due to CVS.9 The COVID-19 pandemic has intensified these issues as educational institutions globally, especially in Bangladesh, shifted to online learning, significantly increasing students’ screen time and potentially exacerbating CVS symptoms.10 Although these studies focused on adults, they underscore the high prevalence of CVS among the younger population, highlighting the need for greater awareness, particularly among students. Furthermore, research indicates that preschoolers who use smartphones excessively often report various physical and mental health issues, including attention deficit and hyperactivity disorder, emotional instability, aggression, depression, lack of self-control, poor vision and hearing, obesity, body imbalance and underdeveloped cognitive abilities.11 To protect the well-being of our future generations, it is essential to implement measures that restrict children’s smartphone use.12
There are different causes of CVS, such as uncorrected refractive error, and they include common terms used to define this condition, for example, digital eye strain, visual fatigue and asthenopia. Researchers noted that decreases in blink rate and completeness, partial or uncorrected refractive error and/or underlying binocular vision abnormalities, along with the cognitive demands of the task and variations in position, size, brightness and glare in comparison to an equivalent non-digital task, are the main mechanisms linked to the exacerbation of ocular surface disease.13 It is important to note that teachers, alongside parents, play a crucial role in understanding the ocular symptoms associated with digital device use and their long-term impact on quality of life.
Primary school students, with their developing eyes, are a particularly vulnerable population as they are increasingly exposed to screen time due to online education and entertainment. Research indicates that prolonged screen exposure can lead to a range of eye problems, including CVS, which may have significant long-term consequences on health.14 The potential long-term impact of CVS on children’s vision health is a serious concern, as excessive screen time can lead to vision problems that negatively impact their academic performance and overall well-being.15 Studies revealed that children aged 9–10 years had an average of 4.0 hours of screen time daily.16 A study by the American Optometric Association found that almost 25% of children aged 6–18 years have experienced symptoms of CVS.2 Another study among school-aged children during the COVID-19 pandemic in the Jazan region of Saudi Arabia found that the prevalence of CVS was 35.4% among children aged 6–18 years.17 Researchers pointed out that during the COVID-19 era, students have faced several challenges,18 including high school students’ daily screen time increasing by 4 hours, with 70.1% experiencing CVS due to an average of 7 hours spent on online learning in Thailand.19 Researchers found that more than half of school children who engage in prolonged screen time report symptoms consistent with CVS, such as eye strain and headaches, in India.20 Children are in a critical phase of both physical and cognitive development, so understanding and addressing CVS at this stage is crucial for safeguarding their future well-being.21 The effects of screen time on children’s academic performance and overall health underscore the need for parental awareness and preventive strategies to mitigate these risks.22
A comprehensive strategy to mitigate CVS requires a multifaceted approach incorporating clinical, behavioural and ergonomic interventions grounded in current evidence. Although widely recommended, interventions such as the 20-20-20 rule and blue light-blocking lenses have shown limited or inconclusive effectiveness in recent randomised controlled trials. For instance, blue light-blocking lenses have not demonstrated significant advantages over standard lenses with anti-reflective coating in reducing eye strain, and evidence supporting the 20-20-20 rule remains weak.23 24 Given the multifactorial nature of CVS and the difficulty in directly linking symptoms to specific causes like blue light exposure, it is important to prioritise alternative, evidence-informed strategies. These include addressing underlying ocular conditions such as uncorrected refractive errors, accommodation anomalies, binocular vision issues and tear film dysfunction.25 Additionally, oral omega-3 fatty acid supplementation has shown potential, although low-certainty, benefits for alleviating dry eye symptoms associated with CVS.26 For children, parental involvement is also crucial. Encouraging screen breaks, promoting outdoor activities and ensuring ergonomic furniture are all vital in managing screen-related visual discomfort.
The post-pandemic era offers an opportunity to explore the long-term effects of increased screen time and develop strategies to address associated health concerns.27 Primary school students are experiencing greater screen time due to the widespread availability of digital devices and the shift to online education following COVID-19.28 While significant research has been conducted on CVS among adults and university students, studies focusing on primary school children remain limited, especially in non-Western countries.29 30 Understanding and addressing the effects of CVS is vital for the well-being and academic success of children in Bangladesh. However, there is a lack of literature on CVS among primary school children in this context. Therefore, this research aims to assess the prevalence and risk factors of CVS among primary school students in Dhaka, Bangladesh, in order to fill this gap. Additionally, it seeks to develop a predictive model for CVS that uses identified risk factors to estimate a student’s likelihood of developing the syndrome. This model could serve as a valuable tool for early intervention and preventive strategies. The study will also examine the impact of CVS on students’ academic performance. The findings will provide insights for creating strategies to improve visual health, reduce screen time and raise awareness among parents, educators and policymakers, ultimately enhancing the well-being of primary school students.
Methods and materials
Study design and setting
A cross-sectional study was conducted involving parents of primary-level students in northern Dhaka, Bangladesh. In the Bangladeshi education system, the primary level includes students in classes 1–5 (equivalent to grades 1–5), which typically corresponds to the ages of 5–10. The secondary and higher secondary levels encompass classes 6–12 (grades 6–12), usually associated with ages 11–17. Tertiary education consists of undergraduate and postgraduate studies (grades 13 and above), typically pursued by individuals aged 18 and older.19 31 This study specifically focused on children in grades 1–5, all of whom had access to at least one smartphone.
Sampling procedure
The participants in this study included parents of children enrolled in primary schools in Dhaka, selected through convenience sampling. Convenience sampling is a non-probability sampling method in which samples are chosen based on the researcher’s preferences. Researchers frequently employ a non-probability sampling strategy for data collection when obtaining a probability sample is either impractical or impossible, despite the fact that it may introduce biases since it does not provide all eligible students an equal chance to participate. The authors selected a convenient sample for three reasons: (1) no sample frame was available, (2) resources were few and (3) data collection time limits. The data collection team reached out to eight primary schools in the northern area of Dhaka and included parents who agreed to participate in the study. A formal letter outlining the study objectives was provided to the school authorities, seeking permission to conduct the survey. On approval, the authorities facilitated the recruitment of parents of children from classes 1–5 who were willing to participate in the study. A total of 516 responses were initially collected, but 16 responses with missing information, that is, incomplete cases, were excluded, resulting in a final sample of 500 participants. All incomplete/missing data were considered missing at random. Parents whose children had access to at least one smartphone were included in the study. This criterion was set to focus on the relationship between screen use via smart devices and the risk of CVS. Parents of children without access to any smart devices were excluded from the study to maintain a consistent sample group. To determine the optimum sample size, the authors assumed a prevalence of CVS is 50% due to the lack of prior studies among this age group in Bangladesh.22 This approach maximises the sample size for better precision. The final sample size was calculated as approximately 405, ensuring a 95% confidence level, 5% precision and accounting for a 5% non-response rate.
Data collection and study tools
Data were collected using a well-defined, structured questionnaire through face-to-face interviews with the parents of primary school students. The data enumerators explained the study objectives to the participants and obtained their oral consent to participate in the survey. They assured the participants that their personally identifiable information would remain confidential and would not be shared. Clear instructions were provided for completing the questionnaire. Initially developed in English, the questionnaire was later translated into the local language (Bengali) to enhance comprehension and gather accurate responses from the participants. Sociodemographic characteristics such as age, gender, school year, mother’s education, economic status, types of devices used, duration of use, device brightness, taking breaks while using devices, personal history and use of spectacles were assessed first. The questionnaire also contained questions regarding the environmental conditions of the students, such as room lighting, screen distance and screen level. By using the Computer Vision Syndrome Questionnaire (CVSQ), the frequency and intensity of 16 CVS symptoms were collected separately. The frequency scoring criteria employed were as follows: never (score=0), sometimes (score=1) (occurring once weekly, irregular episodes) and always (score=2) (occurring more than 2–3 times weekly). Intensity was classified as moderate (score=1) and intense (score=2).17 The CVSQ was calculated using the following formula
The frequency of each symptom score was multiplied by its intensity score, and the resulting value was adjusted according to the following criteria: 0 remains 0; scores of 1 or 2 are adjusted to 1; a score of 4 is adjusted to 2. The total score was calculated by aggregating the recorded results for each of the 16 symptoms. A score of 6 or above was categorised as a CVS case.32 In addition to the CVSQ, the authors evaluate parental knowledge of CVS to understand and awareness of parents regarding their children’s health. This was done using a series of statements concerning CVS symptoms and preventive measures, with responses classified as ‘True’, ‘False’ or ‘Don’t know’.33 There is no dedicated CVSQ for the children; however, the authors are motivated to use it for children from the previous studies.17 19 Additionally, parents were requested to report their children’s average screen time during COVID-19, along with their academic scores in mathematics, science and English from the latest annual or semi-annual examination. These three subjects were chosen because they are frequently used as key indicators of academic performance in various international research studies.34 35 The student’s academic scores were documented on a scale of 100 points. A trained team consisting of 15 graduate students from the science faculty conducted the data-gathering procedure from 21 November 2024 to 4 December 2024 under the authors’ supervision. All authors, except for the corresponding author, along with six trained graduate students from the science faculty, actively participated in the data collection process. Each face-to-face interview lasted 18–25 min, allowing for a brief 2–3 min break if needed. Children were present during the interview sessions to assist with symptom recall when necessary.
Patient and public involvement
It was not appropriate or possible to involve patients or the public in the design, conduct, reporting or dissemination plans of our research.
Statistical analysis
Data cleaning and cross-checking were performed using Microsoft Excel, and the dataset was subsequently imported into RStudio V.4.4.1 for a comprehensive statistical analysis. The χ2 and Fisher’s exact tests were employed to evaluate the significance of the association among the specified variables. Different summary statistics and visualisations were used to present the findings.36 The CVS status was treated as a categorical variable. The normality assumptions were assessed using Q-Q plots and the Anderson-Darling test.36 Consequently, the Wilcoxon signed-rank test was used to evaluate the alterations in screen time from the COVID-19 era to the post-COVID period. The analysis employed multivariable logistic regression to evaluate the risk factors of CVS among the participants. In the logistic regression analysis, variables were considered statistically significant if their p values were less than 0.05.
Results
The reliability of the CVSQ scale was confirmed by a Cronbach’s alpha value of 0.82, indicating a good level of internal consistency for the indicators of CVS. The Q-Q plots presented in online supplemental figure 1 and the Anderson-Darling test (A=28.913, p<0.001) indicated a violation of the normality assumption. The overall prevalence of CVS among the 500 surveyed primary school students was 16.4%. The prevalence of CVS by different characteristics is presented in table 1.
Table 1. Prevalence of computer vision syndrome (CVS) by demographic characteristics (n=500).
| Variables | Labels | n (%) | CVS status, n (%) | P value of χ2 and Fisher’s exact test | |
|---|---|---|---|---|---|
| Present, n (%) | Absent, n (%) | ||||
| Age (years) | 5–7 | 84 (16.8) | 2 (2.4) | 82 (97.6) | <0.001 |
| 8–11 | 350 (70.0) | 66 (18.9) | 284 (81.1) | ||
| 12–14 | 66 (13.2) | 14 (21.2) | 52 (78.8) | ||
| Gender | Female | 283 (56.6) | 42 (14.8) | 241 (85.2) | 0.340 |
| Male | 217 (43.4) | 40 (18.4) | 177 (81.6) | ||
| School year | Grade 1 | 91 (18.2) | 2 (2.2) | 89 (97.8) | <0.001 |
| Grade 2 | 50 (10.0) | 6 (12.0) | 44 (88.0) | ||
| Grade 3 | 69 (13.8) | 14 (20.3) | 55 (79.7) | ||
| Grade 4 | 135 (27.0) | 33 (24.4) | 102 (75.6) | ||
| Grade 5 | 155 (31.0) | 27 (17.4) | 128 (82.6) | ||
| Mothers’ education | Uneducated | 9 (1.8) | 3 (33.3) | 6 (66.7) | 0.015* |
| Primary | 61 (12.2) | 10 (16.4) | 51 (83.6) | ||
| Secondary | 66 (13.2) | 13 (19.7) | 53 (80.3) | ||
| Higher secondary | 95 (19.0) | 6 (6.3) | 89 (93.7) | ||
| Graduate | 269 (53.8) | 50 (15.6) | 219 (81.4) | ||
| Economic status (Taka) | <10 000 | 18 (3.6) | 6 (33.3) | 12 (66.7) | 0.010* |
| 10 000–30 000 | 133 (26.6) | 22 (16.5) | 111 (83.5) | ||
| 30 000–40 000 | 97 (19.4) | 10 (10.3) | 87 (89.7) | ||
| 40 000–50 000 | 80 (16.4) | 7 (8.8) | 73 (91.2) | ||
| 50000 or more | 172 (34.4) | 37 (21.5) | 135 (78.5) | ||
| Types of device use | Mobile/tab | 125 (25.0) | 23 (18.4) | 102 (81.6) | 0.078* |
| Television | 44 (8.8) | 4 (9.1) | 40 (90.9) | ||
| Computer (laptop and desktop) | 4 (0.8) | 2 (50.0) | 2 (50.0) | ||
| Mobile and television | 235 (47.0) | 32 (13.6) | 203 (86.4) | ||
| Mobile and computer | 18 (3.6) | 4 (22.2) | 14 (77.8) | ||
| All three devices | 74 (14.8) | 17 (23.0) | 57 (77.0) | ||
| Duration of use (hours) | <1 | 177 (23.4) | 17 (14.5) | 100 (85.5) | <0.001 |
| 1–2 | 189 (37.8) | 25 (13.2) | 164 (86.8) | ||
| 2–3 | 114 (22.8) | 13 (11.4) | 101 (88.6) | ||
| 3–4 | 44 (8.8) | 13 (29.5) | 31 (70.5) | ||
| 4 or more | 36 (7.2) | 14 (38.9) | 22 (61.1) | ||
| Brightness of device | Low | 47 (9.4) | 6 (12.8) | 41 (87.2) | 0.778 |
| Medium | 400 (80.0) | 67 (16.8) | 333 (83.2) | ||
| High | 53 (10.6) | 9 (17.0) | 44 (83.0) | ||
| Taking breaks while using | No break | 59 (11.8) | 11 (18.6) | 48 (81.4) | 0.488 |
| Every 30 min | 121 (24.2) | 23 (19.0) | 98 (81.0) | ||
| Every 1 hour | 95 (19.0) | 11 (11.6) | 84 (88.4) | ||
| More than 1 hour | 225 (45.0) | 37 (83.4) | 188 (16.4) | ||
| Personal history | No disease history | 275 (55.0) | 16 (5.8) | 259 (94.2) | <0.001 |
| Only eye problem | 74 (14.8) | 21 (28.4) | 53 (71.6) | ||
| Only headache | 98 (19.6) | 22 (22.4) | 76 (77.6) | ||
| Both headache and eye problems | 53 (10.6) | 23 (43.4) | 30 (56.6) | ||
| Use of spectacles | Yes | 99 (19.8) | 30 (30.3) | 349 (69.7) | <0.001 |
| No | 401 (80.2) | 52 (13.0) | 69 (87.0) | ||
P value obtained by performing Fisher’s exact test.
Significant heterogeneity in CVS prevalence was observed among different age groups (p<0.001). The highest prevalence of CVS (21.2%) was observed among students aged 12–14 years, followed by the 8–11 years group (18.9%). In contrast, the youngest students, aged 5–7 years, had the lowest prevalence of CVS (2.4%). Moreover, a significant relationship was found between class level and CVS occurrence (p<0.001). Students who were in grade 4 exhibited the highest prevalence (24.4%) of CVS, followed by class 3 (20.3%) and class 5 (17.4%). Students in grade 1 had the lowest prevalence of CVS (2.2%). Another significant association was noted with the mothers’ educational level. The prevalence of CVS was 16.4% and 19.7% among children whose mothers’ educational qualification was primary and secondary, respectively. Students from graduate degree-holding mothers were likewise linked to relatively low CVS prevalence. Students from families earning less than 10 000 Taka (Bangladeshi currency) per month had the highest prevalence of CVS at 33.3%. In contrast, the prevalence rate for students from families with monthly incomes exceeding 50 000 Taka was 21.5%. Additionally, a significant correlation was found between the duration of device usage and the occurrence of CVS (p<0.001). The highest prevalence of CVS, at 38.9%, was observed among students who used screens for more than 4 hours a day, followed by those who used screens for three to 4 hours. The lowest prevalence, at 14.5%, was recorded among students who used screens for less than 1 hour daily. Furthermore, participants’ personal medical histories were significantly associated with CVS. Children who reported experiencing both headaches and eye problems had the highest prevalence of CVS at 43.4%, whereas those with no prior medical conditions showed the lowest prevalence at 5.8% (table 1).
Table 2 delineated the ambient conditions for CVS participants, including room lighting, screen distance and screen level, categorised by gender characteristics. More than half of the students (52.4%) who exhibited CVS symptoms reported the presence of overhead ceiling lights in their rooms. The analysis considered the screen distance used by students, with 47.6% of those in the CVS group observing the screen at a distance shorter than arm’s length, which may have exacerbated their symptoms. The findings presented in table 2 also revealed no statistically significant difference between the presence and absence of CVS under different environmental conditions considered in this study. It is also observed that the screen distance is not statistically different between those with CVS and those without.
Table 2. Environmental conditions of the students (n=500).
| Variable | Labels | n (%) | CVS status, n (%) | P value of χ2 and Fisher’s exact test | |
|---|---|---|---|---|---|
| Present, n (%) | Absent, n (%) | ||||
| Room lighting | Darkroom | 21 (4.2) | 3 (14.3) | 18 (85.7) | 0.560* |
| Using overhead lighting from the ceiling | 241 (48.2) | 43 (17.8) | 198 (82.2) | ||
| Using a desk or light, hitting directly on the eyes | 10 (2.0) | 3 (30.0) | 7 (70.0) | ||
| Using other sources of light | 6 (1.2) | 1 (16.7) | 5 (83.3) | ||
| Using window light | 222 (44.4) | 32 (14.4) | 190 (85.6) | ||
| Screen distance | Less than arm and forearm length | 246 (49.2) | 39 (15.9) | 207 (84.1) | 0.838 |
| More than arm or forearm length | 254 (18.4) | 43 (16.9) | 211 (83.1) | ||
| Screen level | Above the level of the eyes | 92 (18.4) | 17 (18.5) | 75 (81.5) | 0.348 |
| Below the level of the eyes | 134 (26.8) | 26 (19.4) | 108 (80.6) | ||
| The same level of the eyes | 274 (54.8) | 39 (14.2) | 235 (85.8) | ||
P value obtained by performing Fisher’s exact test.
CVS, computer vision syndrome.
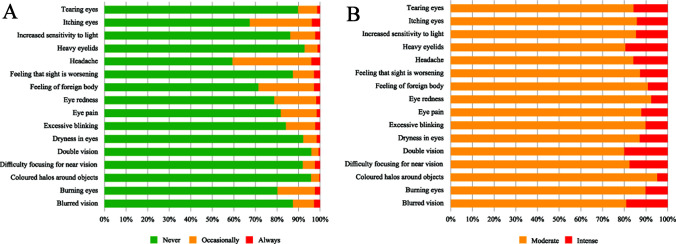
Figure 1A illustrates the frequency of ocular and extraocular symptoms among 500 children. Findings revealed that among 16 categories of CVS symptoms, three symptoms were markedly more prevalent: eye itching, headaches and the sensation of a foreign body in the eye. The stacked bar showed that over 40% of students experienced headaches, more than 30% reported itchy eyes and over 20% felt the presence of a foreign body. Figure 1B displays the intensity of each symptom, indicating that, among all reported symptoms, double vision and heavy eyelids had the highest intensity.
Figure 1. (A) The frequency and (B) the intensity of ocular and extraocular symptoms among the children (n=500).
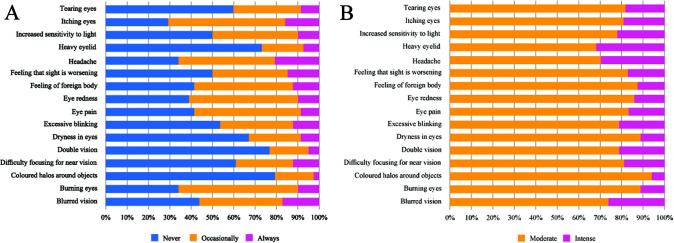
Figure 2A depicts the prevalence of ocular and extraocular symptoms among 82 children who suffer from CVS. Findings show that eye itchiness, headaches and burning eyes were the predominant symptoms among children having CVS. The stacked bar revealed that more than 70% of participants experienced itchy eyes, while more than 60% reported headaches and burning eyes. Figure 2B illustrates the severity of each symptom, and it is observed that heavy eyelids and headaches had the greatest intensity among all reported symptoms.
Figure 2. (A) The frequency and (B) the intensity of ocular and extraocular symptoms among the participants having computer vision syndrome (n=82).
A comparison of children’s academic achievement based on the presence or absence of CVS is presented in table 3. The findings indicated that students with CVS had lower mean scores in all three subjects compared with those without CVS. In mathematics, students with CVS achieved a mean score of 74.76, whereas their counterparts without CVS attained a mean score of 81.30. In science, the average score for individuals with CVS was 73.62, while those without CVS had an average score of 81.51. In English, the results were similarly varied: students with CVS averaged 70.98, while those without CVS achieved an average of 80.67. To determine whether these differences were statistically significant, a Mann-Whitney U test was conducted for each subject. The results revealed a significant difference in mathematics scores (p=0.002), science scores (p<0.001) and English scores (p<0.001) between students with and without CVS. These findings suggest that the presence of CVS is associated with significantly lower academic performance across all three subjects.
Table 3. Academic performance of students according to CVS status and subjects (n=500).
| Subjects | CVS status | Mean score with SD |
|---|---|---|
| Mathematics | Yes | 74.76±19.37 |
| No | 81.30±16.69 | |
| Science | Yes | 73.62±19.04 |
| No | 81.51±16.31 | |
| English | Yes | 70.98±20.41 |
| No | 80.67±16.37 |
CVS, computer vision syndrome.
Figure 3 shows that students spent significantly less screen time during the COVID-19 pandemic compared with the post-pandemic period. The pandemic resulted in a notable increase in screen time on electronic devices. During the COVID-19 pandemic, a higher percentage of students (63.2%) reported using screens for less than an hour each day. However, this percentage fell to 23.4% in the post-COVID era. The number of students who spent 1–2 hours on screens daily increased from 21.6% to 37.8%. Similarly, the proportion of students using screens for 2–3 hours per day rose from 9.2% to 22.8%. Furthermore, the percentage of students spending more than 4 hours a day on screens more than doubled, increasing from 2.6% to 7.2% (figure 3). The Wilcoxon signed-rank test also indicated a statistically significant increase in screen time after COVID-19 compared with the pandemic period (p<0.001).
Figure 3. Change in screen time from the COVID-19 era to the post-COVID era.
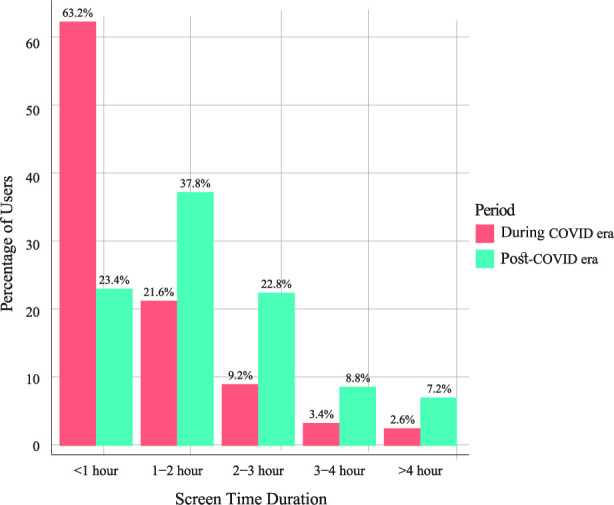
Table 4 displays the percentage distribution of parental awareness of CVS based on a sample of 500 respondents. Our research revealed that only 18.8% of parents were aware of CVS, while 67.4% reported ignorance of its meaning. Similarly, just 16.4% of parents were aware of the causes of CVS, while 69.4% were unaware. Furthermore, only 11.0% of parents knew how to prevent CVS, with the majority lacking knowledge of the prevention protocols. Findings also suggest that there is no significant association between awareness and the presence of CVS.
Table 4. Awareness and knowledge of CVS among parents (n=500).
| Variables | Labels | n (%) | CVS status, n (%) | P value of χ2 | |
|---|---|---|---|---|---|
| Present, n (%) | Absent, n (%) | ||||
| I know about computer vision syndrome | True | 94 (18.8) | 16 (17.0) | 78 (83.0) | 0.317 |
| False | 69 (13.8) | 7 (10.1) | 62 (89.9) | ||
| Don’t know | 337 (67.4) | 59 (17.5) | 278 (17.0) | ||
| I know about the causes of computer vision syndrome | True | 82 (16.4) | 15 (18.3) | 67 (81.7) | 0.871 |
| False | 71 (14.2) | 11 (15.5) | 60 (84.5) | ||
| Don’t know | 347 (69.4) | 56 (16.1) | 291 (83.9) | ||
| I know the problems that can happen if CVS is not treated | True | 83 (16.6) | 11 (13.3) | 72 (86.7) | 0.619 |
| False | 67 (13.4) | 10 (14.9) | 57 (85.1) | ||
| Don’t know | 350 (70.0) | 61 (17.4) | 289 (82.6) | ||
| I am aware of the signs and symptoms of CVS | True | 92 (18.4) | 20 (21.7) | 72 (78.3) | 0.244 |
| False | 65 (13.0) | 8 (12.3) | 57 (87.7) | ||
| Don’t know | 343 (68.6) | 54 (15.7) | 289 (84.3) | ||
| I know about the treatment of CVS | True | 39 (7.8) | 7 (17.9) | 32 (82.1) | 0.913 |
| False | 86 (17.2) | 15 (17.4) | 71 (82.6) | ||
| Don’t know | 375 (75.0) | 60 (16.0) | 315 (84.0) | ||
| I know how to prevent CVS | True | 55 (11.0) | 16 (29.1) | 39 (70.9) | 0.018 |
| False | 77 (15.4) | 9 (11.7) | 68 (88.3) | ||
| Don’t know | 368 (73.6) | 57 (15.5) | 311 (84.5) | ||
CVS, computer vision syndrome.
The results of logistic regression that identified the major predictors of CVS are presented in table 5. The authors checked the collinearity, and the results of VIF suggest that no significant multicollinearity exists. The unadjusted model revealed that children aged 12–14 years had 11.03 times greater odds (crude OR (COR): 11.03, 95% CI 2.40 to 50.55) of developing CVS compared with those aged 5–7 years. Gender seems to have an insignificant effect on developing CVS. The school year demonstrated marked differences, with grade 4 students having the highest odds (COR: 14.39, 95% CI 3.35 to 61.70) of reporting CVS compared with those in grade 1. Even grade 5 students showed more odds of having CVS (COR: 9.38, 95% CI 2.17 to 40.48), although the adjusted model slightly reduced this effect (adjusted OR (AOR): 6.87, 95% CI 0.67 to 70.89). Additionally, the education level of mothers played a critical role, with higher secondary education being associated with reduced odds (COR: 0.13, 95% CI 0.02 to 0.67) of their children experiencing CVS. Furthermore, economic status revealed an interesting trend, as children from households earning between 40 000 and 50 000 Taka had significantly lower odds of experiencing CVS (AOR: 0.13, 95% CI 0.02 to 0.69) compared with those from households earning less than 10 000 Taka (table 5).
Table 5. Results of the logistic regression model (n=500).
| Variables | Labels | Unadjusted model | Adjusted model | ||
|---|---|---|---|---|---|
| COR | 95% CI | AOR | 95% CI | ||
| Age (years) | 5–7 | Ref. | – | Ref. | – |
| 8–11 | 9.52** | 2.28 to 39.73 | 2.59 | 0.24 to 27.65 | |
| 12–14 | 11.03** | 2.40 to 50.55 | 3.63 | 0.27 to 48.85 | |
| Gender | Female | Ref. | – | Ref. | – |
| Male | 1.29 | 0.80 to 2.08 | 1.04 | 0.50 to 2.17 | |
| School year | Grade 1 | Ref. | – | Ref. | – |
| Grade 2 | 6.06* | 1.17 to 31.29 | 4.17 | 0.44 to 39.59 | |
| Grade 3 | 11.32** | 2.47 to 51.75 | 10.85** | 1.02 to 115.80 | |
| Grade 4 | 14.39*** | 3.35 to 61.70 | 11.57** | 1.17 to 114.09 | |
| Grade 5 | 9.38** | 2.17 to 40.48 | 6.87 | 0.67 to 70.89 | |
| Mothers’ education | Uneducated | Ref. | – | Ref. | – |
| Primary | 0.49 | 0.10 to 2.22 | 0.25 | 0.04 to 1.64 | |
| Secondary | 0.39 | 0.08 to 1.83 | 0.37 | 0.06 to 2.37 | |
| Higher Secondary | 0.13* | 0.02 to 0.67 | 0.09** | 0.01 to 0.60 | |
| Graduate | 0.45 | 0.11 to 1.88 | 0.30 | 0.05 to 1.82 | |
| Economic status (Taka) | <10 000 | Ref. | – | Ref. | – |
| 10 000–30 000 | 0.39* | 0.13 to 1.16 | 0.56 | 0.14 to 2.13 | |
| 30 000–40 000 | 0.22** | 0.07 to 0.74 | 0.25* | 0.06 to 1.12 | |
| 40 000–50 000 | 0.19** | 0.05 to 0.66 | 0.13** | 0.02 to 0.69 | |
| 50000 or more | 0.54 | 0.19 to 1.55 | 0.33 | 0.07 to 1.48 | |
| Types of device use | Mobile/tab | Ref. | – | Ref. | – |
| Television | 0.44 | 0.14 to 1.36 | 0.60 | 0.15 to 2.39 | |
| Computer | 4.43 | 0.59 to 33.14 | 9.10* | 0.66 to 125.30 | |
| Mobile and television | 0.69 | 0.38 to 1.25 | 1.11 | 0.51 to 2.40 | |
| Mobile and computer | 1.26 | 0.38 to 4.20 | 1.26 | 0.26 to 6.02 | |
| All three devices | 1.32 | 0.65 to 2.67 | 1.37 | 0.51 to 3.84 | |
| Duration of use (hours) | <1 | Ref. | – | Ref. | – |
| 1–2 | 0.89 | 0.46 to 1.74 | 1.11 | 0.48 to 2.55 | |
| 2–3 | 0.75 | 0.34 to 1.64 | 0.69 | 0.26 to 1.84 | |
| 3–4 | 2.46** | 1.07 to 5.63 | 4.50** | 1.51 to 13.41 | |
| 4 or more | 3.74** | 1.60 to 8.71 | 5.34** | 1.79 to 15.86 | |
| Brightness of device | Low | Ref. | – | Ref. | – |
| Medium | 1.37 | 0.56 to 3.36 | 1.09 | 0.34 to 3.48 | |
| High | 1.39 | 0.45 to 4.27 | 0.89 | 0.21 to 3.81 | |
| Taking breaks while using | No break | Ref. | – | Ref. | – |
| Every 30 min | 1.02 | 0.46 to 2.27 | 0.76 | 0.26 to 2.23 | |
| Every 1 hour | 0.57 | 0.23 to 1.41 | 0.44 | 0.14 to 1.54 | |
| More than 1 hour | 0.85 | 0.40 to 1.80 | 0.68 | 0.24 to 1.91 | |
| Personal history | No disease history | Ref. | – | Ref. | – |
| Only eye problem | 6.41*** | 3.13 to 13.10 | 6.50*** | 2.53 to 16.73 | |
| Only headache | 4.68*** | 2.34 to 9.36 | 5.42*** | 2.42 to 12.13 | |
| Both headache and eye problems | 12.41*** | 5.91 to 26.05 | 14.66*** | 5.47 to 39.26 | |
| Use of spectacles | Yes | Ref. | – | Ref. | – |
| No | 0.34*** | 0.20 to 0.57 | 0.99 | 0.44 to 2.20 | |
*0.05≤p<0.1; **p<0.05; ***p<0.001; CVS status (yes=1, no=0).
AOR, adjusted OR; COR, crude OR; CVS, computer vision syndrome.
The findings of the adjusted model depict that the duration of digital device use was significantly associated with the development of CVS. Children using digital devices for 3–4 hours exhibited 4.50 times higher odds of developing CVS (AOR: 4.50, 95% CI 1.51 to 13.41) compared with those using devices for less than 1 hour. The odds are higher for those using devices for more than 4 hours, with 5.34 times higher odds (AOR: 5.34, 95% CI 1.79 to 15.86). Additionally, a notable predictor was the presence of a personal history of eye problems or headaches. Children exhibiting both headaches and visual problems had 14.66 times higher chances (AOR: 14.66, 95% CI 5.47 to 39.26) of developing CVS. In contrast, individuals with only optical issues or isolated headaches had increased chances of 6.50 times (AOR: 6.50, 95% CI 2.53 to 16.73) and 5.42 times (AOR: 5.42, 95% CI 2.42 to 12.13), respectively, after controlling for all pertinent variables in the logistic regression analysis.
Discussion
In Bangladesh, literature on CVS in children is scarce, making this study more effective in offering valuable insights into this important area. The overall prevalence of CVS among primary school students is 16.4%. Other research reported high prevalences.17 37 The differences may be due to regional factors, study populations and varying levels of screen exposure among children. Key factors included age, economic status, maternal education and screen time duration, which were associated with CVS in this study. Students aged 12–14 years exhibited significantly higher CVS rates that are consistent with existing studies, and they pointed out that older students were more likely to have CVS because of increased exposure to digital devices and academic expectations.17 38 Previous studies also highlighted the trend that older children, who often spend more time on screens for educational purposes, face intensified CVS risk.19 39 Economic status also emerged as a significant predictor, with students from lower-income families (earning less than 10 000 Taka/month) showing the highest CVS prevalence at 33.3%. While the literature on direct links between CVS and economic status varies, studies indicate that lower socioeconomic status often correlates with increased screen time due to fewer alternative recreational activities and limited awareness of digital health risks.40 41 This socioeconomic influence on screen time can contribute to higher CVS rates.42
Higher maternal education was associated with lower CVS rates, with children of mothers holding secondary or graduate education showing CVS prevalence as low as 6.3%. This aligns with findings of a previous study,43 suggesting that educated mothers are more likely to implement preventive measures for digital eye strain, fostering better screen habits in their children.43 Previous studies identified that maternal education positively impacted children’s preventive health behaviours.44 45 Students who used screens for more than 4 hours daily had a significantly higher risk of developing CVS. This finding is consistent with research highlighting prolonged screen time as a primary driver of digital eye strain.46 Extended exposure to screens increases strain, reduces blink rate and leads to symptoms like dryness, fatigue and overall eye strain. Researchers identified a direct correlation between screen time and CVS symptoms, reinforcing the current study’s findings.46 47
The most commonly reported symptoms of CVS included eye itching, headaches and a sensation of a foreign body in the eye, findings that are consistent with previous studies identifying these as prevalent CVS symptoms.48 The reasons for these symptoms include reduced blink rates and increased eye strain from extended screen use. These results support existing evidence that points to these symptoms as hallmark indicators of CVS and highlight the importance of managing screen time to prevent discomfort and related issues.32 48 The COVID-19 pandemic brought a substantial increase in screen time, with many students shifting from using screens for less than an hour daily to prolonged usage. This change aligns with other studies that report increased screen exposure due to remote learning and reduced outdoor activities during lockdowns.49 50 The primary reason for this shift after the pandemic is the global shift to digital learning, which has normalised longer screen time. Literature confirms that this increase contributed to higher rates of digital eye strain and CVS among children, underscoring the need for strategies to mitigate screen-related health issues post-pandemic.50
It is observed that students with CVS scored lower on average in mathematics, science and English than their peers without CVS. This aligns with studies indicating a negative impact of CVS on cognitive performance, potentially due to discomfort and concentration issues during study sessions.51 The discomfort from CVS symptoms, such as headaches, eye strain and dryness, can interfere with a child’s ability to focus and perform academically. A study also reported that symptoms associated with CVS can decrease productivity and accuracy, linking ocular health with academic performance.52 Parental awareness of CVS was notably low, with only a small fraction of parents informed about the syndrome, its causes, symptoms and prevention. This finding is consistent with research that indicates a widespread gap in parental knowledge regarding digital eye health.53 54 The main reason for this knowledge gap may be the lack of sufficient public health information on managing children’s screen exposure. Studies reinforce that improving parental education is crucial for preventing CVS and promoting healthier screen habits for children.53 54
Logistic regression analysis revealed that several factors, including class level, personal health history, maternal education and duration of device use, were significant predictors of CVS. Higher class levels were associated with greater CVS prevalence, which aligns with another study showing that older students experience increased eye strain due to more intensive academic workloads and screen use for educational and recreational purposes prevalence.17 Literature supports that older students are more susceptible to CVS due to prolonged exposure to digital devices.38 Personal health history was also a strong predictor, particularly for children with pre-existing eye conditions or frequent headaches. The reason for this is that prior eye or neurological issues can heighten sensitivity to screen exposure,55 making the eyes more prone to strain and discomfort during extended use. Evidence in the literature confirms that children with existing eye problems or a history of headaches are at higher risk for developing CVS, as these pre-existing conditions exacerbate the symptoms of digital eye strain and reduce the ability to recover from prolonged screen exposure.56
Maternal education was influential; children of mothers with lower education levels were more likely to have CVS, reflecting studies that link parental education to children’s health outcomes.57 This could be because mothers with less education may have limited awareness of eye health practices. The duration of device use was another key predictor, with prolonged screen exposure correlating with higher CVS odds, which is consistent with a broad range of literature that emphasises continuous eye strain and reduced blink rates as major contributors to CVS.58 Although the type of device used was not identified as a statistically significant predictor of CVS in the analysis, it remains an important factor to consider. Trends observed in the study indicated slightly higher CVS rates among students using computers compared with those using mobile devices or tablets. This may be due to differences in screen size, brightness and viewing distance. Computer use often involves closer viewing distances and prolonged focus on larger screens, which can intensify eye strain. While the statistical insignificance might be due to similar usage patterns across devices, existing literature suggests that different types of devices can affect visual strain differently.59
The main limitation of this study is the use of a semi-purposive convenience sampling method, resulting from the absence of a comprehensive sampling frame and constraints related to time and funding. This approach may restrict the generalisability of the findings to all primary school children in Bangladesh. However, efforts were made to ensure diversity by collecting data from multiple schools across northern Dhaka. Additionally, the study relied on parental self-reporting through structured questionnaires to assess children’s screen usage and symptom experiences, which may introduce biases related to recall and reporting. Although face-to-face interviews were conducted to enhance data accuracy, the lack of clinical or physical examinations prevented validation of reported symptoms. Third, the academic performance measure might not accurately reflect general academic aptitude because it was restricted to three key courses. Fourth, because the study primarily looked at Dhaka’s urban students, the results might not be applicable to students in other areas. Finally, this study did not account for additional unmeasured factors that might influence CVS status, such as pre-existing neurological diseases or undiagnosed vision abnormalities. Despite these drawbacks, the study highlights the necessity for focused treatments and provides valuable insights on the prevalence, risk factors and parental knowledge of CVS among urban primary school students in the post-pandemic era.
Conclusion
The prevalence of CVS is 16.4% among primary school students in Dhaka, Bangladesh. The association of CVS with age, grade level, maternal education, economic status and daily screen time is significant. It was found that students exposed to more screen time had lower family incomes, were in higher grade levels and were more likely to develop CVS. Students with CVS reported experiencing symptoms like headaches, eye itching and burning in their eyes. In particular, children with and without CVS showed significant differences in academic performance, which may indicate that CVS hinders academic success. Parents who were unaware of CVS and the COVID-19 pandemic increased their children’s screen time. Parents and educational institutions should work together to resolve CVS among children. Parents should always suggest that their children play outdoor games when they are free and also try to spend an adequate amount of quality time with their children. Additionally, they must monitor their children’s screen time daily and reduce it as much as possible to decrease the chances of CVS. The government should take proper strategies, for example, some promotional activities through TV, newspapers or radio, to raise awareness among parents and children of CVS and its harmful effects. A different option that would help kids would be to incorporate information about CVS, its causes and prevention methods into the textbooks that kids go through during their school years. The authors recommend a further large-scale study incorporating other possible factors to find more insightful findings about CVS among children in Bangladesh.
Supplementary material
Acknowledgements
The authors sincerely thank Mst. Samiha Salma, Abu Rumman, Farzana Afroze Tasnim, Samiur Rahman, Al Amin Dewan and Md. Mishal Patwary for their invaluable assistance in data collection; their dedication and commitment were instrumental to the successful completion of this research. We are also grateful to all the participants who willingly provided their information and consented to the publication of the survey results in an anonymised form. In addition, the authors extend their appreciation to the editor and reviewers for their insightful comments and constructive feedback, which significantly improved the quality of the manuscript.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-098366).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Consent obtained directly from patient(s).
Ethics approval: This study involves human participants. The ethical approval for this study was taken from the Biosafety, Biosecurity, and Ethical Committee of Jahangirnagar University, Bangladesh, with reference number BBEC, JU/M 2024/11 (140), on 19 November 2024. Additionally, verbal consent was secured from the participants before the beginning of the survey, and the study objectives were explained to them. Participants were sufficiently informed that their data would remain confidential and no identifiable information would be shared. Additionally, it is presumed that participants may withdraw from the survey at any time. Participants gave informed consent to participate in the study before taking part.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Data availability statement
Data are available upon reasonable request.
References
- 1.Reddy SC, Low CK, Lim YP, et al. Computer vision syndrome: a study of knowledge and practices in university students. Nep J Oph. 2013;5:161–8. doi: 10.3126/nepjoph.v5i2.8707. [DOI] [PubMed] [Google Scholar]
- 2.Randolph SA. Computer Vision Syndrome. Workplace Health Saf. 2017;65:328. doi: 10.1177/2165079917712727. [DOI] [PubMed] [Google Scholar]
- 3.Al Tawil L, Aldokhayel S, Zeitouni L, et al. Prevalence of self-reported computer vision syndrome symptoms and its associated factors among university students. Eur J Ophthalmol. 2020;30:189–95. doi: 10.1177/1120672118815110. [DOI] [PubMed] [Google Scholar]
- 4.Zenbaba D, Sahiledengle B, Bonsa M, et al. Prevalence of Computer Vision Syndrome and Associated Factors among Instructors in Ethiopian Universities: A Web-Based Cross-Sectional Study. ScientificWorldJournal. 2021;2021:1–8. doi: 10.1155/2021/3384332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ccami-Bernal F, Soriano-Moreno DR, Romero-Robles MA, et al. Prevalence of computer vision syndrome: A systematic review and meta-analysis. J Optom. 2024;17:100482. doi: 10.1016/j.optom.2023.100482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dessie A, Adane F, Nega A, et al. Computer Vision Syndrome and Associated Factors among Computer Users in Debre Tabor Town, Northwest Ethiopia. J Environ Public Health. 2018;2018:1–8. doi: 10.1155/2018/4107590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang L, Wei X, Deng Y. Computer Vision Syndrome During SARS-CoV-2 Outbreak in University Students: A Comparison Between Online Courses and Classroom Lectures. Front Public Health. 2021;9:696036. doi: 10.3389/fpubh.2021.696036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ranasinghe P, Wathurapatha WS, Perera YS, et al. Computer vision syndrome among computer office workers in a developing country: an evaluation of prevalence and risk factors. BMC Res Notes. 2016;9:1–9. doi: 10.1186/s13104-016-1962-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roy S. Dangers of Computer Vision Syndrome. 2022. https://today.thefinancialexpress.com.bd/editorial/dangers-of-computer-vision-syndrome-1667740757 Available.
- 10.Roy S, Sharif AB, Chowdhury S, et al. Unavoidable online education due to COVID-19 and its association to computer vision syndrome: a cross-sectional survey. BMJ Open Ophth . 2022;7:e001118. doi: 10.1136/bmjophth-2022-001118. [DOI] [Google Scholar]
- 11.Abdulla F, Hossain MdM, Huq MN, et al. Prevalence, determinants and consequences of problematic smartphone use among preschoolers (3–5 years) from Dhaka, Bangladesh: A cross-sectional investigation. J Affect Disord. 2023;329:413–27. doi: 10.1016/j.jad.2023.02.094. [DOI] [PubMed] [Google Scholar]
- 12.Abdulla F, Huq MN, Hossain MM. Problematic Smartphone Use Among Children Requires Immediate Attention. Asia Pac J Public Health. 2024;36:278–9. doi: 10.1177/10105395231226284. [DOI] [PubMed] [Google Scholar]
- 13.Wolffsohn JS, Lingham G, Downie LE, et al. TFOS Lifestyle: Impact of the digital environment on the ocular surface. Ocul Surf. 2023;28:213–52. doi: 10.1016/j.jtos.2023.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Chu GCH, Chan LYL, Do C, et al. Association between time spent on smartphones and digital eye strain: A 1-year prospective observational study among Hong Kong children and adolescents. Environ Sci Pollut Res . 2023;30:58428–35. doi: 10.1007/s11356-023-26258-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muppalla SK, Vuppalapati S, Reddy Pulliahgaru A, et al. Effects of Excessive Screen Time on Child Development: An Updated Review and Strategies for Management. Cureus. 2023;15:e40608. doi: 10.7759/cureus.40608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagata JM, Iyer P, Chu J, et al. Contemporary screen time usage among children 9–10‐years‐old is associated with higher body mass index percentile at 1‐year follow‐up: A prospective cohort study. Pediatr Obes. 2021;16:e12827. doi: 10.1111/ijpo.12827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abuallut I, Ajeebi RE, Bahari AY, et al. Prevalence of Computer Vision Syndrome among School-Age Children during the COVID-19 Pandemic, Saudi Arabia: A Cross-Sectional Survey. Children (Basel) 2022;9:1718. doi: 10.3390/children9111718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rahman A, Abdulla F, Karimuzzaman M, et al. Burden of COVID‐19 on health and wellbeing, education, and economy of Bangladesh. Clin Case Rep. 2022;10:e6639. doi: 10.1002/ccr3.6639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seresirikachorn K, Thiamthat W, Sriyuttagrai W, et al. Effects of digital devices and online learning on computer vision syndrome in students during the COVID-19 era: an online questionnaire study. Bmjpo. 2022;6:e001429. doi: 10.1136/bmjpo-2022-001429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mohan A, Sen P, Shah C, et al. Prevalence and risk factor assessment of digital eye strain among children using online e-learning during the COVID-19 pandemic. Indian J Ophthalmol. 2021;69:140–4. doi: 10.4103/ijo.IJO_2535_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Priftis N, Panagiotakos D. Screen Time and Its Health Consequences in Children and Adolescents. Children (Basel) 2023;10:1665. doi: 10.3390/children10101665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ishtiaq A, Ashraf H, Iftikhar S, et al. Parental perception on screen time and psychological distress among young children. J Family Med Prim Care. 2021;10:765–72. doi: 10.4103/jfmpc.jfmpc_1720_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson S, Rosenfield M. 20-20-20 Rule: Are These Numbers Justified? Optom Vis Sci. 2023;100:52–6. doi: 10.1097/OPX.0000000000001971. [DOI] [PubMed] [Google Scholar]
- 24.Singh S, Downie LE, Anderson AJ. Do Blue-blocking Lenses Reduce Eye Strain From Extended Screen Time? A Double-Masked Randomized Controlled Trial. Am J Ophthalmol. 2021;226:243–51. doi: 10.1016/j.ajo.2021.02.010. [DOI] [PubMed] [Google Scholar]
- 25.Singh S, Keller PR, Busija L, et al. Blue-light filtering spectacle lenses for visual performance, sleep, and macular health in adults. Cochrane Database Syst Rev. 2023;8:CD013244. doi: 10.1002/14651858.CD013244.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Singh S, McGuinness MB, Anderson AJ, et al. Interventions for the Management of Computer Vision Syndrome. Ophthalmology. 2022;129:1192–215. doi: 10.1016/j.ophtha.2022.05.009. [DOI] [PubMed] [Google Scholar]
- 27.Chaturvedi N, Singh P, Bhattacharya M. Screen exposure time and computer vision syndrome in school-age children during COVID-19 era. J Clin Ophthal Res. 2022;10:105–9. doi: 10.4103/jcor.jcor_157_21. [DOI] [Google Scholar]
- 28.Qi J, Yan Y, Yin H. Screen time among school-aged children of aged 6-14: a systematic review. Glob Health Res Policy. 2023;8:12. doi: 10.1186/s41256-023-00297-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abudawood GA, Ashi HM, Almarzouki NK. Computer Vision Syndrome among Undergraduate Medical Students in King Abdulaziz University, Jeddah, Saudi Arabia. J Ophthalmol. 2020;2020:1–7. doi: 10.1155/2020/2789376. [DOI] [Google Scholar]
- 30.Issa R, Sfeir M, Azzi V, et al. Association of Computer Vision Syndrome with Depression/Anxiety among Lebanese Young Adults: The Mediating Effect of Stress. Healthcare (Basel) 2023;11:2674. doi: 10.3390/healthcare11192674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Akter F, Ahmed CM, Ahmed SA. School Meals Case Study: Bangladesh. The State of Food Security and Nutrition in the World 2022. 2022. http://www.fao.org/documents/card/en/c/cc0639en Available.
- 32.Seguí M del M, Cabrero-García J, Crespo A, et al. A reliable and valid questionnaire was developed to measure computer vision syndrome at the workplace. J Clin Epidemiol. 2015;68:662–73. doi: 10.1016/j.jclinepi.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 33.Alatawi SK, Allinjawi K, Alzahrani K, et al. Self-Reported Student Awareness and Prevalence of Computer Vision Syndrome During COVID-19 Pandemic at Al-Baha University. Clin Optom (Auckl) 2022;14:159–72. doi: 10.2147/OPTO.S374837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davis EK, Ntow FD, Beccles C. Factors Influencing Ghanaian Public Junior High School Students’ Performance in English Language, Mathematics and Science and its Implications on the National Policy on Progression. Sage Open. 2022;12 doi: 10.1177/21582440221123912. [DOI] [Google Scholar]
- 35.Di Pietro G. The impact of Covid-19 on student achievement: Evidence from a recent meta-analysis. Educ Res Rev. 2023;39:100530. doi: 10.1016/j.edurev.2023.100530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rahman A, Abdulla F, Hossain MM. Scientific data analysis with R: biostatistical applications. 1st. Boca Raton, USA: Chapman & Hall/CRC; 2024. edn. [Google Scholar]
- 37.Li R, Ying B, Qian Y, et al. Prevalence of Self-Reported Symptoms of Computer Vision Syndrome and Associated Risk Factors among School Students in China during the COVID-19 Pandemic. Ophthalmic Epidemiol. 2022;29:363–73. doi: 10.1080/09286586.2021.1963786. [DOI] [PubMed] [Google Scholar]
- 38.Khalaj M, Ebrahimi M, Shojai P, et al. Computer Vision Syndrome in Eleven to Eighteen-Year-Old Students in Qazvin. Biotech Health Sci. 2015;2:e28234. doi: 10.17795/bhs-28234. [DOI] [Google Scholar]
- 39.Mrayyan MT, Alseid ARH, Ghoolah TS, et al. Investigating the Prevalence of Computer Vision Syndrome (CVS) Among Undergraduate Nursing Students: A Cross-Sectional Study. SAGE Open Nursing . 2023;9:1–12. doi: 10.1177/23779608231191883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ke Y, Chen S, Hong J, et al. Associations between socioeconomic status and screen time among children and adolescents in China: A cross-sectional study. PLoS ONE. 2023;18:e0280248. doi: 10.1371/journal.pone.0280248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kwon S, Armstrong B, Wetoska N, et al. Screen Time, Sociodemographic Factors, and Psychological Well-Being Among Young Children. JAMA Netw Open . 2024;7:e2354488. doi: 10.1001/jamanetworkopen.2023.54488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McArthur BA, Browne D, Racine N, et al. Screen Time as a Mechanism Through Which Cumulative Risk is Related to Child Socioemotional and Developmental Outcomes in Early Childhood. Res Child Adolesc Psychopathol . 2022;50:709–20. doi: 10.1007/s10802-021-00895-w. [DOI] [PubMed] [Google Scholar]
- 43.Kothari G. Working with women to improve child and community eye health. Community Eye Health. 2009;22:20–1. https://pmc.ncbi.nlm.nih.gov/articles/PMC2760275/ Available. [PMC free article] [PubMed] [Google Scholar]
- 44.Huq MN, Tasnim T. Maternal Education and Child Healthcare in Bangladesh. Matern Child Health J. 2008;12:43–51. doi: 10.1007/s10995-007-0303-3. [DOI] [PubMed] [Google Scholar]
- 45.Desai S, Alva S. Maternal education and child health: Is there a strong causal relationship? Demography. 1998;35:71–81. doi: 10.2307/3004028. [DOI] [PubMed] [Google Scholar]
- 46.Mallik C. Computer Vision Syndrome among Children Using Online E-Learning during the COVID-19 Pandemic. J Chittagong Med Coll Teachers Ass . 2021;32:48–52. doi: 10.3329/jcmcta.v32i1.66537. [DOI] [Google Scholar]
- 47.Dyrek M, Sikorska E, Partyka A, et al. Prolonged screen-time as the cause of ocular disorders: what can we do with the problem? – a review. Eur J Clin Exp Med . 2024;22:222–31. doi: 10.15584/ejcem.2024.1.26. [DOI] [Google Scholar]
- 48.Peter RG, Giloyan A, Harutyunyan T, et al. Computer vision syndrome (CVS): the assessment of prevalence and associated risk factors among the students of the American University of Armenia. J Public Health (Berl) 2025;33:1703–12. doi: 10.1007/s10389-023-02138-2. [DOI] [Google Scholar]
- 49.Resende MAA, Fonseca ML da, Freitas JT de, et al. Impacts caused by the use of screens during the COVID-19 pandemic in children and adolescents: an integrative review. Rev Paul Pediatr. 2024;42:e2022181. doi: 10.1590/1984-0462/2024/42/2022181. [DOI] [Google Scholar]
- 50.Agarwal R, Tripathi A, Khan IA, et al. Effect of increased screen time on eyes during COVID-19 pandemic. J Family Med Prim Care. 2022;11:3642–7. doi: 10.4103/jfmpc.jfmpc_2219_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pavel IA, Bogdanici CM, Donica VC, et al. Computer Vision Syndrome: An Ophthalmic Pathology of the Modern Era. Med Bogota Colomb. 2023;59:412. doi: 10.3390/medicina59020412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Abed Alah M, Abdeen S, Selim N, et al. Computer vision syndrome among students during remote learning periods: harnessing digital solutions for clear vision. Front Public Health. 2023;11:1273886. doi: 10.3389/fpubh.2023.1273886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.AlHarkan DH. Parent’s Awareness of Preventive Measures for Digital Eye Strain Syndrome among Saudi Students after 1 Year of Online Studies – A Survey. Middle East Afr J Ophthalmol. 2023;30:13–8. doi: 10.4103/meajo.meajo_72_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu S-M, Chang F-C, Chen C-Y, et al. Effects of Parental Involvement in a Preschool-Based Eye Health Intervention Regarding Children’s Screen Use in China. IJERPH. 2021;18:11330. doi: 10.3390/ijerph182111330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Arif K, Alam K. Computer Vision Syndrome. Faridpur Med College J. 2015;10:33–5. [Google Scholar]
- 56.Sheppard AL, Wolffsohn JS. Digital eye strain: prevalence, measurement and amelioration. BMJ Open Ophth. 2018;3:e000146. doi: 10.1136/bmjophth-2018-000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zill N. Parental schooling & children’s health. Public Health Rep. 1996;111:34–43. [PMC free article] [PubMed] [Google Scholar]
- 58.Wadhwani M, Manika M, Jajoo M, et al. Online survey to assess computer vision syndrome in children due to excessive screen exposure during the COVID 19 pandemic lockdown. J Family Med Prim Care. 2022;11:5387–92. doi: 10.4103/jfmpc.jfmpc_1771_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rosenfield M, Mcoptom MR. Computer vision syndrome (a.k.a. digital eye strain) Optom Pract. 2016:1–10. https://www.researchgate.net/publication/295902618 Available. [Google Scholar]