Abstract
Generalised Anxiety Disorder (GAD) is a prevalent, chronic mental health disorder. The measurement of regional brain gamma-aminobutyric acid (GABA) offers insight into its role in anxiety and is a potential biomarker for treatment response. Research literature suggests Piper methysticum (Kava) is efficacious as an anxiety treatment, but no study has assessed its effects on central GABA levels. This study investigated dorsal anterior cingulate (dACC) GABA levels in 37 adult participants with GAD. GABA was measured using proton magnetic resonance spectroscopy (1H-MRS) at baseline and following an eight-week administration of Kava (standardised to 120 mg kavalactones twice daily) (n = 20) or placebo (n = 17). This study was part of the Kava for the Treatment of GAD (KGAD; ClinicalTrials.gov: NCT02219880), a 16-week intervention study. Compared with the placebo group, the Kava group had a significant reduction in dACC GABA (p = 0.049) at eight weeks. Baseline anxiety scores on the HAM-A were positively correlated with GABA levels but were not significantly related to treatment. Central GABA reductions following Kava treatment may signal an inhibitory effect, which, if considered efficacious, suggests that GABA levels are modulated by Kava, independent of reported anxiety symptoms. dACC GABA patterns suggest a functional role of higher levels in clinical anxiety but warrants further research for symptom benefit. Findings suggest that dACC GABA levels previously un-examined in GAD could serve as a biomarker for diagnosis and treatment response.
Keywords: anterior cingulate, GABA, generalised anxiety disorder, kava, magnetic resonance spectroscopy
1. Introduction
Generalised Anxiety Disorder (GAD) is a clinically challenging, prevalent, and chronic affective disorder associated with functional disablement, frequent comorbidities, and high psychological distress [1,2]. It is characterised by the two leading cognitive symptoms of persistent worry and anticipatory anxiety [3]. GAD prevalence and severity may be underreported, due in part to low diagnostic reliability [4,5,6,7]. Current stepped-care treatment for GAD typically involves antidepressant and benzodiazepine pharmacotherapies as well as cognitive behavioural therapy (CBT) [8,9,10]. These approaches, however, provide modest clinical effect and have limited utility for many patients [11,12,13,14,15,16]. Moreover, novel drug development has not progressed for two decades [6,17,18,19,20,21], leading many consumers to utilise anxiolytic phytomedicines [22,23].
GAD remains the most understudied of the anxiety disorders [6,24]. One promising avenue to advance GAD diagnosis and the assessment of treatment efficacy is to investigate the neuroimaging biomarkers [25,26,27,28] that may offer insight into the mechanisms of anxiety; however, the extent to which brain metabolic processes are instrumental in pathology remains unclear.
1.1. Gamma-Aminobutyric Acid (GABA) and Quantification in the CNS
GABA (C4H9NO2C4) is a non-standard amino acid that acts as the major inhibitory neurotransmitter [29,30]. GABA is distributed throughout the brain but is highly concentrated in cortical and limbic areas associated with ‘anxiety circuitry’ [31,32]. In these regions, multi-modal neuroimaging studies demonstrate a trend of emotion task-dependent stronger negative BOLD signal observed with a higher resting state GABA [33,34,35].
In pre-clinical rodent models, high anxiety-behaviour mice exhibit higher levels of amygdala GABA and a greater expression of GABA pathway components GAD65 and GAD67 than normal anxiety-behaviour mice [36]. Clinical studies place GABA in a central role in neuropathology across anxiety states and disorders [15,32,34,37,38,39], whereby elevated GABA is associated with anxiety cognitions in healthy samples in the ventral-medial prefrontal cortex (vmPFC) [40] and the medial pre-frontal cortex in post-traumatic stress disorder (PTSD) [41]. However, in PTSD, GABA levels are reduced compared to controls in the lateral temporal lobe, ACC, insula, and parieto-occipital cortices, but no differences are observed in the dACC region [42,43]. In panic disorder, GABA is reduced in the occipital and ACC regions and the basal ganglia [44,45], but it is not different in the pre-frontal cortex [46]. Social Anxiety Disorder (SAD) research suggests reduced thalamic GABA levels but no other regional differences compared with controls [47]. Taken together, the evidence suggests that GABA varies by region and disorder, but no research has yet directly assessed regional levels in GAD adults compared with healthy controls. In GAD intervention research, other metabolites such as n-acetyl aspartate following riluzole or paroxetine administration [48,49,50] have been investigated, but no study has thus far assessed GABA levels as a product of anxiolytic treatment.
1.2. The Dorsal Anterior Cingulate Cortex (dACC) as a Region of Interest
The ACC has a central role in the organisation of affective and cognitive information that underpin anxiety states via its connectivity to prefrontal-cortical, lower limbic, and hippocampal regions [51,52,53,54,55]. Sub-regions of the ACC are implicated in GAD symptomatology—notably, anticipatory anxiety and negative bias cognitions [56,57,58,59]. Structural and functional studies support a rostral/affective and a dorsal/cognitive division of ACC sub-regions, with a heterogeneous and integrative role of the latter in the cognitive components of emotional processing [51,53,60,61,62].
This dorsal region comprises a fear network along with the ventromedial prefrontal cortex and amygdala [63,64], with GABA levels in this region contributing to the maintenance of anxiety cognition–emotion fear responses and reducing fear extinction [61,62], suggesting that the cognitive control of worry thoughts is a hallmark of GAD. Yet, despite the evidence that ACC sub-regions are a significant predictor in intervention studies—at least in structural and functional studies [26,64]—it has received little focus in terms of metabolic data quantification to establish patterns in GAD symptomology, and for these reasons, the dACC is of particular interest in this investigation.
1.3. Kava for the Treatment of GAD Symptoms
The phytomedicine Piper methysticum (Kava) holds a compelling evidence base for the alleviation of anxiety symptoms [65,66,67,68], and it is a popular consumer treatment with over 1.2 million Kava extract tablets prescribed or purchased annually in Australia [69]. The water extraction method is the only allowable process in Australia, and tableted Kava products are typically standardised to 30% kavalactones, constituting quantities of 80 to 250 mg.
The Kava plant is a perennial shrub of the pepper family Piperaceae, and it is native to the South Pacific, where the rootstock lipid resin has been used for millennia in traditional medicine for its anxiolytic, nootropic, neuroprotective, nociceptive, and anti-dysphoria effects [70,71,72,73]. The chief bioactive constituents are kavalactones, six of which comprise the majority of Kava’s pharmacodynamic effects: dihydrokavain/dihydrokawain, kavain/kawain, dihydromethysticin, methysticin, yangonin, and demethoxyyangonin, in order of typical proportion [74,75,76,77].
The proposed mechanism of the GABAergic effect occurs through the positive modulation of multiple benzodiazepine binding sites, including GABA-A and GABA-B from kavain, yangonin, dehydromethysticin, and desmethoxyyangonin, through both enhanced ligand displacement and binding [75,78,79,80]. Pre-clinical studies also suggest mechanisms occurring within the GABA metabolic shunt, such as the modulation of the calcium ion channel blockade of the monoamine oxidase-B receptor substrate, thereby inhibiting glutamate and promoting GABA synthesis [70,81,82,83].
Previous Kava investigations in anxiety report significant improvements on anxiety scales, such as the HAM-A [22,84,85]. However, only one study has investigated the modulation of brain markers. In an electroencephalography (EEG) resting state study [86], acute doses of kavain (200, 400, 600 mg), placebo, and 30 mg of clobazam were administered to a healthy sample (n = 15). Significant dose-dependent increases were observed in frontal lobe delta, theta, and alpha 1 activity in the frontal lobe and, together with improvements to mood and wellbeing measures, were reported in the kavain group. The psychotropic effects and topographic pattern differed from the benzodiazepine, particularly with 200 mg, where benefits to mood measures were reported, but sedation was reported at higher doses. The data are consistent with pre-clinical models on kavain as a positive allosteric modulator of the GABA-A receptor outside the typical benzodiazepine site binding [75]. Data from this study contribute to the evidence of unique GABAergic action with kavalactones, supported by pre-clinical tissue studies. This single study also highlights the need to examine Kava effects via other neuroimaging modalities to better understand its neurobiological mechanisms.
To this end, this study aimed to investigate changes to GABA levels in the dorsal ACC in a GAD sample following the daily ingestion of Kava extract for eight weeks in comparison with a placebo group. This study also aimed to assess the relationship between GABA levels and changes to reported anxiety symptoms as a product of Kava consumption over the same period. It was expected that dACC GABA levels would decrease after Kava treatment and a reduction to anxiety symptoms would also be observed in comparison with the placebo group.
2. Methods and Materials
2.1. Design
This neuroimaging sub-study was conducted as part of the Kava for the Treatment of Generalised Anxiety Disorder clinical trial (KGAD) [87], a double-blinded, placebo-controlled investigation of 16-week’s administration of Kava in individuals with GAD. The sub-study’s eight-week duration was selected based on kava pharmacodynamics in both pre-clinical and clinical efficacy studies. The KGAD trial was registered via ClinicalTrials.gov (NCT02219880), with approval from the University of Melbourne/Alfred Hospital, the University of Queensland, and Swinburne University’s Human Research Ethics Committee. The clinical trial was conducted in accordance with the Declaration of Helsinki.
2.2. Participants
Participants involved in the neuroimaging component of the study were adults aged 18–65 years with Generalized Anxiety Disorder; n = 37 (male n = 18). Screening and eligibility criteria can be found in both the protocol and main outcome papers for the KGAD study [87,88] and are summarised in Appendix A. All enrolled participants received a bursary of $200 to cover expenses. Written and informed consent was collected from all participants before comprehensive screening for eligibility.
2.3. Sample Size
With an a priori population sample size of N = 40 (n = 20 per group), a 95% confidence interval, a 5% margin of error (for a standard alpha of 0.05), and a small-to-medium effect size (confidence interval reporting was the chosen parameter), a minimum total sample size of n = 37 was determined using the G.Power calculation program [89].
2.4. Measures
2.4.1. Screening and Eligibility
The Mini-International Neuropsychiatric Interview (MINI 6.0) [90] was used to confirm the presence of current GAD according to the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5) [91], as well as identify secondary anxiety disorders and major depressive disorder (MDD) and the exclusion of other disorders. To ensure current GAD, moderate levels of anxiety (minimum 18 score) were required for enrolment to the study, assessed via the Hamilton Anxiety Rating Scale (HAM-A) [92]. The Montgomery–Asberg Depression Rating Scale (MADRS) [93] was utilised at both time points in the GAD group to ensure that symptoms of depression were not primary upon enrolment nor emergent following treatment (maximum score 18). The Structured Interview Guide for the MADRS was administered using a standardised line of questioning to ensure reliability and consistency (SIGMA) [94].
2.4.2. Assessment of Comorbidity in GAD
Comorbidity (anxiety disorder or major depression) is not typically accounted for in neuroimaging studies with GAD samples. The prevalence of comorbidity in GAD is higher compared with other affective disorders, amplifying impairment [95,96]. Allowable secondary conditions were SAD, panic disorder with/without agoraphobia, and phobic disorder. MDD history was allowable if no episodes had occurred in the previous three years. This approach considers the likelihood of overlap in diagnoses in GAD where symptoms might be best explained by comorbidities such as MDD. Additional comorbid conditions may imply an increased severity of symptoms where higher anxiety measure scores may be observed. For this reason, a comorbid presence was either defined as a separate GAD group or used as a covariate in regression models.
2.4.3. Assessment of Anxiety
The HAM-A is a 14-item 5-point Likert scale to quantify the severity of anxiety symptomatology. The Structured Interview version (SIGH-A) was used in this study to ensure a standardised questioning format in the assessment of anxiety levels at baseline and eight-week time points. The reliability and validity of the SIGH-A was assessed to be moderate to high [97].
2.5. H-MRS Protocol
A 3T Siemens TIM Trio magnetic resonance imaging system (Erlangen, Germany) with a 32-channel head coil housed at Swinburne Neuroimaging Centre (Hawthorn, Australia) was used for collecting 1H-MRS and T1-weighted structural imaging data. T1-weighted images were acquired for the localisation of the MRS voxel at dorsal anterior cingulate cortex (high-resolution 1 mm3, 176 slices, voxel resolution = 1.0 × 1.0 × 7.0 mm3, TR = 1900 ms, TE = 2.52 ms, flip angle = 9°, field of view 256 × 256 mm, orientation sagittal, acquisition time = ~3 min).
GABA quantification was conducted using Mescher–Garwood algorithm (MEGA) [98] in a Point RESolved Spectroscopy sequence (MEGA-PRESS), which is sensitive to GABA by editing the J-coupling between GABA-3 (peak at 3.01 ppm) and GABA-4 (peak at 1.89 ppm). The details of the sequences are as follows: TE = 68, TR = 2000, suppression freq. = 1.95 ppm, Ave = 64, ~5 min, editing pulse at 1.95 ppm (edit-on) interleaved with scans with a pulse at 7.5 ppm (edit-off). The water signal (unsuppressed signal) was acquired at the identical location with 16 averages for two minutes’ duration. Shimming was automatic and manual until the linewidth was less than 20 Hz for the 80/68 TE PRESS and MEGA-PRESS sequences.
2.5.1. Voxel Placement and Check
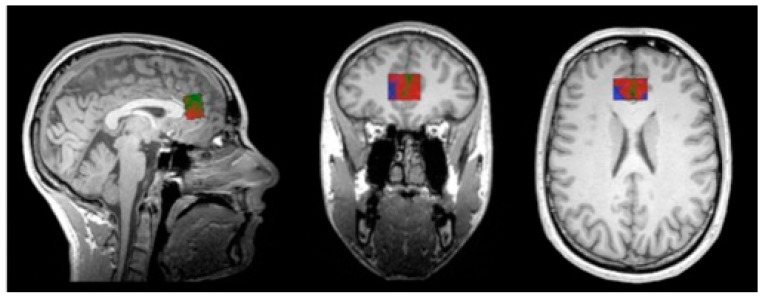
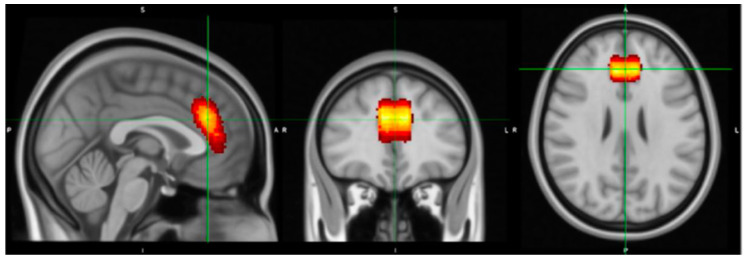
The MRS voxel was 25 × 25 × 15 mm and covered the dACC. An in-house MATLAB (R2013b) script was applied to build a voxel image based on the location information on the head of MRS data. This voxel image indicates the location of the MRS voxel, when overlapping on the corresponding structural image at the same scan session. To check whether the location of the MRS voxel covered the target region, i.e., dACC at coordinates [0, 34, 26] in MNI (standard) space, individual structural images were co-registered to a MNI template, and the same transform matrix was applied on the corresponding voxel images. Finally, tissue segmentation was conducted at individual space to segment grey matter (GM), white matter (WM), and CSF. The volumetric proportion (percentage) of each tissue type within the MRS voxel was further calculated for partial volume correction and quality check (refer to Figure 1). All individual voxel images were summarised and plotted on top of an MNI template using MRIcron [99], visible in Figure 2, where the dACC was well covered.
Figure 1.
An example of tissue segmentation at individual space to segment grey matter (GM), white matter (WM), and CSF. The volumetric proportion (percentage) of each tissue type within the MRS voxel was further calculated for a partial volume correction check.
Figure 2.
The averaged voxel location for MRS for all scans transferred into MNI space; the target region is the dorsal subregion of the anterior cingulate cortex (dACC).
2.5.2. GABA Analysis
The difference spectrum (edit-on versus edit-off) was used to quantify the concentration of metabolites, including GABA. Fit checks were performed during preprocessing using GANNET, which utilises a peak fitting/integration method and applies a stricter model in its Fit Error quality control, aiding the removal of spurious cases [100]. Following vetting of the data against quality check parameters (SNR > 5, SD < 20%, FWHM < 0.15), the voxel location was also visually inspected by overlapping the reconstructed voxel image and the T1-weighted MR image using in-house script and the MRIcron program. The LCModel toolbox (version 6.1) [101,102] is a widely used program for 1H-MRS analyses, and a standard GABA basis set, matching the imaging protocol, was used for model fittings.
Partial volume correction (e.g., voxel segmentation) is a crucial component of the imaging pipeline when assessing voxel metabolite levels to prevent the inflation of quantification data that come from variances in grey and white matter [103,104,105,106]. As the concentration of GABA in grey matter is substantially higher than in white matter, further partial volume effects were corrected approximately by considering the grey matter volume ratio of the voxel of interest [107]. Briefly, tissue segmentation was conducted at a whole brain level by SPM12; then, the reconstructed MRS voxel (detailed in Section 2.5.1) were overlapped on tissue maps to determine the volume of grey matter, white matter, and CSF. The corrected GABA concentration was converted using the equation below, where GMV, WMV, and CSF represents the volume of grey matter, white matter, and CSF.
2.6. Treatment Handling
Procedures relating to treatment randomisation, the handling of treatment-related adverse events, and liver function assessment, as well as treatment compliance, are detailed in the KGAD study protocol and main outcome papers.
2.7. Statistical Analyses
Data were analysed using the IBM Statistical Package for Social Sciences software (SPSS; v.22, Armonk, NY, USA). All relevant demographic data were assessed at baseline treatment group differences via simple significance testing (t-tests and non-parametric tests were used when parametric criteria were not met), following quality checks for outliers and missing or incorrect data. Volumetric data, GABA QC variables, and GABA concentration results were reported separately by means and SDs for the variable of interest. It is feasible that age and sex-related differences would be observable in the samples tested in this study, potentially affecting results if not accounted for. For this reason, age and sex were employed in all group-based analyses to best delineate treatment group-based differences in function and GABA. An initial correlation test was performed to assess the relationship between GABA concentration levels and anxiety baseline data with covariates of sex, age, and comorbidity.
Intervention analyses were performed using a custom main effects format for GABA outcomes, with the main outcome reported from the interaction of treatment x time on GABA concentration and a linear mixed model format for treatment x time x GABA significance on anxiety symptoms change. Confidence intervals were reported to establish parameter estimates, with a proportion of variance (reported in the text as a percent) for significant predictors. Statistical findings were considered significant if the probability value p ≤ 0.05.
3. Procedure
Participants attended a screening session at the study site (Swinburne University of Technology, Melbourne) to assess study eligibility, followed by a baseline session, a supply of study treatment (240 mg daily tablets of kava or placebo), and a follow-up at eight weeks. Sociodemographic information included age in years, sex (male/female), BMI, medical conditions, alcohol consumption per week, allowable medication use (prophylactics), and eligible vitamins and supplements as determined by the protocol for the KGAD study [87]. Blood samples were collected at screening and follow up to assess liver function following overnight fasting, without alcohol or caffeine in the previous 24 h period. A standardised breakfast was provided followed by demographic data collection and psychiatric assessments. The scan was conducted in the same building one hour following arrival for the testing sessions. Processes, including the time of visit and scheduled scan, were replicated at the second time point (eight weeks).
4. Results
4.1. Description of the Study Population
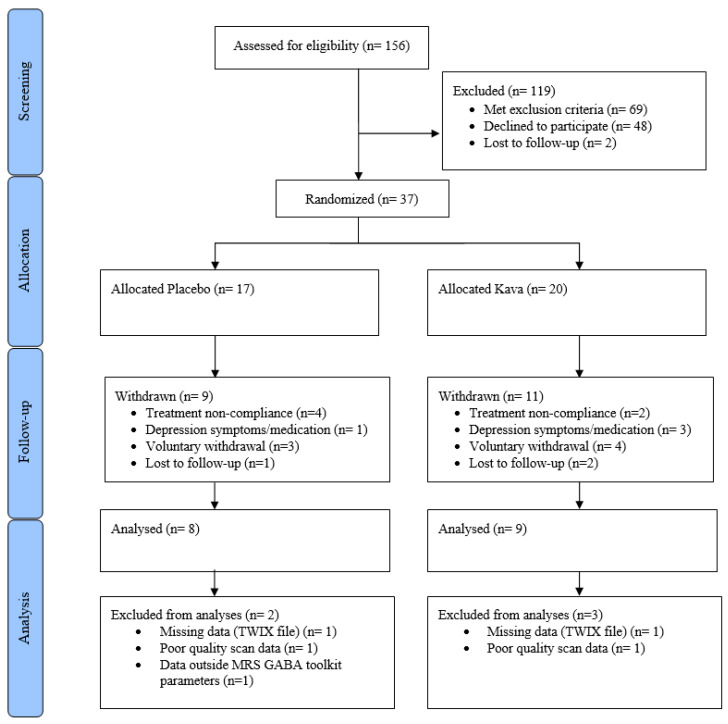
The CONSORT diagram in Figure 3 illustrates the study processes as well as participant numbers at screening, allocation, follow-up, and analysis. Demographic statistics overall and per treatment groups, including HAM-A scores and GABA data, are reported in Table 1. Treatment groups at baseline showed no significant differences in demographic data including age, sex, years of education, medication use, and caffeine or alcohol use. Baseline HAM-A scores for anxiety and the MADRS for depression symptoms were not significantly different between treatment groups (p = 0.714; p = 0.456, respectively).
Figure 3.
CONSORT diagram for intervention.
Table 1.
Demographics and GABA data for treatment groups and time points.
| Demographics Mean (S.D.), n or % where relevant |
Baseline Whole Group |
Baseline Placebo | Baseline Kava | Tmt p-Value * |
Week 8 Whole Group |
Week 8 Placebo | Week 8 Kava |
|---|---|---|---|---|---|---|---|
| Participants (n) | 37 | 17 (9 male) | 20 (11 male) | 0.653 | 20 | 9 | 11 |
| Age | 36.16 (13.09) | 36.06 (11.31) | 36.25 (14.73) | 0.965 | - | - | - |
| Education (years) | 17.65 (3.91) | 18.59 (4.70) | 16.85 (2.98) | 0.181 | - | - | - |
| Psychiatric | |||||||
| Comorbid condition | 21 | 12 | 9 | 0.110 | - | - | - |
| Comorbid: SAD | 11 | 6 | 5 | 0.395 | - | - | - |
| Comorbid: PD | 9 | 7 | 2 | 0.034 * | - | - | - |
| Comorbid: AGO | 17 | 9 | 8 | 0.324 | - | - | - |
| Comorbid: PTSD | 1 | 1 | 0 | 0.460 | - | - | - |
| Comorbid: MDD | 20 | 9 | 11 | 0.581 | - | - | - |
| HAM-A a | 23.05 (3.60) | 23.29 (4.19) | 22.85 (3.10) | 0.714 | 15.55 (5.69) | 14.00 (6.20) | 16.82 (5.17) |
| MADRS b | 13.59 (2.99) | 14.00 (2.91) | 13.25 (3.09) | 0.456 | 10.38 (5.30) | 10.67 (4.82) | 10.17 (5.84) |
| Medical | |||||||
| Medications | 15 | 7 | 6 | 0.357 | - | - | - |
| Supplements | 9 | 2 | 7 | 0.103 | - | - | - |
| Substance | |||||||
| Caffeine (mg/daily) | 135.54 (127.64) | 156.47 (132.96) | 117.75 (123.51) | 0.365 | 100.55 (83.71) | 107.27 (68.93) | 94.50 (98.52) |
| Alcohol (SD/weekly) | 2.86 (3.08) | 1.88 (2.02) | 3.70 (3.60) | 0.073 | 4.10 (3.65) | 1.67 (1.50) | 6.09 (3.73) |
| Volumetric | |||||||
| dACC GM (%, mm3) | 60.29 (13.20) | 59.41 (12.22) | 61.05 (14.25) | 0.712 | 58.35 (12.33) | 53.11 (15.89) | 62.64 (6.45) |
| dACC WM (%, mm3) | 23.48 (11.46) | 24.58 (11.86) | 22.55 (11.34) | 0.597 | 23.40 (10.78) | 27.67 (13.90) | 19.91 (6.02) |
| dACC CSF (%, mm3) | 15.57 (5.04) | 14.53 (3.93) | 16.47 (5.77) | 0.249 | 18.01 (6.18) | 19.44 (4.56) | 16.84 (7.26) |
| GABA toolkit | |||||||
| LCModel GABA/GM | 3.67 (0.88) | 3.66 (1.01) | 3.69 (0.77) | 0.932 | 3.59 (0.74) | 4.07 (0.75) | 3.23 (0.53) |
| LCModel SD (%) | 9.39 (2.30) | 9.47 (1.58) | 9.31 (2.83) | 0.843 | 9.50 (2.68) | 8.89 (0.78) | 10.00 (3.55) |
| LCModel SNR | 9.00 (2.58) | 9.70 (2.26) | 8.37 (2.75) | 0.123 | 9.05 (2.42) | 9.44 (2.13) | 8.73 (2.69) |
| LCModel FWHM | 0.08 (0.04) | 0.06 (0.02) | 0.09 (0.05) | 0.025 * | 0.07 (0.03) | 0.06 (0.02) | 0.08 (0.04) |
* Significance values derived from independent sample t-tests or Chi Square tests where appropriate and significant, where p < 0.05; a Hamilton Anxiety Rating Scale; b Montgomery–Asberg Scale of Depression; AGO—Agoraphobia; MDD—Major depressive disorder; PD—panic disorder; PTSD—Post-traumatic stress disorder; SAD—social anxiety disorder; SD—standard drink/10 g of alcohol; CSF—cerebrospinal fluid; df—degrees of freedom; dACC—dorsal anterior cingulate cortex; GM—grey matter; Fit Err—Fit error %; FWHM—full width at half-maximum; GABA—gamma amino-butyric acid; ROI—Region of interest, SNR—signal–noise ratio; SD—standard deviation; Tmt—treatment (group difference); WM—White Matter.
4.2. Adverse Events
Adverse events reported during the study enrolment were not significantly different between participants in the kava and placebo groups (p = 0.508). The active treatment P. methysticum extract was well tolerated, with one participant reporting an adverse event of dizziness and a headache of mild severity with a probable association to kava. There were no serious adverse events reported in this study.
4.3. Withdrawals
The attrition of the sample size following the baseline visit was 46% (n = 17) and was not significantly different between the two groups (p = 0.482) for the following reasons and frequencies: non-compliance with study protocol (n = 6), lost to follow-up (n = 3), personal reasons/unspecified (n = 5), psychiatric status change (depression symptoms worsening, n = 2), medication status change (antidepressant course, n = 2), and pregnancy (n = 1).
4.4. Structural Data and Metabolite Quantification
The volumetric analysis showed no significant treatment group differences. The only quality parameter to display significant group differences was FWHM, t(37)2.29, p = 0.025, which was higher in the kava group (m 0.09, SD 0.05) than placebo (m 0.06, 0.02), meaning a better quality signal for the placebo group.
4.4.1. GABA Concentration Levels and HAMA at Baseline
The t-test for the treatment group difference on anxiety levels via the HAMA at baseline was not significant (p = 0.932). Partial correlation revealed a significant moderate positive relationship between HAMA scores and GABA concentration level, r(24) = 0.40, p = 0.05.
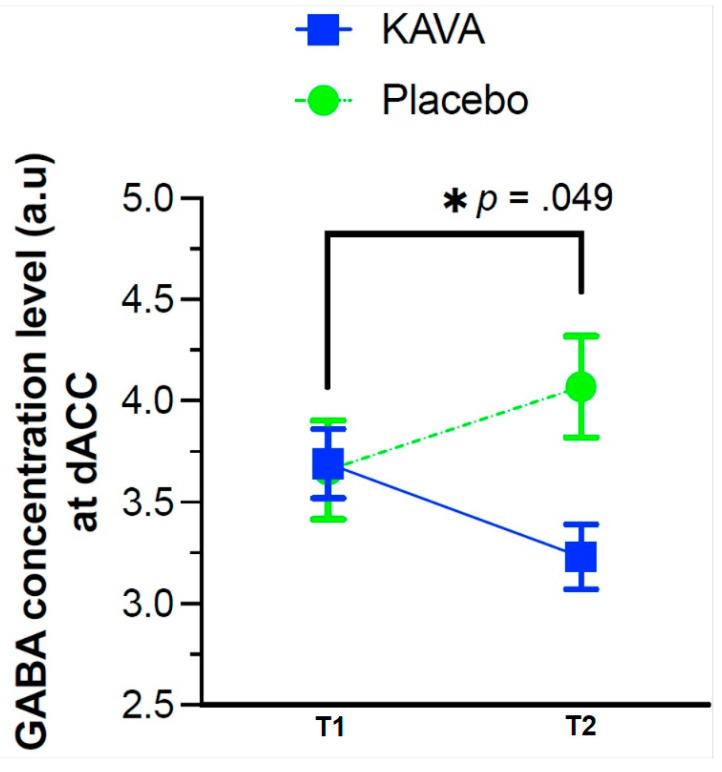
4.4.2. GABA Concentration Level Changes as a Function of the Eight-Week Kava Treatment
The partial volume-corrected GABA concentration in the grey matter model showed a significant treatment by time interaction, F(1, 21) = 4.36, p = 0.049. The model is shown in Table 2. Pairwise comparisons at the second time point indicated that the kava group was 1.06 units lower than the placebo group, and this was statistically significant (p = 0.008), 95% CI [−1.83, −0.28]. Refer to Figure 4.
Table 2.
Corrected GABA concentration changes, baseline to eight weeks.
| GABA Model | B/Estimate | 95% CI | t | df | p-Value |
|---|---|---|---|---|---|
| Corrected GABA concentration | |||||
| Time | 0.48 | −0.09, 1.06 | 1.74 | 21 | 0.097 a |
| Treatment | 1.06 | 0.28, 1.83 | 2.75 | 46 | 0 0.008 * |
| Sex | −0.28 | −0.78, 0.23 | −1.14 | 21 | 0 0.268 |
| Age | 0.01 | 0.00, 0.03 | 1.58 | 19 | 0.129 |
| Comorbid | 0.13 | −0.39, 0.65 | 0.53 | 24 | 0.603 |
| Baseline alcohol | 0.05 | −0.04, 0.03 | 1.58 | 21 | 0.129 |
| Time*Treatment | −0.87 | −1.74, 0.00 | −2.09 | 21 | 0 0.049 * |
* Significant at p < 0.05; a Marginally significant at p = 0.05–0.10; B/coefficient unit decimal places are variable due to LCModel level ranges; df—degrees of freedom.
Figure 4.
LCModel GABA means per group, baseline (T1) to eight weeks (T2).
5. Discussion
The purpose of the study was to investigate GABA concentration in the dorsal ACC in adults with diagnosed GAD and to assess whether these levels were modified by Kava. A significant difference in GABA concentration was observed in the Kava group at eight weeks compared with the placebo group, showing a reduction in GABA concentration levels in the ROI.
The study operated as a ‘proof of concept’ investigation, both in establishing the measurement of GABA in GAD and in evidencing neural mechanisms amenable to Kava. It addressed these aims through assessing GAD symptoms and biological outcomes before examining the role of Kava on both GABA levels and anxiety symptoms.
This study found that baseline anxiety levels were positively associated with GABA levels in the dACC but that a daily dose of 240 mg P. methysticum extract for eight weeks was not successful in reducing anxiety symptomatology at the eight-week time point. The overarching clinical trial for which this study was conducted similarly found no anxiety improvements in the Kava group over the 16-week treatment period [88]. These findings contribute evidence for a lack of efficacy of the particular Kava extract in GAD, which is in contrast to earlier studies, reviews, and meta-analyses suggesting otherwise [22,108,109]. A caveat may be the small–moderate effect sizes in intervention efficacy studies [10], where many findings were also equivocal, supporting the observation in the literature that GAD is a clinically challenging disorder to treat.
Despite these findings, results suggest that Kava modifies brain GABA levels, as GABA level reductions were observed in the Kava group in the dACC region compared with the placebo group. This reduction could represent a ‘normalisation’ in GABA levels, which is reflected in the handful of studies in the area that show that raised GABA is linked to anxiety levels in healthy samples, as well as elevations in PTSD compared with healthy controls [41,42]. Overall, the evidence is not sufficient to conclude trends in the dorsal ACC or within GAD groups.
Given the bioactive constituent profile of the extract used in this study and the GABAergic mechanisms exerted by kavain, dihydrokavain, and methysticin in particular, it is feasible that the observed effects have occurred via enhancement to particular GABA-A receptor subtypes in the ROI through direct ligand-binding enhancement or indirectly via reductions to thromboxane A (2), which antagonises GABA-A receptor functions. It is also likely that modulations have occurred elsewhere in the shunt, such as the excitatory glutaminergic corollary through calcium ion channel blockades via the MAO-B receptor substrate, and there is increasing evidence of glutaminergic modulation in preclinical research [110]. The precise mechanisms, and the relationship to GABA levels, are yet to be understood through pre-clinical studies, but modulation within the shunt could improve the physiology of the GABA substrate, shown through reduction to GABA levels in the ROI.
5.1. Limitations in This Current Study
Importantly, a sample size attrition of 46% from baseline to the second time point (n = 8 kava; n = 9 placebo), resulting in the reduced power of this study overall and the reduced accuracy of predictor effects, will impact the interpretation of the results. A borderline p-value for the interaction terms in the model may reflect this attrition. The reporting of confidence intervals, illustrating appropriate variance ranges, may have added some support to a significant result. Although the use of linear mixed modelling is partly protective against such impacts, the results need to be considered in this context.
Secondly, GABA concentration levels in the brain derived from spectral data requires high amounts of data modelling to expose GABA peaks, and there is debate on the optimal methods for sequencing, spectral analysis, quality parameters, or data modelling of ‘contaminants’ such as macromolecules. All magnify the risk of measurement errors, among other methodological issues [111,112,113]. However, an advantage was the MEGA-PRESS protocol, which is able to derive metabolite data separate from macromolecules, and the use of GANNET in the processing pipeline. Furthermore, LCModel’s toolbox-specific quality parameters could identify technical factors affecting the analysis of GABA levels. Despite removing scans of spurious quality, group differences were still observed for these variables in this current study. FWHM, as a measure of linewidth in the spectrum quantifying the signal decay rate in the time-domain as a result of shimming, was significantly different between the treatment groups. It is possible that the methods applied within the toolbox have influenced the observed GABA concentration, thereby requiring caution in interpreting the results and subsequent conclusions. However, the baseline GABA concentration was not related to FWHM, so the different quality parameters had limited impact on the reported findings.
Thirdly, scan novelty may also be an influencing factor in participants with clinical anxiety. This current study did not collect data as to whether participants were familiar with MRI scan environments. A ‘sham’ scan session for each participant might have reduced this confound.
For these reasons, this study’s novel findings should be considered pilot data at best, offering a novel insight into the pattern of GABA levels in a GAD as a product of Kava, as well as an example of greatly needed biomarker research for the benefit of clinical anxiety.
5.2. Future Research Directions
The findings in this study between Kava treatment, anxiety symptoms, and GABA levels warrant further examination. Given the role the dACC may play in hallmark anxiety cognition symptoms in GAD, as well as evidence of kava efficacy in the literature, it would be of value to examine whether kava-based modulations were observed on selected HAM-A items (such as cognitive over somatic symptoms), which might clarify the pattern observed in the ROI. Similarly, a division of higher anxiety and low anxiety may reveal different Kava responses. Secondly, beyond the modulation of GABA by Kava, given the likely mechanisms in the GABA metabolic shunt of Kava in preclinical studies on NMDA receptors, an examination of glutamate levels may also reveal Kava mechanisms beyond GABA, supporting recent preclinical research and offering potential avenues for future therapeutic approaches.
This current study was valuable for understanding the mechanisms of Kava in GAD, and future research should extend Kava dosing in other anxiety cohorts and healthy controls and assess patterns of GABA levels in comparison with GAD. This could include major depressive disorder or state-based anxiety disorders, such as phobias and panic disorder, to delineate differences in ROI GABA levels and determine the relationship to anxiety symptoms.
There remains a shortfall in brain biomarker research in anxiety disorders, especially GAD. Emerging approaches now exist to guide the identified need, such as the Research Domain Criteria (RDoC) framework [114,115], which was founded on the premise that it is insufficient to assess symptoms alone to treat (or diagnose) GAD, yet there is insufficient data serving as biomarker evidence. This current study serves to address this shortfall. Biomarker treatment approaches assert that biological patterns may not fit with current diagnostic categories, signalling a vital need for research that clarifies neurobiological marker roles in symptom maintenance and response patterns with treatment [115,116,117,118]. These markers also have potential to identify disorders before the onset of anxiety symptoms and to identify variants or clinically meaningful subsets [18,119,120]. What is measured as biomarkers in neuroimaging is arguably closer to the exact substrates that underpin disorders, and we are therefore able to more precisely gauge the relationship between biomarkers and clinical endpoints for the individual [18,25,115,121].
This current study showed that GABA metabolic data were successful in producing differences that could be utilised as GAD biomarkers, with some considerations. The assessment of the neurobiological effects of Kava is novel in GAD samples and shows how our methodology could be applied to other anxiolytic phytomedicines. Data from MRS GABA can contribute to an integrative efficacy model of imaging modalities and psychological measures for future efficacy studies of biological substrates. More work is needed in the establishing of biomarkers for clinical benefit, but there is a strong translational rationale for the investigation of novel anxiolytics like Kava as GAD treatment, as demonstrated in this current study.
6. Conclusions
In order to elucidate the role of GABA or its metabolic components either as a predisposing, preventative, or therapeutic utility, it is important to quantify GABAergic processes. This research represents the first study to assess brain GABA concentration levels in adults with GAD, as well as the first to assess modulations following a treatment intervention using Kava. This study demonstrated that GABA levels are modulated via Kava treatment, and regional brain GABA concentration levels could be linked to anxiety symptoms in GAD. The findings also indicate that GABA levels can change without concomitant changes in anxiety symptoms, suggesting that symptom profiles in GAD is complex and multi-factorial. Further studies quantifying brain anxiety markers over time, controlling for other associated variables, and the use of a benzodiazepine comparator could clarify the role of GABA as a marker of anxiety in brain regions associated with cognitive anxiety symptoms. It is also vital for future studies to determine levels of GABA in brain regions using wider healthy cohorts.
Appendix A
| Enrolment Criteria |
| Generalised Anxiety Disorder Group |
| Inclusion Criteria |
|
|
| Exclusion Criteria |
|
| Imaging eligibility criteria—exclusions |
|
Author Contributions
K.S.: Conceptualization, Investigation, Methodology, Data curation, Formal Analysis, Writing—original draft, Writing—review and editing. J.S.: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing—review and editing. M.H.: Investigation, Methodology, Project administration, Resources, Supervisory, Writing—review and editing. C.A.B.: Investigation, Methodology, Project administration, Writing—review and editing. S.R.: Funding acquisition, Investigation, Methodology, Project administration, Resources, Writing—review and editing. A.S.: Investigation, Methodology, Project administration, Resources, Writing—review and editing. C.S.: (Con Stough) Investigation, Methodology, Project administration, Resources, Supervisory, Writing—review and editing. C.S.: (Chao Suo) Investigation, Formal Analysis, Methodology, Project administration, Resources, Supervisory, Writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Swinburne University Human Ethics Committee (SUHREC; No. HREC2014/204), 8 August 2014.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data were collected exclusively for the purpose of fulfilling the NHMRC grant research within a clinical group. Additionally, provision to third parties may not comply with Australian clinical trial grant mandates. To this end, the data from this study are not publicly available.
Conflicts of Interest
J. Sarris has received either presentation honoraria, travel support, clinical trial grants, book royalties, or independent consultancy payments from the following: Integria Healthcare and MediHerb (a kava product manufacturer), Pfizer, Scius Health, Key Pharmaceuticals, Taki Mai, Fiji Kava, Noetic Foundry, FIT-BioCeuticals, Blackmores, Soho-Flordis, Healthworld, HealthEd, HealthMasters, Kantar Consulting, Angelini Pharmaceuticals, Grunbiotics, Polistudium, Global Pharma Group, Australian Natural Therapeutics Group, Research Reviews, Elsevier, Chaminade University, International Society for Affective Disorders, Complementary Medicines Australia, SPRIM, Terry White Chemists, ANS, Society for Medicinal Plant and Natural Product Research, Sanofi-Aventis, Omega-3 Centre, the National Health and Medical Research Council, CR Roper Fellowship, and the Medical Research Futures Fund. A Scholey has received either presentation honoraria, travel support, clinical trial grants, book royalties, or independent consultancy payments from the following: Abbott Nutrition, Ārepa Nootropics, Arla Foods, Australian Research Council, Australian Wine Research Institute, Barilla, Bayer, Biotechnology and Biological Sciences Research Council, Blackmores, Coca Cola, Cognis, Cyvex, Dairy Health Innovation Consortium, Danone, Delica Therapeutics, DuPont, European Commission Framework 5 Research and Innovation initiative, Fonterra, Frutarom, GlaxoSmithKline, Ginsana, High Value Nutrition Fund, Kemin Foods, Martek, Masterfoods, National Health and Medical Research Council, Naturex, Nestlé, Neurobrands, Novartis, Nutricia-Danone, Pepsico, Pfizer, Pharmavite, Pharmaton, Red Bull, REVIV, Sanofi, Sen- Jam Pharmaceuticals, Verdure Sciences, Unilever, and the Wrigley Science Institute. He is Chief Scientific Officer for Ārepa Nootropics and is on the Scientific Advisory Board of Sen-Jam Pharmaceutical.
Funding Statement
Data were derived from the larger KGAD clinical trial, funded by an Australian National Health and Medical Research Council (NHMRC) grant (No. APP1063383) and co-funded by Integria Healthcare. The Kava used as treatment in this study was sourced specifically for the trial and therefore represents a different product than the one currently marketed by Integria Healthcare. We acknowledge the facilities and technical assistance of the National Imaging Facility, a National Collaborative Research Infrastructure Strategy (NCRIS) capability, at the Swinburne Neuroimaging Facility, Swinburne University of Technology. KS was the recipient of an Australian Government Research Training Program (RTP) Stipend Scholarship. The aforementioned grant and sponsor funding sources also provided support for research included in this manuscript to obtain a PhD (KS). JS was supported by NHMRC Clinical Research Fellowship (APP1125000). SLR holds a Senior National Health and Medical Research Council (NHMRC) Fellowship (GNT1154651).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Merikangas K.R., Zhang H., Avenevoli S., Acharyya S., Neuenschwander M., Angst J. Longitudinal Trajectories of Depression and Anxiety in a Prospective Community Study: The Zurich Cohort Study. Arch. Gen. Psychiatry. 2003;60:993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- 2.Wittchen H.U., Zhao S.Y., Kessler R.C., Eaton W.W. DSM-III-R Generalized Anxiety Disorder in the National Comorbidity Survey. Arch. Gen. Psychiatry. 1994;51:355–364. doi: 10.1001/archpsyc.1994.03950050015002. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Press; Washington, DC, USA: 2022. Text Revision. [Google Scholar]
- 4.Barlow D.H., Wincze J. DSM-IV and beyond: What is generalized anxiety disorder? Acta Psychiatr. Scand. 1998;98:23–29. doi: 10.1111/j.1600-0447.1998.tb05962.x. [DOI] [PubMed] [Google Scholar]
- 5.Freedman R., Lewis D.A., Michels R., Pine D.S., Schultz S.K., Tamminga C.A., Yager J. The initial field trials of DSM-5: New blooms and old thorns. Am. J. Psychiatry. 2013;170:1–5. doi: 10.1176/appi.ajp.2012.12091189. [DOI] [PubMed] [Google Scholar]
- 6.Starcevic V. Generalized anxiety disorder: Psychopharmacotherapy update on a common and commonly overlooked condition. Australas Psychiatry. 2015;23:338–342. doi: 10.1177/1039856215587233. [DOI] [PubMed] [Google Scholar]
- 7.Stein M.B., Sareen J. Clinical Practice. Generalized Anxiety Disorder. New Engl. J. Med. 2015;373:2059–2068. doi: 10.1056/NEJMcp1502514. [DOI] [PubMed] [Google Scholar]
- 8.Cuijpers P., Sijbrandij M., Koole S., Huibers M., Berking M., Andersson G. Psychological treatment of generalized anxiety disorder: A meta-analysis. Clin. Psychol. Rev. 2014;34:130–140. doi: 10.1016/j.cpr.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 9.Baldwin D.S., Waldman S., Allgulander C. Evidence-based pharmacological treatment of generalized anxiety disorder. Int. J. Neuropsychopharmacol. 2011;14:697–710. doi: 10.1017/S1461145710001434. [DOI] [PubMed] [Google Scholar]
- 10.Slee A., Nazareth I., Bondaronek P., Liu Y., Cheng Z., Freemantle N. Pharmacological treatments for generalised anxiety disorder: A systematic review and network meta-analysis. Lancet. 2019;393:768–777. doi: 10.1016/S0140-6736(18)31793-8. [DOI] [PubMed] [Google Scholar]
- 11.Gale C.K., Millichamp J. Generalised anxiety disorder. BMJ Clin. Evid. 2011;2011:1002. [PMC free article] [PubMed] [Google Scholar]
- 12.Gale C.K., Millichamp J. Generalised anxiety disorder in children and adolescents. BMJ Clin. Evid. 2016;2016:1002. [PMC free article] [PubMed] [Google Scholar]
- 13.Gunter R.W., Whittal M.L. Dissemination of cognitive-behavioral treatments for anxiety disorders: Overcoming barriers and improving patient access. Clin. Psychol. Rev. 2010;30:194–202. doi: 10.1016/j.cpr.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Hoffman E.J., Mathew S.J. Anxiety disorders: A comprehensive review of pharmacotherapies. Mt. Sinai J. Med. 2008;75:248–262. doi: 10.1002/msj.20041. [DOI] [PubMed] [Google Scholar]
- 15.Nasir M., Trujillo D., Levine J., Dwyer J.B., Rupp Z.W., Bloch M.H. Glutamate Systems in DSM-5 Anxiety Disorders: Their Role and a Review of Glutamate and GABA Psychopharmacology. Front. Psychiatry. 2020;11:548505. doi: 10.3389/fpsyt.2020.548505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weisberg R.B. Overview of generalized anxiety disorder: Epidemiology, presentation, and course. J. Clin. Psychiatry. 2009;70((Suppl. 2)):4–9. doi: 10.4088/JCP.s.7002.01. [DOI] [PubMed] [Google Scholar]
- 17.Farach F.J., Pruitt L.D., Jun J.J., Jerud A.B., Zoellner L.A., Roy-Byrne P.P. Pharmacological treatment of anxiety disorders: Current treatments and future directions. J. Anxiety Disord. 2012;26:833–843. doi: 10.1016/j.janxdis.2012.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kapur S., Phillips A.G., Insel T.R. Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it? Mol. Psychiatry. 2012;17:1174–1179. doi: 10.1038/mp.2012.105. [DOI] [PubMed] [Google Scholar]
- 19.Miller G. Is pharma running out of brainy ideas? Science. 2010;329:502–504. doi: 10.1126/science.329.5991.502. [DOI] [PubMed] [Google Scholar]
- 20.Murrough J.W., Yaqubi S., Sayed S., Charney D.S. Emerging drugs for the treatment of anxiety. Expert Opin. Emerg. Drugs. 2015;20:393–406. doi: 10.1517/14728214.2015.1049996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sartori S.B., Singewald N. Novel pharmacological targets in drug development for the treatment of anxiety and anxiety-related disorders. Pharmacol. Ther. 2019;204:107402. doi: 10.1016/j.pharmthera.2019.107402. [DOI] [PubMed] [Google Scholar]
- 22.Sarris J., McIntyre E., Camfield D.A. Plant-based medicines for anxiety disorders, part 1: A review of preclinical studies. CNS Drugs. 2013;27:207–219. doi: 10.1007/s40263-013-0044-3. [DOI] [PubMed] [Google Scholar]
- 23.Savage K., Firth J., Stough C.K., Sarris J. GABA-modulating phytomedicines for anxiety: A systematic review of preclinical and clinical evidence. Phytother. Res. 2017;32:3–18. doi: 10.1002/ptr.5940. [DOI] [PubMed] [Google Scholar]
- 24.Bandelow B., Michaelis S., Wedekind D. Treatment of anxiety disorders. Dialogues Clin. Neurosci. 2017;19:93–107. doi: 10.31887/DCNS.2017.19.2/bbandelow. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bandelow B., Baldwin D., Abelli M., Bolea-Alamanac B., Bourin M., Chamberlain S.R., Riederer P. Biological markers for anxiety disorders, OCD and PTSD: A consensus statement. Part II: Neurochemistry, neurophysiology and neurocognition. World J. Biol. Psychiatry. 2017;18:162–214. doi: 10.1080/15622975.2016.1190867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ferreira-Garcia R., Mochcovitch M., do Cabo M.C., Nardi A.E., Freire R.C. Predictors of pharmacotherapy response in generalized anxiety disorder: A systematic review. Harv. Rev. Psychiatry. 2017;25:65–79. doi: 10.1097/HRP.0000000000000127. [DOI] [PubMed] [Google Scholar]
- 27.Maron E., Nutt D. Biological Markers of Generalized Anxiety Disorder. Focus. 2018;16:210–218. doi: 10.1176/appi.focus.16205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Strawn J.R., Levine A. Treatment response biomarkers in anxiety disorders: From neuroimaging to neuronally-derived extracellular vesicles and beyond. Biomark. Neuropsychiatry. 2020;3:100024. doi: 10.1016/j.bionps.2020.100024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hayashi T., Nagai K. Action of ω-amino acids on the motor cortex of higher animals, especially γ-amino-β-oxybutyric acid as the real inhibitory principle in brain; Proceedings of the Twentieth International Physiological Congress; Brussels, Belgium. March 1955–January 1956. [Google Scholar]
- 30.Killam K., Bain J. Convulsant hydrazides I: In vitro and in vivo inhibition of vitamin B6 enzymes by convulsant hydrazides. J. Pharmacol. Exp. Ther. 1957;119:255–262. [PubMed] [Google Scholar]
- 31.Etkin A., Wager T.D. Functional neuroimaging of anxiety: A meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am. J. Psychiatry. 2007;164:1476–1488. doi: 10.1176/appi.ajp.2007.07030504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nuss P. Anxiety disorders and GABA neurotransmission: A disturbance of modulation. Neuropsychiatr. Dis. Treat. 2015;11:165–175. doi: 10.2147/NDT.S58841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Northoff G., Walter M., Schulte R.F., Beck J., Dydak U., Henning A., Boesiger P. GABA concentrations in the human anterior cingulate cortex predict negative BOLD responses in fMRI. Nat. Neurosci. 2007;10:1515–1517. doi: 10.1038/nn2001. [DOI] [PubMed] [Google Scholar]
- 34.Puts N.A.J., Edden R.A.E. In vivo magnetic resonance spectroscopy of GABA: A methodological review. Prog. Nucl. Magn. Reson. Spectrosc. 2012;60:29–41. doi: 10.1016/j.pnmrs.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rae C. A guide to the metabolic pathways and function of metabolites observed in human brain 1H magnetic resonance spectra. Neurochem. Res. 2014;39:1–36. doi: 10.1007/s11064-013-1199-5. [DOI] [PubMed] [Google Scholar]
- 36.Tasan R.O., Bukovac A., Peterschmitt Y.N., Sartori S.B., Landgraf R., Singewald N., Sperk G. Altered GABA transmission in a mouse model of increased trait anxiety. Neuroscience. 2011;183:71–80. doi: 10.1016/j.neuroscience.2011.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nemeroff C.B. The role of GABA in the pathophysiology and treatment of anxiety disorders. Psychopharmacol. Bull. 2003;37:133–146. [PubMed] [Google Scholar]
- 38.Nutt D.J., Malizia A.L. New insights into the role of the GABA(A)-benzodiazepine receptor in psychiatric disorder. Br. J. Psychiatry. 2001;179:390–396. doi: 10.1192/bjp.179.5.390. [DOI] [PubMed] [Google Scholar]
- 39.Schur R.R., Draisma L.W., Wijnen J.P., Boks M.P., Koevoets M.G., Joels M., Vinkers C.H. Brain GABA levels across psychiatric disorders: A systematic literature review and meta-analysis of (1) H-MRS studies. Hum. Brain Mapp. 2016;37:3337–3352. doi: 10.1002/hbm.23244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Delli Pizzi S., Padulo C., Brancucci A., Bubbico G., Edden R.A., Ferretti A., Bonanni L. GABA content within the ventromedial prefrontal cortex is related to trait anxiety. Soc. Cogn. Affect. Neurosci. 2015;11:758–766. doi: 10.1093/scan/nsv155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Michels L., Schulte-Vels T., Schick M., O’Gorman R.L., Zeffiro T., Hasler G., Mueller-Pfeiffer C. Prefrontal GABA and glutathione imbalance in posttraumatic stress disorder: Preliminary findings. Psychiatry Res. Neuroimaging. 2014;224:288–295. doi: 10.1016/j.pscychresns.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 42.Pennington D.L., Abé C., Batki S.L., Meyerhoff D.J. A preliminary examination of cortical neurotransmitter levels associated with heavy drinking in posttraumatic stress disorder. Psychiatry Res. 2014;224:281–287. doi: 10.1016/j.pscychresns.2014.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rosso I.M., Weiner M.R., Crowley D.J., Silveri M.M., Rauch S.L., Jensen J.E. Insula and anterior cingulate GABA levels in posttraumatic stress disorder: Preliminary findings using magnetic resonance spectroscopy. Depress. Anxiety. 2014;31:115–123. doi: 10.1002/da.22155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goddard A.W., Mason G.F., Almai A., Rothman D.L., Behar K.L., Petroff O.A., Krystal J.H. Reductions in occipital cortex GABA levels in panic disorder detected with 1h-magnetic resonance spectroscopy. Arch. Gen. Psychiatry. 2001;58:556–561. doi: 10.1001/archpsyc.58.6.556. [DOI] [PubMed] [Google Scholar]
- 45.Ham B.-J., Sung Y., Kim N., Kim S.J., Kim J.E., Kim D.J., Lyoo I.K. Decreased GABA levels in anterior cingulate and basal ganglia in medicated subjects with panic disorder: A proton magnetic resonance spectroscopy (1H-MRS) study. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2007;31:403–411. doi: 10.1016/j.pnpbp.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 46.Hasler G., van der Veen J.W., Geraci M., Shen J., Pine D., Drevets W.C. Prefrontal cortical gamma-aminobutyric Acid levels in panic disorder determined by proton magnetic resonance spectroscopy. Biol. Psychiatry. 2009;65:273–275. doi: 10.1016/j.biopsych.2008.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pollack M.H., Jensen J.E., Simon N.M., Kaufman R.E., Renshaw P.F. High-field MRS study of GABA, glutamate and glutamine in social anxiety disorder: Response to treatment with levetiracetam. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2008;32:739–743. doi: 10.1016/j.pnpbp.2007.11.023. [DOI] [PubMed] [Google Scholar]
- 48.Abdallah C.G., Coplan J.D., Jackowski A., Sato J.R., Mao X., Shungu D.C., Mathew S.J. A pilot study of hippocampal volume and N-acetylaspartate (NAA) as response biomarkers in riluzole-treated patients with GAD. Eur. Neuropsychopharmacol. 2013;23:276–284. doi: 10.1016/j.euroneuro.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mathew S.J., Price R.B., Mao X., Smith E.L., Coplan J.D., Charney D.S., Shungu D.C. Hippocampal N-acetylaspartate concentration and response to riluzole in generalized anxiety disorder. Biol. Psychiatry. 2008;63:891–898. doi: 10.1016/j.biopsych.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mathew S., Price R., Shungu D., Mao X., Smith E., Amiel J., Coplan J. A pilot study of the effects of chronic paroxetine administration on hippocampal N-acetylaspartate in generalized anxiety disorder. J. Psychopharmacol. 2010;24:1175–1181. doi: 10.1177/0269881108101796. [DOI] [PubMed] [Google Scholar]
- 51.Bush G., Luu P., Posner M.I. Cognitive and emotional influences in anterior cingulate cortex. Trends Cogn. Sci. 2000;4:215–222. doi: 10.1016/S1364-6613(00)01483-2. [DOI] [PubMed] [Google Scholar]
- 52.Critchley H.D., Mathias C.J., Josephs O., O’Doherty J., Zanini S., Dewar B.K., Dolan R.J. Human cingulate cortex and autonomic control: Converging neuroimaging and clinical evidence. Brain. 2003;126:2139–2152. doi: 10.1093/brain/awg216. [DOI] [PubMed] [Google Scholar]
- 53.Etkin A., Egner T., Kalisch R. Emotional processing in anterior cingulate and medial prefrontal cortex. Trends Cogn. Sci. 2011;15:85–93. doi: 10.1016/j.tics.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Luu P., Pederson S.M. Cognitive Neuroscience of Attention. Guilford Publication, Inc.; New York, NY, USA: 2004. The anterior cingulate cortex: Regulating actions in context; pp. 232–242. [Google Scholar]
- 55.Vogt B.A., Finch D.M., Olson C.R. Functional heterogeneity in cingulate cortex: The anterior executive and posterior evaluative regions. Cereb. Cortex. 1992;2:435–443. doi: 10.1093/cercor/2.6.435-a. [DOI] [PubMed] [Google Scholar]
- 56.Buckner R.L., Andrews-Hanna J.R., Schacter D.L. The brain’s default network: Anatomy, function, and relevance to disease. Ann. N. Y. Acad. Sci. 2008;1124:1–38. doi: 10.1196/annals.1440.011. [DOI] [PubMed] [Google Scholar]
- 57.Cohen J.D., Botvinick M., Carter C.S. Anterior cingulate and prefrontal cortex: Who’s in control? Nat. Neurosci. 2000;3:421. doi: 10.1038/74783. [DOI] [PubMed] [Google Scholar]
- 58.Pizzagalli D.A., Peccoralo L.A., Davidson R.J., Cohen J.D. Resting anterior cingulate activity and abnormal responses to errors in subjects with elevated depressive symptoms: A 128-channel EEG study. Hum. Brain Mapp. 2006;27:185–201. doi: 10.1002/hbm.20172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Raichle M.E., MacLeod A.M., Snyder A.Z., Powers W.J., Gusnard D.A., Shulman G.L. A default mode of brain function. Proc. Natl. Acad. Sci. 2001;98:676–682. doi: 10.1073/pnas.98.2.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vogt B.A. Pain and emotion interactions in subregions of the cingulate gyrus. Nat. Rev. Neurosci. 2005;6:533–544. doi: 10.1038/nrn1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Levar N., van Leeuwen J., Puts N.A., Denys D., Van Wingen G.A. GABA concentrations in the anterior cingulate cortex are associated with fear network function and fear recovery in humans. Front. Hum. Neurosci. 2017;11:202. doi: 10.3389/fnhum.2017.00202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Makkar S.R., Zhang S.Q., Cranney J. Behavioral and neural analysis of GABA in the acquisition, consolidation, reconsolidation, and extinction of fear memory. Neuropsychopharmacology. 2010;35:1625–1652. doi: 10.1038/npp.2010.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Phelps E.A., Delgado M.R., Nearing K.I., LeDoux J.E. Extinction learning in humans: Role of the amygdala and vmPFC. Neuron. 2004;43:897–905. doi: 10.1016/j.neuron.2004.08.042. [DOI] [PubMed] [Google Scholar]
- 64.Shin L.M., Liberzon I. The Neurocircuitry of Fear, Stress, and Anxiety Disorders. Neuropsychopharmacology. 2010;35:169–191. doi: 10.1038/npp.2009.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.LaPorte E., Sarris J., Stough C., Scholey A. Neurocognitive effects of kava (Piper methysticum): A systematic review. Hum. Psychopharmacol. 2011;26:102–111. doi: 10.1002/hup.1180. [DOI] [PubMed] [Google Scholar]
- 66.Pittler M.H., Ernst E. Kava extract for treating anxiety. Cochrane Database Syst. Rev. 2003:CD003383. doi: 10.1002/14651858.CD003383. [DOI] [PubMed] [Google Scholar]
- 67.Singh Y.N., Singh N.N. Therapeutic potential of kava in the treatment of anxiety disorders. CNS Drugs. 2002;16:731–743. doi: 10.2165/00023210-200216110-00002. [DOI] [PubMed] [Google Scholar]
- 68.Stevinson C., Huntley A., Ernst E. A systematic review of the safety of kava extract in the treatment of anxiety. Drug Saf. 2002;25:251–261. doi: 10.2165/00002018-200225040-00003. [DOI] [PubMed] [Google Scholar]
- 69.Bensoussan A., Myers S.P., Wu S.M., O’Connor K. Naturopathic and Western herbal medicine practice in Australia—A workforce survey. Complement. Ther. Med. 2004;12:17–27. doi: 10.1016/j.ctim.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 70.Lebot V., Merlin M., Lindstrom L. Kava: The Pacific Drug. Yale University Press; New Haven, CT, USA: 1992. [Google Scholar]
- 71.Pittler M.H., Ernst E. Efficacy of kava extract for treating anxiety: Systematic review and meta-analysis. J. Clin. Psychopharmacol. 2000;20:84–89. doi: 10.1097/00004714-200002000-00014. [DOI] [PubMed] [Google Scholar]
- 72.Singh Y. Kava: An overview. J. Ethnopharmacol. 1992;37:13–45. doi: 10.1016/0378-8741(92)90003-A. [DOI] [PubMed] [Google Scholar]
- 73.Tzeng Y.M., Lee M.J. Neuroprotective properties of kavalactones. Neural Regen. Res. 2015;10:875–877. doi: 10.4103/1673-5374.158335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bilia A.R., Bergonzi M.C., Lazari D., Vincieri F.F. Characterization of commercial kava-kava herbal drug and herbal drug preparations by means of nuclear magnetic resonance spectroscopy. J. Agric. Food Chem. 2002;50:5016–5025. doi: 10.1021/jf020049j. [DOI] [PubMed] [Google Scholar]
- 75.Chua H.C., Christensen E.T., Hoestgaard-Jensen K., Hartiadi L.Y., Ramzan I., Jensen A.A., Chebib M. Kavain, the Major Constituent of the Anxiolytic Kava Extract, Potentiates GABAA Receptors: Functional Characteristics and Molecular Mechanism. PLoS ONE. 2016;11:e0157700. doi: 10.1371/journal.pone.0157700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Duffield A., Jamieson D., Lidgard R., Duffield P., Bourne D. Identification of some human urinary metabolites of the intoxicating beverage kava. J. Chromatogr. A. 1989;475:273–281. doi: 10.1016/S0021-9673(01)89682-5. [DOI] [PubMed] [Google Scholar]
- 77.Meyer H.J. Ethnopharmacologic Search for Psychoactive Drugs. Raven Press; New York, NY, USA: 1979. Pharmacology of kava. [Google Scholar]
- 78.Boonen G., Haberlein H. Influence of genuine kavapyrone enantiomers on the GABA-A binding site. Planta Med. 1998;64:504–506. doi: 10.1055/s-2006-957502. [DOI] [PubMed] [Google Scholar]
- 79.Davies L.P., Drew C.A., Duffield P., Johnston G.A., Jamieson D.D. Kava pyrones and resin: Studies on GABAA, GABAB and benzodiazepine binding sites in rodent brain. Pharmacol. Toxicol. 1992;71:120–126. doi: 10.1111/j.1600-0773.1992.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 80.Yuan C.S., Dey L., Wang A., Mehendale S., Xie J.T., Aung H.H., Ang-Lee M.K. Kavalactones and dihydrokavain modulate GABAergic activity in a rat gastric-brainstem preparation. Planta Medica. 2002;68:1092–1096. doi: 10.1055/s-2002-36338. [DOI] [PubMed] [Google Scholar]
- 81.Boonen G., Ferger B., Kuschinsky K., Haberlein H. In Vivo effects of the kavapyrones (+)-dihydromethysticin (+/−)-kavain on dopamine, 3,4-dihydroxyphenylacetic acid, serotonin and 5-hydroxyindoleacetic acid levels in striatal and cortical brain regions. Planta Medica. 1998;64:507–510. doi: 10.1055/s-2006-957503. [DOI] [PubMed] [Google Scholar]
- 82.Gleitz J., Beile A., Peters T. (+/−)-Kavain inhibits veratridine-activated voltage dependent Na(+)-channels in synaptosomes prepared from rat cerebral cortex. Neuropharmacology. 1995;34:1133–1138. doi: 10.1016/0028-3908(95)00090-S. [DOI] [PubMed] [Google Scholar]
- 83.Jamieson D.D., Duffield P.H. Positive interaction of ethanol and kava resin in mice. Clin. Exp. Pharmacol. Physiol. 1990;17:509–514. doi: 10.1111/j.1440-1681.1990.tb01350.x. [DOI] [PubMed] [Google Scholar]
- 84.Lehmann E., Klieser E., Klimke A., Krach H., Spatz R. The efficacy of Cavain in patients suffering from anxiety. Pharmacopsychiatry. 1989;22:258–262. doi: 10.1055/s-2007-1014611. [DOI] [PubMed] [Google Scholar]
- 85.Sarris J., Kavanagh D.J., Adams J., Bone K., Byrne G. Kava Anxiety Depression Spectrum Study (KADSS): A mixed methods RCT using an aqueous extract of Piper methysticum. Complement. Ther. Med. 2009;17:176–178. doi: 10.1016/j.ctim.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 86.Saletu B., Grünberger J., Linzmayer L., Anderer P. EEG-Brain mapping, psychometric and psychophysiological studies on central effects of kavain—A kava plant derivative. Hum. Psychopharmacol.: Clin. Exp. 1989;4:169–190. doi: 10.1002/hup.470040304. [DOI] [Google Scholar]
- 87.Savage K.M., Stough C.K., Byrne G.J., Scholey A., Bousman C., Murphy J., Sarris J. Kava for the treatment of generalised anxiety disorder (K-GAD): Study protocol for a randomised controlled trial. Trials. 2015;16:493. doi: 10.1186/s13063-015-0986-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sarris J., Byrne G.J., Bousman C.A., Cribb L., Savage K.M., Holmes O., Stough C. Kava for generalised anxiety disorder: A 16-week double-blind, randomised, placebo-controlled study. Aust. New Zealand J. Psychiatry. 2020;54:288–297. doi: 10.1177/0004867419891246. [DOI] [PubMed] [Google Scholar]
- 89.Faul F., Erdfelder E., Lang A.G., Buchner A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods. 2007;39:175–191. doi: 10.3758/BF03193146. [DOI] [PubMed] [Google Scholar]
- 90.Sheehan D.V., Lecrubier Y., Sheehan K.H., Amorim P., Janavs J., Weiller E., Dunbar G.C. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 91.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Press; Washington, DC, USA: 2013. [Google Scholar]
- 92.Hamilton M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 93.Montgomery S.A., Åsberg M. A new depression scale designed to be sensitive to change. Br. J. Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 94.Williams J., Kobak K. Structured Interview Guide for the Montgomery Asberg Depression Rating Scale (SIG-MA) Biometrics Research Department; New York, NY, USA: 1996. [Google Scholar]
- 95.Noyes R., Jr. Comorbidity in generalized anxiety disorder. Psychiatr. Clin. North Am. 2001;24:41–55. doi: 10.1016/S0193-953X(05)70205-7. [DOI] [PubMed] [Google Scholar]
- 96.Nutt D.J., Ballenger J.C., Sheehan D., Wittchen H.-U. Generalized anxiety disorder: Comorbidity, comparative biology and treatment. Int. J. Neuropsychopharmacol. 2002;5:315–325. doi: 10.1017/S1461145702003048. [DOI] [PubMed] [Google Scholar]
- 97.Shear M.K., Vander Bilt J., Rucci P., Endicott J., Lydiard B., Otto M.W., Frank D.M. Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH-A) Depress. Anxiety. 2001;13:166–178. doi: 10.1002/da.1033. [DOI] [PubMed] [Google Scholar]
- 98.Mescher M., Merkle H., Kirsch J., Garwood M., Gruetter R. Simultaneous in vivo spectral editing and water suppression. NMR Biomed. 1998;11:266–272. doi: 10.1002/(SICI)1099-1492(199810)11:6<266::AID-NBM530>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 99.Rorden C., Brett M. Stereotaxic display of brain lesions. Behav. Neurol. 2000;12:191–200. doi: 10.1155/2000/421719. [DOI] [PubMed] [Google Scholar]
- 100.Edden R.A., Puts N.A., Harris A.D., Barker P.B., Evans C.J. Gannet: A batch-processing tool for the quantitative analysis of gamma-aminobutyric acid-edited MR spectroscopy spectra. J. Magn. Reson. Imaging. 2014;40:1445–1452. doi: 10.1002/jmri.24478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Provencher S.W. Estimation of metabolite concentrations from localized in vivo proton NMR spectra. Magn. Reson. Med. 1993;30:672–679. doi: 10.1002/mrm.1910300604. [DOI] [PubMed] [Google Scholar]
- 102.Provencher S.W. Automatic quantitation of localized in vivo 1H spectra with LCModel. NMR Biomed. 2001;14:260–264. doi: 10.1002/nbm.698. [DOI] [PubMed] [Google Scholar]
- 103.Ganji S.K., An Z., Banerjee A., Madan A., Hulsey K.M., Choi C. Measurement of regional variation of GABA in the human brain by optimized point-resolved spectroscopy at 7 T in vivo. NMR Biomed. 2014;27:1167–1175. doi: 10.1002/nbm.3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Harris A.D., Puts N.A., Edden R.A. Tissue correction for GABA-edited MRS: Considerations of voxel composition, tissue segmentation, and tissue relaxations. J. Magn. Reson. Imaging. 2015;42:1431–1440. doi: 10.1002/jmri.24903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kreis R., Ernst T., Ross B.D. Development of the human brain: In vivo quantification of metabolite and water content with proton magnetic resonance spectroscopy. Magn. Reson. Med. 1993;30:424–437. doi: 10.1002/mrm.1910300405. [DOI] [PubMed] [Google Scholar]
- 106.Mikkelsen M., Singh K.D., Brealy J.A., Linden D.E., Evans C.J. Quantification of γ-aminobutyric acid (GABA) in 1H MRS volumes composed heterogeneously of grey and white matter. NMR Biomed. 2016;29:1644–1655. doi: 10.1002/nbm.3622. [DOI] [PubMed] [Google Scholar]
- 107.Kirkovski M., Suo C., Enticott P.G., Yucel M., Fitzgerald P.B. Short communication: Sex-linked differences in gamma-aminobutyric acid (GABA) are related to social functioning in autism spectrum disorder. Psychiatry. Res. Neuroimaging. 2018;274:19–22. doi: 10.1016/j.pscychresns.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 108.Sarris J., LaPorte E., Schweitzer I. Kava: A comprehensive review of efficacy, safety, and psychopharmacology. Aust. N. Z. J. Psychiatry. 2011;45:27–35. doi: 10.3109/00048674.2010.522554. [DOI] [PubMed] [Google Scholar]
- 109.Witte S., Loew D., Gaus W. Meta-analysis of the efficacy of the acetonic kava-kava extract WS® 1490 in patients with non-psychotic anxiety disorders. Phytother. Res. Int. J. Devoted Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2005;19:183–188. doi: 10.1002/ptr.1609. [DOI] [PubMed] [Google Scholar]
- 110.Krum B.N., de Freitas C.M., Busanello A., Schaffer L.F., Fachinetto R. Ex vivo and in vitro inhibitory potential of Kava extract on monoamine oxidase B activity in mice. J. Tradit. Complement. Med. 2022;12:115–122. doi: 10.1016/j.jtcme.2021.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Mikkelsen M., Barker P.B., Bhattacharyya P.K., Brix M.K., Buur P.F., Cecil K.M., Edden R.A. Big GABA: Edited MR spectroscopy at 24 research sites. Neuroimage. 2017;159:32–45. doi: 10.1016/j.neuroimage.2017.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Mullins P.G., McGonigle D.J., O’Gorman R.L., Puts N.A., Vidyasagar R., Evans C.J., Edden R.A. Current practice in the use of MEGA-PRESS spectroscopy for the detection of GABA. Neuroimage. 2014;86:43–52. doi: 10.1016/j.neuroimage.2012.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Stagg C.J., Bachtiar V., Johansen-Berg H. What are we measuring with GABA magnetic resonance spectroscopy? Commun. Integr. Biol. 2011;4:573–575. doi: 10.4161/cib.16213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Insel T.R. The NIMH Research Domain Criteria (RDoC) Project: Precision medicine for psychiatry. Am. J. Psychiatry. 2014;171:395–397. doi: 10.1176/appi.ajp.2014.14020138. [DOI] [PubMed] [Google Scholar]
- 115.Williams L.M., Goldstein-Piekarski A.N., Chowdhry N., Grisanzio K.A., Haug N.A., Samara Z., Yesavage J. Developing a clinical translational neuroscience taxonomy for anxiety and mood disorder: Protocol for the baseline-follow up Research domain criteria Anxiety and Depression (“RAD”) project. BMC Psychiatry. 2016;16:68. doi: 10.1186/s12888-016-0771-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.McNaughton N. Development of a theoretically-derived human anxiety syndrome biomarker. Transl. Neurosci. 2014;5:137–146. doi: 10.2478/s13380-014-0220-z. [DOI] [Google Scholar]
- 117.Sanislow C.A., Pine D.S., Quinn K.J., Kozak M.J., Garvey M.A., Heinssen R.K., Cuthbert B.N. Developing constructs for psychopathology research: Research domain criteria. J. Abnorm. Psychol. 2010;119:631–639. doi: 10.1037/a0020909. [DOI] [PubMed] [Google Scholar]
- 118.Cuthbert B.N., Insel T.R. Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Med. 2013;11:126. doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Fernandes B.S., Williams L.M., Steiner J., Leboyer M., Carvalho A.F., Berk M. The new field of ‘precision psychiatry’. BMC Med. 2017;15:80. doi: 10.1186/s12916-017-0849-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Singh I., Rose N. Biomarkers in psychiatry. Nature. 2009;460:202–207. doi: 10.1038/460202a. [DOI] [PubMed] [Google Scholar]
- 121.Lueken U., Zierhut K.C., Hahn T., Straube B., Kircher T., Reif A., Domschke K. Neurobiological markers predicting treatment response in anxiety disorders: A systematic review and implications for clinical application. Neurosci. Biobehav. Rev. 2016;66:143–162. doi: 10.1016/j.neubiorev.2016.04.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data were collected exclusively for the purpose of fulfilling the NHMRC grant research within a clinical group. Additionally, provision to third parties may not comply with Australian clinical trial grant mandates. To this end, the data from this study are not publicly available.