Abstract
Background
The burden of stroke is increasing in India, but there is limited understanding of the distribution of reported risk factors in the Indian setting. It is vital to generate robust data on these modifiable risk factors to scale up appropriate strategies for the prevention of cerebrovascular diseases in this setting.
Summary
The objective of this study is to estimate the overall proportion of life style risk factors of patients with stroke in the Indian setting. We searched PubMed and Google Scholar and relevant studies published till February 2022 were included. The risk of bias assessment was considered for the study selection criterion in the meta-analysis. The publication bias was evaluated by funnel plots and Egger’s test. We identified 61 studies in the systematic review and after quality assessment, 36 studies were included for meta-analysis. Random effect model was used due to the significant inconsistency among the included studies (I2 > 97%). The mean age of the participants was 53.84±9.3 years and patients with stroke were predominantly males (64%). Hypertension (56.69%; 95% CI: - 48.45 – 64.58), obesity (36.61%; 95% CI: - 19.31 – 58.23), dyslipidemia (30.6%; 95% CI: - 22 – 40.81) and diabetes mellitus (23.8%; 95% CI: - 18.79 – 29.83) are the leading intermediate conditions associated with stroke. The Physical inactivity - 29.9% (95% CI: - 22.9 – 37.1), history of tobacco use (28.59 %; 95% CI: - 22.22 – 32.94) and alcohol use (28.15 %; 95% CI: - 20.49 – 37.33) were reported as the behavioral risk factors for stroke in this setting.
Key Messages
The current meta-analysis provides robust estimates of the life style related risk-factor of stroke in India based on the observational studies conducted from 1994 to 2019. Estimating the pooled analysis of stroke risk factors is crucial to predict the imposed burden of the illness and ascertain the treatment and prevention strategies for controlling the modifiable risk factors in this setting.
Keywords: Stroke, Lifestyle, Risk factors, Patients, India
Introduction
Cardiovascular diseases accounted for the majority of deaths globally [18·6 million (17·1–19·7)] in both sexes combined in 2019, amongst which stroke is the second leading cause of death, 3·33 million (3·04–3·62) stroke deaths in males and 3·22 million (2·86–3·54) deaths in females. 1 Disability-adjusted life years (DALYs) for cardiovascular diseases were 393 million (95% UI 368–417) and 143 million (95% UI 133–153) for stroke, making stroke the third-leading cause of disease burden. 2 In India, cardiovascular diseases attributed the highest percent of total death for all ages in which stroke was the fifth leading cause of death in the year 2016, with a mean percent change in the number of DALYs of 52.9% (40.4–66.7) between 1990 and 2016. 3 Within India, a wide variation in the burden of stroke was observed across the states. To cite, a recent meta-analysis reported a one-month case fatality rate of stroke varied from 41.08% to 42.06% in the urban population and 18% to 46.3%.in the rural population. 4 This wide variation could be because of the variability in the distribution of risk factors in the population, effectiveness of health services in preventive, curative, and rehabilitative services, and data availability. 5
The available empirical data reported the risk factors for stroke, such as sociodemographic, behavioral, anthropometric, clinical, and biochemical, from multiple settings in India.6, 7 The significant lifestyle-related risk factors include hypertension, diabetes, hyperlipidemia, obesity, smoking, heart disorders, congestive cardiac failure, atrial fibrillation, left ventricular hypertrophy), and so on, and the burden of each risk factor remains unknown. 8 The global burden of disease study (1990–2016) reported a gross variation in the risk factors for cardiovascular disease across the states of India. 9 It is also evident that South Asians, including Indians, are highly vulnerable to cardiovascular disease because of their cardiometabolic risk profile and ethnically mediated cardiometabolic dysfunction. 10
The burden of stroke is increasing in India, but there is scanty evidence on the systematic understanding of the distribution of its lifestyle risk factors in the Indian setting. It is vital to generate robust data on these risk factors to scale-up appropriate strategies for preventing cerebrovascular diseases in this setting.
Objective
The objective of this study was to estimate the overall proportion of lifestyle risk factors of patients with stroke in the Indian setting.
Materials and Methods
Search Strategy and Selection Criteria
This systematic review is reported following the PRISMA checklist. 11 We searched PubMed and Google Scholar, and relevant studies published till February 2022 were included. We used the combination of Medical Subject Headings (MeSH) and keywords of the following search concepts: “stroke,” “risk factors,” “patients,” and “India.” The details of the search strategy in PubMed are given as supplementary material 1. The data search was carried out by two investigators (BPV and MD). The archives of relevant Indian journals were reviewed for maximum inclusion of available studies. No attempts are made to acquire grey/unpublished literature considering the inherent conflict of interest, which might increase the risk of bias. The screening was performed by two investigators (RK and SS) who further appraised the full texts of appropriated records to reach a common consensus regarding the inclusion and exclusion of individual studies.
Inclusion and Exclusion Criteria
Observational studies, both hospital and community-based stroke registry studies, conducted in the Indian setting reporting the risk factors of various types of strokes and published in the English language were included. Stroke registries are observational databases focusing on the clinical information and outcomes of stroke patients. Stroke is a chronic disease with an acute event, so the hospitalization rate is high. As we were not estimating any incidence or prevalence of stroke, we also included hospital-based clinical studies recognizing its limitations and inherent biases.
Studies were included if participants had a confirmed history of stroke as defined by the World Health Organization (WHO) 12 or as defined according to clinical criteria or confirmed by imaging. Global or Indian studies that exclusively estimated the prevalence, incidence, and mortality data among patients with stroke were excluded. Besides, studies with inadequate data, published as editorials or letters to the editor, conference abstracts, expert opinion, or suggestions were excluded. The lifestyle risk factors for stroke were operationally defined as the conditions and behaviors that increases the chances of an individual to have, develop, or be adversely affected by a disease process. In this study, this was categorized into behavioral risk factors and intermediate conditions. The data on the nonmodifiable risk factors of stroke, such as age, previous history of stroke, and family history of stroke, were not estimated.
Data Extraction
The data extraction was done based on the following study characteristics: author (year of publication)/study region, period of study (year), types of stroke, mean age, gender, sample size, and risk factors (hypertension, diabetes mellitus, tobacco use, alcohol use, dyslipidemia, and others). Three investigators (BPV, JJ, and AV) were involved in the data extraction after reading and discussing the full-text version of the shortlisted publications based on the eligibility criteria. The extracted data were cross-verified by the author VLN and SD. A mutual consensus resolved disagreements between the authors (BV, JJ, AV, VLN, and SD).
Quality Assessment
The Joanna Briggs Institute (JBI) critical appraisal checklist was used for the risk of bias assessment (available from https://synthesismanual.jbi.global). The assessment of each study was done based on whether it met the following eight conditions: (a) Were the criteria for inclusion in the sample clearly defined? (b) Were the study subjects and the setting described in detail? (c) Was the exposure measured validly and reliably? (d) Were objective and standard criteria used to measure the condition? (e) Were confounding factors identified? (f) Were strategies to deal with confounding factors stated? (g) Were the outcomes measured validly and reliably? (h) Was appropriate statistical analysis used? Each study was graded as 1–Yes; 0–No; UC–Unclear after rigorous review. The total scores of the included studies were considered for the study selection criterion in the meta-analysis. Three review authors independently assessed the risk of bias in the included studies (SKS, EM, and JJ). This process was performed iteratively. First, each author reviewed the studies and made the risk of bias assessment based on the criteria. A third independent reviewer (SSD) addressed discrepancies in the quality scoring of two reviewers. Disagreements were resolved by group consensus.
Statistical Analysis
The R software was used to perform this meta-analysis, and the pooled estimate of the distribution of lifestyle risk factors of stroke was estimated using inverse variance weighting methods. Assuming the significant inconsistency among the studies, a random-effects meta-analysis model was used, and I2 statistics were calculated to measure heterogeneity among studies. The heterogeneity was considered mild, moderate, or high when the I2 values were from 25% to 50%, 51% to 75%, and >75%, respectively. The funnel plot and Egger’s test were used to assess the potential publication bias.
Results
Identification of Studies
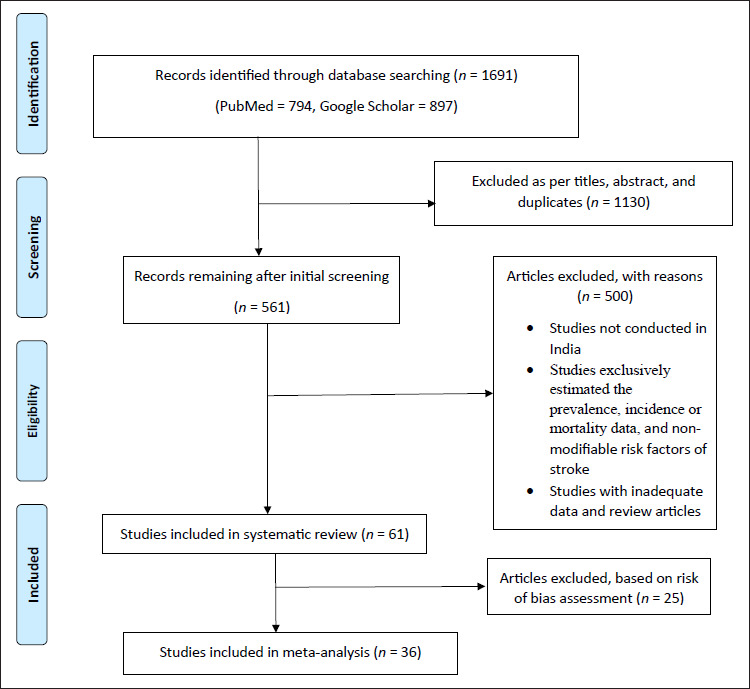
The database search identified 1691 reports: 1130 were excluded based on title and abstract screening, and after eliminating duplicates, 561 articles were retrieved for detailed evaluation, and 500 were excluded for the reasons summarized in Figure 1. Finally, 61 eligible articles were identified after applying the inclusion and exclusion criteria and included in the systematic review, out of which 36 were included in the meta-analysis based on the risk of bias assessment.
Figure 1. Flowchart of Search Strategy and Selection Process.
Characteristics of the Studies Included in the Systematic Review
We have included 61 studies in our systematic review, conducted across various states in India, estimating the various lifestyle risk factors for stroke (Table 1).13–73 Out of 61, 56 studies were conducted and 58 were published after 2000. In 51 studies, patients were enrolled from the hospital-based stroke registries (HBSR) maintained in various treatment settings across India, while in 10 studies, the enrollment was using population-based stroke registries (PBSR). The sample size of included studies varied from 32 to 4989. The number of patients with ischemic stroke and hemorrhagic stroke in the included studies ranged from 19 to 3260 and 3 to 1656, respectively. Other types of strokes reported in a few studies varied from 8 to 271.
Table 1. Characteristics of the Included Studies in the Systematic Review (N = 61).
| Author (Year of Publication)/Study Region | Period of Study (Year) | Study Type | Sample Size | Type of stroke | JBI Score | ||
| Ischemic | Hemorrhagic | Other | |||||
| Singla et al. (2022)/Punjab 13 | 2010–2013 | PBSR | 2948 | 1890 | 787 | 271 | 7 |
| Jayadevappa and Ravishankar (2021)/Karnataka 14 | 2013–2014 | HBSR | 230 | 200 | 30 | NA | 5 |
| Ram et al. (2021)/Across India 15 | 2016–2017 | HBSR | 526 | 299 | 98 | 129 | 4 |
| Rathore et al. (2021)/Rajastan 16 | 2019 | HBSR | 100 | 72 | 28 | NA | 4 |
| Kumar et al. (2021)/Uttarakhand 17 | 2018–2019 | HBSR | 48 | 39 | 9 | NA | 5 |
| Ahmed et al. (2020)/Uttarakhand 18 | 2019–2020 | HBSR | 129 | 122 | 07 | NA | 3 |
| Prabhakar et al. (2020)/Telengana 19 | 2016–2017 | PBSR | 144 | NM | NM | NM | 8 |
| Kaur et al. (2020)/Rajasthan 20 | 2015–2016 | HBSR | 360 | 290 | 70 | NA | 5 |
| Somasundaran and Potty (2020)/Kerala 21 | 2014–2015 | HBSR | 464 | 335 | 129 | NA | 3 |
| Moond et al. (2020)/New Delhi 22 | 2014–18 | HBSR | 160 | 160 | NA | NA | 3 |
| Karri and Ramasamy (2019)/Tamil Nadu 23 | 2014–2017 | HBSR | 186 | 186 | NA | NA | 5 |
| Patel and Vagadiya (2019)/Gujarat 24 | 2014 | HBSR | 46 | 46 | NA | NA | 4 |
| Panwar et al. (2019)/Madhya Pradesh 25 | 2013–2014 | HBSR | 50 | 39 | 11 | NA | 5 |
| Muralidharan et al. (2019)/Kerala 26 | 2018–2019 | HBSR | 200 | 173 | 27 | NA | 4 |
| Rajan et al. (2019)/Karnataka 27 | 2013–2014 | PBSR | 150 | 52 | 05 | 93 | 4 |
| Behera and Mohanty (2019)/Odisha 28 | 2018–2019 | HBSR | 796 | 481 | 315 | NA | 5 |
| Pathak et al. (2018)/New Delhi 29 | 2012–2014 | HBSR | 268 | 169 | 60 | 39 | 5 |
| Hussain et al. (2018)/Meghalaya 30 | 2016–2017 | HBSR | 150 | 76 | 62 | 12 | 3 |
| Sylaja et al. (2018)/Across India 31 | 2012–2014 | HBSR | 2066 | NM | NM | NM | 5 |
| Diwan et al. (2018)/Maharashtra 32 | 2016–2017 | HBSR | 70 | 35 | 35 | NA | 3 |
| Kaur et al. (2017)/Punjab 33 | 2011–2013 | PBSR | 4989 | 3260 | 1656 | 47 | 8 |
| Kabi et al. (2017)/Odisha 34 | 2014–2016 | HBSR | 367 | 218 | 149 | NA | 3 |
| Chandran et al. (2017)/Kerala 35 | 2010 | PBSR | 40 | 37 | 03 | NA | 3 |
| Mahanta et al. (2018)/Assam 36 | 2013–2015 | HBSR | 450 | 163 | 287 | NA | 7 |
| Chandana and Kalyani (2017)/Andhra Pradesh 37 | 2016–2017 | HBSR | 50 | 30 | 11 | 9 | 4 |
| Jacob and Kulkarni (2017)/Karnataka 38 | 2012–2013 | PBSR | 53 | NM | NM | NM | 3 |
| Kumar and Rai (2017)/Uttar Pradesh 39 | NM | HBSR | 100 | NM | NM | NM | 5 |
| Manorenj et al. (2016)/Telengana 40 | 2015–2016 | HBSR | 100 | 76 | 24 | NA | 7 |
| Nayak et al. (2016)/Madhya Pradesh 41 | 2011–2013 | HBSR | 104 | 104 | NA | NA | 6 |
| Huliyappa and Kotrabasappa (2016)/Karnataka 42 | 2013–2014 | HBSR | 52 | NM | NM | NA | 5 |
| Khan et al. (2015)/Chhattisgarh 43 | 2014 | HBSR | 281 | 190 | 91 | NA | 2 |
| Jadhav and Bondarde (2015)/Maharashtra 44 | 2011–2013 | HBSR | 40 | 22 | 10 | 8 | 4 |
| Subha et al. (2015)/Kerala 45 | 2013 | HBSR | 100 | 71 | 29 | NA | 8 |
| Vaidya et al. (2015)/Gujarat 46 | 2012–2013 | HBSR | 175 | 175 | NA | NA | 4 |
| Kawle et al. (2015)/Maharashtra 47 | 2012–2014 | HBSR | 104 | 104 | NA | NA | 6 |
| Shravani et al. (2015)/Karnataka 48 | 2010–2011 | HBSR | 100 | 74 | 26 | NA | 7 |
| Renjen et al. (2015)/New Delhi 49 | 2004–2006 | HBSR | 244 | 244 | NA | NA | 7 |
| Jan et al. (2015)/Jammu & Kashmir 50 | 2011 | HBSR | 209 | NM | NM | NA | 4 |
| Gupta et al. (2014)/Chandigarh 51 | NM | HBSR | 73 | 73 | NA | NA | 5 |
| Kapoor et al. (2014)/Himachal Pradesh 52 | 2012–2013 | HBSR | 32 | 19 | 13 | NA | 3 |
| Sorganvi et al. (2014)/Karnataka 53 | NM | HBSR | 100 | NM | NM | NM | 8 |
| Dash et al. (2014)/New Delhi 54 | 2005–2010 | HBSR | 440 | 440 | NA | NA | 6 |
| Kulshrestha and Vidyanand (2013)/Uttar Pradesh 55 | 2011–2012 | HBSR | 157 | 112 | 45 | NA | 5 |
| Singh et al. (2013)/Punjab 56 | 2006–2011 | HBSR | 1156 | 838 | 318 | NA | 8 |
| Deoke et al. (2012)/Maharashtra 57 | NM | HBSR | 101 | 86 | 15 | NA | 8 |
| Narayan et al. (2012)/Telengana 58 | 2002–2010 | HBSR | 428 | NA | NA | 428 | 4 |
| Kumar et al. (2011)/Karnataka 59 | 1998–2008 | HBSR | 109 | 84 | 25 | NA | 6 |
| Raju et al. (2010)/Punjab 60 | 2008–2010 | HBSR | 162 | 125 | 37 | NA | 3 |
| Kalita et al. (2009)/Uttar Pradesh 61 | 2004–2006 | HBSR | 198 | 198 | NA | NA | 6 |
| Nagaraja et al. (2009)/Karnataka 62 | 2005 | HBSR | 1174 | 797 | 148 | NA | 5 |
| Sridharan et al. (2009)/Kerala 63 | 2005 | PBSR | 541 | 311 | 61 | 169 | 7 |
| Dalal et al. (2008)/Maharashtra 64 | 2005–2006 | PBSR | 456 | 366 | 81 | 9 | 4 |
| Lipska et al. (2007)/Kerala 65 | 2002 | HBSR | 214 | 97 | NM | 117 | 8 |
| Dalal (2006)/Across India 66 | 2002–2004 | HBSR | 2162 | 1656 | 461 | 45 | 5 |
| Bhattacharya et al. (2005)/West Bengal 67 | 1992–1998 | PBSR | 128 | NM | NM | NM | 8 |
| Pandiyan et al. (2005)/Tamil Nadu 68 | 2003–2004 | HBSR | 402 | NM | NM | NM | 6 |
| Mehndiratta et al. (2004)/New Delhi 69 | 1988–1997 | HBSR | 127 | 109 | 18 | NA | 5 |
| Kaul et al. (2000)/Telengana 70 | 2000–2001 | HBSR | 893 | 893 | NA | NA | 5 |
| Nayak et al. (1997)/Kerala 71 | 1988–1994 | HBSR | 177 | 125 | 9 | 43 | 6 |
| Razdan et al. (1989)/Jammu and Kashmir 72 | 1986 | PBSR | 91 | NM | NM | NM | 2 |
| Chopra and Prabhakar (1979)/Chandigarh 73 | 1970–1977 | HBSR | 251 | 109 | 64 | 78 | 3 |
Abbreviations: NA, not applicable; NM, not mentioned; PBSR, population-based stroke registry; HBSR, hospital-based stroke register; JBI Score, JBI critical appraisal checklist for analytical cross-sectional studies (score range: 0–8).
Description of Studies Included the Meta-Analysis
The characteristics of the studies included in the meta-analysis are summarized in Table 2. The meta-analysis included 36 studies, out of which two studies31, 66 were multicentric and the remaining included data from various states of the Indian subcontinent (North: 13,13, 17, 20, 29, 33, 39, 49, 51, 54–56, 69, 61 South: 14,14, 19, 23, 40, 45, 48, 53, 59, 62, 63, 65, 68, 70, 71 East: 3,28, 36, 6 West: 2,47, 57 and Central: 225, 41). The majority of the studies were published in the past decade.13, 14, 17, 19, 20, 23, 25, 28, 29, 31, 36, 39–41, 45, 47–49, 51, 53–57, 59 Overall, 18,315 stroke patients were included, in which the predominant proportion of subjects were males (64%) compared to females (36%). The mean age of the participants was 53.84 ± 9.3 years.
Table 2. Lifestyle-Related Risk Factors of Stroke Based on the Included Studies in the Meta-Analysis (N = 36).
| Author(Year of Publication)/Study Region | Mean Age ± SD(Years) | Male/Female | Sample Size# | HTN | DM | Tobacco Use | Alcohol Use | Dyslipidemia | IHD/CAD | RHD/VHD | AF | Others |
| Singla et al. (2022)/Punjab 13 | NM | 1811/1137 (2948) | 1736 | 1506 | 777 | 417 | 887 | 347 | 203 | 58 | 184 | Postpartum-7 |
| Jayadevappa and Ravishankar (2021)/Karnataka 14 | 59.6 ± 6.1 | 140/60 | 200 | 32 | 12 | 44 | 80 | 132 | NM | NM | NM | D & H-120, T & A-80 |
| Kumar et al. (2021)/Uttarakhand 17 | 55.25 ± 1.32 | 44/4 | 48 | 33 | NM | 24 | 15 | NM | NM | NM | NM | Hyperhomocysteinemia-12 |
| Prabhakar et al. (2020)/Telengana 19 | 61.63 | 100/44 | 144 | 92 | 24 | 53 | 83 | NM | NM | NM | NM | Obesity-50 |
| Kaur et al. (2020)/Rajastan 20 | 60.46 ± 14.84 | 217/143 | 360 | 189 | 68 | 73 | NM | 93 | 27 | – | – | Anemia-29 |
| Karri and Ramasamy (2019)/Tamil Nadu 23 | 38.9 ± 5.74 | 137/49 | 186 | 69 | 55 | 92 | 88 | 105 | 29 | NM | NM | Hyperhomocysteinemia-23 |
| Panwar et al. (2019)/Madhya Pradesh 25 | 31.70 ± 7.42 | 29/21 | 50 | 16 | 12 | 20 | 16 | NM | 1 | NM | NM | Overweight-8 Homocystinaemia-6 |
| Behera and Mohanty (2019)/Odisha 28 | 61.4 ± 13.1 | 287/194 | 481 | 336 | 57 | 140 | 67 | 249 | 1 | 2 | 3 | D & H-46, CKD-105, Anemia-128 |
| Pathak et al. (2018)/New Delhi 29 | 50.3 | 200/60 | 260 | 169 | 60 | 88 | 64 | NM | NM | NM | NM | Myocardial infarction-38 |
| Sylaja et al. (2018)/Across India 31 | 58.3 ± 14.7 | 1389/699 | 2066 | 1257 | 737 | 668 | 707 | 298 | 349 | 115 | 82 | NA |
| Kaur et al. (2017)/Punjab 33 | 59 ± 15 | 3124/1865 (4989) | 3330 | 2849 | 1564 | 573 | 1835 | 631 | 344 | 53 | 352 | Postpartum-13 |
| Mahanta et al. (2018)/Assam 36 | 54.3 ± 13 | 273/177 | 450 | 163 | 52 | 319 | 242 | NM | 3 | 1 | 4 | NM |
| Kumar and Rai (2017)/Uttar Pradesh 39 | NM | 59/41 | 100 | 51 | 12 | 36 | 4 | NM | 4 | 3 | 4 | NM |
| Manorenj et al. (2016)/Telengana 40 | 54 | 69/31 | 100 | 83 | 34 | 43 | 61 | 59 | 13 | NM | NM | Obesity-21, Physical inactivity-28 |
| Nayak et al. (2016)/Madhya Pradesh 41 | NM | 73/31 | 104 | 70 | 29 | 8 | 11 | NM | 5 | NM | NM | NM |
| Subha et al. (2015)/Kerala 45 | 65.30 ± 12.80 | 55/45 | 100 | 83 | 49 | 41 | 21 | 24 | 48 | 10 | 10 | Physical inactivity-37 |
| Kawle et al. (2015)/Maharashtra 47 | NM | 73/31 | 104 | 70 | 29 | 8 | 11 | NM | 5 | NM | NM | NM |
| Shravani et al. (2015)/Karnataka 48 | 50 | 73/27 | 100 | 70 | 27 | 24 | 20 | 22 | 15 | NM | NM | NM |
| Renjen et al. (2015)/New Delhi 49 | 57.1 ± 1.7 | 165/79 | 244 | 139 | 85 | 95 | NM | 58 | 44 | NM | 13 | NM |
| Gupta et al. (2014)/Chandigarh 51 | 59.9 ± 11.2 | 49/24 | 73 | 64 | 42 | 21 | NM | 63 | 17 | NM | 4 | Obesity-40 |
| Sorganvi et al. (2014)/Karnataka 53 | 62.8 | 59/41 | 100 | 62 | 38 | 49 | 32 | 66 | NM | NM | NM | Obesity-84 |
| Dash et al. (2014)/New Delhi 54 | 38.9 ± 7.1 | NM | 440 | 196 | 61 | 42 | 42 | 115 | 24 | 56 | 29 | Cardiomyopathy-12 |
| Kulshrestha and Vidyanand (2013)/Uttar Pradesh 55 | NM | 92/65 | 157 | 26 | 14 | 6 | NM | 9 | NM | 1 | 1 | D & H-23, Anemia-54 |
| Singh et al. (2013)/Punjab 56 | 57.3 ± 13.8 | 650/506 | 1156 | 734 | 454 | 246 | 832 | 220 | NM | NM | 96 | NM |
| Deoke et al. (2012)/Maharashtra 57 | 59.30 ± 12.44 | 65/36 | 101 | 47 | 23 | 61 | 20 | NM | 14 | NM | NM | Physical inactivity-25, Overweight-16 |
| Kumar et al. (2011)/Karnataka 59 | NM | 74/35 | 109 | 79 | 59 | 76 | 53 | 56 | NM | NM | NM | Obesity-53, Homocystienemia-7, |
| Kalita et al. (2009)/Uttar Pradesh 61 | 53.5 ± 15.9 | 162/36 | 198 | 109 | 49 | 61 | 57 | 23 | NM | NM | NM | Overweight-57 |
| Nagaraja et al. (2009)/Karnataka 62 | 54.5 ± 17.0 | 787/387 | 1174 | 563 | 271 | 383 | 295 | NM | NM | NM | 114 | D & H-217 |
| Sridharan et al. (2009)/Kerala 63 | 67 (Median) | 262/279 | 541 | 450 | 271 | 70 | NM | 138 | NM | NM | 42 | NM |
| Lipska et al. (2007)/Kerala 65 | NM | 141/73 | 214 | 102 | 47 | 79 | NM | 66 | NM | NM | NM | NM |
| Dalal (2006)/Across India 66 | NM | 1576/586 | 2162 | 611 | 88 | NM | NM | NM | 82 | NM | NM | D & H-391, D & H and CAD-154 |
| Bhattacharya et al. (2005)/West Bengal 67 | 61 | 60/68 | 128 | 40 | 18 | 72 | NM | NM | 17 | NM | NM | NM |
| Pandiyan et al. (2005)/Tamil Nadu 68 | 61.7 ± 13.4 | 265/137 | 402 | 289 | 200 | 95 | NM | 105 | 136 | 14 | 13 | Anemia-40 |
| Mehndiratta et al. (2004)/New Delhi 69 | 31.97 | 61/66 | 127 | 25 | 8 | 29 | 5 | 36 | 9 | 16 | NM | Homocystenemia-1 |
| Kaul et al. (2000)/Telengana 70 | 56.9 | NM | 893 | 553 | 250 | 25 | NM | NM | NM | NM | NM | NM |
| Nayak et al. (1997)/Kerala 71 | 34.7 ± 8 | 135/42 | 177 | 32 | 13 | 64 | 30 | 18 | NM | NM | NM | NM |
Note:# Calculated based on the analysis of risk factors.
Abbreviations: PHo/S, previous history of stroke; FHo/S, family history of stroke; NM, not mentioned; HTN, hypertension; DM, diabetic mellitus; CAD/IHD, coronary artery disease/ischemic heart disease; CKD, chronic kidney disease; AF, atrial fibrillation; RHD/VHD, rheumatic heart disease/valvular heart disease; D & H, diabetes and hypertension; T & A, tobacco and alcohol use.
The total score of risk of bias assessment according to the JBI critical appraisal checklist for analytical cross-sectional studies is eight, and the individual scores of the included studies in the systematic review ranged from two to eight. We took an arbitrary cutoff based on the mean and the median scores as there is no specified cutoff for the classification of studies for risk of bias. The mean score of the 38 studies was 5.06, and the median score was five. We considered five as a cutoff point. Finally, 36 studies were included in the meta-analysis. Most studies had credible information about the eligibility criteria, study population, setting, and outcome measures. The reporting structure of the measurement of risk factors for stroke and the influence of confounding variables was poorly followed in more than half of the studies. The details of the quality assessment of the studies using the JBI checklist are described in Table 3.
Table 3. Risk of Bias Assessment of Included Studies.
| Author (Year of Publication) | Study Design | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Total | Meta-Analysis |
| Singla et al. (2022) | PBSR | 1 | 1 | UC | 1 | 1 | 1 | 1 | 1 | 7 | Included |
| Jayadevappa and Ravishankar (2021) | HBSR | 1 | 1 | UC | 1 | 1 | 0 | 1 | 0 | 5 | Included |
| Kumar et al. (2021) | HBSR | 1 | 1 | UC | 1 | 1 | 0 | 1 | 0 | 5 | Included |
| Prabhakar et al. (2020) | PBSR | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Included |
| Kaur et al. (2020) | HBSR | 1 | 1 | UC | 1 | 1 | 0 | 1 | 0 | 5 | Included |
| Karri and Ramasamy (2019) | HBSR | 1 | 1 | UC | 1 | 1 | 0 | 1 | 0 | 5 | Included |
| Panwar et al. (2019) | HBSR | 1 | 1 | UC | 1 | 1 | 0 | 1 | 0 | 5 | Included |
| Behera and Mohanty (2019) | HBSR | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 5 | Included |
| Pathak et al. (2018) | HBSR | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 5 | Included |
| Sylaja et al. (2018) | HBSR | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 5 | Included |
| Kaur et al. (2017) | PBSR | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Included |
| Mahanta et al. (2018) | HBSR | 1 | 1 | UC | 1 | 1 | 1 | 1 | 1 | 7 | Included |
| Kumar and Rai (2017) | HBSR | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 5 | Included |
| Manorenj et al. (2016) | HBSR | UC | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | Included |
| Nayak et al. (2016) | HBSR | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 6 | Included |
| Subha et al. (2015) | HBSR | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Included |
| Kawle et al. (2015) | HBSR | 1 | 1 | 1 | 1 | 1 | UC | 1 | 0 | 6 | Included |
| Shravani et al. (2015) | HBSR | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 | Included |
| Renjen et al. (2015) | HBSR | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 | Included |
| Gupta et al. (2014) | HBSR | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 5 | Included |
| Sorganvi et al. (2014) | HBSR | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Included |
| Dash et al. (2014) | HBSR | 1 | 1 | UC | 1 | 1 | 1 | 1 | 0 | 6 | Included |
| Kulshrestha and Vidyanand (2013) | HBSR | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 5 | Included |
| Singh et al. (2013) | HBSR | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Included |
| Deoke et al. (2012) | HBSR | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Included |
| Kumar et al. (2011) | HBSR | 1 | 1 | 1 | 1 | 1 | UC | 1 | UC | 6 | Included |
| Kalita et al. (2009) | HBSR | 1 | 1 | 1 | 1 | 1 | UC | 1 | UC | 6 | Included |
| Nagaraja et al. (2009) | HBSR | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 5 | Included |
| Sridharan et al. (2009) | PBSR | 1 | 1 | 1 | 1 | 1 | 1 | 1 | UC | 7 | Included |
| Lipska et al. (2007) | HBSR | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Included |
| Dalal (2006) | HBSR | 1 | 1 | 1 | 1 | UC | UC | 1 | UC | 5 | Included |
| Bhattacharya et al. (2005) | PBSR | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Included |
| Pandiyan et al. (2005) | HBSR | 1 | 1 | 1 | 1 | UC | UC | 1 | 1 | 6 | Included |
| Mehndiratta et al. (2004) | HBSR | 1 | 1 | 1 | 1 | UC | UC | 1 | 0 | 5 | Included |
| Kaul et al. (2000) | HBSR | 1 | 1 | UC | 1 | 1 | 0 | 1 | 0 | 5 | Included |
| Nayak et al. (1997) | HBSR | 1 | 1 | 1 | 1 | 1 | UC | 1 | 0 | 6 | Included |
Note: Mean, 5.06; Median, 5.
Abbreviations: PBSR, population-based stroke registry; HBSR, hospital-based stroke register; UC, unclear.
Lifestyle Risk Factors for Stroke
Stroke being an end-stage disease, we distributed the risk factors for stroke as behavioral risk factors and intermediate conditions (Figure 2). Hypertension (56.69%; 95% CI [48.45, 64.58]; n = 36 studies), obesity (36.61%; 95% CI [19.31, 58.23]; n = 8 studies), dyslipidemia (30.6%; 95% CI [22, 40.81]; n = 23 studies), and diabetes mellitus (23.8%; 95% CI [18.79, 29.83]; n = 35 studies) were identified as the leading intermediate conditions associated with stroke. The presence of various forms of anemia was associated with 13.3% (95% CI [7.0, 21.2]; n = 9 studies) of the patients with stroke. The occurrence of ischemic heart disease or coronary artery diseases was reported in 8.46% (95% CI [5.07, 13.80]; n = 22 studies) of the study subjects, and 2.82% (95% CI [1.19, 6.54]; n = 11 studies) of the participants had rheumatic heart disease or valvular heart disease. An ECG diagnosis of atrial fibrillation was identified for 4.66% (95% CI [2.87, 7.46]; n = 15 studies) of patients. Approximately 4% (3.94%; 95% CI [2.0, 6.0]) of the patients experienced an episode of stroke during postpartum period.
Figure 2. The Distribution of Lifestyle Risk Factors Among Patients with Stroke in India.
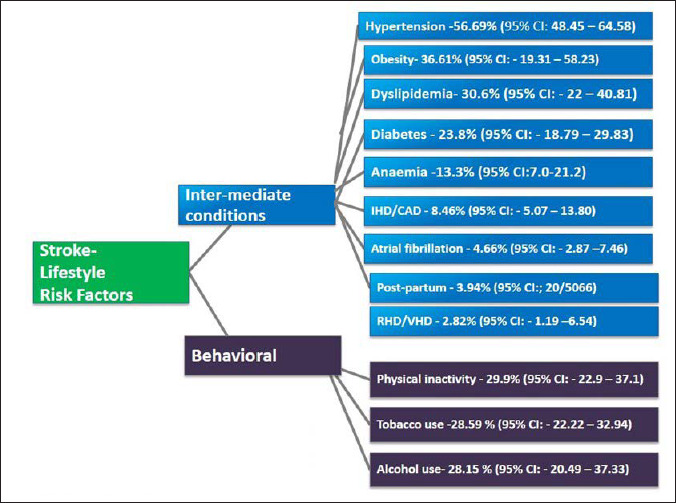
The physical inactivity–29.9% (95% CI [22.9, 37.1]), history of tobacco use, both smoking and smokeless forms (28.59%; 95% CI [22.22, 32.94]), and alcohol use (28.15%; 95% CI [20.49, 37.33]) were the behavioral risk factors for stroke in this setting.
We used the DerSimonian and Laird method of random-effects models to calculate the pooled estimates as there was a significant heterogeneity in the outcome measures (hypertension–I2 = 98.8%, tau squared = 0.92, Q = 2932.05, P < .001; diabetes–I2 = 97.9%, tau squared = 0.74, Q = 1641.78, P < .001; dyslipidemia–I2 = 97.6%, tau squared = 1.03, Q = 909.22, P < .001; atrial fibrillation–I2 = 90.9%, tau squared = 0.70, Q = 154.50, P < .001; tobacco–I2 = 97.3%, tau squared = 0.09, Q = 1238.27, P < .001; alcohol–I2 = 98.2%, tau squared = 1.02, Q = 1422.63, P < .001; IHD/CAD–I2 = 96%, tau squared = 1.40, Q = 525.33, P < .001; RHD/VHD–I2 = 94.5%, tau squared = 1.50, Q = 182.64, P < .001; obesity–I2 = 94.3%, tau squared = 1.04, Q = 122.53, P < .001; previous history of stroke–I2 = 96%, tau squared = 0.61, Q = 447.43, P < .001; family history of stroke–I2 = 92.6%, tau squared = 0.70, Q = 162.83, P < .001). The pooled analysis of the proportion of individual risk factors and heterogeneity are depicted in supplementary materials (Figure S1.1–S1.9)
With the exception of the proportion of studies that estimated diabetes (P = .01), dyslipidemia (P = .02), alcohol (P = .01), and atrial fibrillation (P = .01), Egger’s test revealed no publication bias in the outcome measures (hypertension: P = .53; tobacco: P = .39; RHD/VHD: P = .52; IHD/CAD: P = .39; previous history of stroke P = .12; family history of stroke P = .44). The funnel plot regarding the publication bias of individual risk factors based on the included studies is presented in supplementary materials (Figure S2.1–S2.9).
Discussion
Reducing the burden of stroke in the Indian population requires the identification of modifiable risk factors, and the current meta-analysis provides an aggregate of the distribution of various lifestyle-related risk factors for patients with stroke in the Indian setting. We identified that hypertension (56.69%), obesity (36.61%), dyslipidemia (30.6%), and diabetes mellitus (23.8%) are the leading intermediate conditions associated with stroke. However, physical inactivity (29.9%), history of tobacco use (28.59%), and alcohol use (28.15%) were reported as the behavioral risk factors for stroke in this setting. Referring to some previous studies, there are conflicting results regarding pooled estimates of the risk factors for stroke across Asian countries. 74 Hypertension remains the most common vascular risk factor for stroke in the Asian population74–76 which is consistent with current study findings.
However, the comparisons of the aggregate estimate of the lifestyle risk factors of stroke in this setting should be interpreted based on several contextual factors. First, the high or low frequencies of the occurrence of the risk factors for the noncommunicable disease of a country need to be considered while estimating the specific risk factors for stroke in other countries. For example, a high prevalence of hypertension is seen in Mongolia and Pakistan, which is low in Korea and Singapore. 74 Therefore, a countrywide comparison would be made based on the magnitude of the risk factors predisposing stroke. Second, most of the information on the risk factors among stroke patients was derived from HBSR studies in which data were collected at differing time points with varying definitions limiting its generalization for the estimation of risk factors across countries.77, 78 It is worth noting that estimating stroke risk based on valid risk scoring systems is of pivotal importance for better understanding risk factors to maximize the efficacy of risk reduction efforts. 79
Currently, the burden of stroke is increasing in India, 80 and the findings of this meta-analysis reflect a comprehensive report on the trends of risk factors for stroke in India over a long period. Although several HBSR and PBSR studies were conducted in different parts of India, there is a dearth of evidence of a systematic summary of the risk factor profile of stroke in this setting. This study provides robust estimates of the lifestyle risk factor of stroke in India from 1994 to 2019. The mean age of the participants was 53.84 ± 9.3 years, and a predominant proportion of subjects were males (64%). In contrast to our findings, earlier epidemiological studies in India have found hypertension, diabetes, and cigarette smoking as the leading lifestyle risk factors for stroke. 81 One of the reasons for this change in the risk factor profile for stroke might be because of the varied epidemiological transition among the different states of India. 82 The current findings emphasize that, although the proportion of risk factors for stroke varied considerably across the states of India, the prevalence of hypertension remains the pivotal risk factor across all state groups since 1994. The burden of stroke in the developing world is likely to increase substantially, partly because of ongoing demographic changes, including the aging of the population and health transitions in these countries. 83
The current meta-analysis indicates an urgent need for controlling the vascular and lifestyle risk factors of stroke by focusing more on the public campaign to build the protective factors against cerebrovascular diseases in this setting. There was a significant inconsistency among the included studies as the level of heterogeneity was high (I2 > 94%). The risk of bias assessment of the included studies has implications for the generalization of our findings. Therefore, we exclusively selected stroke epidemiological studies with a low risk of bias conducted in the Indian setting. The current findings provide an evidence base to successfully meet the challenges while devising appropriate strategies to curtail the strategies targeted for risk factor modification.
Strength and Limitations
The primary uniqueness of this study is the novelty of a meta-analysis reflecting the pooled estimate of the proportion of various risk factors of stroke from an Indian perspective. There are certain limitations to generalizing our findings. The results are purely based on observational studies with methodological limitations, such as sampling bias and respondent bias. The level of heterogeneity of the included studies was high because of differences in the study contexts. There might be a chance of contamination of the study subjects, as our estimation is based on the pooled analysis of both hospital and population-based studies, including stroke register studies. The data on clustering risk factors for stroke were not estimated as it was poorly reported in most studies. Despite the limitations, the current meta-analysis provides robust estimates of the lifestyle-related risk factor of stroke in India based on the observational studies conducted from 1994 to 2019.
Conclusion
The present meta-analysis elucidates the overall estimates of lifestyle risk factors for patients with stroke in India. Estimating the pooled analysis of stroke risk factors is crucial to predict the imposed burden of the illness and ascertain the treatment and prevention strategies for controlling the modifiable risk factors in this setting.
Supplemental Material
Supplemental Material for The Distribution of Lifestyle Risk Factors Among Patients with Stroke in the Indian Setting: Systematic Review and Meta-Analysis by Biji P. Varkey, Jaison Joseph, Abin Varghese, Suresh K. Sharma, Elezebeth Mathews, Manju Dhandapani, Venkata Lakshmi Narasimha, Radha Kuttan, Saleena Shah, Surekha Dabla and Sivashanmugam Dhandapani, in Annals of Neurosciences
Acknowledgement
Elezebeth Mathews would like to thank DBT, India for the Clinical and Public Health Early Career Fellowship (grant number IA/CPHE/17/1/503345).
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Elezebeth Mathews is supported by a Clinical and Public Health Early Career Fellowship (grant number IA/CPHE/17/1/503345) from the DBT India Alliance/Welcome Trust-Department of Biotechnology, India Alliance (2018–2023).
ORCID iDs: Jaison Joseph  https://orcid.org/0000-0002-6628-2165
https://orcid.org/0000-0002-6628-2165
Abin Varghese  https://orcid.org/0000-0002-6274-3876
https://orcid.org/0000-0002-6274-3876
Suresh K. Sharma  https://orcid.org/0000-0003-1214-8865
https://orcid.org/0000-0003-1214-8865
Venkata Lakshmi Narasimha  https://orcid.org/0000-0001-9111-8714
https://orcid.org/0000-0001-9111-8714
Authors’ Contribution
BPV: conceptualization, data search, data extraction; JJ: data extraction, risk of bias assessment and manuscript drafting; AV: data extraction; EM: risk of bias assessment and intellectual revision including manuscript drafting; MD: data search and editing; RK and SS: screening of the potential references according to the inclusion and exclusion criteria; VLN and SD: cross-verification of data extraction; SKS: risk of bias assessment; SSD: risk of bias assessment (third independent reviewer).
Statement of Ethics
Not applicable.
References
- 1.Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J Am Coll Cardiol December 22, 2020; 76(25): 2982–3021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Masaebi F, Salehi M, Kazemi M, et al. Trend analysis of disability adjusted life years due to cardiovascular diseases: Results from the global burden of disease study 2019. BMC Public Health 2021; 21: 1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dandona L, Dandona R, Kumar GA, et al. Nations within a nation: Variations in epidemiological transition across the states of India, 1990–2016 in the global burden of disease study. Lancet December 2, 2017; 390(10111): 2437–2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khurana S, Gourie-Devi M, Sharma S, et al. Burden of stroke in India during 1960 to 2018: A systematic review and meta-analysis of community based surveys. Neurol India 2021; 69: 547–559. [DOI] [PubMed] [Google Scholar]
- 5.Dalal PM and Bhattacharjee M.. Stroke epidemic in India: Hypertension-stroke control programme is urgently needed. J Assoc Physicians India 2007; 55: 689–691. [PubMed] [Google Scholar]
- 6.Pandian JD and Sudhan P.. Stroke epidemiology and stroke care services in India. J Stroke 2013; 15: 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Katan M and Luft A.. Global burden of stroke. Semin Neurol 2018; 38: 208–211. [DOI] [PubMed] [Google Scholar]
- 8.Prabhakaran D, Jeemon P, Sharma M, et al. The changing patterns of cardiovascular diseases and their risk factors in the states of India: The global burden of disease study 1990–2016. Lancet Glob Health December 1, 2018; 6(12): e1339–e1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hankey GJ.Nutrition and the risk of stroke. Lancet Neurol 2012; 11: 66–81. [DOI] [PubMed] [Google Scholar]
- 10.Singh V, Prabhakaran S, Chaturvedi S, et al. An examination of stroke risk and burden in South Asians. J Stroke Cerebrovasc Dis 2017; 26: 2145–2153. [DOI] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ (Online) 2009; 339: 332–336. [PMC free article] [PubMed] [Google Scholar]
- 12.Hatano S.The experience from a multicentric stroke register: A pre¬liminary report. Bull World Health Organ 1976; 54: 541–543. [PMC free article] [PubMed] [Google Scholar]
- 13.Singla M, Singh G, Kaur P, et al. Epidemiology of young stroke in the Ludhiana population-based stroke registry. Ann of Indian Acad Neurol January 1, 2022; 25(1): 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jayadevappa G and Ravishankar SN. Risk factors and clinical profile of ischemic stroke patients attending emergency care facility in Bangalore city. Sch J App Med Sci April 2021; 4: 572–577. [Google Scholar]
- 15.Ram CV, Kumar S, Renjen PN, et al. Risk factors predisposing to acute stroke in India: A prospective study. J Hypertens November 1, 2021; 39(11): 2183–2189. [DOI] [PubMed] [Google Scholar]
- 16.Rathore K, Choudhary R, Sankhla N, et al. An observational study to analyze the risk factors associated with stroke in West Rajasthan, India. Natl J Physiol Pharm Pharmacol 2021; 11.(11): 1225–1228. [Google Scholar]
- 17.Kumar R, Kataria N, Radhakrishnan DM, et al. Clinico-epidemiological profile of stroke patients in the Himalayan Subcontinent: A retrospective study. Natl J Physiol Pharm Pharmacol 2021;11(01): 17–22 [Google Scholar]
- 18.Ahmed T, Kumar R, and Bahurupi Y.. Factors affecting quality of life among post-stroke patients in the Sub-Himalayan region. J Neurosci. Rural Pract October 2020; 11(04): 616–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prabhakar S, Suravarapu S, Mathai D, et al. Risk factors for stroke in rural population of Telangana state of India, an unmatched case control study. J Neurosci Rural Pract July 2020; 11(03): 448–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaur G, Samar N, Sharma J, et al. A study of clinico-radiological and socio-demographic profile of patients with stroke in a tertiary care hospital of South West Rajasthan. J Assoc Physicians India March 1, 2020; 68(3): 54–58. [PubMed] [Google Scholar]
- 21.Somasundaran A and Potty SN. Epidemiological profile of stroke in central Kerala. Int J Sci Study 2020; 8(4): 61–65. [Google Scholar]
- 22.Moond V, Bansal K, and Jain R.. Risk factors and subtyping of ischemic stroke in young adults in the Indian population. Cureus November 9, 2020; 12(11): e11388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karri M and Ramasamy B. Risk factors, etiology, and clinical outcome of ischemic stroke in young adults admitted in a tertiary care hospital in India. J Stroke Med June 2019; 2(1): 32–39. [Google Scholar]
- 24.Patel V and Vagadiya A. Clinical profile of acute ischemic cerebrovascular stroke. Int J Contemp Med 2019; 6(10): J10–J13. [Google Scholar]
- 25.Panwar Y, Shivde P, Piplewar P, et al. Aetiology, clinical profile and risk factors in young stroke in central India. J Evid Based Med Health 2019; 6(40): 2671–2675. [Google Scholar]
- 26.Muralidharan PC, Babu B, Chitra G, et al. Quality of life in stroke survivors in central Kerala. JMSCR 2019; 7(6): 986–995. [Google Scholar]
- 27.Rajan B, Pruthvish S, Lalitha K, et al. Assessment of quality of life among stroke survivors: A longitudinal study. Int J Community Med Public Health 2019; 6: 1316–1323. [Google Scholar]
- 28.Behera BP and Mohanty SP.. An observational study from a new tertiary care hospital in North Odisha: Clinical and etiological profile of acute ischemic stroke patients. Int J Adv Med 2019; 6: 1605–1610. [Google Scholar]
- 29.Pathak A, Kumar P, Pandit AK, et al. Is prevalence of hypertension increasing in first-ever stroke patients?: A hospital-based cross-sectional study. Ann Neurosci 2018; 25(4): 219–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hussain M, Sharma SR, and Jamil MD.. A hospital-based study of stroke in young from North East India. Ann Indian Acad Neurol 2018; 21: 184–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sylaja PN, Pandian JD, Kaul S, et al. Ischemic stroke profile, risk factors, and outcomes in India: The Indo-US collaborative stroke project. Stroke January 2018; 49(1): 219–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Diwan G, Diwan A, Barde P, et al. Risk factors determinants for prognosis of stroke patients in Tertiary Care Institute. MVP J Med Sci June 2018; 1: 92–95. [Google Scholar]
- 33.Kaur P, Verma SJ, Singh G, et al. Stroke profile and outcome between urban and rural regions of northwest India: Data from Ludhiana population-based stroke registry. Eur Stroke J December 2017; 2(4): 377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kabi S, Padhy R, Panda BN, et al. A study on clinical and laboratory profiles of hemorrhagic and ischemic strokes in an Eastern Indian teaching Hospital. Int J Res Med Sci 2017; 5: 2419–2421. [Google Scholar]
- 35.Chandran P, Shenoy D, Thavody J, et al. Assessment of quality of life of stroke survivors in a rural area of North Kerala, India. Int J Community Med Public Health 2017; 4: 841–846. [Google Scholar]
- 36.Mahanta BN, Mahanta TG, and Gogoi P.. Clinico-epidemiological profile of stroke patients admitted in a tertiary care hospital of Assam. Clin Epidemiol Glob Health September 1, 2018; 6(3): 122–1229. [Google Scholar]
- 37.Chandana VV and Kalyani N.. Clinical profile of stroke among young adults. Int J Contemp Med 2017; 4(11): 2280–2283. [Google Scholar]
- 38.Jacob GP and Kulkarni MM.. Risk factors of stroke in coastal villages of Uttara Kannada district, Karnataka, India: A case control study. Int J Community Med Public Health 2017; 4: 3145–3149. [Google Scholar]
- 39.Kumar A and Rai ON. Study of risk factors among stroke patients in a tertiary hospital of Northern India. Int J Adv Med 2017; 4: 446–449. [Google Scholar]
- 40.Manorenj S, Inturi S, Jyotsna B, et al. Prevalence, pattern, risk factors and outcome of stroke in women: A clinical study of 100 cases from a tertiary care center in South India. Int J Res Med Sci 2016; 4: 2388–2393. [Google Scholar]
- 41.Nayak AR, Shekhawat SD, Lande NH, et al. Incidence and clinical outcome of patients with hypertensive acute ischemic stroke: An update from Tertiary Care Center of Central India. Basic Clin Neurosci October 2016; 7(4): 351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huliyappa D and Kotrabasappa K. Risk factors and outcome of stroke in young in a tertiary care hospital. Int J Community Med Public Health 2016; 3: 323–327. [Google Scholar]
- 43.Khan Y, Dua A, Pandey S, et al. Study of stroke patients in Chhattisgarh Institute of Medical Sciences (CIMS), Bilaspur Chhattisgarh, India. IOSR J Pharm (IOSR-JDMS) 2015; 14(8): 4–8. [Google Scholar]
- 44.Jadhav YL and Bondarde SA. Study of risk factors and clinical profile of stroke in young adults. MVP J Med Sci 2015; 2(1): 15–19. [Google Scholar]
- 45.Subha PP, Geethakumari SM, Athira M, et al. Pattern and risk factors of stroke in the young among stroke patients admitted in medical college hospital, Thiruvananthapuram. Ann Indian Acad Neurol January 2015; 18(1): 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vaidya CV and Majmudar DK.. A clinical study of ischemic stroke from capital of Gujarat, India. Sahel Med J October 1, 2015; 18(4): 177. [Google Scholar]
- 47.Kawle AP, Nayak AR, Lande NH, et al. Comparative evaluation of risk factors, outcome and biomarker levels in young and old acute ischemic stroke patients. Ann Neurosci April 2015; 22(2): 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shravani K, Parmar MY, Macharla R, et al. Risk factor assessment of stroke and its awareness among stroke survivors: A prospective study. Adv Biomed Res 2015; 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Renjen PN, Beg MA, and Ahmad K.. Epidemiological study of incidence and risk factors of ischemic stroke subtypes according to trial of ORG 10172 in acute stroke treatment criteria: A 3 years, hospital-based study. Int J Public Health 2015; 5(1): 50–54. [Google Scholar]
- 50.Jan R, Gupta RK, Singh P, et al. Risk factors for stroke: A hospital based descriptive study in North India. Int J Stroke 2015; 3: 1–5. [Google Scholar]
- 51.Gupta A, Prabhakar S, Modi M, et al. Vitamin D status and risk of ischemic stroke in North Indian patients. Indian J Endocrinol Metab September 2014; 18(5): 721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kapoor D, Dhiman A, Sharma R, et al. Clinical profile, risk factors and aetiology of young stroke: A tertiary care hospital based study from the Sub-Himalayan region in North India. Int J Res Med Sci 2014; 2: 1355–1399. [Google Scholar]
- 53.Sorganvi V, Kulkarni MS, Kadeli D, et al. Risk factors for stroke: A case control study. Int J Cur Res Rev 2014; 06(03): 46–52. [Google Scholar]
- 54.Dash D, Bhashin A, Kumar PA, et al. Risk factors and etiologies of ischemic strokes in young patients: A tertiary hospital study in North India. J Stroke September 2014; 16(3): 173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kulshrestha MV and Vidyanand. An analysis of the risk factors and the outcomes of cerebrovascular diseases in northern India. J Clin Diagn Res January 2013; 7(1): 127–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Singh JK, Ranjan P, Kumari A, et al. , Types, outcome and risk factors of stroke in tribal patients. Int J Stroke December 2013; 8(8): 675–680. [DOI] [PubMed] [Google Scholar]
- 57.Deoke A, Deoke S, Saoji A, et al. Profile of modifiable and non-modifiable risk factors in stroke in a rural based tertiary care hospital: A case control study. Glob J Health Sci May 2012; 4(3): 158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Narayan D, Kaul S, Ravishankar K, et al. Risk factors, clinical profile, and long-term outcome of 428 patients of cerebral sinus venous thrombosis: Insights from Nizam’s Institute Venous Stroke Registry, Hyderabad (India). Neurol India March 1, 2012; 60(2): 154. [DOI] [PubMed] [Google Scholar]
- 59.Kumar HH, Kalra B, and Goyal N.. A study on stroke and its outcome in young adults (15–45 years) from coastal South India. Indian J Community Med January 2011; 36(1): 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Raju RS, Sarma PS, and Pandian JD.. Psychosocial problems, quality of life, and functional independence among Indian stroke survivors. Stroke December 1, 2010; 41(12): 2932–2937. [DOI] [PubMed] [Google Scholar]
- 61.Kalita J, Kumar G, Bansal V, et al. Relationship of homocysteine with other risk factors and outcome of ischemic stroke. Clin Neurol Neurosurg May 1, 2009; 111(4): 364–367. [DOI] [PubMed] [Google Scholar]
- 62.Nagaraja D, Gururaj G, Girish N, et al. Feasibility study of stroke surveillance: Data from Bangalore, India. Indian J Med Res October 1, 2009; 130(4): 396. [PubMed] [Google Scholar]
- 63.Sridharan SE, Unnikrishnan JP, Sukumaran S, et al. Incidence, types, risk factors, and outcome of stroke in a developing country: The Trivandrum Stroke Registry. Stroke April 1, 2009; 40(4): 1212–1218. [DOI] [PubMed] [Google Scholar]
- 64.Dalal PM, Bhattacharjee M, Vairale J, et al. Mumbai stroke registry (2005-2006)-surveillance using WHO steps stroke instrument-challenges and opportunities. JAPI September 2008; 56: 675–680. [PubMed] [Google Scholar]
- 65.Lipska K, Sylaja PN, Sarma PS, et al. Risk factors for acute ischaemic stroke in young adults in South India. J Neurol Neurosurg Psychiatry September 1, 2007; 78(9): 959–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dalal PM.Burden of stroke: Indian perspective. Int J Stroke 2006; 1: 164–166 [DOI] [PubMed] [Google Scholar]
- 67.Bhattacharya S, Saha SP, Basu A, et al. A 5 years prospective study of incidence, morbidity and mortality profile of stroke in a rural community of eastern India. J. Indian Med Assoc December 1, 2005; 103(12): 655–659. [PubMed] [Google Scholar]
- 68.Pandiyan U, Arjundas G, and Arjundas D.. Risk factors and stroke outcome: An Indian study. Hypertension 2005; 289: 71–79. [Google Scholar]
- 69.Mehndiratta MM, Agarwal P, Sen K, et al. Stroke in young adults: A study from a university hospital in North India. Med Sci Monit August 20, 2004; 10(9): CR535–CR5341. [PubMed] [Google Scholar]
- 70.Kaul S, Venketswamy P, Meena AK, et al. Frequency, clinical features and risk factors of lacunar infarction (data from a stroke registry in South India). Neurol India April 1, 2000; 48(2): 116. [PubMed] [Google Scholar]
- 71.Nayak SD, Nair M, Radhakrishnan K, et al. Ischaemic stroke in the young adult: Clinical features, risk factors and outcome. Natl Med J India May 1, 1997; 10(3): 107–102. [PubMed] [Google Scholar]
- 72.Razdan S, Koul RL, Motta A, et al. Cerebrovascular disease in rural Kashmir, India. Stroke December 1989; 20(12): 1691–1693. [DOI] [PubMed] [Google Scholar]
- 73.Chopra JS and Prabhakar S.. Clinical features and risk factors in stroke in young. Acta Neurol Scand November 1979; 60(5): 289–300. [DOI] [PubMed] [Google Scholar]
- 74.Venketasubramanian N, Yoon BW, Pandian J, et al. Stroke epidemiology in South, East, and South-East Asia: A review. J Stroke September 2017; 19(3): 286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tan KS, Navarro JC, Wong KS, et al. Clinical profile, risk factors and aetiology of young ischaemic stroke patients in Asia: A prospective, multicentre, observational, hospital-based study in eight cities. Neurol Asia 2014; 19(2): 117–127. [Google Scholar]
- 76.Venketasubramanian N and Mannan M.. Stroke burden and stroke services in Bangladesh. Cerebrovasc Dis Extra 2021; 11(2): 69–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Li F, Yang L, Yang R, Xu W, et al. Ischemic stroke in young adults of Northern China: Characteristics and risk factors for recurrence. Europ Neurol 2017; 77(3–4): 115–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bhowmik NB, Abbas A, Saifuddin M, et al. Ischemic strokes: Observations from a hospital based stroke registry in Bangladesh. Stroke Res Treat 2016; 2016: 5610797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yeboah J, Young R, McClelland RL, et al. Utility of nontraditional risk markers in atherosclerotic cardiovascular disease risk assessment. J Am Coll Cardiol 2016; 67: 139–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jones SP, Baqai K, Clegg A, et al. Stroke in India: A systematic review of the incidence, prevalence, and case fatality. Int J Stroke 2021; 17(2): 132–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kaul S.Stroke in India: Are we different from the world? Pak J Neurol Sci 2007; 2(3): 158–164. [Google Scholar]
- 82.Collaborators. India State-Level Disease Burden Initiative Nations within a nation: Variations in epidemiological transition across the states of India, 1990–2016 in the global burden of disease study. Lancet 2017; 390: 2437–2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Donkor ES.Stroke in the 21st Century: A snapshot of the burden, epidemiology, and quality of life. Stroke Res Treat 2018; 2018: 3238165. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for The Distribution of Lifestyle Risk Factors Among Patients with Stroke in the Indian Setting: Systematic Review and Meta-Analysis by Biji P. Varkey, Jaison Joseph, Abin Varghese, Suresh K. Sharma, Elezebeth Mathews, Manju Dhandapani, Venkata Lakshmi Narasimha, Radha Kuttan, Saleena Shah, Surekha Dabla and Sivashanmugam Dhandapani, in Annals of Neurosciences


