Abstract
Purpose:
To identify and assess differences in oral hygiene parameters in patients undergoing orthodontic treatment with clear aligners compared to fixed appliances.
Materials and Methods:
Published and unpublished literature was searched in seven databases until May 31st 2021. Representative keywords included ‘orthodontic aligner’, ‘fixed appliance’, ‘oral hygiene’, ‘plaque index’, ‘caries’. Study selection, data extraction, risk of bias and certainty of evidence assessment were undertaken independently by three reviewers. Random effects meta-analyses with respective confidence intervals (95% CI) were conducted, where applicable.
Results:
A total of 882 unique records were screened, with a final number of 21 articles being eligible for qualitative synthesis, while 4 of those contributed to meta-analyses. Risk of bias was rated within the range of low to high or serious overall, while certainty of evidence was low to very low according to GRADE. For periodontal parameters, adults undergoing aligner orthodontic treatment presented summary plaque scores 0.58 lower than those treated with fixed appliances, within the first 6 to 12 weeks (4 studies: mean difference: -0.58; 95%CI: -0.82, -0.34; p < 0.001; I2 squared: 71.3%), while no evidence of difference was recorded for inflammation indices. Microbiologic parameters such as presence of S. mutans and lactobacilli were more pronounced in patients with fixed appliances for the first 3 to 6 months (synthesised data from 2 studies).
Conclusions:
In the short-term after initiation of orthodontic treatment, patients treated with aligners and no additional attachments/adjuncts presented potentially higher levels of oral health overall. However, the evidence is supported by low to very low certainty.
Key words: fixed appliances, oral hygiene, orthodontic aligners, systematic review
Technological advancements in dentistry and orthodontics have increased treatment expectations of patients seeking orthodontic treatment, while being driven by both aesthetic and functional demands. The biomechanical background of orthodontic tooth movement with aligners has undergone rapid development during the last years. The aligner industry is an aspiring counterpart to standard conventional fixed-appliance orthodontic treatment.22,33,53 Aesthetic advantages and claims of increased comfort,29 easy application, and decreased treatment duration support aligner industries’ assertions and subsequently influence patient expectations.36
With the introduction of aligner use in clinical practice, reports have emerged about their potential advantages in terms of oral hygiene, dental and periodontal health.1,33 The specific target indices are the plaque index score (PI) and pocket probing depth (PPD) as well as the full-mouth bleeding score (FMBS),3,26,34,51 which are further exaggerated by the patient’s age and duration of orthodontic treatment.3,9 Importantly, critical factors for maintaining optimal oral hygiene levels during orthodontic treatment are patient cooperation, motivation, and personal knowledge about their periodontal health.5,7,27
In this respect, one might argue that improving the gingival and periodontal health indices might be expected during aligner treatment. It has been speculated that the part-time and removable nature of such appliances may result in potentially higher levels of oral hygiene maintenance, lowering the risk of developing gingivitis or tooth demineralisation.1,6,26,31 Conversely, awareness has been raised concerning oral microbiome and periodontal health status of patients undergoing treatment with aligners, mainly due to the ‘full-coverage’ effect of such appliances and adjuncts.10,34,45,54
Several reviews have been published lately, comparing aligner to fixed-appliance therapy; however, their focus has been somewhat variable, with specific interest on orthodontic treatment outcome,42,43 forces and moments generated by aligners4,23 and safety considerations.24 Furthermore, no comprehensive approach has been followed-up to date to review the existing evidence on oral health conditions overall, including dental and gingival-periodontal health of patients undergoing aligner treatment vs fixed-appliance therapy. The two available reviews26,45 focussed solely on periodontal health indices, with the most recent reporting a search strategy from almost four years ago.26 Since then, many primary studies have been published, with an increased dynamic being documented during the last 3 years.2,8,11,32
Therefore, the present systematic review aimed to answer the question: ‘Is aligner treatment for orthodontic tooth movement superior to the gold standard of fixed appliances with regard to oral hygiene status and, more specifically, the periodontal status and caries formation?’. The null hypothesis is that there is no difference between aligners and fixed appliances concerning oral hygiene maintenance during treatment.
Materials and Methods
Protocol and Reporting
Cochrane’s protocol was followed in this review, using Review Manager 5.4.1, the official software of Cochrane’s database (Review Manager [RevMan] computer program, version 5.4.1 Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2020). Furthermore, the reporting of this review followed the recommendations of the PRISMA statement.37 The protocol was registered with the Open Science Framework (https://osf.io/txgj6/).
Search Strategy
An electronic search was conducted of the published and unpublished literature, separately, and by two examiners (EO, PF). The primary formal databases utilised in this study were MEDLINE via Pubmed, Scopus, Cochrane Central, and Cochrane Database for Systematic Reviews. Studies from the grey literature, defined as theses, dissertations, product reports, and unpublished studies, were found using ClinicalTrials.com, Open Grey, and ISRCTN. Hand searching was conducted in the retrieved literature for full-text evaluation of any additional articles with potential for inclusion. No filters were used. The search was performed on August 21, 2020 and updated on May 31, 2021. The entire search strategy for PubMed is presented in Appendix 1.
Eligibility Criteria
Eligibility criteria for study selection were:
Study design: Randomised controlled trials (RCTs), prospective clinical trials (PCTs), and observational studies were included in the review. Studies comparing at least two groups were considered. Specifically, these comprised full-arch treatment with orthodontic aligners either with fixed appliances or with a different type of orthodontic aligner (i.e. Invisalign vs clear aligners or removable appliances).
Participants: All patients undergoing orthodontic treatment (no age or gender restriction).
Intervention: orthodontic treatment (any) with aligners (any).
Comparators: fixed-appliance orthodontic treatment, other aligner treatment/removable appliances.
Outcome: oral hygiene measures, including but not confined to: gingival index (GI), plaque index (PI), bleeding on probing (BoP), probing depth (PD), clinical attachment loss (CAL), recession, the concentration of cariogenic and periodontal microflora in the surrounding tissues, as well as formation of incipient (i.e. white lesions) or advanced caries lesions.
Exclusion criteria: Animal studies, case reports/series, non-clinical studies, and studies not performed in vivo were excluded. Studies without at least one control and one test group, studies including previously treated orthodontic patients, studies without comprehensive orthodontic management, and studies with ineligible results for this review were excluded. Only RCTs and prospective clinical studies were included in the quantitative data synthesis.
Study Selection Process
The studies collected from all databases were cross-checked for the exclusion of duplicates. According to the study’s main characteristics of interest, titles and abstracts were screened independently by 3 reviewers (EO, PF, AT), with further exploration of the full text. Each reviewer forwarded the studies for inclusion and exclusion, according to eligibility criteria. Potential discrepancies were discussed among reviewers until a consensus was established. A fourth and fifth reviewer (CR, DK) were consulted when necessary to settle disagreements.
Data Collection
Data were extracted and recorded in standardised piloted forms (Zotero 5.0.47, Corporation for Digital Scholarship; Vienna, VA, USA, and the Roy Rosenzweig Center for History and New Media; George Mason University, Fairfax, VA, USA). These forms included specific characteristics of the study (type, title, authors, abstract, publication, volume, issue, pages, date, series, series title, series text, journal abbreviation, language, DOI, URL, ISSN, short title, mean of access, archive, location in the archive, library catalogue, call number, date added, date modified). Data were extracted by three of the reviewers (EO, PF, AT) and re-examined by another two (CR, DK). Inconsistencies were discussed among reviewers until a consensus was reached.
Risk of Bias in Individual Studies
The methodological quality of the studies was assessed by the Cochrane Risk of Bias tool 2.0 for Randomized Controlled Trials49 and the ROBINS-I (Risk of Bias in Non-randomized Studies – of Interventions) for controlled trials and observational studies.48
Summary Measures and Data Synthesis
Quantitative syntheses of the studies’ findings were performed, if applicable, and after exploring heterogeneity levels across individual reports. Clinical heterogeneity was examined related to individual study settings as well as participants’ characteristics and eligibility criteria. Statistical heterogeneity was also assessed, visually first, via inspection of the confidence limits within the Forest plots, and also statistically using an I2 test, where a p-value < 0.10 was indicative of non-homogeneity. Random effects meta-analysis was conducted in view of the potential heterogeneity anticipated, under the DerSimonian and Laird variance estimator. Pooled estimates and 95% confidence intervals (95%CIs) were presented if two or more studies were deemed eligible for a single comparison. Prediction intervals were also computed, where applicable (at least 3 studies needed), in order to incorporate an assessment of a range of effects in future clinical settings. Effect measures were either mean differences (MD), or risk ratios (RR), depending on the nature of the retrieved outcome. Study authors were contacted for additional data requests if not all available information was provided within the published document.
Risk of Bias across Studies
It was planned to explore publication bias through standard funnel plots and Egger’s regression test, if applicable.13
Additional Analyses
Sensitivity analyses were considered, if applicable, to explore and isolate the effect of studies with serious/critical/high risk of bias on the overall impact, if studies of both serious/critical/high or low risk of bias were ultimately included in the quantitative synthesis.
Assessment of the Quality of the Evidence
Grading of Recommendations Assessment, Development, and Evaluation (GRADE) was implemented to assess the overall quality of the evidence as formulated by the question, treatments, and outcomes for evaluation. According to GRADE, the overall body of evidence was rated as high, moderate, low, and very low. Assessment of the body of evidence primarily involves assessment of study design. Assessment is made on the following domains: risk of bias, inconsistency, indirectness, imprecision, and publication bias. For the first 4 domains, the quality of evidence may be downgraded based on either ‘serious’ or ‘very serious’ risks (1 or 2 levels respectively); publication bias may either be suspected or undetected. For non-randomised/observational designs in particular, which theoretically start from a ‘low’ level of evidence, the possibilities for an upgrade are as follows: a large or very large effect, plausible residual confounding that may alter the effect, or a dose-response gradient. The level of evidence may be upgraded by 1 or 2 levels (large effect), or 1 level (plausible confounding, dose-response gradient).20
Results
Search Details
The complete study selection process, from searching to inclusion, is presented in Fig 1. From an initial hit of 971 articles, after additional hand searching and duplicate removal (882 unique records screened), 21 articles passed the full-text screening process and were included in the qualitative synthesis. Of those, 4 qualified28,30,39,40 for quantitative syntheses (meta-analyses).
Fig 1.
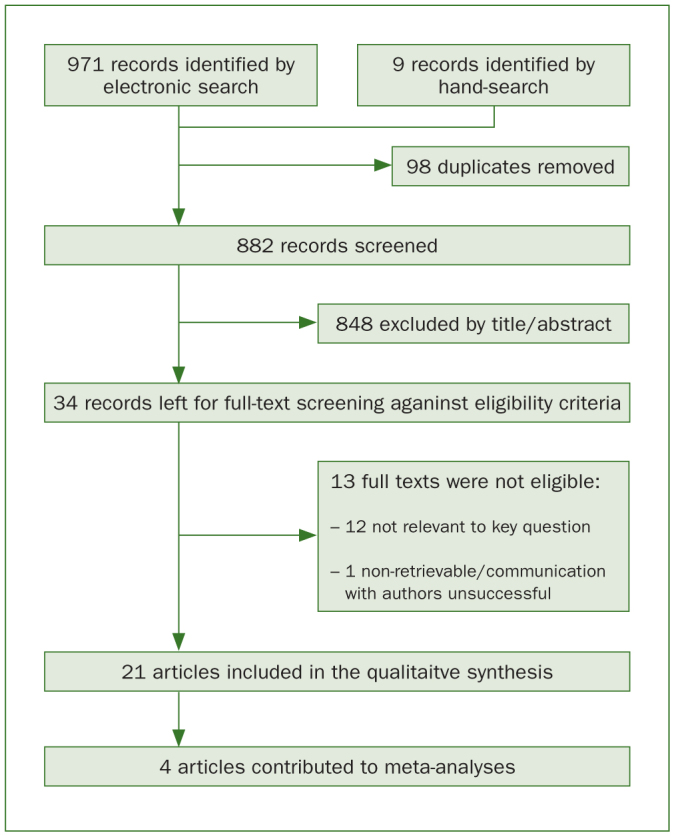
Flow diagram of study selection and inclusion.
Study Design and Characteristics
Detailed characteristics of included studies and findings of the data extraction process are presented in Table 1. Of a total of 21 publications, the study design breakdown was as follows: 6 RCTs, 11 prospective clinical trials (PCTs), 3 retrospective cohorts, and one cross-sectional study. Publication dates of these studies varied from 2005 to 2020, with the majority being published within the years 2018 and 2020 (11/21; 52.4%).
Table 1.
Characteristics of included studies
| Authors (year), type | Participants | Intervention | Comparator | Outcomes | Additional information |
|---|---|---|---|---|---|
| Abbate et al (2015), RCT | 50 teenagers (10–18) treatment with fixed brackets (n = 25) Treatment with Invisalign aligners (n = 25) |
Invisalign | Fixed labial brackets | Full mouth plaque score Full mouth bleeding score Plaque index Bleeding on probing Probing depth Oral hygiene compliance |
3 dropouts on aligner group Timeline: 3, 6, 12 months |
| Albhaisi et al (2020), RCT | 49 participants, 39 female, 10 male, 21.25±3, range 17–24 | Clear aligners | Fixed labial appliances | Fluorescence loss (ΔF) Number of newly developed lesions Deepest point in the lesion (ΔFMax) Lesion area (pixels) and plaque surface area (DR30) were measured as secondary outcomes. Fluorescence was assessed using QLF. |
Timeline: 3 months (use of attachments) |
| Azaripour et al (2015), retrospective cohort | 100 participants: 50 with Invisalign (11 males and 39 females, mean age 31.9 ± 13.6 years; range: 12–61 years) and 50 with fixed appliances (34 females and 16 males, mean age 16.3 ± 6.9 years old; range 11–61 years) | Invisalign | Fixed labial appliances | API SPI GI |
Timeline: 12 months (at least 6 months in treatment) |
| Bushang et al (2018), retrospective cohort | 450 participants, aligners (30.4 ± 14 years), fixed (29.2 ± 11.5 years), aligners (64% females, 36% males), fixed (63% females, 37% males) | Clear aligners | Fixed labial appliances | OH WSLs |
85% of the aligner cases and 48% of the fixed cases were taken from private practice Timeline: throughout treatment duration |
| Chhibber et al (2017), RCT | 71 participants 41 boys 30 girls. Mean ages of participants 16.56 + 3.99 in CLA group (27 participants), 15.39 + 3.54 in SLB group (22 participants), and 14.56 ± 3.92 in ELB group (22 participants) | Invisalign | Self-ligating brackets Elastomeric ligating brackets |
PI GI PBI |
Three in the CLA group, 5 in the SLB group, and 2 in the ELB group were completely lost to follow-up, and 2 in the SLB group and 1 in the ELB group were partially followed-up. Timeline: 9 and 18 months |
| Dallel et al (2020), PCT | 112 participants, 10–20 years of age, 49.1% females, 50.9% males | Invisalign | Fixed labial appliances Andresen type II activator |
Volume and salivary flow Biochemical parameter measurement Trolox equivalent antioxidant capacity WSLs |
Timeline: 1 and 9 months |
| Gujar et al (2019), RCT | 40 participants (age 12–32 years; mean 28±4 years), 23 females, 17 males | Clear aligners (probably Invisalign, but not clearly specified) | Fixed labial appliances | Cytokine levels PI GI POB |
Timeline: 21 days |
| Gujar et al (2020), PCT | 60 participants, 11–29 years of age | Invisalign | Fixed labial appliances Fixed lingual appliances |
Microbial level changes using checkerboard DNA-DNA hybridisation | Samples were collected only from the maxillary arch Timeline: 30 days |
| Han et al (2015), retrospective cohort | 35 participants with periodontitis, 21 females, 14 males, mean age 52.97 ± 9.42 years, range 35–74 | Clear aligners | Fixed labial appliances | PI reduction GI reduction PD reduction Bone level improvement |
The male:female ratio was statistically significantly different between the 2 groups 1 patient smoked CAT was used for severely mobile or labial inclined teeth Timeline: throughout treatment duration |
| Karkhanetci et al (2013), PCT | 42 participants, FA group: 16 females, 6 males, 34 ± 7.18 years of age, range 18–44. Invisalign group: 12 females, 8 males, 28 ± 6.86 years of age, range 18–44 | Invisalign | Fixed labial appliances | PI GI BoP PPD BANA (secondary outcome) |
Modest sample size 17% attrition rate Timeline: 1.5, 6, 12 months |
| Levrini et al (2013), RCT | 30 adults (10 Invisalign, 10 fixed appliances, 10 no intervention)(9 males, 21 females, aged 25.1 ± 4.6) | Invisalign | Fixed appliances, no intervention | PI PD BOP Compliance with OH Subgingival microbial samples |
Timeline: 1 and 3 months |
| Levrini et al (2015), RCT | 77 participants (5 male Invisalign, 18 male fixed appliances, 2 control, 27 male Invisalign, 17 male fixed appliances, 8 control) age range 16–60 years | Invisalign | Fixed appliances, no intervention | PI PD BOP Biofilm mass Periodontal pathogens (PCR) |
Timeline: 1 and 3 months |
| Madariaga et al (2020), PCT | 40 participants with permanent dentition (26 females, 14 males) mean age 27.6 ± 12.6 years, 20 treated with aligners 20 with fixed appliances | Clear aligners | Fixed appliances | PD PI BOP REC (gingival recession) |
Timeline: 3 months |
| Miethke and Vogt (2005), PCT | 60 participants (43 female, 17 male, 30 Invisalign, 30 fixed appliances) Mean age 30.1 years, range 18–51 |
Invisalign | Fixed appliances | Modified GI Modified PI Modified PBI SPI |
It is possible, though not stated, that at least 1 patient was treated with both brackets and aligners concurrently Timeline: after 1, 2, and 3 months (patients in treatment for at least 6 months) |
| Miethke and Brauner (2007), PCT | 60 participants 30 with Invisalign, 30 with fixed lingual appliances. Age information in the fixed appliances group 16–48 years, mean age: 39.6 years | Invisalign | Fixed lingual appliances | Modified GI Modified PI Modified PBI SPI |
Invisalign group was used in a previous study (Miethke et al, 2005). Some participants were recruited from private practices Timeline: after 1, 2, 3 months (patients in treatment for at least 6 months) |
| Mulla Issa et al (2020), cross sectional | 80 participants, 50% males, 50% females, mean age: 27±5.8 years; range: 23–29 years | Clear aligners (Angle Align, China / Invisalign) | Fixed labial appliances with conventional brackets (a), ceramic brackets (b), self-ligating brackets (c) | PI GI GBI SBI PBI BPE BOP |
Timeline: at least 6 months in treatment, recorded once |
| Mummolo et al (2020a), PCT | 90 participants (30 had Invisalign, mean age 21.5±1.5 years, 30 had fixed appliances, mean age 23.3±1.6 years, 30 had removable positioners, mean age 18.2 ±1.5 years) | Invisalign | Fixed appliances, removable positioners (RP) (Occlus-o-Guide) | Salivary concentrations of S. mutans and lactobacilli (CRT bacteria) PI |
Timeline: 3 and 6 months |
| Mummolo et al (2020b), PCT | 80 participants (40 [16 females, 24 males] Invisalign with mean age 20.4±1.7 years; 40 [18 females, 22 males] fixed appliances with mean age 21.3±1.7,) | Invisalign | Fixed labial appliances | PI Salivary flow (CRT prevention system) Buffering power of saliva (CRT buffer) Salivary levels of S. mutans and lactobacilli (CRT bacteria) |
Timeline: 3 and 6 months |
| Sifakakis et al (2018), PCT | 30 participants, 17 females, 13 males, mean age 13.8 years, range 12–18 years | Clear aligners | Fixed labial appliances | Simplified PI Simplified GI DMFT qPCR (for cariogenic bacteria) |
Self-ligating fixed appliances Timeline: 2 weeks, 1 month |
| Srinath et al (2016), PCT | 46 participants. Fixed appliances group: 18 women and 8 men with a mean age of 34 ± 7.18 years, range of 22–44 years. Aligners group: 8 men and 12 women, mean age: 35 ± 6.86 years, range: 18–38 years |
Clear aligners | Fixed appliances | GI, PD, BOP | Timeline: 6 weeks, 6 months, 12 months |
| Wang et al (2019), PCT | 26 participants, 20–25 years | Invisalign | Fixed labial appliances | 16S rRNA gene identified through pyrosequencing | Only 5 subjects were selected randomly from each group for high-throughput pyrosequencing analysis Timeline: one single saliva sample collection (at least 6 months in treatment) |
API: approximal bleeding index; BPE: basic periodontal examination index; BOP: bleeding on probing; CAT: clear aligner technique; CLA: clear aligners; DMFT: decayed, missing, filled teeth; ELB: elastomeric ligated brackets; FA: fixed appliances; GBI: gingival bleeding index; GI: gingival index; OH: oral hygiene; PBI: papillary bleeding index; PCT: prospective clinical trial; PI: plaque index; PPD: pocket probing depth; REC: gingival recession; RCT: randomised controlled trial; SBI: sulcus bleeding index; SLB: self-ligating brackets.
Fifteen studies examined the effects of treatment in adult patients, with one of those in participants with chronic periodontitis.21 Four involved only teen/adolescent participants, while two included a wide range of ages including both teenagers and adults. Sample sizes ranged from 26 to 112 patients for RCTs and prospective clinical trials, while those of retrospective and cross-sectional studies were between 35 and 450.
In 13 of 21 studies, the intervention group comprised Invisalign (Align Technology; San Jose, CA, USA) clear-aligner treatment, while in the rest of the studies, thermoformed clear-aligner appliances were used. Traditional labial fixed-appliance treatment was provided in comparator groups in 20 out of 21 studies, with one including patients with both labial and lingual multi-bracket appliances and another one in which the comparator group had lingual fixed appliances. A number of outcomes related to oral and periodontal hygiene were recorded. Briefly, plaque indices, bleeding scores, probing depth, and gingival indices were the most frequently recorded outcomes. In addition, salivary concentrations of microbial and cariogenic bacteria, such as S. mutans and lactobacilli were reported. Outcomes related to carious lesions and lesion characteristics, such as fluorescence loss or lesion area, were also recorded. The range of follow-up times for outcome assessment was between 1 month after initiation of treatment and 18 months; however, two retrospective studies8,21 reported outcomes pertaining to evaluation after completion of orthodontic treatment, considering the whole treatment duration.
Risk of Bias within Studies
The risk of bias for the RCTs included in the present systematic review ranged from low to high overall. The latter primarily pertained to suboptimal reporting of randomisation practices in 2 of the studies; a classification of high risk of bias was decided in this respect, as identified problems with randomisation practices would potentially induce selection bias. Identified issues with inadequate reporting were also related to deviations from intended interventions and missing outcome data (Table 2, supplementary Table 1).
Table 2.
Risk of bias of included randomised controlled trials with the RoB 2.0 tool
| Study | Randomisation | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported result | Overall |
|---|---|---|---|---|---|---|
| Abbate et al, 2015 | Low | Low | Low | Some concerns | Some concerns | Some concerns |
| Albhaisi et al, 2020 | Low | Some concerns | Low | Low | Low | Some concerns |
| Chhibber et al, 2017 | Low | Low | Some concerns | Low | Low | Some concerns |
| Gujar et al, 2019 | Low | Low | Low | Low | Low | Low |
| Levrini et al, 2013 | High | Low | Low | Low | Low | High |
| Levrini et al, 2015 | High | Some concerns | High | Low | Low | High |
Supplementary Table 1.
Detailed assessment of RoB 2.0 tool.
| Domain | Reference | Abbate et al. 2015 | Albhaisi et al. 2020 | Chibber et al. 2017 | Gujar et al. 2019 | Levrini et a. 2013 | Levrini et al. 2015 |
|---|---|---|---|---|---|---|---|
| 1. Randomization process | 1.1 | Y | Y | Y | NI | Y | Y |
| 1.2 | NI | PY | Y | NI | NI | NI | |
| 1.3 | PN | M | N | N | Y | Y | |
| Assessor’s Judgement | Low | Low | Low | Low | High | High | |
| 2. Deviations from intended interventions | 2.1 | Y | Y | Y | Y | Y | Y |
| 2.2 | Y | Y | Y | Y | Y | Y | |
| 2.3 | N | NA | PN | N | PN | NI | |
| 2.4 | NA | NA | NA | NA | NA | NA | |
| 2.5 | NA | NA | NA | NA | NA | NA | |
| 2.6 | PY | PN | PN | Y | PY | PY | |
| 2.7 | NA | NA | NA | NA | NA | NA | |
| Assessor’s Judgement | Low | Some concerns | Low | Low | Low | Some concerns | |
| 3. Mising outcome data | 3.1 | N | Y | N | Y | PY | NI |
| 3.2 | PN | NA | PN | NA | NA | PN | |
| 3.3 | PN | NA | PY | NA | NA | NI | |
| 3.4 | NA | NA | PN | NA | NA | NI | |
| Assessor’s judgement | Low | Low | Some concerns | Low | Low | High | |
| 4. Measurement of the outcome | 4.1 | N | N | N | N | N | N |
| 4.2 | PN | N | N | N | PN | PN | |
| 4.3 | NI | N | N | N | PN | PN | |
| 4.4 | PY | NA | NA | NA | NA | NA | |
| 4.5 | N | NA | NA | NA | NA | NA | |
| Assessor’s Judgement | Some concerns | Low | Low | Low | Low | Low | |
| 5. Selection of the reported result | 5.1 | Y | Y | Y | Y | PY | PY |
| 5.2 | NI | N | N | N | PN | PN | |
| 5.3 | PN | N | N | N | PN | PN | |
| Assessor’s Judgement | Some concerns | Low | Low | Low | Low | Low | |
| Overall | Assessor’s Judgement | Some concerns | Some concerns | Some concerns | Low | High | High |
| Note | - | - | - | - | - | - |
N, no; NA, not applicable; NI, no information; PN, probably no; PY, probably yes; Y, yes
Among the non-randomised studies, those that were not prospective were deemed to be at serious risk of bias, mainly due to confounding issues or bias related to selection of participants to be included in the studies. With regard to prospective clinical trials, studies were categorised within the range of low to serious risk of bias. The most severely impacted domains were undetected confounding and subsequent risk for selection bias, while also the risk of detection bias and systematic differences in the measurement of the outcomes could not be neglected (Table 3, supplementary Table 2).
Table 3.
Risk of bias of included non-randomised studies according to the ROBINS-I tool
| Bias due to / in… | ||||||||
|---|---|---|---|---|---|---|---|---|
| Confounding | Selection of participants for the study | Classification of interventions | Deviations from intended interventions | Missing data | Measurement of outcomes | Selection of the reported result | Overall | |
| Azaripour et al, 2015 | Serious | Serious | Low | Low | Low | Moderate | Low | Serious |
| Buschang et al, 2018 | Serious | Serious | Low | Low | Low | Low | Low | Serious |
| Dallel et al, 2020 | Moderate | Low | Low | Low | Low | Moderate | Low | Moderate |
| Gujar et al, 2020 | Low | Low | Low | Low | Low | Low | Low | Low |
| Han et al, 2015 | Serious | Serious | Low | Low | Low | Moderate | Low | Serious |
| Karkhanetci et al, 2013 | Moderate | Low | Low | Low | Moderate | Moderate | Low | Moderate |
| Madariaga et al, 2020 | No Information | No Information | Low | Low | Low | No Information | Low | No Information |
| Miethke et al 2005 | Serious | No Information | Low | Low | No Information | No Information | No Information | Serious |
| Miethke et al, 2007 | Serious | No Information | Low | Low | No Information | No Information | No Information | Serious |
| Mulla Issa et al, 2020 | Serious | Serious | Low | Low | Low | Moderate | Low | Serious |
| Mummolo et al, 2020a | Serious | Low | Low | Low | Low | Low | Low | Serious |
| Mummolo et al, 2020b | Serious | Low | Low | Low | Low | Low | Low | Serious |
| Sifakakis et al, 2018 | Moderate | Low | Low | Low | Low | Low | Low | Moderate |
| Srinath et al, 2016 | No Information | No Information | Low | Low | No Information | Moderate | No Information | Moderate |
| Wang et al, 2019 | Low | Low | Low | Low | Low | Low | Low | Low |
Supplementary Table 2.
Detailed assessment of included non-randomized studies with the ROBINS-I tool.
| Domain | Reference | Azaripour et al. 2015 | Buschang et al. 2018 | Dallel et al. 2020 | Gujar et al. 2020 | Han et al. 2015 | Karhanetci et al. 2013 | Madariaga et al. 2020 | Miethke et al. 2005 | Miethke et al. 2007 | Mulla Issa et al. 2020 | Mummolo et al. 2020a | Mummolo et al. 2020b | Sifakakis et al. 2018 | Srinath et al. 2016 | Wang et al. 2019 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Confounding | 1.1 | Y | Y | Y | Y | Y | PY | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 1.2 | N | N | N | N | N | N | N | N | N | N | N | N | N | PN | N | |
| 1.3 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| 1.4 | PN | PN | Y | Y | PN | Y | PY | PN | PN | PN | PN | PN | Y | NI | Y | |
| 1.5 | NA | NA | Y | Y | NA | Y | PY | NA | NA | NA | NA | NA | Y | NA | Y | |
| 1.6 | N | NA | N | N | NA | N | N | NA | NA | NA | NA | NA | N | NI | N | |
| 1.7 | PN | PN | NA | Y | PN | Y | NI | PN | PN | PN | PN | PN | Y | NI | Y | |
| 1.8 | NA | NA | NA | Y | NA | Y | NA | NA | NA | NA | NA | NA | Y | NA | Y | |
| Judgement | Serious | Serious | Moderate | Low | Serious | Moderate | NI | Serious | Serious | Serious | Serious | Serious | Moderate | NI | Low | |
| 2. Selection of participants into the study | 2.1 | PY | PY | N | N | PY | N | N | NI | NI | PY | N | N | N | NI | N |
| 2.2 | PY | PY | NA | NA | PY | NA | NA | NA | NA | PY | NA | NA | NA | NI | NA | |
| 2.3 | PY | PY | NA | NA | PY | NA | NA | NA | NA | PY | NA | NA | NA | NI | NA | |
| 2.4 | Y | Y | Y | Y | Y | Y | PN | NI | NI | Y | Y | Y | Y | PY | Y | |
| 2.5 | PN | PN | NA | NA | PN | NA | NI | NA | NA | PN | NA | NA | NA | NI | NA | |
| Judgement | Serious | Serious | Low | Low | Serious | Low | NI | NI | NI | Serious | Low | Low | Low | NI | Low | |
| 3. Classification of interventions | 3.1 | Y | Y | Y | Y | Y | Y | Y | NI | NI | Y | Y | Y | Y | Y | Y |
| 3.2 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | |
| 3.3 | N | PN | N | N | N | N | N | Y | Y | NI | N | N | N | PN | N | |
| Judgement | Low | Low | Low | Low | Low | Low | Low | PN | PN | Low | Low | Low | Low | Low | Low | |
| 4. Deviations from intended interventions | 4.1 | N | N | N | N | N | N | PN | PN | PN | N | N | N | N | PN | N |
| 4.2 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| 4.3 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| 4.4 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| 4.5 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| 4.6 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| Judgement | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | |
| 5. Missing data | 5.1 | PY | Y | Y | Y | Y | N | PY | NI | NI | Y | Y | Y | Y | NI | N |
| 5.2 | NP | N | N | N | N | Y | PN | NI | NI | N | N | N | N | NI | N | |
| 5.3 | PN | N | N | N | N | N | PN | NI | NI | N | N | N | N | NI | N | |
| 5.4 | NA | NA | NA | NA | NA | PY | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| 5.5 | NA | NA | NA | NA | NA | N | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| Judgement | Low | Low | Low | Low | Low | Moderate | Low | NI | NI | Low | Low | Low | Low | NI | Low | |
| 6. Measurement of outcomes | 6.1 | PN | N | PN | N | PN | PN | PN | N | N | PY | PN | PN | N | N | N |
| 6.2 | PY | NI | Y | N | Y | PY | NI | NI | NI | Y | N | N | PN | Y | NI | |
| 6.3 | Y | Y | Y | Y | Y | Y | Y | PY | PY | Y | Y | Y | Y | Y | Y | |
| 6.4 | N | N | N | N | N | N | PN | PN | PN | PN | N | N | N | PN | N | |
| Judgement | Moderate | Low | Moderate | Low | Moderate | Moderate | NI | NI | NI | Moderate | Low | Low | Low | Moderate | Low | |
| 7. Selection of the reported result | 7.1 | N | N | N | N | PN | N | PN | N | N | N | PN | PN | N | NI | N |
| 7.2 | N | N | N | N | PN | N | PN | NI | NI | N | N | N | N | NI | N | |
| 7.3 | N | N | N | N | PN | N | PN | PN | PN | N | N | N | N | NI | N | |
| Judgement | Low | Low | Low | Low | Low | Low | Low | NI | NI | Low | Low | Low | Low | NI | Low | |
| Overall | Judgement | Serious | Serious | Moderate | Low | Serious | Moderate | NI | Serious | Serious | Serious | Serious | Serious | Low | Moderate | Low |
N, no; NA, not applicable; NI, no information; PN, probably no; PY, probably yes; Y, yes
Effects of Interventions, Meta-Analysis and Additional Analyses
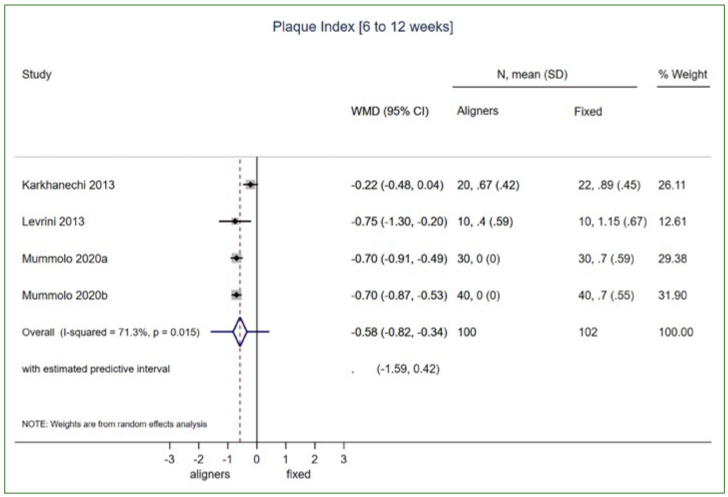
Overall, 4 studies were included in the meta-analysis, all related to periodontal outcomes (Table 4). Synthesised data were available only for adult patients undergoing treatment with either aligners of fixed appliances. Again, synthesised data (i.e. ≥ 2 studies) of the 4 eligible studies involved only patients treated with Invisalign (Align Technology). Patients undergoing aligner orthodontic treatment presented summary PI scores 0.58 lower than those treated with standard fixed appliances, within the first 6 to 12 weeks of treatment (4 studies: MD: -0.58; 95%CI: -0.82, -0.34; p < 0.001; I2: 71.3%; prediction interval: -1.59, 0.42; Fig 2). This finding was supported by a decreased PD of 0.42 mm in aligner patients (2 studies: MD: -042; 95%CI: -0.71, -0.12; p = 0.006; I2: 85.8%). In contrast, inflammation and bleeding indices, such as BOP and GI, did not reveal statistically significant differences between the aligner and fixed-appliance treatment groups during the same timeline of 6 to 12 weeks in adult patients (Table 4).
Table 4.
Results of meta-analyses and single study estimates related to periodontal outcomes (aligners vs fixed appliances)
| Synthesis | No. of studies | Effect measure (MD) | 95% CI | p-value | I2 (%) | Tau-squared (T2) |
|---|---|---|---|---|---|---|
| Adults | ||||||
| PI (6 to 12 weeks)1 | 4 | -0.58 | -0.82, -0.34 | <0.001 | 71.3 | 0.04 |
| BOP (6 to 12 weeks)2 | 2 | -0.26 | -0.77, 0.26 | 0.33 | 85.8 | 0.12 |
| PD (6 to 12 weeks)2 | 2 | -0.42 | -0.71, -0.12 | 0.006 | 34.7 | 0.02 |
| GI (6 to 12 weeks)3 | 1 | -0.10 | -0.35, 015 | 0.43 | – | – |
| Adolescents | ||||||
| PI (18 months)4 | 1 | -0.40 | -0.77, -0.03 | 0.04 | – | – |
| s-PI (1 month)5 | 1 | -14.78 | -16.74, -12.82 | <0.001 | – | – |
| GI (18 months)4 | 1 | -0.57 | -0.93, -0.21 | 0.002 | – | – |
| s-GI (1 month)5 | 1 | -8.46 | -10.47, -6.45 | <0.001 | – | – |
| FMPS (12 months)6 | 1 | -43.48 | -47.65, -39.31 | <0.001 | – | – |
| FMBS (12 months)6 | 1 | -20.44 | -22.98, -17.90 | <0.001 | – | – |
BOP, bleeding on probing; CI, confidence interval; FMBS, fullmouth bleeding score; FMPS, fullmouth plaque score; GI, gingival index; MD, mean difference; PI, plaque Index; PD, pocket depth; s-PI, simplified plaque index; s-GI, simplified gingival index. 1Karkhanechi et al 2013, Levrini et al 2013, Mummolo et al 2020a, Mummolo et al 2020b; 2Karkhanechi et al 2013, Levrini et al 2013; 3Karkhanechi et al 2013; 4Chhibber et al 2018; 5Sifakakis et al 2018; 6Abbate et al 2015.
Fig 2.
Random effects meta-analysis for summary mean difference (with 95% CI) in overall plaque index (PI) scores in adults undergoing aligner orthodontic treatment compared to standard fixed appliances, within the first 6 to 12 weeks of treatment initiation.
Based on the available studies, only single study estimates could be recorded in relation to adolescent patients, while no mathematical synthesis was possible. Based on these estimates, plaque and gingival/ bleeding scores appeared lower for teenagers treated with aligners. According to the single study10 with the longer follow-up period (i.e. 18 months), PI scores for the aligner group was 0.40 lower than the corresponding figure for fixed appliances (1 study: MD: -0.40; 95%CI: -0.77, -0.03; p = 0.04); additionally, GI was 0.57 lower in aligners compared to fixed appliances (1 study: MD: -0.57; 95%CI: -0.93, -0.21; p = 0.002). Results from the other two studies28,46 with shorter follow-up periods confirmed this (Table 4).
Regarding microbiological parameters in adult patients, 4 meta-analyses, each comprising 2 studies from the same group, were deemed possible (Table 5). The risk of S. mutans presence in detectable concentrations (colony forming units, CFU > 105) for a period of 3 to 6 months after initiation of treatment was 74% to 93% lower in aligner patients (2 studies/3 months: RR: 0.07; 95%CI: 0.01, 0.49; p = 0.008; I2 = 0.0%; 2 studies/6 months: RR: 0.22; 95%CI: 0.10, 0.51; p = 0.001; I2 = 0.0%). Likewise, the risk of lactobacilli occurrence (CFU > 105) in a similar time interval was 81% to 91% lower in aligner groups (2 studies/3 months: RR: 0.09; 95%CI: 0.02, 0.47; p = 0.004; I2 = 0.0%; 2 studies/ 6 months: RR: 0.19; 95%CI: 0.08, 0.45; p < 0.001; I2 = 56.9%) (Table 5).
Table 5.
Results of meta-analyses and single study estimates, related to microbiologic parameters (aligners vs fixed appliances)
| Synthesis | No. of studies | Effect measure | 95% CI | p-value | I2 (%) | Tau-squared (T2) |
|---|---|---|---|---|---|---|
| Adults | ||||||
| S. mutans (CFU > 105, 3 months)1 | 2 | RR: 0.07 | 0.01, 0.49 | 0.008 | 0.0 | – |
| S. mutans (CFU > 105, 6 months)1 | 2 | RR: 0.22 | 0.10, 0.51 | 0.001 | 0.0 | – |
| Lactobacilli (CFU > 105, 3 months)1 | 2 | RR: 0.09 | 0.02, 0.47 | 0.004 | 0.0 | – |
| Lactobacilli (CFU > 105, 6 months)1 | 2 | RR: 0.19 | 0.08, 0.45 | <0.001 | 56.9 | – |
| Adolescents | ||||||
| S. mutans (presence, 1 month)2 | 1 | RR: 0.86 | 0.64, 1.14 | 0.29 | – | – |
| S. mutans (counts: 5th root, 1 month)2 | 1 | MD: -2.22 | -6.82, 2.38 | 0.34 | – | – |
In contrast, in adolescents, evidence from a single study estimate46 on the risk of S. mutans colonisation did not showe a statistically significant difference between the groups under examination. However, these findings were derived from a short-term evaluation of 1 month after initiation of treatment (1 study: aligners vs fixed appliances, RR: 0.86; 95%CI: 0.64, 1.14; p = 0.29) (Table 5).
Data related to incipient caries/WSLs were derived only from single-study estimates of two recently published studies.2,11 According to these findings, adult patients presented a 28% lower risk for the development of WSLs (on tooth level) when assessed over a 3-month period (1 study, RR: 0.72; 95%CI: 0.60, 0.86; p < 0.001). Moreover, average fluorescence loss, denoting mineral tissue loss, was lower in aligner-treated patients (1 study, mean difference [MD]: -1.40; 95%CI: -2.15, -0.65; p < 0.001). Interestingly, however, when the lesion area (in pixels) was examined, patients treated with aligners presented an increased area of decalcification (1 study, MD: 80.50; 95%CI: 60.52, 100.48; p < 0.001). In contrast, no difference in the formation of WSLs (patient level) was detected in adolescent patients between the two different orthodontic treatment techniques (1 study, aligners vs fixed appliances, RR: 0.33; 95%CI: 0.10, 1.04; p = 0.06) (Table 6).
Table 6.
Results of single study estimates, related to WSLs (aligners vs fixed appliance)
| Synthesis | No. of studies | Effect measure | 95% CI | p-value | I2 (%) | Tau-squared (T2) |
|---|---|---|---|---|---|---|
| Adults | ||||||
| WSLs (tooth level/3 months)1 | 1 | RR: 0.72 | 0.60, 0.86 | <0.001 | – | – |
| Average fluorescence loss (ΔF%), 3 months1 | 1 | MD: -1.40 | -2.15, -0.65 | <0.001 | – | – |
| Lesion area (pixels), 3 months1 | 1 | MD: 80.50 | 60.52, 100.48 | <0.001 | – | – |
| Adolescents | ||||||
| WSLs (patient level/ 9 months)2 | 1 | RR: 0.33 | 0.10, 1.04 | 0.06 | – | – |
Further sensitivity analysis or publication bias assessment was ultimately not conducted due to the paucity of existing studies contributing to the quantitative synthesis.
Quality of Evidence
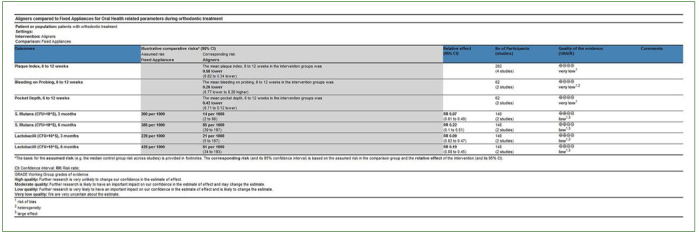
The quality of the existing evidence for the outcomes assessed after data synthesis ranged from very low to low overall, based on a limited number of pooled studies. Specifically, for PI and PD indices, the quality of the evidence was recorded as very low, based on a combination of randomised and non-randomised (prospective) studies and due to risk of bias suspected for contributing studies. In addition, for BOP, the certainty of the evidence was downgraded for heterogeneity reasons as well. For microbiological parameters, and based on the syntheses of non-randomised (prospective) data, the quality of evidence was downgraded due to problems with the internal validity of the contributing studies, while it was upgraded as a result of identification of a large pooled effect. As such, the certainty of evidence was ultimately rated as low overall (Fig 3).
Fig 3.
Assessment of the quality of the available evidence based on synthesised data, according to GRADE
Discussion
Findings in Context and Previous Research
Aligner treatment has become a popular option among patients, thanks to aesthetic considerations and perceived ease and comfort of the therapeutic procedures. Maintaining an acceptable level of oral hygiene is of paramount importance for the duration of treatment to avoid any adverse effects related to loss of tooth integrity and periodontal health.
While acknowledging all limitations of the present study and the synthesised data, there is some evidence that orthodontic treatment with aligners might prove beneficial at least in the short-term, especially for adult patients. The present study is the first systematic review to consider all contemporary evidence on oral hygiene parameters related to orthodontic treatment with aligners, including periodontal parameters, microbiological parameters as well as incipient caries/white spot lesions. It thus constitutes a global and comprehensive evaluation of the efficacy of contemporary orthodontic appliances in helping maintain high levels of oral hygiene during treatment.
Previous studies in the field of oral hygiene and competing intervention procedures for orthodontic tooth movement have either shown a scarcity of evidence, being based on very few early reports up to 2015,45 or found clear aligner treatment to be more effective. The evidence was still heterogeneous and not of high quality, with a specific focus on periodontal health.26 Jiang et al16 concluded superior periodontal health status based on evidence from PI and GI, although the quality of the evidence was not high, mainly due to the risk of bias and inconsistency of the results. It is noteworthy that increased variability in synthesised data contributed to the pooled estimate concerning types of study designs included in this earlier review, as well as follow-up times and patient ages.17
Based on our findings from a short-term evaluation period (up to 6 months under treatment) mainly concerning adult patients, plaque scores along with microbial counts related to tooth decay demonstrate that aligner treatment may qualify as a treatment option that potentially offers improved oral hygiene status. However, it may be argued that such findings cannot be directly related to permanent effects on the periodontal apparatus or tooth integrity of a patient undergoing orthodontic treatment with standard fixed appliances. In addition, the clinical implications of the identified differences might be negligible or constitute a somewhat fragile and transient component. In support of that, and based on the prediction interval related to the meta-analysis of PI scores, the expected effects of aligner treatment in future trials or settings might document improved oral hygiene status – or not.
Following the initial use of orthodontic aligner and their utilisation in more complex orthodontic cases, thanks to the latest technological developments, attachment grips bonded onto the enamel have been introduced, with growing and large-scale applications in practice.16,24 Such adjuncts may vary in dimensions and morphology, ranging from 2 mm to 5 mm, and also demonstrate increased width, often exceeding 1 mm.12 Such variations are usually required to increase aligner retention to the dentition while also facilitatiing force generation and induction of 3-dimensional movements. The shortcomings of the wide use of bonded grips and bulky composites on tooth enamel are associated with an increased potential for food, plaque, and microbial accumulation, as well as biofilm formation,50 thus compromising the oral health of the treated individual. Intraoral aging of both the aligner material and the attachment have been linked to alteration of material properties, which may, in turn, influence oral hygiene.41 Plaque can accumulate very soon after initial bonding, while a crucial determinant of biofilm adhesion ability is surface roughness.44 A rough surface enables bacterial adhesion to the material, forming a relatively protected environment for microbes against oral hygiene measures.14 A recent in vitro study demonstrated no differences between different types of aligner materials in terms of initial bacterial attachment levels and biofilm formation with metal brackets.50 Only one of the studies included in the present systematic review reported on the use of attachments.2 That study concluded that at least within the first 3 months of treatment, both fixed appliances and aligners induced incipient caries in the form of WSLs, although the WSLs differed. Orthodontic aligners were associated with shallower lesions with a larger area, which were mainly attributed to the bulky shape of the attachments. In contrast, patients treated with fixed appliances developed smaller lesions but with increased mineral loss and sites of decalcified tissue. Future studies should be designed for a more in-depth assessment of the influence of different types and shapes of attachment grips on enamel and tooth integrity.
Considering the synthesised data, indices related to periodontal inflammation, such as BOP in adults, did not strictly follow the findings from microbiological and plaque-related parameters. This, in turn, might indicate the reversible nature of the initial disruption of oral hygiene parameters shortly after the beginning of orthodontic treatment, at least for adult patients. On the other hand, findings from single studies examining the response of adolescents to orthodontic appliances confirm a more thorough short-term disruption of oral health parameters; thus, certain groups of patients might be considered more prone to limited compliance with oral hygiene measures and qualify as high-susceptibility patients during standard-appliance orthodontic treatment, at least in the short term. Apparently, additional measures of oral hygiene reinforcement in adolescent patients should be considered.25 In contrast, another single study reported no statistically significant differences in periodontal parameters related to fixed vs aligner therapy, indicating better oral-hygiene maintenance in such patients.21 However, in this respect, further and more comprehensive studies are needed to strengthen the available evidence.
Clinically, appliance type and treatment strategy for orthodontic tooth movement should be selected to optimise treatment outcome and safety, bearing in mind the long-term nature of orthodontic treatment and the retention period. Recently, it has been argued that orthodontic treatment with aligners – compared to gold-standard fixed appliances – in adult patients yields less effective treatment outcomes in terms of achieving occlusal goals.42,43 Hence, one should carefully weigh clinical outcomes, potential temporary adverse effects during treatment, treatment duration, and patient values before treatment initiation, ensuring that the patient is well-informed and consulted about treatment planning.15
Strengths and Limitations
The present systematic review and meta-analysis provide the current state of evidence regarding oral hygiene parameters in general and during orthodontic treatment, comparing traditional fixed appliances with contemporary orthodontic aligners. It was performed strictly following prospective protocol development and registration, while an unconditional search strategy was applied to both published and unpublished literature for study identification and selection. Quantitative syntheses, risk of bias assessment, and evaluation of the certainty of the evidence were performed in line with reporting guidelines. Heterogeneity problems were acknowledged, and populations of different ages were examined separately, as these may demonstrate different mentalities in relation to oral hygiene measures and parameters. Pooled estimates were solely based on prospectively collected data, to ensure bias elimination.
However, limitations do exist. First and foremost are the quality and certainty of the evidence identified, although this is chiefly related to the primary studies included in the review. In addition, a relatively small number of studies were included in the quantitative synthesis. This may have allowed imprecision in the pooled estimates overall, while no additional analyses were conducted due to the scarcity of studies eligible for syntheses. Moreover, no follow-up time longer than 6 months of treatment could be included in the meta-analyses, given the available primary data and the heterogeneity of individual study settings.
Conclusions
Aligner orthodontic therapy is associated with better oral hygiene levels in the short term; however, this is not corroborated by a high level of certainty of the available evidence. Therefore, any extrapolation to contemporary aligner techniques and adjuncts, such as attachment grips, is only speculative.
Acknowledgements
We would like to thank the authors of the studies for kindly providing additional data on their studies (registration: Open Science Framework https://osf.io/txgj6/)
Appendix 1. Search strategy for Medline (via PubMed)
PubMed (MEDLINE)
All Fields
Date: May 31st, 2021
Filters: none
Orthodontic aligner
Orthodontic aligner*
Invisalign
Clear orthodontic aligner
Thermoplastic orthodontic aligner
Vacuum-formed orthodontic aligner
Vacuum-formed orthodontic aligner
1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7
Gingival index
Plaque index
Early caries
Incipient caries
Caries
Tooth decay
Bleeding
Oral hygiene
Periodontal health
Recession
Probing depth
S. mutans
Streptococcus mutans
Lactobacilli
Lactobacillus
Oral microbiome
9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24
8 AND 25
References
- Abbate GM, Caria MP, Montanari P, Mannu C, Orrù G, Caprioglio A, et al. Periodontal health in teenagers treated with removable aligners and fixed orthodontic appliances. J Orofac Orthop. 2015;76:240–250. doi: 10.1007/s00056-015-0285-5. [DOI] [PubMed] [Google Scholar]
- Albhaisi Z, Al-Khateeb SN, Abu Alhaija ES. Enamel demineralization during clear aligner orthodontic treatment compared with fixed appliance therapy, evaluated with quantitative light-induced fluorescence: A randomized clinical trial. Am J Orthod Dentofacial Orthop. 2020;157:594–601. doi: 10.1016/j.ajodo.2020.01.004. [DOI] [PubMed] [Google Scholar]
- Alhaija ESA, Al-Saif EM, Taani DQ. Periodontal health knowledge and awareness among subjects with fixed orthodontic appliance. Dental Press J Orthod. 2018;23:40, e41–40.e49. doi: 10.1590/2177-6709.23.5.40.e1-9.onl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Zainal MH, Anvery S, Al-Jewair T. Clear aligner therapy may not prevent but may decrease the incidence of external root resorption compared to full fixed appliances. J Evid Based Dent Pract. 2020;20:101438. doi: 10.1016/j.jebdp.2020.101438. [DOI] [PubMed] [Google Scholar]
- Atack NE, Sandy JR, Addy M. Periodontal and microbiological changes associated with the placement of orthodontic appliances. A review. J Periodontol. 1996;67:78–85. doi: 10.1902/jop.1996.67.2.78. [DOI] [PubMed] [Google Scholar]
- Azaripour A, Weusmann J, Mahmoodi B, Peppas D, Gerhold-Ay A, Van Noorden CJ, et al. Braces versus Invisalign®: gingival parameters and patients’ satisfaction during treatment: a cross-sectional study. BMC Oral Health. 2015;15:69. doi: 10.1186/s12903-015-0060-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baheti M, Toshniwal N. Survey on oral hygiene protocols among orthodontic correction-seeking individuals. J Edu Ethics Dentistry. 2015;5:8–13. [Google Scholar]
- Buschang PH, Chastain D, Keylor CL, Crosby D, Julien KC. Incidence of white spot lesions among patients treated with clear aligners and traditional braces. Angle Orthod. 2019;89:359–364. doi: 10.2319/073118-553.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerroni S, Pasquantonio G, Condò R, Cerroni L. Orthodontic fixed appliance and periodontal status: an updated systematic review. Open Dent J. 2018;12:614–622. doi: 10.2174/1745017901814010614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chhibber A, Agarwal S, Yadav S, Kuo CL, Upadhyay M. Which orthodontic appliance is best for oral hygiene? A randomized clinical trial. Am J Orthod Dentofacial Orthop. 2018;153:175–183. doi: 10.1016/j.ajodo.2017.10.009. [DOI] [PubMed] [Google Scholar]
- Dallel I, Ben Salem I, Merghni A, Bellalah W, Neffati F, Tobji S, et al. Influence of orthodontic appliance type on salivary parameters during treatment. Angle Orthod. 2020;90:532–538. doi: 10.2319/082919-562.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasy H, Dasy A, Asatrian G, Rózsa N, Lee HF, Kwak JH. Effects of variable attachment shapes and aligner material on aligner retention. Angle Orthod. 2015;85:934–940. doi: 10.2319/091014-637.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliades T, Eliades G, Brantley WA. Microbial attachment on orthodontic appliances: I. Wettability and early pellicle formation on bracket materials. Am J Orthod Dentofacial Orthop. 1995;108:351–360. doi: 10.1016/s0889-5406(95)70032-3. [DOI] [PubMed] [Google Scholar]
- Eliades T, Koletsi D. Minimizing the aerosol-generating procedures in orthodontics in the era of a pandemic: Current evidence on the reduction of hazardous effects for the treatment team and patients. Am J Orthod Dentofacial Orthop. 2020;158:330–342. doi: 10.1016/j.ajodo.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliades T, Papageorgiou SN, Ireland AJ. The use of attachments in aligner treatment: Analyzing the “innovation” of expanding the use of acid etching-mediated bonding of composites to enamel and its consequences. Am J Orthod Dentofacial Orthop. 2020;158:166–174. doi: 10.1016/j.ajodo.2020.04.008. [DOI] [PubMed] [Google Scholar]
- Flores-Mir C. Clear aligner therapy might provide a better oral health environment for orthodontic treatment among patients at increased periodontal risk. J Evid Based Dent Pract. 2019;19:198–199. doi: 10.1016/j.jebdp.2019.05.006. [DOI] [PubMed] [Google Scholar]
- Gujar AN, Al-Hazmi A, Raj AT, Patil S. Microbial profile in different orthodontic appliances by checkerboard DNA-DNA hybridization: An in-vivo study. Am J Orthod Dentofacial Orthop. 2020;157:49–58. doi: 10.1016/j.ajodo.2019.01.026. [DOI] [PubMed] [Google Scholar]
- Gujar AN, Baeshen HA, Alhazmi A, Bhandi S, Raj AT, Patil S, et al. Cytokine levels in gingival crevicular fluid during orthodontic treatment with aligners compared to conventional labial fixed appliances: a 3-week clinical study. Acta Odontol Scand. 2019;77:474–481. doi: 10.1080/00016357.2019.1607548. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han J-Y. A comparative study of combined periodontal and orthodontic treatment with fixed appliances and clear aligners in patients with periodontitis. J Periodontal Implant Sci. 2015;45:193–204. doi: 10.5051/jpis.2015.45.6.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennessy J, Al-Awadhi EA. Clear aligners generations and orthodontic tooth movement. J Orthod. 2016;43:68–76. doi: 10.1179/1465313315Y.0000000004. [DOI] [PubMed] [Google Scholar]
- Iliadi A, Koletsi D, Eliades T. Forces and moments generated by aligner-type appliances for orthodontic tooth movement: A systematic review and meta-analysis. Orthod Craniofac Res. 2019;22:248–258. doi: 10.1111/ocr.12333. [DOI] [PubMed] [Google Scholar]
- Iliadi A, Koletsi D, Papageorgiou SN, Eliades T. Safety considerations for thermoplastic-type appliances used as orthodontic aligners or retainers. a systematic review and meta-analysis of clinical and in-vitro research. Materials (Basel) 2020;13:1843. doi: 10.3390/ma13081843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang C, Fan C, Yu X, Xu T, Cai J, Fan X, et al. Comparison of the efficacy of different periodic periodontal scaling protocols for oral hygiene in adolescents with fixed orthodontic appliances: A prospective cohort study. Am J Orthod Dentofacial Orthop. 2021;159:435–442. doi: 10.1016/j.ajodo.2020.01.026. [DOI] [PubMed] [Google Scholar]
- Jiang Q, Li J, Mei L, Du J, Levrini L, Abbate GM, et al. Periodontal health during orthodontic treatment with clear aligners and fixed appliances: A meta-analysis. J Am Dent Assoc. 2018;149:712–720. e712. doi: 10.1016/j.adaj.2018.04.010. [DOI] [PubMed] [Google Scholar]
- Kadu A, Chopra S, Jayan B, Kochar GD. Effect of the personality traits of the patient on pain perception and attitude toward orthodontic treatment. J Indian Orthod Soc. 2015;49:89. [Google Scholar]
- Karkhanechi M, Chow D, Sipkin J, Sherman D, Boylan RJ, Norman RG, et al. Periodontal status of adult patients treated with fixed buccal appliances and removable aligners over one year of active orthodontic therapy. Angle Orthod. 2013;83:146–151. doi: 10.2319/031212-217.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ke Y, Zhu Y, Zhu M. A comparison of treatment effectiveness between clear aligner and fixed appliance therapies. BMC Oral Health. 2019;19:24. doi: 10.1186/s12903-018-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levrini L, Abbate GM, Migliori F, Orrù G, Sauro S, Caprioglio A. Assessment of the periodontal health status in patients undergoing orthodontic treatment with fixed or removable appliances. A microbiological and preliminary clinical study. Cumhuriyet Dent J. 2013;16:296–307. [Google Scholar]
- Levrini L, Mangano A, Montanari P, Margherini S, Caprioglio A, Abbate GM. Periodontal health status in patients treated with the Invisalign(®) system and fixed orthodontic appliances: A 3 months clinical and microbiological evaluation. Eur J Dent. 2015;9:404–410. doi: 10.4103/1305-7456.163218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madariaga ACP, Bucci R, Rongo R, Simeon V, D’Antò V, Valletta R. Impact of fixed orthodontic appliance and clear aligners on the periodontal health: a prospective clinical study. Dent J (Basel) 2020;8:4. doi: 10.3390/dj8010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maspero C, Farronato D, Giannini L, Farronato G. Orthodontic treatment in elderly patients. Prog Orthod. 2010;11:62–75. doi: 10.1016/j.pio.2010.04.008. [DOI] [PubMed] [Google Scholar]
- Miethke RR, Brauner K. A Comparison of the periodontal health of patients during treatment with the Invisalign system and with fixed lingual appliances. J Orofac Orthop. 2007;68:223–231. doi: 10.1007/s00056-007-0655-8. [DOI] [PubMed] [Google Scholar]
- Miethke R-R, Vogt S. A comparison of the periodontal health of patients during treatment with the Invisalign system and with fixed orthodontic appliances. J Orofacial Orthop [Fortschritte der Kieferorthopadie] 2005;66:219–229. doi: 10.1007/s00056-005-0436-1. [DOI] [PubMed] [Google Scholar]
- Miller KB, McGorray SP, Womack R, Quintero JC, Perelmuter M, Gibson J, et al. A comparison of treatment impacts between Invisalign aligner and fixed appliance therapy during the first week of treatment. Am J Orthod Dentofacial Orthop. 2007;131:302.e301–309. doi: 10.1016/j.ajodo.2006.05.031. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- Mulla Issa FHK, Mulla Issa ZHK, Rabah AF, Hu L. Periodontal parameters in adult patients with clear aligners orthodontics treatment versus three other types of brackets: A cross-sectional study. J Orthod Sci. 2020;9:4. doi: 10.4103/jos.JOS_54_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mummolo S, Nota A, Albani F, Marchetti E, Gatto R, Marzo G, et al. Salivary levels of Streptococcus mutans and Lactobacilli and other salivary indices in patients wearing clear aligners versus fixed orthodontic appliances: An observational study. PLoS One. 2020;15:e0228798. doi: 10.1371/journal.pone.0228798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mummolo S, Tieri M, Nota A, Caruso S, Darvizeh A, Albani F, et al. Salivary concentrations of Streptococcus mutans and Lactobacilli during an orthodontic treatment. An observational study comparing fixed and removable orthodontic appliances. Clin Exp Dent Res. 2020;6:181–187. doi: 10.1002/cre2.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papadopoulou AK, Cantele A, Polychronis G, Zinelis S, Eliades T. Changes in roughness and mechanical properties of Invisalign(®) appliances after one- and two-weeks use. Materials (Basel) 2019;12:2406. doi: 10.3390/ma12152406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papageorgiou SN, Koletsi D, Iliadi A, Peltomäki T, Eliades T. Comment on: Treatment outcome with orthodontic aligners and fixed appliances: a systematic review with meta-analyses. Eur J Orthod. 2020;42:344–346. doi: 10.1093/ejo/cjz101. [DOI] [PubMed] [Google Scholar]
- Papageorgiou SN, Koletsi D, Iliadi A, Peltomaki T, Eliades T. Treatment outcome with orthodontic aligners and fixed appliances: a systematic review with meta-analyses. Eur J Orthod. 2020;42:331–343. doi: 10.1093/ejo/cjz094. [DOI] [PubMed] [Google Scholar]
- Quirynen M, Bollen CM. The influence of surface roughness and surface-free energy on supra- and subgingival plaque formation in man. A review of the literature. J Clin Periodontol. 1995;22:1–14. doi: 10.1111/j.1600-051x.1995.tb01765.x. [DOI] [PubMed] [Google Scholar]
- Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Periodontal health during clear aligners treatment: a systematic review. Eur J Orthod. 2015;37:539–543. doi: 10.1093/ejo/cju083. [DOI] [PubMed] [Google Scholar]
- Sifakakis I, Papaioannou W, Papadimitriou A, Kloukos D, Papageorgiou SN, Eliades T. Salivary levels of cariogenic bacterial species during orthodontic treatment with thermoplastic aligners or fixed appliances: a prospective cohort study. Prog Orthod. 2018;19:25. doi: 10.1186/s40510-018-0230-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinath M, Reddy V, Reddy G, Ramyasree K, Swetha T, Sridhar M. Aligners: A boon for the gingival health of orthodontic patients. J Int Oral Health. 2016;8:490–493. [Google Scholar]
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- Tektas S, Thurnheer T, Eliades T, Attin T, Karygianni L. Initial bacterial adhesion and biofilm formation on aligner materials. Antibiotics (Basel) 2020;9:908. doi: 10.3390/antibiotics9120908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberg MJ, Riolo CS, Bayirli B, Riolo ML, Van Tubergen EA, Kulbersh R. Periodontal pathogen levels in adolescents before, during, and after fixed orthodontic appliance therapy. Am J Orthod Dentofacial Orthop. 2009;135:95–98. doi: 10.1016/j.ajodo.2007.02.057. [DOI] [PubMed] [Google Scholar]
- Wang Q, Ma J-B, Wang B, Zhang X, Yin Y-L, Bai H. Alterations of the oral microbiome in patients treated with the Invisalign system or with fixed appliances. Am J Orthod Dentofacial Orthop. 2019;156:633–640. doi: 10.1016/j.ajodo.2018.11.017. [DOI] [PubMed] [Google Scholar]
- Weir T. Clear aligners in orthodontic treatment. Aust Dent J. 2017;62(suppl 1):58–62. doi: 10.1111/adj.12480. [DOI] [PubMed] [Google Scholar]
- Zhao R, Huang R, Long H, Li Y, Gao M, Lai W. The dynamics of the oral microbiome and oral health among patients receiving clear aligner orthodontic treatment. Oral Dis. 2020;26:473–483. doi: 10.1111/odi.13175. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.