Abstract
Background
Transgender and gender-diverse (TGD) population represents an underserved group across the cancer care continuum. To assess the perspective of both oncology health care providers (OHPs) and TGD individuals in Italy, we conducted two national surveys: one among 2407 OHPs about their attitudes, knowledge and behavior toward TGD patients, and one among TGD persons about their health needs, experiences and barriers encountered in the use of health services across the cancer continuum.
Materials and methods
The surveys were self-compiled web-based computer-aided web interview, conducted in Italy within the ‘OncoGender—Promoting Inclusion in Oncology’ project, led by the Italian national cancer society [Associazione Italiana di Oncologia Medica (AIOM)]-associated researchers. All members of AIOM were invited by e-mail to participate in the OHP survey. TGD persons were reached through advocacy groups and consumers’ panel. The recruitment was completed on a voluntary basis. Survey data were collected and managed using an online platform managed by ELMA Research, an independent pharmaceutical marketing agency.
Results
A total of 305 OHPs (13% of AIOM members) and 190 TGD individuals participated in the surveys. Only 19% of OHPs felt competent in providing care to TGD patients and 21% declared not to feel comfortable in treating TGD patients. Seventy-one percent of TGD persons reported that they had never joined any cancer screening program; 32% reported one or more acts of discrimination by health care providers. Seventy-two percent of OHPs recognized the lack of specific education on cancer care for TGD patients and deemed it necessary to receive adequate training.
Conclusions
A general lack of knowledge among OHPs about TGD health issues seems to be the main driver of difficulties in providing assistance and of discriminatory attitudes against TGD individuals. Ultimately, this whole issue generates access barriers and contributes to lack of trust in health care services. Educational interventions and an implementation of person-centric cancer policies are urgently needed.
Key words: gender medicine, transgender, gender identity, cancer, survey, discrimination
Highlights
-
•
There is a knowledge gap among OHPs about TGD health issues.
-
•
32% of TGD persons reported one or more episodes of discrimination by health care providers.
-
•
Adherence to cancer screening programs among TGD persons in Italy is low.
-
•
Educational interventions for health care providers are claimed as useful by both providers and target population.
Introduction
Recent estimates indicate that 0.3%-0.5% of adults and 1.2%-2.7% of children and adolescents self-identify as transgender individuals, with regional variations, cognizant that most of the estimates belong to Anglo-Saxon and north-European studies.1 Transgender people are those whose gender identity does not correspond with society’s expectations based on sex registered at birth, whereas ‘gender diverse’ is an umbrella term used to describe those individuals whose gender identity or gender expression does not align with what is believed to be the gender norm. Transgender and gender-diverse (TGD) population represents an underserved group across the cancer care continuum from prevention to survivorship. Evident disparities in cancer risk, adherence to prevention and screening programs and access to cancer treatments have been reported in literature.2 TGD individuals report several forms of discrimination occurring in medical settings along with violence, social oppression and marginalization.3,4 Additionally, most oncology providers worldwide reported lack of knowledge about sexual and gender minority patients’ health.5, 6, 7, 8, 9, 10, 11, 12, 13 Low awareness, lack of specific medical training and socioeconomic variables may be the drivers of delays in cancer diagnosis and treatments, resulting in worse survival outcomes compared to cisgender patients.14, 15, 16
Despite a growing literature and attention to such issues, there is still a gap in the TGD-specific and evidence-based recommendations for proper cancer care. Furthermore, most of the literature and available data are US-based with a paucity of data about the specific needs of TGD population in other countries. To address such a gap and to assess the perspective of both cancer care providers and TGD individuals in Italy, we conducted two national surveys: one among the oncology health care providers (OHPs) about their attitudes, knowledge and behavior toward TGD patients, and one among TGD persons living in Italy about their health needs, experiences and barriers encountered in the use of health services across the various stages of cancer prevention and treatment. The two surveys are an integral part of the project ‘OncoGender–Promoting Inclusion in Oncology’, led by researchers from various scientific institutions associated to the Italian Association of Medical Oncology [Associazione Italiana di Oncologia Medica (AIOM)]. The project is involving oncologists, cancer researchers, TGD advocacy groups and other relevant stakeholders from various scientific institutions with the aim of supporting an effective stakeholder engagement with the ultimate goal of improving cancer care delivery to TGD individuals.
Materials and methods
We developed a preparatory literature research to explore previously published surveys directed to TGD persons; in addition, we scanned the literature with a scoping review, to identify areas of gaps and of priority interest for cancer care in TGD persons.2 Previous surveys were mapped; key questions were grouped in thematic areas, and specific questions were annotated and adapted to the context of cancer care. Both questionnaires were developed in English and translated into Italian by a mother tongue translator; the survey directed to TGD persons was also translated into Spanish and Portuguese by certified translators to include non-Italian- or non-English-speaking individuals.
The surveys were conducted in Italy; eligible respondents were OHPs or TGD persons aged 18 years or older.
Survey data were collected using an online platform managed by ELMA Research, an independent for-profit agency with 15 years of experience in pharmaceutical marketing and insights. The surveys were self-compiled web-based computer-aided web interview.
Subjects were provided with a privacy policy statement, which was specific for each of the two surveys. The statement included information about the survey aims, data protection officer (i.e. Fondazione IRCCS Istituto Nazionale dei Tumori, INT) and the purposes and legal bases of the data treatment. Participation was voluntary and survey access was made available only to subjects who provided their consent to participate through the web system.
The data were collected and held anonymously, and the results presented only in aggregate form. The study was approved by the INT institutional review board for ethics (code: INT89/22, date of approval: 4 May 2022). The study is consistent with the European regulation for data protection [General Data Protection Regulation (GDPR)] and the corresponding Italian regulations. The checklist for reporting results for internet e-surveys (CHERRIES) was followed. The surveys were launched in May 2022 and open for 8 weeks.
Survey to oncology health care providers
This survey was administered to 2407 OHPs of the AIOM and was aimed to: (i) gain insights into knowledge about health issues and barriers to oncologic health care services for TGD persons; (ii) describe the attitudes toward gender identity and professional experience with TGD persons; (iii) evaluate the need for specific training of OHPs; and (iv) gather suggestions to improve cancer health services for TGD persons.
The survey also collected demographic and other person-related variables including sex assigned in birth certificate and gender identity (Supplementary Appendix S1, available at https://doi.org/10.1016/j.esmoop.2023.101578).
Survey to transgender and gender-diverse persons
This survey (Supplementary Appendix S2, available at https://doi.org/10.1016/j.esmoop.2023.101578) was directed to Italian TGD persons; we invited individuals through advocacy groups (i.e. Associazione per la Cultura e l’Etica Transgenere, Centro Salute Trans e Gender Variant, Movimento Identità Trans) and consumers’ panel (i.e. CINT).
The main purposes of this survey were to: (i) describe personal characteristics, economic and social context and present or past history of chronic diseases, specifically cancer; (ii) describe lived experience of discrimination, harassment or violence based on sexual orientation and gender identity, occurring during the request or provision of health services; (iii) assess health needs, perceived risk of cancer and participation in any screening or prevention programs; (iv) identify gender-related barriers that are perceived to limit or prevent TGD persons from accessing health care services; and (v) collect suggestions for improving health services.
The questionnaire was piloted among a small sample of three TGD persons, who evaluated the comprehensibility of the questions and of the answer options, and suggested improvements by adding relevant aspects not taken into account in the original survey draft. This evaluation has led to re-formulation of some questions and layout changes, resulting in the final survey here reported.
Statistical methods
The survey questions were formulated on the basis of the information to be conveyed. All the questions were closed-ended, based on Likert scales, or formulated as multiple choices (allowing the respondents to select one or more options from a list of predefined answers), or mutually exclusive answers. Predefined answers were presented in rotated or randomized order to break down any impact due to the reading order. As a result, the surveys collected both quantitative and qualitative information.
The data of the two surveys were separately analyzed. Standard descriptive statistics were calculated for categorical data (i.e. frequency and percentage) and numerical data [i.e. median and interquartile range (IQR)]. The OHP questionnaire results were analyzed using clustering analysis to compare the answers and find similarities among the professionals by applying a model-based cluster analysis.17 Demographic and professional characteristics were not included in the cluster analysis but were descriptively analyzed to characterize the resulting clusters of OHP.
Results
Survey to oncology health care providers
Demographics
A total of 305 OHPs (13% of AIOM members) decided to participate in the survey. Supplementary Table S1, available at https://doi.org/10.1016/j.esmoop.2023.101578, shows the responders’ characteristics stratified according to sex assigned at birth. Most responders were medical oncologists (85%) with female as sex assigned at birth (61%), cisgender (99% among women, 98% among men) and heterosexual (89%). More than half of the participants (58%) exerted their professional activities in the northern regions of Italy, 28% in the southern regions and islands and 14% in the regions of central Italy. Responders were equally distributed as early, intermediate and advanced career professionals, and the majority of them (70%) declared to spend 25% of time or less in research activities.
Knowledge
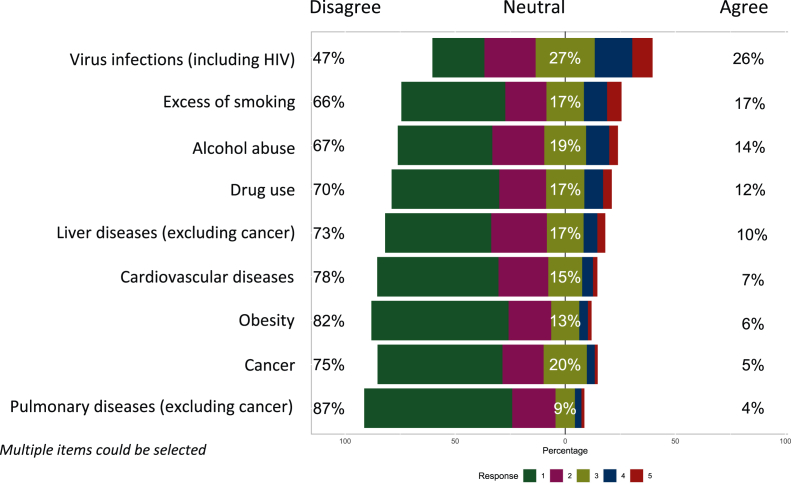
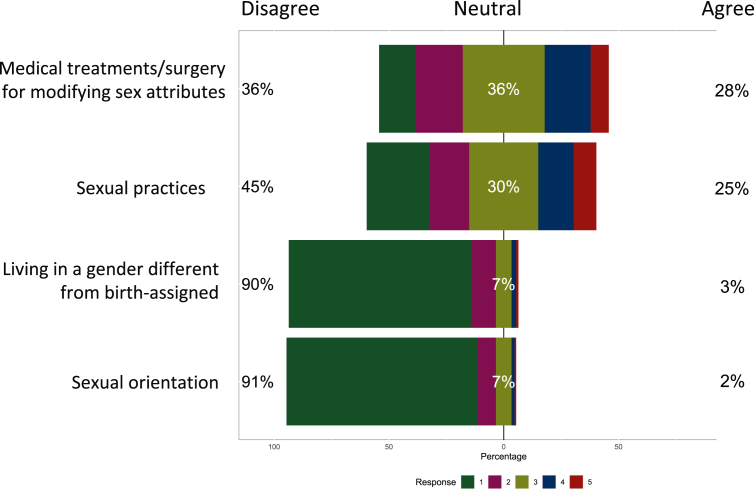
Most of the responders were able to identify the correct definitions of gender identity (90%) and sex assigned at birth (87%). However, there was a common lack of knowledge about the existing disparities in primary prevention and modifiable risk factors for TGD persons. For example, while TGD people have been recognized as being at high risk of substance abuse,18 mainly tobacco consumption19,20 and alcohol use,21,22 both factors playing a role in increasing the risk of cancer,23 a low frequency of responders felt the TGD population to be at higher risk of smoking, alcohol and drug abuse (17%, 14% and 12%, respectively) or at higher risk of cancer (5%) as compared with the general population (Figure 1). Sexual practices and gender-affirming medical treatments were recognized as potential risk factors for cancer only by 25% and 28% of responders, respectively (Figure 2).
Figure 1.
OHP answers to the item ‘as compared with the general population, in the TGD population there is a high incidence of:’.
HIV, human immunodeficiency virus; OHP, oncology health care providers; TGD, transgender and gender-diverse.
Figure 2.
OHP answers to the item ‘the risk of developing cancer differs based on:’.
OHP, oncology health care providers.
The oncology professionals recognized the lack of specific education on cancer care for TGD patients and 72% deemed necessary to receive such a training regarding the unique health care needs of TGD patients; 56% believed that it should be mandatory during the course of the studies. Furthermore, only 19% felt competent in providing assistance to TGD patients.
Barriers
One hundred and forty-one OHPs (46%) believed that TGD patients could be at risk of discrimination in terms of access to oncologic health care services, and 89% believed that TGD patients may receive negative reactions from some health care professionals. Lack of knowledge (77%), fear and/or prejudice (72%), lack of experience with TGD patients (63%), unwillingness or inability to establish effective communication (54%), lack of health care providers’ sensitivity (52%) and lack of appropriate spaces and conditions ensuring privacy (35%) were recognized as possible reasons for such discriminatory attitudes.
Fifty-six OHPs (18% of the sample) have witnessed discriminatory attitudes by colleagues against TGD patients in the form of inappropriate curiosity (46%), misgendering (45%), specific needs ignored (43%), less courtesy and/or respect than what is shown to cisgender patients (32%), harsh or abusive language (30%), excessive precautions (23%), poorer services than what is offered to cisgender patients (9%), pressure to carry out medical tests (5%) and/or blaming for medical problems (5%). As a consequence of these discriminatory or negative attitudes, TGD patients might not participate in cancer screening programs according to 73% of respondents and might not receive appropriate oncologic care (23%). A lack of trust toward OHPs could be a further consequence, suggested by 57% of respondents (Supplementary Figure S1, available at https://doi.org/10.1016/j.esmoop.2023.101578).
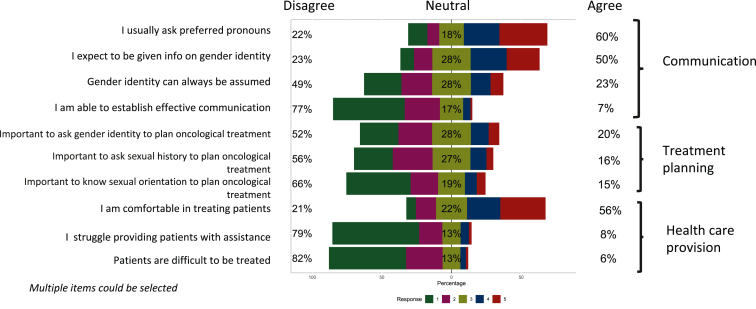
Attitudes and experiences
Only 7% of responders declared to be able to establish effective communication with TGD patients; 60% usually ask preferred pronouns whereas around one out of four (23%) believed gender identity can always be assumed. With regard to treatment planning, only a minority believed it is important to know gender identity, sexual orientation and sexual history of the patient (20%, 15% and 16%, respectively). Finally, 21% of respondents declared not to feel comfortable in treating TGD patients (Figure 3). One hundred and twenty-six professionals (41%) have treated or followed up TGD patients in the 5 years before the interview (68% of whom have treated 1 or 2 patients and only 6% have treated 10 or more patients), mostly for colorectal cancer (49%), lung cancer (30%), genitourinary cancers (20%) and breast cancer (15%) (Supplementary Table S2, available at https://doi.org/10.1016/j.esmoop.2023.101578).
Figure 3.
OHP attitudes toward TGD patients.
OHP, oncology health care providers; TGD, transgender and gender-diverse.
The most common problems perceived by OHPs in establishing an effective doctor–patient relationship regarded patients’ concern for discrimination (90%), or their reluctance to disclose their gender identity (72%). Communication was deemed as sometimes or always difficult according to 50% of OHPs, whilst 36% of responders found it challenging to manage cancer in TGD patients (Supplementary Figure S2, available at https://doi.org/10.1016/j.esmoop.2023.101578).
Cluster analysis
The cluster analysis identified possible patterns in the profile of the OHP responders (Supplementary Table S3, available at https://doi.org/10.1016/j.esmoop.2023.101578). The largest group was cluster 2 composed of the highest proportion of heterosexuals and highest proportion of northern region-based providers. This cluster of respondents felt able to establish effective communication and tended not to believe that TGD individuals bear a higher incidence of harmful behaviors and/or are discriminated against in the access to cancer health care. The second largest group was cluster 4, including younger professionals and the highest rate of homosexuals. They tended to believe that cancer risk might be related to sexual practices and gender-affirming treatments, TGD individuals face discrimination by health providers and, as a consequence, they might not receive proper cancer care. These providers self-reported more experience in treating TGD patients, got the highest percentage of correct answers in the knowledge section and thought it is important to know gender identity, sexual orientation and sexual history of patients. Cluster 3 shared some similarities with cluster 2 but with a lower proportion of experienced responders who, in general, did not feel able to establish effective communication with TGD patients. Cluster 1 included the lowest proportion of northern region-based providers, who felt trained and familiar in providing assistance to TGD patients, think that cancer risk is related to sexual practices and gender-affirming treatments like cluster 4 providers but, in contrast, did not see any discrimination problem for TGD patients in accessing oncological services.
Survey to transgender and gender-diverse persons
Demographics
A total of 190 TGD individuals participated in the survey, equally distributed for sex assigned at birth (56% female, 44% male). Responders self-identified as women (17%), men (23%), transgender (38%) or non-binary (21%). The median age was 30 years old (IQR 23.6-41.4 years), with 60% of the sample based in northern Italy and 40% in center-southern regions. One or more gender-affirming medical procedures were declared by 77% of responders (88% psychological counseling, 70% hormone therapy, 23% surgery) (Supplementary Table S4, available at https://doi.org/10.1016/j.esmoop.2023.101578).
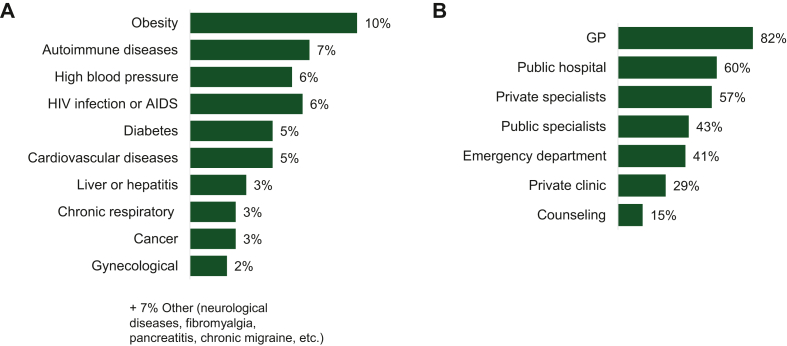
Experiences with cancer health care services
Responders had accessed health care services in the 5 years before in 96% of cases [82% general practitioner (GP), 60% public hospital]. Chronic diseases affected 40% of the sample [obesity 10%, human immunodeficiency virus (HIV) infection and/or acquired immunodeficiency syndrome 6%, cancer 3%] (Figure 4). Five responders reported to be affected by any cancer (two colorectal, one genitourinary tract, one blood, one other). On average, TGD people reported that only one health care professional out of three were aware or informed of their gender identity. Only 47% of respondents believed that gender identity might have an impact on cancer risk and 71% had never joined any cancer screening program with no differences between individuals with male and female as sex assigned at birth. Participation in screening or prevention programs was dominated by breast cancer (49%) and colorectal cancer (44%) (Supplementary Table S5, available at https://doi.org/10.1016/j.esmoop.2023.101578) and remained low also in the population over 50 years of age (50%). One-third of the individuals revealed to be unable to find health-related information specific to the transgender population and the overall satisfaction for available information was poor to moderate (mean score 3.8/7). The level of satisfaction for the health care services was overall modest (mean 5.7/10).
Figure 4.
Health care utilization by TGD individuals. (A) Chronic diseases reported by TGD respondents; (B) health care services accessed by TGD respondents in the last 5 years.
TGD, transgender and gender-diverse.
Discrimination
One or more episodes of discrimination had been experienced and perceived as related to their gender identity by 82% of responders; the most common forms of violence were psychological and/or physical (47% verbal insult and/or humiliation, 34% bullying, 12% violence and assaults, 8% sexual assault) (Supplementary Figure S3, available at https://doi.org/10.1016/j.esmoop.2023.101578).
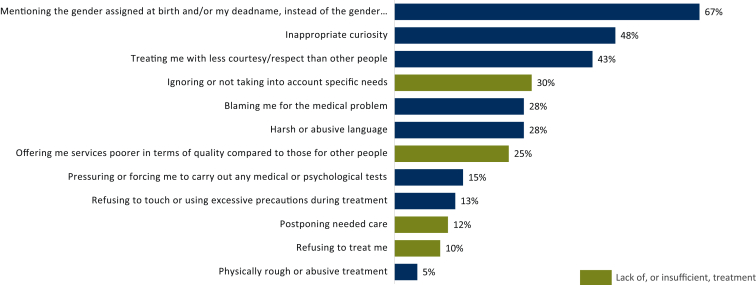
Hospitals and GP’s offices were ranked as the fifth most frequent setting of discrimination (23%) and one out of three reported acts of discrimination by health providers (32%). Prevalence of HIV or hepatitis virus infection was significantly higher among those who experienced discrimination in medical settings (12% versus 4%). The most common expressions of such discriminatory attitudes were misgendering (67%) and inappropriate curiosity (48%). Only 5% reported physical and/or abusive violence (Figure 5). Most individuals did not react to discrimination or violence episodes (40%), and 50% changed specialists or openly stated their disappointment; however, a still-in-double figures percentage of individuals (25%) have been compelled to treatment discontinuation or renunciation. Responders indicated lack of experience (63%) and lack of knowledge (63%) about TGD health issues as the major reasons behind discriminatory attitudes, immediately followed by fear and prejudice (58%), lack of sensitivity (54%), inability to establish effective communication (50%) and lack of appropriate spaces and conditions ensuring privacy (36%). The level of satisfaction for the health care services was poorer in those individuals who had experienced discrimination in medical settings (4.6/10 versus 6.2/10)
Figure 5.
Forms of discrimination by health care providers reported by TGD respondents as patients.
TGD, transgender and gender-diverse.
Providers and individuals’ suggestions for improving health care services dedicated to TGD persons
Both TGD persons and health care providers expressed the need for implementing educational resources for health care professionals (81% OHPs and 78% TGD persons, respectively). Additional strategies indicated by 50% of participants were: implementing national policies to prevent discrimination based on gender identity (57% versus 61%), encouraging health care professionals to respect more gender identity (53% versus 60%) and getting TGD patients more involved in the planning of clinical studies (49% versus 58%). OHPs were also asked to indicate the key benefits deriving from the initiatives aimed at improving health services for TGD patients; the possibility to increase oncologists’ communication ability appeared to be the most important one (76%). Furthermore, OHPs felt that also the patients could be advantaged by improving their compliance to oncological treatments (62%) and being offered more ethical (58%) and patient-centric (54%) treatment approaches.
Discussion
We report the results from one of the few studies investigating the experience of health care providers and TGD persons on cancer care disparities among European lesbian, gay, bisexual, transgender, queer, intersex and asexual (LGBTQIA+) communities and, to our knowledge, this is the first study of its kind specifically focused on TGD individuals.
Our findings show an evident gap of knowledge on the unique health issues of TGD persons self-reported by the Italian OHPs. Our results are consistent with results of previous surveys conducted among OHPs in the United States5, 6, 7, 8 and UK,9 and report for the first time the findings in Italy.
Adherence to cancer screening programs and the perception of cancer risk specifically related to gender identity remain low. The last available data about cancer screening adherence in Italy show that during the period 2018-2021 79% of individuals assigned female at birth (AFAB) between 25 and 64 years had undergone a Pap test in the prior 5 years, 73% of AFAB between 50 and 69 years had got a mammography in the prior 2 years and 47% of persons between 50 and 69 years had undergone a procedure for colorectal cancer screening in the prior 5 years.24 Our results suggest a lower adherence among TGD individuals. This seems to be mainly due to a lack of high-quality information, which might be in turn due to socioeconomic exclusion and a paucity of informative materials specifically related to the transgender population, and a general sense of uneasiness in referring to health care services, as consistently reported in the literature.25 The rate (32%) of TGD individuals who experienced discrimination by health providers is in line with the findings of the last official European report (34%)4 and the last assessment done among the TGD community in the United States.3 The most common form of discrimination in a medical setting is misgendering. The intentional or negligent misuse of pronouns has negative effects on TGD individuals’ psyche26 and it was one of the main barriers to proper cancer care in recent studies.27,28 Meyer’s minority stress theory proposes that unique stressors specific to minorities, such as identity-based discrimination and negative internalized evaluations of these discriminatory experiences, contribute to poor mental and physical health.29 Some researchers suggested a direct correlation between minority stress and worse oncological outcomes such as treatment side-effects30 and expression of single genes and pathways related to cancer in LGBTQIA+ patients.31
It could be argued that a roadmap toward better TGD cancer care should be shaped by experts in the field, and that our survey results are not relevant for such a purpose. We believe that the first step to tackle health care in groups potentially excluded as a minority is based on a situational analysis, aimed at portraying the status quo and understanding the needs. It is valuable to collect the perspectives and perplexities of all the involved stakeholders. For instance, it is notable that both OHPs and TGD respondents suggested the implementation of educational resources to health professionals as the most effective strategy to improve the health care services to TGD patients. Several learning tools about LGBTQIA+ health have been developed in the last few years showing a real impact on health providers’ confidence with such issues.32, 33, 34, 35, 36 Interestingly, both groups of interviewees highlighted the need of more involvement of TGD cancer patients in clinical trials, highlighting the importance of integration under the adage ‘not for us, without us’. In this regard, we believe that only a comprehensive and prospective data collection of gender identity as well as the inclusion of TGD patients in clinical trials would enrich the incomplete knowledge of clinicians and improve the quality of care provided to the patients at the same time, creating a win–win scenario.37
The survey studies presented in this paper are part of the programmatic work of AIOM OncoGender working group, aiming at evaluating the status of cancer care in Italy for TGD persons, as perceived by patients and health providers. We developed the surveys to identify priority areas and unmet needs, to tailor the actions toward relevant areas in TGD care. We believe that the Italian health care contexture may benefit from educational interventions from cancer societies, supported by governmental bodies and academic groups, to increase awareness on the needs and specifics of cancer care in TGD persons. While we do not advocate for a ‘separate’ health care channel that would deepen discrimination,2 we emphasize the importance of integrated, gender-sensitive and non-judgmental attitudes, to be empowered through specific educational resources. Currently, AIOM is working on a set of recommendations, informed by the present surveys, aiming at delivering a paradigmatic, multi-stakeholder case study to inspire similar work in other settings. We believe that the only way to drive impact on people’s well-being is to frame person-centric health policies, framed in a ‘one-society’ approach, by shaping policies based on the lived experience of TGD persons, cognizant that no population health benefit will be delivered when a group of patients is socially and economically excluded or experiencing discrimination. Our action aligns with the national, European and global goals for inclusive health care, with a primary intent of evidence-based policy implementation, to turn the commitment into tangible impact. Presently, investing in patients’ empowerment and increasing providers’ awareness and confidence to deliver inclusive health care is the way to end discrimination toward vulnerable populations. The ‘leave no-one behind’ and gender equality commitments for TGD persons can only be pursued if health policies will take into account TGD persons’ experiences.38
Our study presents objective limitations. We acknowledge potential lack of representativeness of both the samples, relatively small with respect to the full groups. Since OHPs and TGD persons completed the questionnaires on a voluntary basis, this might have led to over-optimistically biased study outcomes. The sample of OHPs was not equally distributed by geographical region and profession with most respondents working as medical oncologists in northern Italy. OHPs who decided to participate in the study could have some reasons to be LGBTQIA+-friendly, or are in general more participating in the activities of AIOM. Furthermore, our surveys did not gather information about setting of living. Our study could have reached those TGD individuals living in urban areas in closest contact with advocacy groups and with a higher health literacy, thus missing persons living in suburban and rural areas, who may have different experience and needs. Finally, the sample of TGD responders was young and not representative of all age groups, making a comparison with the population of Italian cancer registries not possible. These limitations are intrinsic to all survey-type studies.
Our study also has objective strengths. This is one of the largest studies on TGD cancer care, the first in Italy and the only one developed as two-twin studies, launched contemporary. These studies have the sense to trigger the formulation of new strategies to address disadvantaged populations. A ready-to-use survey-derived practice for OHPs could be creating a welcoming environment for TGD patients (i.e. improving communication skills, rejecting prejudices, avoiding stigmatizing and paternalistic behaviors). Importantly, surveys cannot be considered as the sole source or evidence base. A strategic approach to tackle disparities in health care should include the development of tools to enhance accountability, monitoring and evaluation, reaching all who are in need.
Conclusions
A general lack of knowledge among Italian OHPs about TGD health issues is evident and seems to be the main driver of diffuse discriminatory attitudes. Discrimination against TGD individuals in oncology medical settings contributes to lack of trust in health care services as highlighted by the low adherence to cancer screening programs, in a population already burdened by social and economic exclusion. Educational interventions and an implementation of person-centric cancer policies are urgently needed.
Acknowledgments
Funding
Partial support was obtained by non-conditional grants from Merck-Serono and Gilead (no grant number). The data property belongs to AIOM (Associazione Italiana di Oncologia Medica) and Fondazione IRCCS Istituto Nazionale dei Tumori.
Disclosure
ML acted in a consulting/advisory role for Roche, Novartis, Lilly, Pfizer, Merck Sharp and Dohme (MSD), Seagen, Gilead, Exact Sciences, AstraZeneca and received speakers’ honoraria from Takeda, Ipsen, Roche, Lilly, Novartis, Pfizer, Sandoz, Libbs, Knight. FPe reports grants from Roche and Pfizer; personal fees from Sandoz, Celgene, Pierre Fabre and Janssen Cilag; grants and personal fees from Incyte and AstraZeneca; and grants, personal fees and non-financial support from Bayer. NLV reports grants from Eisai; speaker bureau from GSK; travel expenses for conferences from Gentili, Celgene, Pfizer; advisory role from Novartis and Celgene; advisor role, travel expenses for conference from Pfizer; advisory board from MSD, Roche, Novartis and Astrazeneca. DD reports grants from Gentili, and travel expenses from Roche, Gentili and Eisai. FM has served as speaker for Servier. MDM received honoraria from Pfizer, Takeda, AstraZeneca, Janssen, Eisai, Novartis, Roche, Astellas Pharma, MSD; research grants from Tesaro and GlaxoSmithKline; acted in a consulting/advisory role for AstraZeneca, Pfizer, Takeda, Janssen, Eisai, Novartis, Roche, MSD, Amgen. FPi received honoraria from Amgen, Merck-Serono, Sanofi, Lilly, Bayer, Servier, Astrazeneca, MSD, BMS, Astellas, Organon, Pierre-Fabre; research grants from Astrazeneca, BMS, Incyte, Agenus. RB received honoraria and/or research grant from BI, EISAI, MSD, Amgen, Roche, Pfizer, Astra Zeneca, Lilly, GSK, BMS. GDB received honoraria and/or research grants from Roche, MSD, Tahio, Servier, Celgene, Ipsen, Sanofi; acted in consultory/advisory role for Roche, Lilly, Eisai, Incyte; has served as speaker for Servier, Clovis Oncology, Ipsen, Lilly, Merck Serono, Amgen, Novartis, BMS. MM declares ELMA is a for-profit agency. All other authors have declared no conflicts of interest.
Supplementary data
References
- 1.Zhang Q., Goodman M., Adams N., et al. Epidemiological considerations in transgender health: a systematic review with focus on higher quality data. Int J Transgend Health. 2020;21(2):125–137. doi: 10.1080/26895269.2020.1753136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leone A.G., Trapani D., Schabath M.B., et al. Cancer in transgender and gender-diverse persons: a review. JAMA Oncol. 2023;9(4):556–563. doi: 10.1001/jamaoncol.2022.7173. [DOI] [PubMed] [Google Scholar]
- 3.James S.E., Herman J.L., Rankin S., Keisling M., Mottet L.A., Anafi M. National Center for Transgender Equality; Washington, DC: 2016. The Report of the 2015 U.S. Transgender Survey. [Google Scholar]
- 4.EU agency for fundamental rights (FRA) LGBTI survey II report “a long way to go for LGBTI equality” and data explorer. 2020. https://fra.europa.eu/sites/default/files/fra_uploads/fra-2020-lgbti-equality-1_en.pdf Available at.
- 5.Shetty G., Sanchez J.A., Lancaster J.M., Wilson L.E., Quinn G.P., Schabath M.B. Oncology healthcare providers’ knowledge, attitudes, and practice behaviors regarding LGBT health. Patient Educ Couns. 2016;99(10):1676–1684. doi: 10.1016/j.pec.2016.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schabath M.B., Blackburn C.A., Sutter M.E., et al. National survey of oncologists at National Cancer Institute-designated comprehensive cancer centers: attitudes, knowledge, and practice behaviors about LGBTQ patients with cancer. J Clin Oncol. 2019;37(7):547–558. doi: 10.1200/JCO.18.00551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Banerjee S.C., Walters C.B., Staley J.M., Alexander K., Parker P.A. Knowledge, beliefs, and communication behavior of oncology health-care providers (HCPs) regarding lesbian, gay, bisexual, and transgender (LGBT) patient health care. J Health Commun. 2018;23(4):329–339. doi: 10.1080/10810730.2018.1443527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sutter M.E., Bowman-Curci M.L., Duarte Arevalo L.F., Sutton S.K., Quinn G.P., Schabath M.B. A survey of oncology advanced practice providers’ knowledge and attitudes towards sexual and gender minorities with cancer. J Clin Nurs. 2020;29(15-16):2953–2966. doi: 10.1111/jocn.15302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berner A.M., Hughes D.J., Tharmalingam H., et al. An evaluation of self-perceived knowledge, attitudes and behaviours of UK oncologists about LGBTQ+ patients with cancer. ESMO Open. 2020;5(6) doi: 10.1136/esmoopen-2020-000906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ussher J.M., Perz J., Allison K., et al. Attitudes, knowledge and practice behaviours of oncology health care professionals towards lesbian, gay, bisexual, transgender, queer and intersex (LGBTQI) patients and their carers: a mixed-methods study. Patient Educ Couns. 2022;105(7):2512–2523. doi: 10.1016/j.pec.2021.12.008. [DOI] [PubMed] [Google Scholar]
- 11.Sampson A., Block R., Lake P.W., et al. “No one size fits all” a multi-method survey of oncology allied health professionals experiences with lesbian, gay, bisexual, transgender/queer questioning adolescent, and young adult patients with cancer and reproductive and sexual health”. J Adolesc Young Adult Oncol. 2023;12(2):250–258. doi: 10.1089/jayao.2021.0208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tamargo C.L., Mitchell E.P., Wagner L., et al. “I need more knowledge”: qualitative analysis of oncology providers’ experiences with sexual and gender minority patients. Front Psychol. 2022;13 doi: 10.3389/fpsyg.2022.763348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saloustros E., Ferrari A., Bozovic-Spasojevic I., et al. 1824P Attitudes, knowledge, and need for education about LGBTQ patients with cancer: a survey by the ESMO/SIOPE AYA with cancer Working Group. Ann Oncol. 2021;32(suppl 5):S1236. [Google Scholar]
- 14.Dhejne C., Lichtenstein P., Boman M., Johansson A.L., Långström N., Landén M. Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PLoS One. 2011;6(2) doi: 10.1371/journal.pone.0016885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jackson S.S., Han X., Mao Z., et al. Cancer stage, treatment, and survival among transgender patients in the United States. J Natl Cancer Inst. 2021;113(9):1221–1227. doi: 10.1093/jnci/djab028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eckhert E., Lansinger O., Ritter V., et al. Breast cancer diagnosis, treatment, and outcomes of patients from sex and gender minority groups. JAMA Oncol. 2023;9(4):473–480. doi: 10.1001/jamaoncol.2022.7146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marbac M., Sedki M. Variable selection for model-based clustering using the integrated complete-data likelihood. Stat Comput. 2017;27(4):1049–1063. [Google Scholar]
- 18.Ruppert R., Kattari S.K., Sussman S. Review: prevalence of addictions among transgender and gender diverse subgroups. Int J Environ Res Public Health. 2021;18(16):8843. doi: 10.3390/ijerph18168843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Becasen J.S., Denard C.L., Mullins M.M., Higa D.H., Sipe T.A. Estimating the prevalence of HIV and sexual behaviors among the US transgender population: a systematic review and meta-analysis, 2006-2017. Am J Public Health. 2019;109(1):e1–e8. doi: 10.2105/AJPH.2018.304727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Conron K.J., Scott G., Stowell G.S., Landers S.J. Transgender health in Massachusetts: results from a household probability sample of adults. Am J Public Health. 2012;102(1):118–122. doi: 10.2105/AJPH.2011.300315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.De Pedro K.T., Gilreath T.D., Jackson C., Esqueda M.C. Substance use among transgender students in California public middle and high schools. J Sch Health. 2017;87(5):303–309. doi: 10.1111/josh.12499. [DOI] [PubMed] [Google Scholar]
- 22.Day J.K., Fish J.N., Perez-Brumer A., Hatzenbuehler M.L., Russell S.T. Transgender youth substance use disparities: results from a population-based sample. J Adolesc Health. 2017;61(6):729–735. doi: 10.1016/j.jadohealth.2017.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Islami F., Goding Sauer A., Miller K.D., et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018;68(1):31–54. doi: 10.3322/caac.21440. [DOI] [PubMed] [Google Scholar]
- 24.I Numeri Del Cancro in Italia 2022. https://www.aiom.it/wp-content/uploads/2022/12/2022_AIOM_NDC-web.pdf Available at.
- 25.Lombardo J., Ko K., Shimada A., et al. Perceptions of and barriers to cancer screening by the sexual and gender minority community: a glimpse into the health care disparity. Cancer Causes Control. 2022;33(4):559–582. doi: 10.1007/s10552-021-01549-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McLemore K.A. A minority stress perspective on transgender individuals’ experiences with misgendering. Stigma Health. 2018;3(1):53–64. [Google Scholar]
- 27.Kamen C.S., Alpert A., Margolies L., et al. “Treat us with dignity”: a qualitative study of the experiences and recommendations of lesbian, gay, bisexual, transgender, and queer (LGBTQ) patients with cancer. Support Care Cancer. 2019;27(7):2525–2532. doi: 10.1007/s00520-018-4535-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burns Z.T., Bitterman D.S., Perni S., et al. Clinical characteristics, experiences, and outcomes of transgender patients with cancer. JAMA Oncol. 2021;7(1) doi: 10.1001/jamaoncol.2020.5671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meyer I.H. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129:674. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boehmer U., Glickman M., Winter M., Clark M.A. Long-term breast cancer survivors’ symptoms and morbidity: differences by sexual orientation? J Cancer Surviv. 2013;7:203–210. doi: 10.1007/s11764-012-0260-8. [DOI] [PubMed] [Google Scholar]
- 31.Flentje A., Kober K.M., Carrico A.W., et al. Minority stress and leukocyte gene expression in sexual minority men living with treated HIV infection. Brain Behav Immun. 2018;70:335–345. doi: 10.1016/j.bbi.2018.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seay J., Hernandez E.N., Pérez-Morales J., Quinn G.P., Schabath M.B. Assessing the effectiveness of a LGBT cultural competency training for oncologists: study protocol for a randomized pragmatic trial. Trials. 2022;23(1):314. doi: 10.1186/s13063-022-06274-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Russell S., Corbitt N. Addressing cultural competency: lesbian, gay, bisexual, transgender, and queer cancer care. Clin J Oncol Nurs. 2022;26(2):183–189. doi: 10.1188/22.CJON.183-189. [DOI] [PubMed] [Google Scholar]
- 34.Block R.G., Sampson A., Gagliardi J., et al. The LOvE ECHO training: developing a web-based LGBTQ cultural competency training module for oncology allied health professionals. J Adolesc Young Adult Oncol. 2022;11(6):556–563. doi: 10.1089/jayao.2021.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pratt-Chapman M.L., Goltz H., Latini D., et al. Affirming care for sexual and gender minority prostate cancer survivors: results from an online training. J Cancer Educ. 2022;37(4):1137–1143. doi: 10.1007/s13187-020-01930-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.ESMO E-Learning: Oncological Considerations for the LGBTQ Patients. 2021. https://oncologypro.esmo.org/education-library/esmo-e-learning-and-v-learning/oncological-considerations-for-the-lgbtq-patient Available at.
- 37.Alpert A.B., Scout N.F.N., Schabath M.B., Adams S., Obedin-Maliver J., Safer J.D. Gender- and sexual orientation- based inequities: promoting inclusion, visibility, and data accuracy in oncology. Am Soc Clin Oncol Educ Book. 2022;42:1–17. doi: 10.1200/EDBK_350175. [DOI] [PubMed] [Google Scholar]
- 38.UN General Assembly, ‘Transforming our world: the 2030 Agenda for Sustainable Development’, 21 October 2015, A/RES/70/1. https://documents-dds-ny.un.org/doc/UNDOC/GEN/N15/291/89/PDF/N1529189.pdf?OpenElement Available at.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.