Abstract
To our knowledge, no systematic review with meta-analysis has separately synthesized the effects of Mediterranean diet-based interventions in children and adolescents in relation to the effects on anthropometric measures. A better understanding of the effects of Mediterranean diet-based interventions on anthropometric variables could facilitate their implementation in efforts to prevent obesity in the young population. The aim of the present meta-analysis was to evaluate the effects of Mediterranean diet-based interventions on anthropometric and obesity indicators among children and adolescents. Four databases were systematically searched (PubMed, Scopus, Web of Science, and Cochrane Database of Systematic Reviews), including all studies up until 15 March, 2023. Eligible articles were randomized controlled trials measuring the effect of an intervention based on the promotion of the Mediterranean diet and obesity-associated parameters. The effect size of each study was estimated by Cohen’s d for continuous variables or risk difference for categorical variables. Compared to the control group, the Mediterranean diet-based interventions showed small and significant reductions in body mass index (d = −0.14; 95% CI: −0.26, −0.01; I2 = 77.52%). Participants in the Mediterranean diet-based interventions had a significant reduction in the percentage of obesity (risk difference = 0.12; 95% CI: 0.01, 0.23; I2 = 84.56%) in comparison with the control group. Interventions had greater effects when aiming at participants with excess weight (that is, overweight or obesity), both for body mass index, waist circumference, waist-to-height ratio, percentage of obesity, and percentage of abdominal obesity. Mediterranean diet-based interventions have a significant effect on reducing the body mass index as well as reducing obesity in children and adolescents (aged 3–18 y). This trial was registered at PROSPERO as CRD42023386789.
Keywords: obesity, overweight, lifestyle, eating healthy, youths, young population, preschoolers
Statement of Significance.
-
-
No systematic review with meta-analysis has synthesized the effects of Mediterranean diet-based interventions in children and adolescents in relation to the effects on anthropometric measures.
-
-
Mediterranean diet-based interventions seem to be a useful tool in the interest of reversing the high prevalence of obesity.
Introduction
Childhood obesity has been postulated as one of the most serious public health problems of the 21st century due to its chronic adverse consequences [1]. Globally, excess weight (overweight or obesity) in childhood represents a major public health threat, especially in Europe, where the latest round of the Childhood Obesity Surveillance Initiative (COSI) [2], involving 33 European countries, indicated that 29% of children aged 7 to 9 y had excess weight according to WHO criteria (31% in boys and 28% in girls). Furthermore, the risk of morbidity and mortality in adult life increases in those with excess weight in childhood or adolescence [3]. For this reason, the member states of the WHO have committed themselves to prevent further increases in childhood obesity rates after 2025 [4].
The etiology of obesity is complex [5] and involves the interaction of social [6], biological [6], genetic [7], and environmental factors [6,8], among others [6]. Concerning genetics, between 40% and 70% of the variation in BMI could be attributable to hereditary factors [9]. Polygenic obesity is the most common, whereas single-gene (monogenic) obesity-related syndromes and defects account for <1% of childhood obesity [10,11]. Regarding environmental factors, the WHO has especially attributed 2 factors to the current increase in the prevalence of obesity: first, the consumption of high-calorie foods that are rich in sugar and fat has increased significantly; second, people are becoming more sedentary due to changes in work patterns, transportation methods, and the growing urbanization trend [12]. Furthermore, diet quality has been suggested to play a moderating role in the relationship between some health outcomes (for example, inflammatory biomarkers [13] and psychosocial health [14]) and excess weight. In addition, the recommended levels of physical activity, sedentary behavior, and sleep duration in adolescence have been related to a lower risk of abdominal obesity later in life [15]. Therefore, lifestyle modifications, including dietary modifications aimed at reducing total energy intake, increasing physical activity, and decreasing sedentary time, seem to be crucial for the control of body weight [3].
Among healthy dietary patterns, the Mediterranean diet (MedDiet) has been recognized worldwide due to its distinctive health benefits [16,17]. The MedDiet is characterized by a pattern rich in fruits and vegetables (seasonal), legumes, whole grains, nuts, and olive oil as the main dietary fat, with greater consumption of white or lean meats than of red or processed meats, moderate consumption of dairy products (cheese and milk), moderate consumption of fish and eggs, and intake of small amounts of wine with meals [18]. Supporting this notion, scientific evidence supports an inverse relationship between MedDiet and noncommunicable diseases (for example, cancer, metabolic syndrome, hypertension, or cardiovascular diseases) [19], as well as mortality [20], with some of the dietary components mentioned above having a substantial influence on this relationship [20]. Specifically, in young people, greater adherence to an MedDiet [16] has been associated with greater anti-inflammatory potential [21], physical fitness [22], or health-related quality of life [23]. However, despite being an evidence-based healthy pattern, a systematic review has pointed out the clear trend of decreasing MedDiet adherence in Mediterranean countries between 2004 and 2014, especially among children [24].
Despite the large number of studies published to date, there is only limited evidence of the beneficial effect of adherence to traditional MedDiet in maintaining a healthy body weight in childhood [25]. Moreover, with scientific evidence coming from mostly cross-sectional studies, it is difficult to draw conclusions on the effects of MedDiet adherence for improving anthropometric indicators among youth [25]. To our knowledge, no systematic review with meta-analysis has separately synthesized the effects of MedDiet-based interventions in children and adolescents in relation to the effects on anthropometric measures. A better understanding of the effects of MedDiet-based interventions on anthropometric variables could facilitate their implementation in efforts to reduce obesity in the young population. Therefore, the aim of the present meta-analysis was to evaluate the effects of MedDiet-based interventions on anthropometric and obesity indicators among children and adolescents.
Methods
Search strategy and selection of studies
The present review and meta-analysis were reported in accordance with the principles of the PRISMA statement [26] and following the recommendations of the Cochrane Collaboration Manual for Systematic Reviews of Interventions [27]. This systematic review and meta-analysis were registered at PROSPERO (registry number CRD42023386789).
Eligibility criteria
Eligible articles were randomized controlled trials (RCTs) measuring the effect of an intervention based on the promotion of MedDiet and obesity-associated parameters. The search and selection of studies were performed by 2 independent reviewers who examined the titles and abstracts. Inclusion criteria were as follows: 1) children or adolescents ≤18 y old; 2) outcomes, assessments of anthropometric indicators using standardized tests; 3) study design: RCTs; and 4) studies with MedDiet-based interventions. Studies were excluded if they were review articles, editorials, or case reports.
Information sources and search strategy
A systematic search of the MEDLINE (via PubMed), Scopus, Cochrane, and Web of Science databases included all studies up until 15 March, 2023. The search strategy included the following terms: 1) “children,” “adolescents,” “youths,” or “preschoolers,” “teenagers”; 2) “Mediterranean diet”; 3) “anthropometric measurements,” “body mass index,” “obesity,” “overweight,” “excess weight,” “adiposity,” “abdominal obesity,” “body fat,” “fat mass,” or “high trunk fat mass”; and 4) “intervention,” “clinical trial,” “randomized clinical trial,” “randomized clinical trial,” “randomized controlled trial,” “randomized controlled trial,” or “RCT.” Finally, the reference lists of the studies included in this systematic review were examined to find any relevant studies. Supplemental Table 1 shows the complete MEDLINE search strategy.
The selection process
The strategy was designed around the Participants, Intervention, Comparison, Outcome, and Study design (PICOS) question format: Are there differences in children and adolescents (participants) who participate in an MedDiet-based intervention (intervention) compared with those who do not participate (comparator) in anthropometric or obesity indicators (BMI, waist circumference [WC], waist-to-height ratio [WHtR], percentage of obesity, or percentage of abdominal obesity) (outcome) in RCTs (study design)?
Data collection process and data items
The following information was extracted from the included studies: 1) reference (y); 2) country of intervention; 3) characteristics of subjects, including total sample size, size of intervention and control group, sex ratio, age range, mean age, and baseline weight status; 4) duration of intervention (wk); 5) type of intervention; and 6) outcome information, including information on the anthropometric indicators and obesity prevalence analyzed. All results compatible with each outcome domain in each study were included. In the case of missing information in the published article, the corresponding authors of these studies were contacted directly to request the information.
Study risk of bias assessment
The risk of bias of the RCTs was assessed using the Cochrane risk of bias tool for randomized trials or cluster randomized trials (RoB 2.0) [28], in which 5 domains were assessed: randomization process, deviations from intended interventions, missing outcome data, outcome measurement, and selection of the reported outcome. The risk of bias was assessed in each domain. Studies were classified as 1) “low risk” of bias when a low risk of bias was determined for all domains; 2) “some concerns” if ≥1 domain was assessed as raising some concerns but did not have a high risk of bias for any individual domain; or 3) “high risk” of bias when a high risk of bias was obtained for ≥1 domain or the study judgment included “some concerns” across multiple domains [28].
Effect measures
The effect size of each study was estimated by Cohen’s d and included in the meta-analysis to verify the effect of MedDiet-based interventions on continuous markers related to childhood obesity (BMI, WC, and WHtR). For categorical markers (that is, percentage of obesity and abdominal obesity), the risk difference and the number needed to treat (NNT) were determined [27]. The risk difference is the difference between the observed risks (proportions of individuals with the outcome of interest) in the 2 groups. The NNT was applied, being the expected number of people who need to receive the experimental rather than the comparator intervention for one additional person to either incur or avoid an event in a given time frame. Analyses were performed using Stata 17.0 software (Stata, College Station, TX, United States) for Windows.
Synthesis methods
Different meta-analyses were independently performed to examine the effect of MedDiet promotion-based interventions on anthropometric and weight management indicators, such as BMI, WC, WHtR, percentage of obesity, and percentage of abdominal obesity. We used a common interpretation to report effect sizes as small (d ∼ 0.2), medium (d ∼ 0.5), and large (d ∼ 0.8) [29]. For both, the Hartung–Knapp–Sidik–Jonkman method for random effects was used to calculate the overall estimate of the effect size and its respective 95% CIs. This decision is justified by the fact that the Hartung–Knapp–Sidik–Jonkman method consistently provides better error rates than the traditional DerSimonian and Laird method, especially when the number of studies is small [30]. Furthermore, prior to analyses, multiple groups from Lisón et al. [31] were combined groups to create a single pairwise comparison (as recommended by the Cochrane Collaboration Manual for Systematic Reviews of Interventions [27]). Heterogeneity was examined using the I2 statistic, which ranges from 0% to 100% [32]. The I2 values were interpreted as not important (0% to 30%), moderate (30% to 60%), substantial (60% to 75%), or considerable (75% to 100%).
To assess the robustness of the estimates obtained, sensitivity analyses were performed by eliminating (one at a time) each study from the total estimates. In addition, subgroup analyses were performed according to the type of country in which the intervention was carried out (that is, Mediterranean or nonMediterranean country), as well as according to the baseline weight status of the participants (that is, all weight statuses or only participants with overweight/obesity). Meta-regression analyses were also performed to address whether the duration of the intervention or the mean age of participants could modify the effect of MedDiet-based interventions on the weight management indicators analyzed.
Reporting bias assessment
Small study effects and publication biases were examined using the Doi plot and the Luis Furuya-Kanamori (LFK) index [33]. No asymmetry, minor asymmetry, or major asymmetry were assigned values of 1, between 1 and 2, and 2, respectively [33].
Results
Study selection
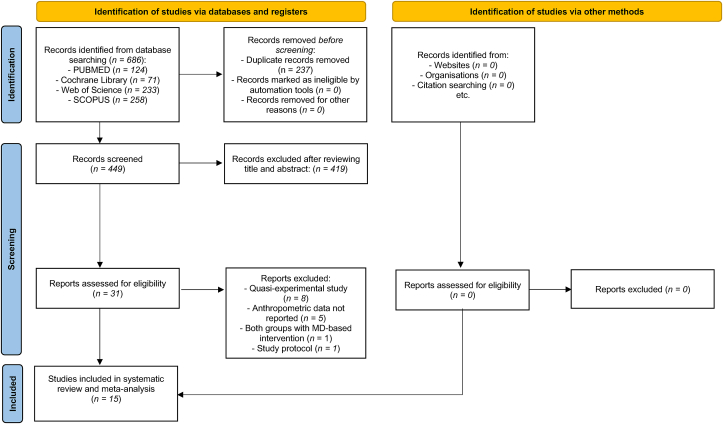
A total of 15 RCTs were included in the meta-analysis [31,[34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47]]. The PRISMA flow chart is shown in Figure 1. Excluded studies and reasons for exclusion are provided in Supplemental Table 2.
FIGURE 1.
PRISMA 2020 flow chart for systematic reviews that included database searches. MedDiet, Mediterranean diet.
Study characteristics
Table 1 includes a summary of the 15 RCTs included in this study. All children and adolescents were recruited from educational centers (schools, high schools) or hospitals. The RCTs included a total of 7184 participants (intervention groups: n = 3356) aged between 3 [35,[38], [39], [40]] and 18 [39,44,47] y. Fourteen studies included participants of both sexes, with the exception of one study that included only girls. The duration of the MedDiet-based interventions was ≥8 wk. A summary of the type of actions carried out in both the intervention and control groups can be found in Supplemental Table 3. Similarly, detailed information about the RCTs is presented in Supplemental Table 4.
TABLE 1.
A summary of the characteristics of the included studies (n = 15)
| Authors | Country | Age group | Sample | Weight status (baseline) | Duration (wk) | Intervention (type) | Indicators examined |
|---|---|---|---|---|---|---|---|
| Lisón et al. [31] | Spain | 6–16 | n = 110 | Excess weight § | 36 | The prescribed diet and physical exercise | BMI, WC, WHtR, %OB, %AO |
| IG a = 45 | |||||||
| IG b = 41 | |||||||
| CG = 24 | |||||||
| Velázquez-López et al. [39] | Mexico | 3–18 | n = 49 | Excess weight § | 16 | The prescribed diet | BMI, WC, WHtR, %OB, %AO |
| IG = 24 | |||||||
| CG = 25 | |||||||
| Muros et al. [45] | Spain | 10–11 | n = 135 | All group † | 24 | Nutritional education | BMI, WC, %OB |
| IG c = 21 | |||||||
| CG = 41 | |||||||
| Peñalvo et al. [40] | Spain | 3–5 | n = 1779 | All group † | 52–156 | Nutritional education and physical activity | BMI, WC, WHtR, %OB, %AO |
| IG = 948 | |||||||
| CG = 831 | |||||||
| Akdemir et al. [34] | Turkey | 6–14 | n = 1288 | All group † | 32 | Nutritional education | BMI, %OB |
| IG = 647 | |||||||
| CG = 641 | |||||||
| Bibiloni et al. [35] | Spain | 3–7 | n = 1119 | All group † | 48 | Nutritional education | BMI, WHtR, %OB, %AO |
| IG = 319 | |||||||
| CG = 880 | |||||||
| Gómez et al. [37] | Spain | 8–10 | n = 2086 | All group † | 60 | Nutritional education and physical activity | BMI, WC, WHtR, %OB, %AO |
| IG = 974 | |||||||
| CG = 1112 | |||||||
| Ojeda-Rodríguez et al. [41] | Spain | 7–16 | n = 107 | Excess weight § | 8 | The prescribed diet and physical activity | BMI, WC, WHtR, %OB, %AO |
| IG = 81 | |||||||
| CG = 26 | |||||||
| Akbulut et al. [43] | Turkey | 9–17 | n = 45 | Excess weight § | 12 | The prescribed diet and physical exercise | BMI |
| IG = 23 | |||||||
| CG = 22 | |||||||
| Fernández-Ruiz et al. [36] | Spain | 6–12 | n = 101 | Excess weight § | 40 | Nutritional education and physical exercise | BMI, WC, WHtR, %OB, %AO |
| IG = 51 | |||||||
| CG = 50 | |||||||
| Prieto-Zambrano et al. [42] | Spain | 11–15 | n = 82 | All group † | 20 | Nutritional education | BMI, WC, WHtR, %OB, %AO |
| IG = 46 | |||||||
| CG = 36 | |||||||
| Yurtdaş et al. [47] | Turkey | 11–18 | n = 44 | Excess weight § | 12 | The prescribed diet | BMI, WC, WHtR |
| IG = 22 | |||||||
| CG = 22 | |||||||
| Blancas-Sánchez et al. [46] | Spain | 9–15 | n = 29 | All group † | 20 | Nutritional education | BMI, WC, WHtR, %OB, %AO |
| IG = 14 | |||||||
| CG = 15 | |||||||
| Martíncrespo-Blanco et al. [38] | Spain | 3–5 | n = 133 | All group † | 36 | Nutritional education | BMI, %OB |
| IG = 65 | |||||||
| CG = 68 | |||||||
| Asoudeh et al. [44] | Iran | 13–18 | n = 70 | Excess weight § | 12 | The prescribed diet | BMI, WC, WHtR |
| IG = 35 | |||||||
| CG = 35 |
AO, abdominal obesity; BMI, body mass index; CG, control group; IG, intervention group; OB, obesity; WC, waist circumference; WHtR, waist-to-height ratio.
Intervention carried out in hospital.
Intervention carried out at home.
Group that only received nutritional education.
Participants with any weight status (thinness, normal weight, overweight, or obesity).
Participants with excess weight (overweight or obesity).
Risk of bias in studies
Fifteen RCTs were evaluated according to the RoB 2.0 tool [28], of which 6 were rated as “low risk” of bias [36,38,40,43,46,47], 8 as “some concerns” of bias [31,34,35,39,41,42,44,45], and one as “high risk” [37] (Supplemental Figure 1).
Summary of the results
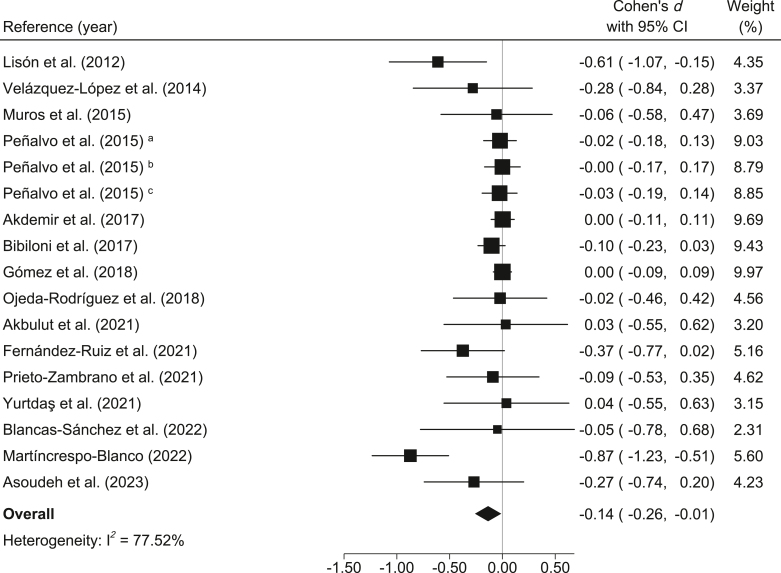
BMI: Compared to the control group, the MedDiet-based interventions showed small and significant reductions in BMI (d = −0.14; 95% CI: −0.26, −0.01; I2 = 77.52%) (Figure 2). Furthermore, the reduction in absolute BMI was −0.35 kg/m2 (95% CI: −0.59, −0.04; I2 = 75.00%).
FIGURE 2.
Meta-analysis of Mediterranean diet-based interventions to determine the combined effect size on BMI. a3-y age group; b4-y age group; c5-y age group.
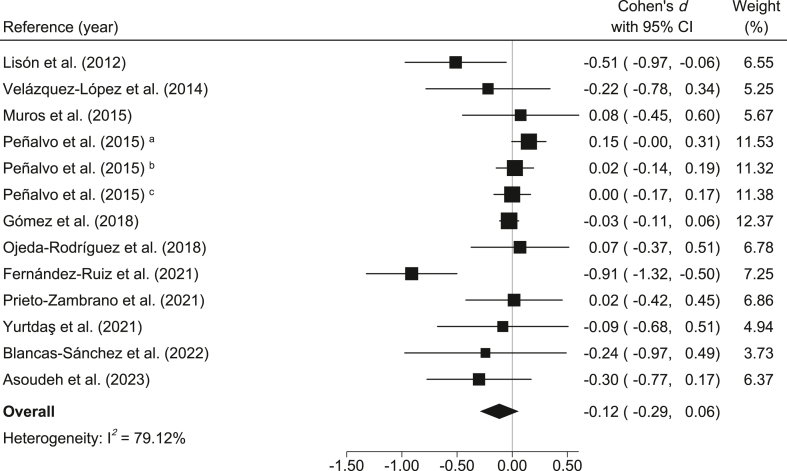
WC: When comparing the control groups with the MedDiet-based intervention groups, small and nonsignificant decreases in WC were found (d = −0.12; 95% CI: −0.29, 0.06; I2 = 79.12%) (Figure 3). In addition, the reduction in absolute WC was −0.56 cm (95% CI: −1.41, 0.29; I2 = 76.68%).
FIGURE 3.
Meta-analysis of Mediterranean diet-based interventions to determine the combined effect size on the waist circumference. a3-y age group; b4-y age group; c5-y age group.
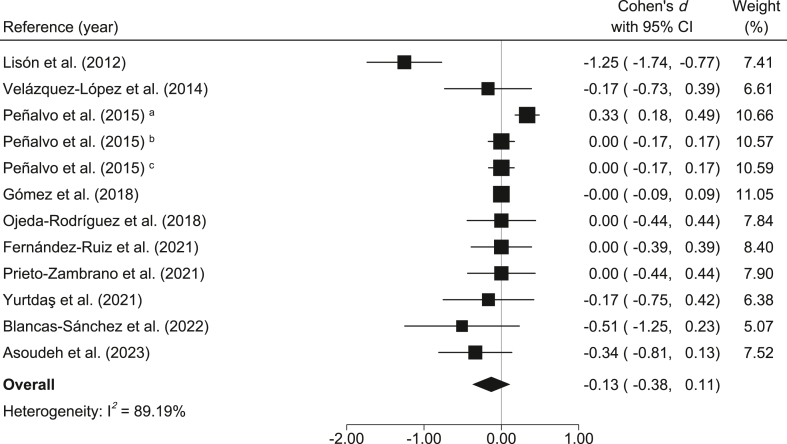
WHtR: Compared to the control group, the MedDiet-based interventions showed small and nonsignificant reductions in WHtR (d = −0.13; 95% CI: −0.38, 0.11; I2 = 89.19%) (Figure 4). Moreover, the reduction in absolute WHtR was −0.001 (95% CI: −0.006, 0.004; I2 = 86.43%).
FIGURE 4.
Meta-analysis of Mediterranean diet-based interventions to determine the combined effect size on waist-to-height ratio. a3-y age group; b4-y age group; c5-y age group.
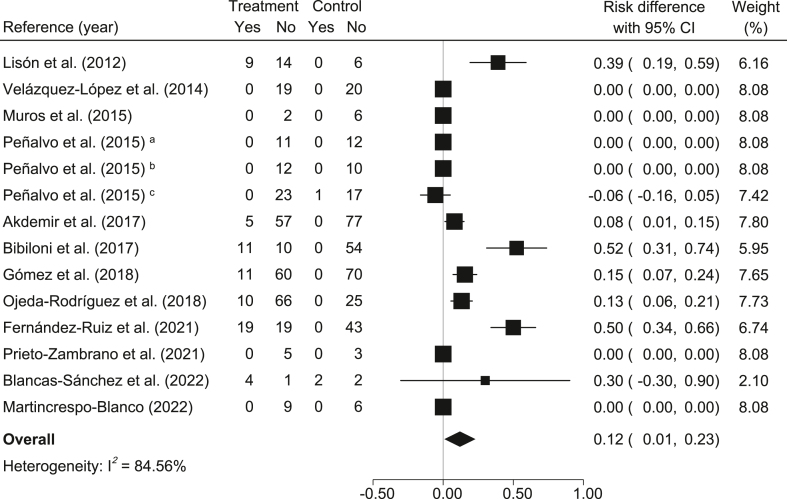
The percentage of obesity: In relation to the control group, participants in the MedDiet-based interventions had a significant reduction in the percentage of obesity (risk difference = 0.12; 95% CI: 0.01, 0.23; I2 = 84.56%) (Figure 5). Furthermore, the NNT for one participant to benefit was ∼7 (100% / 12% ≃ 6.67).
FIGURE 5.
Meta-analysis of Mediterranean diet-based interventions to determine the combined effect size on the relative risk difference for obesity percentage. a3-y age group; b4-y age group; c5-y age group.
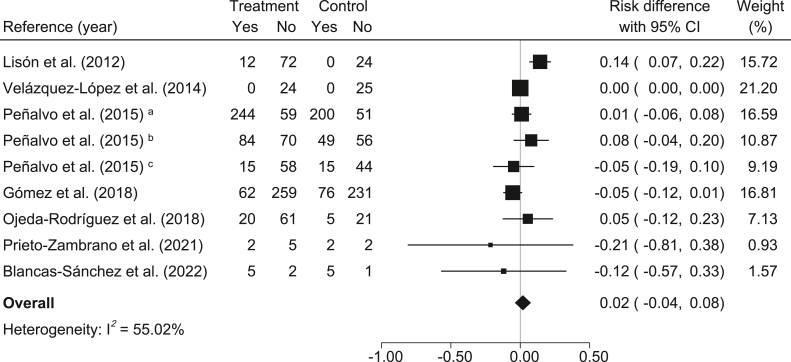
The percentage of abdominal obesity: In relation to the control group, participants in the MedDiet-based interventions had a nonsignificant reduction in the percentage of abdominal obesity (risk difference = 0.02; 95% CI: −0.04, 0.08; I2 = 55.02%) (Figure 6). In addition, the NNT for one participant to benefit was 50 (100% / 2% = 50).
FIGURE 6.
Meta-analysis of Mediterranean diet-based interventions to determine the combined effect size on the relative risk difference for abdominal obesity percentage. a3-y age group; b4-y age group; c5-y age group.
Sensitivity analysis, subgroup analysis, and meta-regression
After removing the studies from the analyses individually by sensitivity analysis, none of the RCTs substantially changed the estimate of effects (BMI, percentage of obesity) in the intervention group versus the control group (p < 0.10 for all cases) (Supplemental Figures 2–6).
In relation to subgroup analyses, the effects of the interventions were verified according to the regions where the interventions were conducted (Mediterranean or nonMediterranean) or the weight status of the participants (all weight statuses or only participants with overweight/obesity) (Table 2). A further subgroup analysis according to the type of intervention (that is, prescribed diet, nutritional education, or prescribed diet or nutritional education and physical activity or exercise) is shown in Supplemental Table 5. Concerning the type of country where the intervention was conducted, significant reductions were found in interventions performed in Mediterranean countries (that is, Spain and Turkey) for BMI (risk difference = 0.13; 95% CI: 0.01, 0.25; I2 = 86.15%) but were not significant for interventions performed in a nonMediterranean country (that is, Mexico). In addition, subgroup analysis by weight status showed that the interventions had greater effects when aiming at participants with excess weight for BMI, WC, WHtR, percentage of obesity, and percentage of abdominal obesity. However, statistically significant differences were only found for WC (p = 0.030). The NNT for one participant to reduce obesity was ∼4 (100% / 24% ≃ 4.17).
TABLE 2.
Subgroup analyses according to the type of country or baseline weight status
| Variables | # | d | LLCI | ULCI | I2 | p |
|---|---|---|---|---|---|---|
| Country | ||||||
| BMI | ||||||
| MedDiet countries | 13 | −0.13 | −0.27 | 0.01 | 81.54 | 0.45 |
| Non-MedDiet countries | 2 | −0.27 | −0.34 | −0.20 | 0.00 | |
| WC | ||||||
| MedDiet countries | 9 | −0.10 | −0.31 | 0.11 | 83.94 | 0.43 |
| Non-MedDiet countries | 2 | −0.27 | −0.78 | 0.24 | 0.11 | |
| WHtR | ||||||
| MedDiet countries | 9 | −0.12 | −0.42 | 0.18 | 92.25 | 0.51 |
| Non-MedDiet countries | 2 | −0.27 | −1.30 | 0.76 | 1.68 | |
| % Obesity | ||||||
| MedDiet countries | 11 | 0.13 | 0.01 | 0.25 | 86.15 | 1.00 |
| Non-MedDiet country | 1 | 0.00 | 0.00 | 0.00 | — | |
| % Abdominal obesity | ||||||
| MedDiet countries | 6 | 0.02 | −0.05 | 0.10 | 62.21 | 1.00 |
| Non-MedDiet country | 1 | 0.00 | 0.00 | 0.00 | — | |
| Weight status (baseline) | ||||||
| BMI | ||||||
| All group † | 8 | −0.11 | −0.29 | 0.06 | 87.52 | 0.48 |
| Excess weight § | 7 | −0.22 | −0.45 | 0.02 | 28.64 | |
| WC | ||||||
| All group † | 5 | 0.02 | −0.07 | 0.11 | 42.25 | 0.03 |
| Excess weight § | 6 | −0.34 | −0.74 | 0.05 | 54.62 | |
| WHtR | ||||||
| All group † | 4 | 0.04 | −0.16 | 0.24 | 77.88 | 0.08 |
| Excess weight § | 6 | −0.34 | −0.86 | 0.18 | 72.31 | |
| % Obesity | ||||||
| All group † | 8 | 0.06 | −0.06 | 0.18 | 77.90 | 0.10 |
| Excess weight § | 4 | 0.24 | −0.03 | 0.51 | 78.60 | |
| % Abdominal obesity | ||||||
| All group † | 4 | −0.01 | −0.09 | 0.07 | 53.21 | 0.28 |
| Excess weight § | 3 | 0.05 | −0.08 | 0.19 | 27.19 | |
BMI, body mass index; MedDiet, Mediterranean diet; LLCI, lower limit confidence interval; ULCI, upper limit confidence interval; WC, waist circumference; WHtR, waist-to-height ratio. #, number of studies examined.
Participants with any weight status (thinness, normal weight, overweight, or obesity).
Participants with excess weight (overweight or obesity).
Random-effects meta-regression models are shown in Table 3. Both intervention duration and age mean were not statistically significant in terms of effect sizes (BMI, WC, WHtR, percentage of obesity, and percentage of abdominal obesity) (Table 3).
TABLE 3.
Meta-regression analyses by intervention duration and mean age
| Variables | B | SE | LLCI | ULCI | p |
|---|---|---|---|---|---|
| BMI | |||||
| Duration (wk) | 0.001 | 0.001 | −0.002 | 0.004 | 0.388 |
| Mean age (y) | 0.004 | 0.017 | −0.033 | 0.041 | 0.833 |
| WC | |||||
| Duration (wk) | 0.002 | 0.002 | −0.001 | 0.006 | 0.203 |
| Mean age (y) | −0.026 | 0.022 | −0.075 | 0.023 | 0.270 |
| WHtR | |||||
| Duration (wk) | 0.004 | 0.002 | −0.001 | 0.009 | 0.123 |
| Mean age (y) | −0.048 | 0.029 | −0.112 | 0.016 | 0.128 |
| % Obesity | |||||
| Duration (wk) | −0.001 | 0.001 | −0.004 | 0.002 | 0.584 |
| Mean age (y) | 0.006 | 0.017 | −0.031 | 0.042 | 0.732 |
| % Abdominal obesity | |||||
| Duration (wk) | −0.001 | 0.001 | −0.001 | 0.001 | 0.972 |
| Mean age (y) | −0.001 | 0.008 | −0.019 | 0.019 | 0.975 |
LLCI, lower limit confidence interval; SE, standard error; ULCI, upper limit confidence interval; WC, waist circumference; WHtR, waist-to-height ratio; B, unstandardized beta coefficient.
Reporting biases
A major asymmetry suggestive of small study effects was observed for BMI (LFK index = −3.36) (Supplemental Figure 7), WC (LFK index = −2.48) (Supplemental Figure 8), WHtR (LFK index = −2.13) (Supplemental Figure 9), percentage of obesity (LFK index = 3.47) (Supplemental Figure 10), and percentage of abdominal obesity (LFK index = −2.21) (Supplemental Figure 11).
Discussion
To our knowledge, this is the first systematic review with meta-analysis that separately synthesized the effects of MedDiet-based interventions in children and adolescents in relation to the effects on anthropometric measures. Overall, we found that MedDiet-based interventions (15 RCTs with a minimum duration of 8 wk) decreased BMI and the percentage of obesity. Our analyses indicate that for every 7 young people treated with MedDiet-based interventions, one would no longer have obesity. Additionally, such interventions had greater effects in reducing obesity when conducted in Mediterranean countries (that is, Spain and Turkey) and when they included only young people with excess weight. Because heterogeneity for most outcomes was substantial to considerable, the results should be interpreted with caution. There are certain factors that could explain this high heterogeneity. For example, the fact that the interventions included diet-based interventions, nutrition education, or a combination of diet plus physical activity or exercise could explain this inconsistency between studies. Likewise, having interventions in Mediterranean and nonMediterranean countries, the different age groups included (that is, preschoolers, children, adolescents), or performing the interventions only on young people or including parents/families could be other reasons justifying this aspect.
Previous systematic reviews have shown inconclusive results in relation to adherence to MedDiet and obesity-related markers among children/adolescents [25,48]. However, none of these reviews provided a meta-analysis of RCTs, which could explain the discrepancy. In this line, Iaccarino Idelson et al. [48] found mixed results on the association between MedDiet and anthropometric indicators or body composition in a previous systematic review of children and adolescents. In that review, only 10 of 26 papers reported that higher adherence to MedDiet was associated with lower BMI values or prevalence of excess weight. Furthermore, these authors pointed out that the results are even less consistent (due to the lack of studies) when analyzing the relationship between MedDiet and abdominal obesity (through WC) or level of adiposity. A possible explanation for this discrepancy may be due to the design of the studies analyzed in this systematic review since most of them were observational (that is, cross-sectional, longitudinal), in which it is not possible to infer cause-effect relationships. Conversely, Lassale et al. [25] concluded in a recent systematic review that, despite the large number of published studies, there is only limited evidence of the beneficial effect of following a traditional MedDiet in maintaining a healthy body weight in childhood. However, these same authors only conducted their systematic review using the MEDLINE database, excluding several studies that could have affected the results obtained.
There are several plausible mechanisms by which following an MedDiet can help maintain a healthy body weight and prevent obesity early in life. First, one of the basic tenets of MedDiet is the intake of plant-based foods, such as fruits and vegetables, which are characterized by high volumes with low energy density. Thus, high-volume foods may require more time to be ingested than low-volume foods, and prolonging the duration of the meal may increase satiety and reduce energy intake [49]. In addition, some essential components of the MedDiet (that is, fruits, vegetables, whole grains, nuts, or seeds), which are high fiber-rich, nutrient-dense, energy-poor foods [50], as well as family meals [51] (characteristic of the MedDiet), may promote consuming fewer calories. Moreover, specific compounds such as olive oil phenolic compounds, omega-3 polyunsaturated fatty acids, vitamins, trace elements, and polyphenols are found in abundance in a traditional MedDiet [17]. They have been shown to modulate and maintain healthy gut microbiota, as well as improve gut barrier integrity, which has been shown to be altered in the presence of obesity and metabolic syndrome [52].
On the other hand, the intake of ultra-processed foods (away from the basic principles of MedDiet) has been associated with an increased dietary risk of associated noncommunicable diseases (for example, excess weight), as they are high in calories and low in nutrients, and may contribute to a higher caloric intake [53]. Likewise, a dietary pattern characterized by a diet based on energy-dense, low-fiber ultra-processed foods at the age of 3 y is associated with excess weight and elevated BMI later in childhood [54]. In addition, a diet high in ultra-processed foods (for example, snacks, cookies), which are usually rich in added sugars, salt, or saturated fats, is consumed significantly faster than an unprocessed diet (for example, fruits, vegetables), which may contribute to higher caloric intake [55].
Concerning subgroup analysis according to the type of country where the intervention was conducted, we found that the interventions had greater effects in reducing obesity when conducted in Mediterranean countries (that is, Spain, Turkey), than they were when conducted in a nonMediterranean country (that is, Mexico). However, these results should be interpreted with some caution when ruling out this type of intervention in nonMediterranean countries. First, with respect to nonMediterranean countries, only a single study examining the reduction of obesity with complete data was included [39]. Further studies are required to verify whether MedDiet-based interventions work in nonMediterranean countries. Notwithstanding, some MedDiet-based interventions performed in nonMediterranean countries have shown beneficial effects on health outcomes [56,57]. Second, we observed a quantitative interaction since the size of the effect for nonMediterranean country interventions varied but not the direction [58]. Third, despite the traditional definition of MedDiet as the typical dietary habit of individuals living in countries surrounding the Mediterranean Sea, other Mediterranean-type ecosystems can be located from the 30th parallel to the 45th parallel of the south or north latitude with their coasts facing west (for example, central Chile). In addition, agriculture produced at some of these latitudes offers food similar to that of Mediterranean countries [59] due to their latitude, climate, biodiversity, and agriculture being similar to the Mediterranean-type ecosystem.
In relation to the baseline weight status of the participants, interventions had higher effects when the targets were young participants with excess weight than when they included all weight statuses (that is, underweight, normal weight, overweight, or obesity). This result could be a clinically relevant finding since it seems to suggest that MedDiet-based interventions could be a useful strategy for the treatment of obesity in the young population. A possible explanation for this discrepancy could lie in the fact that by including young people with normal weight and possibly increasing the number of participants, the interventions may have lower effects. Furthermore, the relationship between anthropometric or obesity-related markers and health is not linear [1]. Decreases in BMI for young people with normal weight could change their weight status toward underweight, which would not lead to health benefits. Another possible reason is that young people with excess weight have higher baseline BMI levels and, therefore, a greater margin of benefit from interventions. In addition, caution is necessary when interpreting the results of studies that included participants with all weight statuses. It is possible that by segmenting the results according to weight status, the results would have reported greater effects in the young population with excess weight.
The interpretation of these results should be viewed with caution as they have some limitations. First, the main limitation of this review is the low quality of the included studies. Second, only a few RCTs considered important confounding factors such as physical activity, sedentary behavior, or sleep duration. Third, not all interventions were exclusively based on MedDiet content. Some of them also incorporated physical activity promotion or physical exercise (among other components), which could have overestimated the pooled effects obtained. However, given that some groups included physical activity or exercise in the control and intervention groups, our results seem to suggest that MedDiet could offer additional benefits to the effect of physical activity or exercise on anthropometric and obesity markers in this population. Fourth, not all RCTs reported compliance with intervention sessions (for example, number of sessions attended), and it is essential to know whether participants acted as planned and adhered to the planned program. Fifth, not all RCTs reported on prior knowledge/adherence to the MedDiet. Sixth, the use of BMI z score could be more appropriate as an anthropometric indicator than crude BMI. However, we were unable to perform an analysis of the BMI z score due to the low number of studies that reported it and the use of different criteria (that is, WHO, International Obesity Task Force). Nonetheless, the percentage of obesity in all studies was adjusted for age and sex, and significant effects of the MedDiet on reducing obesity were also observed. Finally, publication bias may have affected the results of this review, as the Doi plot and LFK index showed larger asymmetries for all the indicators examined.
To conclude, MedDiet-based interventions have a significant effect on reducing BMI as well as reducing the risk of obesity (percentage of obesity) in children and adolescents (aged 3–18 y). The findings suggest that interventions conducted in young people with excess weight could have greater effects in improving these parameters. Furthermore, as no episodes of serious adverse effects were reported during the interventions in any of the RCTs included in the present meta-analysis, these results suggest that MedDiet-based interventions in the trial setting can be safely conducted in children and adolescents. This finding could be clinically relevant since it highlights the efficacy of MedDiet-based interventions as a useful tool in the interest of reversing the high prevalence of obesity.
Acknowledgments
JFL-G is a Margarita Salas Fellow (Universidad Pública de Navarra–1225/2022). AG-H is a Miguel Servet Fellow (Instituto de Salud Carlos III–CP18/0150).
Author contributions
The authors’ responsibilities were as follows—JFL-G: designed the study; JFL-G, and AG-H: contributed to the interpretation and analysis of the data; JFL-G wrote the initial draft; AG-H, MS-P, IC-R, VM-V, and SK contributed to the revision of the manuscript; and all authors: read and approved the final manuscript.
Conflict of interest
The authors report no conflicts of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author disclosures
The authors report no conflicts of interest.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.advnut.2023.04.011.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . 2022. Report on the fifth round of data collection, 2018–2020: WHO European Childhood Obesity Surveillance Initiative (COSI)https://apps.who.int/iris/rest/bitstreams/1476879/retrieve Geneva, Switzerland. [Internet] Available from: [Google Scholar]
- 3.Kumar S., Kelly A.S. Review of childhood obesity: from epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clin. Proc. 2017;92:251–265. doi: 10.1016/j.mayocp.2016.09.017. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . World Health Organization; Geneva: 2016. Report of the commission on ending childhood obesity.https://apps.who.int/iris/handle/10665/204176 [Internet] Available from: [Google Scholar]
- 5.Torres-Carot V., Suárez-González A., Lobato-Foulques C. The energy balance hypothesis of obesity: do the laws of thermodynamics explain excessive adiposity? Eur. J. Clin. Nutr. 2022;76:1374–1379. doi: 10.1038/s41430-021-01064-4. [DOI] [PubMed] [Google Scholar]
- 6.Blüher M. Obesity: global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019;15:288–298. doi: 10.1038/s41574-019-0176-8. [DOI] [PubMed] [Google Scholar]
- 7.Gao W., Liu J.-L., Lu X., Yang Q. Epigenetic regulation of energy metabolism in obesity. J. Mol. Cell Biol. 2021;13:480–499. doi: 10.1093/jmcb/mjab043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nicolaidis S. Environment and obesity. Metabolism. 2019;100 doi: 10.1016/j.metabol.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 9.Pigeyre M., Yazdi F.T., Kaur Y., Meyre D. Recent progress in genetics, epigenetics, and metagenomics unveils the pathophysiology of human obesity. Clin. Sci. 2016;130:943–986. doi: 10.1042/CS20160136. [DOI] [PubMed] [Google Scholar]
- 10.Reinehr T., Hinney A., de Sousa G., Austrup F., Hebebrand J., Andler W. Definable somatic disorders in overweight children and adolescents. J. Pediatr. 2007;150:618–622. doi: 10.1016/j.jpeds.2007.01.042. [DOI] [PubMed] [Google Scholar]
- 11.Speiser P.W., Rudolf M.C.J., Anhalt H., Camacho-Hubner C., Chiarelli F., Eliakim A., et al. Childhood obesity. J. Clin. Endocrinol. Metab. 2005;90:1871–1887. doi: 10.1210/jc.2004-1389. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization . 2021. Obesity and overweight.https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight Geneva, Switzerland. [Internet] Available from: [Google Scholar]
- 13.Arouca A., Moreno L.A., Gonzalez-Gil E.M., Marcos A., Widhalm K., Molnár D., et al. Diet as moderator in the association of adiposity with inflammatory biomarkers among adolescents in the HELENA study. Eur. J. Nutr. 2019;58:1947–1960. doi: 10.1007/s00394-018-1749-3. [DOI] [PubMed] [Google Scholar]
- 14.López-Gil J.F., Cavero-Redondo I., Jiménez-López E., Bizzozero-Peroni B., Saz-Lara A., Mesas A.E. Role of diet quality in the association between excess weight and psychosocial problems in a large sample of children in Spain. JAMA Netw. Open. 2022;5 doi: 10.1001/jamanetworkopen.2022.9574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.García-Hermoso A., Ezzatvar Y., Alonso-Martinez A.M., Ramírez-Vélez R., Izquierdo M., López-Gil J.F. Twenty-four-hour movement guidelines during adolescence and its association with obesity at adulthood: results from a nationally representative study. Eur. J. Pediatr. 2023;182:1009–1017. doi: 10.1007/s00431-022-04760-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Serra-Majem L., Ribas L., Ngo J., Ortega R.M., García A., Pérez-Rodrigo C., et al. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean diet quality index in children and adolescents. Public Health Nutr. 2004;7:931–935. doi: 10.1079/phn2004556. [DOI] [PubMed] [Google Scholar]
- 17.Willett W.C. The Mediterranean diet: science and practice. Public Health Nutr. 2006;9:105–110. doi: 10.1079/phn2005931. [DOI] [PubMed] [Google Scholar]
- 18.Radd-Vagenas S., Kouris-Blazos A., Singh M.F., Flood V.M. Evolution of Mediterranean diets and cuisine: concepts and definitions, Asia Pac. J. Clin. Nutr. 2017;26:749–763. doi: 10.6133/apjcn.082016.06. [DOI] [PubMed] [Google Scholar]
- 19.Martínez-Lacoba R., Pardo-Garcia I., Amo-Saus E., Escribano-Sotos F. Mediterranean diet and health outcomes: a systematic meta-review. Eur. J. Public Health. 2018;28:955–961. doi: 10.1093/eurpub/cky113. [DOI] [PubMed] [Google Scholar]
- 20.Eleftheriou D., Benetou V., Trichopoulou A., La Vecchia C., Bamia C. Mediterranean diet and its components in relation to all-cause mortality: meta-analysis. Br. J. Nutr. 2018;120:1081–1097. doi: 10.1017/S0007114518002593. [DOI] [PubMed] [Google Scholar]
- 21.Bawaked R.A., Schröder H., Ribas-Barba L., Izquierdo-Pulido M., Pérez-Rodrigo C., Fíto M., et al. Association of diet quality with dietary inflammatory potential in youth. Food Nutr. Res. 2017;61 doi: 10.1080/16546628.2017.1328961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.García-Hermoso A., Ezzatvar Y., López-Gil J.F., Ramírez-Vélez R., Olloquequi J., Izquierdo M. Is adherence to the Mediterranean diet associated with healthy habits and physical fitness? A systematic review and meta-analysis including 565 421 youths. Br. J. Nutr. 2022;128:1433–1444. doi: 10.1017/S0007114520004894. [DOI] [PubMed] [Google Scholar]
- 23.Romero-Robles M.A., Ccami-Bernal F., Ortiz-Benique Z.N., Pinto-Ruiz D.F., Benites-Zapata V.A., Casas Patiño D. Adherence to Mediterranean diet associated with health-related quality of life in children and adolescents: a systematic review. BMC Nutr. 2022;8:57. doi: 10.1186/s40795-022-00549-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cabrera S.G., Herrera Fernández N., Rodríguez Hernández C., Nissensohn M., Román-Viñas B., Serra-Majem L. KIDMED test; prevalence of low adherence to the Mediterranean diet in children and young; a systematic review. Nutr. Hosp. 2015;32:2390–2399. doi: 10.3305/nh.2015.32.6.9828. [DOI] [PubMed] [Google Scholar]
- 25.Lassale C., Fitó M., Morales-Suárez-Varela M., Moya A., Gómez S.F., Schröder H. Mediterranean diet and adiposity in children and adolescents: a systematic review. Obes. Rev. 2022;23 doi: 10.1111/obr.13381. [DOI] [PubMed] [Google Scholar]
- 26.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Higgins J.P.T. 2nd ed. Wiley-Blackwell; Hoboken, NJ: 2020. Cochrane Collaboration, Cochrane Handbook for Systematic Reviews of Interventions. [Google Scholar]
- 28.Sterne J.A.C., Savović J., Page M.J., Elbers R.G., Blencowe N.S., Boutron I., et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 29.Cohen J. Routledge; 2013. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- 30.IntHout J., Ioannidis J.P., Borm G.F. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med. Res. Methodol. 2014;14:25. doi: 10.1186/1471-2288-14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lisón J.F., Real-Montes J.M., Torró I., Arguisuelas M.D., Álvarez-Pitti J., Martínez-Gramage J., et al. Exercise intervention in childhood obesity: a randomized controlled trial comparing hospital-versus home-based groups. Acad. Pediatr. 2012;12:319–325. doi: 10.1016/j.acap.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 32.Higgins J.P.T., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Statist. Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 33.Furuya-Kanamori L., Barendregt J.J., Doi S.A.R. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int. J. Evid. Based Healthc. 2018;16:195–203. doi: 10.1097/XEB.0000000000000141. [DOI] [PubMed] [Google Scholar]
- 34.Akdemir M., Donmez L., Polat H. The effect of nutritional and physical activity interventions on nutritional status and obesity in primary school children: a cluster randomized controlled study. Kuwait Med. J. 2018;49:105–113. [Google Scholar]
- 35.Bibiloni del Mar M., Fernández-Blanco J., Pujol-Plana N., Martín-Galindo N., Fernández-Vallejo M.M., Roca-Domingo M., et al. Improving diet quality in children through a new nutritional education programme: INFADIMED. Gac. Sanit. 2017;31:472–477. doi: 10.1016/j.gaceta.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 36.Fernández-Ruiz V.E., Solé-Agustí M., Armero-Barranco D., Cauli O. Weight loss and improvement of metabolic alterations in overweight and obese children through the I2AO2 family program: a randomized controlled clinical trial. Biol. Res. Nurs. 2021;23:488–503. doi: 10.1177/1099800420987303. [DOI] [PubMed] [Google Scholar]
- 37.Gómez S.F., Casas Esteve R., Subirana I., Serra-Majem L., Fletas Torrent M., Homs C., et al. Effect of a community-based childhood obesity intervention program on changes in anthropometric variables, incidence of obesity, and lifestyle choices in Spanish children aged 8 to 10 years. Eur. J. Pediatr. 2018;177:1531–1539. doi: 10.1007/s00431-018-3207-x. [DOI] [PubMed] [Google Scholar]
- 38.Martíncrespo-Blanco M.C., Varillas-Delgado D., Blanco-Abril S., Cid-Exposito M.G., Robledo-Martín J. Effectiveness of an intervention programme on adherence to the Mediterranean diet in a preschool child: a randomised controlled trial. Nutrients. 2022;14:1536. doi: 10.3390/nu14081536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Velázquez-López L., Santiago-Díaz G., Nava-Hernández J., Muñoz-Torres A.V., Medina-Bravo P., Torres-Tamayo M. Mediterranean-style diet reduces metabolic syndrome components in obese children and adolescents with obesity. BMC Pediatr. 2014;14:175. doi: 10.1186/1471-2431-14-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peñalvo J.L., Santos-Beneit G., Sotos-Prieto M., Bodega P., Oliva B., Orrit X., et al. The SI! program for cardiovascular health promotion in early childhood: a cluster-randomized trial. J. Am. Coll. Cardiol. 2015;66:1525–1534. doi: 10.1016/j.jacc.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 41.Ojeda-Rodríguez A., Zazpe I., Morell-Azanza L., Chueca M., Azcona-Sanjulian M., Marti A. Improved diet quality and nutrient adequacy in children and adolescents with abdominal obesity after a lifestyle intervention. Nutrients. 2018;10:1500. doi: 10.3390/nu10101500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Prieto-Zambrano P., Pache-Iglesias L., Domínguez-Martín A.T., Panea-Pizarro I., Gómez-Luque A., López-Espuela F. Impacto de una intervención educacional sobre la calidad de la dieta mediterránea, la actividad física y el estado ponderal en adolescentes: ensayo clínico aleatorizado. Enferm. Clín. 2021;31:51–56. doi: 10.1016/j.enfcli.2020.03.003. [DOI] [PubMed] [Google Scholar]
- 43.Akbulut U.E., Isik I.A., Atalay A., Eraslan A., Durmus E., Turkmen S., et al. The effect of a Mediterranean diet vs. a low-fat diet on non-alcoholic fatty liver disease in children: a randomized trial. Int. J. Food Sci. Nutr. 2022;73:357–366. doi: 10.1080/09637486.2021.1979478. [DOI] [PubMed] [Google Scholar]
- 44.Asoudeh F., Fallah M., Djafarian K., Shirzad N., Clark C.C.T., Esmaillzadeh A. The effect of Mediterranean diet on inflammatory biomarkers and components of metabolic syndrome in adolescent girls. J. Endocrinol. Invest. 2023 doi: 10.1007/s40618-023-02027-1. [DOI] [PubMed] [Google Scholar]
- 45.Muros J.J., Zabala M., Oliveras-López M.J., Bouzas P.R., Knox E., Rufián-Henares J.Á., et al. Effect of physical activity, nutritional education, and consumption of extra virgin olive oil on lipid, physiological, and anthropometric profiles in a pediatric population. J. Phys. Act. Health. 2015;12:1245–1252. doi: 10.1123/jpah.2014-0236. [DOI] [PubMed] [Google Scholar]
- 46.Blancas-Sánchez I.M., Del Rosal Jurado M., Aparicio-Martínez P., Quintana Navarro G., Vaquero-Abellan M., Castro Jiménez R.A., et al. A Mediterranean-diet-based nutritional intervention for children with prediabetes in a rural town: a pilot randomized controlled trial. Nutrients. 2022;14:3614. doi: 10.3390/nu14173614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yurtdaş G., Akbulut G., Baran M., Yılmaz C. The effects of Mediterranean diet on hepatic steatosis, oxidative stress, and inflammation in adolescents with non-alcoholic fatty liver disease: a randomized controlled trial. Pediatr. Obes. 2022;17 doi: 10.1111/ijpo.12872. [DOI] [PubMed] [Google Scholar]
- 48.Iaccarino Idelson P., Scalfi L., Valerio G. Adherence to the Mediterranean diet in children and adolescents: a systematic review. Nutr. Metab. Cardiovasc. Dis. 2017;27:283–299. doi: 10.1016/j.numecd.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 49.de Graaf C. Texture and satiation: the role of oro-sensory exposure time. Physiol. Behav. 2012;107:496–501. doi: 10.1016/j.physbeh.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 50.Planes-Muñoz D., Frontela-Saseta C., Ros-Berruezo G., López-Nicolás R. Effect of gazpacho, hummus and ajoblanco on satiety and appetite in adult humans: a randomised crossover study. Foods. 2021;10:606. doi: 10.3390/foods10030606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.de la Torre-Moral A., Fàbregues S., Bach-Faig A., Fornieles-Deu A., Medina F.X., Aguilar-Martínez A., et al. Family meals, conviviality, and the Mediterranean diet among families with adolescents. Int. J. Res. Public Helth. 2021;18:2499. doi: 10.3390/ijerph18052499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.García-Montero C., Fraile-Martínez O., Gómez-Lahoz A.M., Pekarek L., Castellanos A.J., Noguerales-Fraguas F., et al. Nutritional components in Western diet versus Mediterranean diet at the gut microbiota–immune system interplay. Implications for health and disease. Nutrients. 2021;13:699. doi: 10.3390/nu13020699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Monteiro C.A., Cannon G., Moubarac J.-C., Levy R.B., Louzada M.L.C., Jaime P.C. The UN decade of nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018;21:5–17. doi: 10.1017/S1368980017000234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sirkka O., Fleischmann M., Abrahamse-Berkeveld M., Halberstadt J., Olthof M.R., Seidell J.C., et al. Dietary patterns in early childhood and the risk of childhood overweight: the GECKO Drenthe birth cohort. Nutrients. 2021;13:2046. doi: 10.3390/nu13062046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hall K.D., Ayuketah A., Brychta R., Cai H., Cassimatis T., Chen K.Y., et al. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metab. 2019;30:226. doi: 10.1016/j.cmet.2019.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sotos-Prieto M., Ruiz-Canela M., Song Y., Christophi C., Mofatt S., Rodriguez-Artalejo F., et al. The effects of a Mediterranean diet intervention on targeted plasma metabolic biomarkers among US firefighters: a pilot cluster-randomized trial. Nutrients. 2020;12:3610. doi: 10.3390/nu12123610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Macknin M., Stegmeier N., Thomas A., Worley S., Li L., Hazen S.L., et al. Three healthy eating patterns and cardiovascular disease risk markers in 9 to 18 year olds with body mass index >95%: a randomized trial. Clin. Pediatr. (Phila) 2021;60:474–484. doi: 10.1177/00099228211044841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yusuf S., Wittes J., Probstfield J., Tyroler H.A. Analysis and interpretation of treatment effects in subgroups of patients in randomized clinical trials. JAMA. 1991;266:93–98. [PubMed] [Google Scholar]
- 59.Köppen V. Gebrüder Borntraeger; Berlin, Germany: 1936. Das geographische System der Klimate. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.