Abstract
Background
Inheritance patterns show familial clustering of gastrointestinal cancers, and multiple germline conditions have now been identified that predispose to colorectal, gastric, and pancreatic cancers.
Methods
A narrative review based on recent relevant literature was conducted.
Results
Lynch syndrome, formerly known as hereditary non-polyposis colorectal cancer, increases the risk of several abdominal cancers, with the highest population prevalence. Familial adenomatous polyposis and some of the more infrequent polyposis syndromes have distinct characteristics affecting various organ-specific cancer risks. Hereditary gastric and pancreatic cancer syndromes include those also causing colorectal cancer, while additional genetic disorders predisposing only to upper gastrointestinal malignancies have been recognized more recently. Diagnosing and managing hereditary cancer syndromes requires multidisciplinary expertise and may be best managed in tertiary centres, with a need to consider patient preference and ensure shared decision-making.
Conclusion
Several germline conditions predispose to colorectal, gastric, and pancreatic cancer, which inform identification, surveillance regimens, prevention, cascade screening, counselling, and surgical management. The authors describe developments in the hereditary origin of colorectal, gastric, and pancreatic cancer with current recommendations in surveillance and surgical management.
Hereditary gastrointestinal cancers are under-diagnosed and require attention for identification and differential diagnostics with easy access to germline genetic evaluation to confirm the diagnosis. Awareness of multiple predisposing conditions to cancers in various organs, also outside the gastrointestinal tract, is imperative in identification and prompting surveillance and management according to condition-specific clinical guidelines available.
Introduction
Hereditary cancer refers to an increased probability of developing a malignant tumour due to an inherited genetic defect, polygenic risk, epigenetic factor, or otherwise unknown trait. Germline genetic predispositions can increase the risk of multiple different cancer types in various organs, often at relative early onset, causing a syndromic phenotype with distinct features. Sometimes a genotype–phenotype correlation is less evident, and only systematic tumour and germline testing may identify a hereditary condition. Hereditary cancers caused by germline defects often result in particular molecular alterations that open opportunities for precision medicine by targeted therapies1. Effective cascade testing of relatives should be used as an adjunct to systematic tumour and genetic testing and may improve outcome through surveillance and preventive measures2.
If the risk-modifying factor in a phenotypically high-risk family remains unidentified, the high familial risk may warrant increased surveillance and continued research to identify the responsible genetic factor. Clinical phenotypes have been used to create diagnostic criteria, but the studies the criteria are based on have often been influenced by ascertainment bias, that is returning the inclusion criteria as results of the work.
The most well-known gastrointestinal manifestations of inherited cancer syndromes relate to a high risk of colorectal cancer (CRC), such as Lynch syndrome (LS) and familial adenomatous polyposis (FAP). Both of these are associated with an increased risk of extra-colorectal malignancies, such as biliary tract and pancreatic in LS3, and gastric and small bowel cancers in both3–5. Hereditary diffuse gastric cancer (caused by for example CDH1) and hereditary pancreatic cancer (caused by for example BRCA1/2) have been defined more recently based on identification of gene defects in high-risk phenotype families. The availability and uptake of whole genome sequencing and broad genotyping panels has resulted in the identification of novel genetic associations (for example common low-penetrance alleles that confer a small increased risk), for which surveillance and management guidelines have not yet been developed.
This narrative review aims to summarize the latest guidance on identification, surveillance, and management of the most clinically relevant hereditary cancer syndromes relating to gastrointestinal cancer. Whilst some gene defects may result in cancers at multiple sites, the current review is structured by site for clarity and limited to syndromes predisposing to CRC, gastric cancer, or pancreatic cancer.
Hereditary colorectal cancer
About 20–30 per cent of CRCs have a hereditary component6. Hereditary CRC risk refers to previously diagnosed cancers in first-degree relatives (FDRs) of the proband in question. Where one or more FDRs are affected, the proband has a family history of CRC categorized as average, moderate, or high based on the number of FDRs affected and age of onset7. High familial risk is likely to represent a known or as yet unidentified genetic predisposition to risk of cancer, and may be managed according to respective gene-specific guidelines. In large studies based on systematic next-generation sequencing (NGS) germline testing for cancer susceptibility variants, germline pathogenic variants have been diagnosed in over 7 per cent of all CRCs8,9.
Family history of colorectal cancer
High CRC risk is assigned to probands with a cluster of at least three FDRs with CRC at any age in at least two generations, fulfilling the Amsterdam criteria10 for a high risk of a hereditary condition, but in which no underlying germline variant has been identified. The moderate-risk category includes probands with one FDR diagnosed at early onset, that is before 50 years of age, or two FDRs in the same kinship at any given age. Probands with no family history, or family history not fulfilling criteria for moderate or high risk are considered to be at average risk7. Whilst the presence of adenomas in FDRs does not generally indicate an increased risk in the proband, significant polyp load may indicate a multiple colorectal adenoma (MCRA) phenotype (10 or more adenomas but no constitutional variant detected) and stimulate increased surveillance.
The lifetime incidence of CRC is increased two- to six-fold in moderate- or high-risk probands compared with the general population11. Testing for deficient mismatch repair (dMMR) or microsatellite instability (MSI) in the affected family member’s previously resected tumours should be pursued to identify possible LS or other predisposing syndromes. Probands in the moderate- or high-risk category or those with an already identified familial or personal history of dMMR or polyposis should be referred to a specialist service for surveillance. Average-risk individuals may be managed in primary care with screening programmes targeting the general population. Early-onset CRC (eoCRC) denotes those diagnosed with a CRC before 50 years of age, and distinct guidelines exist for their risk and therapeutic management outside the scope of hereditary conditions caused by pathogenic germline variants that are found in about 13 per cent of those with eoCRC12,13.
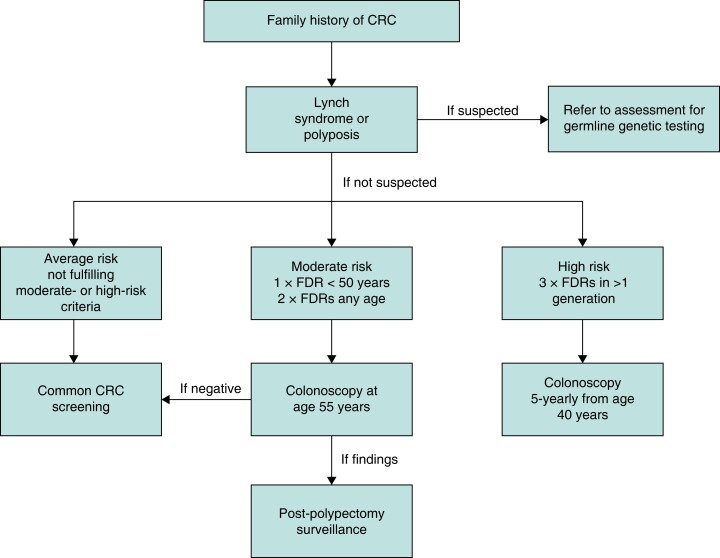
Probands with a moderate familial CRC risk should have a one-off colonoscopy at 55 years of age, while those with a high risk should undergo a 5-yearly colonoscopy from 40 to 75 years of age7, or at an age 5–10 years before the earliest CRC case in the family14–16. A screening and surveillance guidance for familial CRC risk is outlined in Fig. 1, adapted from British Society of Gastroenterology (BSG) guidance7.
Fig. 1.
Surveillance recommendations for individuals with a family history of CRC
CRC, colorectal cancer; FDR, first-degree relative. Modified from British Society of Gastroenterology recommendations7.
Lynch syndrome
LS is the most prevalent predisposing germline condition for hereditary CRC, and is caused by pathogenic germline variants in one of the mismatch repair (MMR) genes (MLH1, MSH2, MSH6, or PMS2) or epigenetic silencing of MSH2. It was first named as cancer family syndrome17, and later denoted as hereditary non-polyposis CRC (HNPCC), until named in 2003 after Dr Henry T. Lynch18.
Epidemiology
Pathogenic (PV) and likely pathogenic (LPV) MMR germline variant alleles are estimated to have a prevalence of up to 1 : 226 in the general population19, but estimates as high as 1 : 125 have been proposed20. An autosomal dominant pattern of inheritance has been demonstrated with the presence of one allele of PV/LPV adequate to cause the phenotype, which will itself vary by gene involved. Homozygous carriership or the presence of two separate germline MMR PV/LPVs results in the rare phenotype of constitutional mismatch repair deficiency (CMMRD), which predisposes to high childhood and adolescence incidence of various cancers with a dMMR phenotype. LS-associated heterozygous PV/LPVs are considered to result in 3–5 per cent of all CRC21.
Penetrance and expressivity
Most historical estimates of penetrance, that is the lifetime cancer risk, have been based on identifying a familial inheritance pattern. Such selection based on phenotype is at risk of ascertainment bias, leading to overestimation. In estimates based on historical segregation analysis, MLH1 and MSH2 are quoted to have a lifetime incidence of any cancer of up to 80–90 per cent without risk-reducing surveillance, whereas MSH6 and PMS2 have been linked with more moderate 40–60 per cent penetrance. Risk of CRC has been retrospectively estimated to be 40–50 per cent for MLH1 and MSH2, and 10–20 per cent for MSH6 and PMS222,23.
Risk estimates from 2015 onwards have been largely based on prospective observational data generated by the Prospective Lynch Syndrome Database (PLSD)24, an international open initiative gathering registry data from specialized LS centres throughout the Western countries and Australia. Inclusion criteria for the PLSD have been a planned surveillance colonoscopy without cancer for individual PV/LPV carriers, which differs from the previous estimates of tracing families back in their cancer history, and therefore rather reflects the cancer risks under surveillance contact to healthcare than true penetrance. The PLSD quotes overall cancer incidence from 25 to 75 years of age up to 75–85 per cent for MLH1 and MSH2, 42–62 per cent for MSH6, and 34 per cent for PMS2 depending on gender3,25. These estimates are derived from 6350 LS carriers under surveillance for a total of 71 000 follow-up years, and can be seen at the interactive website www.plsd.eu. Of course, these figures may not represent the natural course of LS given interventions, namely polypectomy, which LS carriers might undergo as a result of surveillance colonoscopy. Lifetime cumulative incidence of CRC between 25 and 75 years of age is 48–57 per cent for MLH1, 47–51 per cent for MSH2, 18–20 per cent for MSH6, and 10 per cent for PMS2 depending on gender25.
As a general notion to CRC occurrence, MLH1 and MSH2 are high-penetrance genes, MSH6 is of moderate penetrance, and PMS2 is a low-penetrance gene. The risk of cancer varies substantially based on gene and gender and so management should reflect this, rather than treating LS as one general entity26. Emerging evidence indicates that CRC risk varies between LS carriers with the same gene variant, suggesting modifiers of risk such as polygenic or epigenetic, immunological, or environmental factors27.
Carcinogenesis
At the molecular level of LS-associated dMMR cancer development, a constitutionally pathogenic, inherited, germline allele of an MMR gene, present in every cell, is followed by the loss of heterozygosity (LOH), that is loss of function of the second allele in the cell starting the cancer. The LOH results in a reduced capacity to produce a functional MMR protein, which impairs the function of the MMR complex. As the name suggests, MMR deficiency leads to the inability of the cell to correct nucleotide mismatches during DNA replication, which in turn causes accumulation of such mismatches throughout the cell’s genome28. This is observed as an increased abundance of mono-, bi- and multi-nucleotide repetitive sequences that occur randomly, but which may also frequently occur at non-random genomic positions, which can be detected as the genomic hallmark, microsatellites. Accumulation of microsatellite errors is denoted as MSI. Moreover, the mono- and di-nucleotide repeats cause a genomic frameshift that disrupts following sequences, which leads to a dysfunctional end product, that is a truncated protein29. MSI cells typically remain chromosomally stable, but possess a hypermutated phenotype that is prone to be captured by the immune response. However, when mutations occur within a tumour suppressor or oncogenes, carcinogenesis is initiated by accumulating necessary functional advantages to the developing cancer cell, facilitating immune escape and commencement of neoplasia formation when no longer eradicated or detained by the host immune response30,31.
CRC in general is considered to follow an adenoma-carcinoma sequence32, which may be modulated by screening and secondary prevention by removing precursor lesions (adenomas) via colonoscopy and polypectomy. In LS, efforts to prevent CRC by endoscopy have not been as successful, with incident cancers often diagnosed in-between regular surveillance colonoscopies33,34, a phenomenon that has resulted in significant research and hypotheses relating to carcinogenetic processes leading to dMMR CRC30,35.
It is unquestionable that dMMR CRC develops rapidly36, even between yearly or 3-yearly colonoscopies33,37. The adenoma-carcinoma sequence may be accelerated, and there is even debate that the precursor adenoma, which should be endoscopically detectable, may be skipped30,38. Nevertheless, normal-looking colorectal mucosa of random, previously healthy, MMR PV carriers has been demonstrated to contain multiple crypts that have lost their ability for MMR, and it is debated whether these dMMR crypt foci are precursors to manifest neoplasia39. In addition, the normal mucosa of healthy MMR PV/LPV carriers has been shown to contain an increased average abundance of CD3-, CD8-, and FOXP3-positive immune cells40 compared with LS cancer patients and proficient MMR cancer patients, and that time to CRC development is correlated to the relative abundance of these immune cells41.
Subsequent somatic events of cancer cells differ by the germline MMR gene background in developing CRCs. MLH1-deficient CRCs are more often CTNNB1 (β-catenin) mutated and not APC mutated, whereas MSH2-associated CRCs almost always have APC mutations responsible for Wnt up-regulation37. In PMS2-deficient cancers and adenomas, it has been shown that the KRAS mutations take place earlier in the course of development than dMMR, which may indicate that MMR deficiency does not drive the carcinogenesis in PMS2-associated CRC42–44.
Clinical presentation
Pathogenic MMR germline variants predispose to an increased lifetime incidence of both gastrointestinal and extra-intestinal cancer. The cancer spectrum in LS includes at least increased risk of CRC, endometrial, ovarian, duodenal and small bowel, biliary tract, pancreatic, gastric, upper urothelial, bladder, prostate, skin, and brain cancers, as well as some sarcomas25,45. Some cancers are more associated with specific genes, such as urothelial, prostate, and brain cancers, which are closely linked to MSH2 variants3. CRCs and endometrial cancers are detected in carriers of all four genes, yet with different ages of average onset.
The risk of CRC increases rapidly from 25 years of age onwards in MLH1 and MSH2, causing early onset of CRC with a median age of 45–50 years. Onset of CRC is later for MSH6, with few or no cancers detected before 30–35 years of age, and the risk of CRC in PMS2 PV carriers before 50 years of age is negligible if undergoing active colonoscopy surveillance25,46. Colonoscopy may reduce the CRC risk in MSH6 and PMS2 genotypes more than it does in MLH1 and MSH2 due to less frequent involvement of the dMMR crypt foci pathway. The risk of synchronous tumours in the colorectum but also in other organs is increased47, and identifying metachronous cancers by evaluating the entire colorectum and gynaecological organs before therapy or surgical management is important, and may affect decision-making.
The cumulative risk of adenomas and advanced adenomas in MSH2 carriers is higher than in MLH1 carriers under colonoscopy surveillance, whereas there is no difference in the cumulative incidence of CRC between the two37. LS-associated CRCs are more likely to appear first in the right hemicolon for reasons that remain unclear. They present more often with a mucinous component, dense immune infiltrates, and morphological intratumoral heterogeneity28.
Identification of Lynch syndrome
The Amsterdam criteria were developed to identify individuals and families in which to study genetic predisposition, and were later updated as Amsterdam II and Bethesda criteria10,48. While the criteria were never meant as a tool for ascertainment of individuals for clinical genetic testing, they have since been used for that purpose. Over two decades ago, universal tumour screening by MMR immunohistochemistry or MSI testing by PCR was recommended for all new CRCs49, and implemented into clinical guidelines50. Diagnosing dMMR/MSI has now gained direct therapeutic relevance with the use of immune checkpoint inhibitors (CPI) to treat metastatic dMMR/MSI solid cancers51,52. In cases where MSI or the loss of protein staining of MLH1, MSH2, MSH6 and/or PMS2 is detected, germline testing is warranted to confirm or rule out constitutional pathogenic variants in these genes underlying the molecular phenotype. If MLH1 staining is deficient, the presence of BRAF V600E in testing by immunohistochemistry (IHC) protein staining, PCR, or sequencing, or the hypermethylation of MLH1 with pyrosequencing effectively rules out MLH1 constitutional variants and therefore excludes LS without genetic germline testing53. Families fulfilling the Amsterdam criteria but with the phenotype containing proficient MMR CRCs have been denoted as familial CRC type X, with various candidate genes, and some of these cases have been proposed to harbour for example RPS20 pathogenic germline variants.
IHC staining of MMR can be successfully performed from endoscopic preoperative biopsies without compromising the quality of the staining54. Meanwhile, novel germline testing pipelines may be able to return panel NGS results in 2–3 weeks, facilitating the diagnosis of LS in CRC before surgery. A preoperative LS diagnosis has implications for surgical decision-making; however, the diagnosis cannot be based solely on the MMR/MSI status, but requires a demonstrated pathogenic variant to confirm the diagnosis55.
Surgery
LS patients treated for CRC have a substantially high risk of metachronous CRC56–59. If diagnosed before surgery, MLH1 and MSH2 carriers with a colonic cancer should be considered for a subtotal colectomy with ileosigmoid or ileorectal anastomosis, to reduce the risk of metachronous colon cancer55,60. Extended surgery for MSH6 and PMS2 carriers is not currently recommended due to a lower risk of metachronous CRC55. Standard oncological pretherapy and rectal resection based on local advancement is recommended for rectal cancer as the first CRC in LS carriers, and total proctocolectomy is currently not recommended in this situation55. Stand-alone prophylactic procedures solely for risk, without existing neoplasia as an indication, for example prophylactic colectomy, are not currently recommended due to incomplete penetrance and substantial variation in the risk imparted by different genes and variants27,55,61.
Anti-cancer therapy
Although dMMR CRCs are associated with a lower risk of lymph node metastases, adjuvant oncological therapy is recommended when such spread occurs, yet may be less responsive to 5-fluorouracil-based chemotherapy62,63. Immunotherapy for metastatic CRC with dMMR or MSI using CPI targeting CTLA4 and the PD1/PD-L1 axis results in greater complete and partial clinical response rates, with long-term disease control52,64. CPI therapy is now considered as the first-line management of metastatic or unresectable CRC with dMMR/MSI65. Meanwhile, in 2022, studies of CPI in non-metastatic and resectable CRC were published, with very promising results that may represent a paradigm shift in practice for LS-associated CRC66. In a single-institution phase II trial of 16 participants with dMMR rectal cancer, patients were assigned to the CPI agent dostarlimab for 6 months before chemoradiotherapy and surgery. The first 12 patients on the protocol, with many cases of locally advanced tumours, all exhibited a complete clinical response as measured by clinical imaging, rectal examination, and endoscopy, resulting in a watch-and-wait approach without the need for chemoradiotherapy and surgery66. Similar results are reported for dMMR colon cancer67, with 95 per cent of the patients treated with CPI before surgery exhibiting a complete or near-complete pathological response68.
Surveillance
The standard of care for individuals with pathogenic MMR germline variants is to offer regular endoscopic surveillance by colonoscopy with polypectomy and early detection of possible incident CRC. Efficacy of colonoscopy surveillance to prevent CRC was demonstrated in a non-randomized study of individuals who opted for surveillance versus those that did not69,70. Mortality rate from CRC was reduced in those undergoing colonoscopy surveillance, with CRC incidence reduced by 65 per cent in those undergoing surveillance colonoscopies every 3–5 years. Importantly, selection and lead-time bias exist given the non-randomized design.
Colonoscopy surveillance should be initiated at 25 years of age for carriers of MLH1 and MSH2 and at 35 years of age for MSH6 and PMS255. The optimal interval of colonoscopies is debated, with recommendations of between 1-yearly and 3-yearly colonoscopies, given that differences in stage, survival, or CRC incidence have not been demonstrated between 1-, 2- and 3-yearly colonoscopy regimens, or the interval since the previous colonoscopy before incident CRC33,71,72. LS patients with previous CRCs are assumed to have additional modifiers of cancer risk56, and should undergo shorter postoperative intervals between surveillance colonoscopies. In a recent cost-effectiveness study, strategies with a 3-yearly colonoscopy interval were favoured to gain most life-years saved73.
Recent epidemiological studies have shown that the incidence of CRC remains high even under colonoscopy surveillance34, but the overall survival after prospectively observed incident CRCs is good, close to 90 per cent after 10 years25,33,74.
Chemoprevention
In a randomized placebo-controlled study ‘CaPP2’, enteric coated acetylsalicylic acid (ASA) of 600 mg per day for 2–4 years was shown to reduce the incidence of CRC in LS carriers by half, reflecting the trends in general population-based studies on ASA use75,76. There was no statistically significant increase in adverse effects with ASA although the study population was primarily middle-aged or younger. The preventive effect of ASA on CRC was observed 4 years after the therapy, and the incidence reduction was maintained for 10–20 years in follow-up. The number needed to treat with 2 years of ASA to prevent one CRC in LS was 2577.
Familial adenomatous polyposis
FAP is the second most common germline predisposition to CRC with a distinct polyposis phenotype in classical presentation. It was first described in the literature in 1859, long before the role of the adenomatous polyposis coli gene (APC) was identified in 1991.
Epidemiology
The prevalence of FAP is estimated to be between 1 : 8000 and 1 : 18 000 in the general population, accounting for approximately 1 per cent of all CRCs78,79. In the presence of a multiple adenoma phenotype, the probability of APC pathogenic variants is associated with the number of adenomas80.
Penetrance
Classical FAP is a condition of full penetrance in APC pathogenic variant carriers and a gross polyposis phenotype with a 100 per cent risk of CRC, in almost all cases by 40 years of age81. The genomic position of the pathogenic germline variant results in variable penetrance, with an attenuated phenotype (aFAP) caused by variants located in codons less than 157 or greater than 1595, or alternatively spliced ninth exon. Intermediate phenotypes are caused by variants in codons 157–1249 and 1464–1595, excluding alternatively spliced ninth exon. Classical severe phenotypes are associated with variants in codons 1250–1464 and large deletions in the APC gene82. Milder phenotypes attributed to aFAP have a CRC risk of 70 per cent by 80 years of age, with the mean age of CRC onset at approximately 30 years83.
Carcinogenesis
The APC gene is located on chromosome 5q21, and has been termed the ‘gatekeeper’ tumour suppressor gene for CRC. Somatic APC mutations are frequently observed in sporadic CRC. Neoplasia in FAP follows the traditional adenoma-carcinoma sequence and so FAP has served as a model for conventional colorectal carcinogenesis. In FAP, neoplasia is initiated when the germline APC variant develops a second hit or LOH. The APC mutation disturbs the Wnt signalling pathway by leading to the cytoplasmic accumulation of β-catenin due to reduced degradation in crypt cells. APC also promotes defects in chromosome segregation fidelity, leading to increased aneuploidy and LOH in other genes84.
Clinical presentation
Polyposis is defined as greater than 10 cumulative adenomas detected in the colon or rectum, a definition that is sensitive but not specific to FAP. In classical FAP, the number of adenomatous polyps is substantially higher with hundreds or even thousands of adenomas present at a young age, while in aFAP less than 100 adenomas with later onset of CRC is observed. Additional distinction can also be made based on the family history. Approximately 30 per cent of those presenting with FAP have no family history of polyposis. Inheritance of APC pathogenic variants is, however, autosomal dominant. Additionally, desmoid tumours are a major source of morbidity rate and mortality rate in FAP after CRC, and cluster within families with variants in codon 1400 or to a lesser extent in codons 401–1400.
Identification
A personal or familial polyposis phenotype should instigate genetic testing in the proband and FDRs. As polyposis is a heterogenous clinical condition, multigene panel germline NGS including at least APC, MUTYH, BMPR1A, EPCAM, MLH1, MSH2, MSH6, PMS2, POLD1, POLE, PTEN, SMAD4, STK11, and TP53 should be applied. Differential diagnoses also include more infrequent causes of polyposis, and a wider panel of genes associated with rare polyposis may be applied with AXIN2, GREM1, MLH3, MSH3, MBD4, NTHL1, RNF43, and RPS20 included.
Surgery
Timing of prophylactic surgery to prevent CRC is the most relevant question in FAP. Symptoms and CRC are absolute indications for surgery. Colectomy in asymptomatic FAP carriers is indicated when the adenoma burden is no longer manageable by endoscopy or increases rapidly, when large polyps of >10 mm become frequent, or when high-grade dysplasia is identified85. It is usually appropriate to postpone surgery until the patients are physically and emotionally mature enough86,87.
The main options for surgery are restorative total proctocolectomy with ileal pouch-anal anastomosis (PC + IPAA) and total abdominal colectomy with ileorectal anastomosis (TC + IRA). Patients with less than 20 polyps in the rectum and less than 500 polyps in the colon are candidates for TC + IRA. However, patients with a PV between APC codons 1309 and 1328 are considered at high risk of more severe polyposis, and are usually considered for PC. Desmoid risk has implications for the timing of surgery as patients at high risk due to a pathogenic variant genomic position may benefit from postponing surgery to a later age. In aFAP phenotypes, the penetrance is less pronounced, and endoscopic management may be effective until later in life, for example 30–40 years of age.
Surveillance
Yearly colonoscopies are recommended from 15 years of age or from the time of diagnosis (if later) until surgery, after which the surveillance intervals may be relaxed depending on the phenotype and type of resection. If TC + IRA has been performed, the surveillance of the rectum is continued yearly.
Chemoprevention
Several chemoprevention agents have been tested in FAP to reduce the adenoma burden, yet none has provided a sustained response and shown tolerability over a long interval of time. In a placebo-controlled trial, 6 months of celecoxib therapy reduced the number of polyps by 28 per cent compared with placebo of 4.5 per cent at 12 months88. Rofecoxib, sulindac, difluoromethylornithine, and ASA have also been studied in randomized (placebo) controlled trials, without clear efficacy in preventing disease progression requiring surgical intervention89.
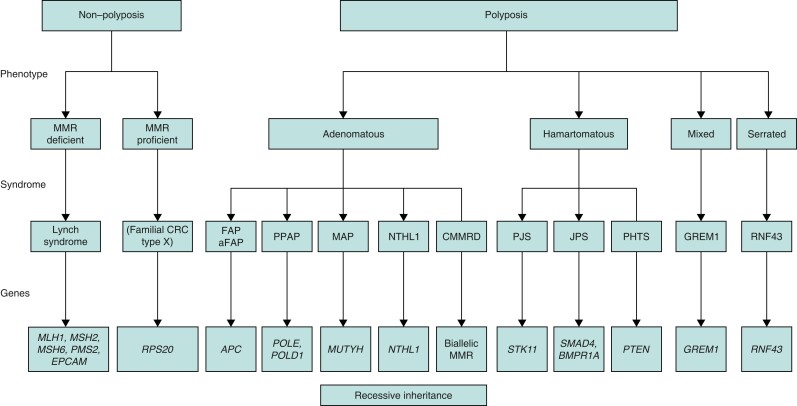
Other polyposis syndromes
Numerous rare polyposis syndromes have been identified with variant confirmation required to guide management. Rarer polyposis syndromes may present with adenomatous, hamartomatous, serrated, and mixed polyposes depending on the genes involved. A simplified schematic classification of CRC predisposing germline disorders is outlined in Fig. 2 according to Daca Alvarez et al.13 and Valle et al.90.
Fig. 2.
Classification of CRC syndromes
MMR, mismatch repair; CRC, colorectal cancer; FAP, familial adenomatous polyposis; aFAP, attenuated familial adenomatous polyposis; PPAP, POLE/POLD1- associated polyposis; MAP, MUTYH-associated polyposis; CMMRD, constitutional mismatch repair deficiency; PJS, Peutz–Jeghers syndrome; JPS, juvenile polyposis syndrome; PHTS, PTEN hamartoma tumour syndrome. Modified from Daca Alvarez et al.13 and Valle et al.90
MUTYH-associated polyposis
MUTYH-associated polyposis (MAP) is a recessively inherited disorder associated with less than 1 per cent of CRCs91. MUTYH is a base excision repair gene on chromosome 1, and, when both alleles are affected, this leads to G → T transversions in somatic genes relevant to CRC carcinogenesis92. CRC lifetime incidence of 80–90 per cent without surveillance and 48 per cent under surveillance for the biallelic MUTYH germline defect have been reported93. Increased risk of CRC in monoallelic germline carriers of MUTYH is debated. The clinical presentation resembles that of aFAP with less than 100 polyps but also includes serrated and hyperplastic lesions primarily in the right hemicolon. Clinical guidance for MAP recommends initiating colonoscopy surveillance at 18–20 years of age with examinations 1–3-yearly and polypectomy of lesions larger than 5 mm94. Due to low polyp burden and rare rectal involvement, abdominal colectomy or subtotal colectomy with ileorectal anastomosis is likely sufficient to prevent metachronous CRC95.
DNA polymerase ɛ/DNA polymerase δ
Polyposis arising from germline variants of DNA polymerase ɛ (POLE) or DNA polymerase δ (POLD1) is a further autosomal dominant polyposis syndrome. Adenomas are present (10–100s) and are phenotypically dMMR/MSI with an incidence of CRC of between 32 and 63 per cent. Being hypermutated, cancers developing through this pathway may be responsive to CPI therapy95. Prophylactic surgery with abdominal subtotal colectomy may be appropriate with a severe polyp phenotype96.
Hamartomatous and juvenile polyposis
Hamartomatous polyposis syndromes have an estimated prevalence of 1 : 100 000–200 000. The polyps are by definition non-neoplastic with an abnormal cellular architecture and a mixture of cell types involved97. Syndromes presenting with hamartomatous polyps include Peutz–Jeghers syndrome (PJS), PTEN hamartoma tumour syndrome (PHTS), juvenile polyposis syndrome (JPS) and hereditary mixed polyposis syndrome (HMPS) (Fig. 2). Some polyps have distinct histomorphological features that indicate genetic germline evaluation for hereditary condition together with clinical criteria.
PJS polyps have branching bands of smooth muscle covered by hyperplastic glandular mucosa that may be present in the stomach, small bowel, and colorectum. The presence of two or more histologically confirmed PJ polyps, or any number of PJ polyps with a family history of PJS, warrant genetic testing for STK11. PJS has an autosomal dominant inheritance pattern with a cumulative CRC risk of 39 per cent, but also increased risk of gastric, pancreatic, breast, and other cancers98.
Juvenile polyps seen in JPS are most often found in the colorectum, and have dilated mucus-filling glands, prominent lamina propria, and Paneth cells, with strong immune cell infiltration. JPS is most often due to SMAD4 and BMPR1A germline pathogenic variants, yet in approximately half of patients meeting clinical diagnostic criteria no causative genetic defect is found. Genetic evaluation is warranted in patients with five or more juvenile polyps in the colorectum or any number of juvenile polyps where there is also a family history of JPS97. Cumulative lifetime risk of CRC of 39 per cent has been quoted with a mean age of onset of 44 years99.
Unlike in most adenomatous polyposis syndromes, prophylactic bowel resections are usually not necessary to prevent cancer in hamartomatous and juvenile polyposis.
Colorectal cancer summary
Relevant inherited CRC syndromes with summarized surveillance and management guidelines are presented in Table 1.
Table 1.
Summary of surveillance and management guidelines in hereditary colorectal cancer syndromes
| Syndrome | Lynch syndrome | FAP/aFAP | MAP | PPAP | PJS | PHTS | JPS | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Genes | MLH1 | MSH2/EPCAM | MSH6 | PMS2 | APC | MUTYH (biallelic) | POLE/POLD | STK11 | PTEN | SMAD4, BMPR1A |
| Phenotype | Non-polyposis colorectal cancer | Adenomatous polyposis | Hamartomatous polyposis | Juvenile polyposis | ||||||
| Surveillance starting age in years | 20–25* | 20–25* | 30–35* | 30–35* | 12–15 | 18–20 | 14 | 18 (8 for baseline) | 35 | 12–15 |
| Colonoscopy interval in years (healthy carriers) | 2–3 | 2–3 | 2–3 | 3–5 | 1–3 | 1–3 | 2 | 1–3 | 5 | 1–3 |
| Colorectal surgery implications | Subtotal abdominal colectomy advised for cancer | Subtotal abdominal colectomy advised for cancer | Standard resections for cancer | Standard resections for cancer | Prophylactic proctocolectomy or colectomy | Prophylactic colectomy | Prophylactic subtotal colectomy in severe phenotypes | Subtotal colectomy sometimes necessary for polyp burden or complications | – | Subtotal colectomy sometimes necessary for polyp burden or complications |
| References | 7,55 | 7,94,95,100 | 7,94,95,100 | 96 | 101,102 | 103 | 104 | |||
FAP, familial adenomatous polyposis; aFAP, attenuated familial adenomatous polyposis; MAP, MUTYH-associated polyposis; PPAP, POLE/POLD1-associated polyposis; PJS, Peutz–Jeghers syndrome; PHTS, PTEN hamartoma tumour syndrome; JPS, juvenile polyposis syndrome. *Or 2–5 years before the earliest age of CRC diagnosis in the family (whichever is earlier).
Hereditary gastric cancer
Epidemiology
Gastric cancer is one of the most common cancers worldwide and is the third most common cause of cancer-related death105. Gastric cancer is classically divided between intestinal, diffuse, and indeterminate subtypes based on the Lauren classification, with the majority being intestinal and up to 20–30 per cent of gastric cancers classified as the diffuse subtype106. There are substantial region-specific differences in gastric cancer incidence, with East Asia, Eastern Europe, Central America, and South America all having increased gastric cancer incidence compared with other parts of the world107. Much of these region-specific differences in incidence likely result from lifestyle and environmental factors, such as Helicobacter pylori infection, which is well known to be associated with increased gastric cancer risk108.
While the majority of gastric cancers are considered sporadic, up to 20 per cent of people diagnosed with gastric cancer have a family history of gastric cancer109. Furthermore, up to 5–10 per cent of gastric cancers have a familial component or are due to a hereditary cancer predisposition syndrome109. Of the known hereditary gastric cancer risk syndromes, hereditary diffuse gastric cancer syndrome (HDGC), due to a PV in either the CDH1 or CTNNA1 gene, confers one of the highest lifetime risks of gastric cancer110–112. Other hereditary cancer risk syndromes associated with increased gastric cancer risk include LS, Li–Fraumeni syndrome (LFS), and multiple polyposis syndromes including FAP, gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS), PJS, and JPS113. Furthermore, familial intestinal gastric cancer (FIGC) is a condition that encompasses individuals with a strong family history of intestinal-type gastric cancer with no identifiable germline PV114.
Mechanisms of carcinogenesis
The classic mechanism for the development of intestinal-type gastric cancer is via the ‘Correa cascade’, which involves gastric inflammation either in the form of chronic gastritis or atrophic gastritis, followed by progression to intestinal metaplasia, dysplasia, and finally carcinoma115. Meanwhile some intestinal-type gastric cancers develop from precursor lesions including gastric adenomas. Diffuse gastric cancer (DGC) also arises independently of the Correa cascade116.
Pathogens play a major role in gastric carcinogenesis, for example H. pylori, estimated to infect at least half of the world’s population117. H. pylori causes chronic gastritis and promotes progression through the Correa cascade, and effective treatment can lead to reductions in gastric cancer risk118,119. Epstein–Barr virus (EBV) is also associated with gastric cancer, with approximately 9 per cent of gastric cancers being associated with EBV120.
Identification
Evaluation for a potential hereditary cancer predisposition syndrome associated with increased gastric cancer risk is triggered by personal and family history as well as tumour analysis, as summarized in Table 2.
Table 2.
Recommendations for genetic testing for hereditary diffuse gastric cancer
| Recommendations from the International Gastric Cancer Linkage Consortium for genetic testing for hereditary diffuse gastric cancer 121 | |
| Family criteria | Family history of at least two gastric cancers with one being DGC |
| One DGC and one lobular breast cancer (at <70 years of age) in different family members | |
| At least two lobular breast cancers in the family younger than 50 years of age | |
| Patient criteria | DGC and is either younger than 50 years of age, is of Māori ethnicity, or has a personal or family history of cleft lip or palate |
| DGC and lobular breast cancer both diagnosed before 70 years of age | |
| Bilateral lobular breast cancer before 70 years of age | |
| Foci of gastric signet ring cells before 50 years of age | |
| National Comprehensive Cancer Network recommendations for genetic testing for a hereditary gastric cancer risk syndrome 122 | |
| Family criteria | Family history of gastric cancer in an FDR or SDR before 40 years of age |
| Gastric cancer in two FDRs or SDRs with one diagnosis before 50 years of age | |
| Gastric cancer in three FDRs or SDRs | |
| Patient criteria | Gastric cancer before 40 years of age |
| Gastric cancer before 50 years of age with an FDR or SDR with gastric cancer | |
| Gastric cancer with at least two FDR/SDRs with gastric cancer | |
| Gastric and breast cancer with one diagnosis before 50 years of age | |
| Gastric cancer and a family history of breast cancer in an FDR or SDR diagnosed before 50 years of age | |
| Other criteria that should prompt consideration for genetic testing for a hereditary gastric cancer risk syndrome | |
| Abnormal MMR IHC of a gastric cancer | |
| Gastric polyposis, including hamartomatous polyposis and fundic gland polyposis, especially when there is dysplasia present and no significant history of chronic proton pump inhibitor use | |
DGC, diffuse gastric cancer; FDR, first-degree relative; SDR, second-degree relative; MMR IHC, mismatch repair immunohistochemical staining.
Genetic testing
Given the increased ease of germline multigene panel testing (MGPT), increased access, and decreased cost123, MGPT should be the primary modality used for evaluation of suspected hereditary gastric cancer risk. In some circumstances, small multigene panel or even single gene testing may be appropriate, especially if there is a known familial PV in a gastric cancer risk gene.
At a minimum, MGPT focused on hereditary gastric cancer risk should include genes associated with HDGC (CDH1 and CTNNA1), LS (MLH1, MSH2, EPCAM, MSH6, PMS2), FAP (APC), PJS (STK11), JPS (SMAD4 and BMPR1A), and LFS (TP53). However, other genes may be added to this list depending on personal and family history or patient preference.
Gastric cancer surveillance and risk management
Gastric cancer surveillance recommendations for hereditary syndromes with increased gastric cancer risk are presented in Table 3.
Table 3.
Summary of recommendations for hereditary syndromes with increased gastric cancer risk
| Syndrome | HDGC | Lynch syndrome | FAP/aFAP | GAPPS | PJS | JPS | LFS | FIGC |
|---|---|---|---|---|---|---|---|---|
| Genes | CDH1, CTNNA1 | MLH1, MSH2/EPCAM, MSH6, PMS2 | APC | APC promoter 1B | STK11 | SMAD4, BMPR1A | TP53 | Unknown |
| Surveillance starting age in years | 18–20 | 30–40 | 20–25 | 15 | 18 (8 for baseline) | 12–15 | 25 | 40–60 (or 5 years before earliest cancer diagnosis) |
| Upper endoscopy interval (healthy carriers) | 1 year (until prophylactic gastrectomy peformed) | 2–4 years | 3 months–5 years | 1 year (until prophylactic gastrectomy peformed) | 2–3 years | 1–3 years | 2–5 years | 1–3 years |
| Surveillance considerations | Modified Cambridge protocol or Bethesda protocol should be used Inlet patches should be documented and biopsied |
Biopsies of the gastric antrum and body should be performed to assess for H. pylori, gastric intestinal metaplasia, and autoimmune gastritis | Surveillance interval should be based on the Spigelman score and/or gastric pathology A baseline upper endoscopy should be performed before 20 years of age if earlier colectomy is planned |
– | – | For a clinical diagnosis of JPS without an SMAD4 or BMPR1A PV, the surveillance interval can be increased to 5 years in the absence of gastric polyps | – | – |
| Surgical considerations | Prophylactic total gastrectomy between 20 and 30 years of age | – | If total gastrectomy is performed, Roux limb should be constructed to allow for continued duodenal surveillance | Prophylactic total gastrectomy by the 30s | – | – | – | – |
| References | 121,124 | 125 | 126 | 126 | 97,126 | 97,126 | 127 | 114,128 |
–, no clear guidance established for the condition; HDGC, hereditary diffuse gastric cancer syndrome; FAP, familial adenomatous polyposis; aFAP, attenuated familial adenomatous polyposis; GAPPS, gastric adenocarcinoma and proximal polyposis of the stomach; PJS, Peutz–Jeghers syndrome; JPS, juvenile polyposis syndrome; LFS, Li–Fraumeni syndrome; FIGC, familial intestinal gastric cancer.
Hereditary diffuse gastric cancer syndrome
HDGC is associated with PVs in either the CDH1 or CTNNA1 gene129–131 and confers the highest risk of DGC amongst all of the known hereditary gastric cancer risk syndromes. For CDH1 carriers, early estimates of DGC risk were as high as 83 per cent by 80 years of age132; however, more recent data, ascertained with less bias toward gastric cancer predominant families, have shown gastric cancer risks of 33–42 per cent by 80 years of age110,111. The first risk estimate in CTNNA1 carriers was also recently reported showing a DGC risk by 80 years of age of 49–57 per cent112, yet only included families with DGC. Therefore, the quoted lifetime gastric cancer risk in CTNNA1 carriers will also likely decrease as more families are identified. Indeed, a recent report of CTNNA1 phenotypes on MGPT showed that only 12 per cent of patients and 21 per cent of families with a CTNNA1 loss-of-function variant had a history of gastric cancer133.
The major gastric cancer risk management decision for carriers of a PV in CDH1 or CTNNA1 is whether to pursue endoscopic surveillance or risk-reducing total gastrectomy. Current gastric surveillance recommendations from the International Gastric Cancer Linkage Consortium (IGCLC) for carriers of a PV in CDH1 or CTNNA1 help inform this decision and are based on family history of DGC121. If there is a family history of DGC along with a PV in CDH1 or CTNNA1, then risk-reducing total gastrectomy should be considered, with preoperative endoscopy performed to identify whether gastric cancer has already developed. If there is no family history of gastric cancer, carriers of a PV in CDH1 or CTNNA1 may consider either risk-reducing total gastrectomy or yearly surveillance.
Current recommendations for endoscopic surveillance support the use of a modified Cambridge biopsy protocol, which includes targeted biopsies of any macroscopic gastric lesions, 28–30 non-targeted biopsies of the antrum (5), transition zone (5), body (10), fundus (5), and cardia (3–5), and documentation and biopsy of any oesophageal inlet patches121. It is important that these biopsies are reviewed by a specialized gastrointestinal pathologist to facilitate identification of foci of signet ring cell carcinoma (SRCC), which indicate the need for risk-reducing total gastrectomy. However, despite extensive biopsy sampling, foci of SRCC are still frequently observed on subsequent gastrectomy specimens, even in the setting of negative biopsies134. The Bethesda protocol124 proposes a total of 88 non-targeted biopsies, with evidence of increased detection of foci of SRCC, yet a false negative rate of 38 per cent. Advanced endoscopic methods including endoscopic ultrasound135 and confocal laser endomicroscopy136 have been studied without clear increases in SRCC detection137. At this time, there are no reliable strategies for chemoprevention of gastric cancer in HDGC, or therapies to selectively target and eliminate SRCC, although this is an area of active research in preclinical models138,139.
Given the lack of reliable methods to adequately identify or treat foci of SRCC in HDGC, risk-reducing total gastrectomy is often the preferred strategy with debate about timing. A recent modelling study recommended the optimal age for risk-reducing total gastrectomy as 39 years for men and 30 years for women140, whereas recommendations from the IGCLC advise risk-reducing total gastrectomy between 20 and 30 years of age121. There is also no role for partial gastrectomy in the management of HDGC and, where risk-reducing total gastrectomy is performed, it should be done in a centre with HDGC expertise. If foci of SRCC are identified on index endoscopy, neoadjuvant therapy is not necessary before gastrectomy in the absence of a more invasive gastric cancer. Furthermore, it is critically important to confirm both proximal and distal margins of the gastrectomy specimen to ensure that no gastric tissue remains. Recent reports have highlighted favourable safety outcomes amongst HDGC patients undergoing risk-reducing total gastrectomy141,142.
Individuals who have a risk-reducing total gastrectomy need long-term follow-up for both nutritional monitoring and other cancer screening. Enhanced breast cancer screening is recommended for carriers of a PV in CDH1 or CTNNA1, yet current guidelines do not recommend regular CRC screening121 given average rates of colorectal neoplasia in CDH1 carriers compared with the general population143. A recent consensus panel provided recommendations for longitudinal monitoring of CDH1 carriers after a risk-reducing gastrectomy focusing on nutrient monitoring and supplementation as well as bone health144.
Lynch syndrome
LS due to a PV in MLH1, MSH2, MSH6, PMS2, or EPCAM is one of the most common gastric cancer predisposition syndromes, affecting 1 in 279 individuals145. Gastric cancer risk in LS can be up to 9 per cent, however, but varies by genotype, with PMS2 variants associated with lower gastric cancer risk than other variants125. Male sex, having an FDR with gastric cancer, and older age are also associated with a higher risk of gastric cancer in LS146. Debate surrounds gastric surveillance in LS: when it should begin and how often it should be performed. The National Comprehensive Cancer Network (NCCN) has recently recommended routine gastric surveillance for MLH1, MSH2, MSH6, and EPCAM carriers beginning between 30 and 40 years of age and repeating every 2–4 years126, while the BSG, the European Hereditary Tumour Group (EHTG), and the European Society of Coloproctology (ESCP) do not recommend routine gastric surveillance in LS outside of clinical trials7,55.
Studies of gastric surveillance in LS from the USA147–149 and Europe125,150 have illustrated that surveillance leads to clinically actionable findings as well as early-stage gastric cancers. A recent meta-analysis of upper gastrointestinal surveillance demonstrated that the pooled event rate for detecting an upper gastrointestinal cancer was 0.9 per cent, a high-risk lesion was 4.2 per cent, and an actionable finding was 6.2 per cent151. However, the impact of upper gastrointestinal surveillance on survival in LS remains unknown.
When gastric surveillance is performed, H. pylori, gastric intestinal metaplasia, and autoimmune gastritis should be assessed via biopsy of the gastric antrum and body125. If H. pylori is detected, the patient should be treated, with confirmation of eradication. Even if a decision is made to forego gastric surveillance in LS, testing for H. pylori should still be performed non-invasively, especially if there is consideration of starting aspirin for chemoprevention. While aspirin has not been shown to have a chemopreventive effect on gastric cancer in LS75, recent evidence from the randomized controlled CaPP2 trial has indicated that resistant starch may decrease upper gastrointestinal cancer risk, including gastric cancer risk152.
Development of gastric cancer in LS during or outside of active surveillance, unlike HDGC, does not immediately dictate the need for a total gastrectomy, with limited resections appropriate depending on tumour location. Furthermore, treatment with immunotherapy can be considered for unresectable, metastatic, dMMR disease153.
Familial adenomatous polyposis/gastric adenocarcinoma and proximal polyposis of the stomach
FAP is associated with increased gastric cancer risk. This risk of gastric cancer in FAP has been reported to be as high as 7.1 per cent. While higher estimates have been seen in primarily East Asian populations126, there are more recent reports of an increase in gastric cancer incidence in FAP in the West as well154. Similar to FAP, GAPPS is an autosomal dominant condition associated with increased gastric cancer risk155. However, unlike FAP, which is due to PVs within the coding region of APC, GAPPS results from point mutations in promoter 1B of the APC gene, which selectively result in gastric polyposis without polyposis noted in the small and large bowel156. Reported estimates of gastric cancer risk in GAPPS are still evolving, but have ranged between 12 and 25 per cent155,157.
Individuals with FAP and GAPPS frequently have fundic gland polyposis, often with low-grade dysplasia158. However, it is thought that high-risk lesions such as gastric adenomas, pyloric gland adenomas, and gastric lesions with high-grade dysplasia are the most likely cancer precursor lesions, as these lesions are observed more frequently in individuals with gastric cancer159. Additionally, carpeting of gastric polyps, gastric polyps larger than 2 cm, and mounds of gastric polyps are other endoscopic features associated with increased gastric cancer risk in FAP159.
Upper gastrointestinal tract surveillance in FAP has classically been guided by the Spigelman stage of duodenal polyposis, with an interval between 3 months and 5 years depending on the duodenal polyp burden126. However, with recent increases in gastric cancer incidence in FAP, gastric polyp burden may be used to dictate gastroduodenal surveillance intervals. Proposed surveillance for gastric polyposis in FAP includes basing surveillance intervals on the number, size, pathology (including presence of dysplasia), and whether or not there are mounds of gastric polyps, and making this recommendation independent of duodenal findings154. Recommendations for when to start upper gastrointestinal surveillance in FAP vary between 20 and 25 years of age; however, if a patient with FAP is undergoing another abdominal surgery and has not yet had a baseline upper endoscopy, it is prudent to first obtain a preoperative oesophagogastroduodenoscopy to rule out upper gastrointestinal neoplasia. Data on gastric surveillance in GAPPS are much more limited, with current recommendations to start gastric surveillance at 15 years of age, and repeat surveillance yearly126.
Risk-reducing total gastrectomy should be offered to patients with GAPPS by approximately 30 years of age, yet earlier surgery may be considered based on patient preference, polyp burden, and family history160. In FAP, gastric surgery should only be considered for individuals who develop gastric cancer, or who develop high-risk gastric lesions that cannot be managed and/or surveilled endoscopically. If surgery for gastric neoplasia is performed in FAP, a total gastrectomy can be considered based on the polyp burden and given the risk of metachronous gastric neoplasia. In the setting of a total gastrectomy, special attention should be paid to construction of the Roux limb, as continued duodenal surveillance will be necessary, and may pose an endoscopic challenge after surgery.
Hamartomatous and juvenile polyposis syndromes
Both PJS and JPS have been associated with increased gastric cancer risk. PJS, which is diagnosed by having a PV in STK11 or through meeting clinical diagnostic criteria, has been associated with a cumulative gastric cancer risk of 29 per cent161. Individuals with PJS are recommended to undergo upper endoscopic surveillance starting in childhood (age 8–10 years); however, at this age surveillance is primarily aimed at detection of polyps, which may lead to anaemia, obstruction, or intussusception97. In adulthood, upper gastrointestinal surveillance is recommended to occur at least every 2–3 years97.
JPS can result from a PV in SMAD4 or BMPR1A; however, in nearly half of cases there is no PV identified and instead patients meet clinical diagnostic criteria for JPS97. In JPS, gastric cancer has primarily been reported in SMAD4 carriers, with a recent study showing a gastric cancer incidence of 27 per cent in SMAD4 PV carriers162. Furthermore, there appears to be a distinct genotype–phenotype correlation with gastric polyposis in JPS between those with and without an identifiable PV. In a recent multicentre study, individuals with JPS without a SMAD4/BMPR1A PV had no reported gastric cancer or any reported gastric polyps163. Upper gastrointestinal cancer surveillance in JPS has been recommended to begin as early as 12–15 years of age and be repeated every 1–3 years; however, consideration can be made to starting upper gastrointestinal cancer surveillance later and using longer intervals in individuals without a PV in SMAD4/BMPR1A97,126.
Other gastric cancer risk syndromes
Other hereditary syndromes associated with increased gastric cancer risk include LFS, hereditary breast and ovarian cancer (HBOC) syndrome, and FIGC. In LFS, 3.3 per cent of individuals and 5.9 per cent of LFS families were reported to have gastric cancer164, with higher rates reported in Asian LFS populations165. Some groups have recommended upper gastrointestinal surveillance as a routine part of LFS care127; however, this recommendation is not uniform166. HBOC due to a PV in BRCA1 or BRCA2 is well documented to increase the risk of breast, ovarian, pancreatic, and prostate cancer167,168. However, several recent studies have also highlighted an increased risk of gastric cancer168,169. Despite this increased risk, there are no recommendations for gastric surveillance in BRCA1/2 PV carriers, although if a carrier does develop a BRCA1/2-related gastric cancer, these individuals may be eligible for specific therapy such as poly ADP ribose polymerase (PARP) inhibitors170. Finally, FIGC is a hereditary intestinal-type gastric cancer risk syndrome that at this time does not have an identifiable genetic aetiology114, but is instead diagnosed based on clinical criteria128. As this is a newly characterized syndrome with limited data, the cancer risk associated with FIGC remains poorly characterized, and at this time there are no consensus guideline recommendations about surveillance for affected individuals.
Hereditary pancreatic cancer
Epidemiology
Pancreatic cancer is a devastating malignancy with a rising worldwide incidence and mortality rate171.
In early-stage disease, diagnosis relies upon the availability of advanced cross-sectional imaging with the capacity to access tissues for diagnostic biopsy (often via endoscopic ultrasonography). Survival is strongly associated with stage at diagnosis, yet patients are often diagnosed at an advanced stage, restricting therapeutic options largely to palliative measures172. There are no early diagnosis tools available for broad generalized use amongst the population. When found at an early stage, cure is achieved with surgical resection with or without systemic chemotherapy.
Mechanisms of carcinogenesis
There are two main histological pathways leading to exocrine cancer of the pancreas, or pancreatic ductal adenocarcinoma. The first involves dysplastic progression of the cells lining the branches of the exocrine collecting system, both the acinar cells and ductal cells. These dysplastic changes on histological examination are accompanied by mutations in four major driver genes commonly seen in pancreatic cancer: KRAS, CDKN2A, TP53, and SMAD4173. Both KRAS mutations and alterations in CDKN2A, including homozygous loss, are thought to be the earliest events in pancreatic tumorigenesis, with SMAD4 loss thought to be a relatively late event174.
The second histological pathway tends to involve cystic growth of the exocrine ductal tree and accumulated dysplasia within these cysts175. These features are termed intraductal papillary mucinous neoplasms (IPMN). Importantly, not all IPMN progress to malignancy and the clinical management of IPMN can be controversial as the only effective strategy thus far employed to eliminate the potential risk of underlying malignancy is surgical resection. The molecular changes that accompany IPMN-associated dysplasia share some common traits to the pathway described in pancreatic intraepithelial neoplasia (PanIN), but, IPMN-associated dysplasia can also be driven by mutations outside the big four, including mutations in GNAS, RNF43, and numerous others176. Given the wider variety of somatic mutations found in this population, individuals with IPMN and a strong family history have been a focus of several studies investigating unique genetic drivers of disease and clinical paradigm screening for high-risk cohorts177. Interestingly, the underlying molecular mechanisms driving the hereditary nature of this disease in many cohorts remain uncertain.
Clinical presentation and identification
Patients at increased risk, such as those carrying a hereditary risk, provide an opportunity to increase the detection of premalignancy or early malignancy through screening and so the ultimate long-term survival and cure of cancer in these patients is more likely than with sporadic cancer178. Screening in pancreatic cancer is limited by the capacity, associated costs, and potential for discovery of other incidental findings of uncertain significance, driving potential harm. Currently proposed screening paradigms rely heavily on short-interval cross-sectional imaging (with CT, MRI, and magnetic resonance cholangiopancreatography (MRCP) alongside endoscopic ultrasound evaluation of the gland. Blood-based diagnostic biomarkers, or liquid biopsy, is an area of active translational research.
Given the intensity of screening paradigms, there is a natural tension in identifying an optimal cohort meeting a threshold whereby the benefits outweigh the risks. A family history of pancreatic cancer is a significant predictor of disease risk, with some series suggesting a six-fold or higher risk compared with the general population179, with an increasing number of family members affected with an elevated risk180. The risk is also increased for kindred in whom disease onset was particularly young (that is less than 50 years of age)180. Taken together, the International Cancer of the Pancreas Screening Consortium recommends that screening programmes are implemented for individuals with an estimated lifetime risk of 5 per cent or greater181. This corresponds to individuals with a known deleterious germline variant for pancreatic cancer as well as individuals with a strong family history of pancreatic cancer. The generally accepted threshold for screening based upon family history alone is the presence of at least two FDRs with a history of pancreatic cancer, or at least one FDR and one second-degree relative with the disease who are themselves directly related181. Genetic testing in the presence of a strong family history is not a prerequisite to enter into screening programmes in this disease—though the two groups, familial risk only and known genetic susceptibility, are often grouped independently for analysis in the literature.
Pancreatic cancer susceptibility gene variants
The value of identifying kindred at risk of pancreatic cancer and potentially intervening prior to cancer development or during early stages, has led to recommendations for example from the NCCN that all patients undergoing therapy for pancreatic cancer receive germline assessment182. When panel testing is utilized in this cohort, even in the absence of known familial risk, nearly 10 per cent of cases are identified as being linked to high-penetrance genetic variants183,184. Common variants identified include BRCA1/BRCA2, MMR genes associated with LS, CDK2NA, and ATM. Less commonly, PVs in genes such as TP53, PRSS1, STK11, and PALB2 can be present, which can increase the relative risk of developing pancreatic cancer 30-fold or more. Many of these gene variants also carry the risk of developing another gastrointestinal malignancy.
The most frequently identified genetic risk factors are pathogenic variants identified in BRCA2 and ATM. When screening is employed for all patients, regardless of familial risk, the prevalence for each approaches 2 per cent184. Founder variants are important to recognize in certain populations such as the Ashkenazi Jewish population and BRCA2 families. In patients with these deleterious founder variants, the lifetime risk of pancreatic cancer development approaches 10 per cent by 80 years of age. The lifetime risk conveyed by BRCA1 in pancreatic cancer is significantly lower (estimated to be 3 per cent) and falls below the general cut-off risk to initiate screening. ATM variants are associated with a clinical diagnosis of ataxia telangiectasia and, similar to BRCA2, convey an approximate lifetime risk of pancreatic cancer approaching 10 per cent185.
The lifetime risk of pancreatic cancer is highest for patients with known germline variants in three unique genes: STK11, CDK2NA, and PRSS1. In addition to the inherited risk of CRC and gastric cancer, PVs in STK11 and a diagnosis of PJS are associated with a lifetime risk of pancreatic cancer that exceeds 30 per cent in some series186. Another founder variant is responsible for many of the cases seen in CDKN2A families (the Dutch founder variant affecting the p16 isoform of the protein). In these cases, the inherited predisposition can be elucidated with a strong familial history of melanoma likely due to impaired cell-cycle regulation. This syndrome, known as familial atypical mole and multiple melanoma syndrome, is associated with a lifetime risk of pancreatic cancer approaching 20 per cent187. Finally, PVs in the PRSS1 gene are most often found when evaluating patients with both a personal and a family history of recurrent acute pancreatitis. The PRSS1 protein encodes a pancreatic trypsinogen that, when mutated, can lead to inappropriate trypsin activation within the pancreatic parenchyma. The resulting clinical syndrome can result in the development of malignancy in up to 40 per cent of patients in some studies188. The risk of malignancy in this pancreatitis cohort is high enough that multidisciplinary programmes are beginning the process of creating shared decision-making models that propose prophylactic total pancreatectomy in highly selected individuals189.
Other less frequently encountered hereditary variants impacting pancreatic cancer risk are found in the MMR genes causing LS (4 per cent lifetime risk), PALB2 (2 per cent lifetime risk), TP53 causing LFS (1–2 per cent lifetime risk), CPA1 and CPB1 (0.5 per cent lifetime risk), and other hereditary pancreatitis genes such as CFTR and SPINK-1 (5–20 per cent lifetime risk)178,186,190.
Pancreatic cancer surveillance and risk management
Once the decision to undertake routine surveillance for patients at high risk has been made, the optimal screening strategy for this disease should include routine interval history and physical exams supplemented by multimodal imaging assessment and, for a select few, laboratory profiling. The optimal strategy is hotly debated in the literature and is perhaps most easily reconciled by focusing first on the underlying patient features associated with each hereditary risk case. One management strategy to manage patients with a hereditary risk, and clinical manifestations resulting in pancreatic cystic disease, is to adapt the Fukuoka guidelines191. The strategy for patients with hereditary risk and clinical manifestations of pancreatitis has been outlined by an international consensus committee from the International Association of Pancreatology, the American Pancreatic Association, the Japan Pancreas Society, and the European Pancreatic Club192. Lastly, and most controversially, the most common screening guidelines used for patients without pancreatic cystic disease or pancreatitis tend to follow along the protocols detailed by the International Cancer of the Pancreas Screening Consortium181.
For patients with pancreatic cystic disease, the risk of developing pancreatic malignancy is assessed by screening for a set of clinical, radiographic, and laboratory criteria defined as ‘high-risk stigmata’ and/or ‘worrisome features.’ These features are identified by a strategy that employs both cross-sectional imaging and endoscopic ultrasound assessment. Importantly, the Fukuoka guidelines do not take hereditary risk or family history into account and, therefore, should be adapted with some recognition of underlying risk. The decision to resect these lesions, particularly in the absence of a tissue diagnosis suggesting high-grade dysplasia or malignancy, relies on shared decision-making to outline the risks for malignancy suggested by these guidelines against the risks associated with a surgical procedure to extirpate the associated cystic disease. Surgical procedures involve formal gland resection with either Whipple’s procedure or a distal pancreatectomy as limited enucleations result in morbid pancreatic leak and are of limited oncological benefit. In the absence of surgical resection, surveillance strategies are suggested by the Fukuoka guidelines in a manner that is tailored to underlying risk191. Notably, this commonly utilized strategy to assess patients with cystic disease does not take underlying hereditary risk into account and conversations during shared decision-making often hinge on estimating this somewhat nebulous added risk. Finally, a comparison of this method for risk identification in patients with cystic disease with the guidelines outlined by the International Cancer of the Pancreas Screening Consortium (that take the presence of cystic disease into limited account) found both methods to be moderately specific but with limited sensitivity, suggesting more work focused in this space may lead to improved outcomes193.
In patients with pancreatitis expert agreement recommends screening in patients with PRSS1 PV but no routine screening for patients with SPINK1 and other PVs192. Screening in this cohort was recommended to be initiated at 40 years of age; however, the ideal screening modality and interval remains controversial. Both CT and MRI were mentioned as reasonable strategies for screening, with preference deferred to locoregional high-volume expert centres. Endoscopic ultrasound, while used in the assessment for cyst patients, was not recommended in the setting of pancreatitis (weak consensus agreement) due to fibrosis, inflammation, and calcification, which can impair assessment. Recommendations to avoid tobacco, limit alcohol, and maintain a healthy diet with integration of physical exercise were strongly agreed to; other meaningful risk mitigation strategies were scarce, reflective of the underlying evidence available for interpretation.
In patients without cystic disease or pancreatitis, pancreatologists rely upon guidelines detailed by the International Cancer of the Pancreas Screening Consortium181. The programme of the International Cancer of the Pancreas Screening Consortium is grounded in a Delphi approach with expert consensus leading to 55 statements of agreement reflective of modern practice. The core of the recommendations included a firm statement on those eligible for enhanced screening programmes (discussed above), the age to begin screening in high-risk individuals, the modality and timing used for screening, and the indications to consider surgical resection. In this consortium, experts recommend beginning screening at 50 years of age or 10 years younger than the age at which the first relative was affected, whichever is sooner. Both MRI/MRCP and endoscopic ultrasound are noted to be effective screening modalities in this cohort, though preference for one over another, strategies to incorporate both, and indications to integrate CT into screening programmes did not reach consensus. Recent data from the Cancer of Pancreas Screening-5 study demonstrated that screening of high-risk individuals led to downstaging of detected pancreatic cancers and dramatically improved survival compared with pancreatic cancers detected outside of screening194. Finally, there were no indications identified for prophylactic pancreatectomy in the absence of identified lesions during screening as the main goals remain to identify high-grade dysplastic precursor lesions and T1N0M0 cancer.
In pancreatic cancer, hereditary predisposition can be assigned in approximately 10 per cent of patients. Screening in both the general population and high-risk individuals remains limited by the occult nature of the disease, a lack of diagnostic biomarkers, and the low sensitivity of high-quality imaging for disease onset. The risk of disease is balanced against the risks involved for treatment, namely radical oncological resection, in modern guidelines for management of high-risk individuals.
Contributor Information
Toni T Seppälä, Faculty of Medicine and Health Technology, Tampere University, Tampere, Finland; Department of Gastrointestinal Surgery, Tampere University Hospital and TAYS Cancer Centre, Tampere, Finland; Applied Tumor Genomics Research Program, University of Helsinki, Helsinki, Finland; Department of Abdominal Surgery, Helsinki University Central Hospital, Helsinki, Finland.
Richard A Burkhart, Department of Surgical Oncology, Johns Hopkins University, Baltimore, Maryland, USA; Department of Oncology, Sidney Kimmel Comprehensive Cancer Center, Baltimore, Maryland, USA.
Bryson W Katona, Division of Gastroenterology and Hepatology, Department of Medicine, Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania, USA.
Summary
Hereditary gastrointestinal cancers are under-diagnosed and require attention for identification and differential diagnostics with easy access to germline genetic evaluation to confirm the diagnosis. Awareness of multiple predisposing conditions to both gastrointestinal and extra-intestinal cancers is imperative in the identification of specific germline syndromes and resulting surveillance and management according to relevant condition-specific clinical guidelines.
Funding
T.T.S. is supported by funding from the Academy of Finland and iCAN Precision Medicine Flagship of Academy of Finland, and research grants from the Jane and Aatos Erkko Foundation, Sigrid Juselius Foundation, Emil Aaltonen Foundation, Cancer Society Finland, and Relander Foundation. B.W.K. is supported by funding from the Jason and Julie Borrelli Lynch Syndrome Research Fund, Scott and Suzi Lustgarten Colon Cancer Research Fund, Smith Family Research Fund, King Family Fund for Lynch Syndrome Education, Outreach and Impact, Basser Center for BRCA, and DeGregorio Family Foundation.
Author contributions
Toni T. Seppälä (Conceptualization, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing—original draft, Writing—review & editing), Richard A. Burkhart (Conceptualization, Investigation, Methodology, Writing—original draft, Writing—review & editing), and Bryson W. Katona (Conceptualization, Investigation, Methodology, Writing—original draft, Writing—review & editing).
Disclosure
The funding bodies had no role in writing the article. T.T.S. reports consultation fees from Boehringer Ingelheim Finland and Amgen Finland, and being a co-owner and CEO of Healthfund Finland. B.W.K. reports research support from Epigenomics, Freenome, Guardant Health, Immunovia, Janssen Pharmaceuticals, and Universal Diagnostics, as well as non-funded research collaborations with Ambry, Myriad, GeneDx, and Invitae. T.T.S. and B.W.K. declare no other conflict of interest. B.A.B. declares no conflict of interest.
Data availability
Not applicable.
References
- 1. Hasanov E, Pimentel I, Cruellas M, Lewis MA, Jonasch E, Balmaña J. Current systemic treatments for the hereditary cancer syndromes: drug development in light of genomic defects. Am Soc Clin Oncol Educ Book 2022;42:1–17 [DOI] [PubMed] [Google Scholar]
- 2. Snowsill T, Coelho H, Huxley N, Jones-Hughes T, Briscoe S, Frayling IMet al. Molecular testing for Lynch syndrome in people with colorectal cancer: systematic reviews and economic evaluation. Health Technol Assess 2017;21:1–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Møller P, Seppälä TT, Bernstein I, Holinski-Feder E, Sala P, Evans DGet al. Cancer risk and survival in path-MMR carriers by gene and gender up to 75 years of age: a report from the Prospective Lynch Syndrome Database. Gut 2018;67:1306–1316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brosens LAA, Keller JJ, Offerhaus GJA, Goggins M, Giardiello FM. Prevention and management of duodenal polyps in familial adenomatous polyposis. Gut 2005;54:1034–1043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Abraham SC. Fundic gland polyps: common and occasionally problematic lesions. Gastroenterol Hepatol (N Y) 2010;6:48–51 [PMC free article] [PubMed] [Google Scholar]
- 6. Lichtenstein P, Holm NV, Verkasalo PK, Iliadou A, Kaprio J, Koskenvuo Met al. Environmental and heritable factors in the causation of cancer–analyses of cohorts of twins from Sweden, Denmark, and Finland. N Engl J Med 2000;343:78–85 [DOI] [PubMed] [Google Scholar]
- 7. Monahan KJ, Bradshaw N, Dolwani S, Desouza B, Dunlop MG, East JEet al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut 2020;69:411–444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pearlman R, Frankel WL, Swanson BJ, Jones D, Zhao W, Yilmaz Aet al. Prospective statewide study of universal screening for hereditary colorectal cancer: the Ohio colorectal cancer prevention initiative. JCO Precis Oncol 2021;5:PO.20.00525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Coughlin SE, Heald B, Clark DF, Nielsen SM, Hatchell KE, Esplin EDet al. Multigene panel testing yields high rates of clinically actionable variants among patients with colorectal cancer. JCO Precis Oncol 2022;6:e2200517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vasen HF, Watson P, Mecklin JP, Lynch HT. New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International Collaborative Group on HNPCC. Gastroenterology 1999;116:1453–1456 [DOI] [PubMed] [Google Scholar]
- 11. Johns LE, Houlston RS. A systematic review and meta-analysis of familial colorectal cancer risk. Am J Gastroenterol 2001;96:2992–3003 [DOI] [PubMed] [Google Scholar]
- 12. Stanich PP, Pelstring KR, Hampel H, Pearlman R. A high percentage of early-age onset colorectal cancer is potentially preventable. Gastroenterology 2021;160:1850–1852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Daca Alvarez M, Quintana I, Terradas M, Mur P, Balaguer F, Valle L. The inherited and familial component of early-onset colorectal cancer. Cells 2021;10:710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stjepanovic N, Moreira L, Carneiro F, Balaguer F, Cervantes A, Balmaña Jet al. Hereditary gastrointestinal cancers: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2019;30:1558–1571 [DOI] [PubMed] [Google Scholar]
- 15. Kastrinos F, Samadder NJ, Burt RW. Use of family history and genetic testing to determine risk of colorectal cancer. Gastroenterology 2020;158:389–403 [DOI] [PubMed] [Google Scholar]
- 16. Stoffel EM, Mangu PB, Gruber SB, Hamilton SR, Kalady MF, Lau MWYet al. Hereditary colorectal cancer syndromes: American Society of Clinical Oncology clinical practice guideline endorsement of the familial risk-colorectal cancer: European Society for Medical Oncology clinical practice guidelines. J Clin Oncol 2015;33:209–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lynch HT, Krush AJ. The cancer family syndrome and cancer control. Surg Gynecol Obstet 1971;132:247–250 [PubMed] [Google Scholar]
- 18. Boland CR. Evolution of the nomenclature for the hereditary colorectal cancer syndromes. Fam Cancer 2005;4:211–218 [DOI] [PubMed] [Google Scholar]
- 19. Haraldsdottir S, Rafnar T, Frankel WL, Einarsdottir S, Sigurdsson A, Hampel Het al. Comprehensive population-wide analysis of Lynch syndrome in Iceland reveals founder mutations in MSH6 and PMS2. Nat Commun 2017;8:14755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Frankel W, Arends M, Frayling IM. Genetic tumour syndromes of the digestive system. In: Arends M, Carniero F, Lax S (eds), Digestive System Tumours, WHO Classification of Tumours, Vol.1 (5th edn). Lyon, France: International Agency for Research on Cancer, 2019, 515–521 [Google Scholar]
- 21. Hampel H. Population screening for hereditary colorectal cancer. Surg Oncol Clin N Am 2018;27:319–325 [DOI] [PubMed] [Google Scholar]
- 22. Bonadona V, Bonaïti B, Olschwang S, Grandjouan S, Huiart L, Longy Met al. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA 2011;305:2304–2310 [DOI] [PubMed] [Google Scholar]
- 23. Dowty JG, Win AK, Buchanan DD, Lindor NM, Macrae FA, Clendenning Met al. Cancer risks for MLH1 and MSH2 mutation carriers. Hum Mutat 2013;34:490–497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Møller P, Seppälä T, Bernstein I, Holinski-Feder E, Sala P, Evans DGGet al. Cancer incidence and survival in Lynch syndrome patients receiving colonoscopic and gynaecological surveillance: first report from the prospective Lynch syndrome database. Gut 2017;66:464–472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dominguez-Valentin M, Sampson JR, Seppälä TT, Ten Broeke SW, Plazzer J-P, Nakken Set al. Cancer risks by gene, age, and gender in 6350 carriers of pathogenic mismatch repair variants: findings from the Prospective Lynch Syndrome Database. Genet Med 2020;22:15–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Seppälä TT, Dominguez-Valentin M, Sampson JR, Møller P. Prospective observational data informs understanding and future management of Lynch syndrome: insights from the Prospective Lynch Syndrome Database (PLSD). Fam Cancer 2021;20:35–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. International Mismatch Repair Consortium . Variation in the risk of colorectal cancer in families with Lynch syndrome: a retrospective cohort study. Lancet Oncol 2021;22:1014–1022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cerretelli G, Ager A, Arends MJ, Frayling IM. Molecular pathology of Lynch syndrome. J Pathol 2020;250:518–531 [DOI] [PubMed] [Google Scholar]
- 29. Ballhausen A, Przybilla MJ, Jendrusch M, Haupt S, Pfaffendorf E, Seidler Fet al. The shared frameshift mutation landscape of microsatellite-unstable cancers suggests immunoediting during tumor evolution. Nat Commun 2020;11:4740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ahadova A, Seppälä TT, Engel C, Gallon R, Burn J, Holinski-Feder Eet al. The ‘unnatural’ history of colorectal cancer in Lynch syndrome: lessons from colonoscopy surveillance. Int J Cancer 2021;148:800–811 [DOI] [PubMed] [Google Scholar]
- 31. Seth S, Ager A, Arends MJ, Frayling IM. Lynch syndrome—cancer pathways, heterogeneity and immune escape. J Pathol 2018;246:129–133 [DOI] [PubMed] [Google Scholar]
- 32. Jackman RJ, Mayo CW. The adenoma-carcinoma sequence in cancer of the colon. Surg Gynecol Obstet 1951;93:327–330 [PubMed] [Google Scholar]
- 33. Engel C, Vasen HF, Seppälä T, Aretz S, Bigirwamungu-Bargeman M, de Boer SYet al. No difference in colorectal cancer incidence or stage at detection by colonoscopy among 3 countries with different Lynch syndrome surveillance policies. Gastroenterology 2018;155:1400–1409.e2 [DOI] [PubMed] [Google Scholar]
- 34. Møller P, Seppälä T, Dowty JG, Haupt S, Dominguez-Valentin M, Sunde Let al. Colorectal cancer incidences in Lynch syndrome: a comparison of results from the prospective lynch syndrome database and the international mismatch repair consortium. Hered Cancer Clin Pract 2022;20:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ahadova A, Gallon R, Gebert J, Ballhausen A, Endris V, Kirchner Met al. Three molecular pathways model colorectal carcinogenesis in Lynch syndrome. Int J Cancer 2018;143:139–150 [DOI] [PubMed] [Google Scholar]
- 36. Jass JR, Stewart SM. Evolution of hereditary non-polyposis colorectal cancer. Gut 1992;33:783–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Engel C, Ahadova A, Seppälä TT, Aretz S, Bigirwamungu-Bargeman M, Bläker Het al. Associations of pathogenic variants in MLH1, MSH2, and MSH6 with risk of colorectal adenomas and tumors and with somatic mutations in patients with Lynch syndrome. Gastroenterology 2020;158:1326–1333 [DOI] [PubMed] [Google Scholar]
- 38. Ahadova A, von Knebel Doeberitz M, Bläker H, Kloor M. CTNNB1-mutant colorectal carcinomas with immediate invasive growth: a model of interval cancers in Lynch syndrome. Fam Cancer 2016;15:579–586 [DOI] [PubMed] [Google Scholar]
- 39. Kloor M, Huth C, Voigt AY, Benner A, Schirmacher P, von Knebel Doeberitz Met al. Prevalence of mismatch repair-deficient crypt foci in Lynch syndrome: a pathological study. Lancet Oncol 2012;13:598–606 [DOI] [PubMed] [Google Scholar]
- 40. Wirta E-V, Seppälä T, Friman M, Väyrynen J, Ahtiainen M, Kautiainen Het al. Immunoscore in mismatch repair-proficient and -deficient colon cancer. J Pathol Clin Res 2017;3:203–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bohaumilitzky L, Kluck K, Hüneburg R, Gallon R, Nattermann J, Kirchner Met al. The different immune profiles of normal colonic mucosa in cancer-free Lynch syndrome carriers and Lynch syndrome colorectal cancer patients. Gastroenterology 2022;162:907–919.e10 [DOI] [PubMed] [Google Scholar]
- 42. ten Broeke SW, Brohet RM, Tops CM, van der Klift HM, Velthuizen ME, Bernstein Iet al. Lynch syndrome caused by germline PMS2 mutations: delineating the cancer risk. J Clin Oncol 2015;33:319–325 [DOI] [PubMed] [Google Scholar]
- 43. ten Broeke SW, van Bavel TC, Jansen AML, Gómez-García E, Hes FJ, van Hest LPet al. Molecular background of colorectal tumors from patients with Lynch syndrome associated with germline variants in PMS2. Gastroenterology 2018;155:844–851 [DOI] [PubMed] [Google Scholar]
- 44. Helderman NC, Bajwa-ten Broeke SW, Morreau H, Suerink M, Terlouw D, van der Werf-’ t Lam ASet al. The diverse molecular profiles of lynch syndrome-associated colorectal cancers are (highly) dependent on underlying germline mismatch repair mutations. Crit Rev Oncol Hematol 2021;163:103338. [DOI] [PubMed] [Google Scholar]
- 45. Dominguez-Valentin M, Sampson JR, Møller P, Seppälä TT; PLSD Collaborators . Analysis in the Prospective Lynch Syndrome Database identifies sarcoma as part of the Lynch syndrome tumor spectrum. Int J Cancer 2021;148:512–513 [DOI] [PubMed] [Google Scholar]
- 46. Broeke SWT, Klift HMV, Tops CMJ, Aretz S, Bernstein I, Buchanan DDet al. Cancer risks for PMS2-associated Lynch syndrome. J Clin Oncol 2018;36:2961–2968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lynch HT, Smyrk TC, Watson P, Lanspa SJ, Lynch JF, Lynch PMet al. Genetics, natural history, tumor spectrum, and pathology of hereditary nonpolyposis colorectal cancer: an updated review. Gastroenterology 1993;104:1535–1549 [DOI] [PubMed] [Google Scholar]
- 48. Umar A, Boland CR, Terdiman JP, Syngal S, de la Chapelle A, Rüschoff Jet al. Revised Bethesda guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst 2004;96:261–268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ramsey SD, Clarke L, Etzioni R, Higashi M, Berry K, Urban N. Cost-effectiveness of microsatellite instability screening as a method for detecting hereditary nonpolyposis colorectal cancer. Ann Intern Med 2001;135:577–588 [DOI] [PubMed] [Google Scholar]
- 50. Giardiello FM, Allen JI, Axilbund JE, Boland CR, Burke CA, Burt RWet al. Guidelines on genetic evaluation and management of Lynch syndrome: a consensus statement by the US Multi-Society Task Force on colorectal cancer. Am J Gastroenterol 2014;109:1159–1179 [DOI] [PubMed] [Google Scholar]
- 51. Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring ADet al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med 2015;372:2509–2520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Diaz LA, Shiu K-K, Kim T-W, Jensen BV, Jensen LH, Punt Cet al. Pembrolizumab versus chemotherapy for microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer (KEYNOTE-177): final analysis of a randomised, open-label, phase 3 study. Lancet Oncol 2022;23:659–670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Syngal S, Brand RE, Church JM, Giardiello FM, Hampel HL, Burt RW. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol 2015;110:223–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Vilkin A, Leibovici-Weissman Y, Halpern M, Morgenstern S, Brazovski E, Gingold-Belfer Ret al. Immunohistochemistry staining for mismatch repair proteins: the endoscopic biopsy material provides useful and coherent results. Hum Pathol 2015;46:1705–1711 [DOI] [PubMed] [Google Scholar]
- 55. Seppälä TT, Latchford A, Negoi I, Sampaio Soares A, Jimenez-Rodriguez R, Sánchez-Guillén Let al. European guidelines from the EHTG and ESCP for Lynch syndrome: an updated third edition of the Mallorca guidelines based on gene and gender. Br J Surg 2021;108:484–498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Møller P, Seppälä T, Bernstein I, Holinski-Feder E, Sala P, Evans DGet al. Incidence of and survival after subsequent cancers in carriers of pathogenic MMR variants with previous cancer: a report from the Prospective Lynch Syndrome Database. Gut 2017;66:1657–1664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Win AK, Parry S, Parry B, Kalady MF, Macrae FA, Ahnen DJet al. Risk of metachronous colon cancer following surgery for rectal cancer in mismatch repair gene mutation carriers. Ann Surg Oncol 2013;20:1829–1836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Parry S, Win AK, Parry B, Macrae FA, Gurrin LC, Church JMet al. Metachronous colorectal cancer risk for mismatch repair gene mutation carriers: the advantage of more extensive colon surgery. Gut 2011;60:950–957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Anele CC, Adegbola SO, Askari A, Rajendran A, Clark SK, Latchford Aet al. Risk of metachronous colorectal cancer following colectomy in Lynch syndrome: a systematic review and meta-analysis. Color Dis 2017;19:528–536 [DOI] [PubMed] [Google Scholar]
- 60. Renkonen-Sinisalo L, Seppälä TT, Järvinen HJ, Mecklin J-P. Subtotal colectomy for colon cancer reduces the need for subsequent surgery in Lynch syndrome. Dis Colon Rectum 2017;60:792–799 [DOI] [PubMed] [Google Scholar]
- 61. Herzig D, Hardimann K, Weiser M, Yu N, Paquette I, Feingold DLet al. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the management of inherited polyposis syndromes. Dis Colon Rectum 2017;60:881–894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Ribic CM, Sargent DJ, Moore MJ, Thibodeau SN, French AJ, Goldberg RMet al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med 2003;349:247–257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sargent DJ, Marsoni S, Monges G, Thibodeau SN, Labianca R, Hamilton SRet al. Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer. J Clin Oncol 2010;28:3219–3226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. André T, Shiu K-K, Kim TW, Jensen BV, Jensen LH, Punt Cet al. Pembrolizumab in microsatellite-instability-high advanced colorectal cancer. N Engl J Med 2020;383:2207–2218 [DOI] [PubMed] [Google Scholar]
- 65. Casak SJ, Marcus L, Fashoyin-Aje L, Mushti SL, Cheng J, Shen Y-Let al. FDA Approval Summary: Pembrolizumab for the first-line treatment of patients with MSI-H/dMMR advanced unresectable or metastatic colorectal carcinoma. Clin Cancer Res 2021;27:4680–4684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Cercek A, Lumish M, Sinopoli J, Weiss J, Shia J, Lamendola-Essel Met al. PD-1 blockade in mismatch repair-deficient, locally advanced rectal cancer. N Engl J Med 2022;386:2363–2376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Chalabi M, Fanchi LF, Dijkstra KK, Van den Berg JG, Aalbers AG, Sikorska Ket al. Neoadjuvant immunotherapy leads to pathological responses in MMR-proficient and MMR-deficient early-stage colon cancers. Nat Med 2020;26:566–576 [DOI] [PubMed] [Google Scholar]
- 68. Chalabi M, Verschoor YL, van den Berg J, Sikorska K, Beets G, Lent AVet al. LBA7—Neoadjuvant immune checkpoint inhibition in locally advanced MMR-deficient colon cancer: the NICHE-2 study. Ann Oncol 2022;33(Suppl 7):S808–S869 [Google Scholar]
- 69. Järvinen HJ, Aarnio M, Mustonen H, Aktan-Collan K, Aaltonen LA, Peltomäki Pet al. Controlled 15-year trial on screening for colorectal cancer in families with hereditary nonpolyposis colorectal cancer. Gastroenterology 2000;118:829–834 [DOI] [PubMed] [Google Scholar]
- 70. Järvinen HJ, Mecklin JP, Sistonen P. Screening reduces colorectal cancer rate in families with hereditary nonpolyposis colorectal cancer. Gastroenterology 1995;108:1405–1411 [DOI] [PubMed] [Google Scholar]
- 71. Seppälä T, Pylvänäinen K, Evans DG, Järvinen H, Renkonen-Sinisalo L, Bernstein Iet al. Colorectal cancer incidence in path_MLH1 carriers subjected to different follow-up protocols: a Prospective Lynch Syndrome Database report. Hered Cancer Clin Pract 2017;15:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Seppälä TT, Ahadova A, Dominguez-Valentin M, Macrae F, Evans DG, Therkildsen Cet al. Lack of association between screening interval and cancer stage in Lynch syndrome may be accounted for by over-diagnosis; a prospective Lynch syndrome database report. Hered Cancer Clin Pract 2019;17:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Kang YJ, Caruana M, McLoughlin K, Killen J, Simms K, Taylor Net al. The predicted effect and cost-effectiveness of tailoring colonoscopic surveillance according to mismatch repair gene in patients with Lynch syndrome. Genet Med 2022;24:1831–1846 [DOI] [PubMed] [Google Scholar]
- 74. Dominguez-Valentin M, Seppälä TT, Sampson JR, Macrae F, Winship I, Evans DGet al. Survival by colon cancer stage and screening interval in Lynch syndrome: a prospective Lynch syndrome database report. Hered Cancer Clin Pract 2019;17:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Burn J, Sheth H, Elliott F, Reed L, Macrae F, Mecklin Jet al. Cancer prevention with aspirin in hereditary colorectal cancer (Lynch syndrome), 10-year follow-up and registry-based 20-year data in the CAPP2 study: a double-blind, randomised, placebo-controlled trial. Lancet 2020;395:1855–1863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Burn J, Gerdes AM, MacRae F, Mecklin JP, Moeslein G, Olschwang Set al. Long-term effect of aspirin on cancer risk in carriers of hereditary colorectal cancer: an analysis from the CAPP2 randomised controlled trial. Lancet 2011;378:2081–2087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Yurgelun MB, Chan AT. Aspirin for Lynch syndrome: a legacy of prevention. Lancet 2020;395:1817–1818 [DOI] [PubMed] [Google Scholar]
- 78. Half E, Bercovich D, Rozen P. Familial adenomatous polyposis. Orphanet J Rare Dis 2009;4:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Mulvihill JJ. The frequency of hereditary large bowel cancer. Prog Clin Biol Res 1983;115:61–75 [PubMed] [Google Scholar]
- 80. Grover S, Kastrinos F, Steyerberg EW, Cook EF, Dewanwala A, Burbidge LAet al. Prevalence and phenotypes of APC and MUTYH mutations in patients with multiple colorectal adenomas. JAMA 2012;308:485–492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Bisgaard ML, Fenger K, Bülow S, Niebuhr E, Mohr J. Familial adenomatous polyposis (FAP): frequency, penetrance, and mutation rate. Hum Mutat 1994;3:121–125 [DOI] [PubMed] [Google Scholar]
- 82. Sarvepalli S, Burke CA, Monachese M, Lopez R, Leach BH, Laguardia Let al. Web-based model for predicting time to surgery in young patients with familial adenomatous polyposis: an internally validated study. Am J Gastroenterol 2018;113:1881–1890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Knudsen AL, Bülow S, Tomlinson I, Möslein G, Heinimann K, Christensen IJet al. Attenuated familial adenomatous polyposis: results from an international collaborative study. Colorectal Dis 2010;12:e243–e249 [DOI] [PubMed] [Google Scholar]
- 84. Minde DP, Anvarian Z, Rüdiger SG, Maurice MM. Messing up disorder: how do missense mutations in the tumor suppressor protein APC lead to cancer? Mol Cancer 2011;10:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Vasen HFA, Möslein G, Alonso A, Aretz S, Bernstein I, Bertario Let al. Guidelines for the clinical management of familial adenomatous polyposis (FAP). Gut 2008;57:704–713 [DOI] [PubMed] [Google Scholar]
- 86. Warrier SK, Kalady MF. Familial adenomatous polyposis: challenges and pitfalls of surgical treatment. Clin Colon Rectal Surg 2012;25:83–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Aoun RJN, Kalady MF. The importance of genetics for timing and extent of surgery in inherited colorectal cancer syndromes. Surg Oncol 2022;43:101765. [DOI] [PubMed] [Google Scholar]
- 88. Steinbach G, Lynch PM, Phillips RK, Wallace MH, Hawk E, Gordon GBet al. The effect of celecoxib, a cyclooxygenase-2 inhibitor, in familial adenomatous polyposis. N Engl J Med 2000;342:1946–1952 [DOI] [PubMed] [Google Scholar]
- 89. Bohan PM K, Mankaney G, Vreeland TJ, Chick RC, Hale DF, Cindass JLet al. Chemoprevention in familial adenomatous polyposis: past, present and future. Fam Cancer 2021;20:23–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Valle L. Recent discoveries in the genetics of familial colorectal cancer and polyposis. Clin Gastroenterol Hepatol 2017;15:809–819 [DOI] [PubMed] [Google Scholar]
- 91. Cleary SP, Cotterchio M, Jenkins MA, Kim H, Bristow R, Green Ret al. Germline MutY human homologue mutations and colorectal cancer: a multisite case-control study. Gastroenterology 2009;136:1251–1260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Ruggieri V, Pin E, Russo MT, Barone F, Degan P, Sanchez Met al. Loss of MUTYH function in human cells leads to accumulation of oxidative damage and genetic instability. Oncogene 2013;32:4500–4508 [DOI] [PubMed] [Google Scholar]
- 93. Lubbe SJ, Di Bernardo MC, Chandler IP, Houlston RS. Clinical implications of the colorectal cancer risk associated with MUTYH mutation. J Clin Oncol 2009;27:3975–3980 [DOI] [PubMed] [Google Scholar]
- 94. van Leerdam ME, Roos VH, van Hooft JE, Dekker E, Jover R, Kaminski MFet al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 2019;51:877–895 [DOI] [PubMed] [Google Scholar]
- 95. Aelvoet AS, Buttitta F, Ricciardiello L, Dekker E. Management of familial adenomatous polyposis and MUTYH-associated polyposis; new insights. Best Pract Res Clin Gastroenterol 2022;58–59:101793. [DOI] [PubMed] [Google Scholar]
- 96. Palles C, Martin L, Domingo E, Chegwidden L, McGuire J, Cuthill Vet al. The clinical features of polymerase proof-reading associated polyposis (PPAP) and recommendations for patient management. Fam Cancer 2022;21:197–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Boland CR, Idos GE, Durno C, Giardiello FM, Anderson JC, Burke CAet al. Diagnosis and management of cancer risk in the gastrointestinal hamartomatous polyposis syndromes: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology 2022;162:2063–2085 [DOI] [PubMed] [Google Scholar]
- 98. Giardiello FM, Brensinger JD, Tersmette AC, Goodman SN, Petersen GM, Booker S Vet al. Very high risk of cancer in familial Peutz-Jeghers syndrome. Gastroenterology 2000;119:1447–1453 [DOI] [PubMed] [Google Scholar]
- 99. Brosens LAA, van Hattem A, Hylind LM, Iacobuzio-Donahue C, Romans KE, Axilbund Jet al. Risk of colorectal cancer in juvenile polyposis. Gut 2007;56:965–967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Yang J, Gurudu SR, Koptiuch C, Agrawal D, Buxbaum JL, Abbas Fehmi SMet al. American Society for Gastrointestinal Endoscopy guideline on the role of endoscopy in familial adenomatous polyposis syndromes. Gastrointest Endosc 2020;91:963–982.e2 [DOI] [PubMed] [Google Scholar]
- 101. Latchford AR, Clark SK. Gastrointestinal aspects of Peutz-Jeghers syndrome. Best Pract Res Clin Gastroenterol 2022;58–59:101789. [DOI] [PubMed] [Google Scholar]
- 102. Wagner A, Aretz S, Auranen A, Bruno MJ, Cavestro GM, Crosbie EJet al. The management of Peutz-Jeghers syndrome: European Hereditary Tumour Group (EHTG) guideline. J Clin Med 2021;10:473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. D’Ermo G, Genuardi M. Gastrointestinal manifestations in PTEN hamartoma tumor syndrome. Best Pract Res Clin Gastroenterol 2022;58–59:101792. [DOI] [PubMed] [Google Scholar]
- 104. Dal Buono A, Gaiani F, Poliani L, Laghi L. Juvenile polyposis syndrome: an overview. Best Pract Res Clin Gastroenterol 2022;58–59:101799. [DOI] [PubMed] [Google Scholar]
- 105. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal Aet al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021;71:209–249 [DOI] [PubMed] [Google Scholar]
- 106. Cisło M, Filip AA, Arnold Offerhaus GJ, Ciseł B, Rawicz-Pruszyński K, Skierucha Met al. Distinct molecular subtypes of gastric cancer: from Laurén to molecular pathology. Oncotarget 2018;9:19427–19442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Wong MCS, Huang J, Chan PSF, Choi P, Lao XQ, Chan SMet al. Global incidence and mortality of gastric cancer, 1980–2018. JAMA Netw Open 2021;4:e2118457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Norwood DA, Montalvan EE, Dominguez RL, Morgan DR. Gastric cancer: emerging trends in prevention, diagnosis, and treatment. Gastroenterol Clin North Am 2022;51:501–518 [DOI] [PubMed] [Google Scholar]
- 109. van der Post RS, Oliveira C, Guilford P, Carneiro F. Hereditary gastric cancer: what’s new? Update 2013–2018. Fam Cancer 2019;18:363–367 [DOI] [PubMed] [Google Scholar]
- 110. Xicola RM, Li S, Rodriguez N, Reinecke P, Karam R, Speare Vet al. Clinical features and cancer risk in families with pathogenic CDH1 variants irrespective of clinical criteria. J Med Genet 2019;56:838–843 [DOI] [PubMed] [Google Scholar]
- 111. Roberts ME, Ranola JMO, Marshall ML, Susswein LR, Graceffo S, Bohnert Ket al. Comparison of CDH1 penetrance estimates in clinically ascertained families vs families ascertained for multiple gastric cancers. JAMA Oncol 2019;5:1325–1331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Coudert M, Drouet Y, Delhomelle H, Svrcek M, Benusiglio PR, Coulet Fet al. First estimates of diffuse gastric cancer risks for carriers of CTNNA1 germline pathogenic variants. J Med Genet 2022;59:1189–1195 [DOI] [PubMed] [Google Scholar]
- 113. Kim W, Kidambi T, Lin J, Idos G. Genetic syndromes associated with gastric cancer. Gastrointest Endosc Clin N Am 2022;32:147–162 [DOI] [PubMed] [Google Scholar]
- 114. Carvalho J, Oliveira P, Senz J, São José C, Hansford S, Teles SPet al. Redefinition of familial intestinal gastric cancer: clinical and genetic perspectives. J Med Genet 2021;58:1–11 [DOI] [PubMed] [Google Scholar]
- 115. Correa P. Human gastric carcinogenesis: a multistep and multifactorial process–first American Cancer Society Award Lecture on Cancer Epidemiology and Prevention. Cancer Res 1992;52:6735–6740 [PubMed] [Google Scholar]
- 116. Waldum H, Fossmark R. Gastritis, gastric polyps and gastric cancer. Int J Mol Sci 2021;22:6548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Venerito M, Vasapolli R, Rokkas T, Malfertheiner P. Gastric cancer: epidemiology, prevention, and therapy. Helicobacter 2018;23(Suppl 1):e12518. [DOI] [PubMed] [Google Scholar]
- 118. Choi IJ, Kim CG, Lee JY, Kim Y-I, Kook M-C, Park Bet al. Family history of gastric cancer and Helicobacter pylori treatment. N Engl J Med 2020;382:427–436 [DOI] [PubMed] [Google Scholar]
- 119. Lee Y-C, Chiang T-H, Chou C-K, Tu Y-K, Liao W-C, Wu M-Set al. Association between Helicobacter pylori eradication and gastric cancer incidence: a systematic review and meta-analysis. Gastroenterology 2016;150:1113–1124.e5 [DOI] [PubMed] [Google Scholar]
- 120. Cancer Genome Atlas Research Network . Comprehensive molecular characterization of gastric adenocarcinoma. Nature 2014;513:202–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Blair VR, McLeod M, Carneiro F, Coit DG, D’Addario JL, van Dieren JMet al. Hereditary diffuse gastric cancer: updated clinical practice guidelines. Lancet Oncol 2020;21:e386–e397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. NCCN . National Comprehensive Cancer Network—Gastric Cancer, Version 2.2022. 2022
- 123. Powers JM, Ebrahimzadeh JE, Katona BW. Genetic testing for hereditary gastrointestinal cancer syndromes: interpreting results in today’s practice. Curr Treat Options Gastroenterol 2019;17:636–649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Curtin BF, Gamble LA, Schueler SA, Ruff SM, Quezado M, Miettinen Met al. Enhanced endoscopic detection of occult gastric cancer in carriers of pathogenic CDH1 variants. J Gastroenterol 2021;56:139–146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Kumar S, Farha N, Burke CA, Katona BW. Upper gastrointestinal cancer surveillance in Lynch syndrome. Cancers (Basel) 2022;14:1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. NCCN . NCCN Guidelines—Genetic/Familial High-Risk Assessment: Colorectal, Version 1.2022. 2022
- 127. Kratz CP, Achatz MI, Brugières L, Frebourg T, Garber JE, Greer M-LCet al. Cancer screening recommendations for individuals with Li-Fraumeni syndrome. Clin Cancer Res 2017;23:e38–e45 [DOI] [PubMed] [Google Scholar]
- 128. Caldas C, Carneiro F, Lynch HT, Yokota J, Wiesner GL, Powell SMet al. Familial gastric cancer: overview and guidelines for management. J Med Genet 1999;36:873–880 [PMC free article] [PubMed] [Google Scholar]
- 129. Hansford S, Kaurah P, Li-Chang H, Woo M, Senz J, Pinheiro Het al. Hereditary diffuse gastric cancer syndrome: CDH1 mutations and beyond. JAMA Oncol 2015;1:23–32 [DOI] [PubMed] [Google Scholar]
- 130. Lobo S, Benusiglio PR, Coulet F, Boussemart L, Golmard L, Spier Iet al. Cancer predisposition and germline CTNNA1 variants. Eur J Med Genet 2021;64:104316. [DOI] [PubMed] [Google Scholar]
- 131. Majewski IJ, Kluijt I, Cats A, Scerri TS, de Jong D, Kluin RJCet al. An α-E-catenin (CTNNA1) mutation in hereditary diffuse gastric cancer. J Pathol 2013;229:621–629 [DOI] [PubMed] [Google Scholar]
- 132. Pharoah PD, Guilford P, Caldas C; International Gastric Cancer Linkage Consortium . Incidence of gastric cancer and breast cancer in CDH1 (E-cadherin) mutation carriers from hereditary diffuse gastric cancer families. Gastroenterology 2001;121:1348–1353 [DOI] [PubMed] [Google Scholar]
- 133. Clark DF, Michalski ST, Tondon R, Nehoray B, Ebrahimzadeh J, Hughes SKet al. Loss-of-function variants in CTNNA1 detected on multigene panel testing in individuals with gastric or breast cancer. Genet Med 2020;22:840–846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Jacobs MF, Dust H, Koeppe E, Wong S, Mulholland M, Choi E-Yet al. Outcomes of endoscopic surveillance in individuals with genetic predisposition to hereditary diffuse gastric cancer. Gastroenterology 2019;157:87–96 [DOI] [PubMed] [Google Scholar]
- 135. Kumar S, Katona BW, Long JM, Domchek S, Rustgi AK, Roses Ret al. Endoscopic ultrasound has limited utility in diagnosis of gastric cancer in carriers of CDH1 mutations. Clin Gastroenterol Hepatol 2020;18:505–508.e1 [DOI] [PubMed] [Google Scholar]
- 136. Schueler SA, Gamble LA, Curtin BF, Ruff SM, Connolly M, Hannah Cet al. Evaluation of confocal laser endomicroscopy for detection of occult gastric carcinoma in CDH1 variant carriers. J Gastrointest Oncol 2021;12:216–225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Kumar S, Long JM, Ginsberg GG, Katona BW. The role of endoscopy in the management of hereditary diffuse gastric cancer syndrome. World J Gastroenterol 2019;25:2878–2886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Bougen-Zhukov N, Decourtye-Espiard L, Mitchell W, Redpath K, Perkinson J, Godwin Tet al. E-cadherin-deficient cells are sensitive to the multikinase inhibitor dasatinib. Cancers (Basel) 2022;14:1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Decourtye-Espiard L, Bougen-Zhukov N, Godwin T, Brew T, Schulpen E, Black MAet al. E-cadherin-deficient epithelial cells are sensitive to HDAC inhibitors. Cancers (Basel) 2021;14:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Laszkowska M, Silver ER, Schrope B, Kastrinos F, Wang TC, Hur C. Optimal timing of total gastrectomy to prevent diffuse gastric cancer in individuals with pathogenic variants in CDH1. Clin Gastroenterol Hepatol 2020;18:822–829.e4 [DOI] [PubMed] [Google Scholar]
- 141. Vos EL, Salo-Mullen EE, Tang LH, Schattner M, Yoon SS, Gerdes Het al. Indications for total gastrectomy in CDH1 mutation carriers and outcomes of risk-reducing minimally invasive and open gastrectomies. JAMA Surg 2020;155:1050–1057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Stillman MD, Kusche N, Toledano S, Hilfrank KJ, Yoon C, Gabre JTet al. Short and long-term outcomes of prophylactic total gastrectomy in 54 consecutive individuals with germline pathogenic mutations in the CDH1 gene. J Surg Oncol 2022;126:1413–1422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Stanich PP, Elgindi D, Stoffel E, Koeppe E, Bansal A, Stetson Ret al. Colorectal neoplasia in CDH1 pathogenic variant carriers: a multicenter analysis. Am J Gastroenterol 2022;117:1877–1879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Roberts G, Benusiglio PR, Bisseling T, Coit D, Davis JL, Grimes Set al. International Delphi consensus guidelines for follow-up after prophylactic total gastrectomy: the Life after Prophylactic Total Gastrectomy (LAP-TG) study. Gastric Cancer 2022;25:1094–1104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Win AK, Jenkins MA, Dowty JG, Antoniou AC, Lee A, Giles GGet al. Prevalence and penetrance of major genes and polygenes for colorectal cancer. Cancer Epidemiol Biomarkers Prev 2017;26:404–412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Kim J, Braun D, Ukaegbu C, Dhingra TG, Kastrinos F, Parmigiani Get al. Clinical factors associated with gastric cancer in individuals with Lynch syndrome. Clin Gastroenterol Hepatol 2020;18:830–837.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Kumar S, Dudzik CM, Reed M, Long JM, Wangensteen KJ, Katona BW. Upper endoscopic surveillance in Lynch syndrome detects gastric and duodenal adenocarcinomas. Cancer Prev Res (Phila) 2020;13:1047–1054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Farha N, Hrabe J, Sleiman J, Beard J, Lyu R, Bhatt Aet al. Clinically actionable findings on surveillance EGD in asymptomatic patients with Lynch syndrome. Gastrointest Endosc 2022;95:105–114 [DOI] [PubMed] [Google Scholar]
- 149. Ceravolo AH, Yang JJ, Latham A, Markowitz AJ, Shia J, Mermelstein Jet al. Effectiveness of a surveillance program of upper endoscopy for upper gastrointestinal cancers in Lynch syndrome patients. Int J Colorectal Dis 2022;37:231–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Ladigan-Badura S, Vangala DB, Engel C, Bucksch K, Hueneburg R, Perne Cet al. Value of upper gastrointestinal endoscopy for gastric cancer surveillance in patients with Lynch syndrome. Int J Cancer 2021;148:106–114 [DOI] [PubMed] [Google Scholar]
- 151. Vedantam S, Katona BW, Sussman DA, Kumar S. Outcomes of upper endoscopy screening in Lynch syndrome: a meta-analysis. Gastrointest Endosc 2023;97:2–10.e1 [DOI] [PubMed] [Google Scholar]
- 152. Mathers JC, Elliott F, Macrae F, Mecklin J, Möslein G, McRonald FEet al. Cancer prevention with resistant starch in Lynch syndrome patients in the CAPP2-randomized placebo controlled trial: planned 10-year follow-up. Cancer Prev Res (Phila) 2022;15:623–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Puliga E, Corso S, Pietrantonio F, Giordano S. Microsatellite instability in gastric cancer: between lights and shadows. Cancer Treat Rev 2021;95:102175. [DOI] [PubMed] [Google Scholar]
- 154. Mankaney G, Leone P, Cruise M, LaGuardia L, O’Malley M, Bhatt Aet al. Gastric cancer in FAP: a concerning rise in incidence. Fam Cancer 2017;16:371–376 [DOI] [PubMed] [Google Scholar]
- 155. Worthley DL, Phillips KD, Wayte N, Schrader KA, Healey S, Kaurah Pet al. Gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS): a new autosomal dominant syndrome. Gut 2012;61:774–779 [DOI] [PubMed] [Google Scholar]
- 156. Li J, Woods SL, Healey S, Beesley J, Chen X, Lee JSet al. Point mutations in exon 1B of APC reveal gastric adenocarcinoma and proximal polyposis of the stomach as a familial adenomatous polyposis variant. Am J Hum Genet 2016;98:830–842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Foretová L, Navrátilová M, Svoboda M, Grell P, Nemec L, Sirotek Let al. GAPPS—gastric adenocarcinoma and proximal polyposis of the stomach syndrome in 8 families tested at Masaryk Memorial Cancer Institute—prevention and prophylactic gastrectomies. Klin Onkol 2019;32(Suppl 2):109–117 [DOI] [PubMed] [Google Scholar]
- 158. Bianchi LK, Burke CA, Bennett AE, Lopez R, Hasson H, Church JM. Fundic gland polyp dysplasia is common in familial adenomatous polyposis. Clin Gastroenterol Hepatol 2008;6:180–185 [DOI] [PubMed] [Google Scholar]
- 159. Leone PJ, Mankaney G, Sarvapelli S, Abushamma S, Lopez R, Cruise Met al. Endoscopic and histologic features associated with gastric cancer in familial adenomatous polyposis. Gastrointest Endosc 2019;89:961–968 [DOI] [PubMed] [Google Scholar]
- 160. Repak R, Kohoutova D, Podhola M, Rejchrt S, Minarik M, Benesova Let al. The first European family with gastric adenocarcinoma and proximal polyposis of the stomach: case report and review of the literature. Gastrointest Endosc 2016;84:718–725 [DOI] [PubMed] [Google Scholar]
- 161. van Lier MGF, Wagner A, Mathus-Vliegen EMH, Kuipers EJ, Steyerberg EW, van Leerdam ME. High cancer risk in Peutz-Jeghers syndrome: a systematic review and surveillance recommendations. Am J Gastroenterol 2010;105:1258–1264; author reply 1265 [DOI] [PubMed] [Google Scholar]
- 162. Blatter R, Tschupp B, Aretz S, Bernstein I, Colas C, Evans DGet al. Disease expression in juvenile polyposis syndrome: a retrospective survey on a cohort of 221 European patients and comparison with a literature-derived cohort of 473 SMAD4/BMPR1A pathogenic variant carriers. Genet Med 2020;22:1524–1532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. MacFarland SP, Ebrahimzadeh JE, Zelley K, Begum L, Bass LM, Brand REet al. Phenotypic differences in juvenile polyposis syndrome with or without a disease-causing SMAD4/BMPR1A variant. Cancer Prev Res (Phila) 2021;14:215–222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Katona BW, Powers J, McKenna DB, Long JM, Le AN, Hausler Ret al. Upper gastrointestinal cancer risk and surveillance outcomes in Li-Fraumeni syndrome. Am J Gastroenterol 2020;115:2095–2097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Ariffin H, Chan ASL, Oh L, Abd-Ghafar S, Ong GB, Mohamed Met al. Frequent occurrence of gastric cancer in Asian kindreds with Li-Fraumeni syndrome. Clin Genet 2015;88:450–455 [DOI] [PubMed] [Google Scholar]
- 166. Frebourg T, Bajalica Lagercrantz S, Oliveira C, Magenheim R, Evans DG; European Reference Network GENTURIS . Guidelines for the Li-Fraumeni and heritable TP53-related cancer syndromes. Eur J Hum Genet 2020;28:1379–1386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Kuchenbaecker KB, Hopper JL, Barnes DR, Phillips K-A, Mooij TM, Roos-Blom M-Jet al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA 2017;317:2402–2416 [DOI] [PubMed] [Google Scholar]
- 168. Li S, Silvestri V, Leslie G, Rebbeck TR, Neuhausen SL, Hopper JLet al. Cancer risks associated with BRCA1 and BRCA2 pathogenic variants. J Clin Oncol 2022;40:1529–1541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Momozawa Y, Sasai R, Usui Y, Shiraishi K, Iwasaki Y, Taniyama Yet al. Expansion of cancer risk profile for BRCA1 and BRCA2 pathogenic variants. JAMA Oncol 2022;8:871–878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Menezes MCS, Raheem F, Mina L, Ernst B, Batalini F. PARP inhibitors for breast cancer: germline BRCA1/2 and beyond. Cancers (Basel) 2022;14:4332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Ilic I, Ilic M. International patterns in incidence and mortality trends of pancreatic cancer in the last three decades: a joinpoint regression analysis. World J Gastroenterol 2022;28:4698–4715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Kamisawa T, Wood LD, Itoi T, Takaori K. Pancreatic cancer. Lancet 2016;388:73–85 [DOI] [PubMed] [Google Scholar]
- 173. Waddell N, Pajic M, Patch A-M, Chang DK, Kassahn KS, Bailey Pet al. Whole genomes redefine the mutational landscape of pancreatic cancer. Nature 2015;518:495–501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Huang W, Navarro-Serer B, Jeong YJ, Chianchiano P, Xia L, Luchini Cet al. Pattern of invasion in human pancreatic cancer organoids is associated with loss of SMAD4 and clinical outcome. Cancer Res 2020;80:2804–2817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Basturk O, Hong S-M, Wood LD, Adsay NV, Albores-Saavedra J, Biankin AVet al. A revised classification system and recommendations from the Baltimore consensus meeting for neoplastic precursor lesions in the pancreas. Am J Surg Pathol 2015;39:1730–1741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Huang B, Trujillo MA, Fujikura K, Qiu M, Chen F, Felsenstein Met al. Molecular characterization of organoids derived from pancreatic intraductal papillary mucinous neoplasms. J Pathol 2020;252:252–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Canto MI, Almario JA, Schulick RD, Yeo CJ, Klein A, Blackford Aet al. Risk of neoplastic progression in individuals at high risk for pancreatic cancer undergoing long-term surveillance. Gastroenterology 2018;155:740–751.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Saba H, Goggins M. Familial pancreatic cancer. Gastroenterol Clin North Am 2022;51:561–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Klein AP, Brune KA, Petersen GM, Goggins M, Tersmette AC, Offerhaus GJAet al. Prospective risk of pancreatic cancer in familial pancreatic cancer kindreds. Cancer Res 2004;64:2634–2638 [DOI] [PubMed] [Google Scholar]
- 180. Porter N, Laheru D, Lau B, He J, Zheng L, Narang Aet al. Risk of pancreatic cancer in the long-term prospective follow-up of familial pancreatic cancer kindreds. J Natl Cancer Inst 2022;114:1681–1688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Goggins M, Overbeek KA, Brand R, Syngal S, Del Chiaro M, Bartsch DKet al. Management of patients with increased risk for familial pancreatic cancer: updated recommendations from the International Cancer of the Pancreas Screening (CAPS) Consortium. Gut 2020;69:7–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Tempero MA, Malafa MP, Al-Hawary M, Behrman SW, Benson AB, Cardin DBet al. Pancreatic adenocarcinoma, version 2.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 2021;19:439–457 [DOI] [PubMed] [Google Scholar]
- 183. Shindo K, Yu J, Suenaga M, Fesharakizadeh S, Cho C, Macgregor-Das Aet al. Deleterious germline mutations in patients with apparently sporadic pancreatic adenocarcinoma. J Clin Oncol 2017;35:3382–3390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Hu C, Hart SN, Polley EC, Gnanaolivu R, Shimelis H, Lee KYet al. Association between inherited germline mutations in cancer predisposition genes and risk of pancreatic cancer. JAMA 2018;319:2401–2409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Hsu F-C, Roberts NJ, Childs E, Porter N, Rabe KG, Borgida Aet al. Risk of pancreatic cancer among individuals with pathogenic variants in the ATM gene. JAMA Oncol 2021;7:1664–1668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Bennett C, Suguitan M, Abad J, Chawla A. Identification of high-risk germline variants for the development of pancreatic cancer: common characteristics and potential guidance to screening guidelines. Pancreatology 2022;22:719–729 [DOI] [PubMed] [Google Scholar]
- 187. Vasen H, Ibrahim I, Ponce CG, Slater EP, Matthäi E, Carrato Aet al. Benefit of surveillance for pancreatic cancer in high-risk individuals: outcome of long-term prospective follow-up studies from three European expert centers. J Clin Oncol 2016;34:2010–2019 [DOI] [PubMed] [Google Scholar]
- 188. Raimondi S, Lowenfels AB, Morselli-Labate AM, Maisonneuve P, Pezzilli R. Pancreatic cancer in chronic pancreatitis; aetiology, incidence, and early detection. Best Pract Res Clin Gastroenterol 2010;24:349–358 [DOI] [PubMed] [Google Scholar]
- 189. Scholten L, Latenstein AE, Aalfs CM, Bruno MJ, Busch OR, Bonsing BAet al. Prophylactic total pancreatectomy in individuals at high risk of pancreatic ductal adenocarcinoma (PROPAN): systematic review and shared decision-making programme using decision tables. United Eur Gastroenterol J 2020;8:865–877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Enjuto DT, Herrera N, Ceinos C J, Ramos Bonilla A, Llorente-Lázaro R, González Guerreiro Jet al. Hereditary pancreatitis related to SPINK-1 mutation. Is there an increased risk of developing pancreatic cancer? J Gastrointest Cancer 2021; DOI: 10.1007/s12029-021-00729-4[Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 191. Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka Tet al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology 2017;17:738–753 [DOI] [PubMed] [Google Scholar]
- 192. Greenhalf W, Lévy P, Gress T, Rebours V, Brand RE, Pandol Set al. International consensus guidelines on surveillance for pancreatic cancer in chronic pancreatitis. Recommendations from the working group for the international consensus guidelines for chronic pancreatitis in collaboration with the International Association of Pancreatology, the American Pancreatic Association, the Japan Pancreas Society, and European Pancreatic Club. Pancreatology 2020;20:910–918 [DOI] [PubMed] [Google Scholar]
- 193. Dbouk M, Brewer Gutierrez OI, Lennon AM, Chuidian M, Shin EJ, Kamel IRet al. Guidelines on management of pancreatic cysts detected in high-risk individuals: an evaluation of the 2017 Fukuoka guidelines and the 2020 International Cancer of the Pancreas Screening (CAPS) consortium statements. Pancreatology 2021;21:613–621 [DOI] [PubMed] [Google Scholar]
- 194. Dbouk M, Katona BW, Brand RE, Chak A, Syngal S, Farrell JJet al. The multicenter cancer of pancreas screening study: impact on stage and survival. J Clin Oncol 2022;40:3257–3266 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.