Abstract
Purpose:
The present work style and lifestyle have increased the digital device use. Therefore, an increase in digital eyestrain is to be expected. We undertook a survey during coronavirus disease 2019 (COVID-19) pandemic to investigate the practice of 20/20/20 rule and its association with digital device use and asthenopic symptoms. While this rule is commonly advised, little is known about its validity.
Methods:
An online survey form was disseminated through social media and emails. The questions for eye-related symptoms were similar to the convergence insufficiency symptom survey (CISS). Participants with age ≥5 years were included, with parents completing the survey for children (≤16 years).
Results:
A total of 432 participants (mean ± standard deviation [SD]: 26.06 ± 13.92 years) were enrolled, of which 125 responses were for children. The 20/20/20 rule was practiced only by 34% of the participants either regularly (n = 38) or occasionally (n = 109). Those who had complaints of burning sensation and headache tended to practice this rule. Among adult participants, more females (47%) practiced this rule when compared to males (23%). Also, adult females significantly (P = 0.04) had more symptoms score when compared to males. In children, no such gender difference was found.
Conclusion:
Only one-third of participants practice the 20/20/20 rule at least occasionally. More number of adult females being symptomatic and practicing in greater number could be due to higher prevalence of dry eye condition in females. While the symptom of burning sensation could be related to dry eye, that of headache could be related to refractive error or binocular vision dysfunctions.
Keywords: 20-20-20 rule, computer vision syndrome, COVID-19 pandemic, digital eye strain
It is now widely accepted that the coronavirus disease 2019 (COVID-19) pandemic has increased the use of digital technologies to minimize in-person interactions. Work and study from home still continues in many parts of the world.[1-4] The convenience of connecting with people in different geographic locations has also promoted the increased use of digital platforms, in spite of travel being less restrictive. Hybrid models of both online and offline meetings, conferences, and classrooms are also increasingly becoming popular. Additionally, health-care services have also increasingly adapted to the digital technology. Now both practitioners and patients are willing to up take telemedicine services, including teleophthalmology.[5-7] This trend would also increase the digital screen time for all stakeholders. This altered work style and lifestyle has become the new normal going forward. While this increased digitization is present on one hand, excessive use of digital devices is known to have an increased risk of digital eyestrain on the other end.[8-10] Such a risk has been confirmed with recent studies that have reported increased eyestrain during this COVID-19 pandemic.[11,12]
The 20/20/20 rule is recommended to reduce symptoms of eye fatigue and eyestrain, particularly for digital device users. The rule suggests taking 20-s break to view objects 20 ft away after 20 min of screen use.[13] For someone working for 8 h on a computer, this would translate to taking a break for 24 times, and overall spending only 8 min of total time to gaze far away. Many eye care practitioners commonly recommend this rule as a clinical advice. This rule also appears in news articles, blogs and health articles on social media, web pages, and in few research articles.[13-16] However, the evidence for the effectiveness of this 20/20/20 rule does not appear to be well established.[17] As a first step, we aimed to investigate how many people practice this rule and if there was any association between their asthenopic symptoms and the practice of the 20/20/20 rule. As a part of a larger study, we undertook a survey to investigate this question and gauge the interest of the public to utilize the teleophthalmology services. The results of the latter have already been published.[6] In this paper, we report on the 20/20/20 rule and its associations.
Methods
A prospective survey was conducted during the COVID-19 pandemic period from October 2020 to January 2021. The survey conducted was in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board. The survey was designed on Google forms and administered through social media platforms. The survey consisted of three sections: (i) demographic details that only included age, gender, country, and state (if from India), (ii) digital device use and practice of 20/20/20 rule and (iii) symptoms questionnaire. No other personal information that can identify the individual was collected.
Before recruitment, participants were given an overview that informed about the purpose, length, and anonymity of the survey. Participants with children were encouraged to answer for their child (≤16 years) and also for themselves in separate forms (i.e., to take the survey more than once). Only those who indicated consent (online consent) to participate in the study were auto directed to the survey form. There were no specific inclusion or exclusion criteria for the survey, except that children should be 5 years or older and up to 16 years of age. Those above 16 years of age were asked to directly fill the forms.
Survey
The survey development is summarized in an earlier study.[6] Briefly, the survey was developed from previous literature and with a closed group discussion amidst optometrists within the institute. A single survey form was developed for both children and adults. The symptoms questionnaire was developed based on convergence insufficiency symptom survey (CISS) and its scoring scale.[18] The survey had 13 questions pertaining to symptoms with five options (never, not very often, sometimes, fairly often, and always) on a Likert scale. The survey questions are given in the supplementary file.
The link to survey questionnaire (Google form) was circulated through emails and social media platforms like WhatsApp and Facebook. Participants were further encouraged to forward the survey link to their social circle (snowball or chain referral sampling technique). Participants who did not provide online consent and those with missing data were excluded. A reminder was sent two times (at 4 weeks interval) via the same media of communication. In the online survey, participants could not alter responses after submitting the questionnaire.
Data analysis
The collected responses were exported into Microsoft Excel sheet. Descriptive statistical data analysis was performed using Statistical Package for the Social Sciences (SPSS) version 20.0 (IBM, SPSS). The symptoms were scored (ranging from never = 0 to always = 4) and added up. The least total score obtainable was 0 and the maximum was 52. A descriptive analysis of all the explanatory and outcome parameters was performed. All the recorded categorical variables were presented in frequencies and percentages. The Pearson Chi-square test was used for associations. P-values ≤ 0.05 were considered significant. Likert scores can be subjected to parametric tests.[19] Hence, independent t-test was used to compare the symptoms scores between children and adults and between males and females.
Results
Demographics
A total of 435 participants viewed the online survey link and 432 participants consented for participation. The mean age ± standard deviation (SD) of the 432 participants was 26.06 ± 13.92 years. Out of the 432 participants, 53% (n = 230) were females and 71% (n = 307) were adults (>16 years). A small percentage 9% (n = 39) of participants were from outside of India. Within India, 51% of the participants were from the southern states of India and the remaining were spread across the rest of the states. Most participants either had a spectacle correction (50%, n = 218) or did not use any refractive correction (45%, n = 195). The remaining few participants either used both spectacles and contact lenses (3%, n = 11) or only contact lenses (1%, n = 4) or had a history of refractive surgery (1%, n = 4).
20/20/20 rule
Only a small proportion (8.8%, n = 38) of participants reported practicing the 20/20/20 rule. Majority (66%, n = 285) of the participants either did not know the rule or did not practice it. The remaining participants (25.2%, n = 109) reported occasionally practicing this rule. For the purpose of further analysis to look at associations, the participants were divided into two broad groups: “practicing” and “nonpracticing” groups. The practicing group comprised those who reported “yes” or “occasionally” practicing the rule (n = 147).
The overall symptoms score was not significantly different (independent t-test, t = 0.63, degrees of freedom [df] = 430, P = 0.53) between the nonpracticing (10.3 ± 8.2) and practicing (mean ± SD = 10.8 ± 8.1) groups. However, with regards to individual symptoms, a significant difference was obtained between those who complained of “burning sensation” (t = 2.58, df = 430, P = 0.01) and “headache” (t = 2.3, df = 430, P = 0.03). The percentage of participants complaining of having these symptoms was higher in the practicing group than in the nonpracticing group [Fig. 1]. There was no significant difference (P > 0.07) for the remaining symptoms between these two groups.
Figure 1.
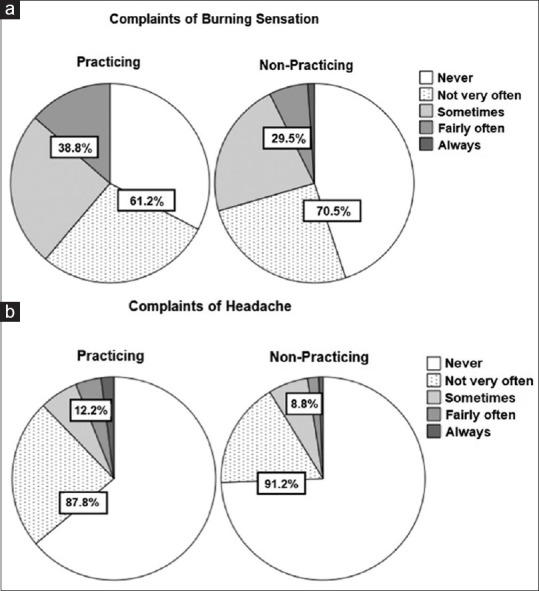
Pie chart showing the percentage of participants having symptoms of (a) burning sensation and (b) headache in the practicing and nonpracticing groups. The percentages shown in the part figures are grouped into two: one for those with “never” and “not very often” presentation and the other for the remaining frequencies of presentation of the symptoms
Upon sub-analysis, no association was found with age, that is, those practicing or nonpracticing was comparable between children and adults (Pearson Chi-square = 0.63, P = 0.43). However, a significant association (Pearson Chi-square = 19.6, P < 0.001) was found between gender and the two groups (practicing and nonpracticing), with a greater number of females practicing the rule. Further, such a gender disparity was not present in children, but was present only in adults [Fig. 2].
Figure 2.
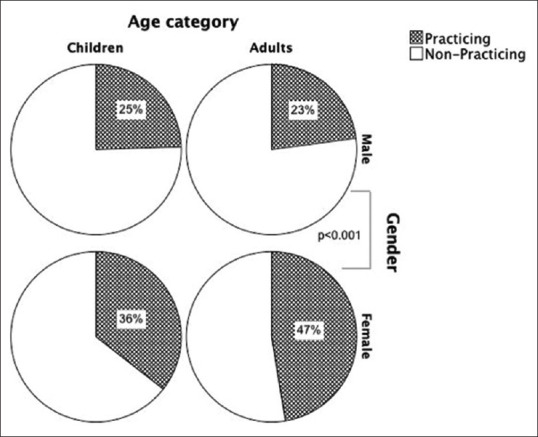
Age and gender distribution of those practicing the 20/20/20 rule and those who do not
There was no significant difference in the hours of electronic gadgets use between the practicing and nonpracticing groups (one-way analysis of variance [ANOVA], P = 0.23). Out of the 432 participants, only six participants (n = 6, 1%) used electronic gadgets for less than 1 h in a day. Most participants used electronic gadgets between 4 and 8 h (37%) or for more than 8 h (33%).
Symptoms score
The results of the survey indicated that “tiredness of eyes,” “eye strain/pain,” and “headache” were the top three symptoms reported by the participants, followed by “burning sensation.” The frequency of distribution for all the symptoms in both children and adults is given in Table 1. The additive score was calculated from the 13 symptom-based questions for each participant. The mean symptom score ±SD of all the participants was 10.4 ± 8.1. Overall, males (mean ±SD: 10 ± 8.2) and females (10.8 ± 8.1) had comparable score (t = 1.08, P = 0.28). Children had significantly (t = 5.07, P < 0.001) lower score (7.4 ± 6.3) when compared to adults (11.7 ± 8.5). Among adults, females significantly (t = 2.07, P = 0.04) had more symptoms (12.7 ± 8.2) when compared to adult males (10.7 ± 8.7). Those not having any refractive correction significantly had lower symptoms when compared to those who have or had refractive correction (9.6 vs. 11.2, t = 2.04, P = 0.04).
Table 1.
Frequency distribution of the 13 symptoms in adults and children
| Symptoms | Adults (%) | Children (%) |
|---|---|---|
| Tiredness | 81.8 | 72.8 |
| Eye strain/pain | 70.7 | 56.8 |
| Headache | 68.7 | 59.2 |
| Burning sensation | 63.8 | 48 |
| Loose concentration | 60.9 | 42.4 |
| Watering | 57.7 | 44.8 |
| Re-reading the same line or words | 55.7 | 38.4 |
| Blurred vision | 50.2 | 36 |
| Difficulty in focusing while shifting view | 49.8 | 30.4 |
| Pulling sensation | 43.3 | 22.4 |
| Nausea | 32.3 | 21.6 |
| Jumping or floating of words on the page | 27.4 | 14.4 |
| Double vision | 25.1 | 16.8 |
Discussion
This survey study showed that about one-third of participants were aware of the 20/20/20 rule and practiced it at least occasionally. It was also observed that those who are symptomatic, particularly those who have burning sensation and headache [Fig. 1], are the ones who are practicing this rule. The other most common symptoms included tiredness and eye strain/pain. All these symptoms were very similar to the results of previous studies that have investigated digital eyestrain.[11,20,21] Some of these symptoms could have resulted from dry eye as well, particularly the burning sensation. In a study that educated participants to practice the 20/20/20 rule, dry eye symptoms were found to be reduced, along with an improvement in the tear breakup time value.[20] Those participants who have headache and thus taking frequent breaks could perhaps have binocular vision dysfunctions of accommodation or vergence or both. Such an association has been described before.[22]
While in general, the symptoms scores were comparable whether the 20/20/20 rule was practiced or not, a strong gender predisposition was observed in this study, particularly for adults [Fig. 2]. Among the adult participants, significantly more females (47%) were practicing the 20/20/20 rule when compared to males (23%). Interestingly, this group (females) also had significantly more symptoms when compared to males. As a consequence of this, more females could have been more compliant to practice the 20/20/20 rule. The gender difference showing up only in adults and not in children could be indicative of hormonal differences after puberty pertaining to dry eye symptoms being more common in females than males.[23-26] Taken together, it appears that only those who are symptomatic practice this rule more commonly. Reduction of symptoms (or not) after practicing this rule still needs further investigation.
Earlier studies have shown increased symptoms during the COVID-19 time period, when compared to pre-COVID time period.[27-31] As our survey did not compare the pre- and post-COVID symptoms, it will be difficult to comment on this trend. Majority of the participants (70%) used their digital devices for 4 h or more in this study. The time spent on digital devices is comparable with the earlier findings observed during the COVID-19 lockdown, which ranged from 4 to 9 h per day.[11,20,31] Another study on digital eye strain reported the maximum hours spent on digital device to be 10 h/day,[12] and in our study, one-third of individuals were spending more than 8 h with the digital devices. We also observed that adults spend more time on digital devices compared to children. This could be due to the restricted online class duration for children, whereas the work hours for adults have no such restrictions. Children were also found to be having significantly low overall symptom score than adults (P < 0.001). It is unclear if the lower symptom score resulted from less time spent on the digital device, or if it was due to better binocular vision parameters (e.g., higher accommodative amplitude) in children, or simply because children may not observe and report symptoms as much as adults would.
There are some limitations in this study. First of all, caution needs to be applied when generalizing this study results to a larger population. Given that the survey originated and was disseminated from an eye institute, it is possible that the numbers particularly for practicing the 20/20/20 rule could be on the higher side than what can be found in the general population. Additionally, it is also not strictly documented how the 20/20/20 rule is practiced. A person may take breaks while working on digital devices, but whether they do it after every 20 min can be questionable. No clinical measurements were performed in real time in this study; therefore, the asthenopic symptoms reported cannot be fully attributed or correlated to the digital device use alone. Any underlying visual problems such as uncorrected, undercorrected, or overcorrected refractive error may also have contributed to these symptoms.[32-34] Even though a larger group of individuals can be reached through the Internet, the number of participants (sample size) was less in this study. This might be due to many online questionnaires and studies being circulated during the COVID-19 lockdown period, resulting in a possible fatigue or aversion for participation in such studies. Another important limitation is that the study used a questionnaire based on CISS that was originally developed for detecting convergence insufficiency and not for digital eyestrain. Few studies have found CISS to be less sensitive for detecting convergence insufficiency as well.[35,36] Hence, it is possible that the symptom score that was collected in this survey may not be very sensitive or specific for asthenopic symptoms due to digital device use. Nevertheless, the symptoms scores still showed some correlation to gender differences, which is in agreement to the existing literature.
Conclusion
In conclusion, only very few participants were found to be regularly practicing the 20/20/20 rule, even though majority of them are using their digital device for longer hours. The preliminary evidence from this survey shows that the symptoms scores are comparable between those who do not and do practice the 20/20/20 rule. Those who practice the 20/20/20 rule seem to do so due to symptoms of burning sensation and headache. Systematic studies will be required to evaluate how the rule is practiced and investigate the effectiveness of practicing the 20/20/20 rule, particularly in those who have binocular vision dysfunction. Future studies can also be planned to look at the correlation of the symptoms score with the measured binocular vision parameters.
Financial support and sponsorship
Hyderabad Eye Research Foundation.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Pandey N, Pal A. Impact of digital surge during Covid-19 pandemic: A viewpoint on research and practice. Int J Inf Manage. 2020;55:102171. doi: 10.1016/j.ijinfomgt.2020.102171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gewin V. Five tips for moving teaching online as COVID-19 takes hold. Nature. 2020;580:295–6. doi: 10.1038/d41586-020-00896-7. [DOI] [PubMed] [Google Scholar]
- 3.Mahmood S. Instructional strategies for online teaching in COVID-19 pandemic. Hum Behav Emerg Technol. 2021;3:199–203. [Google Scholar]
- 4.Mishra L, Gupta T, Shree A. Online teaching-learning in higher education during lockdown period of COVID-19 pandemic. Int J Educ Res Open. 2020;1:100012. doi: 10.1016/j.ijedro.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma M, Jain N, Ranganathan S, Sharma N, Honavar SG, Sharma N, et al. Tele-ophthalmology: Need of the hour. Indian J Ophthalmol. 2020;68:1328–38. doi: 10.4103/ijo.IJO_1784_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sehgal S, Bhattacharya B, Datta S, Satgunam P. Public willingness for accessing teleconsultation services for eye care. Indian J Ophthalmol. 2021;69:3772–3. doi: 10.4103/ijo.IJO_2527_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woodward MA, Ple-Plakon P, Blachley T, Musch DC, Newman-Casey PA, De Lott LB, et al. Eye care providers'attitudes towards tele-ophthalmology. Telemed J E Health. 2015;21:271–3. doi: 10.1089/tmj.2014.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sheppard AL, Wolffsohn JS. Digital eye strain: Prevalence, measurement and amelioration. BMJ Open Ophthalmol. 2018;3:e000146. doi: 10.1136/bmjophth-2018-000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coles-Brennan C, Sulley A, Young G. Management of digital eye strain. Clin Exp Optom. 2019;102:18–29. doi: 10.1111/cxo.12798. [DOI] [PubMed] [Google Scholar]
- 10.Gammoh Y. Digital eye strain and its risk factors among a university student population in Jordan: A cross-sectional study. Cureus. 2021;13:e13575. doi: 10.7759/cureus.13575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bahkir FA, Grandee SS. Impact of the COVID-19 lockdown on digital device-related ocular health. Indian J Ophthalmol. 2020;68:2378–83. doi: 10.4103/ijo.IJO_2306_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alabdulkader B. Effect of digital device use during COVID-19 on digital eye strain. Clin Exp Optom. 2021;104:698–704. doi: 10.1080/08164622.2021.1878843. [DOI] [PubMed] [Google Scholar]
- 13.Turgut B. Ocular ergonomics for the computer vision syndrome. J Eye Vis. 2018;1:1–2. [Google Scholar]
- 14.Jaha JR. Supporting Eye Health Naturally and VDU Eyecare. 2020. [[Last accessed on 2022 Dec 10]]. https://www.barnetunison.me.uk/wp/wp-content/uploads/2020/10/Eye-Health-Webinar-September-2020.pdf.
- 15.Brian Chou O. Deconstructing the 20-20-20 Rule for digital eye strain. Optom Times. 2018;10:21–3. [Google Scholar]
- 16.Hewitt B. Screen time and how it affects our eyes! [[Last accessed on 2022 Dec 10]]. https://www.eyecarefirst.com/blog/186132-screen-time-and-how-it-affects-our-eyes.
- 17.Boulet C. The '20/|s20/20 rule'–When good intentions and axiomatic habit displace best practices. Can J Optom. 2016;78:6. [Google Scholar]
- 18.Convergence Insufficiency Treatment Trial (CITT) Investigator Group. Validity of the convergence insufficiency symptom survey: A confirmatory study. Optom Vis Sci. 2009;86:357–63. doi: 10.1097/OPX.0b013e3181989252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Norman G. Likert scales, levels of measurement and the “laws” of statistics. Adv Health Sci Educ. 2010;15:625–32. doi: 10.1007/s10459-010-9222-y. [DOI] [PubMed] [Google Scholar]
- 20.Mohan A, Sen P, Shah C, Jain E, Jain S. Prevalence and risk factor assessment of digital eye strain among children using online e-learning during the COVID-19 pandemic: Digital eye strain among kids (DESK study-1) Indian J Ophthalmol. 2021;69:140–4. doi: 10.4103/ijo.IJO_2535_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shantakumari N, Eldeeb R, Sreedharan J, Gopal K. Computer use and vision. related problems among university students in Ajman, United Arab Emirate. Ann Med Health Sci Res. 2014;4:258–63. doi: 10.4103/2141-9248.129058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sheedy JE, Hayes J, Engle, Jon Is all asthenopia the same? Optom Vis Sci. 2003;80:732–9. doi: 10.1097/00006324-200311000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Tan LL, Morgan P, Cai ZQ, Straughan RA. Prevalence of and risk factors for symptomatic dry eye disease in Singapore. Clin Exp Optom. 2015;98:45–53. doi: 10.1111/cxo.12210. [DOI] [PubMed] [Google Scholar]
- 24.Matossian C, McDonald M, Donaldson KE, Nichols KK, MacIver S, Gupta PK. Dry eye disease: Consideration for women's health. J Womens Health. 2019;28:502–14. doi: 10.1089/jwh.2018.7041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136:318–26. doi: 10.1016/s0002-9394(03)00218-6. [DOI] [PubMed] [Google Scholar]
- 26.Malet F, Le Goff M, Colin J, Schweitzer C, Delyfer MN, Korobelnik JF, et al. Dry eye disease in French elderly subjects: The Alienor Study. Acta Ophthalmol. 2014;92:e429–36. doi: 10.1111/aos.12174. [DOI] [PubMed] [Google Scholar]
- 27.Hussaindeen JR, Gopalakrishnan A, Sivaraman V, Swaminathan M. Managing the myopia epidemic and digital eye strain post COVID-19 pandemic–What eye care practitioners need to know and implement? Indian J Ophthalmol. 2020;68:1710–2. doi: 10.4103/ijo.IJO_2147_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koh S, Rhee MK. COVID-19 and dry eye. EyeContact Lens. 2021;47:317–22. doi: 10.1097/ICL.0000000000000797. [DOI] [PubMed] [Google Scholar]
- 29.Saldanha IJ, Petris R, Makara M, Channa P, Akpek EK. Impact of the COVID-19 pandemic on eye strain and dry eye symptoms. Ocul Surf. 2021;22:38–46. doi: 10.1016/j.jtos.2021.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Almousa A, Aldofyan M, Kokandi B, Alsubki HE, Alqahtani RS, Gikandi P, et al. Prevalence of computer vision syndrome and patterns of electronic devices usage before and during COVID-19 pandemic among medical students in Riyadh, Saudi Arabia. Int Ophthalmol. 2022:1–9. doi: 10.1007/s10792-022-02525-w. doi: 10.1007/s10792-022-02525-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Regmi A, Suresh J, Asokan R. Changes in work patterns during COVID-19 lockdown and its impact on the eyes and body. Clinical and Experimental Optometry. 2022:1–7. doi: 10.1080/08164622.2022.2029682. doi: 10.1080/08164622.2022.2029682. [DOI] [PubMed] [Google Scholar]
- 32.Rosenfield M. Computer vision syndrome (aka digital eye strain) Optom Pract. 2016;17:1–10. [Google Scholar]
- 33.Heus P, Verbeek JH, Tikka C. Optical correction of refractive error for preventing and treating eye symptoms in computer users. Cochrane Database Syst Rev. 2018;4:CD009877. doi: 10.1002/14651858.CD009877.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gowrisankaran S, Sheedy JE. Computer vision syndrome: A review. Work. 2015;52:303–14. doi: 10.3233/WOR-152162. [DOI] [PubMed] [Google Scholar]
- 35.Horwood AM, Toor S, Riddell PM. Screening for convergence insufficiency using the CISS is not indicated in young adults. Br J Ophthalmol. 2014;98:679–83. doi: 10.1136/bjophthalmol-2013-304533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Horan LA, Ticho BH, Khammar AJ, Allen MS, Shah BA. Is the convergence insufficiency symptom survey specific for convergence insufficiency?A prospective, randomized study. Am Orthopt J. 2015;65:99–103. doi: 10.3368/aoj.65.1.99. [DOI] [PubMed] [Google Scholar]


