Introduction
Individuals with urologic chronic pelvic pain syndrome (UCPPS) exhibit substantial pain symptoms and poor physical and mental health[2; 6; 49]. Approximately 38% of these individuals also meet criteria for at least one other nonurological pain condition[2; 37] and 75% experience widespread, nonpelvic pain in addition to localized pelvic pain[40]. The presence of widespread pain is a critical feature of UCPPS as it may indicate centrally-mediated nociplastic[36] pain processes and portend worse clinical outcomes[11; 40; 54; 67]. The ability to predict which individuals with UCPPS are susceptible to the development of widespread pain may provide novel pathways for intervention[11; 38].
Physical and sexual abuse during childhood have been linked to heightened pain sensitivity[65; 72; 77; 90], although findings are mixed[21; 57; 59; 62]. Other forms of trauma and posttraumatic stress disorder (PTSD) are also associated with pain sensitivity[14; 15; 28; 59; 78], although these findings are also inconsistent[14; 15; 22; 27; 28; 76; 84]. Trauma type[57; 76] and sequelae [15; 16; 28; 78; 90] may be differentially associated with pain perception and partly explain these mixed findings. Additionally, physical and sexual abuse may exhibit differential effects on pain sensitivity[83], although both forms of abuse are associated with chronic pelvic pain[44].
Trauma-related outcomes which overlap with pain-related characteristics may contribute to the association between childhood trauma and pain in adulthood. The Mutual Maintenance Model [71] suggests that PTSD and chronic pain maintain each other through shared mechanisms, such as affective distress and heightened cognitive demands that inhibit adaptive coping[71]. Indeed, childhood trauma is associated with affective distress[46; 51] and cognitive dysfunction[89], which are core features of chronic pain[86]. Fewer studies have focused on shared physiological mechanisms, although models of both trauma and pain include alterations in brain structure and function associated with sensory and somatic experiences[31; 32; 74] and individuals with chronic pain and a history of trauma exhibit evidence of central sensitization[72]. Additionally, childhood trauma has been linked to widespread pain and heightened sensitivity to internal and external stimuli[53; 57; 64; 70; 79], which are important features of nociplastic pain and associated with pain sensitivity among individuals with UCPPS[8; 32; 34; 67; 86].
This study explored the association of sexual and nonsexual violent trauma during childhood with experimental pain sensitivity in adulthood using quantitative sensory testing (QST) data from the Multidisciplinary Approach to the Study of Chronic Pelvic Pain (MAPP) Research Network[10; 11]. We also considered the role of nonviolent childhood trauma and recent trauma in adulthood because these frequently co-occur, may exhibit differential effects, and may impact the associations of violent trauma with pain sensitivity[5; 7; 18; 63]. Pressure stimuli were applied to the pubic region and forearm[4; 13] to compare and contrast local pelvic sensitivity to sensitivity at a remote, asymptomatic nonpelvic site. We hypothesized that childhood sexual and nonsexual violent trauma would be associated with heightened pain sensitivity at the pubic region and the forearm - suggestive of nociplastic pain[52] - and that patient-reported depressive and anxiety symptoms, cognitive dysfunction, and generalized sensory sensitivity would convey indirect effects.
Materials and Methods
Participants and Procedure
The present study utilized data from the MAPP Research Network’s Symptom Pattern Study (SPS), a 3-year observational cohort study described in detail by Clemens et al.[10] Data were collected at six sites across the United States, including Northwestern University (Chicago, Illinois); University of Michigan (Ann Arbor, Michigan); Washington University in St. Louis (St. Louis, Missouri); University of Iowa (Iowa City, Iowa); University of Washington (Seattle, Washington); and University of California, Los Angeles (Los Angeles, California). All study protocols were approved by the Institutional Review Boards at the participating sites. All participants provided informed consent prior to participating in the study.
The present study analyzed data exclusively from UCPPS SPS participants who completed extensive phenotyping including self-report measures and QST (described below). Inclusion and exclusion criteria for UCPSS SPS participants are described in detail elsewhere[10]. Briefly, participants were required to: 1) have UCPPS symptoms present for a majority of the time in the most recent 3 months; 2) be 18 years of age or older; and 3) exhibit a response ≥1 on the bladder/prostate or pelvic pain/pressure/discomfort scale in the past 2 weeks. Participants who had been enrolled in the earlier MAPP Epidemiology and Phenotyping Study (EPS)[43] were permitted to re-enroll with a score of 0 on the pain/pressure/discomfort scale. Exclusion criteria included symptomatic urethral stricture; on-going neurological conditions affecting the bladder; bladder fistula; active autoimmune or infectious disorders; history of cystitis caused by tuberculosis or radiation or chemotherapies; prior augmentation cystoplasty or cystectomy; history of pelvic cancer; current major psychiatric disorders; or severe cardiac, pulmonary, renal, or hepatic disease; unilateral orchalgia (without pelvic symptoms); and prior prostate procedures.
Eligible participants completed an extensive baseline session, including administration of standardized urologic and non-urologic assessment instruments, collection of biosamples, and QST. Participants were followed longitudinally for 6, 18, and 36 months. We focused on baseline QST data in the current study, which was available for most of the participants (n = 523). A small minority (n = 54) did not complete QST at baseline; for these participants, we analyzed the first QST data available.
Measures
Demographics.
Participants were asked to indicate their gender (0 = male; 1 = female) and the highest educational level they attained (0 = less than college; 1 = college degree). Participants were also asked to provide their date of birth, from which age was calculated.
Childhood trauma.
The Childhood Traumatic Events Scale (CTES)[56] was used to assess traumatic events experienced prior to the age of 17, including: death of a very close friend or family member; major upheaval between parents (i.e., divorce, separation); a traumatic sexual experience (i.e., raped, molested); being the victim of violence (i.e., child abuse, mugged or assaulted other than sexual); extreme illness or injury; and any other major upheaval that may have shaped one’s life or personality significantly with an open-ended response option. For each item, participants indicate whether they did or did not experience the event (0 = no; 1 = yes). For the present study, violent interpersonal trauma was of particular interest. Thus, childhood sexual violent trauma (a traumatic sexual experience [i.e., raped, molested]) and childhood nonsexual violent trauma (victim of violence [i.e., child abuse, mugged or assaulted other than sexual]) were retained as binary predictors. To obtain a childhood nonviolent trauma load score, nonviolent trauma experiences were summed (death of a very close friend or family member; major upheaval between parents; extreme illness or injury) to obtain a childhood nonviolent trauma sum with scores ranging from 0 (no nonviolent childhood trauma) to 3 (experienced all forms of nonviolent childhood trauma). Responses to the self-reported other major upheaval category were reviewed for forms of violent trauma; none were found that were not accounted for by the other questions. Thus, this item was not further analyzed. Previous research has frequently analyzed childhood sexual and nonsexual violent trauma independently and, alternatively, sum scores are often reported as a proxy for trauma load[7]. Participants also reported how traumatic the event was and how much they confided in others at the time (see Supplemental Figure 1; available online as supplemental digital content), as well as how old they were when the event occurred (see Supplemental Figure 2; available online as supplemental digital content).
Recent trauma.
The Recent Traumatic Events Scale (RTES)[56] was used to assess traumatic experiences within the last three years, including: death of a very close friend or family member; major upheaval between the participant and the participant’s spouse (i.e., divorce, separation); a traumatic sexual experience (i.e., raped, molested); being the victim of violence other than sexual; extreme illness or injury; a major change in the kind of work one does (e.g., a new job, promotion, demotion, lateral transfer); and any other major upheaval that may have shaped one’s life or personality significantly with an open-ended response option. Sexual and nonsexual violent trauma were incorporated into the sum score because prevalence rates were low and the type of recent trauma was not relevant to our hypotheses. For each item, participants indicated whether they did or did not experience the event (0 = no; 1 = yes). To obtain a recent trauma load score, items were summed for a total score ranging from 0 (no recent trauma) to 7 (experienced all forms of recent trauma).
Depressive and anxiety symptoms.
Depressive and anxiety symptoms were measured using the Hospital Anxiety and Depression Scale[91]. Each scale includes seven items and reference symptoms experienced over the past week. Sample items include, “I still enjoy the things I used to enjoy” (depressive symptoms) and “Worrying thoughts go through my mind” (anxiety symptoms). Response options ranged from 0 (e.g., not at all) to 3 (e.g., most of the time). For each scale, items were summed for total scores ranging from 0 to 21. Higher scores indicate greater depressive or anxiety symptoms.
Cognitive dysfunction.
The 38-item Multiple Ability Self-Report Questionnaire (MASQ)[69] was used to measure cognitive dysfunction. The MASQ includes five subscales assessing language (e.g., “My speech is slow or hesitant”), visual perceptual ability (e.g., I get lost when traveling around”), verbal memory (e.g., “I forget to mention important issues during conversations”), visual-spatial memory (e.g., “I have difficulty remembering the faces of people I have recently met”), and attention/concentration (e.g., “I can focus my attention on a task for more than a few minutes at a time”). Response options ranged from 1 (never) to 5 (always). For the current study, a total sum score was obtained to assess overall cognitive dysfunction, with scores ranging from 38 to 190. Higher scores indicate greater cognitive dysfunction.
Generalized sensory sensitivity.
The Complex Medical Symptoms Inventory[87] and a 2D body map were used to evaluate generalized sensory sensitivity, which is characterized by widespread pain, increased sensitivity to sensations within the body (i.e., interoception), and increased sensitivity to external stimuli[67]. In the present study, these three components were combined into a single brief score, as described in the supplemental material provided by Schrepf et al.[67] The brief measure included the sum score of widespread pain (i.e., sum of painful body regions across seven potential regions), somatic awareness (i.e., sum of three somatic awareness items [dry mouth; rapid heart rate; problems with balance] experienced for 3 months during the last year), and sensory sensitivity (i.e., sum of three sensory sensitivity items [sensitivity to certain chemicals; sensitivity to sound; frequent sensitivity to bright lights] experienced for 3 months during the last year). The sum of widespread pain incorporated all body regions, including the groin and pelvis.
Quantitative sensory testing.
A handheld, analog pressure algometer (FPK Algometer, Wagner Instruments, Greenwich, CT) was used to deliver pressure pain to the suprapubic region (midway between the umbilicus and pubic symphysis) and the dominant forearm (midway between the wrist and elbow with palm facing up) using a 1 cm2 rubber-tipped probe. The suprapubic stimulation site aimed to assess local evoked pain sensitivity at the symptomatic pelvic region, whereas the arm site assessed pain sensitivity at a remote, asymptomatic body area as a control. At each site, the research assistant applied six pressure stimuli, in a pseudo-random order, at a rate of approximately 0.5 kgf/cm2/s using a metronome to reach intensities of 2 or 4 kgf/cm2[39]. Each pressure was held for a 5-second duration, with a 15–20 second interstimulus interval. Participants rated the pain intensity of each pressure using a 0 to 100 numerical rating scale (NRS; 0 = no pain,100 = pain as bad as it could be) following each stimulus presentation. The present study evaluated only NRS scores at 4 kgf/cm2 of pressure because the pressure was rated as painful by the majority of participants and there was good variation in responses (Mpain at 4kg-pubic = 49.04, Med = 50.00, Range = 0–100; Mpain at 4kg-arm = 37.18, Med = 35, Range = 0–100). The three 4 kgf/cm2 NRS ratings for each site were averaged and two scores were obtained: pain sensitivity at the suprapubic region (pain at 4kg-pubic) and pain sensitivity at the arm (pain at 4kg-arm).
Data Analysis Plan
Preliminary analyses.
Descriptive statistics were obtained for study measures. Histograms and Q-Q plots were used to evaluate the distribution of study variables. All variables appeared reasonably normally distributed. Independent samples t-tests were used to evaluate differences on variables of interest among individuals who did and did not experience a sexual or nonsexual violent experience during childhood. Experiences of other forms of childhood and recent trauma were also assessed using contingency analyses and associated χ2 tests. Finally, Pearson correlations were evaluated for all model variables. Each set of analyses were evaluated with alpha at 0.05.
Path analysis: Model building.
Multiple models were then tested and compared to determine the best fitting model for the final analyses. There were no concerns regarding collinearity (all variance inflation factor (VIF) scores < 2). See Figure 1 for the list of models tested. Age, sex, and college education were included in all models with direct associations on all variables of interest to control for their effects. Models were run using full information maximum likelihood (FIML) method of estimation to account for missing data, with bootstrap standard errors (SEs) with 50 draws. These models prioritized the evaluation of model fit, rather than coefficient estimates. Numerous indices were used to evaluate the best fitting model, including the χ2 goodness-of-fit test, the root mean square error of approximation (RMSEA), the comparative fit index (CFI), the Tucker-Lewis index (TLI), Akaike’s Information Criterion (AIC), and Bayesian Information Criterion (BIC). An increase in degrees of freedom was preferred. A nonsignificant increase in the χ2 goodness-of-fit test for more degrees of freedom was considered favorable. A decrease in RMSEA and increase in CFI and TLI indicated a better fitting model. AIC and BIC for each model were also assessed, with the model showing the lowest AIC and BIC considered the best fitting model. This information was considered to determine the preferred model, which was subsequently tested as the final model[3].
Figure 1.
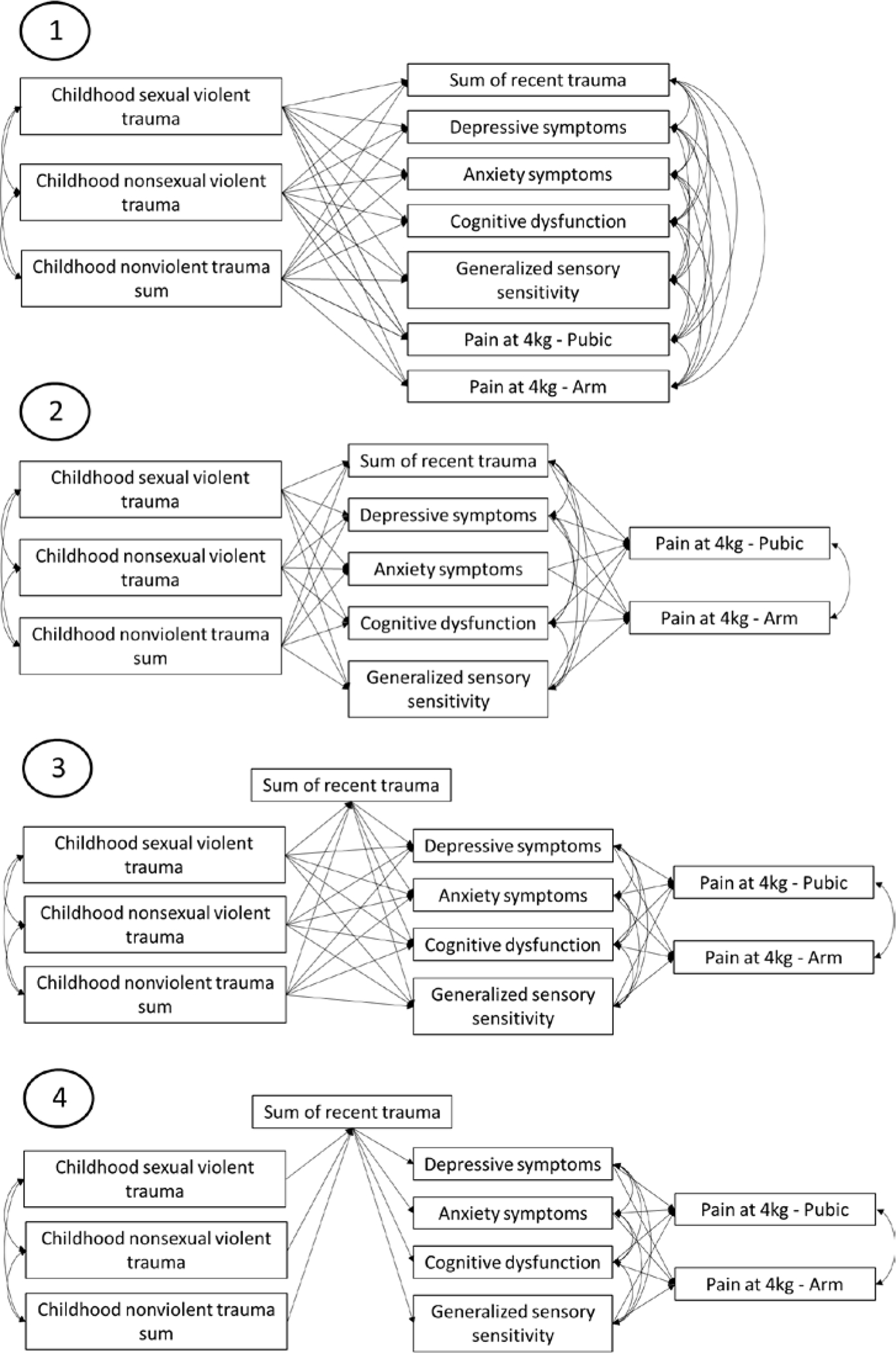
Models for comparison. Model 1 was designed to treat childhood trauma as causal and all adult variables as outcomes at the same level. Model 2 was designed to treat childhood trauma as causal, recent trauma and self-reported adult symptoms as mediators, and pain sensitivity as outcomes. Model 3 was designed to treat childhood trauma as causal, recent trauma as a partial distal mediator, self-reported adult symptoms as proximal mediators, and pain sensitivity as outcomes. Model 4 was designed to treat childhood trauma as causal, recent trauma as a full distal mediator, self-reported adult symptoms as proximal mediators, and pain sensitivity as outcomes. Model fit statistics showed Model 3 as the preferred model.
Path analysis: Final model.
Path analysis was then conducted to assess the final preferred model using FIML method of estimation with bootstrap SEs with 10,000 draws. Age, sex, and college education were included in all models with direct associations on all variables of interest to control for their effects. Childhood sexual violent trauma and childhood nonsexual violent trauma were included as distal binary predictors. Thus, no violent trauma was included as the reference category and direct and indirect effects are relative to this reference group. The childhood nonviolent trauma sum was also included as a distal predictor to account for the co-occurrence of trauma. Overall model fit was evaluated with the χ2 goodness-of-fit test, RMSEA, CFI, and TLI[61]. RMSEA ≤ 0.05 indicates good fit. CFI and TLI ≥ 0.95 indicates good fit. Bentler-Raykov squared multiple correlation coefficients (R2) were assessed to determine the variance explained in the mediators and outcomes of interest. Coefficients in which the bias-corrected bootstrap 95% confidence intervals (95% CI) did not include zero were considered statistically significant.
Path analysis: Probing indirect effects.
In order to further understand the indirect effects, analyses were assessed using seemingly unrelated regression and modeling each indirect pathway simultaneously. Bias-corrected and accelerated (BCa) 95% CIs were then assessed to determine significance, with BCa 95% CIs not including zero considered statistically significant. Complete case analysis was used for probing indirect effects. The proportion of the total indirect effect accounted for in each outcome was calculated by dividing the absolute value of the coefficient for each distal predictor (childhood sexual violent trauma; childhood nonsexual violent trauma; and childhood nonviolent trauma sum) by the sum of the absolute values of indirect effects from each distal predictor on the outcome. Specific indirect effects for each mediator were calculated by dividing the absolute value of the coefficient for each specific indirect path by the sum of the absolute values of indirect effects for each distal predictor. Analyses were conducted using StataIC v.15 (StataCorp, College Station, Texas, USA).
Results
Sample descriptives.
The analyses included 577 UCPPS study participants (Mage = 44.81, SD = 15.68; 66.55% female). Descriptive results are provided in Table 1. Participants who experienced childhood sexual violent trauma or childhood nonsexual violent trauma were more often female, experienced more types of nonviolent childhood trauma, experienced more types of recent trauma, and reported higher depressive symptoms, higher anxiety symptoms, more cognitive dysfunction, higher generalized sensory sensitivity, and higher perceived pain in the pubic region in response to pressure stimuli.
Table 1.
Descriptive data for full sample and differences by history of violent childhood trauma
| Childhood Traumatic Sexual Experience | Childhood Victim of Violence | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Overall M (SD) / n (%) | No n = 440 | Yes n = 129 | p | No n = 463 | Yes n = 107 | p |
|
| |||||||
| Age | 44.81 (15.68) | 45.33 (15.96) | 43.31 (14.71) | 0.201 | 45.07 (16.18) | 44.05 (13.48) | 0.546 |
| Female | 384 (66.55) | 269 (61.14) | 108 (83.72) | < 0.001 | 298 (64.36) | 80 (74.77) | 0.040 |
| College graduate | 389 (67.42) | 304 (69.09) | 81 (62.79) | 0.179 | 319 (68.90) | 67 (62.62) | 0.210 |
| Race | |||||||
| White/Caucasian | 509 (88.21%) | 387 (87.95) | 114 (88.37) | 0.587 | 408 (88.12) | 95 (88.79) | 0.302 |
| Black/African-American | 32 (5.55%) | 22 (5.00) | 10 (7.75) | 26 (5.62) | 6 (5.61) | ||
| American Indian | 3 (.52%) | 3 (.68) | 0 (.00) | 3 (.65) | 0 (.00) | ||
| Native Hawaiian | 1 (.17%) | 1 (.23) | 0 (.00) | 1 (.22) | 0 (.00) | ||
| Asian | 6 (1.04%) | 6 (1.36) | 0 (.00) | 6 (1.30) | 0 (.00) | ||
| Multi-Race | 18 (3.12%) | 15 (3.41) | 3 (2.33) | 11 (2.38) | 6 (5.61) | ||
| Other | 8 (1.39%) | 6 (1.36) | 2 (1.55) | 8 (1.73) | 0 (.00) | ||
| Hispanic/Latino | 37 (6.41%) | 26 (5.92) | 11 (8.53) | 0.292 | 28 (6.06) | 9 (8.41) | 0.374 |
| Sum of nonviolent childhood trauma | 1.02 (0.87) | 0.88 (0.82) | 1.49 (0.87) | < 0.001 | 0.90 (0.84) | 1.54 (0.80) | < 0.001 |
| Sum of recent trauma | 1.79 (1.25) | 1.70 (1.23) | 2.13 (1.28) | < 0.001 | 1.67 (1.23) | 2.32 (1.19) | < 0.001 |
| Depression | 5.76 (4.50) | 5.36 (4.35) | 7.17 (4.76) | < 0.001 | 5.49 (4.40) | 6.91 (4.77) | 0.003 |
| Anxiety | 7.38 (4.73) | 6.96 (4.59) | 8.82 (4.97) | < 0.001 | 7.03 (4.68) | 8.90 (4.72) | < 0.001 |
| Cognitive dysfunction | 78.61 (21.34) | 76.86 (20.51) | 84.58 (23.22) | < 0.001 | 77.13 (20.95) | 84.98 (22.13) | < 0.001 |
| Generalized sensory sensitivity | 2.79 (2.28) | 2.51 (2.12) | 3.77 (2.59) | < 0.001 | 2.51 (2.14) | 3.97 (2.52) | < 0.001 |
| Pain at 4kg - Pubic | 49.04 (25.09) | 46.64 (24.95) | 56.85 (23.62) | < 0.001 | 47.48 (24.85) | 55.45 (24.94) | 0.005 |
| Pain at 4kg - Arm | 37.18 (24.70) | 36.37 (24.79) | 39.26 (23.92) | 0.245 | 36.94 (24.53) | 37.26 (25.04) | 0.906 |
Note. Boldfaced values are significant at p < 0.05.
As shown in Table 2, 22.7% of the overall sample experienced childhood sexual violent trauma and 18.8% reported childhood nonsexual violent trauma. Participants who experienced childhood sexual violent trauma more often experienced all other forms of childhood trauma, as well as many recent traumatic experiences in adulthood, including recent violence, being extremely ill or injured, and experiencing some other major upheaval.
Table 2.
Prevalence of childhood and adulthood trauma types in patients with urologie chronic pelvic pain syndrome (UCPPS) with history of violent childhood trauma
| Overall | Childhood Sexual Violent Trauma | Childhood Nonsexual Violent Trauma | |||||
|---|---|---|---|---|---|---|---|
| n = 577 | No (n = 440) | Yes (n = 129) | p | No (n = 463) | Yes (n = 107) | p | |
| Trauma type | n (%) | n (%) | n (%) | n (%) | n (%) | ||
|
| |||||||
| Childhood experiences | |||||||
| Death of friend or family member | 256 (44.8) | 178 (40.5) | 77 (59.7) | < 0.001 | 203 (43.8) | 52 (48.6) | 0.373 |
| Parents’ divorce or separation | 202 (35.8) | 136 (31.1) | 66 (52.8) | < 0.001 | 132 (28.8) | 70 (66.7) | < 0.001 |
| Traumatic sexual experience | 129 (22.7) | -- | -- | 71 (15.4) | 58 (54.2) | < 0.001 | |
| Victim of violence | 107 (18.8) | 49 (11.2) | 58 (45.0) | < 0.001 | -- | -- | |
| Extremely ill or injured | 125 (22.0) | 75 (17.1) | 49 (38.0) | < 0.001 | 82 (17.8) | 43 (40.2) | < 0.001 |
| Other major upheaval | 213 (37.4) | 144 (32.8) | 69 (53.5) | < 0.001 | 157 (34.0) | 56 (52.3) | < 0.001 |
| Recent experiences (past 3 years) | |||||||
| Death of friend or family member | 288 (50.7) | 217 (49.5) | 70 (54.7) | 0.306 | 219 (47.6) | 68 (63.6) | 0.003 |
| Divorce or separation | 73 (13.0) | 50 (11.6) | 23 (18.1) | 0.053 | 54 (11.8) | 19 (17.9) | 0.093 |
| Traumatic sexual experience | 26 (4.6) | 21 (4.8) | 5 (3.9) | 0.662 | 20 (4.4) | 6 (5.7) | 0.567 |
| Victim of violence | 31 (5.5) | 18 (4.1) | 13 (10.2) | 0.008 | 17 (3.7) | 14 (13.1) | < 0.001 |
| Extremely ill or injured | 164 (29.1) | 114 (26.2) | 50 (39.4) | 0.004 | 115 (25.2) | 48 (45.3) | < 0.001 |
| Major change in work | 279 (49.5) | 211 (48.5) | 67 (52.8) | 0.399 | 224 (49.1) | 54 (50.5) | 0.802 |
| Other major upheaval | 157 (27.7) | 112 (25.7) | 45 (35.2) | 0.036 | 117 (25.6) | 39 (36.5) | 0.023 |
Note. Boldfaced values are significant at p < 0.05.
Participants who reported childhood nonsexual violent trauma also more often reported all other forms of childhood trauma, with the exception of the death of a friend or family member. Reporting childhood nonsexual violent trauma was also associated with recent traumatic events, including the death of a friend or family member, recent violence, being extremely ill or injured, and experiencing some other major upheaval.
Bivariate associations.
As shown in Table 3, the variables of interest were generally intercorrelated. Of note, pain sensitivity in the pubic region was significantly correlated with experiencing childhood sexual violent trauma, childhood nonsexual violent trauma, younger age, female sex, more types of nonviolent childhood trauma, more types of recent traumatic events, higher depressive symptoms, higher anxiety symptoms, higher cognitive dysfunction, and higher generalized sensory sensitivity. Pain sensitivity in the arm was significantly associated with older age, female sex, higher education, higher cognitive dysfunction, and higher generalized sensory sensitivity. Pain sensitivity in the pubic region and the arm were significantly positively associated.
Table 3.
Bivariate correlations among study variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| 1 | Childhood sexual violent trauma | -- | |||||||||||
| 2 | Childhood nonsexual violent trauma | 0.36 | -- | ||||||||||
| 3 | Age | −0.05 | −0.03 | -- | |||||||||
| 4 | Female | 0.20 | 0.09 | −0.17 | -- | ||||||||
| 5 | College graduate | −0.06 | −0.05 | 0.05 | −0.02 | -- | |||||||
| 6 | Childhood nonviolent trauma sum | 0.29 | 0.29 | −0.06 | 0.14 | −0.12 | -- | ||||||
| 7 | Sum of recent trauma | 0.15 | 0.20 | −0.19 | 0.23 | −0.06 | 0.26 | -- | |||||
| 8 | Depressive symptoms | 0.17 | 0.12 | −0.16 | 0.04 | −0.16 | 0.11 | 0.24 | -- | ||||
| 9 | Anxiety symptoms | 0.16 | 0.15 | −0.34 | 0.08 | −0.12 | 0.08 | 0.27 | 0.57 | -- | |||
| 10 | Cognitive dysfunction | 0.15 | 0.14 | −0.13 | 0.11 | −0.21 | 0.05 | 0.22 | 0.55 | 0.48 | -- | ||
| 11 | Generalized sensory sensitivity | 0.23 | 0.25 | 0.02 | 0.18 | −0.08 | 0.14 | 0.26 | 0.38 | 0.36 | 0.43 | -- | |
| 12 | Pain at 4kg - Pubic | 0.17 | 0.12 | −0.09 | 0.30 | −0.002 | 0.09 | 0.12 | 0.16 | 0.14 | 0.20 | 0.24 | -- |
| 13 | Pain at 4kg - Arm | 0.05 | 0.01 | 0.09 | 0.23 | 0.09 | 0.04 | 0.07 | 0.07 | 0.002 | 0.12 | 0.18 | 0.66 |
Note. Pearson correlations are reported. Boldfaced values are significant at p < 0.05. Complete case analyses was used. Thus, sample sizes vary.
Model building.
As seen in Figure 1 and Table 4, four models were compared. Model 3 resulted in a decrease in RMSEA, as well as an increase in CFI and TLI, compared to Model 2. The increase in χ2 was nonsignificant, and the model exhibited a nonsignificant χ2 goodness of fit. Furthermore, AIC and BIC increased minimally. In comparison, further increasing degrees of freedom in Model 4 resulted in a significant increase in χ2, as well as an increase in RMSEA and decrease in CFI and TLI. AIC and BIC for Model 4 also increased. Thus, Model 3 was determined to be the preferred model.
Table 4.
Model comparison for model building
| RMSEA 90% CI | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model | χ2 | df | p | Δχ2 | Δdf | RMSEA | LL | UL | CFI | TLI | AIC | BIC |
|
| ||||||||||||
| Saturated model | ||||||||||||
| (Model 1) | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 33532.06 | 33745.60 |
| Model 2 | 12.92 | 6 | 0.044 | -- | -- | 0.045 | 0.007 | 0.079 | 0.995 | 0.941 | 33544.98 | 33758.52 |
| Model 3 | 13.42 | 8 | 0.098 | 0.50 | 2 | 0.034 | 0.000 | 0.065 | 0.996 | 0.965 | 33545.49 | 33759.02 |
| Model 4 | 58.69 | 20 | <0.001 | 45.27 | 12 | 0.058 | 0.041 | 0.075 | 0.974 | 0.901 | 33590.76 | 33804.29 |
Note. Boldfaced values indicate the preferred model. RMSEA=Root Mean Square Error of Approximation. 90% CI=90% Confidence Interval; LL=Lower Limit; UL=Upper Limit; CFI=Comparative Fit Index. TLI=Tucker-Lewis Index. AIC=Akaike Information Criterion. BIC=Bayesian Information Criterion.
Path analysis.
Direct effects for the final model are displayed in Figure 2 and Table 5. Overall, the model fit the data well (χ2 (df = 8) = 13.42, p = .098; RMSEA = .034 (90% CI [.000, .065]); CFI = .996; TLI = .965). The findings suggest that experiencing violence during childhood and more types of nonviolent childhood trauma were associated with experiencing more types of recent trauma. Experiencing childhood sexual violent trauma and more types of recent trauma were associated with more depressive symptoms and more anxiety symptoms. Experiencing childhood sexual violent trauma, childhood nonsexual violent trauma, and more types of recent trauma were associated with higher cognitive dysfunction and higher generalized sensory sensitivity. In turn, higher cognitive dysfunction and higher generalized sensory sensitivity were associated with higher pain sensitivity in the pubic region and higher pain sensitivity at the arm.
Figure 2.
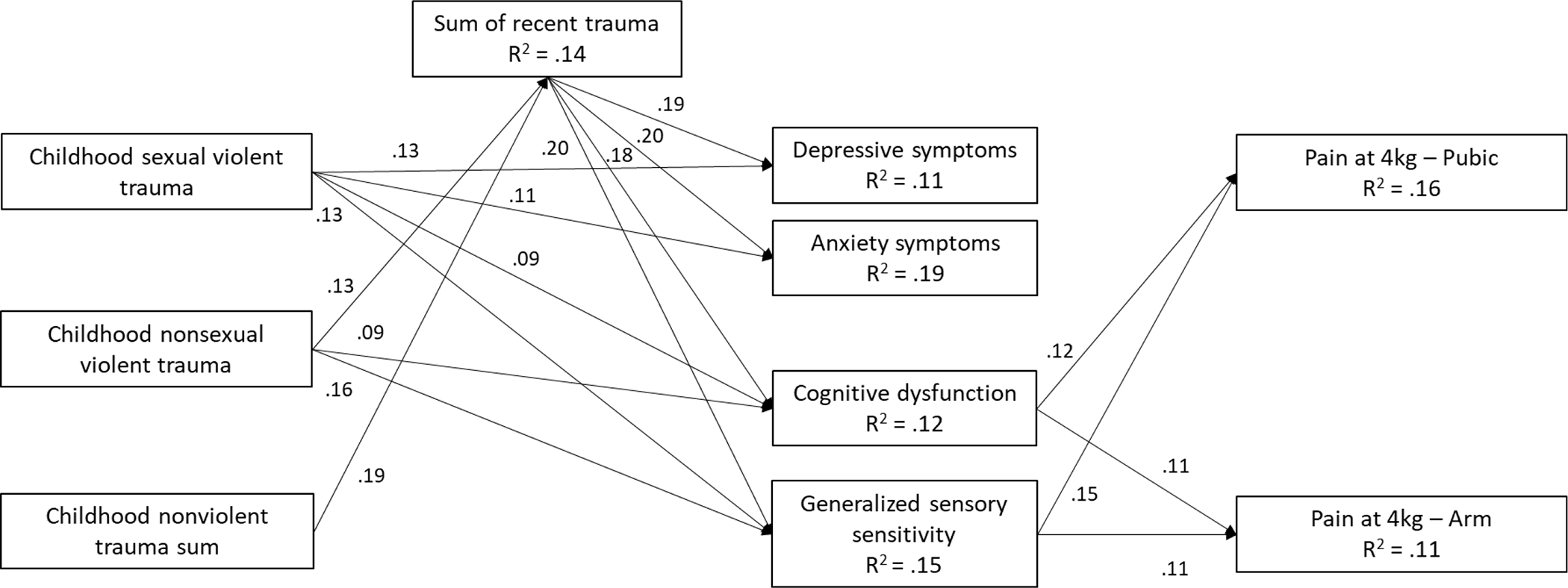
Path model predicting pain sensitivity. Standardized estimates are shown. Only significant paths are shown. Covariates (age, college graduate, and sex) were included with direct associations on study variables. Covariance among variables at the same levels were also included. Covariates and covariance estimates, however, are not included in the figure to ease interpretability. Χ2 (df = 8) = 13.42, p = .098; RMSEA = .034 (90% CI [.000, .065]); CFI = .996; TLI = .965.
Table 5.
Direct effects derived from path analysis predicting pain sensitivity (n = 577)
| Bias-corrected Bootstrap 95% CI | |||||||
|---|---|---|---|---|---|---|---|
| Outcome | Predictor | Coef. | Bootstrap SE | Standardized Coef. | p | LL | UL |
|
| |||||||
| Direct Associations | |||||||
| →Childhood sexual violent trauma | |||||||
| Age | 0.00 | 0.001 | −0.02 | 0.632 | −0.003 | 0.002 | |
| College graduate | −0.05 | 0.04 | −0.05 | 0.214 | −0.123 | 0.027 | |
| Female | 0.17 | 0.03 | 0.19 | <0.001 | 0.109 | 0.236 | |
| →Childhood nonsexual violent trauma | |||||||
| Age | 0.00 | 0.001 | −0.01 | 0.815 | −0.002 | 0.002 | |
| College graduate | −0.04 | 0.04 | −0.05 | 0.237 | −0.114 | 0.027 | |
| Female | 0.07 | 0.03 | 0.08 | 0.032 | 0.004 | 0.130 | |
| →Childhood nonviolent trauma sum | |||||||
| Age | −0.002 | 0.002 | −0.03 | 0.414 | −0.007 | 0.003 | |
| College graduate | −0.22 | 0.08 | −0.12 | 0.006 | −0.377 | 0.068 | |
| Female | 0.24 | 0.08 | 0.13 | 0.002 | 0.087 | 0.386 | |
| →Sum of recent trauma | |||||||
| Childhood sexual violent trauma | 0.002 | 0.13 | 0.00 | 0.988 | −0.250 | 0.258 | |
| Childhood nonsexual violent trauma | 0.42 | 0.14 | 0.13 | 0.002 | 0.149 | 0.687 | |
| Childhood nonviolent trauma sum | 0.27 | 0.06 | 0.19 | <0.001 | 0.152 | 0.388 | |
| Age | −0.01 | 0.003 | −0.14 | <0.001 | −0.017 | −0.006 | |
| College graduate | −0.06 | 0.10 | −0.02 | 0.524 | −0.256 | 0.134 | |
| Female | 0.43 | 0.11 | 0.16 | <0.001 | 0.226 | 0.642 | |
| →Depressive symptoms | |||||||
| Childhood sexual violent trauma | 1.37 | 0.48 | 0.13 | 0.004 | 0.456 | 2.333 | |
| Childhood nonsexual violent trauma | 0.40 | 0.53 | 0.04 | 0.448 | −0.638 | 1.436 | |
| Childhood nonviolent trauma sum | −0.03 | 0.24 | −0.01 | 0.884 | −0.485 | 0.438 | |
| Sum of recent trauma | 0.69 | 0.17 | 0.19 | <0.001 | 0.360 | 1.012 | |
| Age | −0.03 | 0.01 | −0.12 | 0.002 | −0.055 | −0.013 | |
| College graduate | −1.27 | 0.39 | −0.13 | 0.001 | −2.031 | −0.499 | |
| Female | −0.50 | 0.41 | −0.05 | 0.213 | −1.329 | 0.267 | |
| →Anxiety symptoms | |||||||
| Childhood sexual violent trauma | 1.20 | 0.50 | 0.11 | 0.018 | 0.198 | 2.172 | |
| Childhood nonsexual violent trauma | 0.97 | 0.52 | 0.08 | 0.061 | −0.028 | 1.968 | |
| Childhood nonviolent trauma sum | −0.24 | 0.25 | −0.04 | 0.326 | −0.718 | 0.239 | |
| Sum of recent trauma | 0.75 | 0.17 | 0.20 | <0.001 | 0.421 | 1.071 | |
| Age | −0.09 | 0.01 | −0.30 | <0.001 | −0.114 | −0.069 | |
| College graduate | −0.87 | 0.40 | −0.09 | 0.030 | −1.648 | −0.097 | |
| Female | −0.38 | 0.38 | −0.04 | 0.320 | −1.126 | 0.358 | |
| →Cognitive dysfunction | |||||||
| Childhood sexual violent trauma | 4.66 | 2.37 | 0.09 | 0.049 | 0.207 | 9.444 | |
| Childhood nonsexual violent trauma | 4.70 | 2.40 | 0.09 | 0.050 | 0.044 | 9.429 | |
| Childhood nonviolent trauma sum | −2.18 | 1.15 | −0.09 | 0.057 | −4.417 | 0.084 | |
| Sum of recent trauma | 3.09 | 0.82 | 0.18 | <0.001 | 1.498 | 4.694 | |
| Age | −0.10 | 0.06 | −0.08 | 0.065 | −0.213 | 0.005 | |
| College graduate | −8.98 | 1.91 | −0.20 | <0.001 | −12.656 | −5.063 | |
| Female | 1.48 | 1.84 | 0.03 | 0.420 | −2.128 | 5.129 | |
| →Generalized sensory sensitivity | |||||||
| Childhood sexual violent trauma | 0.71 | 0.27 | 0.13 | 0.008 | 0.189 | 1.236 | |
| Childhood nonsexual violent trauma | 0.96 | 0.29 | 0.16 | 0.001 | 0.421 | 1.543 | |
| Childhood nonviolent trauma sum | −0.03 | 0.12 | −0.01 | 0.783 | −0.254 | 0.203 | |
| Sum of recent trauma | 0.37 | 0.08 | 0.20 | <0.001 | 0.212 | 0.532 | |
| Age | 0.01 | 0.01 | 0.09 | 0.021 | 0.002 | 0.025 | |
| College graduate | −0.32 | 0.20 | −0.07 | 0.099 | −0.710 | 0.066 | |
| Female | 0.52 | 0.19 | 0.11 | 0.006 | 0.147 | 0.892 | |
| →Pain at 4kg - Pubic | |||||||
| Depressive symptoms | 0.09 | 0.32 | 0.02 | 0.789 | −0.539 | 0.705 | |
| Anxiety symptoms | 0.15 | 0.29 | 0.03 | 0.623 | −0.438 | 0.720 | |
| Cognitive dysfunction | 0.15 | 0.06 | 0.12 | 0.024 | 0.020 | 0.273 | |
| Generalized sensory sensitivity | 1.71 | 0.52 | 0.15 | 0.001 | 0.674 | 2.720 | |
| Age | −0.03 | 0.07 | −0.02 | 0.692 | −0.163 | 0.109 | |
| College graduate | 2.67 | 2.26 | 0.05 | 0.236 | −1.683 | 7.134 | |
| Female | 14.29 | 2.28 | 0.26 | <0.001 | 9.747 | 18.644 | |
| →Pain at 4kg - Arm | |||||||
| Depressive symptoms | 0.25 | 0.30 | 0.04 | 0.413 | −0.353 | 0.834 | |
| Anxiety symptoms | −0.45 | 0.28 | −0.09 | 0.108 | −0.991 | 0.123 | |
| Cognitive dysfunction | 0.13 | 0.06 | 0.11 | 0.045 | 0.003 | 0.247 | |
| Generalized sensory sensitivity | 1.19 | 0.54 | 0.11 | 0.028 | 0.121 | 2.250 | |
| Age | 0.18 | 0.07 | 0.11 | 0.011 | 0.042 | 0.318 | |
| College graduate | 6.09 | 2.13 | 0.12 | 0.004 | 1.907 | 10.163 | |
| Female | 11.89 | 2.13 | 0.23 | <0.001 | 7.652 | 15.979 | |
| Covariance | |||||||
| Childhood sexual violent trauma↔Childhood nonsexual violent trauma | 0.06 | 0.01 | 0.35 | <0.001 | 0.039 | 0.073 | |
| Childhood sexual violent trauma↔Childhood nonviolent trauma sum | 0.09 | 0.02 | 0.27 | <0.001 | 0.064 | 0.125 | |
| Childhood nonsexual violent trauma↔Childhood nonviolent trauma sum | 0.09 | 0.01 | 0.28 | <0.001 | 0.064 | 0.121 | |
| Generalized sensory sensitivity↔Anxiety symptoms | 2.91 | 0.43 | 0.33 | <0.001 | 2.107 | 3.794 | |
| Generalized sensory sensitivity↔Depressive symptoms | 2.91 | 0.41 | 0.33 | <0.001 | 2.137 | 3.761 | |
| Generalized sensory sensitivity↔Cognitive dysfunction | 16.68 | 1.94 | 0.39 | <0.001 | 13.243 | 20.861 | |
| Anxiety symptoms↔Depressive symptoms | 9.41 | 0.89 | 0.52 | <0.001 | 7.838 | 11.330 | |
| Anxiety symptoms↔Cognitive dysfunction | 36.43 | 4.09 | 0.42 | <0.001 | 29.323 | 45.488 | |
| Depressive symptoms↔Cognitive dysfunction | 44.14 | 4.34 | 0.52 | <0.001 | 36.293 | 53.368 | |
| Pain at 4kg - Pubic↔Pain at 4kg - Arm | 358.22 | 24.37 | 0.66 | <0.001 | 316.690 | 414.432 | |
| Age↔College graduate | 0.33 | 0.32 | 0.05 | 0.302 | −0.308 | 0.960 | |
| Age↔Female | −1.25 | 0.30 | −0.17 | <0.001 | −1.858 | −0.660 | |
| College graduate↔Female | −0.005 | 0.01 | −0.02 | 0.581 | −0.023 | 0.012 | |
Note. SE = Standard Error. CI = Confidence Interval. Boldfaced values are significant coefficients in which the bias-corrected boostrap 95% CI does not contain zero.
Probing indirect effects.
Specific indirect effects are shown in Table 6. Overall, there was a significant total indirect effect of childhood trauma on pain sensitivity at both the pubic region and the arm. Experiencing childhood sexual violent trauma and childhood nonsexual violent trauma were significantly associated with pain sensitivity in the pubic region. Childhood nonsexual violent trauma carried the majority of the total indirect effect. Experiencing childhood sexual violent trauma also contributed a significant minority of the total indirect effect. The impact of nonviolent trauma was small. The proportion of the specific indirect effect for both sexual and nonsexual violent trauma during childhood suggests that generalized sensory sensitivity was the primary mediator of this association.
Table 6.
Specific indirect effects of the association between childhood trauma and pain sensitivity (n = 457)
| BCa Bootstrap 95% CI | Proportion of total indirect effect | Proportion of specific indirect effect | |||||
|---|---|---|---|---|---|---|---|
| Outcome | Indirect path | Coef. | Bootstrap SE | LL | UL | ||
|
| |||||||
| →Pain at 4kg - pubic | |||||||
| Total childhood sexual violent trauma via GSS, Depressive Symptoms, Anxiety Symptoms, and CD | 1.946 | 0.93 | 0.326 | 3.944 | 0.414 | ||
| via GSS | 1.321 | 0.69 | 0.313 | 3.121 | 0.582 | ||
| via Depressive Symptoms | 0.277 | 0.48 | −0.381 | 1.658 | 0.122 | ||
| via Anxiety Symptoms | −0.162 | 0.36 | −1.208 | 0.352 | 0.071 | ||
| via CD | 0.510 | 0.48 | −0.084 | 1.932 | 0.225 | ||
| Total childhood nonsexual violent trauma via GSS, Depressive Symptoms, Anxiety Symptoms, and CD | 2.534 | 1.07 | 0.719 | 5.016 | 0.524 | ||
| via GSS | 1.936 | 0.85 | 0.645 | 4.081 | 0.674 | ||
| via Depressive Symptoms | 0.142 | 0.33 | −0.209 | 1.438 | 0.049 | ||
| via Anxiety Symptoms | −0.169 | 0.37 | −1.250 | 0.375 | 0.059 | ||
| via CD | 0.625 | 0.51 | −0.014 | 2.150 | 0.218 | ||
| Total childhood nonviolent trauma sum via GSS, Depressive Symptoms, Anxiety Symptoms, and CD | 0.067 | 0.39 | −0.697 | 0.846 | 0.062 | ||
| via GSS | 0.130 | 0.23 | −0.291 | 0.664 | 0.386 | ||
| via Depressive Symptoms | 0.072 | 0.16 | −0.099 | 0.613 | 0.214 | ||
| via Anxiety Symptoms | −0.011 | 0.10 | −0.345 | 0.127 | 0.033 | ||
| via CD | −0.124 | 0.19 | −0.666 | 0.141 | 0.368 | ||
| Total indirect effect | 4.547 | 1.37 | 2.199 | 7.630 | |||
| →Pain at 4kg - arm | |||||||
| Total childhood sexual violent trauma via GSS, Depressive Symptoms, Anxiety Symptoms, and CD | 1.025 | 0.78 | −0.428 | 2.708 | 0.447 | ||
| via GSS | 0.904 | 0.53 | 0.139 | 2.360 | 0.335 | ||
| via Depressive Symptoms | 0.588 | 0.52 | −0.056 | 2.094 | 0.218 | ||
| via Anxiety Symptoms | −0.838 | 0.63 | −2.579 | −0.001 | 0.310 | ||
| via CD | 0.370 | 0.38 | −0.065 | 1.576 | 0.137 | ||
| Total childhood nonsexual violent trauma via GSS, Depressive Symptoms, Anxiety Symptoms, and CD | 1.205 | 0.88 | −0.328 | 3.166 | 0.489 | ||
| via GSS | 1.326 | 0.70 | 0.274 | 3.137 | 0.449 | ||
| via Depressive Symptoms | 0.301 | 0.41 | −0.185 | 1.639 | 0.102 | ||
| via Anxiety Symptoms | −0.874 | 0.60 | −2.527 | −0.028 | 0.296 | ||
| via CD | 0.453 | 0.42 | −0.049 | 1.760 | 0.153 | ||
| Total childhood nonviolent trauma sum via GSS, Depressive | 0.093 | 0.32 | −0.539 | 0.735 | 0.064 | ||
| Symptoms, Anxiety Symptoms, and CD | |||||||
| via GSS | 0.089 | 0.17 | −0.182 | 0.521 | 0.229 | ||
| via Depressive Symptoms | 0.152 | 0.19 | −0.063 | 0.778 | 0.391 | ||
| via Anxiety Symptoms | −0.058 | 0.25 | −0.627 | 0.408 | 0.149 | ||
| via CD | −0.090 | 0.15 | −0.557 | 0.087 | 0.231 | ||
| Total indirect effect | 2.323 | 1.13 | 0.266 | 4.718 | |||
Note. SE = Standard Error. BCa = Bias-corrected and Accelerated. CI = Confidence Interval. LL = Lower Limit. UL = Upper Limit. Boldfaced values are significant coefficients in which the bias-corrected and accelerated boostrap 95% CI does not contain zero. Proportion of total and specific indirect effect is calculated by dividing the indirect effect by the sum of absolute values of coefficients included. Proportion of total indirect effect calculates the proportion of the total indirect effect by each distal predictor (childhood sexual violent trauma; childhood nonsexual violent trauma; childhood nonviolent trauma sum) regardless of mediator. Proportion of specific indirect effect calculates the proportion of the impact of each specific mediator for each distal predictor (childhood sexual violent trauma; childhood nonsexual violent trauma; childhood nonviolent trauma sum).
Experiencing childhood sexual and nonsexual violent trauma were both significantly associated with higher pain sensitivity at the arm through generalized sensory sensitivity, although the overall impact of childhood violent trauma was nonsignificant. This is likely due to the counterintuitive impact of experiencing childhood sexual and nonsexual violent trauma on lower pain sensitivity through anxiety symptoms. The calculated proportion of indirect effects was consistent, however, with childhood sexual and nonsexual violent trauma carrying the majority of the total indirect effect. Generalized sensory sensitivity carried the majority of the specific indirect effect.
Discussion
Research evaluating the impact of childhood trauma on experimental pain sensitivity has been mixed[21; 57; 59; 62; 65; 77; 90]. To our knowledge, few studies have considered potential mediators of this association[59], although research suggests that individual-level characteristics such as trauma sequelae may impact this association[15; 16; 28; 78; 90]. Our findings suggest that, among UCPPS participants, childhood trauma may be associated with heightened pain sensitivity to the extent that trauma history is associated with a subsequent increase in generalized sensory sensitivity.
Traumatic experiences are common and associated with worse symptoms.
Our findings suggest that about one out of five individuals with UCPPS experienced childhood sexual violent trauma or childhood nonsexual violent trauma. Combined across both types of sexual and nonsexual violent trauma, 31.3% reported one or both forms. In a nationally representative sample of adults in the United States, approximately 17.9% reported childhood physical abuse and 11.6% reported childhood sexual abuse[47]. Among healthy controls in the MAPP Research Network, 10% reported childhood sexual violent trauma and 9% reported childhood nonsexual violent trauma[66]. Prevalence rates of childhood sexual and physical abuse across previous studies of individuals with pelvic pain are generally higher, but vary widely (19.4%-62.5%)[5; 12; 41; 42; 60; 82]. Our prevalence rates fit within this range. Additionally, other potentially traumatic events during childhood frequently co-occurred. This high rate of co-occurrence has been supported by previous research[18; 20; 63].
Sexual and nonsexual violent trauma during childhood were directly associated with negative health-related outcomes. In particular, childhood sexual violent trauma was associated with higher depressive symptoms, anxiety symptoms, cognitive dysfunction, and generalized sensory sensitivity, whereas childhood nonsexual violent trauma was directly associated with higher cognitive dysfunction and generalized sensory sensitivity. Previous research supports the far-reaching health consequences of childhood trauma[20; 35; 48]. Childhood trauma may lead to a cascade of inter-related biological and psychological outcomes including, but not limited to, alterations in neurobiological systems responsible for threat perception and sensory processing; immune dysregulation; altered physiological reactivity to stress; and higher rates of mental health disorders (e.g., PTSD, depression, and anxiety)[19; 31; 35; 46; 48; 73; 75; 85]. Sexual and nonsexual violent trauma may be especially linked to negative health consequences due to the interpersonal nature of the event and the potential sense of betrayal that accompanies these forms of trauma[24; 26]. Betrayal is a violation of trust that can have a severe impact on one’s sense of self, others, and the world in general and is considered distinct from the stereotypical fear considered as the core of the trauma response[24]. However, we were unable to assess the role of perceived betrayal due to the limitations of our data.
Recent trauma in adulthood may also be an important conduit for the impact of childhood trauma on health-related outcomes. Our findings suggest that a mechanistic model in which recent adult trauma load acts as a partial mediator linking childhood trauma to affective distress, cognitive dysfunction, and generalized sensory sensitivity best fit the observed data structure. Previous research suggests that childhood trauma is associated with trauma load in adulthood[7; 17]. The reasons for this are complex and multifaceted. In addition to the previously mentioned impact of trauma on biological and psychological outcomes, trauma has also been linked to increased risk behavior and alterations in social information processing[45; 80]. The multitudinous consequences of childhood trauma may have contributed to the recent trauma load, particularly reflected by future traumatic health problems, violence exposure, and unspecified trauma, reported in the present sample[35; 48; 55]. These associations may also highlight the persistent contextual disadvantage in which many individuals who experience childhood trauma are embedded across their lifetime[55].
Our findings further suggest that recent trauma load in adulthood is more strongly associated with current symptoms compared to distal childhood trauma experiences. Previous research similarly suggests that proximal traumatic experiences may be more important for pain related outcomes compared to childhood abuse[5]. In addition to temporal proximity, recent trauma load may contribute to overwhelming stress and an inability to adapt resulting in dysregulation of the nervous, endocrine, and immune systems[29]. This dysregulation can impact affective distress, cognitive dysfunction, and indicators of nociplastic pain, which may also overlap with posttraumatic stress symptoms[29; 58]. Importantly, some of the effect of childhood trauma on pain-related outcomes in adulthood may be through its association with an increased trauma load throughout life, representing just one possible mechanistic pathway[55]. The complex and long-term trajectories of childhood trauma highlight the critical need for empathic, trauma-informed care for patients with UCPPS and other chronic pain diagnoses. Additionally, trauma history assessment and PTSD/Complex PTSD screening among patients with UCPPS are necessary as these conditions tend to be underdiagnosed, undertreated, and may lead to worse symptoms and poor treatment response.
Generalized sensory sensitivity plays an important role in the association between childhood trauma and pain sensitivity.
Generalized sensory sensitivity was an important mechanism conveying the effect of childhood trauma on heightened pain sensitivity in both pelvic and nonpelvic sites. These findings echo those in previous research utilizing the MAPP data, in which generalized sensory sensitivity was associated with suprathreshold pain sensitivity at a nonpelvic site[34]. Generalized sensory sensitivity appears to be a core component of the nociplastic pain phenotype[67], in which altered central nervous system factors are believed to lead to the amplification and/or dysregulation of sensory stimuli and the spatial spread of pain[88]. For example, previous research has shown increased visual and auditory sensitivity among patients with fibromyalgia[25; 33]. Although the cause of centralized pain is unclear, numerous precipitating factors have been proposed, including interactions between genetic vulnerability and environmental factors such as traumatic stress[9]. PTSD is also associated with alterations in brain structure and function indicative of disordered multisensory processing[31]; these regions (e.g., thalamus; posterior and anterior insula) at least crudely correspond to those implicated in the experience of physical pain intensity[33; 50; 68; 81]. Indeed, previous research has linked trauma, particularly violent trauma, to the components of generalized sensory sensitivity as well as conditions indicative of nociplastic pain[1; 53; 57]. Recent research also suggests that posttraumatic stress symptoms may uniquely contribute to somatic awareness and external sensory sensitivity after accounting for chronic pain[58]. Thus, some UCPPS patients may exhibit a nociplastic pain phenotype, potentially impacted by traumatic stress during childhood, which in turn affects sensitivity to painful stimuli. Importantly, although self-reported increases in generalized sensory sensitivity requires subjective evaluations filtered through a cognitive and affective lens, it nevertheless likely reflects a physiological component of nociplastic pain. Therefore, clinicians and researchers should recognize the physiological impact of trauma and its consequent role in the pain and broader sensory experience. Incorporating a simple body map or brief measure of generalized sensory sensitivity[67] into research and practice may aid in advancing this goal.
Sexual and nonsexual violent trauma during childhood were associated with higher cognitive dysfunction which, in turn, was associated with higher pain sensitivity. Despite these direct associations, the specific indirect effects failed to reach significance. Previous research supports the link between childhood trauma and worse cognitive functioning[89], which is a cardinal symptom of centralized pain[86]. These findings warrant more extensive evaluations of the role of cognitive dysfunction in the association between trauma and pain sensitivity, particularly in the context of other centralized pain characteristics.
Strengths and Limitations
The MAPP SPS is the largest study evaluating pain perception among UCPPS patients. Additionally, although the survey data included in our model utilized cross-sectional data, the referenced time frames (i.e., childhood, recent events [within the past 3 years], current symptoms) in combination with QST data supports the temporal relationships presented in the mediation model. However, several limitations are worth noting. We considered ratings of standardized, suprathreshold pain stimuli. This included only pain intensity ratings from a single modality (i.e., pressure pain). Other QST measures would be important to consider. We did not assess how specific pelvic pain disorders may have impacted these findings, which may be an important area for future research. Our measure of trauma was also limited. Due to the wording of the questions about sexual and nonsexual violent trauma, participants would need to subjectively consider their past experiences as trauma. Many survivors of childhood abuse, however, do not label the experiences as abuse[30]. Future studies should consider the use of behaviorally specific measures of childhood trauma. Additionally, future studies should evaluate the role of emotional abuse and neglect and other types of adverse childhood experiences[20; 23], which may be differentially associated with health-related and pain perception outcomes. We also did not consider other factors related to the traumatic experience (e.g., age at time of event). Finally, we combined men and women in our model. Future research should explore these associations among men, women, transgender, and non-binary individuals.
Conclusion
Our findings suggest that sexual and nonsexual violent trauma during childhood are indirectly associated with pain sensitivity among adult UCPPS patients. Heightened generalized sensory sensitivity played a unique role in conveying these effects, highlighting the need for clinicians and researchers to recognize the importance of physiological sensitivity to the pain experience for individuals with a history of childhood trauma.
Supplementary Material
Acknowledgments
The MAPP Research Network acknowledges support through NIH grants (DK082370, DK082342, DK082315, DK082344, DK082325, DK082345, DK082333, DK082316). JP was supported by a Postdoctoral Translational Scholar Program training grant from the Michigan Institute for Clinical and Health Research (UL1TR002240) in support of the current study and also receives funding from the National Institute of Mental Health (K01MH126079). SEH has received research support from Aptinyx and Arbor Medical Innovations, and consultation fees from Aptinyx, Memorial Slone Kettering Cancer Research, Indiana University and University of North Carolina – Chapel Hill; not related to the present work. CSB and LVR received royalties from Elsevier not related to this work. SL received research support from National Institute of Diabetes and Digestive and Kidney Diseases. BJT received research funding from the National Institute of Mental Health (T32MH115882). DAW received consultation fees from Swing Therapeutics, Inc., and Community Health Focus, Inc., not related to the present work. The NIDDK and MAPP Network investigators wish to thank the Interstitial Cystitis Association and the Prostatitis Foundation for their assistance in study participant recruitment and other network efforts, as well as all the participants who enrolled in these important research studies.
Funding
Funding for the MAPP Research Network was obtained under a cooperative agreement from National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institutes of Health (Grant numbers DK082370, DK082342, DK082315, DK082344, DK082325, DK082345, DK082333, DK082316). JP was supported by a Postdoctoral Translational Scholar Program training grant from the Michigan Institute for Clinical and Health Research (UL1TR002240; PI: George Mashour) in support of the current study.
References
- [1].Afari N, Ahumada SM, Wright LJ, Mostoufi S, Golnari G, Reis V, & Cuneo JG Psychological trauma and functional somatic syndromes: A systematic review and meta-analysis. Psychosomatic Medicine 2014;76(1):2–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Afari N, Buchwald D, Clauw D, Hong B, Hou X, Krieger JN, Mullins C, Stephens-Shields AJ, Gasperi M, Williams DA, Network MR. A MAPP Network Case-control Study of Urological Chronic Pelvic Pain Compared With Nonurological Pain Conditions. Clin J Pain 2020;36(1):8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin 1988;103(3):411–423. [Google Scholar]
- [4].Arendt-Nielsen L, Yarnitsky D. Experimental and clinical applications of quantitative sensory testing applied to skin, muscles and viscera. J Pain 2009;10(6):556–572. [DOI] [PubMed] [Google Scholar]
- [5].As-Sanie S, Clevenger LA, Geisser ME, Williams DA, Roth RS. History of abuse and its relationship to pain experience and depression in women with chronic pelvic pain. Am J Obstet Gynecol 2014;210(4):317 e311–317 e318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Berry SH, Elliott MN, Suttorp M, Bogart LM, Stoto MA, Eggers P, Nyberg L, Clemens JQ. Prevalence of symptoms of bladder pain syndrome/interstitial cystitis among adult females in the United States. J Urol 2011;186(2):540–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Burgin D, Boonmann C, Schmeck K, Schmid M, Tripp P, Nishimi K, O’Donovan A. Compounding Stress: Childhood Adversity as a Risk Factor for Adulthood Trauma Exposure in the Health and Retirement Study. J Trauma Stress 2021;34(1):124–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Clauw DJ. Fibromyalgia: a clinical review. JAMA 2014;311(15):1547–1555. [DOI] [PubMed] [Google Scholar]
- [9].Clauw DJ, Chrousos GP. Chronic pain and fatigue syndromes: overlapping clinical and neuroendocrine features and potential pathogenic mechanisms. Neuroimmunomodulation 1997;4(3):134–153. [DOI] [PubMed] [Google Scholar]
- [10].Clemens JQ, Kutch JJ, Mayer EA, Naliboff BD, Rodriguez LV, Klumpp DJ, Schaeffer AJ, Kreder KJ, Clauw DJ, Harte SE, Schrepf AD, Williams DA, Andriole GL, Lai HH, Buchwald D, Lucia MS, van Bokhoven A, Mackey S, Moldwin RM, Pontari MA, Stephens-Shields AJ, Mullins C, Landis JR. The Multidisciplinary Approach to The Study of Chronic Pelvic Pain (MAPP) Research Network*: Design and implementation of the Symptom Patterns Study (SPS). Neurourol Urodyn 2020;39(6):1803–1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Clemens JQ, Mullins C, Ackerman AL, Bavendam T, van Bokhoven A, Ellingson BM, Harte SE, Kutch JJ, Lai HH, Martucci KT, Moldwin R, Naliboff BD, Pontari MA, Sutcliffe S, Landis JR, Group MRNS. Urologic chronic pelvic pain syndrome: insights from the MAPP Research Network. Nat Rev Urol 2019;16(3):187–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Collett BJ, Cordle CJ, Stewart CR, Jagger C. A comparative study of women with chronic pelvic pain, chronic nonpelvic pain and those with no history of pain attending general practitioners. Br J Obstet Gynaecol 1998;105(1):87–92. [DOI] [PubMed] [Google Scholar]
- [13].Cruz-Almeida Y, Fillingim RB. Can quantitative sensory testing move us closer to mechanism-based pain management? Pain Med 2014;15(1):61–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Defrin R, Ginzburg K, Solomon Z, Polad E, Bloch M, Govezensky M, Schreiber S. Quantitative testing of pain perception in subjects with PTSD--implications for the mechanism of the coexistence between PTSD and chronic pain. Pain 2008;138(2):450–459. [DOI] [PubMed] [Google Scholar]
- [15].Defrin R, Lahav Y, Solomon Z. Dysfunctional Pain Modulation in Torture Survivors: The Mediating Effect of PTSD. J Pain 2017;18(1):1–10. [DOI] [PubMed] [Google Scholar]
- [16].Defrin R, Schreiber S, Ginzburg K. Paradoxical Pain Perception in Posttraumatic Stress Disorder: The Unique Role of Anxiety and Dissociation. J Pain 2015;16(10):961–970. [DOI] [PubMed] [Google Scholar]
- [17].Desai S, Arias I, Thompson MP, Basile KC. Childhood victimization and subsequent adult revictimization assessed in a nationally representative sample of women and men. Violence Vict 2002;17(6):639–653. [DOI] [PubMed] [Google Scholar]
- [18].Dong M, Anda RF, Dube SR, Giles WH, Felitti VJ. The relationship of exposure to childhood sexual abuse to other forms of abuse, neglect, and household dysfunction during childhood. Child Abuse Negl 2003;27(6):625–639. [DOI] [PubMed] [Google Scholar]
- [19].Fagundes CP, Glaser R, Kiecolt-Glaser JK. Stressful early life experiences and immune dysregulation across the lifespan. Brain Behav Immun 2013;27(1):8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine 1998;14(4):245–258. [DOI] [PubMed] [Google Scholar]
- [21].Fillingim RB, Edwards RR. Is self-reported childhood abuse history associated with pain perception among healthy young women and men? Clin J Pain 2005;21(5):387–397. [DOI] [PubMed] [Google Scholar]
- [22].Fillingim RB, Maixner W, Sigurdsson A, Kincaid S. Sexual and physical abuse history in subjects with temporomandibular disorders: relationship to clinical variables, pain sensitivity, and psychologic factors. J Orofac Pain 1997;11(1):48–57. [PubMed] [Google Scholar]
- [23].Finkelhor D, Shattuck A, Turner H, Hamby S. A revised inventory of Adverse Childhood Experiences. Child Abuse Negl 2015;48:13–21. [DOI] [PubMed] [Google Scholar]
- [24].Freyd JJ, Klest B, Allard CB. Betrayal trauma: relationship to physical health, psychological distress, and a written disclosure intervention. J Trauma Dissociation 2005;6(3):83–104. [DOI] [PubMed] [Google Scholar]
- [25].Geisser ME, Glass JM, Rajcevska LD, Clauw DJ, Williams DA, Kileny PR, Gracely RH. A psychophysical study of auditory and pressure sensitivity in patients with fibromyalgia and healthy controls. J Pain 2008;9(5):417–422. [DOI] [PubMed] [Google Scholar]
- [26].Goldsmith RE, Freyd JJ, DePrince AP. Betrayal trauma: associations with psychological and physical symptoms in young adults. J Interpers Violence 2012;27(3):547–567. [DOI] [PubMed] [Google Scholar]
- [27].Gomez-Perez L, Lopez-Martinez AE. Association of trauma, posttraumatic stress disorder, and experimental pain response in healthy young women. Clin J Pain 2013;29(5):425–434. [DOI] [PubMed] [Google Scholar]
- [28].Granot M, Somer E, Zisman-Ilani Y, Beny A, Sadger R, Mirkin R, Moont R, Yovell Y. Characteristics of response to experimental pain in sexually abused women. Clin J Pain 2011;27(7):616–622. [DOI] [PubMed] [Google Scholar]
- [29].Guidi J, Lucente M, Sonino N, Fava GA. Allostatic Load and Its Impact on Health: A Systematic Review. Psychother Psychosom 2021;90(1):11–27. [DOI] [PubMed] [Google Scholar]
- [30].Hammond CB, Calhoun KS. Labeling of abuse experiences and rates of victimization. Psychology of Women Quarterly 2007;31:371–380. [Google Scholar]
- [31].Harricharan S, McKinnon MC, Lanius RA. How processing of sensory information from the internal and external worlds shape the perception and engagement with the world in the aftermath of trauma: Implications for PTSD. Front Neuroscience 2021;15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Harte S, Harris R, Clauw D. The neurobiology of central sensitization. Journal of Applied Biobehavioral Research 2018;23, 10.1111/jabr.12137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Harte SE, Ichesco E, Hampson JP, Peltier SJ, Schmidt-Wilcke T, Clauw DJ, Harris RE. Pharmacologic attenuation of cross-modal sensory augmentation within the chronic pain insula. Pain 2016;157(9):1933–1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Harte SE, Schrepf A, Gallop R, Kruger GH, Lai HHH, Sutcliffe S, Halvorson M, Ichesco E, Naliboff BD, Afari N, Harris RE, Farrar JT, Tu F, Landis JR, Clauw DJ, Network MR. Quantitative assessment of nonpelvic pressure pain sensitivity in urologic chronic pelvic pain syndrome: a MAPP Research Network study. Pain 2019;160(6):1270–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Kendall-Tackett K. The health effects of childhood abuse: four pathways by which abuse can influence health. Child Abuse Negl 2002;26(6–7):715–729. [DOI] [PubMed] [Google Scholar]
- [36].Kosek E, Cohen M, Baron R, Gebhart GF, Mico JA, Rice AS, Rief W, Sluka AK. Do we need a third mechanistic descriptor for chronic pain states? Pain 2016;157(7):1382–1386. [DOI] [PubMed] [Google Scholar]
- [37].Krieger JN, Stephens AJ, Landis JR, Clemens JQ, Kreder K, Lai HH, Afari N, Rodriguez L, Schaeffer AJ, Mackey SC, Andriole GL, Williams DA, Network MR. Relationship between chronic non-urological associated somatic syndromes (NUAS) and symptom severity in urological chronic pelvic pain syndromes: Baseline evaluation of the Multidisciplinary Approach to the Study of Chronic Pelvic Pain (MAPP) Study. J Urol 2015;193(4):1254–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Lai H, Bayman EO, Bishop MO, Landis R, Harte SE, Clemens Q, Rodriguez LV, Sutcliffe S, Taple BJ, Naliboff BD, Network MR. Longitudinal Changes in the Pelvic Pain Only and Widespread Pain Phenotypes Over One Year in the MAPP-I Urologic Chronic Pelvic Pain Syndrome (UCPPS) Cohort. Urology 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Lai HH, Gardner V, Ness TJ, Gereau RWt. Segmental hyperalgesia to mechanical stimulus in interstitial cystitis/bladder pain syndrome: evidence of central sensitization. J Urol 2014;191(5):1294–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Lai HH, Jemielita T, Sutcliffe S, Bradley CS, Naliboff B, Williams DA, Gereau RWt, Kreder K, Clemens JQ, Rodriguez LV, Krieger JN, Farrar JT, Robinson N, Landis JR, Network MR. Characterization of Whole Body Pain in Urological Chronic Pelvic Pain Syndrome at Baseline: A MAPP Research Network Study. J Urol 2017;198(3):622–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Lampe A, Doering S, Rumpold G, Solder E, Krismer M, Kantner-Rumplmair W, Schubert C, Sollner W. Chronic pain syndromes and their relation to childhood abuse and stressful life events. J Psychosom Res 2003;54(4):361–367. [DOI] [PubMed] [Google Scholar]
- [42].Lampe A, Solder E, Ennemoser A, Schubert C, Rumpold G, & Sollner W Chronic pelvic pain and previous sexual abuse. Obstetrics & Gynecology 2000;96(6):929–933. [DOI] [PubMed] [Google Scholar]
- [43].Landis JR, Williams DA, Lucia MS, Clauw DJ, Naliboff BD, Robinson NA, van Bokhoven A, Sutcliffe S, Schaeffer AJ, Rodriguez LV, Mayer EA, Lai HH, Krieger JN, Kreder KJ, Afari N, Andriole GL, Bradley CS, Griffith JW, Klumpp DJ, Hong BA, Lutgendorf SK, Buchwald D, Yang CC, Mackey S, Pontari MA, Hanno P, Kusek JW, Mullins C, Clemens JQ, & The MAPP Research Network Study Group. The MAPP research network: Design, patient characterization and operations. BMC Urology 2014;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Latthe P, Mignini L, Gray R, Hills R, Khan K. Factors predisposing women to chronic pelvic pain: systematic review. BMJ 2006;332(7544):749–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Layne CM, Greeson JKP, Ostrowski SA, Kim S, Reading S, Vivrette RL, Briggs EC, Fairbank JA, Pynoos RS. Cumulative trauma exposure and high risk behavior in adolescence: Findings from the National Child Traumatic Stress Network core data set. Psychological Trauma: Theory, Research, Practice, and Policy 2014;6:S40–S49. [Google Scholar]
- [46].Lindert J, von Ehrenstein OS, Grashow R, Gal G, Braehler E, Weisskopf MG. Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis. Int J Public Health 2014;59(2):359–372. [DOI] [PubMed] [Google Scholar]
- [47].Merrick MT, Ford DC, Ports KA, Guinn AS. Prevalence of Adverse Childhood Experiences From the 2011–2014 Behavioral Risk Factor Surveillance System in 23 States. JAMA Pediatr 2018;172(11):1038–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol Bull 2011;137(6):959–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Naliboff BD, Stephens AJ, Afari N, Lai H, Krieger JN, Hong B, Lutgendorf S, Strachan E, Williams D, Network MR. Widespread Psychosocial Difficulties in Men and Women With Urologic Chronic Pelvic Pain Syndromes: Case-control Findings From the Multidisciplinary Approach to the Study of Chronic Pelvic Pain Research Network. Urology 2015;85(6):1319–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Napadow V, LaCount L, Park K, As-Sanie S, Clauw DJ, Harris RE. Intrinsic brain connectivity in fibromyalgia is associated with chronic pain intensity. Arthritis Rheum 2010;62(8):2545–2555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Nelson J, Klumparendt A, Doebler P, Ehring T. Childhood maltreatment and characteristics of adult depression: meta-analysis. Br J Psychiatry 2017;210(2):96–104. [DOI] [PubMed] [Google Scholar]
- [52].Neville SJ, Clauw AD, Moser SE, Urquhart AG, Clauw DJ, Brummett CM, Harte SE. Association Between the 2011 Fibromyalgia Survey Criteria and Multisite Pain Sensitivity in Knee Osteoarthritis. Clin J Pain 2018;34(10):909–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Nicol AL, Sieberg CB, Clauw DJ, Hassett AL, Moser SE, & Brummett CM The association between a history of lifetime traumatic events and pain severity, physical function, and affective distress in patients with chronic pain. The Journal of Pain 2016;17(2):1334–1348. [DOI] [PubMed] [Google Scholar]
- [54].International Association for the Study of Pain. Terminology. (2021). Accessed January 19, 2023. https://www.iasp-pain.org/resources/terminology/
- [55].Pearlin LI, Schieman S, Fazio EM, Meersman SC. Stress, health, and the life course: some conceptual perspectives. J Health Soc Behav 2005;46(2):205–219. [DOI] [PubMed] [Google Scholar]
- [56].Pennebaker JW, Susman JR. Disclosure of traumas and psychosomatic processes. Soc Sci Med 1988;26(3):327–332. [DOI] [PubMed] [Google Scholar]
- [57].Pierce J, Hassett AL, Brummett CM, McAfee J, Sieberg C, Schrepf A, Harte SE. Characterizing Pain and Generalized Sensory Sensitivity According to Trauma History Among Patients With Knee Osteoarthritis. Ann Behav Med 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Pierce J, Mohan N, Fatabhoy M, McAfee J, Zhu G, Hassett A. Posttraumatic stress symptoms and chronic pain: Cross-sectional associations with perception of sensory and social stimuli. Mental Health Science 2022;1(1), 23–36. 10.1002/mhs2.8. [DOI] [Google Scholar]
- [59].Pieritz K, Rief W, Euteneuer F. Childhood adversities and laboratory pain perception. Neuropsychiatr Dis Treat 2015;11:2109–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Rapkin AJ, Kames LD, Darke LL, Stampler FM, Naliboff BD. History of physical and sexual abuse in women with chronic pelvic pain. Obstet Gynecol 1990;76(1):92–96. [PubMed] [Google Scholar]
- [61].Raykov T, Marcoulides GA. A first course in structural equation modeling: Lawrence Erlbaum Associates Publishers, Mahwah, New Jersey, 2006. [Google Scholar]
- [62].Ringel Y, Whitehead WE, Toner BB, Diamant NE, Hu Y, Jia H, Bangdiwala SI, Drossman DA. Sexual and physical abuse are not associated with rectal hypersensitivity in patients with irritable bowel syndrome. Gut 2004;53(6):838–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Rosen AL, Handley ED, Cicchetti D, Rogosch FA. The impact of patterns of trauma exposure among low income children with and without histories of child maltreatment. Child Abuse Negl 2018;80:301–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Sansone RA, Gaither GA, Sansone LA. Childhood trauma and adult somatic preoccupation by body area among women in an internal medicine setting: A pilot study. Int J Psychiat Med 2001;31(2):147–154. [DOI] [PubMed] [Google Scholar]
- [65].Scarinci IC, McDonald-Haile J, Bradley LA, Richter JE. Altered pain perception and psychosocial features among women with gastrointestinal disorders and history of abuse: a preliminary model. Am J Med 1994;97(2):108–118. [DOI] [PubMed] [Google Scholar]
- [66].Schrepf A, Naliboff B, Williams DA, Stephens-Shields AJ, Landis JR, Gupta A, Mayer E, Rodriguez LV, Lai H, Luo Y, Bradley C, Kreder K, Lutgendorf SK, Network MR. Adverse Childhood Experiences and Symptoms of Urologic Chronic Pelvic Pain Syndrome: A Multidisciplinary Approach to the Study of Chronic Pelvic Pain Research Network Study. Ann Behav Med 2018;52(10):865–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Schrepf A, Williams DA, Gallop R, Naliboff BD, Basu N, Kaplan C, Harper DE, Landis JR, Clemens JQ, Strachan E, Griffith JW, Afari N, Hassett A, Pontari MA, Clauw DJ, Harte SE, Network MR. Sensory sensitivity and symptom severity represent unique dimensions of chronic pain: a MAPP Research Network study. Pain 2018;159(10):2002–2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Segerdahl AR, Mezue M, Okell TW, Farrar JT, Tracey I. The dorsal posterior insula subserves a fundamental role in human pain. Nat Neurosci 2015;18(4):499–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Seidenberg M, Haltiner A, Taylor MA, Hermann BB, Wyler A. Development and validation of a Multiple Ability Self-Report Questionnaire. J Clin Exp Neuropsychol 1994;16(1):93–104. [DOI] [PubMed] [Google Scholar]
- [70].Serafini G, Gonda X, Pompili M, Rihmer Z, Amore M, & Engel-Yeger B The relationship between sensory processing patterns, alexithymia, traumatic childhood experiences, and quality of life among patients with unipolar and bipolar disorders. Child Abuse & Neglect 2016;62:39–50. [DOI] [PubMed] [Google Scholar]
- [71].Sharp TJ, Harvey AG. Chronic pain and posttraumatic stress disorder: mutual maintenance? Clin Psychol Rev 2001;21(6):857–877. [DOI] [PubMed] [Google Scholar]
- [72].Sherman AL, Morris MC, Bruehl S, Westbrook TD, Walker LS. Heightened Temporal Summation of Pain in Patients with Functional Gastrointestinal Disorders and History of Trauma. Ann Behav Med 2015;49(6):785–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Sigurdardottir S, Halldorsdottir S, Bender SS. Consequences of childhood sexual abuse for health and well-being: gender similarities and differences. Scand J Public Health 2014;42(3):278–286. [DOI] [PubMed] [Google Scholar]
- [74].Teicher MH, Samson JA. Annual Research Review: Enduring neurobiological effects of childhood abuse and neglect. J Child Psychol Psychiatry 2016;57(3):241–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Teicher MH, Samson JA, Anderson CM, Ohashi K. The effects of childhood maltreatment on brain structure, function and connectivity. Nat Rev Neurosci 2016;17(10):652–666. [DOI] [PubMed] [Google Scholar]
- [76].Tesarz J, Baumeister D, Andersen TE, Vaegter HB. Pain perception and processing in individuals with posttraumatic stress disorder: a systematic review with meta-analysis. Pain Rep 2020;5(5):e849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Tesarz J, Eich W, Treede R, & Gerhardt A Altered pressure pain thresholds and increased wind-up in adult patients with chronic back pain with a history of childhood maltreatment: A quantitative sensory testing study. Pain 2016;157(8):1799–1809. [DOI] [PubMed] [Google Scholar]
- [78].Tesarz J, Gerhardt A, Leisner S, Janke S, Treede RD, Eich W. Distinct quantitative sensory testing profiles in nonspecific chronic back pain subjects with and without psychological trauma. Pain 2015;156(4):577–586. [DOI] [PubMed] [Google Scholar]
- [79].van der Kolk BA. The body keeps the score: Memory and the evolving psychobiology of posttraumatic stress. Harvard Rev Psychiatry 1994;1:253–265. [DOI] [PubMed] [Google Scholar]
- [80].van Reemst L, Fischer TF, Zwirs BW. Social Information Processing Mechanisms and Victimization: A Literature Review. Trauma Violence Abuse 2016;17(1):3–25. [DOI] [PubMed] [Google Scholar]
- [81].Wager TD, Atlas LY, Lindquist MA, Roy M, Woo CW, Kross E. An fMRI-based neurologic signature of physical pain. N Engl J Med 2013;368(15):1388–1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Walling MK, O’Hara MW, Reiter RC, Milburn AK, Lilly G, Vincent SD. Abuse history and chronic pain in women: II. A multivariate analysis of abuse and psychological morbidity. Obstet Gynecol 1994;84(2):200–206. [PubMed] [Google Scholar]
- [83].Westermair AL, Stoll AM, Greggersen W, Kahl KG, Huppe M, Schweiger U. All unhappy childhoods are unhappy in their own way: Differential impact of dimensions of adverse childhood experiences on adult mental health and health behavior. Front Psychiatry 2018;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Whitehead WE, Crowell MD, Davidoff AL, Palsson OS, Schuster MM. Pain from rectal distension in women with irritable bowel syndrome: relationship to sexual abuse. Dig Dis Sci 1997;42(4):796–804. [DOI] [PubMed] [Google Scholar]
- [85].Widom CS. Posttraumatic stress disorder in abused and neglected children grown up. Am J Psychiatry 1999;156(8):1223–1229. [DOI] [PubMed] [Google Scholar]
- [86].Williams DA. Phenotypic Features of Central Sensitization. J Appl Biobehav Res 2018;23(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Williams DA, Schilling S. Advances in the assessment of fibromyalgia. Rheum Dis Clin North Am 2009;35(2):339–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Woolf CJ. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 2011;152(2011):S2–S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Yingying S, D’Arcy C, Shuai Y, Xiangfei M. How does childhood maltreatment influence ensuing cognitive functioning among people with the exposure of childhood maltreatment? A systematic review of prospective cohort studies. Journal of Affective Disorders 2019;252:278–293. [DOI] [PubMed] [Google Scholar]
- [90].You DS, & Meagher MW Childhood adversity and pain sensitization. Psychosomatic Medicine 2016;73:1084–1093. [DOI] [PubMed] [Google Scholar]
- [91].Zigmond AS, & Snaith RP The Hospital and Anxiety Depression Scale. Acta Psychiatrica Scandinavica 1983;67(6):361–370. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


