Abstract
Background
The effect of cholecystectomy on the development of colorectal cancer (CRC) has prompted a large number of population-based studies. However, the results of these studies are debatable and inconclusive. Our aim in the present study was to conduct an updated systematic review and meta-analysis to explore the causality between cholecystectomy and CRC.
Methods
Cohort studies published in the PubMed, Web of Science, Embase, Medline, and Cochrane databases up to May 2022 were retrieved. Pooled relative risks (RRs) and 95% confidence intervals (CIs) were analyzed using a random effects model.
Results
Eighteen studies, involving 1,469,880 cholecystectomy and 2,356,238 non-cholecystectomy cases, were eligible for the final analysis. Cholecystectomy was not associated with the development of CRC (P=0.109), colon cancer (P=0.112), or rectal cancer (P=0.184). Subgroup analysis of sex, lag period, geographic region, and study quality revealed no significant differences in the relationship between cholecystectomy and CRC. Interestingly, cholecystectomy was significantly associated with right-sided colon cancer (RR =1.20, 95% CI: 1.04–1.38; P=0.010), especially in the cecum, the ascending colon and/or the hepatic flexure (RR =1.21, 95% CI: 1.05–1.40; P=0.007) but not in the transverse, descending, or sigmoid colon.
Conclusions
Cholecystectomy has no effect on the risk of CRC overall, but a harmful effect on the risk of right-sided colon cancer proximally.
Keywords: Cholecystectomy, colorectal cancer, cohort studies, meta-analysis
Highlight box.
Key findings
• Cholecystectomy has no effect on the overall risk of colorectal cancer (CRC), colon cancer (CC), or rectal cancer (RC), but does have a harmful effect on the risk of right-sided CC, especially in the cecum, ascending colon, and/or hepatic flexure.
What is known and what is new?
• Previous meta-analysis of cohort studies has demonstrated that cholecystectomy carries a high risk of CRC, CC and ascending CC, particularly in Western countries.
• This study indicates that cholecystectomy has a detrimental effect on the risk of right-sided CC, especially in the cecum, ascending colon, and/or hepatic flexure, but not on the risk of CRC, CC, or RC overall.
What is the implication, and what should change now?
• These results have critical implications that may warrant further investigation of colonoscopy surveillance strategies in patients undergoing cholecystectomy.
Introduction
Colorectal cancer (CRC) has become the third most common cancer and the second leading cause of malignancy-related deaths worldwide (1). Large-scale epidemiological studies have identified several risk factors associated with CRC, including smoking, alcohol addiction, excessive consumption of red and processed meat, family history of CRC, obesity, male sex, and age (2-6). However, the etiology of CRC remains debatable and obscure. Therefore, a major challenge in current research is to identify the possible causes of the initiation and progression of CRC.
Functions of the gallbladder include storing bile acids (BAs) and regulating the physiological homeostasis and enterohepatic circulation of BAs. For patients with gallstone disease (GSD), cholecystectomy, which is mostly performed laparoscopically, has become the first-line treatment (7). However, surgical removal of the gallbladder can change the secretion rhythm of BAs (8,9). Furthermore, alternations in BA composition and concentration are characterized by the enhancement of bacterial dehydroxylation of cholic acid to deoxycholic acid (DCA), which is considered to be carcinogenic to the colonic epithelium (10,11).
There is controversy surrounding the results of cohort studies focusing on the association between cholecystectomy and CRC. A previous meta-analysis of cohort studies to demonstrate the pooled effect of cholecystectomy on CRC indicated that cholecystectomy carried a high risk of CRC, colon cancer (CC) and ascending CC, especially in Western countries (12). However, previous meta-analysis had several limitations. An appropriate lag period was not taken into consideration and it should be adopted after cholecystectomy since CRC may already exist at the time the surgery is performed. In addition, significant heterogeneity was observed in the whole and subgroup analyses. These limitations resulted in more well-designed, population-based, confounding factors-adjusted cohort studies in recent years, which have added more solid evidence to the issue. Given the controversial results from previous studies and the need for further clarification, we performed an updated systematic review and meta-analysis of cohort studies to explore the association between cholecystectomy and CRC. We present this article in accordance with the PRISMA reporting checklist (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2049/rc) (13).
Methods
Literature search strategy
This meta-analysis was registered on PROSPERO (ID: CRD42022332769). The review protocol was not published or submitted online. Published articles investigating the association between cholecystectomy and CRC published up to May 2022 were retrieved from the PubMed, Web of Science, Embase, Medline, and Cochrane Library databases. The search strategy was restricted to the English language and included the following terms: (“cholecystectomy” OR “cholecystectomies”) AND (“colorectal” OR “gastrointestinal”) AND (“carcinoma” OR “cancer” OR “neoplasm” OR “adenocarcinoma”) AND “cohort study”.
Selection criteria
The inclusion criteria were as follows: (I) a cohort study with original data provided, including hazard ratio (HR), relative risk (RR), incidence rate ratio, standardized incidence ratio (SIR), and the corresponding 95% confidence intervals (CIs), or data sufficient to compute these measures; (II) explored the effects of cholecystectomy on the development of CRC; (III) the exposure factor was a previous open or laparoscopic cholecystectomy; and (IV) the outcome of interest was the development of CRC. The exclusion criteria were as follows: (I) case reports/series, letters, reviews, guidelines, protocols, replies and cross-sectional studies; (II) studies which did not precisely report HRs and 95% CIs for the outcome; (III) studies with no original data or whose data were not calculable for the outcome; (IV) studies limited to specific populations, such as patients with inflammatory bowel disease or males or females only.
The titles and abstracts of the selected literature were separately screened by two authors (L Mu and W Li). Discrepancies in the review process were verified by the senior author (D Hu). The remaining articles were separately screened through a comprehensive reading of the full text. The reference lists of articles deemed relevant during the full-text review process were cross-checked to find any relevant studies.
Data extraction and quality assessment
Two researchers conducted the data extraction process independently (Y Song and L Mu). Discrepancies that arose between the two researchers during the data collection process were discussed and resolved through consultation with the senior author (D Hu). The basic features of all the relevant studies were recorded, including the author and publication year, study characteristics, diagnosis of cholecystectomy and CRC, outcome (CRC cases), and adjustments. The Newcastle-Ottawa Scale (NOS) (14) was used to assess the study quality. We judged studies with a score of 7 to 9 to be of high quality, studies with a score of 4 to 6 to be of moderate quality, and studies with a score of 0 to 3 to be of low quality.
Two authors (Y Song and W Li) independently rated the certainty of the evidence using the GRADE system on the online GRADEpro software (https://www.gradepro.org/) (15). The GRADE system evaluates the certainty of a study in the following five dimensions: study limitations, consistency of effect, imprecision, indirectness, and publication bias (16). Using the GRADE system, the certainty of evidence in each dimension is categorized as: high, moderate, low, or very low quality.
Statistical analyses
STATA software 17.0 (StataCorp LLC, College Station, TX, USA) was used to perform all data analyses. Pooled RRs and 95% CIs were computed from SIRs, incidence rate ratios, RRs, HRs, and 95% CIs using the DerSimonian and Laird method. For the studies with a time interval following cholecystectomy, RRs were extracted and computed from data with an appropriate lag period. Subgroup analysis was also conducted. The I2 statistic was used to analyze heterogeneity (17). Significant heterogeneity was indicated by either P<0.10 or an I2 value >50%. The presence of publication bias was verified by funnel plot and Egger’s test (18). A sensitivity analysis was performed by removing each study in sequence to find the possible source of heterogeneity. P<0.05 was considered as the significance level.
Results
Study selection and characteristics
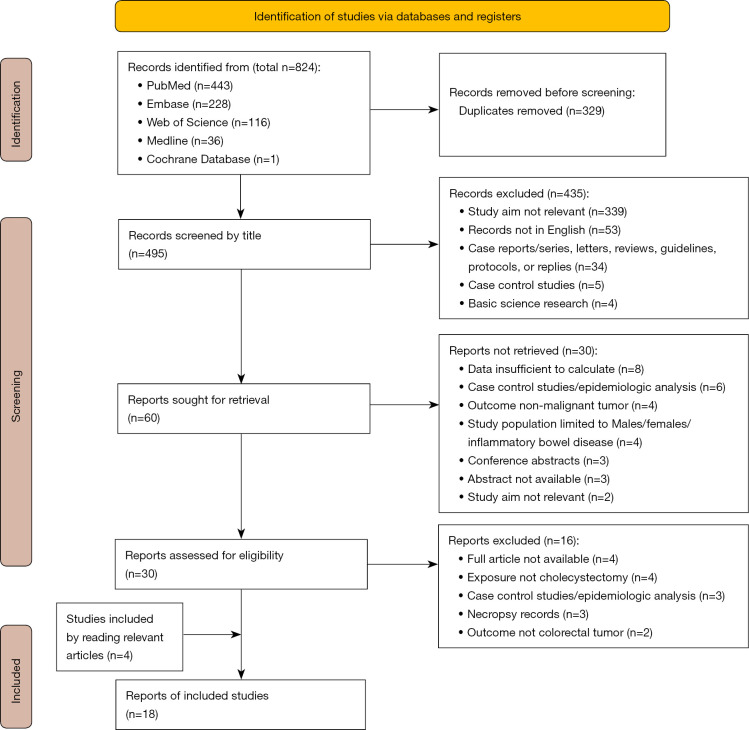
The flow diagram for literature selection is displayed in Figure 1. In total, 824 articles were identified through the database searches. Of these studies, 329 articles were excluded due to being duplicates. The remaining 495 articles were reviewed by title, and subsequently, 435 records were excluded for the following reasons: study aim not relevant (n=339); records not in English (n=53); case report/series, letter, review, guideline, protocol, or reply (n=34); case-control study (n=5); and basic science research (n=4). After further reading of the abstracts and full texts, 18 studies, involving a total of 1,469,880 cholecystectomy cases and 2,356,238 non-cholecystectomy cases, were eventually deemed eligible for inclusion (19-36).
Figure 1.
The flow diagram for the search and selection processes of the meta-analysis.
The main characteristics of the included studies are displayed in Table 1. Of the included studies, 11 were from Europe, 6 were from Asia, and 1 was from the USA. Most of the studies recruited cases either from general populations or from inpatient cohorts of individuals from healthcare programs or insurance systems. The identification of cholecystectomy was mostly based on International Classification of Diseases (ICD) codes, hospital medical records, and insurance claim codes, except in 1 study which used questionnaires (23). The diagnosis of CRC was also mainly validated based on ICD codes (C18–C20). The results of data extraction and NOS scoring are displayed in Table S1. The mean NOS score of the 18 studies was 7.11. The quality of 13 studies was high and that of the remaining 5 studies was moderate.
Table 1. Characteristics of the studies included in the systematic review and meta-analysis.
| Authors, year | Study characteristics | Identification of CS | Diagnosis of CRC | Outcome (CRC cases: CS/non-CS patients) | Adjustment |
|---|---|---|---|---|---|
| Linos et al., 1981, (19) | Retrospective cohort study (Rochester-Olmsted Epidemiology Program Project): 1681 CS cases (460 males and 1,221 females) at baseline | Medical records | Medical records | 42/– | None |
| Follow-up years: 13 years (mean) | |||||
| Lag period: 6 months | |||||
| Adami et al., 1983, (20) | Prospective population-based cohort study: 16,773 CS patients (5,095 males and 11,678 females) at baseline | ICD code | ICD code | 130/– | None |
| Follow-up period: 11–14 completed years | |||||
| Lag period: none | |||||
| Adami et al., 1987, (21) | Prospective population-based cohort study: 16,439 CS patients (4,978 males and 11,461 females) at baseline | ICD code | ICD code | 150/– | None |
| Follow-up period: 14–17 completed years | |||||
| Lag period: none | |||||
| Nielsen et al., 1991, (22) | Prospective cohort study: 3,425 CS individuals (857 males and 2,568 females) at baseline | Icelandic Cancer Registry | Icelandic Cancer Registry | 57/– | None |
| Follow-up period: 8–33 years | |||||
| Lag period: none | |||||
| Goldbohm et al., 1993, (23) | Prospective cohort study: 3,500 subjects (men: 1,688, 5.7% of gallstones and 4.7% of CS; women: 1,812, 14.7% of gallstones and 13.3% of CS) at baseline | Questionnaire | ICD code | 53/408 | Age and large-bowel cancer in first-degree relatives |
| Follow-up years: 3.3 years (mean) | |||||
| Lag period: none | |||||
| Ekbom et al., 1993, (24) | Retrospective population-based cohort study: 62,615 CS patients (20,745 males and 41,870 females) at baseline | ICD code | ICD code | 633/– | None |
| Follow-up end: until the end of 1987 | |||||
| Lag period: 1 year | |||||
| Johansen et al., 1996, (25) | Retrospective cohort study: 42,098 GSD patients (72.4% with CS) at baseline | ICD code | Danish Classification of Surgical Procedures and Therapies | 344/147 | Age, sex, and calendar year |
| Follow-up years: 1–16 years | |||||
| Lag period: 1 year | |||||
| Lagergren et al., 2001, (26) | Retrospective cohort study: 278,460 CS patients (90,987 males and 187,473 females) at baseline | ICD code | Swedish Classification of Operations and Major Procedures | 3,425/– | None |
| Follow-up years: 12.1 years (mean) | |||||
| Lag period: 1 year | |||||
| Shao et al., 2005, (27) | Retrospective cohort study: 55,960 CS patients and 574,668 randomly selected controls at baseline | General Practice Research Database | General Practice Research Database | 297/2,218 | Age |
| Follow-up end: the first diagnosis of CRC, death, dropout, or the end of database entry (i.e., April 2002) | |||||
| Lag period: 1 year | |||||
| Goldacre et al., 2005, (28) | Retrospective cohort study: 39,254 CS individuals and 334,813 reference controls at baseline | Hospital records | Hospital records | 505/3,731 | None |
| Follow-up end: the date of admission for cancer, or death, or March 31, 1999 | |||||
| Lag period: 2 years | |||||
| Goldacre et al., 2012, (29) | Retrospective cohort study: 327,460 CS individuals, 133,114 gallbladder disease individuals, and 3 million controls at baseline | ICD code | ICD code | 2,245/3,622 | Age in 5-year bands, sex, time period in single calendar years, area deprivation score in quintiles, and region of residence |
| Follow-up end: the date of the first record of colon cancer, death, or the end of the data file (March 31, 2008), whichever was the earliest | |||||
| Lag period: 1 year | |||||
| Chen et al., 2014, (30) | Retrospective cohort study: 5,850 cholelithiasis patients with CS and 62,180 controls at baseline | ICD code | Registry for Catastrophic Illness Patient Database | 67/76 | Sex, age, and comorbidities, such as diabetes mellitus, hyperlipidemia, hepatitis B infection, hepatitis C infection, menopause, and cirrhosis |
| Follow-up years: not mentioned | |||||
| Lag period: none | |||||
| Shabanzadeh et al., 2017, (31) | Retrospective cohort study: 187 CS patients and 5,327 controls at baseline | ICD code | ICD code | 11/183 | Age and sex |
| Follow up years: 24.7 years (mean) | |||||
| Lag period: no | |||||
| Lee et al., 2018, (32) | Retrospective cohort study: 11,362 CS patients and 696,301 non-CS controls at baseline | ICD code | ICD code | 34/4,276 | Sex, diabetes mellitus, and inflammatory bowel disease |
| Follow up years: 13.66 years (mean) | |||||
| Lag period: 1 year | |||||
| Chen et al., 2020, (33) | Retrospective cohort study: 83,963 CS patients and 83,963 control subjects at baseline | ICD code | ICD code | 638/1,170 | Age, gender, comorbidities of hypertension, diabetes mellitus, chronic kidney diseases, stroke, coronary artery disease, colorectal adenomas, and chronic obstructive pulmonary disease |
| Follow-up end: the development of CRC, death, withdrawal from the National Health Insurance program due to emigration or death, or 31 December, 2011 | |||||
| Lag period: 6 months | |||||
| Kim et al., 2020, (34) | Retrospective cohort study: 3,588 CS patients at baseline | Single hospital records | Single hospital records | 21/– | None |
| Follow-up years: 15.0 (range, 0–146) months | |||||
| Lag period: 1 year | |||||
| Jung et al., 2021, (35) | Retrospective cohort study: 408,769 CS patients at baseline | Insurance claims codes | ICD code | 1,773/– | None |
| Follow-up years: 4.7 years (mean) | |||||
| Lag period: 1 year | |||||
| Choi et al., 2022, (36) | Retrospective cohort study: A total of 123,295 control subjects and 123,925 age and sex-matched CS subjects at baseline | Insurance claims codes | ICD code | 1,078/1,003 | Age, sex, smoking status, body mass index, hypertension, diabetes mellitus, and dyslipidemia |
| Follow-up years: 4.59 years (mean) | |||||
| Lag period: 1 year |
CS, cholecystectomy; CRC, colorectal cancer; ICD, International Classification of Diseases; GSD, gallstone disease.
Synthesis of the results
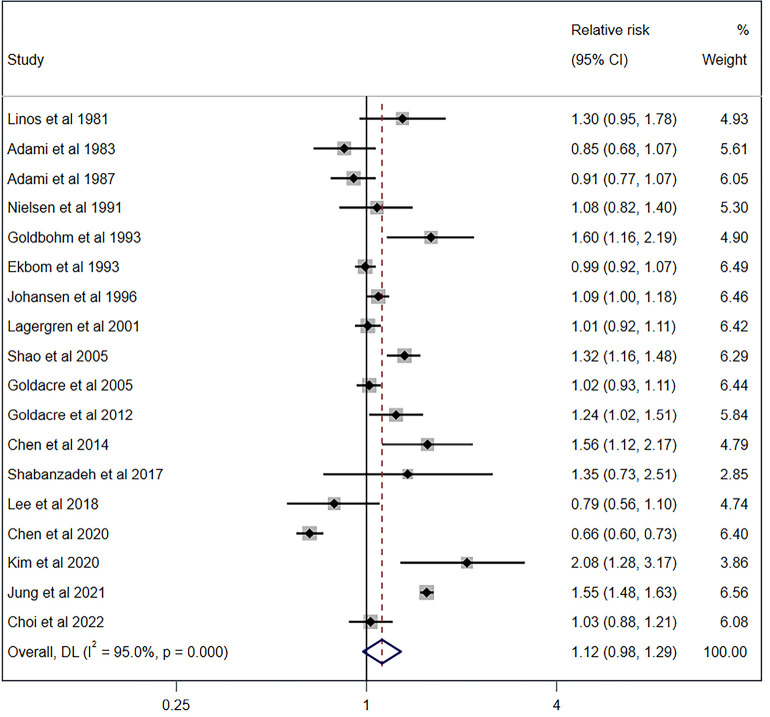
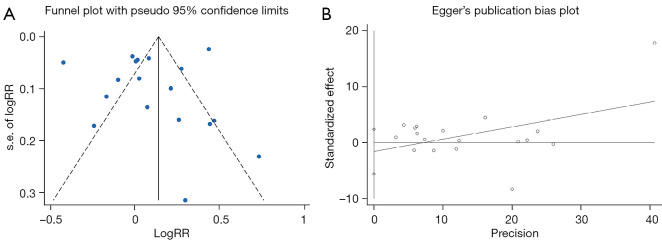
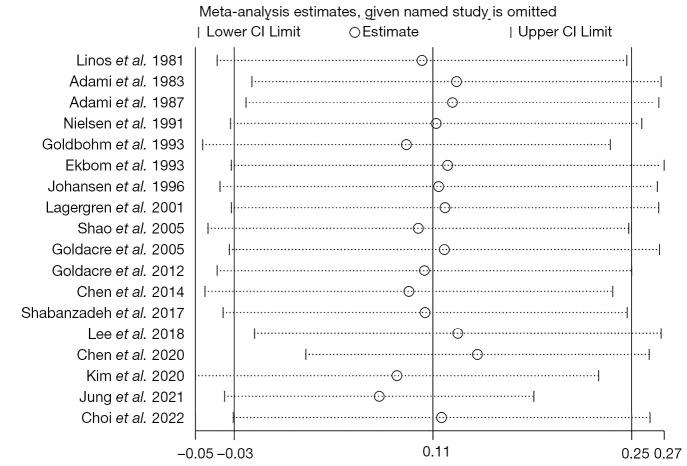
Synthesis of the studies’ results was conducted using a random effects model. As shown in Figure 2, cholecystectomy exhibited no association with CRC (RR =1.12, 95% CI: 0.98–1.29; P=0.109; I2=95.0%). No statistically significant publication bias was detected through funnel plot analysis and Egger’s tests (Figure 3, P=0.411). A sensitivity analysis was also conducted, and the result was not affected by the removal of each study in sequence (Figure 4).
Figure 2.
Forest plot and pooled estimates of the effect of cholecystectomy on the risk of colorectal cancer. Weights are from a random effects model. CI, confidence interval; DL, DerSimonian and Laird.
Figure 3.
Publication bias of the included studies. (A) Funnel plot for publication bias. (B) Egger’s test results. RR, relative risk; s.e., standard error.
Figure 4.
Sensitivity analysis of the colorectal cancer risk associated with cholecystectomy. CI, confidence interval.
Subgroup analyses
Subgroup analyses were conducted based on sex, geographic region, lag period, study quality, time interval since cholecystectomy, and tumor location. Subgroup analyses of sex (male: P=0.365; female: P=0.274), geographic region (Europe: P=0.071; Asia: P=0.471; USA: P=0.101), lag period (with lag period: P=0.238; no lag period: P=0.237), study quality (high: P=0.243; moderate or low: P=0.215) showed no significant differences in the relationship between cholecystectomy and CRC (Table 2). Regarding the time interval after surgery, cholecystectomy was not associated with CC or rectal cancer (RC) in patients who had undergone cholecystectomy ≤4 years or ≥5 years (Table 2).
Table 2. Subgroup analyses of the association between cholecystectomy and the risk of colorectal cancer, stratified by sex, geographic region, lag period, study quality, and time interval since cholecystectomy.
| Group | Subgroup | RR (95% CI) | Test for overall effect (P value) | No. of studies | Heterogeneity I2, % |
|---|---|---|---|---|---|
| Sex | Male | 1.13 (0.87–1.46) | 0.365 | 10 | 94.9 |
| Female | 1.13 (0.91–1.41) | 0.274 | 10 | 92.8 | |
| Geographic region | USA | 1.30 (0.95–1.78) | 0.101 | 1 | 0.0 |
| Europe | 1.07 (0.99–1.16) | 0.071 | 11 | 70.7 | |
| Asia | 1.16 (0.77–1.76) | 0.471 | 6 | 98.0 | |
| Lag period | Lag period | 1.11 (0.94–1.31) | 0.238 | 12 | 96.6 |
| No lag period | 1.14 (0.92–1.43) | 0.237 | 6 | 73.9 | |
| Study quality | High | 1.09 (0.94–1.26) | 0.243 | 13 | 90.0 |
| Moderate or low | 1.18 (0.91–1.55) | 0.215 | 5 | 97.3 | |
| Time interval since cholecystectomy | |||||
| 1–4 years | CC | 1.25 (0.90–1.73) | 0.178 | 3 | 91.5 |
| RC | 1.28 (0.94–1.73) | 0.112 | 3 | 84.4 | |
| ≥5 years | CC | 1.06 (0.98–1.15) | 0.124 | 3 | 0.0 |
| RC | 0.96 (0.82–1.12) | 0.572 | 3 | 44.1 | |
RR, relative risk; CI, confidential interval; CC, colon cancer; RC, rectal cancer.
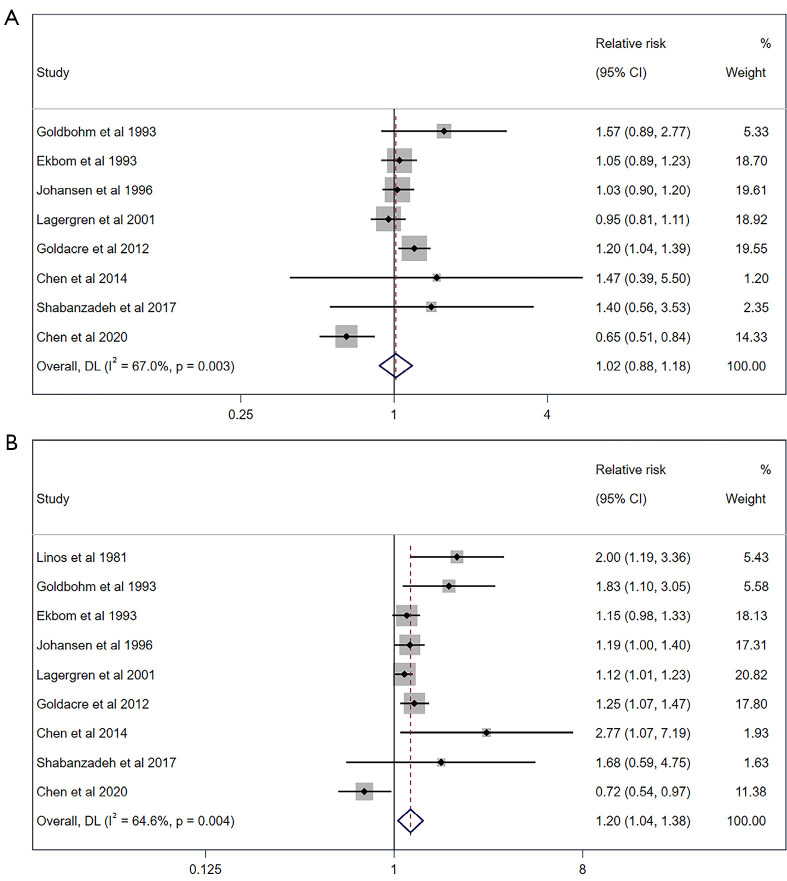
The subgroup analysis of tumor location revealed no association of cholecystectomy with CC overall (P=0.112), RC (P=0.184) or left-sided CC (P=0.836) (Table 3; Figure 5A). However, the association was significant for the risk of right-sided CC (RR =1.20; 95% CI: 1.04–1.38; P=0.010; I2=64.6%; Figure 5B), especially in the cecum, the ascending colon, and/or the hepatic flexure (RR =1.21; 95% CI: 1.05–1.40; P=0.007; I2=49.3%), but not in the transverse (P=0.397), descending (P=0.769), or sigmoid (P=0.635) colon (Table 3).
Table 3. Subgroup analyses of the association between cholecystectomy and the risk of colorectal cancer, stratified by tumor location.
| Subgroup | RR (95% CI) | Test for overall effect (P value) | No. of studies | Heterogeneity I2, % |
|---|---|---|---|---|
| CC | 1.08 (0.98–1.19) | 0.112 | 16 | 76.5 |
| Left-sided | 1.02 (0.88–1.18) | 0.836 | 8 | 67.0 |
| Right-sided | 1.20 (1.04–1.38) | 0.010 | 9 | 64.6 |
| Cecum/ascending colon/hepatic flexure | 1.21 (1.05–1.40) | 0.007 | 3 | 49.3 |
| Transverse | 1.05 (0.94–1.18) | 0.397 | 2 | 0 |
| Descending | 1.08 (0.64–1.85) | 0.769 | 2 | 83.7 |
| Sigmoid | 1.02 (0.94–1.10) | 0.635 | 3 | 0 |
| RC | 0.94 (0.86–1.03) | 0.184 | 16 | 56.7 |
CC, colon cancer; RC, rectal cancer; RR, relative risk; CI, confidential interval.
Figure 5.
Forest plot and pooled estimates of the effect of cholecystectomy on the risk of left-sided colon cancer (A) and right-sided colon cancer (B). Weights are from a random effects model. CI, confidence interval; DL, DerSimonian and Laird.
Discussion
In the current study, we explored the association of cholecystectomy with the development of CRC. The results show that the overall risk of CRC was comparable between patients with cholecystectomy and those without in the general population, as well as in subgroup analysis for sex, lag period, study quality, and geographic origin. However, a positive association was identified between cholecystectomy and the risk of right-sided CC, especially in the cecum, the ascending colon, and/or the hepatic flexure. These results have critical implications that may warrant further investigation for colonoscopy surveillance strategies in individuals who undergo cholecystectomy.
Cholecystectomy has remained one of the most frequently performed and effective treatments for gallbladder diseases, especially symptomatic GSD. However, increasing concern has been raised regarding the long-term risks of cholecystectomy, such as the development of CRC. Numerous case-control and cohort studies, as well as a previous meta-analysis, have provided substantial evidence of an increased CRC risk following cholecystectomy. Several mechanisms may account for this possible association. First, the circadian rhythmicity of BAs after cholecystectomy is diminished, resulting in continuous bile secretion into the bowel (9,37). Second, patients who undergo cholecystectomy have been found to exhibit higher concentrations of total fecal BA and DCA (38). Third, constant exposure to high levels of BAs might cause DNA damage, such as oxidative stress, oncogene mutations, and microsatellite instability (39). Fourth, the composition and abundance of gut microbiota becomes altered after cholecystectomy, which is characterized by an elevated abundance of the Bacteroidetes phylum, specifically members of the Bacteroidaceae family and the genus Bacteroides (40), as well as Blautia obeum and Veillonella parvula (41).
However, the results of studies regarding the above mechanisms remain disputable. For example, several studies have concluded that cholecystectomy has no prominent effect on the concentration and composition of BAs (10,40). This controversy may be attributable to differences in subjects in the control group. In some studies, the control group, namely non-cholecystectomy group, is composed of individuals with normal gallbladder, patients with asymptomatic gall stones, gallbladder polyps, etc. Keren et al. reported that cholecystectomy-treated patients exhibited higher levels of BAs than the controls without GSD or cholecystectomy, but had comparable concentrations to patients with GSD (40). Further analysis indicated that levels of primary and secondary BAs did not differ among the three groups (40). Furthermore, as for microbiota change in relation to cholecystectomy, current studies mainly focused on the analysis limited to phylum and genus, while the real pro-carcinogenic influence of microbiota should be ascribed to specific species, such as the pro-carcinogenic effect of enterotoxigenic Bacteroides fragilis in CRC (42,43).
The main findings of the current study were that cholecystectomy was only associated with an increased risk of right-sided CC, especially in the cecum, the ascending colon, and/or the hepatic flexure, but not with the overall risk of CRC, CC, RC, or cancers in other segments of the colon. These findings represent interesting results which differ from those of a previous meta-analysis of cohort studies (12). The preference of right-sided CC after cholecystectomy partially coincided with previous descriptive analysis indicating that highest proportion of ascending CC (10.5%) was observed following cholecystectomy (44), and with results of previous meta-analyses of case-control studies (45,46). One possible explanation for these findings is that the absorption of secondary BAs is more significant proximally than distally (19). The distribution of BA in different segments of the colon might be another possible explanation. In a human study, the levels of total tissue-bound BA, especially chenodeoxycholic acid, were found to be higher in the ascending colon than in other parts of the colon (47). In animal studies, the levels of DCA and hyodeoxycholic acid in the cecum (16% and 21%, respectively) were higher than those in the colon (8% and 17%, respectively) (48). Based on the pro-carcinogenic effect of DCA on CRC (49,50), it was postulated that the proximal part of the large intestine was continuously exposed to higher concentrations of deleterious BAs, which may account for the predilection of right-sided CC.
Our meta-analysis has several limitations that warrant consideration. First, the certainty of the evidence was low according to assessment of several limitations, indirectness, and imprecision. For several study limitations, the evidence was downgraded due to, for example, the risk of selection bias or suspected potential reporting bias. When considering possible biases, imbalances between study groups, such as genetic differences that may lead to susceptibility to CRC and environmental and lifestyle-related factors, may represent potential sources of biases in this study. In addition, in some studies, the definition of the non-cholecystectomized group was unclear. Since patients with GSD and non-cholecystectomized individuals without GSD showed distinctions in BA concentration and composition, as well as other differences, discrepancies may have existed during the comparison.
Conclusions
This updated meta-analysis shows that while cholecystectomy has no effect on the overall risk of CRC, CC, and RC, it does have a harmful effect on the risk of right-sided CC, especially in the cecum, the ascending colon, and/or the hepatic flexure. However, additional evidence is needed to elucidate this complex association.
Supplementary
The article’s supplementary files as
Acknowledgments
The authors thank Dr. Yao Tong (from Department of Anesthesia, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai) for his excellent assistance in data analysis. The authors also thank all the involved physicians and nurses for their efforts to this study.
Funding: This work was supported by a grant from the National Natural Science Foundation of China (No. 81800543).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2049/rc
Data Sharing Statement: Available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2049/dss
Peer Review File: Available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2049/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2049/coif). The authors have no conflicts of interest to declare.
(English Language Editors: C. Mullens and J. Reylonds)
References
- 1.Baidoun F, Elshiwy K, Elkeraie Y, et al. Colorectal Cancer Epidemiology: Recent Trends and Impact on Outcomes. Curr Drug Targets 2021;22:998-1009. 10.2174/1389450121999201117115717 [DOI] [PubMed] [Google Scholar]
- 2.Botteri E, Borroni E, Sloan EK, et al. Smoking and Colorectal Cancer Risk, Overall and by Molecular Subtypes: A Meta-Analysis. Am J Gastroenterol 2020;115:1940-9. 10.14309/ajg.0000000000000803 [DOI] [PubMed] [Google Scholar]
- 3.O'Sullivan DE, Sutherland RL, Town S, et al. Risk Factors for Early-Onset Colorectal Cancer: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol 2022;20:1229-1240.e5. 10.1016/j.cgh.2021.01.037 [DOI] [PubMed] [Google Scholar]
- 4.Farvid MS, Sidahmed E, Spence ND, et al. Consumption of red meat and processed meat and cancer incidence: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol 2021;36:937-51. 10.1007/s10654-021-00741-9 [DOI] [PubMed] [Google Scholar]
- 5.Sekiguchi M, Kakugawa Y, Nakamura K, et al. Family history of colorectal cancer and prevalence of advanced colorectal neoplasia in asymptomatic screened populations in different age groups. Gastrointest Endosc 2020;91:1361-70. 10.1016/j.gie.2020.01.033 [DOI] [PubMed] [Google Scholar]
- 6.Elangovan A, Skeans J, Landsman M, et al. Colorectal Cancer, Age, and Obesity-Related Comorbidities: A Large Database Study. Dig Dis Sci 2021;66:3156-63. 10.1007/s10620-020-06602-x [DOI] [PubMed] [Google Scholar]
- 7.Lamberts MP. Indications of cholecystectomy in gallstone disease. Curr Opin Gastroenterol 2018;34:97-102. 10.1097/MOG.0000000000000419 [DOI] [PubMed] [Google Scholar]
- 8.Almond HR, Vlahcevic ZR, Bell CC, Jr, et al. Bile acid pools, kinetics and biliary lipid composition before and after cholecystectomy. N Engl J Med 1973;289:1213-6. 10.1056/NEJM197312062892302 [DOI] [PubMed] [Google Scholar]
- 9.Zhang F, Duan Y, Xi L, et al. The influences of cholecystectomy on the circadian rhythms of bile acids as well as the enterohepatic transporters and enzymes systems in mice. Chronobiol Int 2018;35:673-90. 10.1080/07420528.2018.1426596 [DOI] [PubMed] [Google Scholar]
- 10.Kullak-Ublick GA, Paumgartner G, Berr F. Long-term effects of cholecystectomy on bile acid metabolism. Hepatology 1995;21:41-5. 10.1002/hep.1840210109 [DOI] [PubMed] [Google Scholar]
- 11.Yao Y, Li X, Xu B, et al. Cholecystectomy promotes colon carcinogenesis by activating the Wnt signaling pathway by increasing the deoxycholic acid level. Cell Commun Signal 2022;20:71. 10.1186/s12964-022-00890-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang Y, Liu H, Li L, et al. Cholecystectomy can increase the risk of colorectal cancer: A meta-analysis of 10 cohort studies. PLoS One 2017;12:e0181852. 10.1371/journal.pone.0181852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 2021;372:n160. 10.1136/bmj.n160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wells GA, Shea BJ, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Meta-Analysis. Ottawa, ON: Ottawa Hospital Research Institute, 2009. [Google Scholar]
- 15.Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490. 10.1136/bmj.328.7454.1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924-6. 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greenland S. Quantitative methods in the review of epidemiologic literature. Epidemiol Rev 1987;9:1-30. 10.1093/oxfordjournals.epirev.a036298 [DOI] [PubMed] [Google Scholar]
- 18.Harbord RM, Egger M, Sterne JA. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med 2006;25:3443-57. 10.1002/sim.2380 [DOI] [PubMed] [Google Scholar]
- 19.Linos D, Beard CM, O'Fallon WM, et al. Cholecystectomy and carcinoma of the colon. Lancet 1981;2:379-81. 10.1016/S0140-6736(81)90829-1 [DOI] [PubMed] [Google Scholar]
- 20.Adami HO, Meirik O, Gustavsson S, et al. Colorectal cancer after cholecystectomy: absence of risk increase within 11-14 years. Gastroenterology 1983;85:859-65. 10.1016/0016-5085(83)90436-5 [DOI] [PubMed] [Google Scholar]
- 21.Adami HO, Krusemo UB, Meirik O. Unaltered risk of colorectal cancer within 14-17 years of cholecystectomy: updating of a population-based cohort study. Br J Surg 1987;74:675-8. 10.1002/bjs.1800740807 [DOI] [PubMed] [Google Scholar]
- 22.Nielsen GP, Theodors A, Tulinius H, et al. Cholecystectomy and colorectal carcinoma: a total-population historical prospective study. Am J Gastroenterol 1991;86:1486-90. [PubMed] [Google Scholar]
- 23.Goldbohm RA, van den Brandt PA, van 't Veer P, et al. Cholecystectomy and colorectal cancer: evidence from a cohort study on diet and cancer. Int J Cancer 1993;53:735-9. 10.1002/ijc.2910530505 [DOI] [PubMed] [Google Scholar]
- 24.Ekbom A, Yuen J, Adami HO, et al. Cholecystectomy and colorectal cancer. Gastroenterology 1993;105:142-7. 10.1016/0016-5085(93)90019-9 [DOI] [PubMed] [Google Scholar]
- 25.Johansen C, Chow WH, Jørgensen T, et al. Risk of colorectal cancer and other cancers in patients with gall stones. Gut 1996;39:439-43. 10.1136/gut.39.3.439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lagergren J, Ye W, Ekbom A. Intestinal cancer after cholecystectomy: is bile involved in carcinogenesis? Gastroenterology 2001;121:542-7. 10.1053/gast.2001.27083 [DOI] [PubMed] [Google Scholar]
- 27.Shao T, Yang YX. Cholecystectomy and the risk of colorectal cancer. Am J Gastroenterol 2005;100:1813-20. 10.1111/j.1572-0241.2005.41610.x [DOI] [PubMed] [Google Scholar]
- 28.Goldacre MJ, Abisgold JD, Seagroatt V, et al. Cancer after cholecystectomy: record-linkage cohort study. Br J Cancer 2005;92:1307-9. 10.1038/sj.bjc.6602392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldacre MJ, Wotton CJ, Abisgold J, et al. Association between cholecystectomy and intestinal cancer: a national record linkage study. Ann Surg 2012;256:1068-72. 10.1097/SLA.0b013e3182759efb [DOI] [PubMed] [Google Scholar]
- 30.Chen YK, Yeh JH, Lin CL, et al. Cancer risk in patients with cholelithiasis and after cholecystectomy: a nationwide cohort study. J Gastroenterol 2014;49:923-31. 10.1007/s00535-013-0846-6 [DOI] [PubMed] [Google Scholar]
- 31.Shabanzadeh DM, Sørensen LT, Jørgensen T. Association Between Screen-Detected Gallstone Disease and Cancer in a Cohort Study. Gastroenterology 2017;152:1965-1974.e1. 10.1053/j.gastro.2017.02.013 [DOI] [PubMed] [Google Scholar]
- 32.Lee J, Choe S, Park JW, et al. The Risk of Colorectal Cancer After Cholecystectomy or Appendectomy: A Population-based Cohort Study in Korea. J Prev Med Public Health 2018;51:281-8. 10.3961/jpmph.18.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen CH, Lin CL, Kao CH. The Effect of Cholecystectomy on the Risk of Colorectal Cancer in Patients with Gallbladder Stones. Cancers (Basel) 2020;12:550. 10.3390/cancers12030550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim SB, Kim KO, Kim TN. Prevalence and Risk Factors of Gastric and Colorectal Cancer after Cholecystectomy. J Korean Med Sci 2020;35:e354. 10.3346/jkms.2020.35.e354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jung YK, Yoon J, Lee KG, et al. De Novo Cancer Incidence after Cholecystectomy in Korean Population. J Clin Med 2021;10:1445. 10.3390/jcm10071445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choi YJ, Jin EH, Lim JH, et al. Increased Risk of Cancer after Cholecystectomy: A Nationwide Cohort Study in Korea including 123,295 Patients. Gut Liver 2022;16:465-73. 10.5009/gnl210009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pomare EW, Heaton KW. The effect of cholecystectomy on bile salt metabolism. Gut 1973;14:753-62. 10.1136/gut.14.10.753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Breuer NF, Jaekel S, Dommes P, et al. Fecal bile acid excretion pattern in cholecystectomized patients. Dig Dis Sci 1986;31:953-60. 10.1007/BF01303216 [DOI] [PubMed] [Google Scholar]
- 39.Payne CM, Bernstein C, Dvorak K, et al. Hydrophobic bile acids, genomic instability, Darwinian selection, and colon carcinogenesis. Clin Exp Gastroenterol 2008;1:19-47. 10.2147/CEG.S4343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Keren N, Konikoff FM, Paitan Y, et al. Interactions between the intestinal microbiota and bile acids in gallstones patients. Environ Microbiol Rep 2015;7:874-80. 10.1111/1758-2229.12319 [DOI] [PubMed] [Google Scholar]
- 41.Roberts DC, Chidambaram S, Kinross JM. The role of the colonic microbiota and bile acids in colorectal cancer. Curr Opin Gastroenterol 2022;38:179-88. 10.1097/MOG.0000000000000816 [DOI] [PubMed] [Google Scholar]
- 42.Zamani S, Taslimi R, Sarabi A, et al. Enterotoxigenic Bacteroides fragilis: A Possible Etiological Candidate for Bacterially-Induced Colorectal Precancerous and Cancerous Lesions. Front Cell Infect Microbiol 2020;9:449. 10.3389/fcimb.2019.00449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Khodaverdi N, Zeighami H, Jalilvand A, et al. High frequency of enterotoxigenic Bacteroides fragilis and Enterococcus faecalis in the paraffin-embedded tissues of Iranian colorectal cancer patients. BMC Cancer 2021;21:1353. 10.1186/s12885-021-09110-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vernick LJ, Kuller LH, Lohsoonthorn P, et al. Relationship between cholecystectomy and ascending colon cancer. Cancer 1980;45:392-5. [DOI] [PubMed] [Google Scholar]
- 45.Giovannucci E, Colditz GA, Stampfer MJ. A meta-analysis of cholecystectomy and risk of colorectal cancer. Gastroenterology 1993;105:130-41. 10.1016/0016-5085(93)90018-8 [DOI] [PubMed] [Google Scholar]
- 46.Reid FD, Mercer PM, harrison M, et al. Cholecystectomy as a risk factor for colorectal cancer: a meta-analysis. Scand J Gastroenterol 1996;31:160-9. 10.3109/00365529609031981 [DOI] [PubMed] [Google Scholar]
- 47.Nakashima T, Seto Y, Nakajima T, et al. Distribution of tissue bile acids in the human alimentary tract and colon polyps. Jpn J Med 1989;28:25-9. 10.2169/internalmedicine1962.28.25 [DOI] [PubMed] [Google Scholar]
- 48.Yang T, Shu T, Liu G, et al. Quantitative profiling of 19 bile acids in rat plasma, liver, bile and different intestinal section contents to investigate bile acid homeostasis and the application of temporal variation of endogenous bile acids. J Steroid Biochem Mol Biol 2017;172:69-78. 10.1016/j.jsbmb.2017.05.015 [DOI] [PubMed] [Google Scholar]
- 49.Liu L, Dong W, Wang S, et al. Deoxycholic acid disrupts the intestinal mucosal barrier and promotes intestinal tumorigenesis. Food Funct 2018;9:5588-97. 10.1039/C8FO01143E [DOI] [PubMed] [Google Scholar]
- 50.Liu Y, Zhang S, Zhou W, et al. Secondary Bile Acids and Tumorigenesis in Colorectal Cancer. Front Oncol 2022;12:813745. 10.3389/fonc.2022.813745 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as