Abstract
Objectives
To evaluate the comparative effectiveness of sodium-glucose cotransporter-2 (SGLT-2) inhibitors, glucagon-like peptide-1 (GLP-1) receptor agonists, and dipeptidyl peptidase-4 (DPP-4) inhibitors in preventing hyperkalemia in people with type 2 diabetes in routine clinical practice.
Design
Population based cohort study with active-comparator, new user design.
Setting
Claims data from Medicare and two large commercial insurance databases in the United States from April 2013 to April 2022.
Participants
1:1 propensity score matched adults with type 2 diabetes newly starting SGLT-2 inhibitors versus DPP-4 inhibitors (n=778 908), GLP-1 receptor agonists versus DPP-4 inhibitors (n=729 820), and SGLT-2 inhibitors versus GLP-1 receptor agonists (n=873 460).
Main outcome measures
Hyperkalemia diagnosis in the inpatient or outpatient setting. Secondary outcomes were hyperkalemia defined as serum potassium levels ≥5.5 mmol/L and hyperkalemia diagnosis in the inpatient or emergency department setting.
Results
Starting SGLT-2 inhibitor treatment was associated with a lower rate of hyperkalemia than DPP-4 inhibitor treatment (hazard ratio 0.75, 95% confidence interval (CI) 0.73 to 0.78) and a slight reduction in rate compared with GLP-1 receptor agonists (0.92, 0.89 to 0.95). Use of GLP-1 receptor agonists was associated with a lower rate of hyperkalemia than DPP-4 inhibitors (0.79, 0.77 to 0.82). The three year absolute risk was 2.4% (95% CI 2.1% to 2.7%) lower for SGLT-2 inhibitors than DPP-4 inhibitors (4.6% v 7.0%), 1.8% (1.4% to 2.1%) lower for GLP-1 receptor agonists than DPP-4 inhibitors (5.7% v 7.5%), and 1.2% (0.9% to 1.5%) lower for SGLT-2 inhibitors than GLP-1 receptor agonists (4.7% v 6.0%). Findings were consistent for the secondary outcomes and among subgroups defined by age, sex, race, medical conditions, other drug use, and hemoglobin A1c levels on the relative scale. Benefits for SGLT-2 inhibitors and GLP-1 receptor agonists on the absolute scale were largest for those with heart failure, chronic kidney disease, or those using mineralocorticoid receptor antagonists. Compared with DPP-4 inhibitors, the lower rate of hyperkalemia was consistently observed across individual agents in the SGLT-2 inhibitor (canagliflozin, dapagliflozin, empagliflozin) and GLP-1 receptor agonist (dulaglutide, exenatide, liraglutide, semaglutide) classes.
Conclusions
In people with type 2 diabetes, SGLT-2 inhibitors and GLP-1 receptor agonists were associated with a lower risk of hyperkalemia than DPP-4 inhibitors in the overall population and across relevant subgroups. The consistency of associations among individual agents in the SGLT-2 inhibitor and GLP-1 receptor agonist classes suggests a class effect. These ancillary benefits of SGLT-2 inhibitors and GLP-1 receptor agonists further support their use in people with type 2 diabetes, especially in those at risk of hyperkalemia.
Introduction
People with type 2 diabetes are prone to developing hyperkalemia, especially those with comorbid conditions such as heart failure and chronic kidney disease.1 2 3 However, several drugs that improve clinical outcomes in people with type 2 diabetes and related comorbidities increase serum potassium levels, such as inhibitors of the renin-angiotensin-aldosterone system.4 5 6 7 8 9 Hyperkalemia is associated with a risk of life threatening cardiac arrhythmias and increased mortality,10 and the occurrence of hyperkalemia frequently leads to dose reduction or discontinuation of cardiorenal protective drugs. Stopping these drugs is associated with increased risk of adverse cardiovascular outcomes.11 12 13 14 Therefore, strategies that reduce the risk of hyperkalemia in this population are urgently needed.
Sodium-glucose cotransporter-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists have become cornerstone drug classes in the treatment of type 2 diabetes15 16 owing to their cardiovascular and kidney benefits.17 18 19 20 Post hoc analyses of randomized trials have recently shown that SGLT-2 inhibitors also lower the risk of hyperkalemia compared with placebo, an outcome that was not defined as primary or secondary in those trials.21 22 23 However, we do not know whether these benefits are also observed outside the highly controlled setting of randomized trials, and whether all agents within the SGLT-2 inhibitor class similarly reduce the risk of hyperkalemia. Furthermore, large scale epidemiological studies are needed that investigate the effects of GLP-1 receptor agonists on the risk of hyperkalemia in people with type 2 diabetes, with only a few small clinical studies suggesting plausible mechanisms for increased potassium excretion.24 25 GLP-1 receptor agonists might lead to increased potassium secretion owing to enhancement in sodium delivery to the cortical collecting duct and altered tubular electronegativity.25 26 Additionally, long term kidney preservation by SGLT-2 inhibitors or GLP-1 receptor agonists might contribute to reduced hyperkalemia risks. Notably, a recent study found that GLP-1 receptor agonist use was associated with lower hyperkalemia risk in patients with chronic kidney disease, but whether these benefits extend to the broader population with type 2 diabetes is unknown.27 The aim of this study was to investigate the comparative effectiveness of SGLT-2 inhibitors, GLP-1 receptor agonists, and dipeptidyl peptidase-4 (DPP-4) inhibitors in lowering the risk of hyperkalemia among adults with type 2 diabetes.
Methods
Data sources
We used data from Medicare fee-for-service (parts A, B, and D) and two commercial insurance databases: Optum’s deidentified Clinformatics Data Mart Database (CDM) and MarketScan. All three databases contain deidentified longitudinal information on patient demographics, healthcare use, inpatient and outpatient medical diagnoses and procedures, prescription dispensing records, and outpatient laboratory test results (available for approximately 45% of the population in CDM and 5-10% of patients in MarketScan). This study was approved by the Mass General Brigham institutional review board and granted waiver of informed consent because only deidentified claims data were used. Data use agreements were in place.
Study design and study population
We identified three study cohorts of patients who started SGLT-2 inhibitors versus DPP-4 inhibitors (cohort 1), GLP-1 receptor agonists versus DPP-4 inhibitors (cohort 2), and SGLT-2 inhibitors versus GLP-1 receptor agonists (cohort 3) from April 2013 to the end of available data (December 2019 in Medicare, December 2020 in MarketScan, and April 2022 in CDM). Cohort entry was the date of a newly filled prescription of SGLT-2 inhibitors, GLP-1 receptor agonists, or DPP-4 inhibitors. We chose DPP-4 inhibitors as comparator because they were commonly used as second or third line diabetes drugs during our study period, similar to SGLT-2 inhibitors or GLP-1 receptor agonists. In contrast, patients using metformin or insulin probably have less or more advanced diabetes, which would increase the risk of unmeasured confounding by diabetes severity and baseline risk of hyperkalemia. We restricted the study cohorts to patients with a diagnosis of type 2 diabetes and without use of any of the two drug classes being compared for the past 365 days, aged ≥18 years (≥65 years for Medicare), and with at least 12 months of continuous insurance enrollment before cohort entry. We excluded patients who had a history of type 1 diabetes, secondary or gestational diabetes, chronic kidney disease stage 5 or end stage kidney disease, nursing home admission, or a history of organ transplantation, pancreatitis, cirrhosis, acute hepatitis, or multiple endocrine neoplasia type 2 within 365 days before cohort entry. To decrease the risk of reverse causation bias (ie, that early outcomes would be related to a previous hyperkalemia diagnosis before starting the drug and therefore not related to the treatments under study), we further excluded people who had a hyperkalemia diagnosis in the inpatient or outpatient setting or potassium binder use in the 90 days before cohort entry. Supplemental table 1 provides definitions for inclusion and exclusion criteria and supplemental figure 1 gives an overview of the longitudinal design.
Outcomes and follow-up
The primary outcome was the occurrence of a diagnosis code for hyperkalemia in the inpatient or outpatient setting (supplemental table 2 gives definitions). Secondary outcomes were the occurrence of serum potassium ≥5.5 mmol/L during follow-up in the outpatient setting, and hyperkalemia diagnosis in the inpatient or emergency department setting. The laboratory based hyperkalemia outcome definition (serum potassium ≥5.5 mmol/L) was only assessed in CDM because Medicare and MarketScan contain no or too few laboratory test results. For this analysis, we restricted the study population to people who had at least two serum potassium measurements in the 365 days before cohort entry.
To test the specificity and sensitivity of the claims based hyperkalemia definitions, an internal validation study was performed in CDM. Briefly, we included all 12.3 million adults with serum potassium measurements (logical observation identifiers names and codes (LOINC) 6298-4, 77142-8, 12812-4, 12813-2, 42569-4). Then, we assessed whether there was a hyperkalemia diagnosis in the three months after the serum potassium test. For the primary outcome definition (ie, hyperkalemia diagnosis in inpatient or outpatient setting), specificity was 99.5% and sensitivity was 22.3% when we used serum potassium ≥5.5 mmol/L to define hyperkalemia; specificity was 99.3% and sensitivity was 37.1% when serum potassium ≥6.0 mmol/L was used as the gold standard. Relative risk estimates will be unbiased when specificity is high and non-differential, even if sensitivity is low.28 However, absolute rate differences will be biased towards the null when sensitivity is low.
We started follow-up on the day after cohort entry and continued until outcome occurrence or until any of the following occurred: treatment discontinuation or starting a drug in the comparator class, death, end of continuous health plan enrollment, or end of available data. We did not censor participants when they started other diabetes drugs (eg, sulfonylureas) during follow-up. We defined discontinuation as no prescription refill for the index exposure in the 30 days after the end of the days’ supply for the most recent prescription.
Confounders
We measured potential confounders during the 365 days before and including cohort entry date. We identified covariates that were confounders, confounder proxies or predictors for the outcome based on subject matter knowledge and previous studies that evaluated outcomes associated with drug use in people with type 2 diabetes.29 These included age, sex, race (race was only available in CDM and Medicare), and geographical region; comorbidities, such as heart failure and chronic kidney disease; diabetes specific complications, such as diabetic nephropathy, neuropathy, and retinopathy; use of drugs used to treat diabetes and cardiovascular disease, for example, insulin and renin-angiotensin system inhibitors; use of other drugs; measures of healthcare use, such as number of emergency department visits, hospital admissions, endocrinologist and internist visits, and laboratory tests; healthy behavior markers, such as screening and vaccinations; and calendar year. We also adjusted for a claims based frailty index30 to address potential confounding by frailty and for a claims based combined comorbidity score.31 Comorbidities and drug use were assessed in the 365 days before and including the cohort entry date and based on international classification of diseases (version 9 and 10) diagnosis and procedure codes, and generic drug names, respectively. In the subset of patients who had creatinine measurements available, we calculated estimated glomerular filtration rate using the race-free 2021 CKD-EPI (chronic kidney disease epidemiology collaboration) equation.32
Statistical analysis
To adjust for confounding, we used 1:1 propensity score matching with the nearest neighbor method and a caliper of 0.01 of the propensity score.33 We used multivariable logistic regression models to estimate the propensity scores. These models were fitted separately for each of the data sources (ie, CDM, MarketScan, and Medicare) and for each drug comparison (SGLT-2 inhibitors v DPP-4 inhibitors, GLP-1 receptor agonists v DPP-4 inhibitors, and SGLT-2 inhibitors v GLP-1 receptor agonists), for a total of nine propensity score models. All covariates listed in supplemental table 3 were included in the propensity score models, except for the laboratory test results, which were only available for a subset of patients. Because race was only available in CDM and Medicare, it was only used in the six propensity scores developed in the CDM and Medicare cohorts. Continuous covariates (eg, age) were entered as main terms and quadratic terms. We assessed covariate balance before and after propensity score matching with standardized mean differences, with a standardized mean difference <0.10 indicating sufficient balance.34 35 Because laboratory test results were not included in the propensity score, we considered their balance after propensity score matching to reflect residual unmeasured confounding. Hazard ratios were estimated with Cox regression models, and incidence rate differences were estimated with generalized linear regression models using an identity link function and normal error distribution.36 Effect estimates and their standard errors were estimated separately in each of the three data sources, and then pooled with fixed effects meta-analysis. Cumulative incidence curves were estimated with the Aalen-Johansen estimator in the propensity score matched cohort, which accounts for the competing risk of death.37 Absolute risks and risk differences at six month intervals were obtained from the cumulative incidences. There were no missing data for covariates other than the laboratory measurements. Analyses were performed using R version 3.6.2 and the Aetion Evidence Platform version 4.53.38
Subgroup and sensitivity analyses
To investigate potential treatment effect modification, we performed a number of subgroup analyses in the following prespecified strata: age (<65 years v ≥65 years), sex, race (white v black, based on Medicare data only, where the race variable has been validated against self-reported race39), heart failure, cardiovascular disease, chronic kidney disease, use of renin-angiotensin-aldosterone system inhibitors, mineralocorticoid receptor antagonists, loop diuretics and insulin on the cohort entry date, and by baseline hemoglobin A1c level (<7.5% v 7.5-9.0% v ≥9.0%). We re-estimated propensity scores and reperformed matching for each subgroup stratum.40
To examine the robustness of our findings, we performed the following sensitivity analyses: treatment discontinuation was defined as no prescription refill for the index drug within 60 days rather than 30 days; to investigate the potential influence of informative censoring, we followed patients for a maximum of 180 and 365 days, regardless of treatment discontinuation or starting a drug in the comparator class; finally, we excluded patients with a history of hyperkalemia or potassium binder use in the previous 365 days.
Individual agents in SGLT-2 inhibitor and GLP-1 receptor agonist classes
We investigated potential differences in the risk of hyperkalemia for individual agents in the SGLT-2 inhibitor or GLP-1 receptor agonist classes by constructing separate cohorts for empagliflozin, canagliflozin, dapagliflozin, liraglutide, dulaglutide, exenatide, and semaglutide versus DPP-4 inhibitors, re-estimated the propensity scores and reperformed the matching, and calculated effect estimates for the primary outcome. The SGLT-2 inhibitor cohorts were restricted to the dates when both drugs under comparison were on the market (April 2013 for canagliflozin v DPP-4 inhibitors, January 2014 for dapagliflozin v DPP-4 inhibitors, and August 2014 for empagliflozin v DPP-4 inhibitors).
Patient and public involvement
There were no funds or time allocated for patient and public involvement, so we were unable to involve patients. Nevertheless, this study was inspired by conversations with patients in clinical practice. We also asked a member of the public to provide feedback on the article before resubmission. To be compliant with our data use agreements, we are not allowed to reidentify and contact patients who were included in the study dataset to share the results of this research.
Results
Baseline characteristics of study populations
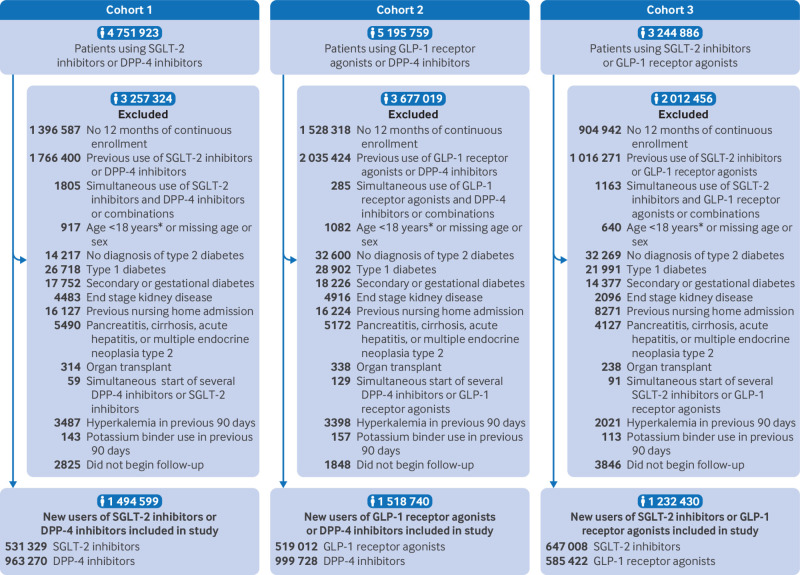
Figure 1 reports patient inclusion flowcharts. After 1:1 propensity score matching, there were 389 454 propensity score matched pairs in the SGLT-2 inhibitor versus DPP-4 inhibitor cohort, 364 910 pairs in the GLP-1 receptor agonist versus DPP-4 inhibitor cohort, and 436 730 matched pairs in the SGLT-2 inhibitor versus GLP-1 receptor agonist cohort. After matching, all baseline characteristics in the three cohorts were well balanced, with standardized mean differences <0.10. Laboratory test results, including potassium, were also balanced, despite not being included in propensity score models (table 1, supplemental tables 3-5).
Fig 1.
Patient flowchart. *<65 years for Medicare. DPP-4=dipeptidyl peptidase-4; GLP-1=glucagon-like peptide-1; SGLT-2=sodium-glucose cotransporter-2
Table 1.
Selected baseline characteristics of people with type 2 diabetes starting SGLT-2 inhibitors versus DPP-4 inhibitors, GLP-1 receptor agonists versus DPP-4 inhibitors, and SGLT-2 inhibitors versus GLP-1 receptor agonists after 1:1 propensity score matching
| Characteristics | SGLT-2 inhibitors v DPP-4 inhibitors | GLP-1 receptor agonists v DPP-4 inhibitors | SGLT-2 inhibitors v GLP-1 receptor agonists | |||||
|---|---|---|---|---|---|---|---|---|
| SGLT-2 inhibitors | DPP-4 inhibitors | GLP-1 receptor agonists | DPP-4 inhibitors | SGLT-2 inhibitors | GLP-1 receptor agonists | |||
| Total No of participants | 389 454 | 389 454 | 364 910 | 364 910 | 436 730 | 436 730 | ||
| Age, mean (SD) | 62.7 (9.5) | 62.6 (9.5) | 62.3 (9.5) | 62.2 (9.5) | 62.0 (9.6) | 62.1 (9.6) | ||
| Men | 209 774 (53.9) | 209 725 (53.9) | 175 506 (48.1) | 175 496 (48.1) | 218 999 (50.1) | 219 612 (50.3) | ||
| Race or ethnicity* | ||||||||
| White | 174 543 (70.6) | 174 447 (70.6) | 169 932 (72.2) | 170 330 (72.3) | 202 025 (71.7) | 201 210 (71.4) | ||
| Black | 26 576 (10.8) | 26 595 (10.8) | 27 134 (11.5) | 26 972 (11.5) | 31 322 (11.1) | 31 444 (11.2) | ||
| Hispanic | 10 047 (4.1) | 10 077 (4.1) | 6022 (2.6) | 5734 (2.4) | 7985 (2.8) | 8445 (3.0) | ||
| Asian | 24 361 (9.9) | 24 491 (9.9) | 21 824 (9.3) | 21 886 (9.3) | 27 183 (9.7) | 27 333 (9.7) | ||
| Other | 11 830 (4.8) | 11 747 (4.8) | 10 588 (4.5) | 10 578 (4.5) | 13 169 (4.7) | 13 252 (4.7) | ||
| Burden of comorbidities | ||||||||
| Combined comorbidity score, mean (SD) | 1.1 (2.0) | 1.1 (1.9) | 1.3 (2.0) | 1.3 (2.0) | 1.2 (2.0) | 1.2 (1.9) | ||
| Frailty score, mean (SD) | 0.16 (0.05) | 0.16 (0.05) | 0.16 (0.05) | 0.16 (0.05) | 0.16 (0.05) | 0.16 (0.05) | ||
| Comorbidities | ||||||||
| Hypertension | 304 807 (78.3) | 304 512 (78.2) | 288 327 (79.0) | 288 447 (79.0) | 345 667 (79.1) | 346 112 (79.3) | ||
| Hyperlipidemia | 304 587 (78.2) | 304 319 (78.1) | 283 838 (77.8) | 283 746 (77.8) | 342 881 (78.5) | 343 544 (78.7) | ||
| Cardiovascular disease† | 117 292 (30.1) | 118 619 (30.5) | 110 719 (30.3) | 111 001 (30.4) | 131 703 (30.2) | 131 728 (30.2) | ||
| Acute myocardial infarction | 7046 (1.8) | 6919 (1.8) | 5773 (1.6) | 5787 (1.6) | 7064 (1.6) | 7163 (1.6) | ||
| Heart failure | 30 258 (7.8) | 29 856 (7.7) | 30 446 (8.3) | 30 430 (8.3) | 34 535 (7.9) | 34 862 (8.0) | ||
| Atrial fibrillation | 28 818 (7.4) | 28 444 (7.3) | 26 880 (7.4) | 26 898 (7.4) | 31 381 (7.2) | 31 448 (7.2) | ||
| Ischemic stroke | 27 158 (7.0) | 26 909 (6.9) | 25 207 (6.9) | 25 176 (6.9) | 29 450 (6.7) | 29 512 (6.8) | ||
| Peripheral arterial disease | 30 878 (7.9) | 30 640 (7.9) | 30 505 (8.4) | 30 299 (8.3) | 35 457 (8.1) | 35 803 (8.2) | ||
| Acute kidney injury | 10 108 (2.6) | 9964 (2.6) | 12 602 (3.5) | 12 640 (3.5) | 12 198 (2.8) | 12 370 (2.8) | ||
| Chronic kidney disease stage 3-4 | 26 571 (6.8) | 26 061 (6.7) | 39 986 (11.0) | 40 063 (11.0) | 35 547 (8.1) | 36 485 (8.4) | ||
| Hyperkalemia‡ | 4048 (1.0) | 3997 (1.0) | 4637 (1.3) | 4622 (1.3) | 5099 (1.2) | 5209 (1.2) | ||
| Hypokalemia | 8566 (2.2) | 8595 (2.2) | 8975 (2.5) | 9015 (2.5) | 9614 (2.2) | 9614 (2.2) | ||
| Diabetes related conditions | ||||||||
| Diabetic nephropathy | 44 852 (11.5) | 44 602 (11.5) | 51 426 (14.1) | 51 345 (14.1) | 57 905 (13.3) | 58 320 (13.4) | ||
| Diabetic retinopathy | 34 775 (8.9) | 34 610 (8.9) | 35 787 (9.8) | 35 378 (9.7) | 42 897 (9.8) | 43 186 (9.9) | ||
| Diabetic neuropathy | 73 165 (18.8) | 72 803 (18.7) | 77 527 (21.2) | 77 020 (21.1) | 91 832 (21.0) | 92 506 (21.2) | ||
| Hypoglycemia | 37 841 (9.7) | 37 954 (9.7) | 38 539 (10.6) | 38 397 (10.5) | 46 861 (10.7) | 47 085 (10.8) | ||
| No of distinct drugs, mean (SD) | 12.11 (5.90) | 12.09 (5.98) | 12.90 (6.00) | 12.90 (6.27) | 12.92 (6.15) | 12.94 (5.95) | ||
| Diabetes drugs on day of cohort entry | ||||||||
| No of diabetes drugs, mean (SD) | 2.20 (0.83) | 2.20 (0.78) | 2.24 (0.90) | 2.24 (0.84) | 2.37 (0.94) | 2.37 (0.96) | ||
| Metformin | 315 259 (80.9) | 316 007 (81.1) | 278 632 (76.4) | 279 537 (76.6) | 342 059 (78.3) | 341 792 (78.3) | ||
| Sulfonylureas | 148 938 (38.2) | 149 790 (38.5) | 136 649 (37.4) | 137 785 (37.8) | 173 718 (39.8) | 173 516 (39.7) | ||
| DPP-4 inhibitors | — | — | — | — | 126 648 (29.0) | 127 553 (29.2) | ||
| SGLT-2 inhibitors | — | — | 51 830 (14.2) | 51 994 (14.2) | — | — | ||
| GLP-1 receptor agonists | 38 561 (9.9) | 35 525 (9.1) | — | — | — | — | ||
| Insulin | 77 967 (20.0) | 76 981 (19.8) | 96 000 (26.3) | 94 123 (25.8) | 114 963 (26.3) | 115 746 (26.5) | ||
| Other drug use | ||||||||
| ACEi or ARB | 281 918 (72.4) | 281 578 (72.3) | 263 230 (72.1) | 262 922 (72.1) | 319 598 (73.2) | 319 716 (73.2) | ||
| ARNI | 1485 (0.4) | 1409 (0.4) | 1098 (0.3) | 1113 (0.3) | 1592 (0.4) | 1678 (0.4) | ||
| Mineralocorticoid receptor antagonists | 14 276 (3.7) | 14 108 (3.6) | 14 902 (4.1) | 14 821 (4.1) | 17 491 (4.0) | 17 622 (4.0) | ||
| β blockers | 137 684 (35.4) | 136 690 (35.1) | 130 890 (35.9) | 130 648 (35.8) | 155 722 (35.7) | 156 071 (35.7) | ||
| Calcium channel blockers | 106 730 (27.4) | 106 158 (27.3) | 100 578 (27.6) | 100 012 (27.4) | 120 189 (27.5) | 120 647 (27.6) | ||
| Loop diuretics | 46 067 (11.8) | 45 439 (11.7) | 51 757 (14.2) | 51 596 (14.1) | 56 323 (12.9) | 56 592 (13.0) | ||
| Statins | 277 161 (71.2) | 276 857 (71.1) | 257 353 (70.5) | 257 159 (70.5) | 314 054 (71.9) | 314 785 (72.1) | ||
| Antiplatelet agents | 39 170 (10.1) | 38 620 (9.9) | 35 038 (9.6) | 34 732 (9.5) | 42 626 (9.8) | 42 905 (9.8) | ||
| Anticoagulants | 26 476 (6.8) | 26 452 (6.8) | 25 522 (7.0) | 25 527 (7.0) | 29 630 (6.8) | 29 736 (6.8) | ||
| Potassium binders‡ | 248 (0.1) | 230 (0.1) | 364 (0.1) | 357 (0.1) | 358 (0.1) | 353 (0.1) | ||
| Potassium supplements | 28 010 (7.2) | 27 929 (7.2) | 29 695 (8.1) | 29 744 (8.2) | 33 029 (7.6) | 33 069 (7.6) | ||
| Healthcare use markers | ||||||||
| No of hospital admissions, mean (SD) | 0.12 (0.45) | 0.12 (0.43) | 0.13 (0.48) | 0.13 (0.46) | 0.12 (0.44) | 0.12 (0.45) | ||
| No of emergency department visits, mean (SD) | 0.40 (1.25) | 0.40 (1.15) | 0.46 (1.41) | 0.46 (1.27) | 0.41 (1.23) | 0.41 (1.27) | ||
| No of internist visits, mean (SD) | 14.56 (18.90) | 14.56 (19.34) | 14.94 (19.41) | 14.99 (19.59) | 14.94 (19.18) | 14.96 (19.47) | ||
| No of cardiologist visits, mean (SD) | 2.38 (6.39) | 2.35 (6.19) | 2.34 (6.27) | 2.33 (6.14) | 2.31 (6.03) | 2.32 (6.29) | ||
| No of endocrinologist visits, mean (SD) | 1.14 (4.99) | 1.11 (4.99) | 1.35 (5.48) | 1.32 (5.39) | 1.45 (5.51) | 1.46 (5.69) | ||
| No of nephrologist visits, mean (SD) | 0.18 (2.23) | 0.18 (1.65) | 0.28 (2.13) | 0.28 (2.13) | 0.21 (2.30) | 0.22 (1.90) | ||
| Potassium test order | 9266 (2.4) | 9238 (2.4) | 9808 (2.7) | 9841 (2.7) | 10 873 (2.5) | 10 923 (2.5) | ||
| Laboratory measurements, mean (SD) | ||||||||
| eGFR, mL/min/1.73 m2 | 80 (23) | 79 (23) | 79 (24) | 79 (24) | 80 (23) | 79 (24) | ||
| Serum potassium, mmol/L | 4.4 (0.4) | 4.4 (0.4) | 4.4 (0.4) | 4.4 (0.4) | 4.4 (0.4) | 4.4 (0.4) | ||
Data are numbers (%) unless stated otherwise.
ACEi=angiotensin-converting enzyme inhibitor; ARB=angiotensin II receptor blocker; ARNI=angiotensin-receptor neprilysin inhibitor; CKD=chronic kidney disease; DPP-4=dipeptidyl peptidase-4; eGFR=estimated glomerular filtration rate; GLP-1=glucagon-like peptide-1; HbA1c=hemoglobin A1c; SD=standard deviation; SGLT-2=sodium-glucose cotransporter-2.
Only available in Optum’s deidentified Clinformatics Data Mart (CDM) and Medicare databases. Percentages are relative to sample size of CDM and Medicare databases so total adds up to 100%.
Cardiovascular disease was defined as a composite of myocardial infarction, stable angina, acute coronary syndrome, coronary atherosclerosis, history of coronary procedure, heart failure, ischemic stroke and peripheral vascular disease.
People diagnosed with hyperkalemia or those who used potassium binders in 90 days before cohort entry were excluded. Number represents patients with hyperkalemia diagnosis or use of potassium binders more than 90 days before cohort entry.
In the SGLT-2 inhibitor versus DPP-4 inhibitor cohort, the mean age was 63 years, 54% were male, and 30% had a history of cardiovascular disease. Commonly used drugs included metformin (81%), angiotensin converting enzyme inhibitors or angiotensin II receptor blockers (72%), statins (71%), and β blockers (35%). Mean estimated glomerular filtration rate was 79 mL/min/1.73 m2 and mean serum potassium level was 4.4 mmol/L among the subset with available laboratory test results. Baseline characteristics were comparable in the GLP-1 receptor agonist versus DPP-4 inhibitor cohort, and the SGLT-2 inhibitor versus GLP-1 receptor agonist cohort. In the SGLT-2 inhibitor versus DPP-4 inhibitor cohort, 40.7% started empagliflozin, 38.7% started canagliflozin, and 20.3% started dapagliflozin (supplemental table 6). The most commonly used GLP-1 receptor agonists were liraglutide (37.2%), dulaglutide (31.8%), exenatide (15.7%), and semaglutide (13.0%).
Risk of hyperkalemia after starting SGLT-2 inhibitors, GLP-1 receptor agonists, and DPP-4 inhibitors
Mean on-treatment follow-up ranged between 8.1 and 8.8 months, reflecting the large rate of discontinuation in routine clinical practice (supplemental table 7). Use of SGLT-2 inhibitors versus DPP-4 inhibitors was associated with a lower rate of hyperkalemia in the propensity score matched cohort, with an adjusted hazard ratio of 0.75 (95% confidence interval (CI) 0.73 to 0.78). Incidence rates were 25.3 versus 18.5 events per 1000 person years, corresponding to an incidence rate difference of −6.88 (95% CI −7.65 to −6.11) events per 1000 person years (table 2). Similarly, use of GLP-1 receptor agonists versus DPP-4 inhibitors was associated with a lower rate of hyperkalemia, with an adjusted hazard ratio of 0.79 (0.77 to 0.82). Incidence rates were 28.5 versus 22.1 events per 1000 person years, corresponding to an incidence rate difference of −6.36 (−7.24 to −5.48) per 1000 person years. The adjusted hazard ratio for SGLT-2 inhibitors versus GLP-1 receptor agonists was 0.92 (0.89 to 0.95). Incidence rates were 22.1 versus 19.8 events per 1000 person years, corresponding to an incidence rate difference of −2.31 (−3.05 to −1.57). Figure 2 shows cumulative incidence curves for all three cohorts and supplemental table 8 reports corresponding absolute risks and risk differences at six month intervals. The lower risk of hyperkalemia for SGLT-2 inhibitors and GLP-1 receptor agonists versus DPP-4 inhibitors appeared within six months of follow-up. At three years of follow-up, the absolute risk was 2.4% (95% CI 2.1% to 2.7%) lower for SGLT-2 inhibitors than DPP-4 inhibitors (4.6% v 7.0%), and 1.8% (1.4% to 2.1%) lower for GLP-1 receptor agonists than DPP-4 inhibitors (5.7% v 7.5%).
Table 2.
Comparative effectiveness of SGLT-2 inhibitors versus DPP-4 inhibitors, GLP-1 receptor agonists versus DPP-4 inhibitors, and SGLT-2 inhibitors versus GLP-1 receptor agonists in reducing risk of hyperkalemia in inpatient or outpatient setting after 1:1 propensity score matching
| Participants, events, follow-up, rates, and hazard ratios | SGLT-2 inhibitors v DPP-4 inhibitors | GLP-1 receptor agonists v DPP-4 inhibitors | SGLT-2 inhibitors v GLP-1 receptor agonists | |||||
|---|---|---|---|---|---|---|---|---|
| SGLT-2 inhibitors | DPP-4 inhibitors | GLP-1 receptor agonists | DPP-4 inhibitors | SGLT-2 inhibitors | GLP-1 receptor agonists | |||
| No of participants | 389 454 | 389 454 | 364 910 | 364 910 | 436 730 | 436 730 | ||
| Total events | 5351 | 7093 | 5296 | 7549 | 6169 | 6169 | ||
| Follow-up, person years | 290 105 | 280 045 | 239 221 | 264 892 | 308.736 | 279 265 | ||
| Incidence rate per 1000 person years (95% CI) | 18.45 (17.95 to 18.95) | 25.33 (24.74 to 25.92) | 22.14 (21.55 to 22.74) | 28.50 (27.86 to 29.15) | 19.78 (19.29 to 28.77) | 22.09 (21.54 to 22.65) | ||
| Rate difference per 1000 person years (95% CI) | −6.88 (−7.65 to −6.11) | Reference | −6.36 (−7.24 to −5.48) | Reference | −2.31 (−3.05 to −1.57) | Reference | ||
| Hazard ratio (95% CI) | 0.75 (0.73 to 0.78) | Reference | 0.79 (0.77 to 0.82) | Reference | 0.92 (0.89 to 0.95) | Reference | ||
CI=confidence interval; DPP-4=dipeptidyl peptidase-4; GLP-1=glucagon-like peptide-1; SGLT-2=sodium-glucose cotransporter-2.
Fig 2.
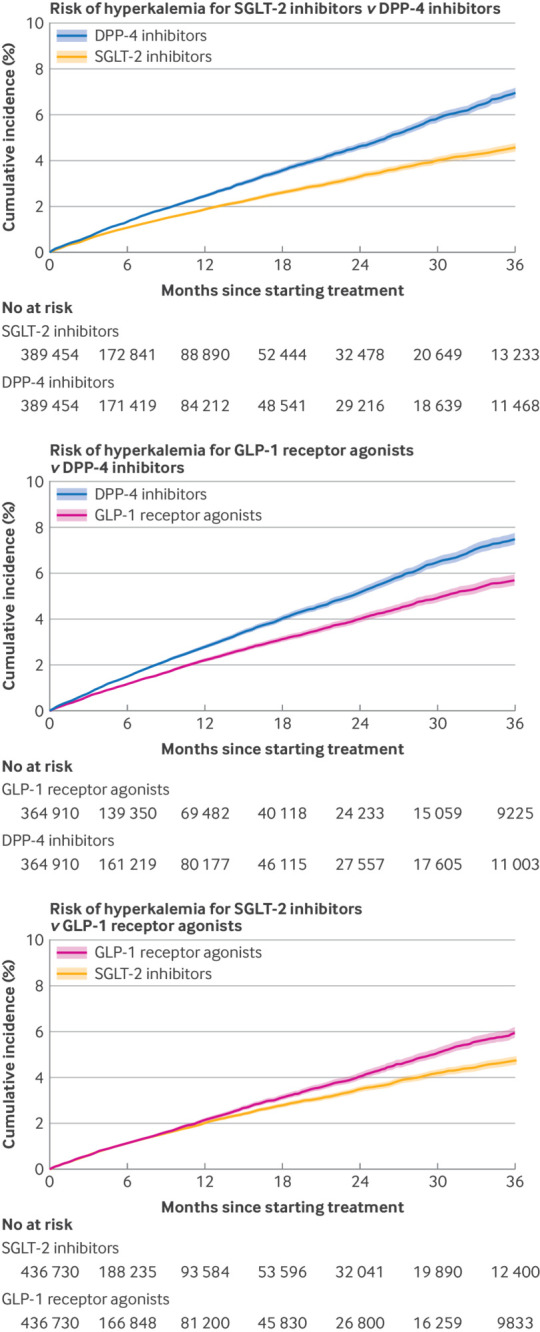
Cumulative incidence curves for SGLT-2 inhibitors versus DPP-4 inhibitors (upper panel), GLP-1 receptor agonists versus DPP-4 inhibitors (middle panel), and SGLT-2 inhibitors versus GLP-1 receptor agonists (lower panel) for primary outcome of risk of hyperkalemia diagnosis in inpatient or outpatient setting after 1:1 propensity score matching. DPP-4=dipeptidyl peptidase-4; GLP-1=glucagon-like peptide-1; SGLT-2=sodium-glucose cotransporter-2
When using serum potassium ≥5.5 mmol/L as the outcome definition, hazard ratios were 0.86 (0.78 to 0.95) for SGLT-2 inhibitors versus DPP-4 inhibitors, 0.82 (0.73 to 0.91) for GLP-1 receptor agonists versus DPP-4 inhibitors, and 1.01 (0.91 to 1.12) for SGLT-2 inhibitors versus GLP-1 receptor agonists (supplemental table 9). Furthermore, when using hyperkalemia diagnosis in the inpatient or emergency department setting, adjusted hazard ratios were 0.77 (0.69 to 0.85), 0.65 (0.59 to 0.72), and 0.96 (0.86 to 1.06), respectively (supplemental table 10).
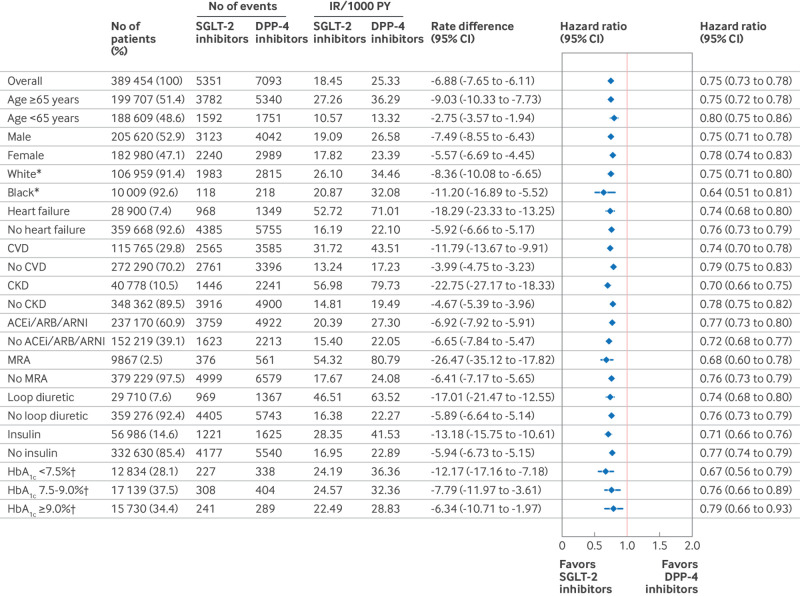
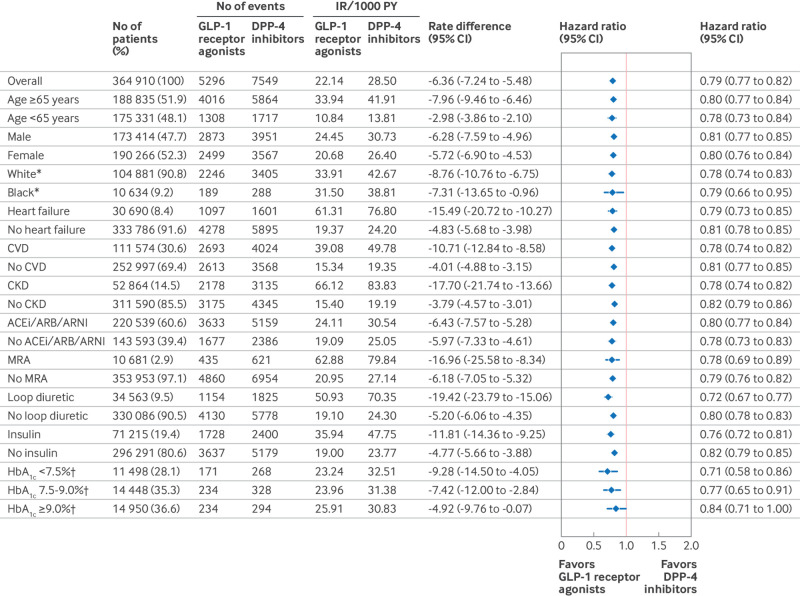
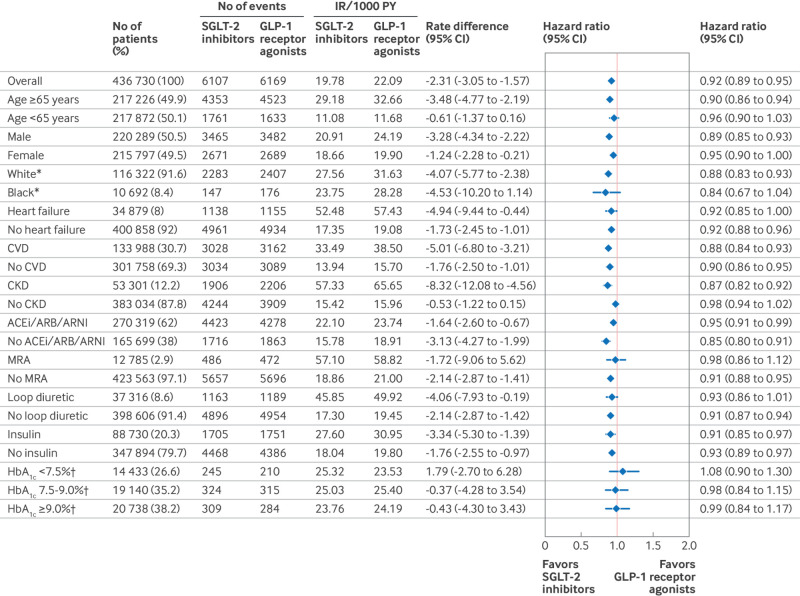
Subgroup and sensitivity analyses
SGLT-2 inhibitors and GLP-1 receptor agonists showed protective associations for hyperkalemia across all subgroups compared with DPP-4 inhibitors (fig 3, fig 4). Benefits for SGLT-2 inhibitors and GLP-1 receptor agonists on the absolute scale were largest for those with heart failure, chronic kidney disease, or those using mineralocorticoid receptor antagonists. Findings for the SGLT-2 inhibitor versus GLP-1 receptor agonist cohort were consistent, with absence of large differences in hyperkalemia rate between the two drug classes across subgroups (fig 5). Findings were also consistent across sensitivity analyses (supplemental table 11).
Fig 3.
Comparative effectiveness of SGLT-2 inhibitors versus DPP-4 inhibitors for primary outcome of risk of hyperkalemia diagnosis in inpatient or outpatient setting among subgroups after 1:1 propensity score matching. Number of propensity score matched patients in subgroups do not exactly add up to overall number of propensity score matched patients in main analysis because propensity score matching was performed within each subgroup; therefore, it is possible that more patients are matched within subgroups. ACE=angiotensin converting enzyme inhibitor; ARB=angiotensin II receptor blocker; ARNI=angiotensin receptor/neprilysin inhibitor; CI=confidence interval; CVD=cardiovascular disease; CKD=chronic kidney disease; DPP-4=dipeptidyl peptidase-4; IR=incidence rate; MRA=mineralocorticoid receptor antagonist; PY=person years; SGLT-2=sodium-glucose cotransporter-2. *Only data from Medicare; †only data from Optum’s deidentified Clinformatics Data Mart Database
Fig 4.
Comparative effectiveness of GLP-1 receptor agonists versus DPP-4 inhibitors for primary outcome of risk of hyperkalemia diagnosis in inpatient or outpatient setting among subgroups after 1:1 propensity score matching. Number of propensity score matched patients in subgroups do not exactly add up to overall number of propensity score matched patients in main analysis because propensity score matching was performed within each subgroup; therefore, it is possible that more patients are matched within subgroups. ACE=angiotensin converting enzyme inhibitor; ARB=angiotensin II receptor blocker; ARNI=angiotensin receptor/neprilysin inhibitor; CI=confidence interval; CVD=cardiovascular disease; CKD=chronic kidney disease; DPP-4=dipeptidyl peptidase-4; GLP-1=glucagon-like peptide-1; IR=incidence rate; MRA=mineralocorticoid receptor antagonist; PY=person years. *Only data from Medicare; †only data from Optum’s deidentified Clinformatics Data Mart Database
Fig 5.
Comparative effectiveness of SGLT-2 inhibitors versus GLP-1 receptor agonists for primary outcome of risk of hyperkalemia diagnosis in inpatient or outpatient setting among subgroups after 1:1 propensity score matching. Number of propensity score matched patients in subgroups do not exactly add up to overall number of propensity score matched patients in main analysis because propensity score matching was performed within each subgroup; therefore, it is possible that more patients are matched within subgroups. ACE=angiotensin converting enzyme inhibitor; ARB=angiotensin II receptor blocker; ARNI=angiotensin receptor/neprilysin inhibitor; CI=confidence interval; CVD=cardiovascular disease; CKD=chronic kidney disease; GLP-1=glucagon-like peptide-1; IR=incidence rate; MRA=mineralocorticoid receptor antagonist; PY=person years; SGLT-2=sodium-glucose cotransporter-2. *Only data from Medicare; †only data from Optum’s deidentified Clinformatics Data Mart Database
Effectiveness of individual agents in SGLT-2 inhibitor and GLP-1 receptor agonist classes compared with DPP-4 inhibitors
Compared with DPP-4 inhibitors, the lower rate of hyperkalemia was consistent for single agents within the SGLT-2 inhibitor class: hazard ratios were 0.76 (0.72 to 0.80) for canagliflozin, 0.85 (0.79 to 0.91) for dapagliflozin, and 0.75 (0.71 to 0.78) for empagliflozin (table 3). Hazard ratios were consistent among individual GLP-1 receptor agonist agents compared with DPP-4 inhibitors, with hazard ratios of 0.80 (0.76 to 0.84) for dulaglutide, 0.78 (0.73 to 0.84) for exenatide, 0.79 (0.75 to 0.83) for liraglutide, and 0.74 (0.68 to 0.80) for semaglutide (table 4).
Table 3.
Comparative effectiveness of individual SGLT-2 inhibitor agents versus DPP-4 inhibitors in reducing risk of hyperkalemia in inpatient or outpatient setting after 1:1 propensity score matching
| Participants, events, follow-up, rates, and hazard ratios | Canagliflozin v DPP-4 inhibitors | Dapagliflozin v DPP-4 inhibitors | Empagliflozin v DPP-4 inhibitors | |||||
|---|---|---|---|---|---|---|---|---|
| Canagliflozin | DPP-4 inhibitors | Dapagliflozin | DPP-4 inhibitors | Empagliflozin | DPP-4 inhibitors | |||
| No of participants | 172 464 | 172 464 | 124 349 | 124 349 | 210 866 | 210 866 | ||
| Total events | 2348 | 3379 | 1402 | 1734 | 2854 | 3702 | ||
| Follow-up, person years | 134 040 | 142 681 | 84 154 | 85 008 | 143 456 | 136 671 | ||
| Incidence rate per 1000 person years (95% CI) | 17.52 (16.82 to 18.24) | 23.68 (22.89 to 24.49) | 16.66 (15.80 to 17.56) | 20.40 (19.45 to 21.38) | 19.89 (19.17 to 20.64) | 27.09 (26.22 to 27.97) | ||
| Rate difference per 1000 person years (95% CI) | −6.17 (−7.23 to −5.10) | Reference | −3.74 (−5.04 to −2.44) | Reference | −7.19 (−8.33 to −6.05) | Reference | ||
| Hazard ratio (95% CI) | 0.76 (0.72 to 0.80) | Reference | 0.85 (0.79 to 0.91) | Reference | 0.75 (0.71 to 0.78) | Reference | ||
SGLT-2 inhibitor cohorts were restricted to dates when both drugs under comparison were on the market (ie, April 2013 for canagliflozin v DPP-4 inhibitors, January 2014 for dapagliflozin v DPP-4 inhibitors, and August 2014 for empagliflozin v DPP-4 inhibitors). CI=confidence interval; DPP-4=dipeptidyl peptidase-4; SGLT-2=sodium-glucose cotransporter 2.
Table 4.
Comparative effectiveness of individual GLP-1 receptor agonist agents versus DPP-4 inhibitors in reducing risk of hyperkalemia in inpatient or outpatient setting after 1:1 propensity score matching
| Participants, events, follow-up, rates, and hazard ratios | Dulaglutide v DPP-4 inhibitors | Exenatide v DPP-4 inhibitors | Liraglutide v DPP-4 inhibitors | Semaglutide v DPP-4 inhibitors | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Dulaglutide | DPP-4 inhibitors | Exenatide | DPP-4 inhibitors | Liraglutide | DPP-4 inhibitors | Semaglutide | DPP-4 inhibitors | ||||
| No of participants | 183 669 | 183 669 | 87 825 | 87 825 | 180 747 | 180 747 | 88 687 | 88 687 | |||
| Total events | 2988 | 3,585 | 1019 | 1834 | 2598 | 4146 | 842 | 1311 | |||
| Follow-up, person years | 134 568 | 124 691 | 49 312 | 69 226 | 112 743 | 142 599 | 42 147 | 47 594 | |||
| Incidence rate per 1000 person years (95% CI) | 22.20 (21.42 to 23.02) | 28.75 (27.82 to 29.71) | 20.66 (19.41 to 21.97) | 26.49 (25.29 to 27.73) | 23.04 (22.17 to 23.95) | 29.07 (28.20 to 29.97) | 19.98 (18.65 to 21.37) | 27.55 (26.07 to 29.08) | |||
| Rate difference per 1000 person years (95% CI) | −6.55 (−7.78 to −5.31) | Reference | −5.83 (−7.58 to −4.07) | Reference | −6.03 (−7.28 to −4.78) | Reference | −7.57 (−9.58 to −5.56) | Reference | |||
| Hazard ratio (95% CI) | 0.80 (0.76 to 0.84) | Reference | 0.78 (0.73 to 0.84) | Reference | 0.79 (0.75 to 0.83) | Reference | 0.74 (0.68 to 0.80) | Reference | |||
CI=confidence interval; DPP-4=dipeptidyl peptidase-4; GLP-1=glucagon-like peptide-1.
Discussion
Statement of principal findings
In this cohort study using three nationwide administrative claims databases in the United States, we found a lower rate of hyperkalemia in people with type 2 diabetes who started SGLT-2 inhibitors or GLP-1 receptor agonists compared with DPP-4 inhibitors. These observations were consistent in subgroups and several sensitivity analyses, and across comparisons of single agents within the SGLT-2 inhibitor and GLP-1 receptor agonist classes.
Novelty and comparison with previous studies
Our study provides several new findings and builds upon current evidence. An individual participant meta-analysis using data from six randomized clinical trials and comprising 49 875 patients found that SGLT-2 inhibitors reduced the risk of hyperkalemia compared with placebo.21 Our study provides additional evidence by extending these results to a broader group of >750 000 people with type 2 diabetes in routine clinical practice. Additionally, our study provides evidence of the association between GLP-1 receptor agonists and hyperkalemia, which has been lacking in large scale epidemiological studies or trial analyses. The relative rate reduction observed for GLP-1 receptor agonists versus DPP-4 inhibitors (21% reduction) was similar to the reduction observed for SGLT-2 inhibitors versus DPP-4 inhibitors (25% relative reduction in hazard). In head-to-head comparisons of SGLT-2 inhibitors versus GLP-1 receptor agonists, we only observed small differences (hazard ratio 0.92 in the primary analysis), and in several secondary and sensitivity analyses we observed no association. We interpret these findings to indicate that no large differences exist in the rate of hyperkalemia between SGLT-2 inhibitors and GLP-1 receptor agonists, although the subgroup with chronic kidney disease showed a larger effect size on the relative scale. However, these subgroup findings should be considered hypothesis generating and interpreted with caution because many subgroup analyses were performed. Finally, our large study population allowed us to investigate associations with a precision sufficient to exclude the presence of clinically meaningful treatment effect heterogeneity by relevant patient subgroups. We were also able to exclude the presence of large differences in the reduction of hyperkalemia risk across individual SGLT-2 inhibitor and GLP-1 receptor agonist agents compared with DPP-4 inhibitors.
Possible explanations and clinical implications
There are several potential mechanisms by which SGLT-2 inhibitors and GLP-1 receptor agonists might lower the risk of hyperkalemia. SGLT-2 inhibitors and GLP-1 receptor agonists could increase the delivery of sodium and water to the cortical collecting duct of the kidney. Increased absorption of sodium by the principal cells might increase the electronegative charge, leading to increased potassium secretion.25 26 41 42 A small randomized trial of 35 participants with type 2 diabetes showed increased fractional and absolute excretion of potassium after eight weeks of treatment with the GLP-1 receptor agonist lixisenatide.24 Furthermore, both drug classes have been shown to slow progression of kidney function decline and albuminuria, and the preserved kidney function might contribute to the prevention of hyperkalemia in the long term.43 44 45 46 47 48
Our findings have important clinical implications. Hyperkalemia is a common electrolyte disorder among patients with type 2 diabetes, especially in those with concurrent heart failure or decreased kidney function, and who use guideline recommended treatments that increase potassium levels, such as angiotensin converting enzyme inhibitors, angiotensin II receptor blockers, or mineralocorticoid receptor antagonists.10 The occurrence of hyperkalemia frequently leads to dose reduction or discontinuation of these drugs, and this discontinuation is associated with adverse cardiovascular and kidney outcomes.11 12 13 Although newer potassium binders such as patiromer and sodium zirconium cyclosilicate might allow the use of renin-angiotensin system inhibitors,49 50 51 they add to the pill burden, and their benefits on hard clinical outcomes are unknown. Identifying additional strategies that prevent hyperkalemia is therefore a key priority. Our findings suggest that SGLT-2 inhibitors and GLP-1 receptor agonists are associated with lower risk of hyperkalemia. This ancillary benefit further supports the use of SGLT-2 inhibitors and GLP-1 receptor agonists in people with type 2 diabetes.
Unanswered questions and future research
In our analyses, we focused on hyperkalemia as an outcome. A recent post hoc analysis of the CREDENCE (canagliflozin and renal events in diabetes with established nephropathy clinical evaluation) and DAPA-CKD (dapagliflozin and prevention of adverse outcomes in chronic kidney disease) trials found that SGLT-2 inhibitor use was associated with a lower rate of discontinuation of renin-angiotensin-aldosterone system inhibitors compared with placebo during follow-up in patients with albuminuric chronic kidney disease. Future studies should investigate whether these effects are also observed for GLP-1 receptor agonists, and whether this is mediated by a lower risk of hyperkalemia. Similarly, studies could investigate whether SGLT-2 inhibitors or GLP-1 receptor agonists have an effect on the use of loop diuretics.
Strengths and weaknesses of the study
The strengths of our study include its large sample size, more than 15-fold larger than the individual participant meta-analysis of randomized trials previously discussed,21 which allowed investigation of important subgroups and individual agents, and rich adjustment for >140 potential confounders. Furthermore, we applied rigorous methods, including the use of an active comparator and new user cohort design, which reduces confounding and mitigates time related and selection bias caused by prevalent users.52 53
Our study has several limitations. We cannot rule out the presence of unmeasured confounding. However, our analysis accounted for a wide set of confounders,53 and balance was achieved even among the laboratory test results that were not included in the adjustment. Furthermore, confounding by indication is less likely because hyperkalemia is an unintended effect of glucose lowering drugs and currently not an indication that would drive a choice of one of the three investigated drug classes.54 55 We also used a claims based definition for our primary outcome, with excellent specificity (>99%), but low sensitivity (22.3%). Therefore, although relative risk estimates are not expected to be biased under the assumption of non-differential measurement error, differences on the absolute scale are probably an underestimate of the true benefit of SGLT-2 inhibitors and GLP-1 receptor agonists. We believe non-differential measurement error might be a plausible assumption in our study because hyperkalemia has not been a safety concern for either of these drug classes. Furthermore, we adjusted for a wide number of measures of healthcare use (eg, number of outpatient visits and number of laboratory tests) to ensure patients were comparable at baseline with respect to healthcare surveillance and would have a similar opportunity for potassium monitoring during follow-up.
Mean follow-up in our study was relatively short (around eight to nine months) owing to high rates of treatment discontinuation. Nevertheless, this represents the reality of routine clinical practice in which many patients discontinue their treatment during follow-up. Therefore, our results reflect the outcomes that could be expected in patients from clinical practice after starting these drugs. We believe this timeframe should be sufficient to show the effects of GLP-1 receptor agonists and SGLT-2 inhibitors because mechanistic studies have found rapid effects of GLP-1 receptor agonists on potassium handling,24 25 and post hoc analyses of randomized trials of SGLT-2 inhibitors have shown separation of survival curves within one year for hyperkalemia.22 23 Finally, our findings are representative of the insured population in the United States, but might not be generalizable to uninsured patients.
Conclusion
In this analysis of three nationwide US databases, use of SGLT-2 inhibitors and GLP-1 receptor agonists was associated with a lower rate of hyperkalemia compared with DPP-4 inhibitors. This study further supports the use of these agents in a broad range of people with type 2 diabetes.
What is already known on this topic
Hyperkalemia is associated with increased mortality and limits the use of guideline recommended drugs such as renin-angiotensin system inhibitors among people with type 2 diabetes
Sodium-glucose cotransporter-2 (SGLT-2) inhibitors, glucagon-like peptide-1 (GLP-1) receptor agonists, and dipeptidyl peptidase-4 (DPP-4) inhibitors are increasingly being used in the treatment of type 2 diabetes
The comparative effectiveness of these drugs in preventing hyperkalemia in routine clinical practice is unclear
What this study adds
In this population based cohort study of people with type 2 diabetes in the United States, starting SGLT-2 inhibitors or GLP-1 receptor agonists was associated with a lower risk of hyperkalemia compared with DPP-4 inhibitors
Benefits were consistent among demographic and clinical subgroups, and among single agents within the SGLT-2 inhibitor and GLP-1 receptor agonist classes
In addition to improving cardiovascular and kidney outcomes, the potential benefit of preventing hyperkalemia further solidifies the use of SGLT-2 inhibitors and GLP-1 receptor agonists in people with type 2 diabetes
Acknowledgments
The authors thank Julianna Mastrorilli for help with Aetion and administrative support.
Web extra.
Extra material supplied by authors
Web appendix: Supplemental material
Contributors: Concept and design: ELF, EP. Acquisition, analysis of interpretation of data: all authors. Drafting of the manuscript: ELF. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: ELF. Administrative, technical or material support: all authors. Supervision: EP. EP is the guarantor.
Funding: This study was funded by the Division of Pharmacoepidemiology and Pharmacoeconomics, Department of Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA. ELF is supported by a Rubicon grant from the Netherlands Organization for Scientific Research. EP is supported by research grants from the Patient-Centered Outcomes Research Institute (DB-2020C2-20326) and the Food and Drug Administration (5U01FD007213). JMP is supported by a National Institute of Health grant AR 075117. KB is supported by a grant from the National Institute on Aging (K01AG068365). SJC is supported by the American Diabetes Association (grant No 7-21-JDFM-005). The funders had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare the following: support from Brigham and Women’s Hospital, Harvard Medical School, the Netherlands Organization for Scientific Research, Patient-Centered Outcomes Research Institute, Food and Drug Administration, National Institutes of Health, National Institute on Aging, American Diabetes Association for the submitted work. EP is principal investigator of an investigator initiated grant to the Brigham and Women’s Hospital from Boehringer Ingelheim, not directly related to the topic of the submitted work; DJW reports serving on data monitoring committees for Novo Nordisk not related to the topic of this work; SJC reports serving on advisory boards for Alexion Pharmaceuticals and employment of a family member by a Johnson and Johnson company. No other potential conflicts of interest relevant to this article were reported.
Transparency: The lead author (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: The authors intend to disseminate these results through social media, press releases, and their website (bwhpromise.org).
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Ethical approval
This study was approved by the Mass General Brigham institutional review board and granted waiver of informed consent since only deidentified claims data were used.
Data availability statement
A data use agreement is required for each of these data sources. These data use agreements do not permit the authors to share patient level source data or data derivatives with individuals and institutions not covered under the data use agreements. The databases used in this study are accessible to other researchers by contacting the data providers and acquiring data use agreements or licenses.
References
- 1. Nilsson E, Gasparini A, Ärnlöv J, et al. Incidence and determinants of hyperkalemia and hypokalemia in a large healthcare system. Int J Cardiol 2017;245:277-84. 10.1016/j.ijcard.2017.07.035 [DOI] [PubMed] [Google Scholar]
- 2. Humphrey T, Davids MR, Chothia MY, Pecoits-Filho R, Pollock C, James G. How common is hyperkalaemia? A systematic review and meta-analysis of the prevalence and incidence of hyperkalaemia reported in observational studies. Clin Kidney J 2021;15:727-37. 10.1093/ckj/sfab243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kovesdy CP, Matsushita K, Sang Y, et al. CKD Prognosis Consortium . Serum potassium and adverse outcomes across the range of kidney function: a CKD Prognosis Consortium meta-analysis. Eur Heart J 2018;39:1535-42. 10.1093/eurheartj/ehy100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Palmer BF. Managing hyperkalemia caused by inhibitors of the renin-angiotensin-aldosterone system. N Engl J Med 2004;351:585-92. 10.1056/NEJMra035279 [DOI] [PubMed] [Google Scholar]
- 5. Agarwal R, Joseph A, Anker SD, et al. FIDELIO-DKD Investigators . Hyperkalemia risk with finerenone: results from the FIDELIO-DKD trial. J Am Soc Nephrol 2022;33:225-37. 10.1681/ASN.2021070942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Juurlink DN, Mamdani MM, Lee DS, et al. Rates of hyperkalemia after publication of the Randomized Aldactone Evaluation Study. N Engl J Med 2004;351:543-51. 10.1056/NEJMoa040135 [DOI] [PubMed] [Google Scholar]
- 7. Fu EL, Kutz A, Desai RJ. Finerenone in chronic kidney disease and type 2 diabetes: the known and the unknown. Kidney Int 2023;103:30-3. 10.1016/j.kint.2022.09.012 [DOI] [PubMed] [Google Scholar]
- 8. Bandak G, Sang Y, Gasparini A, et al. Hyperkalemia after initiating renin-angiotensin system blockade: the Stockholm Creatinine Measurements (SCREAM) project. J Am Heart Assoc 2017;6:e005428. 10.1161/JAHA.116.005428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Desai AS, Swedberg K, McMurray JJ, et al. CHARM Program Investigators . Incidence and predictors of hyperkalemia in patients with heart failure: an analysis of the CHARM Program. J Am Coll Cardiol 2007;50:1959-66. 10.1016/j.jacc.2007.07.067 [DOI] [PubMed] [Google Scholar]
- 10. Clase CM, Carrero JJ, Ellison DH, et al. Conference Participants . Potassium homeostasis and management of dyskalemia in kidney diseases: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int 2020;97:42-61. 10.1016/j.kint.2019.09.018 [DOI] [PubMed] [Google Scholar]
- 11. Leon SJ, Whitlock R, Rigatto C, et al. Hyperkalemia-related discontinuation of renin-angiotensin-aldosterone system inhibitors and clinical outcomes in CKD: a population-based cohort Study. Am J Kidney Dis 2022;80:164-173.e1. 10.1053/j.ajkd.2022.01.002 [DOI] [PubMed] [Google Scholar]
- 12. Xu Y, Fu EL, Trevisan M, et al. Stopping renin-angiotensin system inhibitors after hyperkalemia and risk of adverse outcomes. Am Heart J 2022;243:177-86. 10.1016/j.ahj.2021.09.014 [DOI] [PubMed] [Google Scholar]
- 13. Trevisan M, Fu EL, Xu Y, et al. Stopping mineralocorticoid receptor antagonists after hyperkalaemia: trial emulation in data from routine care. Eur J Heart Fail 2021;23:1698-707. 10.1002/ejhf.2287 [DOI] [PubMed] [Google Scholar]
- 14. Leon SJ, Carrero JJ. Adverse effects during treatment with renin-angiotensin-aldosterone system inhibitors; should we stay or should we stop? Curr Opin Nephrol Hypertens 2023;32:290-6. 10.1097/MNH.0000000000000878 [DOI] [PubMed] [Google Scholar]
- 15. Lyu B, Sang Y, Selvin E, et al. Pharmacologic treatment of type 2 diabetes in the U.S., Sweden, and Israel. Diabetes Care 2022;45:2926-34. 10.2337/dc22-1253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Harris ST, Patorno E, Zhuo M, Kim SC, Paik JM. Prescribing trends of antidiabetes medications in patients with type 2 diabetes and diabetic kidney disease, a cohort study. Diabetes Care 2021;44:2293-301. 10.2337/dc21-0529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rossing P, Caramori ML, Chan JCN, et al. Executive summary of the KDIGO 2022 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease: an update based on rapidly emerging new evidence. Kidney Int 2022;102:990-9. 10.1016/j.kint.2022.06.013 [DOI] [PubMed] [Google Scholar]
- 18. ElSayed NA, Aleppo G, Aroda VR, et al. on behalf of the American Diabetes Association . 9. Pharmacologic approaches to glycemic treatment: standards of care in diabetes-2023. Diabetes Care 2023;46(Suppl 1):S140-57. 10.2337/dc23-S009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kaze AD, Zhuo M, Kim SC, Patorno E, Paik JM. Association of SGLT2 inhibitors with cardiovascular, kidney, and safety outcomes among patients with diabetic kidney disease: a meta-analysis. Cardiovasc Diabetol 2022;21:47. 10.1186/s12933-022-01476-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fu EL, Patorno E, Everett BM, et al. Sodium-glucose cotransporter 2 inhibitors vs. sitagliptin in heart failure and type 2 diabetes: an observational cohort study. Eur Heart J 2023;44:2216-30. 10.1093/eurheartj/ehad273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Neuen BL, Oshima M, Agarwal R, et al. Sodium-glucose cotransporter 2 inhibitors and risk of hyperkalemia in people with type 2 diabetes: a meta-analysis of individual participant data from randomized, controlled trials. Circulation 2022;145:1460-70. 10.1161/CIRCULATIONAHA.121.057736 [DOI] [PubMed] [Google Scholar]
- 22. Ferreira JP, Zannad F, Butler J, et al. Empagliflozin and serum potassium in heart failure: an analysis from EMPEROR-Pooled. Eur Heart J 2022;43:2984-93. 10.1093/eurheartj/ehac306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Neuen BL, Oshima M, Perkovic V, et al. Effects of canagliflozin on serum potassium in people with diabetes and chronic kidney disease: the CREDENCE trial. Eur Heart J 2021;42:4891-901. 10.1093/eurheartj/ehab497 [DOI] [PubMed] [Google Scholar]
- 24. Tonneijck L, Muskiet MHA, Blijdorp CJ, et al. Renal tubular effects of prolonged therapy with the GLP-1 receptor agonist lixisenatide in patients with type 2 diabetes mellitus. Am J Physiol Renal Physiol 2019;316:F231-40. 10.1152/ajprenal.00432.2018 [DOI] [PubMed] [Google Scholar]
- 25. Tonneijck L, Smits MM, Muskiet MHA, et al. Acute renal effects of the GLP-1 receptor agonist exenatide in overweight type 2 diabetes patients: a randomised, double-blind, placebo-controlled trial. Diabetologia 2016;59:1412-21. 10.1007/s00125-016-3938-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Palmer BF. Regulation of potassium homeostasis. Clin J Am Soc Nephrol 2015;10:1050-60. 10.2215/CJN.08580813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fu EL, Mastrorilli J, Bykov K, et al. A population-based cohort defined risk of hyperkalemia after initiating SGLT-2 inhibitors, GLP1 receptor agonists or DPP-4 inhibitors to patients with chronic kidney disease and type 2 diabetes. Kidney Int 2024;105:618-28. 10.1016/j.kint.2023.11.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lash TL, Fox MP, Fink AK. Applying Quantitative Bias Analysis to Epidemiologic Data. Springer, 2009. 10.1007/978-0-387-87959-8. [DOI] [Google Scholar]
- 29. Fu EL, D’Andrea E, Wexler DJ, Patorno E, Paik JM. Safety of sodium-glucose cotransporter-2 inhibitors in patients with CKD and type 2 diabetes: population-based US cohort study. Clin J Am Soc Nephrol 2023;18:592-601. 10.2215/CJN.0000000000000115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kim DH, Schneeweiss S, Glynn RJ, Lipsitz LA, Rockwood K, Avorn J. Measuring frailty in Medicare data: development and validation of a claims-based frailty index. J Gerontol A Biol Sci Med Sci 2018;73:980-7. 10.1093/gerona/glx229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol 2011;64:749-59. 10.1016/j.jclinepi.2010.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Inker LA, Eneanya ND, Coresh J, et al. Chronic Kidney Disease Epidemiology Collaboration . New creatinine- and cystatin c-based equations to estimate GFR without race. N Engl J Med 2021;385:1737-49. 10.1056/NEJMoa2102953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fu EL, Groenwold RHH, Zoccali C, Jager KJ, van Diepen M, Dekker FW. Merits and caveats of propensity scores to adjust for confounding. Nephrol Dial Transplant 2019;34:1629-35. 10.1093/ndt/gfy283 [DOI] [PubMed] [Google Scholar]
- 34. Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput 2009;38:1228-34 10.1080/03610910902859574. [DOI] [Google Scholar]
- 35. Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 2009;28:3083-107. 10.1002/sim.3697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Xu Y, Cheung YB, Lam KF, Tan SH, Milligan P. A simple approach to the estimation of incidence rate difference. Am J Epidemiol 2010;172:334-43. 10.1093/aje/kwq099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Putter H, Fiocco M, Geskus RB. Tutorial in biostatistics: competing risks and multi-state models. Stat Med 2007;26:2389-430. 10.1002/sim.2712 [DOI] [PubMed] [Google Scholar]
- 38.Evidence A. Platform® (2022). Software for real-world data analysis. Aetion, Inc. http://aetion.com.
- 39.A Resource Guide for Using Medicare’s Enrollment Race and Ethnicity Data OEI-02-21-00101 2023. https://oig.hhs.gov/oei/reports/OEI-02-21-00101.pdf.
- 40. Izem R, Liao J, Hu M, et al. Comparison of propensity score methods for pre-specified subgroup analysis with survival data. J Biopharm Stat 2020;30:734-51. 10.1080/10543406.2020.1730868 [DOI] [PubMed] [Google Scholar]
- 41. Wilcox CS. Antihypertensive and renal mechanisms of SGLT2 (sodium-glucose linked transporter 2) inhibitors. Hypertension 2020;75:894-901. 10.1161/HYPERTENSIONAHA.119.11684 [DOI] [PubMed] [Google Scholar]
- 42. Palmer BF, Clegg DJ. SGLT2 inhibition and kidney potassium homeostasis. Clin J Am Soc Nephrol 2024;19:399-405. 10.2215/CJN.0000000000000300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Xie Y, Bowe B, Gibson AK, et al. Comparative effectiveness of SGLT2 inhibitors, GLP-1 receptor agonists, DPP-4 inhibitors, and sulfonylureas on risk of kidney outcomes: emulation of a target trial using health care databases. Diabetes Care 2020;43:2859-69. 10.2337/dc20-1890 [DOI] [PubMed] [Google Scholar]
- 44. Xu Y, Fu EL, Clase CM, Mazhar F, Jardine MJ, Carrero JJ. GLP-1 receptor agonist versus DPP-4 inhibitor and kidney and cardiovascular outcomes in clinical practice in type-2 diabetes. Kidney Int 2022;101:360-8. 10.1016/j.kint.2021.10.033 [DOI] [PubMed] [Google Scholar]
- 45. Sattar N, Lee MMY, Kristensen SL, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of randomised trials. Lancet Diabetes Endocrinol 2021;9:653-62. 10.1016/S2213-8587(21)00203-5 [DOI] [PubMed] [Google Scholar]
- 46. Wanner C, Inzucchi SE, Lachin JM, et al. EMPA-REG OUTCOME Investigators . Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med 2016;375:323-34. 10.1056/NEJMoa1515920 [DOI] [PubMed] [Google Scholar]
- 47. Mosenzon O, Wiviott SD, Cahn A, et al. Effects of dapagliflozin on development and progression of kidney disease in patients with type 2 diabetes: an analysis from the DECLARE-TIMI 58 randomised trial. Lancet Diabetes Endocrinol 2019;7:606-17. 10.1016/S2213-8587(19)30180-9 [DOI] [PubMed] [Google Scholar]
- 48. Neal B, Perkovic V, Mahaffey KW, et al. CANVAS Program Collaborative Group . Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 2017;377:644-57. 10.1056/NEJMoa1611925 [DOI] [PubMed] [Google Scholar]
- 49. Butler J, Anker SD, Lund LH, et al. Patiromer for the management of hyperkalemia in heart failure with reduced ejection fraction: the DIAMOND trial. Eur Heart J 2022;43:4362-73. 10.1093/eurheartj/ehac401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Packham DK, Rasmussen HS, Lavin PT, et al. Sodium zirconium cyclosilicate in hyperkalemia. N Engl J Med 2015;372:222-31. 10.1056/NEJMoa1411487 [DOI] [PubMed] [Google Scholar]
- 51. Haller H, Bianchi S, McCafferty K, et al. Safety and efficacy of patiromer in hyperkalemic patients with CKD: a pooled analysis of three randomized trials. Kidney360 2022;3:2019-26. 10.34067/KID.0001562022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lund JL, Richardson DB, Stürmer T. The active comparator, new user study design in pharmacoepidemiology: historical foundations and contemporary application. Curr Epidemiol Rep 2015;2:221-8. 10.1007/s40471-015-0053-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Schneeweiss S, Patorno E. Conducting real-world evidence studies on the clinical outcomes of diabetes treatments. Endocr Rev 2021;42:658-90. 10.1210/endrev/bnab007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Vandenbroucke JP. Observational research, randomised trials, and two views of medical science. PLoS Med 2008;5:e67. 10.1371/journal.pmed.0050067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Fu EL. Target trial emulation to improve causal inference from observational data: what, why, and how? J Am Soc Nephrol 2023;34:1305-14. 10.1681/ASN.0000000000000152 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplemental material
Data Availability Statement
A data use agreement is required for each of these data sources. These data use agreements do not permit the authors to share patient level source data or data derivatives with individuals and institutions not covered under the data use agreements. The databases used in this study are accessible to other researchers by contacting the data providers and acquiring data use agreements or licenses.