Abstract
A rich literature shows that early life conditions shape later life outcomes, including health and migration events. However, analyses of geographic disparities in mortality outcomes focus almost exclusively on contemporaneously measured geographic place (e.g., state of residence at death), thereby potentially conflating the role of early life conditions, migration patterns, and effects of destinations. We use the newly available Mortality Disparities in American Communities (MDAC) dataset, which links respondents in the 2008 ACS to official death records and estimate consequential differences by method of aggregation; the unweighted mean absolute deviation of the difference in life expectancy at age 50 measured by state of birth versus state of residence is 0.58 years for men and 0.40 years for women. These differences are also spatially clustered, and we show that regional inequality in life expectancy is higher based on life expectancies by state of birth, implying that interstate migration mitigates baseline geographical inequality in mortality outcomes. Finally, we assess how state-specific features of in-migration, out-migration, and non-migration together shape measures of mortality disparities by state (of residence), further demonstrating the difficulty of clearly interpreting these widely used measures.
Keywords: Geographic Disparities, Mortality, Place of Birth, Migration
1. Introduction
For decades the U.S. has lagged comparably high-income nations and some middle-income countries on major population health indicators (Kulkarni et al., 2011; NRC and IOM 2013), including life expectancy (Currie et al., 2018). Recently, life expectancy in the U.S. has declined (Case and Deaton, 2015), while mortality inequalities increased (Chetty et al., 2016; Currie and Schwandt, 2016; Dwyer-Lindgren et al., 2017; Ezzati et al., 2008; Montez and Zajacova, 2013; Murray et al., 2006; Wang et al., 2013). Understanding longevity disparities across sub-populations is a critical step in addressing America’s growing health disadvantages.
Geography – encompassing physical, social, and policy environments – is a key axis of mortality disparities (Chetty et al., 2016; Dwyer-Lindgren, 2017; Ezzati et al., 2008; Murray et al., 2006; Wang et al., 2013; Woolf and Schoomaker, 2019). Places have a causal impact on mortality among older adults (Deryugina and Molitor, 2020; Finkelstein et al., 2019) and early life exposures have long-term impacts on subsequent health and longevity (Galobardes et al., 2006; Haas, 2008; Hayward and Gorman, 2004; Palloni, 2008; Schwandt and Von Wachter, 2020; Warner and Hayward, 2006). Linking together these processes between place effects in early life and place effects later in life is migration. Not surprisingly, when faced with circumstances that threaten lives and livelihoods, (e.g. Boustan et al., 2020; Deryugina and Molitor, 2020; Hornbeck, 2012; Hornbeck and Naidu, 2014) or when hoping for better prospects (e.g., Kennan and Walker, 2011), individuals often migrate. Indeed, over thirty percent of US born adults in recent cohorts leave their state of birth (Molloy et al. 2011), raising the possibility of consequential differences in geographic mortality disparities calculations using alternative measures of “place”.
Nonetheless, most research on spatial disparities in mortality implicitly or explicitly aggregates death outcomes by individuals’ place of residence at death (e.g. Dwyer-Lindgren et al. 2017) or at some point during late adulthood (Chetty et al. 2016; Finkelstein et al. 2019). Conceptually, the resulting measurements of spatial disparities are difficult to interpret, as they are a mixture of persistent early life health differences among non-migrants, life course migration patterns (which are shaped by early life health) of both in-migrants and out-migrants, as well as later life health environments (e.g. quality of medical care) of residents. This mixture of factors suggests major hurdles for both learning about the causes of measured spatial disparities and in suggesting remedies for the disparities.
At the same time, a rapidly advancing literature is beginning to tie together (contemporaneously measured) state level factors with geographic disparities in mortality in order to understand key sources of health differences at a point in time and across decades (e.g. Montez et al. 2020. Montez et al. 2019, Montez and Farina 2021). For example, Montez, Beckfield et al. (2020) shows that individuals residing in US state with more liberal policies live over 2 years longer than those living in less liberal states. Data limitations often do not allow these analyses to examine life course exposures to state policies and thus face similar interpretation issues as the larger literature on geographic disparities in (mostly) old age outcomes such as mortality. Specifically, it is difficult to estimate whether the policies causally affect health in old age, since policy environments are chosen through in- and out-migration, and it is also difficult to examine the cumulative and/or dynamic effects of exposures to policies in earlier life on old age mortality without information on where individuals lived in early life.
Indeed, there is limited work that attempts to decompose these factors and no work that contrasts alternative measures of spatial disparities based on place of birth and place of death. A recent exception is Xu et al. (2020), which shows that state of birth explains a similar amount of variation in late-life mortality compared to state of residence, suggesting these two alternative measures of geographic disparities could differ, but does not otherwise directly estimate these measurements nor have large enough samples to fully decompose state-specific migration experiences to understand the sources of these differences. We expand on the empirical findings of Xu et al. (2020) by providing the first quantification of the extent that mortality disparities differ when measured by state of birth vs. state of residence and disentangling the role of in-migrants and out-migrants in explaining the differences across life expectancy measures.
Using the Mortality Disparities in American Communities (MDAC) dataset, we find important differences between measures of life expectancy by states of residence and states of birth. Overall, we find that the method of aggregating individuals by state of residence in later life underestimates the extent of geographical inequality in mortality outcomes compared to the method that aggregates individuals by state of birth.
We then proceed by decomposing the difference in the life expectancy by state of residence and state of birth into the difference in the life expectancy of in-migrants relative to stayers, the difference in the life expectancy of out-migrants relative to stayers, and in- and out-migration rates. Surprisingly, we find that state in- and out-migration rates are largely uncorrelated with the life expectancy of stayers, which is inconsistent with a simple story that migrants select destinations based on health environments. Instead, we show that states both lose healthy out-migrants and gain healthy in-migrants and the net effect of these flows both differs widely across states but also is clustered by region. For example, we find that the mortality risk of in-migrants is substantially lower than the mortality risk of non-migrants in many Southern states, while in many states in the Northeast and Midwest, the mortality risk of these two sub-groups is similar.
Finally, we explore several counterfactual simulations in order to decompose the roles of selective migration and potential “place effects” that aggregate to produce life expectancy differences by state of birth and state of residence. We find evidence that the non-random sorting of migrants to destinations based on state of birth and unobserved mortality risk plays an important role in explaining why life expectancies by state of residence are significantly different than life expectancies by state of birth for certain states. “Place effects” also contribute to the patterns in the data.
The rest of the paper proceeds as follows. Sections 2 and 3 introduce the data and the methods we use to compute life expectancies, respectively. Section 4 describes the differences between life expectancy by state of residence and life expectancy by state of birth. Sections 5–7 present an assessment of our mortality models and robustness checks to validate that our results are not sensitive to alternative assumptions. Section 8 concludes.
2. Data
The analysis of geographical heterogeneities in mortality patterns requires a considerable amount of mortality data across different locations. We make use of the newly available Mortality Disparities in American Communities (MDAC) restricted dataset to perform our analysis. The MDAC dataset links respondents in the 2008 American Community Survey (ACS) to official death records from the National Death Index. The current follow-up period extends until December 31, 2015.
The MDAC dataset contains approximately 4.5 million individuals who were surveyed as part of the original 2008 ACS. More than 300,000 of these individuals die over the next seven years. We restrict our analysis to individuals who were born in one of the fifty U.S. states or in Washington D.C and who were 50+ in 2008.2 We further drop individuals who did not provide valid personal information that allow them to be matched to official death records (dropping ~0.8% of the sample). In total, our sample has close to 1.5 million individuals.
In Table 1 we provide descriptive statistics of our sample by gender, age group, and mortality status by 2015. Since very few prior papers have used the MDAC dataset to analyze mortality (e.g., Miller et al., 2019), Table 1 also presents comparable statistics from the National Vital Statistics System (NVSS) over a roughly similar follow-up period3. Further details about the validation of the MDAC and NVSS samples is available in Appendix A.
Table 1:
Descriptive statistics, by gender and age group
| Panel A: Comparison of mortality rates and population at risk between MDAC and NVSS | ||||||
|---|---|---|---|---|---|---|
| MDAC | Deaths NVSS + 2008 ACS Population | |||||
| Individuals (thousands) | Deaths (thousands) | Mortality rate | Population (millions) | Deaths (millions) | Mortality rate | |
| Panel A: Men | ||||||
| 50–64 | 394 | 31 | 8% | 23.2 | 2.1 | 8.9% |
| 65–79 | 208 | 53 | 25% | 11.1 | 2.9 | 25.8% |
| 80+ | 66 | 42 | 63% | 3.5 | 2.2 | 64.5% |
| All | 668 | 125 | 19%. | 37.7 | 7.2 | 19.0% |
| Panel B: Women | ||||||
| 50–64 | 424 | 22 | 5% | 24.5 | 1.4 | 5.6% |
| 65–79 | 244 | 47 | 19% | 13.1 | 2.6 | 19.8% |
| 80+ | 115 | 66 | 57% | 6.2 | 3.7 | 59.1% |
| All | 782 | 135 | 17% | 43.9 | 7.7 | 17.5% |
| Panel B: Proportion of movers and mortality rates by migration status in 2008 | |||
|---|---|---|---|
| Proportion of stayers | Mortality rate of stayers | Mortality rate of movers | |
| Panel A: Men | |||
| 50–64 | 61% | 8% | 7% |
| 65–79 | 58% | 26% | 24% |
| 80+ | 57% | 63% | 63% |
| All | 59% | 19% | 18% |
| Panel B: Women | |||
| 50–64 | 59% | 5% | 5% |
| 65–79 | 60% | 20% | 19% |
| 80+ | 61% | 58% | 57% |
| All | 59% | 18% | 17% |
Note: Panel A of Table 1 compares descriptive statistics using information of the MDAC and the National Vital Statistics System (NVSS). Individuals that were born or reside outside of the 50 states and D.C. have been excluded from both datasets. Information for the MDAC has been constructed from tables disclosed by the Census with release authorizations: CBDRB-FY19–304 and CBDRB-FY20–092. Given the Census disclosure rules, the MDAC statistics are subject to rounding error. The column of deaths in NVSS correspond to all the deaths registered in the period July 2008 – December 2015. All the deaths that occurred in the first half of 2008 are dropped to account for the fact that the ACS 2008 data was collected in a rolling basis between January and December of 2008. The estimates of population at risk by state, age group, and gender in the NVSS data were generated from the IPUMS version of the 2008 ACS. Panel B of Table 1 further disaggregates mortality rates by migration status at the time of the 2008 ACS interview in the MDAC, depending on whether the individual was surveyed in the same state as their state of birth.
3. Methods: Primary Calculations
Due to the restricted nature of the data, we use “cell counts” as opposed to individual-level data. We construct aggregated death rates from the linked 2008 ACS respondents and official death records from 2008 to 2015 in two different ways. We aggregate individuals based on (1) their state of residence at the time of the 2008 ACS interview or (2) their reported state of birth.4 We further stratify the sample by five-year age group and gender to calculate the raw probability of surviving throughout the 7+-year follow-up period by gender, five-year age group, and either state of residence or state of birth. Using these cells as inputs, we compute period life expectancies at age 50 and age 65 by state of birth and then by state of residence.
The computation of period life expectancies involves two steps. We first need to obtain traditional one-year mortality rates as a function of age from the disclosed mortality probabilities by age group in the follow-up period. To do this, we re-write the probability of surviving throughout the follow-up period for a given age group in terms of one-year mortality rates as a function of age. We further assume that mortality rates grow exponentially with age, which leads us to expressing the probability of surviving throughout the follow-up period across age-groups as a non-linear equation with two parameters.5 We use weighted Non-Linear Least Squares (NLLS) to fit these two parameters for each state of birth and gender and for each state of residence and gender. In total, we run 204 (2 genders × 51 states × 2 aggregation methods) different regressions. After age 90, we impute sex-specific mortality rates that are equal to the observed mortality rates at the national level following the methodology presented in Chetty et al. (2016).6
Next, we apply standard life table formulas to compute life expectancies at age 50 and age 65 from the age schedules of mortality estimated in the first step (Olshansky et al., 1997; Preston et al., 2000). We obtain standard errors for the 204 life expectancy estimates using parametric bootstrap (Chetty et al., 2016). We validate the magnitude of our standard errors by comparing our estimates to estimates that follow the classical approach introduced by Chiang (1984). Further technical details surrounding these computations can be found in Appendix B.7
4. Life expectancies by state of residence and state of birth
Figure 1 displays life expectancy at age 50 for each state (aggregating (1) those born in the state and (2) those who reside in it at the time of their death) using the mortality events that occurred in the period 2008–2015. Panel A compares the two state-based measures for men and Panel B for women. A state would lie on the dashed 45-degree line if the two measures of life expectancy were identical. This would happen, for example, if there was no migration into and out of the state, or if the mortality patterns of in-migrants and out-migrants was the same. States that are located to the right of the 45-degree line are those that have a higher life expectancy when mortality is aggregated by state of birth than by state of residence. Ohio is one such example, for both men and women. The estimated male life expectancy at age 50 by state of birth in Ohio is 30.5 years (s.e. = 0.20), while the estimated male life expectancy by state of residence is 29.6 years (s.e. = 0.15). In contrast, states located to the left of the 45-degree line have a higher life expectancy when individuals are aggregated by location of adult residence than by birth. For example, the estimated life expectancy for males born in Florida is 29.5 years (s.e. = 0.17), while the estimated life expectancy for men residing in Florida is 30.7 years (s.e. = 0.26). These differences of close to one year in life expectancy are significant in both a substantive and statistical sense.
Figure 1:
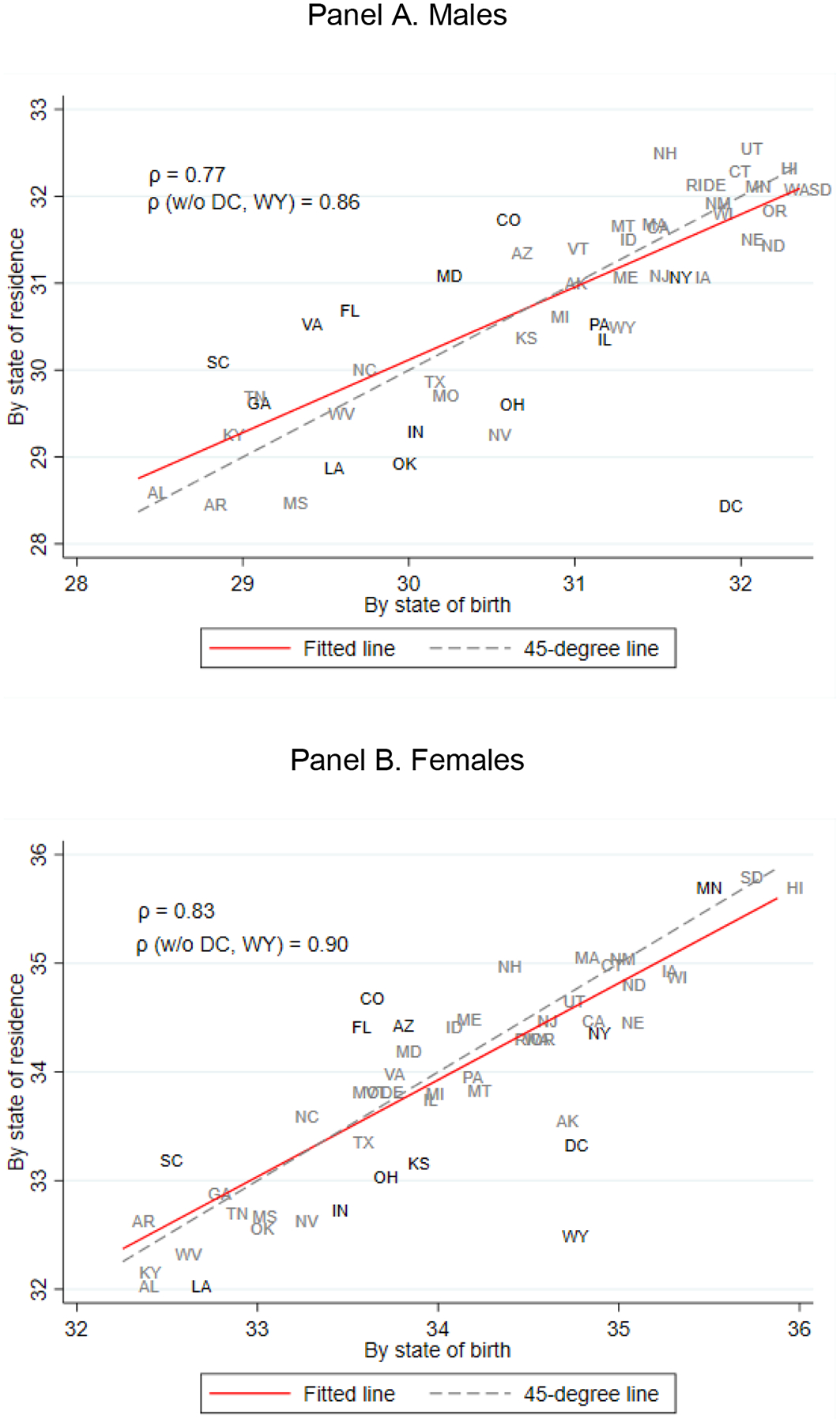
Life expectancies at age 50 by state of birth and state of residence
Note: Figure 1 shows the relationship between life expectancy at age 50 by state of birth and state of residence separately by gender. Life expectancies were constructed using data disclosed from the MDAC dataset with Census disclosure numbers CBDRB-FY19–304 and CBDRB-FY20–092, using the methods explained in the paper and further detailed in Technical Appendix A. Panel A shows the relationship between the two alternative measures of life expectancy at age 50 for men. Panel B shows the same relationship for women. States that have a significant difference between life expectancy measures at the 10% level are marked in black. The rest of the states are shown in gray.
Comparing across panels A and B of Figure 1, the link between the two life expectancy measures is weaker for men than for women. For men, the unweighted (weighted) correlation coefficient between the two measures of life expectancy is equal to 0.77 (0.82).8 In contrast, the unweighted (weighted) correlation coefficient for women is higher and equal to 0.83 (0.91).9 Less susceptible to the presence of outliers, the unweighted (weighted) mean absolute deviation of the difference in the two life expectancy measures across states is equal to 0.58 (0.50) years for men and 0.40 (0.29) years for women. The difference between genders is close to being statistically significant (p-value: 0.06).
Previous literature has shown that the American South has the lowest levels of life expectancy by state of residence (Chetty et al., 2016; Murray et al., 2006; Wang et al., 2013, among many other papers). We confirm this pattern in Panel A of Figure 2, where we show male life expectancies at age 50 by state of residence. In Panel B of Figure 2 we instead show male life expectancies at age 50 by state of birth. To ease the comparison of differences between the maps in Panels A and B, Panel C displays the difference between the two life expectancy measures (state of residence – state of birth) for each state. Panel C shows that the sign of the difference is geographically clustered and varies substantially by Census division. All states in the East North Central, West North Central, and Middle Atlantic divisions except for Minnesota have higher life expectancy point estimates by state of birth than by state of residence. The opposite result is true for almost all states in the South Atlantic and East South Central divisions, which already had the lowest life expectancies by state of residence.
Figure 2:
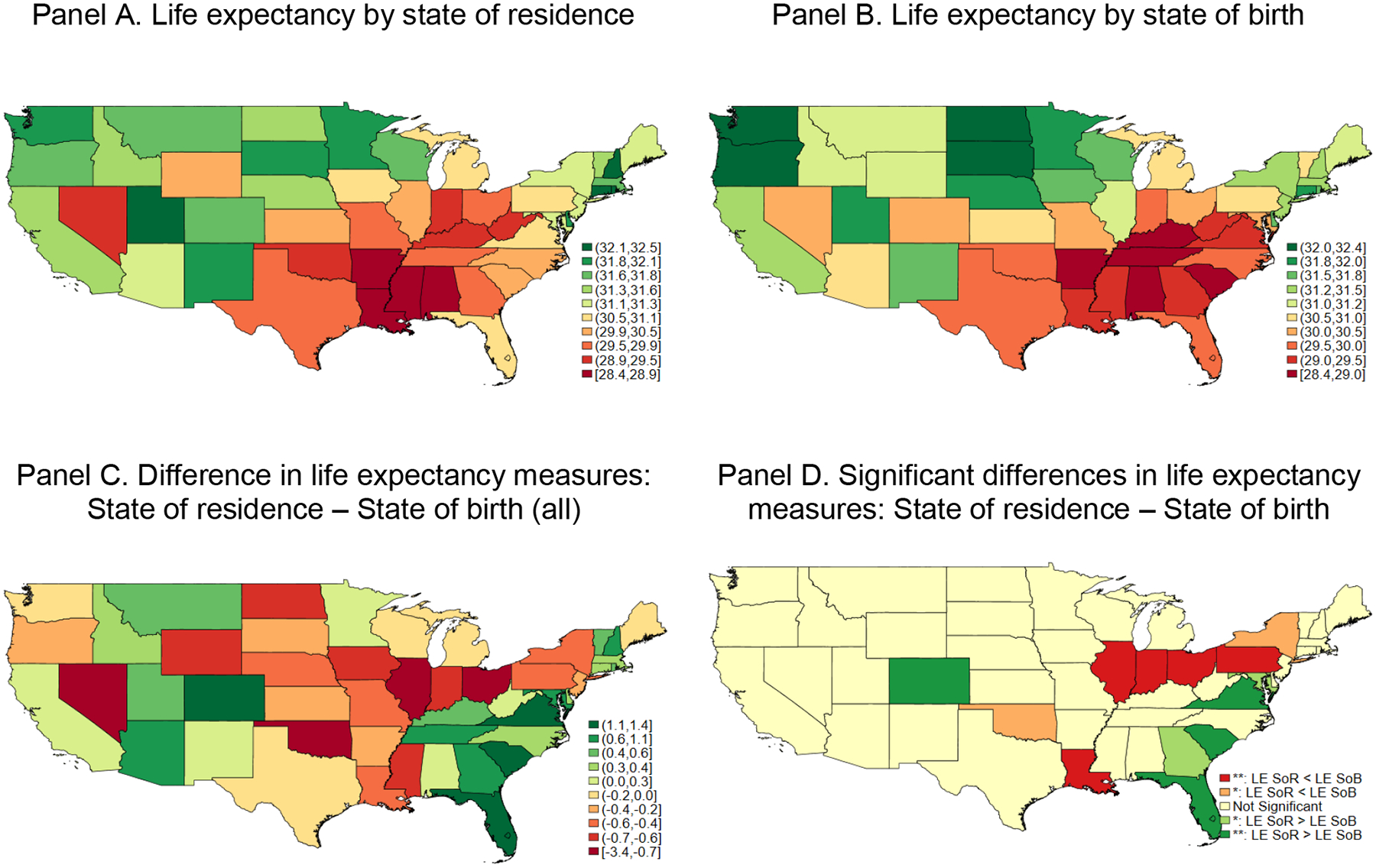
Male life expectancies at age 50, 2008–2015
Note: Panel A of Figure 2 presents male life expectancies at age 50 grouping individuals by their state of residence in 2008, while Panel B of Figure 2 presents life expectancies at age 50 grouping individuals by their state of birth. Panel C of Figure 2 shows the differences between life expectancies by state of residence and life expectancies by state of birth for each of the states. Panel D of Figure 2 shows in red states in which the life expectancy by state of residence is significantly lower than the life expectancy by state of birth at the 5 and 10 percent significance levels. States in which the life expectancy by state of residence is significantly higher than the life expectancy by state of birth at the 5 and 10 significance levels are shown in green.
Thus, the extent of inequality in mortality outcomes across divisions is higher if we measure life expectancy based on state of birth than the typically used state of residence. In Panel D we highlight the states where the difference in life expectancy measures is statistically significant at a 10 percent level. Most of the states that have statistically significant higher life expectancies by state of residence than life expectancies by state of birth are in the South Atlantic division: Florida, Georgia, Maryland, South Carolina, and Virginia. Those where life expectancy is higher when calculated by place of birth are mainly in the East North Central and Middle Atlantic divisions: Illinois, Indiana, New York, Ohio, and Pennsylvania.
In Figure 3 we present life expectancies at age 50 for women. The patterns are similar to those we documented for men, but differences in life expectancy are slightly smaller in magnitude. One potential explanation for this gender difference is that the overall migration rate is higher for men than women. We can directly assess this by analyzing the IPUMS version of the 2008 ACS sample. By the time of the 2008 ACS interview, 41.7 percent of women and 42.1 percent of men ages 50 and above are not residing in their state of birth. Although this difference is statistically significant, it is unlikely to be the driver of the weaker relationship of the two life expectancy measures, as it only represents a 0.4 percentage point increase in the baseline migration probability for women.10 Instead, the relationship between health status and migration decisions might be different by gender. For example, Halliday and Kimmitt (2008) find that a lower reported health status is associated with a lower propensity to migrate for men below 60 years of age but not for women. Thus, different migration motives across genders might help explain why the discrepancies between life expectancy by state of birth and state of residence for women are lower than for men.
Figure 3:
Female life expectancies at age 50, 2008–2015
Note: Panel A of Figure 3 presents female life expectancies at age 50 grouping individuals by their state of residence in 2008, while Panel B of Figure 3 presents life expectancies at age 50 grouping individuals by their state of birth. Panel C of Figure 3 shows the differences between life expectancies by state of residence and life expectancies by state of birth for each of the states. Panel D of Figure 3 shows in red states in which life expectancy by state of residence is significantly lower than life expectancy by state of birth at the 5 and 10 percent significance levels. States in which the life expectancy by state of residence is significantly higher than the life expectancy by state of birth at the 5 and 10 significance levels are shown in green.
Due to disclosure rules for minimum sample sizes in each “cell” for the MDAC dataset, we were unable to consider separately mortality rates for racial minority groups or mortality rates at younger ages. In order to indirectly assess the former, we repeat the above analysis with a sub-sample that excludes Black and Latino individuals and find similar patterns (see Appendix Figure 3).11 In order to consider the possibility of differences in results based on age, we also calculate life expectancies at age 65 for men and women and find very similar patterns at this older age. The relationship between life expectancies at age 65 by state of residence and state of birth is included in Appendix Figure 4. Appendix Figure 5 shows that the disparities across male life expectancies at age 65 are closely linked to geographical regions. Appendix Figure 6 shows the geographical patterns in life expectancies at age 65 for women. Overall, the results are evidence that the empirical patterns in the discrepancies between life expectancy by state of residence and state of birth are not driven by any specific age group or racial/ethnic group.
5. Analysis of sub-populations: Stayers, in-migrants, and out-migrants
Three broad groupings of individuals are considered in the construction of life expectancies by state of residence and state of birth for a given state : individuals who were born in and are residing in by the time of the ACS interview (“stayers”),12 individuals who were born in but are observed in a different state (“out-migrants”), and individuals who were not born in but that are observed in (“in-migrants”). For each state, we estimate life expectancies for the three different sub-groups of individuals. The calculation of life expectancies by state of birth only assigns positive weight to the first two sub-groups, while life expectancies by state of residence only consider stayers and in-migrants. The weights assigned to each sub-group are closely related to the state in-migration and out-migration rates. We pay particular attention to the differences in male life expectancy of out-migrants and in-migrants relative to stayers across states.
We first compute the life expectancy of stayers based on the 2008 ACS matched with official death records. As in the previous analysis, we stratify the stayer population by five-year age group and gender. Based on disclosure requirements, we are unable to report match rates and number of stayers in cells that have fewer than twenty deaths. To obtain reliable life expectancy measures at age 50, we drop states that have missing information in three or more of the eight different age groups.13 We calculate life expectancies at age 50 for stayers using the same two-step approach as before. First, we use a weighted NLLS model based on the Gompertz mortality model to estimate age-specific mortality rates. Then, we follow standard life table procedures to calculate life expectancies in a second step. Appendix B presents the details.
To calculate mortality rates and cell sizes of in-migrants and out-migrants, we combine the information about mortality rates and number of stayers in each cell with our previous data on natives and residents.14 Then, we calculate life expectancies for in-migrants and out-migrants with our two-step estimation strategy.
We re-write the difference in the age-specific mortality rates by state of residence and by state of birth in each state in terms of the mortality rates of stayers, in-migrants, and out-migrants as follows:
Where corresponds to the number of deaths of individuals of sub-population and is the total number of individuals from that sub-population.
Thus, differences in mortality rates by state of residence and state of birth can be decomposed into two additive terms. The first term considers the difference in mortality rates of in-migrants relative to stayers , while the second term considers the difference in mortality rates of out-migrants relative to stayers . The terms are weighted by the in-migration and out-migration rate in that specific age group, respectively.
Life expectancy estimates are calculated from age-specific mortality rates. Even though the previous expression holds with equality for mortality rates, it might not be exact for life expectancies. However, under an assumption that the relative weights of in-migrants and out-migrants do not substantially vary across age groups, the following equation approximately holds:15,16
This equation shows that the difference in life expectancy by state of residence and state of birth can be (approximately) decomposed into two additive terms: 1) the difference in life expectancy between in-migrants and stayers and 2) the difference in life expectancy between out-migrants and stayers. The combination of these two additive terms explains the discrepancy for any given state between life expectancy calculated for residents and life expectancy calculated for those born in the state.17
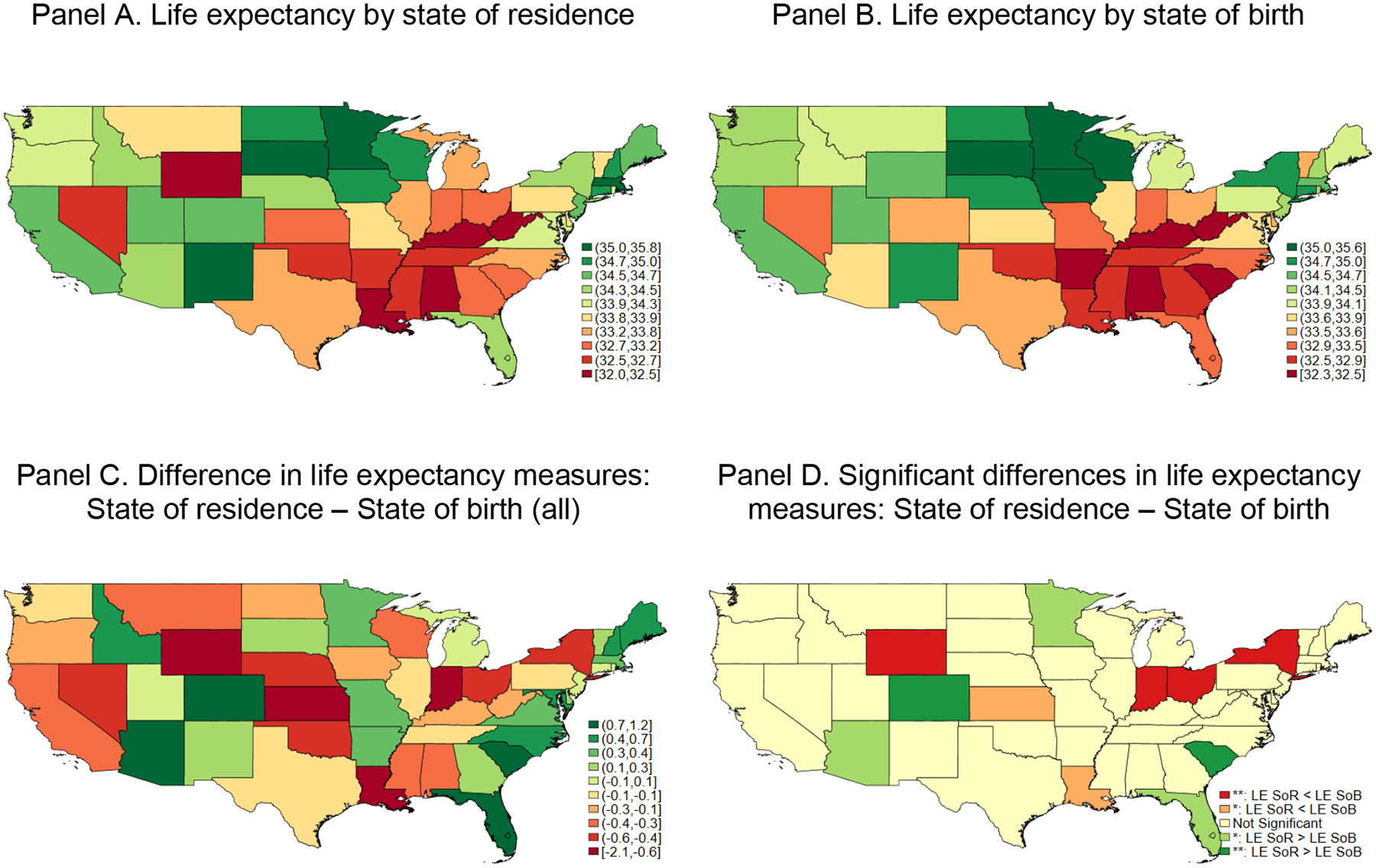
As a first step to determine the contribution of these factors to variation in differences in male life expectancy at age 50 by state of residence and state of birth, Figure 4 plots the relationship between the two factors at the state level,18 showing no significant relationship between the relative mortality advantage of in-migrants and out-migrants. The slope of the fitted line is equal to 0.05 (s.e. 0.09), suggesting that states with higher in-migrant life expectancy are not systematically experiencing out-migrant life expectancy.
Figure 4:
Relationship between the relative mortality advantage of out-migrants and the relative mortality advantage of in-migrants across states
Note: Figure 4 shows the difference in male life expectancy at age 50 of in-migrants relative to stayers on the horizontal axis and the difference in male life expectancy at age 50 of out-migrants relative to stayers on the vertical axis. States are weighted by the inverse variance of the difference between the life expectancy by state of residence and life expectancy by state of birth. States in green (red) have a male life expectancy at age 50 by state of residence that is significantly higher (lower) than the equivalent life expectancy by state of birth. The red dashed line corresponds to the fitted line of the weighted regression at the state level. The line in black corresponds to the weighted mean of the relative advantage of out-migrants (0.69 years).
A second takeaway from Figure 4 is that the cross-state standard deviation in the in-migrant mortality advantage is higher (0.92) than the cross-state standard deviation in the out-migrant mortality advantage (0.67),19 suggesting that a larger component of the difference between life expectancy by state of residence compared to state of birth is differential state gains from in-migrants rather than differential state losses from out-migrants (see Appendix Table 1). Importantly, there is a difference in the right tails of these two distributions. In seven states, the difference in life expectancy of in-migrants and stayers is above 2 years. Six of these seven states are in the South region. In contrast, only Louisiana and Mississippi have an out-migrant mortality advantage that is higher than 2 years.20
Two different mechanisms can be behind the differences in mortality advantage of in-migrants across states—place based selection and causation.21 The first mechanism is ex-ante health advantage of in-migrants relative to stayers, where the difference in mortality risk between in-migrants and the stayer sub-population at the destination at the time of the move is different across states. The second one is the presence of differences in causal “place effects” across locations.22 The interaction between the two can also be relevant. For example, detrimental place effects might have a bigger effect on the mortality outcomes of more vulnerable sub-groups. Thus, place effects might exacerbate or mitigate ex-ante differences in mortality outcomes between sub-groups. While we do not attempt to formally disentangle these two different channels, we provide suggestive evidence below that the selection channel is playing an important role in explaining the cross-state variation in the mortality advantage of in-migrants.
The relationship between the levels of life expectancies of stayers, in-migrants, and out-migrants is also informative. We find that the correlation between the life expectancy of stayers and out-migrants is high and equal to 0.75 for men. In contrast, the correlation between the life expectancy of stayers and in-migrants is lower and equal to 0.55.23,24
In Figure 5 we present the baseline levels of the life expectancy of in-migrants, out-migrants, and stayers for the thirteen states in which the difference between the male life expectancy at age 50 by state of residence and state of birth is statistically significant at a 10 percent significance level. In all selected states except Colorado, the life expectancy of stayers is lower than the life expectancy of out-migrants. This suggests that the “healthy migrant hypothesis” (Palloni and Morenoff 2001) holds in our data, even for the states in the South where the difference between the life expectancy by state of residence and state of birth is positive. However, we do not have information about the health of out-migrants at the time of migration to formally test this hypothesis.
Figure 5:
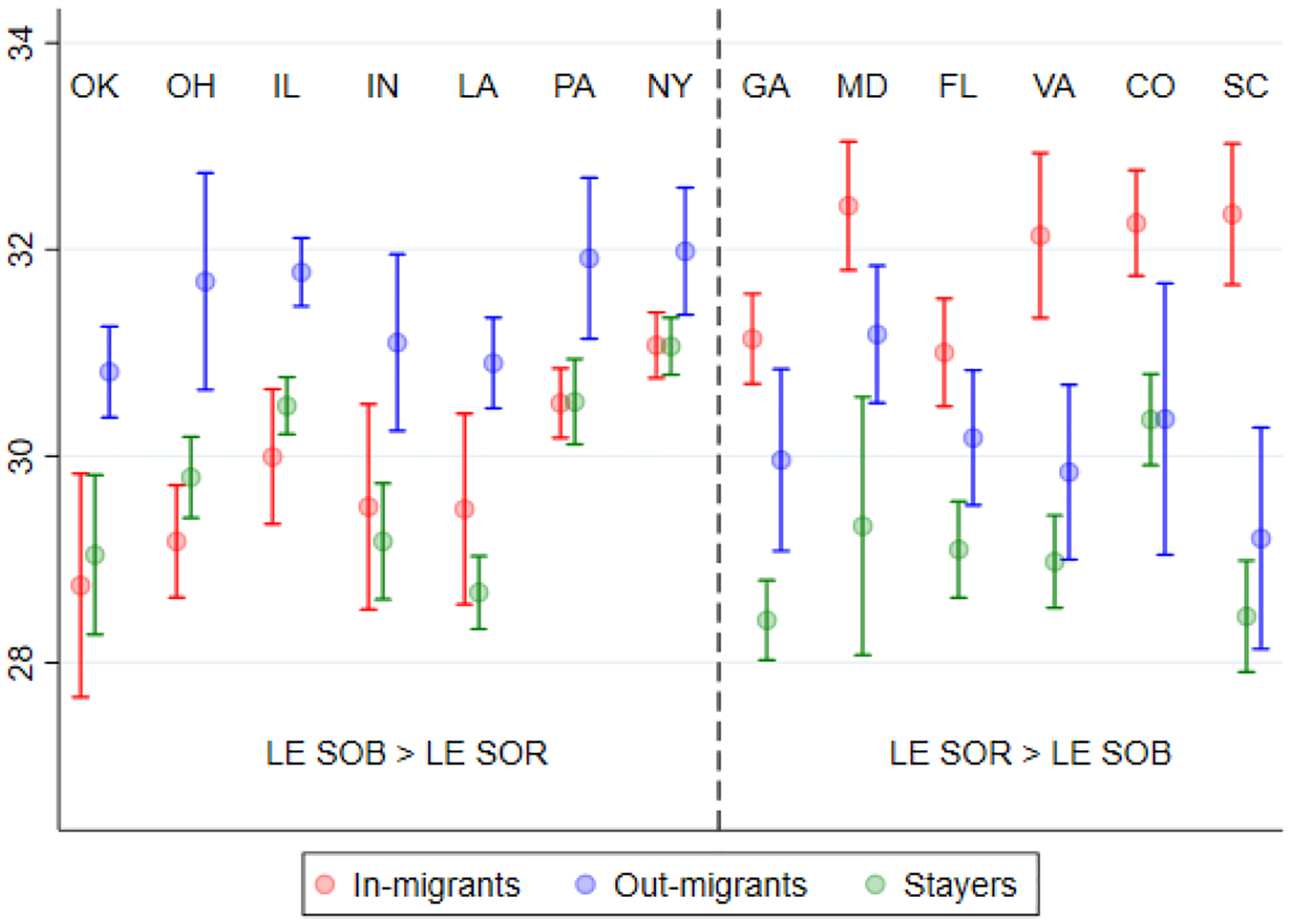
Male life expectancies of stayers, movers-in, and movers-out at age 50 in selected states
Note: Figure 5 shows the male life expectancy at age 50 for stayers, in-migrants, and out-migrants in the 13 states where the difference in life expectancy by state of residence and state of birth is statistically significant at conventional levels. Point estimates and 95% confidence intervals of the life expectancy of each type of individual in each state are also included.
Finally, Figure 5 shows that the life expectancy of stayers is on average lower in the South Atlantic and East South Central states than in the Middle Atlantic and East North Central states. This suggests the underlying causal place effects of states in the South could be more detrimental than in the Midwest and Northeast.25 However, the life expectancy of in-migrants relative to stayers is substantially higher in this set of Southern states. Thus, in-migrants shift up the life expectancy by state of residence in these states. This does not happen in the Middle Atlantic and East North Central states, where the life expectancy of in-migrants and stayers is similar in magnitude.
We are unable to formally quantify the cross-state difference in the relative ex-ante health selection of in-migrants relative to stayers at the time of migration. As mentioned before, the ex-ante differences can be exacerbated if detrimental place effects have a bigger effect on individuals with already vulnerable health status.26 The empirical patterns that we highlighted from Figures 4 and 5 are consistent with a higher ex-ante health selection of in-migrants in Southern states than in Midwestern and Northeast states. If the role of “place effects” was substantial, we would expect to observe a positive correlation between the mortality advantage of in-migrants and out-migrants.27 However, we showed in Figure 4 that these two variables are virtually uncorrelated.
6. Assessing the role of migration flows
In the previous section, we abstracted away from the role of migration in-flows and out-flows and focused entirely on the cross-state variation in mortality differences between in-migrants, out-migrants, and stayers. In this section we further investigate which aspects of migration are descriptively important in explaining the differences between life expectancy by state of residence and by state of birth across states.
Individuals who are born in locations with detrimental “place effects” on health outcomes might be able to mitigate the adverse effects of their place on birth on health by migrating to healthier locations. For example, some research has shown that one important way in which individuals respond to natural disasters like the American Dust Bowl or Hurricane Katrina is by migrating to unaffected locations (Boustan et al., 2020, Hornbeck, 2012; Deryugina and Molitor, 2020). A broader literature has documented that most migration is motivated by employment, education, and family considerations (Wolf and Longingo 2005, Cook 2011, Kaplan and Schulhofer-Wohl 2017), though whether these migration processes would be linked to geographic differences in life expectancy has not been examined.
To understand whether in-migration and out-migration flows appear to be reacting to detrimental place effects on health outcomes, we run descriptive regressions with the following structure, separately for each gender :
where is a migration outcome of interest in state and the explanatory variable is the life expectancy of the sub-population of stayers in state .
Migration patterns might be substantially different for working age population and retirees. For example, return migration might be more prevalent after retirement. We primarily focus on the population that is between 50 and 64 years old by the time of the 2008 ACS interview to mitigate survivorship bias as well as classification error from return migrants. Our outcomes are state out-migration and in-migration rates.
We use the life expectancy of stayers as a proxy for the place effects on health of different states. As has been highlighted in the previous section, life expectancy by state of residence and state of birth are a combination of many different factors, including the life expectancy of stayers, in-migrants, out-migrants, and migration rates. In Panel A of Figure 6 we show the linear relationship between out-migration rates and life expectancy of stayers at age 50 for men. We weigh each state by the inverse variance of the life expectancy of stayers to address the concern that our dependent variable is subject to measurement error and that it is estimated with a different level of precision across states. Finally, we omit the eight states in which the population of stayers is too small to obtain reliable estimates of life expectancy for the stayer sub-population.
Figure 6:
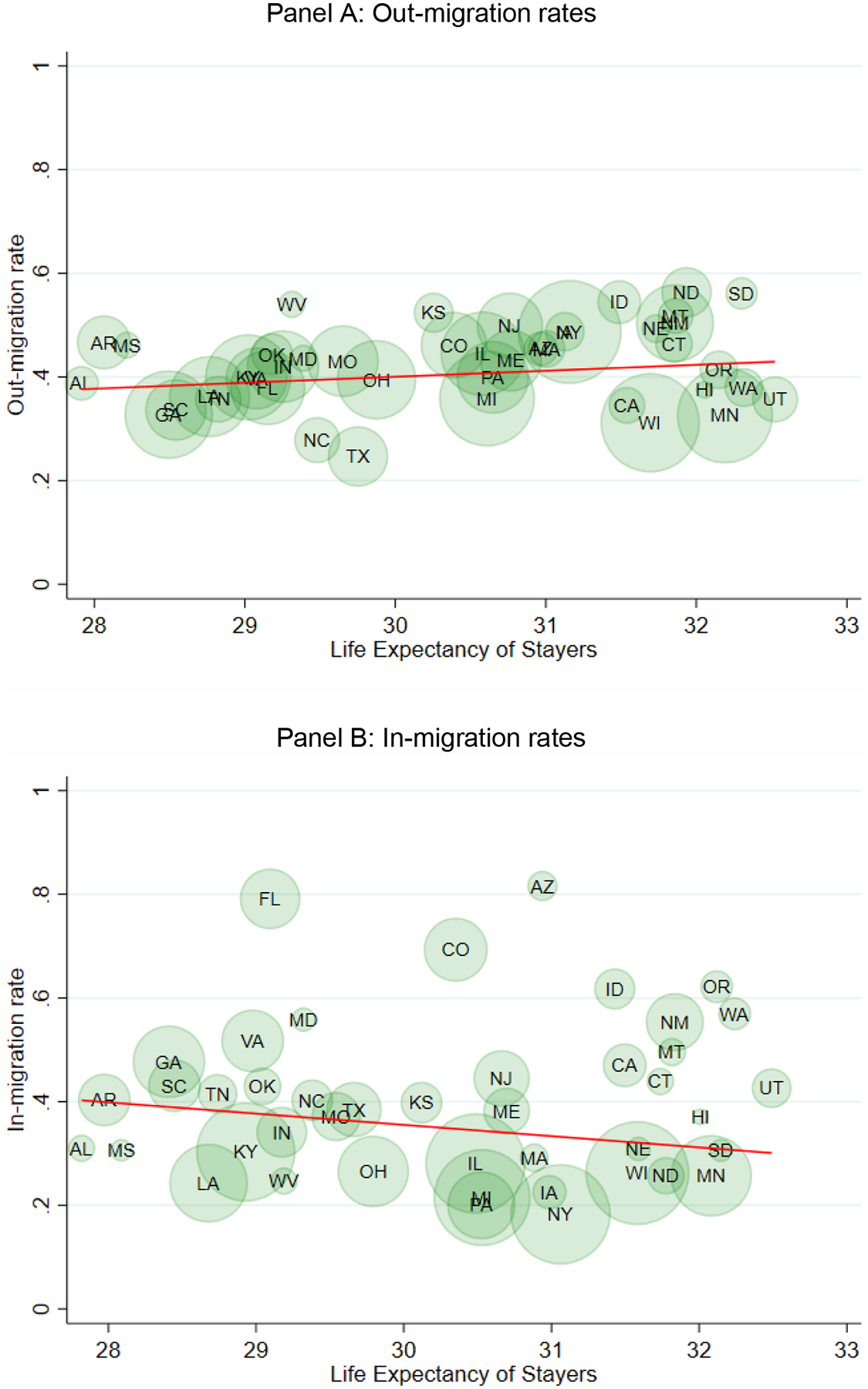
Relationship between life expectancy of male stayers at age 50 and migration rates
Note: Panel A (B) of Figure 6 shows the relationship between male life expectancy of the stayer sub-population at age 50 and out-migration (in-migration) rates at the state level. The out-migration rate of state is calculated as the proportion of 50–64 year-old men that were born in state that are out of their state of birth by the time of the 2008 ACS interview. Similarly, the in-migration rate of state is calculated as the proportion of 50–64 year-old men that are observed in by the time of the ACS interview that were born in a different state. In both panels, states are weighted by the inverse variance of the male life expectancy of stayers at age 50.
As can be seen from Panel A of Figure 6, the relationship between out-migration rates and the life expectancy of stayers is virtually flat.28 The estimated slope is equal to 0.01 (s.e. 0.01). Overall, there is no evidence that out-migration rates are higher in locations where the life expectancy of stayers is lower than average.
In Panel B of Figure 6 we show the relationship between the in-migration rates and life expectancy of stayers. As before, the relationship is flat. The estimated coefficient is equal to −0.02 (s.e. 0.02), and it is not statistically significant. States where stayers have a higher life expectancy at age 50 do not appear to be attracting relatively more immigrants than states with potentially more detrimental place effects.29,30 In unreported results, we verify that this pattern is driven by the White non-Hispanic subpopulation.
Although the results do not consider individual characteristics that might help explain self-selection into migration, the aggregate patterns of in- and out-migration are not consistent with a narrative where net migration flows primarily from locations with lower life expectancy to locations with higher life expectancy. A potential explanation is that individuals give a higher priority to wage differentials and other work amenities over health considerations when deciding where to settle.31 This pattern is consistent with findings from the literature on the rural-urban migration process.
7. Understanding Differences in Place Based Life Expectancy Measures
Even though the magnitudes of the migration flows across states do not appear to be systematically associated with the life expectancy of stayers, migration can still make the interpretation of life expectancies by state of residence difficult. In particular, the representative state of origin and the health composition of who moves in and out of a state relative to the health of the population of stayers may vary substantially across states.
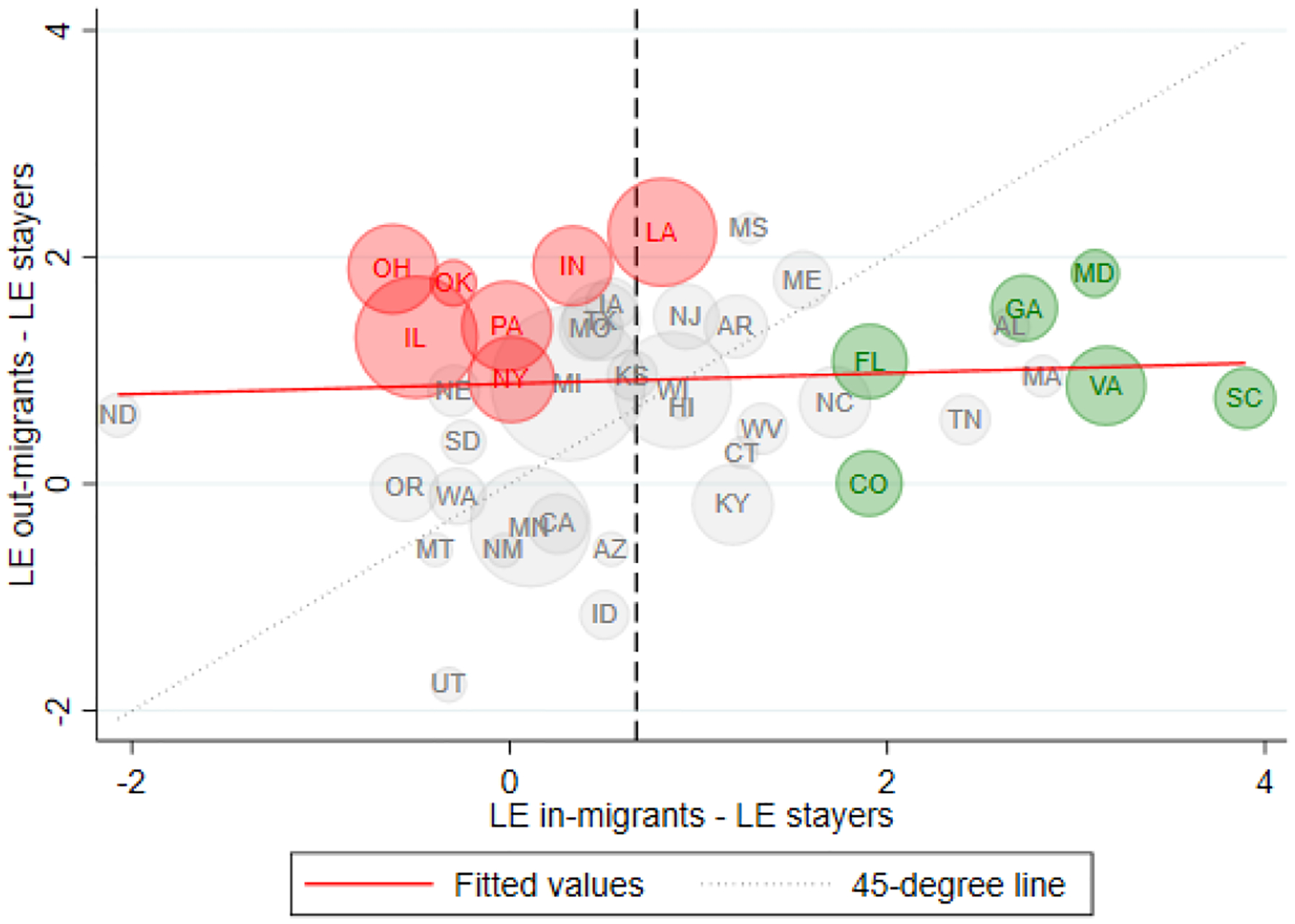
We first describe differences in the states of origin of in-migrants across states by showing the relationship between the life expectancy of male stayers in a given state and a summary measure of the states of origin of its in-migrants in terms of life expectancy. Specifically, for a given state , we weigh the life expectancy of stayers in all other states by the share of in-migrants who come from each state. This measurement does not allow a “healthy migrant” effect at the individual level but focuses only on the composition of in-migrants from “healthy” or “unhealthy” states of origin. We obtain these shares from the IPUMS ACS 2008.32
Panel A of Figure 7 presents the relationship between the life expectancy of stayers and this summary measure of the states of origin of in-migrants. The positive relationship indicates that on average, states with a higher life expectancy of stayers receive in-migrants who come from states of origin where stayers also have high levels of life expectancy. Instead, if destination choice was independent of state of origin, we would expect to observe a flat relationship between the life expectancy of stayers and the representative state of origin of in-migrants.
Figure 7:
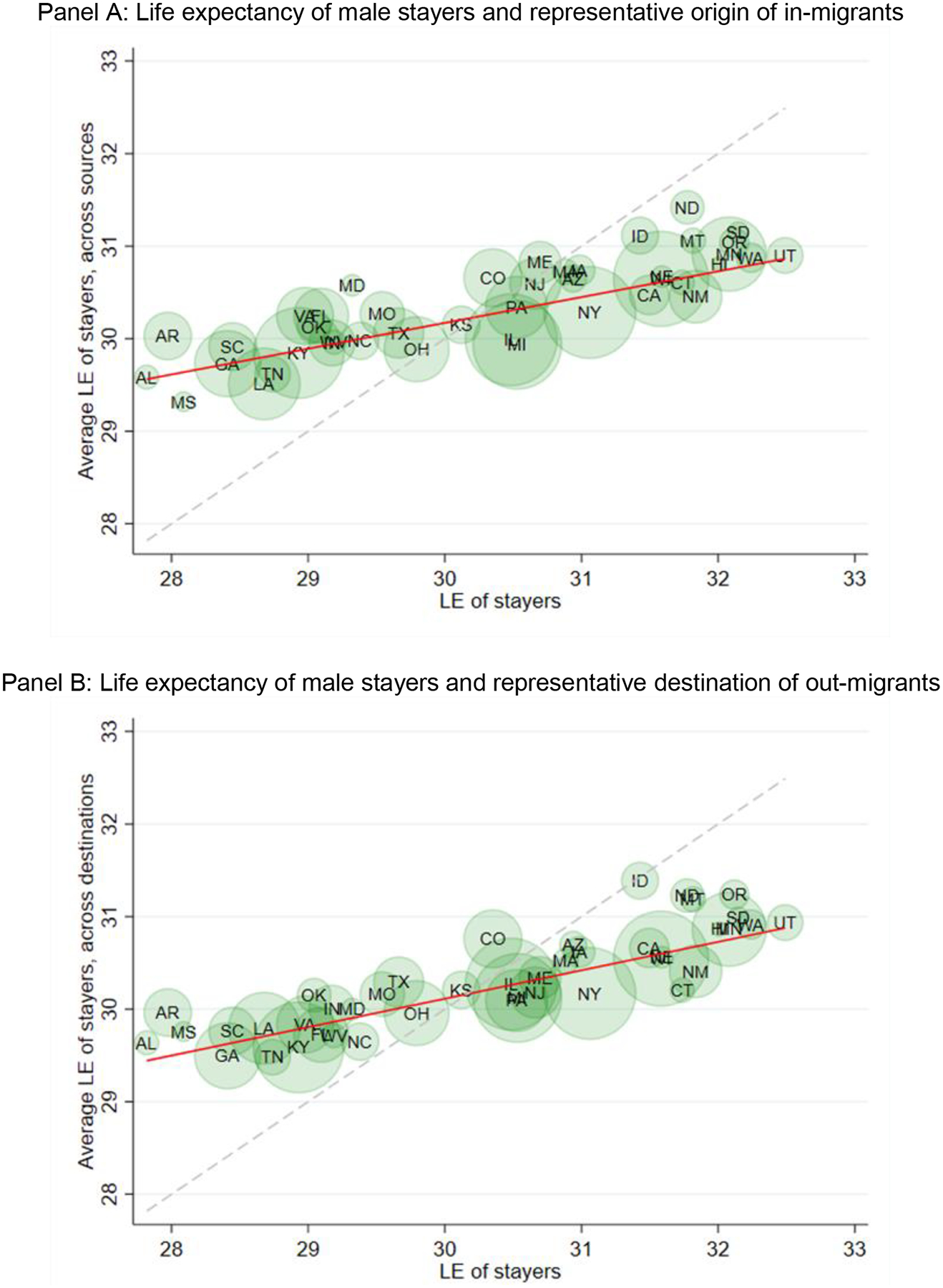
Relationship between male life expectancy of stayers at age 50 and representative origin / destination states
Note: Panel A (B) of Figure 7 shows the relationship between the life expectancy of stayers and a measure that proxies for the place effect of the representative source (destination) of in-migrants (out-migrants). For more details on the construction of the proxies see the main text. In both panels, states are weighted by the inverse variance of the male life expectancy of stayers at age 50.
However, the slope of this relationship is also significantly lower than one (slope = 0.28, s.e. = 0.28). This implies that in states where life expectancy is lower (higher) than average, in-migrants come on average from states of origin that are healthier (unhealthier) relative to the destination. For example, the estimated life expectancy gap between the states of origin of in-migrants and stayers is equal to 1.32 years in Georgia, where life expectancy of stayers is low, and −1.37 years in the state of Washington, where life expectancy of stayers is high. These differences across states illustrate the way in which migration mitigates state-of-birth based disparities—migration induces convergence in state life expectancies. The least (most) healthy locations receive in-migrants who on average come from more (less) healthy locations.33
We construct a similar measure to summarize the destinations of the out-migrants from each state. To construct this measure, we weigh the life expectancy of male stayers from all destinations of by the share of out-migrants from who relocate to each state. Analogous to Panel A, Panel B of Figure 7 shows that there is a positive relationship between the life expectancy of stayers in a given state and the destinations of its out-migrants. Out-migrants who move from “healthy” locations relocate (on average) to destinations where the life expectancy of stayers is also high.34
The previous analysis abstracts from the possibility that different locations might attract in-migrants based on their health, even after controlling for the state of origin of its in-migrants. To quantify how migration, both flows in levels and flows based on specific purposeful sorting regularities, affects differences between state-based life expectancy measures, we perform a series of counterfactual exercises where we modify the extent to which the final destinations of out-migrants are tied to their original health and state of origin.
A full description of the analysis and results is contained in Appendix D. Briefly, we decouple purposeful selection of migration destinations and place effects by taking the set of migrants in the data and “shuffling” their destinations based on three different assignment procedures independently of their health status at the time of migration, either by observed “popularity” of the destinations for all migrants, by equalizing in-migration rates, or by equalizing net migration rates across states. In addition to assignment of migrants to destinations, the counterfactual exercise also allows “place effects” of destinations to be present or absent.35 We focus on the subset of thirteen states where the difference in male life expectancy measures at age 50 is statistically significant at conventional levels.
In the counterfactuals that use popularity and no place effects, we find substantial reductions in the difference between counterfactual state of birth and state of residence life expectancies compared to the empirical data in the sub-set of selected states. Allowing for constant place effects moves our counterfactuals farther away from the empirical data. We calculate that the cross-state standard deviation in life expectancy measures is reduced by 36 to 49 percent in our counterfactual reshuffling exercise, suggesting that the non-random sorting of out-migrants to destinations is an important component of the differences in state of birth and state of residence life expectancy estimates in our sub-set of thirteen states. Importantly, many states in the South appear to be attracting in-migrants who have lower mortality risk than what would be expected in a counterfactual scenario where the destination choices of out-migrants do not depend on state of origin and mortality risk. The opposite pattern appears to hold for many states in the Midwest. One explanation of these patterns is that migrants likely seek out economic opportunities, which during our data window are generally better in the South than in the Midwest (Kennan and Walker 2011).
When we compare the results across settings of our counterfactual exercises, we find additional evidence that once we equalize the unobserved mortality risk and state of origin of in-migrants across destinations, equalizing the in-migration or net migration rates across states still contributes to reducing the difference in life expectancy measures across states. However, the contribution of the equalization of migration rates is quantitively smaller than the equalization of unobserved mortality risk and state of origin of in-migrants. Together, our findings suggest that (1) maximizing life expectancy does not appear to be a primary driver of migrants’ destination choices (2) there is substantial variation in the composition of in-migrants across states; and (3) “place matters” for migrant life expectancy.
8. Conclusion
While place/state of residence is nearly universally used in research measuring geographic inequalities in mortality, we outline a set of conception issues in interpreting these measures that could limit their usefulness in both understanding the sources of mortality disparities and proposing solutions. An alternative aggregation is place/state of birth, which is not subject to issues of migration and uncertain timing of exposure effects, though both aggregations face limitations regarding the duration of exposure to the “place”. While over thirty percent of individuals in recent cohorts die in a state they were not born in, it is unclear whether considering an alternative “place” of aggregation is consequential for estimated geographic mortality inequalities. We used the novel MDAC dataset and estimated consequential differences by method of aggregation; the mean absolute deviation of the difference in life expectancy at age 50 measured by state of birth versus state of residence is 0.58 (0.50) years for men and 0.40 (0.29) years for women.
Further, we show that these differences in life expectancy measures are clustered geographically. The difference in life expectancy by state of residence and state of birth is positive and statistically significant in states in the East South Central and South Atlantic divisions. In contrast, the difference in life expectancy measures is negative and statistically significant in states in the East North Central and Middle Atlantic divisions. States in the South have been recognized by a broad literature as the states with the lowest levels of life expectancy. Our findings imply that regional disparities in mortality outcomes are even more unequal when life expectancies are constructed by aggregating individuals based on their state of birth than by the usual life expectancies by state of residence. Life course migration patterns serve to reduce these disparities, making them less visible in nearly all search in this literature
While the culprit of the differences is life course migration, the specific patterns are complex and reflect flows (levels) of in-migration and out-migration in each state as well as the differential health of individuals (characteristics) who stay, move in, and move out. Flows and characteristics of migrants also may interact with “place effects” of origins and destinations.
Overall, we do not find any evidence that out-migration and in-migration flows (in levels) are correlated with the life expectancy of stayers. Thus, the states where stayers have the highest levels of life expectancy do not appear to be receiving a higher or lower inflow of immigrants. The same result holds for out-migration flows. This result provides suggestive evidence that health factors might not be a strong pull or push factor in determining which locations send or receive more individuals, at least at the state level.
In order to provide some descriptive evidence about the relative importance of state-specific experiences of migration flows, we compute the life expectancy of the sub-populations of stayers, in-migrants, and out-migrants for each state. By comparing the life expectancy of in-migrants and out-migrants relative to stayers, we find evidence that the mortality advantage of in-migrants across states plays a more important role than the mortality advantage/disadvantage of outmigrants in determining differences between life expectancy by state of residence and life expectancy by state of birth. For five states in the South, we document that the male life expectancy of in-migrants is more than two years higher than the life expectancy of stayers.
Thus, rather than the raw magnitude of migration flows leading to differences in our two life expectancy measures, our results point to more subtle state-to-state migration processes that together lead to the differences in life expectancy. Destination decisions are not independent of geography and state of origin. “Healthy” states attract migrants from other “healthy” states and lose migrants to other “heathy” states and the net effects of these processes differ by state but also cluster geographically. For example, in-migrants in the South live longer than stayers by a substantially wider margin than in states where stayers have higher life expectancies. Our counterfactual examinations suggest our main results are driven by a combination of “place effects” and that different places receive different compositions of migrants in terms of state of origin and unobserved mortality risk.
These explanations of the differences between life expectancy calculated at the state of birth versus state of residence level do not prescribe whether and when to focus attention on one versus the other measurement. We note that the interpretation of life expectancy by state of residence is complicated—this is well understood, but our paper shows that the decision to focus on one versus the other is consequential for the measurement of geographic disparities in mortality. While it is the typical focus in the literature, state of residence-based measures of mortality disparities represent a combination of early life health processes of non-migrants, migration inflows and outflows, causal place effects, and the interactions of these processes and therefore blur the interpretation of life expectancies by state of residence. As we describe above, these processes create difficulties in decomposition exercises that attempt to explain state-of-residence based measures of life expectancies using (contemporaneously measured) state conditions and policies (e.g. Montez and Farina 2021), since there is selective migration. Contemporaneously measured conditions also fail to capture life course exposures to “place” conditions that may accumulate over time, lead to migration, and/or be experienced in critical early time periods, such as in utero. The measure of life expectancy by state of birth is more easily interpretable, is consistent with the theoretical assumptions of closed populations used in the construction of life tables and has a higher correlation with the life expectancy of stayers, which can be a reasonable proxy for the causal place effects of locations under certain conditions.
Finally, many papers in the literature have focused on measuring how life expectancy by place of residence has evolved over time across different locations. For example, Dwyer-Lindgren et al. (2017) documents that many counties in the states of Florida saw important gains in life expectancy between 1980 and 2014. We point out that the interpretation of these changes is even more challenging than the interpretation of life expectancy by state of residence at a given time. Our framework can be extended to incorporate multiple periods of time to show that an observed improvement in the life expectancy by state of residence in a given location can be driven by intertemporal changes in the causal place effects of locations, intertemporal changes in the in-migration and out-migration rates in the location, and intertemporal changes in the relative selection of in-migrants and out-migrants.36 We argue that substantially more research is required in this area to disentangle intertemporal changes in “place effects” from changes in migration patterns. This task is crucial in order to evaluate which public policies or government programs are contributing in the improvement of the mortality outcomes of its residents (Miller et al., 2019, Montez et al., 2020).
Supplementary Material
Table 2:
Estimated correlation matrix among the different life expectancy measures at age 50
| Panel A: Men | |||||
|---|---|---|---|---|---|
| State of residence | State of birth | Stayers | In-migrants | Out-migrants | |
| State of residence | 1 | ||||
| State of birth | 0.84 | 1 | |||
| Stayers | 0.90 | 0.97 | 1 | ||
| In-migrants | 0.81 | 0.45 | 0.55 | 1 | |
| Out-migrants | 0.59 | 0.88 | 0.75 | 0.23 | 1 |
| Panel B: Women | |||||
|---|---|---|---|---|---|
| State of residence | State of birth | Stayers | In-migrants | Out-migrants | |
| State of residence | 1 | ||||
| State of birth | 0.91 | 1 | |||
| Stayers | 0.97 | 0.97 | 1 | ||
| In-migrants | 0.91 | 0.76 | 0.79 | 1 | |
| Out-migrants | 0.67 | 0.86 | 0.72 | 0.52 | 1 |
Note: Table 2 shows the correlation between the different life expectancy measures for the sub-set of states where life expectancy of stayers was computed. Panel A shows the correlation matrix for men, while Panel B shows the correlation matrix for women. In both panels, states are weighted by the inverse variance of the male life expectancy of stayers at age 50.
Acknowledgments
Any opinions and conclusions expressed herein are those of the authors and do not reflect the views of the U.S. Census Bureau. All results have been reviewed to ensure that no confidential information is disclosed. The statistical summaries reported in this document have been cleared by the Census Bureau’s Disclosure Review Board release authorization numbers CBDRB-FY19-304, CBDRB-FY20-CES004-090, CBDRB-FY20-092, and CBDRB-FY21-CES004-021. The authors would like to acknowledge financial support from NIA grant R01AG060109 and the Center for Demography of Health and Aging (CDHA) at the University of Wisconsin-Madison under NIA core grant P30 AG17266. The authors would also like to thank Bruce Weinberg and participants at the 2019 Research Data Center Annual Conference, the 31st Annual Colloquium on Aging of the Institute on Aging of the University of Wisconsin-Madison, the Southeastern Demographic Association Annual Meeting, the La Follette School Seminar Series, and the University of Wisconsin-Madison Health/Aging/Place working group.
Footnotes
We exclude all foreign-born individuals from the analysis. The sample sizes by state of residence and country of origin are too small to be disclosed from the MDAC. We restrict the sample to individuals ages 50 and above due to data limitations. The number of disclosed cells decreases for younger age groups, as mortality events become less common in the data.
We note that life expectancy calculations are only one useful calculation to explore. In future work we will also consider life span variability and additional metrics.
We informally refer to Washington D.C. as a state.
This mortality model is based on the Gompertz Law (1825), which has been validated by a huge literature. A more recent mortality model is the Kannisto model (1994) which allows for mortality deceleration at very old ages. We prefer to use the former method over the latter, since the Gompertz model only requires the estimation of two parameters instead of three. However, in unreported results we use instead the Kannisto and Logistic models to obtain one-year mortality rates as a function of age and verify that we obtain similar life expectancies. In Appendix C, we further show that the fit of the mortality models is already excellent with models with two parameters.
In Appendix C we also provide robustness checks of the main results of Section 4 when we vary this age cut-off. We also provide an overall assessment of the fit of the regressions in this same appendix.
Life expectancy estimates can be noisy if there are not enough observed deaths in the data. For each of the 204 life expectancy measures we have more than 100 observed deaths in the follow-up period across all age groups.
We weigh each state by the estimated resident population in 2008. The correlations are virtually unchanged if we instead weigh each state by the estimated population at birth.
Wyoming and Washington D.C. are two outliers in terms of the relationship between life expectancy by state of residence and life expectancy by state of birth. Without the inclusion of those two states, the unweighted (weighted) correlation coefficient between the two life expectancy measures is equal to 0.87 (0.82) for men and 0.91 (0.88) for women.
Conditional on moving, the distribution of type of moves is also similar between genders. In terms of Census regions, 60.3% of male migrants are living in a different region than their region of birth. This percentage is similar and equal to 59.2% for female migrants. Thus, overall migration rates and types of moves do not appear to explain the gender disparities in differences across life expectancy measures.
The small sample sizes of racial and ethnic minorities in the MDAC dataset preclude us for constructing life expectancy measures by state of residence and state of birth for most states.
The stayer group is composed of individuals who have never moved out from their state of birth and return migrants. We are not able to disentangle these groups, which is a limitation of the study.
The states that we exclude in this and following sections are AK, DC, DE, NH, NV, RI, VT, and WY for men, and AK, DC, DE, NH, NV, and WY for women.
More specifically, we compute as follows: . We use an analogous formula to calculate . Given that the number of individuals in each cell are rounded, the ratio of stayers to in-migrants has some measurement error.
We assume that weights are age-invariant as an approximation. This approximation holds under the following assumptions:
(i) proportionate differences between mortality rates and are age invariant; this assumption is met if the force of mortality follows a Gompertz specification.
(ii) the proportionate differences between life expectancy, and can be approximated by where is the average entropy of the survival curves of the two groups being compared.
We acknowledge that we are using an approximation but claim that this approximation does not distort the determinants of differences in life expectancies.
For example, Florida’s current residents might have a higher life expectancy than those born in Florida (and residing in any state) because people who migrate to Florida have a higher life expectancy than those who have stayed in Florida throughout their lives, and/or because the life expectancy of out-migrants from Florida is substantially lower than the life expectancy of stayers.
In order to address the precision in our life expectancy estimates, each state is weighted by the inverse variance of the difference between the life expectancy by state of residence and life expectancy by state of birth. We have performed the same analysis using alternative weights, e.g. the inverse variance of the life expectancy of stayers as well as the squared native or resident population in each state. Figure 6 remains virtually unchanged if we use these alternative weights. An exception occurs when we do not use any weights, and the relationship becomes slightly positive.
Again, each state has been weighted by the inverse variance of the difference in life expectancy by state of residence and life expectancy by state of birth. The unweighted standard deviation in mortality advantage for in-migrants (out-migrants) is equal to 1.23 (0.93) years.
The two distributions are more similar away from the tails. Out of the 43 states in the analysis, 33 (31) have out-migrants (in-migrants) mortality advantage. In Appendix Figure 6, we show the smoothed distribution of both components.
This claim assumes that the mortality profile of stayers is not affected by the composition or magnitude of in-migration flows.
Deryugina and Molitor (2020) and Finkelstein et al (2021) are two recent papers that estimate the causal effect of different locations on mortality probabilities. We adopt the notation in Finkelstein et al (2021). As such, an increase in the “causal effect” of a location increases the mortality hazard rate of the population.
Each state has been weighted by the inverse variance of the life expectancy of stayers. The unweighted correlation between the life expectancy of stayers and life expectancy by state of residence (state of birth) are virtually identical.
These figures are included in Table 2, which shows the correlation matrix between the different life expectancy measures for men and women.
The life expectancy of stayers might be quite informative about the underlying causal place effects of each location on mortality outcomes. For example, this would be the case if the ex-ante relative health selection of out-migrants compared to stayers does not vary substantially across states.
This assumption is common in the recent literature that estimates causal “place effects” (e.g. Finklestein et al. 2019) and means that “place effects” have a higher effect on the probability of dying as individuals get older. It also implies proportional effects: the ratios of the mortality rates at two different ages for individuals originating in place I and moving to place j is the same independently of age.
If differences in the “place effects” are substantial and have a bigger effect on more vulnerable populations, we would expect that the ex-post relative health advantage of out-migrants relative to stayers in the states with the worst place effects to be considerable, as out-migrants are likely healthier than stayers at the time of the move and they relocate to locations with less detrimental “place effects”. The same pattern would hold for the ex-post relative health advantage of in-migrants. In-migrants in these locations come from locations with more favorable “place effects” and are also likely positively selected. The magnitude of the ex-post relative health advantage of out-migrants and in-migrants would be muted in states with favorable place effects.
This pattern is virtually unchanged if we do not use weights or if we use alternative weights, like the size of the out-migrant population for each state.
One caveat of the analysis is that the results could be driven by the geographical level that we are using to distinguish between different locations (states). Individuals might react to amenities that affect their health and mortality outcomes at a more local level. For example, individuals might move to a different neighborhood or a different county but remain in their home state in response to pollution or crime. Unfortunately, the MDAC data does not contain more detailed information about the place of birth of individuals to perform the migration analysis at a more local level. Nonetheless, we perform a robustness check where we instead define stayers more broadly. We compute alternative in-migration and out-migration flows where only moves across regions are considered as valid moves. Appendix Figure 8 shows that the signs of the relationship between migration flows that only consider interregional moves and life expectancy of stayers are the same as the ones in Figure 6.
It is plausible that after retirement the preferences of individuals change. In order to study if this might be the case, we also analyze the relationship between the male life expectancy of stayers at age 65 and migration rates for the sub-population of men that are 65 – 79 years old in the ACS 2008 interview. Appendix Figure 9 presents the scatterplot for these older men. Again, the relationship between both migration rates and male life expectancy is virtually flat. Hence, the descriptive results presented for men with ages 50–64 and 65–79 both point to the same result that net migration flows are uncorrelated to the baseline life expectancy across states.
For example, Kennan and Walker (2011) finds that male individuals respond to wage differentials across states by migrating during their working life.
As was mentioned previously, we are unable to compute precise male life expectancies of stayers for eight states. For these small states we instead replace the life expectancy of stayers by the life expectancy by state of birth.
In unreported results, we verify that the slope is virtually unchanged if we focus only on the migration patterns of the White non-Hispanic population. In contrast, the corresponding slopes for the Black and Hispanic males are closer to unity. This might be a result of minority in-migrants coming mainly from border states in the case of Hispanic males and from the Deep South in the case of Black males.
Panels A and B of Figure 7 are very similar. This is an implication of migration patterns that are quite symmetrical. Out-migrants tend to relocate to states that also send the most in-migrants. Nonetheless, there are subtle differences in the directionality of the in-migration and out-migration flows for some states. For example, out-migrants who were born in the state of Florida relocate on average to destinations where stayers have an average life expectancy of 29.7 years. In contrast, Florida attracts in-migrants from “healthier” locations, where stayers have an average life expectancy of 30.2 years. The opposite pattern is observed in the state of Illinois. Out-migrants relocate on average to destinations where stayers have an average life expectancy of 30.3 years. In contrast, in-migrants who move to Illinois come from states where stayers have an average life expectancy of 30.0 years.
We follow the small literature that has estimated place effects of destinations by assuming that place effects are common for both stayers and in-migrants (Finkelstein et al., 2021). If there are important differences in the health or social environments that in-migrants face compared to stayers across states, the assumption of constant place effects would be invalid.
A change in the composition of stayers, in-migrants, and out-migrants across states is an example of what Dowd and Hamoudi (2014) coined “lagged selection bias” in the interpretation of mortality trends.
Contributor Information
Jason M. Fletcher, University of Wisconsin-Madison
Michal Engelman, University of Wisconsin-Madison.
Norman J. Johnson, U.S. Census Bureau
Jahn Hakes, U.S. Census Bureau.
Alberto Palloni, University of Wisconsin-Madison.
Bibliography
- 1.Black DA, Sanders SG, Taylor EJ, & Taylor LJ (2015). The impact of the Great Migration on mortality of African Americans: Evidence from the Deep South. American Economic Review, 105(2), 477–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boustan LP, Kahn ME, Rhode PW, & Yanguas ML (2020). The effect of natural disasters on economic activity in US counties: A century of data. Journal of Urban Economics, 118, 103257. [Google Scholar]
- 3.Case A, & Deaton A (2015). Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences, 112(49), 15078–15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, … & Cutler D (2016). The association between income and life expectancy in the United States, 2001–2014. Jama, 315(16), 1750–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chiang CL (1984). The life table and its applications (pp. 193–218). Malabar, FL: Krieger. [Google Scholar]
- 6.Cooke TJ (2011). It is not just the economy: Declining migration and the rise of secular rootedness. Population, space and place, 17(3), 193–203. [Google Scholar]
- 7.Deryugina T, & Molitor D (2020). Does When You Die Depend on Where You Live? Evidence from Hurricane Katrina. American Economic Review, 110(11), 3602–3633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dowd JB, & Hamoudi A (2014). Is life expectancy really falling for groups of low socio-economic status? Lagged selection bias and artefactual trends in mortality. International Journal of Epidemiology, 43(4), 983–988. [DOI] [PubMed] [Google Scholar]
- 9.Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, Morozoff C, Kutz MJ, Huynh C, … & Murray CJ (2016). US county-level trends in mortality rates for major causes of death, 1980–2014. Jama, 316(22), 2385–2401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ezzati M, Friedman AB, Kulkarni SC, & Murray CJ (2008). The reversal of fortunes: trends in county mortality and cross-county mortality disparities in the United States. PLoS Med, 5(4), e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farina MP, Zajacova A, Montez JK and Hayward MD, (2021). US state disparities in life expectancy, disability-free life expectancy, and disabled life expectancy among adults aged 25 to 89 years. American Journal of Public Health, 111(4), pp.708–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Finkelstein Amy, Gentzkow Matthew, and Williams Heidi L.. Place-based drivers of mortality: Evidence from migration. No. w25975. National Bureau of Economic Research, 2019. [DOI] [PMC free article] [PubMed]
- 13.Galobardes B, Smith GD, & Lynch JW (2006). Systematic review of the influence of childhood socioeconomic circumstances on risk for cardiovascular disease in adulthood. Annals of epidemiology, 16(2), 91–104. [DOI] [PubMed] [Google Scholar]
- 14.Gompertz B (1825). On the Nature of the Function Expressive of the Law of Human Mortality and on a New Mode of Determining Life Contingencies. Philosophical Transactions of the Royal Society of London, 115, 513–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haas S (2008). Trajectories of functional health: the ‘long arm’ of childhood health and socioeconomic factors. Social science & medicine, 66(4), 849–861. [DOI] [PubMed] [Google Scholar]
- 16.Halliday TJ, & Kimmitt MC (2008). Selective migration and health in the USA, 1984–93. Population studies, 62(3), 321–334. [DOI] [PubMed] [Google Scholar]
- 17.Hayward MD, & Gorman BK (2004). The long arm of childhood: The influence of early-life social conditions on men’s mortality. Demography, 41(1), 87–107. [DOI] [PubMed] [Google Scholar]
- 18.Hornbeck R (2012). The enduring impact of the American Dust Bowl: Short-and long-run adjustments to environmental catastrophe. American Economic Review, 102(4), 1477–1507. [Google Scholar]
- 19.Hornbeck R, & Naidu S (2014). When the levee breaks: black migration and economic development in the American South. American Economic Review, 104(3), 963–90. [Google Scholar]
- 20.Johnson JE, & Taylor EJ (2019). The long run health consequences of rural‐urban migration. Quantitative Economics, 10(2), 565–606. [Google Scholar]
- 21.Kannisto V (1994). Development of Oldest-Old Mortality, 1950–1990: Evidence From 28 Developed Countries. Odense, Denmark: Odense. University Press; 1994. [Google Scholar]
- 22.Kaplan G, & Schulhofer‐Wohl S (2017). Understanding the long‐run decline in interstate migration. International Economic Review, 58(1), 57–94. [Google Scholar]
- 23.Kennan J, & Walker JR (2011). The effect of expected income on individual migration decisions. Econometrica, 79(1), 211–251. [Google Scholar]
- 24.Kulkarni SC, Levin-Rector A, Ezzati M, & Murray CJ (2011). Falling behind: life expectancy in US counties from 2000 to 2007 in an international context. Population health metrics, 9(1), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller S, Johnson N, & Wherry LR (2019). Medicaid and mortality: new evidence from linked survey and administrative data (No. w26081). National Bureau of Economic Research.
- 26.Molloy R, Smith CL, Wozniak A. Internal migration in the United States. The Journal of Economic Perspectives. 2011;25(3):173–96 [Google Scholar]
- 27.Montez JK, & Zajacova A (2013). Explaining the widening education gap in mortality among US white women. Journal of health and social behavior, 54(2), 166–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Montez JK, Hayward MD and Wolf DA, 2017. Do US states’ socioeconomic and policy contexts shape adult disability?. Social Science & Medicine, 178, pp.115–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Montez JK, Zajacova A, Hayward MD, Woolf SH, Chapman D and Beckfield J, 2019. Educational disparities in adult mortality across US states: How do they differ, and have they changed since the mid-1980s?. Demography, 56(2), pp.621–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Montez JK, Hayward MD and Zajacova A, 2019. Educational disparities in adult health: US states as institutional actors on the association. Socius, 5, p.2378023119835345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Montez JK and Farina MP, 2021. Do liberal US state policies maximize life expectancy?. Public Policy & Aging Report, 31(1), pp.7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Montez JK, Beckfield J, Cooney JK, Grumbach JM, Hayward MD, Koytak HZ, … & Zajacova A (2020). US state policies, politics, and life expectancy. The Milbank Quarterly, 98(3), 668–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Murray CJ, Kulkarni SC, Michaud C, Tomijima N, Bulzacchelli MT, Iandiorio TJ, & Ezzati M (2006). Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Med, 3(9), e260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Németh L, & Missov TI (2018). Adequate life-expectancy reconstruction for adult human mortality data. Plos one, 13(6), e0198485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.NRC and IOM. 2013. U.S. health in international perspective: Shorter lives, poorer health. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- 36.Olshansky SJ, & Carnes BA (1997). Ever since gompertz. Demography, 34(1), 1–15. [PubMed] [Google Scholar]
- 37.Palloni A (2006). Reproducing inequalities: Luck, wallets, and the enduring effects of childhood health. Demography, 43(4), 587–615. [DOI] [PubMed] [Google Scholar]
- 38.Palloni A, & Morenoff J (2001). Interpreting the Paradoxical in the Hispanic Paradox: Demographic and Epidemiologic Approaches. Annals of the New York Academy of Sciences, 954, 140–174. [DOI] [PubMed] [Google Scholar]
- 39.Preston S, Heuveline P, & Guillot M (2000). Demography: Measuring and Modeling Population Processes. 2000. Malden, MA: Blackwell Publishers. [Google Scholar]
- 40.Schwandt H, & Von Wachter TM (2020). Socioeconomic decline and death: Midlife Impacts of graduating in a recession (No. w26638). National Bureau of Economic Research.
- 41.Wang H, Schumacher AE, Levitz CE, Mokdad AH, & Murray CJ (2013). Left behind: widening disparities for males and females in US county life expectancy, 1985–2010. Population health metrics, 11(1), 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Warner DF, & Hayward MD (2006). Early-life origins of the race gap in men’s mortality. Journal of health and social behavior, 47(3), 209–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wolf DA, & Longino CF Jr (2005). Our “increasingly mobile society”? The curious persistence of a false belief. The Gerontologist, 45(1), 5–11. [DOI] [PubMed] [Google Scholar]
- 44.Woolf SH, & Schoomaker H (2019). Life expectancy and mortality rates in the United States, 1959–2017. Jama, 322(20), 1996–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xu W, Engelman M, Palloni A, & Fletcher J (2020). Where and When: Sharpening the lens on geographic disparities in mortality. SSM-population health, 12, 100680. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


