Abstract
Objective
Cupping therapy is an ancient technique of healing used to treat a variety of ailments. An evidence-mapping study was conducted to summarize the existing evidence of cupping therapy for pain-related outcomes and indicate the effect and the quality of evidence to provide a comprehensive view of what is known.
Methods
PubMed, Cochrane Library, Embase, and Web of Science were searched to collect the meta-analyses investigating the association between cupping therapy and pain-related outcomes. The methodological quality was assessed by using the AMSTAR 2 tool. Significant outcomes (p < 0.05) were assessed using the GRADE system. The summary of evidence is presented by bubble plots and human evidence mapping.
Results
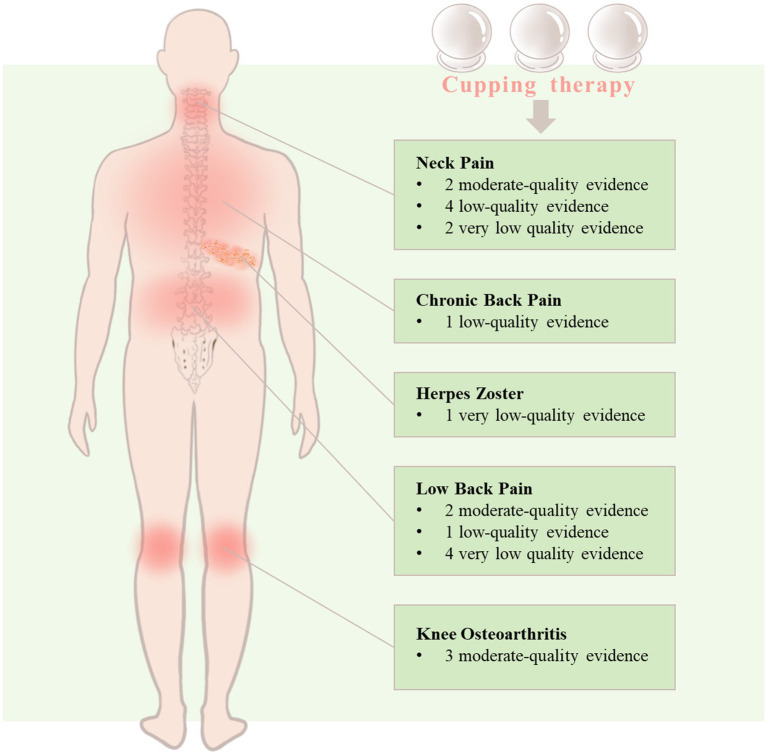
Fourteen meta-analyses covering five distinct pain-related conditions were identified and assessed for methodological quality using the AMSTAR 2, which categorized the quality as critically low (36%), low (50.0%), moderate (7%), and high (7%). In accordance with the GRADE system, no high-quality evidence was found that demonstrates the efficacy of cupping therapy for pain-related outcomes. Specifically, for neck pain, there were two moderate-quality, four low-quality, and two very low-quality evidence, while only one very low-quality evidence supports its efficacy in treating herpes zoster and one low-quality evidence for chronic back pain. Additionally, for low back pain, there were two moderate-quality, one low-quality, and four very low-quality evidence, and for knee osteoarthritis, three moderate-quality evidence suggest that cupping therapy may alleviate pain score.
Conclusion
The available evidence of very low-to-moderate quality suggests that cupping therapy is effective in managing chronic pain, knee osteoarthritis, low back pain, neck pain, chronic back pain, and herpes zoster. Moreover, it represents a promising, safe, and effective non-pharmacological therapy that warrants wider application and promotion.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021255879, identifier: CRD42021255879.
Keywords: cupping therapy, pain-related conditions, systematic review, meta-analysis, evidence mapping
1. Introduction
The definition of pain has been revised to an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage according to the International Association for the Study of Pain (IASP) (1). Pain is the principal reason why individuals seek medical care, with three of the top ten reasons being osteoarthritis, back pain, and headaches (2). Chronic pain poses a significant personal and economic burden, affecting over 30% of the global population and causing psychological distress and sleep issues (3). The Global Burden of Diseases study identified low back pain and migraine as two of the five leading causes of years lived with disability (YLDs) (4). In China, the annual total treatment cost of chronic pain may surpass 500 billion yuan (approximately 685 billion dollars) (5). Although many medications may have limited effectiveness, they often come with significant side effects that can be compounded (6). As a result, alternative complementary treatments are increasingly crucial in the management of pain-related conditions. The demand for complementary and integrative medicine approaches has been on the rise, including mind–body interventions, acupuncture therapy, and other traditional Chinese medicine (TCM) practices (7). Among these, cupping therapy stands out due to its simplicity, safety, and efficacy. Cupping therapy has been widely used in various fields of medicine, including internal medicine, external medicine, gynecology, pediatrics, and particularly in conditions related to pain, skin diseases, knee osteoarthritis, migraines, and other ailments (8).
Cupping therapy, an ancient healing modality, has long been a mainstay in TCM, as well as being documented in the historical records of other regions, including ancient Egypt, Greece, and India. This valuable therapeutic technique has been utilized for thousands of years, and its benefits have been recognized and applied worldwide. It is not only a part of TCM but also recorded in ancient Egypt, Greece, India, and other regions. It is a precious asset to people and has been used worldwide. Cupping therapy involves the application of cups to targeted acupoints or specific skin regions, which creates a negative pressure (9, 10). The modalities of cupping can be broadly classified into dry cupping, wet cupping, massage cupping, etc. (11).
Cupping therapy, initially used as a pain relief method, has now been extended to a broad range of medical conditions (12). Recent evidence shows that this therapy may offer potential benefits for a variety of conditions such as myofascial pain (13), low back pain, ankylosing spondylitis, knee osteoarthritis, neck pain, herpes zoster, migraine, plaque psoriasis, and chronic urticaria (14). For pain-related conditions, cupping might be used as a useful intervention because it decreases the pain level and improves blood flow to the affected area with low adverse effects (15). A clinical study has confirmed that cupping was more effective in improving pain and functional disability in people with persistent non-specific low back pain when compared to sham therapy (16). A single session of dry cupping therapy may be an effective short-term treatment method for immediately reducing pain (17). However, it is worth noting that there exist clinical research findings that do not align with this conclusion. Cupping therapy was not superior to sham cupping for improving pain, physical function, mobility, quality of life, psychological symptoms, or medication use in people with non-specific chronic low back pain (18). Despite this, the National Center for Complementary and Integrative Health (NCCIH) (U.S.) states that although cupping therapy may have some effect in reducing pain, the available evidence is currently insufficient (19). Moreover, although research on this form of therapy has increased, there remains a lack of comprehensive surveys that summarize the efficacy of cupping therapy in managing pain-related conditions. To bridge this gap, the present study endeavors to furnish a comprehensive evaluation of related meta-analyses pertaining to cupping therapy, with a particular focus on the outcomes of pain, as well as to carry out evidence mapping. The primary aim of this study was to provide insights for forthcoming research endeavors.
2. Methods
2.1. Protocol and registration
The protocol of this evidence mapping was registered at the PROSPERO (CRD 42021255879).
2.2. Data sources and search strategy
PubMed, Cochrane Library, Embase, and Web of Science were searched to identify the systematic reviews with meta-analyses on the relationship between cupping therapy and any pain-related conditions published from inception until 15 April 2023. Medical Subject Heading (MeSH) terms and their variants were used for the search strategy for the following terms: “cupping therapy,” “cupping,” “cupping treatment,” “meta-analysis,” “meta-analysis as topic,” “systematic review.” Only published articles in English were considered. We also conducted an extensive review of the pertinent literature, encompassing a range of narrative synopses within the domain. Such a comprehensive approach allowed us to ensure that no substantive sources were overlooked. The details of the search strategies for all databases are given in Supplementary Table S1.
2.3. Inclusion and exclusion criteria
All systematic reviews with meta-analysis related to cupping therapy (including but not limited to dry cupping, wet cupping, moving cupping, etc.) for any pain-related outcomes were included. Conference abstracts, letters, protocols, overviews, and systematic reviews without quantitative meta-analysis were excluded.
2.4. Study selection
All records identified from four databases were imported into Endnote X9 software, and duplicate records removed before screening. After eliminating duplicates, two authors (LW and XL) independently read the titles, abstracts, or full text until all studies are confirmed. Ambiguity was resolved by group discussion.
2.5. Data extraction
For each eligible study, two authors (LW and ZC) extracted the following data independently: first author, publication year, country, study type, type of disease or disorder, number of studies, sample size, intervention, comparison, outcome, type of metric with 95% confidence interval [CI] (i.e., odds ratio [OR], relative risk [RR], risk ratio [HR], standardized mean deviation [SMD], mean deviation [MD]), adverse effect, and the main findings. Ambiguity was resolved by group discussion with the other author (AZ).
2.6. Methodological quality assessment
A measurement tool to assess systematic reviews 2 (AMSTAR 2) (20), which contains 16 items, was used to assess the methodological quality and ranks the quality from critical low to high of the included studies. Two researchers (LW and ZC) independently evaluated the quality of the included studies. The items of the AMSTAR 2 checklist are shown in Supplementary Table S2.
2.7. Evidence quality assessment
We used Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) (21) to assess the quality of evidence for each outcome on four degrees (high, moderate, low, and very low quality) by two reviewers (LW and XL) independently. Any disagreement between reviewers was resolved by discussion, and consistent results were reached finally.
2.8. Evidence mapping presentation
The evidence mapping findings were depicted using bubble plots in a graphical form. Each bubble in the chart denotes clinical evidence from studies that explored the efficacy of cupping for specific pain-related conditions and clinical indications. Excel 2021 was utilized to design the evidence mapping. The X-axis indicates the effect size of the primary outcome visual analog scale (VAS) (p < 0.05), while the Y-axis denotes the number of articles. The size of the bubbles corresponds to the total population’s sample size for the effects of cupping, with bigger bubbles representing a larger sample size. The colors symbolize the different interventions of cupping and non-cupping groups. In addition, we aimed to summarize all the distinct qualities of evidence relating to different pain conditions in human evidence mapping.
3. Results
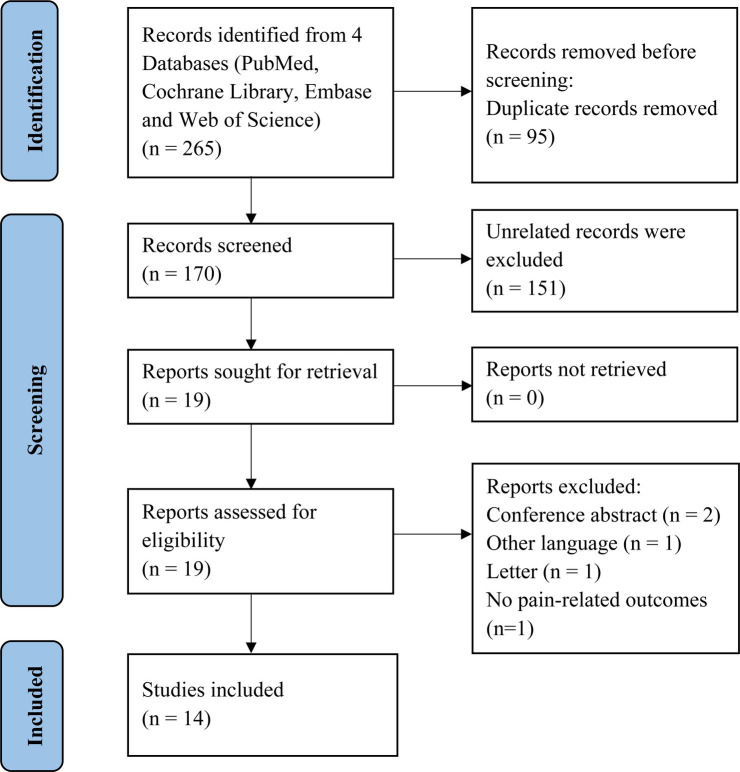
3.1. Study selection
A total of 265 records were identified. After removing duplicates and screening the titles and abstracts, there were 19 potentially eligible studies. We finally included 14 studies (22–35) after assessing for eligibility including five types of pain-related conditions. The study selection process is shown in Figure 1.
Figure 1.
Flow chart of the literature search and screening process.
3.2. Study characteristics
Five studies (23, 26, 28, 30, 31) contained less than ten original studies, while twelve (85.7%) studies (23–30, 32–35) had a combined total sample of over 500 participants. The majority of studies, eight (57.1%) in total (23, 26, 29–31, 33–35), were conducted in China, followed by two (25, 28) in Korea, and one each in Germany (24), Brazil (27), Australia (32), and Iran (22). The included studies investigated various conditions, including low back pain (n = 4), neck pain (n = 3), knee osteoarthritis (n = 2), chronic back pain (n = 1), migraine (n = 1), chronic pain (n = 1), pain-related conditions (n = 1), musculoskeletal pain (n = 1), and herpes zoster (n = 1). The characteristics of included studies are shown in Table 1.
Table 1.
Characteristics of included studies.
| Study | Country | Clinical condition | No. of databases searched | No. of studies | No. of participants | Outcome | Tool for risk of bias assessment |
|---|---|---|---|---|---|---|---|
| Cramer et al. (24) | Germany | Chronic pain | 3 | 18 | 1,172 | Pain intensity | ROB tool |
| Moura et al. (27) | Brazil | Chronic back pain | 7 | 16 | 1,049 | Pain intensity score | Jadad scale |
| Wang 2018 (30) | China | Knee osteoarthritis | 7 | 5 | 535 | VAS, WOMAC-pain | ROB tool |
| Seo et al. (28) | Korea | Migraine | 8 | 6 | 510 | VAS | ROB tool |
| Li et al. (26) | China | Knee osteoarthritis | 7 | 7 | 661 | VAS, WOMAC-pain | ROB tool |
| Zhang et al. (35) | China | Pain-related conditions | 6 | 23 | 2,845 | VAS | ROB tool |
| Wood et al. (32) | Australia | Musculoskeletal pain | 7 | 21 | 1,049 | VAS, NRS, SMPQ, PPT | Downs & Black (D&B) quality assessment scale |
| Kim et al. (25) | Korea | Neck pain | 9 | 18 | 1,683 | VAS, NPQ | ROB tool |
| Wang et al. (31) | China | Low back pain | 3 | 6 | 458 | VAS, MPPI | Jadad scale |
| Azizkhani et al. (22) | Iran | Non-specific neck pain | 10 | 10 | 441 | VAS | ROB tool |
| Cao et al. (23) | China | Herpes zoster | 5 | 8 | 651 | Number of patients with PHN after treatment | Agency for Healthcare Research and Quality |
| Yuan et al. (34) | China | Neck Pain and Low Back Pain | 7 | 11 | 666 | VAS | Cochrane Back Review Group |
| Shen et al. (29) | China | Low Back Pain | 5 | 10 | 690 | VAS, PPI | ROB tool |
| Xie et al. (33) | China | Non-specific low back pain | 7 | 13 | 1,088 | VAS, NRS | ROB tool |
MPPI, McGill present pain index; NPQ, Northwick Park Neck Pain Questionnaire; NRS, numerical rating scale; PHN, postherpetic neuralgia; PPI, present pain intensity; PPT, pain pressure threshold; ROB, risk of bias; SMPQ, Short Form McGill Pain Questionnaire; VAS, visual analog scale; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
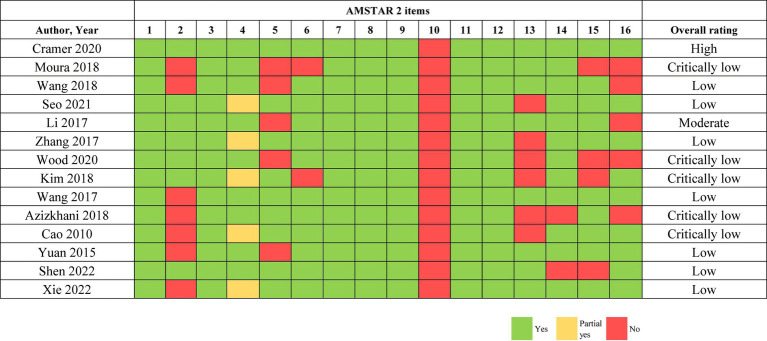
3.3. Methodology quality
One high-quality study (24) and one moderate-quality study (26) were included. However, five studies (22, 23, 25, 27, 32) were rated as critically low quality, and seven studies (28–31, 33–35) were rated as low quality. The primary reasons for these downgraded ratings were noted as the absence of registration and protocols (item 2), poor information regarding the source of funding for the original studies in the systematic review and meta-analysis (item 10), and an inadequate explanation of the risk of bias when discussing the results of the review (item 13). The assessment of methodology quality of included studies by AMSTAR 2 is presented in Figure 2.
Figure 2.
AMSTAR 2 quality assessment.
3.4. Evidence quality
Among the 21 outcomes, the quality of evidence was rated as moderate quality, low quality, and very low quality. Eight moderate-quality evidence are for knee osteoarthritis (n = 3), neck pain (n = 2), low back pain (n = 2), and chronic pain (n = 1). Six low-quality evidence are for neck pain (n = 4), chronic back pain (n = 1), and low back pain (n = 1). Seven very low-quality evidence are for low back pain (n = 4), neck pain (n = 2), and herpes zoster (n = 1). On the basis of two moderate-quality, four low-quality, and two very low-quality evidence, cupping therapy is found to be effective for treating neck pain. Similarly, two moderate-quality, one low-quality, and four very low-quality evidence support the efficacy of cupping therapy in alleviating low back pain. Additionally, three moderate-quality evidence indicate that cupping therapy is useful in managing knee osteoarthritis, while only one very low-quality evidence supports its efficacy in treating herpes zoster and one low-quality evidence for chronic back pain. Furthermore, one moderate-quality evidence supports the use of cupping therapy in managing chronic pain. Table 2 and Supplementary Table S3 provide a detailed account of the GRADE assessment.
Table 2.
Evidence quality of cupping therapy and pain-related outcomes.
| Study | Condition | NO. of studies | NO. of participants | Outcome | Metrics | ES (95%) CI | I2 (%) | Comparison | Evidence quality |
|---|---|---|---|---|---|---|---|---|---|
| Cramer et al. (24) | Chronic Pain | 13 | 718 | Pain intensity | SMD | −1.03 [−1.41, −0.65] | 81 | Cupping vs. no treatment | ⨁⨁⨁〇Moderate |
| Moura et al. (27) | Chronic back pain | 10 | 595 | Pain intensity score | AD | −1.59 [−2.07, −1.10] | 67.7 | Cupping therapy compared to one or more of the following groups: sham, active treatment, waiting list, standard medical treatment, or no treatment | ⨁⨁〇〇Low |
| Wang et al. (30) | Knee osteoarthritis | 2 | 211 | VAS | MD | −1.79 [−2.40, −1.18] | 0 | Dry cupping therapy + Western medicine vs. Western medicine | ⨁⨁⨁〇Moderate |
| 2 | 211 | WOMAC- Pain | MD | −0.73 [−1.03, −0.43] | 0 | Dry cupping therapy + Western medicine vs. Western medicine | ⨁⨁⨁〇Moderate | ||
| Li et al. (26) | Knee osteoarthritis | 2 | 211 | WOMAC- pain | MD | −1.10 [−1.61, −0.41] | 0 | Dry cupping therapy + Western medicine vs. Western medicine | ⨁⨁⨁〇Moderate |
| Wood et al. (32) | Musculoskeletal pain (non-specific neck pain) | 5 | 239 | VAS | MD | −1.29 [−2.05, −0.53] | 94 | Dry cupping vs. no treatment | ⨁〇〇〇Very low |
| 4 | 191 | PPT | SMD | −0.40 [−0.69, −0.11] | 0 | Dry cupping vs. no treatment | ⨁⨁〇〇Low | ||
| Musculoskeletal pain (low back pain) | 2 | 196 | VAS | MD | −19.38 [−28.09, −10.66] | 59 | Dry cupping vs. comparative or control group | ⨁〇〇〇Very low | |
| 2 | 160 | SMPQ | MD | −11.20 [−13.76, −8.64] | 76 | Dry cupping vs. comparative or control group | ⨁〇〇〇Very low | ||
| Kim et al. (25) | Neck pain | 5 | 241 | VAS | MD | −2.42 [−3.98, −0.86] | 93 | Cupping vs. no treatment | ⨁〇〇〇Very low |
| 9 | 870 | VAS | MD | −0.89 [−1.42, −0.37] | 88 | Cupping vs. active control | ⨁⨁〇〇Low | ||
| 1 | 95 | NPQ | MD | 3.59 [2.02, 5.16] | / | Cupping vs. active control | ⨁⨁〇〇Low | ||
| 5 | 534 | VAS | MD | −0.87 [−1.14, −0.61] | 19 | Cupping + active control vs. active control | ⨁⨁⨁〇Moderate | ||
| Wang et al. (31) | Low back pain | 4 | 280 | VAS | SMD | −0.73 [−1.42, −0.04] | 87 | Cupping vs. medication or usual care | ⨁〇〇〇Very low |
| Azizkhani et al. (22) | non-specific neck pain | 5 | 282 | VAS | MD | −0.84 [−1.22, −0.46] | 54.7 | Cupping therapy vs. other or no treatment | ⨁⨁〇〇Low |
| Cao et al. (23) | Herpes zoster | 3 | 326 | Number of patients with PHN after treatment | RR | 0.11 [0.02, 0.56] | 0 | Wet cupping versus medications | ⨁〇〇〇Very low |
| Yuan et al. (34) | Chronic neck pain | 2 | 93 | VAS | WMD | −19.0 [−27.61, −10.58] | 0 | Cupping vs. waitlist | ⨁⨁⨁〇Moderate |
| Chronic low back pain | 7 | 430 | VAS | WMD | −0.54 [−0.89, −0.19] | 84.5 | Cupping vs. medications | ⨁⨁⨁〇Moderate | |
| Shen et al. (29) | Low Back Pain | 3 | 146 | VAS | MD | −1.54 [−1.81, −1.26] | 0 | et cupping vs. non-cupping group | ⨁⨁〇〇Low |
| 4 | 275 | PPI | MD | −2.22 [−3.92, −0.52] | 97 | wet cupping vs. non-cupping group | ⨁〇〇〇Very low | ||
| Xie et al. (33) | Non-specific low back pain | 9 | 736 | VAS | MD | −1.43 [−2.31, −0.54] | 95 | blood pricking and cupping vs. other treatments | ⨁⨁⨁〇Moderate |
AD, absolute difference; CI, confidence interval; ES, effect size; MD, mean deviation; MPPI, McGill present pain index; NPQ, Northwick Park Neck Pain Questionnaire; NRS, numerical rating scale; PHN, postherpetic neuralgia; PPI, present pain intensity; PPT, pain pressure threshold; RR, risk ratio; SMD, standard mean deviation; SMPQ, Short Form McGill Pain Questionnaire; VAS, visual analog scale; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
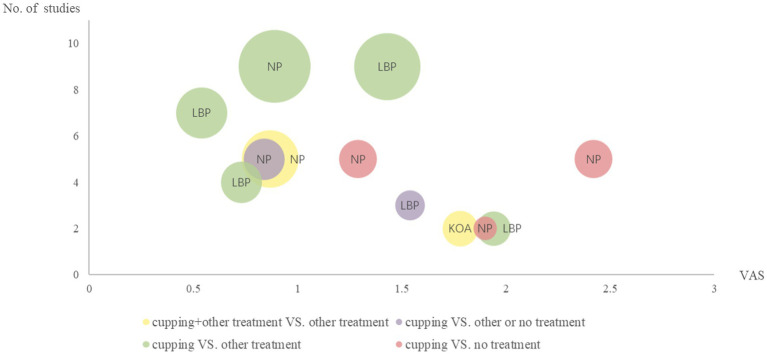
3.5. Evidence mapping
Figure 3 displays the outcomes of the evidence mapping, which graphically presents the evidence in the form of bubbles. The findings of the evidence mapping revealed that cupping therapy effectively alleviates pain (measured via VAS scores) for neck pain, low back pain, and knee osteoarthritis.
Figure 3.
Evidence mapping of cupping therapy. KOA, knee osteoarthritis; NP, neck pain; LBP, low back pain; VAS, visual analog scale. The size of the bubbles corresponds to the total population’s sample size for the effects of cupping, with bigger bubbles representing a larger sample size. The colors symbolize the different interventions of cupping and non-cupping groups.
Figure 4 further elucidates the evidence quality for specific pain conditions. For neck pain, there exist two moderate-quality, four low-quality, and two very low-quality evidence. There exists one low-quality evidence for chronic back pain and one very low-quality evidence for herpes zoster that demonstrates cupping therapy’s effectiveness. Moreover, there are two moderate-quality, one low-quality, and four very low-quality evidence for low back pain, while for knee osteoarthritis, three moderate-quality evidence indicate that cupping therapy can alleviate osteoarthritis pain.
Figure 4.
Grade distribution of evidence of cupping therapy for pain-related conditions.
4. Discussion
4.1. Main findings
In the present evidence-mapping study, comprising 14 meta-analyses, the findings highlight the effectiveness of cupping therapy for various pain-related conditions. This comprehensive overview of systematic reviews summarizes the evidence on the efficacy of cupping therapy for several different pain conditions (chronic back pain, knee osteoarthritis, low back pain, neck pain, and herpes zoster). However, none of the meta-analyses provided high-quality evidence on the effectiveness of cupping therapy on pain-related outcomes. In addition, this study shows that cupping therapy is supported by moderate-quality evidence in the relief of a wide range of pain conditions, including chronic pain, knee osteoarthritis pain, low back pain, and neck pain. Some very low to low-quality evidence supports that cupping therapy for chronic back pain, low back pain, neck pain, and herpes zoster. The quality of current evidence provides good support for the clinical use of cupping therapy and direction for future cupping therapy to play a role in the treatment of other pain outcomes.
4.2. Potential mechanism of cupping therapy
Cupping therapy is an integral part of TCM, in which its effectiveness is increasingly recognized and substantiated by modern clinical medicine, but its physiological mechanisms have no consensus. The mechanisms of cupping therapy that have been proposed include the promotion of blood circulation, neurological reflex, the gate theory of pain, inflammation-immune reaction, and skin tension increase (36).
4.2.1. Neural
There is converging evidence that cupping therapy can induce comfort and relaxation on a systemic level, and the resulting increase in endogenous opioid production in the brain leads to improved pain control (37). Furthermore, cupping therapy has been found to increase immediate pressure pain thresholds in certain areas (38). In addition, the study has revealed that wet cupping therapy can decrease pain in rats via the upregulation of heat shock protein 70 (HSP70) and β-endorphin expression (39).
4.2.2. Hematological
Studies have demonstrated that cupping therapy can augment blood volume and tissue oxygenation at the affected site, whereas reductions in those parameters were observed in the surrounding tissue (40). Moreover, the drawing force in cupping may bring about alteration in blood flow dynamics along with the variation in dermal vascular arrangement. Cupping could positively affect erythrocyte diapedesis from superficial dermal venules. The extravasated erythrocyte may play a mediating role in the proteolytic degradation cascade of hemoglobin. The hemoglobin-derived hemorphins engage opioid receptor signaling and induce the local analgesic effect of cupping (41).
4.2.3. Immune
A study suggests that the mechanism of cupping therapy is that cupping regulates local immunomodulation. The microenvironment is changed when stimulating the surface of the skin, and physical signals transform into biological signals, which also interact with each other in the body. These signaling cascades activate the neuroendocrine-immune system, which produces the therapeutic effect (42).
The mechanisms of cupping therapy for pain reduction are closely related to pain gate theory, diffuse noxious inhibitory controls theory, and reflex zone theory. In summary, several theories have been proposed to explain the effects produced by cupping therapy, and these theories may overlap or alternate, producing various therapeutic effects in a specific disease (43).
4.3. Strengths and limitations
To sum up, our study presents the inaugural overview and evidence mapping of cupping therapy for pain-related outcomes, which comprehensively summarizes the extant evidence. The available evidence quality for the effectiveness of cupping therapy ranges from very low to moderate, with an absence of high-quality evidence. Future research endeavors should concentrate on elucidating the underlying mechanisms of cupping therapy, prioritizing avoidance of adverse events, and optimizing the design and execution of clinical investigations.
Unlike the protocol, our study was limited to pain-related outcomes. The rest of the methods and steps basically followed the contents of the protocol. First of all, the increase of the literature of cupping therapy for pain makes it possible to conduct an evidence mapping. Furthermore, there is consensus among authors that in registration, outcomes cover diverse diseases, but focusing on a certain area after literature screening could better reduce bias. Therefore, we proceeded with the evaluation of pain-related outcomes. We utilized stringent inclusion criteria and restricted our review to English-language literature, which may have increased the likelihood of missing relevant studies. Furthermore, we focused solely on pain-related outcomes, potentially neglecting the impact of cupping therapy on other symptoms, such as functional activities. It is worth noting that non-specific and chronic neck pain were included in our analysis under the umbrella term “neck pain,” while non-specific and chronic low back pain were considered collectively as “low back pain.” Nonetheless, it is essential for better-quality research to validate the current evidence.
5. Conclusion
Cupping therapy appears to be a promising treatment modality for various pain-related disorders. It is effective in the treatment of chronic pain, knee osteoarthritis, low back pain, neck pain, chronic back pain, and herpes zoster. However, the quality of the evidence supporting these outcomes is mostly low quality, with moderate-quality evidence still less available and no high-quality. Therefore, to strengthen these findings, more high-quality clinical studies are also needed to obtain a higher level of evidence. Nonetheless, the potential benefits of cupping therapy in clinical practice make it a valuable intervention for further research and implementation.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
LW: Software, Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Investigation, Methodology. ZC: Data curation, Formal analysis, Investigation, Methodology, Software, Writing – review & editing. XL: Data curation, Formal analysis, Investigation, Methodology, Software, Writing – review & editing. AZ: Conceptualization, Investigation, Supervision, Writing – review & editing.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was funded by the National Key R&D Program of the Ministry of Science and Technology of China Key Special Program for “Modernization Research of Traditional Chinese Medicine” (grant number 2019YFC1708701) and Zhejiang Chinese Medical University’s 2022 School-level Scientific Research Project Talent Project (grant number 2022RCZXZK19).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1266712/full#supplementary-material
References
- 1.Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised international association for the study of pain definition of pain: concepts, challenges, and compromises. Pain. (2020) 161:1976–82. doi: 10.1097/j.pain.0000000000001939, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.St Sauver JL, Warner DO, Yawn BP, Jacobson DJ, McGree ME, Pankratz JJ, et al. Why patients visit their doctors: assessing the most prevalent conditions in a defined american population. Mayo Clin Proc. (2013) 88:56–67. doi: 10.1016/j.mayocp.2012.08.020, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. Lancet. (2021) 397:2082–97. doi: 10.1016/S0140-6736(21)00393-7, PMID: [DOI] [PubMed] [Google Scholar]
- 4.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet. (2017) 390:1211–59. doi: 10.1016/S0140-6736(17)32154-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fan BF. Blue book of pain prevention and health promotion strategy in China: Report on the development of pain medicine in China (2020). Beijing: Tsinghua University Press; (2020). [Google Scholar]
- 6.Dale R, Stacey B. Multimodal treatment of chronic pain. Med Clin N Am. (2016) 100:55–64. doi: 10.1016/j.mcna.2015.08.012 [DOI] [PubMed] [Google Scholar]
- 7.Chen L, Michalsen A. Management of chronic pain using complementary and integrative medicine. BMJ. (2017) 357:j1284. doi: 10.1136/bmj.j1284 [DOI] [PubMed] [Google Scholar]
- 8.Wang SZ, Lu YH, Wu M, Chen KJ, Liu Y, Liu LT. Cupping therapy for diseases: an overview of scientific evidence from 2009 to 2019. Chin J Integr Med. (2021) 27:394–400. doi: 10.1007/s11655-020-3060-y, PMID: [DOI] [PubMed] [Google Scholar]
- 9.Chen B, Guo Y, Chen ZL, Shang XK. Cupping: the common wealth of world traditional medicine. World J Acupunct Moxibust. (2016) 26:1–13. doi: 10.1016/S1003-5257(17)30055-7 [DOI] [Google Scholar]
- 10.Mehta P, Dhapte V. Cupping therapy: a prudent remedy for a plethora of medical ailments. J Tradit Complement Med. (2015) 5:127–34. doi: 10.1016/j.jtcme.2014.11.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aboushanab TS, Alsanad S. Cupping therapy: an overview from a modern medicine perspective. J Acupunct Meridian Stud. (2018) 11:83–7. doi: 10.1016/j.jams.2018.02.001, PMID: [DOI] [PubMed] [Google Scholar]
- 12.Hasbani GE, Jawad A, Uthman I. Cupping (hijama) in rheumatic diseases: the evidence. Mediterr J Rheumatol. (2021) 32:316–23. doi: 10.31138/mjr.32.4.316, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chiu YC, Manousakas I, Kuo SM, Shiao JW, Chen CL. Influence of quantified dry cupping on soft tissue compliance in athletes with myofascial pain syndrome. PLoS One. (2020) 15:e0242371. doi: 10.1371/journal.pone.0242371, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choi TY, Ang L, Ku B, Jun JH, Lee MS. Evidence map of cupping therapy. J Clin Med. (2021) 10:1750. doi: 10.3390/jcm10081750, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mohamed AA, Zhang X, Jan YK. Evidence-based and adverse-effects analyses of cupping therapy in musculoskeletal and sports rehabilitation: a systematic and evidence-based review. J Back Musculoskelet Rehabil. (2023) 36:3–19. doi: 10.3233/BMR-210242, PMID: [DOI] [PubMed] [Google Scholar]
- 16.Salemi MM, Gomes VMDSA, Bezerra LMR, Melo TMS, Alencar GG, Montenegro IHPM, et al. Effect of dry cupping therapy on pain and functional disability in persistent non-specific low Back pain: a randomized controlled clinical trial. J Acupunct Meridian Stud. (2021) 14:219–30. doi: 10.51507/j.jams.2021.14.6.219, PMID: [DOI] [PubMed] [Google Scholar]
- 17.Stephens SL, Selkow NM, Hoffman NL. Dry cupping therapy for improving nonspecific neck pain and subcutaneous hemodynamics. J Athl Train. (2020) 55:682–90. doi: 10.4085/1062-6050-236-19, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Almeida Silva HJ, Barbosa GM, Scattone Silva R, Saragiotto BT, Oliveira JMP, Pinheiro YT, et al. Dry cupping therapy is not superior to sham cupping to improve clinical outcomes in people with non-specific chronic low back pain: a randomised trial. J Physiother. (2021) 67:132–9. doi: 10.1016/j.jphys.2021.02.013 [DOI] [PubMed] [Google Scholar]
- 19.National Center for Complementary and Integrative Health . (2018). Cupping [EB/OL]. Available at: https://www.nccih.nih.gov/health/cupping (Accessed June 19, 2021)
- 20.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. Amstar 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:j4008. doi: 10.1136/bmj.j4008, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. Grade: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. (2008) 336:924–6. doi: 10.1136/bmj.39489.470347.AD, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Azizkhani M, Ghorat F, Soroushzadeh S, Karimi M, Yekaninejad S. The effect of cupping therapy on non-specific neck pain: a systematic review and meta-analysis. Iran Red Crescent Med J. (2018) 20:e55039. doi: 10.5812/ircmj.55039 [DOI] [Google Scholar]
- 23.Cao H, Zhu C, Liu J. Wet cupping therapy for treatment of herpes zoster: a systematic review of randomized controlled trials. Altern Ther Health Med. (2010) 6:364–70. doi: 10.1016/j.explore.2010.08.001, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cramer H, Klose P, Teut M, Rotter G, Ortiz M, Anheyer D, et al. Cupping for patients with chronic pain: a systematic review and meta-analysis. J Pain. (2020) 21:943–56. doi: 10.1016/j.jpain.2020.01.002, PMID: [DOI] [PubMed] [Google Scholar]
- 25.Kim S, Lee SH, Kim MR, Kim EJ, Hwang DS, Lee J, et al. Is cupping therapy effective in patients with neck pain? A systematic review and meta-analysis. BMJ Open. (2018) 8:e21070: e021070. doi: 10.1136/bmjopen-2017-021070, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li JQ, Guo W, Sun ZG, Huang QS, Lee EY, Wang Y, et al. Cupping therapy for treating knee osteoarthritis: the evidence from systematic review and meta-analysis. Complement Ther Clin Pract. (2017) 28:152–60. doi: 10.1016/j.ctcp.2017.06.003, PMID: [DOI] [PubMed] [Google Scholar]
- 27.Moura CC, Chaves É, Cardoso A, Nogueira DA, Corrêa HP, Chianca T. Cupping therapy and chronic back pain: systematic review and meta-analysis. Rev Lat Am Enfermagem. (2018) 26:e3094. doi: 10.1590/1518-8345.2888.3094, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Seo J, Chu H, Kim CH, Sung KK, Lee S. Cupping therapy for migraine: a prisma-compliant systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. (2021) 2021:7582581. doi: 10.1155/2021/7582581, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shen WC, Jan YK, Liau BY, Lin Q, Wang S, Tai CC, et al. Effectiveness of self-management of dry and wet cupping therapy for low back pain: a systematic review and meta-analysis. Medicine. (2022) 101:e32325. doi: 10.1097/MD.0000000000032325, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang YL, An CM, Song S, Lei FL, Wang Y. Cupping therapy for knee osteoarthritis: a synthesis of evidence. Complement Med Res. (2018) 25:249–55. doi: 10.1159/000488707, PMID: [DOI] [PubMed] [Google Scholar]
- 31.Wang YT, Qi Y, Tang FY, Li FM, Li QH, Xu CP, et al. The effect of cupping therapy for low back pain: a meta-analysis based on existing randomized controlled trials. J Back Musculoskelet Rehabil. (2017) 30:1187–95. doi: 10.3233/BMR-169736, PMID: [DOI] [PubMed] [Google Scholar]
- 32.Wood S, Fryer G, Tan L, Cleary C. Dry cupping for musculoskeletal pain and range of motion: a systematic review and meta-analysis. J Bodyw Mov Ther. (2020) 24:503–18. doi: 10.1016/j.jbmt.2020.06.024, PMID: [DOI] [PubMed] [Google Scholar]
- 33.Xie CJ, Sun ZY, Ji CC, Jinsheng Y. Efficacy and safety of blood pricking and cupping for treating nonspecific low back pain: a systematic review and meta-analysis. J Tradit Chin Med. (2022) 42:869–76. doi: 10.19852/j.cnki.jtcm.20220922.003, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yuan QL, Guo TM, Liu L, Sun F, Zhang YG. Traditional Chinese medicine for neck pain and low back pain: a systematic review and meta-analysis. PLoS One. (2015) 10:e117146. doi: 10.1371/journal.pone.0117146, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang YJ, Cao HJ, Li XL, Yang XY, Lai BY, Yang GY, et al. Cupping therapy versus acupuncture for pain-related conditions: a systematic review of randomized controlled trials and trial sequential analysis. Chin Med. (2017) 12:21. doi: 10.1186/s13020-017-0142-0, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hou X, Bai ZM, Liu JM. Physiological mechanisms and clinical research progress of cupping therapy. Acupunct Res. (2021) 46:254–8. doi: 10.13702/j.1000-0607.200334, PMID: [DOI] [PubMed] [Google Scholar]
- 37.Rozenfeld E, Kalichman L. New is the well-forgotten old: the use of dry cupping in musculoskeletal medicine. J Bodyw Mov Ther. (2016) 20:173–8. doi: 10.1016/j.jbmt.2015.11.009, PMID: [DOI] [PubMed] [Google Scholar]
- 38.Emerich M, Braeunig M, Clement HW, Lüdtke R, Huber R. Mode of action of cupping--local metabolism and pain thresholds in neck pain patients and healthy subjects. Complement Ther Med. (2014) 22:148–58. doi: 10.1016/j.ctim.2013.12.013 [DOI] [PubMed] [Google Scholar]
- 39.Subadi I, Nugraha B, Laswati H, Josomuljono H. Pain relief with wet cupping therapy in rats is mediated by heat shock protein 70 and ß-endorphin. Iranian J Med Sci. (2017) 42:384–91. PMID: [PMC free article] [PubMed] [Google Scholar]
- 40.Kim S, Kim E, Jung G, Lee S, Kim JG. The hemodynamic changes during cupping therapy monitored by using an optical sensor embedded cup. J Biophotonics. (2019) 12:e201800286. doi: 10.1002/jbio.201800286, PMID: [DOI] [PubMed] [Google Scholar]
- 41.Song C, Wang Q, Song N. Hemorphin-based analgesia: a mechanism of cupping technique? J Pain Res. (2023) 16:1751–4. doi: 10.2147/JPR.S413021, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guo Y, Chen B, Wang DQ, Li MY, Lim CH, Guo Y, et al. Cupping regulates local immunomodulation to activate neural-endocrine-immune worknet. Complement Ther Clin Pract. (2017) 28:1–3. doi: 10.1016/j.ctcp.2017.04.005, PMID: [DOI] [PubMed] [Google Scholar]
- 43.Al-Bedah A, Elsubai IS, Qureshi NA, Aboushanab TS, Ali G, El-Olemy AT, et al. The medical perspective of cupping therapy: effects and mechanisms of action. J Tradit Complement Med. (2018) 9:90–7. doi: 10.1016/j.jtcme.2018.03.003, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.