Abstract
Purpose
Postoperative complications increase mortality, disability and costs. Advanced understanding of the risk factors for postoperative complications is needed to improve surgical outcomes. This paper discusses the rationale and profile of the BIGPROMISE (biomarkers to guide perioperative management and improve outcome in high-risk surgery) cohort, that aims to investigate risk factors, pathophysiology and outcomes related to postoperative complications.
Participants
Adult patients undergoing major surgery in two tertiary teaching hospitals. Clinical data and blood samples are collected before surgery, at the end of surgery and on the first, second and third postoperative day. At each time point a panel of cardiovascular, inflammatory, renal, haematological and metabolic biomarkers is assessed. Aliquots of plasma, serum and whole blood of each time point are frozen and stored. Data on severe complications are prospectively collected during 30 days after surgery. Functional status is assessed before surgery and after 120 days using the WHO Disability Assessment Schedule (WHODAS) 2.0. Mortality is followed up until 2 years after surgery.
Findings to date
The first patient was enrolled on 8 October 2021. Currently (1 January 2024) 3086 patients were screened for eligibility, of whom 1750 (57%) provided informed consent for study participation. Median age was 66 years (60; 73), 28% were female, and 68% of all patients were American Society of Anaesthesiologists (ASA) physical status class 3. Most common types of major surgery were cardiac (49%) and gastro-intestinal procedures (26%). The overall incidence of 30-day severe postoperative complications was 16%.
Future plans
By the end of the recruitment phase, expected in 2026, approximately 3000 patients with major surgery will have been enrolled. This cohort allows us to investigate the role of pathophysiological perioperative processes in the cause of postoperative complications, and to discover and develop new biomarkers to improve risk stratification for adverse postoperative outcomes.
Trial registration number
Keywords: cardiothoracic surgery, colorectal surgery, pancreatic surgery, vascular surgery, risk factors, adult surgery
STRENGTHS AND LIMITATIONS OF THIS STUDY.
A large prospective collection of perioperative blood samples and clinical data in a high-risk surgical population.
Postoperative complications and functional outcomes are defined according to international standards to facilitate research collaborations.
A perioperative biomarker panel is prospectively assessed on fresh blood samples to elucidate the role of pathophysiological processes in the cause of postoperative complications.
Multiple sample aliquots of plasma, serum and whole blood are frozen and stored in a central archive, allowing future perioperative biomarker discovery and development.
This study is limited to blood samples that are collected and stored until 72 hours after surgery.
Introduction
Worldwide, more than 330 million patients have surgery each year.1 Depending on type of surgery and coexisting diseases, 10%–30% of patients suffer severe postoperative complications.2–5 Common adverse events are infections (eg, pneumonia, surgical site infection), myocardial infarction, respiratory failure and acute kidney injury. Postoperative complications are important determinants of long-term mortality and poor health after surgery,6–8 impair quality of life and may increase hospital costs up to four times.9 10
Surgical trauma triggers a systemic stress response that involves a complex neuroendocrine and immunological reaction to local tissue injury. Local tissue trauma activates the innate immune system, with proinflammatory and anti-inflammatory cytokines triggering systemic inflammation and the hypothalamic–pituitary–adrenal (HPA) axis. This results in stimulation of the sympathetic nervous system, alongside several other hormonal pathways, to maintain physiological homeostasis.11 The effects of these pathways change perioperative organ perfusion, water balance and cellular metabolism. A postoperative dysregulated stress response can be detrimental as excessive systemic inflammation, immunosuppression, hypermetabolism and hypercoagulation can lead to organ failure and death.11 12 The most important determinant of a postoperative dysregulated stress response is the nature and extent of surgery. In addition, non-surgical factors such as ageing, coexisting diseases and deconditioning, are contributing factors (figure 1).13
Figure 1.
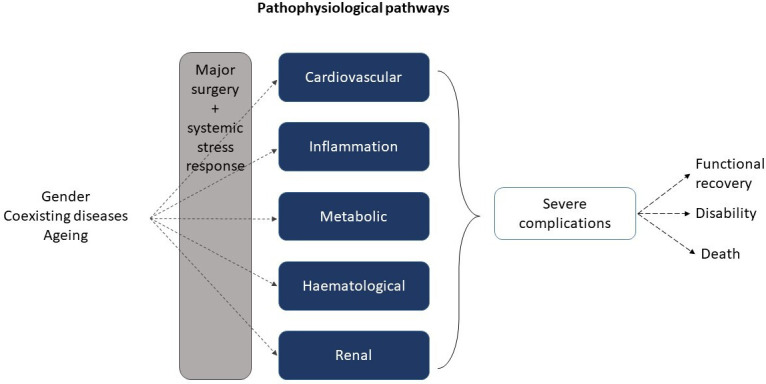
Potential perioperative pathways in the pathogenesis of postoperative complications.
In perioperative medicine, a biomarker is considered an indicator of a preoperative (patho)physiological process (eg, ageing, chronic disease), or response to surgery (eg, organ injury, inflammation). Numerous publications have raised awareness of the added value of biomarkers in perioperative medicine. However, heterogeneity in study design and methodological limitations have hindered implementation. First, many studies focused on the cardiovascular pathophysiology of postoperative complications, but used a wide range of clinical (non-standardised) outcomes. This complicates the interpretation of results, and makes the usefulness of perioperative biomarkers unclear.14 15 Second, researchers often use a single-marker approach (eg, cardiac troponin, interleukin-6 (IL-6)) to study perioperative risk and pathophysiology of complications.16 17 However, the complex aetiology of postoperative complications involves multiple pathophysiological processes, which are likely better reflected by a panel of multiple biomarkers.11 A concept that has not been well studied in perioperative medicine, yet.18 19 Third, in addition to risk stratification, and prognosis, the application of perioperative biomarkers covers early diagnosis of complications, and targeted interventions to improve postoperative outcomes, both of which have been incompletely studied. As a result, few biomarkers make it from bench to bedside, despite significant investment in perioperative biomarker research.20 21 The ‘biomarkers to guide perioperative management and improve outcome in high-risk surgery’ (BIGPROMISE) cohort will prospectively assess a wide range of perioperative biomarkers in fresh blood samples, and systematically collect and store plasma, serum and whole blood samples to allow for future biomarker discovery. This manuscript describes the rationale and design of the BIGPROMISE cohort, which primarily aims to facilitate biomarker research on risk factors, pathophysiology and outcomes related to standardised postoperative complications in patients undergoing major elective surgery.
Cohort description
The BIGPROMISE cohort prospectively studies patients undergoing elective major cardiac or non-cardiac surgery, and is an initiative of the departments of Anaesthesiology, Intensive Care and Pain Medicine of St. Antonius Hospital and Amphia Hospital in the Netherlands. The study protocol was filed at Clinicaltrials.gov under registration number NCT05199025, and received approval from the Medical research Ethics Committees United (NL74076.100.20). The current protocol version is 6.1 (21-06-2023) and available on request. The biobank samples are stored by a third-party biobank provider (Azenta, Griesheim, Germany).
Setting
Patients are recruited in two tertiary teaching hospitals (St. Antonius Hospital and Amphia Hospital, the Netherlands). Based on the historical surgical volumes of both facilities, approximately 2500–3000 patients are eligible for inclusion each year. BIGPROMISE biobank aims to collect clinical data and blood samples of at least 1000 patients per year. BIGPROMISE will be recruiting at least until 2025, and possibly longer depending on capacity and funding.
BIGPROMISE biobank is an investigator-initiated research collaboration between anaesthesiologists, intensivists and clinical chemists, in collaboration with surgeons, and Roche Diagnostics International (Penzberg, Germany), a large biotech company, and worldwide provider of in-vitro diagnostics.
Inclusion criteria and patient recruitment
Adult patients (>18 years) undergoing elective major surgery under general anaesthesia are eligible for participation. Surgical risk is an estimate of procedure-specific risk of 30-day mortality, without taking age, gender, frailty or coexisting diseases into account.22 23 The following types of major surgery are considered in our study: cardiac, vascular, gastrointestinal, hepatobiliary, urologic and pulmonary surgery. A full list of surgical procedures is provided in online supplemental appendix 1. Patients not providing written informed consent, patients not able to complete questionnaires in Dutch, patients who are pregnant, patients undergoing emergency surgery, and patients with a life expectancy less than 6 months are excluded from participation in this study.
bmjopen-2023-078307supp001.pdf (117.5KB, pdf)
Eligible patients scheduled for surgery are contacted by telephone by trained study personnel. Patients are informed about the purposes of the biobank and will receive an information letter by (e-)mail, if they consider to participate. Written informed consent is obtained at time of hospital admission by a member of the study team. This includes the collection of patient characteristics and clinical data, blood samples for biomarker analysis in fresh blood samples during hospital stay and a functional status questionnaire. Additionally, a written permission is separately obtained for collection, handling and storage of blood samples in a dedicated biobank for future biomarker discovery, permission to be contacted for further research.
Data collection
Prior to surgery, baseline data are collected regarding patient characteristics, medical history, chronic pain, previous laboratory results, frailty and functional status (online supplemental table 1). Preoperative study data are collected from electronic patient records, from dedicated questionnaires (12-item WHO Disability Assessment Schedule (WHODAS) 2.0 for functional status) and a numeric rating scale (NRS) for pain.24 25 Study data during hospital admission are variables related to surgery and anaesthesia, clinical course, laboratory results, complications and pain, which will be extracted from electronic patient records. After hospital discharge, postoperative complications will be registered until 30 days after surgery. Further outcome data consist of days alive and out of hospital after 120 days, patient-reported information on functional status and pain after 120 days, and mortality up to 2 years.
bmjopen-2023-078307supp004.pdf (91.1KB, pdf)
Study data are collected and managed using REDCap which is an electronic data capture tool. REDCap is a secure, web-based software platform and compliant with Good Clinical Practice guidelines.26 Postoperative pain scores, vital parameters (modified early warning scores) and the results of perioperative biomarker panels are extracted semiautomatically from electronic medical files (Epic Systems Corporation, United States; Metavision, iMD Soft, Israel), and the local laboratory information management systems (GLIMS, Clinisys GLIMS, Belgium, and MOLIS, CompuGroup, Belgium). Postoperative complications are noted and classified by a dedicated researcher (TCDR, MSYT), and validated by an experienced perioperative physician (PGN, TCDR), prior to manual registration in the database. Follow-up data for functional outcomes are registered using electronic and paper questionnaires (WHODAS 2.0). Long-term mortality is assessed using the Dutch municipality register of deceased persons to obtain date of death. Quality assurance of study data is annually performed by an independent monitor. Data records are coded, the key to the code is kept securely in each participating centre.
Blood sample collection and processing
Blood samples are collected at five perioperative time points: after induction of general anaesthesia (baseline), at the end of surgery and on the morning of the first, second and third postoperative day. Blood is collected from an arterial line (if applicable) or venepuncture into vacuum blood collecting tubes, according to the schedule presented in online supplemental table 2.
bmjopen-2023-078307supp005.pdf (15KB, pdf)
In all study patients, blood samples are centrifuged at 1800×g for 5 min and used to analyse a panel of 50 biomarkers at each perioperative time point (table 1, figure 2). Biomarker analyses are performed at the local hospital laboratory on Roche Cobas 8000 and Sysmex XN platforms. Results of perioperative biomarker analysis are captured in local laboratory information management systems and uploaded to a central web application for research data (REDCap).
Table 1.
Perioperative biomarkers and analyser systems
| Analyser system | Biomarkers |
| Sysmex XN | Haemoglobin, haematocrit, erythrocytes, mean corpuscular volume, mean corpuscular haemoglobin, red cell distribution width, mean platelet volume, mean corpuscular haemoglobin concentration, leucocytes, trombocytes, neutrophils, lymphocytes, monocytes, eosinophils, basophils, reticulocytes, reticulocyte haemoglobin equivalent, neutrophil-to-lymphocyte ratio. |
| Cobas 8000 | Albumin, aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, bilirubin, calcium, cholesterol, C reactive protein, chloride, creatinin kinase, cystatin C, ferritin, growth differentiation factor-15, gamma-glutamyl transferase, glucose, high-density lipoprotein, high-sensitive troponin T, insulin-like growth factor-1, creatinin, interleukin-6, iron, lactate dehydrogenase, low-density lipoprotein, magnesium, neutrophil gelatinase associated lipocalin, N-terminal pro B-type natriuretic peptide, pro-calcitonin, phosphate, potassium, sex hormone binding globulin, soluble fms-like tyrosine kinase-1, sodium, triglycerides, thyroid stimulating hormone, free thyroxine, 25 hydroxyvitamin D. |
Figure 2.
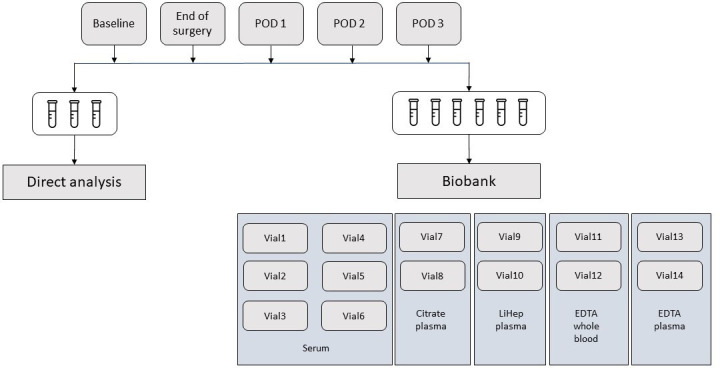
Perioperative collection, analysis and storage of blood samples.
In patients with written consent for biobanking, an additional 21 mL blood is processed for storage at −80°C as whole blood (3 mL), and serum and plasma after centrifugation at 2000 g for 10 min or 4000 g for 5 min (figure 2). Aliquots of plasma, serum and whole blood are frozen and stored within 6 hours after collection. Aliquots are stored in a dedicated biobank facility (Azenta, Griesheim, Germany).
Biomarker panel
The selection of biomarkers is based on the hypothesis that a postoperative dysregulated stress response, which we briefly explained in the Introduction section, is associated with postoperative complications, through systemic inflammation, immunosuppression, hypermetabolism, hypercoagulation and organ injury, and that serum biomarkers reflect (part of) these pathways or any downstream effect.11–13 Furthermore, we considered previous literature reports on the pathophysiology of postoperative complications, availability and reproducibility of biomarker assays, current practice and costs. For pragmatic reasons, biomarkers are categorised according to pathways involved in the pathogenesis of postoperative complications, as follows (figure 1):
Cardiovascular
Chronic cardiac diseases, such as coronary artery disease (CAD) and heart failure (HF), are key risk factors for postoperative complications. Common risk factors (eg, diabetes mellitus, renal insufficiency, peripheral artery disease) are strongly associated with undiagnosed cardiac disease. In these patients, biomarkers may improve preoperative cardiac risk assessment. Surgery leads to activation of the sympathetic nervous system, inflammation, hypercoagulable and catabolic states, which put patients at risk for postoperative myocardial infarction/injury (PMI). PMI is the most common CV complication and asymptomatic in the vast majority of surgical patients, but has been associated with myocardial dysfunction, respiratory and renal failure, mortality, and disability.27–30
Inflammation
Low-grade inflammation causes endothelial and organ dysfunction in chronic disease (eg, CAD, HF, renal insufficiency, diabetes mellitus) and puts patients at increased risk for PMI and renal dysfunction.17 31 32 Biomarkers reflecting these processes may identify patients with (subclinical) organ dysfunction. Surgery activates the innate immune system, and the production of proinflammatory and anti-inflammatory processes in the body. Although this is essential for healing, a postoperative dysregulated inflammatory response increases the risk of infectious complications by immune suppression, and organ dysfunction through endothelial injury.32 Biomarkers may aid physicians in discriminating between postoperative dysregulated inflammation and infection.
Metabolic
Preoperative deficiencies of nutrients or vitamins are risk factors for endothelial dysfunction, immune dysfunction and cardiovascular disease.33 34 Activation of the HPA axis and several other hormonal pathways change the production of cortisol, growth hormone, thyroid hormone and insulin. The negative effects are hypermetabolism and hypercatabolism, leading to hyperglycaemia, release of fatty acids and muscle wasting, which can be detrimental for postoperative recovery.11
Haematological
Anaemia is a risk factor for postoperative complications and disability, most likely trough tissue hypoxaemia, organ injury and poor functional capacity.35 36 In surgical patients, anaemia is often caused by (functional) iron deficiency, blood loss and inflammation. Besides erythropoiesis, iron deficiency also impairs oxidative metabolism and cellular immunity. The negative effects of poor iron metabolism are aggravated by increased hepcidin concentrations in response to a postoperative dysregulated inflammatory response, for instance due to blood loss after major surgery. Besides, systemic inflammation initiates bone marrow reprogramming and a decreased erythrocyte lifespan. This may explain why an abnormal iron status has been associated with postoperative complications, even without anaemia.37 A high red cell distribution width is a common marker of oxidative stress, chronic inflammation, cardiovascular disease, and is associated with adverse events after surgery.38
Renal
Chronic kidney disease-associated azotaemia, hypervolaemia and anaemia increase after surgery, and are considered to be major risks for postoperative complications. As a result of sympathetic nervous activation, vasoconstriction may decrease renal blood flow and glomerular filtration rate. The renin–angiotensin–aldosterone system is activated resulting in water and salt retention and further systemic vasoconstriction.11 Up to 20% of major surgery patients sustain acute kidney injury. Even when renal function returns to baseline at the time of hospital discharge, the risk for long-term mortality and disability remains increased.33
Outcome measures
Postoperative outcomes are registered after review of medical charts and diagnostic test results. Causes of outcome measures are classified according to international criteria (online supplemental appendix 2) as follows:
bmjopen-2023-078307supp002.pdf (355.3KB, pdf)
Respiratory failure, defined according to European Perioperative Clinical Outcome definitions, including ARDS, pleural effusion, pneumothorax, atelectasis, respiratory infection, aspiration pneumonitis, bronchospasm, cardiopulmonary oedema and pulmonary embolism. Postoperative hypoxaemia (ie, saturation <90% on room air, or oxygen therapy>5 L O2/min) will be registered as respiratory failure.
Major adverse cardiac events, defined in agreement with the Standardised Endpoints in Perioperative medicine (StEP) criteria for cardiovascular outcomes and the fourth universal definition of myocardial infarction, including cardiac death, non-fatal cardiac arrest, coronary revascularisation, myocardial infarction/injury, heart failure, pulmonary embolism, atrial fibrillation and stroke.
Infections, defined according to StEP criteria for infection and sepsis, including sepsis, pneumonia, empyema, surgical site infection, urinary system infection and blood stream infection. For all events, the probability of infection will be categorised using a four-point scale (none, possible, probable and definite infection).
Acute kidney injury, defined by the StEP criteria and classified as stage 1–3 based on postoperative serum creatinine concentrations or initiation of renal replacement therapy.
Bleeding, according to the standardised definitions from the Bleeding Academic Research Consortium for cardiac surgery. Postoperative bleeding after non-cardiac surgery is graded according to the modified Clavien-Dindo classification.
Postoperative pain, registered daily using the NRS. Scores range from 0 (no pain) to 10 (maximum pain). Chronic pain is defined as surgery related pain >3 months after surgery. The impact of chronic pain is assessed with the 12-item WHODAS 2.0 questionnaire, supplemented with several dedicated questions regarding surgery-related pain (ie, duration of pain, severity of pain and relation with the surgical procedure).
Disability, measured according to the self-assessment 12-item WHODAS 2.0 before and after surgery, and reported as a percentage score of functional limitations. Scores range from 0% (no disability) to 100% (fully disabled). New clinically important disability is defined as a change>5% or more after surgery.
Mortality, registered as failure to rescue (ie, hospital mortality following a major postoperative complication), 30-day mortality, days alive and out of the hospital at 120 days, 1-year mortality and 2-year mortality.
The severity of a complication is graded according to the modified Clavien-Dindo classification.39
Study size
By the end of the recruitment phase approximately 3000 patients with major surgery will have been enrolled. Our study cohort allows us to validate, update and/or develop prediction models including 55 candidate predictors, based on an incidence of 15% for severe complications, a global shrinkage factor ≥0.9 and a c-statistics of 0.80.40 To investigate pathophysiological differences between patients with and without severe postoperative complications, a minimal effect size of 0.25 can be demonstrated using an α of 0.05 and a β of 0.95.
Future study design
The extensive collection of blood samples in our biorepository, combined with clinical data and prospectively collected patient-reported outcomes, provides the opportunity to answer a broad range of research questions. For aetiological research on the pathophysiology of postoperative complications, perioperative biomarker dynamics will be studied. The use of DAGs (Directed acyclic graphs) will be encouraged to assess the risk of potential residual confounding.41 Furthermore, BIGPROMISE enables us to do prediction studies, using biomarkers to improve risk stratification. This includes new model development, but also updating and validating existing risk models. To assess the potential for clinical use, reclassification measures and decision curve analysis will be performed. In addition, we will compare the predictive accuracy of new or non-standard biomarkers (eg, GDF-15, IL-6) for postoperative complications, with biomarkers that are currently often used in clinical practice (eg, C-reactive protein, leucocytes). Sensitivity, specificity and positive and negative predictive values will be calculated for biomarker cut-off values, and compared with prior literature reports.
Public and patient involvement
During the design of this study, we did not involve patient organisations.
Findings to date
Recruitment for BIGPROMISE started in October 2021. The first patient was enrolled on 12 October 2021. Currently (1 January 2024), 3086 patients were screened for eligibility, of whom 1785 (58%) provided informed consent for study participation (online supplemental figure 1). Most common types of major surgery are cardiac (49%) and gastrointestinal procedures (26%). Median age is 66 years (60; 73), 28% are female, and 68% of all patients are classified as ASA physical status class 3 (online supplemental table 3). The overall incidence of a severe postoperative complications is 16%. We anticipate to enrol approximately 1000 patients annually.
bmjopen-2023-078307supp003.pdf (88.5KB, pdf)
bmjopen-2023-078307supp006.pdf (24.7KB, pdf)
Collaboration
To enable research collaborations in the field of perioperative medicine, the outcome parameters of BIGPROMISE are defined according to international standards as described in PLUTO (perioperative longitudinal study of complications and long-term outcomes).42 The design of the BIGPROMISE biobank is based on the results of scientific research and the social interest in reducing the harmful consequences of postoperative complications. Data and biomaterials from BIGPROMISE can be used for future research within the scope of the scientific aim of the study and the informed consent provided by participants: to facilitate biomarker research on risk factors, pathophysiology and outcomes related to postoperative complications. Investigators who are interested in scientific collaboration may contact the study team through www.bigpromise.nl/contact. Applications will be reviewed by a scientific board according to methodological, statistical, ethical and legal criteria, in agreement with BIGPROMISE biobank regulations.
Funding
Expenses for personnel, materials, biomarker assays and storage of blood samples are financed with an external research grant from Roche Diagnostics International. Roche had no role in the design of our study, collection of data, preparation and publication of this manuscript.
Discussion
The BIGPROMISE biobank is designed to study the postoperative dysregulated stress response in its cause of postoperative complications, by analysing a large collection of perioperative biomarkers in a high-risk surgical population. In recent years, perioperative research on the pathophysiology of postoperative complications has mainly focused on myocardial injury and inflammation.17 27–31 However, randomised trials that studied interventions targeting one of these pathways did not result in new recommendations for perioperative treatments.22 For example, while systemic inflammation is associated with poor outcome, treatment with corticosteroids did not improve outcome in two large international randomised controlled trials in patients who underwent cardiac surgery.43 44 This may be explained by two reasons: first, different contributors to the dysregulated stress response may currently be under-recognised. Interventions targeting only a single known pathophysiological pathway may be insufficient to prevent postoperative organ injury and adverse outcomes. Second, perioperative interventions that use a ‘one size fits all approach’ overlook the fact that not all patients are identical. That is, some patients may develop an overwhelming stress response to surgery, while others exhibit a more balanced or even an underwhelming response. Treating these patients in the same way may have a beneficial effect in some and a detrimental effect in others, with no net result at all. Biomarkers can inform clinicians on which phenotype of dysregulated stress they are dealing with, and guide targeted interventions. Thus, a refined understanding of the postoperative dysregulated stress response is required to find new strategies to improve surgical outcomes. The BIGPROMISE study will use clinical and molecular data to construct (and validate) perioperative prediction models to improve risk stratification and early diagnosis and treatment of severe complications following major surgery. Our study has several limitations: first, blood samples are collected and stored for study purposes until 72 hours after surgery. As a result, pathophysiological mechanism related to complications that occur after that period may remain incompletely studied. Second, postoperative complications were defined in agreement with StEP criteria, as a result perioperative neurocognitive disorders are not recorded.
Currently, perioperative biomarkers are mainly used for risk management, but their use for the early diagnosis of complications or targeted interventions has potential added value. Despite that a lot is being invested in perioperative biomarker discovery, few biomarkers have made it from bench to bedside (eg, cardiac troponin, N-terminal pro B-type natriuretic peptide).22 Partly because few large, well-designed studies have been performed on the association between perioperative biomarker levels and adverse outcomes in surgical patients. BIGPROMISE will prospectively assess existing biomarker panels on fresh blood samples to validate their prognostic value for outcomes related to postoperative complications, and systematically collect and store plasma, serum and whole blood samples to allow for future perioperative biomarker discovery and development.
Supplementary Material
Acknowledgments
The authors would like to thank all colleagues in the participating centres (St. Antonius Hospital Nieuwegein, Amphia Hospital, Breda) for their support in conducting the BIGPROMISE study.
Footnotes
@AGE_antonius
Contributors: PGN, HJTR, IMD, TCDR initiated the study, PGN, TCDR wrote the draft manuscript. PGN acts as guarantor, RI, MSYT, OLC, NH, KNS, LMV and IMD critically reviewed the draft manuscript. All authors read and approved the final manuscript.
Funding: This study is supported by a research grant from Roche Diagnostics International.
Competing interests: PGN has participated in advisory boards for perioperative use of biomarkers, for which he has received a honorarium by Roche Diagnostics (Rotkreuz, Switzerland). PGN and TCDR have held lectures on perioperative biomarkers for which they have received a honorarium by Roche Diagnostics. OC has received research grants from ImmuneXpress Inc. (Seattle, WA) and Abionic SA (Epalinges, Switzerland) for related work.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. Data sharing not applicable as a preliminary dataset was generated for this report.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by Medical ethics Research Committees United ID: NL74076.100.20.
References
- 1. Weiser TG, Haynes AB, Molina G, et al. Estimate of the global volume of surgery in 2012: an assessment supporting improved health outcomes. The Lancet 2015;385:S11. 10.1016/S0140-6736(15)60806-6 [DOI] [PubMed] [Google Scholar]
- 2. Crawford TC, Magruder JT, Grimm JC, et al. Complications after cardiac operations: all are not created equal. Ann Thorac Surg 2017;103:32–40. [DOI] [PubMed] [Google Scholar]
- 3. Paun BC, Cassie S, MacLean AR, et al. Postoperative complications following surgery for rectal cancer. Ann Surg 2010;251:807–18. 10.1097/SLA.0b013e3181dae4ed [DOI] [PubMed] [Google Scholar]
- 4. Paul S, Sedrakyan A, Chiu YL, et al. Outcomes after lobectomy using thoracoscopy vs thoracotomy: a comparative effectiveness analysis utilizing the nationwide inpatient sample database. Eur J Cardiothorac Surg 2013;43:813–7. 10.1093/ejcts/ezs428 [DOI] [PubMed] [Google Scholar]
- 5. International Surgical Outcomes Study Group . Global patient outcomes after elective surgery: prospective cohort study in 27 Low-, middle- and high-income countries. Br J Anaesth 2016;117:601–9. 10.1093/bja/aew316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Khuri SF, Henderson WG, DePalma RG, et al. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg 2005;242:326–41; . 10.1097/01.sla.0000179621.33268.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Archer S, Pinto A, Vuik S, et al. Surgery, complications, and quality of life: a longitudinal cohort study exploring the role of psychosocial factors. Ann Surg 2018. 10.1097/SLA.0000000000002745 [DOI] [PubMed] [Google Scholar]
- 8. Verwijmeren L, Noordzij PG, Daeter EJ, et al. Preoperative frailty and one-year functional recovery in elderly cardiac surgery patients. J Thorac Cardiovasc Surg [Preprint] 2022. [DOI] [PubMed]
- 9. Vonlanthen R, Slankamenac K, Breitenstein S, et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg 2011;254:907–13. 10.1097/SLA.0b013e31821d4a43 [DOI] [PubMed] [Google Scholar]
- 10. Healy MA, Mullard AJ, Campbell DA, et al. Hospital and payer costs associated with surgical complications. JAMA Surg 2016;151:823–30. 10.1001/jamasurg.2016.0773 [DOI] [PubMed] [Google Scholar]
- 11. Cusack B, Buggy DJ. Anaesthesia, analgesia, and the surgical stress response. BJA Educ 2020;20:321–8. 10.1016/j.bjae.2020.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Castellheim A, Brekke OL, Espevik T, et al. Innate immune responses to danger signals in systemic inflammatory response syndrome and sepsis. Scand J Immunol 2009;69:479–91. 10.1111/j.1365-3083.2009.02255.x [DOI] [PubMed] [Google Scholar]
- 13. Manou-Stathopoulou V, Korbonits M, Ackland GL. Redefining the perioperative stress response: a narrative review. Br J Anaesth 2019;123:570–83. 10.1016/j.bja.2019.08.011 [DOI] [PubMed] [Google Scholar]
- 14. Lurati Buse G, Bollen Pinto B, Abelha F, et al. ESAIC focused guideline for the use of cardiac biomarkers in perioperative risk evaluation. Eur J Anaesthesiol 2023;40:888–927. 10.1097/EJA.0000000000001865 [DOI] [PubMed] [Google Scholar]
- 15. Vernooij LM, van Klei WA, Moons KG, et al. The comparative and added Prognostic value of biomarkers to the revised cardiac risk index for preoperative prediction of major adverse cardiac events and all‐cause mortality in patients who undergo noncardiac surgery. Cochrane Database Syst Rev 2021;12. 10.1002/14651858.CD013139.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Devereaux PJ, Biccard BM, Sigamani A, et al. Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. JAMA 2017;317:1642–51. 10.1001/jama.2017.4360 [DOI] [PubMed] [Google Scholar]
- 17. Rettig TCD, Verwijmeren L, Dijkstra IM, et al. Postoperative Interleukin-6 level and early detection of complications after elective major abdominal surgery. Ann Surg 2016;263:1207–12. 10.1097/SLA.0000000000001342 [DOI] [PubMed] [Google Scholar]
- 18. Zethelius B, Berglund L, Sundström J, et al. Use of multiple biomarkers to improve the prediction of death from cardiovascular causes. N Engl J Med 2008;358:2107–16. 10.1056/NEJMoa0707064 [DOI] [PubMed] [Google Scholar]
- 19. Blankenberg S, Zeller T, Saarela O, et al. Contribution of 30 biomarkers to 10-year cardiovascular risk estimation in 2 population cohorts. Circulation 2010;121:2388–97. 10.1161/CIRCULATIONAHA.109.901413 [DOI] [PubMed] [Google Scholar]
- 20. Siontis KC, Siontis GCM, Contopoulos-Ioannidis DG, et al. Diagnostic tests often fail to lead to changes in patient outcomes. J Clin Epidemiol 2014;67:612–21. 10.1016/j.jclinepi.2013.12.008 [DOI] [PubMed] [Google Scholar]
- 21. Ioannidis JPA, Bossuyt PMM. Waste, leaks, and failures in the biomarker pipeline. Clin Chem 2017;63:963–72. 10.1373/clinchem.2016.254649 [DOI] [PubMed] [Google Scholar]
- 22. Halvorsen S, Mehilli J, Cassese S, et al. ESC guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery. Eur Heart J 2022 Oct 2022;43:3826–924. [DOI] [PubMed] [Google Scholar]
- 23. Noordzij PG, Poldermans D, Schouten O, et al. Postoperative mortality in the Netherlands: a population-based analysis of surgery-specific risk in adults. Anesthesiology 2010;112:1105–15. 10.1097/ALN.0b013e3181d5f95c [DOI] [PubMed] [Google Scholar]
- 24. Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs 2005;14:798–804. 10.1111/j.1365-2702.2005.01121.x [DOI] [PubMed] [Google Scholar]
- 25. World health Organization . International classification of functioning, disability and health (ICF) practical manual V.0.9. n.d. Available: https://www.who.int/classifications/icf/en/
- 26. Harris PA, Taylor R, Minor BL, et al. The Redcap consortium: building an international community of software platform partners. J Biomed Inform 2019;95. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vascular Events In Noncardiac Surgery Patients Cohort Evaluation (VISION) Study Investigators, Devereaux PJ, Chan MTV, et al. Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. JAMA 2012;307:2295. 10.1001/jama.2012.5502 [DOI] [PubMed] [Google Scholar]
- 28. Devereaux PJ, Xavier D, Pogue J, et al. Characteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: a cohort study. Ann Intern Med 2011;154:523–8. 10.7326/0003-4819-154-8-201104190-00003 [DOI] [PubMed] [Google Scholar]
- 29. Beattie WS, Wijeysundera DN, Chan MTV, et al. Survival after isolated post-operative troponin elevation. J Am Coll Cardiol 2017;70:907–8. 10.1016/j.jacc.2017.06.023 [DOI] [PubMed] [Google Scholar]
- 30. Beattie WS, Wijeysundera DN, Chan MTV, et al. Implication of major adverse postoperative events and myocardial injury on disability and survival: a planned subanalysis of the ENIGMA-II trial. Anesth Analg 2018;127:1118–26. 10.1213/ANE.0000000000003310 [DOI] [PubMed] [Google Scholar]
- 31. Ackland GL, Abbott TEF, Cain D, et al. Preoperative systemic inflammation and perioperative myocardial injury: prospective observational multicentre cohort study of patients undergoing non-cardiac surgery. Br J Anaesth 2019;122:180–7. 10.1016/j.bja.2018.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bain CR, Myles PS, Corcoran T, et al. Postoperative systemic inflammatory dysregulation and corticosteroids: a narrative review. Anaesthesia 2023;78:356–70. 10.1111/anae.15896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Verwijmeren L, Bosma M, Vernooij LM, et al. Associations between preoperative biomarkers and cardiac surgery-associated acute kidney injury in elderly patients: a cohort study. Anesth Analg 2021;133:570–7. 10.1213/ANE.0000000000005650 [DOI] [PubMed] [Google Scholar]
- 34. Turan A, Artis AS, Hanline C, et al. Preoperative vitamin D concentration and cardiac, renal, and infectious morbidity after noncardiac surgery. Anesthesiology 2020;132:121–30. 10.1097/ALN.0000000000003000 [DOI] [PubMed] [Google Scholar]
- 35. Hazen Y, Noordzij PG, Gerritse BM, et al. Cardiothoracic surgery registration committee of the Netherlands heart registration. preoperative anaemia and outcome after elective cardiac surgery: a Dutch national Registry analysis. Br J Anaesth 2022;128:636–43. [DOI] [PubMed] [Google Scholar]
- 36. Smoor RM, Rettig TCD, Vernooij LM, et al. Postoperative anaemia and disability-free survival in older cardiac surgery patients. Br J Anaesth 2022;129:e27–9. 10.1016/j.bja.2022.04.017 [DOI] [PubMed] [Google Scholar]
- 37. Rössler J, Schoenrath F, Seifert B, et al. Iron deficiency is associated with higher mortality in patients undergoing cardiac surgery: a prospective study. Br J Anaesth 2020;124:25–34. 10.1016/j.bja.2019.09.016 [DOI] [PubMed] [Google Scholar]
- 38. Yoshida N, Horinouchi T, Toihata T, et al. Clinical significance of pretreatment red blood cell distribution width as a predictive marker for postoperative morbidity after esophagectomy for esophageal cancer: a retrospective study. Ann Surg Oncol 2022;29:606–13. 10.1245/s10434-021-10719-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205–13. 10.1097/01.sla.0000133083.54934.ae [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Riley RD, Snell KI, Ensor J, et al. Minimum sample size for developing a multivariable prediction model: PART II - binary and time-to-event outcomes. Stat Med 2019;38:1276–96. 10.1002/sim.7992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. VanderWeele TJ, Hernán MA, Robins JM. Causal directed Acyclic graphs and the direction of unmeasured confounding bias. Epidemiology 2008;19:720–8. 10.1097/EDE.0b013e3181810e29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. de Mul N, Verlaan D, Ruurda JP, et al. Cohort profile of PLUTO: a perioperative Biobank focusing on prediction and early diagnosis of postoperative complications. BMJ Open 2023;13:e068970. 10.1136/bmjopen-2022-068970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Dieleman JM, Nierich AP, Rosseel PM, et al. Intraoperative high-dose dexamethasone for cardiac surgery: a randomized controlled trial. JAMA 2012;308:1761–7. 10.1001/jama.2012.14144 [DOI] [PubMed] [Google Scholar]
- 44. Whitlock RP, Devereaux PJ, Teoh KH, et al. SIRS investigators. methylprednisolone in patients undergoing cardiopulmonary bypass (SIRS): a randomised, double-blind, placebo-controlled trial. Lancet 2015;386:1243–53. 10.1016/S0140-6736(15)00273-1 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-078307supp001.pdf (117.5KB, pdf)
bmjopen-2023-078307supp004.pdf (91.1KB, pdf)
bmjopen-2023-078307supp005.pdf (15KB, pdf)
bmjopen-2023-078307supp002.pdf (355.3KB, pdf)
bmjopen-2023-078307supp003.pdf (88.5KB, pdf)
bmjopen-2023-078307supp006.pdf (24.7KB, pdf)
Data Availability Statement
No data are available. Data sharing not applicable as a preliminary dataset was generated for this report.


