Abstract
Pregnancy is a time of increased vulnerability to psychopathology, yet limited work has investigated the extent to which variation in psychopathology during pregnancy is shared and unshared across syndromes and symptoms. Understanding the structure of psychopathology during pregnancy, including associations with childhood experiences, may elucidate risk and resilience factors that are transdiagnostic and/or specific to particular psychopathology phenotypes. Participants were 292 pregnant individuals assessed using multiple measures of psychopathology. Confirmatory factor analyses found evidence for a structure of psychopathology consistent with the Hierarchical Taxonomy of Psychopathology (HiTOP; Kotov et al., 2017). A common transdiagnostic factor accounted for most variation in psychopathology, and both adverse and benevolent childhood experiences (ACEs and BCEs) were associated with this transdiagnostic factor. Furthermore, pregnancy-specific anxiety symptoms most closely reflected the dimension of Fear, which may suggest shared variation with manifestations of fear that are not pregnancy-specific. ACEs and BCEs also linked to specific prenatal psychopathology involving thought problems, detachment, and internalizing, externalizing, antagonistic, and antisocial behavior. These findings extend the dimensional and hierarchical HiTOP model to pregnant individuals and show how maternal childhood risk and resilience factors relate to common and specific forms of psychopathology during pregnancy as a period of enhanced vulnerability.
Keywords: pregnancy, adverse childhood experiences (ACEs), benevolent childhood experiences (BCEs), Hierarchical Taxonomy of Psychopathology (HiTOP), resilience
Pregnancy is a sensitive period when risk for psychopathology is high (O’Hara & McCabe, 2013; Viswasam et al., 2019). Mental health symptoms and distress during pregnancy have profound implications for the mother and fetus (Davis & Narayan, 2020; Demers et al., 2021). More research is needed, however, to understand transdiagnostic and specific risk and resilience factors that have been hypothesized to affect propensity to experience psychopathology during pregnancy. Despite the importance of the topic, the preponderance of empirical work investigating vulnerability and protective factors, both within and outside of pregnancy, has focused on specific diagnoses, with the majority of attention to maternal prenatal depression and anxiety disorders as defined by the predominant Diagnostic and Statistical Manual of Mental Disorders (DSM) classification system from the American Psychiatric Association (APA), DSM-III, 1980, DSM-III-R, 1987, DSM-IV, 1994, and now DSM-5, 2013a). Numerous limitations have been identified about DSM as a categorical classification system for psychopathology (e.g., Conway et al., 2019; Kotov et al., 2017; Waszczuk et al., 2017) including especially high levels of comorbidity among putatively separate and specific diagnoses of anxiety and depression (Angold et al., 1999; Hankin et al., 2016) as well as substantial within-syndrome phenotypic heterogeneity (Feczko et al., 2019; Fried, 2015).
To improve upon these well-known shortcomings of DSM-defined disorders, alternative dimensional structures have been proposed to more accurately and parsimoniously represent common forms of psychopathology. In particular, the Hierarchical Taxonomy of Psychopathology (HiTOP) (Kotov et al., 2017) organizes psychopathology dimensionally and hierarchically. This novel conceptual model provides innovative opportunities to understand the extent to which various risk and resilience factors contribute to potentially broad-based (e.g., general psychopathology, the internalizing and externalizing spectra) and relatively specific (e.g., pregnancy-specific fear) psychopathology symptoms.
This study was designed to characterize common and specific forms of psychopathology in pregnant individuals in order to advance knowledge on risk and resilience factors that are associated with psychopathology during pregnancy, beyond the usual select focus on depression and anxiety (e.g., Hutchens & Kearney, 2020; Monk et al., 2019). We implemented a comparatively comprehensive set of measures that represent multiple forms of psychopathology in a population of pregnant individuals (N = 292) overenrolled at recruitment for elevated psychological distress. Further, we leveraged the HiTOP conceptual model to examine the relative contributions of hypothesized childhood risk and resilience factors [adverse childhood experiences (ACEs) and benevolent childhood experiences (BCEs)] to common and specific dimensional aspects of psychopathology experienced during pregnancy.
Early Risk and Resilience Factors to Psychopathology
Adverse Childhood Experiences (ACEs) are some of the most potent correlates of transdiagnostic forms psychopathology across the lifespan (Hoppen & Chalder, 2018; McLaughlin et al., 2020). ACEs are strongly linked to both internalizing and externalizing forms of psychopathology during the childbearing period (Currie & Tough, 2021; McDonald et al., 2019; Narayan et al., 2018; Olsen, 2018; Racine et al., 2020). Seminal research on mechanisms of risk and resilience following ACEs points to distinct pathways through which ACEs influence specific forms of psychopathology, as well as risk mechanisms that are transdiagnostic (McLaughlin et al., 2020; McLaughlin & Lambert, 2017; McLaughlin & Sheridan, 2016). However, prior work on risk for psychopathology during pregnancy has limited its scope to syndrome- or disorder-specific outcomes, so the hypothesis that ACEs affect both general and specific liabilities for psychopathology during pregnancy has not been tested. Furthermore, there is need to better characterize how risk and resilience factors interact to influence psychopathology during pregnancy—a particularly sensitive developmental window for mothers and their children (Davis & Narayan, 2020).
Benevolent Childhood Experiences (BCEs) are defined as experiences of support, security, and dependability during childhood, and they have been identified as a key resilience factor that promotes psychological wellbeing in adults exposed to a range of adverse experiences (Narayan et al., 2018). From the developmental psychopathology perspective, BCEs promote resilience because they reflect the presence of safe and secure interpersonal relationships and a positive and predictable quality of life, that together lay the groundwork for a healthy self-concept and positive interpersonal relationships across the lifespan (Narayan et al., 2021). In pregnant individuals, positive childhood experiences have been associated with lower levels of PTSD symptoms, less risky reproductive planning, and less exposure to prenatal stressful life events, all of which have implications for reducing the risk for intergenerational trauma (Chung et al., 2008; Merrick et al., 2020; Narayan et al., 2018). Because BCEs are thought to directly influence adaptive life outcomes regardless of risk exposure (that is, in both low- and high-risk contexts), BCEs are generally conceptualized as promotive factors (Narayan et al., 2018, 2021). However, the literature on the beneficial effects of BCEs on psychopathology in pregnant individuals is limited in ways that are similar to the research on ACEs in that most work has operationalized psychopathology outcomes unidimensionally.
The Hierarchical Taxonomy of Psychopathology (HiTOP) System
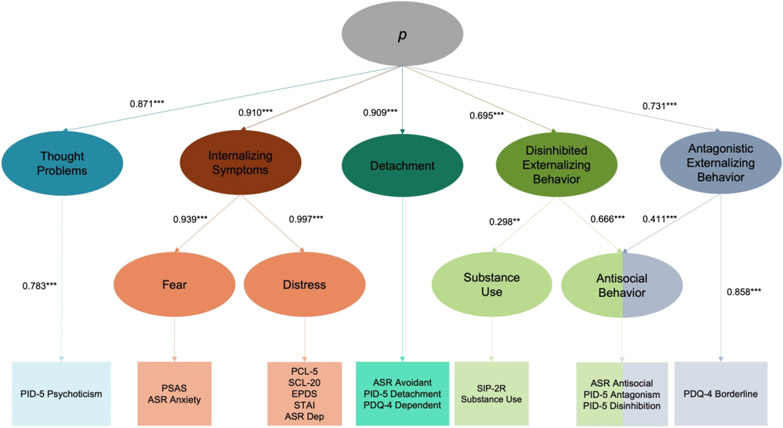
The conceptual structure of psychopathology advanced by the Hierarchical Taxonomy of Psychopathology (HiTOP) system offers a unique opportunity to address the need to more precisely understand the ways that risk and resilience factors are associated with transdiagnostic versus specific forms of psychopathology during pregnancy. The HiTOP system has the potential to parsimoniously organize psychopathology across hierarchical dimensions with greater verisimilitude than traditional psychiatric categorical approaches (DeYoung et al., 2022; Kotov et al., 2017). The HiTOP system addresses limitations of, and extends beyond, traditional syndrome- or disorder-specific psychiatric nosologies (such as the DSM-5). HiTOP aims to better capture the known co-occurrence among disorders, reduce within-disorder heterogeneity, and characterize psychiatric symptoms as dimensional (as opposed to categorical) phenomena across hierarchical levels. Figure 1 illustrates those psychopathology dimensions across hierarchies that were empirically investigated in this study.
Figure 1. Hierarchical Taxonomy of Psychopathology (HiTOP) Model Estimates.
Note. All factor loadings were standardized. **p < .01, ***p < .001. PSAS = Pregnancy-Specific Anxiety Scale; ASR = Adult Self-Report; PCL-5 = PTSD Checklist for the DSM 5; SCL-20 = Hopkins Symptom Checklist – Depression; EPDS = Edinburgh Postnatal Depression Scale; STAI = State Trait Anxiety Inventory; SIP-2R = Short Inventory of Problems; PID-5 = Personality Inventory for DSM 5 – Brief Form; PDQ-4 = Personality Disorder Questionnaire.
The HiTOP model is hierarchically organized to structure psychopathological phenomena and symptoms within coherent latent dimensions. Factors at the top of the hierarchy represent psychopathology at the broadest level (i.e., transdiagnostic liability for mental illness). This highest level of the model includes the phenotypic variability that is common to all disorders, analogous to the p factor (Caspi et al., 2014). The second tier of the hierarchy includes dimensions seeking to capture the heterogeneity across various symptoms of psychopathology into increasingly more specific domains. Below the highest-order, HiTOP proposes five primary dimensions (termed spectra), corresponding to Internalizing Symptoms, Thought Problems, Disinhibited Externalizing Behavior, Antagonistic Externalizing Behavior, and Detachment pathologies. Several subfactors—positioned below the spectra on the HiTOP hierarchy—are hypothesized to more specifically contribute to manifestation of the primary dimensions of psychopathology. In this study we focused specifically on the most predominant constituent subfactors of the Internalizing dimension (Fear and Distress), as well as the Substance Use and Antisocial Behavior subfactors that are proposed to contribute to Disinhibited Externalizing Behavior facets of psychopathology. Below the subfactors, at the fourth level of HiTOP’s hierarchy, are traditional syndromes and psychiatric disorders. The HiTOP system proposes these various disorders or syndromes contribute to their respective higher-order dimensions (either spectra or subfactors) to further reduce symptom heterogeneity and organize the presentation of myriad forms of psychopathology in a systemic, coherent structure. For example, within the broader dimension of the Internalizing Symptoms spectrum, Major Depressive Disorder/Dysthymia, Borderline Personality Disorder and Posttraumatic Stress Disorder (PTSD) are hypothesized to contribute to the lower-order Distress subfactor, whereas Social Phobia and Panic Disorder are proposed to load onto the lower-order Fear subfactor.
Empirical Support for the HiTOP Model: Missing Pieces and Next Steps
Evidence from general population and community samples lends support for the proposed hierarchical structure of individual components of the HiTOP model, indicating that aspects of psychopathology can be usefully arranged via increasing levels of granularity, and providing initial validity. Recent reviews organized around each of the spectra of higher-order latent dimensions, including externalizing behavior (Krueger et al., 2021), internalizing symptoms (Eaton et al., 2013; Snorrason et al., 2021), and thought problems and detachment dimensions (Kotov et al., 2020) are consistent with HiTOP’s hierarchical structure, and a recent meta-analysis reported a final model consistent with HiTOP’s posited model of psychopathology (Ringwald et al., 2021).
Research on the structural organization of psychopathology in pregnant populations is in its incipient phases and has primarily evaluated affective symptoms. For example, one study using data from over 20,000 pregnant women from three separate cohorts found evidence for a broad factor representing liability for affective problems, with three distinct subdimensions comprising somatic symptoms, anxiety and depression symptoms, and pregnancy-specific worries (Szekely et al., 2021). Notably, the anxiety/depression factor from Szekely et al.’s (2021) study closely resembled the HiTOP’s Distress factor, and pregnancy-specific worries were assessed using measures that captured feelings of fear or panic about being pregnant (e.g., the Pregnancy-Specific Anxiety Scale; Rini et al., 1999), consistent with the Fear dimension from the HiTOP model. This suggests that pregnancy-specific anxiety may share processes and etiological factors with Fear psychopathology that occurs outside of pregnancy.
To our knowledge, Szekely et al.’s (2021) is the only investigation of the organization of psychopathology in pregnant individuals. Additional empirical work that captures a broader range of psychopathology is needed, especially given past work suggesting differential symptom presentation and enhanced heterogeneity within traditional diagnostic categories during pregnancy relative to non-pregnant individuals (Fox et al., 2018; Gordon-Smith et al., 2020; Starcevic et al., 2020). For example, Fox et al. (2018) found qualitative differences between postpartum depression (PPD) and major depressive disorder (MDD) in pregnant individuals examined longitudinally, such that worry was more characteristic of PPD whereas anhedonia was more prominent in MDD. Fox et al. (2018) note that differing manifestations of psychopathology during and outside of pregnancy imply that different assessment and screening tools may be needed in order to optimize care for pregnant individuals in distress. Thus, there is need for empirical work to examine further the structure of psychopathology among pregnant individuals—especially in order to accurately characterize transdiagnostic and specific risk and resilience factors for psychopathology during pregnancy. Accurate characterization of psychopathology during pregnancy is critical both for the pregnant individual, and also for understanding and addressing the intergenerational transmission of risk to the offspring (Davis & Narayan, 2020).
The Present Study
The aims of the present study are threefold. First, we used confirmatory structural equation modeling (SEM) to evaluate the hierarchical structure of psychopathology as proposed via the HiTOP model in pregnant individuals. By using multiple measures of a wide and broad range of symptoms and manifestations of psychopathology, we aimed for dimensional assessment of a broader array of psychopathologies that could be used as manifest indicators in our latent variable confirmatory SEM analyses. This approach provides a more complete characterization of the structure of psychopathology among pregnant individuals than has been conducted in past work. We hypothesized that psychopathology symptoms and syndromes in pregnant individuals would be dimensionally and hierarchically organized using the structure advanced by the HiTOP system, with pregnancy-specific fear symptoms loading onto the Fear subdomain along with anxiety symptoms that were not pregnancy-specific. Figure 1 provides a graphical depiction of the structural model tested in these analyses.
Our second study aim was to examine the extent to which ACEs and BCEs were associated with general and specific forms of psychopathology as instantiated via the latent HiTOP dimensions as obtained in the first goal. For this second aim, we hypothesized that ACEs would be significantly, positively associated with transdiagnostic psychopathology constructs at the highest levels of the HiTOP structure and have weaker associations with more specific forms of psychopathology (i.e., subfactors at lower levels of the HiTOP hierarchy). Prior research supports this hypothesized pattern of results, as risk for specific syndromes or disorders is explained by variation among disorders that is shared rather than specific (for review, see Conway et al., 2019). Given that higher levels of BCEs have been found to associate with lower levels of various types of psychopathology (e.g., depression, PTSD) that may share transdiagnostic elements, we hypothesized that BCEs would have negative and significant associations with transdiagnostic psychopathology factors, with weaker links to psychopathology subdomains at lower levels of the HiTOP structure.
Finally, we aimed to examine relations between BCEs and psychopathology during pregnancy, in the context of ACEs. Both ACEs and BCEs were tested together in association with the general and specific HiTOP dimensions to investigate the potential of BCEs to promote lower prenatal psychopathology. Consistent with prior work showing that BCEs have a promotive or direct effect on outcomes (Narayan et al., 2018; Nevarez-Brewster et al., 2022), we expected that ACEs and BCEs would each account for variance in psychopathology during pregnancy. In other words, we expected evidence for BCEs as a promotive factor for psychopathology during pregnancy, beyond participants’ reported ACEs.
Method
Participants
Participants (N = 292) were drawn from the Care Project, which took place in Denver, Colorado, and surrounding communities (Davis et al., 2018). Participants were eligible for the study if they were English-speaking, 18-45 years of age (M = 30.0, SD = 5.8), carrying a singleton intrauterine pregnancy, and 25 weeks gestational age or less. Participants’ average gestational age at assessment was 16.9 weeks (SD = 4.4). Participants were socioeconomically diverse; median annual income was US$55,000.0 (M = US$71,019.8, SD = US$57,996.5). Income-to-needs ratio (INR) was calculated by dividing participants’ household income by the federal poverty level (United States Census Bureau, 2021) in the corresponding year. The median INR was 2.7 (M = 3.6, SD = 3.2), with 38.2% of participants having low (less than 200%) INR (Luby et al., 2013). Participants’ highest reported level of education ranged from some high school to graduate degree. 48.3% of participants identified as non-Hispanic White, 14.7% as Black, African American, or Haitian, 5.1% as Asian, 1.0% as Native Hawaiian or Pacific Islander, 7.2% as American Indian or Alaska Native, and 5.8% identified with more than one race. Approximately one in four (26.6%) participants endorsed a Hispanic/Latinx ethnicity; among these, 65.0% identified as White, 2.5% as Black, African American, or Haitian, 23.8% as American Indian or Alaska Native, and 8.8% as more than one race. Participants were overenrolled for distress (10 or higher on the EPDS administered as part of routine obstetric screening, see below), with 193 (70%) reporting elevated distress when recruited. Participants were excluded from the study if they reported psychosis, mania, or current use of illicit drugs or methadone.
Procedure
After providing informed consent, pregnant individuals meeting eligibility criteria completed a battery of self-report measures, described below. All measures and procedures were approved by the University Institutional Review Board and participants provided written and informed consent.
Measures
Thought Problems.
The Personality Inventory for DSM 5 – Brief Form (PID-5-BF; described below) (American Psychiatric Association (APA), 2013b; Krueger et al., 2012) was administered at a baseline assessment to capture the Thought Problems dimension (see Figure 1).
Personality Inventory for DSM 5 – Brief Form (PID-5-BF).
The PID-5-BF (American Psychiatric Association (APA), 2013b; Krueger et al., 2012) is a 25-item instrument that measures the facets of a dimensional structural model of personality pathology proposed for consideration in the DSM-5, including Antagonism, Detachment, Disinhibition, and Psychoticism. Respondents rate the extent to which each item describes their personality on a scale ranging from 0-3, with higher scores indicating more severe pathology. Example items include: “My thoughts often don’t make sense to others.” Five items comprise each subscale, and total scores for each subscale are calculated by summing the scores of corresponding items (with possible subscale scores ranging from 0 to 15). The Psychoticism subscale of the PID-5-BF was used to characterize the Thought Problems dimension. The psychometric properties of the PID-5-BF are well supported (Anderson et al., 2018; Gomez et al., 2020). Internal consistency of the PID Psychoticism subscale used in the present study was Cronbach’s α = .75 (Psychoticism).
Internalizing Symptoms.
The following instruments were administered at a baseline assessment to capture the Fear and Distress dimensions of Internalizing Symptoms (see Figure 1):
Fear.
The Pregnancy-Specific Anxiety Scale (PSAS) (Rini et al., 1999) and Anxiety Problems subscale of the Adult Self-Report (ASR) (Achenbach & Rescorla, 2003) were used to capture symptoms and syndromes along the Fear subdomain of the Internalizing Symptoms spectrum. The PSAS is a ten-item measure of fears and worries unique to pregnancy (e.g., “I am concerned or worried about losing my baby”). Items are rated on a scale ranging from 1-4 and summed to create a total score ranging from 10-40, with higher scores indicating greater pregnancy-specific anxiety. Other work using the PSAS has supported its reliability and validity (Buss et al., 2011; Rini et al., 1999), and internal consistency of the measure in this study was Cronbach’s α = .86. The ASR, part of the Achenbach System of Empirically Based Assessment (ASEBA), comprises 126 items across six DSM-5-oriented scales that assess broadband functioning. DSM-oriented scales for this study included Antisocial Personality Problems, Anxiety Problems, Avoidant Personality Problems, and Depressive Problems; the Anxiety Problems subscale was loaded onto the Fear subdomain of our model. Items on the ASR evaluate functioning over the past 6 months, and respondents are asked to rate the extent to which each item applies on a scale from 0 to 2. Subscale scores are generated by summing responses to each item on the subscale, with higher scores indicating greater severity. The ASR is widely used in research and its psychometric properties are strong (de Vries et al., 2020; Guerrero et al., 2020). The internal consistency of the ASR Anxiety Problems subscale was Cronbach’s α = .84.
Distress.
To assess the Distress subdomain of the Internalizing Symptoms spectrum of psychopathology in our study, we administered the following measures: PTSD Checklist for DSM 5 (PCL-5) (Weathers et al., 2013b), Symptom Checklist (SCL-20) (Derogatis et al., 1974), Edinburgh Postnatal Depression Scale (EPDS) (Cox et al., 1987), State Trait Anxiety Inventory (STAI) (Spielberger et al., 1970), and the Depressive Problems subscale from the ASR (Achenbach & Rescorla, 2003). Inclusion of the STAI within the Distress subdomain of Internalizing Symptoms was informed by prior literature indicating that items on the STAI predominantly tap into general distress, consistent with generalized anxiety, which involves pervasive negative emotionality (Watson et al., 2017). Additionally, the STAI associates and covaries more strongly with other distress disorders (e.g., PTSD and depressive disorders) than it does with other, fear-based forms of anxiety (Kotov et al., 2017; Watson et al., 2022).
The 20 items of the PCL-5 (Weathers et al., 2013b) evaluate symptoms of Posttraumatic Stress Disorder (PTSD) and correspond to symptoms of PTSD as characterized by the DSM-5 (American Psychiatric Association (APA), 2013a). Items are rated on a scale from 0-4, with possible total scores ranging from 0 to 80 and higher scores suggesting greater severity of posttraumatic stress. The psychometric properties of the PCL-5 are well established across diverse populations (Gelaye et al., 2017; Wortmann et al., 2016). The reliability of the measure in the present study was excellent, Cronbach’s α = .95.
The SCL-20 includes the 20 items of the Symptom Checklist-90-R (Derogatis et al., 1974) that measure depressive symptoms. Items are rated on a scale from 0 to 4, with higher ratings indicating greater symptom severity. Ratings on each item are averaged to generate a total score, with possible scores ranging from 0 to 4 and higher scores indicating higher levels of depressive symptoms. Prior work points to the strong reliability and validity of the SCL-20 (Williams et al., 2004), and internal consistency of the measure in the present study was excellent, Cronbach’s α = .93.
The EPDS (Cox et al., 1987) is used to screen for perinatal depression. Its ten items index depressive symptoms over the past week, with severity ratings ranging from 0 to 3 and possible total scores ranging from 0 to 30. The EPDS is a ubiquitous and well-established measure of perinatal depression, and its psychometric properties are strong (Dennis, 2004; Murray & Carothers, 1990). The internal consistency of the EPDS in this study was reliable, Cronbach’s α = .89.
The 20-item STAI (Spielberger et al., 1970) was used to assess participants’ general distress and generalized anxiety symptoms. Items on the STAI are rated on a scale from 1 to 4 and summed to generate a total score ranging from 20 to 80, with higher ratings indicating more severe general distress and broad anxiety concerns. Extant evidence points to the validity and reliability of the STAI in capturing general distress and broad anxiety symptoms during the perinatal period (Gunning et al., 2010; Tendais et al., 2014). The STAI had excellent internal consistency reliability in this study, Cronbach’s α = .96.
Finally, the Depressive Problems subscale of the ASR (Achenbach & Rescorla, 2003; described above) had strong internal consistency in this study (Cronbach’s α = .88), and prior factor analytic research supports its construct validity (Guerrero et al., 2020).
Detachment.
To capture the Detachment dimension (see Figure 1), the Avoidant Problems subscale of the ASR (Achenbach & Rescorla, 2003; described above) and the Detachment subscale of the PID-5-BF (APA, 2013b; Krueger et al., 2012; described above) were used. Internal consistency for the ASR Avoidant Problems subscale was Cronbach’s α = .80, and it was .73 for the Detachment subscale of the PID-5-BF.
Additionally, participants responded to items on the Personality Disorder Questionnaire (PDQ-4) (Hyler, 1994). The PDQ-4 includes 99 true-false items that assess personality pathology as characterized by the Diagnostic and Statistical Manual of Mental Disorders (4th ed.,; DSM-IV; American Psychiatric Association (APA), 1994). Each item corresponds to one of the ten Personality Disorder (PD) diagnoses from the DSM-IV, and items for each diagnosis are summed to indicate PD symptom severity. Only items corresponding to symptoms of Borderline PD and Dependent PD were administered in the present study, and the Dependent PD subscale was loaded onto the Detachment spectrum. The internal consistency of the Dependent PDQ-4 subscales was moderate, Cronbach’s α = .63.
Disinhibited Externalizing Behavior.
The following instruments were administered to capture the Substance Use and Antisocial Behavior subdomains of the Disinhibited Externalizing Behavior dimension (see Figure 1):
Substance Use.
The 15 items of the Short Inventory of Problems (SIP-2R) (Miller et al., 1995) were administered to evaluate alcohol use and associated problems over the past 3 months. Each item is rated on a scale from 0 to 3, with higher scores indicating more frequent experiences with alcohol-related problems. Example items include: “I have been unhappy because of my drinking,” and, “I have had money problems because of my drinking.” The SIP-2R has strong reliability and validity (Kiluk et al., 2013). Cronbach’s α for the SIP-2R in this study was .90. Participants also responded to a Substance Use Questionnaire developed for this study in which they were asked whether they had ever tried any of the following illicit substances: marijuana, inhalants, and other substances not mentioned. Participants’ responses to the substance use questions were summed to generate a substance use score indicating the total number of illicit substances used at least once.
Antisocial Behavior.
Several measures were administered to assess participants’ antisocial behavior, including the Antisocial Personality Problems subscale of the ASR (Achenbach & Rescorla, 2003; described above), and the Antagonism and Disinhibition subscales of the PID-5-BF (APA, 2013b; Krueger et al., 2012; described above). Internal consistency for these subscales was: ASR Antisocial Personality Problems Cronbach’s α = .72; PID-5 Antagonism Cronbach’s α = .78; PID-5 Disinhibition Cronbach’s α = .70.
Antagonistic Externalizing Behavior.
Consistent with the HiTOP conceptual structure, the Antisocial Behavior subdomain described above was loaded onto both the Antagonistic and Disinhibited Externalizing Behavior dimensions (see Figure 1). Additionally, the Borderline PD subscale of the PDQ-4 (Hyler, 1994; described above) was used to capture Borderline PD symptoms that, together with the Antisocial Behavior subdomain, contribute to Antagonistic Externalizing Behaviors. The Borderline PD subscale of the PDQ-4 had moderate internal consistency, Cronbach’s α = .67.
Maternal Childhood Experiences: Risk and Resilience Factors
Adverse Childhood Experiences (ACEs).
Ten dichotomous (1 = yes, 0 = no) ACEs items were administered to assess adversity prior to age 18 (Felitti et al., 1998). ACEs items included five reflecting pregnant individuals’ childhood maltreatment (emotional/verbal, physical, and sexual abuse; and emotional and physical neglect) and five reflecting individuals’ exposure to family/household dysfunction (parental separation/divorce and domestic violence, and parental/family member substance use, mental illness, and incarceration). Total ACEs scores were generated by summing responses to all ten items, with higher scores suggesting greater cumulative stress in childhood (M = 2.64, SD = 2.35, range = 0 – 10).
Benevolent Childhood Experiences (BCEs).
To assess positive childhood experiences prior to age 18, participants indicated whether they had experienced any of 10 BCEs from the Benevolent Childhood Experiences scale (Narayan et al., 2018), such as supportive caregivers and teachers, a positive self-concept, predictable home routines, and other childhood assets and resources. Response categories were dichotomous (1 = yes, 0 = no) and total BCE scores were generated by summing responses to all ten items (M = 8.58, SD = 1.93, range = 1 – 10). Higher total scores were indicative of greater numbers of favorable experiences and resources during childhood. Prior work with the BCEs scale points to its strong psychometric properties (Narayan et al., 2018).
Covariates.
Participants reported on contemporaneous negative life events (NLEs) that occurred during pregnancy. NLEs were assessed and included as a covariate in order to assess the extent to which early childhood experiences related to psychopathology during pregnancy, beyond current life events.
Negative life events (NLEs) during pregnancy.
The Life Events Checklist (LEC) (Weathers et al., 2013a) comprises 17 potentially traumatic events that meet Criterion A for the diagnosis of PTSD as conceptualized in the DSM-5. Example events include: “Exposure to a toxic substance” and, “Sudden accidental death,” and response categories are: “Happened to me,” “Witnessed it,” “Learned about it,” “Part of my job,” “Not sure,” and, “Doesn’t apply.” Responses were coded dichotomously, with all responses except “Not sure” and “Doesn’t apply” receiving a score of 1, and “Not sure” and “Doesn’t apply” receiving a 0. Total LEC scores were calculated by summing responses to all items, with possible scores ranging from 0 to 17 and higher scores indicating greater cumulative exposure to potentially traumatic events. Participants were asked to respond to the LEC with reference to events that occurred during their pregnancy, and this summary score was used to operationalize NLEs during pregnancy in this study (M = 0.83, SD = 2.45, range = 0 – 17).
Gestational age.
Participants’ gestational age (in weeks) at the time of assessment was included as an auxiliary variable in all analyses. Gestational age was determined using guidelines from the American College of Obstetricians and Gynecologists (2009); specifically, via medical records that included date of last menstrual period and early obstetric ultrasonographic biometry.
Analytic Strategy
Prior to data analysis, the analytic strategy and hypothesized relations between ACEs, BCEs, and latent psychopathology constructs were pre-registered to the Open Science Framework (osf.io/2mb5h).
Missing Data.
Data were complete for all 292 participants on the EPDS and STAI; the proportion of data missing on other manifest indicators in the HiTOP model ranged from 1.0% (ASR Depressive Problems) to 8.2% (SCL-20). Data (i.e., participants’ responses to all measures of interest in the study) were examined for missingness using Little’s missing completely at random (MCAR) test, which indicated that data were not MCAR (X2(165) = 230.36, p = .001). Missing data patterns were explored in relation to participants’ sociodemographic characteristics (e.g., age, race, ethnicity, income, highest level of education) as well as gestational age. Exploration of missing data patterns supported the assumption that data were missing at random (MAR), as missingness on all variables of interest was associated with participants’ gestational age (all ps < .001). Accordingly, missing data were addressed via full information maximum likelihood (FIML) estimation, including gestational age as an auxiliary variable in the structural equation models (Graham, 2003).
Latent Structural Models of Psychopathology.
Using structural equation modeling in Mplus Version 8 (Muthén & Muthén, 2017), a series of measurement models were tested to evaluate the structure of psychopathology. Given prior work that has called into question the benefits of hierarchically structured models of psychopathology compared to general psychopathology and correlated-factors models (Watts et al., 2019), we tested increasingly specific structural models and compared fit indices (e.g., CFI, TLI, RMSEA, SRMR) to determine the best-fitting model.
First, we tested a general psychopathology model, where all manifest indicators loaded on to a single latent factor. Next, we specified a correlated two-factor model that included internalizing and externalizing dimensions, as well as a correlated five-factor model that included all of the higher-order HiTOP spectra (Thought Problems, Internalizing Symptoms, Detachment, Disinhibited Externalizing Behavior, and Antagonistic Externalizing Behavior; see Supplemental Figure S1). Finally, a latent hierarchical (HiTOP) model was constructed that included a common higher-order (p) factor; specific Internalizing Symptoms, Disinhibited Externalizing Behavior, Antagonistic Externalizing Behavior, Detachment, and Thought Problems factors; specific Fear and Distress factors common to the Internalizing factor; and specific Antisocial Behavior and Substance Use factors common to the Disinhibited Externalizing Behavior factor. Consistent with the HiTOP model, the Antisocial Behavior factor also loaded onto the Antagonistic Externalizing factor, along with the manifest indicator of Borderline PD. Orthogonality of higher-order factors was achieved by constraining correlations between factors to 0. Table 1 provides a list of manifest indicators for each factor in the latent HiTOP model.
Table 1.
Manifest Indicators and Descriptive Statistics for Latent Factors of Psychopathology
| Factor | Indicators | Range | Mean (SD) |
|---|---|---|---|
| Fear | PSAS | 10 – 39 | 20.53 (5.97) |
| ASR Anxiety Problems Subscale | 0 – 14 | 5.68 (3.97) | |
| Distress | PCL-5 | 0 – 72 | 18.97 (16.80) |
| SCL-20 | 0 – 4 | 1.14 (0.77) | |
| EPDS | 0 – 26 | 9.41 (5.96) | |
| STAI | 20 – 80 | 42.98 (14.45) | |
| ASR Depressive Problems Subscale | 0 – 24 | 7.24 (5.37) | |
| Substance Use | SIP-2R | 0 – 15 | 0.32 (1.54) |
| Substance Use Questionnaire | 0 – 3 | 0.96 (0.59) | |
| Antisocial Behavior | ASR Antisocial Problems Subscale | 0 – 13 | 3.34 (3.20) |
| PID-5 Antagonism Subscale | 0 – 8 | 1.23 (1.53) | |
| PID-5 Disinhibition Subscale | 0 – 11 | 2.08 (2.33) | |
| Thought Problems | PID-5 Psychoticism Subscale | 0 – 12 | 2.18 (2.62) |
| Detachment | ASR Avoidant Problems Subscale | 0 – 12 | 3.92 (2.96) |
| PID-5 Detachment Subscale | 0 – 11 | 3.70 (3.03) | |
| PDQ-4 Dependent PD Subscale | 0 – 3 | 0.62 (0.91) | |
| Antagonistic Externalizing Behavior | PDQ-4 Borderline PD Subscale | 0 – 7 | 1.67 (1.69) |
| Adverse Childhood Experiences | ACEs | 0 – 10 | 2.64 (2.35) |
| Benevolent Childhood Experiences | BCEs | 1 – 10 | 8.58 (1.93) |
| Negative Life Events | LEC | 0 – 17 | 0.83 (2.45) |
Note. N = 292. PSAS = Pregnancy-Specific Anxiety Scale; ASR = Adult Self-Report; PCL-5 = PTSD Checklist for the DSM 5; SCL-20 = Hopkins Symptom Checklist – Depression; EPDS = Edinburgh Postnatal Depression Scale; STAI = State Trait Anxiety Inventory; SIP-2R = Short Inventory of Problems; PID-5 = Personality Inventory for DSM 5 – Brief Form; PDQ-4 = Personality Disorder Questionnaire; SD = Standard Deviation.
The HiTOP model was refined according to recommendations outlined by Mueller and Hancock (2008), provided that the resulting model was justified theoretically and methodologically. Specifically, modification indices were examined to ascertain sources of model misspecification and indicator residual variance correlations were included (from largest to smallest modification index value) until the fit of the model was acceptable, so long as these correlations were consistent with a theoretically and methodologically sound model. Goodness of model fit was evaluated across multiple indices according to Hu and Bentler's (1999) criteria (i.e., TLI and CFI close to .95, SRMR close to .08, and RMSEA close to .06). Convergence across fit indices was prioritized for judgments of goodness of fit, rather than relying on any single measure of model fit (Barrett, 2007).
Linking Risk and Resilience Factors to HiTOP Dimensions.
To examine the extent to which ACEs were associated with psychopathology dimensions across the HiTOP hierarchy during pregnancy, the latent dimensions of psychopathology in the HiTOP model were regressed onto participants’ self-reported ACEs. A similar model was run to test the extent to which BCEs were associated with broad and specific forms of psychopathology. Next, models were run regressing the HiTOP dimensions onto early risk and resilience factors (ACEs and BCEs) and NLEs to examine the extent to which early childhood experiences, beyond current life events, related to psychopathology during pregnancy. Finally, latent HiTOP factors were regressed onto both ACEs and BCEs to assess the promotive role of BCEs in the context of ACEs in relation to dimensions of psychopathology.
Power Analysis.
To evaluate power to detect the relations among ACEs, BCEs, and psychopathology, a series of Monte Carlo simulations were run using parameters estimated in prior research (Muthén & Muthén, 2002). Extant work on the direct effects of ACEs and BCEs on psychopathology outcomes suggests standardized regression coefficients ranging from −0.15 to −0.35 for BCEs and 0.25 to 0.32 for ACEs, with moderate correlations between ACEs and BCEs (Merrick et al., 2019; Narayan et al., 2018). In our Monte Carlo simulations, we conservatively estimated residual variance for our common p factor at 0.75, standardized regression coefficients of −0.20 and 0.30 for BCEs and ACEs, respectively, and BCEs and ACEs moderately correlated at r = −0.40. Regarding the direct relations between ACEs and psychopathology in the context of recent NLEs, our estimates of standardized regression coefficients were 0.20 and 0.25 for NLEs and ACEs, respectively; ACEs and NLEs were estimated to be moderately correlated at 0.25, and residual variance was set to 0.70 (Albott et al., 2018; Nurius et al., 2015). With a sample size of 292, results across 500 simulations estimated 94% power to detect an effect for BCEs and 99% power to detect an effect for ACEs.
Results
Summary Statistics
Descriptive statistics and correlations among manifest variables are reported in Tables 1 and 2. Most manifest indicators were positively correlated and moderate to strong in magnitude; the SIP-2R (used to evaluate alcohol use as a part of the Substance Use subdomain of Disinhibited Externalizing Behavior) had the weakest associations with other measures of psychopathology and adversity in the present study.
Table 2.
Correlations between Manifest Indicators of Psychopathology and Risk and Resilience Factors
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | 17. | 18. | 19. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. PSAS | |||||||||||||||||||
| 2. ASR Anx | .508*** | ||||||||||||||||||
| 3. PCL-5 | .286*** | .554*** | |||||||||||||||||
| 4. SCL-20 | .373*** | .644*** | .713*** | ||||||||||||||||
| 5. EPDS | .371*** | .656*** | .612*** | .836*** | |||||||||||||||
| 6. STAI | .394*** | .727*** | .651*** | .778*** | .802*** | ||||||||||||||
| 7. ASR Dep | .460*** | .743*** | .604*** | .767*** | .735*** | .715*** | |||||||||||||
| 8. SIP-2R | .043 | .103 | .378 | .066 | .474 | .137* | .089 | ||||||||||||
| 9. Substance Use | .046 | .239*** | .198** | .179** | .260*** | .273*** | .189** | .188** | |||||||||||
| 10. ASR APD | .214*** | .548*** | .541*** | .522*** | .504*** | .539*** | .571*** | .196** | .319*** | ||||||||||
| 11. PID-5 Antag | .102 | .227*** | .170** | .179** | .184** | .221*** | .228*** | .095 | .048 | .404*** | |||||||||
| 12. PID-5 Disinh | .188** | .253*** | .356*** | .358*** | .318*** | .352*** | .376*** | .137* | .208*** | .472*** | .403*** | ||||||||
| 13. PID-5 Psych | .196*** | .442*** | .539*** | .539*** | .469*** | .475*** | .557*** | .143* | .176** | .526*** | .310*** | .573*** | |||||||
| 14. ASR Avoid | .399*** | .674*** | .539*** | .613*** | .506*** | .559*** | .729*** | −.007 | .174** | .539*** | .247*** | .352*** | .541*** | ||||||
| 15. PID-5 Det | .315*** | .557*** | .561*** | .628*** | .606*** | .579*** | .647*** | .055 | .140* | .554*** | .290*** | .484*** | .602*** | .625*** | |||||
| 16. PDQ-4 Dep | .218*** | .433*** | .312*** | .393*** | .328*** | .367*** | .448*** | −.023 | .063 | .241*** | .134* | .173** | .271*** | .435*** | .279*** | ||||
| 17. PDQ-4 BPD | .210*** | .479*** | .483*** | .439*** | .457*** | .478*** | .514*** | .198*** | .272*** | .623*** | .269*** | .449*** | .527*** | .458*** | .504*** | .350*** | |||
| 18. ACEs | .094 | .228*** | .380*** | .308*** | .241*** | .292*** | .223*** | .051 | .165* | .399*** | .175** | .215*** | .320*** | .249*** | .315*** | .131* | .400*** | ||
| 19. Recent NLEs | .084 | −.017 | .123 | .076 | .016 | .038* | −.026 | −.030 | .165* | .028 | −.012 | −.023 | −.007 | −.051 | −.113 | −.033 | −.016 | −.010 | |
| 20. BCEs | −.080 | −.179** | −.202** | −.194** | −.123 | −.186** | −.173* | −.007 | −.209** | −.282*** | −.196** | −.108 | −.209** | −.255*** | −.218** | −.001 | −.142* | −.315*** | .014 |
Note.
p < .05
p < .01
p < .001. PSAS = Pregnancy-Specific Anxiety Scale; ASR = Adult Self-Report; ASR Anx = ASR Anxiety Problems subscale; PCL-5 = PTSD Checklist for the DSM 5; SCL-20 = Hopkins Symptom Checklist – Depression; EPDS = Edinburgh Postnatal Depression Scale; STAI = State Trait Anxiety Inventory; ASR Dep = ASR Depressive Problems subscale; SIP-2R = Short Inventory of Problems; ASR APD = ASR Antisocial Problems subscale; PID-5 = Personality Inventory for DSM 5 – Brief Form; PID-5 Antag = PID-5-BF Antagonism subscale; PID-5 Disinh = PID-5-BF Disinhibition subscale; PID-5 Psych = PID-5 Psychoticism subscale; ASR Avoid = ASR Avoidant Problems subscale; PID-5 Det = PID-5-BF Detachment subscale; PDQ-4 = Personality Disorder Questionnaire; PDQ-4 Dep = PDQ-4 Dependent PD subscale; BPD = PDQ-4 Borderline PD subscale; ACEs = Adverse Childhood Experiences. NLEs = Negative Life Experiences. BCEs = Benevolent Childhood Experiences.
Latent Structural Models of Psychopathology
The general psychopathology model, the correlated two-factor model, and the correlated five-factor model were all poor fits for the data. Specifically, the general psychopathology model X2(120, N = 292) = 592.36, p < .0001; AIC = 20,081.72; BIC = 20,323.56; RMSEA = 0.120 (90% CI = 0.111 – 0.130); CFI = 0.825; TLI = 0.776; SRMR = 0.086. Fit indices for the correlated two- factor model were: X2(120, N = 292) = 518.28, p < .0001; AIC = 20,007.65; BIC = 20,249.48; RMSEA = 0.110 (90% CI = 0.101 – 0.120); CFI = 0.852; TLI = 0.811; SRMR = 0.107. The correlated five-factor model X2(111, N = 292) = 475.39, p < .0001; AIC = 19,982.75; BIC = 20,257.07; RMSEA = 0.110 (90% CI = 0.100 – 0.120); CFI = 0.865; TLI = 0.813; SRMR = 0.122.
Fit indices for the initial HiTOP model were superior to those of the general psychopathology and correlated factors models, but indicated that it would benefit from refinement [X2(116, N = 292) = 418.94, p < .0001; AIC = 19,916.31; BIC = 20,172.58; RMSEA = 0.098 (90% CI = 0.088 – 0.108); CFI = 0.888; TLI = 0.852; SRMR = 0.062]. Modification indices suggested correlating the residual variance of manifest indicators derived from the same measure (i.e., indicators derived from the ASR, the PID, and the PDQ) as well as indicators belonging to the same higher-order construct (i.e., within-construct correlations for manifest indicators of Fear, Distress, Detachment, Substance Use, and Antisocial Behavior). Model fit improved with the addition of these specifications [X2(86, N = 292) = 175.94, p < .0001; AIC = 19,733.30; BIC = 20,097.86; RMSEA = 0.062 (90% CI = 0.049 – 0.075); CFI = 0.967; TLI = 0.941; SRMR = 0.035]. Because the correlation of residual variance for manifest indicators from the same measure and from measures of the same construct was theoretically sound and supported by psychometric research (Brown, 2006; Kenny, 2011; Mueller & Hancock, 2008), this model was retained for analyses examining ACEs and BCEs as common and specific risk and resilience factors.
Table 3 summarizes the standardized manifest indicator loadings onto latent factors in the HiTOP model. All indicator loadings were positive and significant (ps < .005) and ranged from 0.358 (PID-5 Antagonism Subscale) to 0.942 (ASR Antisocial Problems Subscale). Higher-order factor loadings were also all positive and significant (ps < .005), ranging in magnitude from 0.298 (Substance Use onto Disinhibited Externalizing Behavior) to 0.997 (Distress onto the Internalizing Symptoms factor). The Internalizing Symptoms factor loaded most strongly onto the transdiagnostic p factor (β = 0.910), and Disinhibited Externalizing Behavior was the least strongly associated with the p factor among the higher-order dimensions (β = 0.695).
Table 3.
Standardized Factor Loading, Intercept, and Variance for Manifest Indicators in the Latent HiTOP Model
| Factor | Indicators | Loading (SE) | Intercept (SE) | Variance (SE) |
|---|---|---|---|---|
| Fear | PSAS | 0.488 (0.046) | 3.832 (0.271) | 0.751 (0.046) |
| ASR Anxiety Problems Subscale | 0.869 (0.027) | 1.615 (0.249) | 0.245 (0.048) | |
| Distress | PCL-5 | 0.758 (0.037) | 0.853 (0.246) | 0.422 (0.056) |
| SCL-20 | 0.844 (0.029) | 1.306 (0.245) | 0.286 (0.048) | |
| EPDS | 0.812 (0.032) | 1.276 (0.246) | 0.335 (0.051) | |
| STAI | 0.864 (0.027) | 2.925 (0.270) | 0.254 (0.047) | |
| ASR Depressive Subscale | 0.929 (0.029) | 1.047 (0.246) | 0.130 (0.053) | |
| Substance Use | SIP-2R | 0.665 (0.032) | 0.394 (0.242) | 0.555 (0.042) |
| Substance Use Questionnaire | 0.668 (0.252) | 1.691 (0.257) | 0.831 (0.079) | |
| Antisocial Behavior | ASR Antisocial Subscale | 0.942 (0.051) | 0.546 (0.243) | 0.093 (0.094) |
| PID-5 Antagonism Subscale | 0.358 (0.071) | 0.178 (0.240) | 0.843 (0.054) | |
| PID-5 Disinhibition Subscale | 0.615 (0.062) | 0.339 (0.242) | 0.599 (0.076) | |
| Thought Problems | PID-5 Psychoticism Subscale | 0.783 (0.032) | 0.240 (0.239) | 0.360 (0.049) |
| Detachment | ASR Avoidant Subscale | 0.815 (0.030) | 0.835 (0.247) | 0.318 (0.047) |
| PID-5 Detachment Subscale | 0.847 (0.034) | 0.791 (0.246) | 0.271 (0.056) | |
| PDQ-4 Dependent PD Subscale | 0.484 (0.059) | 0.418 (0.244) | 0.761 (0.057) | |
| Antagonistic Externalizing Behavior | PDQ-4 Borderline PD Subscale | 0.858 (0.029) | 0.479 (0.243) | 0.245 (0.049) |
Note. All factor loadings were significant, p < .001, except the Substance Use Questionnaire, p = .004. PSAS = Pregnancy-Specific Anxiety Scale; ASR = Adult Self-Report; PCL-5 = PTSD Checklist for the DSM 5; SCL-20 = Hopkins Symptom Checklist – Depression; EPDS = Edinburgh Postnatal Depression Scale; STAI = State Trait Anxiety Inventory; SIP-2R = Short Inventory of Problems; PID-5 = Personality Inventory for DSM 5 – Brief Form; PDQ-4 = Personality Disorder Questionnaire; SE = Standard Error.
Figure 1 depicts the latent HiTOP model and higher-order factor loadings. Of note, the Fear subfactor included manifest indicators of fear that were both specific (PSAS) and nonspecific to pregnancy (ASR Anxiety Problems subscale). The fit of our confirmatory model using this specification suggests that the components of the Fear subfactor shared variation regardless of whether these fear and anxiety symptoms were specific to pregnancy.
To further probe the properties of the latent HiTOP model, a series of statistical indices were computed (Rodriguez et al., 2016). First, construct replicability (H) was calculated for each latent factor, and results indicated that most psychopathology dimensions were well defined using established criteria (Hancock & Mueller, 2001). However, low H values for the Substance Use (H = 0.472) and Thought Problems factors (H = 0.613) suggest that these constructs as measured in the present study may be less reliable, likely due to reliance on fewer manifest indicators (See Table 4). Similarly, factor determinacy (FD) scores for the latent psychopathology dimensions indicated strong correlations between factors and factor scores, apart from Substance Use (FD = 0.682). The manifest indicators for the Substance Use factor had relatively low factor loadings, and the latent construct explained a low proportion of the variance in manifest scores (R2 = .089). The Disinhibited and Antagonistic Externalizing Behavior dimensions had moderate R2 values (.483 and .535, respectively), whereas the variance explained by higher-order factors on all other psychopathology dimensions was high [ranging from .759 (Thought Problems) to .993 (Distress)]. Omega (ω) estimates for each latent construct indicated generally acceptable reliability, although Disinhibited Externalizing Behavior ω = .474 and the Substance Use subfactor ω = .561. Compared to latent factors at the lower level of the HiTOP model, higher-order constructs tended to have greater ω values.
Table 4.
Latent HiTOP Model Properties
| Statistic | H | FD | ω | R2 |
|---|---|---|---|---|
| p | .937 | .945 | .885 | |
| Thought Problems | .613 | .895 | .853 | .759 |
| Internalizing Symptoms | .994 | .987 | .968 | .829 |
| Detachment | .828 | .954 | .824 | .827 |
| Disinhibited Externalizing Behavior | .472 | .875 | .474 | .483 |
| Antagonistic Externalizing Behavior | .750 | .905 | .734 | .535 |
| Fear | .773 | .954 | .649 | .881 |
| Distress | .938 | .989 | .784 | .993 |
| Substance Use | .615 | .682 | .561 | .089 |
| Antisocial Behavior | .896 | .980 | .700 | .891 |
Note. p = General psychopathology higher-order factor; H = construct replicability; FD = factor determinacy; ω = omega (reliability) estimate.
Associations with Risk and Resilience Factors
Tables 5 and 6 show these results, and Figure 2 illustrates the strength and patterning across all risk and resilience factors with HiTOP general and specific psychopathology dimensions.
Table 5.
Standardized Estimates for Latent HiTOP Dimensions Regressed onto Risk & Resilience Factors
| Adverse Childhood Experiences | |||
|---|---|---|---|
| Construct | Estimate | Standard Error | p-value |
| p | 0.397 | 0.059 | <.001 |
| Thought Problems | 0.347 | 0.065 | <.001 |
| Internalizing Symptoms | 0.336 | 0.096 | <.001 |
| Detachment | 0.348 | 0.070 | <.001 |
| Disinhibited Externalizing Behavior | 0.231 | 0.070 | .001 |
| Antagonistic Externalizing Behavior | 0.284 | 0.042 | <.001 |
| Fear | −0.063 | 0.051 | .216 |
| Distress | −0.014 | 0.041 | .727 |
| Substance Use | 0.070 | 0.057 | .219 |
| Antisocial Behavior | 0.120 | 0.052 | .021 |
| Benevolent Childhood Experiences | |||
| p | −0.268 | 0.068 | <.001 |
| Thought Problems | −0.284 | 0.079 | <.001 |
| Internalizing Symptoms | −0.197 | 0.068 | .004 |
| Detachment | −0.249 | 0.068 | <.001 |
| Disinhibited Externalizing Behavior | −0.352 | 0.093 | <.001 |
| Antagonistic Externalizing Behavior | −0.175 | 0.075 | .022 |
| Fear | 0.015 | 0.055 | .785 |
| Distress | 0.016 | 0.042 | .703 |
| Substance Use | −0.032 | 0.035 | .358 |
| Antisocial Behavior | −0.119 | 0.055 | .032 |
Note. p = General psychopathology higher-order factor.
Table 6.
Independent Effects of ACEs, BCEs, and Recent NLEs on Latent HiTOP Dimensions
| Construct | ACEs Estimate (SE) |
p-value | NLEs Estimate (SE) |
p-value |
|---|---|---|---|---|
| p | 0.398 (0.059) | <.001 | −0.034 (0.064) | .598 |
| Thought Problems | 0.350 (0.065) | <.001 | 0.006 (0.074) | .941 |
| Internalizing Symptoms | 0.335 (0.095) | <.001 | −0.019 (0.082) | .818 |
| Detachment | 0.345 (0.069) | <.001 | −0.122 (0.078) | .119 |
| Disinhibited Externalizing | 0.260 (0.082) | .001 | 0.048 (0.058) | .407 |
| Antagonistic Externalizing | 0.285 (0.043) | <.001 | −0.022 (0.049) | .650 |
| Fear | −0.063 (0.051) | .220 | 0.044 (0.049) | .360 |
| Distress | −0.011 (0.041) | .794 | 0.049 (0.038) | .197 |
| Substance Use | 0.066 (0.050) | .188 | 0.035 (0.044) | .425 |
| Antisocial Behavior | 0.128 (0.053) | .015 | 0.072 (0.045) | .113 |
| Construct | ACEs Estimate (SE) |
p-value | BCEs Estimate (SE) |
p-value |
| p | 0.341 (0.071) | <.001 | −0.161 (0.073) | .028 |
| Thought Problems | 0.363 (0.083) | <.001 | −0.188 (0.088) | .033 |
| Internalizing Symptoms | 0.241 (0.074) | .001 | −0.127 (0.074) | .087 |
| Detachment | 0.273 (0.073) | <.001 | −0.160 (0.076) | .034 |
| Disinhibited Externalizing | 0.314 (0.096) | .001 | −0.254 (0.095) | .007 |
| Antagonistic Externalizing | 0.445 (0.068) | <.001 | −0.010 (0.077) | .898 |
| Fear | −0.106 (0.055) | .053 | −0.029 (0.053) | .592 |
| Distress | −0.013 (0.049) | .799 | 0.007 (0.046) | .886 |
| Substance Use | 0.011 (0.033) | .727 | −0.027 (0.035) | .447 |
| Antisocial Behavior | 0.113 (0.066) | .086 | −0.114 (0.062) | .065 |
| Construct | BCEs Estimate (SE) |
p-value | NLEs Estimate (SE) |
p-value |
| p | −0.273 (0.068) | <.001 | −0.001 (0.071) | .993 |
| Thought Problems | −0.297 (0.078) | <.001 | 0.053 (0.082) | .513 |
| Internalizing Symptoms | −0.199 (0.068) | .003 | 0.009 (0.069) | .902 |
| Detachment | −0.249 (0.068) | <.001 | −0.038 (0.069) | .587 |
| Disinhibited Externalizing | −0.366 (0.093) | <.001 | 0.103 (0.087) | .238 |
| Antagonistic Externalizing | −0.178 (0.077) | .021 | −0.034 (0.078) | .658 |
| Fear | 0.017 (0.055) | .753 | 0.013 (0.054) | .805 |
| Distress | 0.016 (0.042) | .711 | 0.032 (0.041) | .438 |
| Substance Use | −0.034 (0.037) | .349 | 0.008 (0.022) | .718 |
| Antisocial Behavior | −0.127 (0.056) | .022 | 0.072 (0.051) | .155 |
Note. ACEs = Adverse Childhood Experiences. NLEs = Negative Life Experiences. BCEs = Benevolent Childhood Experiences. p = General psychopathology higher-order factor.
Figure 2. Associations among Latent Psychopathology Dimensions and Risk and Resilience Factors.
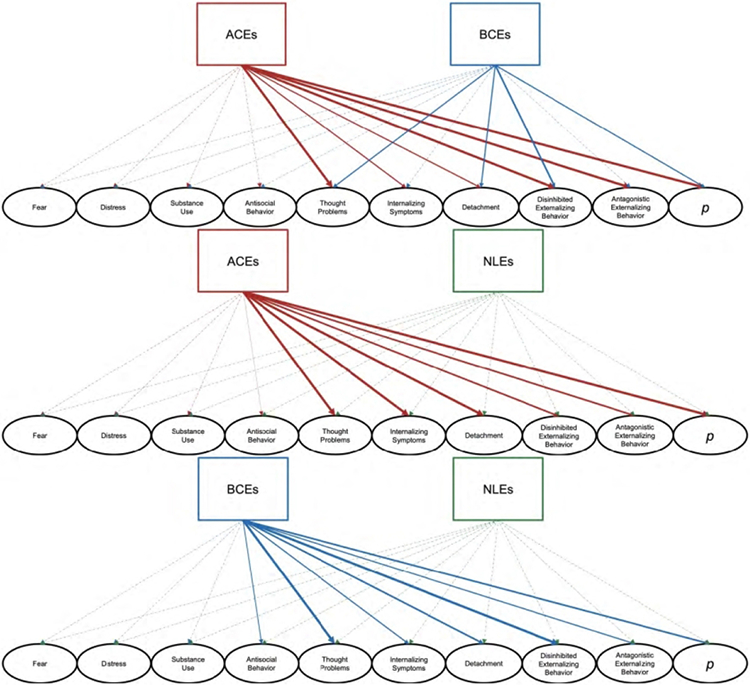
Note. ACEs = Adverse Childhood Experiences. NLEs = Negative Life Experiences. BCEs = Benevolent Childhood Experiences. p = General psychopathology higher-order factor.
Adverse Childhood Experiences.
Results from the latent HiTOP constructs regressed onto ACEs suggested that ACEs were positively associated with transdiagnostic psychopathology risk (p) in pregnancy (β = 0.397, p < .001), as well as higher-order dimensions of Internalizing Symptoms (β = 0.336, p < .001), Detachment (β = 0.348, p < .001), Disinhibited Externalizing Behavior (β = 0.231, p = .001), Antagonistic Externalizing Behavior (β = 0.284, p < .001), and Thought Problems (β = 0.347, p < .001; see Table 5). Among lower order subfactors ACEs were only significantly associated with Antisocial Behavior in pregnancy (β = 0.120, p = .021).
Benevolent Childhood Experiences.
BCEs were associated with the latent HiTOP dimensions in a pattern that was similar to that of ACEs. BCEs were inversely linked to the general psychopathology p-factor (β = −0.268, p < .001) and all higher-order spectra (Thought Problems, β = −0.284, p < .001; Internalizing Symptoms, β = −0.197, p = .004; Detachment β = −0.249, p < .001; Disinhibited Externalizing Behavior, β = −0.352, p < .001; Antagonistic Externalizing Behavior, β = −0.175, p = .022; see Table 5). No significant associations were found between BCEs and Fear, Distress, or Substance Use, but BCEs were negatively related to Antisocial Behavior during pregnancy (β = −0.119, p = .032).
Effects of Risk and Resilience Factors.
After accounting for recent NLEs, ACEs were still significantly positively associated with all higher-order latent HiTOP constructs (General psychopathology β = 0.398, p < .001; Thought Problems, β = 0.350, p < .001; Internalizing Symptoms, β = 0.335, p <.001; Detachment β = 0.345, p < .001; Disinhibited Externalizing Behavior, β = 0.260, p = .001; Antagonistic Externalizing Behavior, β = 0.285, p < .001; see Table 6), as well as the Antisocial Behavior subfactor (β = 0.128, p = .015). Recent NLEs were not significantly linked to any of the latent HiTOP dimensions after controlling for ACEs.
BCEs were also significantly associated with all higher-order latent HiTOP constructs when NLEs were accounted for (General psychopathology β = −0.273, p < .001; Thought Problems, β = −0.297, p < .001; Internalizing Symptoms, β = −0,199, p = .003; Detachment β = −0.249, p < .001; Disinhibited Externalizing Behavior, β = −0.366, p < .001; Antagonistic Externalizing Behavior, β = −0.178, p = .021; see Table 6), in addition to Antisocial Behavior specifically (β = −0.127, p = .022). Links between NLEs and latent HiTOP constructs were not significant when controlling for BCEs.
Associations between ACEs and the higher-order HiTOP dimensions remained significant after accounting for BCEs, and the magnitude of these associations was generally diminished (see Table 6). BCEs, in general, were also linked to latent higher-order HiTOP dimensions when ACEs were taken into account (General psychopathology β = −0.161, p = .028; Thought Problems β = −0.188, p = .033; Detachment β = −0.160, p =.034; Disinhibited Externalizing Behavior β = −0.254, p = .007), with the exception of Internalizing Symptoms, β = −0.127, p = .087 and Antagonistic Externalizing Behavior, β = −0.010, p = .898.
Risk and resilience factors were also examined in association with the latent HiTOP dimensions while accounting for additional sociodemographic covariates (age, education level, and income). Overall, we found the same pattern of associations among ACEs, BCEs, NLEs, and the latent HiTOP dimensions in the presence of these additional covariates, although the strength of some relations was attenuated (see Supplemental Table S1 for full model results). Participants’ highest reported level of education was the sociodemographic covariate most robustly associated with latent psychopathology dimensions, such that higher education was associated with lower general psychopathology (p), Thought Problems, Internalizing Symptoms, Detachment, Disinhibited Externalizing Behavior, and Antagonistic Externalizing Behavior. Age was also linked to some forms of psychopathology: older participants exhibited higher general psychopathology (p), Internalizing Symptoms, and Detachment.
Discussion
The present study provides empirical evidence that adverse and benevolent childhood experiences (ACEs and BCEs) are both associated with broad psychopathology during pregnancy, even after accounting for contemporaneous negative or traumatic life events during pregnancy, and that psychopathology during pregnancy can be organized dimensionally and hierarchically in a structure consistent with the Hierarchical Taxonomy of Psychopathology (HiTOP) model. By demonstrating that most of the variation in psychopathology during pregnancy is shared across disorders, and that early childhood risk and resilience factors are robustly associated with a common psychopathology factor, this study extends prior work that has evaluated the implications of childhood experiences for perinatal mental health on a disorder-by-disorder basis. Critically, our work sets the stage for future research on the intergenerational transmission of psychopathology from a transdiagnostic perspective, opening the door to mechanistic areas of inquiry that probe the shared processes through which maternal risk, resilience, and psychopathology factors shape offspring development. As we elaborate upon below, such work could also highlight potent avenues for intervention to efficiently optimize parent and child outcomes by targeting transdiagnostic risk and resilience pathways.
In the present study, links between childhood experiences (ACEs and BCEs) and latent psychopathology constructs were strongest for forms of psychopathology closer to the top of the HiTOP hierarchy. This pattern of associations suggests that the majority of risk engendered by ACEs—and the promotive effects of BCEs—can be attributed to processes and etiological factors that are commonly shared across various forms of psychopathology during pregnancy. These findings extend prior work suggestive of transdiagnostic risk processes (Hankin et al., 2017; Keyes et al., 2012; Rodriguez-Seijas et al., 2015; Snyder et al., 2019; Swales et al., 2022) by emphasizing the critical, promotive role of positive childhood experiences that can have a sizeable impact on psychopathology during a particularly sensitive developmental period for both mothers and children. Numerous studies have demonstrated that maternal prenatal psychological distress has intergenerational consequences (Davis et al., 2020; Davis & Sandman, 2012; Demers et al., 2021; Monk et al., 2019). The present work indicates that transdiagnostic characterization of prenatal psychopathology may increase ability to detect risk in the offspring.
Furthermore, this study extends past work on associations between childhood experiences (ACEs and BCEs) and specific forms of psychopathology (e.g., depression, PTSD) during pregnancy (Narayan et al., 2019; Olsen, 2018; Racine et al., 2020; Yule et al., 2019) to illustrate that ACEs and BCEs are linked to common, shared forms of transdiagnostic psychopathology. More specifically, higher levels of BCEs were associated with lower levels of psychopathology even after accounting for ACEs, indicating the robust promotive role of positive childhood experiences for better prenatal psychological adjustment above and beyond the effects of childhood adversity. These findings echo previous research that capturing the effects of positive childhood experiences on adulthood outcomes is equally important to understanding the effects of childhood adversity on adulthood maladjustment (Narayan et al., 2018; 2021). Furthermore, while both adverse and benevolent childhood experiences were associated with broad forms of psychopathology, recent NLEs experienced during pregnancy were not associated with any latent psychopathology dimensions after accounting for ACEs or BCEs. This pattern lends further support to the conclusion that childhood experiences may have even stronger effects on adult psychopathology than recent NLEs, although NLEs may be additional risk factors that increase risk for adult psychopathology (Albott et al., 2018; Mosley-Johnson et al., 2021). These findings may be tempered by the observation that in this study population, rates of NLEs were relatively low, suggesting that many pregnant individuals did not report a high level of exposure to stressful or traumatic life events during pregnancy.
More specific associations observed in this study, such as between childhood risk and resilience factors and Antisocial Behavior, indicate that childhood experiences are uniquely linked to forms of disinhibition and antagonism during pregnancy in ways that are distinct from other forms of psychopathology. Prior work in behavioral genetics suggests that antisocial behavior exhibits a distinct genetic risk mechanism separable from genetic substrates specific to internalizing pathologies (Kendler & Myers, 2014), which is consistent with the pattern of results observed in this study population. Overall, these general and specific findings coincide with research on transdiagnostic genetic etiological factors that find both shared and unique genetic liabilities for psychopathology.
Our confirmatory factor analysis lends compelling support for the HiTOP system’s approach to organize the structure of psychopathology hierarchically and across domains to better capture phenotypic heterogeneity in psychopathology during pregnancy (Kotov et al., 2017). Results extend prior work pointing to the validity of the HiTOP conceptual structure in general population samples (e.g., Caspi & Moffitt, 2018; Eaton et al., 2013; Lahey et al., 2017; Snorrason et al., 2021) by providing confirmatory evidence of its utility for pregnant populations as well. Most of the phenotypic variation in psychopathology in the present study was common across symptoms and syndromes. The general p factor accounted for considerable variance across the five predominant spectra in the hierarchical model. The Internalizing Symptoms, Detachment, and Thought Problems spectra exhibited the highest loadings onto the general p factor, whereas the two Externalizing Behavior spectra of Disinhibited and Antagonistic Behavior were relatively less strongly associated with the general p factor. At the third level of HiTOP’s proposed hierarchical model, Antisocial Behavior contributed strongly to the Disinhibited Externalizing Behavior dimension, whereas loadings were only moderate for Substance Use as an indicator of Disinhibited Externalizing Behavior and Antisocial Behavior as the indicator for Antagonistic Externalizing Behavior. The subfactors of Fear and Distress were potent indicators of the Internalizing Symptoms dimension. Of particular interest in this population of pregnant individuals, results showed that pregnancy-specific anxiety symptoms were conceptualized as forms of Fear; our findings parallel prior work in pregnant populations (Szekely et al., 2021) indicating that most of the variation in pregnancy-specific internalizing symptoms is shared with other forms of Fear. Overall, this study’s psychopathology assessments, which covered a more comprehensive range of lower-order disorders/syndromes, all showed high loadings on their respective expected latent factors.
Strengths and Limitations
This study was designed to test risk and resilience factors for prenatal transdiagnostic psychopathology using the HiTOP model in a pregnant population from diverse racial, ethnic, and socioeconomic backgrounds. The population we recruited is one that has been underrepresented in other research examining the organizational structure of psychopathology, as over 50% of participants in this study endorsed a minoritized ethno-racial identity and nearly 40% fell below 200% of the federal poverty line. Furthermore, this study provided deeper understanding of the role of early life experiences on mental health during the sensitive period of pregnancy. Importantly, this is one of few investigations of transdiagnostic and specific psychopathology during pregnancy that examines childhood experiences that can contribute to both risk and resilience, aligning with and extending prior work in this area (Narayan et al., 2021; Olsen, 2018).
There are also certain limitations to this study that provide avenues for future research. First, although a broad range of psychopathology was collected to evaluate HiTOP’s structure and aspects of validity, nevertheless some components of the HiTOP proposed organizational model were not measured, including the Somatoform spectrum and the Eating Pathology, Sexual Problems, and Mania subfactors of the Internalizing Symptoms spectrum. Some constructs (e.g., the Thought Problems superspectrum) had single-indicator latent factors, so construct replicability could be strengthened by adding manifest indicators to each dimension. Participants reporting active psychosis symptoms were excluded from this study, which likely limited our ability to measure fully the variability that can capture the spectrum of Thought Problems that may occur during pregnancy. Additionally, not all HiTOP dimensions were assessed, as manifest indicators to index Sexual Problems and Eating Pathology were not administered for practical reasons of feasibility. Future work is needed to validate the Thought Problems superspectrum, as well as Sexual Problems and Eating Pathology dimensions, in pregnant populations. Furthermore, the Substance Use latent factor in the present study explained a low portion of the variation, likely due to relatively little variation in the manifest substance use scores among pregnant individuals in this study. A likely reason for this is that active illicit substance use was an exclusion criterion for the study. Future work can recruit study populations that exhibit greater variability in substance use behaviors.
Further research on the structure of psychopathology in pregnant individuals may also benefit from the use of a single comprehensive assessment of psychopathology, such as the Minnesota Multiphasic Personality Inventory (MMPI) (Ben-Porath & Tellegen, 2020) or the Personality Assessment Inventory (PAI) (Morey, 1991). The MMPI and the PAI are both broad measures of psychopathology that have subscales that could be feasibly mapped on to the HiTOP organizational structure. These assessments have the added benefit of reducing measurement error because the time scale and scoring is consistent across subscales/domains of psychopathology. Although the choice was made in the present study to reduce participant burden by administering briefer assessments of the forms of psychopathology that are most frequently experienced by pregnant individuals (e.g., internalizing symptoms), future work in the field would do well to evaluate the HiTOP structure of psychopathology using a single, comprehensive assessment of psychopathology in pregnant individuals.
All data in the present study were self-report, which may have inflated parameter estimates due to shared method variance. Validity could further be enhanced by incorporating assessments of psychopathology from multiple informants and/or structured clinical interviews, as well as additional psychopathology risks. Participants in this study provided retrospective reports of their ACEs and BCEs, which may have introduced bias that could be mitigated in a study with a prospective longitudinal design. Lastly, although our results provide evidence that a substantial portion of variation was shared between pregnancy-specific and non-pregnancy-specific forms of Fear, we did not directly test a model that included a separate, pregnancy-specific subfactor of internalizing psychopathology. It is possible that pregnancy-specific psychopathology has mechanisms and implications for infant/child outcomes that are distinct from other forms of psychopathology during pregnancy and this possibility should be tested in future work.
Clinical Implications and Future Directions
Dimensions of mental health and distress, as organized via HiTOP and assessed during pregnancy, can be linked with childhood experiences to begin to better understand developmental origins of the intergenerational transmission of both general and specific forms of psychopathology. Such work may also begin to answer questions about processes through which maternal psychopathology influences offspring functioning (Davis & Sandman, 2012; O’Donnell & Meaney, 2017) by illuminating mediating pathways that are shared across traditionally evaluated diagnostic categories. With a more accurate characterization of psychopathology informed by HiTOP, future research can examine processes associated with common and distinct forms of psychopathology as well as factors that mediate links among risk and promotive factors and dimensions of psychopathology.
Clinically, study results can inform mental health intervention with pregnant individuals through integrating HiTOP into clinical practice (cf., Ruggero et al. 2019). For example, by distinguishing common and specific forms of psychopathology, study results suggested that there may be specific liability for particular aspects of mental health during pregnancy (Disinhibited Externalizing Behavior, Substance Use, and Antisocial Behavior). Such findings raise new questions and translational hypotheses to evaluate the possibility that more targeted interventions may be needed to address antisocial behavior, substance use, or disinhibited externalizing symptoms among pregnant individuals. Further, study results emphasize the need for intervention programs to mitigate risk as well as promotive programs to leverage positive childhood experiences among individuals who have experienced childhood adversity, given strong links among participants’ ACEs, BCEs, and the general, higher-order dimensions of psychopathology. Accordingly, clinical efforts that help underserved, traumatized, pregnant individuals to reflect on their positive childhood experiences may also have the benefit of buffering the transmission of trauma into the next generation (Narayan et al., 2019). In current and future generations, intervention and prevention for youth experiencing ACEs may also benefit from emphasizing the specific role of BCEs in disrupting pathways to adult psychopathology.
Conclusions
Moving beyond the traditional focus of measuring depression and anxiety among pregnant individuals by using a broader assessment of multiple forms of mental health symptoms and distress, results showed that psychopathology during pregnancy can be organized using the HiTOP model’s dimensional and hierarchal structure. As such, common and relatively specific representations of psychopathology can be assessed and studied parsimoniously and effectively in a reliable and valid manner. Additionally, risk and resilience factors were associated with the higher order, more general psychopathology dimension as well as some more specific features of mental health. Childhood experiences, both adverse and positive, may play a critical role in relating to psychopathology during pregnancy. Positive childhood experiences were significantly linked to transdiagnostic psychopathology during pregnancy, over and above childhood adversity and contemporaneous negative life events, underscoring the need for future empirical, prevention, and policy effects to continue to assess early life experiences to better understand the long-term pathways of psychopathology and the potential for intergenerational resilience.
Supplementary Material
Acknowledgements
The authors thank the families who participated in these projects. We also thank the dedicated research team at the Care Project. This research was supported by grants from the National Institutes of Health R01 MH109662 and R01 HL155744 to EPD and BLH.
Footnotes
Declaration of Interest
The authors have no conflicts of interest to report.
References
- Achenbach TM, & Rescorla LA (2003). Manual for the ASEBA adult forms & profiles. University of Vermont Research Center for Children, Youth, & Families. [Google Scholar]
- Albott CS, Forbes MK, & Anker JJ (2018). Association of childhood adversity with differential susceptibility of transdiagnostic psychopathology to environmental stress in adulthood. JAMA Network Open, 1(7), e185354. 10.1001/jamanetworkopen.2018.5354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College of Obstetricians and Gynecologists. (2009). ACOG Practice Bulletin No. 101: Ultrasonography in pregnancy. Obstetrics and Gynecology, 113(2 Pt 1), 451–461. 10.1097/AOG.0b013e31819930b0. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (APA). (1980). Diagnostic and Statistical Manual of Mental Disorders (DSM-III) (3rd ed.). American Psychiatric Association. [Google Scholar]
- American Psychiatric Association (APA). (1987). Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) (3rd ed., revised). American Psychiatric Association. [Google Scholar]
- American Psychiatric Association (APA). (1994). Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (4th ed.). American Psychiatric Association. [Google Scholar]
- American Psychiatric Association (APA). (2013a). Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (5th ed.). American Psychiatric Association. [Google Scholar]
- American Psychiatric Association (APA). (2013b). The Personality Inventory for DSM-5-Brief Form (PID-5-BF)-Adult. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/APA_DSM5_The-Personality-Inventory-For-DSM-5-Brief-Form-Adult.pdf
- Anderson JL, Sellbom M, & Salekin RT (2018). Utility of the Personality Inventory for DSM-5-Brief Form (PID-5-BF) in the measurement of maladaptive personality and psychopathology. Assessment, 25(5), 596–607. 10.1177/1073191116676889 [DOI] [PubMed] [Google Scholar]
- Angold AE, Costello J, & Erkanli A (1999). Comorbidity. Journal of Child Psychology and Psychiatry, 40(1), 57–87. 10.1111/1469-7610.00424 [DOI] [PubMed] [Google Scholar]
- Barrett P (2007). Structural equation modelling: Adjudging model fit. Personality and Individual Differences, 42(5), 815–824. 10.1016/j.paid.2006.09.018 [DOI] [Google Scholar]
- Ben-Porath YS, & Tellegen A (2020). Minnesota Multiphasic Personality Inventory-3 (MMPI-3): Manual for administration, scoring, and interpretation. University of Minnesota Press. [Google Scholar]
- Brown TA (2006). Specification and interpretation of CFA models. In Confirmatory factor analysis for applied research (pp. 103–156). Guilford Press. [Google Scholar]
- Buss C, Davis EP, Hobel CJ, & Sandman CA (2011). Maternal pregnancy-specific anxiety is associated with child executive function at 6–9 years age. Stress, 14(6), 665–676. 10.3109/10253890.2011.623250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, Meier MH, Ramrakha S, Shalev I, Poulton R, & Moffitt TE (2014). The p Factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2(2), 119–137. 10.1177/2167702613497473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, & Moffitt TE (2018). All for one and one for all: Mental disorders in one dimension. American Journal of Psychiatry, 175(9), 831–844. 10.1176/appi.ajp.2018.17121383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung EK, Mathew L, Elo IT, Coyne JC, & Culhane JF (2008). Depressive symptoms in disadvantaged women receiving prenatal care: The influence of adverse and positive childhood experiences. Ambulatory Pediatrics, 8(2), 109–116. 10.1016/j.ambp.2007.12.003 [DOI] [PubMed] [Google Scholar]
- Conway CC, Forbes MK, Forbush KT, Fried EI, Hallquist MN, Kotov R, Mullins-Sweatt SN, Shackman AJ, Skodol AE, South SC, Sunderland M, Waszczuk MA, Zald DH, Afzali MH, Bornovalova MA, Carragher N, Docherty AR, Jonas KG, Krueger RF, … Eaton NR (2019). A hierarchical taxonomy of psychopathology can transform mental health research. Perspectives on Psychological Science, 14(3), 419–436. 10.1177/1745691618810696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox JL, Holden JM, & Sagovsky R (1987). Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry: Journal of Mental Science, 150, 782–786. 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- Currie CL, & Tough SC (2021). Adverse childhood experiences are associated with illicit drug use among pregnant women with middle to high socioeconomic status: Findings from the All Our Families Cohort. BMC Pregnancy and Childbirth, 21(1), 133–142. 10.1186/s12884-021-03591-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis EP, Hankin BL, Glynn LM, Head K, Kim DJ, & Sandman CA (2020). Prenatal maternal stress, child cortical thickness, and adolescent depressive symptoms. Child Development, 91(2), e432–e450. 10.1111/cdev.13252 [DOI] [PubMed] [Google Scholar]
- Davis EP, Hankin BL, Swales DA, & Hoffman MC (2018). An experimental test of the fetal programming hypothesis: Can we reduce child ontogenetic vulnerability to psychopathology by decreasing maternal depression? Development and Psychopathology, 30(3), 787–806. 10.1017/S0954579418000470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis EP, & Narayan AJ (2020). Pregnancy as a period of risk, adaptation, and resilience for mothers and infants. Development and Psychopathology, 32(5), 1625–1639. 10.1017/S0954579420001121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis EP, & Sandman CA (2012). Prenatal psychobiological predictors of anxiety risk in preadolescent children. Psychoneuroendocrinology, 37(8), 1224–1233. 10.1016/j.psyneuen.2011.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vries LP, van de Weijer MP, Ligthart L, Willemsen G, Dolan CV, Boomsma DI, Baselmans BML, & Bartels M (2020). A comparison of the ASEBA Adult Self Report (ASR) and the Brief Problem Monitor (BPM/18-59). Behavior Genetics, 50(5), 363–373. 10.1007/s10519-020-10001-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demers CH, Bagonis MM, Al-Ali K, Garcia SE, Styner MA, Gilmore JH, Hoffman MC, Hankin BL, & Davis EP (2021). Exposure to prenatal maternal distress and infant white matter neurodevelopment. Development and Psychopathology, 33(5), 1526–1538. 10.1017/S0954579421000742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis C (2004). Can we identify mothers at risk for postpartum depression in the immediate postpartum period using the Edinburgh Postnatal Depression Scale? Journal of Affective Disorders, 78(2), 163–169. 10.1016/S0165-0327(02)00299-9 [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, & Covi L (1974). The Hopkins Symptom Checklist (HSCL): A measure of primary symptom dimensions. In Pichot P (Ed.), Psychological measurements in psychopharmacology (pp. 79–110). Karger International. 10.1159/000395070 [DOI] [PubMed] [Google Scholar]
- DeYoung CG, Chmielewski M, Clark LA, Condon DM, Kotov R, Krueger RF, Lynam DR, Markon KE, Miller JD, Mullins-Sweatt SN, Samuel DB, Sellbom M, South SC, Thomas KM, Watson D, Watts AL, Widiger TA, Wright AGC, & the HiTOP Normal Personality Workgroup. (2022). The distinction between symptoms and traits in the Hierarchical Taxonomy of Psychopathology (HiTOP). Journal of Personality, jopy.12593. 10.1111/jopy.12593 [DOI] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Markon KE, Keyes KM, Skodol AE, Wall M, Hasin DS, & Grant BF (2013). The structure and predictive validity of the internalizing disorders. Journal of Abnormal Psychology, 122(1), 86–92. 10.1037/a0029598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feczko E, Miranda-Dominguez O, Marr M, Graham AM, Nigg JT, & Fair DA (2019). The heterogeneity problem: Approaches to identify psychiatric subtypes. Trends in Cognitive Sciences, 23(7), 584–601. 10.1016/j.tics.2019.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. American Journal of Preventive Medicine, 14(4), 245–258. 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Fox M, Sandman CA, Davis EP, & Glynn LM (2018). A longitudinal study of women’s depression symptom profiles during and after the postpartum phase. Depression and Anxiety, 35(4), 292–304. 10.1002/da.22719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI (2015). Problematic assumptions have slowed down depression research: Why symptoms, not syndromes are the way forward. Frontiers in Psychology, 6. 10.3389/fpsyg.2015.00309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelaye B, Zheng Y, Medina-Mora ME, Rondon MB, Sánchez SE, & Williams MA (2017). Validity of the posttraumatic stress disorders (PTSD) checklist in pregnant women. BMC Psychiatry, 17(1), 179–189. 10.1186/s12888-017-1304-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez R, Watson S, & Stavropoulos V (2020). Personality Inventory for DSM-5, Brief Form: Factor structure, reliability, and coefficient of congruence. Personality Disorders: Theory, Research, and Treatment, 11, 69–77. 10.1037/per0000364 [DOI] [PubMed] [Google Scholar]
- Gordon-Smith K, Perry A, Di Florio A, Forty L, Fraser C, Casanova Dias M, Warne N, MacDonald T, Craddock N, Jones L, & Jones I (2020). Symptom profile of postpartum and non-postpartum manic episodes in bipolar I disorder: A within-subjects study. Psychiatry Research, 284, 112748. 10.1016/j.psychres.2020.112748 [DOI] [PubMed] [Google Scholar]
- Graham JW (2003). Adding missing-data-relevant variables to FIML-based structural equation models. Structural Equation Modeling: A Multidisciplinary Journal, 10(1), 80–100. 10.1207/S15328007SEM1001_4 [DOI] [Google Scholar]
- Guerrero M, Hoffmann M, & Pulkki-Råback L (2020). Psychometric properties of the Adult Self-Report: Data from over 11,000 American adults. Stats, 3(4), 465–474. 10.3390/stats3040029 [DOI] [Google Scholar]
- Gunning MD, Denison FC, Stockley CJ, Ho SP, Sandhu HK, & Reynolds RM (2010). Assessing maternal anxiety in pregnancy with the State-Trait Anxiety Inventory (STAI): Issues of validity, location and participation. Journal of Reproductive and Infant Psychology, 28(3), 266–273. 10.1080/02646830903487300 [DOI] [Google Scholar]
- Hancock GR, & Mueller RO (2001). Rethinking construct reliability within latent variable systems. In Cudeck R, du Toit S, & Sorbom D (Eds.), Structural equation modeling: Present and future (pp. 195–216). Scientific Software International. [Google Scholar]
- Hankin BL, Davis EP, Snyder H, Young JF, Glynn LM, & Sandman CA (2017). Temperament factors and dimensional, latent bifactor models of child psychopathology: Transdiagnostic and specific associations in two youth samples. Psychiatry Research, 252, 139–146. 10.1016/j.psychres.2017.02.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Snyder HR, Gulley LD, Schweizer TH, Bijttebier P, Nelis S, Toh G, & Vasey MW (2016). Understanding comorbidity among internalizing problems: Integrating latent structural models of psychopathology and risk mechanisms. Development and Psychopathology, 28(4pt1), 987–1012. 10.1017/S0954579416000663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoppen TH, & Chalder T (2018). Childhood adversity as a transdiagnostic risk factor for affective disorders in adulthood: A systematic review focusing on biopsychosocial moderating and mediating variables. Clinical Psychology Review, 65, 81–151. 10.1016/j.cpr.2018.08.002 [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hutchens BF, & Kearney J (2020). Risk factors for postpartum depression: An umbrella review. Journal of Midwifery & Women’s Health, 65(1), 96–108. 10.1111/jmwh.13067 [DOI] [PubMed] [Google Scholar]
- Hyler SE (1994). The Personality Diagnostic Questionnaire 4. New York State Psychiatric Institute. [Google Scholar]
- Kendler KS, & Myers J (2014). The boundaries of the internalizing and externalizing genetic spectra in men and women. Psychological Medicine, 44(3), 647–655. 10.1017/S0033291713000585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DA (2011). Respecification of latent variable models. http://davidakenny.net/cm/respec.htm [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, McLaughlin KA, Wall MM, Grant BF, & Hasin DS (2012). Childhood maltreatment and the structure of common psychiatric disorders. British Journal of Psychiatry, 200(2), 107–115. 10.1192/bjp.bp.111.093062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiluk BD, Dreifuss JA, Weiss RD, Morgenstern J, & Carroll KM (2013). The Short Inventory of Problems – Revised (SIP-R): Psychometric properties within a large, diverse sample of substance use disorder treatment seekers. Psychology of Addictive Behaviors, 27(1), 307–314. 10.1037/a0028445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Jonas KG, Carpenter WT, Dretsch MN, Eaton NR, Forbes MK, Forbush KT, Hobbs K, Reininghaus U, Slade T, South SC, Sunderland M, Waszczuk MA, Widiger TA, Wright AGC, Zald DH, Krueger RF, Watson D, & HiTOP Utility Workgroup. (2020). Validity and utility of Hierarchical Taxonomy of Psychopathology (HiTOP): I. Psychosis superspectrum. World Psychiatry, 19(2), 151–172. 10.1002/wps.20730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, Brown TA, Carpenter WT, Caspi A, Clark LA, Eaton NR, Forbes MK, Forbush KT, Goldberg D, Hasin D, Hyman SE, Ivanova MY, Lynam DR, Markon K, & Zimmerman M (2017). The hierarchical taxonomy of psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4), 454–477. 10.1037/abn0000258 [DOI] [PubMed] [Google Scholar]
- Krueger RF, Derringer J, Markon KE, Watson D, & Skodol AE (2012). Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychological Medicine, 42(9), 1879–1890. 10.1017/S0033291711002674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Hobbs KA, Conway CC, Dick DM, Dretsch MN, Eaton NR, Forbes MK, Forbush KT, Keyes KM, Latzman RD, Michelini G, Patrick CJ, Sellbom M, Slade T, South SC, Sunderland M, Tackett J, Waldman I, Waszczuk MA, … HiTOP Utility Workgroup. (2021). Validity and utility of Hierarchical Taxonomy of Psychopathology (HiTOP): II. Externalizing superspectrum. World Psychiatry, 20(2), 171–193. 10.1002/wps.20844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, & Zald DH (2017). A hierarchical causal taxonomy of psychopathology across the life span. Psychological Bulletin, 143(2), 142–186. 10.1037/bul0000069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luby J, Belden A, Botteron K, Marrus N, Harms MP, Babb C, Nishino T, & Barch D (2013). The effects of poverty on childhood brain development: The mediating effect of caregiving and stressful life events. JAMA Pediatrics, 167(12), 1135–1142. 10.1001/jamapediatrics.2013.3139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald SW, Madigan S, Racine N, Benzies K, Tomfohr L, & Tough S (2019). Maternal adverse childhood experiences, mental health, and child behaviour at age 3: The all our families community cohort study. Preventive Medicine, 118, 286–294. 10.1016/j.ypmed.2018.11.013 [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Colich NL, Rodman AM, & Weissman DG (2020). Mechanisms linking childhood trauma exposure and psychopathology: A transdiagnostic model of risk and resilience. BMC Medicine, 18(1), 96–107. 10.1186/s12916-020-01561-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Lambert HK (2017). Child trauma exposure and psychopathology: Mechanisms of risk and resilience. Current Opinion in Psychology, 14, 29–34. 10.1016/j.copsyc.2016.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Sheridan MA (2016). Beyond cumulative risk: A dimensional approach to childhood adversity. Current Directions in Psychological Science, 25(4), 239–245. 10.1177/0963721416655883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrick JS, Narayan AJ, Atzl VM, Harris WW, & Lieberman AF (2020). Type versus timing of adverse and benevolent childhood experiences for pregnant women’s psychological and reproductive health. Children and Youth Services Review, 114, 105056. 10.1016/j.childyouth.2020.105056 [DOI] [Google Scholar]
- Merrick JS, Narayan AJ, DePasquale CE, & Masten AS (2019). Benevolent Childhood Experiences (BCEs) in homeless parents: A validation and replication study. Journal of Family Psychology, 33(4), 493–498. 10.1037/fam0000521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, & Longabaugh R (1995). The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse. https://pubs.niaaa.nih.gov/publications/projectmatch/match04.pdf [Google Scholar]
- Monk C, Lugo-Candelas C, & Trumpff C (2019). Prenatal developmental origins of future psychopathology: Mechanisms and pathways. Annual Review of Clinical Psychology, 15(1), 317–344. 10.1146/annurev-clinpsy-050718-095539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey LC (1991). Personality Assessment Inventory: Professional manual. Psychological Assessment Resources. [Google Scholar]
- Mosley-Johnson E, Campbell JA, Garacci E, Walker RJ, & Egede LE (2021). Stress that endures: Influence of adverse childhood experiences on daily life stress and physical health in adulthood. Journal of Affective Disorders, 284, 38–43. 10.1016/j.jad.2021.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller RO, & Hancock GR (2008). Best practices in structural equation modeling. In Osborne J (Ed.), Best practices in quantitative methods (pp. 488–508). Sage Publications. 10.4135/9781412995627.d38 [DOI] [Google Scholar]
- Murray L, & Carothers AD (1990). The validation of the Edinburgh Post-natal Depression Scale on a community sample. British Journal of Psychiatry, 157(2), 288–290. 10.1192/bjp.157.2.288 [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2002). How to use a Monte Carlo study to decide on sample size and determine power. Structural Equation Modeling: A Multidisciplinary Journal, 9(4), 599–620. 10.1207/S15328007SEM0904_8 [DOI] [Google Scholar]
- Muthén LK, & Muthén BO (2017). Mplus User’s Guide (8th ed.). Muthén & Muthén. [Google Scholar]
- Narayan AJ, Ippen CG, Harris WW, & Lieberman AF (2019). Protective factors that buffer against the intergenerational transmission of trauma from mothers to young children: A replication study of angels in the nursery. Development and Psychopathology, 31(1), 173–187. 10.1017/S0954579418001530 [DOI] [PubMed] [Google Scholar]
- Narayan AJ, Lieberman AF, & Masten AS (2021). Intergenerational transmission and prevention of adverse childhood experiences (ACEs). Clinical Psychology Review, 85, 101997. 10.1016/j.cpr.2021.101997 [DOI] [PubMed] [Google Scholar]
- Narayan AJ, Rivera LM, Bernstein RE, Harris WW, & Lieberman AF (2018). Positive childhood experiences predict less psychopathology and stress in pregnant women with childhood adversity: A pilot study of the benevolent childhood experiences (BCEs) scale. Child Abuse & Neglect, 78, 19–30. 10.1016/j.chiabu.2017.09.022 [DOI] [PubMed] [Google Scholar]
- Nevarez-Brewster M, Aran Ö, Narayan AJ, Harrall KK, Brown SM, Hankin BL, & Davis EP (2022). Adverse and Benevolent Childhood Experiences Predict Prenatal Sleep Quality. Adversity and Resilience Science. 10.1007/s42844-022-00070-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurius PS, Green S, Logan-Greene P, & Borja S (2015). Life course pathways of adverse childhood experiences toward adult psychological well-being: A stress process analysis. Child Abuse & Neglect, 45, 143–153. 10.1016/j.chiabu.2015.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donnell KJ, & Meaney MJ (2017). Fetal origins of mental health: The developmental origins of health and disease hypothesis. American Journal of Psychiatry, 174(4), 319–328. 10.1176/appi.ajp.2016.16020138 [DOI] [PubMed] [Google Scholar]
- O’Hara MW, & McCabe JE (2013). Postpartum depression: Current status and future directions. Annual Review of Clinical Psychology, 9, 379–407. 10.1146/annurev-clinpsy-050212-185612 [DOI] [PubMed] [Google Scholar]
- Olsen JM (2018). Integrative review of pregnancy health risks and outcomes associated with Adverse Childhood Experiences. Journal of Obstetric, Gynecologic & Neonatal Nursing, 47(6), 783–794. 10.1016/j.jogn.2018.09.005 [DOI] [PubMed] [Google Scholar]
- Racine N, Zumwalt K, McDonald S, Tough S, & Madigan S (2020). Perinatal depression: The role of maternal adverse childhood experiences and social support. Journal of Affective Disorders, 263, 576–581. 10.1016/j.jad.2019.11.030 [DOI] [PubMed] [Google Scholar]
- Ringwald WR, Forbes MK, & Wright AGC (2021). Meta-analysis of structural evidence for the Hierarchical Taxonomy of Psychopathology (HiTOP) model. Psychological Medicine, 1–14. 10.1017/S0033291721001902 [DOI] [PubMed] [Google Scholar]
- Rini CK, Dunkel-Schetter C, Wadhwa PD, & Sandman CA (1999). Psychological adaptation and birth outcomes: The role of personal resources, stress, and sociocultural context in pregnancy. Health Psychology, 18(4), 333–345. 10.1037/0278-6133.18.4.333 [DOI] [PubMed] [Google Scholar]
- Rodriguez A, Reise SP, & Haviland MG (2016). Applying bifactor statistical indices in the evaluation of psychological measures. Journal of Personality Assessment, 98(3), 223–237. 10.1080/00223891.2015.1089249 [DOI] [PubMed] [Google Scholar]
- Rodriguez-Seijas C, Stohl M, Hasin DS, & Eaton NR (2015). Transdiagnostic factors and mediation of the relationship between perceived racial discrimination and mental disorders. JAMA Psychiatry, 72(7), 706–713. 10.1001/jamapsychiatry.2015.0148 [DOI] [PubMed] [Google Scholar]
- Ruggero CJ, Kotov R, Hopwood CJ, First M, Clark LA, Skodol AE, Mullins-Sweatt SN, Patrick CJ, Bach B, Cicero DC, Docherty A, Simms LJ, Bagby RM, Krueger RF, Callahan JL, Chmielewski M, Conway CC, De Clercq B, Dornbach-Bender A, … Zimmermann J (2019). Integrating the Hierarchical Taxonomy of Psychopathology (HiTOP) into clinical practice. Journal of Consulting and Clinical Psychology, 87(12), 1069–1084. 10.1037/ccp0000452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snorrason I, Conway CC, Beard C, & Björgvinsson T (2021). The comorbidity structure of fear, distress and compulsive disorders in an acute psychiatric sample. Journal of Anxiety Disorders, 79, 102370. 10.1016/j.janxdis.2021.102370 [DOI] [PubMed] [Google Scholar]
- Snyder HR, Young JF, & Hankin BL (2019). Chronic stress exposure and generation are related to the p-factor and externalizing specific psychopathology in youth. Journal of Clinical Child & Adolescent Psychology, 48(2), 306–315. 10.1080/15374416.2017.1321002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, & Lushene RE (1970). The State-Trait Anxiety Inventory (Self-Evaluation Questionnaire). Consulting Psychologists Press. [Google Scholar]
- Starcevic V, Eslick GD, Viswasam K, & Berle D (2020). Symptoms of Obsessive-Compulsive Disorder during pregnancy and the postpartum period: A systematic review and meta-analysis. Psychiatric Quarterly, 91(4), 965–981. 10.1007/s11126-020-09769-8 [DOI] [PubMed] [Google Scholar]
- Swales DA, Snyder HR, Hankin BL, Sandman CA, Glynn LM, & Davis EP (2022). Maternal depressive symptoms predict general liability in child psychopathology. Journal of Clinical Child & Adolescent Psychology, 51(1), 85–96. 10.1080/15374416.2020.1723598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szekely E, Neumann A, Sallis H, Jolicoeur-Martineau A, Verhulst FC, Meaney MJ, Pearson RM, Levitan RD, Kennedy JL, Lydon JE, Steiner M, Greenwood CMT, Tiemeier H, Evans J, & Wazana A (2021). Maternal prenatal mood, pregnancy-specific worries, and early child psychopathology: Findings from the DREAM BIG Consortium. Journal of the American Academy of Child & Adolescent Psychiatry, 60(1), 186–197. 10.1016/j.jaac.2020.02.017 [DOI] [PubMed] [Google Scholar]
- Tendais I, Costa R, Conde A, & Figueiredo B (2014). Screening for depression and anxiety disorders from pregnancy to postpartum with the EPDS and STAI. The Spanish Journal of Psychology, 17, E7. 10.1017/sjp.2014.7 [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. (2021). Poverty thresholds by size of family member and number of related children under 18 years. United States Census Bureau. https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html [Google Scholar]
- Viswasam K, Eslick GD, & Starcevic V (2019). Prevalence, onset and course of anxiety disorders during pregnancy: A systematic review and meta analysis. Journal of Affective Disorders, 255, 27–40. 10.1016/j.jad.2019.05.016 [DOI] [PubMed] [Google Scholar]
- Waszczuk MA, Kotov R, Ruggero C, Gamez W, & Watson D (2017). Hierarchical structure of emotional disorders: From individual symptoms to the spectrum. Journal of Abnormal Psychology, 126(5), 613–634. 10.1037/abn0000264 [DOI] [PubMed] [Google Scholar]
- Watson D, Levin-Aspenson HF, Waszczuk MA, Conway CC, Dalgleish T, Dretsch MN, Eaton NR, Forbes MK, Forbush KT, Hobbs KA, Michelini G, Nelson BD, Sellbom M, Slade T, South SC, Sunderland M, Waldman I, Witthöft M, Wright AGC, … Zinbarg RE (2022). Validity and utility of Hierarchical Taxonomy of Psychopathology (HiTOP): III. Emotional dysfunction superspectrum. World Psychiatry, 21(1), 26–54. 10.1002/wps.20943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Stanton K, & Clark LA (2017). Self-report indicators of negative valence constructs within the research domain criteria (RDoC): A critical review. Journal of Affective Disorders, 216, 58–69. 10.1016/j.jad.2016.09.065 [DOI] [PubMed] [Google Scholar]
- Watts AL, Poore HE, & Waldman ID (2019). Riskier tests of the validity of the bifactor model of psychopathology. Clinical Psychological Science, 7(6), 1285–1303. 10.1177/2167702619855035 [DOI] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013a). The PTSD Checklist for DSM-5 – LEC-5 and Extended Criterion A. National Center for PTSD. www.ptsd.va.gov [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013b). The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD. www.ptsd.va.gov [Google Scholar]
- Williams JW, Stellato CP, Cornell J, & Barrett JE (2004). The 13- and 20-Item Hopkins Symptom Checklist Depression Scale: Psychometric properties in primary care patients with minor depression or dysthymia. International Journal of Psychiatry in Medicine, 34(1), 37–50. 10.2190/U1B0-NKWC-568V-4MAK [DOI] [PubMed] [Google Scholar]
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, Foa EB, Young-McCaughan S, Yarvis JS, Hembree EA, Mintz J, Peterson AL, & Litz BT (2016). Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment, 28(11), 1392–1403. 10.1037/pas0000260 [DOI] [PubMed] [Google Scholar]
- Yule K, Houston J, & Grych J (2019). Resilience in children exposed to violence: A meta-analysis of protective factors across ecological contexts. Clinical Child and Family Psychology Review, 22(3), 406–431. 10.1007/s10567-019-00293-1 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.