Abstract
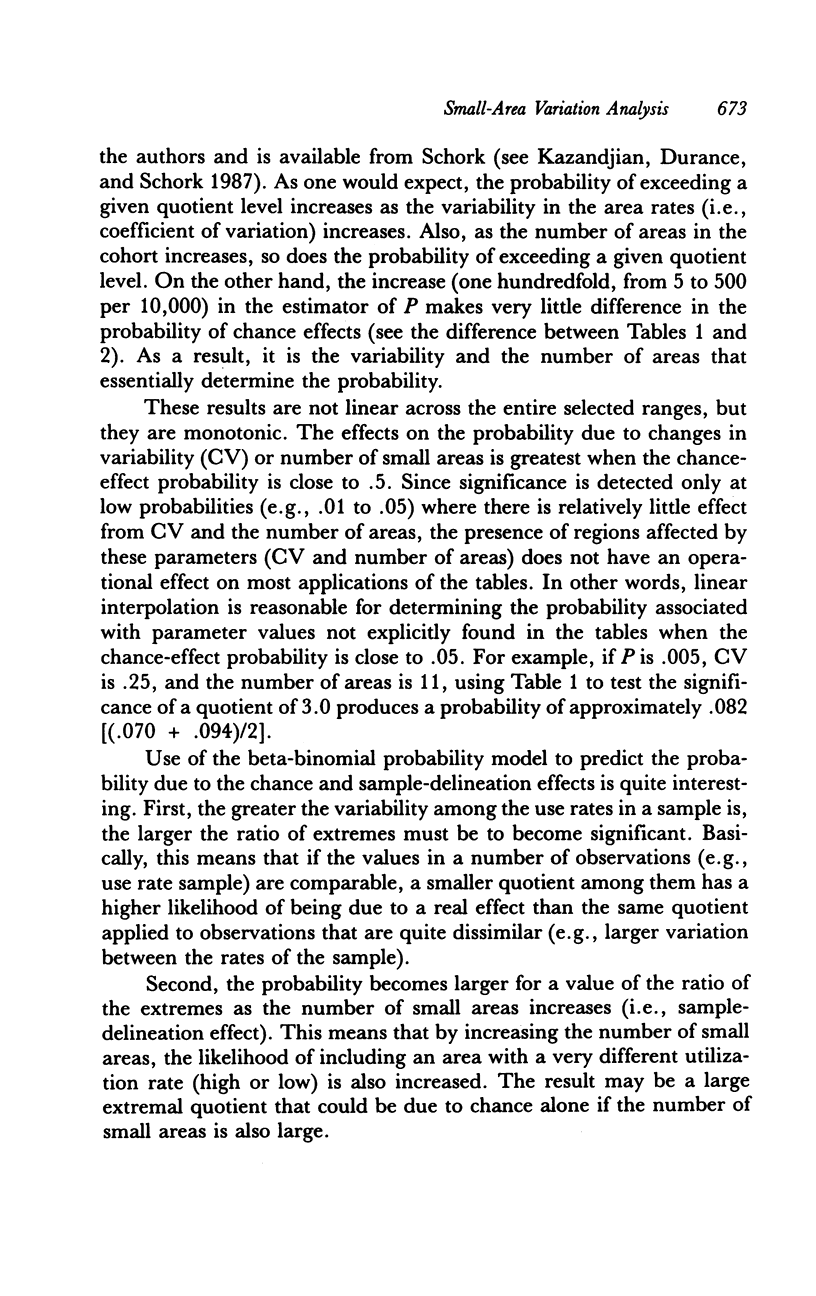
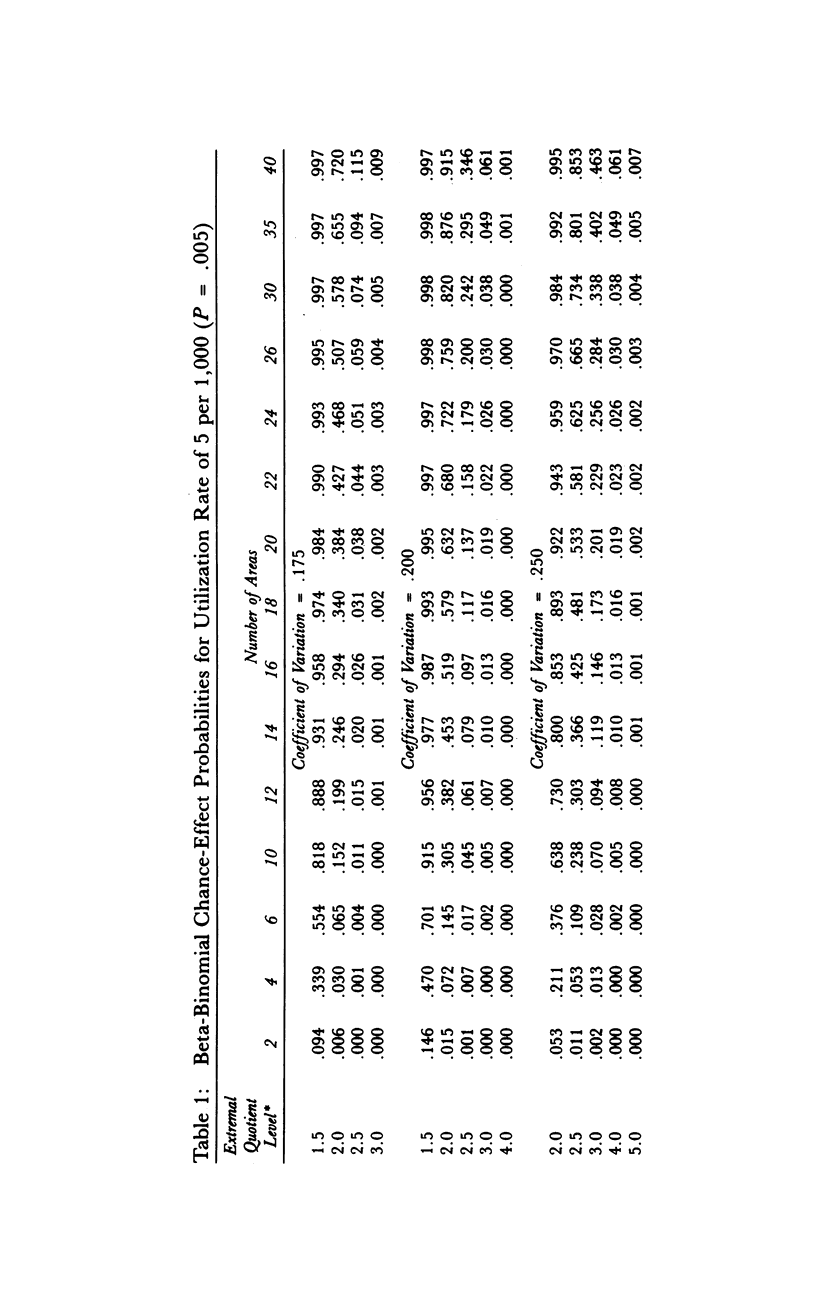
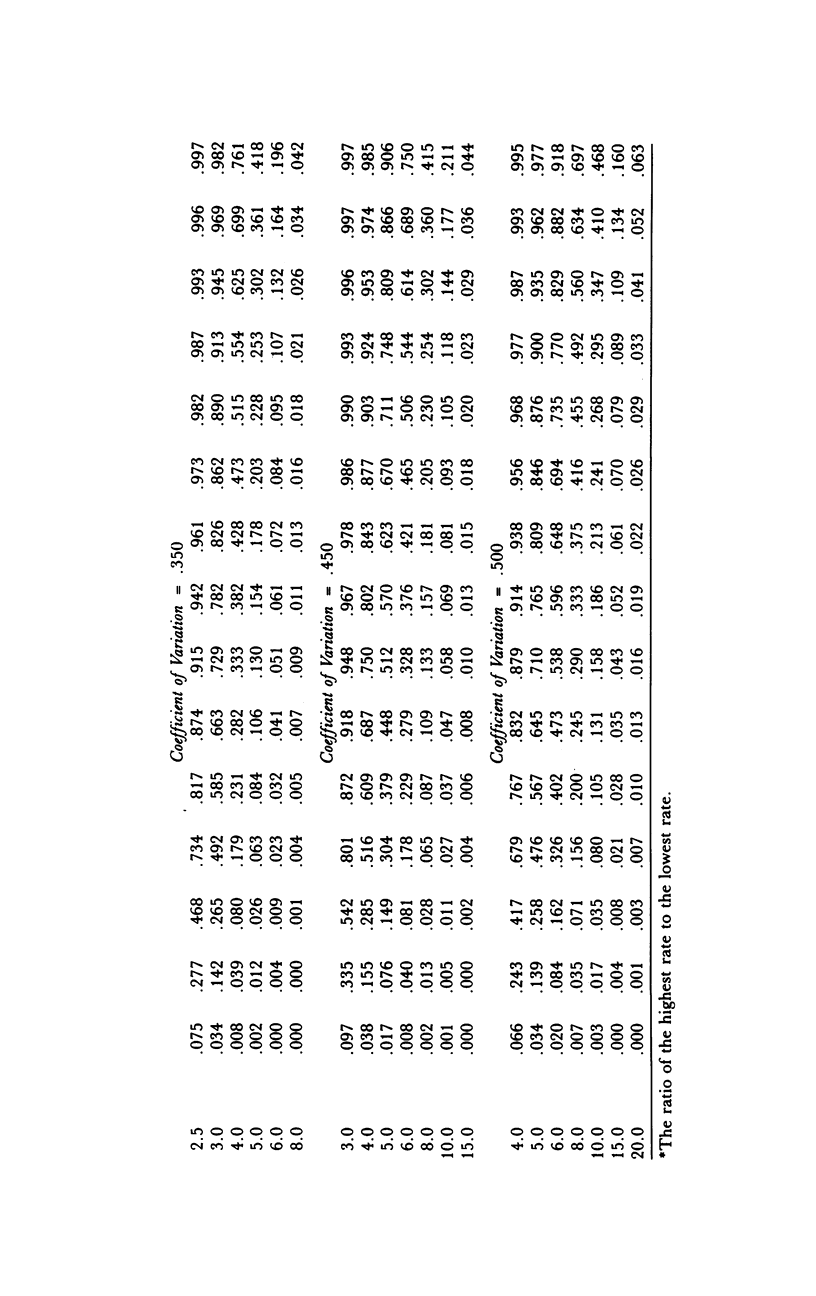
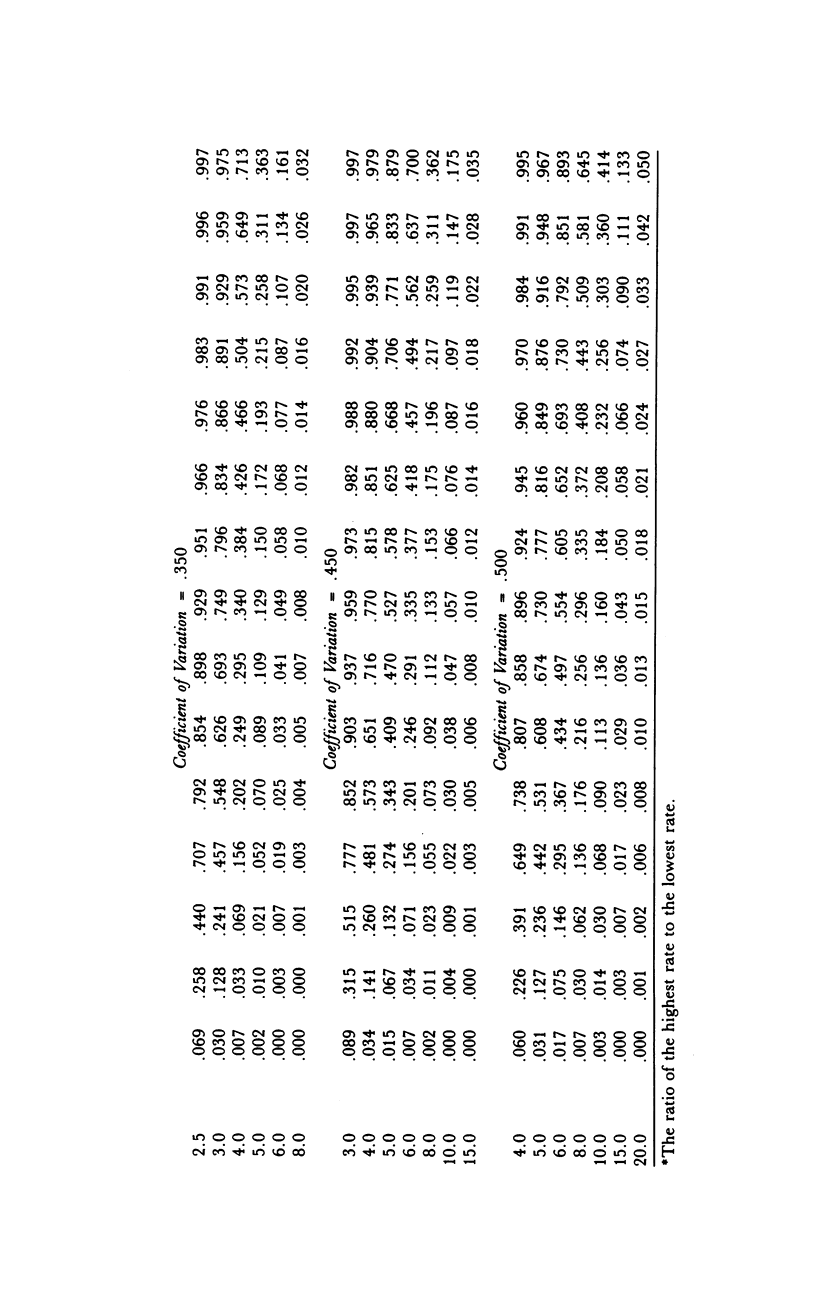
This article reviews the current small-area variation analysis (SAVA) approach to population-based rates of surgery, and describes a new method for ascertaining variance based on the beta-binomial probability distribution of small-area rates. The critical review of the current SAVA approach focuses (1) on how incidence rates are calculated, and (2) on how the significance of the observed magnitude between the largest and smallest rates (i.e., the external quotient) is ascertained. While reducing the problems of calculating rates by considering only certain operative procedures, the new method addresses the current inadequacies of ascertaining significant differences among small areas. Not only does it correctly assess likelihood of an extermal quotient, it also can determine the particular area's rate, producing an unlikely extermal quotient. The method evaluates the probability that the observed magnitude of the extremal quotient is due solely to chance and study design effects, and tables of these probabilities are available for the method's application. A mathematical model, based on a combination of the binomial and beta distributions, uses (1) the sample size, (2) the average of the areas' rates, (3) the variance among the rates, and (4) a specific quotient level to determine the probability of observing the quotient by chance. After computerizing this calculation, probability tables for reasonable values of these four parameters are generated. In addition to looking at just one quotient for each sample, the probability tables facilitate the easy examination of intermediate quotients when the extremal quotient is unlikely due to chance. By alternatively ignoring the highest and lowest rates, two new quotients can be produced and tested. Given that one of these two quotients is likely due to chance, the excluded rate (i.e., producing the unlikely extremal quotient) can be classified as an outliner, and the associated small area should be the focus of more detailed investigation. The probability tables reveal that the external quotient is not the appropriate statistic to be applied in studies where many small areas are to be included. The probability of seeing even a "large" extremal quotient simply by chance rapidly approaches one as the sample size increases. However, an extremal quotient modeled from a beta-binomial distribution can be useful for studies with small sample sizes (e.g., six counties). The use of this beta-binomial model for small-area rates provides a new method of designing and evaluating small-area studies where costs or domain limit the number of areas under consideration.(ABSTRACT TRUNCATED AT 400 WORDS)
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brook R. H., Lohr K., Chassin M., Kosecoff J., Fink A., Solomon D. Geographic variations in the use of services: do they have any clinical significance? Health Aff (Millwood) 1984 Summer;3(2):63–73. doi: 10.1377/hlthaff.3.2.63. [DOI] [PubMed] [Google Scholar]
- Cageorge S. M., Roos L. L., Jr When surgical rates change. Workload and turnover in Manitoba, 1974-1978. Med Care. 1984 Oct;22(10):890–900. [PubMed] [Google Scholar]
- Chassin M. R., Brook R. H., Park R. E., Keesey J., Fink A., Kosecoff J., Kahn K., Merrick N., Solomon D. H. Variations in the use of medical and surgical services by the Medicare population. N Engl J Med. 1986 Jan 30;314(5):285–290. doi: 10.1056/NEJM198601303140505. [DOI] [PubMed] [Google Scholar]
- Connell F. A., Blide L. A., Hanken M. A. Clinical correlates of small area variations in population-based admission rates for diabetes. Med Care. 1984 Oct;22(10):939–949. doi: 10.1097/00005650-198410000-00006. [DOI] [PubMed] [Google Scholar]
- Diehr P. Small area statistics: large statistical problems. Am J Public Health. 1984 Apr;74(4):313–314. doi: 10.2105/ajph.74.4.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gornick M. Medicare patients: geographic differences in hospital discharge rates and multiple stays. Soc Secur Bull. 1977 Jun;40(6):22–41. [PubMed] [Google Scholar]
- Griffith J. R., Wilson P. A., Wolfe R. A., Bischak D. P. Clinical profiles of hospital discharge rates in local communities. Health Serv Res. 1985 Jun;20(2):131–151. [PMC free article] [PubMed] [Google Scholar]
- Kazandjian V. A., Dans P. E., Scherlis L. What physicians should know about small area variation analysis. Md Med J. 1989 Jun;38(6):477–481. [PubMed] [Google Scholar]
- Knickman J. R., Foltz A. M. Regional differences in hospital utilization. How much can be traced to population differences? Med Care. 1984 Nov;22(11):971–986. doi: 10.1097/00005650-198411000-00001. [DOI] [PubMed] [Google Scholar]
- Kuder J. M., Demlo L. K., Curry J. P., Levey S. Small-area variations in Iowa hospital utilization. Iowa Med. 1985 May;75(5):213–217. [PubMed] [Google Scholar]
- LEMBCKE P. A. Measuring the quality of medical care through vital statistics based on hospital service areas; I. Comparative study of appendectomy rates. Am J Public Health Nations Health. 1952 Mar;42(3):276–286. doi: 10.2105/ajph.42.3.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis C. E. Variations in the incidence of surgery. N Engl J Med. 1969 Oct 16;281(16):880–884. doi: 10.1056/NEJM196910162811606. [DOI] [PubMed] [Google Scholar]
- McCarthy E. G., Finkel M. L. Surgical utilization in the U.S.A. Med Care. 1980 Sep;18(9):883–892. doi: 10.1097/00005650-198009000-00002. [DOI] [PubMed] [Google Scholar]
- McCracken G., Bognanni S. Iowa employers use small area analysis in benefits reform. Bus Health. 1986 Sep;3(9):14–16. [PubMed] [Google Scholar]
- McPherson K., Strong P. M., Epstein A., Jones L. Regional variations in the use of common surgical procedures: within and between England and Wales, Canada and the United States of America. Soc Sci Med A. 1981 May;15(3 Pt 1):273–288. doi: 10.1016/0271-7123(81)90011-0. [DOI] [PubMed] [Google Scholar]
- McPherson K., Wennberg J. E., Hovind O. B., Clifford P. Small-area variations in the use of common surgical procedures: an international comparison of New England, England, and Norway. N Engl J Med. 1982 Nov 18;307(21):1310–1314. doi: 10.1056/NEJM198211183072104. [DOI] [PubMed] [Google Scholar]
- Roos L. L., Jr, Roos N. P. Assessing existing technologies: the Manitoba study of common surgical procedures. Med Care. 1983 Apr;21(4):454–462. doi: 10.1097/00005650-198304000-00008. [DOI] [PubMed] [Google Scholar]
- Roos L. L., Jr, Roos N. P., Henteleff P. D. Assessing the impact of tonsillectomies. Med Care. 1978 Jun;16(6):502–518. doi: 10.1097/00005650-197806000-00007. [DOI] [PubMed] [Google Scholar]
- Roos N. P., Gilbert P. Tonsillectomy in Manitoba: who are the patients? the surgeons? the hospitals? J Community Health. 1979 Winter;5(2):101–112. doi: 10.1007/BF01324012. [DOI] [PubMed] [Google Scholar]
- Roos N. P., Henteleff P. D., Roos L. L., Jr A new audit prodecure applied to an old question: Is the frequency of T&A justified? Med Care. 1977 Jan;15(1):1–18. doi: 10.1097/00005650-197701000-00001. [DOI] [PubMed] [Google Scholar]
- Roos N. P. Hysterectomy: variations in rates across small areas and across physicians' practices. Am J Public Health. 1984 Apr;74(4):327–335. doi: 10.2105/ajph.74.4.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos N. P., Roos L. L., Jr, Henteleff P. D. Elective surgical rates--do high rates mean lower standards? Tonsillectomy and adenoidectomy in Manitoba. N Engl J Med. 1977 Aug 18;297(7):360–365. doi: 10.1056/NEJM197708182970705. [DOI] [PubMed] [Google Scholar]
- Stockwell H., Vayda E. Variations in surgery in Ontario. Med Care. 1979 Apr;17(4):390–396. doi: 10.1097/00005650-197904000-00007. [DOI] [PubMed] [Google Scholar]
- Wennberg J. E., Blowers L., Parker R., Gittelsohn A. M. Changes in tonsillectomy rates associated with feedback and review. Pediatrics. 1977 Jun;59(6):821–826. [PubMed] [Google Scholar]
- Wennberg J. E., Bunker J. P., Barnes B. The need for assessing the outcome of common medical practices. Annu Rev Public Health. 1980;1:277–295. doi: 10.1146/annurev.pu.01.050180.001425. [DOI] [PubMed] [Google Scholar]
- Wennberg J., Gittelsohn A. Variations in medical care among small areas. Sci Am. 1982 Apr;246(4):120–134. doi: 10.1038/scientificamerican0482-120. [DOI] [PubMed] [Google Scholar]
- Wilson P. A., Griffith J. R., Tedeschi P. J. Does race affect hospital use? Am J Public Health. 1985 Mar;75(3):263–269. doi: 10.2105/ajph.75.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson P., Tedeschi P. Community correlates of hospital use. Health Serv Res. 1984 Aug;19(3):333–355. [PMC free article] [PubMed] [Google Scholar]


