ABSTRACT
Background
While third‐level educational institutions have long provided counselling, a sharp rise in demand has led to limited access to mental health supports for many students, including those with ongoing difficulties. Digital mental health interventions represent one response to this unmet need, given the potential low cost and scalability associated with no‐to‐low human resources involved.
Objective
The aim of this study was to conduct a systematic review and meta‐analysis of the literature examining effectiveness of digital mental health interventions for university students with ongoing mental health difficulties.
Methods
The following databases were searched: PubMed, EBSCOhost (CINHAHL/PsycINFO/PsycArticles) and Web of Science. Two‐armed randomised‐control trials were included in the meta‐analysis. A random‐effects meta‐analysis was conducted and standardised mean differences were calculated. Effect sizes were then compared in terms of therapeutic approach, and whether interventions were fully automated or guided interventions. This study was registered with PROSPERO, CRD42024504265.
Results
Thirty four eligible studies were included in this narrative synthesis, of which 21 randomised‐controlled trials were included in the meta‐analysis. Random‐effects meta‐analysis indicated an overall medium effect size in favour of digital interventions for both depression (Cohen's d = 0.55), and anxiety (Cohen's d = 0. 46). Of note, for anxiety outcomes, fully automated interventions appeared more effective (d = 0.55) than guided interventions (d = 0.35).
Conclusions
Digital mental health interventions are associated with beneficial effects for college students when measured in terms of anxiety and depression symptom severity. For anxiety, fully automated interventions may be more effective than guided interventions to reduce symptom severity.
Keywords: digital mental health interventions, mental health difficulties, university students
1. Introduction
Mental health difficulties represent a growing global burden with up to 60% of young people meet the criteria for a diagnosis of depression and/or anxiety at any given point during their young adulthood (McGorry et al. 2024). The rising incidence of mental health difficulties in young people have consequently been described as representing a “dangerous phase” and an ignored risk factor for age‐related medical illness later in life (McGorry et al. 2024). Rates of mental health difficulties among young people have risen substantially in the last decade, representing a 78% increase in 2017 compared to 2008 (Twenge et al. 2019). Studies conducted in the US report that since the COVID‐19 pandemic, approximately 75% of young people have reported worsening mental health (Bell et al. 2023). These changes are reflected in multiple indicators, including perceived poor mental health (Wiens et al. 2020), anxiety disorders (Goodwin et al. 2020), and depression (Goodwin et al. 2022). Given that approximately 63% of mental health problems are established by the age of 25 (Solmi et al. 2022), early intervention for mental health difficulties in young adulthood is important and has potential to yield significant benefits across the lifespan (Kessler et al. 2005; D'Adamo et al. 2023). In western countries, a majority of 18–25‐year‐old attend some form of third level education; for example, the OECD (2022) estimate that an average of 54% attend some form of third level, siding to 59% in the EU22. By taking action long before mental health problems worsen or by preventing their onset (Colizzi, Lasalvia, and Ruggeri 2020), early intervention has the potential to avoid significant burden among college students including academic failure, interpersonal problems and substance abuse (King et al. 2021).
For young adults, the college years are particularly important as they can involve multiple social and academic stressors such as academic demands, financial worries, and loneliness, which increases the risk for mental health difficulties (Duffy et al. 2019; Campbell et al. 2022). Further, emerging adulthood, which coincides with transition to college, represents the peak period of risk for the onset of mental health problems (Kessler et al. 2007; Duffy et al. 2020). According to a 2017 WHO study of approximately 14 000 students from across eight countries, approximately one in three screened positive for at least one common DSM‐IV anxiety, mood, or substance disorder. Previous evidence shows that 25% of university students experience depression and 14% experience suicide related outcomes (Auerbach et al. 2018). Similarly, a longitudinal study by Duffy et al. (2020) revealed that one‐third of first‐year undergraduate students endorse clinically significant depressive and anxiety symptoms at entry to university.
Rates of mental health service utilisation among college students have also increased considerably (Lipson, Lattie, and Eisenberg 2019; Oswalt et al. 2020; Osborn et al. 2022). For example, in 2017, 94% of universities in the UK reported an increase in demand for counselling services compared to the prior five years (Thorley 2017; Worsley, Pennington, and Corcoran 2022). Similarly, a study in the US by Oswalt et al. (2020) using national data reported an increase of 4.3% in service utilisation among college students between 2009 and 2015. This has been challenging for students' mental health services, in terms of service provision and financing, resulting in longer waiting times (Walsh et al. 2022) and only short‐term interventions being made available with the consequent risk of not being able to provide quality treatment (Hallett 2012; Harrison and Gordon 2021).
In response to this high demand for mental health services among college students, there is a growing interest in the use of digital mental health interventions (DMHIs). DMHIs are digitally delivered interventions which may be based on well‐established psychological treatments (Gan et al. 2021). DMHIs have the potential to offer a scalable, cost‐effective, and accessible solution to increase access to mental health services and reduce burden on college service delivery systems (Lipson, Lattie, and Eisenberg 2019; Schueller and Torous 2020; Ha and Kim 2020), as they are capable of being directly accessible to people with no‐to‐low human resources, at any time of the day at the point of need, and have the potential to promote self‐management of mental health problems (Andersson and Titov 2014; Gan et al. 2021). Moreover, previous research on self‐help interventions for depressive symptoms and anxiety disorders on adult populations has shown promising results, suggesting that the effectiveness of these interventions is similar to in‐person mental health treatment (van't Hof, Cuijpers, and Stein 2009; Cuijpers et al. 2010; Leung et al. 2022).
1.1. Guided Versus Fully Automated Digital Interventions
Digital interventions have been sub‐categorised as either interventions that are fully digitally based/automated or interventions with some level of human support/guidance, e.g. from a therapist or peer. The later have been variously termed as ‘guided’ digital interventions (Pineda et al. 2023) or ‘blended’ digital interventions (Erbe et al. 2017; Valentine et al. 2020). In this study, we refer to the former as ‘fully automated’ interventions and the later as ‘guided’ interventions. Guided interventions can be further sub‐categorised into asynchronous therapy, where there is a delay between responses (e.g., emails and text), and synchronous therapy, which refers to methods where providers and clients communicate at the same time, such as a phone call or a video conference (Philippe et al. 2022).
This distinction between guided and fully automated digital interventions may be important in terms of level of engagement and adherence (Lattie et al. 2019). Forbes et al. (2023) defined adherence as “the actual digital intervention use compared with intended use” and engagement as “to which extent patients interact with an intervention.” Moreover, study attrition refers to “failure to complete the research protocol associated with an online intervention” (Linardon and Fuller‐Tyszkiewicz 2020). A wide range of engagement rates (26% and 100%; Stanic et al. 2021; Winter et al. 2022), and attrition rates (23%–64%; Linardon and Fuller‐Tyszkiewicz 2020) have been reported for digital interventions. A systematic review by Borghouts et al. (2021) suggested that interventions that include some levels of prompting were associated with improved adherence but appeared agnostic about whether this needed to come from another human or was simply an automated reminder. By comparison, research on traditional mental health care has suggested that human guidance is an important factor that increases intervention efficacy and therefore intervention engagement (Ebert et al. 2018; Musiat et al. 2022).
A number of psychological theories have provided suggestions as to why human support or guidance may be important for adherence. For example, the therapeutic alliance is suggested to benefit outcomes because of a collaborative agreement between therapist and client on the goals of the treatment, the tasks, and the development of a personal bond (Ardito and Rabellino 2011). By comparison, the supportive‐accountability model (Mohr, Cuijpers, and Lehman 2011) proposes that adherence to online interventions increases when human support is provided on account of a sense of accountability to a coach that is seen as trustworthy. However, mixed results have been reported on the influence of support in DMHIs, especially among college students, as some studies such as Harrer et al. (2018) reported that support did not affect intervention effectiveness, whereas others such as Conley et al. (2016) concluded that support yielded greater effects. Some of the reasons for this may be that the effectiveness of human support varies across populations and based on the characteristics (e.g., training level) of the support provider, which may explain the variability of these results (Werntz et al. 2023). Moreover, Harrer et al. (2018) proposed that for university students, there may be other factors that are more important than the provision of guidance but more research is needed to determine what these factors may be. The relevance of these hypothesised factors need to be evaluated in order to better understand the relationship between engagement and level of automaticity/guidance for college students (Harith et al. 2022).
1.2. Therapeutic Approach and Mode of Delivery
Other relevant factors in understanding young people's engagement with digital mental health interventions include the therapeutic approach and the mode of delivery. In terms of therapeutic approach, cognitive behavioural therapy (CBT) represents the leading therapeutic approach among DMHIs (Balcombe and De Leo 2022). Recent studies have demonstrated the positive effects of internet‐based CBT (iCBT) in reducing mental health symptoms among college students (McCall et al. 2018). Acceptance and commitment therapy (ACT) has also been adopted for online treatment (Levin, Hicks, and Krafft 2022) and has been found to effectively treat mental health issues such as anxiety and depression among university students (Hemmings et al. 2021). Modes of delivery may include mobile applications (apps), virtual or augmented‐reality, web‐based interventions, chatbots or conversational agents to name a few. A systematic overview by Lehtimaki et al. (2021) found that computerised CBT was effective at alleviating symptoms of depression and anxiety in young people, whereas the effectiveness of other DMHIs such as therapeutic video games or mobile apps remained inconclusive.
1.3. The Present Study
Considering the rapid growth of DMHIs and the high prevalence of mental health difficulties among university students, further systematic examination of the existing literature is needed, as evidence suggests that engagement with DMHIs among college students is low (Melcher et al. 2022; D'Adamo et al. 2023), and students in need of care may not be reached or do not utilise these treatment tools (Fleming et al. 2018). Moreover, although previous reviews have focused on the effectiveness of DMHIs among university students (D'Adamo et al. 2023; Montagni et al. 2020; Riboldi et al. 2023) there seems to be a gap of knowledge in terms of systematic reviews of DMHIs among clinical and sub‐clinical college student populations. Students are exposed to a large variety of stressors, which increases their level of anxiety and stress, and therefore the risk of developing mental health difficulties. Thus, the current systematic review and meta‐analysis aims to (a) estimate the effectiveness of DMHIs directed at university students that already present with mental health difficulties, and (b) to determine if guided interventions are more effective than fully automated ones. We expect to find that DMHIs will be effective for university students with mental health difficulties and that for both anxiety and depressive outcomes, guided interventions will be more effective than fully automated ones.
2. Methods
The reporting of the present systematic review was based on the Preferred Reporting Items for Systematic Review and Meta‐Analyses (PRISMA; Page et al. 2021). A protocol of the present review was previously registered in PROSPERO (February 3, 2024; CRD42024504265) (Figure 1).
FIGURE 1.
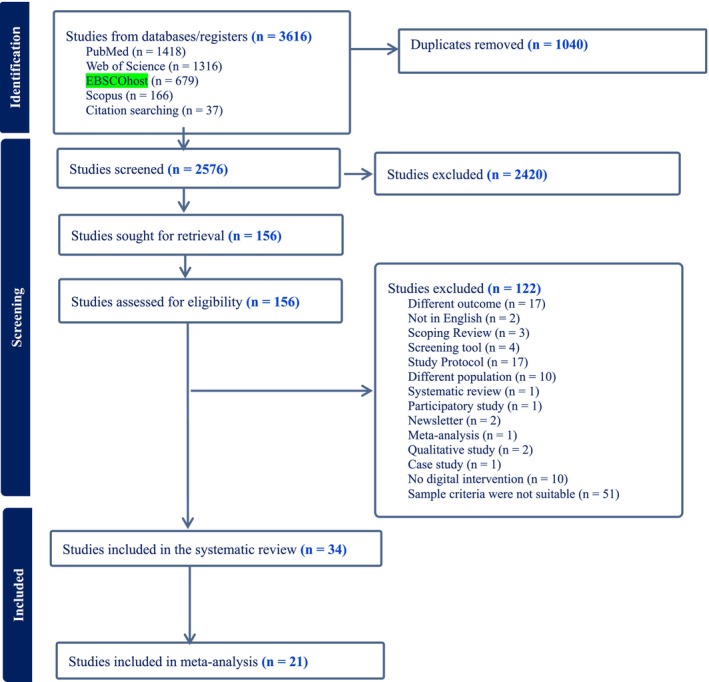
PRISMA flow diagram.
2.1. Inclusion Criteria
The Population, Intervention, Comparator, Outcome, and Study design (PICOS) framework (McKenzie et al. 2019) was used to guide inclusion criteria eligibility.
In terms of population (1), only studies that included university students with mental health difficulties, by inclusion of assessment (i.e., GAD‐7, PHQ‐9), were included. Studies of adolescents, children or young people that are not enrolled in a third‐level institution were excluded. University students had to be in the 18–25 age range to be eligible. Eligible interventions (2) included any studies that used a digital mental health intervention based on standardised psychological interventions, such as CBT, mindfulness, ACT, etc. All types of digital tools were included. In terms of comparator (3), eligible studies included those employing usual care or control groups that received no intervention, or an alternative intervention. Studies that employed a waiting list were also included. Studies reporting any type of mental health outcome measure (4) were included. Finally, (5) peer‐reviewed English language feasibility studies, randomised controlled trials, non‐randomised controlled trials, other types of randomised trials, longitudinal studies, and mixed methods pilot, published in the last 6 years were included in this review.
2.2. Search Strategy
A scoping of the literature was conducted by using Google Scholar and PubMed to identify the types of available studies for synthesis. Moreover, results from a parallel scoping review revealed that the vast majority of research on digital mental health interventions for university students was conducted since 2018 onwards. Therefore, to ensure that our study reports on the most up to date literature, we decided to include studies that were conducted in the last 6 years. As a follow up, we conducted a search in February 2024 of the following databases: PubMed, EBSCOhost (CINHAHL/PsycINFO/PsycArticles), and Web of Science using the keywords and search terms presented in Table 1. Searches were limited to English language peer‐reviewed articles published from 2018 to 2024.
TABLE 1.
Keywords and search terms used in the systematic review.
| 1 |
(“Mental health issues” OR “mental health problems” OR “mental illness” OR “mental problems” OR “mental disorders” OR “mental health disorders” OR “psychiatric diagnosis” OR “psychiatric disorder”) AND |
| 2 |
(“University students” OR “college students” OR “third‐level students” OR “undergraduate students” OR “postgraduate students” OR students OR “graduate students” OR “first‐year students” OR “second‐year students” OR “third‐year students” OR “fourth‐year students” OR “final‐year students”) AND |
| 3 |
(Interventions OR program* OR therap* OR implementation OR evaluation OR develop*) AND |
| 4 | (“digital interventions” or “Computer Assisted Therapy” or “Online Therapy” or Mhealth or Ehealth or M‐Health or E‐Health or “M Health” or “E Health” or Web‐based or “Web based” or Internet‐based or “Internet based” or App or Application or “Mobile phone” or Text or SMS or Computer* or “artificial intelligence” or AI or online or Virtual or Cyber or Interactive or Digital Technolog* or “conversational user interface” or “chatbot*”) |
2.3. Selection Process
A three‐step approach was used to evaluate studies according to the selection criteria. First, all records were imported to Covidence (Veritas Health Innovation 2020), where duplicates were removed. In the second stage, title and abstract screening was conducted by at least 2 of the 3 reviewers for agreement (A.M., C.K., C.P.) and full‐text articles were retrieved. In the third stage, the full‐text articles were screened for eligibility (A.M., C.K., C.P.). Differences between the reviewers were resolved by consensus.
2.4. Data Extraction
Details about the DMHI used in each study were extracted independently by two reviewers (A.M. and C.K.). Relevant information included study design, age, and participant characteristics. We also included details about the measurements used as eligibility criteria reported in the studies to justify the presence of mental health difficulties (e.g., He et al. 2022: “average score of the depression subscale in the College Students Mental Health Screening Scale (CSMHSS) within 2 to 3”). Discrepancies were resolved by consensus (A.M. and G.D.).
2.5. Quality Assessment
To assess for risk of bias, two reviewers (A.M. and C.K.) conducted the assessments independent. The reviewers used the Cochrane Risk of Bias Tool (version 1) for Randomised Controlled Trials (Higgins et al. 2011). Regarding non‐randomised studies, the Risk of Bias in Non‐Randomised Studies of Interventions (ROBINS‐I) tool (Sterne et al. 2016) was used. Assessment of risk of bias based was judged as low/high/unclear risk of bias based on each of the criteria.
2.6. Meta‐Analysis
Eligibility criteria for the meta‐analysis included studies with a two‐armed RCT that reported anxiety and depression outcomes. Two studies (Hides et al. 2019; Six et al. 2022) were excluded from the meta‐analysis as these did not have available outcome data. The Comprehensive Meta‐Analysis Software package (CMA, version 4; Borenstein et al. 2013) was used to conduct the analysis, based on a random effects model.
Two analyses of effectiveness were conducted: the first focused on DMHIs that reported outcomes for severity of anxiety symptoms (Salamanca‐Sanabria et al. 2020; Harrer et al. 2018; Karyotaki et al. 2022; Ponzo et al. 2020; Papini et al. 2023; O'Bryan et al. 2021; Sun et al. 2022; Suffoletto et al. 2021; McCall et al. 2018; Bautista et al. 2022; Short and Schmidt 2020; Newman et al. 2021; Levin, Hicks, and Krafft 2022; Dumarkaite et al. 2022); the second focused on DMHIs that reported outcomes for depressive symptom severity (Salamanca‐Sanabria et al. 2020; Bruhns et al. 2021; Harrer et al. 2018; Karyotaki et al. 2022; Kim and Lee 2023; Ponzo et al. 2020; Zhao et al. 2022; Kingston et al. 2020; Sun et al. 2022; Suffoletto et al. 2021; Ruehlman and Karoly 2023; Newman et al. 2021; Levin, Hicks, and Krafft 2022; Räsänen, Muotka, and Lappalainen 2023; Dumarkaite et al. 2022).
Between‐groups standardised mean differences (SMD) were calculated and used as effect sizes. Sensitivity analyses were performed to examine robustness of the overall findings. The Q statistic was used to assess study heterogeneity (Borenstein et al. 2009). The I 2 statistic was also calculated to estimate the percentage of variance in the observed effects owing to the variance in true effects; with I 2 ≥ 75% indicating considerable heterogeneity (Higgins et al. 2003).
Subgroup analyses were also performed to ascertain the effect of level of guidance on effectiveness of interventions. Finally, publication bias was examined by visual examination of funnel plots and the trim‐and‐fill method (Duval and Tweedie 2000).
3. Results
3.1. Search and Selection
A total of 3616 references were imported into Covidence for initial abstract screening. After removing duplicates, the titles, and abstracts of 2576 studies were screened and 2420 studies were excluded as not meeting inclusion criteria. A total of 156 studies were then assessed for full‐text eligibility screening, resulting in 34 studies that met the inclusion criteria; 21 of these studies had 2‐armed RCTs that could be included in the meta‐analysis.
3.2. Study Characteristics
Table 2 summarises the characteristics of included studies. In terms of study location, 13 (38%) of the studies were conducted in the United States (Haeger, Davis, and Levin 2022; Thomas et al. 2023; Palacios et al. 2018; Attridge et al. 2020; Six et al. 2022; Papini et al. 2023; Newman et al. 2021; Short and Schmidt 2020; Ruehlman and Karoly 2023; O'Bryan et al. 2021; Bautista et al. 2022; Rackoff et al. 2022; Suffoletto et al. 2021; Levin, Hicks, and Krafft 2022); 4 (12%) in the United Kingdom (Cook, Mostazir, and Watkins 2019; Ponzo et al. 2020; Broglia, Millings, and Barkham 2019; Kingston et al. 2020) and China (Sit et al. 2022; He et al. 2022; Zhao et al. 2022; Sun et al. 2022); 3 (9%) in Germany (Hennemann et al. 2022; Harrer et al. 2018; Bruhns et al. 2021); 2 (6%) in Australia (Dear et al. 2019; Hides et al. 2019); 1 (3%) in Canada (McCall et al. 2018), Republic of Korea (Kim and Lee 2023), Colombia (Salamanca‐Sanabria et al. 2020), the Netherlands (Karyotaki et al. 2022), Lithuania (Dumarkaite et al. 2022), Finland (Räsänen, Muotka, and Lappalainen 2023), India (Newman et al. 2021), and Pakistan (Akram and Arshad 2022). A total of 6234 participants were included in this systematic review. Sample size ranged from 11 (Haeger, Davis, and Levin 2022) to 1080 (Dear et al. 2019); and participants' mean age ranged from 18.53 to 25 (mean = 21.21, SD = 3.03). Regarding study design, 74% (25/34) of studies were RCTs (Räsänen, Muotka, and Lappalainen 2023; Cook, Mostazir, and Watkins 2019; He et al. 2022; Six et al. 2022; Salamanca‐Sanabria et al. 2020; Harrer et al. 2018; Karyotaki et al. 2022; Kim and Lee 2023; Papini et al. 2023; Newman et al. 2021; Short and Schmidt 2020; McCall et al. 2018; Ruehlman and Karoly 2023; O'Bryan et al. 2021; Bautista et al. 2022; Zhao et al. 2022; Ponzo et al. 2020; Rackoff et al. 2022; Bruhns et al. 2021; Suffoletto et al. 2021; Sun et al. 2022; Levin, Hicks, and Krafft 2022; Dumarkaite et al. 2022; Kingston et al. 2020; Hides et al. 2019), 9% (3/34) were within groups pre‐post trials (Haeger, Davis, and Levin 2022; Sit et al. 2022; Akram and Arshad 2022); 6% (2/34) were non‐randomised trials (Palacios et al. 2018; Broglia, Millings, and Barkham 2019); and the remaining papers included a longitudinal study (Attridge et al. 2020), an exploratively secondary analysis (Hennemann et al. 2022), a prospective study (Dear et al. 2019), and a micro‐randomised trial (Thomas et al. 2023). Of note, out of the 25 RCTs, 16 (64%) used a waitlist control (Räsänen, Muotka, and Lappalainen 2023; Salamanca‐Sanabria et al. 2020; Harrer et al. 2018; Kim and Lee 2023; Papini et al. 2023; Newman et al. 2021; McCall et al. 2018; Hides et al. 2019; Ruehlman and Karoly 2023; Bautista et al. 2022; Zhao et al. 2022; Ponzo et al. 2020; Bruhns et al. 2021; Levin, Hicks, and Krafft 2022; Akram and Arshad 2022; Dumarkaite et al. 2022), 8 (32%) used an active control (He et al. 2022; Six et al. 2022; Karyotaki et al. 2022; Short and Schmidt 2020; Rackoff et al. 2022; Suffoletto et al. 2021; Sun et al. 2022; Kingston et al. 2020), and 1 (4%) used a placebo control (O'Bryan et al. 2021).
TABLE 2.
Summary of the 34 studies included in the systematic review.
| Study and country | Total N | Mean age (SD) | Sample mental health criteria | Study design | Control | Psychological treatment | Duration | Mental health measures | Human support | Main findings |
|---|---|---|---|---|---|---|---|---|---|---|
|
1. Haeger, Davis, and Levin (2022) USA |
11 | 23.55 (5.11) | Eligibility criteria included placement on the CCC waiting list with at least 2 weeks before their first scheduled face‐to‐face therapy appointment, and having a presenting problem of depression and/or anxiety. The study did not actively screen participants for depression and anxiety, and instead relied on the CCC clinician's discretion to provide materials to individuals with these presenting problems. | A pre‐post, open trial design | Not Applicable | ACT | 8 weeks |
DASS—Depression, Anxiety and Stress AAQ‐II—Psychological inflexibility CFQ—Cognitive fusion PHLMS—Mindfulness VQ‐valued living ESAS—Emotional self‐awareness |
No | Participants improved on depression and anxiety symptoms as well as psychological inflexibility processes. |
|
2. Thomas et al. (2023) USA |
35 | 18.53 (0.53) | First‐generation status students (parents had not completed a 4‐year college degree) had to report distress on 4 or more or the las 7 days that interfered with functioning. | Micro‐randomised trial (MRT) | Yes, no intervention | ACT | 2 weeks |
PHQ‐2—Depression PSS‐4—Perceived Stress |
No | The intervention increased values‐based behaviour but did not decrease avoidance behaviour. The intervention reduced depressive symptoms but not perceived stress. |
|
3. Räsänen, Muotka, and Lappalainen (2023) Finland |
123 | 25 (4.52) | To be eligible, students had to report experiencing some form of psychological distress, such as stress, low mood, and/or anxiety. | 2‐armed RCT | Yes, waitlist | ACT | 8 sessions (1 per week) |
MHC‐SF—Subjective psychological, emotional, and social well‐being PSS‐10—Perceived Stress PHQ‐9—Depression |
Yes | ACT‐based, blended internet interventions with semi‐structured coach feedback and minimally tailored features can be as effective as interventions with fully personalised feedback. |
|
4. Sit et al. (2022) China |
39 | 18.9 (0.94) | Students were included if they had a score of Patient Health Questionnaire‐9 (PHQ‐9) of 10 or higher | An uncontrolled, single‐armed pilot trial | Not Applicable | BAT | 6 weeks; 3‐, and 6‐month follow‐up |
PHQ‐9—Depression GAD‐7—Anxiety WHO‐5—Anxiety and well‐being PSYCHOLOPS—Stress |
Yes | Significant decrease of depression, anxiety, and self‐defined problems. |
|
5. Palacios et al. (2018) USA |
102 | N/A | Students had to meet the threshold for mild depression (score of 5+ on the PHQ‐9), anxiety (5+ on the GAD‐7), or stress (15+ on the DASS‐21 stress subscale, after multiplying score by 2) | Non‐Randomised Trial of acceptability, effectiveness, and satisfaction | Not Applicable | CBT | 7 weeks; 3‐month follow‐up |
PHQ‐9—Depression GAD‐7—Anxiety DASS‐21—Stress |
Yes | Significant decrease in depression, anxiety, and stress. |
|
6. Cook, Mostazir, and Watkins (2019) UK |
235 | 20.41 (1.5) | Students had to score above the 75th percentile on at least one measure of worry/rumination: ≥ 50 on the Penn State Worry Questionnaire (PSWQ); ≥ 40 on the Ruminative Response Scale (RRS) | 3‐armed RCT | Yes, waitlist | CBT | 6 weeks |
PSWQ—Worry PHQ‐9—Depression GAD‐7—Anxiety RRS—Rumination |
Yes | Significant improvements in rumination, worry, and depressive symptoms. |
|
7. Hennemann et al. (2022) Germany |
149 | 24.60 (5.16) | Eligibility criteria included students with elevated somatic symptom distress, as indicated by a score ≥ 4 on the Patient Health Questionnaire, somatic symptom scale (PHQ‐15) | Exploratively secondary analysis of a two armed, group RCT | Yes, waitlist | CBT | 3‐,6‐15‐months follow‐up |
PHQ‐15—Somatic symptoms of distress SSD‐12—Adverse psycho‐behavioural symptoms of the somatic symptom disorder PHQ‐9—Depression GAD‐7—Anxiety PDI—Functional disability |
Yes | Internet‐delivered cognitive behavioural therapy with regular guidance is not unequivocally superior to guidance‐on‐demand |
|
8. Dear et al. (2019) Australia |
1080 | 23 | Students who presented to the CAPS, and self‐reported symptoms of stress, anxiety, low mood, or depression and wanted psychological treatment. | A large, prospective, single‐group Phase‐IV clinical trial | Not Applicable | CBT | 8 weeks |
PHQ‐9—Depression GAD‐7—Anxiety |
Yes | Large clinical reductions in symptoms of both anxiety and depression were observed. |
|
9. He et al. (2022) China |
148 | 18.78 (0.89) | College students with an average score of the depression subscale in the College Students Mental Health Screening Scale (CSMHSS) within 2 to 3. | A single‐blind, 3‐armed randomised controlled trial | Yes, active control | CBT | 8 sessions (twice per week) 1 month. | PHQ‐9—Depression | Yes | Significant reductions in depression. |
|
10. Attridge et al. (2020) USA |
951 | 23.79 (6.93) | Users had to be from a customer of Learn to Live in the higher education market segment (i.e., a college or university). Users were required to be at a sufficient level of clinical severity (clinical status) at the start of program use | Longitudinal, repeated measures research design | Not Applicable | CBT | 5 weeks; 3‐month follow‐up |
PHQ‐9—Depression GAD‐7—Anxiety SPIN—Social Anxiety MOS—Insomnia |
Yes | Significant improvements for stress, anxiety, worry, and insomnia. |
|
11. Six et al. (2022) USA |
94 | 20.77 (2.54) | Students having a score of five or higher on the PHQ‐8 | 2‐armed RCT | Yes, active control | CBT | 4‐months |
PHQ‐8—Depression GAD‐7—Anxiety PSS‐10—Stress PANAS—Positive and Negative Affect |
No | These results indicate that CBT mental health apps, such as AirHeart, have the potential to reduce depressive symptoms over a short intervention period |
|
12. Salamanca‐Sanabria et al. (2020) Colombia |
150 | 22.15 (4.74) | College students with mild to moderately severe depressive symptoms determined by the Patient Health Questionnaire—9 scores of 10–19 | 2‐armed RCT | Yes, waitlist | CBT | 5 sessions |
PHQ‐9—Depression GAD‐7—Anxiety |
Yes | Significant effects for depression and anxiety |
|
13. Harrer et al. (2018) Germany |
150 | 24.1 (4.1) | University students with elevated levels of perceived stress (PSS‐4 ≥ 8) | 2‐armed RCT | Yes, waitlist | CBT | 8 weeks |
PSS‐4—Perceived Stress CES‐D—Depression STAI—State Anxiety WHO‐5—General well‐being MBI—Emotional Exhaustion |
Yes | Significant effects for stress, depression, anxiety, well‐being, and emotional exhaustion. |
|
14. Karyotaki et al. (2022) Netherlands |
100 | 21.91 (2.61) | College students with mild to moderate symptoms of depression defined by scoring above the cut‐off score of 4 on the Patient Health Questionnaire (PHQ‐9) and/or anxiety symptoms as defining by scoring above the cut‐off score of 4 on the Generalised Anxiety Disorder scale—7 items (GAD‐7). | 2‐armed RCT | Yes, active control | CBT | 8 weeks; 3‐month follow‐up |
PHQ‐9—Depression GAD‐7—Anxiety |
Yes | No evidence of a difference between the intervention and the control. |
|
15. Kim and Lee (2023) Republic of Korea |
34 | N/A | The participants had to be female college students with a traumatic experience and posttraumatic stress symptom scores of 22–66, which is a cutoff that can be diagnosed as PTSD; anything above 66 is a severe PTSD condition that cannot be suitably addressed in this study | 2‐armed RCT | Yes, waitlist | CBT | 7 weekly sessions +4 weeks boost session. |
SLESQ—Traumatic experiences IES‐R—Post‐traumatic stress CES‐D—Depression Functional Health Pattern Assessment Screening Tool |
Yes | The program reduced post‐traumatic stress and depression symptoms and improved functional health and adjustment. |
|
16. Papini et al. (2023) USA |
159 | 19.72 (1.42) | Students were invited to participate in this study if they had high anxiety sensitivity, defined as an ASI‐3 total score greater than 22 | 2‐armed RCT | Yes, waitlist | CBT | 2‐months follow‐up | SSAI—Anxiety Sensitivity | No | Significant mean reduction in anxiety. |
|
17. Newman et al. (2021) India |
222 | 19.90 (1.56) | Students met criteria for clinical or subthreshold GAD | 2‐armed RCT | Yes, waitlist | CBT | 6 sessions in 3‐months; 6‐month follow‐up |
GAD‐Q‐IV—Anxiety PSWQ—Worry DASS‐D—Depression |
Yes | Significant reductions in GAD severity, worry, and depressive symptoms |
|
18. Short and Schmidt (2020) USA |
61 | 19.43 (2.04) | Students were invited to participate if they completed a screening survey, and scored at least 1 SD above the sample mean on abbreviated anxiety (Penn State Worry Questionnaire), and insomnia (Insomnia Severity Index) | 2‐armed RCT | Yes, active control | CBT | 6‐, and 12‐month follow‐up |
SAS—Safety aids related to various anxiety disorders. SRBQ—Insomnia‐related safety behaviours ISI—Severity of insomnia PSWQ—Worry BAI—Anxiety DOCS—Obsessive compulsive PCL‐5—PTSD |
No | Findings suggest that targeting safety aids for anxiety and insomnia is acceptable and effective in reducing the target mechanism, safety aids, as well as worry. |
|
19. McCall et al. (2018) Canada |
101 | 21.86 (5.50) | Students that were experiencing some degree of social anxiety. | 2‐armed RCT | Yes waitlist | CBT | Single session; 1‐month follow‐up |
SIAS‐6—Social anxiety FNE—Negative evaluation Q‐LES‐Q‐SF—Quality of life, enjoyment, and satisfaction |
No | Significant reduction in social anxiety. |
|
20. Ruehlman and Karoly (2023) USA |
68 | 19.42 (1.84) | Students with symptoms of depression, assessed using the PHQ‐8 | 2‐armed RCT | Yes, waitlist | CBT | 1 week; 1‐monht follow up |
PHQ‐8—Depression CD‐Quest—Cognitive distortions |
No | Significant lower levels of depression. |
|
21. O'Bryan et al. (2021) USA |
68 | 19.68 | Students who reported elevated levels of health anxiety as determined by a SHAI score at least 1 SD above the student mean; and that reported elevated AS as determined by an ASI‐3 score falling at least 1 SD above the nonclinical mean | 2‐armed RCT | Yes, placebo | CBT | Single session, 2‐week follow‐up |
ASI‐3—Anxiety sensitivity SHAI—Health anxiety |
No | Individuals in the active condition exhibited greater reductions in AS compared to the control condition. |
|
22. Bautista et al. (2022) USA |
35 | 21.86 (4.82) | Students with a score of 6 or higher on the Mini Social Phobia Inventory (Mini‐SPIN) | 2‐armed RCT | Yes, waitlist | CBT | 7 weeks; 3‐month follow‐up | SIAS‐6—Social anxiety | Yes | Significant rate of decline in social anxiety scores over time. |
|
23. Zhao et al. (2022) China |
182 | 21.75 (1.33) | Students with depressive symptoms, according to the Beck Depression Inventory‐II, and a semi‐structured interview. | 2‐armed RCT | Yes, waitlist | CBT + ACT | 3 years |
BDI‐II—Depressive symptoms MHC‐SF—Positive mental health |
No | Significant reductions in depressive symptoms and improvement in positive mental health. |
|
24. Ponzo et al. (2020) UK |
262 | 19.87 (1.79) | Students that scored > 14 points on the Depression, Anxiety and Stress Scale‐21 items (DASS‐21) stress subscale or > 7 points on the DASS‐21 anxiety subscale | 2‐armed RCT | Yes, waitlist | CBT + BAT | 7 weeks |
STAI‐S‐6—State anxiety DASS‐21—Anxiety, stress, and depression WEMWBS—Perceived well‐being |
No | Significant reductions in anxiety and increased perceived well‐being. |
|
25. Broglia, Millings, and Barkham (2019) UK |
38 | 22 (3.67) | Help‐seeking students who had been accepted for counselling and met moderate clinical criteria on one of two standardised outcome measures for anxiety or depression. | 2‐armed, nonrandomized design | Yes, active control | CBT + Mindfulness | Single session, 1‐week follow‐up, and 1‐month follow‐up. |
PHQ‐9—Depression GAD‐7—Anxiety CORE‐10—changes in general psychological functioning. CCAPS‐62—changes in mental health |
Yes | No significant differences |
|
26. Rackoff et al. (2022) USA |
585 | 20.44 (4.50) | Students who reported moderate or higher stress during the COVID‐19 pandemic | 2‐armed RCT | Yes, active control | CBT + PA | 2 weeks | DASS‐21—stress, anxiety, and depression | No | No significant changes in stress and depression. |
|
27. Bruhns et al. (2021) Germany |
523 | 22.95 (3.35) | Students having depressive symptoms measured by the PHQ‐9. | 2‐armed RCT | Yes, waitlist | CBT + PA + DBT | 6 weeks; 3‐momth follow‐up |
PHQ‐9—depression RSE—self‐esteem WHOWOL‐BREF—quality of life |
No | Significant reduction in depressive symptoms and a significant increase in self‐esteem. |
|
28. Suffoletto et al. (2021) USA |
52 | 18.7 (0.45) | Inclusion criteria: current mental health diagnosis documented in their electronic medical record or received mental health services within 3 months per self‐, parent‐, or clinician‐report, graduated high school, plan to attend college or higher education within 6 weeks. | 2‐armed RCT | Yes, active control | CBT + PA + DBT | 4 weeks; 6‐week follow‐up |
MHSES—Mental health self‐efficacy CCAPS—psychological symptoms |
No | Reductions in mental health symptoms over time and significant between‐group effects. |
|
29. Sun et al. (2022) China |
114 | N/A | Students experiencing elevated psychological distress, such that their depression or anxiety symptoms at or above the mild cutoff on the Patient Health Questionnaire‐9 (PHQ‐9) and the 7‐item Generalised Anxiety Disorder Scale (GAD‐7) | 2‐armed RCT | Yes, active control | Mindfulness | 1‐monht; 3‐monht follow‐up |
GAD‐7—Anxiety PHQ‐9—Depression MAAS—dispositional mindfulness MSPSS—perceived social support |
Yes | Both mindfulness and social support, delivered via mHealth, show promise in reducing distress and addressing anxiety. |
|
30. Levin, Hicks, and Krafft (2022) USA |
23 | 20.43 (2.46) | Students on the waitlist for the Counselling and Psychological Services centre, currently seeking treatment at CAPS with an expected wait time of at least 2 weeks for services | 2‐armed RCT | Yes, waitlist | Mindfulness | 3‐months |
CCAPS‐34—psychological symptoms MHC‐SF—positive mental health |
No | Very preliminary support was found for potential app efficacy relative to the control condition, particularly for depression, anxiety, and overall distress. |
|
31. Dumarkaite et al. (2022) Lithuania |
70 | 23.31 (3.11) | Students who met the clinical significance criteria for PTSD, CPTSD, or disturbances in self‐organisation symptoms with or without functional impairment as measured with the International Trauma Questionnaire | 2‐armed RCT | Yes, waitlist | Mindfulness | 8 sessions (1 per day) Intervention access for 3 months |
LEC‐5—Traumatic events ITQ—Symptoms of PTSD and CPTSD |
Yes | Significant changes in CPTSD scores between groups. |
|
32. Kingston et al. (2020) UK |
206 | 23.4 (6.53) | Students with elevated levels of depressive symptoms (DASS‐D; ≥ 10) | 2‐armed RCT | Yes, active control | Mindfulness | 4 weeks | DASS‐D‐21—Depression | No | Significant reductions in depression. |
|
33. Akram and Arshad (2022) Pakistan |
20 | 20 (1.5) | The inclusion of these participants was determined based on whether or not they obtained moderate (scores between 52 and 60) or high (scores 61 or above) scores on the Toronto Alexithymia Scale (TAS‐20) | A pilot quasi‐experimental study | Yes, waitlist | Other (Alexithymia reduction treatment, ART) | 4 sessions (1 per week) |
TAS‐20—Alexithymia MHSQ—presence of psychological disorders or physical disabilities SCL‐R—symptoms of common psychological disorders |
No | The statistical analysis showed a significant reduction in the participants' alexithymia, as well as depression and anxiety. |
|
34. Hides et al. (2019) Australia |
169 | 19.2 (2.5) | Students who reported mild distress in the past month on the Kessler 10 Psychological Distress scale (K10 > 17) | 2‐armed RCT | Yes, waitlist | Other (Dynamic info‐motivation‐behavioural skills health behaviour model) | 4 weeks; 2‐month follow‐up |
DERS‐SF—Emotion dysregulation K10—psychological distress MHC‐SF—mental well‐being |
No | Lack of significant differences between groups. |
Abbreviations: ACT, acceptance and commitment therapy; BAT, behavioural activation; CBT, cognitive‐behavioural therapy; DBT, dialectical behaviour therapy; PA, positive psychology.
Table S3 (Supporting Information) provides an overview of the sample characteristics. It is important to highlight that only four studies (Karyotaki et al. 2022; Broglia, Millings, and Barkham 2019; Palacios et al. 2018; Kingston et al. 2020) provided details about the inclusion of international students in their sample, and only six studies (Salamanca‐Sanabria et al. 2020; Bruhns et al. 2021; Harrer et al. 2018; Räsänen, Muotka, and Lappalainen 2023) provided details about the field of study of their sample. Therefore, it was difficult to draw conclusions on the impact of these factors on the effect of the interventions.
3.3. Types of Intervention
Regarding the focus of the interventions, 53% (18/34) of the studies were based on CBT only (Palacios et al. 2018; Cook, Mostazir, and Watkins 2019; Hennemann et al. 2022; Dear et al. 2019; He et al. 2022; Attridge et al. 2020; Six et al. 2022; Salamanca‐Sanabria et al. 2020; Harrer et al. 2018; Karyotaki et al. 2022; Kim and Lee 2023; Papini et al. 2023; Newman et al. 2021; Short and Schmidt 2020; McCall et al. 2018; Ruehlman and Karoly 2023; O'Bryan et al. 2021; Bautista et al. 2022); 18% (6/34) were based on a multicomponent treatment (Zhao et al. 2022; Ponzo et al. 2020; Broglia, Millings, and Barkham 2019; Rackoff et al. 2022; Bruhns et al. 2021; Suffoletto et al. 2021); 12% (4/34) were based on mindfulness (Sun et al. 2022; Levin, Hicks, and Krafft 2022; Dumarkaite et al. 2022; Kingston et al. 2020); 9% (3/34) were based on ACT (Akram and Arshad 2022; Hides et al. 2019); 6% (2/34) were based on other types of treatment (Akram and Arshad 2022; Hides et al. 2019); and one study (3%) was based on behavioural activation (BAT) (Sit et al. 2022). Digital interventions were designed to address a range of mental health symptoms, including depression, anxiety, and stress. The included studies used either the Beck Depression Inventory (Beck, Ward, and Mendelson 1961; Beck, Steer, and Brown 1996), the Centre for Epidemiological Studies Depression Scale (Radloff 1977), the Patient Health Questionnaire (Kroenke et al. 1998, 2009; Kroenke, Spitzer, and Williams 2001) or the Depression, Anxiety and Stress Scale (Lovibond and Lovibond 1995) as outcomes measures of depressive symptoms. Moreover, the Generalised Anxiety Disorder scale (Spitzer et al. 2006), the Beck Anxiety Inventory (Beck et al. 1988), and the Depression, Anxiety and Stress Scale (Lovibond and Lovibond 1995) were used as outcomes measures of anxiety symptoms.
3.4. Type of Support
Half (17/34) of the studies were based on guided DMHIs that included some level of human support (Räsänen, Muotka, and Lappalainen 2023; Sit et al. 2022; Palacios et al. 2018; Cook, Mostazir, and Watkins 2019; Hennemann et al. 2022; Dear et al. 2019; He et al. 2022; Attridge et al. 2020; Salamanca‐Sanabria et al. 2020; Harrer et al. 2018; Karyotaki et al. 2022; Kim and Lee 2023; Newman et al. 2021; Bautista et al. 2022; Broglia, Millings, and Barkham 2019; Sun et al. 2022; Dumarkaite et al. 2022) and the other half (17/34) were based on fully automated DMHIs (Haeger, Davis, and Levin 2022; Thomas et al. 2023; Six et al. 2022; Papini et al. 2023; Short and Schmidt 2020; McCall et al. 2018; Ruehlman and Karoly 2023; O'Bryan et al. 2021; Zhao et al. 2022; Ponzo et al. 2020; Rackoff et al. 2022; Bruhns et al. 2021; Suffoletto et al. 2021; Levin, Hicks, and Krafft 2022; Kingston et al. 2020; Akram and Arshad 2022; Hides et al. 2019).
Table S4 (Supporting Information) provides an overview of the support provided in the nine guided interventions included in the meta‐analysis. Six studies (67%) reported that the support was provided by a postgraduate level student in Psychology (Räsänen, Muotka, and Lappalainen 2023; Salamanca‐Sanabria et al. 2020; Harrer et al. 2018; Karyotaki et al. 2022; Sun et al. 2022; Dumarkaite et al. 2022), 1 (11%) by a trained rational emotive behaviour therapy counsellor (Kim and Lee 2023), one (11%) by trained clinicians in Psychology (Newman et al. 2021), and one (11%) by a peer‐support worker (Bautista et al. 2022). Moreover, the support provided was generally asynchronous and provided online. Finally, it is important to highlight that the studies included in this review that were based on guided interventions reported mixed results in terms of whether human guidance increased adherence to the digital interventions (see Table S4).
3.5. Meta‐Analysis of Effectiveness
Of the 34 studies included in our review, 21 (62%) reported data that could be included in the meta‐analysis. Of these, six studies (28%) reported depression outcomes only (Räsänen, Muotka, and Lappalainen 2023; Kim and Lee 2023; Bruhns et al. 2021; Kingston et al. 2020; Ruehlman and Karoly 2023; Zhao et al. 2022), nine studies (43%) reported both anxiety and depression outcomes (Suffoletto et al. 2021; Ponzo et al. 2020; Rackoff et al. 2022; Levin, Hicks, and Krafft 2022; Newman et al. 2021; Dumarkaite et al. 2022; Karyotaki et al. 2022; Harrer et al. 2018), and six studies (29%) reported anxiety outcomes only (Bautista et al. 2022; Papini et al. 2023; McCall et al. 2018; O'Bryan et al. 2021; Short and Schmidt 2020; Sun et al. 2022). No evidence of publication bias was observed throughout the studies (see Supporting Information).
3.5.1. Depression
The aggregate effect of treatment on depression, as displayed on Figure 2, d = 0.55, suggested a medium effect size across the studies included (k = 16; n = 2316; Cohen's d = 0.55, 95% CI 0.37–0.72; p < 0.001). There was evidence of significant heterogeneity (Q 15 = 54.71; p < 0.001; I 2 = 72.58; T 2 = 0.08; t = 0.23), which may be explained due to differences in the digital interventions that were used; including length, intervention type (i.e., blended or self‐help), and psychological treatment (i.e., CBT, ACT, multicomponent). Additionally, there were differences in the measurements of outcomes (i.e., PHQ‐9, DASS‐D, CCAPS, BDI‐II) (Cordero and Dans 2021).
FIGURE 2.
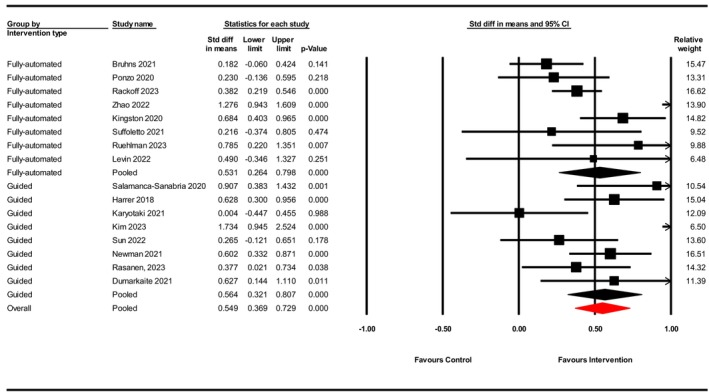
Forest plot of summary statistics (SMD—Cohen's d) for digital interventions targeting depression among university students.
3.5.2. Anxiety
The aggregate effect of treatment on anxiety, as displayed on Figure 3, d = 0.46, suggested a medium effect size across the studies included (k = 15; n = 1848; Cohen's d = 0.46, 95% CI 0.31–0.61; p < 0.001). There was also evidence of significant heterogeneity (Q 14 = 28.16; p = 0.001; I 2 = 5.28; T 2 = 0.04; t = 0.20), which can be explained due to differences in the type of interventions, delivery type, psychological treatment, and measurements of outcomes (i.e., GAD‐7, BAI, DASS‐21).
FIGURE 3.
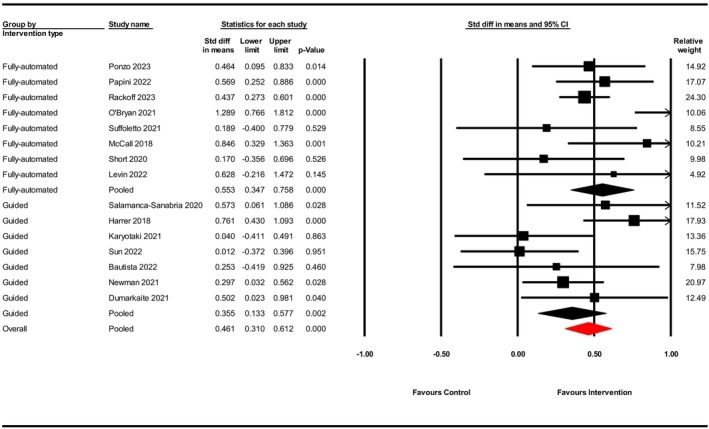
Forest plot of summary statistics (SMD—Cohen's d) for digital interventions targeting anxiety among university students.
3.6. Subgroup Analyses
Subgroup analyses were conducted for both anxiety and depression to examine whether the treatment effect differed across psychological treatment (see Table 3) and intervention type (see Table 4). For depression, the largest effect size was observed for CBT (k = 6; Cohen's d = 0.69, 95% CI 0.37–1.02, p < 0.001), followed by mindfulness (k = 4; Cohen's d = 0.55, 95% CI 0.34–0.75, p < 0.001), and multicomponent interventions (k = 5; Cohen's d = 0.46, 95% CI 0.01–0.83, p = 0.013). Guided interventions (k = 8; Cohen's d = 0.56, 95% CI 0.32–0.80, p < 0.001) appeared to be slightly more effective than fully automated interventions (k = 8; Cohen's d = 0.53, 95% CI 0.26–0.80, p < 0.001).
TABLE 3.
Subgroup analysis of digital mental health interventions based on type of psychological treatment compared to controls.
| Number of studies (n = 20) | Cohen's d (95% CI) | p | |
|---|---|---|---|
| Depression (n = 15) | |||
| CBT | 6 | 0.69 (0.33–1.72) | < 0.001 |
| Mindfulness | 4 | 0.55 (0.07–1.02) | < 0.001 |
| Multicomponent | 5 | 0.46 (0.01–0.83) | 0.01 |
| Anxiety (n = 15) | |||
| CBT | 9 | 0.53 (0.23–0.77) | < 0.001 |
| Mindfulness | 3 | 0.23 (0.09–0.67) | 0.13 |
| Multicomponent | 3 | 0.43 (0.28–0.57) | < 0.001 |
Note: Two separate meta‐analysis were conducted; one for depressive outcomes (n = 16), and one for anxiety outcomes (n = 15); of which n = 11 studies reported both anxiety and depressive outcomes, n = 6 reported depressive outcomes only, and n = 5 reported anxiety outcomes only. Subgroup analyses were conducted with n = 20 studies for type of psychological treatment. One study based on ACT (Räsänen, Muotka, and Lappalainen 2023) was excluded as it disrupted the even distribution of studies in each category.
TABLE 4.
Subgroup analysis of digital mental health interventions based on type of intervention compared to controls.
| Number of Studies (n = 21) | Cohen's d (95% CI) | p | |
|---|---|---|---|
| Depression (n = 16) | |||
| Guided interventions | 8 | 0.56 (0.32–0.80) | < 0.001 |
| Fully automated | 8 | 0.53 (0.26–0.80) | < 0.001 |
| Anxiety (n = 15) | |||
| Guided interventions | 7 | 0.35 (0.13–0.58) | 0.002 |
| Fully automated | 8 | 0.55 (0.35–0.61) | < 0.001 |
Note: Two separate meta‐analysis were conducted; one for depressive outcomes (n = 16), and one for anxiety outcomes (n = 15); of which n = 11 studies reported both anxiety and depressive outcomes, n = 6 reported depressive outcomes only, and n = 5 reported anxiety outcomes only. Subgroup analyses were conducted with n = 21 studies for intervention type.
In regard to the studies that focused on anxiety, subgroups analyses revealed that CBT was also the most effective (k = 9; Cohens' d = 0.53, 95% CI 0.23–0.76, p < 0.01), followed by mindfulness (k = 4; Cohens' d = 0.50, 95% CI 0.02–0.98, p = 0.04), and multicomponent interventions (k = 3; Cohens' d = 0.43, 95% CI 0.03–0.57, p < 0.001). For anxiety, contrary to our hypotheses, larger effect sizes were observed for fully automated interventions (k = 8; Cohen's d = 0.55, 95% CI 0.35–0.61, p = 0.002) compared to guided interventions (k = 7; Cohen's d = 0.35, 95% CI 0.13–0.58, p < 0.001).
3.7. Risk of Bias
In relation to the study design, 76% (26/34) of studies were RCTs and were rated according to the RoB‐1 (Higgins et al. 2011), and 24% (8/34) were non‐randomised controlled trials and were rated according to the ROBINS‐I (Sterne et al. 2016). As shown in Figure 4, overall, 46% (12/26) of studies were rated on the RoB‐1 with “some concerns” (22, 6, 31, 34, 30, 17, 21, 16, 26, 20, 19, 23) in relation to risk of bias; 31% (8/26) were rated with “low risk” (24, 27, 13, 9, 14, 15, 3, 28); and 23% (6/26) were rated with “high risk” (32, 19, 12, 11, 29, 2). Performance bias was the most prevalent domain of concern, followed by attrition bias resulting from unblinding of participants and self‐report measures. A total of 24% (3/34) of non‐RCTs were rated using the Risk of Bias in Non‐Randomised Studies of Interventions (ROBINS‐I) tool; 71% (5/7) of the studies were rated with “moderate risk” (33, 10, 25, 1, 7), and 29% (2/7) were rated with “low risk” (8, 5).
FIGURE 4.
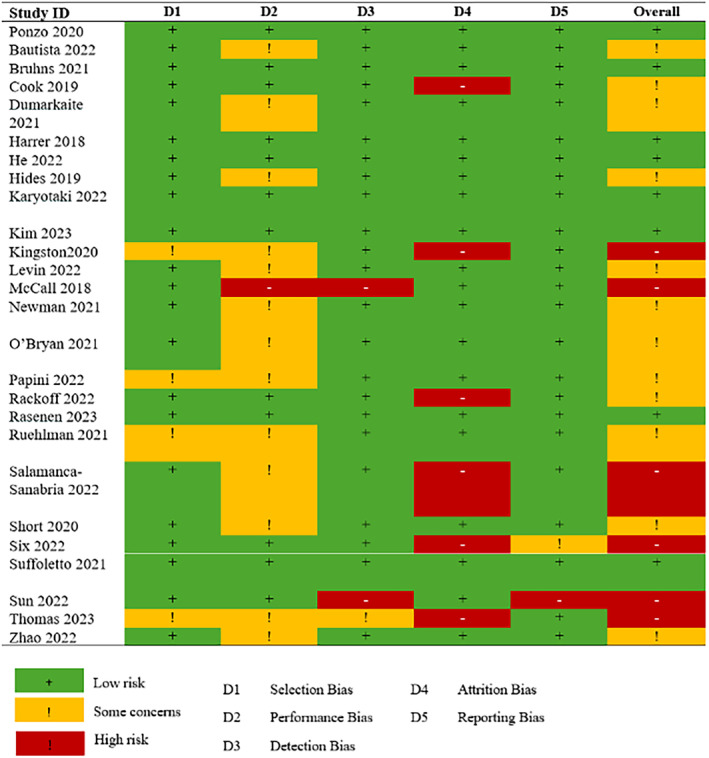
Risk of bias assessment using the Cochrane risk of bias tool (version 1) for RCTs.
4. Discussion
4.1. Summary of Findings
This systematic review and meta‐analysis aimed to synthesise the published literature on the effectiveness of digital mental health interventions for university students with mental health difficulties. While previous reviews had focused on non‐clinical student populations (i.e., Harrer et al. 2018; Lattie et al. 2019; D'Adamo et al. 2023) this study focused specifically on mental health symptoms as measured by standardised psychological measures such as the GAD‐7 and the PHQ‐9. We hypothesised that DMHIs would be effective for university students with ongoing mental health difficulties, and that interventions incorporating human interventions would be more effective than fully automated interventions.
Overall, in terms of efficacy and size of effect, our results suggested significant, medium‐sized benefits of DMHIs when measured in terms of either depressive symptom severity or anxious symptom severity in participating students. These beneficial effects are consistent with past systematic reviews and meta‐analyses. For example, Lattie et al. (2019) conducted a systematic review that aimed to synthesise the literature on the effectiveness, usability, acceptability, uptake and adoption of DMHIs for anxiety and depression, and enhancing well‐being among university students. These authors reported that these interventions were effective in producing beneficial changes in the psychological outcome variables measured. In terms of meta‐analyses, Ferrari et al. (2022) found small‐to‐moderate effects in favour to DMHIs on improving psychological wellbeing in university students. However, our review extends these previous findings by focusing on changes in severity of symptoms of depression and anxiety among college students, as well as providing evidence of the effectiveness of human support on these interventions. More recent reviews such as D'Adamo et al. (2023) have focused on examining reach and uptake of DMHIs based on CBT for college students. Our study expands this literature by focusing on the effectiveness of these interventions for college students with mental health difficulties, as well as not limiting the inclusion of the studies to those that included interventions based on CBT.
Finally, results from our sub‐group analyses further suggested that the effectiveness of these interventions varied in terms of the presence or absence of human guidance, and in terms of the type of psychological treatment behind the intervention (CBT, mindfulness, etc.).
4.2. The Role of Human Guidance
In terms of depressive symptom severity, the presence of human guidance was observed to significantly influence the size of the effect observed, which aligns with the results of previous meta‐analytic reviews on digital interventions in the treatment of depression (Richards and Richardson 2012; Moshe et al. 2021). These reviews focused mostly on adult populations, however, our study focused on the potential of human guidance in digital interventions to improve depression symptom severity for university students with mental health difficulties.
Contrary to our hypothesis, when considering symptom severity in anxiety, we observed a somewhat higher overall effect size for fully automated interventions (d = 0.55) compared to guided interventions (d = 0.35). A recent meta‐analysis by Pauley et al. (2023) reported no differences between guided and unguided interventions in the treatment of anxiety disorders for adult samples. These differing findings may reflect differences in the study population, and the amount and type of guidance provided.
Regarding why 1:1 human guidance appeared to be more important to outcome when measured in terms of depressive symptom severity rather than anxiety symptom severity, in the absence of an a priori hypothesis we can only speculate about why this was observed. For example, motivation could be one factor that explains why our results suggest a benefit for human guidance in symptoms of depression severity compared to anxiety severity for university students with mental health difficulties. It has been suggested that motivation acts as a moderator of the effect of accountability; more specifically, the more intrinsically motivated clients are, the less support they require (Mohr, Cuijpers, and Lehman 2011). In this context, the self‐determination theory (Ryan and Deci 2000) differentiates between intrinsic motivation, referring to doing something because it is inherently interesting, and extrinsic motivation, which refers to doing something because it leads to an external outcome. Clinically, individuals experiencing anxiety related difficulties may have higher intrinsic motivation (Winch, Moberly, and Dickson 2015) than individuals experiencing higher levels of depressive symptoms given that lower motivation and a need for extrinsic motivation (e.g., the support of others) is a clinical feature often associated with this group (Ling et al. 2016). Human support as part of a DMHI may provide a therapeutic alliance that increases extrinsic motivation, explaining why this group might benefit more from the human guidance component. This hypothesis will be important to test in future studies, particularly given the well‐established overlap in anxious and depressive symptom presentation in many individuals.
It is important to note that the majority of guided interventions included in this study were provided by graduate psychology students instead of trained clinicians. Although previous reviews (Leung et al. 2022; Werntz et al. 2023) have reported no significant differences for clinician versus non‐clinician guidance on DMHIs, there are important limitations that need to be considered. Firstly, the authors of previous reviews have highlighted the lack of detail available regarding the level of training or background of the individuals' providing support, limiting their ability to draw conclusions about the actual role of training of support providers on the efficacy of human support for DMHIs. Moreover, these reviews were not limited to college student samples; it is likely that the benefits of human guidance may well vary in terms of sample characteristics and outcome. We speculate that for the studies included in this review, which focused specifically on university students with mental health difficulties, engaging non‐clinicians in digital interventions may have represented a risk for the quality of support provided and the effectiveness of digital interventions. Again, future studies will benefit from an examination of the influence of clinically versus non‐clinically trained guidance in digital mental health interventions for university students with mental health difficulties. It is also important to note that our results might not guarantee maintenance of treatment gains. Therefore, future research should address this issue in order to guarantee the value of these DMHIs as an alternative to traditional face to face interventions (perhaps for students presenting with mild symptom severity), or for students who are either waiting to start 1:1 intervention or who have completed a brief 1:1 psychological intervention and are seeking to sustain their recovery.
4.3. Type of Psychological Interventions
Unsurprisingly, CBT‐based interventions were the most widely reported (similar to the literature on traditional 1:1 psychological interventions). CBT‐based interventions also appeared to be the most effective for reducing severity of symptoms of depression and anxiety when compared to other psychological therapies such as mindfulness. This evidence is in line with an umbrella review that synthesised evidence on digital health interventions targeting university students, which indicated that computer‐based CBT was one of the factors associated with effectiveness (Harith et al. 2022). CBT is a widely used intervention modality that aims to identify maladaptive patterns of thinking, emotional responses, or behaviour and replace these with more adaptive responses (Lehtimaki et al. 2021). Several reviews have identified that most digital interventions focus on evaluating CBT (Lattie et al. 2019; Lattie, Stiles‐Shields, and Graham 2022; Lehtimaki et al. 2021), while other interventions such as mindfulness, acceptance and commitment therapy (ACT), or interpersonal therapy remain somewhat under‐evaluated. In line with these reviews, further studies of other digital psychological interventions are needed to confirm whether CBT‐based interventions are in fact more effective than these other modalities.
4.4. Limitations
Our work has some limitations. First of all, we note the heterogeneity in digital interventions including length, intervention type, psychological treatment, and differences in the measurements of outcomes. Our search strategy was not limited to RCTs and the inclusion of multiple trial designs is likely to have led to higher heterogeneity of the data included. However, we performed sub‐groups analyses to examine the sources of heterogeneity. Secondly, the majority of studies included in this review were based on CBT (53%), which may have impacted the favourable effects of this treatment in comparison with other psychological treatments, as these appeared to be under‐represented. Thus, the results of this review should be interpreted with caution. Finally, for the meta‐analysis, we could not extract data from 13 studies, due to a lack of available outcome data, which made the pool of data of included studies smaller.
Overall, the existing studies included in this review focused only on mental health symptom severity. It is not clear how long participants had been struggling with these mental health difficulties and whether students had entered university with these symptoms or developed them during college. This lack of evidence concerning the longevity of mental health symptoms among college students is a notable gap in current datasets. Similarly, symptom severity is not the same as a clinically confirmed diagnosis, which typically was not reported in these studies, preventing us from drawing specific conclusions about illness subtypes.
4.5. Conclusions
Digital mental health interventions have the potential to improve the mental health of university students that present with mental health difficulties. To date, the majority of research on DMHIs has focused on non‐clinical populations rather than on clinical interventions that can be integrated with the counselling services in third‐level institutions. This review demonstrates that DMHIs are an effective approach to improve the mental health of university students with mental health difficulties. The findings suggests that while human guidance may be beneficial when targeting depressive symptom severity, fully automated interventions may be sufficient to achieve a reduction in symptom severity. These results are encouraging, as designing interventions that require minimal clinical guidance or support can increase the accessibility and cost efficiency of digital interventions for students experiencing anxiety. Moreover, this review further supports the integration of guidance in digital interventions aimed at improving depression.
Conflicts of Interest
The authors declare no conflicts of interest.
Supporting information
Data S1. Supporting Information.
Acknowledgements
The authors would like to acknowledge the funders which supported this work through the Atlantic Futures project. Atlantic Futures is a €4 million 4‐year cross‐border research project funded by The North–South Research Programme (422560). The North–South Research Programme is a collaborative scheme funded through the Government's Shared Island Fund. It is administered by the Higher Education Authority (HEA) on behalf of the Department of Further and Higher Education, Research, Innovation and Science. The authors would also like to acknowledge Prof Siobhan O'Neill and Jamie McNulty as part of this research project.
Funding: This work was supported by Atlantic Futures North South Research Program, 422560.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Akram, A. , and Arshad T.. 2022. “Alexithymia Reduction Treatment: A Pilot Quasi‐Experimental Study for Remediation of Alexithymia and Its Consequent Effects on the General Mental Health of University Students.” Counselling and Psychotherapy Research 22, no. 4: 902–912. 10.1002/capr.12571. [DOI] [Google Scholar]
- Andersson, G. , and Titov N.. 2014. “Advantages and Limitations of Internet‐Based Interventions for Common Mental Disorders.” World Psychiatry 13, no. 1: 4–11. 10.1002/wps.20083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardito, R. B. , and Rabellino D.. 2011. “Therapeutic Alliance and Outcome of Psychotherapy: Historical Excursus, Measurements, and Prospects for Research.” Frontiers in Psychology 2: 270. 10.3389/fpsyg.2011.00270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attridge, M. D. , Morfitt R. C., Roseborough D. J., and Jones E. R.. 2020. “Internet‐Based Cognitive‐Behavioral Therapy for College Students With Anxiety, Depression, Social Anxiety, or Insomnia: Four Single‐Group Longitudinal Studies of Archival Commercial Data and Replication of Employee User Study.” JMIR Formative Research 4, no. 7: e17712. 10.2196/17712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach, R. P. , Mortier P., Bruffaerts R., et al. 2018. “WHO World Mental Health Surveys International College Student Project: Prevalence and Distribution of Mental Disorders.” Journal of Abnormal Psychology 127, no. 7: 623–638. 10.1037/abn0000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balcombe, L. , and De Leo D.. 2022. “Evaluation of the Use of Digital Mental Health Platforms and Interventions: Scoping Review.” International Journal of Environmental Research and Public Health 20, no. 1: 362. 10.3390/ijerph20010362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bautista, C. L. , Ralston A. L., Brock R. L., and Hope D. A.. 2022. “Peer Coach Support in Internet‐Based Cognitive Behavioral Therapy for College Students With Social Anxiety Disorder: Efficacy and Acceptability.” Cogent Psychology 9, no. 1: 2040160. 10.1080/23311908.2022.2040160. [DOI] [Google Scholar]
- Beck, A. T. , Ward C., and Mendelson M.. 1961. “Beck Depression Inventory (BDI).” Archives of General Psychiatry 4: 561–571. [DOI] [PubMed] [Google Scholar]
- Beck, A. T. , Epstein N., Brown G., and Steer R. A.. 1988. “An Inventory for Measuring Clinical Anxiety: Psychometric Properties.” Journal of Consulting and Clinical Psychology 56: 893–897. [DOI] [PubMed] [Google Scholar]
- Beck, A. , Steer R., and Brown G.. 1996. BDI‐II, Beck Depression Inventory: Manual. Psychological Corporation. [Google Scholar]
- Bell, I. H. , Nicholas J., Broomhall A., et al. 2023. “The Impact of COVID‐19 on Youth Mental Health: A Mixed Methods Survey.” Psychiatry Research 321: 115082. 10.1016/j.psychres.2023.115082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein, M. , Hedges L., Higgins J., and Rothstein H.. 2013. Comprehensive Meta‐Analysis Version 3. Biostat. [Google Scholar]
- Borenstein, M. , Hedges L. V., Higgins J. P. T., and Rothstein H. R.. 2009. Introduction to Meta‐Analysis. John Wiley & Sons. [Google Scholar]
- Borghouts, J. , Eikey E., Mark G., et al. 2021. “Barriers to and Facilitators of User Engagement With Digital Mental Health Interventions: Systematic Review.” Journal of Medical Internet Research 23, no. 3: e24387. 10.2196/24387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broglia, E. , Millings A., and Barkham M.. 2019. “Counseling With Guided Use of a Mobile Well‐Being App for Students Experiencing Anxiety or Depression: Clinical Outcomes of a Feasibility Trial Embedded in a Student Counseling Service.” JMIR mHealth and uHealth 7, no. 8: e14318. 10.2196/14318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruhns, A. , Lüdtke T., Moritz S., and Bücker L.. 2021. “A Mobile‐Based Intervention to Increase Self‐Esteem in Students With Depressive Symptoms: Randomized Controlled Trial.” JMIR mHealth and uHealth 9, no. 7: e26498. 10.2196/26498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, F. , Blank L., Cantrell A., et al. 2022. “Factors That Influence Mental Health of University and College Students in the UK: A Systematic Review.” BMC Public Health 22: 1778. 10.1186/s12889-022-13943-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colizzi, M. , Lasalvia A., and Ruggeri M.. 2020. “Prevention and Early Intervention in Youth Mental Health: Is It Time for a Multidisciplinary and Trans‐Diagnostic Model for Care?” International Journal of Mental Health Systems 14: 23. 10.1186/s13033-020-00356-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conley, C. S. , Durlak J. A., Shapiro J. B., Kirsch A. A., and Zahniser E.. 2016. “A Meta‐Analysis of the Impact of Universal and Indicated Preventative Technology‐Delivered Interventions for Higher Education Students.” Prevention Science: the Official Journal of the Society for Prevention Research 17, no. 6: 659–678. 10.1007/s11121-016-0662-3. [DOI] [PubMed] [Google Scholar]
- Cook, L. , Mostazir M., and Watkins E.. 2019. “Reducing Stress and Preventing Depression (RESPOND): Randomized Controlled Trial of Web‐Based Rumination‐Focused Cognitive Behavioral Therapy for High‐Ruminating University Students.” Journal of Medical Internet Research 21, no. 5: e11349. 10.2196/11349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordero, C. P. , and Dans A. L.. 2021. “Key Concepts in Clinical Epidemiology: Detecting and Dealing With Heterogeneity in Meta‐Analyses.” Journal of Clinical Epidemiology 130: 149–151. 10.1016/j.jclinepi.2020.09.045. [DOI] [PubMed] [Google Scholar]
- Cuijpers, P. , Donker T., van Straten A., Li J., and Andersson G.. 2010. “Is Guided Self‐Help as Effective as Face‐To‐Face Psychotherapy for Depression and Anxiety Disorders? A Systematic Review and Meta‐Analysis of Comparative Outcome Studies.” Psychological Medicine 40, no. 12: 1943–1957. 10.1017/S0033291710000772. [DOI] [PubMed] [Google Scholar]
- D'Adamo, L. , Paraboschi L., Grammer A. C., et al. 2023. “Reach and Uptake of Digital Mental Health Interventions Based on Cognitive‐Behavioral Therapy for College Students: A Systematic Review.” Journal of Behavioral and Cognitive Therapy 33, no. 2: 97–117. 10.1016/j.jbct.2023.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dear, B. F. , Johnson B., Singh A., et al. 2019. “Examining an Internet‐Delivered Intervention for Anxiety and Depression When Delivered as a Part of Routine Care for University Students: A Phase IV Trial.” Journal of Affective Disorders 256: 567–577. 10.1016/j.jad.2019.06.044. [DOI] [PubMed] [Google Scholar]
- Duffy, A. , Keown‐Stoneman C., Goodday S., et al. 2020. “Predictors of Mental Health and Academic Outcomes in First‐Year University Students: Identifying Prevention and Early‐Intervention Targets.” BJPsych Open 6, no. 3: e46. 10.1192/bjo.2020.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy, A. , Saunders K. E., Malhi G. S., et al. 2019. “Mental Health Care for University Students: A Way Forward?” Lancet Psychiatry 6, no. 11: 885–887. 10.1016/S2215-0366(19)30275-5. [DOI] [PubMed] [Google Scholar]
- Dumarkaite, A. , Truskauskaite‐Kuneviciene I., Andersson G., and Kazlauskas E.. 2022. “The Effects of Online Mindfulness‐Based Intervention on Posttraumatic Stress Disorder and Complex Posttraumatic Stress Disorder Symptoms: A Randomized Controlled Trial With 3‐Month Follow‐Up.” Frontiers in Psychiatry 13: 799259. 10.3389/fpsyt.2022.799259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval, S. , and Tweedie R.. 2000. “Trim and Fill: A Simple Funnel‐Plot‐Based Method of Testing and Adjusting for Publication Bias in Meta‐Analysis.” Biometrics 56, no. 2: 455–463. 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Ebert, D. D. , Buntrock C., Lehr D., et al. 2018. “Effectiveness of Web‐ and Mobile‐Based Treatment of Subthreshold Depression With Adherence‐Focused Guidance: A Single‐Blind Randomized Controlled Trial.” Behavior Therapy 49, no. 1: 71–83. 10.1016/j.beth.2017.05.004. [DOI] [PubMed] [Google Scholar]
- Erbe, D. , Eichert H. C., Riper H., and Ebert D. D.. 2017. “Blending Face‐To‐Face and Internet‐Based Interventions for the Treatment of Mental Disorders in Adults: Systematic Review.” Journal of Medical Internet Research 19, no. 9: e306. 10.2196/jmir.6588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari, M. , Allan S., Arnold C., et al. 2022. “Digital Interventions for Psychological Well‐Being in University Students: Systematic Review and Meta‐Analysis.” Journal of Medical Internet Research 24, no. 9: e39686. 10.2196/39686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming, T. , Bavin L., Lucassen M., Stasiak K., Hopkins S., and Merry S.. 2018. “Beyond the Trial: Systematic Review of Real‐World Uptake and Engagement With Digital Self‐Help Interventions for Depression, Low Mood, or Anxiety.” Journal of Medical Internet Research 20, no. 6: e199. 10.2196/jmir.9275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes, A. , Keleher M. R., Venditto M., and DiBiasi F.. 2023. “Assessing Patient Adherence to and Engagement With Digital Interventions for Depression in Clinical Trials: Systematic Literature Review.” Journal of Medical Internet Research 25: e43727. 10.2196/43727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan, D. Z. , McGillivray L., Han J., Christensen H., and Torok M.. 2021. “Effect of Engagement With Digital Interventions on Mental Health Outcomes: A Systematic Review and Meta‐Analysis.” Frontiers in Digital Health 3: 764079. 10.3389/fdgth.2021.764079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin, R. D. , Weinberger A. H., Kim J. H., Wu M., and Galea S.. 2020. “Trends in Anxiety Among Adults in the United States, 2008–2018: Rapid Increases Among Young Adults.” Journal of Psychiatric Research 130: 441–446. 10.1016/j.jpsychires.2020.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin, R. D. , Dierker L. C., Wu M., Galea S., Hoven C. W., and Weinberger A. H.. 2022. “Trends in US Depression Prevalence From 2015 to 2020: The Widening Treatment Gap.” American Journal of Preventive Medicine 63, no. 5: 726–733. 10.1016/j.amepre.2022.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ha, S. W. , and Kim J.. 2020. “Designing a Scalable, Accessible, and Effective Mobile App Based Solution for Common Mental Health Problems.” International Journal of Human‐Computer Interaction 36, no. 14: 1354–1367. 10.1080/10447318.2020.1750792. [DOI] [Google Scholar]
- Haeger, J. A. , Davis C. H., and Levin M. E.. 2022. “Utilizing ACT Daily as a Self‐Guided App for Clients Waiting for Services at a College Counseling Center: A Pilot Study.” Journal of American College Health 70, no. 3: 742–749. 10.1080/07448481.2020.1763366. [DOI] [PubMed] [Google Scholar]
- Hallett, C. 2012. “Is There Time Enough? Ethical Dilemmas Inherent in Offering Time Limited Work in the University.” British Journal of Psychotherapy 28: 249–263. 10.1111/j.1752-0118.2012.01285.x. [DOI] [Google Scholar]
- Harith, S. , Backhaus I., Mohbin N., Ngo H. T., and Khoo S.. 2022. “Effectiveness of Digital Mental Health Interventions for University Students: An Umbrella Review.” PeerJ 10: e13111. 10.7717/peerj.13111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrer, M. , Adam S. H., Fleischmann R. J., et al. 2018. “Effectiveness of an Internet‐ and App‐Based Intervention for College Students With Elevated Stress: Randomized Controlled Trial.” Journal of Medical Internet Research 20, no. 4: e136. 10.2196/jmir.9293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison, G. , and Gordon E.. 2021. “Counsellors' Experiences of Providing Counselling to Students in University‐Level Institutions in Ireland: An Evolving Phenomenon.” Counselling and Psychotherapy Research 21, no. 4: 805–815. 10.1002/capr.12441. [DOI] [Google Scholar]
- He, Y. , Yang L., Zhu X., et al. 2022. “Mental Health Chatbot for Young Adults With Depressive Symptoms During the COVID‐19 Pandemic: Single‐Blind, Three‐Arm Randomized Controlled Trial.” Journal of Medical Internet Research 24, no. 11: e40719. 10.2196/40719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemmings, N. R. , Kawadler J. M., Whatmough R., et al. 2021. “Development and Feasibility of a Digital Acceptance and Commitment Therapy–Based Intervention for Generalized Anxiety Disorder: Pilot Acceptability Study.” JMIR Formative Research 5, no. 2: e21737. 10.2196/21737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennemann, S. , Böhme K., Kleinstäuber M., et al. 2022. “Is Therapist Support Needed? Comparing Therapist‐ and Self‐Guided Internet‐Based CBT for Somatic Symptom Distress (iSOMA) in Emerging Adults.” Behavior Therapy 53, no. 6: 1205–1218. 10.1016/j.beth.2022.06.006. [DOI] [PubMed] [Google Scholar]
- Hides, L. , Dingle G., Quinn C., et al. 2019. “Efficacy and Outcomes of a Music‐Based Emotion Regulation Mobile App in Distressed Young People: Randomized Controlled Trial.” JMIR mHealth and uHealth 7, no. 1: e11482. 10.2196/11482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P. , Altman D. G., Gøtzsche P. C., et al. 2011. “The Cochrane Collaboration's Tool for Assessing Risk of Bias in Randomised Trials.” BMJ 343: d5928. 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P. , Thompson S. G., Deeks J. J., and Altman D. G.. 2003. “Measuring Inconsistency in Meta‐Analyses.” BMJ (Clinical Research Edition) 327, no. 7414: 557–560. 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karyotaki, E. , Klein A. M., Ciharova M., et al. 2022. “Guided Internet‐Based Transdiagnostic Individually Tailored Cognitive Behavioral Therapy for Symptoms of Depression and/or Anxiety in College Students: A Randomized Controlled Trial.” Behaviour Research and Therapy 150: 104028. 10.1016/j.brat.2021.104028. [DOI] [PubMed] [Google Scholar]
- Kessler, R. C. , Amminger G. P., Aguilar‐Gaxiola S., Alonso J., Lee S., and Ustün T. B.. 2007. “Age of Onset of Mental Disorders: A Review of Recent Literature.” Current Opinion in Psychiatry 20, no. 4: 359–364. 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C. , Berglund P., Demler O., Jin R., Merikangas K. R., and Walters E. E.. 2005. “Lifetime Prevalence and Age‐Of‐Onset Distributions of DSM‐IV Disorders in the National Comorbidity Survey Replication.” Archives of General Psychiatry 62, no. 6: 593–602. [DOI] [PubMed] [Google Scholar]
- Kim, S. , and Lee K.. 2023. “Development and Evaluation of an Online Mental Health Program for Traumatized Female College Students: A Randomized Controlled Trial.” Archives of Psychiatric Nursing 43: 118–126. 10.1016/j.apnu.2023.01.003. [DOI] [PubMed] [Google Scholar]
- King, N. , Pickett W., McNevin S. H., et al. 2021. “Mental Health Need of Students at Entry to University: Baseline Findings From the U‐Flourish Student Well‐Being and Academic Success Study.” Early Intervention in Psychiatry 15, no. 2: 286–295. 10.1111/eip.12939. [DOI] [PubMed] [Google Scholar]
- Kingston, J. , Becker L., Woeginger J., and Ellett L.. 2020. “A Randomised Trial Comparing a Brief Online Delivery of Mindfulness‐Plus‐Values Versus Values Only for Symptoms of Depression: Does Baseline Severity Matter?” Journal of Affective Disorders 276: 936–944. 10.1016/j.jad.2020.07.087. [DOI] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer R. L., and Williams J. B.. 2001. “The Phq‐9.” Journal of General Internal Medicine 16: 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer R. L., deGruy F. V., and Swindle R.. 1998. 15‐Item Patient Health Questionnaire (PHQ‐15) [Database Record]. APA PsycTests.
- Kroenke, K. , Spitzer R. L., Williams J. B. W., and Löwe B.. 2009. Patient Health Questionnaire‐4 (PHQ‐4) [Database Record]. APA PsycTests.
- Lattie, E. G. , Stiles‐Shields C., and Graham A. K.. 2022. “An Overview of and Recommendations for More Accessible Digital Mental Health Services.” Nature Reviews Psychology 1, no. 2: 87–100. 10.1038/s44159-021-00003-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lattie, E. G. , Adkins E. C., Winquist N., Stiles‐Shields C., Wafford Q. E., and Graham A. K.. 2019. “Digital Mental Health Interventions for Depression, Anxiety, and Enhancement of Psychological Well‐Being Among College Students: Systematic Review.” Journal of Medical Internet Research 21, no. 7: e12869. 10.2196/12869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehtimaki, S. , Martic J., Wahl B., Foster K. T., and Schwalbe N.. 2021. “Evidence on Digital Mental Health Interventions for Adolescents and Young People: Systematic Overview.” JMIR Mental Health 8, no. 4: e25847. 10.2196/25847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung, C. , Pei J., Hudec K., Shams F., Munthali R., and Vigo D.. 2022. “The Effects of Non‐Clinician Guidance on Effectiveness and Process Outcomes in Digital Mental Health Interventions: Systematic Review and Meta‐Analysis.” Journal of Medical Internet Research 24, no. 6: e36004. 10.2196/36004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin, M. E. , Hicks E. T., and Krafft J.. 2022. “Pilot Evaluation of the Stop, Breathe & Think Mindfulness App for Student Clients on a College Counselling Centre Waitlist.” Journal of American College Health 70, no. 1: 165–173. 10.1080/07448481.2020.1728281. [DOI] [PubMed] [Google Scholar]
- Linardon, J. , and Fuller‐Tyszkiewicz M.. 2020. “Attrition and Adherence in Smartphone‐Delivered Interventions for Mental Health Problems: A Systematic and Meta‐Analytic Review.” Journal of Consulting and Clinical Psychology 88, no. 1: 1–13. 10.1037/ccp0000459. [DOI] [PubMed] [Google Scholar]
- Ling, Y. , He Y., Wei Y., Cen W., Zhou Q., and Zhong M.. 2016. “Intrinsic and Extrinsic Goals as Moderators of Stress and Depressive Symptoms in Chinese Undergraduate Students: A Multi‐Wave Longitudinal Study.” BMC Psychiatry 16: 1–8. 10.1186/s12888-016-0842-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipson, S. K. , Lattie E. G., and Eisenberg D.. 2019. “Increased Rates of Mental Health Service Utilization by U.S. College Students: 10‐Year Population‐Level Trends (2007‐2017).” Psychiatric Services (Washington, DC) 70, no. 1: 60–63. 10.1176/appi.ps.201800332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond, S. H. , and Lovibond P. F.. 1995. Depression Anxiety Stress Scales (DASS—21, DASS—42) [Database record]. APA PsycTests.
- McCall, H. C. , Richardson C. G., Helgadottir F. D., and Chen F. S.. 2018. “Evaluating a Web‐Based Social Anxiety Intervention Among University Students: Randomized Controlled Trial.” Journal of Medical Internet Research 20, no. 3: e91. 10.2196/jmir.8630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGorry, P. D. , Mei C., Dalal N., et al. 2024. “The Lancet Psychiatry Commission on Youth Mental Health.” Lancet Psychiatry 11, no. 9: 731–774. [DOI] [PubMed] [Google Scholar]
- McKenzie, J. E. , Brennan S. E., Ryan R. E., Thomson H. J., Johnston R. V., and Thomas J.. 2019. “Defining the Criteria for Including Studies and How They Will Be Grouped for the Synthesis.” Cochrane Handbook for Systematic Reviews of Interventions, edited by Higgins J. P., Thomas J., Chandler J., 33–65. Wiley. 10.1002/9781119536604.ch3. [DOI] [Google Scholar]
- Melcher, J. , Camacho E., Lagan S., and Torous J.. 2022. “College Student Engagement With Mental Health Apps: Analysis of Barriers to Sustained Use.” Journal of American College Health 70, no. 6: 1819–1825. 10.1080/07448481.2020.1825225. [DOI] [PubMed] [Google Scholar]
- Mohr, D. C. , Cuijpers P., and Lehman K.. 2011. “Supportive Accountability: A Model for Providing Human Support to Enhance Adherence to eHealth Interventions.” Journal of Medical Internet Research 13, no. 1: e30. 10.2196/jmir.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montagni, I. , Tzourio C., Cousin T., Sagara J. A., Bada‐Alonzi J., and Horgan A.. 2020. “Mental Health‐Related Digital Use by University Students: A Systematic Review.” Telemedicine Journal and e‐Health: The Official Journal of the American Telemedicine Association 26, no. 2: 131–146. 10.1089/tmj.2018.0316. [DOI] [PubMed] [Google Scholar]
- Moshe, I. , Terhorst Y., Philippi P., et al. 2021. “Digital Interventions for the Treatment of Depression: A Meta‐Analytic Review.” Psychological Bulletin 147, no. 8: 749–786. 10.1037/bul0000334. [DOI] [PubMed] [Google Scholar]
- Musiat, P. , Johnson C., Atkinson M., Wilksch S., and Wade T.. 2022. “Impact of Guidance on Intervention Adherence in Computerised Interventions for Mental Health Problems: A Meta‐Analysis.” Psychological Medicine 52, no. 2: 229–240. 10.1017/S0033291721004621. [DOI] [PubMed] [Google Scholar]
- Newman, M. G. , Kanuri N., Rackoff G. N., Jacobson N. C., Bell M. J., and Taylor C. B.. 2021. “A Randomized Controlled Feasibility Trial of Internet‐Delivered Guided Self‐Help for Generalized Anxiety Disorder (GAD) Among University Students in India.” Psychotherapy (Chicago, IL) 58, no. 4: 591–601. 10.1037/pst0000383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Bryan, E. M. , McLeish A. C., Norr A. M., et al. 2021. “A Randomized Controlled Trial Evaluating the Efficacy of a Brief Computerized Anxiety Sensitivity Reduction Intervention for Health Anxiety.” Journal of Anxiety Disorders 82: 102425. 10.1016/j.janxdis.2021.102425. [DOI] [PubMed] [Google Scholar]
- OECD Indicators . 2022. “Education at a Glance, 2022, Editions OECD 2021.” https://www.oecd.org/en/publications/education‐at‐a‐glance‐2022_3197152b‐en.html.
- Osborn, T. G. , Li S., Saunders R., and Fonagy P.. 2022. “University Students' Use of Mental Health Services: A Systematic Review and Meta‐Analysis.” International Journal of Mental Health Systems 16, no. 1: 57. 10.1186/s13033-022-00569-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oswalt, S. B. , Lederer A. M., Chestnut‐Steich K., Day C., Halbritter A., and Ortiz D.. 2020. “Trends in College Students' Mental Health Diagnoses and Utilization of Services, 2009‐2015.” Journal of American College Health 68, no. 1: 41–51. 10.1080/07448481.2018.1515748. [DOI] [PubMed] [Google Scholar]
- Page, M. J. , McKenzie J. E., Bossuyt P. M., et al. 2021. “The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews.” Systematic Reviews 10: 89. 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palacios, J. E. , Richards D., Palmer R., et al. 2018. “Supported Internet‐Delivered Cognitive Behavioral Therapy Programs for Depression, Anxiety, and Stress in University Students: Open, Non‐Randomised Trial of Acceptability, Effectiveness, and Satisfaction.” JMIR Mental Health 5, no. 4: e11467. 10.2196/11467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papini, S. , Jacquart J., Zaizar E. D., Telch M. J., and Smits J. A.. 2023. “Targeting Anxiety Sensitivity With Evidence‐Based Psychoeducation: A Randomized Waitlist‐Controlled Trial of a Brief Standalone Digital Intervention.” Cognitive and Behavioral Practice 30, no. 4: 678–691. 10.1016/j.cbpra.2022.04.001. [DOI] [Google Scholar]
- Pauley, D. , Cuijpers P., Papola D., Miguel C., and Karyotaki E.. 2023. “Two Decades of Digital Interventions for Anxiety Disorders: A Systematic Review and Meta‐Analysis of Treatment Effectiveness.” Psychological Medicine 53, no. 2: 567–579. 10.1017/S0033291721001999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philippe, T. J. , Sikder N., Jackson A., et al. 2022. “Digital Health Interventions for Delivery of Mental Health Care: Systematic and Comprehensive Meta‐Review.” JMIR Mental Health 9, no. 5: e35159. 10.2196/35159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pineda, B. S. , Mejia R., Qin Y., Martinez J., Delgadillo L. G., and Muñoz R. F.. 2023. “Updated Taxonomy of Digital Mental Health Interventions: A Conceptual Framework.” mHealth 9: 28. 10.21037/mhealth-23-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponzo, S. , Morelli D., Kawadler J. M., Hemmings N. R., Bird G., and Plans D.. 2020. “Efficacy of the Digital Therapeutic Mobile App BioBase to Reduce Stress and Improve Mental Well‐Being Among University Students: Randomized Controlled Trial.” JMIR mHealth and uHealth 8, no. 4: e17767. 10.2196/17767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rackoff, G. N. , Fitzsimmons‐Craft E. E., Taylor C. B., Eisenberg D., Wilfley D. E., and Newman M. G.. 2022. “A Randomized Controlled Trial of Internet‐Based Self‐Help for Stress During the COVID‐19 Pandemic.” Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine 71, no. 2: 157–163. 10.1016/j.jadohealth.2022.01.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff, L. S. 1977. “The CES‐D Scale a Self‐Report Depression Scale for Research in the General Population.” Applied Psychological Measurement 1: 385–401. [Google Scholar]
- Räsänen, P. , Muotka J., and Lappalainen R.. 2023. “Examining Coaches' Asynchronous Written Feedback in Two Blended ACT‐Based Interventions for Enhancing University students' Wellbeing and Reducing Psychological Distress: A Randomized Study.” Journal of Contextual Behavioral Science 29: 98–108. 10.1016/j.jcbs.2023.06.006. [DOI] [Google Scholar]
- Riboldi, I. , Cavaleri D., Calabrese A., et al. 2023. “Digital Mental Health Interventions for Anxiety and Depressive Symptoms in University Students During the COVID‐19 Pandemic: A Systematic Review of Randomized Controlled Trials.” Revista de Psiquiatria y Salud Mental 16: 47–58. 10.1016/j.rpsm.2022.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards, D. , and Richardson T.. 2012. “Computer‐Based Psychological Treatments for Depression: A Systematic Review and Meta‐Analysis.” Clinical Psychology Review 32, no. 4: 329–342. 10.1016/j.cpr.2012.02.004. [DOI] [PubMed] [Google Scholar]
- Ruehlman, L. , and Karoly P.. 2023. “A Pilot Test of Internet‐Delivered Brief Interactive Training Sessions for Depression: Evaluating Dropout, Uptake, Adherence, and Outcome.” Journal of American College Health 71, no. 7: 2131–2139. 10.1080/07448481.2021.1961781. [DOI] [PubMed] [Google Scholar]
- Ryan, R. M. , and Deci E. L.. 2000. “Intrinsic and Extrinsic Motivations: Classic Definitions and New Directions.” Contemporary Educational Psychology 25, no. 1: 54–67. 10.1006/ceps.1999.1020. [DOI] [PubMed] [Google Scholar]
- Salamanca‐Sanabria, A. , Richards D., Timulak L., et al. 2020. “A Culturally Adapted Cognitive Behavioral Internet‐Delivered Intervention for Depressive Symptoms: Randomized Controlled Trial.” JMIR Mental Health 7, no. 1: e13392. 10.2196/13392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schueller, S. M. , and Torous J.. 2020. “Scaling Evidence‐Based Treatments Through Digital Mental Health.” American Psychologist 75, no. 8: 1093–1104. 10.1037/amp0000654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short, N. A. , and Schmidt N. B.. 2020. “Developing and Testing a Novel, Computerized Insomnia and Anxiety Intervention to Reduce Safety Aids Among an At‐Risk Student Sample: A Randomized Controlled Trial.” Behavior Therapy 51, no. 1: 149–161. 10.1016/j.beth.2019.05.012. [DOI] [PubMed] [Google Scholar]
- Sit, H. F. , Hong I. W., Burchert S., et al. 2022. “A Feasibility Study of the WHO Digital Mental Health Intervention Step‐By‐Step to Address Depression Among Chinese Young Adults.” Frontiers in Psychiatry 12: 812667. 10.3389/fpsyt.2021.812667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Six, S. G. , Byrne K. A., Aly H., and Harris M. W.. 2022. “The Effect of Mental Health App Customization on Depressive Symptoms in College Students: Randomized Controlled Trial.” JMIR Mental Health 9, no. 8: e39516. 10.2196/39516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solmi, M. , Radua J., Olivola M., et al. 2022. “Age at Onset of Mental Disorders Worldwide: Large‐Scale Meta‐Analysis of 192 Epidemiological Studies.” Molecular Psychiatry 27, no. 1: 281–295. 10.1038/s41380-021-01161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer, R. L. , Kroenke K., Williams J. B. W., and Löwe B.. 2006. Generalized Anxiety Disorder 7 (GAD‐7) [Database Record]. APA PsycTests. [DOI] [PubMed]
- Stanic, J. , Barth J., Danon N., Bondolfi G., Jermann F., and Eicher M.. 2021. “Adherence to Standardized 8‐Week Mindfulness‐Based Interventions Among Women With Breast or Gynecological Cancer: A Scoping Review.” Journal of Psychosocial Oncology Research and Practice 3, no. 2: e048. 10.1097/OR9.0000000000000048. [DOI] [Google Scholar]
- Sterne, J. A. , Hernán M. A., Reeves B. C., et al. 2016. “ROBINS‐I: A Tool for Assessing Risk of Bias in Non‐Randomised Studies of Interventions.” BMJ 355: i4919. 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suffoletto, B. , Goldstein T., Gotkiewicz D., Gotkiewicz E., George B., and Brent D.. 2021. “Acceptability, Engagement, and Effects of a Mobile Digital Intervention to Support Mental Health for Young Adults Transitioning to College: Pilot Randomized Controlled Trial.” JMIR Formative Research 5, no. 10: e32271. 10.2196/32271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun, S. , Lin D., Goldberg S., et al. 2022. “A Mindfulness‐Based Mobile Health (mHealth) Intervention Among Psychologically Distressed University Students in Quarantine During the COVID‐19 Pandemic: A Randomized Controlled Trial.” Journal of Counseling Psychology 69, no. 2: 157–171. 10.1037/cou0000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, E. B. K. , Sagorac Gruichich T., Maronge J. M., et al. 2023. “Mobile Acceptance and Commitment Therapy With Distressed First‐Generation College Students: Microrandomized Trial.” JMIR Mental Health 10: e43065. 10.2196/43065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorley, C. 2017. Not by Degrees: Improving Student Mental Health in the UK's Universities. Institute for Public Policy Research [IPPR]. www.ippr.org/publications/not‐by‐degrees. [Google Scholar]
- Twenge, J. M. , Cooper A. B., Joiner T. E., Duffy M. E., and Binau S. G.. 2019. “Age, Period, and Cohort Trends in Mood Disorder Indicators and Suicide‐Related Outcomes in a Nationally Representative Dataset, 2005–2017.” Journal of Abnormal Psychology 128, no. 3: 185–199. 10.1037/abn0000410. [DOI] [PubMed] [Google Scholar]
- Valentine, L. , McEnery C., Bell I., et al. 2020. “Blended Digital and Face‐To‐Face Care for First‐Episode Psychosis Treatment in Young People: Qualitative Study.” JMIR Mental Health 7, no. 7: e18990. 10.2196/18990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van't Hof, E. , Cuijpers P., and Stein D. J.. 2009. “Self‐Help and Internet‐Guided Interventions in Depression and Anxiety Disorders: A Systematic Review of Meta‐Analyses.” CNS Spectrums 14, no. 2 Suppl 3: 34–40. 10.1017/s1092852900027279. [DOI] [PubMed] [Google Scholar]
- Veritas Health Innovation . 2020. Covidence Systematic Review Software. http://www.covidence.org.
- Walsh, S. , Cullinan J., Flannery D., and Kennelly B.. 2022. “Modelling Student Preferences for the Design of Campus Counselling Services.” Studies in Higher Education 47, no. 2: 305–317. 10.1080/03075079.2020.1744124. [DOI] [Google Scholar]
- Werntz, A. , Amado S., Jasman M., Ervin A., and Rhodes J. E.. 2023. “Providing Human Support for the Use of Digital Mental Health Interventions: Systematic Meta‐Review.” Journal of Medical Internet Research 25: e42864. 10.2196/42864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiens, K. , Bhattarai A., Pedram P., et al. 2020. “A Growing Need for Youth Mental Health Services in Canada: Examining Trends in Youth Mental Health From 2011 to 2018.” Epidemiology and Psychiatric Sciences 29: e115. 10.1017/S2045796020000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winch, A. , Moberly N. J., and Dickson J. M.. 2015. “Unique Associations Between Anxiety, Depression and Motives for Approach and Avoidance Goal Pursuit.” Cognition & Emotion 29, no. 7: 1295–1305. 10.1080/02699931.2014.976544. [DOI] [PubMed] [Google Scholar]
- Winter, N. , Russell L., Ugalde A., White V., and Livingston P.. 2022. “Engagement Strategies to Improve Adherence and Retention in Web‐Based Mindfulness Programs: Systematic Review.” Journal of Medical Internet Research 24, no. 1: e30026. 10.2196/30026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worsley, J. D. , Pennington A., and Corcoran R.. 2022. “Supporting Mental Health and Wellbeing of University and College Students: A Systematic Review of Review‐Level Evidence of Interventions.” PLoS One 17, no. 7: e0266725. 10.1371/journal.pone.0266725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, C. , Wampold B. E., Ren Z., Zhang L., and Jiang G.. 2022. “The Efficacy and Optimal Matching of an Internet‐Based Acceptance and Commitment Therapy Intervention for Depressive Symptoms Among University Students: A Randomized Controlled Trial in China.” Journal of Clinical Psychology 78, no. 7: 1354–1375. 10.1002/jclp.233. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting Information.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


