Abstract
Hyperglycemia is a key risk factor for death and disability worldwide. To better inform prevention strategies, we aimed to delineate and predict the temporal, spatial, and demographic patterns in mean fasting plasma glucose (FPG) levels and their related disease burden globally. Based on the Global Burden of Disease Study 2019, we estimated the distributions of mean FPG levels and high FPG-related disease burden by age, sex, year, socioeconomic status (SES), and geographical region from 1990 to 2050. We also investigated the possible associations of demographic, behavioral, dietary, metabolic, and environmental factors with FPG levels and high FPG-related disease burden. In 2019, the global mean FPG level was 5.40 mmol/L (95% uncertainty interval [UI]: 4.86–6.00), and high FPG contributed to 83.0 deaths (95% UI, 64.5–107.1) and 2,104.3 DALYs (95% UI: 1,740.7–2,520.7) per 100,000 people. For both historical (1990–2019) and future (2020–2050) periods, the mean FPG levels and the high FPG-related disease burden increased globally, with greater increases among the middle-aged and elderly, and people in low-to-middle SES countries, relative to their counterparts. Aging, unhealthy lifestyles, elevated body mass index, and lower air temperatures were potential risk factors for high FPG levels and the high FPG-related disease burden. This study demonstrates that high FPG continues to contribute to the global disease burden and is expected to do so for at least the next 30 years. Older people and those living in low-to-middle SES countries should receive more attention in glycemic management health interventions. In addition, effective interventions that target identified risk factors should be adopted to handle the increasingly large disease burden of high FPG.
Graphical abstract
Public summary
-
•
Mean fasting plasma glucose (FPG) levels increased globally from 1990 to 2019.
-
•
High FPG-related disease burden increased globally from 1990 to 2050.
-
•
FPG levels and their disease burden showed age and socioeconomic heterogeneities.
-
•
Aging, unhealthy lifestyles, elevated body mass index, and low temperatures are risk factors.
Introduction
Hyperglycemia is a key risk factor for both communicable diseases and non-communicable diseases, such as tuberculosis,1 diabetes mellitus (DM),2 cardiovascular disease,3 and cancers.4 A recent study predicted that the global economic burden of DM in adults will rise to > 2 trillion $US by 2030.5 Moreover, the coronavirus disease 2019 pandemic may have increased the risk of hyperglycemia and insulin resistance, further aggravating the global burden of hyperglycemia.6 Collectively, hyperglycemia has become a formidable challenge to human health and deserves more attention.
Several pieces of information are critical for addressing hyperglycemia. First, detailed information on the epidemiology and disease burden of hyperglycemia is needed to inform health policies, the allocation of healthcare resources, and decision-making on grant allocations. Second, predictions of the upcoming hyperglycemia-related disease burden are necessary for forward-looking policy designs. Third, identifying risk factors for hyperglycemia and its disease burden is critical for individuals, health professionals, and policymakers to develop targeted primary interventions. The World Health Organization (WHO) has recommended periodically collecting and analyzing data on the epidemiology and determinants of human diseases (including hyperglycemia) to decrease health inequalities.7
These necessary pieces of information to address hyperglycemia are limited. For instance, the most recent global estimates of glycemic levels does not extend beyond 2008.8 Contemporary glycemic levels may differ from past estimates, because of changed lifestyles, environmental exposures, and other factors. Also, available estimates of hyperglycemia-related disease burden are limited by their focus on a local rather than a global scale, or reporting only part of the disease burden attributable to hyperglycemia.9 In addition, previous efforts to predict the disease burden of hyperglycemia were largely limited to single countries or regions,10,11,12,13,14 and evidence on future global trends remains unknown.9,15 Finally, prior studies did not investigate potential risk factors for hyperglycemia and its disease burden on a global scale.
To overcome these evidence and knowledge gaps, we used data from the Global Burden of Disease (GBD) Study 2019 to delineate the spatial, temporal, and demographic patterns in glycemic levels (referring to fasting plasma glucose [FPG] in the GBD) and hyperglycemia (referring to high FPG in the GBD)-related disease burden, and also to predict the trends in the disease burden for the next 30 years. In addition, we employed Bayesian spatiotemporal models to explore potential risk factors for elevated FPG levels and high FPG-related disease burden. These analyses spanned nearly 60 years (1990–2050) and covered 204 countries (or territories).
Results
Global patterns and trends in mean FPG levels from 1990 to 2019
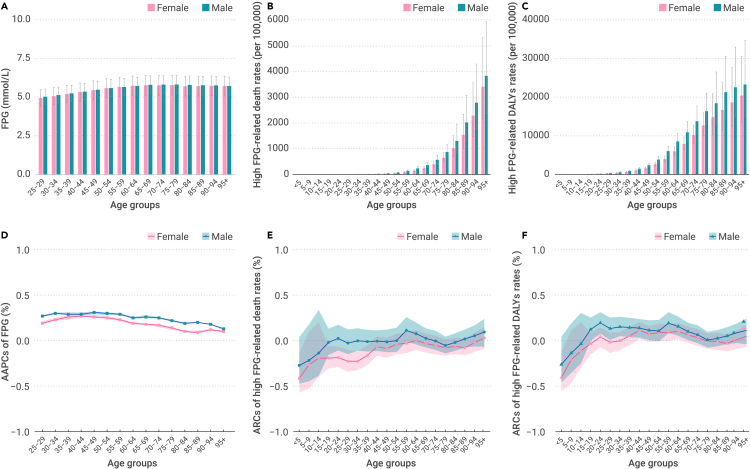
The global mean FPG level in 2019 among people ≥25 years was 5.40 mmol/L (95% uncertainty interval [UI], 4.86–6.00) (Table S1). The levels increased with age, peaked at 75–79 years, and then subsequently declined (Figure 1A). No significant differences in mean FPG levels were observed between males and females. From 1990 to 2019, the global mean FPG levels increased with an average annual percent change (AAPC) of 0.28% (95% confidence interval [CI], 0.27%–0.29%) (Table S2). Increasing trends over time were also observed in all age groups, with the fastest increase occurring in populations aged 45–49 years (Figure 1D). In addition, increasing trends over time were observed for both men and women, and AAPCs were greater among males than females.
Figure 1.
Global age- and sex-specific mean FPG levels and high FPG-related death and DALYs rates in 2019 along with their annual changes from 1990 to 2019
(A) Global mean FPG levels by age and sex in 2019.
(B) High FPG-related death rates globally in 2019, by age and sex.
(C) High FPG-related DALYs rates globally in 2019, by age and sex.
(D) Global annual changes of mean FPG levels from 1990 to 2019, by age and sex.
(E) Global annual changes of high FPG-related death rates from 1990 to 2019, by age and sex.
(F) Global annual changes of high FPG-related DALYs rates from 1990 to 2019, by age and sex. Error bars indicate the 95% UIs of mean FPG levels and high FPG-related death and DALYs rates in 2019. Shaded areas indicate the 95% CIs of AAPCs in mean FPG levels and ARCs in high FPG-related disease burden.
When dividing the countries (or territories) into four World Bank income levels, the highest and lowest mean FPG levels in 2019 were observed in upper- to middle-income countries (5.48 mmol/L [95% UI, 4.94–6.08]) and low-income countries (4.94 mmol/L [95% UI, 4.43–5.51]), respectively (Table S3). From 1990 to 2019, lower- to middle-income countries experienced the fastest increase in mean FPG levels (AAPC, 0.41% [95% CI, 0.39%–0.42%]), whereas low-income countries experienced the slowest increase (AAPC, 0.09% [95% CI, 0.07%–0.11%]) (Table S4). Stratified analyses by socio-demographic index (SDI) quintiles suggested that both mean FPG levels in 2019 and AAPCs in FPG levels from 1990 to 2019 were the lowest in the low SDI region (Tables S3 and S4). When stratifying by GBD super-regions, South Asia experienced the greatest increase in mean FPG levels from 1990 to 2019 (AAPC, 0.55% [95% CI, 0.51%–0.60%]) and had the highest mean FPG levels in 2019 (5.63 mmol/L [95% UI, 5.06–6.26]). In contrast, sub-Saharan Africa had the smallest change in mean FPG levels from 1990 to 2019 (AAPC, 0.11% [95% CI, 0.09%–0.13%]) and had the lowest mean FPG levels in 2019 (4.90 mmol/L [95% UI, 4.40–5.46]).
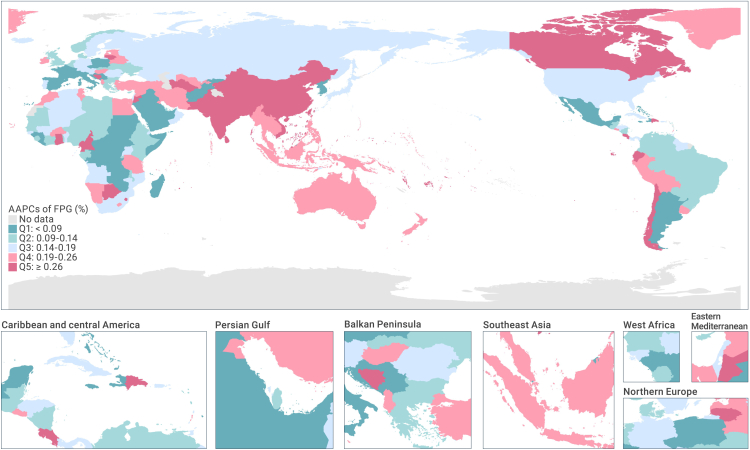
Across the 204 studied countries (or territories), the highest and lowest mean FPG levels in 2019 were observed in American Samoa (6.49 mmol/L [95% CI, 5.83–7.22]) and Malawi (4.31 mmol/L [95% CI, 3.87–4.79]), respectively (Table S3). From 1990 to 2019, a total of 188, 9, and 7 countries (or territories) experienced increases, no changes, or decreases in mean FPG levels, respectively. The most marked increases and decreases in mean FPG levels were recorded in Sri Lanka (AAPC, 0.70% [95% CI, 0.66%–0.74%]) and the Democratic Republic of the Congo (AAPC, −0.17% [95% CI, −0.20% to −0.14%]), respectively (Figure 2, Table S4).
Figure 2.
AAPCs of mean FPG levels from 1990 to 2019 by country (or territory)
Global patterns and trends in high FPG-related disease burden from 1990 to 2019
Globally, in 2019, the rates of high FPG-related deaths and disability-adjusted life-years (DALYs) were 84.02 (95% UI, 66.05–108.09) and 2,223.84 (95% UI, 1,842.14–2,648.23) per 100,000 people, respectively. Similar estimates were observed after age standardization (Tables S5 and S6). These rates generally increased with age, and no significant gender differences were detected (Figures 1B and 1C). From 1990 to 2019, significant increases were observed in high FPG-related mortality (annualized rate of change [ARC], 0.54% [95% UI, 0.44%–0.65%]), DALYs rate (ARC, 0.54% [95% UI, 0.45%–0.63%]), and age-standardized DALYs rate (ASDR) (ARC, 0.07% [95% UI, 0.01%–0.14%]), but not in the age-standardized mortality rate (ASMR) (Tables S7 and S8). Stratification by age groups only observed significant increases in high FPG-related DLAY rates among people aged 20–24 and 35–69 years (Figures 1E and 1F). The increasing trends over time in high FPG-related disease burden were not significantly different between males and females either.
When dividing the countries (or territories) by World Bank income levels, lower- to middle-income countries had the greatest high FPG-related disease burden in 2019 (123.32 deaths [95% UI, 96.84–158.00] and 2,999.85 DALYs [95% UI, 2,500.61–3,550.29] per 100,000 people in 2019) and experienced the highest ARCs in high FPG-related disease burden from 1990 to 2019 (0.32% [95% UI, 0.20%–0.45%] increase in ASMR and 0.34% [95% UI, 0.23%, 0.46%] increase in ASDR) (Tables S6 and S8). In contrast, high-income countries had the lowest high FPG-related disease burden in 2019 and experienced the greatest decrease in high FPG-related disease burden from 1990 to 2019. A similar pattern in the economic disparities in disease burden was also observed in stratified analysis by SDI quintile. Further, when stratified by GBD super-region, the highest high FPG-related ASMR and ASDR in 2019 were observed in the region encompassing North Africa and the Middle East (143.83 deaths [95% UI, 105.00–195.54] and 3,332.73 DALYs [95% UI, 2,650.14–4,117.87] per 100,000 people), while the lowest ASMR and ASDR were observed in the high-income region (50.51 deaths [95% UI, 37.02–68.00] and 1,368.68 DALYs [95% UI, 1,093.79–1,690.36] per 100,000 people). From 1990 to 2019, the high FPG-related burden increased fastest in South Asia (ARC of ASMR, 0.26% [95% UI, 0.09%–0.45%]; ARC of ASDR, 0.30% [95% UI, 0.15%–0.45%]), and decreased fastest in the high-income regions (ARC of ASMR, −0.29% [95% UI, −0.35% to −0.21%]; ARC of ASDR, −0.12% [95% UI, −0.20% to −0.04%]).
Across the 204 GBD countries (or territories), in 2019, the highest high FPG-related ASMR and ASDR were observed in Kiribati (435.35 deaths [95% UI, 346.98–540.47] and 12,255.20 DALYs [95% UI, 9,799.69–15,073.04] per 100,000 people) (Table S6). The lowest high FPG-related ASMR and ASDR were detected in Japan (21.22 [95% UI, 14.86–30.20] per 100,000 people) and France (599.80 [95% UI, 464.55–761.83] per 100,000 people), respectively. From 1990 to 2019, high FPG-related disease burden increased fastest in Uzbekistan (ARC of ASMR, 4.69% [95% UI, 3.35%–6.24%]; ARC of ASDR, 3.34% [95% UI, 2.44%–4.42%]) and decreased fastest in Singapore (ARC of ASMR, −0.63% [95% UI, −0.70% to −0.56%]; ARC of ASDR, −0.52% [95% UI, −0.59% to −0.45%]) (Figure 3, Table S8).
Figure 3.
ARCs of high FPG-related ASMRs and ASDRs from 1990 to 2019 by country (or territory)
Predicted global patterns and trends in high FPG-related disease burden from 2020 to 2050
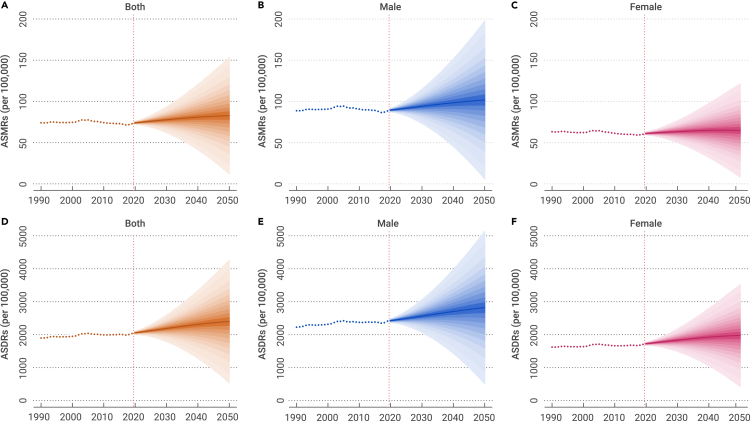
By 2050, the global high FPG-related disease burden is predicted to increase to 204.51 deaths (standard deviation [SD], 648.82) and 4,462.00 DALYs (SD, 7,812.76) per 100,000 people. The age-standardized disease burden is predicted to cause 82.72 deaths (SD, 35.92) and 2,397.85 DALYs (SD, 946.22) per 100,000 people by 2050 (Figures 4A and 4D, Tables S9 and S10). The rates of high FPG-related deaths and DALYs in 2050 are expected to be significantly greater in males than females, and generally increase with age (Figures 4B, 4C, 4E, and 4F, Tables S9 and S10). From 2020 to 2050, significantly increased AAPCs in high FPG-related deaths rate (2.90% [95% CI, 2.87%–2.93%]), DALYs rate (2.27% [95% CI, 2.26%–2.28%]), ASMR (0.37% [95% CI, 0.37%–0.38%]) and ASDR (0.52% [95% CI, 0.51%–0.53%]) are predicted (Tables S11 and S12). Rates of high FPG-related deaths and DALYs are predicted to increase among people aged ≥45 years and ≥40 years, respectively, but to decrease among people at other age groups. In addition, rates of high FPG-related disease burden are expected to grow significantly faster among males than females.
Figure 4.
Global predictions of high FPG-related ASMRs and ASDRs from 2020 to 2050
(A) Global predictions of high FPG-related ASMRs for both sexes.
(B) Global predictions of high FPG-related ASMRs for males.
(C) Global predictions of high FPG-related ASMRs for females.
(D) Global predictions of high FPG-related ASDRs for both sexes.
(E) Global predictions of high FPG-related ASDRs for males.
(F) Global predictions of high FPG-related ASDRs for females. Shaded areas indicate the 95% CIs of predicted high FPG-related ASMRs and ASDRs.
By World Bank income levels, in 2050, lower- to middle-income countries will have the greatest high FPG-related disease burden (153.63 deaths [SD, 81.92] and 4,271.06 DALYs [SD, 2,248.80] per 100,000 people) (Table S10). In contrast, upper to middle-income countries are expected to have the lowest burden (47.85 deaths [SD, 41.79] and 1,420.88 DALYs [SD, 877.91] per 100,000 people). From 2020 to 2050, the fastest increases in high FPG-related ASMR and ASDR are predicted to be in in lower- to middle-income countries (AAPC, 1.09% [95% CI, 1.08%–1.10%]) and high-income countries (AAPC, 1.61% [95% CI, 1.61%–1.62%]), respectively (Table S12). The fastest decreases in high FPG-related ASMR (AAPC, −1.17% [95% CI, –1.18% to −1.15%]) and ASDR (AAPC, −0.85% [95% CI, –0.86% to −0.84%]) are predicted to be in upper- to middle-income countries. Stratified analyses by SDI quintile indicated that lower SDI regions are expected to have greater high FPG-related disease burden than higher SDI regions (Tables S10 and S12). By GBD super-regions, South Asia is expected to experience the most pronounced increase in high FPG-related disease burden from 2020 to 2050 (2.74% [95% CI, 2.73%–2.74%] increase in ASMR and 2.97% [95% CI, 2.97%–2.98%] increase in ASDR) and bear the highest high FPG-related disease burden in 2050 (233.92 [SD, 258.39] deaths and 6,875.15 [SD, 6,811.10] DALYs per 100,000 people) (Tables S10 and S12). In contrast, the most marked decrease in high FPG-related disease burden from 2020 to 2050 is predicted to be in sub-Saharan Africa. The lowest high FPG-related ASMR and ASDR in 2050 are expected to be in the high-income regions and the region encompassing Southeast Asia, East Asia, and Oceania, respectively.
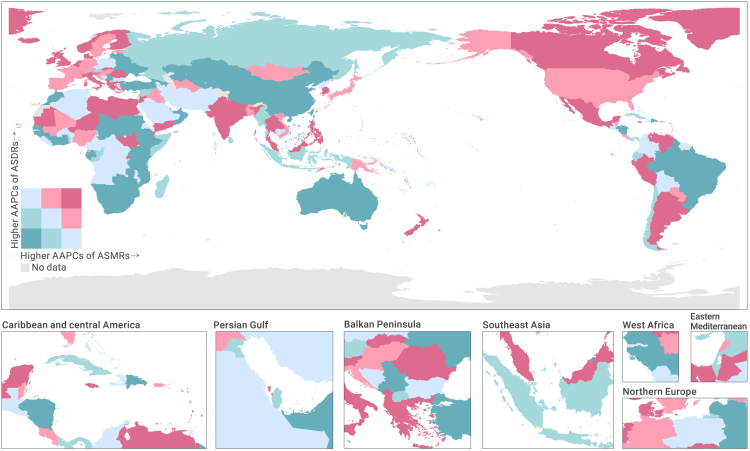
Across the 204 countries (or territories), in 2050, the highest high FPG-related ASMR and ASDR are predicted to be in Tokelau (1,137.93 [SD, 1,235.46] per 100,000 people) and the Marshall Islands (18,541.25 [SD, 10,621.80] per 100,000 people), respectively (Table S10). The lowest high FPG-related ASMR and ASDR are predicted to be in Singapore (8.59 [SD, 6.97] per 100,000 people) and Lithuania (742.83 [SD, 2,316.47] per 100,000 people), respectively. From 2020 to 2050, the most marked increases in high FPG-related ASMR and ASDR are predicted to occur in Venezuela (AAPC, 5.39%; 95% CI, 5.38%–5.40%) and South Sudan (AAPC, 6.75%; 95% CI, 6.75%–6.76%), respectively (Figure 5, Table S12). The greatest decreases in high FPG-related ASMR and ASDR are expected to occur in the United Arab Emirates (AAPC of ASMR, −6.09% [95% CI, −6.12% to −6.06%]; AAPC of ASDR, −4.14% [95% CI, −4.18% to −4.11%).
Figure 5.
AAPCs of high FPG-related ASMRs and ASDRs from 2020 to 2050 by country (or territory)
Risk factors for mean FPG levels and high FPG disease burden
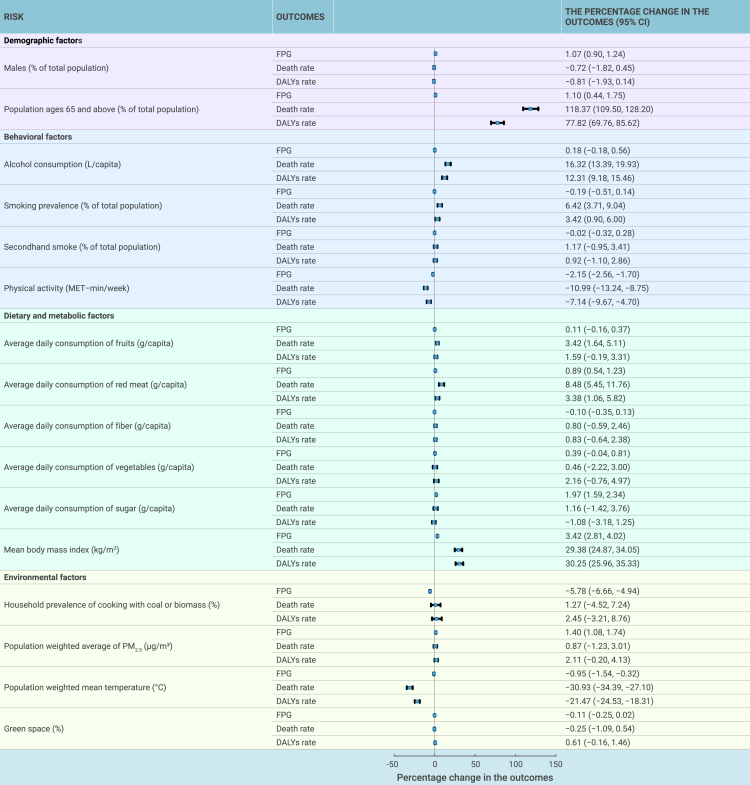
Results from the Bayesian spatiotemporal models suggest that greater proportions of the elderly, physical inactivity, higher consumption of red meat and body mass index (BMI), as well as lower mean air temperature were significantly and consistently associated with both high FPG levels and high FPG-related disease burden (Figure 6). More specifically, an interquartile range (IQR) increment in the above risk factors were associated with 0.89%–3.42% increases in mean FPG levels, 8.48%–118.37% increases in high FPG-related mortality, and 3.38%–77.82% increases in high FPG-related DALYs rate.
Figure 6.
Percentage changes in FPG levels and high FPG-related death and DALYs rates with per IQR increment of demographic, behavioral, dietary, metabolic and environmental factors
Error bars indicate the 95% CIs of the percentage changes in the outcomes.
Greater alcohol consumption levels and cigarette smoking prevalence were significantly associated with higher high FPG-related disease burden (i.e., an IQR increment in the two factors were associated with 6.42%–16.32% and 3.42%–12.31% increases in high FPG-related mortality rate and DALYs rate, respectively). No significant associations were observed between alcohol consumption and cigarette smoking and mean FPG levels (Figure 6).
A higher proportion of males and a higher household prevalence of cooking with coal or biomass as well as higher levels of sugar consumption and fine particulate matter (PM2.5) exposure were significantly associated with mean FPG levels, but not with high FPG-related disease burden; however, the directions of the above significant associations were mixed or unexpected (Figure 6). Consumption of fruits was associated with high FPG-related mortality. No significant associations were observed for consumption of fibers and vegetables, secondhand smoke, and green space exposure with either mean FPG levels or high FPG-related disease burden.
Discussion
To our knowledge, this is the first comprehensive and systematic analysis of current and future global patterns of FPG levels and high FPG-related disease burden. We found that the burden of high FPG-related disease was substantial for both historical (1990–2019) and future (2020–2050) periods. In addition, we observed that the magnitudes and trends of mean FPG levels and high FPG-related disease burden varied by sex, age, socioeconomic status (SES) and geographic location. Larger estimates were observed for the middle-aged and elderly population, and people living in low-to-middle income countries. We also found that aging, unhealthy lifestyles (i.e., alcohol use and tobacco smoking, physical inactivity, and excessive consumption of red meat), elevated BMI, and lower air temperature were potential risk factors for elevated FPG levels and high FPG-related disease burden. Collectively, these findings portray the urgent need at both individual and population levels to decrease the disease burden caused by high FPG.
Temporal trends
This is one of the few studies that estimated global patterns in mean FPG levels over time, to our knowledge.8 We found that FPG levels varied by sex, age, regions and showed an increasing trend from 1990 to 2019. The available estimates on global FPG levels were performed as early as 2008.8 The current analysis provides updated evidence and includes a large number of studied countries. The substantial and ever-increasing trends in the high FPG-related disease burden from 1990 to 2019 are consistent with past study.15 In addition, our current study extends previous estimations in the disease burden to predictions in the future 30 years, which suggests a long-term and sustained pattern of the increasing disease burden.
The exact reasons for the increasing global FPG levels and high FPG-related disease burden are unclear, but people’s increasing exposure to known risk factors may be involved. Accumulating evidence has documented that obesity, unhealthy lifestyle, and environmental hazard exposures can increase FPG levels.16,17,18,19 Our current analysis supports such evidence and documented that older age, alcohol drinking, tobacco smoking, consumption of red meat, physical inactivity, higher BMI levels, and lower air temperature levels were associated with elevated FPG levels or high FPG-related disease burden (detailed discussion on these risk factors are listed in a below section). Moreover, we found that most of these risk factors have been increasing in strength over the past 30 years (Figure S1). An aging population and urbanization in particular are expected to continue to increase, further exasperating the high FPG-related disease burden, as predicted by International Diabetes Federation20 and the current study.
In addition, policies tailored to these risk factors may not have kept pace with relevant health needs in many countries. Researchers have proposed that opportunistic screening for DM and impaired glucose tolerance is beneficial and cost-effective, but this strategy has not been regularly implemented.21 In the United States, for example, the prevalence of DM screening during office visits in 2015 was only 13%.22 Methods to improve glycemic control when high FPG is detected remains a great challenge. For example, lifestyle modifications aiming at weight loss are compelling approaches for the management of high FPG, especially in developing countries, but such interventions are hard to be maintained because of the need for long-term adherence and the shortage of eligible lifestyle coaches.23 Pharmacological treatments such as metformin are complementary solutions for glycemic control, but adverse effects (e.g., biochemical B12 deficiency and anemia) are possible.24 To address the above obstacles, more effective and feasible management strategies for high FPG should be explored.
Spatial variation
We found that mean FPG levels and high FPG-related disease burden varied greatly across geographic locations. In addition to genetic predisposition,25 SES levels may explain much of this variation. We observed that populations in countries with low to middle SES levels experienced the fastest increases in both mean FPG levels and high FPG-related disease burden from 1990 to 2019. These populations are also predicted to experience the greatest increase in high FPG-related disease burden from 2020 to 2050. Countries (or territories) with the low to middle SES levels also have relatively higher exposures to environmental hazards and lower health expenditure.26 To address such health inequities, cost-effective measures should be explored to mitigate the increasing high FPG-related disease burden in contexts beyond higher income countries.
National-level interventions for hyperglycemia may also contribute to the observed spatial variations. For example, the lowest high FPG-related ASMR and ASDR in 2019 were observed in Japan and France, respectively, and the highest declines in high FPG-related ASMR and ASDR from 1990 to 2019 were observed in Singapore. These countries take effective health care policies and provide higher levels of universal health coverage than others.27 Correspondingly, residents in such countries are more likely to receive comprehensive health services. Singapore, for example, has implemented a series of measures to control and reduce high FPG, including the annual National Healthy Lifestyle Campaign in 1992 and the War on Diabetes policy in 2016.28 These policies aim to raise health awareness, promote healthy lifestyles, enhance the skills of healthcare providers, generate community-based recommendations, and raise medical care investment, thus creating an environment conducive to glycemic control.
Finally, the disparity in high FPG-related disease burden might also be explained by regional differences in dietary habits. For example, the typical Japanese diet, which includes high intakes of soy/isoflavones and fish/n-3 fatty acids as well as low intakes of red meat, has been shown to protect against high FPG.29
Potential risk factors
We observed that aging was a potential risk factor for high FPG levels and high FPG-related disease burden. Aging is characterized by decreased secretion of sex steroids, growth hormone, and insulin growth factor, which may interactively cause reduced lean body mass and increased adiposity, and further increase FPG levels.30 Our estimates also showed that both historical and predicted rates of high FPG-related deaths and DALYs increased with age. This finding indicates that preventing high FPG among aging populations is critical, especially in countries whose populations are quickly aging.
We also detected several lifestyle risk factors for elevated FPG levels and high FPG-related disease burden, including tobacco smoking, alcohol consumption, physical inactivity, and red meat consumption, which are consistent with numerous prior studies.25,31,32 These unhealthy lifestyles may increase FPG levels directly by affecting hormones like insulin and insulin-like growth factor,31 and indirectly by increasing BMI.31 Both our current analysis and prior research31,33 have demonstrated that BMI is a major risk factor for elevated FPG levels and high FPG-related disease burden. Governments and some organizations have taken preventative efforts to decrease people’s exposure to these lifestyle risk factors in recent decades. For example, as guided by the WHO Framework Convention on Tobacco Control, interventions through taxation, smoke-free polices, and advertisement bans have been widely adopted,34 and the prevalence of tobacco smoking has decreased substantially from 1990 to 2019 (Figure S1). Similar interventions have also been used for controlling alcohol drinking34; however, the intervention effects, at global scale, are minimal (Figure S1). In addition, because of urbanization, the universal use of convenient automobiles, and a plentiful food supply, physical inactivity and red meat consumption are increasingly common.25 Governments and individuals should continue to take more efficient and comprehensive strategies to stimulate substantial improvements in adopting healthier lifestyles with the aim of controlling high FPG and its disease burden.
Finally, we observed that lower air temperature levels may be a risk factor for high FPG-related disease burden. A possible explanation may be that lower air temperature can increase FPG levels by changing diet and exercise patterns, raising infectious probabilities, activating the sympathetic nervous system, and triggering the secretion of catecholamines.35,36 Effects of air temperature on human health (including FPG levels) are often reported to be non-linear; higher and lower than optimal air temperature may be hazardous.35,36 Although we attempted to fit non-linear models, the results supported linear associations between air temperature and high FPG-related disease burden (Table S13). It is noteworthy that our data were at country (or territory) level and annually averaged, which might be too crude to detect potential non-linear relationships. This limitation also might have biased our estimates for other environmental factors including outdoor and indoor air pollution and green space, which were found to be not associated with FPG levels and high FPG-related disease burden or yielded mixed results. Better designed studies using rich data are needed to validate the glycemic effects of outdoor environmental factors, preferably at a global scale.
Limitations
In interpreting our findings, some limitations should be considered. First, our study was bounded to the GBD 2019 data, which were constrained by the availability of the primary data, discordant case definitions, and collinearity between covariates.37,38 Second, GBD 2019 defined high FPG with the theoretical minimum risk exposure level.39 Its cut-off value (4.8–5.4 mM/L) was different from the commonly used 6.1 mM/L. Third, FPG data were unavailable in 77 countries (or territories), which were alternatively imputed by statistical models.38 Trends in FPG levels and high FPG-related disease burden in these countries (or territories) might have been imprecisely estimated. Fourth, we predicted the burden of high FPG-related disease burden by using the Bayesian age-period-cohort (BAPC) model, which contributed the change in the disease burden into age, period, and cohort effects and did not further incorporate other factors that could influence the disease burden.40 This might have affected the accuracy of the predicted estimates. Nonetheless, to our knowledge, this study was the first to predict the global disease burden of high FPG, which not only advances our knowledge of the secular trends in high FPG-related disease burden, but also serves as a baseline for future work. Fifth, although we explored potential risk factors for elevated FPG levels and high FPG-related disease burden at a global scale, we used country-level and annually averaged data, which might have caused misclassification bias. The ecological study design has well-known limitations and places limits on the strength of evidence that can be generated. Sixth, the risk factors explored in our study were based on the existing knowledge of high FPG and were limited to variables that GBD 2019 provided (although we additionally included green space from another resource). Additional risk factors, such as psychosocial stress,41 noise,42 light at night,43 genetic background,25 medicine use,44 and infectious agents,45 were not covered. Last, GBD 2019 estimated the disease burden of high FPG with a limited set of health outcomes, yet emerging evidence has documented that other diseases are also related to high FPG, such as hypertension46 and adverse pregnancy outcomes.47 Thus, the adverse health effects of high FPG might have been underestimated.
Conclusion
This study provides a comprehensive analysis of the epidemiology, current and future disease burden, and possible risk factors for FPG levels and high FPG-related disease burden. High FPG remains an important cause of great disease burden and is predicted to continue to strain health systems through 2050. The magnitude and temporal trends of FPG levels and their related disease burden are heterogeneous. Middle-aged and elderly populations, and people living in countries with low to middle SES levels may suffer more and should receive more attention in glycemic management policies. Furthermore, aging, unhealthy lifestyles, elevated BMI, and lower air temperatures are potential risk factors for mean FPG levels and their related disease burden. More robust and effective interventions that target identified risk factors are needed to handle the increasingly large disease burden of high FPG.
Materials and methods
Data source and definitions
The GBD Study is led by the Institute for Health Metrics and Evaluation (IHME), which aims to collate all available data and use innovative methods to produce comparable estimates of the world’s most important health problems. GBD 2019 is the most updated results of IHME. The GBD 2019 provides a systematic and scientific assessment of disease burden due to 369 diseases and injuries and 87 risk factors across 204 countries (or territories).37
In GBD 2019, high FPG is denoted as FPG levels greater than 4.8-5.4 mM/L.38 GBD 2019 used the World Cancer Research Fund criteria for convincing or probable evidence of risk-outcome pairs. Fifteen GBD cause Level 3 outcomes met the criteria and were included in the analysis of high FPG-related disease burden: DM, ischemic heart disease, stroke, tuberculosis, chronic kidney disease, peripheral artery disease, blindness and vision loss, Alzheimer’s disease and other dementias, liver cancer, breast cancer, ovarian cancer, bladder cancer, pancreatic cancer, colon and rectum cancer, and tracheal, bronchus, and lung cancer.38 High FPG-related disease burden was measured by death and DALYs. DALYs are the sum of years of life lost due to premature mortality and years lived with disability.38
We obtained three families of metrics from the GBD Results Tool48 and GBD Compare Tool26 to assess the global patterns and trends in high FPG and its related disease burden from 1990 to 2019, which included the (1) mean FPG levels among individuals aged 25 years and older, (2) death rates and ASMRs, and (3) DALYs rates and ASDR. Methodological procedures on estimating the above metrics have been described previously.38 The GBD generated 95% UIs for its metrics, which were defined as the 2.5th and 97.5th percentiles of the ordered 1,000 estimations.38
To predict high FPG-related disease burden in the future 30 years (i.e., from 2020 to 2050), we retrieved the numbers of high FPG-related deaths and DALYs by sex, 5-year age group, country or region, and year (1990–2019).48 In addition, we extracted the predictive population data between 1990 and 2050 from the 2022 Revision of World Population Prospects in UNdata: https://population.un.org/wpp/.49 Finally, we downloaded worldwide standard population data from the Surveillance, Epidemiology, and End Results Program supported by the U.S. National Cancer Institute: https://seer.cancer.gov/stdpopulations/.50
To explore potential risk factors for elevated FPG levels and high FPG-related disease burden, we collected data on demographic factors (i.e., the proportion of males and population aged ≥65 years), behavioral factors (i.e., alcohol consumption, smoking prevalence, proportion of population exposed to secondhand smoke, and physical activity levels), dietary and metabolic factors (i.e., average daily consumption of fruits, red meat, fiber, vegetables and sugar, and mean BMI), and environmental factors (i.e., household prevalence of cooking with coal or biomass, population weighted mean PM2.5 levels, and population-weighted mean air temperature levels) from the GBD Compare Tool.26 In addition, considering recent evidence documented a strong association between green space and FPG levels,51,52 we also considered lack of green space as a potential risk factor and obtained data on the percentage of green space from Google Earth Engine platform: https://developers.google.cn/earth-engine/.53 Informed consent was not needed because these databases were deidentified.
Statistical analyses
We delineated patterns and trends in mean FPG levels and high FPG-related disease burden using three analyses. First, we cross-sectionally estimated the distribution of mean FPG levels and high FPG-related disease burden in 2019. Second, we investigated the temporal trends of mean FPG levels from 1990 to 2019 by calculating the AAPCs along with 95% CIs through a Joinpoint regression analysis. The significance of the change was tested using a Monte Carlo Permutation method by the Joinpoint software (the Surveillance Research Program of the U.S. National Cancer Institute; version 4.9.0). Third, we investigated the temporal trends of high FPG-related disease burden using annualized rates of change (ARCs) directly provided by the GBD 2019.
These analyses were performed among the overall population (i.e., at a global level) and then in subgroups stratified by sex (males vs females), age (5-year age groups), and country (or region). For country (region) analyses, we used three types of classifications. First, we divided countries (or territories) into low, lower middle, upper middle, and high income levels based on gross national income per capita recommended by the World Bank. Second, we classified countries (or territories) by SDI quintiles: low, low-middle, middle, high-middle, and high.37 Third, we used the GBD regional classification system to classify countries (or territories) into seven super-regions (Central Europe, Eastern Europe, and Central Asia; high income; Latin America and Caribbean; North Africa and Middle East; South Asia; Southeast Asia, East Asia, and Oceania; Sub-Saharan Africa) based on epidemiological similarity and geographic closeness.37 We also tested the significance of differences in mean FPG levels, high FPG-related diseases burden, AAPCs, and ARCs between sexes using two-sided Z-tests.54
We predicted the trends in high FPG-related disease burden from 2020 to 2050 using a BAPC analysis. The BAPC model is built on the assumption that time-related changes in health outcomes can be separated into age, period, and cohort effects.40 Age effects account for changes over the life course of individuals; period effects represents changes because of the events in particular years; cohort effects corresponds to changes caused by the replacement of older cohorts of individuals with younger ones with different characteristics.40 Bayesian inference in the BAPC model can explicitly incorporate theoretical considerations and qualitative judgments into the inferential process, and shows better coverage and precision than other prediction methods.55 In brief, we arranged high FPG-related disease burden and predictive population data into successive 5-year age intervals from 0 to 4 years to ≥95. The World Standard population was used to standardize the rates of deaths and DALYs. A BAPC model was then fitted using a Poisson model with integrated nested Laplace approximations to generate predictions for age-specific and age-standardized rates of high FPG-related disease burden from 2020 to 2050.
We used Bayesian spatiotemporal models, fitted with Markov chain Monte Carlo (MCMC) simulations, to assess associations of demographic, behavioral, dietary, metabolic, and environmental factors with mean FPG levels as well as high FPG-related mortality and DALYs rates. Before modeling, we constructed a neighborhood matrix, denoting whether each pair of countries (or territories) were close together, to calculate weights corresponding with neighbors. A total of 49 countries (or territories) were excluded because their weights corresponding to neighbors were zero. Ultimately, 155 countries (or territories) were included in the current analysis. We fitted the model using the following equation:
where K represented the number of countries (or territories) (i.e., 155); N was the number of years studied (i.e., 30); Ykt indicated the mean FPG levels or the rates of high FPG-related deaths and DALYs for country k and year t; xkt was the level of the studied risk factor for country k and year t; Conkt = (Conkt1, …, Conktp) was a vector of p known confounders for country k and year t; βx and βCon were regression coefficients for studied risk factors and confounders, respectively; and φkt was the spatiotemporal autocorrelation random effect for country k and year t.
We selected confounders based on a priori knowledge and the criteria that they should be related to both the explored risk factors and outcomes but lie outside the causal pathways between them.56 All confounders were scaled and centered to have a mean (SD) of 0 (1) before being included into the models. To normalize the distribution, all outcome variables were naturally log-transformed. Models were run with 110,000 MCMC iterations, of which the first 10,000 iterations were discarded as burn-in and the remaining 100,000 samples were thinned by 100 to remove almost all of the correlation among the iterations. The estimated effects were reported as percent changes and 95% CIs in relation to per IQR increment in levels of risk factors.
An α-level of 0.05 was adopted to indicate statistical significance. R (version 4.2.0) was used to perform all the above-mentioned data processing and analyses except where otherwise noted.
Acknowledgments
The authors appreciate the great efforts of the GBD 2019 Risk Factor collaborators. This study was funded by the National Key Research and Development Program of China (No. 2018YFC1004300; 2018YFC1004301), the National Natural Science Foundation of China (No.81972992), and the Central Public-interest Scientific Institution Basal Research Fund of South China Institute of Environmental Sciences, and MEE (PM-zx703-202204-124). The funders were not involved in the research and preparation of the article, including study design; collection, analysis, and interpretation of data; writing of the article; or in the decision to submit it for publication.
Author contributions
H.L.Q., S.J.F, B.Y.Y., and G.H.D. conceptualized this paper. H.L.Q. and S.J.F designed the methods, accessed and verified the underlying data, performed the analyses, and wrote the first draft of the manuscript. K.Z., Z.H., M.H.E.M.B., L.D.K., T.Z., Y.N.L., X.X.L., L.X.H., J.X.L., Y.D.Z., Y.T.X., and J.H. critically revised the manuscript and helped to interpret the data. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Declaration of interests
The authors declare no competing interests.
Published Online: May 26, 2023
Footnotes
It can be found online at https://doi.org/10.1016/j.xinn.2023.100450.
Contributor Information
Guang-Hui Dong, Email: donggh5@mail.sysu.edu.cn.
Bo-Yi Yang, Email: yangby23@mail.sysu.edu.cn.
Lead contact website
Supplemental information
References
- 1.Lee P.H., Fu H., Lai T.C., et al. Glycemic control and the risk of tuberculosis: a cohort study. PLoS Med. 2016;13 doi: 10.1371/journal.pmed.1002072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang C.Y., Li H.Y., Sung F.C., et al. Relationship between fasting plasma glucose and incidence of diabetes in children and adolescents. Diabet. Med. 2019;36:633–643. doi: 10.1111/dme.13925. [DOI] [PubMed] [Google Scholar]
- 3.Kaneko H., Itoh H., Kiriyama H., et al. Fasting plasma glucose and subsequent cardiovascular disease among young adults: analysis of a nationwide epidemiological database. Atherosclerosis. 2021;319:35–41. doi: 10.1016/j.atherosclerosis.2020.12.024. [DOI] [PubMed] [Google Scholar]
- 4.Pearson-Stuttard J., Papadimitriou N., Markozannes G., et al. Type 2 diabetes and cancer: an umbrella review of observational and mendelian randomization studies. Cancer Epidemiol. Biomarkers Prev. 2021;30:1218–1228. doi: 10.1158/1055-9965.EPI-20-1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bommer C., Sagalova V., Heesemann E., et al. Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care. 2018;41:963–970. doi: 10.2337/dc17-1962. [DOI] [PubMed] [Google Scholar]
- 6.Mirzaei F., Khodadadi I., Vafaei S.A., et al. Importance of hyperglycemia in Covid-19 intensive-care patients: mechanism and treatment strategy. Prim. Care Diabetes. 2021;15:409–416. doi: 10.1016/j.pcd.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Heath Organization . 2022. Global Action Plan for the Prevention and Control of NCDs 2013-2020.https://www.who.int/publications/i/item/9789241506236 [Google Scholar]
- 8.Danaei G., Finucane M.M., Lu Y., et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 9.Ye L., Xu J., Zhang T., et al. Global burden of noncommunicable diseases attributable to high fasting plasma glucose. J. Diabetes. 2020;12:807–818. doi: 10.1111/1753-0407.13072. [DOI] [PubMed] [Google Scholar]
- 10.Imperatore G., Boyle J.P., Thompson T.J., et al. Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care. 2012;35:2515–2520. doi: 10.2337/dc12-0669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu J., Liu M., Chai Z., et al. Projected rapid growth in diabetes disease burden and economic burden in China: a spatio-temporal study from 2020 to 2030. Lancet Reg. Health. West. Pac. 2023;33 doi: 10.1016/j.lanwpc.2023.100700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Awad S.F., O'Flaherty M., Critchley J., et al. Forecasting the burden of type 2 diabetes mellitus in Qatar to 2050: a novel modeling approach. Diabetes Res. Clin. Pract. 2018;137:100–108. doi: 10.1016/j.diabres.2017.11.015. [DOI] [PubMed] [Google Scholar]
- 13.Awad S.F., Al-Mawali A., Al-Lawati J.A., et al. Forecasting the type 2 diabetes mellitus epidemic and the role of key risk factors in Oman up to 2050: mathematical modeling analyses. J. Diabetes Investig. 2021;12:1162–1174. doi: 10.1111/jdi.13452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Duncan B.B., Cousin E., Naghavi M., et al. The burden of diabetes and hyperglycemia in Brazil: a global burden of disease study 2017. Popul. Health Metr. 2020;18:9. doi: 10.1186/s12963-020-00209-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liang R., Feng X., Shi D., et al. The global burden of disease attributable to high fasting plasma glucose in 204 countries and territories, 1990-2019: an updated analysis for the Global Burden of Disease Study 2019. Diabetes. Metab. Res. Rev. 2022;38 doi: 10.1002/dmrr.3572. [DOI] [PubMed] [Google Scholar]
- 16.GBD 2015 Obesity Collaborators. Afshin A., Forouzanfar M.H., et al. Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 2017;377:13–27. doi: 10.1056/NEJMoa1614362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.GBD 2017 Diet Collaborators Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2019;393:1958–1972. doi: 10.1016/S0140-6736(19)30041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Silveira M.L., Whitcomb B.W., Pekow P., et al. Perceived psychosocial stress and glucose intolerance among pregnant Hispanic women. Diabetes Metab. 2014;40:466–475. doi: 10.1016/j.diabet.2014.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu Y., Fu R., Lei C., et al. Estimates of type 2 diabetes mellitus burden attributable to particulate matter pollution and its 30-year change patterns: a systematic analysis of data from the Global Burden of Disease Study 2019. Front. Endocrinol. 2021;12:689079. doi: 10.3389/fendo.2021.689079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saeedi P., Petersohn I., Salpea P., et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res. Clin. Pract. 2019;157 doi: 10.1016/j.diabres.2019.107843. [DOI] [PubMed] [Google Scholar]
- 21.Simmons D., Zgibor J.C. Should we screen for type 2 diabetes among asymptomatic individuals? Yes. Diabetologia. 2017;60:2148–2152. doi: 10.1007/s00125-017-4397-x. [DOI] [PubMed] [Google Scholar]
- 22.Shealy K.M., Wu J., Waites J., et al. Patterns of diabetes screening and prediabetes treatment during office visits in the US. J. Am. Board Fam. Med. 2019;32:209–217. doi: 10.3122/jabfm.2019.02.180259. [DOI] [PubMed] [Google Scholar]
- 23.Cefalu W.T., Buse J.B., Tuomilehto J., et al. Update and next steps for real-world translation of interventions for type 2 diabetes prevention: reflections from a diabetes care. Diabetes Care. 2016;39:1186–1201. doi: 10.2337/dc16-0873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aroda V.R., Edelstein S.L., Goldberg R.B., et al. Long-term metformin use and vitamin B12 deficiency in the diabetes prevention program outcomes study. J. Clin. Endocrinol. Metab. 2016;101:1754–1761. doi: 10.1210/jc.2015-3754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chan J.C.N., Malik V., Jia W., et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 2009;301:2129–2140. doi: 10.1001/jama.2009.726. [DOI] [PubMed] [Google Scholar]
- 26.Global Burden of Disease Study 2019 (GBD 2019) 2023. Covariates 1980-2019 | GDHx.https://ghdx.healthdata.org/record/global-burden-disease-study-2019-gbd-2019-covariates-1980-2019 [Google Scholar]
- 27.Institute for Health Metrics and Evaluation . 2022. IHME Data | GHDx.https://ghdx.healthdata.org/ihme_data [Google Scholar]
- 28.Singapore Ministry of Health . 2022. War on diabetes.https://www.moh.gov.sg/wodcj [Google Scholar]
- 29.Fan R., Xu M., Wang J., et al. Sustaining effect of intensive nutritional intervention combined with health education on dietary behavior and plasma glucose in type 2 diabetes mellitus patients. Nutrients. 2016;8 doi: 10.3390/nu8090560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chan J.C.N., Lim L.L., Wareham N.J., et al. The Lancet commission on diabetes: using data to transform diabetes care and patient lives. Lancet. 2021;396:2019–2082. doi: 10.1016/S0140-6736(20)32374-6. [DOI] [PubMed] [Google Scholar]
- 31.Eyre H., Kahn R., Robertson R.M., et al. Preventing cancer, cardiovascular disease, and diabetes: a common agenda for the American cancer society, the American diabetes association, and the American heart association. Diabetes Care. 2004;35:1999–2010. doi: 10.2337/diacare.27.7.1812. [DOI] [PubMed] [Google Scholar]
- 32.Ley S.H., Hamdy O., Mohan V., et al. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet. 2014;383:1999–2007. doi: 10.1016/S0140-6736(14)60613-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Afzal S., Brøndum-Jacobsen P., Bojesen S.E., et al. Vitamin D concentration, obesity, and risk of diabetes: a mendelian randomisation study. Lancet Diabetes Endocrinol. 2014;2:298–306. doi: 10.1016/S2213-8587(13)70200-6. [DOI] [PubMed] [Google Scholar]
- 34.GBD 2019 Cancer Risk Factors Collaborators The global burden of cancer attributable to risk factors, 2010-19: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2022;400:563–591. doi: 10.1016/S0140-6736(22)01438-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Clougherty J.E. A growing role for gender analysis in air pollution epidemiology. Environ. Health Perspect. 2010;118:167–176. doi: 10.1289/ehp.0900994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li S., Zhou Y., Williams G., et al. Seasonality and temperature effects on fasting plasma glucose: a population-based longitudinal study in China. Diabetes Metab. 2016;42:267–275. doi: 10.1016/j.diabet.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 37.GBD 2019 Diseases and Injuries Collaborators. Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.GBD 2019 Risk Factors Collaborators. Injuries Collaborators Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Singh G.M., Danaei G., Farzadfar F., et al. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: a pooled analysis. PLoS One. 2013;8 doi: 10.1371/journal.pone.0065174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fosse E. Bayesian age-period-cohort models. 2023. https://scholar.harvard.edu/files/apc/files/bayesianchapteref.pdf
- 41.Kelly S.J., Ismail M. Stress and type 2 diabetes: a review of how stress contributes to the development of type 2 diabetes. Annu. Rev. Public Health. 2015;36:441–462. doi: 10.1146/annurev-publhealth-031914-122921. [DOI] [PubMed] [Google Scholar]
- 42.Kolb H., Martin S. Environmental/lifestyle factors in the pathogenesis and prevention of type 2 diabetes. BMC Med. 2017;15:131. doi: 10.1186/s12916-017-0901-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fleury G., Masís-Vargas A., Kalsbeek A. Metabolic implications of exposure to light at night: lessons from animal and human studies. Obesity. 2020;28(Suppl 1):S18–S28. doi: 10.1002/oby.22807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fathallah N., Slim R., Larif S., et al. Drug-induced hyperglycaemia and diabetes. Drug Saf. 2015;38:1153–1168. doi: 10.1007/s40264-015-0339-z. [DOI] [PubMed] [Google Scholar]
- 45.Macdonald G. Harrison’s internal medicine, 17th edition. Med. J. 2008;38:932. [Google Scholar]
- 46.Geva M., Shlomai G., Berkovich A., et al. The association between fasting plasma glucose and glycated hemoglobin in the prediabetes range and future development of hypertension. Cardiovasc. Diabetol. 2019;18:53. doi: 10.1186/s12933-019-0859-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang C., Wei Y., Yang Y., et al. Evaluation of the value of fasting plasma glucose in the first trimester for the prediction of adverse pregnancy outcomes. Diabetes Res. Clin. Pract. 2021;174 doi: 10.1016/j.diabres.2021.108736. [DOI] [PubMed] [Google Scholar]
- 48.GBD Results 2023. https://vizhub.healthdata.org/gbd-results
- 49.World Population Prospects - Population Division - United Nations 2023. https://population.un.org/wpp/
- 50.Standard populations (millions) for age-adjustment . 2023. SEER Population Datasets.https://seer.cancer.gov/stdpopulations/index.html [Google Scholar]
- 51.Yang B.Y., Zhao T., Hu L.X., et al. Greenspace and human health: an umbrella review. Innovation. 2021;2 doi: 10.1016/j.xinn.2021.100164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hou J., Tu R., Dong Y., et al. Associations of residing greenness and long-term exposure to air pollution with glucose homeostasis markers. Sci. Total Environ. 2021;776 doi: 10.1016/j.scitotenv.2021.145834. [DOI] [PubMed] [Google Scholar]
- 53.Google Earth Engine | Google Developers 2023. https://developers.google.cn/earth-engine
- 54.Altman D.G., Bland J.M. Interaction revisited: the difference between two estimates. BMJ Br. Med. J. (Clin. Res. Ed.) 2003;326:219. doi: 10.1136/bmj.326.7382.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Knoll M., Furkel J., Debus J., et al. An r package for an integrated evaluation of statistical approaches to cancer incidence projection. BMC Med. Res. Methodol. 2020;20:257. doi: 10.1186/s12874-020-01133-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Conference Proceedings. Glasser, S. P. 2014. Bias, Confounding, and Effect Modification (Interaction) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.