Abstract
Background:
Providing continuous health insurance coverage during the perinatal period may increase access to and utilization of labor neuraxial analgesia. This study tested the hypothesis that implementation of the 2010 Dependent Coverage Provision of the Patient Protection and Affordable Care Act, requiring private health insurers to allow young adults to remain on their parent’s plan until age 26, was associated with increased labor neuraxial analgesia use.
Methods:
This study used a natural experiment design and birth certificate data for spontaneous vaginal deliveries in 28 US states between 2009 and 2013. The intervention was the Dependent Coverage Provision, categorized into pre- and post-intervention periods (January 2009-August 2010 and September 2010-December 2013, respectively). The exposure was women age, categorized as exposed (21 to 25 years) and unexposed (27 to 31 years). The outcome was the labor neuraxial analgesia utilization rate.
Results:
Of the 4,515,667 birth certificates analyzed, 3,033,129 (67.2%) indicated labor neuraxial analgesia use. For women aged 21 to 25 years, labor neuraxial analgesia utilization rates were 64.9% during the pre-intervention period and 68.9% during the post-intervention period (difference: 4.0%; 95% CI: 3.9, 4.2). For women aged 27 to 31 years, labor neuraxial analgesia utilization rates were 64.9% during the pre-intervention period and 67.7% during the post-intervention period (difference: 2.8%; 95% CI: 2.7, 2.9). After adjustment, implementation of the Dependent Coverage Provision was associated with a 1.0% (95% CI: 0.8, 1.2) absolute increase in labor neuraxial analgesia utilization rate among women aged 21 to 25 years compared with women aged 27 to 31 years. The increase was statistically significant for White and Hispanic women but not for Black and Other race and ethnicity women.
Conclusions:
Implementation of the Dependent Coverage Provision was associated with a statistically significant increase in labor neuraxial analgesia use, but the small effect size unlikely of clinical significance.
Summary Statement:
The Affordable Care Act Dependent Coverage Provision, requiring private health insurers to allow young adults to remain on their parent’s plan until age 26, is associated with a small increase in labor neuraxial analgesia use.
INTRODUCTION
Labor neuraxial analgesia (i.e., spinal, epidural, or combined spinal epidural analgesia) is the safest and most effective technique to alleviate pain during labor and its use is associated with reduced odds of severe maternal morbidity.1–3 Furthermore, labor neuraxial analgesia avoids the use and risks of general anesthesia if an intrapartum cesarean delivery is required.4 In 2015, labor neuraxial analgesia was used in 73% of U.S. births.5 However, labor neuraxial analgesia use is much lower among births to minoritized racial and ethnic women, who are also at increased risk of severe maternal morbidity.6–8 Increasing access to and utilization of labor neuraxial analgesia is therefore suggested as a possible strategy to improve maternal health outcomes and to reduce racial and ethnic disparities in maternal health outcomes.9
Providing continuous health insurance coverage through federal or state health policies, from the preconception to the postpartum, has been reported to improve healthcare access and healthcare utilization during the perinatal period and could be a feasible strategy to increase access to and utilization of labor neuraxial analgesia.10–12 While 75% of non-Hispanic White women had continuous insurance coverage from the preconception to the postpartum in 2015–2017, only 50% of non-Hispanic Black, Indigenous, and Hispanic English-speaking women, and only 20% of Hispanic non-English speaking women had such continuous coverage.13 Provision of continuous health insurance coverage is associated with an earlier initiation and more adequate prenatal care providing the opportunity for counseling women on the risk and benefit balance of analgesic modalities for labor pain management, and reaching shared decision-making on the selected analgesic technique.14 The Dependent Coverage Provision of the Patient Protection and Affordable Care Act implemented nationwide in September 2010 in the United States provides a natural experiment to assess the association of expanded health insurance coverage with labor neuraxial analgesia use. The Dependent Coverage Provision requires private health insurers to allow young adults to remain on their parent’s plan until their 26th birthday. The Dependent Coverage Provision has led to a significant decrease in uninsured women under age 26, an increase in privately insured women, and an increase in early initiation and adequate prenatal care; however, its effect on labor neuraxial analgesia utilization has not been assessed.12,15,16 In this study, we hypothesized that the Dependent Coverage Provision was associated with a significantly increased labor neuraxial analgesia use in women under age 26. Using data for spontaneous vaginal deliveries in 28 states between 2009 and 2013, we assessed the association between the implementation of the Dependent Coverage Provision and labor neuraxial analgesia utilization rate, overall and for minoritized racial and ethnic women.
MATERIALS AND METHODS
The study protocol was deemed exempt by the Institutional Review Board of the Columbia University Irving Medical Center. We report the study according to the STROBE guidelines. No statistical analysis plan was established a priori nor was a clinically meaningful change in labor neuraxial utilization rate associated with the Dependent Coverage Provision defined a priori. The currently presented analysis was based upon the initial analysis combined with changes requested during the peer review process.
Data systems
We analyzed US birth certificate data contained in the restricted access Natality File of the National Vital Statistics System (National Center for Health Statistics, Centers for Diseases Control and Prevention). The Natality File is based on the 2003 revised US Standard Certificate of Live Birth.17 The Standard Certificate of Live Birth was implemented gradually across states, from two states in 2003 to 50 states and the District of Columbia in 2015. The Natality File is a census of all live births in the United States and contains comprehensive information on the woman, labor, and delivery. It also provides county identifiers for the woman’s residence and for the delivery hospital. These identifiers allow abstraction of county characteristics from the Area Health Resource File.18 Area Health Resource File data contain detailed information abstracted from over 50 data sources on health care professions, health facilities, population characteristics, and economics measured at the county level.
Study design
We used the difference-in-differences method to exploit the natural experiment created by the arbitrary age cut-off of the Dependent Coverage Provision (Figure 1). This method has been used in many prior evaluation studies of the Dependent Coverage Provision, as well as other health insurance expansions.12,19–21 Briefly, the difference-in-differences method compares the difference in the mean labor neuraxial analgesia utilization rate before and after the implementation of the Dependent Coverage Provision in women exposed to the Dependent Coverage Provision (i.e., women aged 25 years or younger; first difference) to the difference in the mean labor neuraxial analgesia utilization rate before and after the implementation of the Dependent Coverage Provision in women not exposed to the Dependent Coverage Provision (i.e., women aged 27 years or older; second difference). The difference between these two differences (i.e., difference-in-differences) can be estimated using the regression coefficient of a 2-way interaction term between the age group (indicator of the 21 to 25 years old group) and the period (indicator of the post intervention period) in a linear regression model. For example, a regression coefficient of 0.015 indicates that the Dependent Coverage Provision is associated with a 1.5% (absolute) increase in the probability of labor neuraxial analgesia in women aged 21 to 25 years compared to women aged 27 to 31 years.
Figure 1:
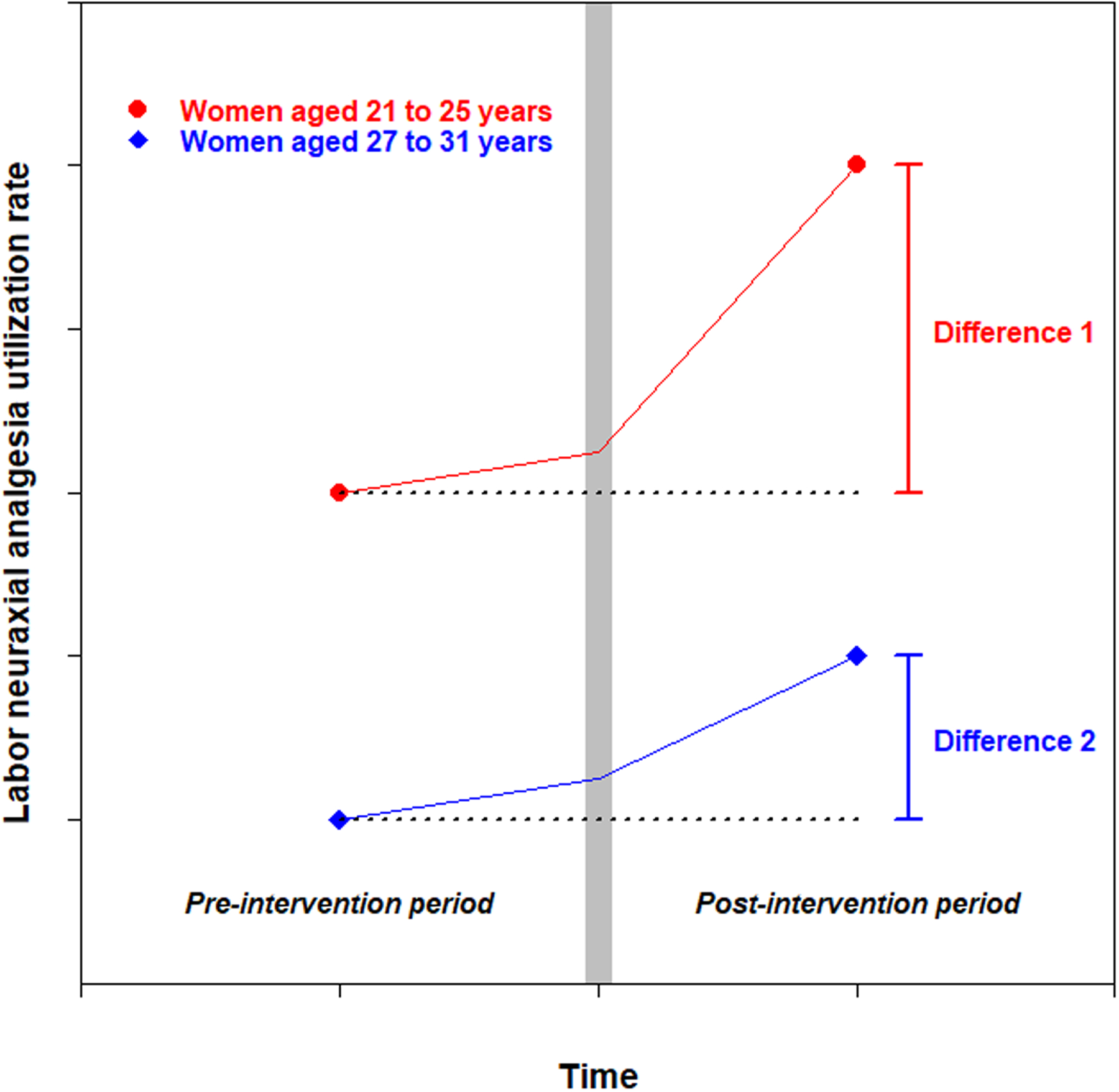
The difference-in-differences method. This method compares the difference in the mean labor neuraxial analgesia utilization rate in women aged 21 to 25 years (red circles) before and after the implementation of the Dependent Coverage Provision (difference 1) to the difference in the mean labor neuraxial analgesia utilization rate in women aged 27 to 31 years (blue squares) before and after the implementation of the Provision (difference 2). The difference between difference 1 and difference 2 (i.e., difference-in-differences) is estimated using the regression coefficient of a two-way interaction term between the age group (indicator of the 21 to 25 years old group) and the period (indicator of the post intervention period) in a linear regression model. For example, a regression coefficient of 0.015 indicates that the Dependent Coverage Provision is associated with a 1.5% (absolute) increase in the probability of labor neuraxial analgesia in women aged 21 to 25 years compared to women aged 27 to 31 years.
For a post hoc analysis requested during the peer review process and analyzing the proportion of women with private health insurance coverage, we used the interrupted time series method instead of the difference-in-differences method.22
Study sample
The study sample included birth certificates for non-operative vaginal deliveries from January 2009 to December 2013 in the 28 states that had implemented the 2003 revised US Standard Certificate of Live Birth as of January 1st, 2009 (CA, CO, DE, FL, GA, ID, IN, IA, KS, KY, MI, MT, NE, NH, NM, NY, ND, OH, OR, PA, SC, SD, TN, TX, UT, VT, WA, and WY). These 28 states accounted for 66% of national births during the study period. We further limited the study sample to women aged 21 to 25 years and to women aged 27 to 31 years.
We did not include birth certificate data after December 2013 because of the implementation in January 2014 of the Medicaid expansion, authorized by the Patient Protection and Affordable Care Act. The 2014 Medicaid Expansion gave states the option to expand Medicaid coverage to non-elderly adults with incomes up to 138% of the Federal Poverty Level and may have superseded the Dependent Coverage Provision.
We did not include birth certificate data before January 2009 because it would have excluded too many states. Only 19 states accounting for 49% of US births had implemented the 2003 revised US Standard Certificate of Live Birth as of January 1st, 2006; 22 states accounting for 53% of US births as of January 1st, 2007; and 27 states accounting for 65% of US births as of January 1st, 2008.
We identified vaginal deliveries without forceps or vacuum extraction using a specific checkbox on the birth certificate.17
Exclusion criteria were: 1) missing information on labor neuraxial analgesia (0.3%); 2) birth not occurring in a hospital or missing information on birth location (2.2%); 3) woman not residing in the United States or missing information on residence country (0.2%); and 4) missing information on woman’s residence county or hospital of delivery county (0.0%) (Figure 2).
Figure 2:
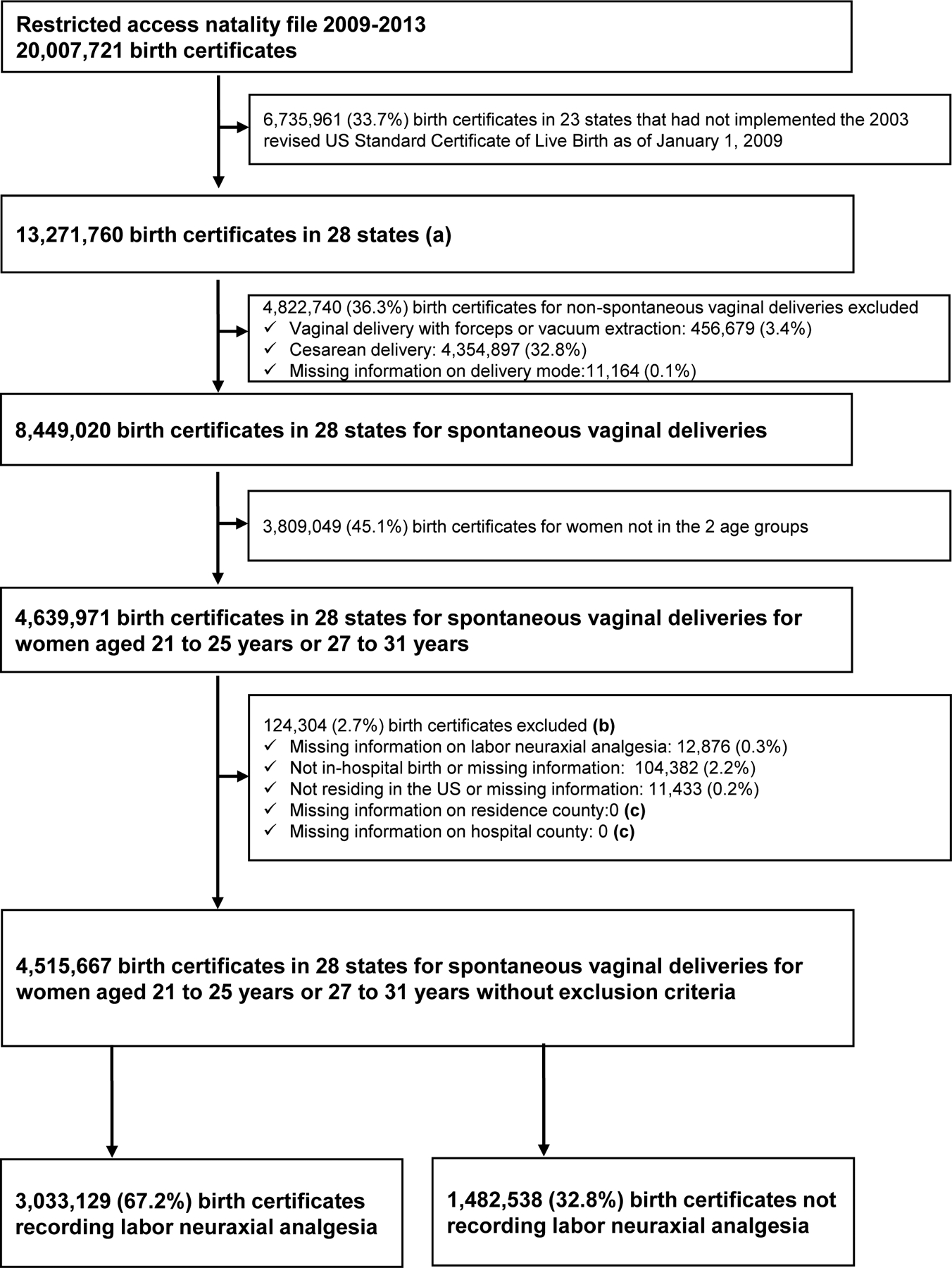
Flowchart of the study.
(a) The 28 states included are: CA, CO, DE, FL, GA, ID, IN, IA, KS, KY, MI, MT, NE, NH, NM, NY, ND, OH, OR, PA, SC, SD, TN, TX, UT, VT, WA, and WY.
(b) Reasons for exclusion are not mutually exclusive.
(c) Hospital county and patient residence county are required for merging birth data with county-level Area Health Resource File data.
Intervention
The intervention was the Dependent Coverage Provision, which requires private health insurers to allow young adults to remain on their parent’s plan until their 26th birthday. Depending on the parents’ health insurance plan, the young dependent adult is covered until the end of the month in which the dependent turns 26 years or until the end of the year in which the dependent turns 26 years. The law took effect for insurance plan renewals beginning on September 23rd, 2010, and applies to all plans in the individual market and to all employer plans.16 The pre-intervention period was January 2009-August 2010 and the post-intervention period was September 2010-December 2013. In a sensitivity analysis, we excluded data from the year 2010 (washout period). In post hoc analyses requested during the peer review process, we limited the post-intervention period to January 2012– December 2013 and to January 2013-December 2013.
Exposure
The exposure of interest was women age group, categorized into exposed (21 to 25 years) and unexposed (27 to 31 years). In a sensitivity analysis, we used a narrower definition of the two women age groups and defined exposed as women aged 24 to 25 years (instead of 21 to 25) and unexposed as women aged 27 to 28 years (instead of 27 to 31).
Outcomes
The primary outcome was labor neuraxial analgesia utilization rate. In the birth certificate, labor neuraxial analgesia is reported in a specific checkbox (“Epidural or spinal anesthesia during labor”), and defined as the “administration to the mother of a regional anesthetic for control of the pain of labor (i.e., delivery of the agent into a limited space with the distribution of the analgesic effect limited to the lower body)”.23 Using individual medical records as the gold standard, the reported sensitivity of labor neuraxial analgesia in birth certificate data in a study conducted in two states in 2009–2011 was greater than 80%.24 The Natality Files do not contain detailed information on the type of neuraxial analgesia precluding the analysis of specific neuraxial techniques (epidural, spinal, or combined spinal-epidural).
The secondary outcome assessing the quality of prenatal care was early initiation of prenatal care, defined as initiation during the first three months of pregnancy. In a post hoc analysis requested during the peer review process, we analyzed the proportion of women with private health insurance coverage as a secondary outcome.
Women and hospital characteristics
Women characteristics and comorbidities directly recorded from birth certificate data included: race and ethnicity; education level (less than high school, high school with no diploma, high school graduate or general educational diploma, and college or higher); marital status (married or unmarried); health insurance (Medicaid, private insurance, self-pay, and other); pre-pregnancy body mass index (≤ 18.4, 18.5–24.9, 25.0–29.9, 30.0–34.9, or ≥ 35 kg/m2); and preexisting or gestational diabetes or hypertension. Maternal race and ethnicity included four mutually exclusive groups: 1) non-Hispanic White (hereafter referred to as White); 2) non-Hispanic Black (Black); 3) non-Hispanic other; and 4) Hispanic. We acknowledge that race is a social construct, and we used race as a proxy for racism and discrimination. Since birth certificate data do not provide information on women’ residence, we estimated the following women characteristics at the county of residence level using the Area Health Resource File: residence location (urban, suburban, or rural), proportion of persons in poverty, and proportion of persons unemployed.
Obstetrical characteristics directly recorded from birth certificate data included: previous cesarean section; delivery during a weekend; woman transferred in (i.e., transfer from another facility for maternal medical or fetal indications for delivery); parity (nulliparous or parous); gestational age at delivery (≤ 33 completed weeks, 34–38 completed weeks, or ≥ 39 completed weeks); multiple gestation; non-cephalic presentation; induction of labor; augmentation of labor; antibiotics during labor; fever or chorioamnionitis during labor; attendant at birth (doctor of Medicine, doctor of Osteopathy, midwife, or other); and birth weight (≤ 2499 grams, 2500–4000 grams, or > 4000 grams).
Since birth certificate data do not provide a hospital identifier, we estimated the following characteristics at the hospital county level using the Area Health Resource File: hospital location (urban, suburban, or rural); number of hospital beds; number of hospital births; number of medical doctors; number of obstetricians and gynecologists; number of physician anesthesiologists; and number of certified registered nurse anesthetists (CRNA).
Statistical analysis
Statistical analysis was performed with R version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria).25
Descriptive statistics
In each age group, we compared women, obstetrical and hospital county characteristics between the pre- and post-intervention periods using the absolute standardized difference, with a value greater than 0.10 (10%) used to define a clinically important imbalance.26 For continuous variables estimated at the county level (e.g., unemployment rate), the absolute standardized difference was calculated using the median and not the mean.
We estimated labor neuraxial analgesia utilization rates overall and according to health insurance type (Medicaid, private, self-pay, or other), race and ethnicity (White, Black, Other, or Hispanic) and parity (nulliparous or parous). Then, in each age group, we estimated labor neuraxial analgesia utilization rates in the pre- and post-intervention periods. For each age group, we calculated the absolute difference in labor neuraxial analgesia utilization rates between the post- and pre-intervention periods.
Crude difference-in-differences estimator
The crude difference-in-differences estimator was the coefficient of a 2-way interaction term between the variable intervention and the variable exposure in the following linear regression model (Model 1): Y = β0 + β1 Intervention + β2 Exposure + β3 Intervention × Exposure. In this model, Y denotes labor neuraxial analgesia, intervention the intervention period (post-intervention period coded as 1 and pre-intervention period as 0), and exposure the women age group (21 to 25 years group coded as 1 and 27 to 31 years group as 0).
The main assumption of the difference-in-differences approach is that the trends in labor neuraxial analgesia utilization rate before the implementation of the Dependent Coverage Provision would not differ between the two age groups (i.e., the “parallel trends assumption”). To validate this assumption, we estimated the statistical significance of the coefficient of an interaction term between the age group and the month of delivery treated as a continuous variable in the pre-intervention period in a linear regression model. The result indicated that there was no significant divergence in labor neuraxial analgesia trends before the implementation of the Dependent Coverage Provision between the two women age (Supplemental Table 1).
Adjusted difference-in-differences estimator
To adjust the difference-in-differences estimator (i.e., β3), we added to Model 1: 1) variables with a plausible association with the exposure and the outcome (Supplemental Figure 1 and Supplemental Table 2); 2) a year fixed effect; 3) a state fixed effect; and 4) secular trends (month of delivery treated as a continuous variable, with January 2009 coded as 1 and December 2013 coded as 60). Health insurance and early initiation of prenatal care were not used for adjustment because they were treated as the outcomes of the Dependent Coverage Provision. We performed a complete case analysis with 4.8% of birth certificates excluded because of missing values for the variables used for adjustment.
Subgroup analyses
To estimate the association between the Dependent Coverage Provision and labor neuraxial analgesia use for specific subgroups, we conducted stratified analyses by estimating the adjusted difference-in-differences coefficient separately by women race and ethnicity and by parity.
RESULTS
Of the 4,515,667 birth certificates analyzed, 3,033,129 (67.2%) indicated use of labor neuraxial analgesia (Table 1). Labor neuraxial analgesia utilization rates ranged from a minimum of 36.2% in the state of New Mexico to a maximum of 82.7%% in the state of Utah (Supplemental Figure 2). The labor neuraxial analgesia utilization rate was higher for women with private insurance (73.6%) than for Medicaid beneficiaries (62.9%). It was also higher for White Women (73.8%) than for Black Women (67.5%), Other race and ethnicity Women (64.0%), or Hispanic women (54.7%), and for nulliparous women (74.5%) than for parous women (63.9%).
Table 1:
Labor neuraxial analgesia utilization rate (28 US states, 2009–2013).
| Missing | Number of birth certificates | Number of birth certificates recording labor neuraxial analgesia | Labor neuraxial analgesia utilization rate | |
|---|---|---|---|---|
| All women | 0 | |||
| 21 to 25- and 27 to 31 years | 4,515,667 | 3,033,129 | 67.2% | |
| Health insurance | 60,559 | |||
| Medicaid | 2,083,661 | 1,310,913 | 62.9% | |
| Private insurance | 1,926,322 | 1,417,916 | 73.6% | |
| Self-pay | 182,240 | 94,000 | 51.6% | |
| Other | 262,885 | 177,289 | 67.4% | |
| Maternal race and ethnicity | 35,582 | |||
| White | 2,401,109 | 1,771,921 | 73.8% | |
| Black | 569,970 | 384,498 | 67.5% | |
| Other | 278,480 | 178,379 | 64.0% | |
| Hispanic | 1,230,526 | 673,623 | 54.7% | |
| Parity | 54,613 | |||
| Parous | 3,056,752 | 1,952,473 | 63.9% | |
| Nulliparous | 1,404,302 | 1,045,904 | 74.5% |
Comparison in each women age group of women, obstetrical, and hospital county characteristics between the pre- and the post-intervention periods are presented in Table 2. In each women age group, no significant difference was observed between the pre- and post-intervention periods, except for a decrease in both groups in the unemployment rate and an increase in the proportion of persons in poverty in the county of residence during the post-intervention period.
Table 2:
Comparison of the pre- and post-intervention periods in the two age groups (28 US states, 2009–2013). The pre-intervention period is from January 2009 to August 2010 and the post-intervention period from September 2010 to December 2013.
| Women aged 27 to 31 years | Women aged 21 to 25 years | |||||||
|---|---|---|---|---|---|---|---|---|
| Missing | Pre intervention (n = 773,345) |
Post intervention (n = 1,574,351) |
Standardized difference (a) | Pre intervention (n = 740,739) |
Post intervention (n =1,427,232) |
Standardized difference (a) | Standardized difference (b) | |
| Demographic characteristics | ||||||||
| Hispanic | 192,285 (25.1%) | 374,160 (24.0%) | 232,622 (31.7%) | 431,459 (30.4%) | ||||
| College and higher | 493,395 (64.7%) | 1,048,060 (67.4%) | 303,745 (41.5%) | 624,122 (44.2%) | ||||
| Not married | 0 | 206,539 (26.7%) | 430,276 (27.3%) | 0.014 | 405,552 (54.7%) | 814,644 (57.1%) | 0.047 | 0.596 |
| Other | 37,471 (4.9%) | 79,576 (5.1%) | 48,672 (6.7%) | 97,166 (6.9%) | ||||
| County of residence | ||||||||
| Non-metro and non-micropolitan | 32,972 (4.3%) | 66,177 (4.2%) | 42,321 (5.7%) | 82,712 (5.8%) | ||||
| Percent persons in poverty (c) | 776 (<0.1%) | 15.4 (12.3–19.0) | 16.0 (12.9–19.1) | 0.114 | 16.6 (13.4–19.0) | 17.2 (1 4.0–20.0) | 0.113 | 0.231 |
| Percent unemployed (c) | 776 (<0.1%) | 9.6 (8.1–11.0) | 8.1 (6.8–9.9) | 0.571 | 9.8 (8.3–12.0) | 8.4 (7.0–10.0) | 0.516 | 0.075 |
| Comorbidites | ||||||||
| ≥ 35 | 96,643 (12.5%) | 189,798 (12.1%) | 95,019 (12.8%) | 175,390 (12.3%) | ||||
| Preexisting diabetes | 8697 (0.2%) | 3242 (0.4%) | 6756 (0.4%) | 0.002 | 2015 (0.3%) | 4147 (0.3%) | 0.004 | 0.025 |
| Gestational diabetes | 8697 (0.2%) | 30,152 (3.9%) | 70,505 (4.5%) | 0.029 | 16,406 (2.2%) | 37,714 (2.6%) | 0.028 | 0.098 |
| Preexisting hypertension | 8697 (0.2%) | 6809 (0.9%) | 15190 (1.0%) | 0.009 | 4325 (0.6%) | 8920 (0.6%) | 0.005 | 0.035 |
| Gestational hypertension | 8697 (0.2%) | 23,564 (3.1%) | 53676 (3.4%) | 0.021 | 22843 (3.1%) | 48468 (3.4%) | 0.018 | 0.002 |
| Pregnancy, labor, and delivery | ||||||||
| Previous cesarean section | 8622 (0.2%) | 14,614 (1.9%) | 35,252 (2.2%) | 0.025 | 9078 (1.2%) | 20,354 (1.4%) | 0.018 | 0.054 |
| Delivery during a weekend | 1,224,441 (27.1%) | 207,408 (26.8%) | 427,999 (27.2%) | 0.008 | 199,784 (27.0%) | 389,250 (27.3%) | 0.007 | 0.003 |
| Woman transferred in | 3220 (<0.1%) | 2244 (0.3%) | 4712 (0.3%) | 0.002 | 2882 (0.4%) | 5612 (0.4%) | 0.001 | 0.017 |
| Nulliparous | 54,613 (1.2%) | 196,632 (25.9%) | 420,055 (26.9%) | 0.025 | 262,872 (36.1%) | 524,743 (37.1%) | 0.022 | 0.223 |
| ≥ 39 completed weeks | 499,707 (64.7%) | 1,049,188 (66.7%) | 470,869 (63.6%) | 933,244 (65.5%) | ||||
| Multiple gestation | 0 | 9955 (1.3%) | 20,863 (1.3%) | 0.003 | 6982 (0.9%) | 13,009 (0.9%) | 0.003 | 0.033 |
| Non-cephalic presentation | 79,775 (1.8%) | 11,835 (1.6%) | 23,505 (1.5%) | 0.004 | 12,285 (1.7%) | 23,635 (1.7%) | 0.001 | 0.011 |
| Induction of labor | 0 | 218,031 (28.2%) | 432,479 (27.5%) | 0.016 | 201,839 (27.2%) | 386,327 (27.1%) | 0.004 | 0.021 |
| Augmentation of labor | 0 | 197,691 (25.6%) | 400,381 (25.4%) | 0.003 | 202,610 (27.4%) | 385,963 (27.0%) | 0.007 | 0.041 |
| Antibiotics during labor | 0 | 123,660 (16.0%) | 269,940 (17.1%) | 0.031 | 121,295 (16.4%) | 255,378 (17.9%) | 0.040 | 0.010 |
| Fever or chorioamnionitis during labor | 0 | 7069 (0.9%) | 16,111 (1.0%) | 0.011 | 7835 (1.1%) | 17,437 (1.2%) | 0.015 | 0.015 |
| Other | 4157 (0.5%) | 8534 (0.5%) | 5036 (0.7%) | 9631 (0.7%) | ||||
| > 4000 grams | 57,908 (7.5%) | 117,632 (7.5%) | 40,583 (5.5%) | 76,784 (5.4%) | ||||
| Hospital county characteristics | ||||||||
| Non-metro and non-micropolitan | 13,615 (1.8%) | 25,949 (1.6%) | 18,287 (2.5%) | 34,290 (2.4%) | ||||
| Number of hospital beds (c) | 702 (<0.1%) | 2203 (683–4981) | 2106 (693–4762) | 0.017 | 1666 (499–4686) | 1613 (494–4616) | 0.009 | 0.093 |
| Number of in-hospital births (c) | 702 (<0.1%) | 10,071 (3255–23,362) | 9524 (3170–23,029) | 0.019 | 7633 (2285–21,659) | 7298 (2226–20,066) | 0.012 | 0.081 |
| Number of medical doctors (c) | 702 (<0.1%) | 1786 (557–5276) | 1892 (568–5276) | 0.016 | 1246 (336–4452) | 1288 (333–4455) | 0.007 | 0.086 |
| Number of obstetricians and gynecologists (c) | 702 (<0.1%) | 92 (27–235) | 92 (27–246) | <0.001 | 67 (16–204) | 66 (16–207) | 0.004 | 0.088 |
| Number of anesthesiologists (c) | 702 (<0.1%) | 104 (27–251) | 108 (28–267) | 0.011 | 74 (17–219) | 70 (17–226) | 0.012 | 0.088 |
| Number of certified registered nurse anesthetists (c) | 702 (<0.1%) | 51 (17–154) | 55 (19–177) | 0.025 | 46 (12–138) | 50 (14–156) | 0.026 | 0.035 |
| Hospital state characteristics | ||||||||
| State identifier | 0 | (d) | (d) | 0.022 | (d) | (d) | 0.028 | 0.123 |
Results are presented as count (%) or median (interquartile range). An absolute standardized difference greater than 0.10 (10%) indicates a clinically relevant imbalance between groups.
For the comparison between the pre- and post-intervention periods in each age group.
For the comparison between the two age groups during the pre-intervention period.
From the county-level Area Health Resource File. For these variables, absolute standardized difference was calculated using the median and not the mean.
For clarity purpose, results for the 28 states are not presented.
For women aged 21 to 25 years, the labor neuraxial analgesia utilization rates were 64.9% during the pre-intervention period and 68.9% during the post-intervention period (difference: 4.0%; 95% CI: 3.9, 4.2) (Table 3 and Figure 3). For women aged 27 to 31 years, the labor neuraxial analgesia utilization rates were 64.9% during the pre-intervention period and 67.7% during the pre-intervention period (difference: 2.8%; 95% CI: 2.7, 2.9). There was no evidence of difference in pre-policy labor neuraxial analgesia utilization trends between the two women age groups (Figure 3 and Supplemental Table 1).
Table 3:
Crude labor neuraxial analgesia utilization rate according to age groups and intervention periods, and difference-in-differences estimator (28 US states, 2009–2013).
| Women aged 27 to 31 years | Women aged 21 to 25 years | ||||||
|---|---|---|---|---|---|---|---|
| Pre Intervention | Post Intervention | Unadjusted difference (95% CI) | Pre Intervention | Post Intervention | Unadjusted Difference (95% CI) | ||
| n=773,345 | n=1,574,351 | n=740,739 | n=1,427,232 | ||||
| 64.9% | 67.7% | 2.8 (2.7, 2.9) | 64.9% | 68.9% | 4.0 (3.9, 4.2) | 0.012 (0.011, 0.014) | 0.010 (0.008, 0.012) |
Abbreviations: CI: confidence interval.
The difference-in-differences estimator is the regression coefficient of a 2-way interaction term between the age group (indicator of the 21 to 25 years old group) and the period (indicator of the post intervention period) in a linear regression model. For example, a regression coefficient of 0.012 indicates that the Dependent Coverage Provision is associated with a 1.2% (absolute) increase in the probability of labor neuraxial analgesia in women aged 21 to 25 years compared to women aged 27 to 31 years.
Adjustment used the following variables: 1) Race and ethnicity, 2) Education level, 3) Marital status, 4) County of residence core base statistical area classification, 5) County of residence percent persons in poverty, 6) County of residence percent unemployed, 7) Pre-pregnancy body mass index, 8) Preexisting diabetes, 9) Gestational diabetes, 10) Preexisting hypertension, 11) Gestational hypertension, 12) Previous cesarean section, 13) Parity, 14) Gestational age at delivery, 15) Multiple gestation, 16) Non-cephalic presentation, 17) Induction of labor, 18) Augmentation of labor, 19) Attendant at birth, 20) Birth weight, 21) Hospital county core base statistical area classification, 22) Hospital county number of in-hospital births, 23) Hospital county number of physician anesthesiologists, 24) Hospital county number of certified registered nurse anesthetists, 25) Year of delivery, 26) State identifier, and 27) Secular trends.
Figure 3:
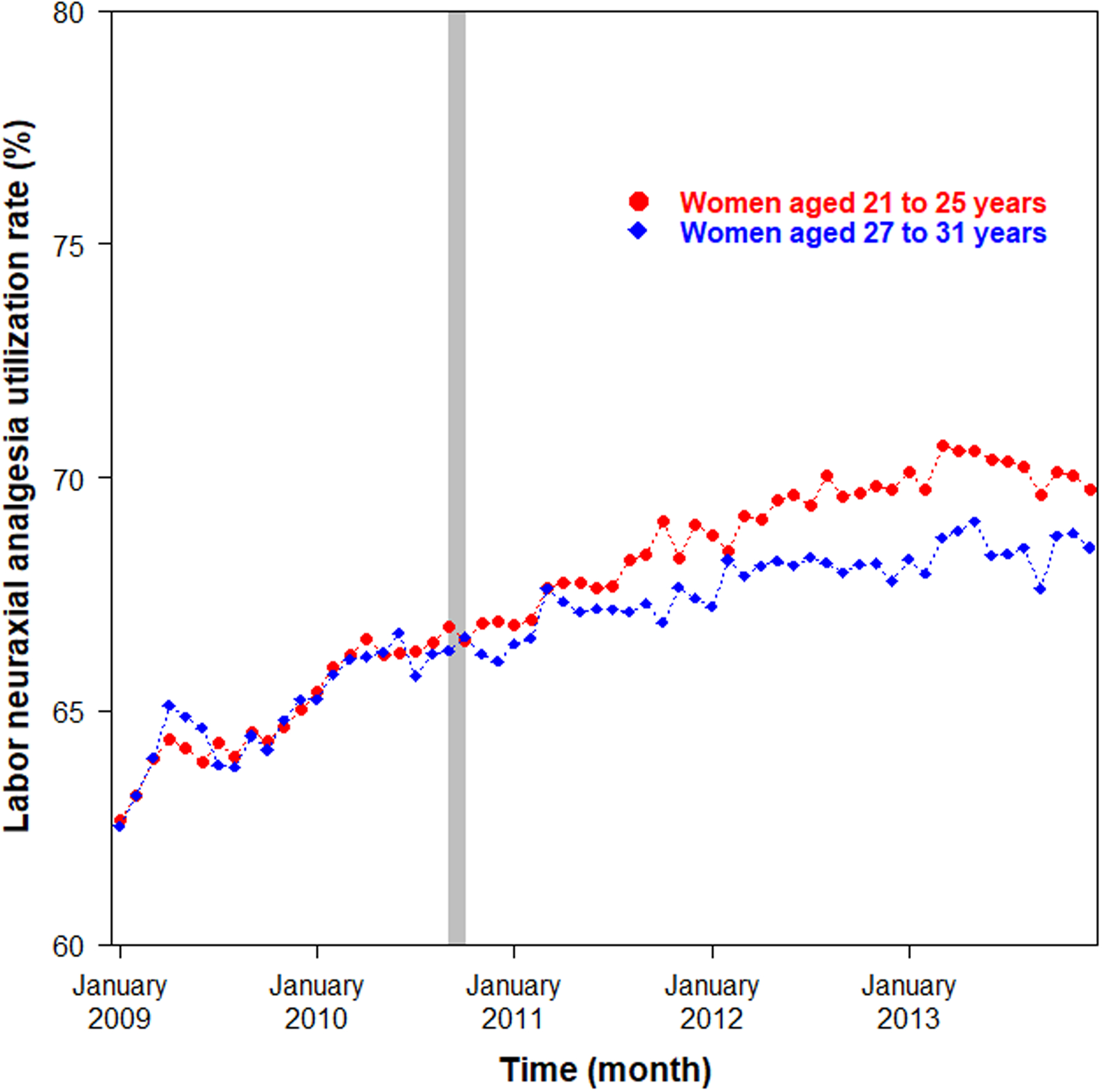
Temporal trends in labor neuraxial analgesia utilization rate in women aged 21 to 25 years (exposed; red color) and in women aged 27 to 31 years (unexposed; blue color). Each point represents the monthly labor neuraxial analgesia utilization rate. The grey rectangle indicates the implementation of the Dependent Coverage Provision (September 2010). For clarity purpose, the y-axis is truncated.
Difference-in-differences estimators
Before adjustment, the Dependent Coverage Provision was associated with a statistically significant 1.2% increase in the labor neuraxial analgesia utilization rate among women aged 21 to 25 years compared with women aged 27 to 31 years (crude difference-in-differences estimator: 0.012; 95% CI: 0.011, 0.014) (Table 3). After adjustment (Supplemental Table 3), the Dependent Coverage Provision was associated with a statistically significant 1.0% increase in the labor neuraxial analgesia utilization rate (adjusted difference-in-differences estimator: 0.010; 95% CI: 0.008, 0.012). Similar finding was observed for early initiation of prenatal care (adjusted difference-in-differences estimator: 0.012; 95% CI: 0.010, 0.014) (Supplemental Table 4). In the post hoc analysis, we also observed a significant increase in the proportion of women with private health insurance coverage associated with the Dependent Coverage Provision (Supplemental Figure 3).
Results were robust in the sensitivity analysis excluding data for the year 2010 and in the sensitivity analysis using a narrower definition of the two women age groups (Table 4). Results were also robust in the post hoc analyses limiting the post-intervention period to 2012–2013 and to 2013 (Supplemental Table 5).
Table 4:
Subgroup analyses for labor neuraxial analgesia utilization rate (28 US states, 2009–2013).
| Women aged 27 to 31 years | Women aged 21 to 25 years | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre intervention | Post intervention | Unadjusted Difference (95% CI) | Pre intervention | Post intervention | Unadjusted difference (95% CI) | Unadjusted difference-in-differences estimator (95% CI) (a) | Adjusted difference-in-differences estimator (95% CI) (a,b) | |
| Time limitation | ||||||||
| Exclusion of 2010 | 64.2% | 67.9% | 3.7 (3.5, 3.8) | 64.1% | 69.2% | 5.1 (4.9, 5.2) | 0.014 (0.012, 0.016) | 0.011 (0.009, 0.013) |
| Age limitation | ||||||||
| 24–25- and 27–28-year-old | 64.9% | 67.8% | 2.9 (2.7, 3.1) | 64.4% | 68.2% | 3.8 (3.6, 4.0) | 0.008 (0.005, 0.011) | 0.007 (0.004, 0.010) |
| Race and ethnicity | ||||||||
| White | 72.3% | 73.4% | 1.1 (1.0, 1.3) | 73.3% | 75.5% | 2.2 (2.0, 2.4) | 0.011 (0.008, 0.013) | 0.008 (0.006, 0.011) |
| Black | 62.8% | 66.6% | 3.8 (3.4, 4.2) | 66.2% | 70.2% | 4.0 (3.7, 4.4) | 0.002 (−0.003, 0.008) | 0.004 (−0.001, 0.009) |
| Other | 63.8% | 66.2% | 2.4 (1.9, 2.8) | 58.8% | 62.2% | 3.4 (2.7, 4.1) | 0.010 (0.002, 0.018) | 0.006 (−0.002, 0.014) |
| Hispanic | 49.3% | 55.1% | 5.8 (5.5, 6.0) | 51.8% | 58.5% | 6.7 (6.4, 6.9) | 0.009 (0.005, 0.013) | 0.007 (0.004, 0.011) |
| Parity | ||||||||
| Parous | 61.9% | 64.8% | 2.9 (2.7, 3.1) | 61.2% | 65.3% | 4.1 (4.0, 4.3) | 0.012 (0.010, 0.015) | 0.010 (0.008, 0.012) |
| Nulliparous | 73.9% | 75.7% | 1.8 (1.6, 2.1) | 71.6% | 75.1% | 3.5 (3.3, 3.7) | 0.017 (0.014, 0.020) | 0.012 (0.009, 0.015) |
Abbreviations: CI: confidence interval.
The difference-in-differences estimator is the regression coefficient of a 2-way interaction term between the age group (indicator of the 21 to 25 years old group) and the period (indicator of the post intervention period) in a linear regression model. For example, a regression coefficient of 0.012 indicates that the Dependent Coverage Provision is associated with a 1.2% (absolute) increase in the probability of labor neuraxial analgesia in women aged 21 to 25 years compared to women aged 27 to 31 years.
Adjustment used the following variables: 1) Race and ethnicity, 2) Education level, 3) Marital status, 4) County of residence CBSA classification, 5) County of residence percent persons in poverty, 6) County of residence percent unemployed, 7) Pre-pregnancy body mass index, 8) Preexisting diabetes, 9) Gestational diabetes, 10) Preexisting hypertension, 11) Gestational hypertension, 12) Previous cesarean section, 13) Parity, 14) Gestational age at delivery, 15) Multiple gestation, 16) Non-cephalic presentation, 17) Induction of labor, 18) Augmentation of labor, 19) Attendant at birth, 20) Birth weight, 21) Hospital county CBSA classification, 22) Hospital county number of in-hospital births, 23) Hospital county number of physician anesthesiologists, 24) Hospital county number of CRNAs, 25) Year of delivery, 26) State identifier, and 27) Secular trends.
Subgroup analyses
The increase in the labor neuraxial analgesia utilization rate associated with the Dependent Coverage Provision was significant among White women (adjusted difference-in-differences estimator: 0.008; 95% CI: 0.006, 0.011), Hispanic women (adjusted difference-in-differences estimator: 0.007; 95% CI: 0.004, 0.011), nulliparous women (adjusted difference-in-differences estimator: 0.012; 95% CI: 0.009, 0.015) and parous women (adjusted difference-in-differences estimator: 0.010; 95% CI: 0.008, 0.012), but not among Black women (adjusted difference-in-differences estimator: 0.004; 95% CI: −0.001, 0.009) and women of Other race and ethnicity (adjusted difference-in-differences estimator: 0.006; 95% CI: −0.002, 0.014) (Table 4).
DISCUSSION
In this natural experiment study of spontaneous vaginal deliveries from 2009 to 2013, we report that the Dependent Coverage Provision was associated with an 1.0% increase in the labor neuraxial analgesia utilization rate among women aged 21 to 25 years compared with women aged 27 to 31 years.
It is noteworthy that albeit statistically significant, this increase in the labor neuraxial analgesia utilization rate associated with the Dependent Coverage Provision is small and unlikely of clinical significance. This small effect size can be explained by the small increases in the proportion of women with private health insurance coverage and with early initiation of prenatal care (as a proxy for better prenatal education) associated with the Dependent Coverage Provision. Of note, the reported effect size for adverse obstetrical or maternal outcomes associated with health policies aiming to increase health insurance coverage is usually modest. For example, Daw et al. reported that the 2010 Dependent Coverage Provision was associated with a 0.20% (95% CI: 0.03, 0.30) adjusted decrease in the odds of preterm birth in the United States;12 we reported that the 2014 Medicaid expansion was associated with a 0.42% (95% CI: 0.07, 0.75) adjusted decrease in the odds of severe maternal morbidity in New York State.22 The small increase in the labor neuraxial analgesia utilization rate associated with the Dependent Coverage Provision also suggests that health insurance coverage alone may not be sufficient to increase the utilization of labor neuraxial analgesia. Efforts focusing on the patient’s anticipated use of neuraxial analgesia may be more effective. For example, reducing misconceptions and fears (e.g., fear of needles or of chronic back pain) about neuraxial analgesia through hospital-based prenatal educational programs have been associated with reduced misconceptions about labor neuraxial analgesia and increased labor neuraxial analgesia use.14 Of note, increased labor neuraxial analgesia use associated with the Dependent Coverage Provision was statistically significant for White and Hispanic women but not for Black and Other Race ethnicity women. This may be explained by the lower proportion of parents with private health insurance coverage in these minority groups.27
Previous research on the association of provision of health insurance coverage with labor neuraxial analgesia use is limited to one study by Xiao et al. on the 2014 Medicaid expansion authorized by the Patient Protection and Affordable Care Act.28 The 2014 Medicaid expansion led to a significant reduction in insurance discontinuity for pregnant people, and to an increase in preconception, prenatal, and postpartum healthcare access and utilization.10,11 Analyzing birth certificate data, Xiao el al. reported that the Medicaid expansion was associated with an 1.5% (95%CI: 0.2, 2.9) increase in the labor neuraxial analgesia utilization rate among nulliparous women in states that expanded Medicaid compared to nulliparous women in states that did not expand Medicaid.28 This effect size is similar to the one observed in our study, and although statistically significant, is also unlikely of clinical significance.
Limitations
First, we have no information in the Natality file on health insurance coverage for parents of the women. Since only women whose parents have private health insurance coverage may have benefited from the Dependent Coverage Provision, our analysis should be restricted to these women. In the absence of data, we included everyone who was eligible based on age to benefit from the Dependent Coverage Provision. Therefore, the estimated increase in labor neuraxial analgesia utilization rate refers to the overall impact of the Dependent Coverage Provision on all women aged 21 to 25 years irrespective of their beneficiary status. The increase in labor neuraxial analgesia utilization rate associated with the Dependent Coverage Provision among the beneficiaries might be greater than the estimated 1% as reported in this study. Second, the duration of the preintervention period (from January 2009 to August 2010, or 20 months) is relatively short which may make the estimate of the pre-intervention labor neuraxial analgesia trends unreliable. However, the duration of the pre-intervention period in our study is similar to the one used in other studies on the effect of the Dependent Coverage Provision.12,15 Third, our results are susceptible to unmeasured confounding. Some important variables known to influence labor neuraxial analgesia utilization, such as actual participation in prenatal educational programs and anticipated use of labor neuraxial analgesia during labor, is not available in the Natality file.14,29 Fourth, we estimated some hospital characteristics (e.g., number of physician anesthesiologists or CRNAs) at the hospital-county level as a proxy for the hospital because the Natality file does not provide an hospital identifier. Furthermore, some hospital characteristics (e.g., teaching status) could not be estimated using the hospital-county level data. Last, our study sample was limited to 28 states. Since labor neuraxial analgesia utilization rates vary markedly by state, the specific states that are included in the study may not necessarily be nationally representative.5 Therefore, our findings may not be directly generalizable to the nation as whole.
Conclusion
Implementation of the Dependent Coverage Provision was associated with a statistically significant increase in labor neuraxial analgesia use, but the small effect size unlikely of clinical significance.
Supplementary Material
Supplemental Figure 1: Conceptual framework
Supplemental Figure 2: Labor neuraxial analgesia utilization rate according to states
Supplemental Table 1: Parallel trend assumption
Supplemental Table 2: Variables used for the adjustment of the difference-in-differences estimator
Supplemental Table 3: Regression coefficients from the linear regression model used to estimate the adjusted difference-in-differences estimator
Supplemental Table 4: Early initiation of prenatal care according to women age groups and
intervention periods
Supplemental Figure 3: Temporal trends in the proportion of women with private health insurance
Supplemental Table 5: Post hoc analysis for labor neuraxial analgesia utilization rate using different durations of the post-intervention period
Funding Statement:
Jean Guglielminotti is supported by grant R21 MD016414 from the National Institute on Minority Health and Health Disparities.
Conflicts of Interest:
Jean Guglielminotti is supported by grant R21 MD016414 from the National Institute on Minority Health and Health Disparities and grant R21 MH126096 from the National Institute of Mental Health, National Institutes of Health.
Ruth Landau was a consultant for Pacira Pharmaceuticals Incorporated and serves on the editorial board of the journal Regional Anesthesia and Pain Medicine.
Footnotes
Prior presentations:
None
REFERENCES
- 1.Anim-Somuah M, Smyth RM, Cyna AM, Cuthbert A: Epidural versus non-epidural or no analgesia for pain management in labour. Cochrane Database Syst Rev 2018; 5: CD000331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guglielminotti J, Landau R, Daw J, Friedman AM, Chihuri S, Li G: Use of labor neuraxial analgesia for vaginal delivery and severe maternal morbidity. JAMA Netw Open 2022; 5: e220137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Driessen M, Bouvier-Colle MH, Dupont C, Khoshnood B, Rudigoz RC, Deneux-Tharaux C, Pithagore G: Postpartum hemorrhage resulting from uterine atony after vaginal delivery: factors associated with severity. Obstet Gynecol 2011; 117: 21–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guglielminotti J, Landau R, Li G: Adverse events and factors associated with potentially avoidable use of general anesthesia in cesarean deliveries. Anesthesiology 2019; 130: 912–922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Butwick AJ, Bentley J, Wong CA, Snowden JM, Sun E, Guo N: United States state-level variation in the use of neuraxial analgesia during labor for pregnant women. JAMA Netw Open 2018; 1: e186567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guglielminotti J, Wong CA, Friedman AM, Li G: Racial and ethnic disparities in death associated with severe maternal morbidity in the United States: failure to rescue. Obstet Gynecol 2021; 137: 791–800 [DOI] [PubMed] [Google Scholar]
- 7.Admon LK, Winkelman TNA, Zivin K, Terplan M, Mhyre JM, Dalton VK: Racial and ethnic disparities in the incidence of severe maternal morbidity in the United States, 2012–2015. Obstet Gynecol 2018; 132: 1158–1166 [DOI] [PubMed] [Google Scholar]
- 8.Kozhimannil KB, Interrante JD, Tofte AN, Admon LK: Severe maternal morbidity and mortality among indigenous women in the United States. Obstet Gynecol 2020; 135: 294–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pankiv E, Yang A, Aoyama K: Neuraxial labor analgesia for vaginal delivery and severe maternal morbidity. JAMA Netw Open 2022; 5: e220142. [DOI] [PubMed] [Google Scholar]
- 10.Sun EP, Guglielminotti J, Chihuri S, Li G: Association of Medicaid expansion under the Affordable Care Act with perinatal care access and utilization among low-income women: a systematic review and meta-analysis. Obstet Gynecol 2022; 139: 269–276 [DOI] [PubMed] [Google Scholar]
- 11.Bellerose M, Collin L, Daw JR: The ACA Medicaid expansion and perinatal insurance, health care use, and health outcomes: a systematic review. Health Aff (Millwood) 2022; 41: 60–68 [DOI] [PubMed] [Google Scholar]
- 12.Daw JR, Sommers BD: Association of the Affordable Care Act Dependent Coverage Provision with prenatal care use and birth outcomes. JAMA 2018; 319: 579–587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daw JR, Kolenic GE, Dalton VK, Zivin K, Winkelman T, Kozhimannil KB, Admon LK: Racial and ethnic disparities in perinatal insurance coverage. Obstet Gynecol 2020; 135: 917–924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Togioka BM, Seligman KM, Werntz MK, Yanez D, Noles LM, Treggiari MM: Education program regarding labor epidurals increases utilization by Hispanic Medicaid beneficiaries. A randomized controlled trial. Anesthesiology 2019; 131: 840–849 [DOI] [PubMed] [Google Scholar]
- 15.Akosa Antwi Y, Ma J, Simon K, Carroll A: Dependent coverage under the ACA and Medicaid coverage for childbirth. N Engl J Med 2016; 374: 194–6 [DOI] [PubMed] [Google Scholar]
- 16.Sommers BD, Schwartz K. ASPE Issue Brief: 2.5 million young adults gain health insurance due to the Affordable Care Act. Available at: https://aspe.hhs.gov/reports/25-million-young-adults-gain-health-insurance-due-affordable-care-act-0. Last accessed: March 8, 2023.
- 17.Centers for Disease Control and Prevention. U.S. standard certificate of live birth. Available at: https://www.cdc.gov/nchs/data/dvs/birth11-03final-ACC.pdf. Last accessed: February 17, 2023.
- 18.Health Resources and Services Administration. Area Health Resources Files (AHRF). 2018–2019. Available at: https://data.hrsa.gov/topics/health-workforce/ahrf. Last accessed: February 17, 2023.
- 19.Wing C, Simon K, Bello-Gomez RA: Designing difference in difference studies: best practices for public health policy research. Annu Rev Public Health 2018; 39: 453–469 [DOI] [PubMed] [Google Scholar]
- 20.Dimick JB, Ryan AM: Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA 2014; 312: 2401–2 [DOI] [PubMed] [Google Scholar]
- 21.Clapp MA, James KE, Kaimal AJ, Sommers BD, Daw JR: Association of Medicaid expansion with coverage and access to care for pregnant women. Obstet Gynecol 2019; 134: 1066–1074 [DOI] [PubMed] [Google Scholar]
- 22.Guglielminotti J, Landau R, Li G: The 2014 New York State Medicaid expansion and severe maternal morbidity during delivery hospitalizations. Anesth Analg 2021; 133: 340–348 [DOI] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics. Guide to completing the facility worksheets for the certificate of live birth and report of fetal death. Available at: https://www.cdc.gov/nchs/data/dvs/GuidetoCompleteFacilityWks.pdf. Last accessed: February 17, 2023.
- 24.Martin JA, Wilson EC, Osterman MJ, Saadi EW, Sutton SR, Hamilton BE: Assessing the quality of medical and health data from the 2003 birth certificate revision: results from two states. Natl Vital Stat Rep 2013; 62: 1–19 [PubMed] [Google Scholar]
- 25.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Available at: https://www.R-project.org/. Last accessed: February 17, 2023. [Google Scholar]
- 26.Austin P: Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Communications in Statistics - Simulation and Computation 2009; 38: 1228–1234 [Google Scholar]
- 27.Branch B, Conway D. American Community Survey Briefs: health insurance coverage by race and Hispanic origin, 2021. Available at: https://www.census.gov/content/dam/Census/library/publications/2022/acs/acsbr-012.pdf. Last accessed: March 16, 2023.
- 28.Xiao MZX, Whitney D, Guo N, Sun EC, Wong CA, Bentley J, Butwick AJ: Association of Medicaid expansion with neuraxial labor analgesia use in the United States: a retrospective cross-sectional analysis. Anesth Analg 2022; 134: 505–514 [DOI] [PubMed] [Google Scholar]
- 29.Toledo P, Sun J, Grobman WA, Wong CA, Feinglass J, Hasnain-Wynia R: Racial and ethnic disparities in neuraxial labor analgesia. Anesth Analg 2012; 114: 172–8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1: Conceptual framework
Supplemental Figure 2: Labor neuraxial analgesia utilization rate according to states
Supplemental Table 1: Parallel trend assumption
Supplemental Table 2: Variables used for the adjustment of the difference-in-differences estimator
Supplemental Table 3: Regression coefficients from the linear regression model used to estimate the adjusted difference-in-differences estimator
Supplemental Table 4: Early initiation of prenatal care according to women age groups and
intervention periods
Supplemental Figure 3: Temporal trends in the proportion of women with private health insurance
Supplemental Table 5: Post hoc analysis for labor neuraxial analgesia utilization rate using different durations of the post-intervention period


