Abstract
Background
The Middle East and North Africa (MENA) region faces unique challenges in promoting physical activity and reducing sedentary behaviors, as the prevalence of insufficient physical activity is higher than the global average. Mobile technologies present a promising approach to delivering behavioral interventions; however, little is known about the effectiveness and user perspectives on these technologies in the MENA region.
Objective
This study aims to evaluate the effectiveness of mobile interventions targeting physical activity and sedentary behaviors in the MENA region and explore users’ perspectives on these interventions as well as any other outcomes that might influence users’ adoption and use of mobile technologies (eg, appropriateness and cultural fit).
Methods
A systematic search of 5 databases (MEDLINE, Embase, CINAHL, Scopus, and Global Index Medicus) was performed. Any primary studies (participants of all ages regardless of medical condition) conducted in the MENA region that investigated the use of mobile technologies and reported any measures of physical activity, sedentary behaviors, or user perceptions were included. We conducted a narrative synthesis of all studies and a meta-analysis of randomized controlled trials (RCTs). The Cochrane risk-of-bias tool was used to assess the quality of the included RCTs; quality assessment of the rest of the included studies was completed using the relevant Joanna Briggs Institute critical appraisal tools.
Results
In total, 27 articles describing 22 interventions (n=10, 37% RCTs) and 4 (15%) nonexperimental studies were included (n=6141, 46% women). Half (11/22, 50%) of the interventions included mobile apps, whereas the other half examined SMS. The main app functions were goal setting and self-monitoring of activity, whereas SMS interventions were primarily used to deliver educational content. Users in experimental studies described several benefits of the interventions (eg, gaining knowledge and receiving reminders to be active). Engagement with the interventions was poorly reported; few studies (8/27, 30%) examined users’ perspectives on the appropriateness or cultural fit of the interventions. Nonexperimental studies examined users’ perspectives on mobile apps and fitness trackers, reporting several barriers to their use, such as perceived lack of usefulness, loss of interest, and technical issues. The meta-analysis of RCTs showed a positive effect of mobile interventions on physical activity outcomes (standardized mean difference=0.45, 95% CI 0.17-0.73); several sensitivity analyses showed similar results. The trim-and-fill method showed possible publication bias. Only 20% (2/10) of the RCTs measured sedentary behaviors; both reported positive changes.
Conclusions
The use of mobile interventions for physical activity and sedentary behaviors in the MENA region is in its early stages, with preliminary evidence of effectiveness. Policy makers and researchers should invest in high-quality studies to evaluate long-term effectiveness, intervention engagement, and implementation outcomes, which can inform the design of culturally and socially appropriate interventions for countries in the MENA region.
Trial Registration
PROSPERO CRD42023392699; https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=392699
Keywords: mobile apps; fitness trackers; SMS; SMS text messaging; physical activity; exercise; sedentary behavior; Middle East; Africa, Northern; movement; physical inactivity; smartphone; mobile phone; mobile health; mHealth; digital health; behavior change; intervention
Introduction
Background
Chronic diseases were responsible for >70% of deaths worldwide in 2019, making them the leading cause of mortality and morbidity [1]. In the Middle East and North Africa (MENA) region [2], chronic conditions accounted for 79% of deaths in 2020 [3]. Although there are many factors contributing to the prevalence of chronic diseases, physical inactivity and sedentary behaviors are well-established risk factors [4-8]. Worldwide studies have revealed that the MENA region has higher rates of physical inactivity compared with the global average, with 32.8% of adults and 85% of adolescents considered insufficiently active compared with 28% of adults and 81% of adolescents worldwide [9,10].
There are specific factors unique to the MENA region that might influence physical inactivity and sedentary behaviors, such as environmental conditions or infrastructure. Specifically, extreme weather conditions, particularly during the hot summer months, can make outdoor exercise uncomfortable or even hazardous [11,12]. Limited access to sports facilities is another barrier to physical activity, and high urbanization associated with dependence on motor vehicles likely increases sedentary time [11,12]. Given these regional factors, interventions targeting physical activity and sedentary behaviors in the MENA region need to be tailored to a regional and population context.
Mobile interventions such as mobile apps, fitness trackers, and SMS text messages can be a powerful tool for promoting physical activity and reducing sedentary behaviors. The high mobile penetration rate in the MENA region [13,14] makes mobile technologies a possible solution for delivering large-scale real-time interventions. Moreover, the advanced capability of these technologies to automate and process data can allow interventions to be tailored according to the specific individual, context, and region [15-18]. Mobile apps or fitness trackers can also incorporate theory-based behavior change techniques that are known to be effective [19], such as automating self-monitoring of activity and providing feedback or allowing users to set goals.
Despite this potential, to date, little is known about the effectiveness of mobile technologies targeting physical activity and sedentary behaviors in the MENA region. Although some systematic reviews have reported a positive effect of mobile technologies on behavioral outcomes [18,20-31], none of these studies have focused on evidence from the MENA region. A systematic review explored physical activity interventions in 6 Arabian Gulf countries (ie, Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, and United Arab Emirates) [32]—a subset of the MENA region—but did not solely focus on mobile interventions or explore interventions for sedentariness. Thus, it remains unclear whether mobile technologies are particularly effective in changing physical activity and sedentary behaviors in the MENA region. In addition, given the unique barriers that the MENA population faces, there is also a need to understand users’ acceptability and the implementation outcomes of these mobile interventions (eg, the appropriateness or cultural fit of the interventions). Finally, it is worth noting that there is diversity among the countries in the MENA region regarding income level, economic and social stability [2], and mobile penetration rate [14]. Socioeconomic disparities have been linked to inequitable access to technologies and varying levels of digital literacy, creating a “digital divide” [33-35]. Understanding the geographical scope of mobile health research in the MENA region is crucial to gauge whether findings are applicable across the region and identify potential signs of a digital divide.
Objectives
The aim of this systematic review and meta-analysis was to summarize the characteristics and evaluate the effectiveness of mobile interventions targeting physical activity and sedentary behaviors in the MENA region. A secondary aim was to explore users’ perspectives on these interventions as well as any other outcomes that might influence users’ adoption and use of mobile technologies (eg, appropriateness and cultural fit).
Methods
This systematic review is reported in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 statement (Multimedia Appendix 1 [36]). We followed the protocol registered in PROSPERO (CRD42023392699).
Search Strategy
A systematic search of the literature was conducted in MEDLINE, Embase, CINAHL, Scopus, and Global Index Medicus from database inception to January 19, 2023. The search strategy was developed after consultation with a research librarian and comprised three strings: (1) mobile technology terms, (2) physical activity and sedentary behavior terms, and (3) MENA countries (Multimedia Appendix 2). The reference lists of relevant articles and other reviews on similar topics were also screened to ensure that all eligible studies were captured. A gray literature search was performed using Google Scholar. We contacted the authors to obtain additional information when needed. We also contacted the authors to request the full text when it was not available. If the authors did not provide the full text, we excluded the studies.
Eligibility Criteria
We included studies that met the following population, intervention, comparator, outcome, and study design criteria: (1) participants of all ages regardless of medical condition, (2) interventions that used mobile technologies (ie, mobile apps, fitness trackers, or SMS text messages), (3) presence or absence of a comparator, (4) any outcomes related to physical activity or sedentary behaviors (eg, active minutes and sitting time) or to users’ perceptions of mobile technologies, (5) conducted in MENA countries as listed by the World Bank [2], and (6) primary research studies (eg, randomized controlled trials [RCTs], quasi-experimental studies, or qualitative studies). Studies in all languages were included.
Studies were excluded if (1) the intervention did not have a mobile technology component (eg, web-based only) or (2) they only reported measures related to physical function (eg, sit-to-stand test). Multimedia Appendix 3 [2,20,37] provides a detailed outline of the eligibility criteria.
Screening and Data Extraction
The screening procedure was piloted before beginning. In total, 4 pairs of investigators independently conducted a 2-phase screening using Rayyan (Rayyan Systems, Inc) [38] for title and abstract and full text. Disagreements were resolved through discussion.
The data extraction form was developed in Microsoft Excel (Microsoft Corp) and piloted before extraction. The following data were collected for each study: author; year; country; study design; study population, sample size, participant demographics, and baseline characteristics; details of the intervention and control conditions; retention rates (ie, percentage that completed the follow-up assessment); outcomes and times of measurement; and source of funding and conflicts of interest. Data were extracted by one researcher and checked for accuracy by another. RCTs were assessed by 2 independent researchers using the Cochrane risk-of-bias tool [39], and disagreements were resolved through discussion. To assess outcome reporting bias, we compared the outcomes specified in the trial protocols with the outcomes reported in the corresponding trial publications; if the trial protocols were unavailable, we compared the outcomes reported in the methods and results sections of the trial publications. Quality assessment of the rest of the included studies was completed using the Joanna Briggs Institute (JBI) critical appraisal tools, including the checklists for quasi-experimental studies, cross-sectional studies, and qualitative research [40].
Strategies for Data Synthesis
A narrative synthesis was conducted of all included studies. A meta-analysis was conducted for RCTs in which the control group did not have a mobile technology component. This was because the study aimed to examine the effectiveness of mobile technologies on physical activity or sedentary behaviors compared with nonmobile interventions. Cluster randomized trials were also included in the meta-analysis by calculating the effective sample size using the Cochrane guideline [41] (Multimedia Appendix 4 [42,43]). We planned to perform 2 separate meta-analyses to combine outcome measures of physical activity and sedentary behaviors. However, only 2 trials measured sedentary behaviors; given this small number, a meta-analysis was used to combine physical activity outcomes only. Sedentary outcomes were summarized narratively.
Whenever a single study reported multiple outcomes for the same behavior (eg, reporting both daily step count and daily active minutes for physical activity), the outcome that was included in the meta-analysis was selected through the consensus of the authors favoring (1) the included studies’ primary outcomes, (2) the most meaningful outcomes to intended users (eg, step count), and (3) the longest follow-up. All reported outcomes (from data collected after the intervention) were pooled, and all effect sizes were transformed into standardized mean differences. We used a random-effects model for all analyses; the restricted maximum likelihood estimator was used to calculate the heterogeneity variance (τ2). To assess heterogeneity, I2 was used.
The presence and potential impact of publication bias were explored using a funnel plot, the Egger test, and the trim-and-fill method by Duval and Tweedie [44]. In total, 2 sensitivity analyses were conducted including only (1) studies that were randomized at the individual level and (2) studies that had a low risk of bias in at least 3 out of 5 categories. Owing to an insufficient number of studies, a planned meta-regression was not conducted. We used the Grading of Recommendations Assessment, Development, and Evaluation system for grading the body of evidence [45]. All computations were conducted in R (version 4.2.3; R Foundation for Statistical Computing) [46]. The 2-tailed significance level for all statistical tests was set at P<.05.
Results
Study Selection
The search retrieved 2038 unique articles (Figure 1). After abstract and full-text screening, 23 articles were included. Multimedia Appendix 5 provides a list of excluded studies at full-text screening. In total, 2 articles were found through the reference lists of relevant articles, and 2 were included from the Google Scholar search. Finally, the systematic review included 27 articles: 11 (41%) articles describing 10 unique RCT studies (n=2, 20% cluster RCTs [42,43,47]) [42,43,47-55], 12 (44%) quasi-experimental studies [56-67], 3 (11%) surveys [68-70], and 1 (4%) interview study [71] (Tables 1-3).
Figure 1.
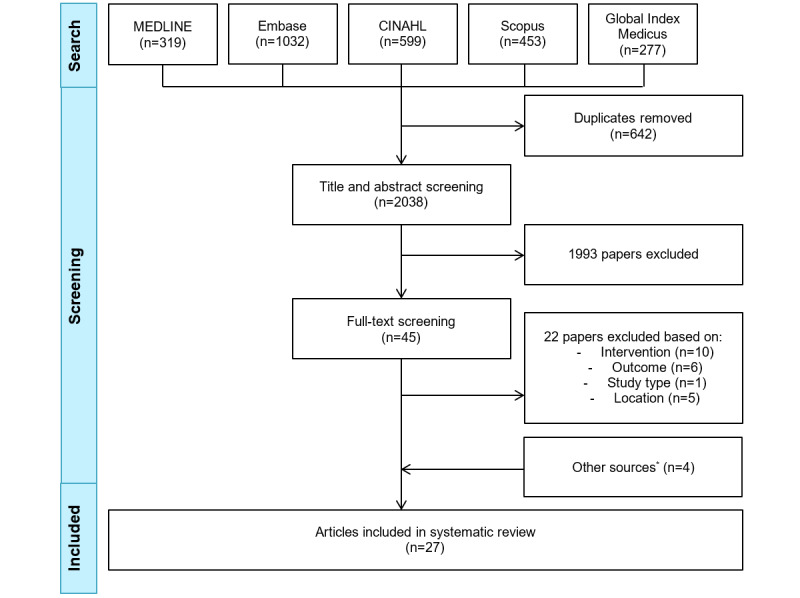
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram of the study selection process. *Other sources include reference lists of relevant articles (n=2) and Google Scholar (n=2).
Table 1.
Study and intervention characteristics of the included randomized controlled trials (RCTs).
| Study, year, and country | Study population | Study length | Sample size, N | Female participants, n (%) | Age (y), mean | Details about the intervention | Details about the control |
| Ansari et al [55], 2022, Iran | Women aged 40-60 y | 12 wk | IGa: 55; CGb: 55 | 110 (100) | 52 | The sample was divided into 2 groups: SMS text messaging or mobile social networking app; both received information about benefits and how to overcome potential barriers to physical activity. | No true control |
| Eslami et al [50], 2022, Iran | Pregnant women with overweight and obesity (ie, BMI >25 kg/m2) | 8 wk | IG: 70; CG: 70 | 140 (100) | NRc; >55% in the 20-30–y age group | SMS text messages about physical activity (recommendations of amount and intensity, benefits, safe exercises, and precautions during pregnancy), diet, and supplements; educational booklet; and 1 face-to-face training session | Usual care |
| Saleh et al [48], 2022, Jordan | Patients with heart failure | 8 wk | IG: 76; CG: 76 | 52 (39) | 60.8 | 2 apps: Samsung Health app (goal setting and self-monitoring of activity) and social media app (posts about the benefits of physical activity, exercise videos, and discussion forum with a health expert; participants were encouraged to post and comment in the group) | Usual care; participants also received the setup for the Samsung Health app without receiving details about its features |
| Alshahrani et al [49], 2021, Saudi Arabia | Female university students | 10 wk | IG: 53; CG: 50 | 103 (100) | NR; 70% were aged ≥20 y | WhatsApp group: a 15-min orientation and 3-4 messages/wk about physical activity | No intervention |
| Abbaspoor et al [51], 2020, Iran | Pregnant women with prediabetes | 12 wk | IG: 50; CG: 50 | 100 (100) | IG: 27.8; CG: 29 | 2 SMS text messages every second day about gestational diabetes and 4 face-to-face training sessions | 4 face-to-face training sessions |
| Alghafri et al [43,47], 2020 and 2018, Oman | Inactive adults with type 2 diabetes | 1 y | Cluster RCT; IG: 122; CG: 110 | 137 (59) | 44 | Monthly WhatsApp messages, 3 face-to-face 20-min consultations about physical activity, and pedometers | Usual care |
| Parandeh et al [52], 2019, Iran | Women aged 30-45 y | 8 wk | IG: 63; CG: 63 | 126 (100) | IG: 36.1; CG: 35.8 | Daily SMS text messages about osteoporosis prevention (including physical activity and diet) | Educational SMS text messages about cancers in women |
| Quronfulah [42], 2019, Saudi Arabia | Male office workers | 12 wk | Cluster RCT; IG: 33; CG: 33 | 0 (0) | 43.5 | Weekly SMS text messages targeting self-efficacy and self-regulation of physical activity, workplace computer prompts to take a break, videos of short bursts of exercise, and group and 1-1 educational sessions | No intervention |
| Alsaleh et al [53], 2016, Jordan | Outpatients with coronary heart disease | 26 wk | IG: 71; CG: 85 | 72 (46) | IG: 57.7; CG: 58 | SMS text messages (2/wk for the first 3 mo and 1/wk for the last 3 mo) with reminders to be active and meet personal goals; 1 face-to-face consultation to discuss barriers and facilitators and increase self-efficacy for physical activity; 6 phone calls to provide tailored feedback, review goals, and discuss any arising barriers; and paper diary to self-monitor physical activity | Usual care |
| Goodarzi et al [54], 2012, Iran | Adults with type 2 diabetes aged >30 y | 12 wk | IG: 43; CG: 38 | 63 (77) | IG: 51; CG: 56.7 | 4 SMS text messages/wk about exercise, diet, diabetes medication, and importance of self-monitoring blood glucose levels | No intervention |
aIG: intervention group.
bCG: control group.
cNR: not reported.
Table 3.
Study information and summary of users’ perspectives and experiences in nonexperimental studies.
| Study, year, and country | Study population | Study design | Sample size, N | Female participants, n (%) | Age (y), mean | Mobile technologies examined | Main findings |
| Al Ansari et al [68], 2023, Saudi Arabia | People aged >15 y | Survey | 195 | 122 (63) | NRa; 40% were aged >40 y | Mobile apps |
|
| Altabtabaei and Alhuwail [71], 2021, Kuwait | Students | Interviews | 20 | NR | NR | Fitness trackers |
|
| Bardus et al [69], 2021, Lebanon | Student athletes | Survey | 200 | 70 (35) | 20 | Mobile apps and fitness trackers |
|
| Zaman et al [70], 2021, Saudi Arabia | People with sleep problems | Survey | 45 | 23 (51) | NR; 51% were aged 20-30 y | Mobile apps |
|
aNR: not reported.
bNS: not significant.
Description of All Studies
Most of the included studies were conducted in Iran [50-52,54,55,57,59,62,64,65] (10/27, 37%) or Saudi Arabia [42,49,56,58,63,66,68,70] (8/27, 30%). In total, 7% (2/27) of the studies were conducted in Jordan [48,53] and Oman [43,47], and 4% (1/27) of the studies were conducted in Egypt [61], Kuwait [71], Lebanon [69], Qatar [60], and the United Arab Emirates each [67]. The included studies were published between 2012 and 2023. The average duration of experimental studies was 20 (SD 14.4; range 6-52) weeks. The total number of participants was 6141 (1/27, 4% of the studies had 2600 participants). Among the study participants, 46% were women; 7% (2/27) of the studies did not report gender distribution [60,71]. A total of 33% (9/27) of the studies were conducted in populations with chronic conditions, including cardiovascular diseases [48,53,61], diabetes [54,58,59,64,66], and sleep problems [70]. The funding sources and conflicts of interest are summarized in Multimedia Appendix 6 [42,43,47-71].
Description of the Included Experimental Studies
Description of the Interventions
Half (11/22, 50%) of the interventions included a mobile app as a component [43,47-49,55-58,60-63,67]; 36% (4/11) of them used WhatsApp [43,47,49,57,58] (Tables 1 and 2). The other commercial apps used were Samsung Health [48] and Telegram [56,62]. In total, 19% (5/27) of the studies examined apps designed by the authors [55,60,61,63,67]. The main functions of mobile apps were to set goals, self-monitor activity, and receive educational information about physical activity [43,47-49,55-58,60-63,67]. Half (11/22, 50%) of the interventions used SMS text messaging to deliver educational content [42,50-55,59,64-66]; the frequency of delivery varied from 2 messages per day to 1 message per week.
Table 2.
Study and intervention characteristics of the included quasi-experiments.
| Study, year, and country | Study population | Study length | Sample size, N | Female participants, n (%) | Age (y), mean | Details about the intervention and control (if applicable) | Physical activity and other outcomes |
| Al-Daghri et al [56], 2022, Saudi Arabia | Adolescents aged 12-16 y | 12 mo | 1 arm: 2600 | 343 (53) | 14.8 |
|
|
| Ghofranipour et al [57], 2022, Iran | Mothers of children aged 3-5 y | 6 wk | 1 arm: 13 | 13 (100) | Mothers: 38; children: 4 |
|
|
| Ali et al [67], 2021, United Arab Emirates | Female university students with overweight or obesity aged 18-35 y | 16 wk | 2 arms—website: 54; website+app: 111 | 246 (100) | 22 |
|
|
| Alyousef [58], 2021, Saudi Arabia | Women with type 2 diabetes | 8 wk | 1 arm: 20 | 20 (100) | 54.8 |
|
|
| Biglar Chopoghlo et al [59], 2021, Iran | Female adolescents aged 14-18 y with type 1 diabetes | 12 wk | 2 arms—IGc: 38; CGd: 38 | 76 (100) | 15.9 |
|
|
| Khidir et al [60], 2021, Qatar | University staff and students | 2 phases, 16 wk each | 288 in phase 1 and 109 in phase 2 | NRf; 56 women participated in both phases | NR |
|
|
| Yahia and Bayoumi [61], 2021, Egypt | Outpatients with type 2 diabetes | 12 wk | 1 arm: 150 | 63 (42) | 40.3 |
|
|
| Jorvand et al [62], 2020, Iran | Health care workers | 6 mo | 2 arms—IG: 59; CG: 55 | 57 (50) | IG: 37.6; CG: 37.5 |
|
|
| Alnasser et al [63], 2019, Saudi Arabia | Women with overweight or obesity | 16 wk | 1 arm: 240 | 240 (100) | 31 |
|
|
| Lari et al [64], 2018, Iran | Outpatients with type 2 diabetes | 12 wk | IG: 40; CG: 40 | 34 (47) | IG: 46.1; CG: 49.1 |
|
|
| Peyman et al [65], 2018, Iran | Women | 6 mo | 2 arms—IG: 180; CG: 180 | 360 (100) | IG: 33.4; CG: 31.9 |
|
|
| Sani et al [66], 2018, Saudi Arabia | People who were diagnosed with type 2 diabetes within the last 5 y | 6 mo | 2 arms—IG: 100; CG: 100 | 100 (50) | NR; 75% were in the 30-49–y age group |
|
|
aNS: not significant.
bHbA1c: glycated hemoglobin.
cIG: intervention group.
dCG: control group.
eMMS: Multimedia Messaging Service.
fNR: not reported.
gMET: metabolic equivalent of task.
In total, 36% (8/22) of the interventions also included a nonmobile component; the most popular were face-to-face sessions [42,43,47,50,51,53,60,66] (Tables 1 and 2). Other nonmobile components included websites [65,67], phone calls [53], computer prompts [42], pedometers [43,47,60], and an educational booklet and CD [50,65]. In total, 37% (10/27) of the studies mentioned that the interventions were designed using behavior change theories [42,43,48,51,53,57,58,63,64,67], the most popular being social cognitive theory (4/10, 40%) [42,53,63,67]. Self-efficacy constructs [53,57] and the health promotion model [58,64] were used in 20% (2/10) of the studies each.
Description of the Control Groups
Of the 10 included RCTs, 3 (30%) had a true control group (ie, no intervention) [42,49,54] (Table 1). A total of 30% (3/10) had an active mobile control [48,52,55]. Specifically, in 10% (1/10) of the studies, the control group received usual care (ie, clinical consultation) as well as the Samsung Health app without being told about its features [48]; the intervention was guided by the theory of planned behavior. In another study, the intervention group received daily SMS text messages about physical activity, whereas the control group received educational SMS text messages about cancers; no theory was mentioned [52]. In the third study, the content of the intervention and comparator arms used the same behavior change techniques (ie, information about health consequences), the only difference being the delivery platform (ie, mobile app vs SMS text messaging); no theory was mentioned [55]. A total of 40% (4/10) of the RCTs had nonmobile controls [43,47,50,51,53]; all mentioned the use of a theory. In total, 75% (3/4) of these RCTs involved usual care in the control arm [43,47,50,53], and 25% (1/4) involved face-to-face education [51].
A total of 50% (6/12) of the quasi-experiments also had a control arm, of which 33% (2/6) were true controls (ie, no intervention [62,65]) and 33% (2/6) were usual care [64,66]. A total of 33% (2/6) of the studies involved an active digital control. In one study, the control group received SMS text messages that were not related to physical activity [59]; no theory was mentioned. In another study, the control group had access to a website with the self-monitoring, receiving feedback, goal setting, and information about health consequences behavior change techniques [67]; social cognitive theory was used to develop the intervention.
Engagement and Retention Metrics
None of the included RCTs reported metrics of engagement with the interventions. A total of 25% (3/12) of the quasi-experiments reported engagement metrics [57,60,63]. Specifically, one study reported that 23% (3/13) of mothers watched all videos delivered via WhatsApp (Multimedia Appendix 6) [57]. Another study reported a higher use of mobile apps than pedometers to monitor activity [60]. One study measured use rates and reported that, at 6 months, 55% (26/47) of the participants used the app at least once every 2 weeks [63].
The retention rate in the intervention groups ranged from 18% to 100%. The average retention rate for the intervention arms was 85%, with most falling within the 86% to 100% range. A total of 22% (6/27) of the studies had a 100% retention rate [50,55,57,61,62,65], and 7% (2/27) had a retention rate of <25% [56,63] (Multimedia Appendix 6).
Users’ Perspectives in Experimental Studies
Of the 27 studies, 4 (15%) experimental studies (n=3, 75% RCTs [42,47,53] and n=1, 25% quasi-experiments [58]) examined users’ perspectives and experiences with the mobile interventions (Table 2 and Multimedia Appendix 7 [42,43,47-67]). Most of the participants reported finding the interventions useful; some reported benefits such as gaining knowledge about how to change their behaviors, receiving reminders to be more active, and building a relationship with clinicians [53]. One study reported barriers to using the mobile intervention such as lack of reliable internet connection and lack of time and an appropriate place to exercise [58]. In one study, participants mentioned a preference for the intervention material to be linguistically adapted [67].
Users’ Perspectives in Nonexperimental Studies
Of the 4 nonexperimental studies, 2 (50%) examined the role of mobile apps [68,70], 1 (25%) focused on fitness trackers [71], and 1 (25%) investigated both [69] (Table 3). A total of 50% (2/4) of the studies found that the main purpose of use was to self-monitor their activity [69,71]. Barriers to adoption and use included perceived lack of usefulness, lack of knowledge about potential benefits, loss of interest, and technical issues [69,71]. One survey found that people aged <40 years reported higher perceived ease of use than those aged >40 years [68]. A survey of people with sleep problems reported improved physical activity after using a health app [70].
Quality Assessment
The risk of bias was assessed as low in 3 out of 5 categories in half (5/10, 50%) of the included RCTs [43,48,50,53,55] (Table 4). Half (5/10, 50%) of the included RCTs described a low-risk randomization process [48,51-53,55]. In 20% (2/10) of the trials, the allocation sequence was not concealed until participants were enrolled [42,49]. Of the 10 RCTs, 2 (20%) cluster RCTs were assessed as low risk in an additional domain (ie, “timing of identification or recruitment of participants”). The risk of “deviations from intended interventions” was assessed as low in 40% (4/10) of the studies [43,50,53,55], there were “some concerns” in 40% (4/10) of the studies [42,48,51,52], and the risk was high in 20% (2/10) of the studies as an appropriate analysis (eg, intention-to-treat) was not used. Half (5/10, 50%) of the included RCTs had a low level of incomplete data [42,43,47,48,55], whereas the other half were assessed as having some concerns [49,51-54]. Most of the studies (7/10, 70%) were assessed as having some concerns regarding the measurement of the outcomes because of the self-report nature, and participants (ie, outcome assessors in this case) were aware of the intervention allocation [43,49-51,53-55]. More than half (6/10, 60%) of the included studies scored as having a low risk in the selection of the reported results [43,49-51,53,55], whereas 40% (4/10) of the studies were assessed as having some concerns because of the lack of details regarding a preplanned analysis [42,48,52,54].
Table 4.
Risk-of-bias assessment of the included randomized controlled trials. Green: low risk; yellow: some concerns; red: high risk.
| Study, year | Randomization process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported result | Overall |
| Abbaspoor et al [51], 2020 |

|

|

|

|

|

|
| Alghafri et al [43], 2018 |

|

|

|

|

|

|
| Alsaleh et al [53], 2016 |

|

|

|

|

|

|
| Alshahrani et al [49], 2021 |

|

|

|

|

|

|
| Ansari et al [55], 2022 |

|

|

|

|

|

|
| Eslami et al [50], 2022 |

|

|

|

|

|

|
| Goodarzi et al [54], 2012 |

|

|

|

|

|

|
| Parandeh et al [52], 2019 |

|

|

|

|

|

|
| Quronfulah [42], 2019 |

|

|

|

|

|

|
| Saleh et al [48], 2022 |

|

|

|

|

|

|
Table 5 provides a summary of the quality assessment of the quasi-experimental studies using the JBI checklist for quasi-experiments. All 12 quasi-experimental studies [56-67] made clear what was the cause versus the effect (question 1), had multiple measurements of the outcome both before and after the intervention (question 5), and measured the outcomes of participants in the comparison groups in the same way as those of participants in the intervention groups (question 7). In all except one study (11/12, 92%) where this was unclear [67], participants in the comparison group were similar to participants in the intervention group. In one study [65], it was unclear whether participants in the comparison group received similar treatment; the other 92% (11/12) of the studies met this criterion (question 3). In half (6/12, 50%) of the studies, there was no control group (question 4). Only 8% (1/12) of the studies provided information about whether follow-up was complete and how follow-up data were treated [62] (question 6). In total, 83% (10/12) of the studies measured outcomes in a reliable way; this information was unclear in 17% (2/12) of the studies [57,61] (question 8). Appropriate statistical analyses were conducted in 92% (11/12) of the studies; this was unclear in 8% (1/12) of the studies [61] (question 9).
Table 5.
Quality assessment of the included quasi-experimental studies.
| Study, year | Q1a | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 |
| Al-Daghri et al [56], 2022 | Yb | Y | Y | Nc | Y | Ud | Y | Y | Y |
| Ghofranipour et al [57], 2022 | Y | Y | Y | N | Y | U | Y | U | Y |
| Ali et al [67], 2021 | Y | U | Y | Y | Y | N | Y | Y | Y |
| Alyousef [58], 2021 | Y | Y | Y | N | Y | U | Y | Y | Y |
| Biglar Chopoghlo et al [59], 2021 | Y | Y | Y | Y | Y | N | Y | Y | Y |
| Khidir et al [60], 2021 | Y | Y | Y | N | Y | U | Y | Y | Y |
| Yahia and Bayoumi [61], 2021 | Y | Y | Y | N | Y | U | Y | U | U |
| Jorvand et al [62], 2020 | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Alnasser et al [63], 2019 | Y | Y | Y | N | Y | N | Y | Y | Y |
| Lari et al [64], 2018 | Y | Y | Y | Y | Y | N | Y | Y | Y |
| Peyman et al [65], 2018 | Y | Y | U | Y | Y | U | Y | Y | Y |
| Sani et al [66], 2018 | Y | Y | Y | Y | Y | N | Y | Y | Y |
aQ: question.
bY: yes.
cN: no.
dU: unclear.
The survey studies (3/27, 11%) [68-70] were assessed using the JBI checklist for cross-sectional studies (Table 6). The criteria for inclusion were not clearly defined in those 3 studies (question 1). The study participants and settings were described in detail in 67% (2/3) of the studies [68,69] (question 2). Owing to poor reporting, it was unclear in all 3 studies whether exposure and outcomes were measured in a valid and reliable way (questions 3 and 7) and whether confounding factors and strategies to deal with them were identified (questions 5 and 6). In 33% (1/3) of the studies, appropriate statistical analysis was used (question 9).
Table 6.
Quality assessment of the included survey studies.
| Study, year | Q1a | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 |
| Al Ansari et al [68], 2023 | Nb | Yc | Ud | N/Ae | U | U | U | U |
| Bardus et al [69], 2021 | N | Y | U | N/A | U | U | U | Y |
| Zaman et al [70], 2021 | N | N | U | N/A | U | U | U | U |
aQ: question.
bN: no.
cY: yes.
dU: unclear.
eN/A: not applicable.
The interview study [71] was assessed using the JBI checklist for qualitative research. It was assessed as meeting the criteria in 5 domains (ie, congruity between the research methodology and the research question, congruity between the research methodology and the methods to collect data, congruity between the research methodology and the representation and analysis of data, representation of participants and their voices, and ethics approval by an appropriate body). In total, 3 domains were unclear (ie, congruity between the stated philosophical perspective and the research methodology, congruity between the research methodology and the interpretation of results, and the relationship between the conclusions and the analysis or interpretation of the data). There was no statement locating the researcher culturally or theoretically or on the influence of the researcher on the study.
Meta-Analysis of RCTs and Outcomes in Quasi-Experiments
Of the 10 included RCTs, 7 (70%) were deemed eligible for inclusion in the meta-analysis of physical activity outcomes. Specifically, 20% (2/10) of the RCTs were excluded because they had a mobile component in the control arm [48,55], and 10% (1/10) were excluded for only reporting behavioral practices regarding diabetes care (combining physical activity and other health measures) [54]. In line with the strategies for data synthesis, for 71% (5/7) of the studies [43,49-52], the measures of metabolic equivalent of task minutes per week were included in the meta-analysis; for the other 29% (2/7) of the studies, the duration of moderate to vigorous physical activity was included [42,53].
The meta-analysis showed a positive effect of mobile interventions on physical activity outcomes (standardized mean difference=0.45, 95% CI 0.17-0.73; Figure 2 [42,43,49-53]). The I2 was 74%, indicating a high heterogeneity. One study in particular [42] seemed to be the source of high heterogeneity. This was the only study that delivered an intervention in the workplace, with part of the intervention including regular computer prompts throughout the day. The high frequency of the computer prompts might have had an effect on behavior changes. The funnel plot appeared to indicate signs of publication bias (Multimedia Appendix 8). The Egger test had an intercept of 3.65 (P=.02), indicating possible publication bias. The trim-and-fill method imputed an effect size of 0.30 (95% CI −0.65 to 1.25), indicating a possible nonsignificant effect. In total, 3 sensitivity analyses were conducted, including only (1) studies that were randomized at the individual level and (2) studies that had a low risk of bias in at least 3 categories and excluding the study by Quronfulah [42] as an outlier. All 3 sensitivity analyses showed a statistically significant positive result for physical activity (P<.05; Multimedia Appendix 9). Subgroup analyses were conducted among studies with patients who were chronically ill and studies with healthy individuals; both reported nonsignificant changes in physical activity (Multimedia Appendix 9). Only 20% (2/10) of the RCTs reported measures regarding sedentary behaviors; both reported a greater reduction in sedentary time in the intervention group than in the control group [42,43] (Multimedia Appendix 7).
Figure 2.
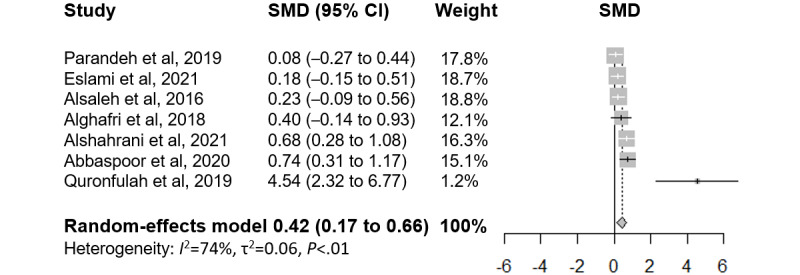
Forest plot of effect sizes and 95% CIs of physical activity outcomes ordered by descending effect size of the individual studies. SMD: standardized mean difference.
Quasi-experiments were not included in the meta-analysis because of the generally lower quality and lack of a control group. Over half (7/12, 58%) of the quasi-experiments reported significant changes in physical activity [57,58,61,62,64,65,67]. Other anthropometric (eg, BMI and weight) or clinical (eg, glycated hemoglobin) outcomes were also reported (Table 2). It is worth noting that most experimental studies (19/22, 86%) measured physical activity outcomes using a validated questionnaire (eg, the International Physical Activity Questionnaire); only 20% (2/10) of the RCTs [42,43] and 8% (1/12) of the quasi-experiments [48] (3/27, 11% in total) used an objective method (eg, accelerometer).
Discussion
Principal Findings
Our review revealed that the use of mobile technologies for physical activity and sedentary behaviors in the MENA region is at an early stage of research given the predominance of small and heterogeneous studies and very few RCTs. The meta-analysis provided preliminary evidence of a small to moderate positive effect of mobile interventions on physical activity in the short term; only 7% (2/27) of the studies measured sedentary behaviors, reporting positive outcomes from the interventions. It is important to note that this evidence is of low to moderate quality according to the Grading of Recommendations Assessment, Development, and Evaluation system [45] because of the high risk of bias in half (5/10, 50%) of the assessed RCTs, heterogeneity in intervention delivery and context, short study duration, possible small-study effects, and publication bias. The reporting standards of the included studies varied widely, and only a small number of studies (3/22, 14%) provided metrics of engagement with the mobile interventions. Nonexperimental studies revealed that users mainly used mobile apps and fitness trackers for self-monitoring of physical activity. Users also revealed several barriers to technology adoption; few studies (1/27, 4%) evaluated the implementation outcomes (eg, context-specific or cultural appropriateness) of the interventions.
Comparison With Existing Literature
This systematic review and meta-analysis focused on the MENA region and provided insights into the effectiveness of mobile technologies on physical activity and sedentary behaviors. Similar to the findings of our meta-analysis, a number of systematic reviews have found a small to moderate effect of mobile technologies on behavioral outcomes [18,20-31]; however, these reviews did not focus on a specific region, and thus, evidence applicable to the MENA region was limited. Furthermore, as these reviews were not MENA specific, it is unclear what would be the most promising interventions given the unique barriers that the MENA region faces. Our review found that particularly favorable interventions were those that conducted user needs assessments, considered daily lives and cultural contexts, and had multicomponent approaches. These findings are in line with those of a review focused on the Asian population that found that Asian apps are largely culturally adapted and multifunctional [72]. A few reviews have explored the use of technologies in specific regions, such as low- and middle-income countries or Asia [72,73], which also showed promising evidence of using these technologies for physical activity and other behavior changes. One systematic review explored physical activity interventions in only 6 Arabian Gulf countries [32] and did not exclusively examine mobile interventions or explore interventions for sedentariness. This review found limited evidence suggesting that pedometer-based interventions encouraging step counting and walking were effective in promoting physical activity, which might suggest the potential of using mobile technologies that can automate self-monitoring of behavior [32]. Thus, our review expands on existing evidence by investigating the use of mobile interventions in MENA countries for both physical activity and sedentary behaviors and, hence, is able to assess whether mobile technologies were effective for this population and what the users’ perspectives were. Combined with the findings from previous reviews, there is evidence suggesting that mobile technologies might be helpful in changing physical activity; however, these interventions likely need to be tailored to users’ daily lives and cultural contexts.
Our meta-analysis suggests that mobile technologies may be promising for changing physical activity and sedentary behavior in the MENA region. Particularly favorable interventions were those that conducted user needs assessments, considered daily lives and cultural contexts, and had multicomponent approaches. For example, one study assessed users’ preferred method of communication and intervention frequency to tailor the design accordingly, resulting in a high level of acceptability and perceived usefulness [42]. Interestingly, WhatsApp was identified as a preferred platform and used in several studies to deliver educational content or send reminders [43,47,49,57,58]. Conducting needs assessments during intervention development will allow researchers and policy makers to determine whether existing technologies can be leveraged or whether additional apps or features are required to meet users’ needs. Incorporating cultural contexts, such as scheduling intervention messages during cultural or health events (eg, Ramadhan and World Hypertension Day) [43], was also a promising approach. In addition, successful interventions combined mobile technologies with face-to-face consultations, suggesting that mobile technologies can complement the role of periodic in-person consultations by delivering more frequent support in daily contexts. It is worth noting that, in the meta-analysis, studies that had a true control group also tended to report larger effect sizes and significant results. Overall, our findings emphasize the potential of mobile technologies to promote behavior changes in the MENA region, necessitating strategies that consider user needs, cultural fit, and multicomponent approaches.
Our review revealed several gaps involving country-specific contexts, targeted populations, and behaviors that should be addressed by researchers and policy makers. First, two-thirds of the included studies (18/27, 67%) were conducted in Saudi Arabia and Iran, and thus, evidence on the use of mobile technologies in other MENA countries was limited. It is likely that more research has been conducted in stable and high-income countries given the diversity of countries in the MENA region regarding income level, economic and social stability [2], and mobile penetration rate [14]. This finding flags the issues of equitable access to mobile technologies across the region, potentially worsening the digital divide and widening health gaps [33-35]. The benefits of mobile health will be limited if it can only reach people with a high socioeconomic status. Thus, concentrated efforts are essential to increase technology access across the region and promote broader research initiatives across countries and contexts.
Second, evidence on mobile interventions for children and adolescents remains limited, with only one included intervention targeting mothers with the ultimate aim of changing preschoolers’ physical activity and diet. Given the importance of promoting healthy behaviors from an early age, policy makers should invest in the development and evaluation of mobile interventions for children and adolescents in the MENA region. Third, only 7% (2/27) of the studies intervened on and measured sedentary behaviors, highlighting the need for future research and investment from policy makers to address sedentariness so as to holistically address inactive lifestyles.
In addition, none of the experimental studies examined fitness trackers as part of the intervention despite interest in these devices (as reported in 2/4, 50% of the nonexperimental studies [69,71]) and existing evidence of their positive effects on physical activity [18,20,22,23,25]. Finally, most RCTs (7/10, 70%) measured behavioral outcomes using self-reporting methods (eg, validated questionnaires). Future research might consider using objective measures provided by mobile apps and fitness trackers, which can improve the accuracy and reliability of the data and provide more robust evidence for policy decision-making.
The reporting standards of the included studies in our review varied greatly, with few details provided regarding the intervention, study procedure, and methodology in some studies. Notably, few of the included experimental studies (3/22, 14%) assessed user engagement even though a large body of research has suggested that engagement with digital interventions is a precondition for effectiveness and highlighted issues of high dropout or nonuse attrition in mobile interventions. Future studies should adhere to reporting guidelines (eg, CONSORT [Consolidated Standards of Reporting Trials], STROBE [Strengthening the Reporting of Observational Studies in Epidemiology], and COREQ [Consolidated Criteria for Reporting Qualitative Research]) [74-76] to enable evidence synthesis and assess engagement metrics consistently to allow for future evaluation of the right “dose” of use of these mobile technologies for effectiveness.
Finally, our review also identified qualitative evidence on barriers to adoption and user preferences that policy makers and researchers should consider. Factors such as perceived lack of usefulness, loss of interest, and technical issues can hinder the effectiveness of mobile interventions [77,78]. In addition, although some participants mentioned a preference for intervention material being culturally and linguistically adapted, few studies (1/27, 4%) examined the context fit or cultural appropriateness of the interventions, highlighting the need for future evaluation of these implementation outcomes.
Strengths and Limitations
Our study has several strengths. We followed a prespecified protocol registered in the PROSPERO database. Our search included peer-reviewed and gray literature. We also hand searched related reviews to ensure that relevant studies were captured. Data extraction and risk-of-bias assessment were conducted by 2 reviewers, and the authors were contacted for additional information. Finally, we conducted several sensitivity analyses (which were consistent with our main results) and assessed risk of bias and publication bias to better understand the limitations of our findings.
Our findings should be interpreted within the context of the study’s limitations. The poor reporting of the included studies affected our synthesis capability. Owing to the small number of studies targeting sedentary behaviors, it was not possible to conduct a meta-analysis of this behavioral outcome. The meta-analysis findings were affected by the quality of the included studies, including a large proportion of self-reported outcomes, small sample sizes, and possible publication bias. Our data synthesis strategy selected one outcome from each study to be included in the meta-analysis; future research might consider performing a multilevel meta-analysis to include all reported outcomes of the studies [79]. In addition, as most of the included studies (18/27, 67%) were conducted in Saudi Arabia or Iran, it is important to acknowledge the potential limitations in generalizing the findings to other countries in the MENA region. However, the insights derived from this review can still serve as a valuable guide for future research endeavors and inform policy-making processes in other MENA countries.
Implications
Our findings have important implications for policy, practice, and future research in the MENA region. First, regarding policy implications, policy makers should support and fund RCTs with longer durations to determine the long-term effectiveness of mobile technologies on physical activity and sedentary behavior. Investment should also be made in technology infrastructure and research initiatives in countries with lower socioeconomic status to promote equitable access to mobile technologies across the MENA region. In addition, policy makers need to ensure that interventions are culturally sensitive and linguistically adapted to enhance their acceptability and effectiveness. Finally, it is important to recognize that mobile technologies alone are unlikely to address behavioral challenges in the MENA region given the variability in mobile ownership and social and economic conditions [2,14,80,81]. Thus, policy makers will need to direct efforts into designing and evaluating multifaceted interventions that can appropriately target physical activity and sedentary behaviors while considering the diverse country contexts.
The evidence of the preliminary effectiveness of mobile interventions found in this review needs to be supported by future rigorous evaluations, with the ultimate goal of assisting clinical practice. If there is sufficient, high-quality evidence, clinicians may consider discussing the use of mobile interventions with people who need to change their activity levels as part of a shared decision-making process [82,83]. Potentially, mobile technologies can enhance patient-clinician collaboration by capturing data to facilitate period review while also empowering individuals to manage their health more actively [84]. As research in the MENA region continues to evolve, evidence of the effectiveness of mobile technologies can be used to determine whether their use can become part of routine clinical care. It is important to note that, although technology prescription is a promising prospect, clinicians have reported several barriers to this practice—the most prominent concern being the lack of knowledge of prescribable technologies and lack of reliable sources to access this information [85,86]. Therefore, a nationally accessible repository of vetted and curated technologies for health care professionals is needed to promote the sustainability and scalability of mobile technologies in clinical practice [85,86].
Implications for future research encompass the need for well-designed RCTs, adherence to reporting standards, and assessment of implementation outcomes. First, well-designed and fully powered RCTs are needed to provide high-quality evidence on the effectiveness of mobile technologies on physical activity and sedentary behaviors, especially over a long-term follow-up. Second, it is crucial for future studies to adhere to existing reporting guidelines [74,75,87] to facilitate evidence synthesis on the most effective intervention, “dosage,” or delivery channel. Finally, researchers should consistently assess and report intervention engagement, acceptability, and implementation outcomes (eg, cultural fit, sustainability, and cost-effectiveness) [76] to determine the viability of mobile technologies for behavior change and successful implementation in the MENA context.
Conclusions
Our systematic review and meta-analysis found that research in the MENA region on the use of mobile interventions for physical activity and sedentary behaviors is in its early stages, with preliminary evidence indicating their effectiveness. However, the studies varied greatly in terms of intervention components, methodology, and study quality, and therefore, the findings must be interpreted with caution. Policy makers and researchers need to invest in high-quality studies to evaluate the effectiveness, engagement, and implementation process of mobile interventions in the MENA region.
Acknowledgments
This work was supported by the King Faisal Specialist Hospital and Research Center and the World Bank. Rekha Menon, Practice Manager at the World Bank, and Issam Abousleiman, Country Director for the Gulf Cooperation Council Countries at the World Bank, provided input and support on the manuscript. The authors would like to thank Ms Isabelle Raison for her input on the search strategy. Funding was provided by the Ministry of Finance of Saudi Arabia under the World Bank Reimbursable Advisory Services program (P179873). The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the King Faisal Specialist Hospital and Research Center or the World Bank.
Abbreviations
- CONSORT
Consolidated Standards of Reporting Trials
- COREQ
Consolidated Criteria for Reporting Qualitative Research
- JBI
Joanna Briggs Institute
- MENA
Middle East and North Africa
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT
randomized controlled trial
- STROBE
Strengthening the Reporting of Observational Studies in Epidemiology
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.
Search strategy.
Eligibility criteria.
Calculating the effective sample size of cluster randomized controlled trials for the meta-analysis using Cochrane guidelines.
List of excluded studies after full-text review for not meeting the inclusion criteria regarding intervention or outcome.
Information about funding sources and conflicts of interest of the included studies.
Retention rates, engagement metrics, and other outcomes from the experimental studies.
Funnel plot of SE by standardized mean difference.
Sensitivity and subgroup analyses.
Data Availability
The data sets generated during and analyzed during this study are available from the corresponding author on reasonable request.
Footnotes
Authors' Contributions: All authors contributed to study conceptualization and design. HLT, AA, NZA, RAB, and RA contributed to article screening. HLT, AA, RAB, and RA contributed to data extraction. HLT, AA, and NZA contributed to quality assessment. HLT contributed to the meta-analysis. HLT and NZA contributed to the first draft. All authors contributed to critical revision of the drafts for important intellectual content. All authors contributed to final approval of the version to be published.
Conflicts of Interest: None declared.
References
- 1.Global health estimates: leading causes of death. World Health Organization. [2023-04-19]. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death .
- 2.Middle East and North Africa. The World Bank. [2023-04-24]. https://www.worldbank.org/en/region/mena .
- 3.Cause of death, by non-communicable diseases (% of total) - Middle East and North Africa. The World Bank. 2020. [2023-04-24]. https://data.worldbank.org/indicator/SH.DTH.NCOM.ZS?locations=ZQ .
- 4.Katzmarzyk PT, Friedenreich C, Shiroma EJ, Lee IM. Physical inactivity and non-communicable disease burden in low-income, middle-income and high-income countries. Br J Sports Med. 2022 Jan 29;56(2):101–6. doi: 10.1136/bjsports-2020-103640. https://europepmc.org/abstract/MED/33782046 .bjsports-2020-103640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012 Jul 21;380(9838):219–29. doi: 10.1016/S0140-6736(12)61031-9. https://europepmc.org/abstract/MED/22818936 .S0140-6736(12)61031-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park JH, Moon JH, Kim HJ, Kong MH, Oh YH. Sedentary lifestyle: overview of updated evidence of potential health risks. Korean J Fam Med. 2020 Nov;41(6):365–73. doi: 10.4082/kjfm.20.0165. https://europepmc.org/abstract/MED/33242381 .kjfm.20.0165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li S, Lear SA, Rangarajan S, Hu B, Yin L, Bangdiwala SI, Alhabib KF, Rosengren A, Gupta R, Mony PK, Wielgosz A, Rahman O, Mazapuspavina MY, Avezum A, Oguz A, Yeates K, Lanas F, Dans A, Abat ME, Yusufali A, Diaz R, Lopez-Jaramillo P, Leach L, Lakshmi PV, Basiak-Rasala A, Iqbal R, Kelishadi R, Chifamba J, Khatib R, Li W, Yusuf S. Association of sitting time with mortality and cardiovascular events in high-income, middle-income, and low-income countries. JAMA Cardiol. 2022 Aug 01;7(8):796–807. doi: 10.1001/jamacardio.2022.1581. https://europepmc.org/abstract/MED/35704349 .2793521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, Alter DA. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015 Jan 20;162(2):123–32. doi: 10.7326/M14-1651.2091327 [DOI] [PubMed] [Google Scholar]
- 9.Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1.6 million participants. Lancet Child Adolesc Health. 2020 Jan;4(1):23–35. doi: 10.1016/s2352-4642(19)30323-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob Health. 2018 Oct;6(10):e1077–86. doi: 10.1016/s2214-109x(18)30357-7. [DOI] [PubMed] [Google Scholar]
- 11.Chaabane S, Chaabna K, Abraham A, Mamtani R, Cheema S. Physical activity and sedentary behaviour in the Middle East and North Africa: an overview of systematic reviews and meta-analysis. Sci Rep. 2020 Jun 09;10(1):9363. doi: 10.1038/s41598-020-66163-x. doi: 10.1038/s41598-020-66163-x.10.1038/s41598-020-66163-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chaabane S, Chaabna K, Doraiswamy S, Mamtani R, Cheema S. Barriers and facilitators associated with physical activity in the Middle East and North Africa region: a systematic overview. Int J Environ Res Public Health. 2021 Feb 09;18(4):1647. doi: 10.3390/ijerph18041647. https://www.mdpi.com/resolver?pii=ijerph18041647 .ijerph18041647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mobile consumption in a post-growth world: global Mobile Consumer Survey 2019. Deloitte. [2023-04-24]. https://www2.deloitte.com/xe/en/pages/technology-media-and-telecommunications/articles/global-mobile-consumer-survey-2019.html .
- 14.Mobile economy report Middle East and North Africa. GSM Association. 2023. [2023-04-24]. https://www.gsma.com/mobileeconomy/mena/
- 15.Steinhubl SR, Muse ED, Topol EJ. Can mobile health technologies transform health care? JAMA. 2013 Dec 11;310(22):2395–6. doi: 10.1001/jama.2013.281078.1762473 [DOI] [PubMed] [Google Scholar]
- 16.Eapen ZJ, Peterson ED. Can mobile health applications facilitate meaningful behavior change?: time for answers. JAMA. 2015 Sep 22;314(12):1236–7. doi: 10.1001/jama.2015.11067.2442914 [DOI] [PubMed] [Google Scholar]
- 17.Insel TR. Digital phenotyping: technology for a new science of behavior. JAMA. 2017 Oct 03;318(13):1215–6. doi: 10.1001/jama.2017.11295.2654782 [DOI] [PubMed] [Google Scholar]
- 18.Tong HL, Quiroz JC, Kocaballi AB, Fat SC, Dao KP, Gehringer H, Chow CK, Laranjo L. Personalized mobile technologies for lifestyle behavior change: a systematic review, meta-analysis, and meta-regression. Prev Med. 2021 Jul;148:106532. doi: 10.1016/j.ypmed.2021.106532.S0091-7435(21)00116-X [DOI] [PubMed] [Google Scholar]
- 19.Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009 Nov;28(6):690–701. doi: 10.1037/a0016136.2009-20990-006 [DOI] [PubMed] [Google Scholar]
- 20.Laranjo L, Ding D, Heleno B, Kocaballi B, Quiroz JC, Tong HL, Chahwan B, Neves AL, Gabarron E, Dao KP, Rodrigues D, Neves GC, Antunes ML, Coiera E, Bates DW. Do smartphone applications and activity trackers increase physical activity in adults? Systematic review, meta-analysis and metaregression. Br J Sports Med. 2021 Apr 21;55(8):422–32. doi: 10.1136/bjsports-2020-102892.bjsports-2020-102892 [DOI] [PubMed] [Google Scholar]
- 21.Romeo A, Edney S, Plotnikoff R, Curtis R, Ryan J, Sanders I, Crozier A, Maher C. Can smartphone apps increase physical activity? Systematic review and meta-analysis. J Med Internet Res. 2019 Mar 19;21(3):e12053. doi: 10.2196/12053. https://www.jmir.org/2019/3/e12053/ v21i3e12053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tang MS, Moore K, McGavigan A, Clark RA, Ganesan AN. Effectiveness of wearable trackers on physical activity in healthy adults: systematic review and meta-analysis of randomized controlled trials. JMIR Mhealth Uhealth. 2020 Jul 22;8(7):e15576. doi: 10.2196/15576. https://mhealth.jmir.org/2020/7/e15576/ v8i7e15576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brickwood KJ, Watson G, O'Brien J, Williams AD. Consumer-based wearable activity trackers increase physical activity participation: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2019 Apr 12;7(4):e11819. doi: 10.2196/11819. https://mhealth.jmir.org/2019/4/e11819/ v7i4e11819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McDonough DJ, Su X, Gao Z. Health wearable devices for weight and BMI reduction in individuals with overweight/obesity and chronic comorbidities: systematic review and network meta-analysis. Br J Sports Med. 2021 Aug;55(16):917–25. doi: 10.1136/bjsports-2020-103594. https://europepmc.org/abstract/MED/33731385 .bjsports-2020-103594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Larsen RT, Wagner V, Korfitsen CB, Keller C, Juhl CB, Langberg H, Christensen J. Effectiveness of physical activity monitors in adults: systematic review and meta-analysis. BMJ. 2022 Jan 26;376:e068047. doi: 10.1136/bmj-2021-068047. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=35082116 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shariful Islam SM, Farmer AJ, Bobrow K, Maddison R, Whittaker R, Pfaeffli Dale LA, Lechner A, Lear S, Eapen Z, Niessen LW, Santo K, Stepien S, Redfern J, Rodgers A, Chow CK. Mobile phone text-messaging interventions aimed to prevent cardiovascular diseases (Text2PreventCVD): systematic review and individual patient data meta-analysis. Open Heart. 2019;6(2):e001017. doi: 10.1136/openhrt-2019-001017. https://openheart.bmj.com/lookup/pmidlookup?view=long&pmid=31673381 .openhrt-2019-001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yerrakalva D, Yerrakalva D, Hajna S, Griffin S. Effects of mobile health app interventions on sedentary time, physical activity, and fitness in older adults: systematic review and meta-analysis. J Med Internet Res. 2019 Nov 28;21(11):e14343. doi: 10.2196/14343. https://www.jmir.org/2019/11/e14343/ v21i11e14343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baumann H, Fiedler J, Wunsch K, Woll A, Wollesen B. mHealth interventions to reduce physical inactivity and sedentary behavior in children and adolescents: systematic review and meta-analysis of randomized controlled trials. JMIR Mhealth Uhealth. 2022 May 11;10(5):e35920. doi: 10.2196/35920. https://mhealth.jmir.org/2022/5/e35920/ v10i5e35920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mönninghoff A, Kramer JN, Hess AJ, Ismailova K, Teepe GW, Tudor Car L, Müller-Riemenschneider F, Kowatsch T. Long-term effectiveness of mHealth physical activity interventions: systematic review and meta-analysis of randomized controlled trials. J Med Internet Res. 2021 Apr 30;23(4):e26699. doi: 10.2196/26699. https://www.jmir.org/2021/4/e26699/ v23i4e26699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Daryabeygi-Khotbehsara R, Shariful Islam SM, Dunstan D, McVicar J, Abdelrazek M, Maddison R. Smartphone-based interventions to reduce sedentary behavior and promote physical activity using integrated dynamic models: systematic review. J Med Internet Res. 2021 Sep 13;23(9):e26315. doi: 10.2196/26315. https://www.jmir.org/2021/9/e26315/ v23i9e26315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ludwig K, Arthur R, Sculthorpe N, Fountain H, Buchan DS. Text messaging interventions for improvement in physical activity and sedentary behavior in youth: systematic review. JMIR Mhealth Uhealth. 2018 Sep 17;6(9):e10799. doi: 10.2196/10799. https://mhealth.jmir.org/2018/9/e10799/ v6i9e10799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nash EA, Critchley JA, Pearson F, Awad SF, Abu-Raddad LJ, Abu-Hijleh FM, Huangfu P. A systematic review of interventions to promote physical activity in six Gulf countries. PLoS One. 2021 Oct 28;16(10):e0259058. doi: 10.1371/journal.pone.0259058. https://dx.plos.org/10.1371/journal.pone.0259058 .PONE-D-21-18255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Western MJ, Armstrong ME, Islam I, Morgan K, Jones UF, Kelson MJ. The effectiveness of digital interventions for increasing physical activity in individuals of low socioeconomic status: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2021 Nov 09;18(1):148. doi: 10.1186/s12966-021-01218-4. https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-021-01218-4 .10.1186/s12966-021-01218-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Western MJ, Smit ES, Neter E, Busse H, Ainsworth B, König LM. Charting new territories in health psychology: a reflection on the EHPS 2022 ‘digital divide’ hybrid roundtable by chairs, presenters, and participants. Eur Health Psychol. 2023 May 11;23(2):1017. [Google Scholar]
- 35.Rodriguez JA, Clark CR, Bates DW. Digital health equity as a necessity in the 21st century Cures Act era. JAMA. 2020 Jun 16;323(23):2381–2. doi: 10.1001/jama.2020.7858.2766776 [DOI] [PubMed] [Google Scholar]
- 36.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021 Apr;88:105906. doi: 10.1016/j.ijsu.2021.105906. https://linkinghub.elsevier.com/retrieve/pii/S1743-9191(21)00040-6 .S1743-9191(21)00040-6 [DOI] [PubMed] [Google Scholar]
- 37.Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P T. 2014 May;39(5):356–64. https://europepmc.org/abstract/MED/24883008 . [PMC free article] [PubMed] [Google Scholar]
- 38.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016 Dec 05;5(1):210. doi: 10.1186/s13643-016-0384-4. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-016-0384-4 .10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Assessing risk of bias in a randomized trial. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions. London, UK: The Cochrane Collaboration; 2019. Sep 20, [Google Scholar]
- 40.Critical appraisal tools. Joanna Briggs Institute. [2023-11-26]. https://jbi.global/critical-appraisal-tools .
- 41.Higgins JP, Eldridge S, Li T. Including variants on randomized trials. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions. London, UK: The Cochrane Collaboration; 2019. [Google Scholar]
- 42.Quronfulah BS. Development and implementation of a health promotion intervention to reduce sedentary behaviour among male office workers in Saudi Arabia: the slim (sit less, impress and motivate) study. Queensland University of Technology. 2019. [2024-02-15]. https://eprints.qut.edu.au/134422/
- 43.Alghafri TS, Alharthi SM, Al-Farsi Y, Alrawahi AH, Bannerman E, Craigie AM, Anderson AS. 'MOVEdiabetes': a cluster randomized controlled trial to increase physical activity in adults with type 2 diabetes in primary health in Oman. BMJ Open Diabetes Res Care. 2018 Oct 31;6(1):e000605. doi: 10.1136/bmjdrc-2018-000605. https://drc.bmj.com/lookup/pmidlookup?view=long&pmid=30487976 .bmjdrc-2018-000605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000 Jun;56(2):455–63. doi: 10.1111/j.0006-341x.2000.00455.x. https://tinyurl.com/ttp4y93c . [DOI] [PubMed] [Google Scholar]
- 45.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008 Apr 26;336(7650):924–6. doi: 10.1136/bmj.39489.470347.AD. https://europepmc.org/abstract/MED/18436948 .336/7650/924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.R Core Team R: a language and environment for statistical computing. R Foundation for Statistical Computing. 2019. [2024-02-15]. https://www.R-project.org/
- 47.Alghafri TS, Al Harthi SM, Al-Ajmi F, Al-Farsi Y, Craigie AM, Bannerman E, Anderson AS. Acceptability of the "MOVEdiabetes" physical activity intervention in diabetes primary care settings in Oman: findings from participants and practitioners. BMC Public Health. 2020 Jun 08;20(1):887. doi: 10.1186/s12889-020-09029-1. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-09029-1 .10.1186/s12889-020-09029-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Saleh ZT, Elshatarat RA, Elhefnawy KA, Helmi Elneblawi N, Abu Raddaha AH, Al-Za'areer MS, Mofdy Almarwani A, Alzahrani NS, Aqel AA, Shawashi TO, Tayeh M. Effect of a home-based mobile health app intervention on physical activity levels in patients with heart failure: a randomized controlled trial. J Cardiovasc Nurs. 2023;38(2):128–39. doi: 10.1097/JCN.0000000000000911.00005082-990000000-00002 [DOI] [PubMed] [Google Scholar]
- 49.Alshahrani A, Siddiqui A, Khalil S, Farag S, Alshahrani N, Alsabaani A, Korairi H. WhatsApp-based intervention for promoting physical activity among female college students, Saudi Arabia: a randomized controlled trial. East Mediterr Health J. 2021 Aug 26;27(8):782–9. doi: 10.26719/emhj.21.012. doi: 10.26719/emhj.21.012. [DOI] [PubMed] [Google Scholar]
- 50.Eslami E, Mohammad Alizadeh Charandabi S, Farshbaf Khalili A, Asghari Jafarabadi M, Mirghafourvand M. The effect of a lifestyle training package on physical activity and nutritional status in obese and overweight pregnant women: a randomized controlled clinical trial. Int J Nurs Pract. 2022 Dec 27;28(6):e12992. doi: 10.1111/ijn.12992. [DOI] [PubMed] [Google Scholar]
- 51.Abbaspoor Z, Amani A, Afshari P, Jafarirad S. The effect of education through mobile phone short message service on promoting self-care in pre-diabetic pregnant women: a randomized controlled trial. J Telemed Telecare. 2018 Sep 07;26(4):200–6. doi: 10.1177/1357633x18791419. [DOI] [PubMed] [Google Scholar]
- 52.Parandeh L, Shafaie FS, Malakouti J, Mirghafourvand M, Asghari-Jafarabadi M. The effect of educational text message based on health belief model on osteoporosis preventive behaviors in women: a randomized controlled clinical trial. Women Health. 2019 Apr 08;59(10):1128–40. doi: 10.1080/03630242.2019.1590495. [DOI] [PubMed] [Google Scholar]
- 53.Alsaleh E, Windle R, Blake H. Behavioural intervention to increase physical activity in adults with coronary heart disease in Jordan. BMC Public Health. 2016 Jul 26;16(1):643. doi: 10.1186/s12889-016-3313-5. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-016-3313-5 .10.1186/s12889-016-3313-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Goodarzi M, Ebrahimzadeh I, Rabi A, Saedipoor B, Jafarabadi MA. Impact of distance education via mobile phone text messaging on knowledge, attitude, practice and self efficacy of patients with type 2 diabetes mellitus in Iran. J Diabetes Metab Disord. 2012 Aug 31;11(1):10. doi: 10.1186/2251-6581-11-10. https://europepmc.org/abstract/MED/23497632 .2251-6581-11-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ansari K, Afshari P, Abedi P, Haghighizadeh M. Comparing the effects of text messaging and mobile social networking on physical activity and anthropometric indices of middle-aged women: a randomized controlled trial. BMC Womens Health. 2022 Jan 26;22(1):18. doi: 10.1186/s12905-022-01598-0. https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-022-01598-0 .10.1186/s12905-022-01598-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Al-Daghri NM, Amer OE, Hameidi A, Alfawaz H, Alharbi M, Khattak MN, Alnaami AM, Aljohani NJ, Alkhaldi G, Wani K, Sabico S. Effects of a 12-month hybrid (in-person + virtual) education program in the glycemic status of Arab youth. Nutrients. 2022 Apr 22;14(9):1759. doi: 10.3390/nu14091759. https://www.mdpi.com/resolver?pii=nu14091759 .nu14091759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ghofranipour F, Hamzavi Zarghani N, Mohammadi E, Mehrizi AA, Tavousi M, De Craemer M, Cardon G. An internet-based educational intervention for mothers targeting preschoolers' weight management promotion (PWMP): a pilot study. BMC Public Health. 2022 Nov 29;22(1):2220. doi: 10.1186/s12889-022-14543-5. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-022-14543-5 .10.1186/s12889-022-14543-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Alyousef ZM. Diabetes and physical activity among Saudi women. University of Texas at Arlington. 2021. Jul 14, [2024-02-15]. https://rc.library.uta.edu/uta-ir/handle/10106/29979 .
- 59.Biglar Chopoghlo S, Hosseinkhani A, Khedmat L, Zaki-Nejad M, Puryaghoob M. The self-efficacy improvement in adolescent girls with type 1 diabetes mellitus with self-care education through mobile-based social networking. Int J Diabetes Dev Ctries. 2021 Feb 10;41(4):676–82. doi: 10.1007/s13410-021-00929-5. [DOI] [Google Scholar]
- 60.Khidir ED, Stănescu M, Al Sayegh S. Using mobile technology to evaluate the active lifestyle of adults from campuses in Qatar. Proceedings of the International Scientific Conference eLearning and Software for Education; eLSE 2021; April 22-23, 2021; Bucharest, Romania. 2021. [DOI] [Google Scholar]
- 61.Yahia EA, Bayoumi MM. Effectiveness of using SOKARY mobile application on the compliance of patients with type II diabetes: a quasi-experimental study. Pak J Med Health Sci. 2021 Jul;15(7):2001–5. doi: 10.53350/pjmhs211572001. https://www.researchgate.net/publication/354383862_Effectiveness_of_using_SOKARY_Mobile_Application_on_the_compliance_of_patients_with_Type_II_diabetes_A_quasi-experimental_study . [DOI] [Google Scholar]
- 62.Jorvand R, Ghofranipour F, HaeriMehrizi A, Tavousi M. Evaluating the impact of HBM-based education on exercise among health care workers: the usage of mobile applications in Iran. BMC Public Health. 2020 Apr 22;20(1):546. doi: 10.1186/s12889-020-08668-8. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-08668-8 .10.1186/s12889-020-08668-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Alnasser A, Kyle J, Aloumi N, Al-Khalifa A, Marais D. The Twazon Arabic weight loss app: app-based intervention for Saudi women with obesity. JMIR Mhealth Uhealth. 2019 May 28;7(5):e10923. doi: 10.2196/10923. https://mhealth.jmir.org/2019/5/e10923/ v7i5e10923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lari H, Noroozi A, Tahmasebi R. Impact of short message service (SMS) education based on a health promotion model on the physical activity of patients with type II diabetes. Malays J Med Sci. 2018 May;25(3):67–77. doi: 10.21315/mjms2018.25.3.7. https://europepmc.org/abstract/MED/30899188 .07mjms25032018_oa5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Peyman N, Rezai-Rad M, Tehrani H, Gholian-Aval M, Vahedian-Shahroodi M, Heidarian Miri H. Digital media-based health intervention on the promotion of women's physical activity: a quasi-experimental study. BMC Public Health. 2018 Jan 15;18(1):134. doi: 10.1186/s12889-018-5025-5. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-018-5025-5 .10.1186/s12889-018-5025-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sani M, Makeen A, Albasheer OB, Solan YM, Mahfouz MS. Effect of telemedicine messages integrated with peer group support on glycemic control in type 2 diabetics, Kingdom of Saudi Arabia. Int J Diabetes Dev Ctries. 2018 Jan 29;38(4):495–501. doi: 10.1007/s13410-018-0608-3. [DOI] [Google Scholar]
- 67.Ali HI, Attlee A, Alhebshi S, Elmi F, Al Dhaheri AS, Stojanovska L, El Mesmoudi N, Platat C. Feasibility study of a newly developed technology-mediated lifestyle intervention for overweight and obese young adults. Nutrients. 2021 Jul 26;13(8):2547. doi: 10.3390/nu13082547. https://www.mdpi.com/resolver?pii=nu13082547 .nu13082547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Al Ansari FS, Alfayez A, Alsalman D, Alanezi F, Alhodaib H, Al-Rayes S, Aljabri D, Alrawiai S, Alakrawi Z, Saadah A, Al-Juwair MM, Aljaffary A, AlThani B, Mushcab H, Alanzi TM, AlNujaidi H, Al-Saif AK, Attar R, Alumran A, Al-Mubarak S, Alyousef S. Using mobile health applications to enhance physical activity in Saudi Arabia: a cross-sectional study on users' perceptions. Int Health. 2023 Jan 03;15(1):47–55. doi: 10.1093/inthealth/ihac008. https://europepmc.org/abstract/MED/35348719 .6554383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bardus M, Borgi C, El-Harakeh M, Gherbal T, Kharroubi S, Fares EJ. Exploring the use of mobile and wearable technology among university student athletes in Lebanon: a cross-sectional study. Sensors (Basel) 2021 Jun 30;21(13):4472. doi: 10.3390/s21134472. https://www.mdpi.com/resolver?pii=s21134472 .s21134472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zaman TU, Alqahtani F, Alsairafi A, Adetunji HA, Al Areefi M, Al Akhram N, Abdurraheem TM, Hussain MK. The role of mobile health applications in preventing sleep-related health problems – a pilot study in the Makkah city of Saudi Arabia. Int J Healthc Manag. 2020 Apr 28;14(4):1230–6. doi: 10.1080/20479700.2020.1756103. [DOI] [Google Scholar]
- 71.Altabtabaei R, Alhuwail D. Exploring the use and adoption of wearable physical activity trackers in oil-rich nations: a qualitative study of youth perspectives from Kuwait. Stud Health Technol Inform. 2022 Jun 06;290:1100–1. doi: 10.3233/SHTI220287.SHTI220287 [DOI] [PubMed] [Google Scholar]
- 72.Ang SM, Chen J, Liew JH, Johal J, Dan YY, Allman-Farinelli M, Lim SL. Efficacy of interventions that incorporate mobile apps in facilitating weight loss and health behavior change in the Asian population: systematic review and meta-analysis. J Med Internet Res. 2021 Nov 16;23(11):e28185. doi: 10.2196/28185. https://www.jmir.org/2021/11/e28185/ v23i11e28185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Edney S, Chua XH, Müller AM, Kui KY, Müller-Riemenschneider F. mHealth interventions targeting movement behaviors in Asia: a scoping review. Obes Rev. 2022 Apr;23(4):e13396. doi: 10.1111/obr.13396. doi: 10.1111/obr.13396. [DOI] [PubMed] [Google Scholar]
- 74.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007 Dec;19(6):349–57. doi: 10.1093/intqhc/mzm042.mzm042 [DOI] [PubMed] [Google Scholar]
- 75.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007 Oct 16;147(8):573–7. doi: 10.7326/0003-4819-147-8-200710160-00010. https://www.acpjournals.org/doi/abs/10.7326/0003-4819-147-8-200710160-00010?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .147/8/573 [DOI] [PubMed] [Google Scholar]
- 76.Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Griffey R, Hensley M. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011 Mar;38(2):65–76. doi: 10.1007/s10488-010-0319-7. https://europepmc.org/abstract/MED/20957426 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jakob R, Harperink S, Rudolf AM, Fleisch E, Haug S, Mair JL, Salamanca-Sanabria A, Kowatsch T. Factors influencing adherence to mHealth apps for prevention or management of noncommunicable diseases: systematic review. J Med Internet Res. 2022 May 25;24(5):e35371. doi: 10.2196/35371. https://www.jmir.org/2022/5/e35371/ v24i5e35371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yang X, Ma L, Zhao X, Kankanhalli A. Factors influencing user's adherence to physical activity applications: a scoping literature review and future directions. Int J Med Inform. 2020 Feb;134:104039. doi: 10.1016/j.ijmedinf.2019.104039.S1386-5056(19)30850-0 [DOI] [PubMed] [Google Scholar]
- 79.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3):1–48. doi: 10.18637/jss.v036.i03. https://www.jstatsoft.org/article/view/v036i03 . [DOI] [Google Scholar]
- 80.Fawcett L. The Middle East and COVID-19: time for collective action. Global Health. 2021 Nov 22;17(1):133. doi: 10.1186/s12992-021-00786-1. https://globalizationandhealth.biomedcentral.com/articles/10.1186/s12992-021-00786-1 .10.1186/s12992-021-00786-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang H, Yazbeck AS. Benchmarking health systems in Middle Eastern and North African countries. Health Syst Reform. 2017 Jan 02;3(1):7–13. doi: 10.1080/23288604.2016.1272983. [DOI] [PubMed] [Google Scholar]
- 82.Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. N Engl J Med. 2012 Mar 01;366(9):780–1. doi: 10.1056/NEJMp1109283. [DOI] [PubMed] [Google Scholar]
- 83.Torous JB, Chan SR, Gipson SY, Kim JW, Nguyen TQ, Luo J, Wang P. A hierarchical framework for evaluation and informed decision making regarding smartphone apps for clinical care. Psychiatr Serv. 2018 May 01;69(5):498–500. doi: 10.1176/appi.ps.201700423. [DOI] [PubMed] [Google Scholar]
- 84.Whitney RL, Ward DH, Marois MT, Schmid CH, Sim I, Kravitz RL. Patient perceptions of their own data in mHealth technology-enabled N-of-1 trials for chronic pain: qualitative study. JMIR Mhealth Uhealth. 2018 Oct 11;6(10):e10291. doi: 10.2196/10291. https://mhealth.jmir.org/2018/10/e10291/ v6i10e10291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Byambasuren O, Beller E, Glasziou P. Current knowledge and adoption of mobile health apps among Australian general practitioners: survey study. JMIR Mhealth Uhealth. 2019 Jun 03;7(6):e13199. doi: 10.2196/13199. https://mhealth.jmir.org/2019/6/e13199/ v7i6e13199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Byambasuren O, Beller E, Hoffmann T, Glasziou P. Barriers to and facilitators of the prescription of mHealth apps in Australian general practice: qualitative study. JMIR Mhealth Uhealth. 2020 Jul 30;8(7):e17447. doi: 10.2196/17447. https://mhealth.jmir.org/2020/7/e17447/ v8i7e17447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Schulz KF, Altman DG, Moher D, CONSORT Group CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010 Jun 01;152(11):726–32. doi: 10.7326/0003-4819-152-11-201006010-00232. https://www.acpjournals.org/doi/abs/10.7326/0003-4819-152-11-201006010-00232?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .0003-4819-152-11-201006010-00232 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.
Search strategy.
Eligibility criteria.
Calculating the effective sample size of cluster randomized controlled trials for the meta-analysis using Cochrane guidelines.
List of excluded studies after full-text review for not meeting the inclusion criteria regarding intervention or outcome.
Information about funding sources and conflicts of interest of the included studies.
Retention rates, engagement metrics, and other outcomes from the experimental studies.
Funnel plot of SE by standardized mean difference.
Sensitivity and subgroup analyses.
Data Availability Statement
The data sets generated during and analyzed during this study are available from the corresponding author on reasonable request.


