Abstract
Background
The prevalence of high body mass index (BMI) has been increasing over the past three decades, resulting in significant public health challenges. This study aims to comprehensively analyze global, regional, and national trends in death and disability-adjusted life years (DALYs) attributable to high BMI from 1990 to 2021.
Methods
We utilized data from the Global Burden of Disease study to estimate deaths and DALYs linked to high BMI across 204 countries and territories. Temporal trends were analyzed by sex, age group, region, and Socio-demographic index (SDI). Decomposition analyses were conducted to assess the impact of demographic factors on BMI-related disease burden. All estimates are presented with 95% uncertainty interval (UI) to quantify statistical uncertainty. The autoregressive integrated moving average model was employed to project future trends to 2036.
Results
Globally, BMI-related deaths increased from 1.46 million (95% UI 0.72, 2.29) in 1990 to 3.71 million (95% UI 1.85, 5.66) in 2021. DALYs rose from 48 million (95% UI 21.2, 77.3) to 128.5 million (95% UI 56, 202.4) over the same period. Diabetes and kidney diseases have now overtaken cardiovascular diseases as the leading cause of DALYs, despite cardiovascular diseases remain the major contributor to BMI-related deaths. They accounted for 82.01% of deaths and 73.91% of DALYs. Among the four regions with the highest SDI, three showed a decline in BMI-related deaths and DALYs, except for high-income North America. In contrast, low-SDI regions continued to face escalating health burdens. Population aging was a primary driver of the increasing burden, which made up 49.43% of the increase in deaths and 47.03% in DALYs.
Conclusions
The increasing prevalence of high BMI has resulted in significant health burdens over the past three decades, with cardiovascular diseases, diabetes and kidney diseases being primary contributors. Low- and middle-income regions bear a larger share of the burden, while population aging exacerbates these challenges. Developing equitable and effective public health strategies is essential for addressing the growing obesity epidemic.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-025-23237-7.
Keywords: High body mass index, Global burden of disease, Disability-adjusted life years, Health inequality, Trends
Background
High body mass index (BMI) has emerged as one of the most significant health challenges, contributing significantly to the global burden of non-communicable diseases (NCDs), including type 2 diabetes, cardiovascular diseases, certain cancers, and musculoskeletal disorders [1]. It is alarming that the global prevalence of overweight and obesity has almost tripled since 1980, with nearly 2 billion adults now classified as overweight and more than 600 million as obese [2]. Countries with different Socio-demographic index (SDI) levels are witnessing a faster rise in BMI-related health issues, especially in low- and middle-income countries [3, 4]. Despite numerous public health interventions aimed at reducing obesity, the global trends show little sign of abatement, with the disease burden continuing to grow across various regions [5].
Numerous studies have investigated the link between obesity and specific diseases [6, 7]. With ongoing demographic shifts, including an aging population, advancements in medical care, and evolving socioeconomic conditions, the prevalence and characteristics of obesity are expected to change. Additionally, the persistent impact of poor diet and physical inactivity may further complicate its effects on public health [4, 8]. The Global Burden of Disease (GBD) study offers an avenue to address this gap by offering a detailed analysis of BMI-related health outcomes across 204 countries and territories from 1990 to 2021, offering insights into both historical trends and future projections [4]. The persistence of these trends underscores the need for urgent and sustained public health initiatives [9].
This study aims to provide a comprehensive global, regional, and national analysis of the BMI-related burden from 1990 to 2021, examining trends by age groups, sex, and SDI level. Based on SDI level, frontier analysis is employed to determine the optimal frontier value for deaths and DALYs linked to high BMI in each country. These analyses will result in the most comprehensive epidemiological assessment of the disease burden linked to high BMI to date. By examining the association between BMI and health outcomes across diverse socio-demographic contexts, this research aims to inform public health strategies designed to mitigate the increasing global impact of obesity.
Methods
Data sources
This study adheres to the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER Checklist) (https://www.who.int/publications/m/item/gather-checklist) [10]. GBD 2021 assesses health risks related to 371 injuries, diseases, and 88 risk factors in 204 countries and territories, from 1990 to 2021 [11]. Data on the BMI-related burden were sourced from the GBD Results Tool (http://ghdx.healthdata.org/gbd-results-tool). The detailed study validity protocol is available on the Institute of Health Measurement and Evaluation (IHME) website (https://www.healthdata.org/gbd/about/protocol).
Definitions
High BMI is usually categorized as overweight (BMI ≥ 25 kg/m2) or obese (BMI ≥ 30 kg/m2), whether in adults or children.[12–14]. All cause-specific deaths and DALYs by year, age, sex, region, and nation were obtained from GBD 2021, covering the period from 1990 to 2021. DALY provides a comprehensive assessment of disease burden, which represents the aggregate of years lost due to premature death and years spent living with disability [13]. One DALY corresponds to the loss of one year in health [15]. Age groups were categorized into 5-year intervals (< 5, 5–9, 10–14, 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80–84, 85–89, 90–94, and 95 + years) for analysis of age-specific patterns. This study includes two metrics: number and rate, which respectively represent the absolute number of cases and number of cases per 100,000 individuals in GBD 2021. Unless otherwise specified, all rates presented in this study are age-standardized rates, which have been adjusted using the global age structure to allow for meaningful comparisons across different populations and time periods [16].
Causes of deaths and DALYs were organized into 4 levels in GBD 2021 [14].Level 1 comprised four primary groups: communicable, maternal, and neonatal conditions and nutritional disease; NCDs; injuries; and other COVID-19 pandemic-related outcomes. Level 2 included 22 categories of diseases and injuries within level 1, such as diabetes and kidney diseases within NCDs. Level 3 encompassed 175 specific causes under level 2, such as diabetes within diabetes and kidney diseases. Level 4 further detailed sub-causes of level 3. In GBD 2021, high BMI was linked to 7 level 2 causes of death and 9 level 2 causes of DALYs across sexes. Furthermore, the count of level 3 causes linked to high BMI was 24 for death and 28 for DALYs in females, while it was 21 and 25 in males, respectively.
Population attributable fractions (PAFs) represent the proportion of deaths and DALYs that could potentially be avoided if high BMI exposure were reduced to an optimal reference level. PAFs were calculated using the comparative risk assessment methodology from GBD 2021, as previously described [13].
As a comprehensive indicator of a country’s development level, SDI was calculated using the total fertility rate (age < 25 years), average educational attainment (age ≥ 15 years), and per capita income [11, 13]. SDI ranges from 0 to 1, with 0 representing the lowest level and 1 the highest.
Statistical analysis
To assess the disease burden associated high BMI, we calculated the number of deaths and DALYs, percent change, and age-standardized rates, disaggregated by sex, age, year, region, and nation. Decomposition analysis was performed to identify the key drivers of BMI-related disease burden from 1990 to 2021, including population aging, growth, and epidemiological changes [17]. To assess health inequalities, we calculated the slope index of inequality and concentration index. The slope index quantifies the absolute difference in health outcomes between the highest and lowest ends of the socioeconomic spectrum. The concentration index measures the relative concentration of health outcomes across the entire socioeconomic distribution, ranging from − 1 to 1, with positive values indicating a concentration of burden among higher SDI populations and negative values indicating a concentration among lower SDI populations [18]. Frontier analysis was employed to determine the optimal level of deaths and DALYs, and analyze the efficiency of countries in minimizing BMI-related burden relative to their SDI level [19]. We used the autoregressive integrated moving average (ARIMA) model to project trends in age-standardized rate up to 2036. This forecasting model is well-suited to capturing time-series data and making future predictions based on observed trends [4].
The uncertainty intervals (UIs) provided in this study were calculated based on the standard methodology of the GBD 2021 study. The GBD employs Monte Carlo simulation to generate 1,000 estimates, from which the 2.5th and 97.5th percentiles are extracted to form the 95% uncertainty intervals [20]. This approach accounts for random errors in data sources, non-sampling errors, and model specification uncertainty. All statistical analyses were performed using R software (version 4.1.3), with the ‘survey’ package for complex survey data analysis, ‘boot’ package for bootstrapping, and ‘forecast’ package for ARIMA modeling.
Results
Spatiotemporal patterns of BMI-related disease burden
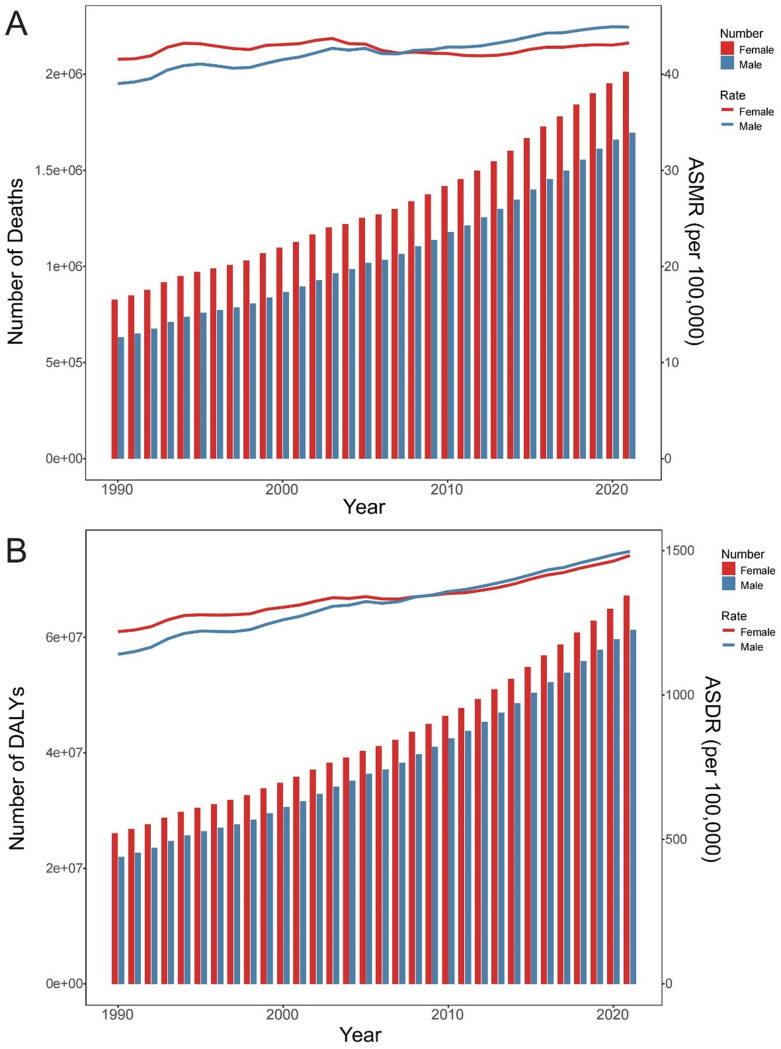
The global burden of high BMI revealed a steady increase in over the past three decade from 1990 to 2021. The global deaths have increased from 1.46 million (95%UI 0.72, 2.29) to 3.71 million (95%UI 1.85, 5.66) and the global DALYs have increased from 48 million (95%UI 21.2, 77.3) to 128.5 million (95%UI 56, 202.4). The trends have steadily increased for both sexes, with females showing higher absolute numbers throughout the period but surpassed by males in rates since 2008. Males experienced a 15.06% increase in age-standardized deaths rates and a 31.22% rise in DALYs, while females saw smaller increases of 4.06% in deaths and 21.6% in DALYs (Fig. 1). Despite these differences, the PAF for females was slightly higher than that for males in 2021 (Table S1).
Fig. 1.
All-age numbers and age-standardized rates of deaths (A) and DALYs (B) attributable to high BMI by sex, 1990–2021. BMI, body mass index; DALYs, disability-adjusted life years
Age-specific crude rates of death and DALY attributable to high BMI increased with advancing age across sexes. The crude death and DALY rates in females exceeded those in males in the 70–74 and 65–69 age groups, respectively. The number of deaths peaked in the 70–74 age group in females and 65–69 age group in males. As for DALYs, the peak was observed in the 65–69 age group in females and 60–64 age group in males (Fig. 2).
Fig. 2.
Age-specific numbers and crude rates of death (A & B) and DALY (C & D) attributable to high BMI by sex, in 2021. The shaded areas represent 95% uncertainty intervals. BMI, body mass index; DALY, disability-adjusted life year
The BMI-related global burden demonstrates significant regional disparities. In 2021, Southern Sub-Saharan Africa reported the highest age-standardized rates of deaths [125.12 (95%UI 71.21, 183.13) per 100,000 individuals] and DALYs [3430.11 (95%UI 1755.89, 5152.18)]. These findings contrast sharply with high-income Asia Pacific, showing the lowest rates in both deaths [10.83 (95%UI 5.23, 17.74)] and DALYs [662.64 (95%UI 253.69, 1110.48)]. From 1990 to 2021, the region with the highest increase in rates was South Asia (91.2% for deaths and 101.92% for DALYs), whereas Western Europe and high-income Asia Pacific experienced a biggest decline in deaths (31.17%) and DALYs (12.06%), respectively. Notably, the PAFs for deaths (> 140%) and DALYs (> 200%) increased significantly in East and South Asia, despite the lower deaths and DALYs rates (Fig. 3 and Table S1).
Fig. 3.
Age-standardized rates of deaths (A) and DALYs (B) attributable to high BMI in 2021 in 204 countries and territories. BMI, body mass index; DALYs, disability-adjusted life years
In 2021, Nauru reported the highest age-standardized rates of deaths [296.35 (95%UI 135.41, 454.58) per 100,000 individuals] and DALYs [9922.73 (95%UI 4581.83, 14859.93)], whereas Japan had the lowest rates of deaths [9.71 (95%UI 4.84, 16.08)] and DALYs [588.23 (95%UI 219.54, 995.7)]. From 1990 to 2021, Lesotho experienced the highest increase in the rates of deaths (135.31%) and DALYs (142.31%), whereas Ireland and Ethiopia experienced a biggest decline in deaths (− 46.98%) and DALYs (− 32.27%), respectively. Among the world’s 10 most populous countries, China, India and Bangladesh experienced the highest increase in the PAFs of deaths (> 150%) and DALYs (> 200%), whereas United Kingdom experienced the biggest percentage decline for deaths (− 14.61%) (Fig. 3 and Table S1).
Impact of high BMI on each disease
The global disease burden attributable to high BMI has shown significant variations across different causes. The GBD level 2 causes of deaths and DALYs are illustrated in Figure S1, S2 and Table S2. In 2021, cardiovascular disease was the main contributor of age-standardized deaths rate [22.77 (95%UI 12.87, 34.24) per 100,000 individuals], followed by diabetes and kidney diseases [13.51 (95%UI 7.14, 19.81)] and neoplasms [4.18 (95%UI 1.71, 6.8)]; they accounted for 91.46% of BMI-related deaths. In contrast, diabetes and kidney diseases was the primary driver of age-standardized DALYs rate [574.62 (95%UI 314.16, 807.45) per 100,000 individuals], followed by cardiovascular diseases [529 (95%UI 277.28, 808.64)] and musculoskeletal disorders [155.33 (95%UI 12.24, 332.41)]; they accounted for 84.31% of BMI-related DALYs. Additionally, of global diabetes and kidney diseases DALYs rates, 39.6% (95%UI 21.32, 54.61) was linked to high BMI; while the corresponding proportions were 10.47% (95%UI 5.6, 15.56) for cardiovascular diseases, 8.12% (95%UI 0.7, 15.66) for musculoskeletal disorders, and 3.46% (95%UI 1.44, 5.52) for neoplasms (Table S2).
For all GBD level 3 causes, global DALYs were highest for diabetes mellitus [452.55 (95%UI 220.36, 650.49) per 100,000 individuals], ischemic heart disease [277.65 (95%UI 109.8, 445.24)], hypertensive heart disease [147.33 (95%UI 109.06, 183.45)], chronic kidney disease [122.08 (95%UI 66.25, 180.18)], low back pain [97.66 (95%UI 9.78, 204)], and stroke [88.84 (95%UI 7.22, 182.93); Table S2]. Of diabetes mellitus DALYs worldwide, 49.36% (95%UI 23.53, 68.15) was linked to high BMI; while the corresponding proportions were 12.55% (95%UI 4.99, 19.71) for ischemic heart disease, 48.88% (95%UI 38.38, 59.61) for hypertensive heart disease, 23.03% (95%UI 12.58, 33.9) for chronic kidney disease, 11.74% (95%UI 1.22, 22.84) for low back pain, and 4.71% (95%UI 0.38, 9.75) for stroke (Fig. 4 and S3–S13).
Fig. 4.
Fraction of hypertensive heart disease, ischemic heart disease, and diabetes mellitus DALYs attributable to high BMI by region (A) and age group (B) in 2021. BMI, body mass index; DALY, disability-adjusted life year
Notably, some categories experienced statistical changes over time. From 1990 to 2021, cardiovascular diseases demonstrated a modest decline, particularly in ischemic heart disease, which saw a reduction of approximately − 14.99% in deaths and − 7.69% in DALYs. In the realm of diabetes and kidney diseases, both diabetes mellitus and chronic kidney disease exhibited a highest increase in both deaths (49.93%) and DALYs (79.2%) rates. Musculoskeletal disorders and neurological disorders also displayed large increases, with DALYs rising by over 40%. Neoplasms presented a mixed picture. Liver cancer experienced a dramatic rise in both deaths (106.81%) and DALYs (103.12%) rates, accompanied by a sharp rise in the PAFs. Similarly, pancreatic cancer displayed a significant, albeit highly variable, increase in both deaths and DALYs rates, with wide confidence intervals reflecting uncertainty in the precise magnitude of this trend. In contrast, other cancers showed more modest changes (Table S2).
Additionally, significant variations were observed in the attributable proportions of age-standardized DALYs linked to high BMI across regions, age groups and sexes (Fig. 4 and S3–S13). Of all GBD level 2 and 3 causes, females generally exhibited higher PAFs of DALYs compared to males. Across the 21 GBD regions, in 2021, high-income North America, Southern Sub − Saharan Africa North Africa and Middle East, and Central Asia had the highest PAFs of DALYs for most GBD level 2 and 3 causes in both sexes, whereas Southeast Asia, South Asia, high − income Asia Pacific, and eastern sub-Saharan Africa had the lowest PAFs. Across age groups, the PAFs of most GBD level 2 and 3 causes rose with age and peaked in adult age groups. For example, diabetes mellitus, ischemic heart disease and hypertensive heart disease had the highest attributable proportions in the age group 40–60 years for both sexes (Fig. 4).
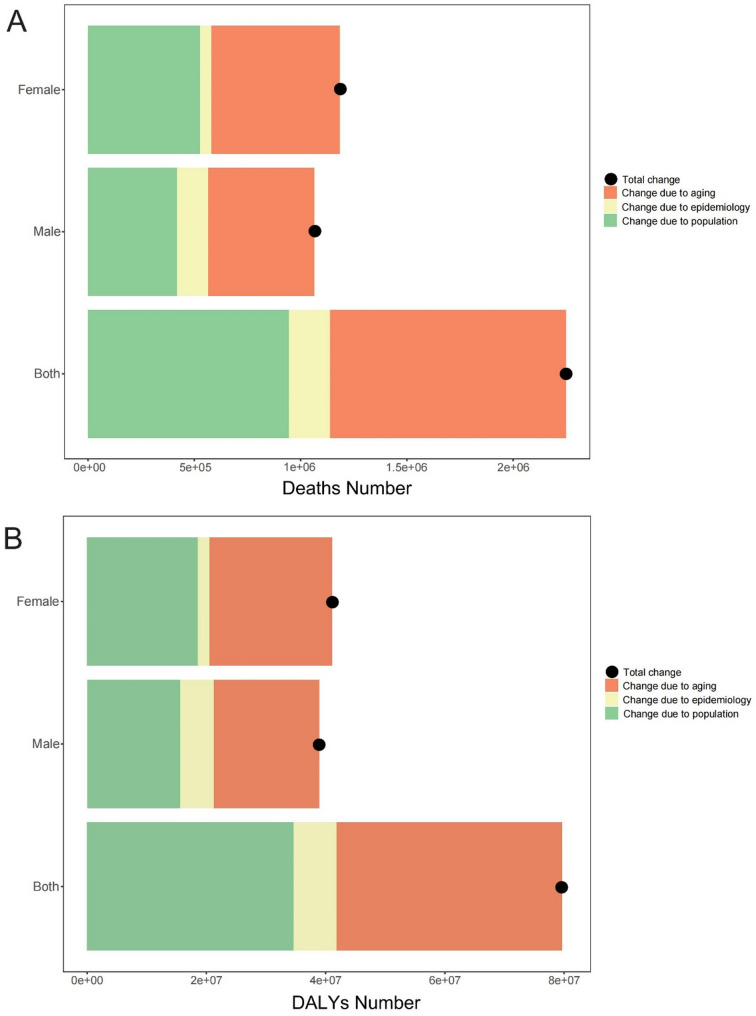
Decomposition of changes in BMI-related deaths and dalys, 1990–2021
Decomposition analysis was conducted to assess the impact of population aging, growth and epidemiological shifts on trends in deaths and DALYs from 1990 to 2021 (Fig. 5 and Table S3). The results showed that the increase in deaths is driven primarily by population aging and growth, which made up 91.47% of the increase in deaths and 91.07% of the increase in DALYs. The impact of aging is particularly pronounced, while epidemiological changes (such as shifts in disease prevalence and risk factors) played a smaller, though still important role.
Fig. 5.
Decomposition of all-age number changes in deaths (A) and DALYs (B) attributable to high BMI from 1990 to 2021. BMI, body mass index; DALYs, disability-adjusted life years
Association between SDI and BMI-related disease burden
In 2021, the lowest age-standardized rates of deaths and DALYs associated with high BMI were recorded respectively in the high-SDI region [35.13 (95% UI 16.59, 54.47) deaths per 100,000 individuals] and low-SDI region [1346.99 (95% UI 674.2, 2106.27) DALYs; Table S1]. Figure 6 displays the changes in deaths and DALYs rates across SDI for 21 regions from 1990 to 2021. Among the four regions with the highest SDI, three (Western Europe, high-income Asia Pacific, and Australasia) showed a decline in BMI-related deaths and DALYs, whereas the deaths rates remained stable and DALYs rates increased in high-income North America. In contrast, low-SDI regions continued to face escalating health burdens. Across countries, as SDI increases, deaths and DALYs rates rise until the SDI reaches approximately 0.62, but then decline with higher SDI. Based on SDI alone, the deaths and DALYs rates were significantly higher than expected in Nauru, Fiji and Marshall Islands in 2021 (Fig. 7).
Fig. 6.
Age-standardized rates of deaths (A) and DALYs (B) attributable to high BMI across 21 GBD regions by Socio-demographic index, 1990–2021. BMI, body mass index; DALYs, disability-adjusted life years; GBD, Global Burden of Disease Study
Fig. 7.
Age-standardized rates of deaths (A) and DALYs (B) attributable to high BMI across 204 countries and territories by Socio-demographic index in 2021. BMI, body mass index; DALYs, disability-adjusted life years; GBD, Global Burden of Disease Study
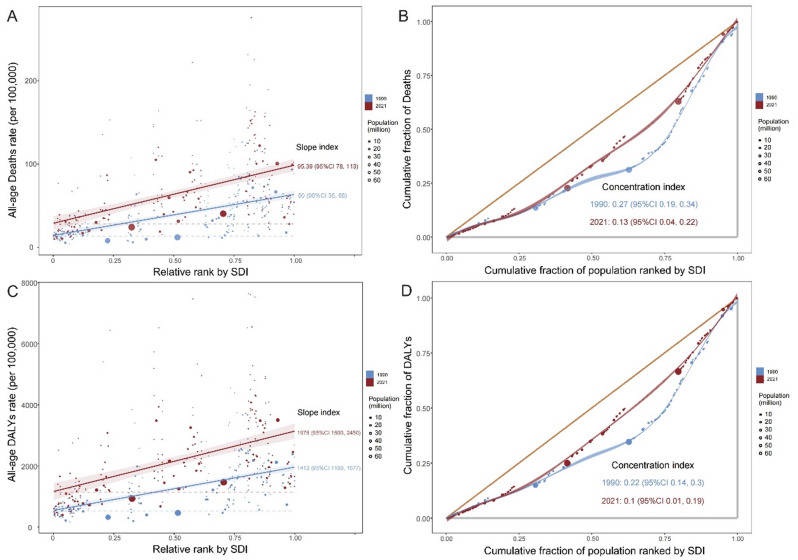
Health inequality in BMI-related deaths and dalys
Building on the earlier conclusion that deaths and DALYs are strongly correlated with SDI, we conducted further analyses to examine health inequities (Fig. 8 and Table S4). The slope index of deaths attributable to high BMI showed a slight increase, rising from 49.72 (95% CI: 34.62, 64.83) in 1990 to 95.39 (95% CI: 77.5, 113.27) in 2021, whereas the concentration index declined from 0.27 (95% CI: 0.19, 0.34) to 0.13 (95% CI: 0.04, 0.22) over the same period. Similarly, the slope index of DALYs rose from 1413.45 (95% CI: 1149.6, 1677.3) in 1990 to 1974.78 (95% CI: 1499.65, 2449.91) in 2021, while the concentration index decreased from 0.22 (95% CI: 0.14, 0.3) to 0.1 (95% CI: 0.01, 0.19) in 2021.
Fig. 8.
Slope and concentration indexes for deaths (A & B) and DALYs (B & D) attributable to high BMI from 1990 to 2021. The shaded areas represent 95% confidence intervals. The yellow line represents the line of perfect equality. BMI, body mass index; CI, confidence interval; DALYs, disability-adjusted life years
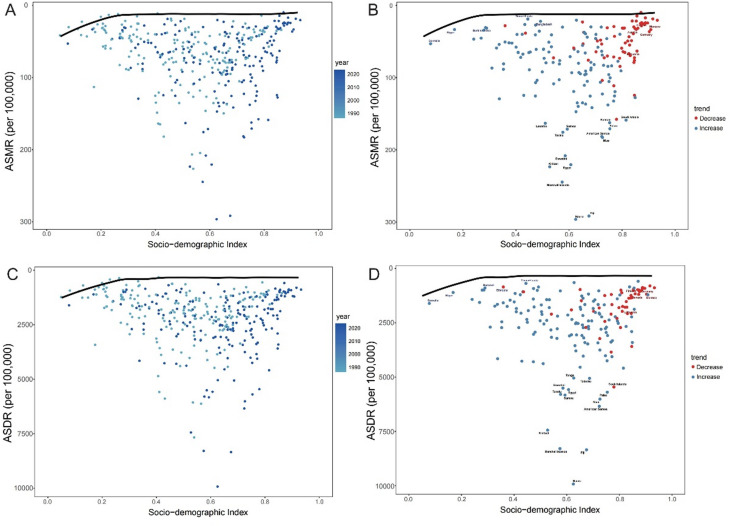
Frontier analysis of BMI-related deaths and dalys by SDI
To investigate the optimal conditions under which countries could effectively control the burden of disease in relation to their SDI, frontier analysis was conducted (Fig. 9). The results identified countries positioned differently concerning their proximity to the frontier fit line: five countries in blue are closest to the line among the low-SDI countries, five in red are furthest from the line among high-SDI countries, and 15 countries in black are furthest from the line across all countries. Specifically, countries such as Fiji, the Marshall Islands, Serbia, Kiribati, Egypt, American Samoa, and Niue were identified as being furthest from the frontier for both deaths and DALYs associated with high BMI. In countries with higher SDI, Lithuania and Germany consistently demonstrated the highest age-standardized death rates linked to high BMI, whereas Timor-Leste and Bangladesh, with lower SDI, exhibited significantly lower death rates. Furthermore, the analysis revealed a consistent decline in BMI-related deaths and DALYs over time in many high-SDI countries, while low-SDI countries exhibited either stable or increasing trends.
Fig. 9.
Frontier analysis based on SDI and age-standardized rates of deaths (A & B) and DALYs (C & D) attributable to high BMI in 204 countries and territories. BMI, body mass index; DALYs, disability-adjusted life years; SDI, socio-demographic index
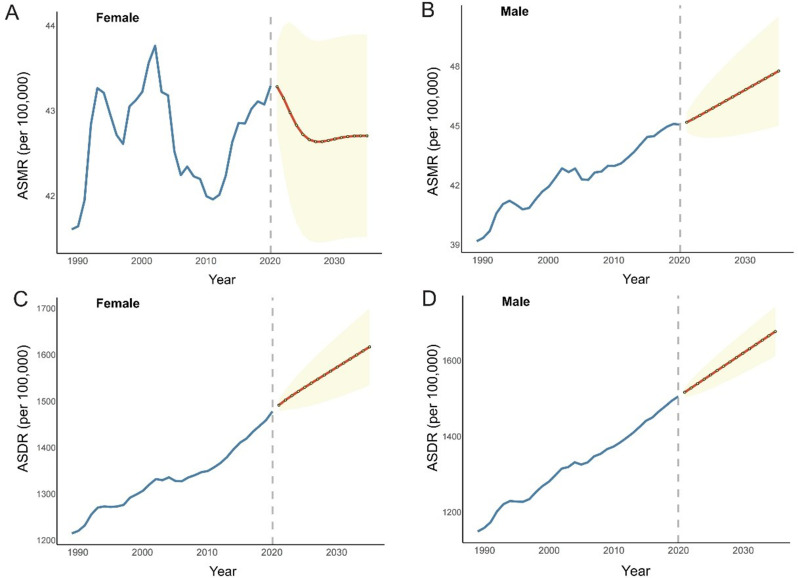
Projections of BMI-related deaths and dalys by sex up to 2036
In this study, the age-standardized rates of deaths and DALYs associated with high BMI were projected respectively for the next 15 years according to the ARIMA model (Fig. 10). With regard to deaths and DALYs, there is an overall upward trend across sexes, except for the deaths rate in female, which is expected to remain stable. Compared to 2021, the rates are projected to increase by 2.71 (95% UI -0.13, 5.45) deaths and 171.54 (106.25, 236.83) DALYs for males, while for females, they are expected to decrease by 0.59 (-0.6, 1.78) deaths and increase by 139.02 (56.4, 221.64) DALYs per 100,000 individuals by 2036 (Table S5). These forecasts highlight the ongoing and increasing global burden of high BMI-related mortality and morbidity, particularly among males, over the next 15 years.
Fig. 10.
Projections of age-standardized rates of deaths (A & B) and DALYs (C & D) attributable to high BMI, for the year 2036. The shaded areas represent 95% uncertainty intervals. BMI, body mass index; DALYs, disability-adjusted life years
Discussion
This study presents a thorough examination of the epidemiological trends in BMI-related disease burden from 1990 to 2021, incorporating multiple dimensions such as age, sex, region, and SDI. Over the past three decades, the BMI-related global burden has increased significantly. Projections using the ARIMA model suggest that this trend will continue by 2036. Decomposition analysis indicated that population aging and growth were the primary drivers of this increasing burden. Regionally, Southern Sub-Saharan Africa experienced the highest age-standardized rates, while High-Income Asia Pacific had the lowest. Our results reflected that diabetes and kidney diseases, cardiovascular diseases, and neoplasms remained the leading causes of death and DALYs associated with high BMI, and significant regional disparities highlighted the disproportionate impact on lower-SDI regions. The frontier analysis highlighted inefficiencies in several countries, where BMI-related health outcomes are worse than expected based on their SDI levels. These findings underscore the urgent need for public health interventions targeted at mitigating the rising impact of high BMI on global health.
Previous study observed that the global burden associated with high BMI had doubled from 1990 to 2017 [21]. Our findings further reinforce this trend, showing a continued upward trajectory from 2017 to 2021. Notably, the deaths rate attributable to high BMI has remained relatively stable, which may reflect increased attention to fatal obesity-related diseases and advancements in prevention and treatment, such as improved measures for cardiovascular disease prevention and management [22, 23]. However, the DALYs rate has shown a rapid increase, indicating a more severe impact of high BMI. Chronic disabling but non-fatal diseases, such as musculoskeletal disorders, which significantly reduce quality of life, have rapidly risen and become the third leading contributor to high BMI-related DALYs rates. Therefore, it is crucial to implement effective measures to curb the spread of obesity and to enhance the focus on chronic disabling diseases.
Our findings revealed notable sex-specific patterns in BMI-related disease burden, with males exhibiting higher age-standardized rates of deaths and DALYs than females since 2008. These differences likely arise from a complex interplay of biological, behavioral, and sociocultural factors [4, 24]. From a biological perspective, males and females differ significantly in body fat distribution and metabolism. Males typically exhibit android (central) obesity patterns with fat accumulation around the abdomen, which is more closely associated with cardiometabolic complications. In contrast, females often present with gynoid obesity patterns (fat distribution in hips and thighs), which may confer relative protection against certain metabolic disorders [25]. Behaviorally, substantial evidence indicates gender differences in healthcare utilization and health-seeking patterns. Women tend to engage more frequently with healthcare services and are more likely to report health concerns, potentially leading to earlier interventions for weight management [26]. Furthermore, sociocultural norms regarding body image and weight management differ between sexes. Women often experience greater social pressure regarding weight and appearance, which may motivate earlier adoption of weight control behaviors [27, 28]. These sex-specific variations have important implications for tailored interventions. For males, interventions should include metabolic risk assessments alongside visceral adiposity screening and approaches that address healthcare engagement barriers [29]. Female interventions should incorporate hormone-sensitive strategies across life stages, target stress-related eating patterns, and employ health-focused messaging that avoids negative body image reinforcement [30]. Gender-specific communication strategies in public health campaigns that avoid reinforcing harmful stereotypes while acknowledging biological differences may enhance the effectiveness of interventions for both populations.
Age-specific analysis demonstrated both death and DALY rates increase progressively with advancing age. This pattern aligns with the cumulative nature of metabolic damage associated with prolonged exposure to elevated BMI [31]. The absolute number of deaths and DALYs peaked in slightly younger age groups compared to rates, likely reflecting population distribution dynamics. For instance, DALYs peaked in the 65–69 age group for females and 60–64 for males, indicating that preventive interventions directed at middle-aged and early elderly populations could potentially yield substantial benefits in reducing overall disease burden. Notably, our study demonstrated that the proportion of disease burden attributable to high BMI (PAFs) peaks in the middle-aged adult groups (40–60 years) for several key conditions, including diabetes mellitus, ischemic heart disease, and hypertensive heart disease. This finding suggests that the relative impact of BMI on disease outcomes is highest during productive working years, resulting in considerable socioeconomic consequences beyond direct health costs [32]. From a life-course perspective, these age-specific patterns underscore the importance of early prevention efforts, as the health consequences of elevated BMI manifest most severely in later adulthood. However, the substantial burden observed in middle-aged populations indicates that interventions targeting this age group remain critical for reducing immediate health impacts. The challenge for public health systems is to implement balanced strategies that address both long-term prevention in younger populations and effective management in middle-aged and older adults already experiencing obesity-related complications [33].
Although cardiovascular diseases remain the major contributor to BMI-related deaths, diabetes and kidney diseases have now overtaken cardiovascular diseases as the leading cause of DALYs, accounting for 574.62 (95%UI 314.16, 807.45) DALYs per 100,000 individuals in 2021. This shift in the disease spectrum offers new insights for the prevention and management of obesity-related comorbidities. In recent years, drugs like GLP-1 receptor agonists have demonstrated effective weight reduction capabilities and significant improvements in glycemic control, with increasing evidence of their advantages in enhancing cardiovascular and renal function [34–36]. These features are particularly important for the comprehensive treatment of obesity and its comorbidities, with the potential to markedly curb the rising prevalence of diabetes and kidney disease induced by obesity. Although early prevention of obesity remains the most favored intervention among healthcare professionals, further advancements and improvements in related pharmacological options are still anticipated to provide a more comprehensive solution for obesity management. Additionally, the role of high BMI in neurological health, especially in cognitive decline, has gained attention in recent years [37, 38]. As Alzheimer’s disease and other dementias experienced a rise in both deaths (49.92%) and DALYs (53.64%) rates, we emphasize the significance of considering BMI in the prevention of dementia.
High-income regions like high-income Asia Pacific and Western Europe experienced significant declines in BMI-related deaths and DALYs, reflecting the success of public health strategies aimed at obesity reduction, such as restricting the marketing of unhealthy foods and beverages to children, increasing taxation on sugar-sweetened beverages, and implementing limitations on food marketing [39–41]. In contrast, lower-income regions like South Asia experienced the largest percentage increase in BMI-related deaths and DALYs, probably due to rapid economic transitions, urbanization, and changes in dietary patterns [42, 43]. Health inequities analysis indicated that the distribution of BMI-related burden across SDI levels has become less concentrated within specific population groups over time, and the situation is that the associated burden is gradually shifting from high-income regions to low- and middle-income regions. From a global perspective, these regional disparities underscore the urgent need for timely and effective intervention measures [44]. It is crucial to implement targeted public health policies that address the unique challenges faced by low- and middle-income countries, focusing on prevention like promoting healthier diets, early intervention, and access to healthcare resources to mitigate the escalating impact of obesity in these vulnerable regions [45, 46].
Frontier analysis allows for a more nuanced understanding of which countries are underperforming or overperforming in managing the health consequences of high BMI, providing a reference for high BMI health governance globally [19, 47]. By highlighting disparities in health outcomes related to high BMI, this analytical framework enables policymakers to identify specific areas for improvement and optimize health interventions tailored to the needs of different nations. For countries with lower SDI, those with minimal deviations from frontier rates should consider reducing their health economic investments in managing high BMI, as the situation is already well controlled, allowing public health resources to be redirected towards other pressing needs. Conversely, in high-SDI countries where substantial gaps still exist, it is advisable to increase health economic inputs to address the significant burden attributable to high BMI that persists. For countries exhibiting the largest gaps regardless of their SDI level, it is essential to intensify their efforts to manage high BMI more effectively, as the current interventions are insufficient to mitigate the associated health risks.
With the global aging population rapidly increasing, addressing the burden of obesity presents even greater challenges. Aging leads to changes in metabolism, decreased physical activity, and a higher prevalence of chronic diseases, all of which contribute to increased risks associated with obesity [48, 49]. This evolving demographic trend necessitates the implementation of targeted interventions to mitigate the growing impact of obesity among older adults. Effective measures should include the promotion of age-specific physical activity programs tailored to improve mobility and reduce obesity risk in older adults [48]. Nutritional guidance is also crucial, focusing on balanced, calorie-appropriate diets that meet the unique needs of the aging population while reducing excess body weight [50]. Furthermore, enhancing community support systems, such as accessible fitness centers and nutritional counseling, can encourage healthier lifestyles among the elderly [51]. Policymakers must prioritize these strategies to adapt healthcare infrastructure and public health policies to adequately address the challenges posed by the convergence of aging and obesity on a global scale.
Despite the strengths of this study, there are several limitations that should be acknowledged. First, the reliance on self-reported data in some regions may introduce bias and inaccuracies in BMI estimates. Second, although our study provides a comprehensive analysis of sex-specific trends, further research is needed to explore the underlying mechanisms driving these differences. Third, while we have used the ARIMA model to project future trends, these projections are based on historical data and assume that current trends will continue. However, future changes in health policies, economic conditions, and public health interventions could alter these trends. Finally, we did not assess the impact of specific interventions or policies on BMI-related health outcomes, which would be valuable for understanding what strategies are most effective in mitigating the burden of high BMI.
Building on the findings and limitations, we propose several research directions to enhance understanding of BMI-related disease patterns. First, investigating the interplay between specific risk factors and high BMI is crucial, particularly across varied socioeconomic contexts. Dietary patterns, physical activity, and environmental exposures influence BMI differently by region [52]. Swinburn et al. demonstrated that food environments and urbanization impact obesity rates with significant variation between high and low-income countries [53]. Second, genetic determinants of BMI require investigation across diverse populations. Recent research suggests genetic variations explain up to 50% of individual BMI differences [54]. Fesinmeyer et al. identified genetic polymorphisms more strongly associated with metabolic dysregulation in Europeans than Asians [55]. Integrating genetics with epidemiological data could inform precision interventions. Third, systematic evaluation of regional health policies is essential for understanding BMI-related disease management in resource-constrained settings. Okunogbe et al. found that obesity interventions’ cost-effectiveness varies significantly across healthcare systems [56]. Research should identify policy combinations that effectively mitigate BMI-related burden in specific contexts. Finally, longitudinal studies are needed to understand high BMI’s long-term impact as demographics evolve. Remais highlighted the synergistic interaction between infectious and non-communicable diseases in low- and middle-income countries, with obesity playing a central role [57]. Exploring these complex interactions could inform more comprehensive interventions.
Furthermore, it is also important to acknowledge the limitations of BMI as a predictive tool, especially for populations in the Global South. Research has demonstrated that BMI cutoffs established in Western populations inadequately reflect body composition and metabolic risk in different ethnic groups. Asian populations often exhibit higher visceral adiposity at lower BMI thresholds, while African populations demonstrate the opposite pattern [58–60]. For instance, Asian populations typically show increased cardiovascular and diabetes risk at BMI values considered normal by conventional standards, with metabolic complications manifesting at BMI levels of 22–25 kg/m² [61]. Conversely, studies suggest that BMI may overestimate health risks in African populations, who tend to have higher lean body mass and potentially different associations between adiposity and health outcomes compared to white populations [62, 63]. These variations in BMI-health relationships across ethnicities may influence the interpretation of our findings, particularly regarding the rapidly increasing burden observed in regions like South Asia and Central Sub-Saharan Africa. While our analysis provides insights into comparative trends across populations, the actual health impact in certain regions might be underestimated or mischaracterized when using standard BMI classifications. Future research should consider incorporating additional anthropometric measures such as waist circumference and waist-to-hip ratio, as well as region-specific BMI thresholds, to more accurately assess obesity-related health risks across diverse global populations [64].
Conclusions
The increasing prevalence of high BMI has resulted in significant health burdens over the past three decades, with cardiovascular diseases, diabetes and kidney diseases being the primary contributors. Low- and middle-income regions have been bearing a larger share of the burden. At the same time, the rapid aging of the population is exacerbating the challenges associated with managing obesity. Given these emerging trends, it is essential to develop more equitable and effective public health strategies for the prevention and management of the growing obesity epidemic in the future.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We highly appreciate the work by the GBD 2021 collaborators.
Abbreviations
- ARIMA
Autoregressive integrated moving average
- BMI
Body mass index
- CI
Confidence interval
- DALYs
Disability-adjusted life years
- GBD
Global burden of disease
- NCDs
Non-communicable diseases
- SDI
Socio-demographic index
- PAFs
Population attributable fractions
- UI
Uncertainty interval
Author contributions
Feng Xie and Fei Xiong: Contributed significantly to the conception and design of the study, performed initial statistical analysis, and contributed to the drafting of the manuscript. Jigui Chen, Hui Qin, Li Chen, and Tiantian Chen: Played a key role in the data analysis, and helped in revising the manuscript critically. Baoqin Yang, Zeng Yan, Yong Shen, and Shaihong Zhu: Provided expertise in the study’s methodology, contributed to the discussion section, and assisted in preparing figures and tables for the manuscript. Yongbiao Xu and Xulong Sun: Supervised the entire study, made substantial contributions to the conception and interpretation of the data, provided final approval of the manuscript for submission, and handled all correspondence related to the paper.
Funding
Not applicable.
Data availability
All data are accessible to the public at http://ghdx.healthdata.org/gbd-results-tool.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Feng Xie and Fei Xiong contributed equally to this work.
Yongbiao Xu and Xulong Sun also contributed equally to this work.
Contributor Information
Yongbiao Xu, Email: xuyongbiao2020@163.com.
Xulong Sun, Email: xulongsun.csu@foxmail.com.
References
- 1.Adolph TE, Tilg H. Western diets and chronic diseases. Nat Med. 30;2133–2147. 10.1038/s41591-024-03165-6. [DOI] [PubMed]
- 2.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass inde X among US adults, 1999–2010. JAMA.307:491–7. 10.1001/jama.2012.39 [DOI] [PubMed]
- 3.Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M, Naghavi M, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27. 10.1056/NEJMoa1614362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collaborators GBDRF. Global burden of 87 risk factors in 204 countries and territories, 199 0-2019: a systematic analysis for the global burden of disease study 2 019. Lancet (London England).396:1223–49. 10.1016/S0140-6736(20)30752-2 [DOI] [PMC free article] [PubMed]
- 5.Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP. The spread of the obesity epidemic in the united States, 1991–1998. JAMA.282:1519–22. 10.1001/jama.282.16.1519 [DOI] [PubMed]
- 6.Singh GM, Danaei G, Farzadfar F, Stevens GA, Woodward M, Wormser D, Kaptoge S, Whitlock G, Qiao Q, Lewington S, et al. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: a pooled analysis. PLoS ONE. 2013;8:e65174. 10.1371/journal.pone.0065174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, Ahmed M, Aksut B, Alam T, Alam K, et al. Global, regional, and National burden of cardiovascular diseases for 1 0 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70:1–25. 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Swinburn BA, Kraak VI, Allender S, Atkins VJ, Baker PI, Bogard JR, Brinsden H, Calvillo A, De Schutter O, Devarajan R, et al. The global syndemic of obesity, undernutrition, and climate change: the lancet commission report. Lancet. 2019;393:791–846. 10.1016/s0140-6736(18)32822-8. [DOI] [PubMed] [Google Scholar]
- 9.Hruby A, Hu FB. The epidemiology of obesity: A big picture. PharmacoEconomics.33:673–89. 10.1007/s40273-014-0243-x [DOI] [PMC free article] [PubMed]
- 10.Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, Grove JT, Hogan DR, Hogan MC, Horton R, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. 2016;388:e19–23. 10.1016/s0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
- 11.Global burden of. 288 Causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet. 2024;403:2100–32. 10.1016/s0140-6736(24)00367-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3. 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Global burden and strength of evidence for. 88 Risk factors in 204 countries and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet. 2024;403:2162–203. 10.1016/s0140-6736(24)00933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Global incidence. prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet. 2024. 10.1016/s0140-6736(24)00757-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, Dicker DJ, Chimed-Orchir O, Dandona R, Dandona L, et al. Global, regional, and National Cancer incidence, mortality, years of life lost, years lived with disability, and Disability-Adjusted life-years for 32 Cancer groups, 1990 to 2015: A systematic analysis for the global burden of disease study. JAMA Oncol. 2017;3:524–48. 10.1001/jamaoncol.2016.5688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu Z, Jiang Y, Yuan H, Fang Q, Cai N, Suo C, Jin L, Zhang T, Chen X. The trends in incidence of primary liver cancer caused by specific etiologies: results from the global burden of disease study 2016 and implications for liver cancer prevention. J Hepatol. 2019;70:674–83. 10.1016/j.jhep.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 17.Chevan A, Sutherland M. Revisiting Das Gupta: refinement and extension of standardization and decomposition. Demography. 2009;46:429–49. 10.1353/dem.0.0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wagstaff A, Paci P, van Doorslaer E. On the measurement of inequalities in health. Soc Sci Med. 1991;33:545–57. 10.1016/0277-9536(91)90212-u. [DOI] [PubMed] [Google Scholar]
- 19.Chen J, Cui Y, Deng Y, Xiang Y, Chen J, Wang Y, Wang T, He M. Global, regional, and National burden of cancers attributable to particulate matter pollution from 1990 to 2019 and projection to 2050: worsening or improving? J Hazard Mater. 2024;477:135319. 10.1016/j.jhazmat.2024.135319. [DOI] [PubMed] [Google Scholar]
- 20.Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. 10.1016/s0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed]
- 21.Dai H, Alsalhe TA, Chalghaf N, Riccò M, Bragazzi NL, Wu J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: an analysis of the global burden of disease study. PLoS Med. 2020;17:e1003198. 10.1371/journal.pmed.1003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Force USPST, Mangione CM, Barry MJ, Nicholson WK, Cabana M, Chelmow D, Coker TR, Davis EM, Donahue KE, Jaén CR et al. Statin use for the primary prevention of cardiovascular disease in Adu Lts: US preventive services task force recommendation statement. JAMA.328:746–53. 10.1001/jama.2022.13044 [DOI] [PubMed]
- 23.Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular dis ease: A report of the American college of cardiology/american heart as sociation task force on clinical practice guidelines. Circulation.140:e596–646. 10.1161/CIR.0000000000000678 [DOI] [PMC free article] [PubMed]
- 24.Kim S, Won CW. Sex-different changes of body composition in aging: a systemic review. Arch Gerontol Geriatr. 2022;102:104711. 10.1016/j.archger.2022.104711. [DOI] [PubMed] [Google Scholar]
- 25.Palmer BF, Clegg DJ. The sexual dimorphism of obesity. Mol Cell Endocrinol. 2015;402:113–9. 10.1016/j.mce.2014.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thompson AE, Anisimowicz Y, Miedema B, Hogg W, Wodchis WP, Aubrey-Bassler K. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract. 2016;17:38. 10.1186/s12875-016-0440-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boaz M, Navarro DA, Raz O, Kaufman-Shriqui V. Dietary changes and anxiety during the coronavirus pandemic: differenc Es between the sexes. Nutrients.13:4193. 10.3390/nu13124193 [DOI] [PMC free article] [PubMed]
- 28.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obes (Silver Spring). 2009;17:941–64. 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 29.Regitz-Zagrosek V, Lehmkuhl E, Weickert MO. Gender differences in the metabolic syndrome and their role for cardiovascular disease. Clin Res Cardiol. 2006;95:136–47. 10.1007/s00392-006-0351-5. [DOI] [PubMed] [Google Scholar]
- 30.Lovejoy JC, Champagne CM, de Jonge L, Xie H, Smith SR. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int J Obes (Lond). 2008;32:949–58. 10.1038/ijo.2008.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abdullah A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract. 2010;89:309–19. 10.1016/j.diabres.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 32.Goettler A, Grosse A, Sonntag D. Productivity loss due to overweight and obesity: a systematic review of indirect costs. BMJ Open. 2017;7:e014632. 10.1136/bmjopen-2016-014632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dietz WH, Baur LA, Hall K, Puhl RM, Taveras EM, Uauy R, Kopelman P. Management of obesity: improvement of health-care training and systems for prevention and care. Lancet. 2015;385:2521–33. 10.1016/s0140-6736(14)61748-7. [DOI] [PubMed] [Google Scholar]
- 34.Yao H, Zhang A, Li D, Wu Y, Wang C-Z, Wan J-Y, Yuan C-S. Comparative effectiveness of GLP-1 receptor agonists on glycaemic Cont Rol, body weight, and lipid profile for type 2 diabetes: systematic re view and network meta-analysis. BMJ (Clinical Res ed).384:e076410. 10.1136/bmj-2023-076410 [DOI] [PMC free article] [PubMed]
- 35.Alkhezi OS, Alahmed AA, Alfayez OM, Alzuman OA, Almutairi AR, Almohammed OA. Comparative effectiveness of glucagon-like peptide-1 receptor agonists for the management of obesity in adults without diabetes: A network m eta-analysis of randomized clinical trials. Obes Reviews: Official J Int Association Study Obes.24:e13543. 10.1111/obr.13543 [DOI] [PubMed]
- 36.Apperloo EM, Neuen BL, Fletcher RA, Jongs N, Anker SD, Bhatt DL, Butler J, Cherney DZI, Herrington WG, Inzucchi SE et al. Efficacy and safety of SGLT2 inhibitors with and without glucagon-like peptide 1 receptor agonists: a SMART-C collaborative meta-analysis of randomised controlled trials. Lancet Diabetes Endocrinol.12:545–57. 10.1016/S2213-8587(24)00155-4 [DOI] [PubMed]
- 37.Whitmer RA, Gunderson EP, Barrett-Connor E, Quesenberry CP Jr., Yaffe K. Obesity in middle age and future risk of dementia: a 27 year longitudinal population based study. BMJ. 2005;330:1360. 10.1136/bmj.38446.466238.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Singh-Manoux A, Dugravot A, Shipley M, Brunner EJ, Elbaz A, Sabia S, Kivimaki M. Obesity trajectories and risk of dementia: 28 years of follow-up in the Whitehall II study. Alzheimers Dement. 2018;14:178–86. 10.1016/j.jalz.2017.06.2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wickramasinghe K, Chatterjee S, Williams J, Weber MW, Rito AI, Rippin H, Breda J. Childhood overweight and obesity abatement policies in Europe. Obes Reviews: Official J Int Association Study Obes.22 Suppl 6:e13300. 10.1111/obr.13300 [DOI] [PubMed]
- 40.Choi SK, Frongillo EA, Blake CE, Thrasher JF. Food availability in school stores in Seoul, South Korea after impleme Ntation of Food- and Nutrient-Based policies. J Sch Health.87:498–505. 10.1111/josh.12518 [DOI] [PubMed]
- 41.Taillie LS, Bercholz M, Popkin B, Rebolledo N, Reyes M, Corvalán C. Decreases in purchases of energy, sodium, sugar, and saturated fat 3 y ears after implementation of the Chilean food labeling and marketing L Aw: an interrupted time series analysis. PLoS Med.21:e1004463. 10.1371/journal.pmed.1004463 [DOI] [PMC free article] [PubMed]
- 42.Misra A, Jayawardena R, Anoop S. Obesity in South Asia: phenotype, morbidities, and mitigation. Curr Obes Rep.8:43–52. 10.1007/s13679-019-0328-0 [DOI] [PubMed]
- 43.Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, Li X, Wang L, Wang L, Liu Y, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2019;394:1145–58. 10.1016/s0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Okunogbe A, Nugent R, Spencer G, Powis J, Ralston J, Wilding J. Economic impacts of overweight and obesity: current and future Estimat Es for 161 countries. BMJ Glob Health.7:e009773. 10.1136/bmjgh-2022-009773 [DOI] [PMC free article] [PubMed]
- 45.McKinnon RA, Orleans CT, Kumanyika SK, Haire-Joshu D, Krebs-Smith SM, Finkelstein EA, Brownell KD, Thompson JW, Ballard-Barbash R. Considerations for an obesity policy research agenda. Am J Prev Med. 2009;36:351–7. 10.1016/j.amepre.2008.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Clarke B, Swinburn B, Sacks G. The application of theories of the policy process to obesity prevention: a systematic review and meta-synthesis. BMC Public Health. 2016;16:1084. 10.1186/s12889-016-3639-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cao F, Xu Z, Li XX, Fu ZY, Han RY, Zhang JL, Wang P, Hou S, Pan HF. Trends and cross-country inequalities in the global burden of osteoarthritis, 1990–2019: A population-based study. Ageing Res Rev. 2024;99:102382. 10.1016/j.arr.2024.102382. [DOI] [PubMed] [Google Scholar]
- 48.McPhee JS, French DP, Jackson D, Nazroo J, Pendleton N, Degens H. Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology.17:567–80. 10.1007/s10522-016-9641-0 [DOI] [PMC free article] [PubMed]
- 49.Evans WJ. Exercise, nutrition, and aging. Clin Geriatr Med.11:725–34. [PubMed]
- 50.Yeung SSY, Kwan M, Woo J. Healthy diet for healthy aging. Nutrients.13:4310. 10.3390/nu13124310 [DOI] [PMC free article] [PubMed]
- 51.Thatcher RM. Community support. Promoting health and self-care. Nurs Clin North Am.24:725–31. [PubMed]
- 52.Worldwide trends in underweight and obesity. From 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet. 2024;403:1027–50. 10.1016/s0140-6736(23)02750-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker SL. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378:804–14. 10.1016/s0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- 54.Bouchard C. Genetics of obesity: what we have learned over decades of research. Obes (Silver Spring). 2021;29:802–20. 10.1002/oby.23116. [DOI] [PubMed] [Google Scholar]
- 55.Fesinmeyer MD, North KE, Ritchie MD, Lim U, Franceschini N, Wilkens LR, Gross MD, Bůžková P, Glenn K, Quibrera PM, et al. Genetic risk factors for BMI and obesity in an ethnically diverse population: results from the population architecture using genomics and epidemiology (PAGE) study. Obes (Silver Spring). 2013;21:835–46. 10.1002/oby.20268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Okunogbe A, Nugent R, Spencer G, Ralston J, Wilding J. Economic impacts of overweight and obesity: current and future estimates for eight countries. BMJ Glob Health. 2021;6. 10.1136/bmjgh-2021-006351. [DOI] [PMC free article] [PubMed]
- 57.Remais JV, Zeng G, Li G, Tian L, Engelgau MM. Convergence of non-communicable and infectious diseases in low- and middle-income countries. Int J Epidemiol. 2013;42:221–7. 10.1093/ije/dys135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002;3:141–6. 10.1046/j.1467-789x.2002.00065.x. [DOI] [PubMed] [Google Scholar]
- 59.Lear SA, Humphries KH, Kohli S, Chockalingam A, Frohlich JJ, Birmingham CL. Visceral adipose tissue accumulation differs according to ethnic background: results of the multicultural community health assessment trial (M-CHAT). Am J Clin Nutr. 2007;86:353–9. 10.1093/ajcn/86.2.353. [DOI] [PubMed] [Google Scholar]
- 60.Camhi SM, Bray GA, Bouchard C, Greenway FL, Johnson WD, Newton RL, Ravussin E, Ryan DH, Smith SR, Katzmarzyk PT. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: sex and race differences. Obes (Silver Spring). 2011;19:402–8. 10.1038/oby.2010.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Appropriate body-mass index. For Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. 10.1016/s0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 62.Heymsfield SB, Peterson CM, Thomas DM, Heo M, Schuna JM. Jr. Why are there Race/ethnic differences in adult body mass index-adiposity relationships? A quantitative critical review. Obes Rev. 2016;17:262–75. 10.1111/obr.12358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sumner AE, Micklesfield LK, Ricks M, Tambay AV, Avila NA, Thomas F, Lambert EV, Levitt NS, Evans J, Rotimi CN, et al. Waist circumference, BMI, and visceral adipose tissue in white women and women of African descent. Obes (Silver Spring). 2011;19:671–4. 10.1038/oby.2010.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Huxley R, James WP, Barzi F, Patel JV, Lear SA, Suriyawongpaisal P, Janus E, Caterson I, Zimmet P, Prabhakaran D, et al. Ethnic comparisons of the cross-sectional relationships between measures of body size with diabetes and hypertension. Obes Rev. 2008;9(Suppl 1):53–61. 10.1111/j.1467-789X.2007.00439.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are accessible to the public at http://ghdx.healthdata.org/gbd-results-tool.