Abstract
Background
Sleep distrurbances involves daytime preoccupation about sleep, which plays a critical role in perpetuating sleep disturbances. Recent cognitive models highlight the importance of daytime processes, like processing sleep-related information and interpretations during waking hours, in influencing sleep quality and quantity. The Sleep Preoccupation Scale (SPS) quantifies this daytime cognitive activity related to sleep. This study aimed to translate and validate an Arabic version of the SPS for assessing sleep preoccupation among Arabic speakers.
Methods
523 Arabic speakers (mean age 23.6 years, 75% female) from four countries completed the Arabic SPS alongside the Athens Insomnia Scale, Generalized Anxiety Disorder-7 Scale, and the Anxiety and Preoccupation about Sleep Questionnaire (APSQ). The sample repeated the SPS after two weeks for test-retest reliability. Confirmatory factor analysis evaluated the SPS’s two-factor structure. Internal consistency, item response theory, and convergent validity with the other scales were examined.
Results
Confirmatory factor analysis supported the two-factor model’s fit. Measurement invariance results suggest that the SPS exhibits a similar basic factor structure across both insomnia and non-insomnia groups. The Arabic SPS demonstrated good internal consistency (Cronbach’s α = 0.92, McDonald’s ω = 0.92) and two-way mixed effects, consistency, single rater/measurement intraclass correlation coefficient (ICC) test-retest reliability (ICC = 0.95). Most items exhibited satisfactory item response theory fit statistics and discrimination. The SPS total score showed strong positive correlations with insomnia severity (r = 0.48, p < 0.001), generalized anxiety (r = 0.57, p < 0.001), and sleep-related anxiety/preoccupation (r = 0.79, p < 0.001), demonstrating convergent validity.
Conclusion
The Arabic version of the SPS demonstrated good psychometric properties and validity, supporting its use for assessing sleep preoccupation among Arabic speakers. This culturally-adapted version enhances sleep assessment capabilities for improving insomnia understanding and treatment within Arabic-speaking populations.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40359-024-02038-4.
Keywords: Harvey’s cognitive model, Insomnia, Reliability, Sleep disturbances
Introduction
Sleep disturbances can have a detrimental effect on one’s health [1], general functioning [2], and quality of life [3]. Early research focused predominantly on nighttime aspects in the development and maintenance of sleep distrubrances [4, 5]. Recent advancements in cognitive models highlighted the critical role of daytime processes in perpetuating sleep disturbances [6]. Allison G. Harvey emphasized that daytime processes are as important as nighttime processes in influencing the perceived and actual quality, quantity, and timing of sleep episodes [5]. This shift in perspective underscores the need to explore how individuals process and interpret information during waking hours, particularly as it relates to their sleep patterns [4].
Studies examining the types of daytime preoccupation that individuals with poor sleep experience further contributed to the conceptualization of sleep preoccupation [7, 8]. These investigations revealed that poor sleepers often experience daytime preoccupation related to the physical after-effects of poor sleep, disruptions to functioning, anxiety about sleep patterns, and feelings of fatigue and distress [7, 8]. The negative power of these daytime preoccupations distinguished them from neutral or positively valenced thoughts typically reported during nocturnal rumination [5].
Understanding and measuring sleep preoccupation is essential in the field of sleep medicine for several reasons [9]. First, studies have shown that daytime factors play a significant role in the development and maintenance of insomnia [4, 5]. Addressing these daytime processes, including sleep preoccupation, is crucial for effective intervention and treatment strategies [4, 9]. By quantifying and assessing sleep-related daytime processing, healthcare providers can tailor interventions to target cognitive processes that contribute to poor sleep outcomes [7].
As a result of these findings and the recognition of the impact of daytime processes on sleep outcomes, researchers sought to develop a standardized measure to assess sleep-related daytime processing. The creation of the Sleep Preoccupation Scale (SPS) in 2006–2007 as a self-report measure aimed to provide a reliable and valid tool for quantifying levels of sleep preoccupation and discriminating between different sleeper groups [7]. The SPS has since become instrumental in capturing the cognitive and affective dimensions of sleep preoccupation, shedding light on the importance of addressing daytime factors in the management of sleep disturbances [7].
The translation of assessment tools, such as the SPS, into different languages, including Arabic, is paramount for ensuring the global relevance and applicability of these measures. Arabic-speaking populations represent a diverse and significant portion of the world’s population, yet there is a scarcity of validated tools in Arabic for assessing sleep-related daytime processing. Cultural issues and language differences may influence individuals’ expressions of sleep-related thoughts and feelings, underscoring the importance of linguistic and cultural adaptation of assessment instruments.
Therefore, this research aims to emphasize the importance of investigating sleep preoccupation in the context of sleep medicine and advocates for the translation of the SPS into Arabic. By expanding the reach of this valuable tool, researchers and healthcare providers can gain insights into the role of daytime processes in sleep disturbances among Arabic-speaking populations. This translation effort holds the potential to enhance the diagnosis, treatment, and overall management of sleep disorders in Arabic-speaking communities, ultimately improving health outcomes and quality of life in this population.
Method
Translation procedure
The objective of this study was to translate the original SPS questionnaire into Arabic and validate it. To translate and validate the scale in Arabic in November 2023, formal consent was first obtained from the developers (Dr. Jason Ellis) via email.
We used a forward-backward translation technique to translate the questionnaire using the guidelines outlined by the international test commission [10]. First, HG and HJ (two study research team members) forward-translated the SPS from English into Modern Standard Arabic, aka Fusha Arabic. Next, the Arabic version was independently backward-translated back into English by a linguist of considerable experience [who is also a member of the study team (ZS)].
Two research team members (WI, SA) evaluated the linguist’s back-translated English version with the original English version of the SPS to verify its accuracy and equivalency. Based on this comparison, any necessary changes were made to the Arabic version. To validate the use of the scale in Arabic-speaking populations, the psychometric qualities of the final translated Arabic version of the SPS, including its validity and reliability, were subsequently assessed in a sample of individuals [11]. Supplementary Material 1 contains the translated Arabic version, whereas other sources offer the original English form [7].
Ethics
The study adhered to ethical principles from the Helsinki Declaration and its amendments. The research was reviewed and approved by the University of Jordan’s Research Committee. Participation was voluntary (Code: REC/HG/23/475/SPS, Date: 25 January 2024). Participants could withdraw at any time without penalty. All participants were adults aged 18 years or older.
Data collection
The Arabic versions of the SPS scale questionnaire were distributed in this study via a variety of social media channels to Arab nations, including Bahrain, Jordan, Saudi Arabia, and Tunisia. In addition to instant messaging services such as LINE, Telegram, Viber, and WhatsApp, social media platforms have also been used [Discord, Facebook, Instagram, LinkedIn, Pinterest, and Twitter/X]. Prior to the start of the survey, the participants provided informed consent.
Factor analysis was shown to require a minimum sample size of approximately 100 participants for the validation of the Arabic version of the questionnaire. For every question on the questionnaire, five to ten participants were required [12]. Thus, we aimed to include a minimum of 400 participants (100 from each country). Nonetheless, 523 participants completed the survey as follows: 104 from Bahrain, 164 from Jordan, 103 from Saudi Arabia, and 152 from Tunisia.
The questionnaire contained the translated Arabic version of the SPS in addition to demographic information (such as age, sex, marital status, and BMI). Additionally, the Generalized Anxiety Disorder Scale-7 (GAD-7), the Athens Insomnia Scale (AIS), and the Anxiety and Preoccupation about Sleep Questionnaire (ASPQ) were completed by the participants. To evaluate test-retest reliability, the subjects were requested to retake the SPS two weeks after the first administration.
We decided to use social networks for recruitment for several reasons. First, our goal was to validate the SPS in a wide and diverse sample of the general Arabic-speaking population, rather than just focusing on individuals diagnosed with sleep disorders. Using social media platforms allowed us to easily reach a large audience in different countries, which increased the geographic and demographic diversity of our sample. Additionally, by using social networks, we were able to include participants from various backgrounds and age groups who may not have been reached through more traditional recruitment methods like clinical settings or research registries. This was especially important for our cross-cultural and multi-country study, where traditional methods may have been less effective or logistically challenging in different regions. The use of social networks or large commercial crowdsourcing platforms is strongly supported in validation studies particularly in the field of sleep medicine [13–16].
Furthermore, it is important to note that the original English language SPS [7] was developed and validated in the general population. Therefore, by recruiting participants from the general population through social networks for our study, we align with the original scale’s development approach and enable a logical cross-examination of results. This consistent sampling methodology enhances the comparability of our findings with the original scale, thereby strengthening the overall validity of the Arabic version of the SPS.
Instruments
Sleep preoccupation scale (SPS)
The SPS is a 22-item self-report measure designed to assess the frequency of sleep-related daytime preoccupation, thoughts, feelings, and behaviors [7]. It comprises two domains/factors: cognitive behavioral consequences (CBC) and affective consequences (AC) [7]. The CBC subscale contains fourteen items and assesses the frequency of monitoring for cognitive and functional impairments due to poor sleep, as well as strategies employed to combat fatigue [7]. Example items of the CBC subscale are: “I try to get to bed early the next day after a bad night’s sleep” and “I find it hard to concentrate during the day after a bad night’s sleep”.
The AC subscale contains eight items and captures the excessively negatively toned cognitive activity proposed in Harvey’s model, with items referring to levels of sleep-specific worry and distress [7]. Example items of the AC subscale are: “I feel anxious about my sleep pattern” and “I feel anxious about what will happen when I try to sleep tonight”.
The respondents rated the frequency of each item over the past month on a 7-point Likert scale from 0 (never) to 6 (all the time) [7]. For the SPS, CBC, and AC scores ranges from 0 to 132, 0–84, and 0–48, respectively. Higher scores indicate greater sleep preoccupation [7]. The original English-language SPS demonstrated good reliability, featuring an overall Cronbach’s alpha of 0.91, with subscale alphas of 0.88 for the CBC subscale and 0.89 for the AC subscale [7].
Generalized anxiety Disorder-7 scale (GAD-7)
The GAD-7 is a 7-item questionnaire designed to capture the key diagnostic features of generalized anxiety disorder (GAD), such as persistent tension, anxiety, and excessive worry about various aspects of life [17]. Respondents rate each item using a 4-point Likert scale, where 0 means “not at all,” 1 means “several days,” 2 means “more than half of the days,” and 3 means “nearly every day.” The total score ranges from 0 to 21, with higher scores indicating more severe symptoms of GAD. A score of 10 has been identified as the optimal cutoff for diagnosing GAD [18]. This study utilized the Arabic version of the GAD-7, which has demonstrated excellent internal consistency, with a reliability coefficient greater than 0.85 [19].
Athens Insomnia Scale (AIS)
The Athens Insomnia Scale (AIS) is an 8-item self-assessment tool created in 2000 to evaluate various aspects of insomnia. It includes questions on sleep onset, morning and night awakenings, sleep duration and quality, the frequency and duration of insomnia complaints, the distress caused by insomnia, and its impact on daytime functioning [20, 21]. Responses are recorded on a 4-point Likert scale, ranging from 0 to 3. Each item assesses various aspects of sleep, including sleep induction, nighttime awakenings, final awakening, total sleep duration, overall sleep quality, sense of well-being, daytime functioning, and levels of sleepiness. A score of 0 indicates no difficulty, while a score of 3 signifies severe difficulty or complete lack of sleep. This scale facilitates a comprehensive evaluation of insomnia symptoms. The total score ranges from 0 to 24, with higher scores indicating more severe insomnia symptoms. A score of 6 or above is considered the optimal threshold for diagnosing pathological insomnia [20, 21]. The AIS has demonstrated excellent internal consistency (0.84, 95% CI: 0.81 to 0.86) and high retest reliability (0.86, 95% CI: 0.80 to 0.92) according to recent meta-analytic findings [22]. In this study, the Arabic version of the AIS was utilized.
Anxiety and preoccupation about Sleep Questionnaire (APSQ)
The APSQ is a 10-item self-report questionnaire designed to measure anxiety and preoccupation related to sleep. It includes two distinct factors [8]. The first factor, comprising six items, addresses worries about the effects of poor sleep quality [8]. The second factor, consisting of four items, focuses on concerns about the uncontrollability of sleep Each item is rated on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree), with higher scores indicating greater anxiety and preoccupation with sleep [8]. The original APSQ was developed and validated in English by Jansson-Fröjmark et al. (2011) [8], demonstrating an internal consistency of 0.93 and a test-retest reliability of 0.77 over two weeks [8]. This study utilized the Arabic version of the APSQ, which has shown an internal consistency (Cronbach’s alpha) of 0.91, McDonald’s omega of 0.91, and test-retest reliability of 0.93 [16].
Statistical analysis
Descriptive statistics
Descriptive statistics, including mean, standard deviation, skewness, and kurtosis, were computed for continuous variables, whereas frequency counts and proportions were used for categorical variables.
Confirmatory factor analysis (CFA)
Confirmatory factor analysis (CFA) was conducted to examine the two-factor structure of the Arabic version of the SPS scale [23]. The Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy and Bartlett’s test of sphericity were used to assess the data’s suitability for factor analysis [23]. Model fit was evaluated using the Comparative Fit Index (CFI > 0.90) and the Tucker–Lewis Index (TLI > 0.90) [24]. Additionally, the root mean square residual (RMSR < 0.08) [25], the chi-square to degrees of freedom ratio (2 < χ²/df < 3), and the root mean square error of approximation (RMSEA) along with its 95% confidence interval (95% CI) were calculated [21]. Model fit was evaluated using the Comparative Fit Index (CFI > 0.90) and the Tucker–Lewis Index (TLI > 0.90) [22]. Additionally, the root mean square residual (RMSR < 0.08) [23], the chi-square to degrees of freedom ratio (2 < χ²/df < 3), and the root mean square error of approximation (RMSEA) along with its 95% confidence interval (95% CI) were calculated.
We repeated a series of multi-group CFA using maximum likelihood estimation to assess the configural, metric, and scalar invariance of the SPS across groups with and without insomnia [26]. Firstly, we tested the configural invariance by simultaneously fitting the proposed two-factor model in both groups, without imposing any equality constraints on factor loadings or intercepts [26]. This established the baseline model [26]. Next, we evaluated metric invariance by constraining the factor loadings to be equal across groups [26]. Finally, for scalar invariance, we added constraints on the item intercepts to make them equal across groups [26].
To assess convergent validity, the average variance extracted (AVE) was computed for each factor, with values ≥ 0.5 considered adequate [23]. Discriminant validity was evaluated using the heterotrait-monotrait ratio of correlations (HTMT), where values below 0.85 indicate acceptable discriminant validity [23].
Reliability analyses
To evaluate the internal consistency of the SPS, Cronbach’s alpha and McDonald’s omega were applied, with values above 0.60 considered acceptable and those above 0.70 regarded as good [27]. The intraclass correlation coefficient (ICC) was used to determine test-retest reliability, reflecting the agreement or consistency between measurements taken at different times [28]. Two-way mixed effects, consistency, single rater/measurement ICC was used [29].
Rasch model/Item response theory
Rasch analysis of the SPS was performed to evaluate its psychometric properties based on item response theory [30]. The Rating Scale Model was employed for analysis [30]. Item fit statistics were computed to provide information about how well item response data fit the expectations of the Rasch model [30]. Values of approximately 1.0 indicate a good fit. Values greater than 1.0 suggest potential misfit, with higher values indicating more severe misfit [30]. The point-biserial correlation for each item was reported, which measures item discrimination [30]. Higher positive values indicate that the item discriminates well between high and low levels of the measured trait [30]. We also reported the ability measure for each item [30]. Positive values indicate more difficult items. Negative values indicate easier items [30]. The standard error of the ability measure was also provided to reflect the precision of the estimate [30].
Other analyses
We also assessed the convergent validity [31] of the Arabic SPS by computing Pearson’s correlation analyses between the SPS and the AIS, the GAD-7 and the ASPQ.
For SPS and its two factors (CBC and AC) we conducted independent samples t-tests to compare participants with insomnia symptoms to those without. We identified individuals with insomnia symptoms using the AIS. Effect size was computed in the form of Cohen’s d.
Participants were divided into two groups: those with insomnia symptoms (AIS ≥ 6) and a reference group without insomnia symptoms (AIS < 6). For AIS A score of 6 or above is considered the optimal threshold for diagnosing pathological insomnia [20, 21]. We used independent samples t-tests to assess differences between these groups on various outcome measures.
All the statistical analyses were performed using R statistical software version 4.3.1 (Beagle Scouts), with an alpha level set at 0.05 for all the analyses.
Results
Descriptive results
This study recruited 523 participants with a mean age of 23.62 years (SD ± 7.5). The mean BMI among the participants was 23.29 (SD ± 4.78). The majority of participants were female (75%), and 83% were single. Table 1 shows descriptive statistics for the total SPS score, SPS individual items and other variables measured for the participants. The items present acceptable skewness (ranging between − 0.69 and 0.48; mainly skewed) and kurtosis (ranging between − 0.77 and 7.85; mainly leptokurtosis) values.
Table 1.
Descriptive results of the Sleep Preoccupation Scale (SPS) n = 523
| Variable | Mean | SD | Skewness | Kurtosis |
|---|---|---|---|---|
| Age | 23.62 | 7.5 | 2.85 | 9.68 |
| Height (kg) | 161.43 | 8.65 | 0.63 | 0.29 |
| Weight (cm) | 61.07 | 15.23 | 1.03 | 1.81 |
| BMI kg/cm2 | 23.29 | 4.78 | 0.72 | 0.52 |
| SPS1 | 3.53 | 1.1 | -0.69 | -0.27 |
| SPS2 | 3.65 | 1.04 | -0.8 | 0.22 |
| SPS3 | 3.37 | 1.08 | -0.37 | -0.56 |
| SPS4 | 3.21 | 1.16 | -0.31 | -0.79 |
| SPS5 | 3.23 | 1.14 | -0.41 | -0.7 |
| SPS6 | 3.33 | 1.15 | -0.48 | -0.56 |
| SPS7 | 3.52 | 1.17 | -0.65 | -0.45 |
| SPS8 | 2.77 | 1.18 | 0.15 | -0.89 |
| SPS9 | 3.41 | 1.15 | -0.54 | -0.47 |
| SPS10 | 2.89 | 1.02 | 0.06 | -0.43 |
| SPS11 | 2.94 | 1.11 | -0.04 | -0.75 |
| SPS12 | 3.07 | 1.18 | -0.11 | -0.92 |
| SPS13 | 3.44 | 1.09 | -0.55 | -0.4 |
| SPS14 | 3.27 | 1.21 | -0.4 | -0.81 |
| SPS15 | 3.18 | 1.1 | -0.28 | -0.78 |
| SPS16 | 2.89 | 1.1 | 0.13 | -0.89 |
| SPS17 | 2.78 | 1.14 | 0.19 | -0.87 |
| SPS18 | 2.52 | 1.15 | 0.48 | -0.65 |
| SPS19 | 3.25 | 1.16 | -0.34 | -0.79 |
| SPS20 | 3.09 | 1.17 | -0.15 | -0.97 |
| SPS21 | 2.66 | 1.18 | 0.29 | -0.83 |
| SPS22 | 3.14 | 1.21 | -0.21 | -0.93 |
| SPS CBC | 45.61 | 10.07 | -0.27 | 0.58 |
| SPS AC | 23.52 | 6.79 | 0.19 | -0.2 |
| SPS Total | 69.13 | 15.25 | -0.01 | 0.67 |
| AIS | 5.43 | 3.27 | 0.33 | -0.65 |
| GAD-7 | 9.73 | 5.32 | 0.2 | -0.65 |
| ASPQ Total | 31.28 | 8.31 | -0.06 | -0.08 |
Notes SPS CBC = Sleep Preoccupation Scale – Factror 1 Cognitive Behavioral Consequences. SPS AC = Sleep Preoccupation Scale – Factor 2 Affective Consequences. SPS Total = Total Sleep Preoccupation Scale Score. AIS = Athens Insomnia Scale. GAD-7 = Generalized Anxiety Disorders. APSQ = Anxiety and Preoccupation About Sleep Questionnaire
CFA results
The KMO value was 0.93, and the result of Bartlett’s test of sphericity was statistically significant (χ² = 4791.01, df = 231, p < 0.001), indicating that the data were suitable for factor analysis. The CFA results revealed that all items loaded significantly on their respective factors, with factor loadings ranging from 0.41 (SPS10) to 0.88 (SPS17). The residual variances of the items also demonstrated statistically significant estimates. The chi-square test indicated a significant difference between the baseline model and the factor model (χ² = 743.04, df = 208, p < 0.001), suggesting that the factor model provided a better fit to the data than the baseline model. The fit indices demonstrated an acceptable to good model fit, with a CFI of 0.89, a TLI of 0.87, an NNFI of 0.87, an NFI of 0.85, a PNFI of 0.76, an RFI of 0.83, an IFI of 0.89, and an RNI of 0.89. The RMSEA was 0.07, with a 90% confidence interval ranging from 0.07 to 0.08, indicating a reasonable fit. The SRMR was 0.05, further supporting the model’s fit. The log-likelihood values were − 15702.88, AIC = 31539.75, BIC = 31825.15, SSABIC = 31612.47, Hoelter’s critical N (α = 0.05: 171.79; α = 0.01: 182.86), GFI = 0.96, and MFI = 0.60.
To assess the construct validity of the SPS, we calculated the AVE for each factor. The AVE for Factor 1 was 0.37, and the AVE for Factor 2 was 0.48, suggesting adequate convergent validity.
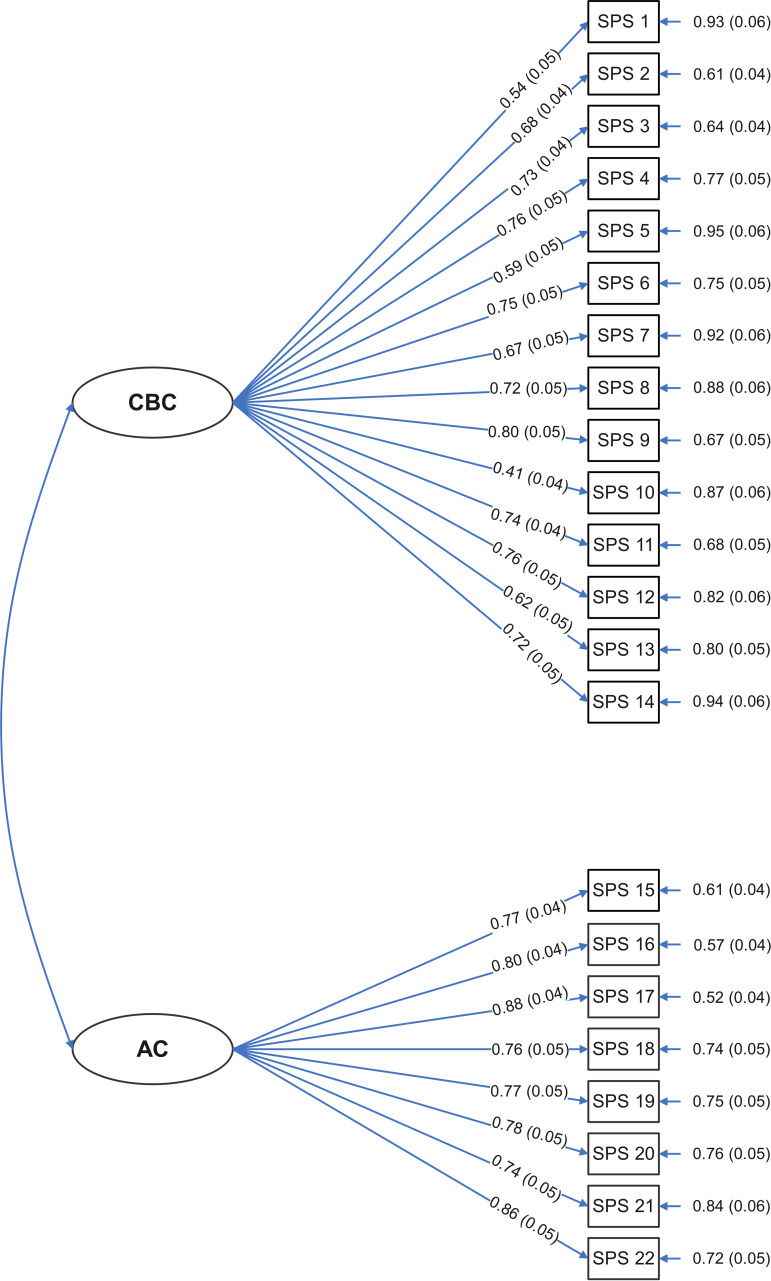
Furthermore, the HTMT between Factor 1 and Factor 2 was 0.70, indicating acceptable discriminant validity between the two factors. Table 2 shows the values of the estimates, standard errors, z values, and p values of 22 items in the SPS. See Fig. 1.
Table 2.
Confirmatory factor analysis of the Sleep Preoccupation Scale (SPS) n = 523
| Factor | Indicator | Factor loading | Residual variances | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | z | p | Estimate | SE | z | p | ||
| CBC | SPS1 | 0.54 | 0.05 | 11.26 | < 0.001 | 0.93 | 0.06 | 15.61 | < 0.001 |
| SPS2 | 0.68 | 0.04 | 16.16 | < 0.001 | 0.61 | 0.04 | 14.73 | < 0.001 | |
| SPS3 | 0.73 | 0.04 | 16.8 | < 0.001 | 0.64 | 0.04 | 14.63 | < 0.001 | |
| SPS4 | 0.76 | 0.05 | 16.16 | < 0.001 | 0.77 | 0.05 | 14.79 | < 0.001 | |
| SPS5 | 0.59 | 0.05 | 12.08 | < 0.001 | 0.95 | 0.06 | 15.51 | < 0.001 | |
| SPS6 | 0.75 | 0.05 | 16.09 | < 0.001 | 0.75 | 0.05 | 14.83 | < 0.001 | |
| SPS7 | 0.67 | 0.05 | 13.74 | < 0.001 | 0.92 | 0.06 | 15.27 | < 0.001 | |
| SPS8 | 0.72 | 0.05 | 14.68 | < 0.001 | 0.88 | 0.06 | 15.09 | < 0.001 | |
| SPS9 | 0.80 | 0.05 | 17.57 | < 0.001 | 0.67 | 0.05 | 14.42 | < 0.001 | |
| SPS10 | 0.41 | 0.04 | 9.16 | < 0.001 | 0.87 | 0.06 | 15.82 | < 0.001 | |
| SPS11 | 0.74 | 0.04 | 16.59 | < 0.001 | 0.68 | 0.05 | 14.64 | < 0.001 | |
| SPS12 | 0.76 | 0.05 | 15.76 | < 0.001 | 0.82 | 0.06 | 14.86 | < 0.001 | |
| SPS13 | 0.62 | 0.05 | 13.59 | < 0.001 | 0.80 | 0.05 | 15.29 | < 0.001 | |
| SPS14 | 0.72 | 0.05 | 14.29 | < 0.001 | 0.94 | 0.06 | 15.21 | < 0.001 | |
| AC | SPS15 | 0.77 | 0.04 | 17.6 | < 0.001 | 0.61 | 0.04 | 14.19 | < 0.001 |
| SPS16 | 0.80 | 0.04 | 18.45 | < 0.001 | 0.57 | 0.04 | 13.89 | < 0.001 | |
| SPS17 | 0.88 | 0.04 | 20.12 | < 0.001 | 0.52 | 0.04 | 13.19 | < 0.001 | |
| SPS18 | 0.76 | 0.05 | 16.36 | < 0.001 | 0.74 | 0.05 | 14.62 | < 0.001 | |
| SPS19 | 0.77 | 0.05 | 16.39 | < 0.001 | 0.75 | 0.05 | 14.57 | < 0.001 | |
| SPS20 | 0.78 | 0.05 | 16.49 | < 0.001 | 0.76 | 0.05 | 14.48 | < 0.001 | |
| SPS21 | 0.74 | 0.05 | 15.2 | < 0.001 | 0.84 | 0.06 | 14.90 | < 0.001 | |
| SPS22 | 0.86 | 0.05 | 17.96 | < 0.001 | 0.72 | 0.05 | 14.00 | < 0.001 | |
Notes Model fit chi-square test: Baseline model: χ² = 4876.48, df = 231, p < 0.001; Factor model: χ² = 743.04, df = 208, p < 0.001. Fit Indices: Comparative Fit Index (CFI): 0.89, Tucker‒Lewis Index (TLI): 0.87, Bentler-Bonett Nonnormed Fit Index (NNFI): 0.87, Bentler-Bonett Normed Fit Index (NFI): 0.85, Parsimony Normed Fit Index (PNFI): 0.76, Bollen’s Relative Fit Index (RFI): 0.83, Bollen’s Incremental Fit Index (IFI): 0.89, Relative Noncentrality Index (RNI): 0.89. The following information criteria were used: log-likelihood: -15702.88, number of free parameters: 67, Akaike information criterion (AIC): 31539.75, Bayesian information criterion (BIC): 31825.15, and sample-size adjusted Bayesian information criterion (SSABIC): 31612.47. Other Fit Measures: Root mean square error of approximation (RMSEA): 0.07, RMSEA 90% CI lower bound: 0.07, RMSEA 90% CI upper bound: 0.08, RMSEA p value: 0.00, Standardized root mean square residual (SRMR): 0.05, Hoelter’s critical N (α = 0.05): 171.79, Hoelter’s critical N (α = 0.01): 182.86, Goodness-of-fit index (GFI): 0.96, McDonald fit index (MFI): 0.60, Expected cross-validation index (ECVI): 1.68, Kaiser‒Meyer‒Olkin (KMO) Test: Overall KMO test: 0.93, Bartlett’s test of Sphericity: Bartlett’s test: χ² = 4791.01, df = 231, p < 0.001. The average variance extracted (AVE) was 0.37 for Factor 1 and 0.48 for Factor 2. HTMT: Factor 1 to Factor 2: 0.70. Note: The confirmatory factor analysis was conducted using the maximum likelihood (ML) estimator
Fig. 1.
Path diagram of the Sleep Preoccupation Scale (SPS). Notes for Fig. 1: SPS CBC = Sleep Preoccupation Scale – Factror 1 Cognitive Behavioral Consequences. SPS AC = Sleep Preoccupation Scale – Factor 2 Affective Consequences. SPS Total = Total Sleep Preoccupation Scale Score
The multi-group CFA results indicated that the insomnia and non-insomnia groups demonstrated acceptable configural, metric, and scalar invariance according to the two-factor model with acceptable fitness. All factor loadings were statistically significant (p < 0.001) in both groups, ranging from 0.40 to 0.80 for the non-insomnia group and 0.40 to 0.90 for the insomnia group.
Reliability analyses
To determine the reliability of the scale, Cronbach’s alphas, McDonald’s omegas, and interclass coefficients were calculated for the total SPS scale, CBC and AC and are listed in Table 3. The overall scale and subscales showed acceptable to excellent reliability (SPS total: α = 0.92, CBC = 0.89; AC: α = 0.88). No item was suggested for deletion to improve McDonald’s omega or Cronbach’s alpha. The test-retest reliability ICC coefficients for the SPS total = 0.95, for CBC = 0.92 and for AC = 0.91 after two weeks Table 3.
Table 3.
Reliability analysis coefficients of the Sleep Preoccupation Scale (SPS) n = 523
| Scale | Cronbach’s α | McDonald’s ω | Intraclass coefficient (ICC) |
|---|---|---|---|
| SPS Total | 0.92 | 0.92 | 0.95 |
| SPS CBC | 0.89 | 0.89 | 0.92 |
| SPS AC | 0.88 | 0.88 | 0.91 |
Notes SPS CBC = Sleep Preoccupation Scale – Factror 1 Cognitive Behavioral Consequences. SPS AC = Sleep Preoccupation Scale – Factor 2 Affective Consequences. SPS Total = Total Sleep Preoccupation Scale Score. ICC was based on two-way mixed effects, consistency, single rater/measurement coefficient
Rasch model/Item response theory
Table 4 shows the Rasch model of 22 items in the SPS. Most items demonstrated satisfactory fit, with infit values ranging from 0.79 (SPS11) to 1.24 (SPS1) and outfit values ranging from 0.79 (SPS15) to 1.26 (SPS1). However, item SPS1 exhibited some misfit, with an infit value of 1.24 and an outfit value of 1.26, which may warrant further investigation or potential removal from the scale. Regarding item difficulty and discrimination, the ability measure reflects the difficulty or endorsability of each item, with positive values indicating more difficult items and negative values indicating easier items. The item difficulty estimates ranged from − 0.64 (SPS2) to 0.74 (SPS18), suggesting a good spread of item difficulties across the continuum of the measured trait. The point-biserial correlations, which indicate the extent to which an item discriminates between respondents with high and low levels of the measured trait, were generally satisfactory, ranging from 0.46 (SPS10) to 0.64 (SPS11). Higher positive values indicate better discrimination. The model fit statistics were used to evaluate the overall fit of the Rasch model to the data. The Akaike information criterion (AIC = 28626.57), Bayesian information criterion (BIC = 29029.02), and consistent Akaike information criterion (CAIC = 29124.02) are information-theoretic measures that can be used for model comparison, with lower values indicating better fit. The log-likelihood value (-14218.28) represents the log-likelihood of the model, with higher values indicating a better fit. The squared standard deviation (SSD = 0.71) and mean squared error (MSE = 0.06) provide additional measures of model fit, with lower values suggesting better fit (See Table 5).
Table 4.
Rasch analysis of the Sleep Preoccupation Scale (SPS) n = 523
| Item | Ability measure | SE | Infit | Outfit | Point biserial |
|---|---|---|---|---|---|
| SPS1 | -0.48 | 0.05 | 1.24 | 1.26 | 0.48 |
| SPS2 | -0.64 | 0.05 | 0.88 | 0.89 | 0.6 |
| SPS3 | -0.27 | 0.05 | 0.83 | 0.87 | 0.62 |
| SPS4 | -0.07 | 0.05 | 0.94 | 0.93 | 0.61 |
| SPS5 | -0.09 | 0.05 | 1.09 | 1.13 | 0.53 |
| SPS6 | -0.22 | 0.05 | 0.99 | 1.02 | 0.59 |
| SPS7 | -0.46 | 0.05 | 1.19 | 1.19 | 0.55 |
| SPS8 | 0.44 | 0.05 | 1.01 | 1.04 | 0.58 |
| SPS9 | -0.32 | 0.05 | 0.95 | 0.93 | 0.62 |
| SPS10 | 0.31 | 0.05 | 1.04 | 1.17 | 0.46 |
| SPS11 | 0.24 | 0.05 | 0.79 | 0.8 | 0.64 |
| SPS12 | 0.1 | 0.05 | 0.96 | 0.96 | 0.61 |
| SPS13 | -0.36 | 0.05 | 1.01 | 1.05 | 0.55 |
| SPS14 | -0.14 | 0.05 | 1.15 | 1.18 | 0.56 |
| SPS15 | -0.04 | 0.05 | 0.82 | 0.79 | 0.63 |
| SPS16 | 0.31 | 0.05 | 0.81 | 0.82 | 0.62 |
| SPS17 | 0.43 | 0.05 | 0.83 | 0.83 | 0.63 |
| SPS18 | 0.74 | 0.05 | 1 | 1.02 | 0.57 |
| SPS19 | -0.13 | 0.05 | 0.94 | 0.92 | 0.62 |
| SPS20 | 0.07 | 0.05 | 1.04 | 1.03 | 0.58 |
| SPS21 | 0.57 | 0.05 | 1.04 | 1.16 | 0.57 |
| SPS22 | 0.01 | 0.05 | 1.02 | 1 | 0.61 |
Note. Item analysis was performed using the Rating Scale Model (RSM). AIC = Akaike information criterion (28626.57), BIC = Bayesian information criterion (29029.02), CAIC = consistent Akaike information criterion (29124.02). The log-likelihood represents the log-likelihood value of the model (-14218.28). SSD = squared standard deviation (0.71) and MSE = mean squared error (0.06)
Table 5.
Intercorrelations of the Sleep Preoccupation Scale (SPS) and convergent validity of the with Athens Insomnia Scale (AIS), generalized anxiety disorders Scale (GAD-7), and anxiety and preoccupation about Sleep Questionnaire (APSQ)
| SPS Total | SPS CBC | SPS AC | AIS | GAD-7 | APSQ | |
|---|---|---|---|---|---|---|
| SPS Total | — | — | — | 0.48 | 0.57 | 0.79 |
| SPS CBC | 0.94 | — | — | 0.41 | 0.49 | 0.68 |
| SPS AC | 0.86 | 0.62 | — | 0.48 | 0.55 | 0.77 |
Notes SPS CBC = Sleep Preoccupation Scale – Factror 1 Cognitive Behavioral Consequences. SPS AC = Sleep Preoccupation Scale – Factor 2 Affective Consequences. SPS Total = Total Sleep Preoccupation Scale Score. AIS = Athens Insomnia Scale. GAD-7 = Generalized Anxiety Disorders. APSQ = Anxiety and Preoccupation About Sleep Questionnaire. All correlations are significant at p < 0.001
Other results
The convergent validity of the Arabic version of the SPS was examined by investigating its correlations with other relevant measures. The results demonstrated good convergent validity, with a significant positive correlation between the SPS total score and the AIS (r = 0.48, p < 0.001). This suggests that higher levels of sleep preoccupation, as measured by the SPS, are associated with greater insomnia severity. Furthermore, the SPS exhibited a strong positive correlation with the GAD-7 score (r = 0.57, p < 0.001), indicating that greater sleep preoccupation is related to elevated levels of generalized anxiety symptoms. The SPS also showed a robust positive correlation with the APSQ (r = 0.79, p < 0.001), providing further evidence of its convergent validity in the context of anxiety and preoccupation related to sleep. The two subscales of the SPS, the CBC and AC subscales, also demonstrated significant positive correlations with the AIS, GAD-7, and APSQ, although they were slightly lower in magnitude than the total SPS (See Table 5).
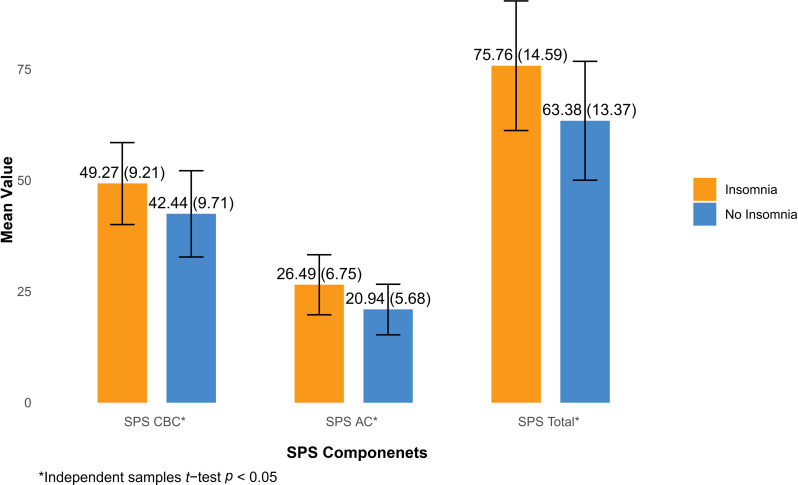
The insomnia group (n = 243) scored higher than the no insomnia group (n = 280) on SPS and both of its subscales, according to series of independent samples t-tests. A significant difference was found in the SPS CBC subscale (t(521) = 8.215, p < 0.001, Cohen’s d = 0.72), with the Insomnia group (M = 49.3, SD = 9.21) scoring higher than the No Insomnia group (M = 42.4, SD = 9.71). The SPS AC subscale also revealed a significant difference (t(521) = 10.22, p < 0.001, Cohen’s d = 0.90), with the Insomnia group (M = 26.5, SD = 6.75) scoring higher than the no insomnia group (M = 20.9, SD = 5.68). Additionally, a significant difference was observed in the SPS Total score (t(521) = 10.12, p < 0.001, Cohen’s d = 0.89), with the insomnia group (M = 75.8, SD = 14.59) scoring higher than the no Insomnia group (M = 63.4, SD = 13.37).
While there were significant differences in scores between the insomnia vs. no insomnia groups on the SPS and its subscales, the overall pattern of results was notably similar. See Fig. 2.
Fig. 2.
Comparision between cases with insomnia vs. no insomnia using the Sleep Preoccupation Scale (SPS). Notes for Fig. 2: Error bars = standard deviation. SPS CBC = Sleep Preoccupation Scale – Factror 1 Cognitive Behavioral Consequences. SPS AC = Sleep Preoccupation Scale – Factor 2 Affective Consequences. SPS Total = Total Sleep Preoccupation Scale Score. Sample sizes for each group (n = 243 for insomnia, n = 280 for no insomnia)
Discussion
The main goal of this research was to assess the reliability and validity of the Arabic version of the SPS. We found that the Arabic SPS demonstrated acceptable reliability and validity. Our results showed that the Cronbach’s alpha/McDonald’s omega coefficient for the total SPS scale was 0.92, which aligns with the original version of the scale [7]. CFA showed a two-factor solution, replicating the original factor structure of the SPS with high model fit [7]. The Rasch analysis results indicated that the SPS generally exhibited satisfactory psychometric properties. Most items demonstrated good fit to the Rasch model and adequate discrimination. However, item SPS1 exhibited some misfit, which warrants further examination or potential removal. The model fit statistics suggested an adequate fit of the Rasch model to the data. These findings supported the use of the SPS as a valid and reliable measure of sleep preoccupation. The insomnia group scored higher than the no insomnia group on SPS and both of its subscales, according to series of independent samples t-tests. These findings suggest that individuals with insomnia experience more severe sleep-related problems across multiple dimensions compared to those without insomnia. Still, while there were significant differences in scores between the insomnia vs. no insomnia groups on the SPS and its subscales, the overall pattern of results was notably similar. Given the findings above, it is clear that the Arabic translation of the Sleep SPS can be suitable for both clinical and non-clinical populations. The high prevalence of insomnia symptoms, which can affect up to 35–40% of any population [32, 33], underscores the importance of reliable assessment tools like the SPS. Its applicability across diverse groups enhances its utility in identifying sleep-related concerns, making it a valuable resource for addressing insomnia symptoms in varied settings.
Measurement invariance results suggest that the SPS exhibits a similar basic factor structure across both insomnia and non-insomnia groups.
This study is the first to translate and validate the Arabic version of the SPS, aiming to fill a significant gap in the literature by providing a culturally appropriate tool for assessing sleep-related concerns in Arabic-speaking populations.
The successful translation of the SPS into Arabic has important clinical and research implications. By adapting the SPS to Arabic, researchers can now explore how sleep-related daytime processing affects the mental health and well-being of Arabic-speaking individuals [14].
The findings of our study underscore the significance of the Arabic version of the SPS as a reliable and valid measure for assessing sleep-related cognitive processes among Arabic-speaking populations. Our results align with previous research demonstrating the critical role of daytime preoccupation in the development and maintenance of sleep disturbances. By adapting the SPS, we provide a culturally relevant tool that enhances the understanding of sleep preoccupation in diverse contexts, facilitating targeted interventions for individuals struggling with insomnia. However, it is important to acknowledge the limitation of our study, as we primarily focused on a non-clinical population. Thus, future research should aim to target individuals diagnosed with insomnia or similar sleep disorders to further validate the Arabic SPS in clinical settings. This will enhance its applicability and effectiveness in identifying and addressing sleep-related concerns in clinical practice.
To highlight the similarities and differences in profiles between the original study and the Arab study, several key aspects emerge. Both studies focus on sleep preoccupation and its impact on daytime functioning, emphasizing how cognitive and emotional responses to poor sleep influence overall well-being. While the original English language study primarily involves participants from the UK, the Arab study enhances our understanding by focusing on a diverse demographic, potentially including a wider age range that influences the nature of sleep preoccupations [7]. Both studies draw upon relevant psychological frameworks, and the Arab study integrates culturally specific models that enhance the interpretation of sleep-related distress. Ultimately, the outcomes of the Arab study resonate with the original research and broaden the implications for understanding sleep-related issues across different cultural contexts, suggesting that interventions may need to be tailored to fit the unique needs of diverse populations.
The availability of a culturally adapted and validated measure like the Arabic SPS opens up opportunities for comparative research on sleep preoccupation across different cultural groups. Researchers can investigate how cultural factors influence sleep behaviors and beliefs, leading to a better understanding of the role of culture in shaping individuals’ experiences of sleep and wakefulness. In clinical practice, the Arabic SPS can be used to assess and monitor sleep-related cognitive processes and behaviors in Arabic-speaking patients with sleep disturbances. By incorporating the Arabic SPS into clinical assessments, healthcare providers can gain insights into the impact of sleep preoccupation on daytime functioning and tailor interventions to address specific sleep-related concerns in Arabic-speaking populations.
Our study has several strengths that support its contribution to the field. First, this study represents the first effort to develop a reliable and consistent tool for assessing sleep disorders in the Arabic community. Second, we implemented a rigorous translation procedure, adhering to best practices to ensure the accuracy and cultural appropriateness of the questionnaire. Finally, we conducted comprehensive psychometric evaluations, including internal consistency, convergent validity, test-retest reliability, and CFA. These thorough evaluations provide robust evidence of the validity of the Arabic version of the SPS.
However, while our study provides valuable insights, it is important to acknowledge its limitations. The use of convenience sampling via social media and instant messaging platforms may have introduced selection bias, potentially limiting the generalizability of our findings. Additionally, the reliance on self-report measures could have led to social desirability and response bias. Furthermore, the sample size may have restricted our ability to detect potential issues with the questionnaire. Moreover, the young age of the participants and the overrepresentation of females (70% of the sample) may limit the applicability of our findings to older individuals and males.
Conclusions
Our study successfully translated the SPS questionnaire into Arabic while preserving its psychometric properties. The reliability and validity of the translation were rigorously tested and found to be statistically comparable to those of the original versions of the SPS. This tool can be used to assess the impact of daytime thoughts on nighttime insomnia effectively, providing a valuable resource for clinicians, researchers, and patients. We believe that the Arabic SPS will significantly improve care and accessibility for Arabic-speaking individuals, significantly advancing sleep research.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
None.
Abbreviations
- AC
Affective Consequences
- AIC
Akaike Information Criterion
- AIS
Athens Insomnia Scale
- APSQ
Anxiety and Preoccupation about Sleep Questionnaire
- AVE
Average Variance Extracted
- BIC
Bayesian Information Criterion
- BMI
Body Mass Index
- CAIC
Consistent Akaike Information Criterion
- CBC
Cognitive Behavioral Consequences
- CFA
Confirmatory Factor Analysis
- CFI
Comparative Fit Index
- GAD-7
Generalized Anxiety Disorder-7 Scale
- HTMT
Heterotrait-Monotrait Ratio of Correlations
- ICC
Intraclass Correlation Coefficient
- KMO
Kaiser–Meyer–Olkin Measure
- RMSEA
Root Mean Square Error of Approximation
- RMSR
Root Mean Square Residual
- SD
Standard Deviation
- SPS
Sleep Preoccupation Scale
Author contributions
S.Y.A., W.I., W.H., A.A., K.T., A.S.B., Z.S., and H.J. were involved in translation and experiments. S.Y.A., W.I., W.H., and H.J. collected data. S.Y.A., W.I., W.H., A.A., K.T., A.S.B., Z.S., A.P., and H.J. wrote the main manuscript text, and HJ performed all analyses. All authors reviewed and approved the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability
The data that support the findings of this study are available from the corresponding author upon request.
Declarations
Ethics approval and consent to participate
Prior to the collection of data, this study was reviewed and approved by the University of Jordan’s Research Committee. Jordan (Code: REC/HG/23/475/SPS, Date: 25 January 2024). All methods were conducted in accordance with relevant guidelines and regulations. The study procedures adhered to the ethical guidelines outlined in the Helsinki Declaration of 1964 and its later amendments (1975, 1983, 1989, and 1996). Informed consent was obtained from all subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Amir Pakpour, Email: amir.pakpour@ju.se.
Haitham Jahrami, Email: haitham.jahrami@outlook.com.
References
- 1.Medic G, Wille M, Hemels ME. Short-and long-term health consequences of sleep disruption. Nat Sci Sleep 2017:151–61. [DOI] [PMC free article] [PubMed]
- 2.Garbarino S, Lanteri P, Durando P, Magnavita N, Sannita WG. Co-morbidity, mortality, quality of life and the healthcare/welfare/social costs of disordered sleep: a rapid review. Int J Environ Res Public Health. 2016;13(8):831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reimer MA, Flemons WW. Quality of life in sleep disorders. Sleep Med Rev. 2003;7(4):335–49. [DOI] [PubMed] [Google Scholar]
- 4.Harvey AG. A cognitive theory and therapy for chronic insomnia. J Cogn Psychother. 2005;19(1):41–59. [Google Scholar]
- 5.Harvey AG. A cognitive model of insomnia. Behav Res Ther. 2002;40(8):869–93. [DOI] [PubMed] [Google Scholar]
- 6.Hiller RM, Johnston A, Dohnt H, Lovato N, Gradisar M. Assessing cognitive processes related to insomnia: a review and measurement guide for Harvey’s cognitive model for the maintenance of insomnia. Sleep Med Rev. 2015;23:46–53. [DOI] [PubMed] [Google Scholar]
- 7.Ellis J, Mitchell K, Hogh H. Sleep preoccupation in poor sleepers: psychometric properties of the Sleep Preoccupation Scale. J Psychosom Res. 2007;63(6):579–85. [DOI] [PubMed] [Google Scholar]
- 8.Jansson-Frojmark M, Harvey AG, Lundh LG, Norell-Clarke A, Linton SJ. Psychometric properties of an insomnia-specific measure of worry: the anxiety and preoccupation about Sleep Questionnaire. Cogn Behav Ther. 2011;40(1):65–76. [DOI] [PubMed] [Google Scholar]
- 9.Espie CA. Insomnia: conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annu Rev Psychol. 2002;53:215–43. [DOI] [PubMed] [Google Scholar]
- 10.Gregoire J. ITC guidelines for translating and adapting tests. Int J Test. 2018;18(2):101–34. [Google Scholar]
- 11.Son J. Back translation as a documentation tool. Translation Interpreting the. 2018;10(2):89–100. [Google Scholar]
- 12.Hussain NM, AlMansouri DH, AlGhareeb M, Almutawa YM, Bucheeri OK, Helmy M, Trabelsi K, Saif Z, Jahrami H. Translating and validating the hoarding rating scale-self report into Arabic. BMC Psychol. 2023;11(1):233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trabelsi K, Almarzooqi MA, Aljaloud KS, Ghazzawi HA, Alenezi AF, Salem A, Kerkeni M, Kerkeni M, Chtourou H, Ammar A, et al. Adapting the athlete sleep behavior questionnaire (ASBQ) for arabic-speaking populations: translation, reliability testing, and validation using classical theory and item response theory. Sleep Med. 2024;119:267–75. [DOI] [PubMed] [Google Scholar]
- 14.AlMashouk Y, Abu-Saleh SY, Ghazzawi H, Trabelsi K, Jahrami H. Translating and establishing the psychometric properties of the Jenkins Sleep Scale for Arabic-speaking individuals. BMC Psychiatry. 2024;24(1):236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alghamdi AA, Abu-Saleh SY, Almohaya YA, Alamri HK, Ghazzawi H, Trabelsi K, Saif Z, BaHammam AS, Pandi-Perumal SR, Jahrami H. Examining the reliability and validity of the arabic version of the Glasgow Sleep Effort Scale (GSES). Sleep Breath. 2024;28(4):1831–8. [DOI] [PubMed] [Google Scholar]
- 16.Alghamdi AA, Abanumai AA, Althobaiti MF, Alzahrani MS, Abu-Saleh SY, Ammar A, Ghazzawi H, Trabelsi K, Bragazzi N, BaHammam AS, et al. The Psychometric properties of the Arabic Version of the anxiety and preoccupation about Sleep Questionnaire (APSQ). Nat Sci Sleep. 2024;16:75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7. [DOI] [PubMed] [Google Scholar]
- 18.Rutter LA, Brown TA. Psychometric properties of the generalized anxiety disorder scale-7 (GAD-7) in outpatients with anxiety and mood disorders. J Psychopathol Behav Assess. 2017;39:140–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sawaya H, Atoui M, Hamadeh A, Zeinoun P, Nahas Z. Adaptation and initial validation of the Patient Health Questionnaire – 9 (PHQ-9) and the generalized anxiety disorder – 7 questionnaire (GAD-7) in an arabic speaking Lebanese psychiatric outpatient sample. Psychiatry Res. 2016;239:245–52. [DOI] [PubMed] [Google Scholar]
- 20.Okajima I, Miyamoto T, Ubara A, Omichi C, Matsuda A, Sumi Y, Matsuo M, Ito K, Kadotani H. Evaluation of severity levels of the Athens Insomnia scale based on the criterion of insomnia severity index. Int J Environ Res Public Health. 2020;17(23):8789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Okajima I, Nakajima S, Kobayashi M, Inoue Y. Development and validation of the J apanese version of the A thens I nsomnia S cale. J Neuropsychiatry Clin Neurosci. 2013;67(6):420–5. [DOI] [PubMed] [Google Scholar]
- 22.Jahrami H, Trabelsi K, Saif Z, Manzar MD, BaHammam AS, Vitiello MV. Reliability generalization meta-analysis of the Athens Insomnia Scale and its translations: examining internal consistency and test-retest validity. Sleep Med. 2023;111:133–45. [DOI] [PubMed] [Google Scholar]
- 23.Kline RB. Principles and practice of structural equation modeling (3. Baskı). New York, NY: Guilford 2011, 14:1497–1513.
- 24.Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equation Modeling: Multidisciplinary J. 1999;6(1):1–55. [Google Scholar]
- 25.Hu L-T, Bentler PM. Evaluating model fit. 1995.
- 26.Van De Schoot R, Schmidt P, De Beuckelaer A, Lek K, Zondervan-Zwijnenburg M. Measurement invariance. Volume 6. Frontiers Media SA; 2015. p. 1064. [DOI] [PMC free article] [PubMed]
- 27.Shrestha N. Factor analysis as a tool for survey analysis. Am J Appl Math Stat. 2021;9(1):4–11. [Google Scholar]
- 28.Chenani KT, Madadizadeh F. Guideline for selecting types of reliability and suitable intra-class correlation coefficients in clinical research. J Biostatistics Epidemiol 2021.
- 29.Koo TK, Li MY. A Guideline of selecting and reporting Intraclass correlation coefficients for Reliability Research. J Chiropr Med. 2016;15(2):155–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.De Ayala RJ. Item response theory and Rasch modeling. The reviewer’s guide to quantitative methods in the social sciences. 2nd ed. New York, NY, US: Routledge/Taylor & Francis Group; 2019. pp. 145–63. [Google Scholar]
- 31.Krabbe PFM. Chap. 7 - Validity. In: The Measurement of Health and Health Status. edn. Edited by Krabbe PFM. San Diego: Academic Press; 2017: 113–134.
- 32.Morin CM, Jarrin DC. Epidemiology of Insomnia: prevalence, course, risk factors, and Public Health Burden. Sleep Med Clin. 2022;17(2):173–91. [DOI] [PubMed] [Google Scholar]
- 33.Morin CM, Buysse DJ. Management of Insomnia. N Engl J Med. 2024;391(3):247–58. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon request.