Abstract
Background
Insomnia and depression are prevalent mental disorders that are often comorbid among older adults. Lifestyle intervention strategies incorporating Tai Chi or conventional exercise have been shown to alleviate symptoms of insomnia and depression. However, the comparative efficacy of these exercise modalities in individuals with both disorders has yet to be determined. Therefore, the aim of this study is to examine the efficacy of Tai Chi and conventional exercise for reducing depressive symptoms in older adults with chronic insomnia and depressive symptoms, when compared to a health education control.
Methods
This study is a prospective, assessor-blinded, three-arm, parallel group, randomized controlled trial. Older adults aged ≥60 years with a diagnosis of chronic insomnia and depressive symptoms will be randomly assigned to a Tai Chi, conventional exercise or health education control condition on a 1:1:1 basis. Interventions will last for 3 months, with a 6-month follow-up period. The primary outcome is depressive symptoms, assessed using the Hospital Anxiety and Depression Scale. Secondary outcomes include subjective sleep quality, 7-day actigraphy, 7-day sleep diary, anxiety symptoms, quality of life, medication usage and physical function. All measurements will be conducted at baseline, 3 months and 9 months by outcome assessors who are blinded to group allocation.
Discussion
This study will compare the efficacy of Tai Chi and conventional exercise in improving depression outcomes in older adults with chronic insomnia and depressive symptoms. Our results will shed light on the clinical potential of these interventions for combating insomnia and depression in older adults.
Keywords: Insomnia, Depressive symptoms, Tai Chi, Exercise, Older adults
1. Introduction
Depression is the main cause of disability worldwide and a primary contributor to the global burden of disease.1 Depression occurs in 7% of older adults and accounts for 5.7% of years lived with disability among individuals aged over 60 years old.2 Up to 16% of community-dwelling older adults develop clinically significant depressive symptoms, of which 32% can advance into a severe chronic course.3,4 Late-life depressive symptoms are associated with cognitive impairment, medical comorbidity and mortality,5, 6, 7 and with an increased risk of hospitalization and cost of medical services.8,9
Insomnia occurs in nearly 50% of the older adult population10,11 and is a strong risk factor for the future development of depressive disorders.12,13 The relationship between depression and insomnia is bidirectional, as sleep difficulties can manifest prior to or after the onset of a depressive episode,14,15 and up to 90% of individuals with depression report sleep quality complaints.16 In fact, depression is the most frequent cause of chronic insomnia in both clinical and general populations.17,18 In a recent randomized clinical study in older adults with insomnia but without depression,19 cognitive behavioral therapy for insomnia (CBT-I) was found to prevent the incidence and recurrence of major depressive disorder when compared to a sleep education therapy control. In addition, the magnitude of the treatment effect on depression incidence was contingent on the rate of insomnia remission in both intervention groups. These findings strengthen the relationship between depression and insomnia, and suggest that treating one disorder can prevent the incidence and recurrence of the other. Among the nonclinical treatments for insomnia, exercise represents a safe and accessible alternative. The use of exercise to improve insomnia symptoms is supported by scientific literature,20, 21, 22 and is endorsed by European and American sleep guidelines.23,24 Similarly, exercise can alleviate symptoms of depression in older adults25, 26, 27 and improve sleep quality outcomes in depressed individuals.28
Conventional exercise programs targeted at improving depression and insomnia commonly involve aerobic (e.g., walking, running, swimming) or resistance (e.g., weightlifting, bodyweight exercises) training activities. These programs are safe and easy to perform for older adults,29,30 yet fear of injury and the inability to execute exercises correctly are strong barriers hindering participation.31 In addition, it remains unclear whether different forms of exercise have differential effects on depressive symptoms in seniors. Further insight regarding the effects of specific exercise modalities is needed to provide older adults with evidence-based training alternatives. Mind-body exercise is a potential alternative to conventional exercise to improve mental and physical outcomes while posing minimal risks. Tai Chi is a traditional Chinese mind-body practice that incorporates multimodal physical and mental components. Unlike conventional exercise, Tai Chi includes meditation and breathing components while performing specific martial art techniques. Epidemiological studies have demonstrated that mind-body exercise such as Tai Chi is widely used in the Chinese community, where over 20% of middle-aged and older adults practice regularly,32 and is becoming increasingly popular in Western countries, where prevalence trends have reached 15%.33 Tai Chi is beneficial for balance, flexibility and strength and is safe to perform without the risk of adverse events or serious injuries.34,35 It is well acknowledged as a suitable activity for older people, even if they are inactive or unfit. Furthermore, Tai Chi can help with osteoarthritis management, reduce the risk of falls, improve cardiorespiratory function, and be used for treatment and prevention of various psychosomatic disorders.35,36
Robust evidence suggests that Tai Chi is effective for improving sleep outcomes in adults with different conditions, such as depression, cancer, osteoarthritis and fibromyalgia.37 Our team recently conducted a study comparing the effects of Tai Chi and conventional exercise in older insomniacs and found that both interventions significantly improved objectively-measured sleep efficiency when compared to a control condition.38 However, little is known regarding the comparative efficacy of these interventions on depression outcomes in older adults with insomnia and depressive symptoms. The targeted study population offers important advantages relating to the application of our anticipated findings to real-life settings. For instance, the inclusion of adults with insomnia and depressive symptoms allows for the opportunity to identify and intervene in individuals who are at higher risk of developing clinical depression, potentially preventing the deterioration of the disease before it fully manifests. In addition, insomnia disorder is generally less stigmatized than depression.39 Therefore, interventional studies involving insomnia as the primary clinical morbidity might be more easily accepted than studies on depression treatment. Preliminary evidence suggests that CBT-I can be effective for treating and preventing both depression and insomnia19; however similar therapeutic efficacy of other nonclinical treatment modalities is currently unknown.
Considering the strong prevalence of depression and insomnia in the older adult population and the health repercussions that they can cause, as well as the clinical potential of exercise modalities for treating these disorders, we designed a comparative randomized controlled trial to examine the efficacy of Tai Chi and conventional exercise in alleviating depressive symptoms in older adults who are coincidently suffering from chronic insomnia and depressive symptoms. The results will be critical to establish whether lifestyle intervention strategies such as Tai Chi and conventional exercise can be used to improve depressive symptoms, as well as several secondary outcomes, in a prevalent yet understudied cohort. We hypothesized that Tai Chi and conventional exercise will significantly improve symptoms of depression, when compared to a health education control group. In addition, we aimed to explore potential differences in treatment efficacy between Tai Chi and conventional exercise.
2. Methods
2.1. Study design and setting
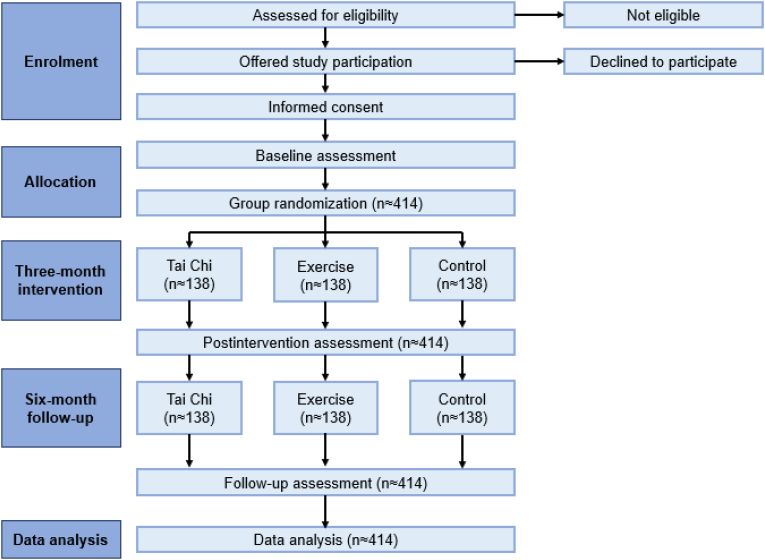
This study is a prospective, assessor-blinded, three-arm, parallel group, randomized controlled trial. Community-dwelling older adults with chronic insomnia and depressive symptoms will be recruited and randomized to a Tai Chi, conventional exercise or health education control group (Fig. 1). The study promotion began in January 2021, however due to the COVID-19-related measures that were in vigour in Hong Kong, the study registration and recruitment period were significantly delayed. After the COVID-19 restrictions were lifted, the protocol of this study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (reference UW 20–026) and was registered on ClinicalTrials.gov with identifier NCT05482646 (August 1, 2022). As a result, participant recruitment began on August 2, 2022, and was completed by December 2023.
Fig. 1.
Study flow diagram of participant enrolment, randomization and interventions.
All outcome assessments for this study will be performed at baseline, 3 months (postintervention) and 9 months (6 months follow-up). The outcome assessments, interviews and control sessions will be conducted at the University of Hong Kong in rooms suited for administering tests and delivering health education classes. The Tai Chi and exercise sessions will be conducted in exercise rooms or in outdoor spaces designated for small-group exercise classes. All data in this study will be reported in accordance with the Consolidated Standards of Reporting Trials (CONSORT) guidelines, and the study protocol will be executed according to the Standard Protocols Items of the Recommendations for Interventional Trials (SPIRIT) guidelines.
2.2. Participants
2.2.1. Recruitment
We will approach potential participants in the community through poster/leaflet distribution and promotional events in community centers and housing estates. We will invite responding individuals to a preliminary visit to confirm eligibility. Eligible participants will be provided a verbal and written description of the study design. Written informed consent will be obtained from each participant before baseline outcome assessments. Participants enrolled in this study will not receive any monetary compensation for joining the study. Instead, the health benefits of the planned interventions and the opportunity to receive free physical and mental health assessments will be used to incentivize enrolment. After ensuring eligibility and completing the baseline assessments, participants will be randomized to Tai Chi, conventional exercise or health education control for 3 months.
2.2.2. Eligibility criteria
We will recruit participants who meet the following inclusion criteria: 1) adults ≥60 years of age; 2) ethnic Chinese; 3) mild-to-moderate depressive symptoms, as ascertained by an HADS-depression score ≥8 and a PHQ-9 score ≤14; and 4) chronic insomnia, defined using the Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria, including difficulties in initiating or maintaining sleep, and/or early morning awakening with complaints of significant distress or impairment of daytime functioning, occurring at least 3 nights per week and present for at least 3 months.
Participants will not be allowed to enter the study if they meet the following exclusion criteria: 1) somatic conditions that prevent participation in Tai Chi or exercise; 2) regular moderate-to-vigorous intensity exercise or mind-body training such as Tai Chi, yoga, qigong or meditation (≥60-min sessions at least 3 times per week) in the past 3 months; 3) with dementia or receiving medications for dementia; 4) diagnosis of schizophrenia or other psychotic disorders, bipolar disorders or alcohol/substance use/abuse; 5) currently using or planning to use potentially confounding treatments, including herbal supplements (e.g., St. John's Worth), acupuncture treatment, cognitive behavioral therapy or other types of psychotherapy, mind-body interventions (e.g., mindfulness training and muscle relaxation training) or muscle relaxants such as carisoprodol, cyclobenzaprine, and diazepam; or 6) suicidal or self-injurious potential that requires immediate clinical follow-up.
We will include participants who take antidepressants or sleep medications to incorporate a wider population. However, the dose and frequency of medications will be strictly monitored by the research personnel to examine potential fluctuations in medications used during the study period. As people with non-psychotic mental disorders (e.g., depressive and anxiety disorders) can also benefit from Tai Chi and exercise, they will be included to further enhance the generalizability of our findings. Nevertheless, participants who might be disruptive to the group, including those with existing uncontrolled violence and psychotic symptoms, will be excluded. Additionally, participants with severe depressive symptoms (PHQ-9 score >14) will be excluded due to the ethical concerns that Tai Chi and conventional exercise are currently not considered established treatments for severe depression.
2.2.3. Blinding
Participants and Tai Chi/fitness instructors will not be blinded to the group allocation due to the nature of the exercise interventions. However, all research personnel involved in the data entry, outcome assessments and data analysis will be blinded to group allocation. Participants will be instructed not to disclose their study group during the assessments.
2.2.4. Randomization and allocation concealment
A computer-generated randomized allocation sequence will be produced using an online randomization software. Participants will be randomly allocated to the Tai Chi, conventional exercise or health education control groups at a 1:1:1 ratio. The allocation sequence will be implemented by a centralized independent randomization list kept by the Principal Investigator (PI), who will not interact with the participants during the recruitment to avoid allocation bias and to ensure allocation concealment. Research personnel will contact the PI to obtain the randomized allocation sequence for each newly recruited participant.
2.3. Interventions
Participants in the Tai Chi, exercise and health education groups will follow a 3-month program consisting of two 1.5-h weekly sessions. All interventions will be conducted in small groups (approximately 10–15 participants per group) and will be supervised by research personnel and/or qualified fitness instructors.
2.3.1. Conventional exercise
Participants assigned to the conventional exercise group will engage in a generic fitness training program delivered by certified fitness instructors (Table S1). Safety measures, basic training principles and correct techniques will be explained to all participants before commencing the first class. Each training session will consist of a 15-min warm-up including light static stretching exercises of the major muscles, followed by a 30-min brisk walking exercise and 30 min of body conditioning activities (e.g., arm curls, arm raises, shoulder press, ¼ squat, heel raises and stepping on the ground). Each class will end with a 15-min cool-down including light static stretching, deep breathing activities, and relaxing body movements. The brisk walking and body conditioning activities will be maintained at moderate intensity equal to 3–4 metabolic equivalents of task (METs), in which 1 ME T refers to the resting metabolic rate during quiet sitting.40 During each session, the exercise intensity will be individually monitored by the fitness instructors using talk tests and the Borg rate of perceived exertion (RPE) scale. This 15-point scale has values ranging from 6 to 20, with higher scores indicating more strenuous exertion.41 The instructors will record participants’ responses to the scale to confirm that they are exercising at the established intensity. This intensity is chosen to ensure that the exercise session is safe for all participants, and to match the intensity of participants performing Tai Chi, as research shows that Tai Chi is equivalent to light-to-moderate exercise (3–4 METs).42, 43, 44, 45 In addition, a random sample of participants will be selected from each training group to wear a heart rate monitor to ensure that participants are exercising at an intensity of 57%–76% of maximum heart rate, which is representative of light-to-moderate intensity.46 To ensure that the exercise sessions are practicable and safe, all movements will be kept simple, and no additional weight will be applied. The range of motion and number of repetitions/sets will be adjusted after the initial adaptation of the subjects.
2.3.2. Tai Chi
Participants assigned to the Tai Chi group will engage in a Tai Chi program with settings similar to those of the conventional exercise program. The 24-form simplified Yang-style Tai Chi will be delivered, as it is the most commonly adopted form of Tai Chi in the literature.47 The Tai Chi instructors will introduce the safety issues, proper training principles, and techniques to the participants in their first class to minimize any avoidable adverse events due to improper skill/practice. The intensity will be maintained at light-moderate by the same means used for the conventional exercise group. An overview of the structure of each Tai Chi session is provided in Table S2.
In both intervention groups, the first month will be considered an adaptation period to allow participants to progressively adjust to the exercise programs. The goal is to accomplish at least 50% of the prescribed exercise volume during the first two weeks, which will increase to 75% during the subsequent two-week period and reach the full exercise volume by the end of the first month. Participants who have difficulty in adapting will be identified during the first two weeks and will be provided with extra support by the instructors to help them adjust to the intervention. Nevertheless, our previous experience shows that almost all older adults are able to adapt to our proposed Tai Chi and exercise programs within the first month of intervention.38,48,49 Participants will be encouraged to achieve ≥80% class attendance.
2.3.3. Health education control
Participants in the control group will attend a health education program emphasizing topics of mental health, sleep hygiene, and general health (Table S3). The topics were chosen based on the information gathered from health authorities’ websites, including the Hong Kong Department of Health, the Hong Kong Elderly Health Centre, the World Health Organization and the National Sleep Foundation websites. The control group will receive an equal amount of contact time as the Tai Chi and exercise groups to control for the attention received.
2.3.4. Treatment fidelity
Both Tai Chi and conventional exercise interventions will be directed by multiple trained instructors to avoid intervention delivery bias due to individual differences in teaching style or skills. The recruited instructors will attend a training session to ensure that they deliver similar Tai Chi and exercise protocols. Research personnel will visit each class biweekly to ensure that instructors and participants adhere to the treatment protocol.
2.4. Outcomes
Outcome measures will be assessed at 0 month (baseline), 3 months (postintervention) and 9 months (follow-up at 6 months postintervention) (Table 1).
Table 1.
Overview of study protocol.
| Time Point | Enrolment |
Baseline Outcome Assessment |
Randomization |
Intervention Phase |
Outcome Assessment |
|
|---|---|---|---|---|---|---|
| Month 0 | Month 3 | Month 9 | ||||
| Enrolment | ||||||
| Eligibility Screen | ✓ | |||||
| Informed Consent | ✓ | |||||
| Allocation |
✓ |
|||||
| Intervention | ||||||
| Tai Chi | ✓ | |||||
| Exercise | ✓ | |||||
| Control |
✓ |
|||||
| Outcome Assessment | ||||||
| HADS | ✓ | ✓ | ✓ | |||
| PHQ-9 | ✓ | ✓ | ✓ | |||
| GAD-7 | ✓ | ✓ | ✓ | |||
| ISI | ✓ | ✓ | ✓ | |||
| PSQI | ✓ | ✓ | ✓ | |||
| SF-12 | ✓ | ✓ | ✓ | |||
| SPPB | ✓ | ✓ | ✓ | |||
| 7-day Actigraphy | ✓ | ✓ | ✓ | |||
| 7-day Sleep Diary | ✓ | ✓ | ✓ | |||
| Adverse Events | ✓ | ✓ | ✓ | |||
2.5. Primary outcome
2.5.1. Depressive symptoms
The depressive symptoms subscale of the Hospital Anxiety and Depression Scale (HADS-D) will be used to assess the severity of depressive symptoms. The scale consists of two seven-item questionnaires (one for depression and one for anxiety). Each item is scored from 0 to 3 based on the severity of the symptoms (“0” representing no depressive symptoms and “3” representing significant depressive symptoms), with an overall score ranging from 0 to 21. Higher scores are indicative of more severe symptoms (i.e., 0–7: normal; 8–10: borderline abnormal depression; ≥11 abnormal depression).50 The Chinese-Cantonese version of the HADS has been demonstrated to be reliable and valid in Hong Kong Chinese participants,51 with a sensitivity and specificity of approximatively 0.80 and a Cronbach's alpha of 0.82.52
2.6. Secondary outcomes
2.6.1. Depression severity
The Patient Health Questionnaire (PHQ-9) will be used to further assess the severity of depression. The questionnaire is composed of 9 items, each scored from 0 to 3 based on the frequency of symptoms, with a total score ranging from 0 to 27. Higher scores reflect higher depression severity (1–4: minimal depression; 5–9: mild depression; 10–14: moderate depression; 15–19: moderately severe depression; 20–27: severe depression). The Chinese version of the PHQ-9 has been validated in the Chinese community, with an alpha internal consistency of 0.86.53
2.6.2. Anxiety symptoms
The anxiety symptoms subscale of the HADS (HADS-A) will be used to assess anxiety symptoms. The Chinese-Cantonese version of the HADS-A was shown to have good internal consistency (Cronbach's alpha = 0.77) and good item-scale correlation (0.66).51
The General Anxiety Disorder Scale (GAD-7) will be supplemented with the HADS-A to confirm the assessment of anxiety symptoms. The GAD-7 is commonly used as a measure of general anxiety symptoms across various settings and populations. The questionnaire assesses feelings of worry, nervousness, restlessness and irritability of the individual over the past 2 weeks. The scale is composed of 7 items, each rated from 0 to 3, with an aggregate maximum score of 21. A score of 0–9 is considered within the normal range, while a score of 10 or above suggests symptoms of general anxiety disorder. The scale was shown to have excellent internal consistency (Cronbach's alpha = 0.88) and high reliability and validity.54
2.6.3. Insomnia severity
The Insomnia Severity Index (ISI) will be used to assess the severity of insomnia symptoms. The ISI is a seven-item questionnaire examining sleep-onset and sleep maintenance difficulties, satisfaction with the current sleep pattern, interference with daily functioning, noticeable impairment due to sleep problems, degree of distress and concerns caused by sleep problems. Each item is rated on a “0–3” Likert scale, with higher scores indicating more perceived severity of insomnia. The Chinese version of the ISI has been shown to have a content validity index of 0.94 and high internal consistency with a Cronbach's alpha of 0.81.55
2.6.4. Sleep quality
The Pittsburgh Sleep Quality Index (PSQI) will be used to estimate sleep quality. The PSQI consists of 19 items that subjectively assess sleep quality based on participants' usual bedtime, wake time, time to fall asleep and time of actual sleep, and based on potential sleep disturbances experienced during the month prior to taking the test. Each item is rated on a “0–3” Likert scale, with higher scores indicating poorer sleep quality. The Chinese version of the PSQI has been commonly used to differentiate individuals with regular sleep patterns from those with primary insomnia, and it has been demonstrated to have good internal consistency (Cronbach's alpha = 0.83) and test-retest reliability (coefficient = 0.85) in Chinese older adults.56
2.6.5. Objective sleep (actigraphy)
A wrist actigraph (GT-9X Link Actigraph, USA) will be used to objectively estimate sleep quantity. The actigraph activity monitor is a three-axis accelerometer that detects daily physical movement or lack thereof correlating with wakefulness and sleep, respectively. Participants will be instructed to wear an actigraph on the non-dominant wrist for 24 h per day for 7 consecutive days during each assessment period. Actigraph data will be analyzed using the Cole-Kripke algorithm provided by the manufacturer's software (ActiLife, Version 6.11.7) to determine the 7-day average of sleep parameters, including sleep onset latency (SOL), wake time after sleep onset (WASO), total sleep time (TST), sleep efficiency (SE), number of awakenings per night (NOA) and average wake time per awakening (AWT).
2.6.6. Subjective sleep (sleep diary)
A sleep diary will be used to subjectively assess sleep quantity. Participants will be instructed to record their sleep patterns for a 7-day period. Parameters related to participants’ sleep habits will be collected to determine SOL, WASO, TST, SE, NOA and AWT. The dose and frequency of hypnotic medications taken during the 7 days will also be reported. Recent studies showed that subjective sleep outcomes assessed through sleep diaries yield significantly different results compared to objectively measured outcomes (e.g., actigraphy, electroencephalography).57,58 As a result, we decided to include both subjective and objective sleep outcomes in this study.
2.6.7. Medication usage
Antidepressants (such as selective serotonin reuptake inhibitors including fluoxetine, sertraline, paroxetine, escitalopram and citalopram; serotonin and norepinephrine reuptake inhibitors including venlafaxine, duloxetine, levomilnacipran and desvenlafaxine; tricyclic antidepressants including amitriptyline, nortriptyline, imipramine, doxepin and desipramine; atypical antidepressants including vortioxetine, vilazodone, trazodone, mirtazapine and bupropion; monoamine oxidase inhibitors including selegiline, tranylcypromine, isocarboxazid and phenelzine) and sleep aid medications (such as narcotics, antihistamines, benzodiazepines such as flurazepam, quazepam, triazolam, estazolam, temazepam, clonazepam, lorazepam and alprazolam, non-benzodiazepine, and benzodiazepine receptor agonists such as zolpidem, zaleplon and eszopiclone) will be recorded with detailed usage information (e.g., drug name, type, dose, and weekly frequency). Participants will be asked to provide the dose and frequency of use of any medications by responding to a checklist with a full list of all the available antidepressants and sleep medications. Data on medication dose and weekly frequency will be presented as the total number of lowest recommended dose (LRD) in 7 days in the analysis.59
2.6.8. Quality of life
The 12-item Short Form Survey (SF-12) will be used to measure health-related quality of life. It consists of 12 items assessing physical functioning, emotional and mental health, bodily pain, general health, vitality, and social functioning. The final score is subdivided into physical and mental health components, with higher scores indicating better quality of life. The Chinese version of the SF-12 has been validated in the Hong Kong Chinese population60 and was shown to have high internal consistency (Cronbach's alpha = 0.91).
2.6.8.1. Physical function and balance
The Short Physical Performance Battery and Balance Test (SPPB) will be used to assess lower extremity physical function and balancing performance. The SPPB involves a series of timed tests of lower extremity physical performance, including standing balance, walking speed and the ability to rise from a chair. Scores ranging from 1 to 4 are assigned to participants based on the time to complete each test, with higher scores indicating better function and balance.
2.7. Statistical analysis and sample size calculation
The maximum error of committing a false positive was set as 1.67% (i.e., 5% divided by 3) to address multiplicity for the sample size estimation. Because evidence on the effects of Tai Chi and conventional exercise in older adults with insomnia and depressive symptoms is limited, the findings of meta-analyses with similar populations and interventions were examined to determine the expected effect size. In a network meta-analysis by Miller et al.,61 mind-body and aerobic exercise reduced depressive symptoms of older adults with effect sizes ranging from 0.27 to 0.51, when compared to control groups. In older adults with chronic diseases, Tai Chi showed moderate benefits on depressive symptoms (standardized mean difference: 0.42),62 while in a meta-analysis on depressed adults Tai Chi and conventional exercise demonstrated effect sizes of 0.28 and 0.68, respectively.63 Taking these results together, a Cohen's d of 0.5 was chosen for sample size calculation. Using an effect size of 0.5 and a statistical power of 0.9, 110 participants per group were deemed necessary for the current study. To predict attrition rates in our study, we inspected participant dropout from previous studies. Studies on the effects of Tai Chi in Chinese individuals with insomnia or depression showed attrition rates ranging from 11% to 27%,38,64, 65, 66 while the attrition from exercise studies was lower but similar (range: 11%–18%).38,67, 68, 69 In line with these findings, a conservative attrition rate of 20% was chosen for the current study, leading to a total sample size of 414 participants.
Data will be expressed as mean ± SD. Statistical analyses will be performed using SAS OnDemand for Academics. The intention-to-treat principle will be applied so that all randomized participants will be included in the analyses. Data will be analyzed using the Generalized Estimating Equations (GEE) model with adjustment for baseline values. Linear contrasts will be performed for pairwise comparisons. The Holm correction will be applied to address multiplicity. Considering that the GEE model can accommodate missing data, missing values will not be replaced. Statistical significance will be accepted as p < 0.05.
2.8. Data management
2.8.1. Data entry
Research personnel blinded to the group allocation of participants will be responsible for performing data entry for all outcomes. Two independent researchers will extract and input participant data to avoid potential data extraction oversights.
3. Discussion
This study will investigate the effects of Tai Chi and conventional exercise in older adults who are coincidently suffering from chronic insomnia and depressive symptoms. We expect that our results will support the beneficial effects of Tai Chi and exercise for improving depressive symptoms in older adults living with insomnia. Furthermore, these findings will provide insights regarding the comparative treatment efficacy of the two exercise modalities when compared to one another and to a health education control condition.
Previous evidence has shown that treating older adults with insomnia using cognitive behavioral therapy can prevent the onset of future depressive disorders.19 This supports the strong relationship between depression and insomnia, and highlights the importance of considering both disorders when designing a treatment plan. However, clinical treatments for insomnia, including sleep medications and psychotherapy, have considerable limitations relative to the accessibility, high costs, and adverse effects to the intervention.70, 71, 72 Lately, lifestyle intervention strategies such as Tai Chi and exercise have gained consensus as alternative treatment approaches for depression and insomnia. Tai Chi was shown to effectively improve depression and sleep outcomes in older adults,37,38 while the benefits of exercise for mental health are well sustained. These benefits include improvements in depression, anxiety, insomnia and cognition.20,25,73, 74, 75 With this study, we aim to corroborate these findings by investigating whether Tai Chi and exercise can effectively ameliorate symptoms of depression in older adults with chronic insomnia and depressive symptoms. Our findings will provide further insight regarding the relationship between the two disorders by determining whether both depression and insomnia can be improved after an exercise intervention, and will further support the role of Tai Chi and exercise in mental health improvements among older cohorts.
The benefits of Tai Chi and exercise for overall health are well documented, yet less is known regarding the comparative efficacy between the two interventions. Tai Chi is a multicomponent mind-body intervention incorporating physical, cognitive, spiritual and behavioral elements to promote fitness and wellbeing.76 Conventional exercise typically involves more strenuous physical effort, but lacks a meditative mind component. There is preliminary evidence suggesting that Tai Chi might be superior to conventional exercise for improving cognitive outcomes in older cohorts.48,77 Furthermore, there is evidence that Tai Chi may stimulate brain plasticity and grey matter volume to a greater extent than conventional exercise.78 A recent randomized controlled study found that Tai Chi was superior to exercise in improving subjective sleep outcomes; however, the same results were not reflected in objective sleep outcomes.38 The mentioned evidence suggests some differences in the treatment efficacy after a Tai Chi or exercise intervention, which are likely attributed to the spiritual nature of Tai Chi, combined with its light-to-moderate physical components. With this study, we intend to explore whether these differences are also reflected in depression outcomes, as well as in several secondary outcomes, including quality of life, insomnia and anxiety symptoms.
This study has several potential limitations. First, the interpretation of our findings will be restricted to adults aged 60 years or older, and cannot be extended to younger age groups. Yet both insomnia and depressive symptoms are common in older adults,79,80 and are associated with a higher incidence of various comorbidities, including dementia, anxiety, chronic pain and metabolic disorders.81,82 It is, therefore, crucial to disseminate the results of the interventions that can be beneficial for the mental and physical health of these cohorts. Second, the Tai Chi and exercise interventions will be delivered in both indoor and outdoor settings. This was done to extend the participation in the study to individuals who live far from our research lab and are not willing to commute for long periods of time several times per week. The difference in setting might lead to within-group discrepancies in relation to the response to the intervention. Nevertheless, individuals exercising indoors and outdoors will experience no other difference regarding the nature of the intervention that they receive. Furthermore, the intervention venue will be noted down to explore the potential influence of the setting on the primary outcome. Third, the recruitment of participants, as well as the adherence and attrition to the interventions, have been negatively impacted by the COVID-19 outbreak and its periodic waves of infections. Indeed, a specified protocol will be followed by all research personnel to reduce the impact of the pandemic, including the optimization of social distance measures and hygiene protocols, and the rescheduling of screening visits for positive COVID-19 cases and close contacts. Further details regarding the nature of the delays, as well as the methods implemented to resolve them, are described in Appendix S1 of the supplementary material.
In conclusion, this study will investigate the efficacy of Tai Chi and conventional exercise for improving depressive symptoms and several secondary outcomes, including sleep, anxiety and quality of life, in older adults affected by chronic insomnia and with considerable depressive symptoms. We expect that our findings will further promote the benefits of Tai Chi and exercise as effective treatment alternatives to alleviate depressive symptoms in older individuals who are suffering from chronic insomnia.
4. Funding acknowledgements
This study is supported by the Health and Medical Research Fund (17182461) of Health Bureau, Hong Kong SAR and the Seed Fund for Basic Research of The University of Hong Kong. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Consent for publication
Not applicable. This manuscript does not contain data from any individual person.
Availability of data and materials
Data collected for this study is available upon request.
Declaration of competing interest
The authors declared no competing interests.
Acknowledgements
Not applicable.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jesf.2024.03.001.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Vos T., Lim S.S., Abbafati C., et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Mental health of older adults. Accessed 13/June/2023, https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults.
- 3.Blazer D.G. Depression in late life: review and commentary. J Gerontol. 2003;58(3):M249–M265. doi: 10.1093/gerona/58.3.M249. [DOI] [PubMed] [Google Scholar]
- 4.Beekman A.T., Geerlings S.W., Deeg D.J., et al. The natural history of late-life depression: a 6-year prospective study in the community. Arch Gen Psychiatr. 2002;59(7):605–611. doi: 10.1001/archpsyc.59.7.605. [DOI] [PubMed] [Google Scholar]
- 5.Han F.-F., Wang H.-X., Wu J.-J., Yao W., Hao C.-F., Pei J.-J. Depressive symptoms and cognitive impairment: a 10-year follow-up study from the survey of health, ageing and retirement in europe. Eur Psychiatr. 2021;64(1):e55. doi: 10.1192/j.eurpsy.2021.2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kong D., Solomon P., Dong X. Comorbid depressive symptoms and chronic medical conditions among US Chinese older adults. JAGS. 2019;67(S3):S545–S550. doi: 10.1111/jgs.15669. [DOI] [PubMed] [Google Scholar]
- 7.Schulz R., Beach S.R., Ives D.G., Martire L.M., Ariyo A.A., Kop W.J. Association between depression and mortality in older adults: the Cardiovascular Health Study. Arch Intern Med. 2000;160(12):1761–1768. doi: 10.1001/archinte.160.12.1761. [DOI] [PubMed] [Google Scholar]
- 8.Unützer J., Patrick D.L., Simon G., et al. Depressive symptoms and the cost of health services in HMO patients aged 65 years and older. A 4-year prospective study. JAMA. 1997;277(20):1618–1623. doi: 10.1001/jama.1997.03540440052032. [DOI] [PubMed] [Google Scholar]
- 9.Huang B.Y., Cornoni-Huntley J., Hays J.C., Huntley R.R., Galanos A.N., Blazer D.G. Impact of depressive symptoms on hospitalization risk in community-dwelling older persons. JAGS. 2000;48(10):1279–1284. doi: 10.1111/j.1532-5415.2000.tb02602.x. [DOI] [PubMed] [Google Scholar]
- 10.Foley D., Ancoli-Israel S., Britz P., Walsh J. Sleep disturbances and chronic disease in older adults: results of the 2003 national sleep foundation sleep in America survey. J Psychosom Res. 2004;56(5):497–502. doi: 10.1016/j.jpsychores.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 11.Patel D., Steinberg J., Patel P. Insomnia in the elderly: a review. JCSM. 2018;14(6):1017–1024. doi: 10.5664/jcsm.7172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baglioni C., Battagliese G., Feige B., et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135(1-3):10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Pigeon W.R., Hegel M., Unützer J., et al. Is insomnia a perpetuating factor for late-life depression in the IMPACT cohort? Sleep. 2008;31(4):481–488. doi: 10.1093/sleep/31.4.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Franzen P.L., Buysse D.J. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. 2008;10(4):473–481. doi: 10.31887/DCNS.2008.10.4/plfranzen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ohayon M.M. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 16.Tsuno N., Besset A., Ritchie K. Sleep and depression. J Clin Psychol. 2005;66(10):1254–1269. doi: 10.4088/jcp.v66n1008. [DOI] [PubMed] [Google Scholar]
- 17.Buysse D.J., Reynolds C.F., 3rd, Kupfer D.J., et al. Clinical diagnoses in 216 insomnia patients using the international classification of sleep disorders (ICSD), DSM-IV and ICD-10 categories: a report from the APA/NIMH DSM-IV field trial. Sleep. 1994;17(7):630–637. doi: 10.1093/sleep/17.7.630. [DOI] [PubMed] [Google Scholar]
- 18.Ohayon M.M., Caulet M., Lemoine P. Comorbidity of mental and insomnia disorders in the general population. Compr Psychiatr. 1998;39(4):185–197. doi: 10.1016/s0010-440x(98)90059-1. [DOI] [PubMed] [Google Scholar]
- 19.Irwin M.R., Carrillo C., Sadeghi N., Bjurstrom M.F., Breen E.C., Olmstead R. Prevention of incident and recurrent major depression in older adults with insomnia: a randomized clinical trial. JAMA Psychiatr. 2022;79(1):33–41. doi: 10.1001/jamapsychiatry.2021.3422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Milne S., Elkins M.R. Exercise as an alternative treatment for chronic insomnia (PEDro synthesis) Br J Sex Med. 2017;51(5):479. doi: 10.1136/bjsports-2016-096349. [DOI] [PubMed] [Google Scholar]
- 21.Hasan F., Tu Y.K., Lin C.M., et al. Comparative efficacy of exercise regimens on sleep quality in older adults: a systematic review and network meta-analysis. Sleep Med Rev. 2022;65 doi: 10.1016/j.smrv.2022.101673. [DOI] [PubMed] [Google Scholar]
- 22.Xie Y., Liu S., Chen X.-J., Yu H.-H., Yang Y., Wang W. Effects of exercise on sleep quality and insomnia in adults: a systematic review and meta-analysis of randomized controlled trials. Front Psychiatr. 2021:12doi. doi: 10.3389/fpsyt.2021.664499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Riemann D., Baglioni C., Bassetti C., et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675–700. doi: 10.1111/jsr.12594. [DOI] [PubMed] [Google Scholar]
- 24.National Sleep Foundation 2013. https://www.sleepfoundation.org/2013poll National Sleep Foundation 2013 poll. Exercise and Sleep.
- 25.Kok R.M., Reynolds C.F., III Management of depression in older adults: a review. JAMA. 2017;317(20):2114–2122. doi: 10.1001/jama.2017.5706. [DOI] [PubMed] [Google Scholar]
- 26.Rodda J., Walker Z., Carter J. Depression in older adults. BMJ. 2011;343:d5219. doi: 10.1136/bmj.d5219. [DOI] [PubMed] [Google Scholar]
- 27.Bridle C., Spanjers K., Patel S., Atherton N.M., Lamb S.E. Effect of exercise on depression severity in older people: systematic review and meta-analysis of randomised controlled trials. BJPsych. 2012;201(3):180–185. doi: 10.1192/bjp.bp.111.095174. [DOI] [PubMed] [Google Scholar]
- 28.Brupbacher G., Gerger H., Zander-Schellenberg T., et al. The effects of exercise on sleep in unipolar depression: a systematic review and network meta-analysis. Sleep Med Rev. 2021;59 doi: 10.1016/j.smrv.2021.101452. [DOI] [PubMed] [Google Scholar]
- 29.García-Hermoso A., Ramirez-Vélez R., Sáez de Asteasu M.L., et al. Safety and effectiveness of long-term exercise interventions in older adults: a systematic review and meta-analysis of randomized controlled trials. Sports Med. 2020;50(6):1095–1106. doi: 10.1007/s40279-020-01259-y. [DOI] [PubMed] [Google Scholar]
- 30.McPhee J.S., French D.P., Jackson D., Nazroo J., Pendleton N., Degens H. Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology. 2016;17(3):567–580. doi: 10.1007/s10522-016-9641-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Crombie I.K., Irvine L., Williams B., et al. Why older people do not participate in leisure time physical activity: a survey of activity levels, beliefs and deterrents. Age Ageing. 2004;33(3):287–292. doi: 10.1093/ageing/afh089. [DOI] [PubMed] [Google Scholar]
- 32.Birdee G.S., Cai H., Xiang Y.-B., et al. T'ai chi as exercise among middle-aged and elderly Chinese in urban China. J Alternative Compl Med. 2013;19(6):550–557. doi: 10.1089/acm.2012.0223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang C.C., Li K., Choudhury A., Gaylord S. Trends in yoga, Tai Chi, and Qigong use among US adults, 2002-2017. Am J Publ Health. 2019;109(5):755–761. doi: 10.2105/AJPH.2019.304998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cui H., Wang Q., Pedersen M., et al. The safety of tai chi: a meta-analysis of adverse events in randomized controlled trials. Contemp Clin Trials. 2019;82:85–92. doi: 10.1016/j.cct.2019.06.004. [DOI] [PubMed] [Google Scholar]
- 35.Wang C., Collet J.P., Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: a systematic review. Arch Intern Med. 2004;164(5):493–501. doi: 10.1001/archinte.164.5.493. [DOI] [PubMed] [Google Scholar]
- 36.Abbott R., Lavretsky H. Tai Chi and Qigong for the treatment and prevention of mental disorders. Psychiatr Clin. 2013;36(1):109–119. doi: 10.1016/j.psc.2013.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li H., Chen J., Xu G., et al. The effect of Tai Chi for improving sleep quality: a systematic review and meta-analysis. J Affect Disord. 2020;274:1102–1112. doi: 10.1016/j.jad.2020.05.076. [DOI] [PubMed] [Google Scholar]
- 38.Siu P.M., Yu A.P., Tam B.T., et al. Effects of Tai Chi or exercise on sleep in older adults with insomnia: a randomized clinical trial. JAMA Netw Open. 2021;4(2) doi: 10.1001/jamanetworkopen.2020.37199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cuijpers P. Indirect prevention and treatment of depression: an emerging paradigm? Clin Psychol Eur. 2021;3(4) doi: 10.32872/cpe.6847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jetté M., Sidney K., Blümchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol. 1990;13(8):555–565. doi: 10.1002/clc.4960130809. [DOI] [PubMed] [Google Scholar]
- 41.Borg G.A. Psychophysical bases of perceived exertion. Inside MS. 1982;14(5):377–381. [PubMed] [Google Scholar]
- 42.Hui SS-c, Xie Y.J., Woo J., Kwok TC-y. Practicing Tai Chi had lower energy metabolism than walking but similar health benefits in terms of aerobic fitness, resting energy expenditure, body composition and self-perceived physical health. Compl Ther Med. 2016;27:43–50. doi: 10.1016/j.ctim.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 43.Lan C., Chen S.-Y., Lai J.-S. Relative exercise intensity of Tai Chi Chuan is similar in different ages and gender. Am J Chin Med. 2004;32(1):151–160. doi: 10.1142/S0192415X04001746. [DOI] [PubMed] [Google Scholar]
- 44.Lan C., Chen S.Y., Lai J.S., Wong M.K. Heart rate responses and oxygen consumption during Tai Chi Chuan practice. Am J Chin Med. 2001;29(3-4):403–410. doi: 10.1142/s0192415x01000423. [DOI] [PubMed] [Google Scholar]
- 45.Lan C., Chen S.Y., Lai J.S. The exercise intensity of tai chi chuan. Inside MS. 2008;52:12–19. doi: 10.1159/000134225. [DOI] [PubMed] [Google Scholar]
- 46.American College of Sports Medicine . eleventh ed. Lippincott Williams & Wilkins; 2021. ACSM's Guidelines for Exercise Testing and Prescription. [Google Scholar]
- 47.Huang J., Wang D., Wang J. Clinical evidence of Tai Chi exercise prescriptions: a systematic review. eCAM. 2021;2021 doi: 10.1155/2021/5558805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yu A.P., Chin E.C., Yu D.J., et al. Tai Chi versus conventional exercise for improving cognitive function in older adults: a pilot randomized controlled trial. Sci Rep. 2022;12(1):8868. doi: 10.1038/s41598-022-12526-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Siu P.M., Yu A.P., Chin E.C., et al. Effects of Tai Chi or conventional exercise on central obesity in middle-aged and older adults : a three-group randomized controlled trial. Ann Intern Med. 2021;174(8):1050–1057. doi: 10.7326/m20-7014. [DOI] [PubMed] [Google Scholar]
- 50.Snaith R.P. The hospital anxiety and depression scale. Health Qual Life Outcome. 2003;1:29. doi: 10.1186/1477-7525-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Leung C.M., Wing Y.K., Kwong P.K., Lo A., Shum K. Validation of the Chinese-Cantonese version of the hospital anxiety and depression scale and comparison with the Hamilton Rating Scale of Depression. Acta Psychiatr Scand. 1999;100(6):456–461. doi: 10.1111/j.1600-0447.1999.tb10897.x. [DOI] [PubMed] [Google Scholar]
- 52.Bjelland I., Dahl A.A., Haug T.T., Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 53.Wang W., Bian Q., Zhao Y., et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatr. 2014;36(5):539–544. doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 54.Johnson S.U., Ulvenes P.G., Øktedalen T., Hoffart A. Psychometric properties of the general anxiety disorder 7-item (GAD-7) scale in a heterogeneous psychiatric sample. Front Psychol. 2019;10:1713. doi: 10.3389/fpsyg.2019.01713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yu D.S. Insomnia Severity Index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs. 2010;66(10):2350–2359. doi: 10.1111/j.1365-2648.2010.05394.x. [DOI] [PubMed] [Google Scholar]
- 56.Tsai P.S., Wang S.Y., Wang M.Y., et al. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual Life Res. 2005;14(8):1943–1952. doi: 10.1007/s11136-005-4346-x. [DOI] [PubMed] [Google Scholar]
- 57.Dietch J.R., Taylor D.J. Evaluation of the Consensus Sleep Diary in a community sample: comparison with single-channel electroencephalography, actigraphy, and retrospective questionnaire. JCSM. 2021;17(7):1389–1399. doi: 10.5664/jcsm.9200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Matthews K.A., Patel S.R., Pantesco E.J., et al. Similarities and differences in estimates of sleep duration by polysomnography, actigraphy, diary, and self-reported habitual sleep in a community sample. Sleep Health. 2018;4(1):96–103. doi: 10.1016/j.sleh.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lichstein K.L., Peterson B.A., Riedel B.W., Means M.K., Epperson M.T., Aguillard R.N. Relaxation to assist sleep medication withdrawal. BMO. 1999;23(3):379–402. doi: 10.1177/0145445599233003. [DOI] [PubMed] [Google Scholar]
- 60.Lam C.L., Tse E.Y., Gandek B. Is the standard SF-12 health survey valid and equivalent for a Chinese population? Qual Life Res. 2005;14(2):539–547. doi: 10.1007/s11136-004-0704-3. [DOI] [PubMed] [Google Scholar]
- 61.Miller K.J., Areerob P., Hennessy D., Gonçalves-Bradley D.C., Mesagno C., Grace F. Aerobic, resistance, and mind-body exercise are equivalent to mitigate symptoms of depression in older adults: a systematic review and network meta-analysis of randomised controlled trials. F1000Res. 2020;9:1325. doi: 10.12688/f1000research.27123.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Choo Y.T., Jiang Y., Hong J., Wang W. Effectiveness of Tai Chi on quality of life, depressive symptoms and physical function among community-dwelling older adults with chronic disease: a systematic review and meta-analysis. Int J Nurs Stud. 2020;111 doi: 10.1016/j.ijnurstu.2020.103737. [DOI] [PubMed] [Google Scholar]
- 63.Seshadri A., Adaji A., Orth S.S., et al. Exercise, yoga, and Tai Chi for treatment of major depressive disorder in outpatient settings: a systematic review and meta-analysis. Prev Controle Cancerol PCC. 2020;23(1) doi: 10.4088/PCC.20r02722. [DOI] [PubMed] [Google Scholar]
- 64.Yeung A.S., Feng R., Kim D.J.H., et al. A pilot, randomized controlled study of Tai Chi with passive and active controls in the treatment of depressed Chinese Americans. J Clin Psychol. 2017;78(5):e522–e528. doi: 10.4088/JCP.16m10772. [DOI] [PubMed] [Google Scholar]
- 65.Yeung A., Lepoutre V., Wayne P., et al. Tai chi treatment for depression in Chinese Americans: a pilot study. Am J Phys Med Rehabil. 2012;91(10):863–870. doi: 10.1097/PHM.0b013e31825f1a67. [DOI] [PubMed] [Google Scholar]
- 66.Lo C.M., Lee P.H. Feasibility and effects of TAI CHI for the promotion of sleep quality and quality of life: a single-group study in a sample of older Chinese individuals in Hong Kong. J Gerontol Nurs. Mar 2014;40(3):46–52. doi: 10.3928/00989134-20131028-08. [DOI] [PubMed] [Google Scholar]
- 67.Stubbs B., Vancampfort D., Rosenbaum S., et al. Dropout from exercise randomized controlled trials among people with depression: a meta-analysis and meta regression. J Affect Disord. 2016;190:457–466. doi: 10.1016/j.jad.2015.10.019. [DOI] [PubMed] [Google Scholar]
- 68.Tseng T.H., Chen H.C., Wang L.Y., Chien M.Y. Effects of exercise training on sleep quality and heart rate variability in middle-aged and older adults with poor sleep quality: a randomized controlled trial. JCSM. 2020;16(9):1483–1492. doi: 10.5664/jcsm.8560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.King A.C., Pruitt L.A., Woo S., et al. Effects of moderate-intensity exercise on polysomnographic and subjective sleep quality in older adults with mild to moderate sleep complaints. J Gerontol A Biol Sci Med Sci. 2008;63(9):997–1004. doi: 10.1093/gerona/63.9.997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Perlis M.L., Smith M.T. How can we make CBT-I and other BSM services widely available? JCSM. 2008;4(1):11–13. [PMC free article] [PubMed] [Google Scholar]
- 71.Smith Michael T., Perlis Michael L., Park Amy, et al. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. Am J Psychiatr. 2002;159(1):5–11. doi: 10.1176/appi.ajp.159.1.5. [DOI] [PubMed] [Google Scholar]
- 72.Fitzgerald T., Vietri J. Residual effects of sleep medications are commonly reported and associated with impaired patient-reported outcomes among insomnia patients in the United States. Sleep Disord. 2015;2015 doi: 10.1155/2015/607148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bridle C., Spanjers K., Patel S., Atherton N.M., Lamb S.E. Effect of exercise on depression severity in older people: systematic review and meta-analysis of randomised controlled trials. BJPsych. Sep 2012;201(3):180–185. doi: 10.1192/bjp.bp.111.095174. [DOI] [PubMed] [Google Scholar]
- 74.Smith P.J., Merwin R.M. The role of exercise in management of mental health disorders: an integrative review. Annu Rev Med. 2021;72:45–62. doi: 10.1146/annurev-med-060619-022943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wegner M., Helmich I., Machado S., Nardi A.E., Arias-Carrion O., Budde H. Effects of exercise on anxiety and depression disorders: review of meta- analyses and neurobiological mechanisms. CNS Neurol Disord: Drug Targets. 2014;13(6):1002–1014. doi: 10.2174/1871527313666140612102841. [DOI] [PubMed] [Google Scholar]
- 76.Wayne P.M., Kaptchuk T.J. Challenges inherent to t'ai chi research: part I--t'ai chi as a complex multicomponent intervention. J Alternative Compl Med. 2008;14(1):95–102. doi: 10.1089/acm.2007.7170a. [DOI] [PubMed] [Google Scholar]
- 77.Taylor-Piliae R.E., Newell K.A., Cherin R., Lee M.J., King A.C., Haskell W.L. Effects of Tai Chi and Western exercise on physical and cognitive functioning in healthy community-dwelling older adults. J Am Psychoanal Assoc (JAPA) 2010;18(3):261–279. doi: 10.1123/japa.18.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cui L., Yin H., Lyu S., et al. Tai Chi Chuan vs general aerobic exercise in brain plasticity: a multimodal MRI study. Sci Rep. 2019;9(1) doi: 10.1038/s41598-019-53731-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zenebe Y., Akele B., Ws M., Necho M. Prevalence and determinants of depression among old age: a systematic review and meta-analysis. Ann Gen Psychiatr. 2021;20(1):55. doi: 10.1186/s12991-021-00375-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Foley D.J., Monjan A.A., Brown S.L., Simonsick E.M., Wallace R.B., Blazer D.G. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18(6):425–432. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- 81.Agustini B., Lotfaliany M., Woods R.L., et al. Patterns of association between depressive symptoms and chronic medical morbidities in older adults. JAGS. 2020;68(8):1834–1841. doi: 10.1111/jgs.16468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mookerjee N., Schmalbach N., Antinori G., et al. Comorbidities and risk factors associated with insomnia in the elderly population. J Prim Care Community Health. 2023;14 doi: 10.1177/21501319231168721. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data collected for this study is available upon request.