Abstract
Background:
Trauma exposure and posttraumatic stress are highly prevalent and comorbid with health problems. Despite the apparent systemic nature of post-traumatic stress, recommended treatments neglect trauma’s deleterious effects on health. Integrative mind-body treatments for posttraumatic stress, such as Tai Chi and Qigong (TCQ), may offer a promising adjunct to first-line treatments.
Method:
A systematic search was conducted to identify trials that examined Tai Chi and/or Qigong as treatments for trauma-exposed populations. Studies were examined for rigor; design, sample and intervention characteristics, dropout, attendance, satisfaction, acceptability, and key findings were systematically extracted.
Results:
The 6 studies included are all pilot or feasibility trials with descriptive or mixed-methods outcomes. No randomized trials or rigorous studies were identified. Dropout rates ranged widely, and adverse reactions were not evident. Reported satisfaction was high and benefits of relaxation, reductions in mental health symptoms, and improvements in pain and physical and cognitive functioning were noted.
Limitations:
All the studies were non-rigorous and relatively small, with no comparison groups, or follow-up assessments; in many cases, posttraumatic stress symptoms were not formally assessed.
Conclusions:
The paucity and lack of rigor of the studies identified for this review highlights the need for larger, methodologically sound clinical trials. The reviewed studies suggest that TCQ practices have the potential to reduce symptoms and improve functioning for individuals exposed to trauma and provide evidence that TCQ is feasible, acceptable, and low risk in these populations. Possible mechanistic pathways supporting TCQ as a treatment for posttraumatic stress are considered.
1. Introduction
Exposure to potentially traumatic events is highly prevalent and has been documented in populations across the globe with rates as high as 75% reported in Australia and South Africa (Mills et al., 2011; Williams et al., 2007) and over 80% in the Netherlands (de Vries & Olff, 2009). Approximately one third of those exposed to trauma go on to develop posttraumatic stress disorder (PTSD; (Santiago et al., 2013). PTSD is defined in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition by four distinct clusters of symptoms that develop after exposure to a traumatic event (American Psychiatric Association, 2013). These symptom clusters include intrusive reminders of the traumatic event through distressing memories and nightmares, avoidance of reminders of the event, negative cognitions and mood, and increased physiologic arousal. PTSD is estimated to affect 6.8% of U.S. adults in their lifetimes (Kessler et al., 2005) and international estimates range from less than 2% in Japan to almost 9% in Northern Ireland (Atwoli et al., 2015). However, prevalence is much higher in populations experiencing high rates of trauma exposure. For example, the prevalence of PTSD has been estimated at 23% in military Veterans seeking care in Veterans Health Administration (VHA) facilities (VHA Office of Public Health and Environmental Hazards, 2009) and near 29% in war refugees (Wulfes et al., 2019). Furthermore, individuals exposed to trauma who experience some of these symptoms but do not meet full diagnostic criteria for PTSD may also continue to experience problematic posttraumatic stress symptoms (Cukor et al., 2010). PTSD is associated with a host of psychosocial issues such as suicidal ideation (Jakupcak et al., 2009), impairments in intimate partner relationships (Franz et al., 2020), and financial and employment instability (Sanderson & Andrews, 2006; Smith et al., 2005).
Although PTSD is categorized as a psychological disorder currently, it has demonstrable deleterious effects on physical health and in recent years has been increasingly considered a systemic disorder, affecting both the brain and the entire body (Dean et al., 2019; McFarlane et al., 2017). Trauma exposure generally and PTSD specifically have long been associated with medical comorbidities and increased healthcare utilization (O’Toole & Catts, 2008; Schnurr, 1996; Scott et al., 2013; Suris et al., 2004). Individuals with PTSD have been shown to be at greater risk for a wide range of medical ailments, such as cardiovascular disease (Coughlin, 2011), stroke (Dobie et al., 2004; Spitzer et al., 2009), metabolic syndrome (Wolf et al., 2016), chronic pain (Shipherd et al., 2007), and ovarian cancer (Roberts et al., 2019). In addition, there are documented increased rates of hypertension (Kibler, 2009), obesity (Bartoli et al., 2015), diabetes (Cohen et al., 2009) and all-cause mortality (Boscarino, 2006). Importantly, trauma exposure and PTSD have also been linked to poor health behaviors, such as smoking, poor diet, and lack of exercise (Hruby et al., 2021; Schnurr et al., 2000; van den Berk-Clark et al., 2018) which may contribute to the development and progression of many medical issues. Recent research into the neurobiological correlates of PTSD indicate that PTSD is associated with accelerated cellular aging (O’Donovan et al., 2011; Tyrka et al., 2010; Wolf et al., 2019) as well as deficits in brain structure (Bromis et al., 2018; Kunimatsu et al., 2019) and function (Koch et al., 2016; Lanius et al., 2010).
Current recommended treatments for posttraumatic stress focus on the mind (e.g. cognition and emotion) with little attention to the impact of trauma exposure on the body (e.g. physical health and health behaviors). Treatment guidelines by various organizations recommend trauma-focused psychotherapies as first-line treatments for PTSD and selective serotonin reuptake inhibitors (SSRIs) as the best medications to treat the disorder (Hamblen et al., 2019). Importantly, these treatments do not address the physical health issues that accompany trauma exposure and PTSD. Furthermore, stigma surrounding mental health treatment (Hoge et al., 2004), preferences for self-reliance to manage distress (Williston et al., 2019), reluctance to take prescribed medications (Kronish et al., 2012), or lack of understanding of the rationale for processing of trauma memories (Hundt et al., 2015) may contribute to reluctance to engage in these treatments. Thus, although these recommended treatments have a substantial evidence base, they do not appeal to or work for all individuals suffering in the aftermath of trauma exposure and do not address physical health comorbidities.
Integrative mind-body treatments, such as mindfulness meditation, yoga, and Tai Chi, have received increasing attention as treatments for mental disorders (e.g., Vancampfort et al., 2021). In clinical settings for trauma populations, for example, almost all specialized PTSD programs in the VHA offer some integrative therapies (Libby et al., 2012) and over 30% of individuals diagnosed with PTSD utilize one or more of these treatments for mental health issues (Libby et al., 2013). The VHA has recognized the potential promise of these complementary and integrative treatments and has specifically recommended Tai Chi as one of the approaches to improve health and wellbeing for veterans with PTSD (Department of Veterans Affairs, 2017). Mind-body treatments aimed at enhancing health behaviors for trauma-exposed individuals may serve multiple purposes, such as engaging individuals who do not want trauma-focused treatments or medications, providing adjunctive intervention for first-line treatments for PTSD, and addressing some of the physical health problems that are associated with trauma exposure. Additionally, these treatments could serve as a “foot in the door” for behavior change as they may be more approachable than trauma-focused psychotherapies or psychoactive medications.
Tai Chi is a Chinese martial art and form of neuromotor exercise that uses an integrated mind-body approach to enhance both physical and mental health (Garber et al., 2011). Often described as “meditation in motion,” Tai Chi is made up of several components: physical activity in the form of slow, graceful, low-impact movements; range of motion exercises and balance training; mental focus, visualization of body position and choreographed sequential forms; and deep diaphragmatic breathing and mindful relaxation (Lan et al., 2002; Solloway et al., 2016; Wayne & Kaptchuk, 2008). In addition, psychosocial interactions, physical touch (e.g., self-massage), spirituality, and ritual are hypothesized to contribute to its therapeutic effects (Wayne & Kaptchuk, 2008).
Tai Chi is often considered to be a form of Qigong and both practices are based on mind-body principles of traditional Chinese medicine. Qigong is loosely translated to mean the cultivation or mastery of Qi. Qi is a broad and complex term that defies a simple definition and refers to vital energy and flow of energy in the body, information, breath, or spirit (Wayne & Kaptchuk, 2008). In a review of the health benefits of these two practices, Jahnke et al. (2010) described Tai Chi and Qigong as “close relatives” (p. 1), with overlapping historical and theoretical roots, exercise forms, supposed mechanisms of action, and health benefits (Jahnke et al., 2010). Both practices include mindfulness, movement, and the cultivation of awareness of posture and breath. The practical difference identified is that Tai Chi typically involves lengthier and more complex choreographed movement forms, whereas Qigong involves simpler and more repetitive movements. However, Tai Chi routines usually include Qigong as warm up exercises and clinical trials examining Tai Chi usually involve simplified forms that are closer to Qigong. Jahnke et al. (2010) found no trends indicating any prominent difference in outcomes between interventions falling under either name and suggested that research literature on Tai Chi and Qigong (including thousands of modified forms, branches, or schools) should be considered as a unified body of evidence. For the purposes of this paper we will use the term “TCQ” to describe the family of Tai Chi and Qigong practices.
TCQ has been shown to be safe and effective at promoting aerobic cardiovascular fitness, muscle strength, emotional functioning, and quality of life in patients with a variety of chronic conditions, such as chronic heart failure, cancer, osteoarthritis, and pulmonary disease (Chen et al., 2016; Song et al., 2017; Taylor-Piliae & Finley, 2020). A study comparing Tai Chi with physical therapy for patients with knee osteoarthritis found the two treatments to be similar in improving pain, physical function, and stiffness, although the Tai Chi group showed significantly better improvements in depression and the physical component of quality of life (Wang et al., 2016). An umbrella review investigating the potential for TCQ to alleviate symptoms of Gulf War Illness concluded that TCQ appears to provide benefit to both physical and mental health symptoms that are commonly associated with this chronic condition (Reid et al., 2019). A recent review of physical interventions (e.g., exercise, yoga) for trauma and stressor-related disorders indicates that these interventions constitute a promising approach for trauma-exposed individuals (Davis et al., 2021). Importantly, the synergy between the physical and mental components of TCQ appears key to its efficacy in benefiting the psychological well-being and quality of life among patients with chronic disorders (Wang et al., 2004). Given the simultaneous focus on body and mind in TCQ, we conjecture that it may be especially well-suited to the treatment of PTSD, a disorder characterized by both physical and mental symptoms.
To aggregate the available literature and elucidate the potential impact of TCQ on PTSD, the aims of this paper are to:
Conduct a systematic review of the extant research on the use of TCQ in the treatment of trauma exposure and posttraumatic stress symptoms; and
Summarize the findings of the identified studies.
2. Methods
Electronic literature searches were conducted by a medical librarian experienced in systematic review searching (EA) in fall 2019, with updates performed through February 9, 2022. Scoping search results identified eighteen TCQ keywords, free text synonyms, and phrases from the databases to be searched: PubMed©, EMBASE©, APA PsycINFO©, Psychological & Behavioral Sciences Collection©, APA PsycARTICLES©, SocINDEX©, PTSDPubs© (formerly known as PILOTS), ProQuest Psychology Database©, and the Cochrane Library©. Each database was searched from the earliest available access year to the present, yielding results from as early as 1977.
For the current review, we included both Tai Chi and Qigong in our search terms and used the study authors’ labels describing the form, branch, or school within this family of practices. Ten PTSD and eighteen TCQ keywords, free text words and phrases were identified using comprehensive scoping searches. (See supplementary materials for specific wording.) These words and phrases were then used as search terms in literature searches that were conducted to include all available materials. Reference lists in relevant articles were searched for possible additional citations, although none were identified.
Inclusion criteria utilized were:
Published empirical peer-reviewed papers available in English with original data (i.e. not secondary analyses or review papers) that were: (a) randomized or non-randomized trials, (b) case studies, (c) observational studies, (d) qualitative research, or (e) quasi-experimental.
Participants under study: (a) were experiencing posttraumatic stress symptoms or (b) had been exposed to trauma.
One or more of the interventions investigated was Tai Chi and/or Qigong and included elements of mindfulness, movement, and cultivation of awareness of posture and breath.
Quantitative outcomes or qualitative themes related to one or more of the four Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) diagnostic criteria of PTSD (i.e. intrusion symptoms, avoidance symptoms, negative alterations in cognitions and mood, or increased arousal and reactivity).
After duplicates were removed, two independent raters (SKW, JWW and/or DHG) determined if the articles generated by the search met the above inclusion criteria. For each study, raters examined and excluded articles in a sequential manner based on titles, examining abstracts or full texts as needed. Discrepancies were resolved through consensus. Included studies were then classified rigorous or non-rigorous. Trials utilizing nonrandom assignment to intervention and comparison condition and pre-post studies (without a comparison) were identified as quasi-experimental and classified as non-rigorous and those with randomized design with a comparison condition were classified as rigorous (Davis et al., 2021). Two authors (BLN and MMM) independently extracted the following information from each study: study and evaluation design, sample characteristics, number of participants, description of the intervention, dropout and attendance, indicators of satisfaction and acceptability, and key findings. Discrepancies were resolved through consensus. After extraction, data were reviewed and checked against source material by a third independent reviewer (DLM).
3. Results
The initial results in PubMed© illustrated the scarcity of articles that discussed both TCQ and PTSD; 2866 citations on TCQ were retrieved after duplications were removed, yet when combined with the over 55,000 PTSD citations in PubMed©, only 17 citations emerged that discussed both concepts. Searches of the other databases named above yielded 140 additional citations. Six studies were included (see Fig. 1 for PRISMA flow chart).
Fig. 1.
PRISMA Flow Diagram for Study Identification.
All six identified studies were feasibility, pilot, or case series studies with descriptive, qualitative, or mixed-methods outcomes and were classified as non-rigorous. It is notable that this literature review detected no randomized trials or large quantitative studies on TCQ in the treatment of trauma or PTSD. Results are summarized in Table 1.
Table 1.
Descriptive summary of reviewed studies.
| Study Study Design | Population (n) Trauma Indicator | Description of Intervention | Dropout and Attendance | Indicators of Satisfaction and Acceptability | Key Findings |
|---|---|---|---|---|---|
|
| |||||
| Grodin et al. (2008) Descriptive Case Study | Refugee survivors of torture (n = 4) met criteria for PTSD and MDD | Simplified Qigong and Wustyle Tai Chi exercises, 10–15 min before and after psychotherapy sessions over 1-year period; daily home practice encouraged. | Not reported | Clients reported looking forward to the sessions and finding them calming and relaxing | Reported greater attunement to bodies and an overall improvement in physical, emotional, and spiritual well-being. Reductions in psychosomatic complaints and use of antidepressant and sleep medications |
| Munro et al. (2019) Pre-Post Mixed Methods | Veterans (n = 13) history of PTSD | 12-week, twice per week sessions of Hunyuan Qigong and other Taijiquan/Qigong exercises including self-massage, breathing, and moving meditation exercises. | 6 of 13 dropped out after enrollment; attendance not reported | Participants reported plans to continue practicing after study completion; encouraged staff to expand the reach of the program to allow more Veterans to benefit from the exercises | Reduced PTSD symptomatology (PCL-C); reductions in self-reported depression, stress, and anxiety; improvements in HbA1C; decreased sedentary time in some, and increased enjoyment of physical activity, as well as improvements in balance and movement awareness. |
| Niles et al. (2016) Descriptive Qualitative | Veterans (n = 17) medical record diagnosis of PTSD or screened positive with at least one reexperiencing symptom | 4-week introductory program with 4 (60- to 90-min) sessions including warm-up, self-massage, review of Tai Chi principles, Tai Chi movement, breathing techniques, and relaxation | No dropouts after enrollment; 82% attended at least 3 of 4 sessions | 93.8% reported being very or mostly satisfied | Helpful for managing distressing symptoms (intrusions, hyperarousal, concentration difficulties) and elicited a feeling of being calm and focused. |
| Reb et al. (2017) Pre-Post Mixed Methods | Active-duty military service members (n = 26) returned from Iraq or Afghanistan and seeking treatment for deployment-related injuries | 20 60-min sessions of Integral Qigong that included four categories of practice: breath practices, gentle movement, self-massage, and meditation | 16 of 26 dropped out after enrollment; overall mean attendance was 8.14 sessions, mean attendance for intervention completers (n = 10) was 17.0 sessions | The CSQ mean score for 7 who completed assessments was 27.28 (SD = 3.03; range 8–32) indicating high satisfaction | Quantitative analysis for 7 who completed assessments showed non-significant but moderate effect size improvements in stress, sleep, and somatic symptoms. Qualitative analysis indicated improvements in coping with stress, resilience and empowerment, mood, sleep, coping with pain, physical functioning, focus, and irritability |
| Tsai et al. (2018) Pre-Post Mixed Methods | Individuals with PTSD (Phase 1: n = 11; Phase 2: n = 10) screened positive for PTSD with a score ≥ 35 on the PTSD Checklist and reported chronic low back, osteoarthritis, or joint pain | Two phase study: Phase 1 involved 60-min Sun-style Tai Chi session; Phase 2 was a 12-week intervention of 3 sessions per week | Phase 2: 1 of 10 participants dropped out; mean attendance of 12.3 (SD = 8.86) classes out of 36 | On a scale of 1–7, positive responses toward practicing Tai Chi were reported, such as: satisfaction (6.45), enjoyment (6.09), liking Tai Chi (6.45), having fun (5.73) | Statistically significant improvements in fear-affect, fear-somatic arousal, working memory, and 6-min walk performance, current level of pain |
| Yost and Taylor (2013) Descriptive Qualitative | Military service members (n = 6) suffered a mTBI during active military service and receiving outpatient neurorehabilitation | Private 1-h Qigong sessions with instructor 4 times a week for 2 weeks, followed by 20-min group sessions 3 times a week for 6 weeks | 1 of 6 dropped out; session attendance not reported | All participants reported that Qigong fit into the military culture, and was appropriate for individuals with mTBI symptoms (e.g., impaired balance) | Participants reported Qigong conferred a greater ability to manage mTBI symptoms, decrease medication reliance, as well as improved general mood and sleep, reduced impact of chronic pain, and decreased stress and anxiety |
These studies examined a variety of styles of TCQ. Although there were varying levels of detail regarding the specific content of the sessions, all reported that sessions included elements of breathing exercises, structured TCQ movement, and meditation. There was considerable variability among the studies in the length and number of intervention sessions with the least intensive being 10- to 15-min sessions to augment psychotherapy sessions occurring over a year or longer (Grodin et al., 2008) and the most intensive being 8 1-h individual sessions plus 18 20-min group sessions over 8 weeks (Yost & Taylor, 2013). Similarly, dropout rates ranged widely from 0% (Niles et al., 2016) to 62% (Reb et al., 2017) and adherence, though not always reported, ranged from 36% (Tsai et al., 2018) to 81% (Niles et al., 2016).
There was substantial variability as to whether or how posttraumatic stress symptoms were assessed. Only one study utilized a cut-off score on a validated self-report instrument (Tsai et al., 2018), while three used less reliable or unclear methods to establish symptoms in the samples (Grodin et al., 2008; Munro et al., 2019; Niles et al., 2016) and two investigated participants with high exposure to trauma (Reb et al., 2017; Yost & Taylor, 2013) but did not require posttraumatic stress symptoms as an inclusion criterion. None of these investigations conducted follow-up assessments to determine if effects were lasting and none provided a gold-standard measure of PTSD symptoms via clinician-administered structured interview. Additionally, all but two of the above studies were conducted on military/veteran samples, possibly limiting the generalizability of their findings to other populations.
Reported satisfaction with the TCQ sessions was universally high. Negative side effects or adverse reactions to TCQ were not evident aside from the study that included chronic pain as an inclusion criterion. In this study (Tsai et al., 2018), participants reported some soreness that diminished from pre-to post-treatment. In terms of benefits, all six studies reported that participants found the interventions to be calming, relaxing, or reduced stress, and reported an improvement in mental health symptoms (e.g., PTSD, depression, anxiety) and/or mental well-being (e.g., resilience, empowerment, engagement). Reductions in trauma intrusion symptoms were noted in three studies (Grodin et al., 2008; Niles et al., 2016; Yost & Taylor, 2013) and an increased feeling of control over symptoms was reported by Yost and Taylor (2013). A reduction in pain was noted in several studies (Grodin et al., 2008; Reb et al., 2017; Tsai et al., 2018; Yost & Taylor, 2013) as well as an improvement in physical functioning (Munro et al., 2019; Niles et al., 2016) and sleep (Reb et al., 2017; Yost & Taylor, 2013). Cognitive improvements and improved focus were also mentioned as benefits (Munro et al., 2019; Niles et al., 2016; Tsai et al., 2018; Yost & Taylor, 2013). Two of the studies commented on how the disciplined nature of the exercises and their connection to the martial arts resonated with military culture (Niles et al., 2016; Yost & Taylor, 2013). Only one study (Tsai et al., 2018) reported perceived barriers to participation, and these included logistical limitations such as transportation and work conflicts, physical or health-related limitations, and emotional issues.
4. Discussion
These six studies present encouraging findings suggesting that TCQ has the potential to reduce symptoms and improve functioning for individuals exposed to trauma. They provide evidence that TCQ is feasible, acceptable, and low risk in these populations. However, important limitations should be noted: most of the studies had small numbers of participants (range 4–26), there were no comparison groups, and no follow-up assessments to determine if the effects persisted. Furthermore, posttraumatic stress symptoms were not formally assessed in most instances and were instead inferred from medical record reports and history. The paucity of sound evidence supporting TCQ for post-traumatic stress is consistent with findings for other mental health issues (Vancampfort et al., 2021). These limitations highlight the need for larger, rigorous, and methodologically sound randomized trials to fully understand the effects of TCQ as a treatment for posttraumatic stress.
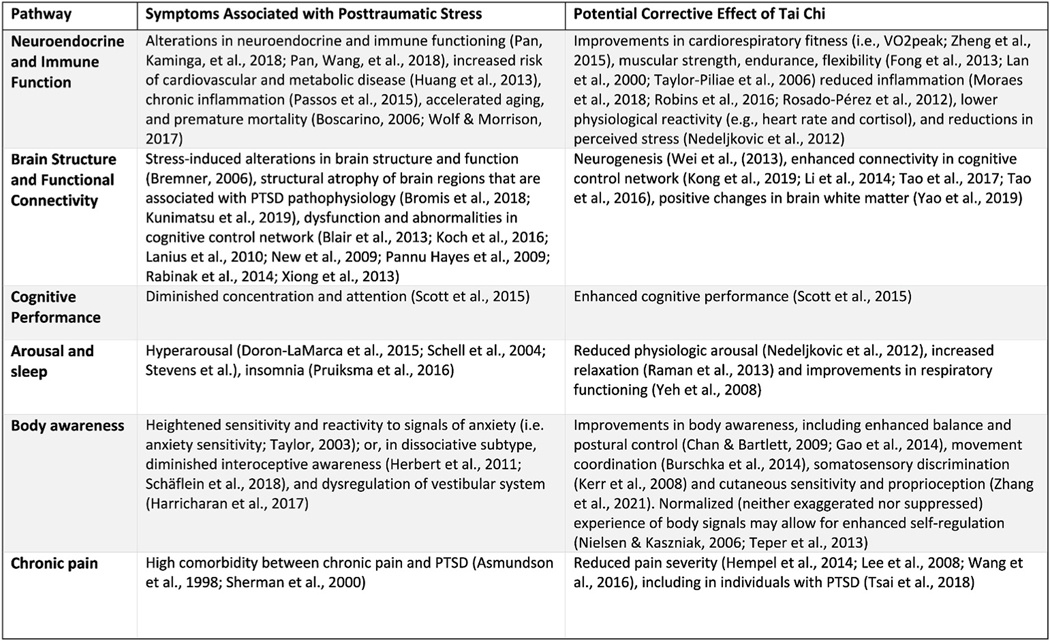
In order to advance the empirical evidence on TCQ for posttraumatic stress, it will be important to explore the potential mechanisms by which the practice of TCQ may improve symptoms and functioning for trauma-exposed individuals. The various components of TCQ may impact symptoms associated with PTSD in multiple individual and synergistic ways, both physiological and psychological. We offer six potential pathways by which TCQ may impact domains of functioning and contribute to positive changes in symptoms associated with PTSD: neuroendocrine and immune function, brain structure and functional connectivity, cognitive performance, arousal and sleep, body awareness, and chronic pain. In Fig. 2 we identified symptoms associated with trauma exposure and posttraumatic stress that are hypothesized to contribute to its physical and psychological sequela along with evidence of TCQ’s potential benefits in these areas. These diverse mechanistic pathways underscore the complexity of TCQ practice and highlight that the multiple potential “active ingredients” included in TCQ interventions are likely interdependent (Wayne & Kaptchuk, 2008). The components of TCQ may shape a gestalt of positive health behaviors and physiological processes that can mitigate the accelerated aging processes associated with chronic stress (Sohn, 2022; Wolf et al., 2019).
Fig. 2.
Proposed mechanistic pathways of Tai Chi’s influence on posttraumatic stress.
Investigation into whether and how TCQ might complement or enhance current treatments could lead to improved physical health outcomes for individuals with posttraumatic stress symptoms. Although it is not yet known whether TCQ may help to reduce the DSM-5 symptoms of PTSD, it is significant to note that the philosophies of integrative practices, such as TCQ, often de-emphasize attention to symptoms and instead emphasize embracing current mind and body sensations, enhancing functioning, and improving well-being and quality of life. Thus, future rigorous research examining TCQ’s effects on a broad range of health and functioning outcomes in trauma-exposed populations is recommended.
5. Conclusions
The empirical evidence to support the use of TCQ in the treatment of posttraumatic stress has not yet been established. The feasibility or descriptive trials reviewed here suggest that future research is warranted to examine the role TCQ may play in reducing suffering in the aftermath of trauma. The multiple interrelated components of TCQ (i.e. physical activity and stretching, mental focus, diaphragmatic breathing, and mindful relaxation) may address the constellation of physical and mental health symptoms associated with posttraumatic stress through a variety of physiological and psychological mechanistic pathways. These components may influence one another and combine synergistically to contribute to enhanced health, improved quality of life, and reduced symptoms. Future rigorous and methodologically sound research in this area has the potential to demonstrate that TCQ can reduce physical and mental health symptoms associated with posttraumatic stress.
Supplementary Material
Acknowledgments
This research was supported by a Clinical Science Research and Development Service award SPLD-004-15S of the US Department of Veterans Affairs (Niles & Mori, PIs)
This research was supported by the Boston Claude D. Pepper Older Americans Independence Center 1P30AG031679 (Reid, PI)
Footnotes
Declaration of competing interest
None.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.mhpa.2022.100449.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Author. [Google Scholar]
- Atwoli L, Stein DJ, Koenen KC, & McLaughlin KA (2015). Epidemiology of posttraumatic stress disorder: Prevalence, correlates and consequences. Curr Opin Psychiatry, 28(4), 307–311. 10.1097/yco.0000000000000167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartoli F, Crocamo C, Alamia A, Amidani F, Paggi E, Pini E, Clerici M, & Carrà G. (2015). Posttraumatic stress disorder and risk of obesity: Systematic review and meta-analysis. [DOI] [PubMed] [Google Scholar]
- van den Berk-Clark C, Secrest S, Walls J, Hallberg E, Lustman PJ, Schneider FD, & Scherrer JF (2018). Association between posttraumatic stress disorder and lack of exercise, poor diet, obesity, and co-occurring smoking: A systematic review and meta-analysis. Health Psychol, 37(5), 407–416. 10.1037/hea0000593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA (2006). Posttraumatic stress disorder and mortality among US Army veterans 30 years after military service. Annals of Epidemiology, 16(4), 248–256. [DOI] [PubMed] [Google Scholar]
- Bromis K, Calem M, Reinders A, Williams SCR, & Kempton MJ (2018). Meta-Analysis of 89 structural MRI studies in posttraumatic stress disorder and comparison with major depressive disorder. American Journal of Psychiatry, 175(10), 989–998. 10.1176/appi.ajp.2018.17111199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y-W, Hunt MA, Campbell KL, Peill K, & Reid WD (2016). The effect of tai chi on four chronic conditions—cancer, osteoarthritis, heart failure and chronic obstructive pulmonary disease: A systematic review and meta-analyses. British Journal of Sports Medicine, 50(7), 397–407. [DOI] [PubMed] [Google Scholar]
- Cohen BE, Marmar C, Ren L, Bertenthal D, & Seal KH (2009). Association of cardiovascular risk factors with mental health diagnoses in Iraq and Afghanistan war veterans using VA health care. JAMA, 302(5), 489–492. 10.1001/jama.2009.1084 [DOI] [PubMed] [Google Scholar]
- Coughlin SS (2011). Posttraumatic stress disorder and cardiovascular disease. The Open Cardiovascular Medicine Journal, 5, 164–170. 10.2174/1874192401105010164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cukor J, Wyka K, Jayasinghe N, & Difede J. (2010). The nature and course of subthreshold PTSD. Journal of Anxiety Disorders, 24(8), 918–923. [DOI] [PubMed] [Google Scholar]
- Davis AA, Zachry CE, & Berke DS (2021). Physical interventions for the treatment of trauma and stressor-related disorders: A comprehensive systematic review. Mental Health and Physical Activity, 20, Article 100401. [Google Scholar]
- Dean KR, Hammamieh R, Mellon SH, Abu-Amara D, Flory JD, Guffanti G, Wang K, Daigle BJ Jr., Gautam A, Lee I, Yang R, Almli LM, Bersani FS, Chakraborty N, Donohue D, Kerley K, Kim TK, Laska E, Young Lee M, … Marmar C. (2019). Multi-omic biomarker identification and validation for diagnosing warzone-related post-traumatic stress disorder. Mol Psychiatry. 10.1038/s41380-019-0496-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Veterans Affairs. (2017). Provision of complementary and integrative health (CIH). [Google Scholar]
- Dobie DJ, Kivlahan DR, Maynard C, Bush KR, Davis TM, & Bradley KA (2004). Posttraumatic stress disorder in female veterans: Association with self-reported health problems and functional impairment. Archives of Internal Medicine, 164(4), 394–400. 10.1001/archinte.164.4.394 [DOI] [PubMed] [Google Scholar]
- Franz MR, Kaiser AP, Phillips RJ, Lee LO, Lawrence AE, Taft CT, & Vasterling JJ (2020). Associations of warzone veteran mental health with partner mental health and family functioning: Family Foundations Study. Depression and Anxiety, 37(11), 1068–1078. 10.1002/da.230831078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, & Swain DP (2011). American college of sports medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med Sci Sports Exerc, 43(7), 1334–1359. 10.1249/MSS.0b013e318213fefb [DOI] [PubMed] [Google Scholar]
- Grodin MA, Piwowarczyk L, Fulker D, Bazazi AR, & Saper RB (2008). Treating survivors of torture and refugee trauma: A preliminary case series using qigong and t’ai chi [case series]. Journal of Alternative and Complementary Medicine, 14(7), 801–806. 10.1089/acm.2007.0736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamblen JL, Norman SB, Sonis JH, Phelps AJ, Bisson JI, Nunes VD, Megnin-Viggars O, Forbes D, Riggs DS, & Schnurr PP (2019). A guide to guidelines for the treatment of posttraumatic stress disorder in adults: An update. Psychotherapy, 56(3), 359–373. 10.1037/pst0000231 [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, & Koffman RL (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351(1), 13–22. [DOI] [PubMed] [Google Scholar]
- Hruby A, Lieberman HR, & Smith TJ (2021). Symptoms of depression, anxiety, and post-traumatic stress disorder and their relationship to health-related behaviors in over 12,000 US military personnel: Bi-directional associations. Journal of Affective Disorders, 283, 84–93. 10.1016/j.jad.2021.01.029 [DOI] [PubMed] [Google Scholar]
- Hundt NE, Mott JM, Miles SR, Arney J, Cully JA, & Stanley MA (2015). Veterans’ perspectives on initiating evidence-based psychotherapy for posttraumatic stress disorder. Psychol Trauma, 7(6), 539–546. 10.1037/tra0000035 [DOI] [PubMed] [Google Scholar]
- Jahnke R, Larkey L, Rogers C, Etnier J, & Lin F. (2010). A comprehensive review of health benefits of qigong and tai chi. Am J Health Promot, 24(6), e1–e25. 10.4278/ajhp.081013-LIT-248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakupcak M, Cook J, Imel Z, Fontana A, Rosenheck R, & McFall M. (2009). Posttraumatic stress disorder as a risk factor for suicidal ideation in Iraq and Afghanistan War veterans. J Trauma Stress, 22(4), 303–306. 10.1002/jts.20423 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey replication. Archives of General Psychiatry, 62(6), 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kibler JL (2009). Posttraumatic stress and cardiovascular disease risk. Journal of Trauma & Dissociation, 10(2), 135–150. 10.1080/15299730802624577 [DOI] [PubMed] [Google Scholar]
- Koch SB, van Zuiden M, Nawijn L, Frijling JL, Veltman DJ, & Olff M. (2016). Aberrant resting-state brain activity in posttraumatic stress disorder: A meta-analysis and systematic review. Depress Anxiety, 33(7), 592–605. 10.1002/da.22478 [DOI] [PubMed] [Google Scholar]
- Kronish IM, Edmondson D, Li Y, & Cohen BE (2012). Post-traumatic stress disorder and medication adherence: Results from the mind your heart study. Journal of Psychiatric Research, 46(12), 1595–1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunimatsu A, Yasaka K, Akai H, Kunimatsu N, & Abe O. (2019). MRI findings in posttraumatic stress disorder. J Magn Reson Imaging. 10.1002/jmri.26929 [DOI] [PubMed] [Google Scholar]
- Lanius R, Bluhm R, Coupland N, Hegadoren K, Rowe B, Theberge J, Neufeld R, Williamson P, & Brimson M. (2010). Default mode network connectivity as a predictor of post-traumatic stress disorder symptom severity in acutely traumatized subjects. Acta Psychiatrica Scandinavica, 121(1), 33–40. [DOI] [PubMed] [Google Scholar]
- Lan C, Lai JS, & Chen SY (2002). Tai Chi Chuan: An ancient wisdom on exercise and health promotion. Sports Medicine, 32(4), 217–224. 10.2165/00007256-200232040-00001 [DOI] [PubMed] [Google Scholar]
- Libby DJ, Pilver CE, & Desai R. (2012). Complementary and alternative medicine in VA specialized PTSD treatment programs. Psychiatric Services, 63(11), 1134–1136. [DOI] [PubMed] [Google Scholar]
- Libby DJ, Pilver CE, & Desai R. (2013). Complementary and alternative medicine use among individuals with posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 5(3), 277. [Google Scholar]
- McFarlane AC, Lawrence-Wood E, Van Hooff M, Malhi GS, & Yehuda R. (2017). The need to take a staging approach to the biological mechanisms of PTSD and its treatment. Current Psychiatry Reports, 19(2), 10. 10.1007/s11920-017-0761-2 [DOI] [PubMed] [Google Scholar]
- Mills KL, McFarlane AC, Slade T, Creamer M, Silove D, Teesson M, & Bryant R. (2011). Assessing the prevalence of trauma exposure in epidemiological surveys. Australian & New Zealand Journal of Psychiatry, 45(5), 407–415. [DOI] [PubMed] [Google Scholar]
- Munro S, Komelski M, Lutgens B, Lagoy J, & Detweiler M. (2019). Improving the health of veterans though moving meditation practices: A mixed-methods pilot study. Journal of Veterans Studies, 5(1), 2019–2020. [Google Scholar]
- Niles BL, Mori DL, Polizzi CP, Kaiser AP, Ledoux AM, & Wang C. (2016). Feasibility, qualitative findings and satisfaction of a brief Tai Chi mind-body programme for veterans with post-traumatic stress symptoms. BMJ Open, 6(11). 10.1136/bmjopen-2016-012464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donovan A, Epel E, Lin J, Wolkowitz O, Cohen B, Maguen S, Metzler T, Lenoci M, Blackburn E, & Neylan TC (2011). Childhood trauma associated with short leukocyte telomere length in posttraumatic stress disorder. Biological Psychiatry, 70(5), 465–471. 10.1016/j.biopsych.2011.01.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Toole BI, & Catts SV (2008). Trauma, PTSD, and physical health: An epidemiological study of Australian vietnam veterans. J Psychosom Res, 64(1), 33–40. 10.1016/j.jpsychores.2007.07.006 [DOI] [PubMed] [Google Scholar]
- Reb AM, Saum NS, Murphy DA, Breckenridge-Sproat ST, Su X, & Bormann JE (2017). Qigong in injured military service members: A feasibility study. Journal of Holistic Nursing, 35(1), 10–24. [DOI] [PubMed] [Google Scholar]
- Reid K, Bannuru R, Wang C, Mori D, & Niles B. (2019). The effects of tai chi mind-body approach on the mechanisms of Gulf war illness: An umbrella review. Integrative Medicine Research, 8, 167–172. 10.1016/j.imr.2019.05.003. Retrieved 2019 May 30, from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AL, Huang T, Koenen KC, Kim Y, Kubzansky LD, & Tworoger SS (2019). Posttraumatic stress disorder is associated with increased risk of ovarian cancer: A prospective and retrospective longitudinal cohort study. Cancer Research, 79(19), 5113–5120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanderson K, & Andrews G. (2006). Common mental disorders in the workforce: Recent findings from descriptive and social epidemiology. Canadian Journal of Psychiatry, 51 (2), 63–75. 10.1177/070674370605100202 [DOI] [PubMed] [Google Scholar]
- Santiago PN, Ursano RJ, Gray CL, Pynoos RS, Spiegel D, Lewis-Fernandez R, Friedman MJ, & Fullerton CS (2013). A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: Intentional and non-intentional traumatic events. PloS One, 8(4), Article e59236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnurr PP (1996). Trauma, PTSD, and physical health. PTSD Research Quarterly, 7(3). [Google Scholar]
- Schnurr PP, Friedman MJ, Sengupta A, Jankowski MK, & Holmes T. (2000). PTSD and utilization of medical treatment services among male Vietnam veterans. The Journal of Nervous and Mental Disease, 188(8), 496–504. [DOI] [PubMed] [Google Scholar]
- Scott KM, Koenen KC, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Benjet C, Bruffaerts R, Caldas-de-Almeida JM, de Girolamo G, Florescu S, Iwata N, Levinson D, Lim CC, Murphy S, Ormel J, Posada-Villa J, & Kessler RC (2013). Associations between lifetime traumatic events and subsequent chronic physical conditions: A cross-national, cross-sectional study. PLoS One, 8(11), Article e80573. 10.1371/journal.pone.0080573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shipherd JC, Keyes M, Jovanovic T, Ready DJ, Baltzell D, Worley V, Gordon-Brown V, Hayslett C, & Duncan E. (2007). Veterans seeking treatment for posttraumatic stress disorder: What about comorbid chronic pain? The Journal of Rehabilitation Research and Development, 44(2). 10.1682/jrrd.2006.06.0065 [DOI] [PubMed] [Google Scholar]
- Smith MW, Schnurr PP, & Rosenheck RA (2005). Employment outcomes and PTSD symptom severity. Mental Health Services Research, 7(2), 89–101. [DOI] [PubMed] [Google Scholar]
- Sohn E. (2022). How the COVID-19 pandemic might age us. Nature, S5–S7. [DOI] [PubMed] [Google Scholar]
- Solloway MR, Taylor SL, Shekelle PG, Miake-Lye IM, Beroes JM, Shanman RM, & Hempel S. (2016). An evidence map of the effect of Tai Chi on health outcomes. Syst Rev, 5(1), 126. 10.1186/s13643-016-0300-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song R, Grabowska W, Park M, Osypiuk K, Vergara-Diaz GP, Bonato P, Hausdorff JM, Fox M, Sudarsky LR, Macklin E, & Wayne PM (2017). The impact of tai chi and qigong mind-body exercises on motor and non-motor function and quality of life in Parkinson’s disease: A systematic review and meta-analysis. Parkinsonism Relat Disord, 41, 3–13. 10.1016/j.parkreldis.2017.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer C, Barnow S, Volzke H, John U, Freyberger HJ, & Grabe HJ (2009). Trauma, posttraumatic stress disorder, and physical illness: Findings from the general population. Psychosomatic Medicine, 71(9), 1012–1017. 10.1097/PSY.0b013e3181bc76b5 [DOI] [PubMed] [Google Scholar]
- Suris A, Lind L, Kashner TM, Borman PD, & Petty F. (2004). Sexual assault in women veterans: An examination of PTSD risk, health care utilization, and cost of care. Psychosom Med, 66(5), 749–756. 10.1097/01.psy.0000138117.58559.7b [DOI] [PubMed] [Google Scholar]
- Taylor-Piliae R, & Finley BA (2020). Benefits of tai chi exercise among adults with chronic heart failure: A systematic review and meta-analysis. Journal of Cardiovascular Nursing, 35(5), 423–434. [DOI] [PubMed] [Google Scholar]
- Tsai PF, Kitch S, Chang JY, James GA, Dubbert P, Roca JV, & Powers CH (2018). Tai chi for posttraumatic stress disorder and chronic musculoskeletal pain: A pilot study [journal article]. Journal of Holistic Nursing : Official Journal of the American Holistic Nurses’ Association, 36(2), 147–158. 10.1177/0898010117697617 [DOI] [PubMed] [Google Scholar]
- Tyrka AR, Price LH, Kao H-T, Porton B, Marsella SA, & Carpenter LL (2010). Childhood maltreatment and telomere shortening: Preliminary support for an effect of early stress on cellular aging. Biological Psychiatry, 67(6), 531–534. 10.1016/j.biopsych.2009.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vancampfort D, Stubbs B, Van Damme T, Smith L, Hallgren M, Schuch F, Deenik J, Rosenbaum S, Ashdown-Franks G, Mugisha J, & Firth J. (2021). The efficacy of meditation-based mind-body interventions for mental disorders: A meta-review of 17 meta-analyses of randomized controlled trials [metaanalysis]. Journal of Psychiatric Research, 134, 181–191. 10.1016/j.jpsychires.2020.12.048 [DOI] [PubMed] [Google Scholar]
- VHA Office of Public Health and Environmental Hazards. (2009). Analysis of VA health care utilization among US global war on terrorism (GWOT) veterans: Operation enduring freedom and operation Iraqi freedom. Washington, DC. [Google Scholar]
- de Vries GJ, & Olff M. (2009). The lifetime prevalence of traumatic events and posttraumatic stress disorder in The Netherlands. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies, 22(4), 259–267. [DOI] [PubMed] [Google Scholar]
- Wang C, Collet JP, & Lau J. (2004). The effect of tai chi on health outcomes in patients with chronic conditions: A systematic review. Archives of Internal Medicine, 164(5), 493–501. [DOI] [PubMed] [Google Scholar]
- Wang C, Schmid CH, Iversen MD, Harvey WF, Fielding RA, Driban JB, Price LL, Wong JB, Reid KF, & Rones R. (2016). Comparative effectiveness of tai chi versus physical therapy for knee osteoarthritis: A randomized trial. Annals of Internal Medicine, 165(2), 77–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wayne PM, & Kaptchuk TJ (2008). Challenges inherent to t’ai chi research: Part II—defining the intervention and optimal study design. The Journal of Alternative and Complementary Medicine, 14(2), 191–197. [DOI] [PubMed] [Google Scholar]
- Williams SL, Williams DR, Stein DJ, Seedat S, Jackson PB, & Moomal H. (2007). Multiple traumatic events and psychological distress: The South Africa stress and health study. Journal of Traumatic Stress, 20(5), 845–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williston SK, Roemer L, & Vogt DS (2019). Cultural and service factors related to mental health beliefs among post-9/11 veterans. Int J Soc Psychiatry, 65(4), 313–321. 10.1177/0020764019842327 [DOI] [PubMed] [Google Scholar]
- Wolf EJ, Bovin MJ, Green JD, Mitchell KS, Stoop TB, Barretto KM, Jackson CE, Lee LO, Fang SC, Trachtenberg F, Rosen RC, Keane TM, & Marx BP (2016). Longitudinal associations between post-traumatic stress disorder and metabolic syndrome severity. Psychol Med, 46(10), 2215–2226. 10.1017/S0033291716000817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf EJ, Morrison FG, Sullivan DR, Logue MW, Guetta RE, Stone A, Schichman SA, McGlinchey RE, Milberg WP, & Miller MW (2019). The goddess who spins the thread of life: Klotho, psychiatric stress, and accelerated aging. Brain Behav Immun, 80, 193–203. 10.1016/j.bbi.2019.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wulfes N, Del Pozo MA, Buhr-Riehm B, Heinrichs N, & Kroger C. (2019). Screening for posttraumatic stress disorder in refugees: Comparison of the diagnostic efficiency of two self-rating measures of posttraumatic stress disorder. J Trauma Stress, 32(1), 148–155. 10.1002/jts.22358 [DOI] [PubMed] [Google Scholar]
- Yost TL, & Taylor AG (2013). Qigong as a novel intervention for service members with mild traumatic brain injury. Explore, 9(3), 142–149. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.