Abstract
Less than 1% of studies on racialized health inequities have empirically examined their root cause: structural racism. Moreover, there has been a disconnect between the conceptualization and measurement of structural racism. This study advances the field by (1) distilling central tenets of theories of structural racism to inform measurement approaches, (2) conceptualizing U.S. states as racializing institutional actors shaping health, (3) developing a novel latent measure of structural racism in states, (4) using multilevel models to quantify the association between structural racism and five individual-level health outcomes among respondents from the Health and Retirement Study (N = 9,020) and the Behavioral Risk Factor Surveillance System (N = 308,029), and (5) making our measure of structural racism publicly available to catalyze research. Results show that structural racism is consistently associated with worse health for Black people but not White people. We conclude by highlighting this study’s contributions (theoretical, methodological, and substantive) and important avenues for future research on the topic.
Keywords: health disparities, methods, population health, race, structural racism
The development of sound measures of structural racism is an urgent public health issue.
—Hardeman et al. (2022: 180)
Racial stratification is an enduring part of the fabric of U.S. society. More than a century ago, Du Bois’s (1899) seminal scholarship provided theoretical and empirical foundations for understanding how the life chances of Black Americans are limited by racism. Contemporary research on race also foregrounds structural forms of racism to understand racial stratification. Structural racism involves interconnected systems of racial discrimination across societal domains (e.g., economic, educational, political, social, and criminal-legal domains) that create and perpetuate the relational subordination of minoritized groups. These conditions are reflected in inequalities within institutions, and they both reinforce—and are reinforced by—cultures of white supremacy (Bonilla-Silva 1997; Brown and Homan 2023; Lee 2024; Mills 1997; Ray 2019).
To develop efficacious health policy and health equity interventions, it is crucial to have a sound empirical understanding of the nature of structural racism and its effects on population health. Despite the centrality of structural explanations for understanding racial inequality within the U.S. racialized social system (Baker and O’Connell 2022; Bonilla-Silva 1997; Williams 2023), less than 1% of studies on race and health have empirically examined the health consequences of structural racism (e.g., Bailey et al. 2017). A variety of factors contribute to the scarcity of empirical research on structural racism, including racial essentialism (attributing racial inequalities to “race” and falsely presumed innate and fixed biological or cultural differences rather than racism; Roth, van Stee, and Regla-Vargas 2023); strategic racial ignorance that preserves the status quo (Mills 1997; Mueller 2020); gatekeeping practices at journals that suppress the publication of scientific research on structural racism (Boyd et al. 2020); methodological individualism, characterized by a disproportionate focus on individual-level mechanisms such as socioeconomic factors and perceived discrimination (Brown et al. 2023); and a scattershot data ecosystem on structural racism that functions as a major barrier to studying its etiology and consequences (Brown and Homan 2023).
A growing body of research has begun to theorize about how health is shaped by structural racism (e.g., Brown 2003; Krieger 2014; Phelan and Link 2015; Williams, Lawrence, and Davis 2019). However, greater conceptual clarity is necessary for developing theoretically grounded approaches to measuring structural racism–a complex and insidious de facto phenomena that is often “hidden” or not directly observed. Notably, although the terms “institutional racism” and “structural racism” are often used interchangeably, scholars have distinguished between these concepts, noting that whereas institutional racism refers to a single institution (e.g., discrimination in the criminal-legal system), structural racism refers to broader racialized phenomena involving a multifaceted, interconnected system of racism across societal domains and institutions (Bailey et al. 2017; Bonilla-Silva 1997; Hicken et al. 2021).
Prior empirical studies on structural racism and health have often been limited in several respects. For example, operationalization of structural racism has often been disconnected from its conceptualizations in theories of racism. Studies have typically relied on single indicators of racism (which are often subject to measurement error) or examined several of them separately (e.g., Lukachko, Hatzenbuehler, and Keyes 2014). Importantly, single indicators of racialized discriminatory contexts are typically measures of institutional racism—not structural racism—because they overlook relationships among multiple forms of racism and how they operate as a system and jointly shape health (Bonilla-Silva 1997; Hardeman et al. 2022; Powell 2008). Not only do these approaches fail to capture the extent to which forms of racism are interconnected and reflect an underlying latent construct, but they also lead to an incomplete understanding—and biased estimates—of the impact of structural racism on health (Adkins-Jackson et al. 2021; Brown, Kamis, and Homan 2022). In addition, prior research on the health effects of structural racism has disproportionately focused on racism at census-tract and neighborhood levels, often overlooking the role U.S. states, which operate as key legal, political, social, and administrative units and vary in types and degrees of structural racism (Baker 2022; Bruch, Rosenthal, and Soss 2019; Riley 2018). Moreover, studies have typically examined a single health outcome, which has limited our understanding of the breadth of the health consequences of structural racism (Aneshensel 2005).
Due to limited progress in translating theories of structural racism into concrete measures, and to scant empirical research on the links between structural racism and health, fundamental questions remain unanswered: Does structural racism across societal domains reflect a latent construct? Are there broad-based health consequences of structural racism? Notably, insufficient progress on both conceptual and methodological fronts enables skeptics to dismiss structural racism as a slippery concept for which robust empirical evidence documenting its effects is lacking (Groos et al. 2018).
This study proposes new conceptual and methodological extensions to address gaps in the literature on structural racism in the United States. In particular, we answer fundamental questions about structural racism by conceptualizing and measuring structural racism and quantifying its impact on the health of Black and White adults. First, we distill four core theoretical tenets (multifaceted, interconnected, institutionalized, and relational subordination/superordination that manifests in racial inequalities in life chances) to create a theory-grounded conceptualization of structural racism that improves our ability to measure structural racism and its relationship with health. Second, we introduce the concept of U.S. states as racializing institutional actors shaping population health. Third, we assess the extent to which indicators of racism across multiple institutions and domains (e.g., economics, education, politics, housing, and the criminal-legal system) are interconnected and reflective of an underlying construct of structural racism. We use structural equation modeling to develop a novel latent measure of structural racism—manifest in discriminatory institutional contexts—that enables us to gain empirical traction on this somewhat elusive phenomenon. This latent variable approach is well suited for minimizing measurement error and capturing conceptual properties of a complex system that is difficult to quantify or directly measure, such as structural racism. Fourth, we use multilevel models to quantify the effects of state-level structural racism on five commonly used health outcomes (in two datasets) among Black and White people, net of potential confounders. Fifth, we make our measure of structural racism publicly available, in an effort to lower barriers and catalyze research on the consequences of structural racism. In sum, we advance the literature theoretically, methodologically and substantively by conceptualizing and measuring structural racism at the state level of the U.S. racialized social stratification system, and by providing a more comprehensive and rigorous investigation of the relationship between structural racism and population health.
THEORIZING STRUCTURAL RACISM
This study identifies central tenets of theories of racism to understand its complex nature and guide how it is measured. We build on prior theoretical innovations by distilling foundational ideas of structural racism in the literature to provide conceptual and analytical clarity on the nature and impact of state-level structural racism on racialized health inequalities. Appendix Table A1 (in the online version of the article) lists key descriptions of structural racism in the literature, highlighting central tenets. The list summarizes how features of structural racism are often conceptualized in multiple disciplines and literatures spanning critical race theory, law, philosophy, public health, and sociology. Synthesizing theoretical insights from this literature, we posit that structural racism involves a multifaceted, interconnected, and institutionalized system of relational subordination for people of color and superordination for White people that is observable as manifest racial inequalities in life chances.1 In the following, we briefly unpack each of these foundational principles.
First, structural racism is multifaceted; it is manifest in a wide array of societal domains (Bonilla-Silva 1997; Carmichael and Hamilton 1967). Rather than viewing cases of structural racism as extraordinary and anomalous, race theorists posit that structural racism is an ordinary and nearly ubiquitous social force (Seamster and Ray 2018). Indeed, there is robust evidence of structural racism in numerous domains, including economic (Darity and Mullen 2020), educational (Tyson and Lewis 2021), political (Manza and Uggen 2006), criminal-legal (Lee 2024), and housing systems (Taylor 2019).
A second central tenet of theories of racism is that the various domains and institutions of structural racism are interconnected (Mills 1997; Reskin 2012). Consistent with the notion that structural racism involves an interconnected system, the individual domains and institutions are theorized to be mutually reinforcing (Brown et al. 2022; Lee 2024). It is well established, for example, that residential segregation (a key form of structural racism) shapes racial exclusion and subordination in many other areas of life, such as education, employment, and experience with the criminal-legal system (Massey and Denton 1993; Sewell 2016), thereby contributing to other forms of structural racism. Taken together, theory and empirical evidence highlighting structural racism as a multifaceted and interconnected system underscore the importance of examining relationships among various domains and institutions of racism and their collective—rather than individual—impact (Gee and Hicken 2021; Reskin 2012).
Third, racism is institutionalized. A primary reason that structural racism leads to myriad racialized inequalities is because it is embedded in societal institutions (Carmichael and Hamilton 1967; Powell 2008). Reskin (2012:23), for example, notes that structural racism constitutes “a system that infects American society and all of its institutions with race discrimination.” Similarly, Sewell (2016:404) foregrounds the role of institutions, positing that structural racism involves “racial domination, whereby inequality is etched into the rules, norms, and logics of institutions in ways that further disadvantage racially marginalized people and privilege racially dominant people.” Contemporary racism is normative and often takes the form of institutional policies and practices that appear to be “race-neutral” (i.e., not explicitly race-based) but have disproportionate negative impacts on racial minorities (Seamster and Ray 2018).
Building on influential new research that highlights the salience of U.S. states for well-being (Montez and Grumbach 2023; Montez, Hayward, and Zajacova 2019), this study conceptualizes U.S. states as “racializing institutional actors” that shape population health. Throughout the history of the United States, states have played a central role in sanctioning, exacerbating, and alleviating racial oppression. In the contemporary era, the ostensibly race-neutral policies and practices that continue the legacy of racial oppression—such as voter disenfranchisement, gerrymandering, welfare state contraction, mandatory minimum sentencing, and three-strikes laws—are often products of political processes within states (Alexander 2011; Homan and Brown 2022). As Bruch et al. (2019:163) note, “The state in which one resides has significant consequences for one’s opportunities and life conditions and . . . for the structure of racial relations one must traverse.” The historical and contemporary roles of state-level institutions in creating and maintaining racialized social systems (Baker 2022; Bruch et al. 2019; Feagin and Bennefield 2014) make U.S. states an important unit of analysis for studying structural racism and its health consequences.
Fourth, structural theories on race underscore how racism involves relational subordination/superordination that manifests in racial inequities in life chances (Du Bois 1899; Mills 1997; Ray 2022). For example, the theory of racialized social systems underscores how racial inequities are not due to biological, behavioral, or cultural deficits among minoritized groups but, rather, are a product of a socially constructed, hegemonic racial hierarchy in which Black people are subordinate and viewed as inferior and White people are superordinate and considered superior (Bonilla-Silva 1997; Williams 2023). Consistent with a relational approach to race, Seamster and Ray (2018:333) note that “whites’ well-being is the manifestation of a hierarchal system. Whites are doing better because the structural relations of race benefit, reward, and empower them.” Indeed, there is overwhelming consensus among race scholars that structural racism is a progenitor, or root cause, of racialized inequalities in life chances (Mills 1997; Tyson and Lewis 2021; Williams 2023), which has important implications for how structural racism should be operationalized. For example, a nascent but growing literature has operationalized structural racism using state-level measures of Black–White inequities in societal institutions (Homan and Brown 2022; Lukachko et al. 2014; Mesic et al. 2018; Wallace et al. 2017), in alignment with the notion that that structural racism pervades institutions and leads to disadvantages for people of color and advantages for White people (Mills 1997; Ray 2019).
Taken together, this literature offers important insights into how tenets of structural theories of racism can be used to inform measurement of structural racism. Namely, structural racism measures should capture racism in multiple domains (multifaceted) and the relationships among them (interconnectedness), how it is embedded in institutions (institutionalized), and relational subordination/superordination manifest in racial inequities in life chances (e.g., poverty, education, political representation, incarceration, and segregation; Adkins-Jackson et al. 2021; Brown et al. 2022; Hardeman et al. 2022).
EMPIRICAL RESEARCH ON STATE-LEVEL STRUCTURAL RACISM AND HEALTH
Although the vast majority of studies on the racism–health relationship have focused on consequences of perceived interpersonal discrimination, there is a growing body of empirical research on the health consequences of structural racism (Dean and Thorpe 2022; Hardeman et al. 2022; Williams et al. 2019). Several recent scoping review articles provide useful overviews of health-related studies that have quantified aspects of structural racism (Groos et al. 2018; Hing et al. forthcoming). These reviews highlight how empirical research on the topic has disproportionately focused on the health consequences of racial residential segregation, which is rampant and extreme in the United States—largely driven by racialized political economic processes, such as historical and contemporary discriminatory governmental policies (e.g., exclusion from financial benefits of the New Deal and GI Bill) and other institutional practices (e.g., unfair lending, redlining, steering and blockbusting; Korver-Glenn 2021; Sewell 2016; Taylor 2019).
In addition to residential segregation, an emerging literature has also explored how health is shaped by place-based racism in other domains. For instance, these studies have examined the health consequences of racism—as measured by areal racial inequities—in economic (O’Brien et al. 2020), educational (Wallace et al. 2017), political (Homan and Brown 2022), and criminal-legal institutions (Lukachko et al. 2014). Findings from these studies show that individual indicators of racism in a single institution (i.e., institutional racism) are predictive of worse health among Black people (and Black–White health inequalities); evidence on the impact of racism on the health of White people is mixed (Groos et al. 2018). Notably, research on the links between place-based racism and health has tended to focus on racism in meso-level environments, such as neighborhoods and counties, leading to calls for research on the structural racism–health relationship to investigate additional meaningful units of analysis, such as U.S. states (Hardeman et al. 2022; Riley 2018). To date, very few empirical studies have investigated the health consequences of racism in U.S. state-level institutions, with several notable exceptions (e.g., Brown et al. 2022; Homan and Brown 2022; Lukachko et al. 2014; Siegel et al. 2022; Wallace et al. 2017).
A study by Lukachko et al. (2014) measured state-level Black–White inequalities in four domains—political participation, education, employment, and judicial treatment—as indicators of place-based racism and examined the impacts of these domains separately. They used dichotomized measures of racism and found that compared to low levels (below the median), high levels (above the median) of Black–White inequality were associated with greater risk of myocardial infarction among Black people. They found the opposite pattern among White people: Higher levels of Black–White inequality across domains were either not associated or were negatively associated with White people’s odds of myocardial infarction. Research on health consequences of state-level racism has also investigated birth outcomes, estimating the impact of individual indicators of discriminatory racialized contexts (e.g., Black–White inequities in unemployment, education, and incarceration) separately and finding that they predict worse birth outcomes for Black people but not White people (Pabayo et al. 2019; Wallace et al. 2017).
One of the few studies on the effects of structural racism on middle-aged and older adults—a population that experiences a disproportionate share of health burdens and whose health has been shaped by decades of differential exposure to racism (Boen et al. 2023; Brown et al. 2023; Garcia et al. 2021)—showed that greater degrees of state-level overrepresentation of Black people among those who have been disenfranchised due to a felony conviction are predictive of worse physical and mental health among Black people but unrelated to the health of their White counterparts (Homan and Brown 2022). In addition, several recent studies have examined associations between population health and state-level summative indices of structural racism across several domains (Homan, Brown, and King 2021; Siegel et al. 2022); however, it is important to note that these summative measures are limited because they make the tenuous assumption that each of the indicators contributes equally to the structural racism construct and its impact on health. Taken together, the handful of empirical studies on links between state-level structural racism and health have provided critical early insights, yet many important questions remain unanswered.
CONTRIBUTIONS OF THIS STUDY
Gaps in our understanding of the health consequences of structural racism are due, in part, to a relative dearth of empirical research on the topic (Bailey et al. 2017; Groos et al. 2018) and a disconnect between theory-grounded conceptualizations of structural racism and the measurement strategies used in population health research. Because prior studies have typically examined the effects of individual indicators of racism across institutions separately (e.g., Homan and Brown 2022; Lukachko et al. 2014; Pabayo et al. 2019; Wallace et al. 2017), we know very little about (a) whether state-level racism across multiple domains and institutional contexts reflects a unified latent construct and (b) whether and how a latent construct of structural racism is associated with population health. Given the multifaceted and interconnected nature of structural racism across domains (Bonilla-Silva 1997; Powell 2008), solely exploring the impact of error-prone observed indicators of place-based racism separately is likely to yield biased estimates and an incomplete picture of the effects of structural racism on health (Bollen 1989; Brown et al. 2022). As Reskin (2012:18) notes, the “unit of analysis from a systems perspective is not individual subsystems but rather the entire system—the forests rather than the trees.” Moreover, because empirical research on links between state-level structural racism and health has tended to focus on a single health measure, the scope of the population health effects of state-level structural racism remains unclear. Examining an array of health outcomes is necessary to enhance our understanding of the breadth of the impact of structural racism on population health (Aneshensel 2005).
In addition to advancing the field by proposing new conceptual extensions, this study addresses fundamental questions and empirical gaps in the literature by measuring structural racism and its impact on the health of Black and White adults. Our approach to measuring state-level structural racism is informed by the key tenets of structural racism theories distilled previously and operationalizations of state-level structural racism used in prior studies (see Brown et al. 2022; Hardeman et al. 2022; Krieger 2020). For example, consistent with the tenet that structural racism is multifaceted, we include nine indicators of state-level racism spanning five domains (economics, education, politics, criminal-legal, and segregation). Moreover, we develop a latent structural racism scale that incorporates relationships among these indicators of racism, which is in line with the idea that structural racism involves an interconnected, multidomain system. In addition, given the institutionalized nature of structural racism and our conceptualization of U.S. states as racializing institutional actors that shape population health, we examine state-level institutionalized racial stratification. Finally, consistent with the tenet that structural racism involves relational subordination/superordination that manifests in racial inequities in life chances, we utilize previously validated measures of institutional manifestations of racism across a range of societal domains, such as state-level White–Black ratios of opportunities (e.g., education, homeownership, voting), Black–White ratios of risks (e.g., poverty, disenfranchisement, and incarceration), and residential segregation (Homan et al. 2021; Krieger 2020; Lukachko et al. 2014; Wallace et al. 2017).
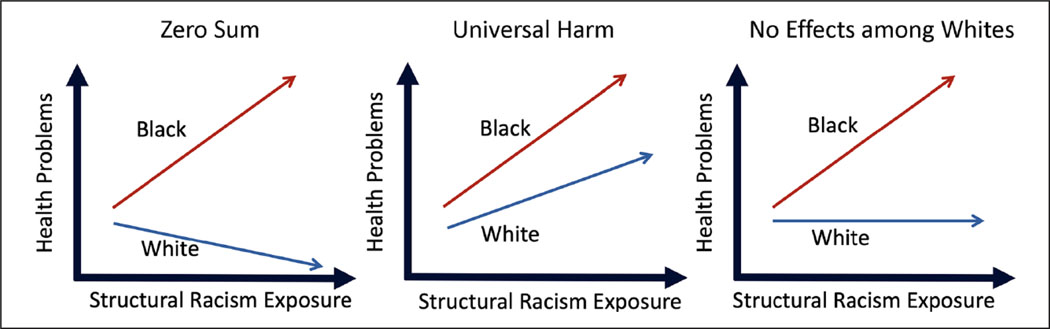
After developing a latent measure of structural racism that is better aligned with key theoretical tenets, we investigate how structural racism shapes multiple health outcomes among Black and White adults (net of several possible state-level confounders) to gain a more comprehensive and robust picture of the health consequences of structural racism. Ecosocial theory (Krieger 2014) posits that structural racism harms the health of Black people via an array of “pathways of embodiment,” such as economic injustice, social deprivation, toxic living conditions, political exclusion, inadequate health care, and psychosocial factors (e.g., social stressors, low control, and stigma of inferiority). A growing literature theorizes about this relationship, but empirical evidence documenting harmful health consequences of structural racism for Black people remains relatively scarce (Bailey et al. 2017; Groos et al. 2018). How structural racism may impact the health of White people is even less clear, with conflicting findings in the literature and multiple theoretical possibilities. Figure 1 illustrates three alternative hypotheses about how the health of Black people and White people is shaped by structural racism (for an example of similar hypotheses, see Homan 2019). On the one hand, it is possible that higher levels of structural racism result in health benefits for White people given their greater relative advantages across many spheres of life (Krieger 2014). A “zero-sum” hypothesis whereby structural racism leads to health disadvantages for Black people and advantages for White people would be consistent with conflict theory and race stratification perspectives (Carmichael and Hamilton 1967; Du Bois 1899). On the other hand, a “universal harm” hypothesis would predict that structural racism is also detrimental to the health of White people (Metzl 2019). This is in line with related theories positing that structural inequalities damage social relationships and make society as a whole less productive, cooperative, safe, and healthy, thereby harming both marginalized and dominant groups—although possibly to different degrees (Homan 2019; McGhee 2021; Wilkinson and Pickett 2011). Finally, it is also possible that White people’s health is unaffected by structural racism or that it appears unaffected because racism benefits White people’s health in some ways (e.g., via control over a greater share of economic resources) while harming their health in other ways (e.g., via decreased social cohesion and investment in public goods) such that the net effect is zero (i.e., structural racism neither helps nor harms the health of White people on balance), consistent with a “no effects/countervailing forces” among White people hypothesis. Thus, the results of this study will provide novel empirical evidence on the racialized health consequences of structural racism.
Figure 1.
Hypotheses about How Structural Racism Affects Health among Black and White people.
DATA AND METHODS
Design Overview
To measure U.S. state-level structural racism manifest in discriminatory institutional contexts and examine its relationship with health among Black and White adults, we used validated indicators of racism at the state level from several sources of publicly available data (see Figure 2) and linked these to geocoded individual-level health and demographic data from the Health and Retirement Study (HRS) and the Behavioral Risk Factor Surveillance System (BRFSS).2
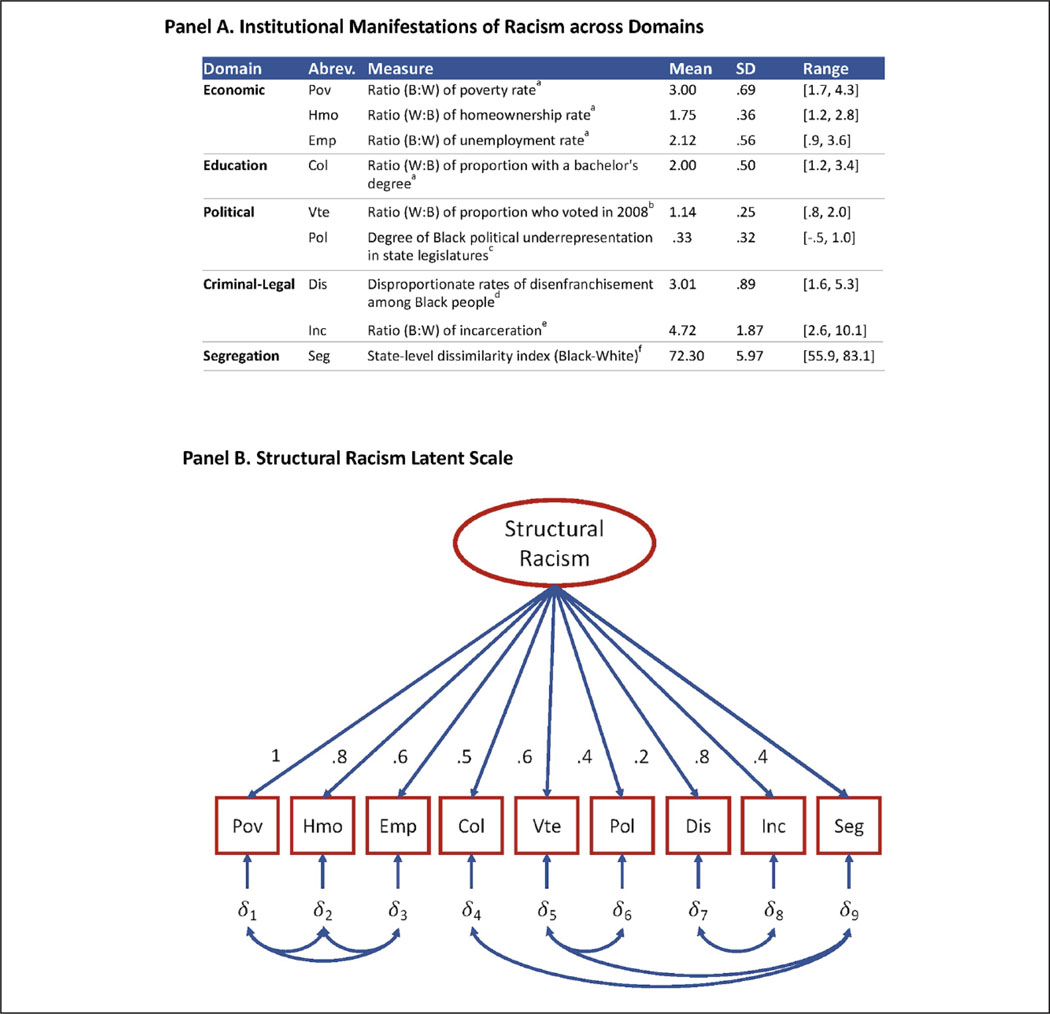
Figure 2.
The Structure of State-Level Racism.
Note: (A) Additional details on the operationalization of the indicators of racism are included in the data and methods section and Appendix B in the online version of the article.
Sources: aIpUMS Current population Survey; bU.S. census; cNational Conference on State Legislatures; dThe Sentencing project; eVera Institute of Justice; fNational Strategic planning and Analysis Research Center. (B) The diagram of the latent scale of structural racism includes factor loadings and correlated errors among state-level indicators of racism as measured by racialized patterns in poverty (pov), home ownership (Hmo), employment (Emp), bachelor’s degrees (Col), voting (Vte), political representation (pol), disenfranchisement (Dis), incarceration (Inc) and segregation (Seg). Model fit statistics: comparative fit index = .959; Tucker-Lewis index = .926, root mean square error of approximation = .076; Bayesian information criterion is negative; chi-squared is not statistically significant. Additional details on confirmatory factor analysis models assessed are included in the data and methods section and Appendix D in the online version of the article.
Sample
The HRS is a nationally representative survey of U.S. civilians over the age of 50 (HRS 2010).3 The HRS includes high-quality an array of health outcomes and demographic factors. This study used HRS data from 2010 (81% response rate). Black people were oversampled to facilitate meaningful assessments of patterns among them. The analytic sample comprised 9,020 U.S.-born respondents, including 2,147 identifying as non-Hispanic Black and 6,873 identifying as non-Hispanic White. Sample sizes varied slightly across health outcomes because there was a small amount of missing health data (<5%).
We also utilized data from the BRFSS, the largest ongoing health survey system in the world (Centers for Disease Control and Prevention 2010). The BRFSS collects health and behavioral data from residents of all 50 states in the United States annually. We used BRFSS data from 2010 to align with our structural racism measures. Our analytic sample consisted of 308,029 individuals, of whom 275,602 identified as non-Hispanic White and 32,427 identified as non-Hispanic Black. To be included in the analytic sample, BRFSS respondents must have had complete data on all variables used in the analysis4 and resided in one of the 37 states for which structural racism measures are available. Similar to prior studies (e.g., Mesic et al. 2018; Montez et al. 2019), 13 states (Alaska, Hawaii, Idaho, Maine, Montana, New Hampshire, New Mexico, North Dakota, Oregon, South Dakota, Utah, Vermont, and Wyoming) were excluded from the analysis because administrative data on Black people were not available due to their very small population size in these states. Two additional states, Delaware and Nebraska, had a Black population size sufficient to calculate a state-level structural racism score but were excluded from the analysis of the relationship between structural racism and health because the samples of Black people from those states in the HRS did not meet the minimum size threshold for disclosure. There were sufficient samples of Black people in the BRFSS, so Delaware and Nebraska were included in those models. It is important to note that based on census data, the 35 states included in the HRS portion of this study account for 99% and 93% of the U.S. Black and White populations, respectively.
Health Outcomes
This study includes five commonly used measures of population health: self-rated health, body mass index (BMI), functional limitations, depressive symptoms, and poor mental health days. Each of these measures have been shown to be reliable and valid among racially diverse samples of community-dwelling U.S. populations. For the sake of concision, details on the operationalization of these variables are included in Appendix B in the online version of the article.
Structural Racism Indicators and Scale
We developed a latent construct scale of state-level structural racism, using (circa) 2010 publicly available data on indicators of racism spanning five domains, including (1) the economy, (2) education, (3) politics, (4) the criminal-legal system, and (5) residential segregation. Figure 2 and Appendix B in the online version of the article provide descriptive statistics and details on each of the indicators of structural racism. Consistent with prior research, state-level racism within the economic domain was assessed using Black-to-White ratios of unemployment (Lukachko et al. 2014) and poverty (Wallace et al. 2017) and White-to-Black ratios of home ownership rates (Mesic et al. 2018). Each of the economic measures was calculated using 2010 IPUMS Current Population Survey (CPS) data (Flood et al. 2023). Racial inequality in educational attainment was measured as the 2010 ratio of the proportion of White people within a state who have a bachelor’s degree to the proportion of Black people with a bachelor’s degree (IPUMS CPS data; Flood et al. 2023; see also Wallace et al. 2017). Racialized political participation measures included indicators of state-level racial inequality in 2008 voting rates (based on data from U.S. Census Bureau n.d.; see also Lukachko et al. 2014) and 2009 political representation (data from National Conference of State Legislatures 2019; see also Brown et al. 2022). State-level variation in racism within the criminal-legal system was reflected by measures of Black–White inequalities in incarceration (data from Vera Institute of Justice 2021; see also Mesic et al. 2018) and felony disenfranchisement in 2010 (based on data from The Sentencing Project by Uggen, Shannon, and Manza 2012; see also Homan and Brown 2022). Finally, our indicator of racial residential segregation—a Black– White dissimilarity index—measures the 2010 spatial distribution of Black and White households (data from the National Strategic Planning and Analysis Research Center; see also Lichter, Parisi, and Taquino 2015).5 This study builds on previous research by using these indicators to develop a latent measure of structural racism and by testing how it is associated with health.
Covariates
The multivariate analyses adjusted for individual-level demographic variables and possible confounding state-level factors. Demographic control measures from HRS and BRFSS data included age (in years) and sex (1 = female, 0 = male). State-level control measures included overall unemployment rate (obtained from 2010 census data); Gini coefficient, a measure of income inequality (data from 2010 census); percentage of the population that is Black (from 2010 census data); and a dummy variable indicating whether the state is in the Southern region of the United States.6
Statistical Analysis
Our statistical analysis addressed fundamental questions by measuring structural racism and quantifying its impact on health. We began with a descriptive approach by examining the means, standard deviations, and ranges of all study variables, which are presented in Appendix B in the online version of the article. Next, we conducted a confirmatory factor analysis (CFA)—a special case of structural equation modeling—to measure the extent to which structural racism across domains was reflective of an underlying construct of structural racism. We used CFA to systematically develop a latent measure of structural racism. In particular, we estimated a series of latent construct models, with varying specifications, to identify the best fitting model based on an array of model fit statistics (e.g., chi-square, Bayesian information criterion [BIC], root mean square error of approximation [RMSEA], comparative fit index [CFI], Tucker-Lewis index [TLI], and omega total). Missing data in measurement models are handled using full information maximum likelihood.
Finally, we estimated multilevel regression models predicting individuals’ health as a function of their structural racism exposure (as measured by factor scores of the latent structural racism construct), controlling for individual demographics and state-level measures of unemployment, income inequality, percentage Black population, and region (see Appendix Tables C1 and C2 in the online version of the article). We used multilevel models to account for the nesting of multiple individuals within a state. Linear regression was used for self-rated health and BMI measures, and negative binomial regression models were used for functional limitation, depressive symptomology, and poor mental health days variables because they were count measures that exhibited overdispersion. Models were stratified by race to examine race-specific associations between structural racism, covariates, and health outcomes. We tested but did not find consistent evidence of statistically significant interactions between socioeconomic status (measured as either income or education) and structural racism exposure on health among either Black or White individuals.
Results from this study were robust to a range of alternative specifications. For example, supplementary analyses that used ordinary least squares (OLS) regression with robust standard errors clustered by U.S. state rather than multilevel models to account for clustering of respondents within states yielded substantively similar results regarding the association between structural racism and health (see Appendix Tables C3 and C4 in the online version of the article). Results using Poisson regression rather than negative binomial also did not notably differ. Robustness checks also showed that OLS and ordinal logit models of the association between structural racism and self-rated health yielded similar results (see Appendix Table C5 in the online version of the article). Further supplemental analyses (available on request) showed that our results were robust to the inclusion of additional state-level controls (e.g., air quality, physician density, the uninsured rate, and percentage of the population living in rural areas) and were not being driven by a few outliers or unusually influential states.
RESULTS
Measuring Structural Racism: A Latent Construct
We use CFA to examine the extent to which indicators of structural racism reflect a latent construct. We systematically examine numerous specifications for measurement models for structural racism. Appendix Table D1 in the online version of the article reports the model fit statistics for the various model specifications related to correlated errors and dimensionality. The best fitting model (Model 3 in Appendix Table D1 in the online version of the article) permits the error terms for racialized poverty, home ownership, college graduation, and unemployment to all be intercorrelated to capture common economic factors; we permit the error terms for racialized voting and political representation to be correlated to capture common political factors; we permit the error terms for racialized disenfranchisement and incarceration to be correlated to capture common criminal-legal factors; and error terms for segregation and racialized college graduation and voting rates, respectively, are permitted to be correlated due to their observed relationships. These correlated errors are all intended to address common sources of variation that are independent of the effect of structural racism on the various indicators. Collectively, the various fit statistics show that the data fit the latent variable model well, as indicated by a nonsignificant chi-square, a negative BIC, a .959 CFI, a .926 TLI, and a .076 RMSEA.
Figure 2 (Panel B) is a diagram of our measurement model (Appendix Table D1, Model 3, in the online version of the article) with factor loadings and correlated errors. The estimates of the unstandardized loadings indicate that the latent variable has relationships in the expected directions with all of the indicators. Furthermore, the latent structural racism scale is strong in terms of reliability, as indicated by the high omega total reliability score of .89 (values above .70 indicate acceptable reliability). In contrast with Cronbach’s alpha, the omega total reliability measure reflects patterns accounted for in the model, such as varying factor loadings and correlated errors (McNeish 2018). The latent structural racism scale’s high reliability score (much higher than the individual item reliabilities) provides evidence of considerable shared variance among indicators of structural racism and supports the use of a latent measure rather than the more error-prone individual observed indicators (McNeish 2018). All considered, a measurement model that specifies a single dimension for structural racism and allows for other common sources of variance in the indicators that are largely conceptually motivated has a good fit with the data and generates reasonable parameter estimates.
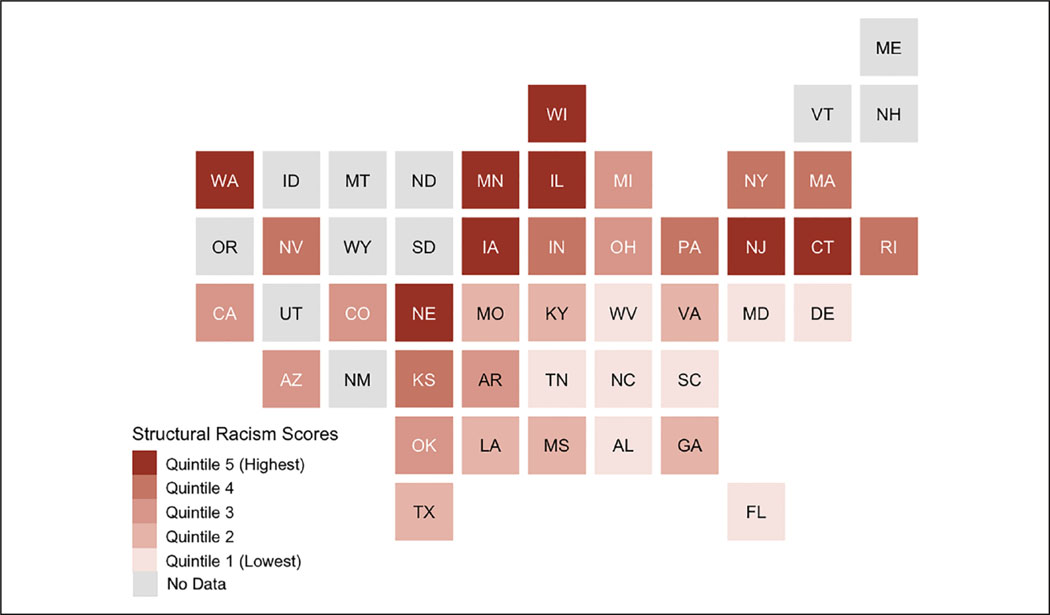
We map structural racism across U.S. states to understand the spatial distribution of racial subordination and exclusion. Figure 3 shows quintiles of the state-level latent structural racism measure. Results reveal that although structural racism is pervasive across the country, there is considerable variation in structural racism across states. Structural racism scores, as measured by the latent scale reflecting discriminatory institutional contexts, are especially severe in Midwestern and Northeastern states, consistent with prior research (Homan et al. 2021; Lichter et al. 2015; Massey and Denton 1993; Mesic et al. 2018; Muller and Wildeman 2016). In the discussion section, we contextualize the broader geography of racism, including aspects of structural racism that are not captured in the latent scale (see also Appendix E, in the online version of the article, for maps of each of the indicators of racism within institutions).
Figure 3.
Structural Racism Latent Scale Scores across U.S. States.
Note: The structural racism latent scale captures state-level structural racial inequality across economic, educational, political, criminal-legal, and segregation domains. Details on the operationalization of the scale are included in the text and Figure 2.
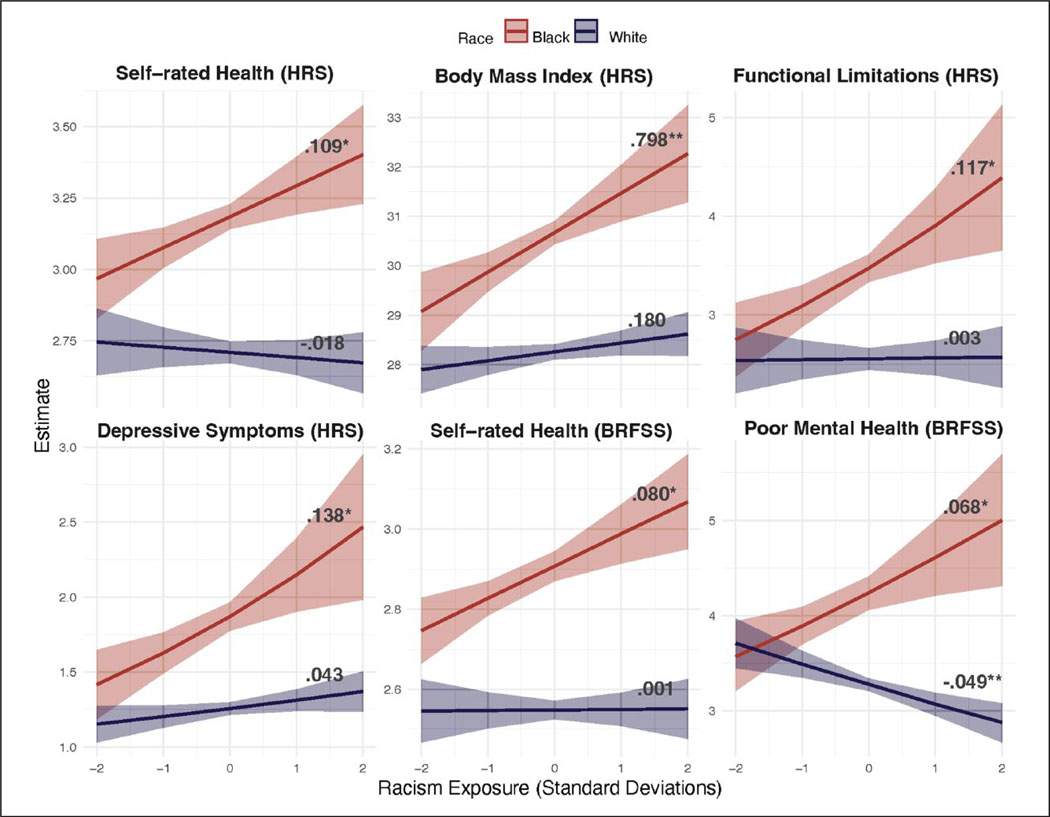
Quantifying the Impact of Structural Racism on Health
Figure 4 presents predicted values of health measures given exposure to state-level structural racism; these are based on multilevel multivariate regression estimates for the associations between the latent measure of structural racism and health measures for Black and White adults (regression estimates based on HRS and BRFSS data are presented in full in Appendix Tables C1 and C2, respectively, in the online version of the article). All regression estimates are net of demographics and state-level covariates (unemployment rate, income inequality, percentage Black population, and region). Greater structural racism scores are associated with worse health among Black people but not White people—a pattern that holds for each of the health outcomes. in the following, we detail estimates of the impact of structural racism for each of the health outcomes by race.
Figure 4.
Relationship between Structural Racism and Health.
Note: Based on estimates from multilevel regression models in Appendix Tables C1 and C2 in the online version of the article. Asterisks indicate slope is significantly different from zero. Scales of y-axes differ across health measures. HRS = Health and Retirement Study; BRFSS = Behavioral Risk Factor Surveillance System.
*p < .05. **p < .01.
Self-rated health (HRS).
Estimates from Figure 4 (and Appendix Table C1 in the online version of the article) show that a 1 SD increase in the state-level structural racism scale is associated with Black people in the HRS having .109 higher (worse) self-rated health (p < .05). Among Black people, going from −2 SD to 2 SD of exposure to structural racism is associated with .436 higher (worse) self-rated health. Notably, White people’s self-rated health is not associated with structural racism.
BMI (HRS).
Whereas structural racism is not predictive of White people’s BMI, it is positively associated with Black people’s BMI (Table 2). Indeed, each additional standard deviation increase in structural racism is associated with Black people having .798 higher BMI (p < .01). This translates to a 3.192 BMI gap between Black people living in states with low (−2 SD) versus high (2 SD) structural racism (Figure 4).
Functional limitations (HRS).
A similar pattern is evident for functional limitations: Structural racism is predictive of more functional limitations for Black people but not White people in the HRS (Table 2). Specifically, among Black people, a 1 SD increase in the state-level structural racism scale is associated with .117 more functional limitations (p < .05), and going from −2 SD to 2 SD of exposure to structural racism is associated with having .468 more functional limitations (Figure 4).
Depressive symptomology (HRS).
Consistent with other findings, structural racism is not predictive of White people’s depressive symptoms, although it is associated with worse depressive symptomology among Black people. For example, each additional standard deviation increase in structural racism is associated with Black people having .138 more depressive symptoms (p < .05). Figure 4 shows that is equivalent to a .552 gap in depressive symptoms for Black people residing in states with low (−2 SD) versus high (2 SD) structural racism.
Self-rated health (BRFSS).
Consistent with results based on the HRS sample, we find that structural racism is harmful for the self-rated health of Black people in the BRFSS (Figure 4; Appendix Table C2 in the online version of the article). Each additional standard deviation increase in structural racism is associated with Black people having .080 higher (worse) self-rated health (p < .05). This translates to a .320 gap in self-rated health between Black people living in states with low (−2 SD) versus high (2 SD) structural racism (Figure 4). Structural racism is not predictive of White people’s self-rated health.
Poor mental health days (BRFSS).
Results from Figure 4 show that structural racism is predictive of worse mental health for Black people. A 1 SD increase in the state-level structural racism scale is associated with .068 more poor mental health days (p < .05), and going from −2 SD to 2 SD of exposure to structural racism is associated with having .272 more poor mental health days. Interestingly, a 1 SD increase in structural racism is associated with .049 fewer poor mental health days for White people (p < .01). This translates to .196 fewer poor mental health days among White people living in states with high (2 SD) versus low (−2 SD) structural racism (Figure 4).
DISCUSSION
A growing body of theoretically oriented research points to the importance of structural racism as an upstream driver of health inequalities (Krieger 2014; Michener and Ford 2023; Phelan and Link 2015). Yet relatively few quantitative studies on the links between race and health have focused on the role of structural racism (Bailey et al. 2017). Moreover, quantitative studies on the topic have often been limited in several respects (e.g., ignoring the collective impact of structural racism across societal domains, inattention to structural racism at the state level, and failing to examine structural racism’s broad-based health consequences). This study makes several contributions to the literature, including (1) distilling central tenets of theories of structural racism to guide measurement strategies, (2) proposing the conceptualization of U.S. states as racializing institutional actors shaping population health, (3) developing a novel latent measure of state-level structural racism across societal domains, (4) examining an array of health measures (in two datasets) to provide a more comprehensive and rigorous investigation of the relationship between state-level structural racism and health, and (5) making our measure of structural racism publicly available to catalyze additional research on its etiology and consequences.
Findings also show that exposure to higher levels of structural racism is associated with worse health for Black people—but not their White counterparts. Overall, results are remarkably consistent across health outcomes. Indeed, structural racism has deleterious consequences among Black people for each of the commonly used measures of measures of population health—self-rated health, BMI, functional limitations, depressive symptomology, poor mental health days. Moreover, the magnitude of the impact of structural racism on their health is substantial. By contrast, the structural racism scale is largely unrelated to the health of White people (as measured by self-rated health, BMI, functional limitations, and depressive symptomology), although it is predictive of fewer poor mental health days among White people. In the following, we detail potential explanations for these findings, theoretical and methodological contributions of the study, and directions for future research.
Theoretical and Methodological Contributions
This study advances the literature theoretically and methodologically in several ways. First, whereas there has often been a disconnect in the literature between the conceptualization and measurement of structural racism, we build on prior theoretical innovations by distilling central tenets of theories of structural racism and concretizing them in a way that improves our ability to measure structural racism and its relationship with health. Standing on the shoulders of giants, we synthesize key theoretical insights in the literature (Bonilla-Silva 1997; Carmichael and Hamilton 1967; Lee 2024; Mills 1997; Powell 2008; Ray 2019; Reskin 2012) with the aim of advancing the field by conceptualizing structural racism as a multifaceted, interconnected, and institutionalized system of relational subordination for people of color and superordination for White people that is observable as manifest, concrete racial inequalities in life chances. This conceptualization enhances our ability to pin down a slippery concept and informs our approach to measuring state-level structural racism across multiple societal domains, allowing us to better quantify its effects. Thus, this study contributes to the literature by developing a conceptual framework and a theoretically informed analytical tool to understand the health consequences of structural racism.
Second, this study advances the field by developing a novel latent measure of structural racism in U.S. states, which enables us to gain empirical traction on this elusive concept. Prior efforts to quantify structural racism and its effects have been hindered by solely exploring the impacts of (error-prone) individual indicators of institutional racism separately—an approach that likely yields biased estimates and an incomplete picture of structural racism and its effects on health (Adkins-Jackson et al. 2021; Brown et al. 2022; Reskin 2012). By contrast, this study assesses how multiple institutional manifestations of racism across societal domains are interrelated and jointly reflect a broad structural racism construct. Findings from CFA provide strong evidence of an underlying latent construct of structural racism. Collectively, structural inequities across domains reflect systematic racialization of power, opportunities, resources, and risks. Although a handful of studies have begun to explore latent measures of structural racism at the public use microdata area, county, and city levels (e.g., Chantarat, Van Riper, and Hardeman 2021; Dougherty et al. 2020; Siegel et al. 2022), this study is among the first to develop a latent measure of state-level structural racism (see also Brown et al. 2022). Consistent with theories of structural racism that emphasize the importance of examining the forest rather than the trees (Mills 1997; Powell 2008; Reskin 2012), our findings point to the utility of using a more comprehensive approach to measuring structural racism across multiple domains that characterize the U.S. racialized social stratification system. Moving forward, it may also be useful to use latent class analysis to examine different typologies of structural racism (Chantarat et al. 2021) and agent-based and system dynamics modeling to better understand the inner workings of the structural racism system (e.g., distinct roles of various components and their interdependence, feedback loops, causal mechanisms, and latency).
Third, results illustrate how population health is a mirror that reflects macro-level societal arrangements, in general, and the toxic nature of structural racism, in particular. By empirically measuring the impact of structural racism on Black Americans’ health, we find evidence to support a central proposition by race theorists that structural forms of racism, despite often being covert and opaque, are nonetheless harmful (e.g., Bonilla-Silva 1997; Carmichael and Hamilton 1967; Du Bois 1899; Phelan and Link 2015). Because structural racism, which operates beyond the individual level and is often not directly observed by individuals, has deleterious effects on Black people’s health, theories that focus solely on individual-level, perceived discrimination are inadequate for understanding how structural forms of racism affect health. Rather, our findings underscore the utility of theoretical perspectives that highlight the roles of “upstream” drivers of population health, such as ecosocial theory (Krieger 2014), which posits that population health is shaped by macro-level discriminatory environments. Our study adds to the growing evidence that structural inequalities harm the health of oppressed groups by documenting the health consequences of structural racism among Black people.
Our study also contributes additional evidence to the debate over how structural inequalities shape the health of dominant groups. Whereas conflict theory and race stratification perspectives would predict that White people reap health advantages from higher levels of structural racism (Carmichael and Hamilton 1967; Du Bois 1899), “universal harm” hypotheses would predict that structural racism negatively impacts societal cohesion, cooperation, productivity, and safety, thereby harming the health of both Black and White people (McGee 2021; Metzl 2019). Results from this study showing that exposure to greater degrees of structural racism is predictive of fewer poor mental health days among White people are in line with a zero-sum, conflict hypothesis. On the other hand, our findings that state-level variation in structural racism is not associated with White people’s health for the other four outcomes considered (self-rated health, BMI, functional limitations, and depressive symptoms) is consistent with the notion that for White people, structural racism conveys both protective factors (e.g., greater relative status, power, resources, and opportunities) and detrimental ones (e.g., diminished social cohesion, productivity, safety, and investment in public goods, etc.), which offset each other.
Fourth, findings from this study support the notion that U.S. states are racializing institutional actors that shape population health. There is a long history of states playing a central role in shaping the well-being of Black people dating back to the eras of chattel slavery and Jim Crow (Bruch et al. 2019; Feagin and Bennefield 2014; Reece 2022), and our findings suggest that states continue to operate as an apparatus of a racialized social stratification system. Specifically, our findings indicate that states—which operate as political, social, legal, and administrative units and vary in their type and degree of structural racism—function as institutional actors contributing to the unequal distribution of health outcomes. This parallels a growing body of research showing that policies, socioeconomic inequality, and structural sexism at the state level lead to educational and gendered health inequalities (Homan 2019; Montez and Grumbach 2023; Montez, Zajacova, and Hayward 2017). However, prior empirical research on racial stratification and health has largely overlooked the role of states (for exceptions, see Lukachko et al. 2014; Wallace et al. 2017). Instead, the vast majority of studies on race and health have focused on individual-level factors (Hing et al. forthcoming). Among those that have examined contextual factors, the focus has typically been on meso-level environments such as neighborhoods and counties (Riley 2018). Although these are influential social determinants of health, ecosocial theory points to the importance of examining the impact of discriminatory environments across a range of spatial scales, including at the state level (Krieger 2014). Thus, our findings contribute to the literature by demonstrating the importance of studying exposure to state-level structural racism.
Fifth, we make our measure of structural racism publicly available (for the data and codebook, see Appendix F in the online version of the article). Our aim is to lower barriers to research on the health, social, political, and economic costs of structural racism. This resource will serve as an analytical tool and catalyst for future research on the causes and consequences of inequitable exposure to structural racism.
Limitations and Future Directions
It is important to note several limitations of this study as well as promising avenues for future research. First, due to the observational and cross-sectional nature of the data, we cannot confirm a causal relationship between state-level structural racism and health. However, it is worth noting that we find that the structural racism–health relationship among Black adults is robust after accounting for potential state-level confounding factors (e.g., income inequality, poverty, racial composition, and region) and that this is consistent with results from a nascent but growing body of empirical studies (Brown et al. 2022; Lukachko et al. 2014; Wallace et al. 2017). Moreover, there are strong theoretical reasons (discussed previously) to expect that contemporary structural racism negatively affects the health of Black people (Garcia et al. 2021; Gee and Ford 2011; Krieger 2014; Phelan and Link 2015; Reskin 2012; Sewell 2016). Thus, although we do not have definitive proof of causality, we view our findings as strongly suggestive that Black people’s health is harmed by structural racism. Further research is needed using longitudinal data and methods that attempt to address causality more thoroughly (Brown and Homan 2023; Graetz, Boen, and Esposito 2022). Longitudinal data are also essential for future life course analyses examining how timing, duration, and cumulative exposure to structural racism impact health and the extent to which the experiences and effects of structural racism are shaped by age, period, and cohort.
Second, this study does not establish the specific mechanisms linking structural racism to health. Although this topic is beyond the scope of this study, ecosocial theory and other theoretical research highlight an array of pathways through which structural racism is likely to affect health, including (but not limited to) access to material and psychosocial resources (e.g., social and economic capital, freedom, autonomy, power, and prestige) and exposure to risks (e.g., social stressors, toxic living conditions, low control, stigma, and relative deprivation; Krieger 2014; Phelan and Link 2015). Life course perspectives illustrate how structural racism sequelae proliferate and compound each other, leading to a racialized accumulation of disadvantages and accelerated aging processes (Boen et al. 2023; Brown et al. 2023; Garcia et al. 2021). Future research should investigate the pathways through which structural racism “gets under the skin” and the extent to which they are similar or different for various health measures. This is an area where qualitative and community-based participatory research approaches are particularly valuable because of their ability to shed light on the lived experiences of people most affected by racism and to illuminate pathways of influence and strategies for mitigating the pernicious effects of structural racism (Hardeman et al. 2022).
Third, although our latent scale of state-level structural racism is among the most comprehensive to date—including nine indicators of racism across five domains that prior theoretical and empirical research suggests are important (e.g., Brown et al. 2022)—it is far from exhaustive. Theory, growing evidence, and logic suggest that there is unlikely to be a universal or single best operationalization of structural racism (Adkins-Jackson et al. 2021; Groos et al. 2018). Approaches to measuring and modeling structural racism ought to vary according to study research questions, historical contexts, spatiotemporal scales, populations being studied, outcomes examined, data availability, and model fit (Brown and Homan 2023).
In addition to the types of racism examined in this study, it is also important to investigate the health consequences of other place-based forms of racism (and their intersections), including those that are embedded in historical and contemporary laws, policies, practices, and cultures (Agénor et al. 2021; Hicken et al. 2021; Michaels et al. 2023; Michener and Ford 2023). Studies have documented state- and county-level differences in historical typologies and forms of racism, such as slavery, lynchings, and Jim Crow (Kramer et al. 2017; O’Connell 2012; Reece 2022; Ruef 2014), reflecting historical racial regimes (Baker 2022). Similarly, given that modern white supremacy is dynamic, flexible, and adaptive to spatial contexts, there are likely distinct contemporary racialized regimes, characterized by different manifestations and modalities of racism across place. Indeed, whereas contemporary discriminatory legal and cultural forms of racism are especially pronounced in states in Southern and Appalachian regions (Chae et al. 2018; Smith, Kreitzer, and Suo 2020), findings from this study illustrate how contemporary structural racism—manifest in discriminatory institutional contexts—is particularly severe in states in Midwestern and Northeastern regions (see also, Brown et al. 2022; Mesic et al. 2018). Although the historical and modern roots of place-based differences in structural racism are not fully understood, scholars have posited that the extreme degrees of contemporary structural racism reflected by racial inequality in institutional contexts in many Northern states stem, in part, from institutionalized policies and practices of social control through racialized exclusion and subordination (e.g., resource hoarding, redlining, racial covenants, and discriminatory policing)—white-supremacist tactics that were increasingly deployed after the Great Migration because White people in the North perceived the increasing Black population as a threat (Blalock 1967; Carmichael and Hamilton 1967; Massey and Denton 1993; Muller and Wildeman 2016; Siegel et al. 2022). Given the fluid, shape-shifting nature of structural racism, it is important for future research to investigate the etiology and consequences of distinct contemporary racialized regimes across time and place. Moreover, because structural racism is a multilevel phenomenon, there is also a need for a better understanding of how forms of structural racism across different levels (e.g., nation, region, state, county, city, and neighborhood) are interrelated and jointly shape population health (Riley 2018).
Finally, although this study focuses on the health consequences of anti-Black structural racism for Black and White people, further research is needed on how additional forms of structural racism that are particularly salient for other racial and ethnic groups (e.g., American Indians, Alaskan Natives, Asians, and Latinx/e) impact their health. In doing so, it is important that future studies take a comprehensive approach to capturing the diverse historical and lived experiences of these understudied groups (Hardeman et al. 2022). Relatedly, future research should investigate the intersecting effects of structural racism, sexism, and other forms of contextual inequality and whether the impact of structural inequalities is contingent on social factors such as skin tone, class, and gender (Homan et al. 2021).7
CONCLUSION
Overall, this study provides a broad and rigorous investigation of the relationship between structural racism and health, highlighting the utility of macro-level structural approaches to better understand and address the unequal distribution of population health. Our finding that the health of Black Americans is undermined by an interinstitutional system of structural racism suggests that incremental, piecemeal health equity policies that focus on a single domain are unlikely to fundamentally alter the distribution of health (see also Gee and Hicken 2021; Hardeman et al. 2022; Phelan and Link 2015; Reskin 2012). Rather, effective approaches for addressing structural oppression and its insidious effects should account for its multifaceted, interconnected, and systemic nature (Brown and Homan 2023). Thus, bold actions to reduce structural racism across numerous societal domains and institutions—including policy bundles (or linked policy systems)—are likely necessary to substantially improve the health of Black Americans.
Supplementary Material
FUNDING
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research received support from two National Institute on Aging grants: P30 AG034424 (awarded to the Center for Population Health and Aging at Duke University) and 2R24AG045061-06 (awarded to the Network on Life Course Health Dynamics and Disparities in 21st Century America).
Biographies
Tyson H. Brown is an associate professor of sociology and medicine at Duke University, where he holds the W.L.F. endowed chair and directs the Center on Health & Society. He earned his PhD in sociology from the University of North Carolina, Chapel Hill. As a race scholar and medical sociologist, Dr. Brown’s research focuses on the scientific study of racism and its effects on health. His current projects aim to enhance theory-grounded conceptualization, measurement, and modeling of structural racism. Brown has authored numerous articles in leading journals in the fields of sociology, demography, and health policy, and his research contributions have been recognized with awards from the American Sociological Association and through keynote addresses and research invitations from the National Academies. Furthermore, he was the inaugural Duke Presidential Fellow, the recipient of Duke University’s Thomas Langford Award, and a resident fellow at Oxford University. In addition, Brown enjoys mentoring students and early career scientists to help build the pipeline of future scholars.
Patricia (Trish) Homan is an associate professor of sociology and the associate director of the Public Health Program at Florida State University. She is also an associate of Florida State University’s Pepper Institute on Aging and Public Policy and the Center for Demography and Population Health. Her research focuses on developing theory and measurement for structural sexism, structural racism, and other forms of structural oppression and examining how these forces shape health. Her work has been published in American Sociological Review, Demography, American Journal of Public Health, The Milbank Quarterly, Health Affairs, Social Forces, Social Science & Medicine, Journal of Health and Social Behavior, The Gerontologist, and The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, among other outlets. Her research has won multiple national awards, including the 2022 National Institutes of Health Matilda White Riley Early Stage Investigator Award, the 2022 Early Career Gender Scholar Award from Sociologists for Women in Society South, the 2021 American Sociological Association (ASA) Sex & Gender Section Distinguished Article Award, and the 2019 Roberta G. Simmons Outstanding Dissertation Award from the ASA Medical Sociology Section. Dr. Homan earned her PhD in sociology from Duke University before joining Florida State University in 2018.
Footnotes
These tenets do not capture all relevant aspects of structural racism for studying racialized health inequities. For example, Lee (2024) highlights additional features of structural racism, including (a) ubiquity and adaptiveness, (b) network configuration, (c) devaluation of human worth, (d) historical amnesia, and (e) perceived rationality and neutrality. For additional examples of relevant theoretical tenets, see Brown (2003) and Lantz (2021).
Although we have employed a relatively broad measure of structural racism, it should be noted that our measure does not include all forms of racism that influence health. Apart from the institutional features of structural racism that we examine, population health is also influenced by historical and contemporary discriminatory policies and practices and white supremacist ideologies and cultures (Agénor et al. 2021; Hicken et al. 2021; Michaels et al. 2023).
Because institutionalized adults were excluded, the study sample may be healthier than the overall population.
Item-level missingness was minimal, with only .03% missing on one or more variables. Listwise deletion was appropriate because such an extremely small amount of missing was unlikely to bias the analysis, and the sample sizes were large enough that the reduction in statistical power was unproblematic.
Data tabulated by Domenico Parisi at the National Strategic Planning and Analysis Research Center.
Prior research has shown that the American South is distinct in terms of racialized social conditions and population health (Baker and O’Connell 2022; Reece 2022; Ruef 2014). We used a binary indicator (South/non-South) for the sake of parsimony and because sensitivity analyses showed that respondents from non-Southern regions had similar health profiles (results available on request).
Our sensitivity analyses did not yield evidence of systematic gender or class differences in the relationship between state-level structural racism and health.
SUPPLEMENTAL MATERIAL
Appendices A to F are available in the online version of the article.
REFERENCES
- Adkins-Jackson Paris B., Chantarat Tongtan, Bailey Zinzi D., and Ponce Ninez A.. 2021. “Measuring Structural Racism: A Guide for Epidemiologists and Other Health Researchers.” American Journal of Epidemiology 191(4):539–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agénor Madina, Perkins Carly, Stamoulis Catherine, Hall Rahsaan H., Samnaliev Mihail, Berland Stephani, and Austin S. Bryn. 2021. “Developing a Database of Structural Racism-Related State Laws for Health Equity Research and Practice in the United States.” Public Health Reports 136(4):428–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander Michelle. 2011. The New Jim Crow: Mass Incarceration in the Age of Colorblindness. New York, NY: The New Press. [Google Scholar]
- Aneshensel Carol S. 2005. “Research in Mental Health: Social Etiology versus Social Consequences.” Journal of Health and Social Behavior 46(3):221–28. [DOI] [PubMed] [Google Scholar]
- Bailey Zinzi D., Krieger Nancy, Madina Agénor Jasmine Graves, Linos Natalia, and Bassett Mary T.. 2017. “Structural Racism and Health Inequities in the U.S.A.: Evidence and Interventions.” The Lancet 389(10077):1453–63. [DOI] [PubMed] [Google Scholar]
- Baker Regina S. 2022. “The Historical Racial Regime and Racial Inequality in Poverty in the American South.” American Journal of Sociology 127(6):1721–81. [Google Scholar]
- Baker Regina S., and O’Connell Heather A.. 2022. “Structural Racism, Family Structure, and Black-White Inequality in Poverty: The Differential Impact of the Legacy of Slavery among Single Mother and Married Parent Households.” Journal of Marriage and Family 84(5):1341–65. [Google Scholar]
- Blalock Hubert M. 1967. Toward a Theory of Minority-Group Relations. New York, NY: Wiley. [Google Scholar]
- Boen Courtney, Yang Y. Claire, Aiello Allison E., Dennis Alexis C., Harris Kathleen Mullan, Kwon Dayoon, and Belsky Daniel. 2023. “Patterns and Life Course Determinants of Black–White Disparities in Biological Age Acceleration: A Decomposition Analysis.” Demography 60(6):1815–41. doi: 10.1215/00703370-11057546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen Kenneth A. 1989. Structural Equations with Latent Variables. New York, NY: John Wiley & Sons. [Google Scholar]
- Bonilla-Silva Eduardo. 1997. “Rethinking Racism: Toward a Structural Interpretation.” American Sociological Review 62(3):465–80. [Google Scholar]
- Boyd Rhea W., Lindo Edwin G., Weeks Lachelle D., and McLemore Monica R.. 2020. “On Racism: A New Standard for Publishing on Racial Health Inequities.” Health Affairs Forefront. https://www.healthaffairs.org/content/forefront/racism-new-standard-publishing-racial-health-inequities. [Google Scholar]
- Brown Tony N. 2003. “Critical Race Theory Speaks to the Sociology of Mental Health: Mental Health Problems Produced by Racial Stratification.” Journal of Health and Social Behavior 44(3):292–301. [PubMed] [Google Scholar]
- Brown Tyson H., Hargrove Taylor W., Homan Patricia A., and Adkins Daniel E.. 2023. “Racialized Health Inequities: Quantifying Socioeconomic and Stress Pathways Using Moderated Mediation.” Demography 60(3):675–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown Tyson H., and Homan Patricia. 2023. “The Future of Social Determinants of Health: Looking Upstream to Structural Drivers.” The Milbank Quarterly 101(S1):36–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown Tyson H., Kamis Christina, and Homan Patricia. 2022. “Empirical Evidence on Structural Racism as a Driver of Racial Inequalities in COVID-19 Mortality.” Frontiers in Public Health 10:1007053. doi: 10.3389/fpubh.2022.1007053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruch Sarah K., Rosenthal Aaron, and Soss Joe. 2019. “Unequal Positions: A Relational Approach to Racial Inequality Trends in the U.S. States, 1940–2010.” Social Science History 43(1):159–84. [Google Scholar]
- Carmichael Stokely, and Hamilton Charles V.. 1967. Black Power: The Politics of Liberation. New York, NY: Vintage Books. [Google Scholar]
- Centers for Disease Control and Prevention. 2010. Behavioral Risk Factor Surveillance System Survey Data. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. [Google Scholar]
- Chae David H., Clouston Sean, Martz Connor D., Hatzenbuehler Mark L., Cooper Hannah L. F., Turpin Rodman, Stephens-Davidowitz Seth, and Kramer Michael R.. 2018. “Area Racism and Birth Outcomes among Blacks in the United States.” Social Science and Medicine 199:49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chantarat Tongtan, Van Riper David, and Hardeman Rachel. 2021. “The Intricacy of Structural Racism Measurement: A Pilot Development of a Latent-Class Multidimensional Measure.” EClinicalMedicine 40:101092. doi: 10.1016/j.eclinm.2021.101092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darity William A., and Mullen Kristen. 2020. From Here to Equality: Reparations for Black Americans in the Twenty-First Century. Chapel Hill: University of North Carolina Press. [Google Scholar]
- Dean Lorraine T., and Thorpe Roland J.. 2022. “What Structural Racism Is (or Is Not) and How to Measure It: Clarity for Public Health and Medical Researchers.” American Journal of Epidemiology 191(9):1521–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty Geoff B., Golden Sherita H., Gross Alden L., Colantuoni Elizabeth, and Dean Lorraine T.. 2020. “Measuring Structural Racism and Its Association with BMI.” American Journal of Preventive Medicine 59(4):530–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Bois WEB 1899. The Philadelphia Negro: A Social Study. Philadelphia: University of Pennsylvania. [Google Scholar]
- Feagin Joe, and Bennefield Zinobia. 2014. “Systemic Racism and U.S. Health Care.” Social Science & Medicine 103:7–14. [DOI] [PubMed] [Google Scholar]
- Flood Sarah, King Miriam, Rodgers Renae, Ruggles Steven, Warren J. Robert, Backman Daniel, Chen Annie, et al. 2023. IPUMS CPS: Version 11.0 [dataset]. Minneapolis, MN: IPUMS. doi: 10.18128/D030.V11.0. [DOI] [Google Scholar]
- Garcia Marc A., Homan Patricia A., García Catherine, and Brown Tyson H.. 2021. “The Color of COVID-19: Structural Racism and the Pandemic’s Disproportionate Impact on Older Blacks and Latinos.” Journal of Gerontology, Series B: Psychological Sciences and Social Sciences 76(3):e75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee Gilbert C., and Ford Chandra L.. 2011. “Structural Racism and Health Inequities: Old Issues, New Directions.” Du Bois Review: Social Science Research on Race 8(1):115–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee Gilbert C., and Hicken Margaret T.. 2021. “Structural Racism: The Rules and Relations of Inequity.” Ethnicity and Disease 31(S1):293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graetz Nick, Boen Courtney, and Esposito Michael. 2022. “Racism and Causal Inference: Identifying the Life Course Determinants of Racial Disparities in Adult Health.” Journal of Health and Social Behavior 63(2):232–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groos Maya, Wallace Maeve, Hardeman Rachel, and Theall Katherine P.. 2018. “Measuring Inequity: A Systematic Review of Methods Used to Quantify Structural Racism.” Journal of Health Disparities Research and Practice 11(2):190–206. [Google Scholar]
- Hardeman Rachel, Homan Patricia, Chantarat Tongtan, Davis Brigette, and Brown Tyson. 2022. “We Can’t Change What We Don’t Measure: Improving Measurement of Structural Racism for Antiracist Health Policy Research.” Health Affairs 41(2):179–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health and Retirement Study. 2010. Core Dataset. Ann Arbor: University of Michigan; [producer and distributor]. [Google Scholar]
- Hicken Margaret T., Miles Lewis, Haile Salome, and Esposito Michael. 2021. “Linking History to Contemporary State-Sanctioned Slow Violence through Cultural and Structural Racism.” Annals of the American Academy of Political and Social Science 694(1):48–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hing Anna K., Chantarat Tongtan, Fashaw-Walters Shekinah, Hunt SL, and Hardeman Rachel R.. Forthcoming. “Instruments for Racial Health Equity: A Scoping Review of Structural Racism Measurement, 2019–2021.” Epidemiologic Reviews. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homan Patricia. 2019. “Structural Sexism and Health in the United States: A New Perspective on Health Inequality and the Gender System.” American Sociological Review 84(3):486–516. [Google Scholar]
- Homan Patricia A., and Brown Tyson H.. 2022. “Sick and Tired of Being Excluded: Structural Racism in Disenfranchisement as a Threat to Population Health.” Health Affairs 41(2):219–27. [DOI] [PubMed] [Google Scholar]
- Homan Patricia A., Brown Tyson H., and King Brittany. 2021. “Structural Intersectionality as a New Direction for Health Disparities Research.” Journal of Health and Social Behavior 62(3):350–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korver-Glenn Elizabeth. 2021. Race Brokers: Housing Markets and Segregation in 21st Century Urban America. New York, NY: Oxford University Press. [Google Scholar]
- Kramer Michael R., Black Nyesha C., Matthews Stephen A., and James Sherman A.. 2017. “The Legacy of Slavery and Contemporary Declines in Heart Disease Mortality in the U.S. South.” SSM Population Health 3:609–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger Nancy. 2014. “Discrimination and Health Inequities.” International Journal of Health Services: Planning, Administration, Evaluation 44(4):643–710. [DOI] [PubMed] [Google Scholar]
- Krieger Nancy. 2020. “Measures of Racism, Sexism, Heterosexism, and Gender Binarism for Health Equity Research: From Structural Injustice to Embodied Harm—An Ecosocial Analysis.” Annual Review of Public Health 41:37–62. [DOI] [PubMed] [Google Scholar]
- Lantz Paula M. 2021. “The Tenets of Critical Race Theory Have a Long-Standing and Important Role in Population Health Science.” Milbank Quarterly Opinion. doi: 10.1599/mqop.2021.0714. [DOI] [Google Scholar]
- Lee Hedwig. 2024. “How Does Structural Racism Operate (in) the Contemporary U.S. Criminal Justice System?” Annual Review of Criminology 7(9):1–23. [Google Scholar]
- Lichter Daniel T., Parisi Domenico, and Taquino Michael C.. 2015. “America’s Segregated States.” Pp. 30–36 in Pathways: Poverty and Inequality Report 2015, edited by Grusky D, Varner C, and Mattingly M. Palo Alto, CA: Stanford Center on Poverty and Inequality. [Google Scholar]
- Lukachko Alicia, Hatzenbuehler Mark L., and Keyes Katherine M.. 2014. “Structural Racism and Myocardial Infarction in the United States.” Social Science & Medicine 103:42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manza Jeff, and Uggen Christopher. 2006. Locked out: Felon Disenfranchisement and American Democracy. New York, NY: Oxford University Press. [Google Scholar]
- McGhee Heather. 2021. The Sum of Us: What Racism Costs Everyone and How We Can Prosper Together. New York, NY: Random House. [Google Scholar]
- McNeish Daniel. 2018. “Thanks Coefficient Alpha, We’ll Take It from Here.” Psychological Methods 23(3):412–33. [DOI] [PubMed] [Google Scholar]
- Mesic Aldina, Franklin Lydia, Cansever Alev, Potter Fiona, Sharma Anika, Knopov Anita, and Siegel Michael. 2018. “The Relationship between Structural Racism and Black–White Disparities in Fatal Police Shootings at the State Level.” Journal of the National Medical Association 110(2):106–16. [DOI] [PubMed] [Google Scholar]
- Metzl Jonathan. 2019. Dying of Whiteness: How the Politics of Racial Resentment Is Killing America’s Heartland. New York, NY: Basic Books. [Google Scholar]
- Michaels Eli K., Tracy Lam-Hine Thu T. Nguyen, Gee Gilbert, and Allen Amani M.. 2023. “The Water Surrounding the Iceberg: Cultural Racism and Health Inequities.” Milbank Quarterly 101(3):768–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michener Jamila, and Ford Tiffany. 2023. “Racism and Health: Three Core Principles.” The Milbank Quarterly 101(S1):333–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills Charles W. 1997. The Racial Contract. Ithaca, NY: Cornell University Press. [Google Scholar]
- Montez Jennifer Karas, and Grumbach Jacob M.. 2023. “U.S. State Policy Contexts and Population Health.” The Milbank Quarterly 101(S1):196–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez Jennifer Karas, Hayward Mark D., and Zajacova Anna. 2019. “Educational Disparities in Adult Health: U.S. States as Institutional Actors on the Association.” Socius 5. doi: 10.1177/2378023119835345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez Jennifer Karas, Zajacova Anna, and Hayward Mark D.. 2017. “Disparities in Disability by Educational Attainment across U.S. States.” American Journal of Public Health 107(7):1101–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller Jennifer C. 2020. “Racial Ideology or Racial Ignorance? An Alternative Theory of Racial Cognition.” Sociological Theory 38(2):142–69. [Google Scholar]
- Muller Chris, and Wildeman Chris. 2016. “Geographic Variation in the Cumulative Risk of Imprisonment and Parental Imprisonment in the United States.” Demography 53(5):1499–509. [DOI] [PubMed] [Google Scholar]
- National Conference of State Legislatures. 2019. “African-American Legislators 2009.” http://www.ncsl.org/research/about-state-legislatures/african-american-legislators-in-2009.aspx.
- O’Brien Rourke, Neman Tiffany, Seltzer Nathan, Evans Linnea, and Venkataramani Atheendar. 2020. “Structural Racism, Economic Opportunity and Racial Health Disparities: Evidence from U.S. Counties.” SSM Population Health 11:100564. doi: 10.1016/j.ssmph.2020.100564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connell Heather A. 2012. “The Impact of Slavery on Racial Inequality in Poverty in the Contemporary U.S. South.” Social Forces 90(3):713–34. [Google Scholar]
- Pabayo Roman, Ehntholt Amy, Davis Kia, Liu Sze Y., Muennig Peter, and Cook Daniel M.. 2019. “Structural Racism and Odds for Infant Mortality among Infants Born in the United States 2010.” Journal of Racial and Ethnic Health Disparities 6(6):1095–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan Jo C., and Link Bruce G.. 2015. “Is Racism a Fundamental Cause of Inequalities in Health?” Annual Review of Sociology 41:311–30. [Google Scholar]
- Powell John A. 2008. “Structural Racism: Building upon the Insights of John Calmore.” North Carolina Law Review 86:791–816. [Google Scholar]
- Ray Victor. 2019. “A Theory of Racialized Organizations.” American Sociological Review 84(1):26–53. [Google Scholar]
- Ray Victor. 2022. On Critical Race Theory: What It Is & Why It Matters. New York, NY: Penguin Random House [Google Scholar]
- Reece Robert L. 2022. “Slave Past, Modern Lives: An Analysis of the Legacy of Slavery and Contemporary Life Expectancy.” Journal of Black Studies 53(7):677–702. [Google Scholar]
- Reskin Barbara. 2012. “The Race Discrimination System.” Annual Review of Sociology 38:17–35. [Google Scholar]
- Riley Alicia R. 2018. “Neighborhood Disadvantage, Residential Segregation, and beyond—Lessons for Studying Structural Racism and Health.” Journal of Racial and Ethnic Health Disparities 5(2):357–65. [DOI] [PubMed] [Google Scholar]
- Roth Wendy D., van Stee Elena G., and Regla-Vargas Alejandra. 2023. “Conceptualizations of Race: Essentialism and Constructivism.” Annual Review of Sociology 49(1):39–58. [Google Scholar]
- Ruef Martin. 2014. Between Slavery and Capitalism: The Legacy of Emancipation in the American South. Princeton, NJ: Princeton University Press. [Google Scholar]
- Seamster Louise, and Ray Victor. 2018. “Against Teleology in the Study of Race and Ethnicity: Towards the Abolition of the Progress Paradigm.” Sociological Theory 36(4):315–42. [Google Scholar]
- Sewell Abigail A. 2016. “The Racism-Race Reification Process: A Mesolevel Political Economic Framework for Understanding Racial Health Disparities.” Sociology of Race and Ethnicity 2(4):402–32. [Google Scholar]
- Siegel Michael, Isabella Critchfield-Jain Mathew Boykin, and Owens Alicia. 2022. “Actual Racial-Ethnic Disparities in COVID-19 Mortality for the non-Hispanic Black Compared to non-Hispanic White Population in 35 U.S. States and Their Association with Structural Racism.” Journal of Racial Ethnic Health Disparities 9(5):1697–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith Candis, Kreitzer Rebecca, and Suo Feiya. 2020. “The Dynamics of Racial Resentment across the 50 US States.” Perspectives on Politics 18(2):527–38. [Google Scholar]
- Taylor Keeanga-Yamahtta. 2019. Race for Profit: How Banks and the Real Estate Industry Undermined Black Homeownership. Chapel Hill: University of North Carolina Press. [Google Scholar]
- Tyson Karolyn, and Lewis Amanda E.. 2021. “The Burden of Oppositional Culture among Black Youth in America.” Annual Review of Sociology 47(1):459–77. [Google Scholar]
- Uggen Christopher, Shannon Sarah, and Manza Jeff. 2012. “State-Level Estimates of Felon Disenfranchisement in the United States, 2010.” https://www.ojp.gov/ncjrs/virtual-library/abstracts/state-level-estimates-felon-disenfranchisement-united-states-2010.
- U.S. Census Bureau. (n.d.). “Voting and Registration.” https://data.census.gov/.
- Vera Institute of Justice. 2021. “Incarceration Trends Data.” https://github.com/vera-institute/incarceration-trends.
- Wallace Maeve, Joia Crear-Perry Lisa Richardson, Tarver Meshawn, and Theall Katherine. 2017. “Separate and Unequal: Structural Racism and Infant Mortality in the U.S.” Health & Place 45:140–44. [DOI] [PubMed] [Google Scholar]
- Wilkinson Richard, and Pickett Kate. 2011. The Spirit Level: Why Greater Equality Makes Societies Stronger. New York, NY: Bloomsbury Publishing. [Google Scholar]
- Williams Deadric T. 2023. “Racism and the Mechanisms Maintaining Racial Stratification in Black Families.” Journal of Family Theory & Review 15(2):206–18. [Google Scholar]
- Williams Deadric T., and Baker Regina S.. 2021. “Family Structure, Risks, and Racial Stratification in Poverty.” Social Problems 68(4):964–85. [Google Scholar]
- Williams David R., Lawrence Jourdyn, and Davis Brigette A.. 2019. “Racism and Health: Evidence and Needed Research.” Annual Review of Public Health 40:105–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.