Abstract
Aim
As periodontitis and dyslipidemia are diseases that occur with high incidence, the relationship between them has attracted much attention. Previous studies on these diseases have tended to focus on lipid parameters and periodontitis, we aimed to investigate the relationship between dyslipidemia and periodontitis.
Materials and methods
A comprehensive search to identify the studies investigating the relationship between dyslipidemia and periodontitis was performed on PubMed, Web of Science and Cochrane Library before the date of August, 2023. Studies were considered eligible if they contained data on abnormal blood lipid parameters and periodontitis. Studies that reported mean differences and 95% confidence intervals or odds ratios were used.
Results
A total of 73 publications were included in the meta-analysis. Hyper total cholesterol (TC), triglycerides (TGs), low-density lipoprotein (LDL), very low-density lipoprotein (VLDL) and lower high-density lipoprotein (HDL) levels are risk factors for periodontitis. Periodontal disease is a risk factor for high TG and low HDL levels. Three months after periodontal treatment, the levels of TC, TG and HDL were significantly improved, and statin treatment only improved gingival index (GI) levels compared to that of the dietary control.
Conclusions
The findings reported here suggest that the mutual promotion of periodontitis and dyslipidemia can be confirmed. Non-surgical periodontal therapy may improve lipid abnormalities. It can’t be demonstrated whether systematic application of statins have a better effect on the improvement in periodontal status in patients with dyslipidemia compared to that of the control.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12903-023-03668-7.
Keywords: Dyslipidemia, Periodontitis, Periodontal treatment, Blood lipid treatment, Meta-analysis
Introduction
Periodontitis involves inflammation that extends deep into tissues and causes loss of supporting connective tissue and alveolar bone [1]. The term ‘periodontal diseases’ encompasses a wide variety of chronic inflammatory conditions involving the gingiva (or gums, which are the soft tissue surrounding the teeth), bone and ligament (the connective tissue collagen fibres that anchor a tooth to alveolar bone) that support teeth [2]. In 2017, the age-standardized prevalence of severe periodontitis was 9.8%, and the number of prevalent cases was 796 million [3]. Gum recession and alveolar bone resorption are typical manifestations of periodontal disease (Pd). Severe periodontitis causes bleeding gums, impaired chewing, and eventually tooth loss. Epidemiologically, periodontitis is associated with several chronic disorders, such as cardiovascular disease, type 2 diabetes mellitus (T2DM), rheumatoid arthritis, inflammatory bowel disease (IBD), Alzheimer’s disease, nonalcoholic fatty liver disease and certain cancers [4]. Multiple parameters, including probing depth (PD), clinical attachment level (CAL), and bleeding on probing (BOP) must be recorded at six locations per tooth to accurately diagnose periodontitis [2]. The plaque index (PI) and gingival index (GI) are also important indicators. The critical risk factor for periodontitis is subgingival plaque. The development of periodontitis is associated with a subgingival microbial community that is imbalanced and enriched with species such as Porphyromonas gingivalis, Tannerella forsythia and Treponema denticola. In addition to bacteria, smoking and some systemic diseases, such as diabetes and osteoporosis, are crucial risk factors for periodontitis [5–7].
Dyslipidemia is a disorder that involves lipoproteins in plasma. Laboratory examination showed elevated TC, elevated TG, elevated LDL, elevated VLDL or reduced HDL. There is now a broad consensus that dyslipidemia is a major risk factor for developing cardiovascular disease (CVD). Dyslipidemia can also contribute to the risk of an ischaemic cerebrovascular accident. Since 2002, Asia has been rapidly urbanized and the dietary habits and lifestyles of people have changed, and the prevalence of dyslipidemia has also increased; a large national survey conducted in 2013–2014 in 163,641 Chinese adults showed that the most common forms of dyslipidemia are low plasma HDL-cholesterol levels (20.4% of the population) and high plasma triglyceride levels (13.8%) [8].
Since the 1990s, the relationship between periodontitis and dyslipidemia has attracted considerable interest due to the damage these diseases cause to human health. However, the conclusions of these studies are not completely consistent. To gain expertise on the current standings of research and clinical implications, we searched multiple databases and identified the following relevant directions of research: 1. The influence of dyslipidemia on periodontitis, 2. The influence of periodontitis on dyslipidemia, 3. The influence of periodontal treatment on dyslipidemia, and 4. The effect of blood lipid treatment on periodontitis. In this review, we produced a comprehensive summary of the connection between periodontitis and dyslipidemia.
Materials and methods
This review was conducted and reported according to the PRISMA statement [9] and the Cochrane Handbook [10].
Principal question
Is there an association between dyslipidemia and periodontitis? Will the treatment of dyslipidemia or periodontitis influence the other disease?
Search strategy
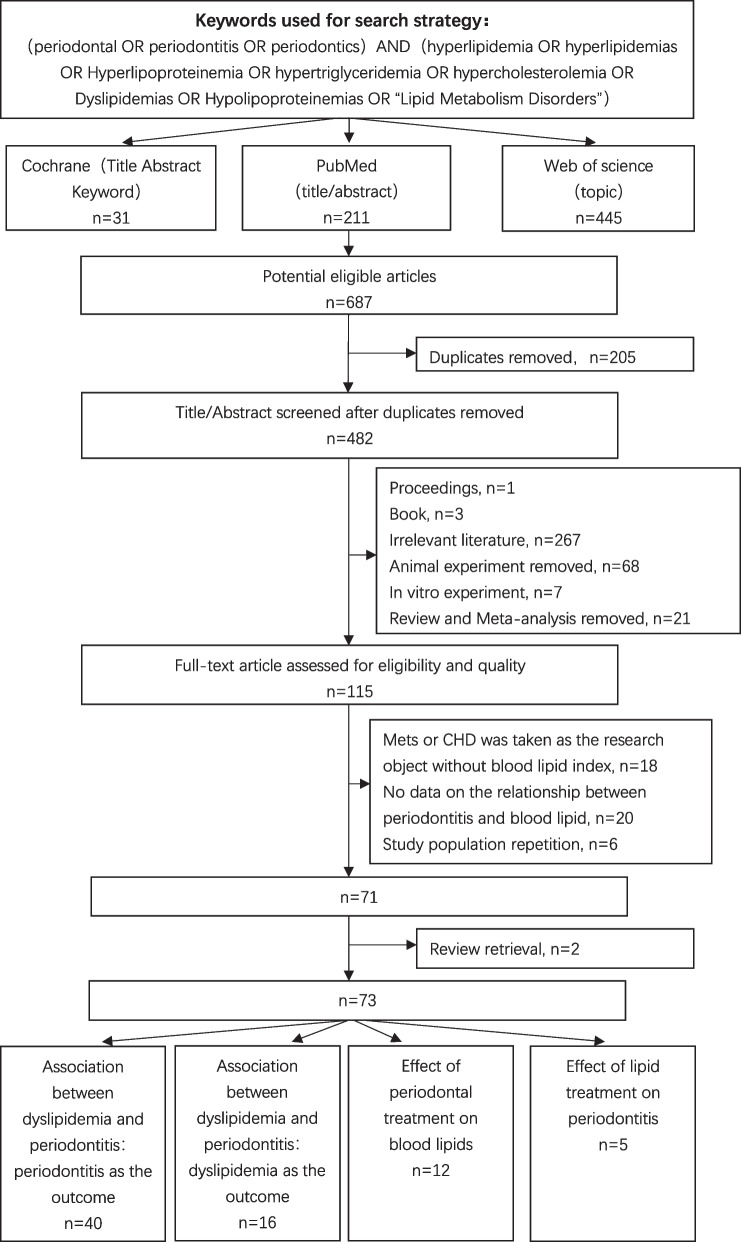
The following electronic databases were searched for dates before August 1st, 2023: PubMed, Web of Science and Cochrane Library. The detailed search strategy is shown in Fig. 1.
Fig. 1.
Flow chart of the screening process in this study
Two independent reviewers screened records for potentially eligible titles and abstracts and subsequently reviewed full texts to determine the inclusion in the meta-analysis. Disagreements were resolved with a third reviewer to reach a consensus.
Study selection
Abstracts and references were managed using EndNote. The criteria for selecting the eligible articles were as follows: (I) cross-sectional studies, cohort studies, case–control studies and clinical trials. (II) The main goal was to research the relationship between dyslipidemia and periodontitis. (III) When the study population was repeated, we used the most recent study that involved the largest study population. (IV) Studies on syndromes, such as metabolic syndrome (MetS) or Coronary heart disease (CHD), in which the blood lipids were described but the blood lipid levels were not described were excluded. (V) All in vitro and in vivo animal experiments were excluded.
Data extraction
We extracted the data on the author, year, country, study design, sample size, diagnosis criteria for periodontal disease, BMI match or correction, mean age, age ratio, sex ratio, matching or correction factor, effect index and quality evaluation. We will list them separately in Tables 1, 2, 3 and 4.
Table 1.
Main characteristic of the eligible studies for the association between dyslipidemia and periodontitis:periodontitis as the outcome
| Author, year | Country | Study design | Sample size (P/ HC) | Diagnosis criteria for periodontitis | Mean age (year) | age Ratio (P: HC) | % Males | Males ratio (P: HC) | Dyslipidemia diagnosis (any of the following indicators, mg/dl) | Lipid Index | Effect index | Matching or adjusted factor | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Al-Otaibi DH, 2008 [11] | Saudi Arabia | Cross-sectional | 60/30 | Insecure | NI | 1 | NI | 1.00 | NI | TC, TG, LDL, HDL | Mean (SD) | Age, gender | Low |
| Anitha A, 2014 [12] | India | Cross-sectional | 25/25 | Insecure | NI | NI | 24 | 0.71 | NI | HDL, TG | Mean | Age, gender | Moderate |
| Banihashemrad SA, 2008 [13] | Iran | Cross-sectional | 71 | Insecure | 26.68 | NI | 78.87 | NI | NI | TG, TC | Mean (SD) | – | Low |
| Bullon P, 2014 [14] | Spain | Cross-sectional | 13/175 | Secure | 31.96 | 1.04 | 0 | – | NI | TC, HDL, LDL, VLDL, TG | Mean (SD) | – | Moderate |
| Cury EZ, 2018 [15] | Brazil | Case-control | 40/40 | Secure | 46.25 | 1.08 | 65.3 | 0.74 | TG > 200; TC > 200; LDL > 130; HDL < 60 | TC, HDL, LDL, TG | Mean (SD), OR | Age, gender | Moderate |
| Cutler CW, 1999 [16] | Korea | Case-control | 26/25 | Secure | 46.10 | 1.21 | 49.02 | 0.64 | NI | TG, TC | Mean (SD), OR | Age, gender, race, LPS reactivity, ELISA titer | Moderate |
| Doraiswamy S, 2017 [17] | India | Case-control | 30/30 | Secure | 43.3 | 1.06 | NI | NI | TC > 200; TG > 200; HDL > 55; LDL > 130; VLDL> 25–35 | TC, HDL, LDL, VLDL | Mean (SD), Post-OR† | Gender, age, | Moderate |
| Fentoglu O, 2020 [18] | Turkey | Case-control | 123/68 | Secure | . NI | NI | NI | . NI | TG > 200; TC > 200; LDL > 130; HDL < 35; VLDL> 40 | TC, TG, LDL, HDL | OR | – | High |
| Gao H, 2015 [19] | China | Case-control | 185/138 | Secure | 27.91 | 0.96 | 40.56 | 1.00 | NI | TC, HDL, LDL, TG | Mean (SD) | Age, gender, smoking, BMI | Moderate |
| Golpasand HL, 2014 [20] | Iran | Case-control | 45/45 | Secure | 34.74 | 0.96 | 46.67 | 0.91 | TC > 220; TG > 200; LDL > 178; HDL < 29 | TC, TG, HDL, LDL | Mean (SD), Post-OR | Age, gender, number of teeth | Moderate |
| Güler B, 2020 [21] | Turkey | Cross-sectional | LagP: 16; GagP: 16 | NI | 34.79 | 1.02 | 25 | 1.00 | NI | HDL | Mean (SD) | – | Moderate |
| Hamissi J, 2011 [22] | Iran | Case-control | 30/30 | Secure | 35.32 | 1.04 | NI | 1.00 | NI | TC, HDL, LDL, TG | Mean (SD) | Age, gender | Moderate |
| Han SJ, 2019 [23] | Korea | Cross-sectional | 4997/12007 | Insecure | 44.61 | 1.29 | 50.2 | 1.28 | TC ≥ 240; HDL-C < 40; HDL-C ≥ 60; TG ≥ 200; LDL-C ≥ 160 | TC, HDL, LDL, TG | OR | Adjust 1 | Moderate |
| Kalburgi V, 2014 [24] | India | Case-control | 40/20 | Insecure | NI | NI | 55 | 1.15 | NI | TC, HDL, LDL, TG | Mean (SD) | – | Moderate |
| Kim, SR, 2020 [25] | Korea | Cross-sectional | 14,608 | Insecure | NI | NI | NI | NI | TC > 240; TG > 200 | TC,TG | OR | Adjust 2 | Moderate |
| Koshy BS, 2017 [26] | India | Cross-sectional | 50/25 | Secure | 40.49 | 1.14 | 56 | 0.90 | NI | TC, TG, HDL, LDL, VLDL | Mean (SD) | – | Moderate |
| Kumar KR, 2014 [27] | India | Cross-sectional | 25/25 | Secure | NI | NI | NI | NI | NI | LDL,HDL, TG | Mean (SD) | – | Low |
| Kushiyama M, 2009 [28] | Japan | Cross-sectional | 316/754 | Secure | NI | NI | 26.26 | NI | HDL-C < 40 for males < 50 for females; TG ≥ 150 | TC, TG, HDL | Mean (range), OR | Age, gender, smoking habits | Moderate |
| Lee JB, 2013 [29] | Korea | Cross-sectional | 5558/9976 | Insecure | 44.20 | 1.28 | 42.55 | 0.63 | TC ≥ 240; TG > 200; HDL-C ≤ 40; LDL ≥ 160 | TC, TG, HDL | OR | Adjust 3 | Moderate |
| Lee S, 2018 [30] | Korea | Cross-sectional | 1365/5540 | Insecure | NI | NI | 41.68 | 1.52 | TC ≥ 240; HDL-C ≤ 40; HDL-C ≥ 60; LDL-C ≥ 160; TG ≥ 200 | TC, HDL, LDL, TG | Mean (95% CI), OR | Adjust 4 | Moderate |
| Losche W, 2000 [31] | Germany | Case-control | 39/40 | Insecure | 55.10 | 0.99 | 41.77 | 1.39 | TC > 230; LDL-C > 160; HDL- C > 45; TG > 200 | TG, TC, LDL, HDL | Mean (SD), Post-OR | – | Moderate |
| Machado AC, 2005 [32] | Brazil | Case-control | 30/30 | Insecure | 43.80 | 0.98 | 56.67 | 1.00 | TC ≥ 240; LDL-C ≥ 160; HDL-C ≤ 35; TG ≥ 200 | TG, TC, LDL,HDL | Mean (SD), Post-OR | Age, gender | Moderate |
| Moeintaghavi A, 2005 [33] | Iran | Case-control | 40/40 | Insecure | 31.90 | 1.03 | 61.25 | 1.04 | TC > 220; LDL-C > 190; HDL-C < 29; TG > 200 | TC, TG, LDL, HDL | Mean (SD), OR | Age, gender | Moderate |
| Moghadam SA, 2015 [34] | Iran | Case-control | 61/60 | Insecure | NI | 1 | 50 | 1.00 | NI | TG, TC | Mean (SD) | Age, gender | Moderate |
| Monteiro AM, 2009 [35] | Brazil | Case-control | 40/40 | Insecure | 44.95 | 1.01 | 42.5 | 1.13 | TC > 200; LDL > 130; HDL < 40; TG > 150 | TC, HDL, LDL, TG | Mean (SD), Post-OR | Age, gender, BMI | High |
| Nibali L, 2007 [36] | United Kingdom | Case-control | 302/183 | Secure | 40.43 | 1.03 | 45.62 | 1.01 | NI | TG, TC, LDL, HDL | Mean (95% CI) | Age, gender, smoking ethnicity | Moderate |
| Penumarthy S, 2013 [37] | India | Case-control | 30/30 | Secure | 33.92 | 1.46 | NI | NI | TG ≥ 150; TC ≥ 200; HDL-C ≤ 60; LDL-C ≥ 130 | TG, TC, LDL, HDL | Mean (SD) | – | Low |
| Sandi RM, 2014 [38] | India | Cross-sectional | 40/40 | Insecure | 44.82 | 1.05 | 52.5 | NI | NI | TC, TG, HDL, LDL | Mean (SD) | Age | Moderate |
| Saxlin T, 2008 [39] | Finland | Cross-sectional | 1297 | Insecure | NI | NI | 39.24 | NI | NI | TG, HDL, LDL | Quintile, RR | Adjust 5 | High |
| Shi D, 2006 [40] | China | Case-control | 40/37 | Insecure | 32.59 | 1.36 | 35.06 | 0.74 | NA | TC, TG | Mean (SD) | – | Moderate |
| Shimazaki Y, 2007 [41] | Japan | Cross-sectional | 37/547 | Insecure | 55.74 | 1.07 | 0 | – | TG > 150; HDL-C < 50 | TG, HDL | Mean (SD), OR | Age, smoking status | Moderate |
| Sridhar R, 2009 [42] | India | Case-control | 30/30 | Secure | 44.43 | 1.09 | 43.33 | 1.17 | NI | HDL,TG | Mean (SD) | – | Low |
| Taleghani F, 2010 [43] | Iran | Cohort (retrospective) | 26/26 | Secure | 46.50 | 0.94 | 34.62 | 1.00 | LDL-C > 180; HDL-C < 30; TG > 200; TC > 250 | TC, TG, HDL, LDL | Mean (SD), Post-OR | – | Moderate |
| Thapa S, 2016 [44] | United States | Cross-sectional | 376/685 | Secure | 49.90 | NI | 51.84 | 0.75 | TC ≥ 240; LDL ≥ 160; HDL < 50; TG ≥ 200 | TC | OR | Adjust 6 | Moderate |
| Thomas B, 2017 [45] | India | Cross-sectional | 300 | Secure | NI | NI | NI | NI | NI | TC, HDL, LDL, VLDL, TG | Mean (SD) | – | Moderate |
| Wang Y, 2007 [46] | China | Cross-sectional | 280/178 | Insecure | 53.50 | NI | 57.64 | NI | TC ≥ 220; TG ≥ 150 | TC, TG | OR | Age, education, oral hygiene habits, | Moderate |
| Zhou SY, 2012 [47] | China | Cross-sectional | 40/20 | Secure | 46.50 | 1.07 | 33.33 | 1.17 | TC > 220; TG > 150; LDL-C > 120 | TC, TG, HDL, LDL | Mean (SD) | – | Moderate |
| Xiaoyuan Guan, 2022 [48] | China | Cross-sectional | 397/285 | Secure | NI | 1.03 | 57.51 | 1.80 | NI | TG, LDL, HDL | Mean (SD) | Gender, age, BMI, alcohol consumption, exercise frequency, smoking habits | Moderate |
| Feng Zhang, 2022 [49] | China | Cross-sectional | 219 | Secure | 30.10 | NI | 0 | 0 | NI | HDL | Mean (SD) | Adjust 7 | Moderate |
| Chunyan Ding, 2023 [50] | China | Cross-sectional | 163/57 | Insecure | NI | NI | 55.00 | 0.97 | TC ≥ 2 mmol/L, TG ≥ 3 mmol/L, HDL-C, < 1.0 mmol/L, LDL-C ≥ 1 mmol/L | TC, TG, LDL, HDL | OR | Age, overweight or obesity, alcohol consumption, cardiovascular history, and hypertension | Moderate |
Adjust 1: age, gender, family income, education level, alcohol consumption experience in a lifetime, smoking status, regular walking, fat intake,number of remaining teeth, active caries, diabetic status, obesity, and hypertension
Adjust 2: Age, gender, BMI, education level, family income, marital status, house ownership, number of people living together, health insurance coverage and economic activities
Adjust 3: age, gender, family income, educational level,use of floss,alcohol consumption experience in a lifetime, present smoking status, active caries,diabetes mellitus and obesity
Adjust 4: age, area, education, BMI, alcohol intake, menopausal status (in women),and smoking status
Adjust 5: Gender, age, education level, frequency of tooth brushing, dental visit pattern, presence of plaque, lipid drugs, alcohol consumption, BMI
Adjust 6: Age, gender, income, education level, calcium level, smoking status, DM and BMI
Adjust 7: Age, gestational age, educational level, household monthly income, parity and pathological abortion, BMI, SBP, DBP, glucose, HbA1c, TG, HDL-c, TBA, AST, TP, and Urine ACR using backward stepwise method
Abbreviation: P periodontitis, HC health control, ABL alveolar bone loss, PD probing depth, CAL clinical attachment loss, TC total cholesterol, TG triglyceride, LDL low density lipoprotein cholesterol, HDL high density lipoprotein cholesterol, VLDL very low density lipoprotein cholesterol, NI not informed, SD standard error, OR odds ratio
† Post-OR was post-hoc calculated using the enough information of the study
Table 2.
Main characteristic of the eligible studies for the association between dyslipidemia and periodontitis:dyslipidemia as the outcome
| Author, year | Country | Study design | Sample size (DLP/HC) | DLP diagnosis (any of the following indicators, mg/dl) | Mean age (year) | Age ratio (DLP:HC) | % Males | Males ratio (DLP:HC) | Periodontal index | Effect index | Matching or adjusted factor | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Almeida AJ, 2013 [51] | Brazil | Cross-sectional | 67/57 | TG > 150; TC > 200; LDL > 100; HDL < 40 in males and < 50 for females | 48.83 | 1.13 | 23.39 | 0.27 | PD, CAL | Mean (SD) | Age, DM2, BMI, Smoking | Moderate |
| Awartani F, 2010 [52] | Saudi Arabia | Cross-sectional | 30/30 | TG > 200; TC > 200; LDL-C > 130; HDL-C < 35 | 46.70 | 1.02 | 0 | – | PI, BOP, PPD, CAL | Mean (SD) | Age | Moderate |
| D’Aiuto F, 2008 [53] | United Kingdom | Cross-sectional | 1919/11758 | TG > 150; HDL-C < 40 for men and < 50 for women | 40.80 | NI | 49.40 | NI | Mild/Moderate/Severe periodontitis | Mean (95% CI), OR | Adjust 1 | Moderate |
| Dogan B, 2015 [54] | Turkey | Cross-sectional | 99/28 | NA | NI | NI | 38.33 | 0.59 | PI, GI, PD, CAL, SBI, | Mean (SD) | – | Moderate |
| Fentoglu O, 2009 [55] | Turkey | Case-control | 51/47 | TG > 200; TC > 200; LDL > 130; HDL < 35 | 48.40 | 1.04 | 43.87 | 0.55 | PI, PD, BOP, CAL | Mean (SD) | Adjust 2 | High |
| Fentoglu O, 2011 [56] | Turkey | Cross-sectional | 123/68 | TRG > 200; TC > 200; LDL > 130; HDL < 35; VLDL> 40 | 43.84 | 1.02 | 49.21 | 1.12 | PI, GI, PPD, BOP, CAL | Median (range) | – | Moderate |
| Fentoglu O, 2015 [57] | Turkey | Case-control | 18/19 | TG > 200; TC > 200; LDL > 130; HDL < 35; VLDL > 40 | 43.13 | 0.99 | 48.65 | 1.06 | PI, GI, BOP, PD, CAL | Mean (SD) | Age, gender, oral hygiene behaviors | Moderate |
| Fukui N, 2012 [58] | Japan | Cross-sectional | 958/5463 | HDL < 40 for males and < 50 for females; TG ≥ 150 | 43.45 | 1.07 | 77.00 | 1.24 | PD, CAL | Mean (IQR), OR | – | Moderate |
| Katz J, 2002 [59] | Israel | Cross-sectional | 10,590 | NA | 31.00 | NI | 89.00 | NI | CPITN | Mean (SD) | Age, smoking, BMI, DBP | Moderate |
| Kemer ES, 2018 [60] | Turkey | Cross-sectional | 67 | TG > 200; TC > 200; LDL > 130; HDL < 35 | NI | NI | 0 | – | PI, GI, PD, CAL | Mean (SD), Correlation efficient | Age | Moderate |
| Lutfioglu M, 2017 [61] | Turkey | Case-control | 15/15 | TC > 200; TG > 200; LDL > 130; HDL < 35 | 41.89 | 1.19 | 46.67 | 1 | PI, GI, BOP, PPD, CAL | Mean (SD) | Age, gender | Moderate |
| Scardina GA, 2011 [62] | Italy | Case-control | 20/20 | TC > 200; 160 < LDL < 190 | 63.07 | 1.09 | 42.86 | 1 | Periodontitis | Mean (SD) | – | Low |
| Shivakumar T, 2013 [63] | India | Case-control | 60/60 | TG > 200; TC > 200; LDL > 130; HDL < 35 | 48.40 | 1.045 | 43.88 | 0.55 | PI, PD, BOP, CAL | Mean (SD) | – | Low |
| Yu Z, 2012 [64] | China | Cross-sectional | 903 | TG ≥ 150; HDL < 40 for male and < 50 for female | 62.58 | NI | 50.50 | NI | No-mild/moderate-severe periodontitis | OR | Adjust 3 | Moderate |
| Haihua Zhu, 2022 [65] | China | Cross-sectional | 874 | TC ≥ 200; HDL < 40 for male and < 50 for female; LDL > 130; TG ≥ 150 | 70.43 | NI | 49.90 | 1.34 | No-mild/moderate-severe periodontitis | OR | Adjust 4 | Moderate |
| YunSook Jung, 2023 [66] | United States | Cross-sectional | 12,254 | TG ≥ 150; HDL < 40 for male and < 50 for female; | NI | 48.31 | NI | NI | CAL, PD | OR | Adjust 5 | Moderate |
Adjust 1: Age, gender, years of education, poverty-to-income ratio, race, general condition, and smoking
Adjust 2: Age, gender, BMI, high blood pressure, number of missing teeth and daily brushing habits
Adjust 3: Age, gender, years of education, economic income, drinking and smoking
Adjust 4: Age, gender, BMI, alcohol drinking frequency (never, seldom, often, everyday), exercise frequency (never, 1–3 times per week, 4–6 times per week, once per day, more than once per day), smoking habits (current smoker; former smoker; nonsmoker)
Adjust 5: Age, sex, race, education, income, missing teeth, smoking, alcohol intake, regularity of dental visits, BMI, and physical activity
Abbreviation: DLP dyslipidemia, HC health control, ABL alveolar bone loss, PD probing depth, CAL clinical attachment loss, BOP bleeding on probing, PI plaque index, GI gingival index, TC total cholesterol, TG triglyceride, LDL low density lipoprotein cholesterol, HDL high density lipoprotein cholesterol, VLDL very low density lipoprotein cholesterol, NI not informed, DBP diastolic blood pressure, SD standard error, IQR interquartile range, OR odds ratio
Table 3.
Main characteristic of the eligible studies for the periodontitis treatment and dyslipidemia
| Author, year | Country | Study design | Sample size (treat / control) | Diagnosis criteria for periodontitis | Mean age (year) | Age ratio (treat: control) | % Males | Male ratio (treat: control) | Therapeutic Schedule | Dyslipidemia diagnosis (any of the following indicators, mg/dl) | Lipids index | Effect index | Matching or correction factor | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Duan JY, 2009 [67] | China | Cohort (prospective) | 20 | Secure | 55.60 | NI | 55 | NI | Initial therapy | TC > 220; TG > 150; HDL < 35; LDL > 140 | TC, TG, LDL, HDL | Mean (SD) | – | High |
| Fentoglu O, 2010 [68] | Turkey | Cohort (prospective) | 20 | Insecure | 51.85 | NI | 40 | NI | Initial therapy | TG > 200; TC > 200; LDL > 130; HDL < 35; VLDL > 40 | TG, TC, LDL, HDL | Mean (SD) | – | High |
| Fu YW, 2016 [69] | Chnia | RCT | 54/55 | Secure | 46.93 | 0.99 | Treat group: Initial therapy; Control group: supragingival scaling | TG > 20; HDL < 40; LDL > 160 | TC, TG, LDL, HDL | Mean (SD) | – | High risk of bias | ||
| Losche W, 2005 [70] | Germany | Cohort (prospective) | 32 | NI | 42.80 | NI | 53.13 | NI | Initial therapy | NI | TC, TG, LDL, HDL | Mean (SD) | – | Moderate |
| Macovei-Surdu A, 2013 [71] | Romania | Cohort (prospective) | 30/30 | Insecure | 39.53 | 0.96 | 60 | 1.36 | Treat group: Initial therapy: Control group: oral hygiene maintenance measures | NI | TC, TG, LDL, HDL | Mean | – | Moderate |
| Nassar PO, 2012 [72] | Brazil | RCT | 10/10 | Secure | NI | NI | NI | NI | Treat group: Initial therapy, Maintenance therapy: Control group: Initial therapy | NI | TC, TG | Mean (SD) | – | Unclear risk of bias |
| Nibali L, 2015 [101] | United Kingdom | Cohort (prospective) | 12 | Secure | NI | NI | NI | NI | Initial therapy, open flap debridement | LDL, HDL, IDL, VLDL | Mean (SD) | Age, gender and number of teeth | High | |
| Nicolaiciuc O, 2016 [74] | Romania | Cohort (prospective) | 20 | Insecure | 49.55 | NI | 40 | NI | Initial therapy | TG > 200; TC > 200; LDL > 130; HDL < 35; VLDL > 40 | TG, TC, LDL, HDL, VLDL | Mean (SD) | – | Moderate |
| Oz SG, 2007 [75] | Turkey | RCT | 25/25 | Insecure | 50.34 | 0.95 | 38 | 1.11 | Treat group: Initial therapy: Control group: without applying periodontal treatment | TC>200; LDL>130; HDL<35; VLDL> 40; TG>200 | TG, TC, LDL, HDL, VLDL | Mean (SD) | – | Unclear risk of bias |
| Tawfig A, 2015 [76] | Saudi Arabia | RCT | 15/15 | Insecure | NI | NI | 63.33 | 1.38 | Treat group: Initial therapy, oral hygiene instructions, Control group: oral hygiene instructions | TC ≥200; LDL ≥130; HDL ≤35; TG ≥150 | TC, TG, LDL, HDL | Mean (SD) | – | Unclear risk of bias |
| Zuza EP, 2016 [77] | Brazil | Cohort (prospective) | 54 | Secure | 44.26 | NI | 25.93 | NI | Initial therapy | NI | TC, TG, LDL, HDL | Mean (SD) | – | High |
| Abhay Pandurang Kolte, 2022 [78] | India | Intervention trial | 60 | Secure | NI | NI | 36.67 | NI | Non-surgical periodontal treatment | NI | TC, TG, LDL, HDL | Mean (SD) | – | – |
Initial therapy: supragingival scaling, subgingival scaling and root planning
Abbreviation: RCT randomised clinical trial, TC total cholesterol, TG triglyceride, LDL low density lipoprotein cholesterol, HDL high density lipoprotein cholesterol, VLDL very low density lipoprotein cholesterol, NI not informed, SD standard error
Table 4.
Main characteristic of the eligible studies for the dyslipidemia treatment and periodontitis
| Author, year | Country | Study design | Sample size (Treat / control) | Diagnosis criteria for periodontitis | Treatment | Mean age (year) | Age ratio (Treat / control) | % Males | Males ratio (Treat / control) | Diagnosis criteria for Hyperlipidemia | Research index | Effect index | Matching or correction factor | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fentoglu O, 2015 [79] | Turkey | Cohort (prospective) | 23/29 | secure | Statins | 44.58 | NI | 50 | NI | TG > 200; TC > 200; LDL > 130; HDL < 35; VLDL> 40 | TC, TG, LDL, HDL, VLDL | Median (range) | – | Moderate |
| Sangwan A, 2013 [80] | India | Cross-sectional | 50/44 | NI | Simvastatin | 43.62 | 1.10 | 57.45 | 1.02 | TG > 200; TC > 200; HDL > 130; HDL < 35 | PD, CAL, GI, PI | Mean (SD) | – | High |
| Sangwan A, 2016 [81] | India | Cohort (prospective) | 36/36 | NI | Atorvastatin | 43.31 | 1.06 | 59.72 | 1.26 | TC > 200; TG > 200; LDL > 130; HDL < 35 | PI, PD, CAL, GI | Mean (SD) | Age, gender, BMI | High |
| Sayar F, 2016 [82] | Iran | Cross-sectional | 50/50 | NI | Simvastatin | 47.04 | 1.00 | 49 | 1.33 | TC > 200; LDL > 130 | PI, CAL, BOP, PD | Mean (SD) | – | High |
| Sayar F, 2017 [83] | Iran | Cross-sectional | 30/30 | NI | Gemfibrozzi | 44.72 | 1.04 | 53.33 | 1.29 | Male TG > 160; female TG > 140 | CAL, PD, PI, BOP | Mean (SD) | Adjust 1 | High |
Adjust 1: Age, number of remaining teeth, PI, BMI
Abbreviation: TC total cholesterol, TG triglyceride, LDL low density lipoprotein cholesterol, HDL high density lipoprotein cholesterol, VLDL very low density lipoprotein cholesterol, NI not informed, SD standard error
Clinical definitions of periodontal disease
To eliminate the diagnosis bias, we made the following definitions:
Secure periodontitis:
At least one site with a probing depth (PD) ≥ 4 mm in every quadrant and radiographic evidence of bone loss, or.
At least two sites in non-adjacent teeth with interproximal attachment loss ≥3 mm, or.
At least two sites with PD ≥ 4 mm and CAL ≥ 3 mm, or.
A community periodontal index (CPI) score of 4 in at least one quadrant, or.
For cases in which no CAL or PD is reported, radiographic marginal alveolar bone loss is ≥30%
-
b.
Insecure periodontitis:
Periodontitis was defined only by PD or CAL but without a clear definition.
Quality assessment
The quality of the included case–control studies and cohort studies was assessed using the Newcastle–Ottawa Scale (NOS). The article quality was assessed as follows: low quality = 0–4; moderate quality = 5–6; high quality = 7–9. The methodological quality of the cross-sectional studies included was assessed using an 11-item checklist recommended by the Agency for Healthcare Research and Quality (AHRQ). An item was scored “0” if it was answered “NO” or “UNCLEAR”; if it was answered “YES”, then the item scored 1″. Article quality was assessed as follows: low quality = 0–3; moderate quality = 4–7; high quality = 8–11 [84]. The quality of the randomized controlled trial was assessed using the Cochrane Collaboration’s tool for assessing the risk of bias in randomized trials. Detailed quality evaluation is listed in Supplementary Tables S1, 2, 3, 4.
Data analysis
For continuous data, the pooled effect was estimated as the mean difference (MD) and the 95% confidence interval (CI). For the dichotomous data, the pooled effect was estimated as the odds ratio (OR) and 95% CI. All pooled estimates were obtained using the random effects model of DerSimonian and Laird, which considers both within-study and between-study variations and provides more conservative estimates than those of a fixed-effects model [85, 86]. The heterogeneity among studies was assessed using the I2 statistic, which determines the proportion of variability across studies that is due to heterogeneity rather than sampling error [87]. A P value less than 0.10 or an I2 -value over 50% indicates substantial heterogeneity.
If heterogeneity existed in the pooled studies, meta-regressions were performed to explain the sources of between-study heterogeneity, and these sources included the published year, region, study design, total sample size, quality of study, age, sex, BMI matched, periodontal diagnosis and multi-variable analysis.
To examine the influence of each study on the pooled estimates, sensitivity analyses were conducted using the leave-one-out method, which removes one study each time and repeats the analysis [88]. Egger’s and Begg’s tests were used to detect publication bias in all meta-analyses.
All statistical analyses were carried out using R 3.6.1 software. P values less than 0.05 were considered statistically significant, except when otherwise specified.
Results
Literature search
The literature search identified 687 relevant publications. A total of 205 duplicates were removed. Screening the titles and abstracts resulted in the elimination of 267 studies that failed to meet any of the inclusion criteria, and all proceedings and books were removed. We also excluded all animal experiments and in vitro experiments.Twenty-one reviews and meta-analyses were removed. A total of 115 papers were selected for full-text screening. In 18 articles, Mets or CHD was used as the research object but without a blood lipid index, and 20 articles did not include data on the relationship between periodontitis and blood lipids; we excluded these articles from our current investigation. 6 studies contained repetitive populations, and we used the most recent study with the largest study population. After the quadratic search for reviews, we finally identified 73 articles. (Fig. 1).
Association between dyslipidemia and periodontitis: periodontitis as the outcome
-
i.
TC and periodontitis
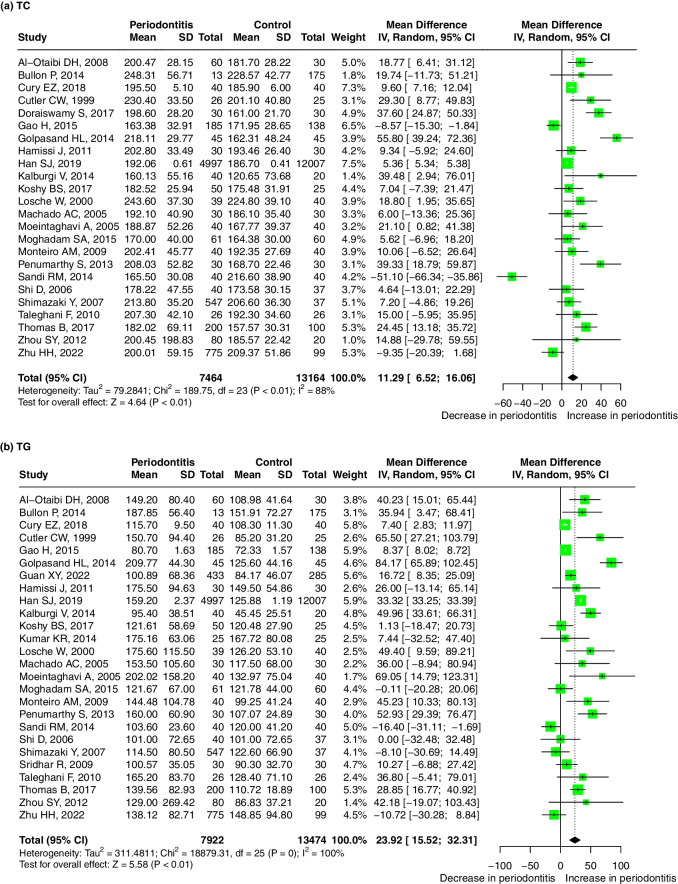
Twenty-four studies evaluated the difference in the serum TC level between periodontitis and healthy control groups with the mean (SD). TC levels were higher in patients with periodontitis than in controls, with a pooled mean difference of 11.29 mg/dL (95%-CI: 6.52, 16.06, p < 0.01). There was significant heterogeneity between the studies (I2 = 88%, p < 0.01) (Fig. 2a). Meta-regression showed that the sources of the heterogeneity may be diagnosis of periodontitis (P diagnosis) (p = 0.041) and BMI matching (p = 0.073) (Table S5). The result was robust regardless if any one study was omitted (Supplementary Fig. 1-a). No significant publication bias was found after Egger’s (p = 0.148) and Begg’s tests (p = 0.275).
Fig. 2.
Forest plot of mean difference for comparisons:periodontitis versus non-periodontitis. (a) periodontitis have high serum TC level; (b) periodontitis have high serum TG level; (c) periodontitis have high serum LDL level; (d) periodontitis have low serum HDL level; (e) periodontitis have high serum VLDL level. Abbreviations: TC:Total cholesterol, TG: triglycerides, LDL: low-density lipoprotein, HDL: high-density lipoprotein, VLDL: very low-density lipoprotein
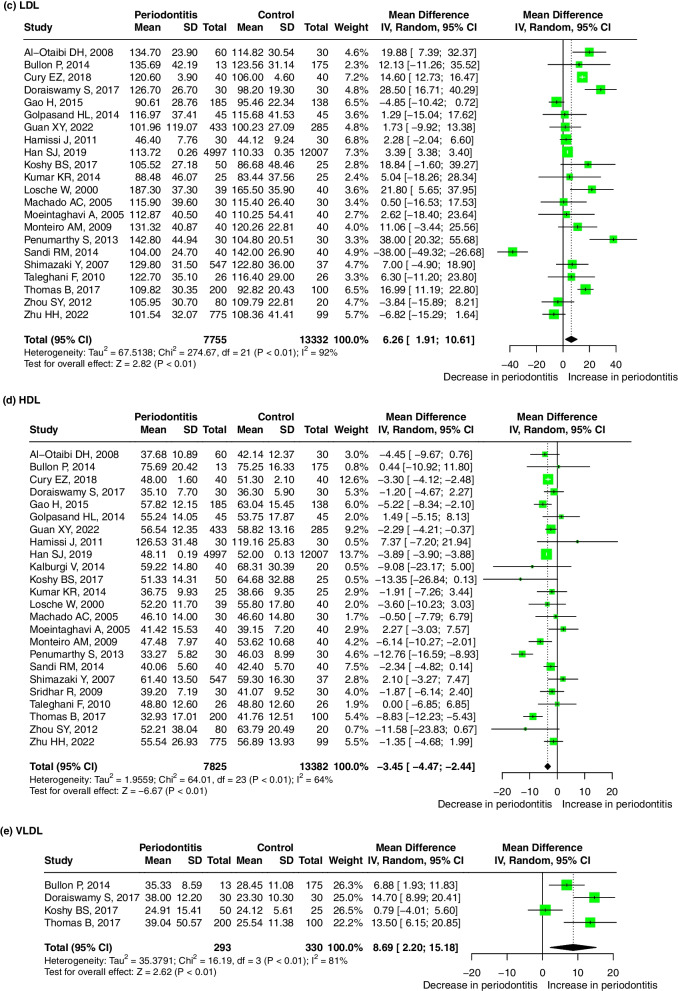
Sixteen studies reported the OR values to evaluate the association between the serum TC level and periodontitis. The pooled OR was 1.83 (95%-CI: 1.40, 2.38, p < 0.01), and substantial heterogeneity between the studies was found (I2 = 77%, p < 0.01) (Fig. 3a), indicating that a high TC level is a risk factor for periodontitis. Meta-regression showed that the sources of the heterogeneity were the year of publication (p < 0.001), study design (p < 0.001), age ratio (p < 0.001), P diagnosis (p = 0.001) and adjusted OR (p = 0.001) (Table S5). The result was robust regardless if any one study was omitted (Supplementary Fig. 2-a). A significant publication bias was found after Egger’s (p < 0.001) and Begg’s tests (p = 0.021).
-
ii.
TG and periodontitis
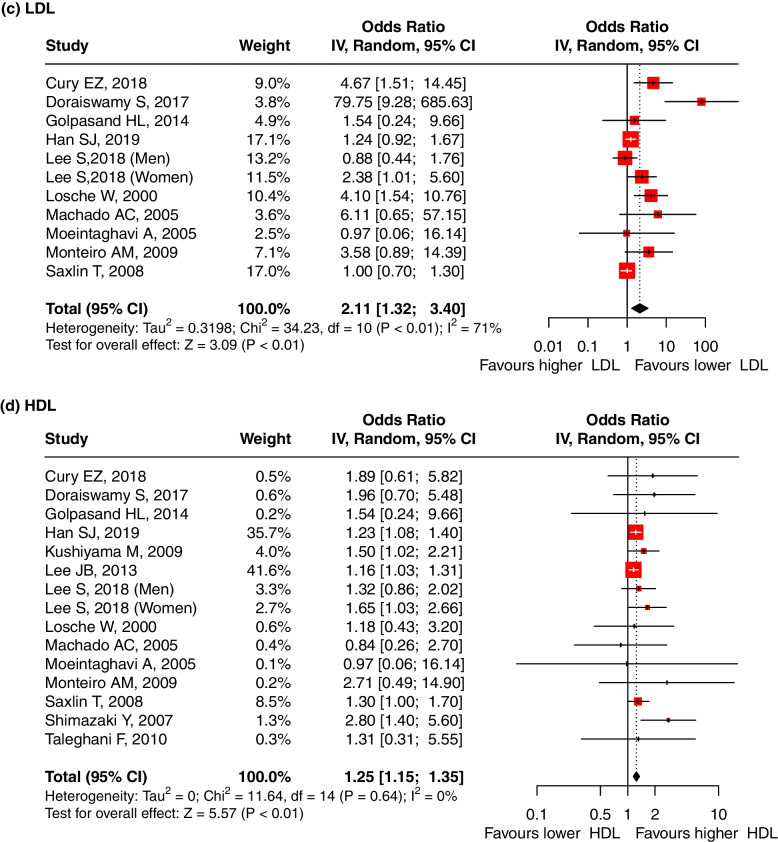
Fig. 3.
Forest plot of OR values for different lipids levels with the risk of periodontitis. a high TC level is associated with the high risk of periodontitis; (b) high TG level is associated with the high risk of periodontitis; (c) high LDL level is associated with the high risk of periodontitis; (d) low HDL level is associated with the high risk of periodontitis. Abbreviations: TC:Total cholesterol, TG: triglycerides, LDL: low-density lipoprotein, HDL: high-density lipoprotein
Twenty-six studies evaluated the difference in the serum TG level between periodontitis and healthy control groups with the mean (SD). TG levels were higher in periodontitis patients than in controls, with a pooled mean difference of 23.92 mg/dL (95%-CI: 15.52, 32.31, p < 0.01). There was significant heterogeneity between the studies (I2 = 100%, p = 0) (Fig. 2b). The meta-regression did not find any significant source of heterogeneity (Table S5). The result was robust regardless if any one study was omitted (Supplementary Fig. 1-b). No significant publication bias was found after Egger’s(p = 0.336) and Begg’s tests (p = 0.061).
Seventeen studies reported the OR values to evaluate the association between the serum TG level and periodontitis. The pooled odds ratio was 1.58 (95%-CI: 1.32, 1.90). We used the random effect model due to the presence of heterogeneity between studies (I2 = 71%, p < 0.01) (Fig. 3b), indicating that TG levels were significantly associated with periodontitis and that high TG levels are a risk factor for periodontitis. Meta-regression showed that the sources of the heterogeneity were the year of publication (p = 0.004), study design (p < 0.001), total sample size (p < 0.001), age (p = 0.001), P diagnosis (p = 0.001) and adjusted OR (p = 0.001) (Table S5). The result was robust regardless of if any one study was omitted (Supplementary Fig. 2-b). A significant publication bias was found after Egger’s(p = 0.003) and Begg’s tests(p = 0.006) .
-
iii.
LDL and periodontitis
Twenty two studies evaluated the difference in the serum LDL level between periodontitis and healthy control groups with the mean (SD). LDL levels were higher in periodontitis patients than in controls, with a pooled mean difference of 6.26 mg/dL (95% CI: 1.91, 10.61, p < 0.01). There was significant heterogeneity between the studies (I2 = 92%, p < 0.01). (Fig. 2c) However, the meta-regression did not find any significant source of heterogeneity (Table S5). The result was robust regardless if any one study was omitted (Supplementary Fig. 1-c). No significant publication bias was found after Egger’s(p = 0.277) and Begg’s tests (p = 0.271).
Nine studies reported the OR values to evaluate the association between the serum LDL level and periodontitis. The pooled OR was 2.11 (95%-CI: 1.32, 3.40, p < 0.01), indicating that LDL levels were significantly associated with periodontitis and that high LDL levels are a risk factor for periodontitis. We used the random effect model due to the presence of heterogeneity between studies (I2 = 71%, p < 0.01) (Fig. 3c). Meta-regression showed that the sources of the heterogeneity were the study design (p < 0.001), total sample size (p = 0.014), and P diagnosis (p = 0.018) (Table S5). The result was robust regardless if any one study was omitted (Supplementary Fig. 2-c). A significant publication bias was found after Egger’s(p = 0.277) and Begg’s tests (p = 0.271).
-
iv.
HDL and periodontitis
Twenty-four studies evaluated the difference in the serum HDL level between periodontitis and healthy control groups with the mean (SD). The HDL levels were lower in periodontitis patients, and the pooled mean difference for the HDL levels in the periodontitis patients and healthy control groups was − 3.45 mg/dL (95%-CI: − 4.47, − 2.44 mg/dL, p < 0.01). There was significant heterogeneity between the studies (I2 = 64%, p < 0.01) (Fig. 2d). Meta-regression showed that age may be the source of the heterogeneity (p = 0.003) (Table S5). The result was robust regardless if any one study was omitted (Supplementary Fig. 1-d). No significant publication bias was found after Egger’s(p = 0.427) and Begg’s tests (p = 0.843).
Thirteen studies reported the OR values to evaluate the association between the serum HDL level and periodontitis. The pooled OR was 1.25 (95% CI: 1.15, 1.35, p < 0.01), indicating that a low HDL level is a risk factor for periodontitis. There was no significant evidence for heterogeneity between the studies (I2 = 0%, p = 0.64) (Fig. 3d). The result was robust regardless if any one study was omitted (Supplementary Fig. 2-d). A significant publication bias was found after Egger’s(p = 0.030) and Begg’s tests (p = 0.961).
-
xxii.
VLDL and periodontitis
Four studies evaluated the difference in the serum VLDL level between periodontitis and healthy control groups with the mean (SD). The VLDL levels were higher in periodontitis patients than in controls, with a pooled mean difference of 8.69 mg/dL (95% CI: 2.20, 15.18, p < 0.01). There was significant heterogeneity between the studies (I2 = 81%, p < 0.01) (Fig. 2e). No significant publication bias was found after Egger’s(p = 0.266). and Begg’s tests (p = 0.174).
Some studies were not included in our meta-analysis due to the lack of information utilized. Saxlin T reported an association between high serum triglycerides and low HDL-cholesterol levels with periodontal pockets by quintiles [39]. Akkaloori Anitha stated that the mean LDL and VLDL levels were significantly higher and the HDL levels were lower in periodontal patients than in healthy controls [12].
Association between dyslipidemia and periodontitis: dyslipidemia as the outcome
Periodontitis and dyslipidemia
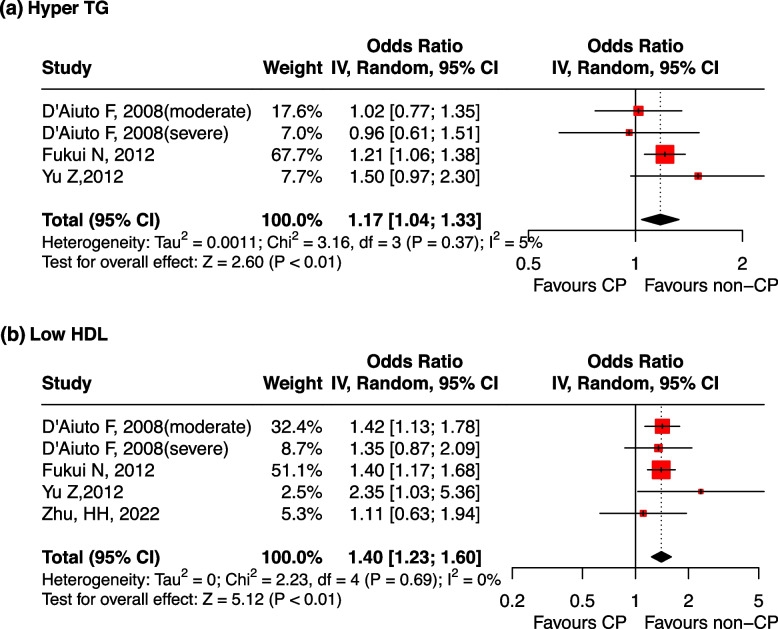
Three studies reported OR values to evaluate the association between periodontitis and dyslipidemia. Periodontitis was a risk factor for abnormal increases in TG levels, with a pooled OR of 1.17 (95% CI: 1.04, 1.33). There was no significant heterogeneity between studies (I2 = 5%, p = 0.37) (Fig. 4a). The result was meaningless when the study by Fukui N, 2012 was omitted (Supplementary Fig. 3-a). No significant publication bias was found after Egger’s(p = 0.769) and Begg’s tests (p = 1.000).
Fig. 4.
Forest plot of OR values for periodontitis with the risk of dyslipidemia. a periodontitis is associated with the high risk of hyper TG; (b) periodontitis is associated with the high risk of low HDL. Abbreviations: TG: triglycerides, HDL: high-density lipoprotein, CP: Chronic Periodontitis
Periodontitis was a risk factor for abnormal decreases in HDL levels, with a pooled OR of 1.40 (95% CI: 1.23, 1.60, p < 0.01), and there was no significant heterogeneity among the studies (I2 = 0%, p = 0.69) (Fig. 4b). The result was robust regardless if any one study was omitted (Supplementary Fig. 3-b). No significant publication bias was found after Egger’s(p = 0.746) and Begg’s tests (p = 1.000).
Since the pathological changes in other indicators, including TC, LDL and VLDL, are often not regarded as classic indicators of dyslipidemia, we only analysed the results of hyper TG and low LDL.
-
i.
PD and dyslipidemia
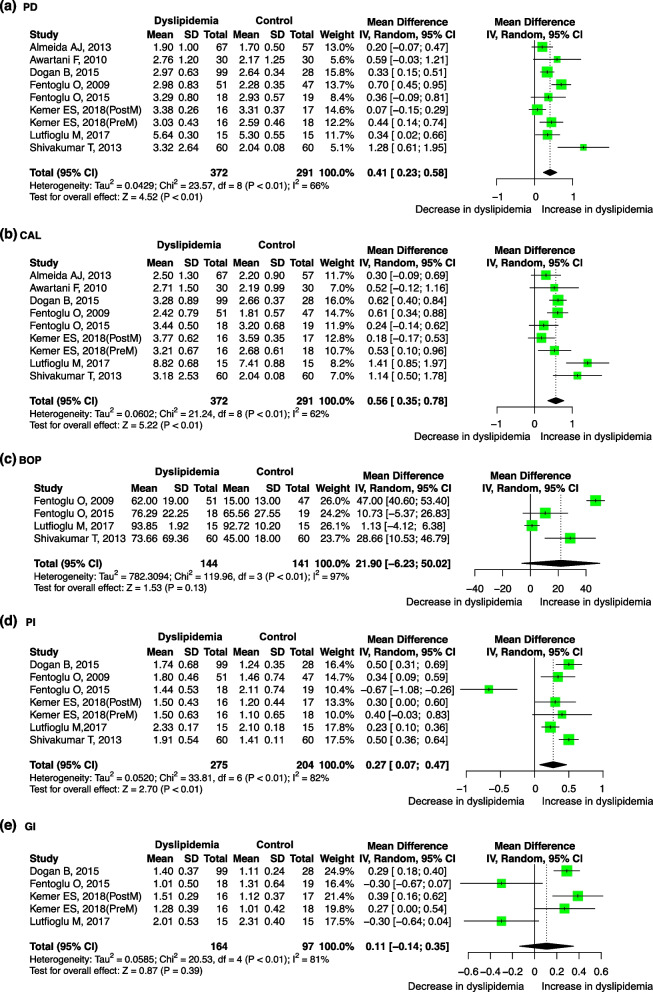
Eight studies evaluated the difference in the PD level between dyslipidemia patients and healthy control groups with the mean (SD). The PD levels were higher in dyslipidemia patients than in controls, with a pooled mean difference of 0.41 mm (95%-CI: 0.23, 0.58, p < 0.01). There was significant heterogeneity between the studies (I2 = 66%, p < 0.01) (Fig. 5a). Meta-regression showed that the sources of the heterogeneity may include the year of publication (p = 0.038) and region (p = 0.038) (Table S6). The result was robust regardless if any one study was omitted (Supplementary Fig. 4-a). No significant publication bias was found after Egger’s(p = 0.178) and Begg’s tests (p = 0.095).
-
ii.
CAL and dyslipidemia
Fig. 5.
Forest plot of mean difference for comparisons: dyslipidemia versus non- dyslipidemia (a) dyslipidemia have deeper PD; (b) dyslipidemia have more CAL (c) dyslipidemia have more BOP but not significant; (d) dyslipidemia have bigger PI; (e) dyslipidemia have bigger GI but not significant, Abbreviations: PD: probing depth, CAL: clinical attachment level, BOP: bleeding on probing, PI: plaque index, GI: gingival index
Eight studies evaluated the difference in the CAL level between dyslipidemia patients and healthy control groups with the mean (SD). The CAL levels were higher in dyslipidemia patients, with a pooled mean difference of 0.56 mm (95%-CI: 0.35, 0.78, p < 0.01). There was significant heterogeneity between studies (I2 = 62%; p < 0.01) (Fig. 5b). However, no significant source of heterogeneity was found through the meta-regression (Table S6). The result was robust regardless if any one study was omitted (Supplementary Fig. 4-b). No significant publication bias was found after Egger’s (p = 0.519) and Begg’s tests (p = 0.532).
-
iii.
BOP and dyslipidemia
Four studies evaluated the difference in the BOP level between dyslipidemia patients and healthy control groups with the mean (SD). No significant difference in BOP levels was found between dyslipidemia patients and healthy controls. There was significant heterogeneity between studies (I2 = 97%; p < 0.01) (Fig. 5c). Meta-regression showed that the sources of the heterogeneity may be the year of publication (p < 0.001), total sample size (p = 0.004), age (p < 0.001) and sex ratio (p = 0.002) (Table S6). The result was significant when the study by Lutfioglu M, 2017 [61] was omitted (Supplementary Fig. 4-c). No significant publication bias was found after Egger’s(p = 0.848) and Begg’s tests (p = 0.497).
-
iv.
PI and dyslipidemia
Six studies evaluated the difference in the PI level between dyslipidemia patients and healthy control groups with the mean (SD). PI levels were higher in dyslipidemia patients, with a pooled mean difference of 0.27 (95%-CI: 0.07, 0.47, p < 0.01). There was significant heterogeneity between studies (I2 = 82%; p < 0.01) (Fig. 5d). Meta-regression showed that the sources of the heterogeneity may be sex (p = 0.013) (Table S6). The result was meaningless when the study of Dogan B, 2015 or Shivakumar T, 2013 was omitted (Supplementary Fig. 4-d). No significant publication bias was found after Egger’s(p = 0.379) and Begg’s tests (p = 0.453).
-
xxii.
GI and dyslipidemia
Four studies evaluated the difference in the GI level between dyslipidemia patients and healthy control groups with a mean (SD). No significant difference in GI level was found between dyslipidemia patients and healthy control groups (Fig. 5e). Meta-regression showed that the sources of the heterogeneity may be Study design(p < 0.001), Quality(p < 0.001) and Gender ratio(p < 0.001) (Table S6). The result was robust regardless if any one study was omitted (Supplementary Fig. 4-e). No significant publication bias was found after Egger’s(p = 0.193) and Begg’s tests (p = 0.050).
Effect of periodontal treatment on blood lipids
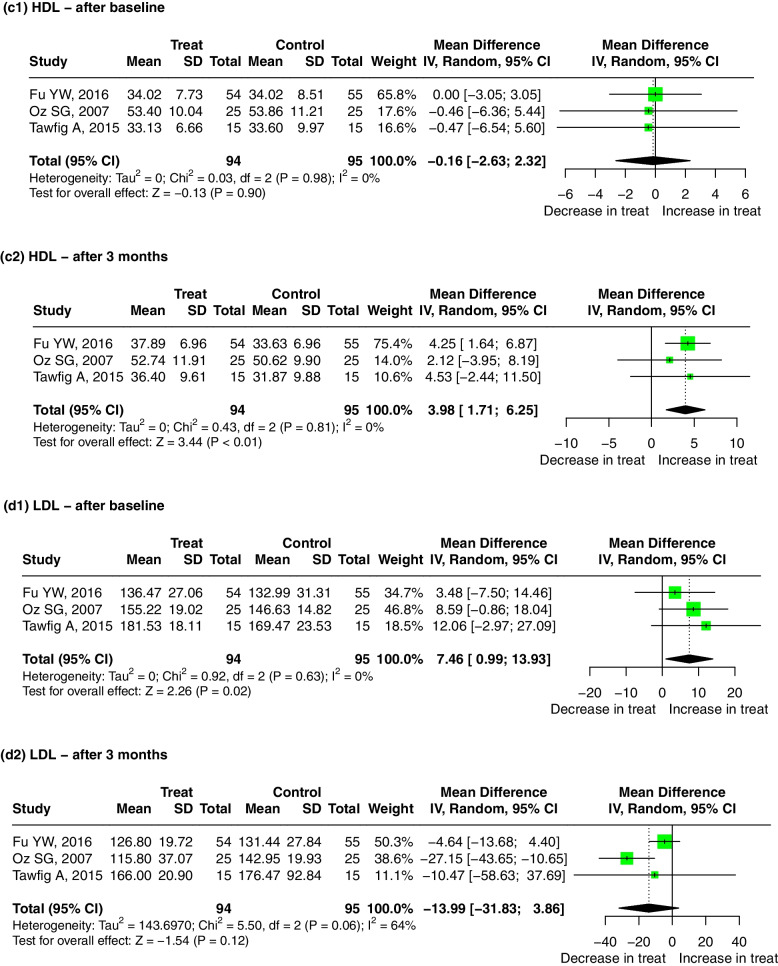
Three studies evaluated the difference in the association between non-surgical periodontal treatment groups and the control groups with the mean (SD). No significant publication bias was found after Egger’s and Begg’s tests (p > 0.05).
-
i.
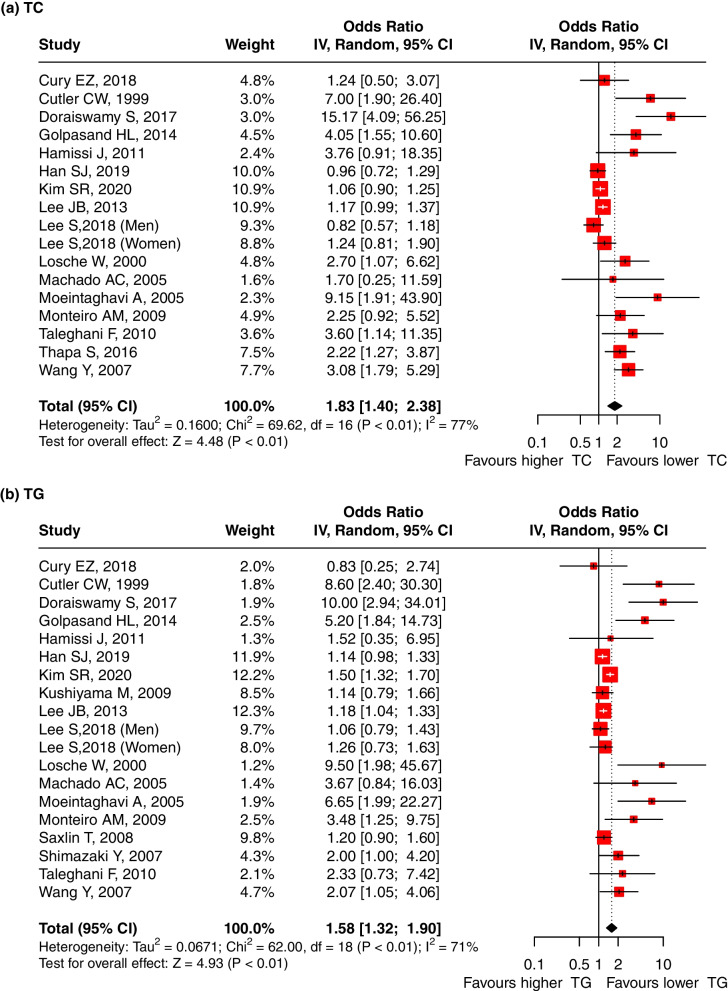
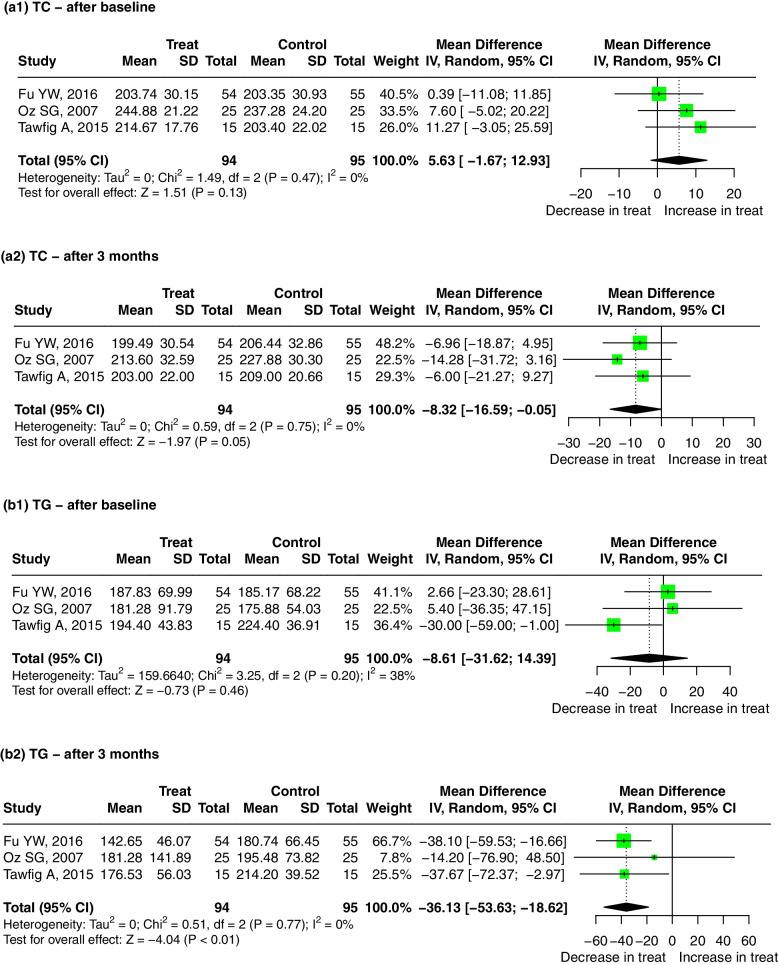
Nonsurgical periodontal treatment and TC
Compared with the control group, the level of TC in the serum of patients who received a non-surgical periodontal treatment was decreased significantly after 3 months, and the pooled mean difference for TC in the treatment and control groups was − 8.32 mg/dL (95% CI: − 16.59, − 0.05, p = 0.05). There was no significant heterogeneity between the studies (I2 = 0, p = 0.75) (Fig. 6a2). The result was meaningless regardless if any one study was omitted (Supplementary Fig. 5-a2).
Fig. 6.
Forest plot of mean difference for comparisons: periodontal treatment versus non-treatment among periodontitis patients. (a1–2) periodontitis treatment can decrease the TC level after 3 months; (b1–2) periodontitis treatment can decrease the TG level after 3 months; (c1–2) periodontitis treatment can increase the HDL level after 3 months; (d1–2) periodontitis treatment do not significantly decrease the LDL level after 3 months. Abbreviations: TC:Total cholesterol, TG: triglycerides, HDL: high-density lipoprotein, LDL: low-density lipoprotein
Several studies that reported positive results were excluded from the meta-analysis because they did not have the standardized clinical data we needed. DUAN Jinyu et al. reported that 3 months after a nonsurgical periodontal treatment, the cholesterol levels were significantly reduced. With 5.72 mmol/l as the diagnostic criterion, four of eight hypercholesterolemia patients returned to normal serum cholesterol levels [67]. The research by A. Surdumacove produced similar results; compared with the control group that received only oral hygiene guidance, the test group that received a non-surgical periodontal treatment exhibited a significant decrease in TC levels after 1 month [71]. Zuza EP et al. reported an interesting result: after non-surgical periodontal treatments, TC levels in obese patients were significantly reduced 3 months later, but the same results were not observed in nonobese patients [77].
-
ii.
Nonsurgical periodontal treatment and TG
Compared with the control group, the level of TG in the serum of patients who received the non-surgical periodontal treatment was decreased significantly after 3 months, with a pooled mean difference of − 36.13 mmol/L (95% CI: − 53.63, − 18.62, p < 0.01). There was no significant heterogeneity between the studies (I2 = 0, p = 0.77) (Fig. 6b2). The result was robust regardless if any one study was omitted (Supplementary Fig. 5-b2).
Considering the results of other studies, with 1.70 mmol/l as the diagnostic criterion, DUAN Jinyu reported that the serum cholesterol levels in five of 15 hypertriglyceridaemia patients returned to normal after the non-surgical periodontal treatment. The observation period was 3 months [71]. This article was not included in the meta-analysis because there were no specific parameters. Zuza EP also reported similar results [77].
-
iii.
Nonsurgical periodontal treatment and HDL
Compared with the control group, the level of HDL in the serum of patients who received the non-surgical periodontal treatment was increased significantly after 3 months, with a pooled mean difference of 3.98 mmol/L (95% CI: 1.71, 6.25, p < 0.01). There was no significant heterogeneity between the studies (I2 = 0, p = 0.81) (Fig. 6c2). The result was meaningless when the study by Fu YW, 2016 was omitted (Supplementary Fig. 5-c2).
-
iv.
Nonsurgical periodontal treatment and LDL
Finally, we performed a meta-analysis of the LDL levels in serum. Analysis of these studies showed that there was no statistically significant difference in the LDL levels between the treatment and control groups after 3 months of treatment (Fig. 6d2). The result was significant when the study by Fu YW, 2016 was omitted (Supplementary Fig. 5-a).
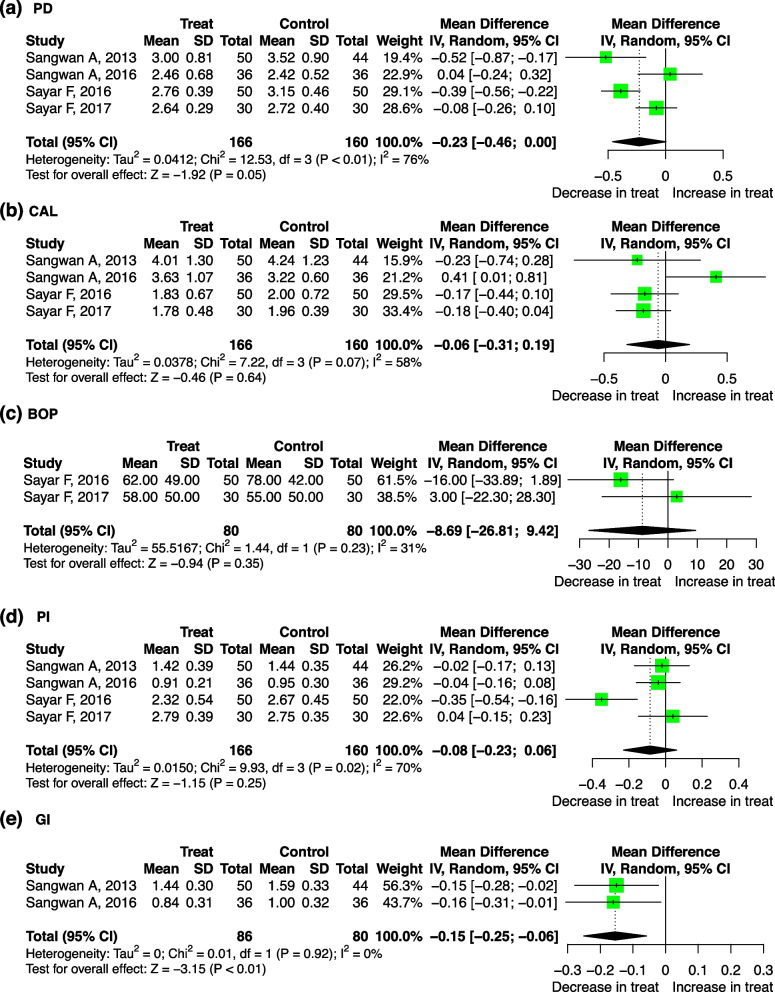
Effect of lipid treatment on periodontitis
Five studies evaluated the difference in the association between the lipid treatment and periodontitis with the mean (SD). No significant publication bias was found after Egger’s and Begg’s tests (p > 0.05).
Compared with that of the control group, the level of GI in the dyslipidemia patients who received the lipid treatment decreased significantly, with a pooled mean difference of − 0.15 (95%-CI: − 0.25, − 0.06, p < 0.01). There was no significant heterogeneity between the studies (I2= 0, p = 0.92) (Fig. 7e).
Fig. 7.
Forest plot of mean difference for comparisons: lipid-lowering treatment versus non-treatment among hyperlipidemia patients. a lipid-lowering treatment can decrease PD; (b) lipid-lowering treatment do not significantly decrease CAL (c) lipid-lowering treatment do not significantly decrease BOP; (d) lipid-lowering treatment do not significantly decrease PI; (e) lipid-lowering treatment can decrease GI. Abbreviations: PD: probing depth, CAL: clinical attachment level, BOP: bleeding on probing, PI: plaque index, GI: gingival index
We found no statistically significant difference in PD, CAL, BOP, or PI between the treatment and control groups (Fig. 7). Through meta-regression, it was determined that the sources of the heterogeneity may be the total sample size for PD (p = 0.017), study design for CAL (p = 0.007), and age for PI (p = 0.028) (Table S7).
The following results are reported in related studies that are not included in the forest map. Özlem FENTOĞLU reported that 2 months after the periodontal treatment and lipid treatment, PI, GI, BOP, and PD in the statin treatment group were significantly reduced, while similar results were observed in the diet control group [57].
Discussion
Dyslipidemia is a representative metabolic disease, which is widely speculated to be the important agents that promotes periodontitis. In our study, we set out to determine whether dyslipidemia has similar effects on periodontitis as diabetes mellitus and if it reduces blood lipid levels to help treat periodontitis in patients with dyslipidemia.
Our research results are as follows: first, increasing plasma TC, TG, LDL and reduced HDL levels were risk factors for periodontitis. The periodontal parameters CAL, PD and PI of patients with dyslipidemia were significantly worse. Second, compared with that of the baseline, the plasma lipid levels of patients with dyslipidemia who completed the periodontal treatment were significantly improved after 3 months. Third, for patients with dyslipidemia, periodontal parameters except GI were not significantly improved with statins when compared with the diet control therapy. Our research has identified the association between dyslipidemia and periodontitis, we speculate that cytokines may be the key to linking the two diseases. Bacteria are the major pathogenic factors of periodontal disease. The stimulation of microbes promotes the secretion of cytokines in hosts to promote inflammation by autocrine or paracrine signalling [89]. Bacteria are very important in promoting the progression of periodontitis and the pathological manifestations of active periodontitis. For example, IL-1 and TNF-α affect the function of endothelial cells, leading to the accumulation of neutrophils and monocytes at the site of inflammation [90]. Probing depth (PD), clinical attachment loss (CAL), and bleeding on probing (BOP) are closely related to the increase in MMP levels, pathogens in dental plaque are able to stimulate host cells to increase their MMP release [91]. By means of the analysis of 10 researches, including 485 periodontitis patients and 379 healthy controls, Lin Zhang find that the salivary MMP-8 levels were significantly higher in periodontitis patients compared with healthy controls [92]. Indeed, a decrease in the levels of MMPs in the crevicular fluid has been observed after the treatment of periodontitis. This demonstrates that the levels of MMPs are in a dynamic balance with the state of hygiene and health of periodontal tissues [93, 94]. These inflammatory factors are also related to the development of dyslipidemia.
Several lines of evidence suggested that patients with dyslipidemia exhibited higher TNF-α plasma concentrations, which correlated significantly with the concentrations of VLDL, triglycerides and cholesterol and correlated negatively with HDL cholesterol [93–95]. The use of fenofibrate to treat hyperlipoproteinemia IIB leads to decreased levels of TC, TG, and LDL, which correlate with a decreased concentration of TNF-α [96].
Özlem Fentoğlu found significant correlations between serum and gingival crevicular fluid cytokines (IL-1β and TNF-α) and the TC/HDL ratio in patients with dyslipidemia [56]. A study showed that plasma free fatty acid and glycerol concentrations increased transiently after an injection of TNF [97].
Based on the studies above, we found that cytokines (especially TNF-α) play a critical role in the occurrence and development of periodontitis and dyslipidemia. Perhaps this is an important reason why the two diseases interact with each other. We speculate that the treatment of one disease may also affect the development of the other.
As a standard method for treating periodontitis, non-surgical periodontal treatment has been used in clinical work for a long time. Many studies have shown that after an effective periodontal treatment, the blood lipid levels in plasma are significantly improved. Research by Fu YW et al. showed that the levels of TNF-α, IL-1β, and IL-6 in the periodontal treatment group were significantly lower than those treated only with supragingival scaling [69].
As a conventional drug for the treatment of dyslipidemia, statins have been reported to inhibit the immune reactivity of inflammatory cells [98]. Lin SK found that simvastatin inhibited the effects of TNF-α in a dose-dependent manner [99]. Several studies have documented that when atorvastatin gel is placed subgingivally as an adjunct to scaling and root planning, it leads to significant periodontal regeneration [100, 101]. However, in our study, one unanticipated result was that for patients with dyslipidemia who received the systemic therapy, statins did not significantly improve periodontal parameters except GI when compared with that of the diet control therapy. The limited number of studies available may undermine the accuracy of the results.
This study indicates that there is a bi-directional correlation between dyslipidemia and chronic periodontitis. Controlling blood lipid levels may improve the effect of non-surgical periodontal treatments on periodontitis. Maintaining periodontal health is also beneficial for the conditions of lipids in dyslipidemia patients. We can also perform combined treatment when necessary.
We are aware that our study has limitations that should be considered. First, studies with invalid or negative results tend not to be published, so it is difficult to completely prevent publication bias. Second, due to the different diagnoses of periodontitis or dyslipidemia in different countries, our inclusion criteria cannot be completely unified. In this study, significant heterogeneity was found, perhaps due to the region (European/Americas or Asian), criterion of Pd diagnosis, publication year, study design, age ratio, etc., which may undermine the validity of the results. Third, regarding the effect of lipid treatments on periodontitis, the limited number of available studies limits the ability to obtain a comprehensive result.
Conclusion
Overall, we can conclude that there is a bi-direction relationship between dyslipidemia and periodontitis. Periodontal therapy can improve the condition of dyslipidemia, but we did not observe a periodontitis-improving effect when statins were systematically used.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- TC
Total Cholesterol
- TGs
Triglycerides
- LDL
Low-density lipoprotein
- HDL
High-density lipoprotein
- GI
Gingival index
- Pd
Periodontal disease
- T2DM
Type 2 diabetes mellitus
- IBD
Inflammatory bowel disease
- PD
Probing Depth
- CAL
Clinical attachment level
- BOP
Bleeding on probing
- PI
Plaque index
- CVD
Cardiovascular disease
- CPI
Community periodontal index
- NOS
Newcastle–Ottawa Scale
- AHRQ
Agency for Healthcare Research and Quality
- MD
Mean difference
- CI
Confidence interval
Authors’ contributions
MWT, ZZL, LB and WZ designed the study. MWT, ZZL, LB and FJ extracted, analyzed, and interpreted the data. MWT drafted the manuscript. ZZL, YLS, LDJ and SZY review the manuscript. GJY and HQN revised the manuscript. All authors read and approved the final version of the manuscript.
Funding
This article was supported by National Natural Science Foundations of China (No. 82101017, 81972532); Guangdong Basic and Applied Basic Research Foundation (2020A1515110741).
Availability of data and materials
All data generated or analyzed during the present study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Wanting Ma and Zhaolei Zou are co-first authors and contributed equally to this article.
Contributor Information
Bin Li, Email: libin48@mail.sysu.edu.cn.
Juan Fang, Email: fangj6@mail2.sysu.edu.cn.
References
- 1.Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet (London, England). 2005;366(9499):1809–1820. doi: 10.1016/S0140-6736(05)67728-8. [DOI] [PubMed] [Google Scholar]
- 2.Kinane DF, Stathopoulou PG, Papapanou PN. Periodontal diseases. Nat Rev Dis Primers. 2017;3:17038. doi: 10.1038/nrdp.2017.38. [DOI] [PubMed] [Google Scholar]
- 3.GBD 2017 Oral Disorders Collaborators. Bernabe E, Marcenes W, Hernandez CR, Bailey J, Abreu LG, Alipour V, Amini S, Arabloo J, Arefi Z, Arora A, Ayanore MA, Bärnighausen TW, Bijani A, Cho DY, Chu DT, Crowe CS, Demoz GT, Demsie DG, Dibaji Forooshani ZS, et al. Global, regional, and National Levels and trends in burden of Oral conditions from 1990 to 2017: A systematic analysis for the global burden of disease 2017 study. J Dent Res. 2020;99(4):362–373. doi: 10.1177/0022034520908533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hajishengallis G, Chavakis T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat Rev Immunol. 2021;21(7):426–440. doi: 10.1038/s41577-020-00488-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leite F, Nascimento GG, Scheutz F, López R. Effect of smoking on periodontitis: A systematic review and Meta-regression. Am J Prev Med. 2018;54(6):831–841. doi: 10.1016/j.amepre.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 6.Preshaw PM, Alba AL, Herrera D, Jepsen S, Konstantinidis A, Makrilakis K, Taylor R. Periodontitis and diabetes: a two-way relationship. Diabetologia. 2012;55(1):21–31. doi: 10.1007/s00125-011-2342-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu S, Zhang G, Guo JF, Tan YH. Associations between osteoporosis and risk of periodontitis: A pooled analysis of observational studies. Oral Dis. 2021;27(2):357–369. doi: 10.1111/odi.13531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pirillo A, Casula M, Olmastroni E, Norata GD, Catapano AL. Global epidemiology of dyslipidaemias. Nat Rev Cardiol. 2021;18(10):689–700. doi: 10.1038/s41569-021-00541-4. [DOI] [PubMed] [Google Scholar]
- 9.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clin Res ed). 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group, Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clin Res ed). 2011;343:d5928. 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed]
- 11.Al-Otaibi DH, Babay NA, Habib SS, Almas K. Assessment of lipid profile in Saudi type 2 diabetic and non-diabetic periodontal patients. Saudi Med J. 2008;29(5):723–727. [PubMed] [Google Scholar]
- 12.Akkaloori A, Parthasarathi P, Anjum MS, Gadde P, Mocherla M, Rao Y. Association between chronic periodontal disease and cardiovascular risk factor hyperlipidemia. J Dr Ntr Univ Health Sci. 2014; 10.4103/2277-8632.146628.
- 13.Banihashemrad SA, Moeintaghavi A, Rafighdoost A. Relationship between cholesterol and triglyceride blood values and periodontal parameters in patients of Mashhad health center. New York State Dent J. 2008;74(5):65–66. [PubMed] [Google Scholar]
- 14.Bullon P, Jaramillo R, Santos-Garcia R, Rios-Santos V, Ramirez M, Fernandez-Palacin A, Fernandez-Riejos P. Relation of periodontitis and metabolic syndrome with gestational glucose metabolism disorder. J Periodontol. 2014;85(2):e1–e8. doi: 10.1902/jop.2013.130319. [DOI] [PubMed] [Google Scholar]
- 15.Cury EZ, Santos VR, Maciel S, Gonçalves T, Zimmermann GS, Mota R, Figueiredo LC, Duarte PM. Lipid parameters in obese and normal weight patients with or without chronic periodontitis. Clin Oral Investig. 2018;22(1):161–167. doi: 10.1007/s00784-017-2095-1. [DOI] [PubMed] [Google Scholar]
- 16.Iacopino AM, Cutler CW. Pathophysiological relationships between periodontitis and systemic disease: recent concepts involving serum lipids. J Periodontol. 2000;71(8):1375–1384. doi: 10.1902/jop.2000.71.8.1375. [DOI] [PubMed] [Google Scholar]
- 17.Doraiswamy S, Yen VA. The plasma lipid level in periodontal health and disease- a case-control study. J Evol Med Dent Sci. 2017;6(48):3728–3730. doi: 10.14260/Jemds/2017/804. [DOI] [Google Scholar]
- 18.Fentoğlu Ö, Tözüm Bulut M, Doğan B, Kırzıoğlu FY, Kemer Doğan ES. Is the relationship between periodontitis and hyperlipidemia mediated by lipoprotein-associated inflammatory mediators? J Periodontal Implant Sci. 2020;50(3):135–145. doi: 10.5051/jpis.2020.50.3.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Golpasand H, Tian Y, Meng H, Hou J, Xu L, Zhang L, Shi D, Lu R, Feng X, Wang X, Chen Z. Associations of apolipoprotein E and low-density lipoprotein receptor-related protein 5 polymorphisms with dyslipidemia and generalized aggressive periodontitis in a Chinese population. J Periodontal Res. 2015;50(4):509–518. doi: 10.1111/jre.12237. [DOI] [PubMed] [Google Scholar]
- 20.Golpasand Hagh L, Zakavi F, Hajizadeh F, Saleki M. The association between hyperlipidemia and periodontal infection. Iran Red Crescent Med J. 2014;16(12):e6577. doi: 10.5812/ircmj.6577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Güler B, Doan E, Onba K. The relationship between monocyte count to high-density lipoprotein ratio and severity of inflammation in aggressive periodontitis: a retrospective analysis. Meandros Med Dent J. 2020;21(2):122–127. doi: 10.4274/meandros.galenos.2020.41033. [DOI] [Google Scholar]
- 22.Hamissi J, Shahsavarani MT, Hamissi H. A comparison of serum lipid profile between periodontitis patients and healthy individuals. Iran Red Crescent Med J. 2011;13(4):283–284. doi: 10.5681/jpid.2010.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Han SJ, Yi YJ. The association between dyslipidemia, oral health behavior, and periodontal disease: The Korea National Health and Nutrition Examination Survey. Quintessence Int (Berlin, Germany : 1985). 2019;50(5):394–401. 10.3290/j.qi.a42294. [DOI] [PubMed]
- 24.Kalburgi V, Leburu S, Warad S. Saliva as a surrogate to explore the association between lipid profiles and chronic periodontitis: A case-control study. Dent Res J. 2014;11(6):619–623. [PMC free article] [PubMed] [Google Scholar]
- 25.Kim SR, Nam SH. Association between periodontal disease and levels of triglyceride and Total cholesterol among Korean adults. Healthcare (Basel, Switzerland). 2020;8(3):337. doi: 10.3390/healthcare8030337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koshy BS, Mahendra J. The association between periodontal status, serum lipid levels, lipoprotein associated Phosholipase A2 (Lp-PLA2) in chronic periodontitis subjects and healthy controls. J Clin Diagnostic Res : JCDR. 2017;11(9):ZC17–21. 10.7860/JCDR/2017/27628.10565. [DOI] [PMC free article] [PubMed]
- 27.Kumar KR, Ranganath V, Naik R, Banu S, Nichani AS. Assessment of high-sensitivity C-reactive protein and lipid levels in healthy adults and patients with coronary artery disease, with and without periodontitis--a cross-sectional study. J Periodontal Res. 2014;49(6):836–844. doi: 10.1111/jre.12172. [DOI] [PubMed] [Google Scholar]
- 28.Kushiyama M, Shimazaki Y, Yamashita Y. Relationship between metabolic syndrome and periodontal disease in Japanese adults. J Periodontol. 2009;80(10):1610–1615. doi: 10.1902/jop.2009.090218. [DOI] [PubMed] [Google Scholar]
- 29.Lee JB, Yi HY, Bae KH. The association between periodontitis and dyslipidemia based on the fourth Korea National Health and nutrition examination survey. J Clin Periodontol. 2013;40(5):437–442. doi: 10.1111/jcpe.12095. [DOI] [PubMed] [Google Scholar]
- 30.Lee S, Im A, Burm E, Ha M. Association between periodontitis and blood lipid levels in a Korean population. J Periodontol. 2018;89(1):28–35. doi: 10.1902/jop.2017.170111. [DOI] [PubMed] [Google Scholar]
- 31.Lösche W, Karapetow F, Pohl A, Pohl C, Kocher T. Plasma lipid and blood glucose levels in patients with destructive periodontal disease. J Clin Periodontol. 2000;27(8):537–541. doi: 10.1034/j.1600-051x.2000.027008537.x. [DOI] [PubMed] [Google Scholar]
- 32.Machado AC, Quirino MR, Nascimento LF. Relation between chronic periodontal disease and plasmatic levels of triglycerides, total cholesterol and fractions. Braz Oral Res. 2005;19(4):284–289. doi: 10.1590/s1806-83242005000400009. [DOI] [PubMed] [Google Scholar]
- 33.Moeintaghavi A, Haerian-Ardakani A, Talebi-Ardakani M, Tabatabaie I. Hyperlipidemia in patients with periodontitis. J Contemp Dent Pract. 2005;6(3):78–85. doi: 10.5005/jcdp-6-3-78. [DOI] [PubMed] [Google Scholar]
- 34.Moghaddam SA, Abbasi S, Moghaddam ES, Moghaddam AA. Triglyceride and cholesterol levels in patients with chronic periodontitis. 2015. [Google Scholar]
- 35.Monteiro AM, Jardini MA, Alves S, Giampaoli V, Aubin EC, Figueiredo Neto AM, Gidlund M. Cardiovascular disease parameters in periodontitis. J Periodontol. 2009;80(3):378–388. doi: 10.1902/jop.2009.080431. [DOI] [PubMed] [Google Scholar]
- 36.Nibali L, D’Aiuto F, Griffiths G, Patel K, Suvan J, Tonetti MS. Severe periodontitis is associated with systemic inflammation and a dysmetabolic status: a case-control study. J Clin Periodontol. 2007;34(11):931–7. 10.1111/j.1600-051X.2007.01133.x. [DOI] [PubMed]
- 37.Penumarthy S, Penmetsa GS, Mannem S. Assessment of serum levels of triglycerides, total cholesterol, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol in periodontitis patients. J Indian Soc Periodontol. 2013;17(1):30–35. doi: 10.4103/0972-124X.107471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sandi RM, Pol KG, Basavaraj P, Khuller N, Singh S. Association of Serum Cholesterol, triglyceride, high and low density lipoprotein (HDL and LDL) levels in chronic periodontitis subjects with risk for cardiovascular disease (CVD): A cross sectional study. J Clin Diagnostic Res: JCDR. 2014;8(1):214–216. doi: 10.7860/JCDR/2014/6686.3927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saxlin T, Suominen-Taipale L, Kattainen A, Marniemi J, Knuuttila M, Ylöstalo P. Association between serum lipid levels and periodontal infection. J Clin Periodontol. 2008;35(12):1040–1047. doi: 10.1111/j.1600-051X.2008.01331.x. [DOI] [PubMed] [Google Scholar]
- 40.Shi D, Meng HX, Xu L, Zhang L, Chen ZB, Feng XH. Zhonghua kou qiang yi xue za zhi = Zhonghua kouqiang yixue zazhi. Chin J Stomatol. 2006;41(7):401–402. [PubMed] [Google Scholar]
- 41.Shimazaki Y, Saito T, Yonemoto K, Kiyohara Y, Iida M, Yamashita Y. Relationship of metabolic syndrome to periodontal disease in Japanese women: the Hisayama study. J Dent Res. 2007;86(3):271–275. doi: 10.1177/154405910708600314. [DOI] [PubMed] [Google Scholar]
- 42.Sridhar R, Byakod G, Pudakalkatti P, Patil R. A study to evaluate the relationship between periodontitis, cardiovascular disease and serum lipid levels. Int J Dent Hyg. 2009;7(2):144–150. doi: 10.1111/j.1601-5037.2008.00318.x. [DOI] [PubMed] [Google Scholar]
- 43.Taleghani F, Shamaei M, Shamaei M. Association between chronic periodontitis and serum lipid levels. Acta Med Iran. 2010;48(1):47–50. doi: 10.2298/VSP1209771P. [DOI] [PubMed] [Google Scholar]
- 44.Thapa S, Wei F. Association between high serum Total cholesterol and periodontitis: National Health and nutrition examination survey 2011 to 2012 study of American adults. J Periodontol. 2016;87(11):1286–1294. doi: 10.1902/jop.2016.150648. [DOI] [PubMed] [Google Scholar]
- 45.Thomas B, Prasad RB, Shetty S, Vishakh R. Comparative evaluation of the lipid profile in the serum of patients with type II diabetes mellitus and healthy individuals with periodontitis. Contemp Clin Dent. 2017;8(1):96–101. doi: 10.4103/ccd.ccd_1160_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang Y, Zhong-Rong WU, Shang SH, Dong WL, Zhong-Qin LI, Hua LI, et al. The investigation of the correlation between serum lipid and periodontitis in officeholders of Wuhan. Chin J Conserv Dent. 2007; 10.1016/j.jaci.2004.04.006.
- 47.Zhou SY, Xiao WM, Ouyang XY. Lipoprotein-associated phospholipase A2 and serum lipid levels in subjects with chronic periodontitis and hyperlipidemia. Chin J Dent Res : Off J Sci Sec Chin Stomatol Assoc (CSA). 2012;15(1):25–9. [PubMed]
- 48.Guan X, Wang X, Li Y, Xu J, He L, Xu L, Xu X, Meng H. Glucose and lipid metabolism indexes and blood inflammatory biomarkers of patients with severe periodontitis: A cross-sectional study. J Periodontol. 2023;94(4):554–563. doi: 10.1002/JPER.22-0282. [DOI] [PubMed] [Google Scholar]
- 49.Zhang F, Zhao D, Xu X, Wen P, Li H, Yu R, Cheng T, Zheng Z, Yang H, Yang C, Yao J, Jin L. Periodontitis links to concurrent metabolic disorders and abnormal liver function in pregnant women. Oral Dis. 2022; 10.1111/odi.14364. Advance online publication. [DOI] [PubMed]
- 50.Chen C, Zhu J, Deng X, Yang Z, Lin W, Ma Y, Huang S, Chen L, Liu Y, Zhu F. Severe periodontitis is associated with the serum levels of hypersensitive C reactive protein and lipoprotein-associated phospholipase A2 in the patients of acute ischemic stroke. J Clin Neurosci : Off J Neurosurg Soc Australasia. 2021;88:232–6. 10.1016/j.jocn.2021.04.007. [DOI] [PubMed]
- 51.Almeida Abdo J, Cirano FR, Casati MZ, Ribeiro FV, Giampaoli V, Casarin R, Pimentel SP. Influence of dyslipidemia and diabetes mellitus on chronic periodontal disease. J Periodontol. 2013;84(10):1401–1408. doi: 10.1902/jop.2012.120366. [DOI] [PubMed] [Google Scholar]
- 52.Awartani F, Atassi F. Evaluation of periodontal status in subjects with hyperlipidemia. J Contemp Dent Pract. 2010;11(2):033–040. doi: 10.5005/jcdp-11-2-33. [DOI] [PubMed] [Google Scholar]
- 53.D’Aiuto F, Sabbah W, Netuveli G, Donos N, Hingorani AD, Deanfield J, Tsakos G. Association of the metabolic syndrome with severe periodontitis in a large U.S. population-based survey. J Clin Endocrinol Metab. 2008;93(10):3989–94. 10.1210/jc.2007-2522. [DOI] [PubMed]
- 54.Doğan B, Fentoğlu Ö, Kırzıoğlu FY, Kemer ES, Köroğlu BK, Aksu O, Çarsancaklı SA, Orhan H. Lipoxin A4 and neutrophil/lymphocyte ratio: A possible Indicator in achieved systemic risk factors for periodontitis. Med Sci Monit : Int Med J Exp Clin Res. 2015;21:2485–93. 10.12659/MSM.895115. [DOI] [PMC free article] [PubMed]
- 55.Fentoğlu O, Oz G, Taşdelen P, Uskun E, Aykaç Y, Bozkurt FY. Periodontal status in subjects with hyperlipidemia. J Periodontol. 2009;80(2):267–273. doi: 10.1902/jop.2009.080104. [DOI] [PubMed] [Google Scholar]
- 56.Fentoğlu Ö, Köroğlu BK, Hiçyılmaz H, Sert T, Özdem M, Sütçü R, Tamer MN, Orhan H, Ay ZY, Öztürk Tonguç M, Kırzıoğlu FY. Pro-inflammatory cytokine levels in association between periodontal disease and hyperlipidaemia. J Clin Periodontol. 2011;38(1):8–16. doi: 10.1111/j.1600-051X.2010.01644.x. [DOI] [PubMed] [Google Scholar]
- 57.Fentoğlu Ö, Kırzıoğlu FY, Bulut MT, Kumbul Doğuç D, Kulaç E, Önder C, Günhan M. Evaluation of lipid peroxidation and oxidative DNA damage in patients with periodontitis and hyperlipidemia. J Periodontol. 2015;86(5):682–688. doi: 10.1902/jop.2015.140561. [DOI] [PubMed] [Google Scholar]
- 58.Fukui N, Shimazaki Y, Shinagawa T, Yamashita Y. Periodontal status and metabolic syndrome in middle-aged Japanese. J Periodontol. 2012;83(11):1363–1371. doi: 10.1902/jop.2012.110605. [DOI] [PubMed] [Google Scholar]
- 59.Katz J, Flugelman MY, Goldberg A, Heft M. Association between periodontal pockets and elevated cholesterol and low density lipoprotein cholesterol levels. J Periodontol. 2002;73(5):494–500. doi: 10.1902/jop.2002.73.5.494. [DOI] [PubMed] [Google Scholar]
- 60.Kemer Doğan ES, Kırzıoğlu FY, Doğan B, Fentoğlu Ö, Kale B. The effect of menopause on the relationship between hyperlipidemia and periodontal disease via salivary 8-hydroxy-2′-deoxyguanosine and myeloperoxidase levels. Acta Odontol Scand. 2018;76(2):92–97. doi: 10.1080/00016357.2017.1386798. [DOI] [PubMed] [Google Scholar]
- 61.Lutfioğlu M, Aydoğdu A, Atabay VE, Sakallioğlu EE, Avci B. Gingival crevicular fluid oxidative stress level in patients with periodontal disease and hyperlipidemia. Braz Oral Res. 2017;31:e110. doi: 10.1590/1807-3107bor-2017.vol31.0110. [DOI] [PubMed] [Google Scholar]
- 62.Scardina GA, Pisano T, Cacioppo A, Messina P. Periodontal alteration of the microcirculation and hypercholesterolemia: a possible correlation? South Med J. 2011;104(2):116–120. doi: 10.1097/SMJ.0b013e318205ddf1. [DOI] [PubMed] [Google Scholar]
- 63.Shivakumar T, Patil VA, Desai MH. Periodontal status in subjects with hyperlipidemia and determination of association between hyperlipidemia and periodontal health: a clinicobiochemical study. J Contemp Dent Pract. 2013;14(5):785–789. doi: 10.5005/jp-journals-10024-1403. [DOI] [PubMed] [Google Scholar]
- 64.Yu ZR, Liu LS, Luan QX, Wang XY, Li P, Sha YQ, Liu X. Beijing da xue xue bao. Yi xue ban = J Peking Univ Health Sci. 2012;44(4):633–638. [PubMed] [Google Scholar]
- 65.Zhu H, Ye G, Xie Y, Zhu K, Zhu F, Chen Q. Association of high-density lipoprotein cholesterol and periodontitis severity in Chinese elderly: a cross-sectional study. Clin Oral Investig. 2022;26(7):4753–4759. doi: 10.1007/s00784-022-04439-4. [DOI] [PubMed] [Google Scholar]
- 66.Jung Y, Kim JH, Shin AR, Song KB, Amano A, Choi YH. Association of Adiposity with periodontitis and metabolic syndrome: from the third National Health and nutrition examination survey of United States. Int J Environ Res Public Health. 2023;20(3):2533. doi: 10.3390/ijerph20032533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Duan JY, Ou-Yang XY, Zhou YX. Beijing da xue xue bao. Yi xue ban = J Peking Univ. Health Sci. 2009;41(1):36–39. [PubMed] [Google Scholar]
- 68.Fentoğlu O, Sözen T, Oz SG, Kale B, Sönmez Y, Tonguç MO, Gürgan CA, Aykaç Y, Kirzioğlu FY. Short-term effects of periodontal therapy as an adjunct to anti-lipemic treatment. Oral Dis. 2010;16(7):648–654. doi: 10.1111/j.1601-0825.2010.01668.x. [DOI] [PubMed] [Google Scholar]
- 69.Fu YW, Li XX, Xu HZ, Gong YQ, Yang Y. Effects of periodontal therapy on serum lipid profile and proinflammatory cytokines in patients with hyperlipidemia: a randomized controlled trial. Clin Oral Investig. 2016;20(6):1263–1269. doi: 10.1007/s00784-015-1621-2. [DOI] [PubMed] [Google Scholar]
- 70.Lösche W, Marshal GJ, Apatzidou DA, Krause S, Kocher T, Kinane DF. Lipoprotein-associated phospholipase A2 and plasma lipids in patients with destructive periodontal disease. J Clin Periodontol. 2005;32(6):640–644. doi: 10.1111/j.1600-051X.2005.00725.x. [DOI] [PubMed] [Google Scholar]
- 71.Surdumacovei, A., Rudnic, I., Martu, I., Solomon, S., Pasarin, L., & Martu, S. (2013). Studies regarding the bidirectional relationship between the periodontal disease and hyperlipidaemia.
- 72.Nassar PO, Walker CS, Salvador CS, Felipetti FA, Orrico SR, Nassar CA. Lipid profile of people with diabetes mellitus type 2 and periodontal disease. Diabetes Res Clin Pract. 2012;96(1):35–39. doi: 10.1016/j.diabres.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 73.Nibali L, Rizzo M, Li Volti G, D’Aiuto F, Giglio RV, Barbagallo I, Pelekos G, Donos N. Lipid subclasses profiles and oxidative stress in aggressive periodontitis before and after treatment. J Periodontal Res. 2015;50(6):890–6. 10.1111/jre.12283. [DOI] [PubMed]
- 74.Nicolaiciuc, O. , IG Ursărescu, I Mârţu, L Păsărin, Zaharescu, A. M. , & Luchian, I. , et al. Study on the Effects of Classical Periodontal Therapy on the Lipid Profile in Hyperlipidemic and Chronic Periodontitis Patients.
- 75.Oz SG, Fentoglu O, Kilicarslan A, Guven GS, Tanrtover MD, Aykac Y, Sozen T. Beneficial effects of periodontal treatment on metabolic control of hypercholesterolemia. South Med J. 2007;100(7):686–691. doi: 10.1097/SMJ.0b013e31802fa327. [DOI] [PubMed] [Google Scholar]
- 76.Tawfig A. Effects of non-surgical periodontal therapy on serum lipids and C-reactive protein among hyperlipidemic patients with chronic periodontitis. J Int Soc Prev Community Dent. 2015;5(Suppl 1):S49–S56. doi: 10.4103/2231-0762.156524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zuza EP, Barroso EM, Fabricio M, Carrareto AL, Toledo BE, Pires R, J. Lipid profile and high-sensitivity C-reactive protein levels in obese and non-obese subjects undergoing non-surgical periodontal therapy. J Oral Sci. 2016;58(3):423–30. 10.2334/josnusd.16-0173. [DOI] [PubMed]
- 78.Kolte AP, Kolte RA, Bawankar PV, Bajaj VA. Assessment and correlation of the influence of non-surgical periodontal therapy on serum lipid profile and cytokines in patients with stage III periodontitis. Int J Dent Hyg. 2023;21(2):298–304. doi: 10.1111/idh.12639. [DOI] [PubMed] [Google Scholar]
- 79.Fentoğlu Ö, Kirzioğlu FY, Tözüm Bulut M, Kurgan Ş, Koçak H, Sütcü R, Kale Köroğlu B, Günhan M. Serum Lp-PLA2: as a novel viewpoint in periodontal treatment of hyperlipidaemics. Turk J Med Sci. 2015;45(3):619–626. doi: 10.3906/sag-1406-75. [DOI] [PubMed] [Google Scholar]
- 80.Sangwan A, Tewari S, Singh H, Sharma RK, Narula SC. Periodontal status and hyperlipidemia: statin users versus non-users. J Periodontol. 2013;84(1):3–12. doi: 10.1902/jop.2012.110756. [DOI] [PubMed] [Google Scholar]
- 81.Sangwan A, Tewari S, Singh H, Sharma RK, Narula SC. Effect of hyperlipidemia on response to nonsurgical periodontal therapy: statin users versus nonusers. Eur J Dentist. 2016;10(1):69–76. doi: 10.4103/1305-7456.175685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sayar F, Fallah S, Akhondi N, Jamshidi S. Association of serum lipid indices and statin consumption with periodontal status. Oral Dis. 2016;22(8):775–780. doi: 10.1111/odi.12545. [DOI] [PubMed] [Google Scholar]
- 83.Sayar F, Akhondi N, Fallah S, Moalemnia AA, Cheraghi A. Association of Serum Triglyceride Level and Gemfibrozil Consumption with Periodontal Status. J Periodontol. 2017;88(5):457–463. doi: 10.1902/jop.2016.160366. [DOI] [PubMed] [Google Scholar]
- 84.Hu J, Dong Y, Chen X, Liu Y, Ma D, Liu X, Zheng R, Mao X, Chen T, He W. Prevalence of suicide attempts among Chinese adolescents: A meta-analysis of cross-sectional studies. Compr Psychiatry. 2015;61:78–89. doi: 10.1016/j.comppsych.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 85.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 86.Li B, Lu Y, Wang L, Zhang CX. Folate intake and breast cancer prognosis: a meta-analysis of prospective observational studies. Eur J Cancer Prevention : Off J Eur Cancer Prevention Org (ECP). 2015;24(2):113–21. 10.1097/CEJ.0000000000000028. [DOI] [PubMed]
- 87.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clin Res ed). 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Patsopoulos NA, Evangelou E, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. 2008;37(5):1148–1157. doi: 10.1093/ije/dyn065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Birkedal-Hansen H. Role of cytokines and inflammatory mediators in tissue destruction. J Periodontal Res. 1993;28(6 Pt 2):500–510. doi: 10.1111/j.1600-0765.1993.tb02113.x. [DOI] [PubMed] [Google Scholar]
- 90.Page RC. The role of inflammatory mediators in the pathogenesis of periodontal disease. J Periodontal Res. 1991;26(3 Pt 2):230–242. doi: 10.1111/j.1600-0765.1991.tb01649.x. [DOI] [PubMed] [Google Scholar]
- 91.Franco C, Patricia HR, Timo S, Claudia B, Marcela H. Matrix metalloproteinases as regulators of periodontal inflammation. Int J Mol Sci. 2017;18(2):440. doi: 10.3390/ijms18020440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhang L, Li X, Yan H, Huang L. Salivary matrix metalloproteinase (MMP)-8 as a biomarker for periodontitis: A PRISMA-compliant systematic review and meta-analysis. Medicine. 2018;97(3):e9642. doi: 10.1097/MD.0000000000009642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Luchian I, Goriuc A, Sandu D, Covasa M. The Role of Matrix Metalloproteinases (MMP-8, MMP-9, MMP-13) in Periodontal and Peri-Implant Pathological Processes. Int J Mol Sci. 2022;23(3):1806. doi: 10.3390/ijms23031806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chen X, Xun K, Chen L, Wang Y. TNF-alpha, a potent lipid metabolism regulator. Cell Biochem Funct. 2009;27(7):407–416. doi: 10.1002/cbf.1596. [DOI] [PubMed] [Google Scholar]
- 95.Jovinge S, Hamsten A, Tornvall P, Proudler A, Båvenholm P, Ericsson CG, Godsland I, de Faire U, Nilsson J. Evidence for a role of tumor necrosis factor alpha in disturbances of triglyceride and glucose metabolism predisposing to coronary heart disease. Metab Clin Exp. 1998;47(1):113–118. doi: 10.1016/s0026-0495(98)90203-7. [DOI] [PubMed] [Google Scholar]
- 96.Madej A, Okopień B, Kowalski J, Zieliński M, Wysocki J, Szyguła B, Kalina Z, Herman Z. Stezenia czynnika martwicy nowotworów alfa w surowicy pacjentów z hiperlipoproteinemia IIb przed i po podjeciu teràpii fenofibratem mikronizowanym [levels of tumor necrosis factor alpha in serum of patients with hyperlipoproteinemia IIB before and after micronized fenofibrate therapy] Polskie Arch Med Wewnetrznej. 1998;99(4):308–313. [PubMed] [Google Scholar]
- 97.Van der Poll T, Romijn JA, Endert E, Borm JJ, Büller HR, Sauerwein HP. Tumor necrosis factor mimics the metabolic response to acute infection in healthy humans. Am J Phys. 1991;261(4 Pt 1):E457–E465. doi: 10.1152/ajpendo.1991.261.4.E457. [DOI] [PubMed] [Google Scholar]
- 98.Kajimoto K, Miyauchi K, Kasai T, Shimada K, Kojima Y, Shimada A, Niinami H, Amano A, Daida H. Short-term 20-mg atorvastatin therapy reduces key inflammatory factors including c-Jun N-terminal kinase and dendritic cells and matrix metalloproteinase expression in human abdominal aortic aneurysmal wall. Atherosclerosis. 2009;206(2):505–511. doi: 10.1016/j.atherosclerosis.2009.03.028. [DOI] [PubMed] [Google Scholar]
- 99.Lin SK, Kok SH, Lee YL, Hou KL, Lin YT, Chen MH, Wang CC, Hong CY. Simvastatin as a novel strategy to alleviate periapical lesions. J Endod. 2009;35(5):657–662. doi: 10.1016/j.joen.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 100.Shirke PY, Kolte AP, Kolte RA, Bawanakar PV. Evaluation of the clinical efficacy of 1.2% atorvastatin in the treatment of periodontal intraosseous defects by CBCT: A randomized controlled clinical trial. J Dent Res, Dent Clin, Dent Prospects. 2019;13(3):183–191. doi: 10.15171/joddd.2019.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Pradeep AR, Kumari M, Rao NS, Martande SS, Naik SB. Clinical efficacy of subgingivally delivered 1.2% atorvastatin in chronic periodontitis: a randomized controlled clinical trial. J Periodontol. 2013;84(7):871–879. doi: 10.1902/jop.2012.120393. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during the present study are included in this published article.