Abstract
Refugees are an often understudied population and vulnerable to poor health outcomes. No large-scale analyses have evaluated the prevalence of overweight and obesity in US-bound refugees. Using data obtained from the Centers for Disease Control (CDC) Electronic Disease Notification system, we quantified the prevalence of overweight and obesity in adult US-bound refugees by nationality from 2009 through 2017. This repeated cross-sectional analysis used CDC data to quantify and examine body mass index (BMI) trends in US-bound adult refugees during 2009–2017. Utilizing data from an overseas medical exam required for all US-bound refugees, we determined BMI for 334,746 refugees ≥ 18 years old who arrived in the United States during January 1, 2009–December 31, 2017. We calculated and compared the prevalence of overweight and obesity as well as changes in demographic characteristics (age, sex, and nationality) by year. Adjusted prevalence and prevalence ratios (APR) for yearly trends were assessed using a modified Poisson regression model with robust error variances. After adjusting for age, sex, and nationality, we observed a significant linear trend in the prevalence of overweight/obesity with an average annual relative percent increase of 3% for refugees entering the United States from 2009 through 2017 (APR = 1.031; 95% CI 1.029–1.033). The adjusted prevalence of overweight/obesity increased from 35.7% in 2009 to 44.7% in 2017. The prevalence of overweight and obesity in US-bound refugees increased steadily over the analysis period. Investigation into pre-migration and post-resettlement interventions is warranted.
Keywords: Obesity, Overweight, Refugee, Refugee populations
Introduction
The US government has resettled over 3 million refugees since 1975. Refugees come from a growing pool of forcibly displaced individuals worldwide who have fled prolonged conflicts, civil unrest, or persecution in their home countries. Before resettlement, a refugee may live years in a temporary settlement in their country of first asylum, usually a country near their country of origin [1]. Approximately 80% of the world’s refugees are currently hosted by low- and middle-income countries [1], which may be strained by the rapid influx of population seen when a bordering nation is engaged in mass conflict. Most refugees now live in urban areas instead of camps [2], a change that has been driven by demographic transition, prolonged conflicts, and increasing urbanization [1]. With the changing demographic profiles of conflict-affected populations, a shift in the burden of disease has been observed, with non-communicable diseases (NCD) becoming more prevalent and accounting for much of the morbidity and mortality in refugee populations [2].
Overweight and obesity are known risk factors for a multitude of NCDs [3, 4] and have been increasing in prevalence around the world. Body Mass Index (BMI) has increased globally as a consequence of the global nutrition transition [5−8], characterized by the increased intake of energy-dense, highly processed foods [7, 8] and driven by rising incomes [4], trade liberalization, marketing by transnational food and beverage corporations, changing labor markets, and urbanization [4, 7, 9].
Large-scale studies have reported on an increase in the prevalence in overweight and obesity in most countries of the world [10, 11]. Several recent large studies have characterized the prevalence of obesity in specific groups of refugees before they migrate [12, 13]. Several other studies have examined the prevalence of obesity in refugees originating from specific countries immediately after resettlement in the United States. However, there is a paucity of data systematically collected on refugee risks for NCDs before resettlement. Refugees are an understudied population at risk for poor health outcomes, and to the authors’ knowledge, there have been no previous investigations evaluating the BMI trends of all adult refugees accepted for resettlement in the United States. Our objective was to quantify and examine trends in BMI in adult refugees who arrived in the United States between 2009 and 2017.
Methods
US regulations require all refugees being considered for resettlement in the United States to be evaluated during an overseas medical examination in accordance with the Centers for Disease Control and Prevention (CDC) Technical Instructions [14]. The exam is completed by panel physicians (medical doctors practicing overseas who are appointed by the local US embassy or consulate). All refugee data are entered in CDC’s Electronic Disease Notification (EDN) system, a reporting system used to collect health information on US-bound refugees and notify state health departments when refugees arrive in their jurisdiction [15]. From EDN, we obtained de-identified height, weight, and demographic information for all refugees ≥ 18 years (N = 358,030) who arrived in the United States between January 1, 2009, and December 31, 2017. In this manuscript, we include as “refugees” all persons who entered the United States under a status eligible for Office of Refugee Resettlement services including all refugees, and certain parolees, asylees, and Iraqis and Afghans with Special Immigrant Visas (SIV) [16] (n = 334,746). This evaluation was reviewed by a CDC human subjects advisor and determined to be non-research, and it qualified for non-research exemption from the Institutional Review Board of Saint Louis University. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of CDC.
BMI Definitions and Analysis Variables
Height and weight measurements obtained during the overseas medical exam were used to calculate BMI for all subjects. The BMI was calculated from an individual’s weight in kilograms divided by height in meters squared (kg/m2). World Health Organization BMI categories were used to define overweight (BMI 25.0 to < 30.0) and obesity (BMI ≥ 30.0) [17]. Pregnant women (N = 4189) and individuals with improbable height (< 1.4 m for men and women; > 2.0 m for men and > 1.9 m for women) [18] or weight (< 40 kg for men and < 35 kg for women; > 136 kg for men and women) [18] (N = 8744) were excluded, as were individuals with missing height or weight (N = 10,351) leaving an analytic sample of 334,746. Demographic characteristics included gender, age at arrival, year of arrival, and nationality.
Data Analysis
This repeated cross-section analysis was conducted using SAS v9.4 (SAS Institute, Cary, NC) at an alpha of 0.05. Overall sample characteristics of refugees entering the United States from 2009 through 2017 were calculated with frequencies or means with standard deviations where appropriate. Bivariate analyses assessed differences in demographics and overweight/obese prevalence by year using chi-square tests. A bivariate analysis also compared differences in overweight/obesity prevalence by nationality using a chi-square test. Prevalence and adjusted prevalence ratios (APR) for yearly trends in overweight/obesity were calculated using a modified Poisson regression model with robust error variances after adjusting for age, gender, nationality, and year as a categorical variable. Using the same model with year as a numerical variable, we also assessed for a yearly linear trend with a likelihood ratio test and calculated an average yearly APR.
Results
Table 1 shows that about 54% of adult refugees entering the United States from 2009 through 2017 were men under 40 years of age. Iraqi (22.7%) and Burmese (22.2%) were the most common nationalities. Overall average BMI was 24.5 (± 5.2). Nearly 40% of refugees were overweight (25.4%) or had obesity (14.1%). Only 8.2% of adult refugees migrating to the United States were underweight by BMI classification.
Table 1.
Sample characteristics for adult refugees entering the United States 2009–2017 (n = 334,746)
| Variable | N (%) or mean (± SD) |
|---|---|
| US arrival year | |
| 2009 | 41,483 (12.4%) |
| 2010 | 40,000 (11.9%) |
| 2011 | 30,562 (9.1%) |
| 2012 | 40,571 (12.1%) |
| 2013 | 37,159 (11.1%) |
| 2014 | 41,347 (12.4%) |
| 2015 | 35,065 (10.5%) |
| 2016 | 45,744 (13.7%) |
| 2017 | 22,815 (6.8%) |
| Sex | |
| Female | 153,853 (46.0%) |
| Male | 180,893 (54.0%) |
| Age category (years) | |
| 18–29 | 143,535 (42.9%) |
| 30–39 | 87,963 (26.3%) |
| 40–49 | 51,072 (15.3%) |
| 50–59 | 28,088 (8.4%) |
| 60–69 | 16,050 (4.8%) |
| ≥ 70 | 8038 (2.4%) |
| Nationality | |
| Afghanistan | 10,060 (3.0%) |
| Bhutan | 55,708 (16.6%) |
| Burma | 74,275 (22.2%) |
| Burundi | 1698 (0.5%) |
| Dem. Rep Congo | 21,213 (6.3%) |
| Cuba | 12,248 (3.7%) |
| Eritrea | 10,055 (3.0%) |
| Ethiopia | 3793 (1.1%) |
| Iran | 20,110 (6.0%) |
| Iraq | 76,102 (22.7%) |
| Somalia | 28,116 (8.4%) |
| Sudan | 5707 (1.7%) |
| Syria | 9045 (2.7%) |
| Ukraine | 6616 (2.0%) |
| BMI, mean (± SD) (kg/m2) | 24.5 (± 5.2) |
| BMI category | |
| Underweight (< 18.5) | 27,349 (8.2%) |
| Normal (18.5 to < 25.0) | 175,169 (52.3%) |
| Overweight (25.0 to < 30.0) | 84,975 (25.4%) |
| Obese (≥ 30.0) | 47,253 (14.1%) |
Adults, non-pregnant women; removed extreme height and weight and missing values for Body Mass Index (BMI)
SD standard deviation
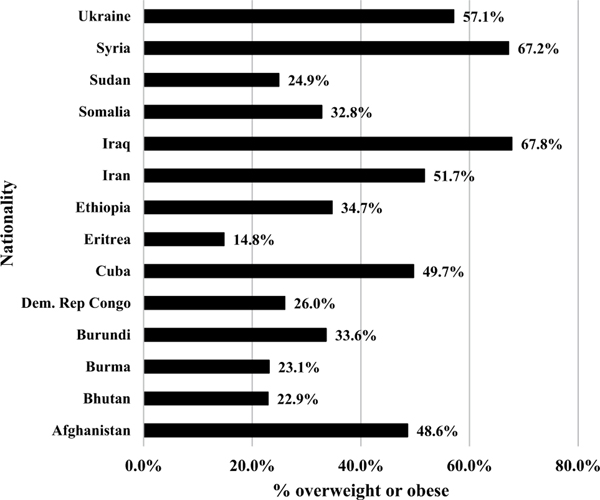
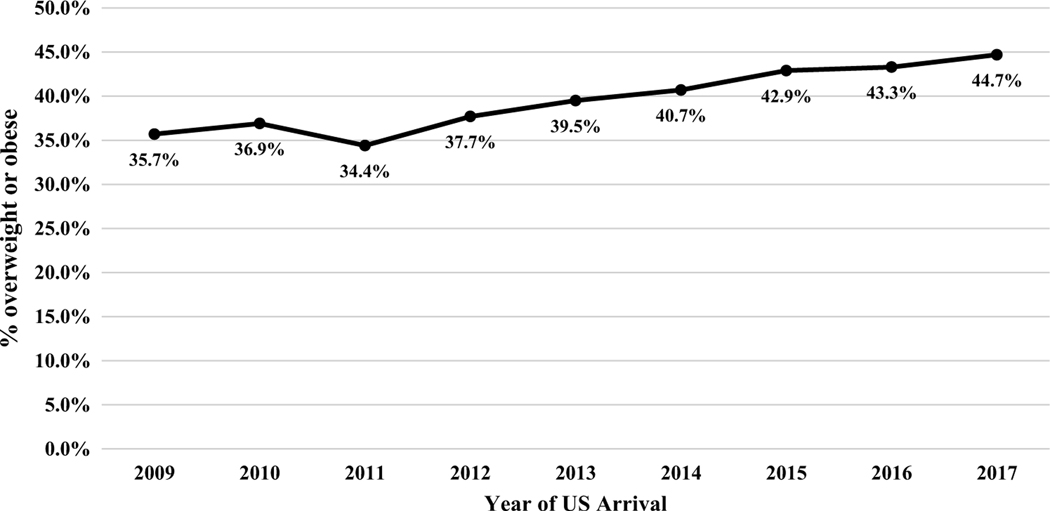
Table 2 shows differences in BMI and demographic characteristics by year. The unadjusted prevalence of overweight/obesity was approximately 36% up to 2012 but increased to over 40% after 2012, with 47.3% of incoming refugees classified as overweight or having obesity in 2017 (p < 0.0001). Mean age and proportion female varied significantly by year. The composition of refugee nationality changed from 2009 to 2017, such that the percentage of African refugees increased while the percentage of refugees from the Near East and south/central Asia decreased, with the exception of 2017, when Afghan refugees (including SIVs) made up the greatest percentage of refugees resettled in the United States. Figure 1 shows significant differences in the prevalence of overweight/obesity by country; Iraq (67.8%) and Syria (67.2%) had the highest prevalence, while Eritrea at 14.8% had the lowest prevalence of adults with overweight or obesity. Table 3 and Fig. 2 show results of the adjusted Poisson regression model. Adjusted prevalence of overweight/obesity increased from 35.7 to 44.7% from 2009 to 2017 (see Fig. 2) after adjusting for age, gender, and nationality. Compared to 2009, all years except for 2011 showed a significant increase in the prevalence of overweight/obesity in a stepwise fashion (APR range 1.04 to 1.26). Test for linear trend was significant, and average annual percent increase in the prevalence of overweight/obesity was 3% (APR = 1.031; 95% CI 1.029–1.033). The greatest average annual percent change (AAPC) in overweight/obesity was demonstrated in adult refugee populations originating from Bhutan and Burundi (see Table 4).
Table 2.
Demographic and overweight/obesity differences by year, adult refugees entering the United States 2009–2017 (n = 334,746)
| % | 2009 (n = 41,483) (%) | 2010 (n = 40,000) (%) | 2011 (n = 30,562) (%) | 2012 (n = 40,571) (%) | 2013 (n = 37,159) (%) | 2014 (n = 41,347) (%) | 2015 (n = 35,065) (%) | 2016 (n = 45,744) (%) | 2017 (n = 22,815) (%) | P-value1 |
|---|---|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||||
| Female | 47.0 | 45.0 | 45.7 | 43.2 | 44.0 | 46.1 | 46.4 | 48.2 | 48.6 | < 0.0001 |
| Male | 53.0 | 55.0 | 54.3 | 56.8 | 56.0 | 53.9 | 53.6 | 51.8 | 51.4 | |
| Age category (years) | ||||||||||
| 18–29 | 42.6 | 44.3 | 46.8 | 44.6 | 41.8 | 41.3 | 41.6 | 41.1 | 42.6 | |
| 30–39 | 24.9 | 25.1 | 24.0 | 25.1 | 25.6 | 25.7 | 28.2 | 28.7 | 30.3 | |
| 40–49 | 15.7 | 15.0 | 14.1 | 14.9 | 16.0 | 15.7 | 15.4 | 15.7 | 13.8 | < 0.0001 |
| 50–59 | 8.6 | 8.3 | 7.9 | 8.3 | 8.9 | 9.1 | 8.2 | 8.2 | 7.6 | |
| 60–69 | 5.3 | 4.9 | 4.8 | 4.7 | 5.1 | 5.4 | 4.3 | 4.4 | 3.8 | |
| ≥ 70 | 2.9 | 2.5 | 2.4 | 2.4 | 2.6 | 2.8 | 2.2 | 1.9 | 1.8 | |
| Nationality | ||||||||||
| Afghanistan | 0.4 | 0.7 | 0.7 | 0.7 | 0.9 | 0.9 | 1.6 | 3.6 | 27.2 | |
| Bhutan | 22.5 | 19.4 | 31.6 | 23.4 | 15.6 | 11.8 | 10.1 | 7.2 | 8.4 | |
| Burma | 24.7 | 23.4 | 29.7 | 23.6 | 23.0 | 22.6 | 28.4 | 13.5 | 8.6 | |
| Burundi | 0.5 | 0.6 | 0.2 | 0.2 | 0.2 | 0.2 | 1.6 | 0.8 | 0.3 | |
| Dem. Rep. Congo | 0.9 | 3.3 | 1.8 | 2.3 | 3.2 | 5.7 | 10.7 | 18.2 | 10.6 | < 0.0001 |
| Cuba | 6.0 | 5.7 | 3.4 | 4.0 | 5.6 | 5.0 | 1.4 | 0.3 | 0.1 | |
| Eritrea | 2.3 | 4.8 | 4.6 | 3.4 | 2.0 | 1.6 | 2.3 | 2.4 | 4.7 | |
| Ethiopia | 0.6 | 1.1 | 1.3 | 1.3 | 1.2 | 0.9 | 1.1 | 1.7 | 1.2 | |
| Iran | 9.1 | 5.5 | 5.4 | 3.9 | 5.1 | 5.7 | 6.8 | 6.8 | 5.1 | |
| Iraq | 27.0 | 28.6 | 13.5 | 25.8 | 29.0 | 31.0 | 17.3 | 14.1 | 12.0 | |
| Somalia | 4.0 | 5.5 | 6.0 | 8.3 | 10.6 | 12.0 | 10.7 | 11.1 | 5.8 | |
| Sudan | 0.9 | 0.7 | 0.8 | 2.4 | 3.3 | 1.2 | 2.4 | 1.9 | 1.6 | |
| Syria | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.3 | 2.8 | 13.9 | 6.3 | |
| Ukraine | 0.9 | 0.7 | 0.9 | 0.5 | 0.3 | 1.0 | 2.9 | 4.6 | 8.1 | |
| Overweight/obese2 | 36.4 | 37.2 | 28.3 | 36.3 | 41.0 | 43.7 | 40.6 | 44.8 | 47.3 | < 0.0001 |
Adults, non-pregnant women; removed extreme height and weight and missing values for body mass index (BMI)
Chi-square test
Overweight (BMI 25.0 to < 30.0) obese (BMI ≥ 30) thus overweight/obese refers to subjects with BMI ≥ 25
Fig. 1.
Prevalence of overweight/obesity among adult refugees entering the United States 2009–2017, by nationality. Chi-square test for independence, p < 0.0001. Overweight (BMI 25.0 to < 30.0) obese (BMI ≥ 30)
Table 3.
Adjusted Poisson regression model of overweight/obesity among adult refugees entering the United States 2009–2017 using robust variances (n = 334,746)
| Year | APR (95% CI) |
|---|---|
| 2009 | 1.00 |
| 2010 | 1.04 (1.02–1.05) |
| 2011 | 0.96 (0.95–0.98) |
| 2012 | 1.06 (1.04–1.07) |
| 2013 | 1.11 (1.09–1.13) |
| 2014 | 1.14 (1.12–1.16) |
| 2015 | 1.20 (1.18–1.22) |
| 2016 | 1.21 (1.19–1.23) |
| 2017 | 1.26 (1.23–1.28) |
| Linear trend1 | 1.031 (1.029–1.033) |
Model adjusted for age, sex, and nationality
Overweight (BMI 25.0 to < 30.0) obese (BMI ≥ 30)
APR adjusted prevalence ratios, CI confidence intervals
p-value for likelihood ratio test of linear trend, p < 0.0001. Represents average percent change (APC) per year
Fig. 2.
Adjusted prevalence of overweight/obesity among adult refugees entering the United States 2009–2017, across years. Prevalence adjusted for yearly differences in age, sex, and nationality. Overweight (BMI 25.0 to < 30.0) obese (BMI ≥ 30)
Table 4.
Adjusted prevalence and average annual percent change (AAPC) in overweight/obesity among adult refugees entering the United States 2009–2017, by nationality (n = 334,746)
| 2009 (%) | 2010 (%) | 2011 (%) | 2012 (%) | 2013 (%) | 2014 (%) | 2015 (%) | 2016 (%) | 2017 (%) | AAPC (%) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Country1 | ||||||||||
| Afghanistan | 47.0 | 47.5 | 53.0 | 51.3 | 51.2 | 43.7 | 48.6 | 47.5 | 61.4 | 4.1 |
| Bhutan | 17.4 | 17.1 | 16.9 | 21.4 | 24.5 | 18.1 | 31.6 | 38.1 | 38.7 | 13.6 |
| Burma | 20.0 | 19.5 | 20.3 | 21.6 | 23.1 | 26.4 | 29.2 | 27.7 | 28.7 | 4.8 |
| Burundi | 20.9 | 30.2 | 32.7 | 36.1 | 29.4 | 41.3 | 23.3 | 23.6 | 36.8 | 12.3 |
| Dem. Rep. Congo | 26.3 | 28.3 | 23.3 | 25.8 | 25.6 | 20.7 | 24.2 | 25.1 | 25.7 | 0.5 |
| Cuba | 44.4 | 49.2 | 47.2 | 49.0 | 51.1 | 48.8 | 49.1 | 56.9 | 57.6 | 3.5 |
| Eritrea | 15.3 | 14.8 | 17.9 | 19.2 | 23.0 | 22.6 | 25.9 | 29.5 | 24.3 | 6.7 |
| Ethiopia | 32.9 | 42.6 | 36.1 | 41.2 | 40.9 | 37.0 | 40.5 | 37.5 | 33.7 | 1.3 |
| Iran | 56.9 | 57.3 | 54.2 | 54.7 | 51.4 | 53.6 | 55.8 | 58.2 | 60.0 | 0.7 |
| Iraq | 71.7 | 74.4 | 71.9 | 72.9 | 74.4 | 75.7 | 75.2 | 77.7 | 74.4 | 0.5 |
| Somalia | 24.7 | 28.4 | 26.4 | 32.7 | 37.6 | 35.8 | 37.7 | 37.0 | 37.6 | 5.9 |
| Sudan | 22.9 | 36.8 | 28.5 | 27.4 | 31.9 | 32.9 | 27.8 | 34.8 | 28.1 | 5.5 |
| Syria | 79.6 | 77.8 | 83.5 | 69.8 | 53.2 | 71.5 | 72.8 | 74.7 | 73.0 | 0.2 |
| Ukraine | 63.9 | 61.7 | 57.9 | 63.7 | 56.3 | 67.4 | 64.3 | 65.1 | 67.8 | 1.2 |
Overweight (BMI 25.0 to < 30.0) obese (BMI ≥ 30)
AAPC geometric average of each year-to-year percent change from 2009 to 2017
Country-specific prevalence adjusted by age, sex
Discussion
In a sample of 334,746 US-bound adult refugees examined during 2009–2017, we observed a significant steady increase in the prevalence of overweight/obesity measured within 6 months before resettlement, after adjusting for age, sex, and nationality. Our adjusted prevalence of overweight/obesity in 2013 (39.5%) was comparable to the estimated worldwide proportion of overweight/obesity (36.9% in males and 38.0% in females) reported by the Global Burden of Disease Study in 2013 [11]. The prevalence of overweight/obesity in all United States-bound refugees during 2009–2017 was still significantly lower than the prevalence of overweight/obesity in adult residents of the United States (68% in 201,311), though refugees originating from Iraq and Syria demonstrated similar rates of overweight and obesity to the US population. The results of this analysis are consistent with other reports of increasing obesity prevalence in pre-migration US-bound refugees using overseas medical exam data [12, 13]. Although these findings may reflect conditions associated with displacement, such as elevated stress exposures, declines in physical activity following work restrictions or urbanization, or increased income to buy food due to remittances sent by already-resettled family members, they are also consistent with a global increase in BMI, especially in low-income countries, for which changes to the global food system are considered a major driver [4, 10].
Elevated BMI is a well-documented risk factor for the development of multiple chronic diseases including cardiovascular disease, renal disease, type 2 diabetes, musculoskeletal diseases, and some cancers [10]. Elevated BMI (> 25) was responsible for 4 million deaths globally in 2015, but only 60% of those people had obesity [10]. The increased burden of pre-migration overweight and obesity has implications on the health of refugees after they resettle in the United States. Refugees have been reported to gain weight after resettlement, which further increases their risk for non-communicable diseases.
Several studies have demonstrated a high prevalence of non-communicable diseases in pre- [12, 13] and post-resettlement refugees [19, 20]. Rhodes et al. [21] demonstrated that an African refugee population developed significant increases in BMI 1 and 5 years after resettlement. In addition to elevated BMI, these refugees had increasing rates of diabetes and hypertension [22]. A longitudinal study found only 2.5% of refugees had diabetes shortly after migrating to the United States, but odds of incident hypertension and type 2 diabetes increased with longer duration of residence in the United States [23].
Limitations
This investigation had several limitations. We do not know how long US-bound refugees in this analysis lived in a country of temporary asylum prior to undergoing their overseas medical examination, or whether duration of asylum affected BMI. Additionally, before 2017, medical examination data for SIVs were not systematically added to EDN; thus their information was included only for 2017. Finally, we used standard WHO BMI guidelines in reporting our results; estimated prevalence of overweight and obesity in the south and eastern Asian populations would be higher using Asian BMI cutoffs [24] (BMI 23–27.5 overweight, > 27.5 obesity).
Conclusion
This investigation provides evidence that the consideration of malnutrition in US-bound refugees should include over-nutrition in addition to undernutrition. The increasing prevalence of overweight/obesity in refugees before they migrate to the United States, mirroring global trends, increasingly places them at risk for the development of NCDs. Chronic illness and poor outcomes may be reduced with weight loss interventions after resettlement. Additional research on interventions that meet the unique needs of refugees pre- and post-migration is warranted.
Footnotes
Compliance with Ethical Standards
Ethical Approval This evaluation was reviewed by a CDC human subjects advisor and determined to be non-research, and it qualified for non-research exemption from the Institutional Review Board of Saint Louis University.
Conflict of interest The authors report no conflict of interest.
Informed Consent Informed consent was not required due to non-research exemption.
References
- 1.Guterres A, Spiegel P. The state of the world’s refugees: adapting health responses to urban environments. JAMA. 2012;308(7):673–4. [DOI] [PubMed] [Google Scholar]
- 2.Spiegel P, Checchi F, Colombo S, Paik E. Health care needs of peoples affected by conflict: future trends and changing frameworks. Lancet (London, England). 2010;375:341–5. [DOI] [PubMed] [Google Scholar]
- 3.Bovet P, Chiolero A, Gedeon J. Health effects of overweight and obesity in 195 countries. N Engl J Med. 2017;377(15):1495–6. [DOI] [PubMed] [Google Scholar]
- 4.Swinburn BA, Sacks G, Hall KD, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet (London, England). 2011;378(9793):804–14. [DOI] [PubMed] [Google Scholar]
- 5.Popkin BM, Gordon-Larsen P. The nutrition transition: worldwide obesity dynamics and their determinants. Int J Obes Relat Metab Disord. 2004;28(Suppl 3):S2–9. [DOI] [PubMed] [Google Scholar]
- 6.Popkin BM, Slining MM. New dynamics in global obesity facing low- and middle-income countries. Obes Rev. 2013;14(Suppl 2):11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baker P, Friel S. Food systems transformations, ultra-processed food markets and the nutrition transition in Asia. Glob Health. 2016;12(1):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Popkin BM. Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. Am J Clin Nutr. 2006;84(2):289–98. [DOI] [PubMed] [Google Scholar]
- 9.Nandi A, Sweet E, Kawachi I, Heymann J, Galea S. Associations between macrolevel economic factors and weight distributions in low- and middle-income countries: a multilevel analysis of 200,000 adults in 40 countries. Am J Public Health. 2014;104(2):e162–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Afshin A, Forouzanfar MH, Reitsma MB, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of disease study 2013. Lancet (London, England). 2014;384(9945):766–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bardenheier BH, Phares CR, Simpson D, et al. Trends in chronic diseases reported by refugees originating from burma resettling to the united states from camps versus urban areas during 2009– 2016. J Immigr Minor Health. 2018;21:246. [DOI] [PubMed] [Google Scholar]
- 13.Yanni EA, Naoum M, Odeh N, Han P, Coleman M, Burke H. The health profile and chronic diseases comorbidities of US-bound Iraqi refugees screened by the international organization for migration in Jordan: 2007–2009. J Immigr Minor Health/Center Minor Public Health. 2013;15(1):1–9. [DOI] [PubMed] [Google Scholar]
- 14.Prevention CfDCa. Technical instructions for panel physicians and civil surgeons. https://www.cdc.gov/immigrantrefugeehealth/exams/ti/panel/technical-instructions-panel-physicians.html. Accessed 10 July 2017.
- 15.Lee D, Philen R, Wang Z, et al. Disease surveillance among newly arriving refugees and immigrants—electronic disease notification system, United States, 2009. Morb Mortal Wkly Rep Surveill Summ (Washington, DC: 2002). 2013;62(7):1–20. [PubMed] [Google Scholar]
- 16.Office of Refugee Resettlement. Status and documentation requirements for the orr refugee resettlement program 2015; 2018. https://www.acf.hhs.gov/orr/resource/status-and-documentation-requirements-for-the-orr-refugee-resettlement-program. Accessed 21 Aug 2018.
- 17.Organization TWH. Obesity and overweight. The World Health Organization; 2015. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 21 Aug 2018.
- 18.Benoit SR, Gregg EW, Zhou W, Painter JA. Diabetes among United States-bound adult refugees, 2009–2014. J Immigr Minor Health. 2016;18:1357. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen MT, Rehkopf DH. Prevalence of chronic disease and their risk factors among Iranian, Ukrainian, Vietnamese refugees in California, 2002–2011. J Immigr Minor Health/Center Minor Public Health. 2015;18:1274. [DOI] [PubMed] [Google Scholar]
- 20.Yun K, Hebrank K, Graber LK, Sullivan MC, Chen I, Gupta J. High prevalence of chronic non-communicable conditions among adult refugees: implications for practice and policy. J Community Health. 2012;37(5):1110–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rhodes CM, Chang Y, Percac-Lima S. Development of obesity and related diseases in African refugees after resettlement to United States. J Immigrant and Minority Health. 2016;18:1386–91. [DOI] [PubMed] [Google Scholar]
- 22.Berkowitz SA, Fabreau GE, Raghavan S, et al. Risk of developing diabetes among refugees and immigrants: a longitudinal analysis. J Community Health. 2016;41:1274. [DOI] [PubMed] [Google Scholar]
- 23.Golub N, Seplaki C, Stockman D, Thevenet-Morrison K, Fernandez D, Fisher S. Impact of length of residence in the United States on risk of diabetes and hypertension in resettled refugees. J Immigr Minor Health/Center Minor Public Health. 2017;20:296. [DOI] [PubMed] [Google Scholar]
- 24.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet (London, England). 2004;363(9403):157–63. [DOI] [PubMed] [Google Scholar]