Abstract
Wildfires are increasing in frequency and intensity, with significant consequences that impact human health. A scoping review was conducted to: (a) understand wildfire‐related health effects, (b) identify and describe environmental exposure and health outcome data sources used to research the impacts of wildfire exposures on health, and (c) identify gaps and opportunities to leverage exposure and health data to advance research. A literature search was conducted in PubMed and a sample of 83 articles met inclusion criteria. A majority of studies focused on respiratory and cardiovascular outcomes. Hospital administrative data was the most common health data source, followed by government data sources and health surveys. Wildfire smoke, specifically fine particulate matter (PM2.5), was the most common exposure measure and was predominantly estimated from monitoring networks and satellite data. Health data were not available in real‐time, and they lacked spatial and temporal coverage to study health outcomes with longer latency periods. Exposure data were often available in real‐time and provided better temporal and spatial coverage but did not capture the complex mixture of hazardous wildfire smoke pollutants nor exposures associated with non‐air pathways such as soil, household dust, food, and water. This scoping review of the specific health and exposure data sources used to underpin these studies provides a framework for the research community to understand: (a) the use and value of various environmental and health data sources, and (b) the opportunities for improving data collection, integration, and accessibility to help inform our understanding of wildfires and other environmental exposures.
Keywords: wildfires, geographic information systems, electronic health records, epidemiology
Key Points
Wildfires are a growing health issue and enhancing geoscience and health data will advance response, recovery, and future preparedness
Linking health and climate exposure data longitudinally and across geographic regions poses a challenge for health researchers
Enhanced exposure data that capture all relevant exposure pathways and the complex composition of wildfire smoke are needed
1. Introduction
Wildfire experiences across 25 states in the United States (US), stemming from the 2023 Canadian wildfires (Choi & Shveda, 2023), as well as the tragedy in Lahaina, Hawaii (EPA, 2023) underscore the fact that wildfires have been increasing in frequency and severity, and in the coming decades, climate change is expected to exacerbate the problem (Dennison et al., 2014; Jain et al., 2022; Parks & Abatzoglou, 2020). Exposure to wildfire smoke has been linked to adverse human health outcomes, including asthma, other respiratory health outcomes, cardiovascular events, adverse birth outcomes, and mortality (Holm et al., 2021; J. C. Liu et al., 2015; Reid & Maestas, 2019; Reid et al., 2016; Xu et al., 2020). Under a changing climate, an estimated 82 million Americans will experience a 57% increase in the frequency of exposures to wildfire‐related smoke (J. C. Liu et al., 2016), but the potential health impacts of wildfires are not limited to only wildfire prone geographical regions of the US as winds can carry pollutants hundreds of kilometers away.
Wildfire smoke is a complex mixture of particulate matter, hazardous pollutants, and other gaseous pollutants. Fires occurring in the wildland urban interface (WUI), areas where homes and other structures meet vegetative fuels, are potentially more hazardous. These fires can emit a broad range of chemicals and pollutants, adding further complexity to the mixture of pollutants for human exposure (National Academies of Sciences, Engineering, and Medicine, 2022).
Researchers are combining geoscience and health data sources using geographic information systems and data science approaches to study the effects of wildfires. However, relevant data are not always available in the spatial and temporal scales needed to study large populations over the relevant time periods. In this scoping review, we describe the commonly used data sources and approaches for combining traditional and non‐traditional data to understand wildfire‐related exposures and health effects. Specifically, this scoping review aims to: (a) understand wildfire‐related health effects, (b) identify and describe environmental exposure and health outcome data sources that have been used to research the impacts of wildfire exposures on various health outcomes, and (c) identify gaps and opportunities to leverage exposure and health data sources to advance research. Understanding and building upon the current state of geoscience and health data systems will enhance our ability to better characterize exposures to wildfires and associated health outcomes, implement prevention strategies, and respond effectively to wildfire impacts on human health.
2. Methods
While this review focused on studies linking wildfire exposures and health outcomes, a broader search was conducted to capture additional wildfire exposure science articles that assessed or identified pollutants from less common exposure media (e.g., water, ash, and soil) or used novel data sources to assess exposures that have relevance to human health. The search strategy was developed by conducting initial searches of PubMed using key words related to wildfires and various health outcomes. Initially, three recent review articles were identified (Holm et al., 2021; J. C. Liu et al., 2015; Reid et al., 2016), and the references from these articles were screened for eligibility. Next, a literature search was performed in PubMed combining search terms related to wildfires, WUI exposures, and human health outcomes. Search terms were used to capture exposures to smoke, ash, soil, and water. Health outcome search terms included respiratory, cardiovascular, pregnancy and perinatal health, mental health, cancer, and population health.
Screening of titles and abstracts was conducted by one reviewer, and then full text articles were screened by two reviewers. Articles published before 31 July 2022 were eligible for inclusion. While the focus for this review was on metrics from the US and North America, research conducted in other geographical areas was included when relevant to the research questions. Additionally, studies that had no direct connection to human health, assessed animal populations or human tissue samples, or focused solely on occupational or non‐wildfire related exposures were excluded. However, after completing the initial review, 14 articles (Beaupied et al., 2022; Black et al., 2017; Buchholz et al., 2022; Delfino et al., 2002, 2010; Ghetu et al., 2022; Huttunen et al., 2012; Liang et al., 2021; Messier et al., 2019; Nguyen et al., 2021; O’Hara et al., 2021; Ré et al., 2021; Solomon et al., 2021; Wan et al., 2021) within these categories were included to capture the use of novel data sources or for potential relevance to human health outcomes. Information from full text articles was organized in a Microsoft Excel spreadsheet. Descriptive article information such as publication titles, authors' names, and year of publication were extracted. The main health and exposure variables were recorded, and specific health and exposure data sources were described and reported in the spreadsheet.
3. Results
3.1. Study Characteristics
As shown in Figure 1, a total of 925 articles were eligible for review, and of these, 83 met the inclusion criteria. Among the included articles, publication dates ranged from 1993 to 2022 and a total of 69 studies assessed the impact of wildfire‐related exposures on human health outcomes, and 14 studies met inclusion criteria for their relevance to human health, including seven exposure science studies, three review articles, three animal studies, and one toxicology study. All articles included in this review are summarized in Table 1. This table presents information on health outcomes, exposures metrics, and the underlying data sources used to obtain these metrics.
Figure 1.
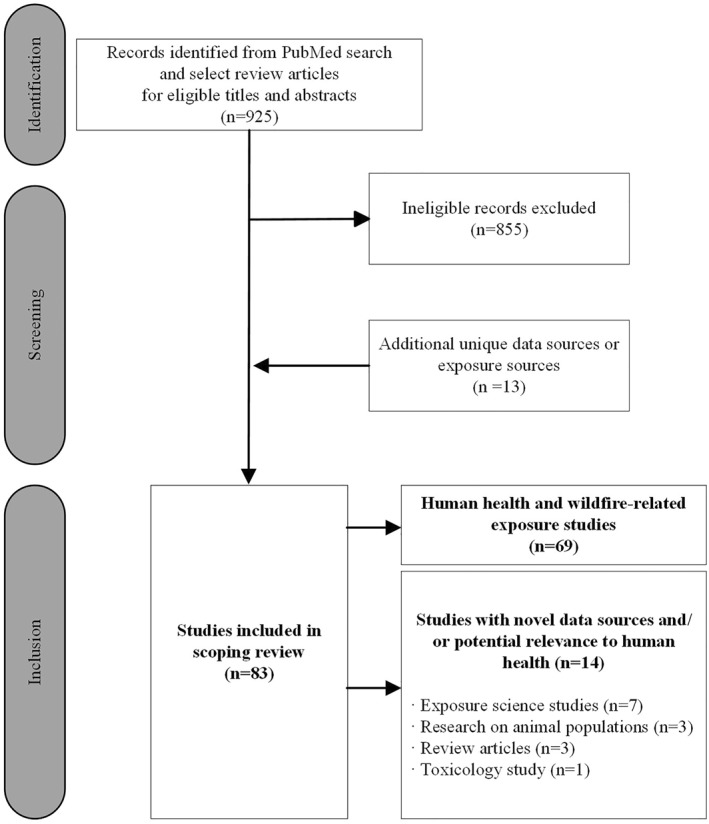
Flow diagram of articles identified, screened, and included for review. Database searches were performed in December 2021 and July 2022.
Table 1.
Summary of Health and Exposure Data Sources Identified From Literature Included in This Scoping Review
| Citation | Health Outcomes | Health Data Sources | Exposures | Exposure Data Sources |
|---|---|---|---|---|
| Abdo et al. (2019) | Perinatal/Infant Development | Administrative | PM2.5 | Monitoring, Satellite |
| Ademu et al. (2022) | Infectious Disease | Surveillance | Air Quality Index, Carbon Monoxide, Nitrogen Oxides, PM2.5 | Monitoring |
| Aguilera, Corringham, Gershunov, and Benmarhnia (2021) | Respiratory | Administrative | PM2.5 | Event, Monitoring, Satellite |
| Aguilera, Corringham, Gershunov, Leibel, and Benmarhnia (2021) | Respiratory | Administrative | PM2.5 | Monitoring, Satellite |
| Aguilera et al. (2020) | Respiratory | Administrative | Smoke | Event, Satellite |
| Alman et al. (2016) | Cardiovascular, Respiratory | Administrative | PM2.5 | Event, Models/Forecasting, Monitoring, Satellite |
| Beaupied et al. (2022) | Not Evaluated a | Biospecimens | Not Evaluated a | Not Evaluated a |
| Black et al. (2017) | Not Evaluated a | Biospecimens, Clinical Test | Not Evaluated a | Not Evaluated a |
| Buchholz et al. (2022) | Not Evaluated b | Not Evaluated b | Carbon Monoxide b | Satellite |
| Burke et al. (2022) | Behavior | Crowdsourced | PM2.5 | Monitoring, Satellite |
| Caamano‐Isorna et al. (2011) | Respiratory, Mental Health | Pharmaceutical | Wildfire Event | Event |
| Cançado et al. (2006) | Respiratory | Administrative | Black Carbon, PM2.5, PM10, Trace Elements | Environmental Sampling |
| Cândido da Silva et al. (2014) | Perinatal/Infant Development | Administrative | Carbon Monoxide, PM2.5 | Models/Forecasting |
| Casey et al. (2021) | Cardiovascular, Respiratory, Mortality | Administrative | PM2.5 | Monitoring, Satellite |
| CDC (2008) | Respiratory | Administrative | Wildfire Event | Event |
| H. J. Cleland et al. (2011) | Injury | Administrative | Wildfire Event | Event |
| S. E. Cleland et al. (2021) | Cardiovascular, Respiratory | Government | PM2.5 | Models/Forecasting, Monitoring, Satellite |
| S. E. Cleland et al. (2022) | Cognitive | Crowdsourced | PM2.5 | Monitoring, Satellite |
| DeFlorio‐Barker et al. (2019) | Cardiovascular, Respiratory | Claims | PM2.5 | Event, Models/Forecasting, Monitoring |
| Delfino et al. (2009) | Cardiovascular, Respiratory | Administrative | PM2.5 | Monitoring, Satellite |
| Delfino et al. (2010) | Inflammatory, Respiratory | Biospecimens | Black Carbon, Carbon Monoxide, Nitrogen Oxides, Organic PM0.25 Components, Ozone, Primary/Secondary Organic Carbon, PM2.5, PM10 | Environmental Sampling, Personal Monitoring |
| Delfino et al. (2002) | Respiratory | Survey | Nitrogen Oxides, Ozone, PM10 | Monitoring |
| Dennekamp et al. (2015) | Cardiovascular | Administrative | Carbon Monoxide, Nitrogen Oxides, Ozone, PM2.5, PM10, Sulfur Dioxide | Monitoring |
| DeYoung et al. (2018) | Perinatal/Infant Development | Survey | Wildfire Event | Event |
| Dodd et al. (2018) | Mental Health | Survey | Wildfire Event | Event |
| Dohrenwend et al. (2013) | Respiratory | Administrative | Air Quality Index, Wildfire Event | Monitoring |
| Doubleday et al. (2020) | Mortality | Administrative | PM2.5 | Models/Forecasting, Monitoring |
| Elliott et al. (2013) | Respiratory | Pharmaceutical | PM2.5 | Monitoring, Satellite |
| Fann et al. (2018) | Mortality, Respiratory | Government | PM2.5 | Models/Forecasting, Satellite |
| Gan et al. (2017) | Cardiovascular, Respiratory | Administrative | PM2.5 | Models/Forecasting, Monitoring, Satellite |
| Gan et al. (2020) | Respiratory | Claims | PM2.5 | Models/Forecasting, Monitoring, Satellite |
| Ghetu et al. (2022) | Not Evaluated b | Not Evaluated b | Polycyclic Aromatic Hydrocarbons b | Environmental Sampling |
| Haikerwal et al. (2021) | Respiratory | Survey | Wildfire Event | Event |
| Heaney et al. (2022) | Cardiovascular, Respiratory | Administrative | PM2.5 | Models/Forecasting |
| Heft‐Neal et al. (2022) | Perinatal/Infant Development | Administrative | PM2.5 | Models/Forecasting, Satellite |
| Henderson et al. (2021) | Respiratory | Pharmaceutical | PM2.5 | Models/Forecasting |
| Holstius et al. (2012) | Perinatal/Infant Development | Administrative | Wildfire Event | Satellite |
| Howard et al. (2021) | Cardiovascular, Respiratory | Administrative, Pharmaceutical | PM2.5, PM10 | Monitoring |
| Hutchinson et al. (2018) | Cardiovascular, Respiratory | Administrative | PM2.5 | Event, Models/Forecasting |
| Huttunen et al. (2012) | Cardiovascular, Inflammatory | Biospecimens, Survey | PM2.5, PM10 | Monitoring, Personal Monitoring |
| Hyde et al. (2021) | Mental Health, Perinatal/Infant Development | Survey | Wildfire Event | Event |
| Isaac et al. (2021) | Mental Health c | Survey | Not Evaluated c | Not Evaluated c |
| Kiser et al. (2020) | Respiratory | Administrative | PM2.5, PM10 | Monitoring |
| Kiser et al. (2021) | Infectious Disease | Surveillance | PM2.5 | Monitoring |
| Koman et al. (2019) | Cardiovascular, Perinatal/Infant Development, Respiratory | Government | PM2.5 | Models/Forecasting, Monitoring, Satellite |
| Korsiak et al. (2022) | Cancer | Government | Wildfire Event | Event |
| Landguth et al. (2020) | Infectious Disease | Surveillance | PM2.5 | Monitoring, Satellite |
| Leibel et al. (2020) | Respiratory | Administrative | PM2.5 | Event, Monitoring, Satellite |
| Li et al. (2021) | Perinatal/Infant Development | Government | PM2.5 | Event, Models/Forecasting |
| Liang et al. (2021) | Not Evaluated b | Not Evaluated b | PM2.5 b | Monitoring |
| J. C. Liu, Wilson, Mickley, Dominici, et al. (2017) | Cardiovascular, Respiratory | Claims | PM2.5 | Event, Monitoring, Models/Forecasting |
| J. C. Liu, Wilson, Mickley, Ebisu, et al. (2017) | Respiratory, Social Vulnerability | Claims | PM2.5 | Event, Monitoring |
| Y. Liu et al. (2021) | Cardiovascular, Mortality, Respiratory | Government | PM2.5 | Monitoring |
| Mahsin et al. (2021) | Cardiovascular, Respiratory | Claims | PM2.5 | Monitoring |
| Masri et al. (2021) | Social Vulnerability | Government | Wildfire Event | Event |
| Messier et al. (2019) | Not Evaluated b | Not Evaluated b | Polycyclic Aromatic Hydrocarbons b | Environmental Sampling, Satellite |
| Naqvi et al. (2022) | Infectious Disease, Mortality | Surveillance | Carbon Monoxide, Nitrogen Oxides, Ozone, PM2.5 | Monitoring |
| Neumann et al. (2021) | Morbidity, Mortality | Government | PM2.5 | Event, Models/Forecasting |
| Nguyen et al. (2021) | Not Evaluated b | Not Evaluated b | Carbon Monoxide, Nitrogen Oxides, PM2.5, Volatile Organic Compounds b | Monitoring |
| O'Dell et al. (2021) | Respiratory, Mortality | Government | Hazardous Air Pollutants, PM2.5 | Monitoring, Satellite |
| O'Hara et al. (2021) | Not Evaluated a | Survey | Not Evaluated a | Not Evaluated a |
| O'Neill et al. (2021) | Mortality | Government | PM2.5 | Models/Forecasting, Monitoring, Satellite |
| Park et al. (2022) | Perinatal/Infant Development | Administrative | Wildfire Event | Event |
| Pazderka, Brown, McDonald‐Harker, et al. (2021) | Mental Health | Survey | Wildfire Event | Event |
| Pazderka, Brown, Agyapong, et al. (2021) | Mental Health | Survey | Wildfire Event | Event |
| Pearson et al. (2019) | Infectious Disease c | Surveillance | Not Evaluated c | Not Evaluated c |
| Postma et al. (2022) | Respiratory | Clinical Test, Survey | PM2.5 | Monitoring |
| Rappold et al. (2017) | Cardiovascular, Respiratory, Social Vulnerability | Government | PM2.5 | Event, Models/Forecasting |
| Rappold et al. (2019) | Behavior, Cardiovascular, Respiratory | Survey | Smoke | Monitoring, Satellite |
| Ré et al. (2021) | Not Evaluated d | Biospecimens | Ash d | Environmental Sampling |
| Requia et al. (2021) | Perinatal/Infant Development | Administrative | Carbon Monoxide, Nitrogen Oxides, Ozone, PM2.5 | Event, Monitoring |
| Rodney et al. (2021) | Mental Health, Respiratory, Sleep | Survey | Wildfire Event | Event |
| Sannigrahi et al. (2022) | Infectious Disease, Mortality | Surveillance | Nitrogen Oxides, PM2.5, PM10 | Monitoring |
| Schwarz et al. (2022) | Infectious Disease, Mortality | Surveillance | Smoke | Satellite |
| Shusterman et al. (1993) | Hospital Visits/Admissions, Injury, Mortality, Respiratory | Administrative | Wildfire Event | Event |
| Solomon et al. (2021) | Not Evaluated b | Not Evaluated b | Volatile Organic Compounds b | Environmental Sampling |
| Sorensen et al. (2021) | Hospital Visits/Admissions | Administrative | Ozone, PM2.5, PM10 | Monitoring, Satellite |
| Sugg et al. (2022) | Mental Health | Crowdsourced | Wildfire Event | Event |
| To et al. (2021) | Mental Health c | Survey | Not Evaluated c | Not Evaluated c |
| Wan et al. (2021) | Not Evaluated b | Not Evaluated b | Ash, Soil b | Environmental Sampling |
| Woo et al. (2020) | Social Vulnerability | Government | PM2.5 | Event, Models/Forecasting, Monitoring |
| Yao et al. (2020) | Cardiovascular, Diabetic Conditions, Respiratory | Administrative | PM2.5 | Models/Forecasting |
| Zhou et al. (2021) | Infectious Disease, Mortality | Surveillance | PM2.5 | Monitoring, Satellite |
Animal Study—animal studies were included for potential relevance to human health, not included in evaluation of human health outcomes and wildfire‐related exposures.
Exposure Science Study—not included in evaluation of human health outcomes and wildfire‐related exposures.
Review Article—included for unique assessment and/or relevance to understudied human health outcomes, not included in evaluation of human health outcomes and wildfire‐related exposures.
Toxicology Study—not included in evaluation of human health outcomes and wildfire‐related exposures.
The distribution of articles by health outcomes (Figure 2) and exposure measures (Figure 3) are shown below. Articles were grouped into 16 health outcome categories and 14 exposure categories as described in Table S1 in Supporting Information S1. These graphs include studies that assessed the relationship between wildfire exposures and health outcomes (n = 69) to show the major focus areas of this research. Health outcome and exposure categories with low article counts were included to highlight potential knowledge gaps.
Figure 2.
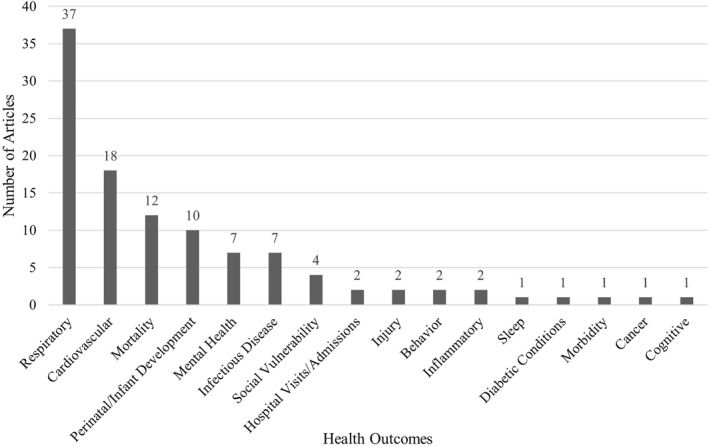
Number of articles by health outcomes assessed (n = 69). All articles that studied human health and wildfire‐related exposures are included. Articles assessed one or more health outcomes. Article counts and percentages are shown in Table S2 in Supporting Information S1.
Figure 3.
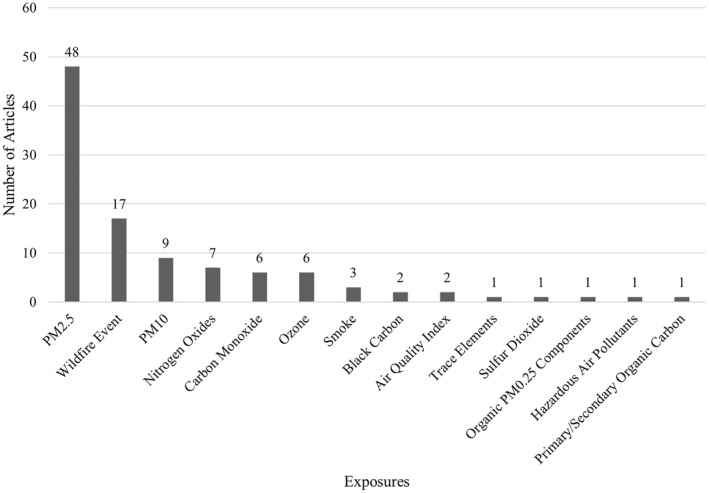
Number of articles by exposure assessed (n = 69). All articles that studied human health and wildfire‐related exposures are included. Articles assessed one or more exposures. Article counts and percentages are shown in Table S3 in Supporting Information S1.
3.1.1. Characterization of Health Outcomes
Most studies identified in the review of articles studying human health and wildfire‐related exposures (n = 69) assessed respiratory (54%) and cardiovascular (26%) health outcomes either separately, together, or in addition to other health outcomes (Figure 2). Studies included in this review also assessed mortality (17%), perinatal health outcomes (15%), mental health outcomes (10%), and infectious diseases (10%). Only four studies (6%) assessed social vulnerability using individual or community‐level risk measures. Studies on cancer, cognitive outcomes, diabetic conditions, morbidity, and sleep were sparse.
3.1.2. Characterization of Exposures
Health outcome data were most commonly linked with wildfire smoke exposure estimates (n = 69), and almost three‐quarters of these articles focused on PM2.5 mass concentration. Articles with other exposure metrics were limited, but researchers did study nitrogen oxides (NO x ) (10%), carbon monoxide (CO) (9%), ozone (O3) (9%), black carbon (3%), and other pollutants from wildfire smoke (Figure 3). These were typically assessed in addition to PM2.5 or PM10 from surface monitors. Most exposures were defined by measuring or estimating specific pollutants from air samples, forecasting systems, or satellite data. Seventeen studies (25%) used wildfire events to define exposure windows or to assess proximity to a wildfire event as a proxy for wildfire exposures. Three studies (4%) used smoke as their main exposure. This was defined by the presence of smoke plumes, typically identified with the National Oceanic and Atmospheric Administration (NOAA) Hazard Mapping System (HMS) or satellite imagery rather than identifying specific pollutants.
Seven exposure science studies and one toxicology study assessed wildfire‐related exposures but did not associate these exposures with human health outcomes; however, these exposure data sources may be relevant to future studies of human health. These studies were included for their identification of pollutants from other exposure media and for their use of exposure data sources relevant to human health (Buchholz et al., 2022; Ghetu et al., 2022; Liang et al., 2021; Messier et al., 2019; Nguyen et al., 2021; Ré et al., 2021; Solomon et al., 2021; Wan et al., 2021). Buchholz et al. (2022) used satellite‐measured CO to investigate seasonal pattern changes in wildfire emissions from wildfires occurring in the Pacific Northwest and the potential impact to air quality over larger regions of North America. Solomon et al. (2021) evaluated patterns of volatile organic compound contamination in drinking water systems following a destructive wildfire in northern California. Two studies used data from indoor air monitors to investigate wildfire smoke infiltration and indoor air quality (Liang et al., 2021; Nguyen et al., 2021). Liang et al. (2021) used crowdsourced, low‐cost sensor data from the PurpleAir monitoring network to assess PM2.5 infiltration ratios in residential buildings. Nguyen et al. (2021) used low‐cost fine particulate matter sensors from Air Quality Eggs to sample PM2.5, CO2, NO2, and VOCs in a large inpatient rehabilitation facility. Additionally, two studies used low‐density polyethylene passive samplers to assess indoor versus outdoor PAH concentrations in residential areas (Ghetu et al., 2022; Messier et al., 2019). Wan et al. (2021) analyzed fire ash and soil samples for trace elements and PAHs and looked at modeled respiratory impacts. Ré et al. (2021) prepared aqueous ash samples to mimic wildfire runoff and assessed potential dermatological effects by exposing human keratinocytes to the samples.
3.2. Summary of Health Data Sources
Seventy‐six articles included in this scoping review included health data sources, tabulated and described in Table 1. Administrative health data (36%) were the most frequently used health data source, followed by government databases (16%) and health surveys (18%) (see Table S4 in Supporting Information S1). Fewer studies used insurance claims data (7%) and surveillance data sources (11%). The frequencies of health data sources used by studies included in this review are shown in Figure 4 and described below.
Figure 4.

Health data sources (n = 76 articles). The size of each rectangle is proportional to the number of articles represented in each category. Articles used one or more health data sources. Article counts and percentages are shown in Table S4 in Supporting Information S1.
3.2.1. Administrative Health Data Sources
Researchers used various levels of administrative and electronic health record (EHR) data, such as emergency department (ED) visits (Aguilera, Corringham, Gershunov, Leibel, & Benmarhnia, 2021; Alman et al., 2016; Casey et al., 2021; CDC, 2008; Dohrenwend et al., 2013; Howard et al., 2021; Shusterman et al., 1993), clinic visits (Aguilera, Corringham, Gershunov, Leibel, & Benmarhnia, 2021; Howard et al., 2021), hospitalizations (Aguilera, Corringham, Gershunov, & Benmarhnia, 2021; Aguilera et al., 2020; Alman et al., 2016; Cançado et al., 2006; S. E. Cleland et al., 2021; DeFlorio‐Barker et al., 2019; Delfino et al., 2009; Gan et al., 2017; Heaney et al., 2022; Howard et al., 2021), and emergency medical services dispatches (H. J. Cleland et al., 2011; Dennekamp et al., 2015; Yao et al., 2020). Administrative health data are collected for administrative or billing purposes and these data capture encounters with the health system such as a visit to a physician's office or diagnostic procedures (Cadarette & Wong, 2015). These data sources were maintained by state and local health departments and individual hospitals or hospital networks. Authors used these data to assess health outcomes from a specific wildfire event or aggregated data over a longer study period to assess the effects of exposures from multiple wildfire events. Researchers commonly used International Classification of Disease Clinical Modification codes (22 of the 76 articles) to define specific health outcomes of interest from these administrative health data sources. State or national vital records registries were commonly used to obtain perinatal health outcomes, such as birth weight (Abdo et al., 2019; Cândido da Silva et al., 2014; Heft‐Neal et al., 2022; Holstius et al., 2012; Koman et al., 2019; Park et al., 2022; Requia et al., 2021).
3.2.2. Government Health Databases
Twelve studies (16% of the 76 articles) used government health databases to assess health outcomes such as cardiorespiratory hospital admissions, birth outcomes, social vulnerability, and mortality. Examples include the American Community Survey (Masri et al., 2021; Woo et al., 2020), Centers for Disease Control and Prevention (CDC) Wide‐ranging ONline Data for Epidemiologic Research (WONDER) (Fann et al., 2018; Koman et al., 2019; Y. Liu et al., 2021; Neumann et al., 2021; O’Neill et al., 2021), the National Health and Nutrition Examination Survey (NHANES) (Rappold et al., 2017), Behavioral Risk Factor Surveillance System (BRFSS) (Rappold et al., 2017), National Healthcare Cost and Utilization Project (Fann et al., 2018; O’Dell et al., 2021), Environmental Protection Agency (EPA) BenMap (S. E. Cleland et al., 2021; Fann et al., 2018; Neumann et al., 2021), and CDC Environmental Public Health Tracking Network (Koman et al., 2019). One study examined cancer outcomes using data from the Canadian Census Health and Environment Cohort (CanCHEC) that was linked to the Canadian Cancer Registry (Korsiak et al., 2022).
3.2.3. Primary Data Collection Tools and Real‐Time Health Data Sources
Researchers also collected health information using primary data collection methods such as surveys, biospecimen collection, and clinical tests. Most of these studies (18% of 76 articles) implemented surveys to collect self‐reported health symptoms or outcomes (Table S4 in Supporting Information S1). Examples include assessment of asthma symptoms, evacuation experiences, and mental health outcomes (Delfino et al., 2002; DeYoung et al., 2018; Haikerwal et al., 2021; Pazderka, Brown, Agyapong, et al., 2021; Pazderka, Brown, McDonald‐Harker, et al., 2021; Rodney et al., 2021). Additionally, two review articles were included for their description of literature using standardized screening tools and assessments for sleep and mental health outcomes (Isaac et al., 2021; To et al., 2021). Two studies conducted serum sampling (Delfino et al., 2010; Huttunen et al., 2012), and two used Smoke Sense, a mobile application developed by the EPA to collect self‐reported data on smoke experiences, health symptoms, and behaviors taken to reduce exposures to smoke (Postma et al., 2022; Rappold et al., 2019).
Primary data collection tools that were deployed during a wildfire event, or data sources that were made available to researchers during a wildfire event, were considered real‐time data sources. Nine studies used real‐time data sources to evaluate various health outcomes (CDC, 2008; Delfino et al., 2010; DeYoung et al., 2018; Haikerwal et al., 2021; Huttunen et al., 2012; Postma et al., 2022; Rappold et al., 2019; Rodney et al., 2021; Sugg et al., 2022). Five of these studies administered surveys during the wildfire event or exposure period of interest (DeYoung et al., 2018; Haikerwal et al., 2021; Postma et al., 2022; Rappold et al., 2019; Rodney et al., 2021). Only two of these studies used health data sources that were collected in real‐time and were also available to researchers during the wildfire events (CDC, 2008; Sugg et al., 2022). In one study, researchers used EHR data from CDC BioSense that were available in less than 24 hr from the patient visit (CDC, 2008). The second study used real‐time data from the Crisis Text Line, a mental health texting service administered by a global non‐profit organization, to assess the impact of wildfire events on youth and adolescent mental health (Sugg et al., 2022). Finally, two studies conducted serum sampling to study the effects of short‐term ambient air pollution exposures among study populations at higher risk for adverse health outcomes (Delfino et al., 2010; Huttunen et al., 2012). These two studies assessed ambient air pollution, but their methods are applicable to real‐time studies of wildfire exposures.
3.2.4. Insurance Claims Data and Surveillance Data Sources
Five studies (7% of 76 articles) used insurance claims data and these data sources were maintained by national (DeFlorio‐Barker et al., 2019; J. C. Liu, Wilson, Mickley, Dominici, et al., 2017; J. C. Liu, Wilson, Mickley, Ebisu, et al., 2017) or state/provincial government agencies (Gan et al., 2020; Mahsin et al., 2021). Eight articles used surveillance data to evaluate respiratory infections such as COVID‐19 (Ademu et al., 2022; Kiser et al., 2021; Naqvi et al., 2022; Sannigrahi et al., 2022; Schwarz et al., 2022; Zhou et al., 2021) and influenza (Landguth, et al., 2020). These studies used publicly available data from state health departments to obtain county‐level case counts of positive diagnoses of COVID‐19 and influenza (Ademu et al., 2022; Landguth et al., 2020). Additionally, a review article described emerging associations between wildfires and coccidioidomycosis (valley fever) using outbreak investigations and state surveillance data (Pearson et al., 2019).
3.2.5. Medication Data Sources
Ten studies utilized insurance claims data, medical records, pharmaceutical databases, and surveys to obtain information on medication dispensations, refills, and self‐reported medication use. These studies commonly assessed cardiovascular and respiratory impacts such as asthma and chronic obstructive pulmonary disease (Caamano‐Isorna et al., 2011; Delfino et al., 2002; Elliott et al., 2013; Gan et al., 2020; Haikerwal et al., 2021; Henderson et al., 2021; Howard et al., 2021; Huttunen et al., 2012; Rappold et al., 2019; Shusterman et al., 1993). In one study, researchers obtained asthma reliever medication information from statewide insurance claims data from the Oregon All Payer All Claims database (Gan et al., 2020). Three of these studies were conducted in Canada, and researchers used state or provincial‐level pharmaceutical databases (Elliott et al., 2013; Henderson et al., 2021; Howard et al., 2021). Another of these studies was conducted in Spain, and researchers used provincial‐level pharmaceutical data (Caamano‐Isorna et al., 2011). A California‐based study reviewed ED records using a standardized extraction form to obtain information on medication refills (Shusterman et al., 1993). Four of these studies gathered self‐reported medication information (Delfino et al., 2002; Haikerwal et al., 2021; Huttunen et al., 2012; Rappold et al., 2019).
3.2.6. Unique Health Data Sources
Other unique health data sources were identified with this scoping review, such as data from the Lumosity brain training game platform to assess the impact of wildfire smoke on cognitive performance (S. E. Cleland et al., 2022) and an analysis of GoogleTrends, Twitter, and SafeGraph cell phone data to assess behavioral responses to wildfires (Burke et al., 2022). Three animal studies were included for the potential to serve as surrogate data sources for human health impacts. One study conducted an indirect assessment of food security by surveying livestock producers on wildfire‐related impacts to production and herd health (O’Hara et al., 2021), and another article assessed the impact of wildfire smoke on cow milk production (Beaupied et al., 2022). Finally, one study assessed immune and lung function in adolescent rhesus macaque monkeys exposed to ambient wildfire smoke during infancy (Black et al., 2017).
3.3. Summary of Exposure Data Sources
Seventy‐seven articles identified in this scoping review included underlying exposure data sources. Researchers often used more than one data source to obtain exposure estimates, and the most common exposure data source was air monitoring data (52%), followed by satellite data (35%) and wildfire event data (38%). The frequencies of exposure data sources used by studies included in this review are shown in Figure 5 and described below.
Figure 5.
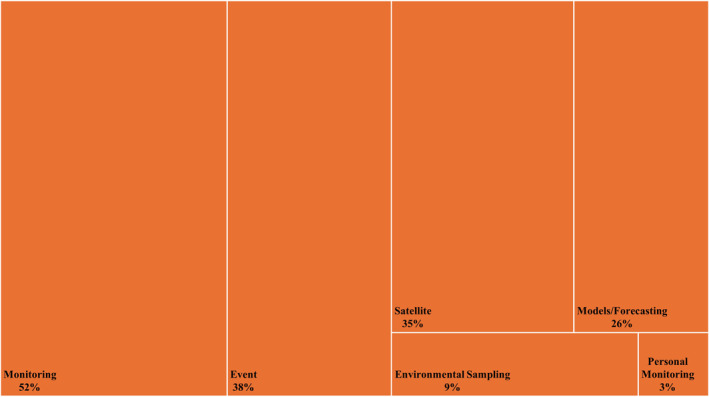
Exposure data sources (n = 77 articles). The size of each rectangle is proportional to the number of articles represented in each category. Articles used one or more exposure data sources. Article counts and percentages are shown in Table S5 in Supporting Information S1.
3.3.1. Air Quality Monitoring Data Sources
Forty studies (52%) used air quality monitoring data from national, state, and locally managed monitors (Figure 5). Data from the US EPA's Air Quality System and AirNow monitoring network were commonly used by researchers to evaluate exposures from wildfire smoke (Abdo et al., 2019; Ademu et al., 2022; Aguilera, Corringham, Gershunov, & Benmarhnia, 2021; Aguilera, Corringham, Gershunov, Leibel, & Benmarhnia, 2021; Alman et al., 2016; Beaupied et al., 2022; Casey et al., 2021; S. E. Cleland et al., 2022; DeFlorio‐Barker et al., 2019; Dohrenwend et al., 2013; Gan et al., 2017, 2020; Kiser et al., 2021; Landguth et al., 2020; Leibel et al., 2020; J. C. Liu, Wilson, Mickley, Dominici, et al., 2017; J. C. Liu, Wilson, Mickley, Ebisu, et al., 2017; Naqvi et al., 2022; O’Dell et al., 2021; O’Neill et al., 2021; Postma et al., 2022; Rappold et al., 2019; Sorensen et al., 2021; Zhou et al., 2021). Most studies included PM2.5 as the main exposure metric, but five studies utilized the air quality index and O3 data from these EPA data sources (Ademu et al., 2022; Beaupied et al., 2022; Dohrenwend et al., 2013; Rappold et al., 2019; Sorensen et al., 2021). Researchers also used data from state monitors like the California Air Resources Board (Black et al., 2017) and Washington's Air Monitoring Network (Y. Liu et al., 2021), and local monitoring networks like the San Diego Air Pollution Control District (Delfino et al., 2002). In three studies, researchers used crowdsourced, low‐cost sensor data from the PurpleAir monitoring network (Burke et al., 2022; S. E. Cleland et al., 2022; Liang et al., 2021).
3.3.2. Satellite Remote Sensing Data Sources
Twenty‐seven studies (35%) used satellite remote sensing data for both quantitative and qualitative estimates of wildfire smoke exposure (Figure 5). Quantitative estimates relied on aerosol optical depth, the amount of scattering and absorption of sunlight by aerosol particles in the atmospheric column, measured by several satellites, including National Aeronautics and Space Administration (NASA) Moderate Resolution Imaging Spectroradiometer (MODIS) satellite instruments (S. E. Cleland et al., 2021; Delfino et al., 2009; Elliott et al., 2013; Gan et al., 2017; Landguth et al., 2020; O’Neill et al., 2021). Qualitative estimates were obtained using NOAA HMS smoke polygons, where trained analysts drew polygons around spatial regions with visible smoke (Aguilera, Corringham, Gershunov, & Benmarhnia, 2021; Aguilera, Corringham, Gershunov, Leibel, & Benmarhnia, 2021; Aguilera et al., 2020; Beaupied et al., 2022; Burke et al., 2022; Casey et al., 2021; S. E. Cleland et al., 2022; Fann et al., 2018; Gan et al., 2017; Heft‐Neal et al., 2022; Messier et al., 2019; O’Dell et al., 2021; Rappold et al., 2019; Schwarz et al., 2022; Sorensen et al., 2021; Zhou et al., 2021).
3.3.3. Models and Forecasting Systems
Twenty studies (26%) used a variety of models and forecasting systems to assess PM2.5 concentrations (Figure 5). Examples include the Community Multiscale Air Quality Modeling System (CMAQ) (S. E. Cleland et al., 2021; DeFlorio‐Barker et al., 2019; Fann et al., 2018; Koman et al., 2019; O’Neill et al., 2021; Rappold et al., 2017), Air Indicator Receptor for Public Awareness and Community Tracking (AIRPACT‐4) (Doubleday et al., 2020), Bluesky Framework (Koman et al., 2019; O’Neill et al., 2021), and the Hybrid Single‐Particle Lagrangian Integrated Trajectory (HYSPLIT) model (Hutchinson et al., 2018). Many studies also integrated meteorological data when constructing models. These meteorological data were obtained from a variety of sources, ranging from NOAA National Centers for Environmental Information (NCEI) (Ademu et al., 2022; Heaney et al., 2022; J. C. Liu Wilson, Mickley, Dominici et al., 2017) to local weather stations (Kiser et al., 2020, 2021).
3.3.4. Wildfire Event Data Sources and Environmental Sampling
Twenty‐nine studies (38%) used wildfire event data. Data sources included the California Fire and Resource Assessment Program (FRAP) (Aguilera, Corringham, Gershunov, & Benmarhnia, 2021; Aguilera et al., 2020; Leibel et al., 2020; Masri et al., 2021), US Geological Survey (USGS) GeoMAC (DeFlorio‐Barker et al., 2019; Rappold et al., 2017; Sugg et al., 2022), the Global Fire Emissions Database (Li et al., 2021; J.C., Liu, Wilson, Mickley, Dominici, et al., 2017; J. C. Liu, Wilson, Mickley, Ebisu, et al., 2017; Neumann et al., 2021), and the National Center for Atmospheric Research Fire Inventory (FINN) (Alman et al., 2016). Researchers commonly used these data to define exposure windows as smoke days versus non‐smoke days. Sixteen studies used spatial proximity to a wildfire event or evacuation perimeters as a proxy exposure method rather than assessing a specific pollutant. Seven of these studies used surveys to obtain self‐reported information on general proximity to fire events and evacuation status as an exposure metric (Haikerwal et al., 2021; Hyde et al., 2021; Masri et al., 2021; O’Hara et al., 2021; Pazderka, Brown, Agyapong, et al., 2021; Pazderka, Brown, McDonald‐Harker, et al., 2021; Rodney et al., 2021). Two studies utilized personal air monitors or photometers to collect particle samples as measures of personal exposures among older adult populations, one in Los Angeles, CA (Delfino et al., 2010) and one in Finland (Huttunen et al., 2012).
4. Discussion
This scoping review identified an evolving body of research (n = 69) directly linking environmental exposure and health data sources to study the impact of wildfires on human health. An additional 14 articles were included for their use of novel data sources and for their potential relevance to human health outcomes. Most studies identified in the review of articles studying human health and wildfire‐related exposures (n = 69) investigated respiratory (54%) and/or cardiovascular (26%) health outcomes. There were fewer studies researching other health endpoints such as perinatal outcomes (15%), mental health (10%), injuries (3%), and cancer (1%). Administrative health data (36% of 76 articles) were the most common health data source, followed by government databases (16% of 76 articles), and health surveys (18% of 76 articles).
Wildfire smoke exposures, and particularly wildfire smoke pollutants (e.g., PM2.5, PM10, NO x , O3), were the most common exposure metrics identified, and of these pollutants, PM2.5 was evaluated in 70% of the studies of human health and wildfire‐related exposures (n = 69). Research has largely focused on various airborne measures of PM2.5 from wildfire smoke. This focus may be due to evidence that PM2.5 has been more consistently linked with adverse health outcomes than larger PM10 (J. C. Liu et al., 2015). Most articles identified in the full review used more than one data source to evaluate exposures. Of these data sources, air monitoring data was the most common (52% of 77 articles), followed by wildfire event data (38% of 77 articles) and satellite data (35% of 77 articles). We identified seven exposure science studies and one toxicology study that investigated other pollutants (e.g., VOCs, PAHs) and characterized pollutants from other exposure media (e.g., drinking water, soil). There remains a vital need for further research of exposure assessments inclusive of ingestion and dermal routes, as well characterization of the complex smoke mixtures beyond particulate estimates, to fully understand the impact of wildfires on human health.
This scoping review applied an innovative approach to not only review the literature for exposure and health associations but to examine specific data resources used in these studies. This comprehensive evaluation of the research landscape and description of available data resources informs our discussion of specific strengths and weaknesses and recommendations for notable paths forward. Several important gaps and opportunities to enhance data linkages to further advance research and disaster response emerged.
First, many of these studies relied upon historical health data, and only nine studies used real‐time or near real‐time health data. This may be due to lack of availability, longer lag times in data collection, and additional privacy and security measures required for health data. Many studies relied upon administrative health data from EHR or vital statistics registries that may be available to the research community years after the wildfire event. Only seven studies used surveillance data, which typically have shorter lag times compared to EHR and can provide insights on early health indicators and identify vulnerable populations. One opportunity to overcome these barriers is to establish relationships with local and state syndromic surveillance system administrators and to partner with these organizations in wildfire response efforts to collect and harmonize surveillance data at EDs and other health care sites. These data would inform both real‐time and future response efforts.
Notably, only four studies collected real‐time health outcomes data along with real‐time exposure data (Delfino et al., 2010; Huttunen et al., 2012; Postma et al., 2022; Rappold et al., 2019). Several studies collected timely health data using surveys and a mobile application that was part of a citizen science approach (Delfino et al., 2002; DeYoung et al., 2018; Haikerwal et al., 2021; Hyde et al., 2021; Pazderka, Brown, Agyapong, et al., 2021; Pazderka, Brown, McDonald‐Harker, et al., 2021; Postma et al., 2022; Rappold et al., 2019; Rodney et al., 2021). These studies evaluated health symptoms and mental health outcomes and included vulnerable populations such as participants who had to evacuate during wildfire events. Interestingly, one study used real‐time data from the Crisis Text Line to evaluate mental health proxies (Sugg et al., 2022). These data have the potential to capture real‐time population‐level mental health impacts during wildfire events. Primary data collection can be more expensive compared to accessing EHR or vital records, but these data are available soon after a wildfire event, and they may describe acute symptoms and provide important opportunities for understanding important health effects that would not be captured in EHR. While our scoping review did not compare the impact of results from studies relying on different data sources, primary data collection tools and surveillance systems are designed for public health purposes; therefore, these data sources can be used to answer specific research questions, more accurately characterize health conditions, and better inform timely public health preparedness and response compared to studies relying on administrative health data that are often collected for billing purposes and analyzed years after a wildfire event.
Health data sources lacked spatial and temporal coverage to study health outcomes with longer latency periods. Some researchers used national government data sources like NHANES, CDC WONDER, and BRFSS, which provide reasonable spatial coverage but are often cross sectional and cannot be linked to follow participants over multiple study years. Three studies (DeFlorio‐Barker et al., 2019; J. C. Liu, Wilson, Mickley, Dominici, et al., 2017; J. C. Liu, Wilson, Mickley, Ebisu, et al., 2017) used Medicare data, which provide greater spatial coverage across the US, but relies on claims data that have certain limitations compared to surveys and EHR. Many of the studies identified in this scoping review relied upon a combination of state and local hospital network data that can be harder to merge across health systems but allows for investigation of outcomes at a shorter frequency compared to annual estimates from current government data sources. Records can be linked when the health system captures the eligible study population and includes the appropriate linkage information. For example, Aguilera, Corringham, Gershunov, Leibel, and Benmarhnia (2021) examined associations between wildfire smoke exposures and pediatric visits for respiratory outcomes between 2011 and 2017 in San Diego County, California. Pediatric ED and urgent care respiratory visit data were obtained from a hospital network that provided medical care for 91% of the county's hospitalized children. Primary health outcomes were assessed using chief complaints, including difficulty breathing, respiratory distress, wheezing, asthma, or cough. These health data were linked with wildfire‐specific fine particulate matter (PM2.5) modeled as daily concentrations at the zip code level. This study examined a longer study period, 7 years, and a larger geographic area compared to previous studies (Aguilera, Corringham, Gershunov, Leibel, & Benmarhnia, 2021).
Studies using health data from existing, prospective observational studies or health registries were sparse. In one study, researchers used the 1996 CanCHEC that followed participants for cancer incidence and mortality over a 19‐year period (Korsiak et al., 2022). Cancer registry data may provide good spatial and temporal coverage for US populations when these data include residential information that can be used to reconstruct exposure histories. Notably, O’Neill et al. (2021) built on prior air pollution research that linked PM2.5 data with health data from the Reasons for Geographic and Racial Differences in Stroke Study; a national, population‐based, longitudinal study of 30,000 African American and white adults aged 45 years and older (Al‐Hamdan et al., 2009, 2014). O’Neill et al. (2021) applied this methodology to their research estimating the number of deaths attributable to wildfire smoke from the October 2017 northern California wildfires. While the study by Al‐Hamdan et al. (2014) did not focus specifically on wildfires, their methods for linking PM2.5 estimates to a national cohort study have been applied to wildfire research, demonstrating the ability to perform exposure data linkages with prospective observational studies.
This review also highlights the absence of wildfire‐specific public health registries. Registries serve as a foundation to collect baseline information in the event of a disaster and to monitor health outcomes over time. Registries have been created in response to a variety of events, including Hiroshima and Nagasaki, the Three Mile Island incident, the Chernobyl disaster, the Oklahoma City bombing, the 2001 World Trade Center attacks, and Hurricane Harvey (Miranda et al., 2021). While launching a registry can take a great deal of coordination, establishing a registry can provide valuable insights into long‐term, population‐level impacts of disasters. The creation of a wildfire‐specific registry could help to build the evidence base and enhance our understanding of wildfire impacts over time. The National Institute of Environmental Health Sciences (NIEHS) Disaster Research Response Program (DR2) has created a tool to help expedite the Institutional Review Board approval process for registry studies and recontact studies (Miller et al., 2016). The Rapid Acquisition of Pre‐ and Post‐Incident Disaster Data (RAPIDD) Protocol Designer is a free online tool researchers can use to build a registry protocol with pre‐approved, validated questionnaires, protocol language, and resources (NIEHS, 2023).
Wildfire smoke exposure data sources are a rich source of information for wildfire researchers because they are publicly available in real‐time or near real‐time, provide good temporal and spatial coverage, and they do not require the same privacy and security protections that are encountered with health data. Many of the epidemiology studies included in this scoping review analyzed measures of PM2.5 concentrations. Most wildfire exposure data focused on particulate pollutants and did not capture the complex mixture of gaseous pollutants or hazardous pollutants, like PAHs, that have been detected in wildfire smoke (EPA, 2022). One study included a measure of gas‐phase hazardous air pollutants (HAPs) in a health impact analysis (O’Dell et al., 2021). HAPs were estimated using observations from the Western Wildfire Experiment on Cloud Chemistry, Aerosol Absorption, and Nitrogen (WE‐CAN), an aircraft‐based field campaign that sampled lofted smoke plumes from large wildfires in the western US during the summer of 2018 (O’Dell et al., 2021). Despite only one study reporting trace elements, toxic metal contaminants may be an important exposure measure to capture, as evidenced by a report from the California Air Resources Board that showed lead concentrations spiked to very high levels in WUI fire smoke during the 2018 Camp Fire in northern California (CARB, 2021).
While many epidemiology studies have focused on PM2.5, exposure studies have examined wildfire smoke to assess other pollutants and to investigate the impact of wildfire smoke on indoor air quality. For instance, two exposure studies utilized stationary monitors to evaluate PAH concentrations from indoor and outdoor air before, during, and after wildfires (Ghetu et al., 2022; Messier et al., 2019). In another exposure study, low‐cost sensors were used to assess CO2, NO2, and VOCs from indoor and outdoor air in a healthcare setting, but these concentrations were not linked to health outcomes (Nguyen et al., 2021). These exposure studies deployed stationary monitors or low‐cost sensors that are more costly for researchers compared to data obtained from existing monitoring networks or satellites, but the measurements provide valuable information on other wildfire smoke contaminants and infiltration. No studies in this review linked indoor air quality to health outcomes. Interestingly, one exposure study (Liang et al., 2021) utilized the open‐source PurpleAir network data to study infiltration of PM2.5 during wildfires. This method could be further developed to study the potential health effects. Enhancing or developing new data sources that capture the complex mixture of WUI and wildfire smoke will further advance wildfire health research.
Lastly, none of the articles included in this review studied wildfire exposure and health associations for non‐air pathways such as soil, household dust, food, or water. Researchers have identified pollutants with potential health considerations such as VOCs in water samples (Solomon et al., 2021), and PAHs in ash samples (Wan et al., 2021), but such exposures were not linked to population‐level health data. Expanding exposure data sources beyond air to water, soil, vegetable gardens, and indoor dust would provide an opportunity to better understand the impact of exposure to other toxicants through ingestion and dermal exposure routes.
There are a few limitations with this scoping review. Due to the inherent methodology of scoping reviews, the quality or strengths of associations of these studies were not assessed. The focus of this review was on metrics from the US and North America. While 11 articles (Caamano‐Isorno et al., 2011; Cândido da Silva et al., 2014; Cançado et al., 2006; H. J. Cleland et al., 2011; Dennekamp et al., 2015; Haikerwal et al., 2021; Huttunen et al., 2012; Li et al., 2021; Ré et al., 2021; Requia et al., 2021; Rodney et al., 2021) from other geographic regions were included, this restriction limits generalizability to other regions and low‐ and middle‐income countries.
5. Conclusions
As the frequency and intensity of wildfires increases, there is a growing need to leverage multiple data sources to rapidly respond to public health concerns. Although this scoping review identified many existing exposure and health data sources that can be used for research on the health impacts of wildfires, a number of these data resources are not readily available to researchers. For example, administrative and EHR data were the most common health data sources; however, data access is not free and requires contractual agreements. Therefore, addressing the immediate need of improving access to these data resources would greatly enhance timely health investigations and our understanding of real‐time exposures and associated health responses, as well as opportunities to identify biomarkers of exposure and effect. There are also opportunities for advancing the available data, including capitalizing on newer modes of data collection such as citizen science or crowdsourced data, new modeling methods, and expanding the focus of exposure assessments beyond air pollutants to water and soil contaminants from wildfires. Investigation of results from studies using real‐time and expanded data sources will continue to advance these data resources and wildfire and health research. Ultimately, the goal of improving data collection and access is more accurate characterization of both the exposures and health outcomes associated with wildfires. Using real‐time data, assessing all exposure routes, and incorporating novel modeling techniques and data streams are examples of some key strategies to achieve that goal. This approach to assessing wildfire health outcomes inclusive of the specific health and exposure data sources used to underpin the research studies provides a framework to help the research community understand the use and value of various environmental and health data sources. Addressing many of the gaps identified in this scoping review would be valuable to other areas of disaster research and could help shape a framework that can be applied to other pressing public health issues.
Conflict of Interest
The authors declare no conflicts of interest relevant to this study.
Supporting information
Supporting Information S1
Acknowledgments
This work was supported by the National Institute of Environmental Health Sciences (NIEHS) Clinical Research Branch, Contract # HHSN273201600002I.
Barkoski, J. , Van Fleet, E. , Liu, A. , Ramsey, S. , Kwok, R. K. , & Miller, A. K. (2024). Data linkages for wildfire exposures and human health studies: A scoping review. GeoHealth, 8, e2023GH000991. 10.1029/2023GH000991
Data Availability Statement
This review paper did not analyze any new data. The list of studies reviewed can be found in Table 1. Only results published in identified previous studies were used. The included studies are provided in the reference list.
References
- Abdo, M. , Ward, I. , O’Dell, K. , Ford, B. , Pierce, J. R. , Fischer, E. V. , & Crooks, J. L. (2019). Impact of wildfire smoke on adverse pregnancy outcomes in Colorado, 2007–2015 [Dataset]. International Journal of Environmental Research and Public Health, 16(19), 3720. 10.3390/ijerph16193720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ademu, L. O. , Gao, J. , Thompson, O. P. , & Ademu, L. A. (2022). Impact of short‐term air pollution on respiratory infections: A time‐series analysis of COVID‐19 cases in California during the 2020 wildfire season [Dataset]. International Journal of Environmental Research and Public Health, 19(9), 5057. 10.3390/ijerph19095057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguilera, R. , Corringham, T. , Gershunov, A. , & Benmarhnia, T. (2021). Wildfire smoke impacts respiratory health more than fine particles from other sources: Observational evidence from southern California [Dataset]. Nature Communications, 12(1), 1493. 10.1038/s41467-021-21708-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguilera, R. , Corringham, T. , Gershunov, A. , Leibel, S. , & Benmarhnia, T. (2021). Fine particles in wildfire smoke and pediatric respiratory health in California [Dataset]. Pediatrics, 147(4), e2020027128. 10.1542/peds.2020-027128 [DOI] [PubMed] [Google Scholar]
- Aguilera, R. , Hansen, K. , Gershunov, A. , Ilango, S. D. , Sheridan, P. , & Benmarhnia, T. (2020). Respiratory hospitalizations and wildfire smoke: A spatiotemporal analysis of an extreme firestorm in San Diego county, California [Dataset]. Environmental Epidemiology, 4(5), e114. 10.1097/ee9.0000000000000114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al‐Hamdan, M. Z. , Crosson, W. L. , Economou, S. A. , Estes, M. G., Jr. , Estes, S. M. , Hemmings, S. N. , et al. (2014). Environmental public health applications using remotely sensed data. Geocarto International, 29(1), 85–98. 10.1080/10106049.2012.715209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al‐Hamdan, M. Z. , Crosson, W. L. , Limaye, A. S. , Rickman, D. L. , Quattrochi, D. A. , Estes, M. G., Jr. , et al. (2009). Methods for characterizing fine particulate matter using ground observations and remotely sensed data: Potential use for environmental public health surveillance. Journal of the Air & Waste Management Association, 59(7), 865–881. 10.3155/1047-3289.59.7.865 [DOI] [PubMed] [Google Scholar]
- Alman, B. L. , Pfister, G. , Hao, H. , Stowell, J. , Hu, X. , Liu, Y. , & Strickland, M. J. (2016). The association of wildfire smoke with respiratory and cardiovascular emergency department visits in Colorado in 2012: A case crossover study [Dataset]. Environmental Health, 15(1), 64. 10.1186/s12940-016-0146-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaupied, B. L. , Martinez, H. , Martenies, S. , McConnel, C. S. , Pollack, I. B. , Giardina, D. , et al. (2022). Cows as canaries: The effects of ambient air pollution exposure on milk production and somatic cell count in dairy cows [Dataset]. Environmental Research, 207, 112197. 10.1016/j.envres.2021.112197 [DOI] [PubMed] [Google Scholar]
- Black, C. , Gerriets, J. E. , Fontaine, J. H. , Harper, R. W. , Kenyon, N. J. , Tablin, F. , et al. (2017). Early Life wildfire smoke exposure is associated with immune dysregulation and lung function decrements in adolescence [Dataset]. American Journal of Respiratory Cell and Molecular Biology, 56(5), 657–666. 10.1165/rcmb.2016-0380OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchholz, R. R. , Park, M. , Worden, H. M. , Tang, W. , Edwards, D. P. , Gaubert, B. , et al. (2022). New seasonal pattern of pollution emerges from changing North American wildfires [Dataset]. Nature Communications, 13(1), 2043. 10.1038/s41467-022-29623-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke, M. , Heft‐Neal, S. , Li, J. , Driscoll, A. , Baylis, P. , Stigler, M. , et al. (2022). Exposures and behavioural responses to wildfire smoke [Dataset]. Nature Human Behaviour, 6(10), 1351–1361. 10.1038/s41562-022-01396-6 [DOI] [PubMed] [Google Scholar]
- Caamano‐Isorna, F. , Figueiras, A. , Sastre, I. , Montes‐Martínez, A. , Taracido, M. , & Piñeiro‐Lamas, M. (2011). Respiratory and mental health effects of wildfires: An ecological study in Galician municipalities (north‐west Spain) [Dataset]. Environmental Health, 10(1), 48. 10.1186/1476-069X-10-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadarette, S. M. , & Wong, L. (2015). An introduction to health care administrative data. Canadian Journal of Hospital Pharmacy, 68(3), 232–237. 10.4212/cjhp.v68i3.1457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cançado, J. E. D. , Saldiva, P. H. N. , Pereira, L. A. A. , Lara, L. B. L. S. , Artaxo, P. , Martinelli, L. A. , et al. (2006). The impact of sugar cane–burning emissions on the respiratory system of children and the elderly [Dataset]. Environmental Health Perspectives, 114(5), 725–729. 10.1289/ehp.848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cândido da Silva, A. M. , Moi, G. P. , Mattos, I. E. , & Hacon, S. d. S. (2014). Low birth weight at term and the presence of fine particulate matter and carbon monoxide in the Brazilian Amazon: A population‐based retrospective cohort study [Dataset]. BMC Pregnancy and Childbirth, 14(1), 309. 10.1186/1471-2393-14-309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CARB . (2021). Camp fire air quality data analysis (pp. 21–30). Retrieved from https://ww2.arb.ca.gov/news/new‐analysis‐shows‐spikes‐metal‐contaminants‐including‐lead‐2018‐camp‐fire‐wildfire‐smoke#:~:text=The%20document%2C%20published%20today%2C%20shows,spiked%20for%20about%2024%20hours
- Casey, J. A. , Kioumourtzoglou, M.‐A. , Elser, H. , Walker, D. , Taylor, S. , Adams, S. , et al. (2021). Wildfire particulate matter in Shasta County, California and respiratory and circulatory disease‐related emergency department visits and mortality, 2013–2018 [Dataset]. Environmental Epidemiology, 5(1), e124. 10.1097/ee9.0000000000000124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC . (2008). Monitoring health effects of wildfires using the BioSense system—San Diego County, California, October 2007 [Dataset]. MMWR. Morbidity and mortality weekly report, 57(27), 741–744. Retrieved from https://www.cdc.gov/mmwr/PDF/wk/mm5727.pdf [PubMed] [Google Scholar]
- Choi, A. , & Shveda, K. (2023). Wildfires in Canada led to dangerous air quality in parts of the US for the first time. See the affected areas. CNN. Retrieved from https://www.cnn.com/2023/09/17/us/air‐quality‐wildfire‐pollution‐allergy‐dg/index.html [Google Scholar]
- Cleland, H. J. , Proud, D. , Spinks, A. , & Wasiak, J. (2011). Multidisciplinary team response to a mass burn casualty event: Outcomes and implications [Dataset]. Medical Journal of Australia, 194(11), 589–593. 10.5694/j.1326-5377.2011.tb03110.x [DOI] [PubMed] [Google Scholar]
- Cleland, S. E. , Serre, M. L. , Rappold, A. G. , & West, J. J. (2021). Estimating the acute health impacts of fire‐originated PM2.5 exposure during the 2017 California wildfires: Sensitivity to choices of inputs [Dataset]. GeoHealth, 5(7), e2021GH000414. 10.1029/2021GH000414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleland, S. E. , Wyatt, L. H. , Wei, L. , Paul, N. , Serre, M. L. , West, J. J. , et al. (2022). Short‐term exposure to wildfire smoke and PM2.5 and cognitive performance in a brain‐training game: A longitudinal study of U.S. Adults [Dataset]. Environmental Health Perspectives, 130(6), 067005. 10.1289/EHP10498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeFlorio‐Barker, S. , Crooks, J. , Reyes, J. , & Rappold, A. G. (2019). Cardiopulmonary effects of fine particulate matter exposure among older adults, during wildfire and non‐wildfire periods, in the United States 2008–2010 [Dataset]. Environmental Health Perspectives, 127(3), 037006. 10.1289/EHP3860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delfino, R. J. , Brummel, S. , Wu, J. , Stern, H. , Ostro, B. , Lipsett, M. , et al. (2009). The relationship of respiratory and cardiovascular hospital admissions to the southern California wildfires of 2003 [Dataset]. Occupational and Environmental Medicine, 66(3), 189–197. 10.1136/oem.2008.041376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delfino, R. J. , Staimer, N. , Tjoa, T. , Arhami, M. , Polidori, A. , Gillen, D. L. , et al. (2010). Associations of primary and secondary organic aerosols with airway and systemic inflammation in an elderly panel cohort [Dataset]. Epidemiology, 21(6), 892–902. 10.1097/ede.0b013e3181f20e6c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delfino, R. J. , Zeiger, R. S. , Seltzer, J. M. , Street, D. H. , & McLaren, C. E. (2002). Association of asthma symptoms with peak particulate air pollution and effect modification by anti‐inflammatory medication use [Dataset]. Environmental Health Perspectives, 110(10), A607–A617. 10.1289/ehp.021100607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennekamp, M. , Straney, L. D. , Erbas, B. , Abramson, M. J. , Keywood, M. , Smith, K. , et al. (2015). Forest fire smoke exposures and out‐of‐hospital cardiac arrests in Melbourne, Australia: A case‐crossover study [Dataset]. Environmental Health Perspectives, 123(10), 959–964. 10.1289/ehp.1408436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennison, P. E. , Brewer, S. C. , Arnold, J. D. , & Moritz, M. A. (2014). Large wildfire trends in the western United States, 1984–2011. Geophysical Research Letters, 41(8), 2928–2933. 10.1002/2014GL059576 [DOI] [Google Scholar]
- DeYoung, S. E. , Chase, J. , Branco, M. P. , & Park, B. (2018). The effect of mass evacuation on infant feeding: The case of the 2016 Fort McMurray wildfire [Dataset]. Maternal and Child Health Journal, 22(12), 1826–1833. 10.1007/s10995-018-2585-z [DOI] [PubMed] [Google Scholar]
- Dodd, W. , Scott, P. , Howard, C. , Scott, C. , Rose, C. , Cunsolo, A. , & Orbinski, J. (2018). Lived experience of a record wildfire season in the Northwest Territories, Canada [Dataset]. Canadian Journal of Public Health, 109(3), 327–337. 10.17269/s41997-018-0070-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dohrenwend, P. B. , Le, M. V. , Bush, J. A. , & Thomas, C. F. (2013). The impact on emergency department visits for respiratory illness during the Southern California wildfires [Dataset]. Western Journal of Emergency Medicine, 14(2), 79–84. 10.5811/westjem.2012.10.6917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doubleday, A. , Schulte, J. , Sheppard, L. , Kadlec, M. , Dhammapala, R. , Fox, J. , & Busch Isaksen, T. (2020). Mortality associated with wildfire smoke exposure in Washington state, 2006–2017: A case‐crossover study [Dataset]. Environmental Health, 19(1), 4. 10.1186/s12940-020-0559-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott, C. T. , Henderson, S. B. , & Wan, V. (2013). Time series analysis of fine particulate matter and asthma reliever dispensations in populations affected by forest fires [Dataset]. Environmental Health, 12(1), 11. 10.1186/1476-069X-12-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EPA . (2022). Why wildfire smoke is a health concern. Retrieved from https://www.epa.gov/wildfire‐smoke‐course/why‐wildfire‐smoke‐health‐concern
- EPA . (2023). Maui wildfires. Retrieved from https://www.epa.gov/maui‐wildfires
- Fann, N. , Alman, B. , Broome, R. A. , Morgan, G. G. , Johnston, F. H. , Pouliot, G. , & Rappold, A. G. (2018). The health impacts and economic value of wildland fire episodes in the U.S.: 2008–2012 [Dataset]. Science of the Total Environment, 610–611, 802–809. 10.1016/j.scitotenv.2017.08.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan, R. W. , Ford, B. , Lassman, W. , Pfister, G. , Vaidyanathan, A. , Fischer, E. , et al. (2017). Comparison of wildfire smoke estimation methods and associations with cardiopulmonary‐related hospital admissions [Dataset]. GeoHealth, 1(3), 122–136. 10.1002/2017GH000073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan, R. W. , Liu, J. , Ford, B. , O’Dell, K. , Vaidyanathan, A. , Wilson, A. , et al. (2020). The association between wildfire smoke exposure and asthma‐specific medical care utilization in Oregon during the 2013 wildfire season [Dataset]. Journal of Exposure Science and Environmental Epidemiology, 30(4), 618–628. 10.1038/s41370-020-0210-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghetu, C. C. , Rohlman, D. , Smith, B. W. , Scott, R. P. , Adams, K. A. , Hoffman, P. D. , & Anderson, K. A. (2022). Wildfire impact on indoor and outdoor PAH air quality [Dataset]. Environmental Science & Technology, 56(14), 10042–10052. 10.1021/acs.est.2c00619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haikerwal, A. , Doyle, L. W. , Wark, J. D. , Irving, L. , & Cheong, J. L. Y. (2021). Wildfire smoke exposure and respiratory health outcomes in young adults born extremely preterm or extremely low birthweight [Dataset]. Environmental Research, 197, 111159. 10.1016/j.envres.2021.111159 [DOI] [PubMed] [Google Scholar]
- Heaney, A. , Stowell, J. D. , Liu, J. C. , Basu, R. , Marlier, M. , & Kinney, P. (2022). Impacts of fine particulate matter from wildfire smoke on respiratory and cardiovascular health in California [Dataset]. GeoHealth, 6(6), e2021GH000578. 10.1029/2021GH000578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heft‐Neal, S. , Driscoll, A. , Yang, W. , Shaw, G. , & Burke, M. (2022). Associations between wildfire smoke exposure during pregnancy and risk of preterm birth in California [Dataset]. Environmental Research, 203, 111872. 10.1016/j.envres.2021.111872 [DOI] [PubMed] [Google Scholar]
- Henderson, S. B. , Morrison, K. T. , McLean, K. E. , Ding, Y. , Yao, J. , Shaddick, G. , & Buckeridge, D. L. (2021). Staying ahead of the epidemiologic curve: Evaluation of the British Columbia asthma prediction system (BCAPS) during the unprecedented 2018 wildfire season [Dataset]. Frontiers in Public Health, 9, 499309. 10.3389/fpubh.2021.499309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holm, S. M. , Miller, M. D. , & Balmes, J. R. (2021). Health effects of wildfire smoke in children and public health tools: A narrative review. Journal of Exposure Science and Environmental Epidemiology, 31(1), 1–20. 10.1038/s41370-020-00267-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holstius, D. M. , Reid, C. E. , Jesdale, B. M. , & Morello‐Frosch, R. (2012). Birth weight following pregnancy during the 2003 Southern California wildfires [Dataset]. Environmental Health Perspectives, 120(9), 1340–1345. 10.1289/ehp.1104515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard, C. , Rose, C. , Dodd, W. , Kohle, K. , Scott, C. , Scott, P. , et al. (2021). SOS! Summer of smoke: A retrospective cohort study examining the cardiorespiratory impacts of a severe and prolonged wildfire season in Canada’s high subarctic [Dataset]. BMJ Open, 11(2), e037029. 10.1136/bmjopen-2020-037029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchinson, J. A. , Vargo, J. , Milet, M. , French, N. H. F. , Billmire, M. , Johnson, J. , & Hoshiko, S. (2018). The San Diego 2007 wildfires and Medi‐Cal emergency department presentations, inpatient hospitalizations, and outpatient visits: An observational study of smoke exposure periods and a bidirectional case‐crossover analysis [Dataset]. PLoS Medicine, 15(7), e1002601. 10.1371/journal.pmed.1002601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huttunen, K. , Siponen, T. , Salonen, I. , Yli‐Tuomi, T. , Aurela, M. , Dufva, H. , et al. (2012). Low‐level exposure to ambient particulate matter is associated with systemic inflammation in ischemic heart disease patients [Dataset]. Environmental Research, 116, 44–51. 10.1016/j.envres.2012.04.004 [DOI] [PubMed] [Google Scholar]
- Hyde, A. , Verstraeten, B. S. E. , Olson, J. K. , King, S. , Brémault‐Phillips, S. , & Olson, D. M. (2021). The Fort McMurray Mommy Baby study: A protocol to reduce maternal stress due to the 2016 Fort McMurray wood Buffalo, Alberta, Canada wildfire [Dataset]. Frontiers in Public Health, 9, 601375. 10.3389/fpubh.2021.601375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaac, F. , Toukhsati, S. R. , Di Benedetto, M. , & Kennedy, G. A. (2021). A systematic review of the impact of wildfires on sleep disturbances [Dataset]. International Journal of Environmental Research and Public Health, 18(19), 10152. 10.3390/ijerph181910152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain, P. , Castellanos‐Acuna, D. , Coogan, S. C. P. , Abatzoglou, J. T. , & Flannigan, M. D. (2022). Observed increases in extreme fire weather driven by atmospheric humidity and temperature. Nature Climate Change, 12(1), 63–70. 10.1038/s41558-021-01224-1 [DOI] [Google Scholar]
- Kiser, D. , Elhanan, G. , Metcalf, W. J. , Schnieder, B. , & Grzymski, J. J. (2021). SARS‐CoV‐2 test positivity rate in Reno, Nevada: Association with PM2.5 during the 2020 wildfire smoke events in the western United States [Dataset]. Journal of Exposure Science and Environmental Epidemiology, 31(5), 797–803. 10.1038/s41370-021-00366-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiser, D. , Metcalf, W. J. , Elhanan, G. , Schnieder, B. , Schlauch, K. , Joros, A. , et al. (2020). Particulate matter and emergency visits for asthma: A time‐series study of their association in the presence and absence of wildfire smoke in Reno, Nevada, 2013–2018 [Dataset]. Environmental Health, 19(1), 92. 10.1186/s12940-020-00646-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koman, P. D. , Billmire, M. , Baker, K. R. , de Majo, R. , Anderson, F. J. , Hoshiko, S. , et al. (2019). Mapping modeled exposure of wildland fire smoke for human health studies in California [Dataset]. Atmosphere, 10(6), 308. 10.3390/atmos10060308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korsiak, J. , Pinault, L. , Christidis, T. , Burnett, R. T. , Abrahamowicz, M. , & Weichenthal, S. (2022). Long‐term exposure to wildfires and cancer incidence in Canada: A population‐based observational cohort study [Dataset]. The Lancet Planetary Health, 6(5), e400–e409. 10.1016/S2542-5196(22)00067-5 [DOI] [PubMed] [Google Scholar]
- Landguth, E. L. , Holden, Z. A. , Graham, J. , Stark, B. , Mokhtari, E. B. , Kaleczyc, E. , et al. (2020). The delayed effect of wildfire season particulate matter on subsequent influenza season in a mountain west region of the USA [Dataset]. Environment International, 139, 105668. 10.1016/j.envint.2020.105668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leibel, S. , Nguyen, M. , Brick, W. , Parker, J. , Ilango, S. , Aguilera, R. , et al. (2020). Increase in pediatric respiratory visits associated with Santa Ana wind–driven wildfire smoke and PM2.5 levels in San Diego county [Dataset]. Annals of the American Thoracic Society, 17(3), 313–320. 10.1513/AnnalsATS.201902-150OC [DOI] [PubMed] [Google Scholar]
- Li, J. , Guan, T. , Guo, Q. , Geng, G. , Wang, H. , Guo, F. , et al. (2021). Exposure to landscape fire smoke reduced birthweight in low‐ and middle‐income countries: Findings from a siblings‐matched case‐control study [Dataset]. Elife, 10, e69298. 10.7554/eLife.69298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang, Y. , Sengupta, D. , Campmier, M. J. , Lunderberg, D. M. , Apte, J. S. , & Goldstein, A. H. (2021). Wildfire smoke impacts on indoor air quality assessed using crowdsourced data in California [Dataset]. Proceedings of the National Academy of Sciences, 118(36). 10.1073/pnas.2106478118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, J. C. , Mickley, L. J. , Sulprizio, M. P. , Dominici, F. , Yue, X. , Ebisu, K. , et al. (2016). Particulate air pollution from wildfires in the western US under climate change. Climate Change, 138(3), 655–666. 10.1007/s10584-016-1762-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, J. C. , Pereira, G. , Uhl, S. A. , Bravo, M. A. , & Bell, M. L. (2015). A systematic review of the physical health impacts from non‐occupational exposure to wildfire smoke. Environmental Research, 136, 120–132. 10.1016/j.envres.2014.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, J. C. , Wilson, A. , Mickley, L. J. , Dominici, F. , Ebisu, K. , Wang, Y. , et al. (2017). Wildfire‐specific fine particulate matter and risk of hospital admissions in urban and rural counties [Dataset]. Epidemiology, 28(1), 77–85. 10.1097/ede.0000000000000556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, J. C. , Wilson, A. , Mickley, L. J. , Ebisu, K. , Sulprizio, M. P. , Wang, Y. , et al. (2017). Who among the elderly is most vulnerable to exposure to and health risks of fine particulate matter from wildfire smoke? [Dataset]. American Journal of Epidemiology, 186(6), 730–735. 10.1093/aje/kwx141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, Y. , Austin, E. , Xiang, J. , Gould, T. , Larson, T. , & Seto, E. (2021). Health impact assessment of the 2020 Washington state wildfire smoke episode: Excess health burden attributable to increased PM2.5 exposures and potential exposure reductions [Dataset]. GeoHealth, 5(5), e2020GH000359. 10.1029/2020GH000359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahsin, M. D. , Cabaj, J. , & Saini, V. (2021). Respiratory and cardiovascular condition‐related physician visits associated with wildfire smoke exposure in Calgary, Canada, in 2015: A population‐based study [Dataset]. International Journal of Epidemiology, 51(1), 166–178. 10.1093/ije/dyab206 [DOI] [PubMed] [Google Scholar]
- Masri, S. , Scaduto, E. , Jin, Y. , & Wu, J. (2021). Disproportionate impacts of wildfires among elderly and low‐income communities in California from 2000–2020 [Dataset]. International Journal of Environmental Research and Public Health, 18(8), 3921. 10.3390/ijerph18083921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messier, K. P. , Tidwell, L. G. , Ghetu, C. C. , Rohlman, D. , Scott, R. P. , Bramer, L. M. , et al. (2019). Indoor versus outdoor air quality during wildfires [Dataset]. Environmental Science and Technology Letters, 6(12), 696–701. 10.1021/acs.estlett.9b00599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, A. , Yeskey, K. , Garantziotis, S. , Arnesen, S. , Bennett, A. , O’Fallon, L. , et al. (2016). Integrating health research into disaster response: The new NIH disaster research response Program. International Journal of Environmental Research and Public Health, 13(7), 676. 10.3390/ijerph13070676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda, M. L. , Callender, R. , Canales, J. M. , Craft, E. , Ensor, K. B. , Grossman, M. , et al. (2021). The Texas flood registry: A flexible tool for environmental and public health practitioners and researchers. Journal of Exposure Science and Environmental Epidemiology, 31(5), 823–831. 10.1038/s41370-021-00347-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naqvi, H. R. , Mutreja, G. , Shakeel, A. , Singh, K. , Abbas, K. , Naqvi, D. F. , et al. (2022). Wildfire‐induced pollution and its short‐term impact on COVID‐19 cases and mortality in California [Dataset]. Gondwana Research, 114, 30–39. 10.1016/j.gr.2022.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine . (2022). The chemistry of fires at the wildland‐urban interface. [PubMed]
- Neumann, J. E. , Amend, M. , Anenberg, S. , Kinney, P. L. , Sarofim, M. , Martinich, J. , et al. (2021). Estimating PM2.5‐related premature mortality and morbidity associated with future wildfire emissions in the western US [Dataset]. Environmental Research Letters, 16(3), 035019. 10.1088/1748-9326/abe82b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen, P. D. M. , Martinussen, N. , Mallach, G. , Ebrahimi, G. , Jones, K. , Zimmerman, N. , & Henderson, S. B. (2021). Using low‐cost sensors to assess fine particulate matter infiltration (PM2.5) during a wildfire smoke episode at a large inpatient healthcare facility [Dataset]. International Journal of Environmental Research and Public Health, 18(18), 9811. 10.3390/ijerph18189811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIEHS . (2023). Disaster research protocols. Retrieved from https://www.niehs.nih.gov/research/programs/disaster/human‐studies/index.cfm
- O’Dell, K. , Bilsback, K. , Ford, B. , Martenies, S. E. , Magzamen, S. , Fischer, E. V. , & Pierce, J. R. (2021). Estimated mortality and morbidity attributable to smoke plumes in the United States: Not just a western US problem [Dataset]. GeoHealth, 5(9), e2021GH000457. 10.1029/2021GH000457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hara, K. C. , Ranches, J. , Roche, L. M. , Schohr, T. K. , Busch, R. C. , & Maier, G. U. (2021). Impacts from wildfires on livestock health and production: Producer perspectives [Dataset]. Animals, 11(11), 3230. 10.3390/ani11113230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill, S. M. , Diao, M. , Raffuse, S. , Al‐Hamdan, M. , Barik, M. , Jia, Y. , et al. (2021). A multi‐analysis approach for estimating regional health impacts from the 2017 Northern California wildfires [Dataset]. Journal of the Air & Waste Management Association, 71(7), 791–814. 10.1080/10962247.2021.1891994 [DOI] [PubMed] [Google Scholar]
- Park, B. Y. , Boles, I. , Monavvari, S. , Patel, S. , Alvarez, A. , Phan, M. , et al. (2022). The association between wildfire exposure in pregnancy and foetal gastroschisis: A population‐based cohort study [Dataset]. Paediatric & Perinatal Epidemiology, 36(1), 45–53. 10.1111/ppe.12823 [DOI] [PubMed] [Google Scholar]
- Parks, S. A. , & Abatzoglou, J. T. (2020). Warmer and drier fire seasons contribute to increases in area burned at high severity in western US forests from 1985 to 2017. Geophysical Research Letters, 47(22), e2020GL089858. 10.1029/2020GL089858 [DOI] [Google Scholar]
- Pazderka, H. , Brown, M. R. G. , Agyapong, V. I. O. , Greenshaw, A. J. , McDonald‐Harker, C. B. , Noble, S. , et al. (2021). Collective trauma and mental health in adolescents: A retrospective cohort study of the effects of retraumatization [Dataset]. Frontiers in Psychiatry, 12, 682041. 10.3389/fpsyt.2021.682041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pazderka, H. , Brown, M. R. G. , McDonald‐Harker, C. B. , Greenshaw, A. J. , Agyapong, V. I. , Noble, S. , et al. (2021). Model of post‐traumatic growth in newly traumatized vs. Retraumatized adolescents [Dataset]. Frontiers in Psychiatry, 12, 682055. 10.3389/fpsyt.2021.682055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson, D. , Ebisu, K. , Wu, X. , & Basu, R. (2019). A review of coccidioidomycosis in California: Exploring the intersection of land use, population movement, and climate change [Dataset]. Epidemiologic Reviews, 41(1), 145–157. 10.1093/epirev/mxz004 [DOI] [PubMed] [Google Scholar]
- Postma, J. M. , Odom‐Maryon, T. , Rappold, A. G. , Haverkamp, H. , Amiri, S. , Bindler, R. , et al. (2022). Promoting risk reduction among young adults with asthma during wildfire smoke: A feasibility study [Dataset]. Public Health Nursing, 39(2), 405–414. 10.1111/phn.12986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rappold, A. G. , Hano, M. C. , Prince, S. , Wei, L. , Huang, S. M. , Baghdikian, C. , et al. (2019). Smoke Sense initiative leverages citizen science to address the growing wildfire‐related public health problem [Dataset]. GeoHealth, 3(12), 443–457. 10.1029/2019GH000199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rappold, A. G. , Reyes, J. , Pouliot, G. , Cascio, W. E. , & Diaz‐Sanchez, D. (2017). Community vulnerability to health impacts of wildland fire smoke exposure [Dataset]. Environmental Science & Technology, 51(12), 6674–6682. 10.1021/acs.est.6b06200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ré, A. , Rocha, A. T. , Campos, I. , Keizer, J. J. , Gonçalves, F. J. M. , Oliveira, H. , et al. (2021). Cytotoxic effects of wildfire ashes: In‐vitro responses of skin cells [Dataset]. Environmental Pollution, 285, 117279. 10.1016/j.envpol.2021.117279 [DOI] [PubMed] [Google Scholar]
- Reid, C. E. , Brauer, M. , Johnston, F. H. , Jerrett, M. , Balmes, J. R. , & Elliott, C. T. (2016). Critical review of health impacts of wildfire smoke exposure. Environmental Health Perspectives, 124(9), 1334–1343. 10.1289/ehp.1409277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid, C. E. , & Maestas, M. M. (2019). Wildfire smoke exposure under climate change: Impact on respiratory health of affected communities. Current Opinion in Pulmonary Medicine, 25(2), 179–187. 10.1097/mcp.0000000000000552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Requia, W. J. , Papatheodorou, S. , Koutrakis, P. , Mukherjee, R. , & Roig, H. L. (2021). Increased preterm birth following maternal wildfire smoke exposure in Brazil [Dataset]. International Journal of Hygiene and Environmental Health, 240, 113901. 10.1016/j.ijheh.2021.113901 [DOI] [PubMed] [Google Scholar]
- Rodney, R. M. , Swaminathan, A. , Calear, A. L. , Christensen, B. K. , Lal, A. , Lane, J. , et al. (2021). Physical and mental health effects of bushfire and smoke in the Australian capital territory 2019–20 [Dataset]. Frontiers in Public Health, 9, 682402. 10.3389/fpubh.2021.682402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sannigrahi, S. , Pilla, F. , Maiti, A. , Bar, S. , Bhatt, S. , kaparwan, A. , et al. (2022). Examining the status of forest fire emission in 2020 and its connection to COVID‐19 incidents in West Coast regions of the United States [Dataset]. Environmental Research, 210, 112818. 10.1016/j.envres.2022.112818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz, L. , Dimitrova, A. , Aguilera, R. , Basu, R. , Gershunov, A. , & Benmarhnia, T. (2022). Smoke and COVID‐19 case fatality ratios during California wildfires [Dataset]. Environmental Research Letters, 17(1), 014054. 10.1088/1748-9326/ac4538 [DOI] [Google Scholar]
- Shusterman, D. , Kaplan, J. Z. , & Canabarro, C. (1993). Immediate health effects of an urban wildfire [Dataset]. Western Journal of Medicine, 158(2), 133–138. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1021964/ [PMC free article] [PubMed] [Google Scholar]
- Solomon, G. M. , Hurley, S. , Carpenter, C. , Young, T. M. , English, P. , & Reynolds, P. (2021). Fire and water: Assessing drinking water contamination after a major wildfire [Dataset]. ACS ES&T Water, 1(8), 1878–1886. 10.1021/acsestwater.1c00129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen, C. , House, J. A. , O'Dell, K. , Brey, S. J. , Ford, B. , Pierce, J. R. , et al. (2021). Associations between wildfire‐related PM2.5 and intensive care unit admissions in the United States, 2006–2015 [Dataset]. GeoHealth, 5(5), e2021GH000385. 10.1029/2021GH000385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugg, M. M. , Runkle, J. D. , Hajnos, S. N. , Green, S. , & Michael, K. D. (2022). Understanding the concurrent risk of mental health and dangerous wildfire events in the COVID‐19 pandemic [Dataset]. Science of the Total Environment, 806, 150391. 10.1016/j.scitotenv.2021.150391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- To, P. , Eboreime, E. , & Agyapong, V. I. O. (2021). The impact of wildfires on mental health: A scoping review [Dataset]. Behavioral Sciences, 11(9), 126. 10.3390/bs11090126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan, X. , Li, C. , & Parikh, S. J. (2021). Chemical composition of soil‐associated ash from the southern California Thomas Fire and its potential inhalation risks to farmworkers [Dataset]. Journal of Environmental Management, 278, 111570. 10.1016/j.jenvman.2020.111570 [DOI] [PubMed] [Google Scholar]
- Woo, S. H. L. , Liu, J. C. , Yue, X. , Mickley, L. J. , & Bell, M. L. (2020). Air pollution from wildfires and human health vulnerability in Alaskan communities under climate change [Dataset]. Environmental Research Letters, 15(9), 094019. 10.1088/1748-9326/ab9270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu, R. , Yu, P. , Abramson, M. J. , Johnston, F. H. , Samet, J. M. , Bell, M. L. , et al. (2020). Wildfires, global climate change, and human health. New England Journal of Medicine, 383(22), 2173–2181. 10.1056/NEJMsr2028985 [DOI] [PubMed] [Google Scholar]
- Yao, J. , Brauer, M. , Wei, J. , McGrail, K. M. , Johnston, F. H. , & Henderson, S. B. (2020). Sub‐daily exposure to fine particulate matter and ambulance dispatches during wildfire seasons: A case‐crossover study in British Columbia, Canada [Dataset]. Environmental Health Perspectives, 128(6), 067006. 10.1289/EHP5792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, X. , Josey, K. , Kamareddine, L. , Caine, M. C. , Liu, T. , Mickley, L. J. , et al. (2021). Excess of COVID‐19 cases and deaths due to fine particulate matter exposure during the 2020 wildfires in the United States [Dataset]. Science Advances, 7(33), eabi8789. 10.1126/sciadv.abi8789 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1
Data Availability Statement
This review paper did not analyze any new data. The list of studies reviewed can be found in Table 1. Only results published in identified previous studies were used. The included studies are provided in the reference list.


